Abstract
This study aims to investigate the patterns and predictors of suicidal ideation (SI) trajectories among college students during extended lockdowns in China. A three-wave survey was conducted during the outbreak period, remission period, and prevention period of COVID-19. Distinct patterns of SI trajectories were established by grouping respondents based on temporal changes in SI. Multivariate logistic regressions were performed to examine predictors for delay-occurrence and persistent SI. From a total of 35,516 college students included in the study, rates of SI increased significantly from T1 to T2 (7.3% v. 9.4%) and from T2 to T3 (9.4% v. 12.6%). Five SI trajectories were observed: resilient (80.5% of the sample), recovery (3.6%), relapsing/remitting (4.8%), persistent dysfunction (2.3%) and delayed dysfunction (8.7%). Further, junior-year undergraduates, postgraduates, only-child families, mental health history, confirmed cases in the community of residence, depressive symptoms, and negative coping strategies were significant predictors of distinct SI trajectories, whereas greater social support, more positive coping strategies, and better family functioning were associated with a lower probability of developing delayed or persistent dysfunction during the lockdown period. These findings suggest that continuous preventive and intervening measures for college students during COVID-19 lockdowns are of global importance, particularly among vulnerable groups who experience the most distress.
Keywords: Suicidal ideation, Lockdown, College students, Longitudinal survey, COVID-19
1. Introduction
The outbreak of novel coronavirus disease 2019 (COVID-19) has become an unprecedented threat to public mental health (Holmes et al., 2020). Early evidence highlights the high prevalence of mental health problems among the general public during the COVID-19 pandemic. A meta-analysis study showed that the pooled prevalence of depression and anxiety between 1 November 2019 to 25 May 2020 were 33%, and 28%, respectively (Luo et al., 2020). In China, 18.8%, 13.3%, 7.2%, and 67.9% of the public suffered from depression, anxiety, clinical insomnia, and moderate-to-high levels of perceived stress, respectively, during the COVID-19 outbreak (Ren et al., 2020). To control the spread of the pandemic, the Chinese government announced a nationwide lockdown to drastically reduce human contact. However, the potential consequences of quarantine, self-isolation and physical distancing may increase the risk of suicide (Gunnell et al., 2020). For example, a national survey in China reported that during the COVID-19 outbreak, the prevalence of SI among the general population reached 16.4% during extended lockdown (Shi et al., 2021). In addition, previous evidence has highlighted an increase in the suicide rate during lockdown in Hong Kong in response to the severe acute respiratory syndrome (SARS) epidemic that occurred in 2003 (Chan et al., 2006). Therefore, the profound effect of COVID-19 lockdown on the population, especially on groups that are at an increased risk of suicide, requires serious attention.
Compared with other populations, measures that led to strict lockdown, school closures, and social isolation from peers placed greater challenges on the mental health of college students (Lee, 2020). It is also noteworthy that university students experienced higher levels of psychological distress during quarantine (Marelli et al., 2021). Over half of all college students might be at high or moderate risk of suicide during periods of quarantine (López Steinmetz et al., 2021); it is therefore necessary to monitor changes in SI among college students during periods of COVID-19 lockdown.
Longitudinal research studies on suicide during periods of lockdown in response to the pandemic produced inconclusive findings. Several short follow-up studies found no significant changes in the risk of suicide or even decreased suicide risk during the first wave of infection (Isumi et al., 2020; López Steinmetz et al., 2021), whereas other study reported increase in the prevalence of SI during the early stage of pandemic (O'Connor et al., 2020). A longitudinal study that explored the trajectory of SI among 811 adults during two separate lockdowns in Greece found that the SI rate (4.32%) during the second lockdown (from November 22 to December 21, 2020) did not differ significantly, remaining close to 4.81% during the first lockdown period (April 7 to May 3, 2020) in response to the COVID-19 pandemic. This was likely due to increased mobility and a 5-month period with no lockdown (Efstathiou et al., 2021). However, according to a 3-month follow-up study in the U.S. during the COVID-19 pandemic, the percentage of individuals experiencing SI was 1.8 times higher among those under a stay-at-home order compared to those who were not (Killgore et al., 2020). Therefore, extended periods of lockdown may increase the risk of SI (Reynolds et al., 2008). Nevertheless, few studies have explored the effects of extended lockdowns on SI among college students.
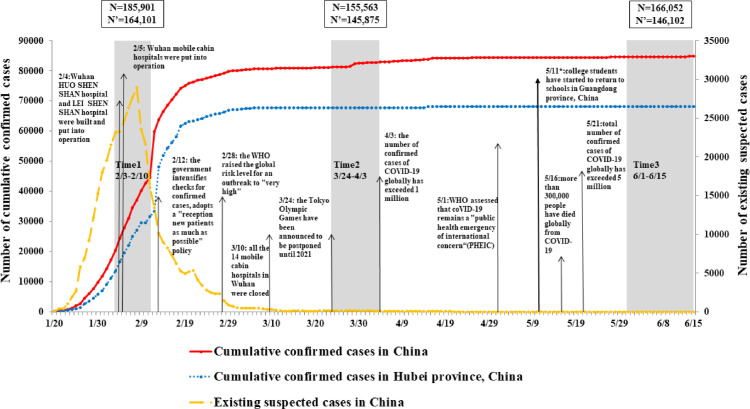
From February 2020 to June 2020, we conducted a three-wave survey among college/university students in Guangdong Province in China. During the initial outbreak phase from January to March 2020, which initially affected areas around Wuhan city, COVID-19 rapidly spread across the whole country. Due to rising concerns about the pandemic, the Chinese government announced a nationwide lockdown, during which the public were instructed to stay at home and restrict interpersonal contact. College students in China were impacted by campus closures, the introduction of online teaching, and a reduction in social activities. As a result of the various measures implemented by the Chinese government, COVID-19 was effectively contained, showing a consistent downtrend trend for newly confirmed cases in March 2020. From the beginning of May 2020, since the COVID-19 pandemic had been brought under nationwide control with the emergence of only localized and sporadic cases, the first batch of college students were allowed to return to school in China subject to strict guidance about movement outside of the campus perimeter (National Health Commission of People's Republic of China, 2020). The development trend of the COVID-19 pandemic in China is shown in Fig. 1 . To the best of our knowledge, few longitudinal studies have been carried out to examine the impact of extended lockdowns during different pandemic periods. Thus, this follow-up survey was an opportunity to explore changes in the SI rate during the COVID-19 lockdown, and to better understand the factors that affected the occurrence of SI in China.
