Abstract
Prostate cancer (PCa) is a major diagnosed cancer among men globally, and about 20% of patients develop metastatic prostate cancer (mPCa) in the initial diagnosis. PCa is a typical androgen-dependent disease; thus, hormonal therapy is commonly used as a standard care for mPCa by inhibiting androgen receptor (AR) activities, or androgen metabolism. Inevitably, almost all PCa will acquire resistance and become castration-resistant PCa (CRPC) that is associated with AR gene mutations or amplification, the presence of AR variants, loss of AR expression toward neuroendocrine phenotype, or other hormonal receptors. Treating CRPC poses a great challenge to clinicians. Research efforts in the last decade have come up with several new anti-androgen agents to prolong overall survival of CRPC patients. In addition, many potential targeting agents have been at the stage of being able to translate many preclinical discoveries into clinical practices. At this juncture, it is important to highlight the emerging strategies including small-molecule inhibitors to AR variants, DNA repair enzymes, cell survival pathway, neuroendocrine differentiation pathway, radiotherapy, CRPC-specific theranostics and immune therapy that are underway or have recently been completed.
Keywords: castration-resistant prostate cancer, recurrent therapy and castration-resistant prostate cancer, precision medicine
1. Introduction
Prostate cancer (PCa) is the most common cancer and the second deadliest cancer among men in the United States, which is mainly due to metastatic disease [1]. In general, surgery or radiation is potentially a curative treatment for localized disease. Since PCa is characterized as a typical androgen-dependent disease [2], hormone therapy (i.e., androgen deprivation therapy (ADT)) is the most effective therapy to control metastatic disease. However, almost all patients eventually develop castration-resistant PCa (CRPC) within 12 to 18 months, with a median survival of 14 to 26 months [3]. Nowadays, new anti-androgens (Enzalutamide or Abiraterone), radiotherapy (Radium-223) or immunotherapy (sipuleucel-T) have been approved for metastatic CRPC (mCRPC) patients to prolong the overall survival. Inevitably, mCRPC further acquires resistance and becomes therapy- and castration-resistant PCa (t-CRPC), which is considered as an end-stage disease [4,5] without effective therapy, and on which new therapeutic strategies have been actively explored.
Clinical observation indicates that about 20–25% of CRPC patients recurred from ADT [6,7], harbored distinct cell features from classical adenocarcinoma in prostate; some carcinoma cells exhibit neuroendocrine phenotypes with neuronal markers expression and neuronal factors secretion in an endocrine fashion [8], which is considered as neuroendocrine PCa (NEPC), a subpopulation of t-CRPC. However, small-cell carcinoma of prostate (SCPC) with very low incidence (1% of the prostatic malignancies) has been identified from the primary site. Although SCPC is associated with a highly proliferative area of tumor mass and poor prognosis, it is still sensitive to chemotherapy [9,10]. On the other hand, NEPC is known to resist many therapeutic regimens. Currently, no effective targeted therapy for NEPC has been approved by the FDA. Based on molecular profiling from NEPC patients, this article has discussed several potential new therapeutic strategies for this disease.
2. Hormone Therapy
2.1. Enzalutamide
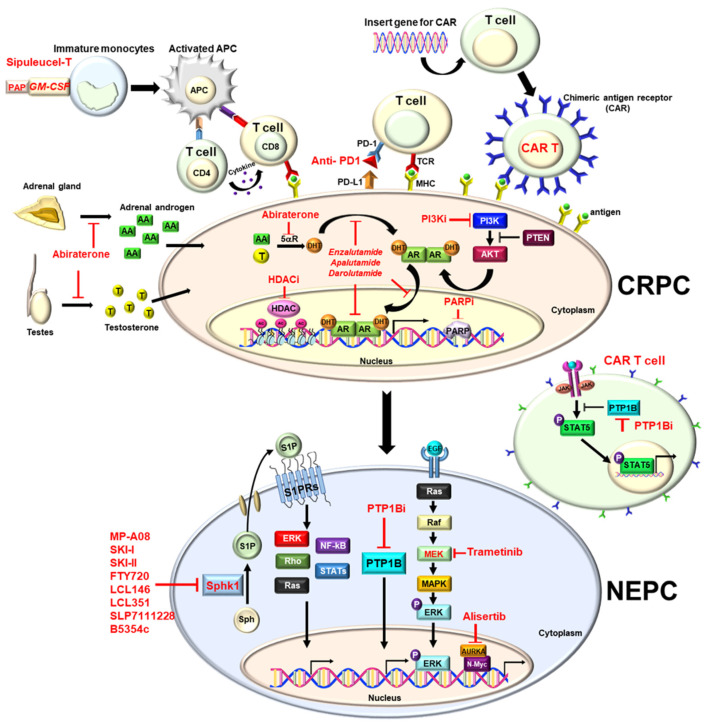
In PCa, androgen receptor (AR) activated by androgens still represents a critical oncogenic pathway. Enzalutamide is a novel antiandrogen agent that can block AR with high affinity compared to traditional antiandrogens such as bicalutamide or flutamide [11]. Besides direct binding to AR, it can reduce AR translocation into the nucleus and prevent its transcription by binding to DNA [12] (Figure 1).
Figure 1.
Molecular mechanism of the therapies for prostate cancer.
Enzalutamide was approved by the Food and Drug Administration (FDA) in 2012 for use on metastatic CRPC based on the randomized, phase III trial study (AFFIRM) [13,14] (Table 1). The study demonstrated that patients who received enzalutamide after chemotherapy improved median survival from 13.6 to 18.4 months (HR: 0.63 p < 0.001). Another phase III, double-blind, randomized study (PREVAIL) (Table 1) compared patients receiving enzalutamide before chemotherapy and showed that radiographic progression-free survival (rPFS) and overall survival (OS) benefit from 31.3 to 35.3 months [15,16]. It also can delay the initiation of chemotherapy in patients with metastatic PCa. In the phase III randomized trial (PROSPER), enzalutamide demonstrated the benefit of metastasis-free survival rate compared to placebo (36.6 months vs. 14.7 months, p < 0.001) in patients with non-metastatic CRPC (nmCRPC) [17] (Table 1). Therefore, the FDA expand the use of enzalutamide in patients with nmCRPC since 2018.
Table 1.
FDA-approved therapies for prostate cancer.
| Drug Class | Therapy | Indication | Clinical Trial |
Efficacy (Mon.) |
Impact on PCa Treatment | Reference |
|---|---|---|---|---|---|---|
| 2nd-generation antiandrogen | Enzalutamide | mCRPC | AFFIRM | OS 18.4 vs. 13.6 | ENZ improves OS after chemotherapy |
[14] |
| PREVAIL | OS 35.3 vs. 31.3 | ENZ improves OS in chemotherapy naïve |
[15,16] | |||
| nmCRPC | PROSPER | MFS 36.6 vs. 14.7 | ENZ decreases the risk of metastasis | [17] | ||
| mCSPC | ENZEMET | 80% vs. 72% (3-year OS) |
ENZ improves OS and decreases disease progression | [18] | ||
| ARCHES | rPFS NR vs. 19.0 |
ENZ decreases the risk of metastatic progression | [19] | |||
| Apalutamide | nmCRPC | SPARTAN | MFS 40.5 vs. 16.2 | APA decreasse the risk of metastasis | [20] | |
| mCSPC | TITAN | 2-year OS 82.4 vs. 73.5 |
APA improves OS and PFS | [21] | ||
| Darolutamide | nmCRPC | ARAMIS | MFS 40.4 vs. 18.4 | DA decreases the risk of metastasis | [22] | |
| Abiraterone | mCRPC | COA-301 | OS 15.8 vs. 11.2 | AB improves OS after chemotherapy |
[23] | |
| COA-302 | OS 34.7 vs. 30.3 | AB improves OS in chemotherapy naïve |
[24] | |||
| High-volume CSPC | LATITUDE | OS 53.3 vs. 36.5 | AB improves OS in high-risk CSPC |
[25,26] | ||
| Radiotherapy | Radium 223 | CRPC with symptomatic bone metastasis, no visceral metastasis | ALSYMPCA | OS 14.9 vs. 11.3 | RA-223 improves OS in symptomatic bony metastatic mCRPC | [27] |
| 177Lu-PSMA 617 | PSMA-positive mCRPC and already treated with ARB and chemotherapy | VISION | OS 15.3 vs. 11.3 rPFS 8.7 vs. 3.4 |
177Lu-PSMA 617 improves OS and rPFS in PSMA-positive mCRPC | [28] | |
| Immunotherapy | Sipuleucel-T | mCRPC | IMPACT | OS 25.8 vs. 21.7 | Sipuleucel-T improves OS in mCRPC | [29] |
| PARP-I | Olaparib | mCRPC with HRR genes mutation after ENZ or AB | PROfound | OS 18.5 vs.15.1 rPFS 7.4 cs. 3.6 |
Olaparib improves OS and rPFS in mCRPC with HRR gene mutation | [30] |
| Rubraca | mCRPC with BRCA genes after ARB or chemotherapy | TRITON2 (phase2) TRITON3 (phase3) |
ORR 43.5% (IRR) PSA response rate 54.8% |
Rubraca has the antitumor activity in mCRPC with BRCA gene mutation | [31,32] |
PCa = prostate cancer; nmCRPC = non-metastatic castration-resistant prostate cancer; mCSPC = metastatic castration-sensitive prostate cancer; mCRPC = metastatic castration-resistant prostate cancer; OS = overall survival; rPFS = Radiographic progression-free survival; FDA = Food and Drug Administration; ENZ = Enzalutamide; APA = Apalutamide; DA = Darolutamide; AB = Abiraterone; MFS = metastatic-free survival; NR = non-reached; RA-223 = Radium 223; ARB = androgen receptor blocker; HRR = homologous recombination repair; ORR = objective response rate; IRR = independent radiology review; PARP-I = Polyadenosine diphosphate ribose polymerase inhibitors.
In patients with metastatic, hormone-sensitive PCa (mHSPC), enzalutamide improved the overall survival rate and progression-free survival over standard care in the phase III, randomized trial (ENZAMET) [18] (Table 1). In another double-blind, randomized trial (ARCHES), enzalutamide also revealed the benefit of rPFS (not-reached vs. 19 months, p < 0.001) in mHSPC patients [19] (Table 1). Regarding the safety and adverse effects of the drug, enzalutamide had the adverse effect to the central nervous system via entering the blood–brain barrier. Therefore, seizure and even posterior encephalopathy syndrome were reported in rare cases [12,17].
2.2. Apalutamide
Apalutamide is a second-generation androgen inhibitor and is already approved for use in nmCRPC and mHSPC. A double-blind, placebo-controlled, phase III trial (SPARTAN) demonstrated that apalutamide improved median metastasis-free survival compared with placebo (40.5 vs. 16.2 months. p < 0.001) in patients with non-mCRPC [20] (Table 1). Time to symptomatic progression was significantly longer with apalutamide than with placebo [20]. Another randomized phase III trial (TITAN), in the patients with mHSPC, apalutamide plus ADT, significantly improved OS and rPFS compared with ADT plus placebo [21] (Table 1).
The adverse effects of interest include fracture, dizziness, and hypothyroidism. Compared with other androgen inhibitors with enzalutamide and darolutamide, skin rash was mostly found in apalutamide [12,20,21].
2.3. Darolutamide
Like other second-generation androgen inhibitors, darolutamide can inhibit AR translocation, DNA binding, and AR-mediated transcription (Figure 1). From the phase I/II study, darolutamide inhibited cell proliferation more efficiently than enzalutamide in a castration animal model [33]. Besides, it also blocks the activity of the mutant ARs like the F876L mutation caused by enzalutamide or apalutamide [33].
In a randomized, double-blind, placebo-controlled, phase III trial (ARAMIS), darolutamide improved metastasis-free survival (40.4 months vs. 18.4 months, p < 0.001) compared with placebo in patients with nmCRPC [22] (Table 1). Additionally, it also demonstrated benefit in OS, time to pain progression, time to cytotoxic chemotherapy, and time to a symptomatic skeletal event [22]. Another randomized, phase III trial (ARASENS), combination therapy with darolutamide, ADT, and docetaxel improve OS over placebo plus ADT and docetaxel in patients with mHSPC [34].
Generally, darolutamide causes less toxic effect because of low blood–brain barrier penetration and low binding affinity for γ-aminobutyric acid type A receptors due to its unique structure, which is different from enzalutamide and apalutamide. Therefore, it causes less central nervous system effect like a seizure [12,22]. The most reported adverse effects were fatigue and asthenic conditions [22].
