Abstract
The susceptibility to gentamicin of N. gonorrhoeae isolates collected in three Chinese provinces and the correlation among the MICs of gentamicin, azithromycin, and ceftriaxone were investigated in this study. The effects of combinations from those three antibiotics were also in the scope of this study to determine the efficacy of gentamicin as a combination therapeutic drug. The agar dilution method was used to measure the minimum inhibitory concentrations (MICs) of ceftriaxone, azithromycin and gentamicin on N. gonorrhoeae isolates. The synergy between these three antimicrobials were determined using the agar dilution checkerboard method. Subgroup studies were conducted to explore differences between azithromycin- and ceftriaxone-sensitive and resistant isolates. A total of 139 (36.60%) and 233 (61.30%) isolates demonstrated full susceptibility and intermediate susceptibility to gentamicin, respectively. The correlation analysis showed that the MICs of ceftriaxone and azithromycin weakly correlated with the value of gentamicin. The overall results of the three antibiotic combinations revealed indifferent effects. Combination therapy established a significant reduction on the MIC value. Most of the N. gonorrhoeae isolates tested in this study demonstrated a certain degree of susceptibility to gentamicin. Overall, antimicrobial combinations of gentamicin with ceftriaxone or azithromycin demonstrate indifferent effects.
Keywords: Neisseria gonorrhoeae, synergy, gentamicin
1. Introduction
The pathogen Neisseria gonorrhoeae (N. gonorrhoeae) is responsible for gonorrhea, which induces urogenital, pharyngeal, or rectal mucosa infections in sexual transmission [1]. In 2016, a study released by the World Health Organization (WHO) estimated that there were 86.9 million gonorrhea cases worldwide among adults aged 15 to 49 years old [2]. Antibiotics are now the mainstay of therapy for N. gonorrhoeae infection [3]. Treatment guidelines developed in the United States, Europe, and by the WHO recommend dual therapy with azithromycin and ceftriaxone for the treatment of gonorrhea [4,5,6]. Notably, since the antibiotics susceptibility of N. gonorrhoeae is declining over time, reports of instances of multidrug-resistant (MDR) N. gonorrhoeae have been frequent in many countries [7,8,9]. Thus, detecting plausible alternative antibiotics and searching for novel treatment options are critical to hindering the progress of N. gonorrhoeae antibiotic resistance [10].
Gentamicin is a widely used aminoglycoside that inhibits bacterial protein synthesis in gram-negative bacteria by directly binding to the decoding A site of the bacterial 30S ribosomal subunit [11]. Gentamicin is currently used as an alternative therapy to ceftriaxone in the US, Europe, and according to the WHO guidelines [4,6,12]. In Malawi, the combination of gentamicin with doxycycline as first-line therapy has been applied to treat genitourinary infections caused by N. gonorrhoeae for nearly 30 years [13]. In China, gentamicin’s in vitro activity against N. gonorrhoeae was investigated by Liu et.al in 2017, which showed that 85.9% of isolates were fully sensitive to gentamicin [14]. However, in a meta-analysis, the combined cure rate of single-dose gentamicin treatment was only 91.5% [15]. In another clinical study, the combination of gentamicin with azithromycin elicited a 100.0% cure rate in patients with uncomplicated gonorrhea [16]. Therefore, gentamicin is suggested to be more appropriate as an antimicrobial agent in a dual treatment regimen rather than as first-line empirical monotherapy [17]. Gentamicin can help decrease the progression of drug resistance when used in combination with ceftriaxone or azithromycin [18].
To promote gentamicin as an alternative antibiotic in China for N. gonorrhoeae infection, monitoring the susceptibility of N. gonorrhoeae isolates in China to gentamicin and antimicrobial combination testing for gentamicin with other antibiotics can be of great interest. In this in vitro study, the susceptibility to gentamicin of N. gonorrhoeae collected in three Chinese provinces from 2019 to 2020 was evaluated and an analysis of the correlation among the MICs of gentamicin, azithromycin and ceftriaxone was established. Ultimately, the effects of the three antimicrobial drug combinations were also investigated to determine the effectiveness of gentamicin in a combination drug therapy.