Fig. 1.
The development trend of COVID-19 in China from January 20, 2020 to June 15, 2020.
Accordingly, the current study aimed to elucidate changes in the prevalence of SI among college students across three periods of the COVID-19 pandemic, and to explore different trajectories of SI as well as its influencing factors during the period of extended lockdown in China.
2. Methods
2.1. Participants and procedure
Based on the geographical distribution and types of colleges/universities, 22 colleges and universities in Guangdong Province were selected. A detailed geographical distribution of the colleges/universities is described in a previous study (Zhang et al., 2021). During the COVID-19 lockdown in China, we conducted a three-wave cross-sectional online survey during the outbreak period (Time1, T1: Feb 3 to 10, 2020), remission period (Time2, T2: March 24 to April 3, 2020), and normal prevention period (Time3, T3: June 1 to June 15, 2020) of COVID-19. A total of 164,101 (88.3% valid questionnaires), 148,343 (95.4% valid questionnaires), and 166,052 (88.0% valid questionnaires) respondents respectively took part in the three surveys. Among the 164,101 Chinese college students who completed the baseline survey, 68,685 (41.9%) students completed the second survey, and 35,516 (21.6%) completed all three surveys. Among 35,516 college students included in the final sample, 1767 (5.0%) respondents returned to school during the third survey. The detailed investigation process can be sourced by referring to a prior study (Wang et al., 2022a).
The Human Research Ethics Committee of South China Normal University has approved this study (SCNU-PSY-2020–01–001). All respondents provided electronic informed consent, and were informed of their right to withdraw from the research at any moment if they no longer wished to participate.
2.2. Measurements
2.2.1. Demographic information and pre-existing mental health conditions
Self-reported questions were designed to collect information relating to the respondents’ background, including their gender, education grade, place of residence, number of children in the family and history of mental illness.
2.2.2. COVID-19 pandemic-related factors
The extent of the respondents’ exposure to the COVID-19 pandemic was measured by reference to two items: (1) whether or not there were confirmed or suspected cases in the respondents’ community or village; (2) whether or not the respondents’ relatives or friends were infected with COVID-19.
2.2.3. Psychosocial factors
This study measured psychosocial factors including social support, coping strategies and family functioning. Given that these variables are relatively stable over a period of time, each factor was measured only once in our study. The Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess individual perceived social support from family, friends and others at T1 (Dahlem et al., 1991; Zimet et al., 1988). It consists of 12 items rated according to a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). In line with previous research, respondents were assigned to three groups (i.e., low, medium and high social support) in this study basing on the 27th and 73rd percentiles of the total score (Fan et al., 2015). Previous studies have shown that MSPSS had good reliability and construct validity in the Chinese population (Wang et al., 1999; Zhang et al., 2018). In the current sample, the Cronbach's α was 0.95.
The Simplified Coping Style Questionnaire (SCSQ) was used to measure college students’ coping strategies at T1. The 20-item scale comprises of two subscales: positive coping strategies (12 items) and negative coping strategies (8 items). Respondents rated their typical coping attitude towards distress according to a 4-point scale ranging from 0 (never or rarely) to 3 (most or all of the time). Coping strategies were recoded into three categories, with low and high categories defined by the 27th and 73rd percentile (Fan et al., 2015). Psychometric properties of the SCSQ have been described in the Chinese population (Jie, 1998; Xie, 1998). In our study, Cronbach's α was 0.90 for positive coping and 0.78 for negative coping.
Family functioning was measured at T2 using the Family APGAR Questionnaire designed by Smilkstein (Smilkstein, 1978; Smilkstein et al., 1982). The five-item scale aims to assess perceived family support based on five components: adaptation, partnership, growth, affection and resolve. Each item was scored using a three-point Likert scale ranging from 0 (never or rarely) to 2 (most or all of the time), and a total score of 7–10 indicates a highly functional family, 4–6 indicates a moderately dysfunctional family and 0–3 indicates a highly dysfunctional family. Its reliability and validity have been demonstrated (Dong et al., 2020; Man et al., 2017). The Cronbach's α was 0.90 in this study.
2.2.4. Depression
The two-item Patient Health Questionnaire (PHQ-2) was used to measure the depressive symptoms at three periods of the pandemic. The items focused on the frequency of depressed mood and little interest or pleasure in doing things over past 2 weeks (Arrieta et al., 2017). Each item was scored from 0 (not at all) to 3 (nearly every day), with a total score ranging from 0 to 6. The cutoff score of 3 has been recommended to detect probable cases of depression (Arrieta et al., 2017; Yu et al., 2011; Zhang et al., 2013). PHQ-2 has demonstrated good reliability and validity to assess depression among Chinese college students (Zhang et al., 2013). The Cronbach's α was 0.80 in our study.
2.2.5. Suicidal ideation (SI)
SI was measured at three time points by referring to the 9th item of the PHQ-9: “How often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” The item was scored from 0 (not at all) to 3 (nearly every day). SI was deemed to be present in respondents who scored 1 and above. The 9th item of PHQ-9 has been widely used as a single measure to assess the prevalence of SI in research studies (Bauer et al., 2013; Denneson et al., 2014; Walker et al., 2008).
2.3. Statistical analysis
Demographic information and other categorical variables were presented as counts and percentages. According to previous studies (Wang et al., 2022a, 2022b), participants were classified into five trajectories based on temporal changes of SI (see Supplemental Material Fig.A1): (1) Resilient: SI was absent at all three time points; (2) Persistent dysfunction: SI were all positive at three time points;(3) Recovery: SI was positive at T1 but negative at T3; (4) Delayed dysfunction: SI was negative at T1 but positive at T3 (5) Relapsing/remitting: SI was positive at T1 and T3 but negative at T2, or SI negative at T1 and T3 but at positive at T2.
Nonparametric tests were performed to examine significant changes in the prevalence of depression and SI at different periods of the COVID-19 pandemic. Further, multivariate logistic regressions were performed to examine predictors for trajectories of SI. Our major interest was to explore the risk factors associated with increased likelihood of developing delay-onset or persistence of SI during the long-term lockdown. Therefore, we set the resilient group as the referent group and compared it with a delayed dysfunction group. We also explored factors associated with increased likelihood of developing persistent SI with the recovery group as the reference group. All analyses were performed with IBM SPSS Statistics version 24.0. Odds ratios (ORs) and their 95% confidence intervals (CIs) were used to quantify the strengths of associations and a two-tailed test with a p-value of less than 0.05 was considered statistically significant.