2.4. Abiraterone
Abiraterone acetate is a selective CYP17 enzyme inhibitor that can decrease the synthesis of androgen of the testis, adrenal gland and prostate gland [35,36,37,38] (Figure 1). In the double-blind, placebo-controlled phase 3 study (CO-AA-301 clinical trial), it demonstrated that abiraterone combined with prednisolone improved OS compared to the placebo plus prednisolone group (15.8 vs. 11.2 months. p < 0.0001) in patients with mCRPC who progressed after chemotherapy [23] (Table 1). Another phase III study (CO-AA-302) further confirmed the benefit of abiraterone used in patients with mCPRC before chemotherapy. It improved rPFS and OS (34.7 months vs. 30.3 months) compared with placebo [24] (Table 1). The FDA approved the use of abiraterone in patients with mCRPC post-chemotherapy in 2011, subsequently, pre-chemotherapy based on these two phases III clinical trials in 2012. Furthermore, the FDA further approved the use of abiraterone in patients with high-risk mHSPC based on the phase III clinical trial (LATITUDE study) in 2018 [25,26] (Table 1). Abiraterone plus ADT and prednisolone improved OS and rPFS in patients with mHSPC compared with placebo plus ADT, because the use of abiraterone may cause the miner alocorticoid increase, which will cause fluid edema, liver function impairment, low potassium level, and high blood pressure [23,24,25]. Therefore, abiraterone must be used in combination with steroid, and regular follow-up of liver function and potassium level is necessary [23,24,25]. Previous study indicated that the E3 ubiquitin ligase adaptor speckle-type pox virus and zinc finger (POZ) protein (SPOP) are involved in controlling protein stability of AR by interacting with steroid receptor coactivator 3 (SRC-3) protein and some of the transcriptional coactivators [39]. Wild-type SPOP can promote the SRC-3 protein and then suppress AR transcriptional activity, thus functioning as a potential tumor suppressor [39]. However, some studies identified mutant SPOP in 6–15% of PCa and it can alleviate the tumor suppressive effect [40,41]. Surprisingly, PCa patients with mutant SPOP appear to delay the onset of ADT resistance to 42.0 (95% CI: 25.7–60.8) months. Also, the better outcomes in patients with mutant SPOP treated with abiraterone and enzalutamide were observed [42,43]. Therefore, it implies that SPOP mutation could enhance ADT effect by maintaining AR dependency. Inflammatory response is related to patients treated with ADT. It can cause a IL-6 increase through testosterone suppression [44] and disease progression to CRPC through the activation STAT3 pathway in PCa [45], because IL-6 is known to induce epithelial–mesenchymal transition (EMT) leading to PCa invasion [46]. It is warranted that inflammation factors can be of prognostic value in PCa progression [45].
3. AR Splice Variant-7 (AR-V7) Inhibitors
For mCRPC patients, drug resistance to 2nd-generation AR signaling inhibitors (ARSi), such as abiraterone and enzalutamide is essentially universal in tumor cells that often come with significantly elevated expression of truncated AR splice variant-7 (AR-V7) [47]. Although enzalutamide had a significant effect on CRPC, about 20–40% of patients had no response to the drug. A study showed that AR-V7 was associated with resistance to abiraterone and enzalutamide [48]. Therefore, developing a novel technique for detecting AR-V7 in circulating cells is helpful for the treatment of patients with CRPC [49]. While the expression of AR-V7 was rare in primary PCa (<1%) but common in mCRPC (75%), AR-V7 protein is expressed after primary ADT alone in those CRPC patients, and further increases during 2nd-generation ARSi therapy [50]. Therefore, there is an urgently needed new treatment to reduce the impact of the elevated AR-V7 expression, leading to lethal progression of CRPC. Niclosamide is an anthelminthic drug approved by the FDA; it can decrease the protein expression of AR-V7 in CRPC cells through the ubiquitin–proteasome pathway [51]. Two in vitro studies indicated that niclosamide combined with abiraterone or enzalutamide significantly decreased tumor volume compared to abiraterone or enzalutamide alone, suggesting that niclosamide treatment can restore sensitivity to 2nd-generation ARSi therapy [51,52]. In addition, two types of clinical research trials assess the combination treatment with enzalutamide (Phase I, NCT03123978) or abiraterone (Phase II, NCT02807805) with niclosamide for CRPC patients.
HSP90 is a molecular chaperon essential for the transcriptional activity of the androgen receptor and enhance stability, function, and regulation in the late stage [53,54]. Ferraldeschi et al. demonstrated that the second-generation HSP90 inhibitor, onalespib, can reduce AR-V7 mRNA levels, and not total AR transcript levels [55]. It may be beneficial for patients with PCa expressing AR-V7 and support further research in HSP90 inhibitors in patients resistant to ARSi.
4. PROTAC (Proteolysis Targeting Chimera) Degrader
The development of PROTEC is a new strategy for cancer therapy. PROTEC is composed of a POI (protein of interest) ligand, E3 ubiquitin ligase ligand, and a linker [56,57]. The heterobifunctional molecule can form a complex between the POI and E3 ligase. Then, the E3 will transfer ubiquitin to the surface of the POI. Finally, the proteasome will identify the polyubiquitination signal and degrade the POI [58,59]. Therefore, many AR PROTEC degraders like ARV-110 [58,59,60], ARD-61 [61], ARV-766 (phase I clinical trial, NCT05067140) [60], AR-LDD [60], ARCC-4 [62] are studied if depletion of AR can overcome the drug resistance of PCa. Another estrogen receptor (ER) PROTEC degrader, ARV-471, is also under clinical study for localized advanced or metastatic breast cancer [58] (Phase I/II clinical trial, NCT04072952). Many mutated genes in AR are identified in circulating cells of advanced PCa patients, including L702H0, T878A, H875Y, W742C, W742L, F877L, and T878S [63]. These findings encourage us to further understand the relationship between AR gene mutation and drug resistance. ARV-110 (bavdegalutamide) is a novel, oral PROTAC degrader targeting wild-type and relevant mutant ARs. According to the data of a phase I/II clinical trial reported in the 2022 GU ASCO (American Society of Clinical Oncology Genitourinary Cancers Symposium, San Francisco), ARV-110 lowers 50% of PSA levels in nearly half of patients with AR T878X (T878X = T878A or T878S) or H875Y mutations [60] who have been validated to be drug targets. PSA decline is also observed in patients without AR T878X or H875Y mutations.
5. Radiotherapy
5.1. Bone Target Agent-RADIUM-223 (Ra-223)
Over 90% of patients with mCRPC will eventually develop bony metastatic diseases [27,64], which usually cause mortality, movement disability, and complications. Traditional bone targeting agents like bisphosphonates and denosumab do not reveal benefits in overall survival and only relieve pain and skeletal events. Ra-223 is an a-particle emitter to target a high turnover area of bone [27] by causing DNA breaks, leading to a bystander effect of adjacent tumor suppression [65,66], in which it minimizes the effect to the surrounding healthy tissues, especially bone marrow [66].
A phase III clinical trial (ALSYMPCA) demonstrated that Ra-223 revealed OS benefit in mCRPC patients with symptomatic bony metastasis (14.9 vs. 11.3 months, p < 0.001) [27]. Ra-223 can provide a potent treatment for CRPC patients with bony metastases and elicit less adverse effects, particularly, myelosuppression [27,67] (Table 1). The occurrence rate of grade 3–4 myelosuppression was low, but much higher in a previous docetaxel group compared with a no chemotherapy group [67].
5.2. 177Lu-PSMA
Prostate-specific membrane antigen (PSMA) is a type II transmembrane glycoprotein expressed in the prostate epithelium [68]. It may perform multiple physiological functions including cell migration, nutrition uptake, and signal transduction [68]. PSMA expression increases from benign prostate epithelium to high-grade prostatic intraepithelial neoplasia or adenocarcinoma [69]. Besides, PSMA expression seems to be inversely related to the androgen level [70,71]. The PSMA activity increases in PCa cells lines as cells become more androgen-independent [71], which is different from PSA [71]. The PSMA receptor has the internalization process that can cause endocytosis in the putative ligand into the cell, which allows PSMA-labelled radioisotope to be more concentrated within the cell [72,73]. Due to the above characteristic, it is helpful to develop novel therapeutic methods to target the delivery of drugs, short-range radioisotope, and toxin specifically for mCRPC. The value of PSMA in position-emission tomography-computed tomography (PET/CT) is confirmed by a prospective study of 314 patients. Caroli et al. demonstrated that, in patients with biochemical recurrence of PCa, 68Ga-PSMA PET/CT showed superior performance and safety compared to choline PET/CT [74]. Ideally, the therapeutic radionuclides should match the lesion size/volume to be treated so that the energy can focus on the lesion, rather than the surrounding tissues [73]. 177Lu is a medium-energy b-particle emitter with a maximum energy of 0.5 MeV and relatively short particle tissue range of about 1.5 mm. The shorter b-range of 177Lu provides better irradiation to a relatively small tumor, compared with longer b-range of 90Y [73]. It also has a relatively long physical half-life of 6.73 days [73]. Therefore, these physical activities make 177Lu-PSMA an ideal therapeutic radionuclide that allows the delivery of high energy to target PCa cells. Anti-PSMA radionuclide therapies consist of monoclonal antibodies targeting the extracellular domain of PSMA (177Lu-PSMA-J591) or radiolabeled small molecules targeting the glutamate carboxypeptidase II pocket of PSMA (177Lu-PSMA- 617) [75]. Several studies reported that 177Lu-PSMA-J591, a monoclonal antibody to PSMA, has effective results showing 11.4% to 59.6% of PSA decline [75,76,77,78,79]. However, it also has higher myelosuppression rates and limited treatment response rates compared with studies using PSMA-labelled smaller molecules (177Lu PSMA-617) [80,81]. In addition, in a two-arm phase II study (TheraP study), 200 mCRPC patients were enrolled to compare the antitumor effect between 177Lu-PSMA-617 and cabazitaxel, which showed the better PSA response rates and fewer adverse effects with 177Lu-PSMA-617 monotherapy [82]. Subsequently, a phase III study (VISION study) was designed to explore the clinical benefit of 177Lu-PSMA-617 in mCRPC patients with progressive disease under hormone or chemo-therapy, and the results indicated that 177Lu-PSMA-617 can prolong rPFS and OS of advanced status of mCRPC patients with PSMA-positive expression [28] (Table 1). Notably, the most common adverse events associated with the 177Lu-PSMA-617, such as fatigue, dry mouth, were mild (grade I-II) [28], which promotes 177Lu-PSMA-617 as a new radiotherapeutic for t-CRPC patients. Furthermore, more clinical trials (phase III, NCT04720157 and phase III, NCT04689828) are underway to explore the clinical applicability of 177Lu-PSMA-617 in the early stages of PCa.
6. Immune Therapy
6.1. GM-CSF
Granulocytic-macrophage colony-stimulating factor (GM-CSF) is used as an adjuvant therapy in immunotherapy and has the potential to enhance antitumor efficacy [29]. Sipuleucel-T is the first immunotherapy approved by the FDA [83] (Table 1), which is an autologous dendritic cell therapeutic vaccine designed to enhance the immune T-cell response. It is prepared from peripheral blood mononuclear cells obtained by leukapheresis. These cells are exposed ex vivo to a novel recombinant protein immunogen with prostatic acid phosphatase and human GM-CSF [29]. Nevertheless, the immunologic effects of GF-CSF are not fully understood. Wei et al. demonstrated that GM-CSF can recruit effector T cells into the tumor microenvironment in localized PCa [84]. However, in the phase III trial, PROSTVAC, a viral vector-based immunotherapy which prolonged median overall survival (OS) in mCRPC [85,86], failed to confirm benefit in OS when in combination with GF-CSF [87].
6.2. PD1 Inhibitor (Pembrolizumab)
Programmed death ligand-1 (PD-L1) is expressed in many human tissues including tumor cells and can bind to PD-1, an immune checkpoint inhibitor expressed on T cells. Through the mechanism, tumor cells can escape the immune toxicity. Therefore, PD-1 inhibitors and PD-L1 inhibitors are studied to kill cancer cells via breaking the immune resistance [88,89] (Figure 1).
In a study, it demonstrated that, in treatment with PD-1 inhibition with nivolumab across tumor types including melanoma, non-small-cell lung cancer (NSCL), renal cancer (RCC), CRPC, and colorectal cancer [89], PD-1 inhibitors showed objective responses in approximately one in four to one in five patients with NSCL, melanoma, or RCC [89]. However, no objective responses (i.e., radiographic responses in soft-tissue) were observed in patients with CRPC [88,89].
The five cohorts, open label, phase II trial, KEYNOTE-199 study demonstrated that the objective response rate of pembrolizumab monotherapy was only 5% (95% CI, 2% to 11%) in patients with CRPC who had positive PD-1 expression and 3% (95% CI, <1% to 11%) in those with negative results. Disease control rates was 10% in those with positive PD-1 expression and 9% in those with negative PD-1 expression [90].
Many studies indicated that the prostate tumor microenvironment is highly immunosuppressive [88,91]. One study demonstrated that tumor-infiltrating lymphocytes (TILs) may contribute to PCa progression by inhibiting the activity of T-effector cells [92].
Another study indicated that adenosine produced by prostatic acid phosphatase and TGF-β can contribute to immunosuppression [91]. Therefore, although there are some immunotherapy trials in PCa, they resulted in limited results because of the immunosuppressive mechanism in PCa.
Nevertheless, the FDA approved the use of pembrolizumab for solid tumors expressing mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H) since 2017 [38,93]. The indication included several cancer types, not PCa specifically. It was based on five MSI-H studies involving treatment with pembrolizumab for colorectal cancers (n = 90) or non-colorectal cancers (n = 49) [93]. Among the non-colorectal cancer patients, two were mCRPC. The total objective response was 40% (59/149) [93]. Of the two patients with mCRPC, one achieved partial response, and the other achieved stable condition over nine months [93]. The prevalence of MSI-high(H)/deficient MMR (dMMR) has been observed in approximately 2–3% of cases in PCa among studies [94,95,96]. Mismatch repair (MMR) and microsatellite instability (MSI) are important mechanisms related to cancer progression. Many MMR enzymes (MLH1, MSH2, MSH6 and PMS2) are related to MSI when deficiency is present [97,98]. MMR is a mechanism which can replace and repair the wrong mismatches in daughter DNA strands [99]. On the other hand, the mechanism of microsatellite generation, consisting of repeated sequences of 1–6 nucleotides, can cause DNA slippage in the process of replication, or mismatch of the basic group of slippage strand, resulting in more repeating units missing [97,99].
