Abstract
Background: Ceftolozane/tazobactam (C/T) is a combination of an antipseudomonal oxyiminoaminothiazolyl cephalosporin with potent in vitro activity against Pseudomonas aeruginosa and tazobactam, a known β-lactamase inhibitor. The aim of this study was to evaluate the activity of C/T against clinical isolates of P. aeruginosa and Enterobacterales collected from five Latin American countries between 2016 and 2017, before its clinical use in Latin America, and to compare it with the activity of other available broad-spectrum antimicrobial agents. Methods: a total of 2760 clinical isolates (508 P. aeruginosa and 2252 Enterobacterales) were consecutively collected from 20 hospitals and susceptibility to C/T and comparator agents was tested and interpreted following the current guidelines. Results: according to the CLSI breakpoints, 68.1% (346/508) of P. aeruginosa and 83.9% (1889/2252) of Enterobacterales isolates were susceptible to C/T. Overall, C/T demonstrated higher in vitro activity than currently available cephalosporins, piperacillin/tazobactam and carbapenems when tested against P. aeruginosa, and its performance in vitro was comparable to fosfomycin. When tested against Enterobacterales, it showed higher activity than cephalosporins and piperacillin/tazobactam, and similar activity to ertapenem. Conclusions: these results show that C/T is an active β-lactam agent against clinical isolates of P. aeruginosa and Enterobacterales.
Keywords: ceftolozane/tazobactam, Pseudomonas aeruginosa, Enterobacterales, antimicrobial resistance, Latin America
1. Introduction
Antibiotic resistance is a global public health problem that compromises the effectiveness of antimicrobial therapy in healthcare settings and in the community, threatening the enormous gains made by the discovery of new antibiotics [1,2]. This scenario is particularly relevant for Gram-negative pathogens such as P. aeruginosa and Enterobacterales. These bacteria are a frequent cause of healthcare-associated infections (HAI) and are among the most common pathogenic organisms acquiring resistance to extended-spectrum cephalosporins and carbapenems, which are the preferred antimicrobial regimens [3,4]. Indeed, once they develop resistance to broad-spectrum β-lactam antibiotics, reliable therapeutic options become scarce.
Ceftolozane/tazobactam (C/T) is a combination of a last-generation cephalosporin, ceftolozane, and a well-known β-lactamase inhibitor, tazobactam [5]. The antibacterial mechanism of ceftolozane, as for any other β-lactam, is based on the inhibition of the bacterial cell wall biosynthesis, specifically mediated by its binding to penicillin-binding proteins (PBPs). Ceftolozane inhibits all of the essential PBPs produced by P. aeruginosa: PBP1b, PBP1c, PBP3 and some of Enterobacterales, like the PBP3 from Escherichia coli [6]. Tazobactam, although having clinically irrelevant in vitro activity against bacterial PBPs, is a potent and irreversible inhibitor of some β-lactamases, which restores the antibacterial activity of ceftolozane and improves the spectrum of activity against ESBL-producing Enterobacterales and some anaerobes [7]. Structurally, the substitution of a pyrazole side chain on the 3-position of the cephem ring improves the outer membrane permeability of ceftolozane and grants increased stability against some AmpC β-lactamases, leading to improved activity against P. aeruginosa [8]. In 2014, the U.S. Food and Drug Administration (FDA) approved this combination for the treatment of complicated urinary tract infections, and also, in combination with metronidazole, for the treatment of complicated intra-abdominal infections. In 2019, C/T was also approved for the treatment of hospital-acquired (HAP) and ventilator-acquired (VAP) pneumonia [9]. Ceftolozane has been reported to have improved outer membrane permeability, is less affected by the activity of efflux pumps, and has enhanced stability against the chromosomal Pseudomonas-derived cephalosporinase (PDC), resulting in potent in vitro activity against P. aeruginosa [10,11]. Hence, C/T remains highly active against most Gram-negative bacteria (GNB) including multidrug-resistant (MDR) P. aeruginosa (i.e., non-susceptible to ≥1 antimicrobial agent in ≥3 different antimicrobial categories) [12], but it has lower in vitro activity than carbapenems against ESBL-producing K. pneumoniae and, in addition, it is not active against carbapenemase-producing isolates independent of the carbapenemase class produced [13,14,15,16].
By documenting local, regional, and global epidemiological patterns and trends of antimicrobial resistance, surveillance programs play a fundamental role in the design of strategies to combat the dissemination and management of MDR pathogens. Studies describing the in vitro activity of C/T and comparator agents against clinical isolates of Enterobacterales and P. aeruginosa have shown that the susceptibility to C/T varies greatly among different regions. For example, while susceptibility to C/T among isolates collected from different European hospitals between 2011 and 2012 was 84.5% for P. aeruginosa and 91.5% for Enterobacterales, in Canada, the susceptibility to C/T in P. aeruginosa in 2013 was >98%, similar to the U.S. and some Western European countries, where susceptibility to this antibiotic was >94% for P. aeruginosa and 90% for Enterobacterales [17,18,19]. In the Latin American region, the susceptibility of clinical isolates collected between 2013 and 2015 showed that 89.6% of P. aeruginosa and 85.9% of Enterobacterales were susceptible to C/T [20]. Due to the increasing global spread of MDR GNB, up-to-date surveillance studies are necessary to closely monitor this impact on the use of new antibiotics such as C/T.
Herein, we extend the information from previous studies, report the activity of C/T against clinical isolates of P. aeruginosa and Enterobacterales retrieved from 20 different Latin American hospitals from January 2016 through October 2017, and compare this to the activity of several broad-spectrum antimicrobials. Our results provide new data on the susceptibility patterns of C/T in this geographical area, which are characterized as being endemic for several antimicrobial-resistance mechanisms [21].
2. Results
2.1. Susceptibility Profile for Phenotypic Subsets
To facilitate analysis of the data, we grouped the P. aeruginosa and Enterobacterales isolates in phenotypic groups. As shown in Table 1, for P. aeruginosa, the piperacillin/tazobactam-NS phenotypic subset was observed in 45.5% (231/508), ceftazidime-NS in 46.8% (238/508), and meropenem-NS in 53.5% (272/508) of the isolates.