3. Results
3.1. Sample characteristics
Among 35,516 participants, 26,272 (74.0%) were male and 9244 (26.0%) were female. Approximately two-fifths lived in rural areas (40.4%, n = 14,347), and most of the students (94.5%, n = 33,578) were undergraduates. Other sample characteristics including place of residence, history of mental illness, COVID-19 related factors, and psychosocial factors are presented in Table 1 .
Table 1.
Prevalence of SI determined by three surveys according to demographics, COVID-19 related factors, and psychosocial factors (N = 35,516).
| Characteristics | N (%) | SI (%) | |||
|---|---|---|---|---|---|
| T1 | T2 | T3 | |||
| Gender | Male | 9244 (26.0) | 7.2 | 10.6 | 13.0 |
| Female | 26,272 (74.0) | 7.3 | 9.1 | 12.1 | |
| χ2 | 0.20 | 18.31⁎⁎⁎ | 5.16* | ||
| Grade | Freshman | 12,726 (35.8) | 7.3 | 9.1 | 11.9 |
| Sophomore | 10,447 (29.4) | 7.5 | 9.8 | 12.8 | |
| Junior | 7258 (20.4) | 7.8 | 9.9 | 13.5 | |
| Senior | 3147 (8.9) | 7.2 | 10.3 | 11.7 | |
| Postgraduate | 1938 (5.5) | 3.7 | 7.0 | 10.0 | |
| χ2 | 41.59⁎⁎⁎ | 21.03⁎⁎⁎ | 23.98⁎⁎⁎ | ||
| Residence location | Rural | 14,347 (40.4) | 7.1 | 9.3 | 12.0 |
| Urban | 21,169 (59.6) | 7.4 | 9.6 | 12.6 | |
| χ2 | 1.19 | 1.05 | 2.61 | ||
| Only-children family | Yes | 7266 (20.5) | 7.2 | 9.5 | 12.6 |
| No | 28,250 (79.5) | 7.3 | 9.4 | 12.3 | |
| χ2 | 0.16 | 0.01 | 0.38 | ||
| History of mental illness | Yes | 296 (0.8) | 27.0 | 30.7 | 33.4 |
| No | 35,220 (99.2) | 7.1 | 9.3 | 12.2 | |
| χ2 | 173.05⁎⁎⁎ | 158.18⁎⁎⁎ | 122.39⁎⁎⁎ | ||
| Confirmed COVID-19 cases in the community or village | Yes | 2352 (6.6) | 10.7 | 13.1 | 15.9 |
| No | 33,164 (93.4) | 7.0 | 9.2 | 12.1 | |
| χ2 | 43.41⁎⁎⁎ | 39.13⁎⁎⁎ | 29.05⁎⁎⁎ | ||
| Relatives or friends being infected with COVID-19 | Confirmed/suspected | 400 (1.1) | 14.0 | 15.3 | 19.0 |
| No | 35,116 (98.9) | 7.2 | 9.4 | 12.3 | |
| χ2 | 27.25⁎⁎⁎ | 15.91⁎⁎⁎ | 16.43⁎⁎⁎ | ||
| Depression at T3 | Yes | 2867 (8.1) | 22.1 | 28.6 | 38.2 |
| No | 32,649 (91.9) | 6.0 | 7.8 | 10.1 | |
| χ2 | 1016.05⁎⁎⁎ | 1332.11⁎⁎⁎ | 1914.46⁎⁎⁎ | ||
| Social support at T1a | Low | 8761 (24.7) | 17.0 | 18.3 | 22.4 |
| Medium | 16,179 (45.6) | 5.4 | 7.9 | 10.7 | |
| High | 10,576 (29.8) | 2.0 | 4.5 | 6.7 | |
| χ2 | 1758.23⁎⁎⁎ | 1153.25⁎⁎⁎ | 1172.77⁎⁎⁎ | ||
| Positive coping at T1b | Low | 9138 (25.7) | 13.5 | 14.5 | 18.3 |
| Medium | 16,233 (45.7) | 6.6 | 9.1 | 11.8 | |
| High | 10,145 (28.6) | 2.8 | 5.5 | 8.0 | |
| χ2 | 852.72⁎⁎⁎ | 460.85⁎⁎⁎ | 478.48⁎⁎⁎ | ||
| Negative coping at T1c | Low | 8304 (23.4) | 2.8 | 5.0 | 7.2 |
| Medium | 17,147 (48.3) | 6.6 | 8.8 | 11.7 | |
| High | 10,065 (28.3) | 12.1 | 14.3 | 17.8 | |
| χ2 | 595.98⁎⁎⁎ | 478.79⁎⁎⁎ | 493.64⁎⁎⁎ | ||
| Family function at T2 | Poor | 2675 (7.5) | 17.8 | 22.2 | 26.0 |
| Fair | 14,755 (41.5) | 9.7 | 13.7 | 16.8 | |
| Good | 18,086 (50.9) | 3.7 | 4.1 | 6.7 | |
| χ2 | 910.67⁎⁎⁎ | 1440.88⁎⁎⁎ | 1254.52⁎⁎⁎ | ||
Note:
The mean (SD) age at baseline for the 35,516 college students was 20.25 (1.85) years.
T1 = measured at Time 1, T2 = measured at Time 2, T3 = measured at Time 3.
p < 0.05, ⁎⁎p < 0.01,.
p < 0.001.
Low, score ≤53; medium, score = 54–69; high, score ≥70.
Low, score ≤19; medium, score = 20–27; high, score ≥28.
Low, score ≤5; medium, score = 6–10; high, score ≥11.
3.2. Prevalence of depressive symptoms and SI
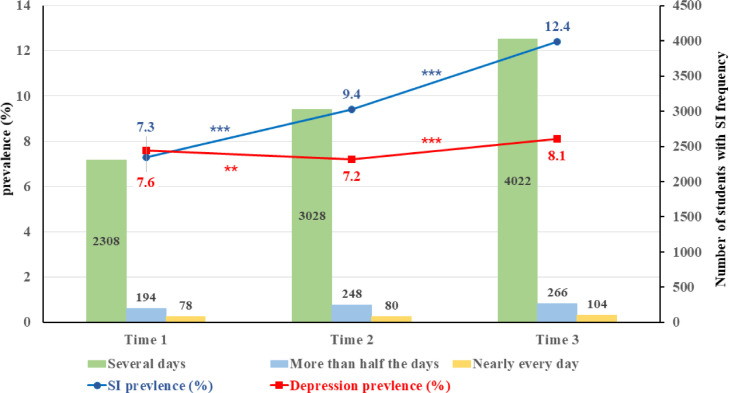
Fig. 2 presents rates of self-reported SI and depressive symptoms. The rates of depressive symptoms fluctuated across three phases of the pandemic (7.6% at T1 v. 7.2% at T2, p < 0.01; 7.2% at T2 v. 8.1% at T3, p < 0.001), while SI significantly increased over time. Specifically, the prevalence of probable SI at T1, T2 and T3 was 7.3%, 9.4%, 12.6%, respectively. Rates of SI increased significantly from T1 to T2 (p < 0.001) and from T2 to T3 (p < 0.001).