A retrospective multi-institutional case series study demonstrated that patients with advanced microsatellite instability-high (MSI-H) prostate adenocarcinoma identified with clinical cell-free DNA (cfDNA) sequence testing treated with PD1 inhibitor (pembrolizumab) after two lines of therapy [97]. Of the total 14 participants, 9 CRPC patients have 56% bone, 33% nodal, 11% soft tissues, and 11% liver metastasis and median PSA level 29.3 ng/dL. PSA 50 was defined as PSA level declined ≥50% from baseline prior to treatment. After a median of 9.9 months of treatment, four (44%) in nine patients with mCRPC achieved PSA50 after a median of 4 weeks after treatment initiation, including three patients with >99% PSA decline [97].
The FDA further approved the use of pembrolizumab in patients with unresectable or metastatic tissue tumor mutational burden (tTMB)-high (≥10) tumors that have progressed with previous treatment without satisfactory outcomes since 2020. It was based on a multi-cohort, open-label, non-randomized, phase II KEYNOTE-158 study. It evaluated patients treated with the anti-PD-1 monoclonal antibody pembrolizumab in patients with selected, previously treated, advanced solid tumors [100]. It included unresected or metastatic tumors, 6 of whom had PCa [101]. Objective responses were observed in 30 (29%; 95% CI 21–39) of 102 patients in the tTMB-high group and 43 (6%; 5–8) of 688 in the non-tTMB-high group [100,101].
In addition, some studies demonstrated that mutant SPOP can stabilize programmed death ligand 1 (PD-L1) protein expression via proteasome-mediated degradation and improve PCa treatment outcome on programmed death 1 (PD-1) immune checkpoint inhibitors [102,103].
7. Chimeric Antigen Receptor (CAR) T-Cells
The recent development of biological engineering techniques has made a significant improvement in overcoming the immune-evasiveness of cancer cells. Clinically, CAR-T cell therapy is the first to be applied on several hematological malignancies [104], which is believed to be the same target antigens applicable for other somatic cancers [105]. However, the physical barriers such as tumor microenvironment of solid tumors probably account for the difficulties in obtaining the same promising results [105]. Nevertheless, PSMA and PSCA are the most important candidates for CAR-T cells targeted antigens in CRPC [105]. The process begins from T-cell collection through leukapheresis. T cells are genetically altered to express CAR which can target tumor-associated antigens (TAA) [106]. Lymphodepletion is usually performed before injection, which can cause CAR-T cells lymphopenia and more suitable to the tumor microenvironment [107]. Finally, purified CAR-T cells are administrated back to patients [106] (Figure 1). Different strategies are developed to create CAR-T cells. Comparing with autologous CAR-T cells, allogeneic CAR-T cells appear to be less expensive, more efficient from a well-established standardized protocol [108]. PSMA-targeted CAR-T cell is superior to other TAA CAR-T therapies for more easily monitored by the 68Ga-PET/CT examination [109,110,111].
Until now, two anti-PSMA CAR-T trials have been reported. In the clinical trial (NCT00664196) of the first generation of anti-PSMA CAR-T-cells therapy, PSA decline in 50% and 70% was found in two patients, but three other patients experienced disease progression [110]. The other clinical trial (NCT01140373) of the second-generation anti-PSMA CAR-T-cells therapy showed promising outcomes: 50% of patients of the first cohort showed no radiological progression over 6 months, and the other half of the patients were stable over 16 months. Three patients of the second cohort developed mild cytokine release syndrome that was self-resolving [111]. Based on this outcome, many clinical trials of anti-PSMA CART-T cells are underway [105,106]. P-PSMA-101 CAR-T cells are autologous purified CART-T cells developed through a novel technique. During manufacturing, the genes are inserted in a DHFR selection gene, anti-PSMA centyrin CAR gene and iCASP-9-based safety switch to purify CAR-T cells. They are characterized by a lot of memory stem T cells [112]. In 2022 GU ASCO data, P-PSMA-101 CAR-T cells demonstrated a significant antitumor effect in patients with mCRPC (clinical trial NCT04249947). Seven of ten heavily pre-treated patients with mCRPC achieved a PSA decrease in the preliminary report [112]. PSMA-targeting TGF-β-insensitive armored CAR-T cells are designed to overcome the suppressive immune microenvironment of PCa [113,114,115]. In phase I clinical trials (NCT03089203, NCT04227275), the preliminary results showed that TGF-β-resistant CAR-T cells are safe and feasible in patients with mCRPC [113,116], and further results are expected to unveil the drug distribution and disease response.
Prostate Stem Cell Antigen (PSCA) is highly expressed in PCa tissues. Although some pre-clinical trials showed that tumors can escape PSCA CAR-T cells [117], many clinical trials of anti-PSCA CAR-T cells, such as phase I study (NCT03873805) to examine the efficacy of PSCA-specific CAR-T cells in patients with PSCA-positive mCRPC [118] and clinical trial (NCT02744287) to study the safety and tolerable dose in patients with PSCA-positive CRPC or pancreatic cancer [119], are still in progress.
8. Targeted Therapies
8.1. Polyadenosine Diphosphate Ribose Polymerase (PARP) Inhibitors
PCa is known as a multiple-focal disease involving abnormalities in a variety of growth factor signaling pathways and aberrations in DNA damage repair pathways [120]. The analysis of germline mutations revealed that approximately 11.8% of mPCa patients harbor mutations in genes-related DNA-repair processes, including BRCA2, ATM, CHEK2 and BRCA1 [121]. Another study reported that an even higher percentage (27%) of PCa patients with local or metastatic disease harbor a germline or somatic alteration in the DNA repair gene [120]. Repair of strand breaks by homologous recombination (high-fidelity) and non-homologous (low fidelity) end-joining are two important mechanisms [122,123] that help cells repair from double-strand breaks, which are very hazardous DNA damage in cells.
PARP is a kind of enzyme that helps repair DNA damage in cells. It is essential for the repair of single-strand DNA breaks via the base excision repair pathway, which is a primary repair pathway for DNA single-strand breaks [124,125]. PARylation or poly-ADP ribosylation is the process by which PARP1 and PARP2 enzymes can sense single-strand DNA breaks and recruit DNA repair complexes to the site in the nucleus and result in post-translational modification of the DNA [124].
PARP inhibitors can block this PARylation, and they may also trap the PARP enzymes on injured DNA, preventing binding of incoming repair proteins [124]. The trapped PARP-DNA complexes are more cytotoxic than unrepaired single-strand breaks caused by PARP inactivation alone [126] (Figure 1).
8.2. Olaparib
The phase II trials demonstrated that germline and somatic mutations in homologous recombination repair (HRR) genes are predictive of the clinical benefit of PARP inhibition in PCa [127]. These genes include BRCA1/2, ATM, Fanconi’s anemia genes, and CHEK2 [127]. It showed that patients who had no response to standard treatment including enzalutamide, abiraterone or cabazitaxel and had DNA repair genes defect will get a high response rate to the PARP inhibitor (Olaparib) [127]. In a randomized, open-label (PROfound), phase III trial of olaparib demonstrated the benefit of disease progression-free survival rate in mCRPC patients who received a new hormonal agent (e.g., enzalutamide or abiraterone) and carried alterations in genes involved in HRR [30] (Table 1). The FDA approved the use of Olaparib in 2020 for patients with mCRPC with at least one germline or somatic mutation in HRR genes (BRCA1, BRCA2, ATM, BARD1, BRIP1, CDK12, CHEK1, CHEK2, FANCL, PALB2, RAD51B, RAD51C, RAD51D, or RAD54L) and who have previously received enzalutamide or abiraterone [93].
In a phase II study, olaparib in combination with abiraterone exhibited significant clinical efficacy benefits for patients with mCRPC compared with abiraterone alone [128]. Furthermore, this combination therapy clearly demonstrated a significant improvement in rPFS compared to abiraterone alone (24.8 vs. 16.6 months p < 0.0001) from a phase III clinical trial (PROpel study) that enrolled newly diagnosed mCRPC patients regardless of the HRR status [129]. Thus, this combination therapy is expected to provide potential therapeutic benefits for mCRPC patients in the future [129].
In addition, some studies indicated that mutant SPOP can deregulate DNA double-strand break (DSB) repair by promoting the error-prone non-homologous end-joining (NHEJ) pathway, like the breast cancer gene 1 (BRCA1) effect and increase the sensitivity of PCa cells to the PARP inhibitor [130]. The therapy outcomes are best for mutant SPOP patients without other (TP53, homologous recombination deficiency (HRD) pathway and PI3K/AKT pathway) concurrent mutations [43].
8.3. Rucaparib
Rucaparib is the second PARP inhibitor which the FDA approved for the use of mCRPC [93]. In a phase II trial (TRITON2), it evaluated 115 patients with a BRCA alteration with or without measurable disease and demonstrated primary end points with an objective response rate of 43.5% (95% CI, 31.0% to 56.7%; 27 of 62 patients). The most treatment-related adverse effect was anemia [31] (Table 1).
A phase III (TRITON3) study of PARP inhibitor rucaparib vs. the physician’s choice of therapy (abiraterone, enzalutamide, and docetaxel) for patients with mCRPC associated with homologous recombination deficiency (HRD) who have previously been treated with novel hormone agents and the results are pending [32] (Table 1).
8.4. Niraparib
Niraparib is a potent inhibitor of PARP-1 and PARP-2. In the phase III clinical trial (MAGNITUDE study), niraparib combined with abiraterone significantly improves rPFS, time to PSA progression and time to cytoloxic in patients with HRR-positive mCRPC [131]. For patients in the HRR-negative group, no clinical benefit has been observed. Thus, the study warrants the importance of genetic testing for achieving the therapeutic efficacy benefit of combination therapy.
8.5. Talazoparib
Talazoparib is a FDA-approved PARP inhibitor for BRCA-mutated, HER2-negative locally advanced or metastatic breast cancer. Currently, another phase I clinical trial (NCT 04703920) is ongoing to study the safety and tolerable dose of talazoparib in combination with belinostat for metastatic breast cancer, mCRPC, and metastatic ovarian cancer [132].
9. Phosphatidylinositol-3-Kinase (PI3K)/AKT Inhibitor
The PI3K/AKT/mTOR pathway is an important mutated pathway in PCa and tumor suppressor phosphate and tensin homolog (PTEN) is the most important negative regulator in this pathway [133,134,135]. Many studies indicated that loss of PTEN may be related to poor prognosis of PCa [133,134,136]. PTEN loss can activate the pathway of the PI3K/AKT/mTOR pathway and regulate the AR transcriptional output associated with hormonal resistance [137,138] (Figure 1). Loss of PTEN expression also demonstrated poor survival response in patients with CRPC to abiraterone [138] and resistance to PARP inhibitor [75]. Therefore, a combination with the PI3K/AKT pathway inhibitor and the PARP-inhibitor is currently a new way to overcome the resistance [139]. In the phase III clinical trial (IPATential150), the ipatasertib (AKT inhibitor) plus abiraterone group significantly improved the rPFS of the patients with mCRPC with PTEN loss compared to the placebo plus abiraterone group (18.5 vs. 16.5 months p = 0.034) [140]. Although the combination therapy failed to show significant improvement of rPFS in the intention-to-treat population, this trial does support the role of PTEN status in determining targeted therapeutic strategy.
10. Aurora Kinase Inhibitor
Alisertib
Beltran et al. indicated that the oncogenic transcriptional factor N-Myc and cell cycle kinase Aurora kinase A (AURKA) are overexpressed in most metastatic neuroendocrine PCa (mNEPC), a subset of CRPC [141] (Figure 1). This study demonstrated that alteration of N-Myc and AURKA are involved in the development of NEPC and Aurora kinase inhibitor shows benefits for NEPC. The AURKA inhibitor, alisertib, disrupts the interaction between the N-Myc-Aurora A protein complex and inhibits N-Myc signaling tumor growth [142]. In a phase I study (NCT01094288), alisertib combined with docetaxel demonstrated antitumor activity. Six of the eighteen patients with CRPC had partial responses [143]. A single-arm, multi-institutional open-label phase II clinical trial (NCT01799278) showed that a subset of patients with advanced PCa (CRPC or NEPC) with molecular features in favor of Aurora-A and N-myc activation achieved significant benefits from a single agent with alisertib [144]. The inclusion criteria of the trial contained patients with metastatic PCa and at least (1) small-cell neuroendocrine morphology, (2) more than 50% neuroendocrine marker expression, (3) development of liver metastasis without PSA progression, or (4) elevated serum neuroendocrine marker [144]. In the molecular analysis, AURKA amplification was associated with OS improvement (p = 0.05) in alisertib but no difference in PFS (p = 0.4). Although N-myc amplification was not associated with outcomes, the responders still showed correlation with MYCN overactivity [144]. However, in another phase I/II study (NCT01848067), combination therapy with alisertib did not reveal significant benefits in patients with CRPC progressing on abiraterone [145].
11. MEK Inhibitor
Trametinib
NEPC is associated with being highly aggressive and associated with EMT and neuroendocrine transdifferentiation (NEtD) [146,147]. Clinically, EMT induction and mesenchymal characteristics are associated with high Gleason grade, biological recurrence and visceral metastasis [8]. NEtD is an important route and the development of targeted therapeutics, which can reverse the molecular and phenotypes traits, may be a possible therapy. Cells transdifferentiate into the neuroendocrine phenotypes such as low AR activity, high cellular plasticity drivers [(Axl, mitogen-activated protein kinase (MEK), AURKA, Brachyury)], high-grade, and low PSA [146] (Figure 1). A phase II clinical trial (NCT02881242) of trametinib, a MEK1/2 inhibitor, is currently ongoing for patients with refractory metastatic PCa [148].