Table 1.
Susceptibility of phenotypic subsets of clinical isolates of P. aeruginosa and Enterobacterales to C/T and comparator agents between 2016 and 2017 from five Latin American countries.
| Percentage of Susceptibility (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Organism | Number of Isolates | C/T | CRO | CTX | CAZ | TZP | ETP | IMI | MEM | DOR | TGC | FOS |
| Pseudomonas aeruginosa | 508 | 68.1 | NA | NA | 53.1 | 54.5 | NA | 10.8 | 36.4 | 38.6 | NA | 72.2 ** |
| piperacillin/tazobactam-NS | 231 | 36.8 | NA | NA | 10.9 | - | NA | 3.46 | 10.8 | 13.4 | NA | 62.8 ** |
| ceftazidime-NS | 238 | 35.7 | NA | NA | - | 13.4 | NA | 14.7 | 21.0 | 26.1 | NA | 40.8 ** |
| meropenem-NS | 272 | 46.7 | NA | NA | 30.9 | 29.8 | NA | 1.1 | - | 12.5 | NA | 64.3 ** |
| Escherichia coli | 1409 | 93.2 | 60.3 | 60.9 | 71.8 | 90.3 | 90.3 | 94.3 | 95.5 | 95.7 | 95.6 | 94.8 |
| ESBL non-CRE phenotype * | 425 | 95.3 | - | 3.5 | 33.4 | 90.3 | - | 99.5 | 100.0 | 100.0 | 98.1 | 90.8 |
| Klebsiella pneumoniae | 610 | 68.7 | 44.9 | 46.9 | 50.0 | 59.2 | 70.0 | 71.0 | 76.6 | 77.7 | 84.4 | 92.5 |
| ESBL non-CRE phenotype * | 153 | 79.7 | - | 8.5 | 24.2 | 52.3 | - | 97.4 | 99.3 | 100.0 | 96.1 | 94.8 |
| Serratia marcescens | 91 | 71.4 | 46.2 | 42.9 | 62.6 | 69.2 | 70.3 | 73.6 | 78.0 | 76.9 | 80.2 | 94.5 |
| ertapenem-susceptible | 64 | 92.2 | 64.0 | 59.4 | 85.9 | 90.6 | - | 93.7 | 100.0 | 98.4 | 90.6 | 100.0 |
| Enterobacter cloacae complex | 112 | 62.5 | 30.4 | 30.4 | 42.9 | 51.8 | 63.4 | 71.4 | 79.5 | 80.4 | 89.3 | 79.5 |
| ertapenem-susceptible | 71 | 84.5 | 45.1 | 45.1 | 63.4 | 79.4 | - | 90.1 | 100.0 | 98.59 | 94.4 | 83.1 |
| Klebsiella aerogenes | 30 | 73.3 | 56.7 | 56.7 | 66.7 | 83.3 | 73.3 | 83.3 | 83.3 | 83.33 | 90.0 | 96.6 |
| ertapenem-susceptible | 22 | 90.9 | 77.3 | 72.7 | 86.4 | 95.4 | - | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
C/T: ceftolozane/tazobactam, CRO: ceftriaxone, CTX: cefotaxime, CAZ: ceftazidime, TZP: piperacillin/tazobactam, ETP: ertapenem, IMI: imipenem, MEM: meropenem, DOR: doripenem, TGC: tigecycline, FOS: fosfomycin. * Ceftriaxone-non-susceptible (MIC >2 mg/L) and ertapenem-susceptible (MIC <1 mg/L) were used as ESBL phenotype indicator. ** ECOFF ≤128 mg/L [22].
For Enterobacterales, in E. coli, the ESBL non-CRE phenotype was observed in 30.2% (425/1409) of the isolates and in 25.1% (153/610) of K. pneumoniae. The ertapenem-susceptible phenotype was observed in 70.3% (64/91) of S. marcescens, 63.4% (71/112) of E. cloacae complex, and 73.3% (22/30) of K. aerogenes isolates, as shown in Table 1. In addition, AmpC derepression, as indicated by resistance to at least one of the third-generation cephalosporins tested (cefotaxime, ceftriaxone, or ceftazidime) and ertapenem susceptibility, was observed in 31.9% (29/91) of S. marcescens, 28.6% (32/112) of E. cloacae complex, and 53.3% (16/30) of K. aerogenes isolates.
2.2. Activity of C/T and Comparator Agents against P. aeruginosa
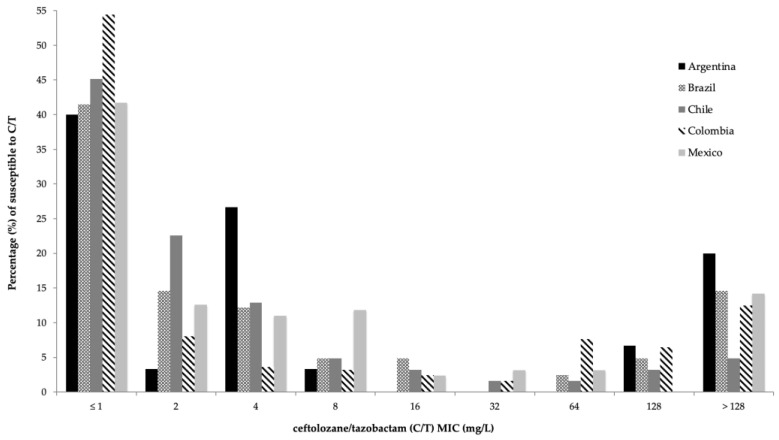
According to the current CLSI M100 guideline breakpoints, 31.9% (162/508) of the P. aeruginosa isolates were non-susceptible to C/T. Relevant phenotypic subsets and their distribution among the five Latin American countries are shown in Table 2. In general, P. aeruginosa exhibited a moderate susceptibility to C/T (68.1%; MIC50 2 mg/L, MIC90 >128 mg/L). C/T MIC values for P. aeruginosa ranged from 1 mg/L to >128 mg/L, as shown in Figure 1. C/T demonstrated better in vitro activity than any other evaluated β-lactam, including carbapenems, and was similar to fosfomycin (susceptibility: 72.2%; MIC50, 64 mg/L and MIC90, >128 mg/L; Table 1).