Fig. 2.
Point prevalence of depressive symptoms and suicidal ideation (SI) in college students across three periods of COVID-19.
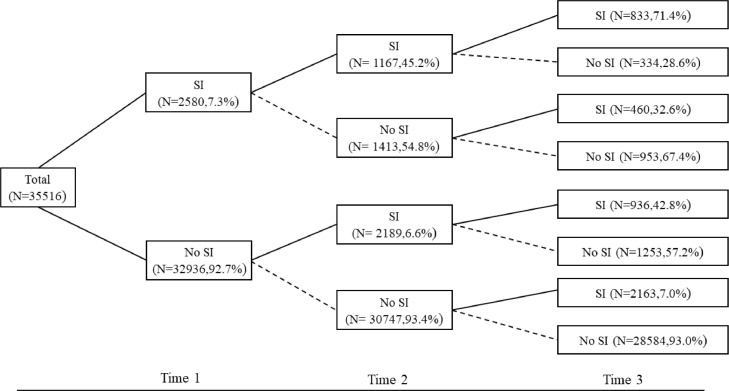
3.3. Trajectories of SI
Fig. 3 illustrates the trajectories of the SI across three waves. Those in the resilient group who did not report SI at all three periods comprised 80.5% of the sample. Approximately 2.3% of the respondents (the persistent dysfunction group) continuously reported SI at all three follow-ups. About 3.6% (the recovery group) of the respondents reported SI at T1 but recovered at T3, while 8.7% of the respondents (the delayed dysfunction group) did not exhibit SI at T1, but went on to develop this pathology at T3. For the relapsing/remitting group whose SI fluctuated and showed a cyclical course were approximately 4.8% of all participants.
Fig. 3.
Changing patterns of suicidal ideation (SI) across three periods of COVID-19. Values represent numbers and percentages of college students screened as having SI at each wave.
3.4. Predictors of SI in the delayed-dysfunction group and persistent dysfunction group
As shown in Table 2 , the likelihood of developing delayed dysfunction was greater if the respondents were junior-year undergraduates (OR = 1.20, p < 0.001) and postgraduates (OR = 1.22, p < 0.05), had a history of mental illness (OR = 1.98, p < 0.001), were living in communities or villages with reported infections or suspected cases (OR = 1.16, p < 0.05), experienced more depressive symptoms at T3 (OR = 3.54, p < 0.001), and adopted more negative coping strategies (OR for medium v. low = 1.47, p < 0.001; OR for high v. low = 2.41, p < 0.001). While higher perceived social support at T1 (OR for medium v. low = 0.68, p < 0.001; OR for high v. low = 0.59, p < 0.001), more positive coping strategies at T1 (OR for medium v. low = 0.80, p < 0.001; OR for high v. low = 0.73, p < 0.001), and higher levels of family functioning at T2 (OR for fair v. poor = 0.88, p < 0.05; OR for good v. poor = 0.41, p < 0.001) were significantly associated with decreased risk of developing delayed dysfunction in the form of SI.
Table 2.
Risk and protective factors of SI trajectory groups.
| Delay v. Resilient | Persistent v. Recovery | ||
|---|---|---|---|
| Gender (Male as Ref.) | Female | 0.92 (0.85,1.01) | 1.09 (0.89,1.34) |
| Grade (Freshman as Ref.) | Sophomore | 1.07 (0.97,1.18) | 1.03 (0.82,1.28) |
| Junior | 1.20 (1.08,1.33)⁎⁎⁎ | 0.86 (0.67,1.09) | |
| Senior | 1.07 (0.92,1.24) | 0.98 (0.70,1.36) | |
| Postgraduate | 1.22 (1.02,1.46)* | 0.87 (0.49,1.53) | |
| Residence location$$(Rural as Ref.) | Urban | 1.03 (0.95,1.12) | 0.99 (0.82,1.20) |
| Only-children family # | Yes | 1.09 (0.99,1.21) | 1.26 (1.01,1.59)* |
| History of mental illness # | Yes | 1.98 (1.39,2.83)⁎⁎⁎ | 1.97 (1.17,3.32)⁎⁎ |
| Confirmed COVID-19 cases in the community or village # | Yes | 1.16 (1.00,1.34)* | 1.06 (0.79,1.44) |
| Relatives or friends being infected with COVID-19 # | Confirmed/suspected | 1.37 (0.99,1.90) | 0.83 (0.44,1.58) |
| Depression at T3 # | Yes | 3.54 (3.18,3.93) ⁎⁎⁎ | 3.92 (3.16,4.87)⁎⁎⁎ |
| Social support at T1a$$(Low as Ref.) | Medium | 0.68 (0.62,0.75)⁎⁎⁎ | 0.76 (0.62,0.94)⁎⁎ |
| High | 0.59 (0.52,0.67) ⁎⁎⁎ | 0.87 (0.59,1.29) | |
| Positive coping at T1b$$(Low as Ref.) | Medium | 0.80 (0.73,0.88) ⁎⁎⁎ | 0.83 (0.68,1.02) |
| High | 0.73 (0.64,0.82) ⁎⁎⁎ | 0.79 (0.56,1.10) | |
| Negative coping at T1c$$(Low as Ref.) | Medium | 1.47 (1.32,1.64) ⁎⁎⁎ | 1.40 (0.99,1.97)* |
| High | 2.41 (2.15,2.71)⁎⁎⁎ | 1.50 (1.06,2.12)* | |
| Family function at T2$$(Poor as Ref.) | Fair | 0.88 (0.77,1.00)* | 0.74 (0.58,0.94)⁎⁎ |
| Good | 0.41 (0.35,0.47)⁎⁎⁎ | 0.38 (0.28,0.51)⁎⁎⁎ |
Note: Data are given as odds ratio (95% confidence interval).