12. Histone Deacetylase Inhibitors (HDAC Inhibitors)
Epigenetic aberrations are known to cause cancer development [149,150,151]. Histone protein balance is controlled by histone acetyl transferases (HATs) and histone deacetylases (HDACs) [152,153] (Figure 1). The change of the histone protein balance influences many genes including oncogenes, tumor suppressor genes, and DNA repair genes [152,153]. Therefore, abnormal HDACs expression is related to the development of cancer [154]. Overexpression of HDAC1, 2 and 3 has been reported in PCa [155,156], and many HDAC inhibitors have been designed for PCa [157,158]. HDAC inhibitors demonstrated promising results in hematological malignancies and the FDA-approved suberoylanilide hydroxamic acid (SAHA, vorinostat) for the treatment of cutaneous T-cell lymphoma in 2006 [159]. However, four HDAC inhibitors (vorinostat, pracinostat, panobinostat and romidepsin) failed in phase II clinical trials for CRPC because of drug toxicity and disease progression [160]. Nevertheless, further investigation for more specific HDAC inhibitors targeting HDAC subtypes still can be used as a promising PCa therapy.
13. SPHK1/S1PRs Inhibitors
It has been found that sphingolipid metabolites are involved in the development of many cancers. Sphingosine is phosphorylated by SPHK1 (Sphingosine kinase type 1) and then becomes sphingosine-1-phosphate (S1P). The S1P is able to bind on the S1P receptors 1, 2, 3, 4, and 5 (S1PRs) for further signaling transduction, including ERK1/2, PI3K/AKT, NF-κB, STATs, Rho/ROCK, and RAS [161]. It also has been found that SPHK1/S1PRs signaling promotes cancer cell motility, angiogenesis, survival, and proliferation [162]. Currently, many cancer studies demonstrate that SPHK1/S1PRs inhibitors, such as MP-A08, SKI-I, SKI-II, FTY720, LCL146, LCL351, SLP7111228 and B5354c, are able to suppress cancer cell proliferation or apoptosis induction in breast cancer, bladder cancer, leukemia cells, and PCa [163,164,165]. Also, recent studies demonstrate that SPHK1/S1PRs-targeting treatment can have a significant impact on PCa cell growth [166], angiogenesis [167], chemotherapy resistance [164,165,168,169,170], radiotherapy resistance [171], migration and invasion [172]. Notably, elevated SPHK1 activity is detected in PCa specimens as compared to normal tissues, suggesting the clinical prevalence of SPHK1/S1PRs in PCa development [173].
Our recent study indicates the critical role of the SPHK1/S1PRs pathway in PCa cell migration and invasion via matriptase regulation [172]. Furthermore, the SPHK1/S1PRs pathway is involved in neuroendocrine PCa development through REST degradation [174]. In these studies, fingolimod (FTY720), an FDA-approved SPHK1 inhibitor (Figure 1) for treating multiple sclerosis [175], shows significant therapeutic efficacy in clinically relevant NEPC xenograft models, supporting the future clinical translation of targeted therapeutics for NEPC.
14. PTP1B Inhibitors
In recent years, the protein tyrosine phosphatase 1B (PTP1B; also known as PTPN1) has emerged as a critical regulator of multiple signaling networks involved in human disorders, such as obesity [176], diabetes [177], and cancers [178]. Moreover, several studies point toward PTP1B serving as a potential therapeutic target in various tumors, such as PCa [179], pancreatic cancer [180], ovarian cancer [181], colon cancer [182] and breast cancer [183]. Wu et al. indicated that PTP1B elevation was detected in neuroendocrine differentiation in PCa specimens [184]. Also, one study suggested that PTP1B deletion or inhibition (PTP1B inhibitor; MSI-1436) could enhance T-cell antitumor activity and improve the therapeutic efficacy of chimeric antigen receptor (CAR) T cells in solid tumors [185] (Figure 1). Generally, the accumulative evidence suggested that PTP1B may serve as a promising therapeutic target for t-CRPC treatment.
15. Conclusions
Despite the fact that the introduction of several advanced therapeutic innovations has shown to improve survival and reduce morbidity and mortality of mCRPC, the onset of t-CRPC imposes a new challenging for curing PCa. Based on the molecular characterizations of subpopulations of t-CRPC, a variety of new agents such as genetically targeted agents, specific small-molecule inhibitors, and immune therapies are underway to explore the precision medicine treatment for individual PCa patients.
Acknowledgments
We thank Rachel Pong’s editorial assistance.
Author Contributions
J.-T.H., C.-H.L. and H.L. conceived the idea; B.-R.W., Y.-A.C. and W.-H.K. wrote the manuscript. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Fellowship program of Ministry of National Defense-Medical Affairs Bureau in Taiwan (to B.-R.W.) and the Ministry of Science and Technology in Taiwan (MOST108-2911-I-005-509 and MOST 110-2926-I-005-502 to H.L.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Taylor B.S., Schultz N., Hieronymus H., Gopalan A., Xiao Y., Carver B.S., Arora V.K., Kaushik P., Cerami E., Reva B., et al. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010;18:11–22. doi: 10.1016/j.ccr.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shafi A.A., Yen A.E., Weigel N.L. Androgen receptors in hormone-dependent and castration-resistant prostate cancer. Pharmacol. Ther. 2013;140:223–238. doi: 10.1016/j.pharmthera.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 3.Gravis G. Systemic treatment for metastatic prostate cancer. Asian J. Urol. 2019;6:162–168. doi: 10.1016/j.ajur.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Virgo K.S., Basch E., Loblaw D.A., Oliver T.K., Rumble R.B., Carducci M.A., Nordquist L., Taplin M.E., Winquist E., Singer E.A. Second-Line Hormonal Therapy for Men with Chemotherapy-Naïve, Castration-Resistant Prostate Cancer: American Society of Clinical Oncology Provisional Clinical Opinion. J. Clin. Oncol. 2017;35:1952–1964. doi: 10.1200/JCO.2017.72.8030. [DOI] [PubMed] [Google Scholar]
- 5.Ritch C.R., Cookson M.S. Advances in the management of castration resistant prostate cancer. Bmj. 2016;355:i4405. doi: 10.1136/bmj.i4405. [DOI] [PubMed] [Google Scholar]
- 6.Conteduca V., Aieta M., Amadori D., De Giorgi U. Neuroendocrine differentiation in prostate cancer: Current and emerging therapy strategies. Crit. Rev. Oncol. Hematol. 2014;92:11–24. doi: 10.1016/j.critrevonc.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Santoni M., Conti A., Burattini L., Berardi R., Scarpelli M., Cheng L., Lopez-Beltran A., Cascinu S., Montironi R. Neuroendocrine differentiation in prostate cancer: Novel morphological insights and future therapeutic perspectives. Biochim. Biophys. Acta. 2014;1846:630–637. doi: 10.1016/j.bbcan.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Parimi V., Goyal R., Poropatich K., Yang X.J. Neuroendocrine differentiation of prostate cancer: A review. Am. J. Clin. Exp. Urol. 2014;2:273–285. [PMC free article] [PubMed] [Google Scholar]
- 9.Grigore A.D., Ben-Jacob E., Farach-Carson M.C. Prostate cancer and neuroendocrine differentiation: More neuronal, less endocrine? Front. Oncol. 2015;5:37. doi: 10.3389/fonc.2015.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grobholz R., Griebe M., Sauer C.G., Michel M.S., Trojan L., Bleyl U. Influence of neuroendocrine tumor cells on proliferation in prostatic carcinoma. Hum. Pathol. 2005;36:562–570. doi: 10.1016/j.humpath.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 11.Tran C., Ouk S., Clegg N.J., Chen Y., Watson P.A., Arora V., Wongvipat J., Smith-Jones P.M., Yoo D., Kwon A., et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324:787–790. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heidegger I., Brandt M.P., Heck M.M. Treatment of non-metastatic castration resistant prostate cancer in 2020: What is the best? Urol. Oncol. 2020;38:129–136. doi: 10.1016/j.urolonc.2019.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Fizazi K., Scher H.I., Miller K., Basch E., Sternberg C.N., Cella D., Forer D., Hirmand M., de Bono J.S. Effect of enzalutamide on time to first skeletal-related event, pain, and quality of life in men with castration-resistant prostate cancer: Results from the randomised, phase 3 AFFIRM trial. Lancet Oncol. 2014;15:1147–1156. doi: 10.1016/S1470-2045(14)70303-1. [DOI] [PubMed] [Google Scholar]
- 14.Scher H.I., Fizazi K., Saad F., Taplin M.E., Sternberg C.N., Miller K., de Wit R., Mulders P., Chi K.N., Shore N.D., et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 2012;367:1187–1197. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 15.Beer T.M., Armstrong A.J., Rathkopf D., Loriot Y., Sternberg C.N., Higano C.S., Iversen P., Evans C.P., Kim C.S., Kimura G., et al. Enzalutamide in Men with Chemotherapy-naïve Metastatic Castration-resistant Prostate Cancer: Extended Analysis of the Phase 3 PREVAIL Study. Eur. Urol. 2017;71:151–154. doi: 10.1016/j.eururo.2016.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beer T.M., Armstrong A.J., Rathkopf D.E., Loriot Y., Sternberg C.N., Higano C.S., Iversen P., Bhattacharya S., Carles J., Chowdhury S., et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N. Engl. J. Med. 2014;371:424–433. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hussain M., Fizazi K., Saad F., Rathenborg P., Shore N., Ferreira U., Ivashchenko P., Demirhan E., Modelska K., Phung D., et al. Enzalutamide in Men with Nonmetastatic, Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2018;378:2465–2474. doi: 10.1056/NEJMoa1800536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis I.D., Martin A.J., Stockler M.R., Begbie S., Chi K.N., Chowdhury S., Coskinas X., Frydenberg M., Hague W.E., Horvath L.G., et al. Enzalutamide with Standard First-Line Therapy in Metastatic Prostate Cancer. N. Engl. J. Med. 2019;381:121–131. doi: 10.1056/NEJMoa1903835. [DOI] [PubMed] [Google Scholar]
- 19.Armstrong A.J., Szmulewitz R.Z., Petrylak D.P., Holzbeierlein J., Villers A., Azad A., Alcaraz A., Alekseev B., Iguchi T., Shore N.D., et al. ARCHES: A Randomized, Phase III Study of Androgen Deprivation Therapy with Enzalutamide or Placebo in Men With Metastatic Hormone-Sensitive Prostate Cancer. J. Clin. Oncol. 2019;37:2974–2986. doi: 10.1200/JCO.19.00799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith M.R., Saad F., Chowdhury S., Oudard S., Hadaschik B.A., Graff J.N., Olmos D., Mainwaring P.N., Lee J.Y., Uemura H., et al. Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer. N. Engl. J. Med. 2018;378:1408–1418. doi: 10.1056/NEJMoa1715546. [DOI] [PubMed] [Google Scholar]
- 21.Chi K.N., Agarwal N., Bjartell A., Chung B.H., Pereira de Santana Gomes A.J., Given R., Juárez Soto Á., Merseburger A.S., Özgüroğlu M., Uemura H., et al. Apalutamide for Metastatic, Castration-Sensitive Prostate Cancer. N. Engl. J. Med. 2019;381:13–24. doi: 10.1056/NEJMoa1903307. [DOI] [PubMed] [Google Scholar]
- 22.Fizazi K., Shore N., Tammela T.L., Ulys A., Vjaters E., Polyakov S., Jievaltas M., Luz M., Alekseev B., Kuss I., et al. Darolutamide in Nonmetastatic, Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2019;380:1235–1246. doi: 10.1056/NEJMoa1815671. [DOI] [PubMed] [Google Scholar]
- 23.Fizazi K., Scher H.I., Molina A., Logothetis C.J., Chi K.N., Jones R.J., Staffurth J.N., North S., Vogelzang N.J., Saad F., et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: Final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13:983–992. doi: 10.1016/S1470-2045(12)70379-0. [DOI] [PubMed] [Google Scholar]
- 24.Ryan C.J., Smith M.R., Fizazi K., Saad F., Mulders P.F., Sternberg C.N., Miller K., Logothetis C.J., Shore N.D., Small E.J., et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): Final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16:152–160. doi: 10.1016/S1470-2045(14)71205-7. [DOI] [PubMed] [Google Scholar]
- 25.Fizazi K., Tran N., Fein L., Matsubara N., Rodriguez-Antolin A., Alekseev B.Y., Özgüroğlu M., Ye D., Feyerabend S., Protheroe A., et al. Abiraterone plus Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. N. Engl. J. Med. 2017;377:352–360. doi: 10.1056/NEJMoa1704174. [DOI] [PubMed] [Google Scholar]
- 26.Fizazi K., Tran N., Fein L., Matsubara N., Rodriguez-Antolin A., Alekseev B.Y., Özgüroğlu M., Ye D., Feyerabend S., Protheroe A., et al. Abiraterone acetate plus prednisone in patients with newly diagnosed high-risk metastatic castration-sensitive prostate cancer (LATITUDE): Final overall survival analysis of a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019;20:686–700. doi: 10.1016/S1470-2045(19)30082-8. [DOI] [PubMed] [Google Scholar]
- 27.Parker C., Nilsson S., Heinrich D., Helle S.I., O’Sullivan J.M., Fosså S.D., Chodacki A., Wiechno P., Logue J., Seke M., et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N. Engl. J. Med. 2013;369:213–223. doi: 10.1056/NEJMoa1213755. [DOI] [PubMed] [Google Scholar]
- 28.Sartor O., de Bono J., Chi K.N., Fizazi K., Herrmann K., Rahbar K., Tagawa S.T., Nordquist L.T., Vaishampayan N., El-Haddad G., et al. Lutetium-177-PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2021;385:1091–1103. doi: 10.1056/NEJMoa2107322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kantoff P.W., Higano C.S., Shore N.D., Berger E.R., Small E.J., Penson D.F., Redfern C.H., Ferrari A.C., Dreicer R., Sims R.B., et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med. 2010;363:411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 30.de Bono J., Mateo J., Fizazi K., Saad F., Shore N., Sandhu S., Chi K.N., Sartor O., Agarwal N., Olmos D., et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2020;382:2091–2102. doi: 10.1056/NEJMoa1911440. [DOI] [PubMed] [Google Scholar]
- 31.Abida W., Patnaik A., Campbell D., Shapiro J., Bryce A.H., McDermott R., Sautois B., Vogelzang N.J., Bambury R.M., Voog E., et al. Rucaparib in Men with Metastatic Castration-Resistant Prostate Cancer Harboring a BRCA1 or BRCA2 Gene Alteration. J. Clin. Oncol. 2020;38:3763–3772. doi: 10.1200/JCO.20.01035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.A Study of Rucaparib Versus Physician’s Choice of Therapy in Patients with Metastatic Castration-Resistant Prostate Cancer and Homologous Recombination Gene Deficiency (TRITON3) [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02975934?term=TRITON3&draw=2&rank=1.