2. Methods
2.1. N. gonorrhoeae Isolates
From December 2019 to December 2020, 380 clinical strains of N. gonorrhoeae isolates were collected in three Chinese provinces: Tianjin (n = 110), Xinjiang (n = 167), and Zhejiang (n = 103)). All of the strains were previously determined to be N. gonorrhoeae through standardized methodologies [19]. The Medical Ethics Committee at the Institute of Dermatology, the Chinese Academy of Medical Sciences & Peking Union Medical College and the National Center for Sexually Transmitted Disease Control all gave their approval to this project (2014-LS-026). This Declaration of Helsinki guidelines were followed in this study. Study participants signed an informed consent form before inclusion in the study. Before the antimicrobial agent susceptibility tests, all of the strains were preserved in skim milk at −80 °C. The WHO reference strains G, P, O, J, and K were used as quality controls for MIC determinations.
2.2. Antimicrobial Susceptibility Testing
The antimicrobial susceptibility of all isolates to ceftriaxone, azithromycin, and gentamicin was evaluated using the WHO’s standard agar dilution method [19]. The drugs were obtained from Sigma Aldrich. Two operators independently read the results on the antibiotic plate at the same time, and in the case of a discrepancy, a third experimental supervisor made the result determination. We classified azithromycin’s MIC into susceptibility (MIC ≤ 0.5 mg/L) or resistance (MIC ≥ 1.0 mg/L), and that of ceftriaxone into susceptibility (MIC ≤ 0.125 mg/L) or resistance (MIC ≥ 0.25 mg/L). The criteria for azithromycin and ceftriaxone susceptibility and resistance were interpreted based on the Clinical and Laboratory standards Institute (CLSI) M100-S29 breakpoints [20]. According to previous studies and interpretation criteria, the breakpoint for gentamicin MIC was set to be ≤4 mg/L as fully susceptible, 8 to 16 mg/L as intermediately susceptible, and ≥32 mg/L as resistant [14,21].
2.3. Synergy Testing
To test the synergy between these three antimicrobials, the agar dilution checkboard method was used [22]. Gentamicin (0.5–32 mg/L in 7 two-fold dilutions) and azithromycin (0.015–8 mg/L in 10 two-fold dilutions), gentamicin (0.5–32 mg/L) and ceftriaxone (0.004–0.5 mg/L), azithromycin (0.015–8 mg/L) and ceftriaxone (0.004–0.5 mg/L) were added to the antimicrobial medium separately. The rest of the procedure was identical to the antimicrobial susceptibility testing.
2.4. Statistical Analysis
Descriptive statistics were used to characterize the MIC distributions. Furthermore, following logarithmic conversion of the MIC values, the correlation coefficient R was used to identify connections between the MIC of various antibiotics. Poor, medium and strong correlations correspond to R values in the range of 0.3–0.5, 0.5–0.8 and 0.8–1, respectively.
The fractional inhibitory concentration index (FICI) was used to assess the interactions. The FICI was calculated as (CA/MICA) plus (CB/MICB), where MICA and MICB are the individual MICs of antibiotics A and B, and CA and CB are their combined MICs, corresponding to the lowest FICI (or highest FICI, in the case of antagonism). When the FICI was less than 0.5; the interaction was categorized as synergistic; between 0.5 and 4.0, it was classified as indifferent; and when the FICI was greater than 4.0, the interaction was classified as antagonistic [23,24]. The numbers of synergistic, indifferent or antagonistic interactions were counted and their ratios were calculated.
Results were stratified into groups based on the MIC of azithromycin and ceftriaxone: ≤0.5 mg/L, or ≥1 mg/L for the azithromycin groups and ≤0.125 mg/L or ≥0.25 mg/L for the ceftriaxone groups. This stratification was designed to explore differences between sensitive and resistant isolates. The geometric means (GM) of MICs and FICIs were calculated. The non-parametric Mann-Whitney U test was implemented to examine the differences between MICs of three aforementioned antimicrobials in monotherapy and combination therapy.