Delay = delayed dysfunction group, Persistent = persistent dysfunction group, Recovery =recovery group, Resilient = resilient group.
T1= measured at Time 1, T2= measured at Time 2, T3= measured at Time 3.
No as the referent variable.
p < 0.05,.
p < 0.01,.
p < 0.001.
Low, score ≤53; medium, score = 54–69; high, score ≥70.
Low, score ≤19; medium, score = 20–27; high, score ≥28.
Low, score ≤5; medium, score = 6–10; high, score ≥11.
Meanwhile, we also set the recovery group as the referent group and compared to the persistent dysfunction group. The likelihood of reporting persistent SI during the 4-month lockdown was more likely among participants who were single child (OR=1.26, p < 0.05) with history of mental illness (OR=1.97, p < 0.01), and those who experienced more depressive symptoms (OR=3.92, p < 0.001) and reported higher level of negative coping (OR for medium v. low=1.40, p < 0.05; OR for high v. low =1.50, p < 0.05). While higher social support (OR for medium v. low=0.76, p < 0.01) and better family function (OR for fair v. poor=0.74, p < 0.01; OR for good v. poor =0.38, p < 0.001) decreased the likelihood of developing persistent SI among college students.
4. Discussion
To our knowledge, this was the first study to examine longitudinal changes in SI among college students across three different stages of the COVID-19 pandemic lockdown in China. Overall, the rates of SI among college students increased significantly during extended lockdown. Further, this study identified five different trajectories of SI. Most of the students were in the resilient group, while a small proportion of students exhibited persistent or delayed onset of SI. Thus, we further explored multiple factors related to distinct SI trajectories. Factors significantly associated with worsening SI included being a junior undergraduate/postgraduate, confirmed COVID-19 cases in the community/village, history of mental illness, depressive symptoms and negative coping strategies.
Although the threat from COVID-19 was largely contained, we found that SI had been aggravated among college students in China. Contrary to findings from short-term longitudinal studies (Isumi et al., 2020; López Steinmetz et al., 2021), our results were consistent with studies that highlighted the passive effect of the 3-month lockdown on SI during the COVID-19 pandemic (Killgore et al., 2020). Previous evidence has found that pandemic-related stress might be a risk factor for SI among college students (Kohls et al., 2021; Sun et al., 2021). The pandemic caused massive disruption to normal college life for students in China who may have experienced intense pressure arising from difficulties adapting to online modes of learning, leading to concerns and uncertainty about their academic performance (Li et al., 2021; Son et al., 2020), their future and their educational prospects (Cao et al., 2020), all of which increased the risk of suicide among college students. Moreover, a growing body of evidence supports the view that home quarantine might explain higher incidences of family conflict, as a result of more intense feelings of loneliness among college students who had a limited amount of personal space and were isolated from their peer groups during the COVID-19 lockdown (Cui and Hong, 2021; Silk et al., 2021;Elbogen et al., 2021). Thus, there is an urgent need to develop psychological prevention measures that target students who have been particularly impacted during the pandemic.
The SI trajectories showed that the majority of the respondents (80.5% resilient to SI) exhibited very mild or no symptoms throughout the 4-month lockdown. This finding was in line with previous studies, which suggested that most individuals who were exposed to traumatic events were able to maintain a stable trajectory of euthymia and healthy functioning (Bonanno et al., 2010; Foa et al., 2006). However, there was still a small percentage of college students who had persistent (2.3%) or delayed onset (8.7%) of SI during the COVID-19 lockdown. There is a need to further explore the sociodemographic backgrounds and psychological characteristics of these groups of students, who may be most at risk of having an adverse response to lockdown.
The current study identified a number of risk factors associated with changes in SI among college students. Specific groups appeared to be affected by the COVID-19 confinement to a greater extent. In terms of educational level, junior-year college students were at a higher risk of delayed occurrence of SI. This finding may be explained by the fact that junior-year college students were at a transitional stage of choosing their career paths (e.g., further education or work) and commencing training for necessary skills to enter their future professions (Parola, 2020). However, confinement had a serious impact on the time horizon, hindering aspirations and plans for the future, which led to higher levels of psychological stress among junior undergraduates. In addition, a significantly higher risk of delayed onset of SI was also found among postgraduate students under lockdown measures, which was consistent with previous findings concerning a mental health crisis among postgraduate students (Byrom et al., 2020; Evans et al., 2018; Kapasia et al., 2020). This might be attributed to the fact that the lockdown measures meant that many students were unable to conduct field or laboratory-based work, an often critical component of certain courses, which may have worsened academic-related stress (Paula, 2020). Similar to prior studies (Chen et al., 2020; Prime et al., 2020), only-child students were found to be more likely to present with persistent SI during the COVID-19 pandemic. One possible explanation was that only-child students were more likely to perceive their parents as overprotective, though they experienced a greater sense of isolation and loneliness compared to students with siblings, which led to an increase in SI during the pandemic (Prime et al., 2020). Further, previous studies have shown that individuals with history of psychiatric illness are more susceptible to SI (Francis et al., 2020; Hao et al., 2020; O'Connor et al., 2020; Papadopoulou et al., 2021), and our findings also supported the close link between history of mental illness and SI during the COVID-19 pandemic. The consistency of the results confirms the severity of the negative psychological impact that the COVID-19 pandemic and strict lockdown measures had on students with a history of mental illness. With respect to COVID-19-related factors, students who were aware of confirmed COVID-19 cases in their community or village were more likely to report delayed dysfunction, which may be related to increasing panic in their neighborhood, given the higher risk of being exposed to COVID-19 (Pokhrel et al., 2020), and more pandemic-related stress in response to stricter quarantine measurements put in place in the communities or villages (Benke et al., 2020). Collectively, these results suggested that specific groups with higher risks of suicide should be regarded as priority groups for suicide prevention.