Table 2.
Susceptibility of P. aeruginosa clinical isolates and phenotypic subsets to C/T and comparator agents between 2016 and 2017 from five Latin American countries.
| Percentage of Susceptibility (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Organism | Number of Isolates | C/T | CAZ | TZP | IMI | MEM | DOR | FOS * | |
| Pseudomonas aeruginosa | 30 | 70.0 | 33.3 | 40.0 | 30.0 | 40.0 | 53.3 | 53.3 | |
| piperacillin/tazobactam-NS | 18 | 50.0 | 5.6 | - | 5.6 | 5.6 | 22.2 | 38.9 | |
| Argentina | meropenem-susceptible | 12 | 66.7 | 91.7 | 91.7 | 75.0 | 100.0 | 100.0 | 75.0 |
| meropenem-NS | 18 | 50.0 | 11.1 | 5.6 | 0.0 | - | 22.2 | 38.9 | |
| ceftazidime-NS | 20 | 55.0 | - | 15.0 | 20.0 | 15.0 | 35.0 | 45.0 | |
| Pseudomonas aeruginosa | 41 | 68.3 | 49.6 | 46.3 | 12.2 | 26.8 | 29.3 | 73.2 | |
| piperacillin/tazobactam-NS | 22 | 50.0 | 40.9 | - | 13.6 | 13.6 | 9.1 | 40.9 | |
| Brazil | meropenem-susceptible | 11 | 100.0 | 90.9 | 72.7 | 36.4 | 100.0 | 72.7 | 72.7 |
| meropenem-NS | 30 | 56.7 | 53.3 | 36.7 | 3.3 | - | 13.3 | 73.3 | |
| ceftazidime-NS | 15 | 33.3 | - | 13.3 | 6.7 | 6.7 | 6.7 | 66.7 | |
| Pseudomonas aeruginosa | 62 | 80.6 | 56.5 | 58.1 | 41.9 | 62.9 | 66.1 | 83.9 | |
| piperacillin/tazobactam-NS | 26 | 61.5 | 11.5 | - | 26.9 | 30.8 | 34.6 | 80.8 | |
| Chile | meropenem-susceptible | 39 | 92.3 | 76.9 | 79.5 | 64.1 | 100.0 | 97.4 | 84.6 |
| meropenem-NS | 23 | 60.9 | 21.7 | 21.7 | 4.3 | - | 13.0 | 82.6 | |
| ceftazidime-NS | 27 | 55.6 | - | 14.8 | 25.9 | 33.3 | 37.0 | 85.2 | |
| Pseudomonas aeruginosa | 248 | 66.1 | 54.8 | 58.9 | 30.2 | 47.2 | 52.4 | 80.2 | |
| piperacillin/tazobactam-NS | 102 | 23.5 | 7.8 | - | 4.9 | 9.8 | 15.7 | 76.5 | |
| Colombia | meropenem-susceptible | 117 | 96.6 | 97.5 | 103.3 | 71.5 | 100.0 | 70.8 | 65.1 |
| meropenem-NS | 131 | 38.9 | 26.7 | 29.8 | 0.8 | - | 13.7 | 73.3 | |
| ceftazidime-NS | 112 | 26.8 | - | 16.1 | 11.6 | 14.3 | 21.4 | 75.9 | |
| Pseudomonas aeruginosa | 127 | 64.4 | 49.6 | 50.4 | 25.2 | 44.9 | 42.5 | 55.1 | |
| piperacillin/tazobactam-NS | 63 | 39.7 | 6.3 | - | 14.3 | 28.6 | 27.0 | 39.7 | |
| Mexico | meropenem-susceptible | 57 | 84.2 | 64.9 | 45.6 | 56.1 | 100.0 | 86.0 | 68.4 |
| meropenem-NS | 70 | 50.0 | 37.1 | 35.7 | 0.0 | - | 7.1 | 44.3 | |
| ceftazidime-NS | 64 | 37.5 | - | 3.1 | 15.6 | 31.3 | 31.3 | 40.6 | |
C/T: ceftolozane/tazobactam, CAZ: ceftazidime, TZP: piperacillin/tazobactam, IMI: imipenem, MEM: meropenem, DOR: doripenem, FOS: fosfomycin. * ECOFF ≤ 128 mg/L [22].
Figure 1.
Susceptibility to C/T of clinical isolates of P. aeruginosa in five Latin American countries between 2016 and 2017 in relation to the minimum inhibitory concentration (MIC) to C/T. Each bar represents one of the five countries evaluated.
Susceptibility rates to C/T in the piperacillin/tazobactam-NS subset and in the ceftazidime-NS subset were particularly low (36.8% and 35.7%, respectively). Similarly, susceptibility to carbapenems was particularly low in these isolates, not exceeding 11% for meropenem in the ceftazidime-NS subset (Table 1). For these phenotypic subsets, fosfomycin showed a moderate susceptibility, ranging from 40.8% in the ceftazidime-NS subset to 62.8% in the piperacillin/tazobactam-NS subset.
When P. aeruginosa clinical isolates were analyzed by country, differences in the susceptibility rates to C/T and comparator agents arose, as seen in Figure 1 and Table 2. The highest susceptibility rates were found in Chile (80.6%; MIC50 2 mg/L, MIC90 32 mg/L), followed by Argentina (70%; MIC50 4 mg/L, MIC90 > 128 mg/L), Brazil (68.3%; MIC50 2 mg/L, MIC90 > 128 mg/L), Colombia (66.1%; MIC50 < 1 mg/L, MIC90 > 128 mg/L) and finally, Mexico (64.4%; MIC50 2 mg/L, MIC90 > 128 mg/L).