3. Results
3.1. Antimicrobial Susceptibility Results of 380 N. gonorrhoeae Isolates
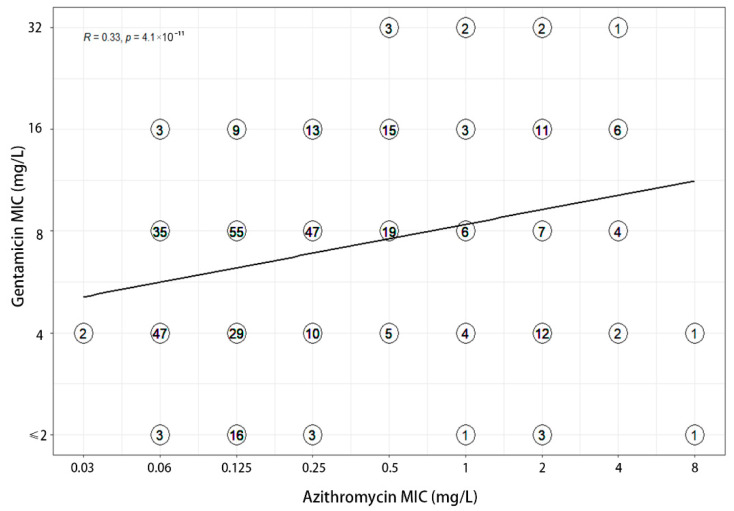
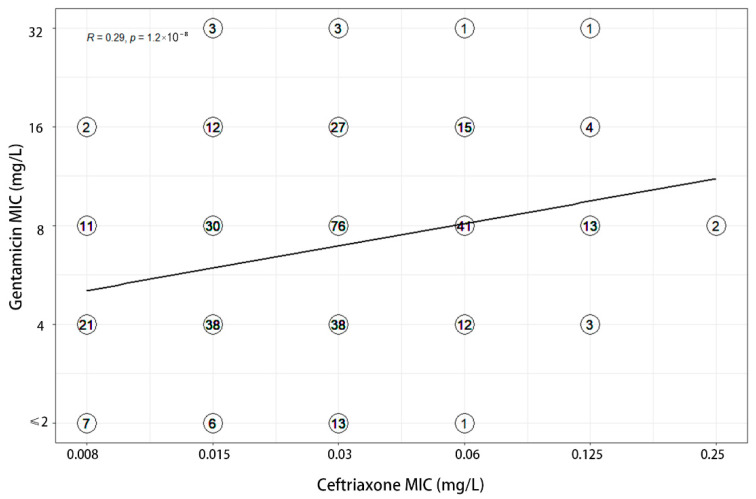
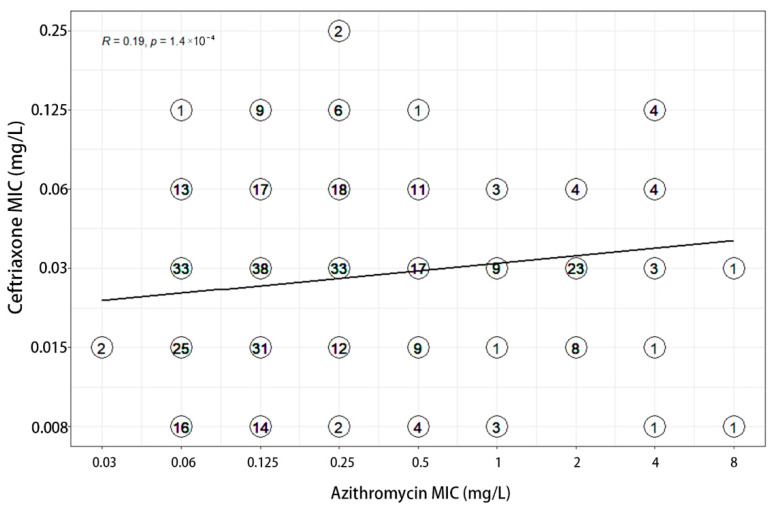
MIC values of three antimicrobials were recorded for each of the 380 clinical isolates (Table 1). MICs of gentamicin ranged from 1 to 32 mg/L, with MIC50 and MIC90 values of 8 and 16 mg/L respectively. A total of 139 (36.60%) and 233 (61.30%) isolates demonstrated full susceptibility and intermediate susceptibility to gentamicin, accordingly. Among the 66 azithromycin-resistant strains, 56.06% were intermediately susceptible to gentamicin and 36.36% were fully susceptible to gentamicin. The MIC values of gentamicin for both strains of ceftriaxone resistant bacteria were 4 mg/L. The correlation analysis showed that the MICs of ceftriaxone (R = 0.29) and azithromycin (R = 0.33) weakly correlated with that of gentamicin (Figure 1 and Figure 2). Furthermore, a weak correlation of r = 0.19 was also observed between azithromycin and ceftriaxone (Figure 3).
Table 1.
N. gonorrhoeae isolates susceptibility to three antibiotics. (Gen, gentamicin).
| Antimicrobial | Characterization | Number of Isolates for Which MIC to GEN Was | Total | Correlation to Gen | ||||
|---|---|---|---|---|---|---|---|---|
| ≤2 mg/L | 4 mg/L | 8 mg/L | 16 mg/L | 32 mg/L | ||||
| Gentamicin | - | 27 | 112 | 173 | 60 | 8 | 380 | - |
| Azithromycin | Susceptible | 22 | 93 | 156 | 40 | 3 | 314 | R = 0.33 |
| Resistant | 5 | 19 | 17 | 20 | 5 | 66 | ||
| Ceftriaxone | Susceptible | 27 | 112 | 171 | 60 | 8 | 378 | R = 0.29 |
| Resistant | 0 | 0 | 2 | 0 | 0 | 2 | ||
Figure 1.