The findings of the current study highlight the predictive effect of psychological factors on the SI trajectory. Indeed, the results suggested that individuals who reported depressive symptoms were at more than a three-fold increased risk of developing persistent or delayed occurrence of SI during the lockdown. This result was in line with previous studies that have repeatedly documented the close association between depression and SI in college students (Garlow et al., 2008; Wang et al., 2019). On the contrary, we found that better family functioning and a higher level of social support were significant protective factors against worsening SI, which was in agreement with recent reports (Ayuso-Mateos et al., 2021; Papadopoulou et al., 2021). Good family functioning might include a family's strong ability to adapt to the pandemic, and to benefit from supportive communication between family members, which can reinforce feelings of social connectedness (Papadopoulou et al., 2021). Greater social connectedness can, to some extent, prevent the incidence of SI among college students during the stay-at-home period (Calati et al., 2019). Moreover, the availability of social support is among the most well-documented variables that influences suicidal behavior (Ayuso-Mateos et al., 2021; Calati et al., 2019; Hegerl and Heinz, 2019). The current results emphasized the buffering effect of social support in times of high psychological stress (Cohen, 2004). Further, our findings are also consistent with existing literature (Papadopoulou et al., 2021), showing that positive coping was a vital protective factor for delayed occurrence of SI during the pandemic, whereas negative coping was a significant risk factor for delayed occurrence or persistent SI. Previous study has indicated that maladaptive coping strategies appear to nurture isolation-based behaviors in time of crisis, which further increased rate of suicide (Gould et al., 2004). In this sense, Klonsky and May's Three-Step Theory of Suicide proposed that social connectedness protects against an escalation in SI and wards off the risk of attempted suicide (Klonsky et al., 2016). Since social distancing and isolation stemming from lockdown are inevitable, strengthening social connectedness through family, friends and others under lockdown is important in order to reduce the risk of suicide.
Although this study considered many factors, our findings still need to be interpreted within the context of its limitations. First, we adopted a repeated cross-sectional web-based research design adopted in this survey, with high sample attrition rates, which may have led to bias in regard to the prevalence of symptoms. It is generally assumed that online surveys are much likely to achieve a low response rate (Nulty, 2008) and attrition rates are indeed sizeable in some psychiatric epidemiological studies (Bellón et al., 2010; de Graaf et al., 2000). In addition, our research was based on self-reports, which may have been impacted by reporting bias in the data collection. Third, a large proportion of the participants were female (74%), similar to previous studies that have examined mental health among college students (Cao et al., 2020; Sun et al., 2021; Tang et al., 2020). Potentially, female students may be more willing to participate in the research, and a higher proportion of females might affect estimates of depression. Fourth, besides the pandemic and its restrictions, some confounding factors might have affected SI among the college students; for example, stressful life events that occurred during isolation were not investigated, which may have led to some deviation in our results. Moreover, some students might have sought some form of psychological help (e.g., the ‘Xinqing’ Hotline, set up by South China Normal University) during the study period, which may have had an effect on SI among this cohort.
5. Conclusion
In conclusion, our findings confirmed that extended lockdown during the COVID-19 pandemic increased SI among college students in China, but only a small number of students showed obvious SI symptoms. Therefore, there is a need to monitor and pay careful attention to college students who may have been at a higher risk of developing persistent or delayed onset SI during lockdown, especially students from only-child families, junior-year undergraduates and postgraduates, and those with a history of mental illness or confirmed COVID-19 cases in their community or village. Meanwhile, it is important to develop psychological interventions that aim to improve family functioning and social support, and to design adaptive coping strategies for students, all of which are essential for the prevention of SI during COVID-19 lockdown.
Author disclosure
Contributors
Shuiqing Huang: Conceptualization, Formal analysis, Writing-original draft. Dongfang Wang, Jingbo Zhao: Formal analysis, Writing-review & editing. Huilin Chen, Zijuan Ma, Ye Pan: Formal analysis, Investigation. Xianchen Liu: Conceptualization, Writing - review & editing. Fang Fan: Conceptualization, Project administration, Methodology, Resources.
Role of the founding source
The present study was funded by National Natural Science Foundation of China (Grant No. 31871129); Research on the Processes and Repair of Psychological Trauma in Youth, Project of Key Institute of Humanities and Social Sciences, MOE (Grant No.16JJD190001); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (GDUPS 2016); and Graduate Research and Innovation Project of School of Psychology, South China Normal University (PSY-SCNU202017, PSY-SCNU202026).
CRediT authorship contribution statement
Shuiqing Huang: Conceptualization, Formal analysis, Writing – original draft. Dongfang Wang: Formal analysis, Writing – review & editing. Jingbo Zhao: Formal analysis, Writing – review & editing. Huilin Chen: Formal analysis, Investigation. Zijuan Ma: Formal analysis, Investigation. Ye Pan: Formal analysis, Investigation. Xianchen Liu: Conceptualization, Writing – review & editing. Fang Fan: Conceptualization, Project administration, Methodology, Resources.
Declaration of Competing Interest
All authors declare that they have no conflict of interest.
Acknowledgements
The authors want to express their sincere gratitude to all participants for participating in the study.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2022.114653.