2.3. Activity of C/T and Comparator Agents against Enterobacterales
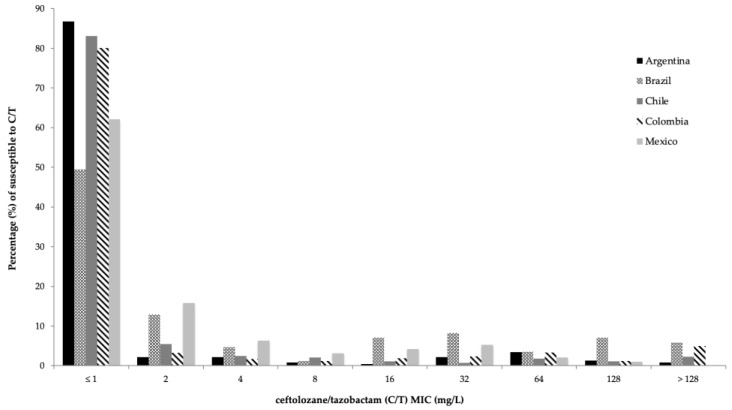
The distribution of the 2252 clinical isolates of Enterobacterales within each relevant phenotypic subset, and their susceptibility to C/T and comparator antimicrobials, are shown in Figure 2 and Table 1. Overall, C/T displayed a good activity against Enterobacterales, with activity against 73.8% (1662/2252) of the isolates. As shown in Figure 2, C/T MIC values ranged from <1 mg/L to >128 mg/L, with MIC50 and MIC90 being 1 mg/L and 32 mg/L, respectively. The highest susceptibility rates to C/T among Enterobacterales were found in E. coli (93.2%; MIC50 1 mg/L, MIC90 1 mg/L), followed by K. aerogenes (73.3%; MIC50 1 mg/L, MIC90 16 mg/L), S. marcescens (71.4%; MIC50 1 mg/L, MIC90 64 mg/L), K. pneumoniae (68.7%; MIC50 1 mg/L, MIC90 128 mg/L) and finally, the E. cloacae complex (62.5%; MIC50 1 mg/L, MIC90 32 mg/L).
Figure 2.
Susceptibility to C/T of clinical isolates of Enterobacterales in five Latin American countries between 2016 and 2017 in relation to the minimum inhibitory concentration (MIC) to C/T. Each bar represents one of the five countries evaluated.
In comparison to other antimicrobial agents, C/T demonstrated higher activity than currently available cephalosporins (susceptibility: 58.8% for ceftazidime, 47.7% for ceftriaxone and 47.6% for cefotaxime), and even piperacillin/tazobactam (susceptibility 70.8%). On the other hand, C/T activity was similar to ertapenem’s (susceptibility 73.5%), but inferior to other carbapenems (susceptibility to doripenem 82.8%, to meropenem 82.6% and imipenem 78.7%). In contrast, tigecycline (87.9%) and fosfomycin (91.6%) susceptibility was higher than C/T (73.8%).
When data were stratified by species, doripenem showed the highest susceptibility rates against E. coli (95.7%), while fosfomycin was the most active in vitro antimicrobial agent against K. pneumoniae, S. marcescens and K. aerogenes (susceptibility: 92.5%, 94.5% and 96.7%, respectively). Tigecycline was the most active antimicrobial drug against E. cloacae complex (susceptibility 89.3%), as shown in Table 1.
As shown in Table S2, susceptibility rates of Enterobacterales to C/T and comparator antimicrobial agents varied considerably among the five Latin American countries included in this study. In general terms, susceptibility to C/T reached 61.3% in Brazil, 64.3% in Mexico, 71.6% in Colombia, 85.6% in Chile and 88.6% in Argentina. MIC frequency distribution of C/T for all Enterobacterales, in every participating country, is shown in Figure 1.
Evaluating each species individually, C/T showed the best activity rates against E. coli, with susceptibility ranging between 80% (Brazil) and 95.6% (Argentina). For K. pneumoniae, this antimicrobial showed a lower activity, not surpassing a susceptibility rate of 80% (in Mexico). For both species, C/T performed better than ceftazidime and piperacillin/tazobactam in all five countries. Despite the variability among countries, C/T performed similarly to carbapenems, tigecycline and fosfomycin in E. coli. On the other hand, carbapenems, tigecycline and fosfomycin displayed better activity than C/T against K. pneumoniae. For E. cloacae complex, K. aerogenes and S. marcescens susceptibility rates to C/T and comparator agents varied greatly among the five evaluated countries. Detailed information for each pathogen, their susceptibility rates, relevant phenotypic subsets and their distribution among the five countries is displayed in Table S2.
3. Discussion
The potent combination of C/T was conceived to circumvent the therapeutic challenges imposed by the concomitant presence of the Pseudomonas-derived cephalosporinase (PDC), ESBLs and intrinsic efflux pump systems [5,16,23,24]. Moreover, C/T also has potent activity against Enterobacterales strains, carrying widely spread ESBLs and AmpC β-lactamases, such as CTX-M-15 and CMY-2, respectively. Therefore, C/T constitutes a carbapenem-sparing option for the clinical treatment of infections caused by these common pathogens. Importantly, C/T lacks activity against all carbapenemases [16,25,26]. Unfortunately, resistance to C/T dramatically narrows treatment options for P. aeruginosa, and despite possible susceptibility to fosfomycin, this antimicrobial has several clinical restrictions, and are limited to combination therapy regimens [27,28].
The results presented here are important for Latin America given the extended dissemination of antimicrobial resistance in this geographical area [21,29,30,31], the endemicity of carbapenem-resistant bacteria in some of these countries [21,32,33], and the limited availability of effective antibiotic therapies for MDR P. aeruginosa and Enterobacterales [34,35]. Epidemiological studies surveying the resistant status of C/T against a set of other antimicrobial agents for nosocomial pathogens retrieve important information that allows for the determination of country-specific and even institution-specific activity of antimicrobial drugs, allowing clinicians to improve empiric therapy, as well as allowing for the design of effective antimicrobial stewardship strategies.