Correlation between MICs to gentamicin and azithromycin. Each symbol with a number signifies one or more isolates. Before computing the regression line, the MIC values were log transformed (log2).
Figure 2.
Correlation between MICs to gentamicin and ceftriaxone.
Figure 3.
Correlation between MICs to azithromycin and ceftriaxone.
3.2. Synergy of Three Dual Antimicrobial Combinations
The results of three antibiotic combinations did not reveal any statistical disparities (Table 2). The mean FICI was 0.832 for the gentamicin and ceftriaxone combination, and 0.987 for the gentamicin and azithromycin combination. The synergistic effect of gentamicin with ceftriaxone was stronger than that of gentamicin with azithromycin, promoting 11.3% (43/380) of N. gonorrhoeae isolates. The combination of gentamicin and ceftriaxone exhibited antagonism only in 0.5% (2/380) strains and indifference in 88.2% (335/380) of strains. For the combination of gentamicin and azithromycin, 365 strains showed indifference, accounting for 96.1% of the total bacteria. For the treatment currently in use, the FICI value of ceftriaxone plus azithromycin is 0.874, which was also considered as no synergy or antagonism.
Table 2.
Synergy testing results for three combinations (gentamicin plus ceftriaxone, gentamicin plus azithromycin, and ceftriaxone plus azithromycin) against 380 N. gonorrhoeae isolates.
| Effect. | GEN and CRO | GEN and AZM | AZM and CRO |
|---|---|---|---|
| Synergistic [n (%)] | 43 (11.3) | 15 (3.9) | 42 (11.1) |
| Indifferent [n (%)] | 335 (88.2) | 365 (96.1) | 333 (87.6) |
| Antagonistic [n (%)] | 2 (0.5) | 0 (0) | 5 (1.3) |
| FICI (geometric mean) | 0.832 (0.370–4.5) | 0.987 (0.280–3) | 0.874 (0.280–6.167) |
| Classification overall | Indifferent | Indifferent | Indifferent |
3.3. MICs of the Indicated Antibiotics as Monotherapy and in Combination
The GM MIC of gentamicin was 6.764 mg/L when tested alone; the GM MIC decreased to 2.327 mg/L (2.91-fold reduction, p < 0.05) when combined with ceftriaxone (Table 3). When tested alone, the MIC of ceftriaxone ranged from 0.008 to 0.25 mg/L; when combined with gentamicin, the GM MIC of ceftriaxone decreased from 0.027 to 0.014 mg/L (1.93-fold reduction, p < 0.05). The synergistic effect of gentamicin with ceftriaxone showed indifference regardless of whether the strain was resistant or sensitive to ceftriaxone.
Table 3.
MICs geometric mean and range of the indicated antibiotics as monotherapy and in combination.
| MIC Geometric Mean (Range) (mg/L) | FICI | Interpretation | ||||
|---|---|---|---|---|---|---|
| MICA | MICA (with B) | MICB | MICB (with A) | |||
| GEN and CRO | ||||||
| CRO MIC ≤ 0.125 mg/L (n = 378) |
6.758 (1–32) | 2.320 (1–16) | 0.027 (0.004–0.125) | 0.013 (0.004–0.125) | 0.833 (0.37–4.5) | indifference |
| CRO MIC ≥ 0.25 mg/L (n = 2) |
8 | 4 | 0.25 | 0.03 | 0.62 | indifference |
| GEN and CRO all isolates (n = 380) |
6.764 (1–32) | 2.327 (1–16) | 0.027 (0.008–0.25) | 0.014 (0.004–0.125) | 0.832 (0.370–4.5) | indifference |
| GEN and AZM | ||||||
| AZM MIC ≤ 0.5 mg/L (n = 314) |
6.515 (1–32) | 3.504 (1–16) | 0.143 (0.03–0.5) | 0.052 (0.015–0.25) | 1.004 (0.365–3) | indifference |
| AZM MIC ≥ 1 mg/L (n = 66) |
8.084 (2–32) | 5.367 (1–16) | 2.021 (1–8) | 0.314 (0.06–4) | 0.919 (0.28–3) | indifference |
| GEN + AZM all isolates (n = 380) |
6.764 (1–32) | 3.773 (1–16) | 0.226 (0.03–8) | 0.072 (0.015–4) | 0.987 (0.280–3) | indifference |
| AZM and CRO all isolates (n = 380) |
0.226 (0.03–8) | 0.1 (0.015–4) | 0.027 (0.008–0.25) | 0.017 (0.004–0.25) | 0.874 (0.280–6.167) | indifference |
The GM MIC of gentamicin combined with azithromycin decreased from 6.764 to 3.773 mg/L (1.79-fold reduction, p < 0.05). In monotherapy, the MIC for azithromycin ranged from 0.03 to 8 mg/L; yet combining with gentamicin led to a reduce of the azithromycin GM MIC from 0.226 to 0.072 mg/L (3.14-fold reduction, p < 0.05). Among azithromycin-resistant bacteria, the MIC values for gentamicin alone and in combination were 8.084 mg/L and 5.367 mg/L, respectively (1.51-fold reduction in combination compared to monotherapy). On the other hand, the GM MIC for azithromycin dropped from 2.021 to 0.314 mg/L (A 6.44-fold reduction, p < 0.05). The synergistic effect of gentamicin with ceftriaxone delineated no discrepancy regardless of whether the strain was azithromycin-resistant or sensitive.