Appendix. Supplementary materials
References
- Arrieta J., Aguerrebere M., Raviola G., Flores H., Elliott P., Espinosa A., Reyes A., Ortiz-Panozo E., Rodriguez-Gutierrez E.G., Mukherjee J., Palazuelos D., Franke M.F. Validity and utility of the patient health questionnaire (PHQ)-2 and PHQ-9 for screening and diagnosis of depression in rural Chiapas, Mexico: a Cross-Sectional study. J. Clin. Psychol. 2017;73(9):1076–1090. doi: 10.1002/jclp.22390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayuso-Mateos J.L., Morillo D., Haro J.M., Olaya B., Lara E., Miret M. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci. 2021;30:e49. doi: 10.1017/s2045796021000408. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Bauer A.M., Chan Y.F., Huang H., Vannoy S., Unützer J. Characteristics, management, and depression outcomes of primary care patients who endorse thoughts of death or suicide on the PHQ-9. J. Gen. Intern. Med. 2013;28(3):363–369. doi: 10.1007/s11606-012-2194-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellón J.A., de Dios Luna J., Moreno B., Montón-Franco C., GildeGómez-Barragán M.J., Sánchez-Celaya M., Díaz-Barreiros M.A., Vicens C., Motrico E., Martínez-Cañavate M.T., Oliván-Blázquez B., Vázquez-Medrano A., Sánchez-Artiaga M.S., March S., del Mar Muñoz-García M., Moreno-Peral P., Nazareth I., King M., Torres-González F. Psychosocial and sociodemographic predictors of attrition in a longitudinal study of major depression in primary care: the predictD-Spain study. J. Epidemiol. Commun. Health. 2010;64(10):874–884. doi: 10.1136/jech.2008.085290. [DOI] [PubMed] [Google Scholar]
- Benke C., Autenrieth L.K., Asselmann E., Pané-Farré C.A. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Brewin C.R., Kaniasty K., Greca A.M. Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychol. Sci. Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Byrom N.C., Dinu L., Kirkman A., Hughes G. Predicting stress and mental wellbeing among doctoral researchers. J. Ment. Health. 2020:1–9. doi: 10.1080/09638237.2020.1818196. [DOI] [PubMed] [Google Scholar]
- Calati R., Ferrari C., Brittner M., Oasi O., Olié E., Carvalho A.F., Courtet P. Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J. Affect. Disord. 2019;245:653–667. doi: 10.1016/j.jad.2018.11.022. [DOI] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan S.M., Chiu F.K., Lam C.W., Leung P.Y., Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2006;21(2):113–118. doi: 10.1002/gps.1432. [DOI] [PubMed] [Google Scholar]
- Chen S., Cheng Z., Wu J. Risk factors for adolescents' mental health during the COVID-19 pandemic: a comparison between Wuhan and other urban areas in China. Global Health. 2020;16(1):96. doi: 10.1186/s12992-020-00627-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59(8):676–684. doi: 10.1037/0003-066x.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cui M., Hong P. COVID-19 and mental Health of young adult children in China: economic impact, family dynamics, and resilience. Fam. Relat. 2021 doi: 10.1111/fare.12573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlem N.W., Zimet G.D., Walker R.R. The multidimensional scale of perceived social support: a confirmation study. J. Clin. Psychol. 1991;47(6):756–761. doi: 10.1002/1097-4679(199111)47:6<756::aid-jclp2270470605>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- de Graaf R., Bijl R.V., Smit F., Ravelli A., Vollebergh W.A. Psychiatric and sociodemographic predictors of attrition in a longitudinal study: the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Am. J. Epidemiol. 2000;152(11):1039–1047. doi: 10.1093/aje/152.11.1039. [DOI] [PubMed] [Google Scholar]
- Denneson L.M., Corson K., Helmer D.A., Bair M.J., Dobscha S.K. Mental health utilization of new-to-care Iraq and Afghanistan Veterans following suicidal ideation assessment. Psychiatry Res. 2014;217(3):147–153. doi: 10.1016/j.psychres.2014.03.017. [DOI] [PubMed] [Google Scholar]
- Dong X., Zhao L., Sun T., Yun F., Qiu L. Prevalence of depressive symptoms and associated factors among internal migrants with tuberculosis: a cross-sectional study in China. Am. J. Trop. Med. Hyg. 2020;102(1):31–35. doi: 10.4269/ajtmh.19-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efstathiou V., Michopoulos I., Yotsidi V., Smyrnis N., Zompola C., Papadopoulou A., Pomini V., Papadopoulou M., Tsigkaropoulou E., Tsivgoulis G., Douzenis A., Gournellis R. Does suicidal ideation increase during the second COVID-19 lockdown? Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen E.B., Lanier M., Blakey S.M., Wagner H.R., Tsai J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: the role of COVID-19-related stress, social isolation, and financial strain. Depress. Anxiety. 2021 doi: 10.1002/da.23162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans T.M., Bira L., Gastelum J.B., Weiss L.T., Vanderford N.L. Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 2018;36(3):282–284. doi: 10.1038/nbt.4089. [DOI] [PubMed] [Google Scholar]
- Fan F., Long K., Zhou Y., Zheng Y., Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol. Med. 2015;45(13):2885–2896. doi: 10.1017/s0033291715000884. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Stein D.J., McFarlane A.C. Symptomatology and psychopathology of mental health problems after disaster. J. Clin. Psychiatry. 2006;67(Suppl 2):15–25. [PubMed] [Google Scholar]
- Francis J.M., Every-Palmer S., Jenkins M., Gendall P., Hoek J., Beaglehole B., Bell C., Williman J., Rapsey C., Stanley J. Psychological distress, anxiety, family violence, suicidality, and wellbeing in New Zealand during the COVID-19 lockdown: a cross-sectional study. PLoS ONE. 2020;15(11) doi: 10.1371/journal.pone.0241658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garlow S.J., Rosenberg J., Moore J.D., Haas A.P., Koestner B., Hendin H., Nemeroff C.B. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress. Anxiety. 2008;25(6):482–488. doi: 10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- Gould M.S., Velting D., Kleinman M., Lucas C., Thomas J.G., Chung M. Teenagers' attitudes about coping strategies and help-seeking behavior for suicidality. J. Am. Acad. Child Adolesc. Psychiatry. 2004;43(9):1124–1133. doi: 10.1097/01.chi.0000132811.06547.31. [DOI] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. doi: 10.1016/s2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hegerl U., Heinz I. Reflections on causes of suicidal behaviour. Epidemiol Psychiatr Sci. 2019;28(5):469–472. doi: 10.1017/s2045796018000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/s2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isumi A., Doi S., Yamaoka Y., Takahashi K., Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110(Pt 2) doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jie Y. Reliablility and validity of the Chinese version of coping style scale. Chin. J. Clin. Psychol. 1998;2:114–115. [Google Scholar]
- Kapasia N., Paul P., Roy A., Saha J., Zaveri A., Mallick R., Barman B., Das P., Chouhan P. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal. India. Child Youth Serv Rev. 2020;116 doi: 10.1016/j.childyouth.2020.105194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Allbright M.C., Dailey N.S. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky E.D., May A.M., Saffer B.Y. Suicide, suicide attempts, and suicidal ideation. Annu. Rev. Clin. Psychol. 2016;12:307–330. doi: 10.1146/annurev-clinpsy-021815-093204. [DOI] [PubMed] [Google Scholar]
- Kohls E., Baldofski S., Moeller R., Klemm S.L., Rummel-Kluge C. Mental health, social and emotional well-being, and perceived burdens of university students during COVID-19 pandemic lockdown in Germany. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.643957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health. 2020;4(6):421. doi: 10.1016/s2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Fu P., Fan C., Zhu M., Li M. COVID-19 stress and mental health of students in locked-down colleges. Int. J. Environ. Res. Public Health. 2021;18(2) doi: 10.3390/ijerph18020771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Steinmetz L.C., Fong S.B., Godoy J.C. Suicidal risk and impulsivity-related traits among young Argentinean college students during a quarantine of up to 103-day duration: longitudinal evidence from the COVID-19 pandemic. Suicide Life Threat. Behav. 2021 doi: 10.1111/sltb.12799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man Y., Mengmeng L., Lezhi L., Ting M., Jingping Z. The psychological problems and related influential factors of left-behind adolescents (LBA) in Hunan, China: a cross sectional study. Int J Equity Health. 2017;16(1):163. doi: 10.1186/s12939-017-0639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marelli S., Castelnuovo A., Somma A., Castronovo V., Mombelli S., Bottoni D., Leitner C., Fossati A., Ferini-Strambi L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2021;268(1):8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of People's Republic of China, 2020. Latest situation of COVID-19.