- 33.Moilanen A.M., Riikonen R., Oksala R., Ravanti L., Aho E., Wohlfahrt G., Nykänen P.S., Törmäkangas O.P., Palvimo J.J., Kallio P.J. Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci. Rep. 2015;5:12007. doi: 10.1038/srep12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith M.R., Hussain M., Saad F., Fizazi K., Sternberg C.N., Crawford E.D., Kopyltsov E., Park C.H., Alekseev B., Montesa-Pino Á., et al. Darolutamide and Survival in Metastatic, Hormone-Sensitive Prostate Cancer. N. Engl. J. Med. 2022;386:1132–1142. doi: 10.1056/NEJMoa2119115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barrie S.E., Haynes B.P., Potter G.A., Chan F.C., Goddard P.M., Dowsett M., Jarman M. Biochemistry and pharmacokinetics of potent non-steroidal cytochrome P450(17alpha) inhibitors. J. Steroid. Biochem. Mol. Biol. 1997;60:347–351. doi: 10.1016/S0960-0760(96)00225-7. [DOI] [PubMed] [Google Scholar]
- 36.Ryan C.J., Smith M.R., de Bono J.S., Molina A., Logothetis C.J., de Souza P., Fizazi K., Mainwaring P., Piulats J.M., Ng S., et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N. Engl. J. Med. 2013;368:138–148. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Molina A., Belldegrun A. Novel therapeutic strategies for castration resistant prostate cancer: Inhibition of persistent androgen production and androgen receptor mediated signaling. J. Urol. 2011;185:787–794. doi: 10.1016/j.juro.2010.10.042. [DOI] [PubMed] [Google Scholar]
- 38.Naseer F., Ahmad T., Kousar K., Anjum S. Advanced Therapeutic Options for Treatment of Metastatic Castration Resistant Prostatic Adenocarcinoma. Front. Pharmacol. 2021;12:728054. doi: 10.3389/fphar.2021.728054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geng C., He B., Xu L., Barbieri C.E., Eedunuri V.K., Chew S.A., Zimmermann M., Bond R., Shou J., Li C., et al. Prostate cancer-associated mutations in speckle-type POZ protein (SPOP) regulate steroid receptor coactivator 3 protein turnover. Proc. Natl. Acad. Sci. USA. 2013;110:6997–7002. doi: 10.1073/pnas.1304502110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barbieri C.E., Baca S.C., Lawrence M.S., Demichelis F., Blattner M., Theurillat J.P., White T.A., Stojanov P., Van Allen E., Stransky N., et al. Exome sequencing identifies recurrent SPOP, FOXA1 and MED12 mutations in prostate cancer. Nat. Genet. 2012;44:685–689. doi: 10.1038/ng.2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blattner M., Lee D.J., O’Reilly C., Park K., MacDonald T.Y., Khani F., Turner K.R., Chiu Y.L., Wild P.J., Dolgalev I., et al. SPOP mutations in prostate cancer across demographically diverse patient cohorts. Neoplasia. 2014;16:14–20. doi: 10.1593/neo.131704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karantanos T., Corn P.G., Thompson T.C. Prostate cancer progression after androgen deprivation therapy: Mechanisms of castrate resistance and novel therapeutic approaches. Oncogene. 2013;32:5501–5511. doi: 10.1038/onc.2013.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nakazawa M., Fang M., Marshall C.H., Lotan T.L., Isaacsson Velho P., Antonarakis E.S. Clinical and genomic features of SPOP-mutant prostate cancer. Prostate. 2022;82:260–268. doi: 10.1002/pros.24269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoogland A.I., Jim H.S.L., Gonzalez B.D., Small B.J., Gilvary D., Breen E.C., Bower J.E., Fishman M., Zachariah B., Jacobsen P.B. Systemic inflammation and symptomatology in patients with prostate cancer treated with androgen deprivation therapy: Preliminary findings. Cancer. 2021;127:1476–1482. doi: 10.1002/cncr.33397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sciarra A., Gentilucci A., Salciccia S., Pierella F., Del Bianco F., Gentile V., Silvestri I., Cattarino S. Prognostic value of inflammation in prostate cancer progression and response to therapeutic: A critical review. J. Inflamm. 2016;13:35. doi: 10.1186/s12950-016-0143-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nguyen D.P., Li J., Tewari A.K. Inflammation and prostate cancer: The role of interleukin 6 (IL-6) BJU Int. 2014;113:986–992. doi: 10.1111/bju.12452. [DOI] [PubMed] [Google Scholar]
- 47.Del Re M., Conteduca V., Crucitta S., Gurioli G., Casadei C., Restante G., Schepisi G., Lolli C., Cucchiara F., Danesi R., et al. Androgen receptor gain in circulating free DNA and splicing variant 7 in exosomes predict clinical outcome in CRPC patients treated with abiraterone and enzalutamide. Prostate Cancer Prostatic. Dis. 2021;24:524–531. doi: 10.1038/s41391-020-00309-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Antonarakis E.S., Lu C., Wang H., Luber B., Nakazawa M., Roeser J.C., Chen Y., Mohammad T.A., Chen Y., Fedor H.L., et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl. J. Med. 2014;371:1028–1038. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hille C., Gorges T.M., Riethdorf S., Mazel M., Steuber T., Amsberg G.V., König F., Peine S., Alix-Panabières C., Pantel K. Detection of Androgen Receptor Variant 7 (ARV7) mRNA Levels in EpCAM-Enriched CTC Fractions for Monitoring Response to Androgen Targeting Therapies in Prostate Cancer. Cells. 2019;8:1067. doi: 10.3390/cells8091067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharp A., Coleman I., Yuan W., Sprenger C., Dolling D., Rodrigues D.N., Russo J.W., Figueiredo I., Bertan C., Seed G., et al. Androgen receptor splice variant-7 expression emerges with castration resistance in prostate cancer. J. Clin. Investig. 2019;129:192–208. doi: 10.1172/JCI122819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu C., Lou W., Zhu Y., Nadiminty N., Schwartz C.T., Evans C.P., Gao A.C. Niclosamide inhibits androgen receptor variants expression and overcomes enzalutamide resistance in castration-resistant prostate cancer. Clin. Cancer Res. 2014;20:3198–3210. doi: 10.1158/1078-0432.CCR-13-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu C., Armstrong C., Zhu Y., Lou W., Gao A.C. Niclosamide enhances abiraterone treatment via inhibition of androgen receptor variants in castration resistant prostate cancer. Oncotarget. 2016;7:32210–32220. doi: 10.18632/oncotarget.8493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Georget V., Térouanne B., Nicolas J.C., Sultan C. Mechanism of antiandrogen action: Key role of hsp90 in conformational change and transcriptional activity of the androgen receptor. Biochemistry. 2002;41:11824–11831. doi: 10.1021/bi0259150. [DOI] [PubMed] [Google Scholar]
- 54.Kirschke E., Goswami D., Southworth D., Griffin P.R., Agard D.A. Glucocorticoid receptor function regulated by coordinated action of the Hsp90 and Hsp70 chaperone cycles. Cell. 2014;157:1685–1697. doi: 10.1016/j.cell.2014.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferraldeschi R., Welti J., Powers M.V., Yuan W., Smyth T., Seed G., Riisnaes R., Hedayat S., Wang H., Crespo M., et al. Second-Generation HSP90 Inhibitor Onalespib Blocks mRNA Splicing of Androgen Receptor Variant 7 in Prostate Cancer Cells. Cancer Res. 2016;76:2731–2742. doi: 10.1158/0008-5472.CAN-15-2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Potjewyd F., Turner A.W., Beri J., Rectenwald J.M., Norris-Drouin J.L., Cholensky S.H., Margolis D.M., Pearce K.H., Herring L.E., James L.I. Degradation of Polycomb Repressive Complex 2 with an EED-Targeted Bivalent Chemical Degrader. Cell Chem. Biol. 2020;27:47–56. doi: 10.1016/j.chembiol.2019.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salami J., Crews C.M. Waste disposal-An attractive strategy for cancer therapy. Science. 2017;355:1163–1167. doi: 10.1126/science.aam7340. [DOI] [PubMed] [Google Scholar]
- 58.Qi S.M., Dong J., Xu Z.Y., Cheng X.D., Zhang W.D., Qin J.J. PROTAC: An Effective Targeted Protein Degradation Strategy for Cancer Therapy. Front. Pharmacol. 2021;12:692574. doi: 10.3389/fphar.2021.692574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zeng S., Huang W., Zheng X., Liyan C., Zhang Z., Wang J., Shen Z. Proteolysis targeting chimera (PROTAC) in drug discovery paradigm: Recent progress and future challenges. Eur. J. Med. Chem. 2021;210:112981. doi: 10.1016/j.ejmech.2020.112981. [DOI] [PubMed] [Google Scholar]
- 60.PROTAC Shrinks Mutated Prostate Tumors. Cancer Discov. 2022;12:Of2. doi: 10.1158/2159-8290.CD-NB2022-0020. [DOI] [PubMed] [Google Scholar]
- 61.Kregel S., Wang C., Han X., Xiao L., Fernandez-Salas E., Bawa P., McCollum B.L., Wilder-Romans K., Apel I.J., Cao X., et al. Androgen receptor degraders overcome common resistance mechanisms developed during prostate cancer treatment. Neoplasia. 2020;22:111–119. doi: 10.1016/j.neo.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Salami J., Alabi S., Willard R.R., Vitale N.J., Wang J., Dong H., Jin M., McDonnell D.P., Crew A.P., Neklesa T.K., et al. Androgen receptor degradation by the proteolysis-targeting chimera ARCC-4 outperforms enzalutamide in cellular models of prostate cancer drug resistance. Commun. Biol. 2018;1:100. doi: 10.1038/s42003-018-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ledet E.M., Lilly M.B., Sonpavde G., Lin E., Nussenzveig R.H., Barata P.C., Yandell M., Nagy R.J., Kiedrowski L., Agarwal N., et al. Comprehensive Analysis of AR Alterations in Circulating Tumor DNA from Patients with Advanced Prostate Cancer. Oncologist. 2020;25:327–333. doi: 10.1634/theoncologist.2019-0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roodman G.D. Mechanisms of bone metastasis. N. Engl. J. Med. 2004;350:1655–1664. doi: 10.1056/NEJMra030831. [DOI] [PubMed] [Google Scholar]
- 65.Lewington V.J. Bone-seeking radionuclides for therapy. J. Nucl. Med. 2005;46((Suppl. S1)):38s–47s. [PubMed] [Google Scholar]
- 66.Henriksen G., Breistøl K., Bruland S.Ø., Fodstad Ø., Larsen R.H. Significant antitumor effect from bone-seeking, alpha-particle-emitting (223)Ra demonstrated in an experimental skeletal metastases model. Cancer Res. 2002;62:3120–3125. [PubMed] [Google Scholar]
- 67.Hoskin P., Sartor O., O’Sullivan J.M., Johannessen D.C., Helle S.I., Logue J., Bottomley D., Nilsson S., Vogelzang N.J., Fang F., et al. Efficacy and safety of radium-223 dichloride in patients with castration-resistant prostate cancer and symptomatic bone metastases, with or without previous docetaxel use: A prespecified subgroup analysis from the randomised, double-blind, phase 3 ALSYMPCA trial. Lancet Oncol. 2014;15:1397–1406. doi: 10.1016/s1470-2045(14)70474-7. [DOI] [PubMed] [Google Scholar]
- 68.Rajasekaran A.K., Anilkumar G., Christiansen J.J. Is prostate-specific membrane antigen a multifunctional protein? Am. J. Physiol. Cell Physiol. 2005;288:C975–C981. doi: 10.1152/ajpcell.00506.2004. [DOI] [PubMed] [Google Scholar]
- 69.Bostwick D.G., Pacelli A., Blute M., Roche P., Murphy G.P. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: A study of 184 cases. Cancer. 1998;82:2256–2261. doi: 10.1002/(SICI)1097-0142(19980601)82:11<2256::AID-CNCR22>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 70.Wright G.L., Jr., Grob B.M., Haley C., Grossman K., Newhall K., Petrylak D., Troyer J., Konchuba A., Schellhammer P.F., Moriarty R. Upregulation of prostate-specific membrane antigen after androgen-deprivation therapy. Urology. 1996;48:326–334. doi: 10.1016/S0090-4295(96)00184-7. [DOI] [PubMed] [Google Scholar]
- 71.Chang S.S. Overview of prostate-specific membrane antigen. Rev. Urol. 2004;6((Suppl. S10)):S13–S18. [PMC free article] [PubMed] [Google Scholar]
- 72.Liu H., Rajasekaran A.K., Moy P., Xia Y., Kim S., Navarro V., Rahmati R., Bander N.H. Constitutive and antibody-induced internalization of prostate-specific membrane antigen. Cancer Res. 1998;58:4055–4060. [PubMed] [Google Scholar]
- 73.Emmett L., Willowson K., Violet J., Shin J., Blanksby A., Lee J. Lutetium (177) PSMA radionuclide therapy for men with prostate cancer: A review of the current literature and discussion of practical aspects of therapy. J. Med. Radiat. Sci. 2017;64:52–60. doi: 10.1002/jmrs.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Caroli P., Sandler I., Matteucci F., De Giorgi U., Uccelli L., Celli M., Foca F., Barone D., Romeo A., Sarnelli A., et al. 68Ga-PSMA PET/CT in patients with recurrent prostate cancer after radical treatment: Prospective results in 314 patients. Eur. J. Nucl. Med. Mol. Imaging. 2018;45:2035–2044. doi: 10.1007/s00259-018-4067-3. [DOI] [PubMed] [Google Scholar]