Compared with similar studies carried out in previous years [20], we found a decrease in the susceptibility of C/T in P. aeruginosa. Indeed, during the period between 2013 and 2015, susceptibility of this pathogen to C/T was reported in 82.4%, while our results show a susceptibility decrease to 68.1%. Pfaller et al. surveyed 12 hospitals (vs. 20 in our study) in 4 countries (not including Colombia), reporting a higher susceptibility rate to C/T. The lower susceptibilities to C/T found in Colombia might contribute to this result. Several publications of P. aeruginosa strains in Colombia reported the production of carbapenemases, such as KPC and VIM, and even co-resistance of KPC/VIM [21,32,33]. This difference, added to the dissemination of other carbapenem resistance determinants among P. aeruginosa and Enterobacterales strains in Latin America, might have contributed to the decreased C/T susceptibility reported in this study. Our data also showed an important reduction in C/T susceptibility when compared to the global study reported from 2015 to 2017 by Shortridge et al. [13], where the susceptibility to C/T in the Latin American region (represented by isolates from Colombia and Mexico) was found to be 90.8%. Furthermore, several studies have reported a significant increase in the VIM carbapenemase in Mexico, as recently reviewed [21]. Regional differences in the presence of β-lactam resistance determinants, including ESBL and carbapenemases [13,16,17,20,26,28,36,37,38,39,40,41], may explain the differences between studies. Therefore, the understanding of the molecular mechanisms involved in the resistant phenotypes and the decrease in susceptibility to C/T in Latin America, particularly for P. aeruginosa, is fundamental to improve therapeutic and stewardship strategies in this geographical region.
Despite the lower susceptibility reported in our study, C/T is still the most active β-lactam antibiotic against P. aeruginosa. Likewise, our study confirms that C/T is highly active against Enterobacterales, with similar susceptibility rates to carbapenems for E. coli and S. marcescens, and slightly lower rates for K. pneumoniae, E. cloacae complex, and K. aerogenes. Our data support the idea that C/T could provide a reasonable therapeutic option for Latin American hospitals with high rates of MDR P. aeruginosa and ESBL-producing Enterobacterales [41].
In particular, it is important to highlight that the susceptibility to C/T in β-lactam resistant P. aeruginosa, such as meropenem-NS, was particularly low, with a mean value of 46.7%, and varying among countries (Chile 60.9% and Colombia 38.9%). These resistant phenotypes represented 53.5% of all P. aeruginosa isolates in this Latin American survey. Molecular analyses are underway to determine the mechanisms of resistance, such as mutations leading to structural modifications and/or overexpression of AmpC, OprD loss, PDC upregulation, the presence of carbapenemases, or amino acid substitutions, insertions or deletions found in PDC variants [24,26,42,43]. These results also highlight the imperative need for routine susceptibility testing prior to its use.
The results from this study also show the importance of frequent regional epidemiological surveys for new therapeutic options, due to the dynamic resistance of P. aeruginosa and Enterobacterales.
4. Materials and Methods
4.1. Sampling Sites and Organisms
A total of 2760 GNB clinical isolates, including Escherichia coli (n = 1409, 51%), Klebsiella pneumoniae ss. pneumoniae (n = 610, 22%), Enterobacter cloacae (n = 112, 4%), Serratia marcescens (n = 91, 3%), Klebsiella aerogenes (n = 30, 1%) and P. aeruginosa (n = 508, 18%), were collected in 5 Latin American countries (Argentina, Brazil, Chile, Colombia and Mexico) at 20 medical facilities during the study period, from January 2016 to October 2017, prior to the approval of C/T in this region. Species identification was performed locally at each participating medical center and reidentified at Clínica Imbanaco (Cali, Colombia) using MALDI-TOF MS (BioMérieux, Marcy-l’Étoile, France). The list of the principal species tested against C/T by country, is presented in Table S1.
4.2. Antimicrobial Susceptibility Testing
Determination of minimum inhibitory concentrations (MIC) was performed using broth microdilution with customized Sensititre plates (TREK Diagnostic Systems, Westlake, OH, USA), and following the CLSI M100 guidelines 2020 [44], where C/T breakpoints are ≤2 mg/L for Enterobacterales and ≤4 mg/L for P. aeruginosa. These breakpoints were determined based on a C/T dosage of 3 g q 8 h for pneumonia, and of 1.5 g q 8 h for any other indication for both Enterobacterales and P. aeruginosa, according to the CLSI guidelines [44]. C/T concentrations are expressed as absolute numbers representing only the concentration of ceftolozane, given that tazobactam remains constant in 4 mg/L. Quality control (QC) was performed in accordance to the CLSI M07-A10 and M100-S27 documents, using the following strains: E. coli ATCC 25922 and P. aeruginosa ATCC 27853. Except for fosfomycin and tigecycline, results were interpreted according to the CLSI M100 breakpoints [44]. Fosfomycin susceptibility results were interpreted according to available breakpoints set by CLSI (susceptible at an MIC of ≤64 mg/L for E. coli and extrapolated to other Enterobacterales) and EUCAST for P. aeruginosa (ECOFF of ≤128 mg/L) [22]. The U.S. FDA product package insert criteria were used as the breakpoint for tigecycline [22,44]. Colistin was not considered as a comparator agent in this study, since there are many conflicting results; Sensititre plates have shown a high rate of false-resistant results [45] and this method is not recommended by the CLSI or EUCAST for antimicrobial susceptibility testing with this antibiotic.