The GM MIC of ceftriaxone decreased from 0.027 to 0.017 mg/L when combined with azithromycin (A 1.58-fold reduction, p < 0.05). The GM MIC for azithromycin decreased from 0.226 to 0.1 mg/L (A 2.26-fold reduction, p < 0.05). Overall, the combination did not produce any statistically significant difference.
4. Discussion
In this research, we studied the resistance profile of 380 clinical isolates of N. gonorrhoeae strains collected from three provinces in China with respect to gentamicin, azithromycin, and ceftriaxone. By the agar dilution method, we found that 36.60% of the isolates were fully susceptible to gentamicin, while 61.30% of the strains showed intermediate susceptibility. In two other studies from China on N. gonorrhoeae susceptibility to gentamicin, moderate susceptibility rates of 97.8% [25] and 91.6% [21] were also reported. The possible reason was that these two studies were both from eastern provinces of China, while the isolates of our study were from the eastern, northern and western regions of China. Through comparison with another study from seven provinces in 2016, a significant increment in gentamicin resistance was observed in this study, with the proportion of moderate susceptibility rates increasing from 14.0% to 61.3% and 2.1% of resistant isolates being identified [14]. This indicated an increasing trend of gentamicin resistance in China. Therefore, monitoring gentamicin resistance is still needed before implementing gentamicin for N. gonorrhoeae infections in China. It may be more appropriate to use gentamicin as an adjunct to combination therapy.
The antibiotic synergistic effects were studied using the agar dilution method. Several laboratory techniques can be applied to detect in vitro synergy between antibiotics, with the checkerboard and E test method being the most widely used techniques [26]. The checkerboard method includes microdilution, tube dilution and agar dilution. The agar dilution method is used to detect the MIC of combined antibiotics application by recording the growth of strains on plates with different concentrations of antibiotic combinations, while the E-test method is used to determine the MIC by placing E-test strips of the two antimicrobials on the agar plates at a 90° angle, with intersections at the points of their individual MICs [26,27,28]. Compared to the E-test method, the agar dilution method allows for the simultaneous detection of hundreds N. gonorrhoeae strains at the same antibiotic combination concentration. Therefore, agar dilution is suitable for studying a large number of isolates. According to a study of 65 dual antibacterial drug combinations, the E-test method and the agar dilution method did not result in a difference in the interpretation of synergy [22].
The synergistic effect of the combined antimicrobials is beneficial in obstructing the development of N. gonorrhoeae antibiotic resistance, and we evaluated the interaction of three antibiotics, of which azithromycin and ceftriaxone are the available treatments for gonorrhea and have different resistance mechanisms than gentamicin. We found no facilitative or antagonistic effects associated with these three combinations through evaluating the interactions. According to the data on antimicrobial combinations, three antibiotic combinations showed indifferent effects on most strains and demonstrated synergistic effects in a small number of strains. Several regional studies have reported FICI values ranging from 0.794 to 1.750 for gentamicin in combination with azithromycin [21,27,29,30], and 0.747 to 1.300 for gentamicin in combination with ceftriaxone [21,26,27,31]. These studies have shown that gentamicin-azithromycin and gentamicin-ceftriaxone combinations were indifferent in most clinical isolates.