- 75.Hernando Polo S., Moreno Muñoz D., Rosero Rodríguez A.C., Silva Ruiz J., Rosero Rodríguez D.I., Couñago F. Changing the History of Prostate Cancer with New Targeted Therapies. Biomedicines. 2021;9:392. doi: 10.3390/biomedicines9040392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bander N.H., Milowsky M.I., Nanus D.M., Kostakoglu L., Vallabhajosula S., Goldsmith S.J. Phase I trial of 177lutetium-labeled J591, a monoclonal antibody to prostate-specific membrane antigen, in patients with androgen-independent prostate cancer. J. Clin. Oncol. 2005;23:4591–4601. doi: 10.1200/JCO.2005.05.160. [DOI] [PubMed] [Google Scholar]
- 77.Tagawa S.T., Milowsky M.I., Morris M., Vallabhajosula S., Christos P., Akhtar N.H., Osborne J., Goldsmith S.J., Larson S., Taskar N.P., et al. Phase II study of Lutetium-177-labeled anti-prostate-specific membrane antigen monoclonal antibody J591 for metastatic castration-resistant prostate cancer. Clin. Cancer Res. 2013;19:5182–5191. doi: 10.1158/1078-0432.CCR-13-0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tagawa S.T., Vallabhajosula S., Christos P.J., Jhanwar Y.S., Batra J.S., Lam L., Osborne J., Beltran H., Molina A.M., Goldsmith S.J., et al. Phase 1/2 study of fractionated dose lutetium-177-labeled anti-prostate-specific membrane antigen monoclonal antibody J591 ((177) Lu-J591) for metastatic castration-resistant prostate cancer. Cancer. 2019;125:2561–2569. doi: 10.1002/cncr.32072. [DOI] [PubMed] [Google Scholar]
- 79.Niaz M.J., Batra J.S., Walsh R.D., Ramirez-Fort M.K., Vallabhajosula S., Jhanwar Y.S., Molina A.M., Nanus D.M., Osborne J.R., Bander N.H., et al. Pilot Study of Hyperfractionated Dosing of Lutetium-177-Labeled Antiprostate-Specific Membrane Antigen Monoclonal Antibody J591 ((177) Lu-J591) for Metastatic Castration-Resistant Prostate Cancer. Oncologist. 2020;25:e477–e895. doi: 10.1634/theoncologist.2020-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hofman M.S., Violet J., Hicks R.J., Ferdinandus J., Thang S.P., Akhurst T., Iravani A., Kong G., Ravi Kumar A., Murphy D.G., et al. [(177)Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): A single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19:825–833. doi: 10.1016/S1470-2045(18)30198-0. [DOI] [PubMed] [Google Scholar]
- 81.Yadav M.P., Ballal S., Sahoo R.K., Dwivedi S.N., Bal C. Radioligand Therapy With (177)Lu-PSMA for Metastatic Castration-Resistant Prostate Cancer: A Systematic Review and Meta-Analysis. AJR Am. J. Roentgenol. 2019;213:275–285. doi: 10.2214/AJR.18.20845. [DOI] [PubMed] [Google Scholar]
- 82.Hofman M.S., Emmett L., Sandhu S., Iravani A., Joshua A.M., Goh J.C., Pattison D.A., Tan T.H., Kirkwood I.D., Ng S., et al. [(177)Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): A randomised, open-label, phase 2 trial. Lancet. 2021;397:797–804. doi: 10.1016/S0140-6736(21)00237-3. [DOI] [PubMed] [Google Scholar]
- 83.Quinn D.I., Shore N.D., Egawa S., Gerritsen W.R., Fizazi K. Immunotherapy for castration-resistant prostate cancer: Progress and new paradigms. Urol. Oncol. 2015;33:245–260. doi: 10.1016/j.urolonc.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 84.Wei X.X., Chan S., Kwek S., Lewis J., Dao V., Zhang L., Cooperberg M.R., Ryan C.J., Lin A.M., Friedlander T.W., et al. Systemic GM-CSF Recruits Effector T Cells into the Tumor Microenvironment in Localized Prostate Cancer. Cancer Immunol. Res. 2016;4:948–958. doi: 10.1158/2326-6066.CIR-16-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kantoff P.W., Schuetz T.J., Blumenstein B.A., Glode L.M., Bilhartz D.L., Wyand M., Manson K., Panicali D.L., Laus R., Schlom J., et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J. Clin. Oncol. 2010;28:1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kantoff P.W., Gulley J.L., Pico-Navarro C. Revised Overall Survival Analysis of a Phase II, Randomized, Double-Blind, Controlled Study of PROSTVAC in Men with Metastatic Castration-Resistant Prostate Cancer. J. Clin. Oncol. 2017;35:124–125. doi: 10.1200/JCO.2016.69.7748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gulley J.L., Borre M., Vogelzang N.J., Ng S., Agarwal N., Parker C.C., Pook D.W., Rathenborg P., Flaig T.W., Carles J., et al. Phase III Trial of PROSTVAC in Asymptomatic or Minimally Symptomatic Metastatic Castration-Resistant Prostate Cancer. J. Clin. Oncol. 2019;37:1051–1061. doi: 10.1200/JCO.18.02031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fay E.K., Graff J.N. Immunotherapy in Prostate Cancer. Cancers. 2020;12:1752. doi: 10.3390/cancers12071752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Topalian S.L., Hodi F.S., Brahmer J.R., Gettinger S.N., Smith D.C., McDermott D.F., Powderly J.D., Carvajal R.D., Sosman J.A., Atkins M.B., et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Antonarakis E.S., Piulats J.M., Gross-Goupil M., Goh J., Ojamaa K., Hoimes C.J., Vaishampayan U., Berger R., Sezer A., Alanko T., et al. Pembrolizumab for Treatment-Refractory Metastatic Castration-Resistant Prostate Cancer: Multicohort, Open-Label Phase II KEYNOTE-199 Study. J. Clin. Oncol. 2020;38:395–405. doi: 10.1200/JCO.19.01638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Stultz J., Fong L. How to turn up the heat on the cold immune microenvironment of metastatic prostate cancer. Prostate. Cancer Prostatic. Dis. 2021;24:697–717. doi: 10.1038/s41391-021-00340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sfanos K.S., Bruno T.C., Maris C.H., Xu L., Thoburn C.J., DeMarzo A.M., Meeker A.K., Isaacs W.B., Drake C.G. Phenotypic analysis of prostate-infiltrating lymphocytes reveals TH17 and Treg skewing. Clin. Cancer Res. 2008;14:3254–3261. doi: 10.1158/1078-0432.CCR-07-5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Schaeffer E., Srinivas S., Antonarakis E.S., Armstrong A.J., Bekelman J.E., Cheng H., D’Amico A.V., Davis B.J., Desai N., Dorff T., et al. NCCN Guidelines Insights: Prostate Cancer, Version 1.2021. J. Natl. Compr. Canc. Netw. 2021;19:134–143. doi: 10.6004/jnccn.2021.0008. [DOI] [PubMed] [Google Scholar]
- 94.Willis J., Lefterova M.I., Artyomenko A., Kasi P.M., Nakamura Y., Mody K., Catenacci D.V.T., Fakih M., Barbacioru C., Zhao J., et al. Validation of Microsatellite Instability Detection Using a Comprehensive Plasma-Based Genotyping Panel. Clin. Cancer Res. 2019;25:7035–7045. doi: 10.1158/1078-0432.CCR-19-1324. [DOI] [PubMed] [Google Scholar]
- 95.Abida W., Cheng M.L., Armenia J., Middha S., Autio K.A., Vargas H.A., Rathkopf D., Morris M.J., Danila D.C., Slovin S.F., et al. Analysis of the Prevalence of Microsatellite Instability in Prostate Cancer and Response to Immune Checkpoint Blockade. JAMA Oncol. 2019;5:471–478. doi: 10.1001/jamaoncol.2018.5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Robinson D., Van Allen E.M., Wu Y.M., Schultz N., Lonigro R.J., Mosquera J.M., Montgomery B., Taplin M.E., Pritchard C.C., Attard G., et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161:1215–1228. doi: 10.1016/j.cell.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Barata P., Agarwal N., Nussenzveig R., Gerendash B., Jaeger E., Hatton W., Ledet E., Lewis B., Layton J., Babiker H., et al. Clinical activity of pembrolizumab in metastatic prostate cancer with microsatellite instability high (MSI-H) detected by circulating tumor DNA. J. Immunother. Cancer. 2020;8:e001065. doi: 10.1136/jitc-2020-001065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shia J., Stadler Z., Weiser M.R., Rentz M., Gonen M., Tang L.H., Vakiani E., Katabi N., Xiong X., Markowitz A.J., et al. Immunohistochemical staining for DNA mismatch repair proteins in intestinal tract carcinoma: How reliable are biopsy samples? Am. J. Surg. Pathol. 2011;35:447–454. doi: 10.1097/PAS.0b013e31820a091d. [DOI] [PubMed] [Google Scholar]
- 99.Li K., Luo H., Huang L., Luo H., Zhu X. Microsatellite instability: A review of what the oncologist should know. Cancer Cell Int. 2020;20:16. doi: 10.1186/s12935-019-1091-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Marabelle A., Fakih M., Lopez J., Shah M., Shapira-Frommer R., Nakagawa K., Chung H.C., Kindler H.L., Lopez-Martin J.A., Miller W.H., Jr., et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: Prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 2020;21:1353–1365. doi: 10.1016/S1470-2045(20)30445-9. [DOI] [PubMed] [Google Scholar]
- 101.Marabelle A., Le D.T., Ascierto P.A., Di Giacomo A.M., De Jesus-Acosta A., Delord J.P., Geva R., Gottfried M., Penel N., Hansen A.R., et al. Efficacy of Pembrolizumab in Patients with Noncolorectal High Microsatellite Instability/Mismatch Repair-Deficient Cancer: Results from the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020;38:1–10. doi: 10.1200/JCO.19.02105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tang Z., Pilié P.G., Geng C., Manyam G.C., Yang G., Park S., Wang D., Peng S., Wu C., Peng G., et al. ATR Inhibition Induces CDK1-SPOP Signaling and Enhances Anti-PD-L1 Cytotoxicity in Prostate Cancer. Clin. Cancer Res. 2021;27:4898–4909. doi: 10.1158/1078-0432.CCR-21-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhang J., Bu X., Wang H., Zhu Y., Geng Y., Nihira N.T., Tan Y., Ci Y., Wu F., Dai X., et al. Author Correction: Cyclin D-CDK4 kinase destabilizes PD-L1 via cullin 3-SPOP to control cancer immune surveillance. Nature. 2018;553:91–95. doi: 10.1038/nature25015. Erratum in Nature 2019, 571, E10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Park J.H., Rivière I., Gonen M., Wang X., Sénéchal B., Curran K.J., Sauter C., Wang Y., Santomasso B., Mead E., et al. Long-Term Follow-up of CD19 CAR Therapy in Acute Lymphoblastic Leukemia. N. Engl. J. Med. 2018;378:449–459. doi: 10.1056/NEJMoa1709919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Schepisi G., Cursano M.C., Casadei C., Menna C., Altavilla A., Lolli C., Cerchione C., Paganelli G., Santini D., Tonini G., et al. CAR-T cell therapy: A potential new strategy against prostate cancer. J. Immunother. Cancer. 2019;7:258. doi: 10.1186/s40425-019-0741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Perera M.P.J., Thomas P.B., Risbridger G.P., Taylor R., Azad A., Hofman M.S., Williams E.D., Vela I. Chimeric Antigen Receptor T-Cell Therapy in Metastatic Castrate-Resistant Prostate Cancer. Cancers. 2022;14:503. doi: 10.3390/cancers14030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Amini L., Silbert S.K., Maude S.L., Nastoupil L.J., Ramos C.A., Brentjens R.J., Sauter C.S., Shah N.N., Abou-El-Enein M. Preparing for CAR T cell therapy: Patient selection, bridging therapies and lymphodepletion. Nat. Rev. Clin. Oncol. 2022;19:342–355. doi: 10.1038/s41571-022-00607-3. [DOI] [PubMed] [Google Scholar]
- 108.Depil S., Duchateau P., Grupp S.A., Mufti G., Poirot L. ‘Off-the-shelf’ allogeneic CAR T cells: Development and challenges. Nat. Rev. Drug Discov. 2020;19:185–199. doi: 10.1038/s41573-019-0051-2. [DOI] [PubMed] [Google Scholar]
- 109.Hupe M.C., Philippi C., Roth D., Kümpers C., Ribbat-Idel J., Becker F., Joerg V., Duensing S., Lubczyk V.H., Kirfel J., et al. Expression of Prostate-Specific Membrane Antigen (PSMA) on Biopsies Is an Independent Risk Stratifier of Prostate Cancer Patients at Time of Initial Diagnosis. Front. Oncol. 2018;8:623. doi: 10.3389/fonc.2018.00623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Junghans R.P., Ma Q., Rathore R., Gomes E.M., Bais A.J., Lo A.S., Abedi M., Davies R.A., Cabral H.J., Al-Homsi A.S., et al. Phase I Trial of Anti-PSMA Designer CAR-T Cells in Prostate Cancer: Possible Role for Interacting Interleukin 2-T Cell Pharmacodynamics as a Determinant of Clinical Response. Prostate. 2016;76:1257–1270. doi: 10.1002/pros.23214. [DOI] [PubMed] [Google Scholar]
- 111.Slovin S. Adoptive Transfer of Autologous T Cells Targeted to Prostate Specific Membrane Antigen (PSMA) for the Treatment of Castrate Metastatic Prostate Cancer (CMPC) [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT01140373?term=NCT01140373&draw=2&rank=1.