4.3. Phenotypic Subsets
Isolates belonging to the order of Enterobacterales were classified in phenotypic subsets based on their MIC profile, as follows: ESBL non-CRE phenotype was defined as E. coli or K. pneumoniae isolates, displaying a MIC ≥ 2 mg/L for ceftriaxone and MIC < 1 mg/L for ertapenem. In addition, AmpC producers (Serratia marcescens, Enterobacter cloacae complex, and Klebsiella aerogenes) were classified as ertapenem-susceptible (MIC < 1 mg/L) and cefotaxime-resistant (MIC ≥ 4 mg/L). P. aeruginosa isolates were classified as piperacillin/tazobactam-non-susceptible (NS) (MIC ≥ 32 mg/L), meropenem-susceptible (MIC ≤ 2 mg/L), meropenem-NS (MIC ≥ 4 mg/L) and ceftazidime-NS (MIC ≥ 16 mg/L).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11081101/s1, Table S1: List of the principal species tested against C/T by country in five Latin American countries between 2016 and 2017; Table S2: List of the principal species tested against C/T by country in five Latin American countries between 2016 and 2017.
Author Contributions
Conceptualization, M.V.V., E.D.L.C., M.F.M. and C.H.-G.; methodology, M.V.V., E.D.L.C., M.F.M. and C.H.-G.; validation, J.C.G.-B., E.D.L.C. and M.F.M.; formal analysis, J.C.G.-B., M.V.V., E.D.L.C., M.F.M., A.C.G. and J.M.M.; investigation, J.C.G.-B., M.V.V., E.D.L.C. and M.F.M.; data curation, E.D.L.C. and J.C.G.-B.; writing—original draft preparation, J.C.G.-B.; writing—review and editing, J.C.G.-B., M.V.V., E.D.L.C., M.F.M., A.C.G., A.C., M.A.R., P.C.-M., D.A.J.-V. and J.M.M.; supervision, M.V.V.; project administration, E.D.L.C.; funding acquisition, M.V.V., E.D.L.C., M.F.M. and C.H.-G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
As this study did not involve human or animal testing, neither the access to any clinical record, it did not require ethical approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. It is not publicly available due to the presence of unpublished data on the original databases.
Conflicts of Interest
C.H.-G. is currently employed by MSD. J.M.M. received funding from FONDECYT #1211947 from the Agencia Nacional de Investigation y Desarrollo (ANID), Government of Chile. M.V.V. have received consulting fees from MSC, Pfizer; WEST, and BioMérieux. All other authors declare no conflict of interest.
Funding Statement
This research was funded by Merck Sharp & Dohme (MSD), grant number 10020230.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kadri S.S., Adjemian J., Lai Y.L., Spaulding A.B., Ricotta E., Prevots D.R., Palmore T.N., Rhee C., Klompas M., Dekker J.P., et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: Retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin. Infect. Dis. 2018;67:1803–1814. doi: 10.1093/cid/ciy378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silver L.L. Challenges of antibacterial discovery. Clin. Microbiol. Rev. 2011;24:71–109. doi: 10.1128/CMR.00030-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rizzo K., Horwich-Scholefield S., Epson E. Carbapenem and cephalosporin resistance among enterobacteriaceae in healthcare- associated infections, california, usa1. Emerg. Infect. Dis. 2019;25:1389–1396. doi: 10.3201/eid2507.181938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pachori P., Gothalwal R., Gandhi P. Emergence of antibiotic resistance Pseudomonas aeruginosa in intensive care unit; a critical review. Genes Dis. 2019;6:109–119. doi: 10.1016/j.gendis.2019.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sucher A.J., Chahine E.B., Cogan P., Fete M. Ceftolozane/Tazobactam: A New Cephalosporin and β-Lactamase Inhibitor Combination. Ann. Pharmacother. 2015;49:1046–1056. doi: 10.1177/1060028015593293. [DOI] [PubMed] [Google Scholar]
- 6.Moya B., Zamorano L., Juan C., Pérez J.L., Ge Y., Oliver A. Activity of a new cephalosporin, CXA-101 (FR264205), against β-lactam-resistant Pseudomonas aeruginosa mutants selected in vitro and after antipseudomonal treatment of intensive care unit patients. Antimicrob. Agents Chemother. 2010;54:1213–1217. doi: 10.1128/AAC.01104-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murano K., Yamanaka T., Toda A., Ohki H., Okuda S., Kawabata K., Hatano K., Takeda S., Akamatsu H., Itoh K., et al. Structural requirements for the stability of novel cephalosporins to AmpC β-lactamase based on 3D-structure. Bioorganic Med. Chem. 2008;16:2261–2275. doi: 10.1016/j.bmc.2007.11.074. [DOI] [PubMed] [Google Scholar]
- 8.Toda A., Ohki H., Yamanaka T., Murano K., Okuda S., Kawabata K., Hatano K., Matsuda K., Misumi K., Itoh K., et al. Synthesis and SAR of novel parenteral anti-pseudomonal cephalosporins: Discovery of FR264205. Bioorganic Med. Chem. Lett. 2008;18:4849–4852. doi: 10.1016/j.bmcl.2008.07.085. [DOI] [PubMed] [Google Scholar]
- 9.Jean S.S., Chang Y.C., Lin W.C., Lee W.S., Hsueh P.R., Hsu C.W. Epidemiology, treatment, and prevention of nosocomial bacterial pneumonia. J. Clin. Med. 2020;9:275. doi: 10.3390/jcm9010275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong M.C., Hsu D.I., Bounthavong M. Ceftolozane/tazobactam: A novel antipseudomonal cephalosporin and β-lactamase-inhibitor combination. Infect. Drug Resist. 2013;6:215–223. doi: 10.2147/IDR.S36140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giancola S.E., Mahoney M.V., Bias T.E., Hirsch E.B. Critical evaluation of ceftolozane–tazobactam for complicated urinary tract and intra-abdominal infections. Ther. Clin. Risk Manag. 