In the subgroup study, it was observed that gentamicin was not synergistic or antagonistic with another antibiotic, either for the ceftriaxone or the azithromycin resistant or sensitive strains. Comparing the MIC values of antibiotic monotherapy and in combination, combined antibiotics application significantly reduced the previous MICs. Especially in azithromycin-resistant strains, the largest fold decrease (A 6.44-fold reduction) in MIC was observed for the azithromycin-gentamicin combination compared to azithromycin alone. For ceftriaxone, when combined with gentamicin, the GM MIC of ceftriaxone was reduced 1.93-fold. Thus, for these strains, combination therapy can contribute to the halting of the development of ceftriaxone and azithromycin resistance.
This study is clinically relevant and can offer a guide for the clinical application of gentamicin for the following reasons. Firstly, most of the N. gonorrhoeae isolates tested in this study were either fully or intermediately susceptible to gentamicin. As a nationwide study with multiple sample sizes, this study was more representative of the overall gentamicin resistance in China. A correlation analysis demonstrated weak correlations among the MICs of gentamicin, azithromycin and ceftriaxone, indicating the feasibility of using gentamicin in azithromycin or ceftriaxone resistant strains. Secondly, an interaction analysis illustrated the overall indifferent effects embodied by gentamicin in combination with azithromycin or ceftriaxone, providing a theoretical basis for multidrug combination therapy in resistant strains. Since dual combinations of three antibiotics demonstrated indifferent effects, this also provided ideas for future research related to the potential feasibility of a triple combination against clinically resistant strains.
However, there are some limitations in this study. First, only in-vitro experiments were conducted in this plan, hence differences in the penetration of various antibiotics in certain organs were out of the scope of this study. Moreover, according to pharmacokinetic studies, the half-life of azithromycin is 68 h, while that of gentamicin is 2 h [32,33]. Therefore, the combination dose of these two antibiotics is worthy of further investigation. Secondly, the amount of collected ceftriaxone-resistant bacteria used in this study is less than that of the other groups, which implies that more clinical isolates with a variety of resistant bacteria are needed to verify our findings.
5. Conclusions
In summary, most of the N. gonorrhoeae isolates tested in this study exhibited a certain degree of susceptibility to gentamicin. Antimicrobial combinations of gentamicin with ceftriaxone or azithromycin demonstrate indifferent effects overall; meanwhile the efficacy of individual antibiotics was enhanced in the presence of other antimicrobial agents. Gentamicin is generally effective in the treatment of gonorrhea and its combination with ceftriaxone or azithromycin can serve as an alternative therapeutic option.
Acknowledgments
The authors thank the patients who provided the specimens and acknowledge Zhong-Jie Zheng, Zhi Qi and Li-Hua Hu for their contribution in isolates collecting.
Author Contributions
Investigation, J.L., Y.Z., X.Z. and B.Z.; Formal Analysis, Q.Z.; Methodology, W.X. and Y.Y.; Resources, Y.Y.; Data Curation, W.X. and Q.Z.; Writing—Original Draft Preparation, W.X. and Q.Z.; Writing—Review & Editing, W.X. and Q.Z.; Visualization, Q.Z.; Supervision, Y.Y.; Project Administration, Y.Y.; Funding Acquisition, W.X. and Y.Y. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Medical Ethics Committee at the Institute of Dermatology, the Chinese Academy of Medical Sciences & Peking Union Medical College and the National Center for Sexually Transmitted Disease Control all gave their approval to this project(2014-LS-026).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available in the article.
Conflicts of Interest
The authors declare that they have no conflicts of interest with regard to the publication of this article.