- 112.Slovin S.F., Dorff T.B., Falchook G.S., Wei X.X., Gao X., McKay R.R., Oh D.Y., Wibmer A.G., Spear M.A., McCaigue J., et al. Phase 1 Study of P-PSMA-101 CAR-T Cells in Patients with Metastatic Castration-Resistant Prostate Cancer (mCRPC) [(accessed on 15 July 2022)]. Available online: https://ascopubs.org/doi/abs/10.1200/JCO.2022.40.6_suppl.098.
- 113.Narayan V., Barber-Rotenberg J.S., Jung I.Y., Lacey S.F., Rech A.J., Davis M.M., Hwang W.T., Lal P., Carpenter E.L., Maude S.L., et al. PSMA-targeting TGFβ-insensitive armored CAR T cells in metastatic castration-resistant prostate cancer: A phase 1 trial. Nat. Med. 2022;28:724–734. doi: 10.1038/s41591-022-01726-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kloss C.C., Lee J., Zhang A., Chen F., Melenhorst J.J., Lacey S.F., Maus M.V., Fraietta J.A., Zhao Y., June C.H. Dominant-Negative TGF-β Receptor Enhances PSMA-Targeted Human CAR T Cell Proliferation and Augments Prostate Cancer Eradication. Mol. Ther. 2018;26:1855–1866. doi: 10.1016/j.ymthe.2018.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang Q., Helfand B.T., Carneiro B.A., Qin W., Yang X.J., Lee C., Zhang W., Giles F.J., Cristofanilli M., Kuzel T.M. Efficacy Against Human Prostate Cancer by Prostate-specific Membrane Antigen-specific, Transforming Growth Factor-β Insensitive Genetically Targeted CD8(+) T-cells Derived from Patients with Metastatic Castrate-resistant Disease. Eur. Urol. 2018;73:648–652. doi: 10.1016/j.eururo.2017.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.A Study of CART-PSMA-TGFβRDN in Patients with Metastatic Castration Resistant Prostate Cancer. [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04227275?term=NCT04227275&draw=2&rank=1.
- 117.Anurathapan U., Chan R.C., Hindi H.F., Mucharla R., Bajgain P., Hayes B.C., Fisher W.E., Heslop H.E., Rooney C.M., Brenner M.K., et al. Kinetics of tumor destruction by chimeric antigen receptor-modified T cells. Mol. Ther. 2014;22:623–633. doi: 10.1038/mt.2013.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.PSCA-CAR T Cells in Treating Patients With PSCA+ Metastatic Castration Resistant Prostate Cancer. [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03873805?term=NCT03873805&draw=2&rank=1.
- 119.Safety and Activity Study of PSCA-Targeted CAR-T Cells (BPX-601) in Subjects with Selected Advanced Solid Tumors. [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02744287?term=NCT02744287&draw=2&rank=1.
- 120.Abida W., Armenia J., Gopalan A., Brennan R., Walsh M., Barron D., Danila D., Rathkopf D., Morris M., Slovin S., et al. Prospective Genomic Profiling of Prostate Cancer Across Disease States Reveals Germline and Somatic Alterations That May Affect Clinical Decision Making. JCO Precis. Oncol. 2017;1:1–16. doi: 10.1200/PO.17.00029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pritchard C.C., Mateo J., Walsh M.F., De Sarkar N., Abida W., Beltran H., Garofalo A., Gulati R., Carreira S., Eeles R., et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N. Engl. J. Med. 2016;375:443–453. doi: 10.1056/NEJMoa1603144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Venkitaraman A.R. Linking the cellular functions of BRCA genes to cancer pathogenesis and treatment. Annu. Rev. Pathol. 2009;4:461–487. doi: 10.1146/annurev.pathol.3.121806.151422. [DOI] [PubMed] [Google Scholar]
- 123.Jasin M., Rothstein R. Repair of strand breaks by homologous recombination. Cold Spring Harb. Perspect Biol. 2013;5:a012740. doi: 10.1101/cshperspect.a012740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Helleday T. The underlying mechanism for the PARP and BRCA synthetic lethality: Clearing up the misunderstandings. Mol. Oncol. 2011;5:387–393. doi: 10.1016/j.molonc.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Fisher A.E., Hochegger H., Takeda S., Caldecott K.W. Poly(ADP-ribose) polymerase 1 accelerates single-strand break repair in concert with poly(ADP-ribose) glycohydrolase. Mol. Cell Biol. 2007;27:5597–5605. doi: 10.1128/MCB.02248-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Murai J., Huang S.Y., Das B.B., Renaud A., Zhang Y., Doroshow J.H., Ji J., Takeda S., Pommier Y. Trapping of PARP1 and PARP2 by Clinical PARP Inhibitors. Cancer Res. 2012;72:5588–5599. doi: 10.1158/0008-5472.CAN-12-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mateo J., Carreira S., Sandhu S., Miranda S., Mossop H., Perez-Lopez R., Nava Rodrigues D., Robinson D., Omlin A., Tunariu N., et al. DNA-Repair Defects and Olaparib in Metastatic Prostate Cancer. N. Engl. J. Med. 2015;373:1697–1708. doi: 10.1056/NEJMoa1506859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Clarke N., Wiechno P., Alekseev B., Sala N., Jones R., Kocak I., Chiuri V.E., Jassem J., Fléchon A., Redfern C., et al. Olaparib combined with abiraterone in patients with metastatic castration-resistant prostate cancer: A randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2018;19:975–986. doi: 10.1016/S1470-2045(18)30365-6. [DOI] [PubMed] [Google Scholar]
- 129.PROpel: Phase III Trial of Olaparib (ola) and Abiraterone (abi) Versus Placebo (pbo) and abi as First-Line (1L) Therapy for Patients (pts) with Metastatic Castration-Resistant Prostate Cancer (mCRPC) [(accessed on 5 July 2022)]. Available online: https://ascopubs.org/doi/abs/10.1200/JCO.2022.40.6_suppl.011.
- 130.Boysen G., Barbieri C.E., Prandi D., Blattner M., Chae S.S., Dahija A., Nataraj S., Huang D., Marotz C., Xu L., et al. SPOP mutation leads to genomic instability in prostate cancer. Elife. 2015;4:e09207. doi: 10.7554/eLife.09207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Phase 3 MAGNITUDE Study: First Results of Niraparib (NIRA) with Abiraterone Acetate and Prednisone (AAP) as First-Line Therapy in Patients (pts) with Metastatic Castration-Resistant Prostate Cancer (mCRPC) with and without Homologous Recombination Repair (HRR) Gene Alterations. [(accessed on 15 July 2022)]. Available online: https://ascopubs.org/doi/abs/10.1200/JCO.2022.40.6_suppl.012.
- 132.Talazoparib in Combination with Belinostat for Metastatic Breast Cancer, Metastatic Castration Resistant Prostate Cancer, and Metastatic Ovarian Cancer. [(accessed on 15 July 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04703920?term=NCT+04703920&draw=2&rank=1.
- 133.Cuzick J., Yang Z.H., Fisher G., Tikishvili E., Stone S., Lanchbury J.S., Camacho N., Merson S., Brewer D., Cooper C.S., et al. Prognostic value of PTEN loss in men with conservatively managed localised prostate cancer. Br. J. Cancer. 2013;108:2582–2589. doi: 10.1038/bjc.2013.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Schmitz M., Grignard G., Margue C., Dippel W., Capesius C., Mossong J., Nathan M., Giacchi S., Scheiden R., Kieffer N. Complete loss of PTEN expression as a possible early prognostic marker for prostate cancer metastasis. Int. J. Cancer. 2007;120:1284–1292. doi: 10.1002/ijc.22359. [DOI] [PubMed] [Google Scholar]
- 135.Carver B.S., Chapinski C., Wongvipat J., Hieronymus H., Chen Y., Chandarlapaty S., Arora V.K., Le C., Koutcher J., Scher H., et al. Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell. 2011;19:575–586. doi: 10.1016/j.ccr.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Leinonen K.A., Saramäki O.R., Furusato B., Kimura T., Takahashi H., Egawa S., Suzuki H., Keiger K., Ho Hahm S., Isaacs W.B., et al. Loss of PTEN is associated with aggressive behavior in ERG-positive prostate cancer. Cancer Epidemiol. Biomark. Prev. 2013;22:2333–2344. doi: 10.1158/1055-9965.EPI-13-0333-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ma Q., Fu W., Li P., Nicosia S.V., Jenster G., Zhang X., Bai W. FoxO1 mediates PTEN suppression of androgen receptor N- and C-terminal interactions and coactivator recruitment. Mol. Endocrinol. 2009;23:213–225. doi: 10.1210/me.2008-0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ferraldeschi R., Nava Rodrigues D., Riisnaes R., Miranda S., Figueiredo I., Rescigno P., Ravi P., Pezaro C., Omlin A., Lorente D., et al. PTEN protein loss and clinical outcome from castration-resistant prostate cancer treated with abiraterone acetate. Eur. Urol. 2015;67:795–802. doi: 10.1016/j.eururo.2014.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.González-Billalabeitia E., Seitzer N., Song S.J., Song M.S., Patnaik A., Liu X.S., Epping M.T., Papa A., Hobbs R.M., Chen M., et al. Vulnerabilities of PTEN-TP53-deficient prostate cancers to compound PARP-PI3K inhibition. Cancer Discov. 2014;4:896–904. doi: 10.1158/2159-8290.CD-13-0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sweeney C., Bracarda S., Sternberg C.N., Chi K.N., Olmos D., Sandhu S., Massard C., Matsubara N., Alekseev B., Parnis F., et al. Ipatasertib plus abiraterone and prednisolone in metastatic castration-resistant prostate cancer (IPATential150): A multicentre, randomised, double-blind, phase 3 trial. Lancet. 2021;398:131–142. doi: 10.1016/S0140-6736(21)00580-8. [DOI] [PubMed] [Google Scholar]
- 141.Beltran H., Rickman D.S., Park K., Chae S.S., Sboner A., MacDonald T.Y., Wang Y., Sheikh K.L., Terry S., Tagawa S.T., et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. Cancer Discov. 2011;1:487–495. doi: 10.1158/2159-8290.CD-11-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Brockmann M., Poon E., Berry T., Carstensen A., Deubzer H.E., Rycak L., Jamin Y., Thway K., Robinson S.P., Roels F., et al. Small molecule inhibitors of aurora-a induce proteasomal degradation of N-myc in childhood neuroblastoma. Cancer Cell. 2013;24:75–89. doi: 10.1016/j.ccr.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Graff J.N., Higano C.S., Hahn N.M., Taylor M.H., Zhang B., Zhou X., Venkatakrishnan K., Leonard E.J., Sarantopoulos J. Open-label, multicenter, phase 1 study of alisertib (MLN8237), an aurora A kinase inhibitor, with docetaxel in patients with solid tumors. Cancer. 2016;122:2524–2533. doi: 10.1002/cncr.30073. [DOI] [PubMed] [Google Scholar]