2016;12:787–797. doi: 10.2147/TCRM.S83844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magiorakos A.P., Srinivasan A., Carey R.B., Carmeli Y., Falagas M.E., Giske C.G., Harbarth S., Hindler J.F., Kahlmeter G., Olsson-Liljequist B., et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012;18:268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- 13.Shortridge D., Pfaller M.A., Streit J.M., Flamm R.K. Antimicrobial activity of ceftolozane/tazobactam tested against contemporary (2015–2017) Pseudomonas aeruginosa isolates from a global surveillance programme. J. Glob. Antimicrob. Resist. 2020;21:60–64. doi: 10.1016/j.jgar.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 14.van Duin D., Bonomo R.A. Ceftazidime/Avibactam and Ceftolozane/Tazobactam: Second-generation β-Lactam/β-Lactamase Inhibitor Combinations. Clin Infect Dis. 2016;63:234–241. doi: 10.1093/cid/ciw243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright H., Bonomo R.A., Paterson D.L. New agents for the treatment of infections with Gram-negative bacteria: Restoring the miracle or false dawn? Clin. Microbiol. Infect. 2017;23:704–712. doi: 10.1016/j.cmi.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Teo J.Q.-M., Lim J.C., Tang C.Y., Lee S.J.Y., Tan S.H., Sim J.H.C., Ong R.T.-H., Kwa A.L.H. Ceftolozane/Tazobactam Resistance and Mechanisms in Carbapenem-Nonsusceptible Pseudomonas aeruginosa. mSphere. 2021;6:e01026-20. doi: 10.1128/mSphere.01026-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sader H.S., Farrell D.J., Castanheira M., Flamm R.K., Jones R.N. Antimicrobial activity of ceftolozane/tazobactam tested against Pseudomonas aeruginosa and Enterobacteriaceae with various resistance patterns isolated in European hospitals (2011-12) J. Antimicrob. Chemother. 2014;69:2713–2722. doi: 10.1093/jac/dku184. [DOI] [PubMed] [Google Scholar]
- 18.Walkty A., Karlowsky J.A., Adam H., Baxter M., Lagacé-Wiens P., Hoban D.J., Zhanel G.G. In vitro activity of ceftolozane-tazobactam against Pseudomonas aeruginosa isolates obtained from patients in Canadian hospitals in the CANWARD study, 2007 to 2012. Antimicrob. Agents Chemother. 2013;57:5707–5709. doi: 10.1128/AAC.01404-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farrell D.J., Sader H.S., Flamm R.K., Jones R.N. Ceftolozane/tazobactam activity tested against Gram-negative bacterial isolates from hospitalised patients with pneumonia in US and European medical centres (2012) Int. J. Antimicrob. Agents. 2014;43:533–539. doi: 10.1016/j.ijantimicag.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 20.Pfaller M.A., Shortridge D., Sader H.S., Gales A., Castanheira M., Flamm R.K. Ceftolozane-tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing healthcare-associated infections in Latin America: Report from an antimicrobial surveillance program (2013–2015) Braz. J. Infect. Dis. 2017;21:627–637. doi: 10.1016/j.bjid.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.García-Betancur J.C., Appel T.M., Esparza G., Gales A.C., Levy-Hara G., Cornistein W., Vega S., Nuñez D., Cuellar L., Bavestrello L., et al. Update on the epidemiology of carbapenemases in Latin America and the Caribbean. Expert Rev. Anti. Infect. Ther. 2021;19:197–213. doi: 10.1080/14787210.2020.1813023. [DOI] [PubMed] [Google Scholar]
- 22.The European Committee on Antimicrobial Susceptibility Testing Breakpoint Tables for Interpretation of MICs and Zone Diameters-EUCAST. [(accessed on 13 March 2022)]. Available online: http://www.eucast.org.
- 23.Fernández-Esgueva M., López-Calleja A.I., Mulet X., Fraile-Ribot P.A., Cabot G., Huarte R., Rezusta A., Oliver A. Characterization of AmpC β-lactamase mutations of extensively drug-resistant Pseudomonas aeruginosa isolates that develop resistance to ceftolozane/tazobactam during therapy. Enferm. Infecc. Microbiol. Clin. 2020;38:474–478. doi: 10.1016/j.eimc.2020.01.017. [DOI] [PubMed] [Google Scholar]
- 24.Fournier D., Carrière R., Bour M., Grisot E., Triponney P., Muller C., Lemoine J., Jeannot K., Plésiat P., GERPA Study Group Mechanisms of resistance to ceftolozane/tazobactam in pseudomonas aeruginosa: Results of the GERPA multicenter study. Antimicrob. Agents Chemother. 2021;65:e01117-20. doi: 10.1128/AAC.01117-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wi Y.M., Greenwood-Quaintance K.E., Schuetz A.N., Ko K.S., Peck K.R., Song J.H., Patel R. Activity of Ceftolozane-Tazobactam against Carbapenem- Resistant, Non-Carbapenemase-Producing Pseudomonas aeruginosa and Associated Resistance Mechanisms. Antimicrob. Agents Chemother. 2018;62:e01970-17. doi: 10.1128/AAC.01970-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hirsch E.B., Brigman H.V., Zucchi P.C., Chen A., Anderson J.C., Eliopoulos G.M., Cheung N., Gilbertsen A., Hunter R.C., Emery C.L., et al. Ceftolozane-tazobactam and ceftazidime-avibactam activity against β-lactam-resistant Pseudomonas aeruginosa and extended-spectrum β-lactamase-producing Enterobacterales clinical isolates from U.S. medical centres. J. Glob. Antimicrob. Resist. 2020;22:689–694. doi: 10.1016/j.jgar.2020.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Shiju K.S., Pallam G., Mandal J., Jindal B., Kumaravel S. Use of fosfomycin combination therapy to treat multidrug-resistant urinary tract infection among paediatric surgical patients–a tertiary care centre experience. Access Microbiol. 2020;2:10–12. doi: 10.1099/acmi.0.000163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lob S.H., DePestel D.D., DeRyke C.A., Kazmierczak K.M., Young K., Motyl M.R., Sahm D.F. Ceftolozane/Tazobactam and Imipenem/Relebactam Cross-Susceptibility among Clinical Isolates of Pseudomonas aeruginosa from Patients with Respiratory Tract Infections in ICU and Non-ICU Wards-SMART United States 2017–2019. Open Forum Infect. Dis. 2021;8:ofab320. doi: 10.1093/ofid/ofab320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Casellas J.M. Resistencia a los antibacterianos en América Latina: Consecuencias para la infectología. Rev. Panam. Salud Publica/Pan Am. J. Public Heal. 2011;30:519–528. [PubMed] [Google Scholar]