Funding Statement
This work was supported by the National Science and Technology Major Project (2018ZX101010 01-004-003), the Nanjing Incubation Program for National Clinical Research Center (2019060001), and Jiangsu Province Youth Fund Project (BK20180156).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Quillin S.J., Seifert H.S. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat. Rev. Microbiol. 2018;16:226–240. doi: 10.1038/nrmicro.2017.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowley J., Vander Hoorn S., Korenromp E., Low N., Unemo M., Abu-Raddad L.J., Chico R.M., Smolak A., Newman L., Gottlieb S., et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019;97:548–562. doi: 10.2471/BLT.18.228486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Unemo M., Seifert H.S., Hook E.W., 3rd, Hawkes S., Ndowa F., Dillon J.R. Gonorrhoea. Nat. Rev. Dis. Primers. 2019;5:79. doi: 10.1038/s41572-019-0128-6. [DOI] [PubMed] [Google Scholar]
- 4.Unemo M., Ross J., Serwin A.B., Gomberg M., Cusini M., Jensen J.S. 2020 European guideline for the diagnosis and treatment of gonorrhoea in adults. Int. J. STD AIDS. 2020;32:956462420949126. doi: 10.1177/0956462420949126. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) Update to CDC’s Sexually transmitted diseases treatment guidelines, 2010: Oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb. Mortal. Wkly. Rep. 2012;61:590–594. [PubMed] [Google Scholar]
- 6.World Health Organization . WHO Guidelines Approved by the Guidelines Review Committee. World Health Organization; Geneva, Switzerland: 2016. [(accessed on 1 June 2022)]. WHO Guidelines for the Treatment of Neisseria gonorrhoeae; pp. 17–18. Available online: https://www.ncbi.nlm.nih.gov/books/NBK379221/ [Google Scholar]
- 7.Dong H.V., Klausner J.D. Neisseria gonorrhoeae resistance driven by antibiotic use. Nat. Rev. Urol. 2019;16:509–510. doi: 10.1038/s41585-019-0206-2. [DOI] [PubMed] [Google Scholar]
- 8.Chen S.C., Han Y., Yuan L.F., Zhu X.Y., Yin Y.P. Identification of Internationally Disseminated Ceftriaxone-Resistant Neisseria gonorrhoeae Strain FC428, China. Emerg. Infect. Dis. 2019;25:1427–1429. doi: 10.3201/eid2507.190172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson D.A., Fairley C.K., Howden B.P., Chen M.Y., Stevens K., De Petra V., Denham I., Chow E.P.F. Trends and Risk Factors for Antimicrobial-Resistant Neisseria gonorrhoeae, Melbourne, Australia, 2007 to 2018. Antimicrob. Agents Chemother. 2019;63:e01211–e1219. doi: 10.1128/AAC.01221-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seña A.C., Bachmann L., Johnston C., Wi T., Workowski K., Hook E.W., 3rd, Hocking J.S., Drusano G., Unemo M. Optimising treatments for sexually transmitted infections: Surveillance, pharmacokinetics and pharmacodynamics, therapeutic strategies, and molecular resistance prediction. Lancet Infect. Dis. 2020;20:e181–e191. doi: 10.1016/S1473-3099(20)30171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campoccia D., Montanaro L., Arciola C.R. A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials. 2013;34:8533–8554. doi: 10.1016/j.biomaterials.2013.07.089. [DOI] [PubMed] [Google Scholar]
- 12.Workowski K.A., Bachmann L.H., Chan P.A., Johnston C.M., Muzny C.A., Park I., Reno H., Zenilman J.M., Bolan G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Morb. Mortal. Wkly. Rep. Recomm. Rep. 2021;70:1–187. doi: 10.15585/mmwr.rr7004a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matoga M., Chen J.S., Krysiak R., Ndalama B., Massa C., Bonongwe N., Mathiya E., Kamtambe B., Jere E., Chikaonda T., et al. Gentamicin susceptibility in Neisseria gonorrhoeae and treatment outcomes for urogenital gonorrhea after twenty-five years of sustained gentamicin use in Malawi. Sex. Transm. Dis. 2022;49:251–256. doi: 10.1097/OLQ.0000000000001580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu J.W., Xu W.Q., Zhu X.Y., Dai X.Q., Chen S.C., Han Y., Liu J., Chen X.S., Yin Y.P. Gentamicin susceptibility of Neisseria gonorrhoeae isolates from 7 provinces in China. Infect. Drug Resist. 2019;12:2471–2476. doi: 10.2147/IDR.S214059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowell D., Kirkcaldy R.D. Effectiveness of gentamicin for gonorrhoea treatment: Systematic review and meta-analysis. Sex. Transm. Infect. 2012;88:589–594. doi: 10.1136/sextrans-2012-050604. [DOI] [PubMed] [Google Scholar]