- 144.Beltran H., Oromendia C., Danila D.C., Montgomery B., Hoimes C., Szmulewitz R.Z., Vaishampayan U., Armstrong A.J., Stein M., Pinski J., et al. A Phase II Trial of the Aurora Kinase a Inhibitor Alisertib for Patients with Castration-resistant and Neuroendocrine Prostate Cancer: Efficacy and Biomarkers. Clin. Cancer Res. 2019;25:43–51. doi: 10.1158/1078-0432.CCR-18-1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lin J., Patel S.A., Sama A.R., Hoffman-Censits J.H., Kennedy B., Kilpatrick D., Ye Z., Yang H., Mu Z., Leiby B., et al. A Phase I/II Study of the Investigational Drug Alisertib in Combination with Abiraterone and Prednisone for Patients With Metastatic Castration-Resistant Prostate Cancer Progressing on Abiraterone. Oncologist. 2016;21:1296–1297e. doi: 10.1634/theoncologist.2016-0297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dicken H., Hensley P.J., Kyprianou N. Prostate tumor neuroendocrine differentiation via EMT: The road less traveled. Asian J. Urol. 2019;6:82–90. doi: 10.1016/j.ajur.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lo U.G., Lee C.F., Lee M.S., Hsieh J.T. The Role and Mechanism of Epithelial-to-Mesenchymal Transition in Prostate Cancer Progression. Int. J. Mol. Sci. 2017;18:2079. doi: 10.3390/ijms18102079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Nickols N.G., Nazarian R., Zhao S.G., Tan V., Uzunangelov V., Xia Z., Baertsch R., Neeman E., Gao A.C., Thomas G.V., et al. MEK-ERK signaling is a therapeutic target in metastatic castration resistant prostate cancer. Prostate. Cancer Prostatic. Dis. 2019;22:531–538. doi: 10.1038/s41391-019-0134-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ducasse M., Brown M.A. Epigenetic aberrations and cancer. Mol. Cancer. 2006;5:60. doi: 10.1186/1476-4598-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Dokmanovic M., Clarke C., Marks P.A. Histone deacetylase inhibitors: Overview and perspectives. Mol. Cancer Res. 2007;5:981–989. doi: 10.1158/1541-7786.MCR-07-0324. [DOI] [PubMed] [Google Scholar]
- 151.Park J.W., Han J.W. Targeting epigenetics for cancer therapy. Arch. Pharm. Res. 2019;42:159–170. doi: 10.1007/s12272-019-01126-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dokmanovic M., Marks P.A. Prospects: Histone deacetylase inhibitors. J. Cell Biochem. 2005;96:293–304. doi: 10.1002/jcb.20532. [DOI] [PubMed] [Google Scholar]
- 153.Yoon S., Eom G.H. HDAC and HDAC Inhibitor: From Cancer to Cardiovascular Diseases. Chonnam. Med. J. 2016;52:1–11. doi: 10.4068/cmj.2016.52.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mottet D., Castronovo V. Histone deacetylases: Target enzymes for cancer therapy. Clin. Exp. Metastasis. 2008;25:183–189. doi: 10.1007/s10585-007-9131-5. [DOI] [PubMed] [Google Scholar]
- 155.Waltregny D., North B., Van Mellaert F., de Leval J., Verdin E., Castronovo V. Screening of histone deacetylases (HDAC) expression in human prostate cancer reveals distinct class I HDAC profiles between epithelial and stromal cells. Eur. J. Histochem. 2004;48:273–290. [PubMed] [Google Scholar]
- 156.Lin J., Wang C., Kelly W.K. Targeting epigenetics for the treatment of prostate cancer: Recent progress and future directions. Semin. Oncol. 2013;40:393–401. doi: 10.1053/j.seminoncol.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 157.Xu X., Huang Y.H., Li Y.J., Cohen A., Li Z., Squires J., Zhang W., Chen X.F., Zhang M., Huang J.T. Potential therapeutic effect of epigenetic therapy on treatment-induced neuroendocrine prostate cancer. Asian J. Androl. 2017;19:686–693. doi: 10.4103/1008-682x.191518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bradley D., Rathkopf D., Dunn R., Stadler W.M., Liu G., Smith D.C., Pili R., Zwiebel J., Scher H., Hussain M. Vorinostat in advanced prostate cancer patients progressing on prior chemotherapy (National Cancer Institute Trial 6862): Trial results and interleukin-6 analysis: A study by the Department of Defense Prostate Cancer Clinical Trial Consortium and University of Chicago Phase 2 Consortium. Cancer. 2009;115:5541–5549. doi: 10.1002/cncr.24597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mann B.S., Johnson J.R., Cohen M.H., Justice R., Pazdur R. FDA approval summary: Vorinostat for treatment of advanced primary cutaneous T-cell lymphoma. Oncologist. 2007;12:1247–1252. doi: 10.1634/theoncologist.12-10-1247. [DOI] [PubMed] [Google Scholar]
- 160.Rana Z., Diermeier S., Hanif M., Rosengren R.J. Understanding Failure and Improving Treatment Using HDAC Inhibitors for Prostate Cancer. Biomedicines. 2020;8:22. doi: 10.3390/biomedicines8020022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Wang P., Yuan Y., Lin W., Zhong H., Xu K., Qi X. Roles of sphingosine-1-phosphate signaling in cancer. Cancer Cell Int. 2019;19:295. doi: 10.1186/s12935-019-1014-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Shida D., Takabe K., Kapitonov D., Milstien S., Spiegel S. Targeting SphK1 as a new strategy against cancer. Curr. Drug Targets. 2008;9:662–673. doi: 10.2174/138945008785132402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Xu G., Yang Z., Sun Y., Dong H., Ma J. Interaction of microRNAs with sphingosine kinases, sphingosine-1 phosphate, and sphingosine-1 phosphate receptors in cancer. Discov. Oncol. 2021;12:33. doi: 10.1007/s12672-021-00430-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Pchejetski D., Doumerc N., Golzio M., Naymark M., Teissie J., Kohama T., Waxman J., Malavaud B., Cuvillier O. Chemosensitizing effects of sphingosine kinase-1 inhibition in prostate cancer cell and animal models. Mol. Cancer Ther. 2008;7:1836–1845. doi: 10.1158/1535-7163.MCT-07-2322. [DOI] [PubMed] [Google Scholar]
- 165.Sauer L., Nunes J., Salunkhe V., Skalska L., Kohama T., Cuvillier O., Waxman J., Pchejetski D. Sphingosine kinase 1 inhibition sensitizes hormone-resistant prostate cancer to docetaxel. Int. J. Cancer. 2009;125:2728–2736. doi: 10.1002/ijc.24640. [DOI] [PubMed] [Google Scholar]
- 166.Brizuela L., Dayon A., Doumerc N., Ader I., Golzio M., Izard J.C., Hara Y., Malavaud B., Cuvillier O. The sphingosine kinase-1 survival pathway is a molecular target for the tumor-suppressive tea and wine polyphenols in prostate cancer. FASEB J. 2010;24:3882–3894. doi: 10.1096/fj.10-160838. [DOI] [PubMed] [Google Scholar]
- 167.Lee S.O., Kim J.S., Lee M.S., Lee H.J. Anti-cancer effect of pristimerin by inhibition of HIF-1alpha involves the SPHK-1 pathway in hypoxic prostate cancer cells. BMC Cancer. 2016;16:701. doi: 10.1186/s12885-016-2730-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Beckham T.H., Cheng J.C., Lu P., Shao Y., Troyer D., Lance R., Marrison S.T., Norris J.S., Liu X. Acid ceramidase induces sphingosine kinase 1/S1P receptor 2-mediated activation of oncogenic Akt signaling. Oncogenesis. 2013;2:e49. doi: 10.1038/oncsis.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Brizuela L., Ader I., Mazerolles C., Bocquet M., Malavaud B., Cuvillier O. First evidence of sphingosine 1-phosphate lyase protein expression and activity downregulation in human neoplasm: Implication for resistance to therapeutics in prostate cancer. Mol. Cancer Ther. 2012;11:1841–1851. doi: 10.1158/1535-7163.MCT-12-0227. [DOI] [PubMed] [Google Scholar]
- 170.Akao Y., Banno Y., Nakagawa Y., Hasegawa N., Kim T.J., Murate T., Igarashi Y., Nozawa Y. High expression of sphingosine kinase 1 and S1P receptors in chemotherapy-resistant prostate cancer PC3 cells and their camptothecin-induced up-regulation. Biochem. Biophys. Res. Commun. 2006;342:1284–1290. doi: 10.1016/j.bbrc.2006.02.070. [DOI] [PubMed] [Google Scholar]
- 171.Pchejetski D., Bohler T., Brizuela L., Sauer L., Doumerc N., Golzio M., Salunkhe V., Teissie J., Malavaud B., Waxman J., et al. FTY720 (fingolimod) sensitizes prostate cancer cells to radiotherapy by inhibition of sphingosine kinase-1. Cancer Res. 2010;70:8651–8661. doi: 10.1158/0008-5472.CAN-10-1388. [DOI] [PubMed] [Google Scholar]
- 172.Lee C.F., Dang A., Hernandez E., Pong R.C., Chen B., Sonavane R., Raj G., Kapur P., Lin H.Y., Wu S.R., et al. Activation of sphingosine kinase by lipopolysaccharide promotes prostate cancer cell invasion and metastasis via SphK1/S1PR4/matriptase. Oncogene. 2019;38:5580–5598. doi: 10.1038/s41388-019-0833-3. [DOI] [PubMed] [Google Scholar]
- 173.Malavaud B., Pchejetski D., Mazerolles C., de Paiva G.R., Calvet C., Doumerc N., Pitson S., Rischmann P., Cuvillier O. Sphingosine kinase-1 activity and expression in human prostate cancer resection specimens. Eur. J. Cancer. 2010;46:3417–3424. doi: 10.1016/j.ejca.2010.07.053. [DOI] [PubMed] [Google Scholar]
- 174.Lee C.F., Chen Y.A., Hernandez E., Pong R.C., Ma S., Hofstad M., Kapur P., Zhau H., Chung L.W., Lai C.H., et al. The central role of Sphingosine kinase 1 in the development of neuroendocrine prostate cancer (NEPC): A new targeted therapy of NEPC. Clin. Transl. Med. 2022;12:e695. doi: 10.1002/ctm2.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Brinkmann V., Billich A., Baumruker T., Heining P., Schmouder R., Francis G., Aradhye S., Burtin P. Fingolimod (FTY720): Discovery and development of an oral drug to treat multiple sclerosis. Nat. Rev. Drug Discov. 2010;9:883–897. doi: 10.1038/nrd3248. [DOI] [PubMed] [Google Scholar]
- 176.Tsou R.C., Bence K.K. The Genetics of PTPN1 and Obesity: Insights from Mouse Models of Tissue-Specific PTP1B Deficiency. J. Obes. 2012;2012:926857. doi: 10.1155/2012/926857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Johnson T.O., Ermolieff J., Jirousek M.R. Protein tyrosine phosphatase 1B inhibitors for diabetes. Nat. Rev. Drug Discov. 2002;1:696–709. doi: 10.1038/nrd895. [DOI] [PubMed] [Google Scholar]
- 178.Lessard L., Stuible M., Tremblay M.L. The two faces of PTP1B in cancer. Biochim. Biophys. Acta. 2010;1804:613–619. doi: 10.1016/j.bbapap.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 179.Lessard L., Labbe D.P., Deblois G., Begin L.R., Hardy S., Mes-Masson A.M., Saad F., Trotman L.C., Giguere V., Tremblay M.L. PTP1B is an androgen receptor-regulated phosphatase that promotes the progression of prostate cancer. Cancer Res. 2012;72:1529–1537. doi: 10.1158/0008-5472.CAN-11-2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Xu Q., Wu N., Li X., Guo C., Li C., Jiang B., Wang H., Shi D. Inhibition of PTP1B blocks pancreatic cancer progression by targeting the PKM2/AMPK/mTOC1 pathway. Cell Death Dis. 2019;10:874. doi: 10.1038/s41419-019-2073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Wang W., Cao Y., Zhou X., Wei B., Zhang Y., Liu X. PTP1B promotes the malignancy of ovarian cancer cells in a JNK-dependent mechanism. Biochem. Biophys. Res. Commun. 2018;503:903–909. doi: 10.1016/j.bbrc.2018.06.094. [DOI] [PubMed] [Google Scholar]
- 182.Hoekstra E., Das A.M., Swets M., Cao W., van der Woude C.J., Bruno M.J., Peppelenbosch M.P., Kuppen P.J., Ten Hagen T.L., Fuhler G.M. Increased PTP1B expression and phosphatase activity in colorectal cancer results in a more invasive phenotype and worse patient outcome. Oncotarget. 2016;7:21922–21938. doi: 10.18632/oncotarget.7829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Tonks N.K., Muthuswamy S.K. A brake becomes an accelerator: PTP1B--a new therapeutic target for breast cancer. Cancer Cell. 2007;11:214–216. doi: 10.1016/j.ccr.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 184.Wu C., Zhang L., Bourne P.A., Reeder J.E., di Sant’Agnese P.A., Yao J.L., Na Y., Huang J. Protein tyrosine phosphatase PTP1B is involved in neuroendocrine differentiation of prostate cancer. Prostate. 2006;66:1125–1135. doi: 10.1002/pros.20412. [DOI] [PubMed] [Google Scholar]
- 185.Wiede F., Lu K.H., Du X., Zeissig M.N., Xu R., Goh P.K., Xirouchaki C.E., Hogarth S.J., Greatorex S., Sek K., et al. PTP1B Is an Intracellular Checkpoint that Limits T-cell and CAR T-cell Antitumor Immunity. Cancer Discov. 2022;12:752–773. doi: 10.1158/2159-8290.CD-21-0694. [DOI] [PMC free article] [PubMed] [Google Scholar]