- 30.Moreno-Switt A.I., Rivera D., Caipo M.L., Nowell D.C., Adell A.D. Antimicrobial Resistance in Water in Latin America and the Caribbean: Available Research and Gaps. Front. Vet. Sci. 2020;7:1–13. doi: 10.3389/fvets.2020.00546. [DOI] [Google Scholar]
- 31.Rojas L.J., Weinstock G.M., De La Cadena E., Diaz L., Rios R., Hanson B.M., Brown J.S., Vats P., Phillips D.S., Nguyen H., et al. An analysis of the epidemic of klebsiella pneumoniae carbapenemase-producing k. pneumoniae: Convergence of two evolutionary mechanisms creates the ‘perfect storm.’ J. Infect. Dis. 2018;217:82–92. doi: 10.1093/infdis/jix524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Correa A., Montealegre M.C., Mojica M.F., Maya J.J., Rojas L.J., De La Cadena E.P., Ruiz S.J., Recalde M., Rosso F., Quinn J.P., et al. First report of a Pseudomonas aeruginosa isolate coharboring KPC and VIM carbapenemases. Antimicrob. Agents Chemother. 2012;56:5422–5423. doi: 10.1128/AAC.00695-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Escandón-Vargas K., Reyes S., Gutiérrez S., Villegas M.V. The epidemiology of carbapenemases in Latin America and the Caribbean. Expert Rev. Anti. Infect. Ther. 2017;15:277–297. doi: 10.1080/14787210.2017.1268918. [DOI] [PubMed] [Google Scholar]
- 34.Losito A.R., Raffaelli F., del Giacomo P., Tumbarello M. New Drugs for the Treatment of Pseudomonas aeruginosa Infections with Limited Treatment Options: A Narrative Review. Antibiotics. 2022;11:579. doi: 10.3390/antibiotics11050579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coyne A.J.K., el Ghali A., Holger D., Rebold N., Rybak M.J. Therapeutic Strategies for Emerging Multidrug-Resistant Pseudomonas aeruginosa. Infect. Dis. Ther. 2022;11:661–682. doi: 10.1007/s40121-022-00591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pfaller M.A., Shortridge D., Sader H.S., Castanheira M., Flamm R.K. Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing healthcare-associated infections in the Asia-Pacific region (minus China, Australia and New Zealand): Report from an Antimicrobial Surveillance Pr. Int. J. Antimicrob. Agents. 2018;51:181–189. doi: 10.1016/j.ijantimicag.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 37.Livermore D.M., Mushtaq S., Meunier D., Hopkins K.L., Hill R., Adkin R., Chaudhry A., Pike R., Staves P., Woodford N., et al. Activity of ceftolozane/tazobactam against surveillance and ‘problem’ Enterobacteriaceae, Pseudomonas Aeruginosa and non-fermenters from the British Isles. J. Antimicrob. Chemother. 2017;72:2278–2289. doi: 10.1093/jac/dkx136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karlowsky J.A., Lob S.H., Young K., Motyl M.R., Sahm D.F. Activity of ceftolozane/tazobactam against Gram-negative isolates from patients with lower respiratory tract infections–SMART United States 2018–2019. BMC Microbiol. 2021;21:4–11. doi: 10.1186/s12866-021-02135-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yin D., Wu S., Yang Y., Shi Q., Dong D., Zhu D., Hu F. Results from the China Antimicrobial Surveillance Network (CHINET) in 2017 of the In Vitro Activities of Ceftazidime-Avibactam and Ceftolozane-Tazobactam against Clinical Isolates of Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2019;63:e02431-18. doi: 10.1128/AAC.02431-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pfaller M.A., Shortridge D., Sader H.S., Flamm R.K., Castanheira M. Ceftolozane–tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing healthcare-associated infections in Australia and New Zealand: Report from an Antimicrobial Surveillance Program (2013–2015) J. Glob. Antimicrob. Resist. 2017;10:186–194. doi: 10.1016/j.jgar.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 41.Pfaller M.A., Bassetti M., Duncan L.R., Castanheira M. Ceftolozane/tazobactam activity against drug-resistant Enterobacteriaceae and Pseudomonas aeruginosa causing urinary tract and intraabdominal infections in Europe: Report from an antimicrobial surveillance programme (2012-15) J. Antimicrob. Chemother. 2017;72:1386–1395. doi: 10.1093/jac/dkx009. [DOI] [PubMed] [Google Scholar]
- 42.Castanheira M., Mills J.C., Farrell D.J., Jones R.N. Mutation-Driven β-Lactam resistance mechanisms among contemporary ceftazidime-nonsusceptible pseudomonas aeruginosa isolates from U.S. hospitals. Antimicrob. Agents Chemother. 2014;58:6844–6850. doi: 10.1128/AAC.03681-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grupper M., Sutherland C., Nicolau D.P. Multicenter Evaluation of CeftazidimeAvibactam and Ceftolozane-Tazobactam Inhibitory Activity against MeropenemNonsusceptible Pseudomonas aeruginosa from Blood, Respiratory Tract, and Wounds. Antimicrob. Agents Chemother. 2017;61:e00875-17. doi: 10.1128/AAC.00875-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weinstein M.P., Kim T.J., Jr., Lewis J.S., II, Limbago B., Bobenchik A.M., Mathers A.J., Campeau S., Mazzulli T., Cullen S.K., Satlin M., et al. Performance Standards for Antimicrobial Testing; CLSI Supplement M100. 30th ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2020. [Google Scholar]
- 45.Pfennigwerth N., Kaminski A., Korte-Berwanger M., Pfeifer Y., Simon M., Werner G., Jantsch J., Marlinghaus L., Gatermann S.G. Evaluation of six commercial products for colistin susceptibility testing in Enterobacterales. Clin. Microbiol. Infect. 2019;25:1385–1389. doi: 10.1016/j.cmi.2019.03.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. It is not publicly available due to the presence of unpublished data on the original databases.