- 16.Kirkcaldy R.D., Weinstock H.S., Moore P.C., Philip S.S., Wiesenfeld H.C., Papp J.R., Kerndt P.R., Johnson S., Ghanem K.G., Hook E.W., 3rd The efficacy and safety of gentamicin plus azithromycin and gemifloxacin plus azithromycin as treatment of uncomplicated gonorrhea. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2014;59:1083–1091. doi: 10.1093/cid/ciu521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unemo M., Shafer W.M. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: Past, evolution, and future. Clin. Microbiol. Rev. 2014;27:587–613. doi: 10.1128/CMR.00010-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bollenbach T. Antimicrobial interactions: Mechanisms and implications for drug discovery and resistance evolution. Curr. Opin. Microbiol. 2015;27:1–9. doi: 10.1016/j.mib.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Unemo M., Ballard R., Ison C., Lewis D., Ndowa F., Peeling R. Laboratory Diagnosis of Sexually Transmitted Infections, including Human Immunodeficiency Virus. World Health Organization; Geneva, Switzerland: 2013. [(accessed on 7 June 2022)]. pp. 39–44. Available online: https://apo.who.int/publications/i/item/9789241505840. [Google Scholar]
- 20.Clinical and Laboratory Standards Institute . Performance Standards for Antimicrobial Susceptibility Testing. 29th ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2019. [(accessed on 10 June 2022)]. pp. 78–82. Available online: https://clsi.org/media/pqlom3b5/_m100_archived_drugs_table.pdf. [Google Scholar]
- 21.Li X., Le W., Lou X., Wang B., Genco C.A., Rice P.A., Su X. In Vitro Efficacy of Gentamicin Alone and in Combination with Ceftriaxone, Ertapenem, and Azithromycin against Multidrug-Resistant Neisseria gonorrhoeae. Microbiol. Spectr. 2021;9:e0018121. doi: 10.1128/Spectrum.00181-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White R.L., Burgess D.S., Manduru M., Bosso J.A. Comparison of three different in vitro methods of detecting synergy: Time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 1996;40:1914–1918. doi: 10.1128/AAC.40.8.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odds F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003;52:1. doi: 10.1093/jac/dkg301. [DOI] [PubMed] [Google Scholar]
- 24.Bidaud A.L., Schwarz P., Chowdhary A., Dannaoui E. In Vitro Antifungal Combination of Terbinafine with Itraconazole against Isolates of Trichophyton Species. Antimicrob. Agents Chemother. 2022;66:e0144921. doi: 10.1128/AAC.01449-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang F., Yan J., Zhang J., van der Veen S. Evaluation of alternative antibiotics for susceptibility of gonococcal isolates from China. Int. J. Antimicrob. Agents. 2020;55:105846. doi: 10.1016/j.ijantimicag.2019.11.003. [DOI] [PubMed] [Google Scholar]
- 26.Barbee L.A., Soge O.O., Holmes K.K., Golden M.R. In vitro synergy testing of novel antimicrobial combination therapies against Neisseria gonorrhoeae. J. Antimicrob. Chemother. 2014;69:1572–1578. doi: 10.1093/jac/dkt540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wind C.M., de Vries H.J., van Dam A.P. Determination of in vitro synergy for dual antimicrobial therapy against resistant Neisseria gonorrhoeae using Etest and agar dilution. Int. J. Antimicrob. Agents. 2015;45:305–308. doi: 10.1016/j.ijantimicag.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Sopirala M.M., Mangino J.E., Gebreyes W.A., Biller B., Bannerman T., Balada-Llasat J.M., Pancholi P. Synergy testing by Etest, microdilution checkerboard, and time-kill methods for pan-drug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2010;54:4678–4683. doi: 10.1128/AAC.00497-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh V., Bala M., Bhargava A., Kakran M., Bhatnagar R. In vitro efficacy of 21 dual antimicrobial combinations comprising novel and currently recommended combinations for treatment of drug resistant gonorrhoea in future era. PLoS ONE. 2018;13:e0193678. doi: 10.1371/journal.pone.0193678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sood S., Agarwal S.K., Singh R., Gupta S., Sharma V.K. In vitro assessment of gentamicin and azithromycin-based combination therapy against Neisseria gonorrhoeae isolates in India. J. Med. Microbiol. 2019;68:555–559. doi: 10.1099/jmm.0.000953. [DOI] [PubMed] [Google Scholar]
- 31.Bharat A., Martin I., Zhanel G.G., Mulvey M.R. In vitro potency and combination testing of antimicrobial agents against Neisseria gonorrhoeae. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2016;22:194–197. doi: 10.1016/j.jiac.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Triggs E., Charles B. Pharmacokinetics and therapeutic drug monitoring of gentamicin in the elderly. Clin. Pharmacokinet. 1999;37:331–341. doi: 10.2165/00003088-199937040-00004. [DOI] [PubMed] [Google Scholar]
- 33.Crokaert F., Hubloux A., Cauchie P. A Phase I Determination of Azithromycin in Plasma during a 6-Week Period in Normal Volunteers after a Standard Dose of 500 mg Once Daily for 3 Days. Clin. Drug Investig. 1998;16:161–166. doi: 10.2165/00044011-199816020-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available in the article.