- Nulty D.D. The adequacy of response rates to online and paper surveys: what can be done? Assessment Evaluat. Higher Educ. 2008;33(3):301–314. [Google Scholar]
- O'Connor R.C., Wetherall K., Cleare S., McClelland H., Melson A.J., Niedzwiedz C.L., O'Carroll R.E., O'Connor D.B., Platt S., Scowcroft E., Watson B., Zortea T., Ferguson E., Robb K.A. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadopoulou A., Efstathiou V., Yotsidi V., Pomini V., Michopoulos I., Markopoulou E., Papadopoulou M., Tsigkaropoulou E., Kalemi G., Tournikioti K., Douzenis A., Gournellis R. Suicidal ideation during COVID-19 lockdown in Greece: prevalence in the community, risk and protective factors. Psychiatry Res. 2021;297 doi: 10.1016/j.psychres.2021.113713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola A. Novel coronavirus outbreak and career development: a narrative approach into the meaning for italian university graduates. Front. Psychol. 2020;11:2255. doi: 10.3389/fpsyg.2020.02255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paula J.R. Lockdowns due to COVID-19 threaten PhD students' and early-career researchers' careers. Nat. Ecol. Evol. 2020;4(8):999. doi: 10.1038/s41559-020-1231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhrel P., Hu C., Mao H. Detecting the Coronavirus (COVID-19) ACS Sens. 2020;5(8):2283–2296. doi: 10.1021/acssensors.0c01153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Ren Y., Qian W., Li Z., Liu Z., Zhou Y., Wang R., Qi L., Yang J., Song X., Zeng L., Zhang X. Public mental health under the long-term influence of COVID-19 in China: geographical and temporal distribution. J. Affect. Disord. 2020;277:893–900. doi: 10.1016/j.jad.2020.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds D.L., Garay J.R., Deamond S.L., Moran M.K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008;136(7):997–1007. doi: 10.1017/s0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi L., Que J.Y., Lu Z.A., Gong Y.M., Liu L., Wang Y.H., Ran M.S., Ravindran N., Ravindran A.V., Fazel S., Bao Y.P., Shi J., Lu L. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur. Psychiatry. 2021;64(1):e18. doi: 10.1192/j.eurpsy.2021.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk J.S., Scott L.N., Hutchinson E.A., Lu C., Sequeira S.L., McKone K.M.P., Do Q.B., Ladouceur C.D. Storm Clouds and Silver Linings: day-to-Day Life in COVID-19 Lockdown and Emotional Health in Adolescent Girls. J. Pediatr. Psychol. 2021 doi: 10.1093/jpepsy/jsab107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smilkstein G. The Family APGAR: a proposal for family function test and its use by physicians. J Fam Pract. 1978;6(6):1231–1239. [PubMed] [Google Scholar]
- Smilkstein G., Ashworth C., Montano D. Validity and reliability of the family APGAR as a test of family function. J. Fam. Pract. 1982;15(2):303–311. [PubMed] [Google Scholar]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on College Students’ Mental Health in the United States: interview Survey Study. J. Med. Internet Res. 2020;22(9):e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S., Goldberg S.B., Lin D., Qiao S., Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Global Health. 2021;17(1):15. doi: 10.1186/s12992-021-00663-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker J., Waters R.A., Murray G., Swanson H., Hibberd C.J., Rush R.W., Storey D.J., Strong V.A., Fallon M.T., Wall L.R., Sharpe M. Better off dead: suicidal thoughts in cancer patients. J. Clin. Oncol. 2008;26(29):4725–4730. doi: 10.1200/jco.2007.11.8844. [DOI] [PubMed] [Google Scholar]
- Wang D., Zhao J., Ross B., Ma Z., Zhang J., Fan F., Liu X. Longitudinal trajectories of depression and anxiety among adolescents during COVID-19 lockdown in China. J. Affect. Disord. 2022;299:628–635. doi: 10.1016/j.jad.2021.12.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D., Zhao J., Zhai S., Huang S., Yang Z., Pan Y., Liu X., Fan F. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J. Psychosom. Res. 2022;157 doi: 10.1016/j.jpsychores.2022.110795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Kou C., Bai W., Song Y., Liu X., Yu W., Li Y., Hua W., Li W. Prevalence and correlates of suicidal ideation among college students: a mental health survey in Jilin Province. China. J Affect Disord. 2019;246:166–173. doi: 10.1016/j.jad.2018.12.055. [DOI] [PubMed] [Google Scholar]
- Wang X., Wang X., Ma H. The Journal of Chinese Psychological Press; China, Beijing: 1999. Rating Scales for Mental health: Social support Rating Scale. [Google Scholar]
- Xie Y. Reliability and validity of the simplified coping style questionnaire. Chinese J. Clin. Psychol. 1998 [Google Scholar]
- Yu X., Stewart S.M., Wong P.T., Lam T.H. Screening for depression with the Patient Health Questionnaire-2 (PHQ-2) among the general population in Hong Kong. J. Affect. Disord. 2011;134(1–3):444–447. doi: 10.1016/j.jad.2011.05.007. [DOI] [PubMed] [Google Scholar]
- Zhang M., Zhang J., Zhang F., Zhang L., Feng D. Prevalence of psychological distress and the effects of resilience and perceived social support among Chinese college students: does gender make a difference? Psychiatry Res. 2018;267:409–413. doi: 10.1016/j.psychres.2018.06.038. [DOI] [PubMed] [Google Scholar]
- Zhang Y.L., Liang W., Chen Z.M., Zhang H.M., Zhang J.H., Weng X.Q., Yang S.C., Zhang L., Shen L.J., Zhang Y.L. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Wang D., Zhao J., Chen X.Y., Chen H., Ma Z., Yu Q., Wang T., Chen Z., Jiang J., Zhu Z., Huang S., Fan F., Liu X. Insomnia and other sleep-related problems during the remission period of the COVID-19 pandemic: a large-scale survey among college students in China. Psychiatry Res. 2021;304 doi: 10.1016/j.psychres.2021.114153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.