Abstract
Simple Summary
Circulating tumor cells (CTCs) are rare cells found in the bloodstream of oncologic patients with a central role in the metastatic spread. In this study, we aim at exploring their heterogeneity levels in metastatic breast cancer patients focusing on single cell single nucleotide variant (SNV) and copy number aberration (CNA) analyses. Our results show high levels of heterogeneity, especially concerning SNVs. Further analysis revealed the presence of CNAs associated with breast tumorigenesis, while longitudinal CNA profiling was demonstrated to track clonal selection of CTCs during treatment. Despite this heterogeneity, we found a group of CTCs from different patients sharing common genomic aberrations, such as losses on 15q. Collectively, our findings demonstrate that single-cell molecular analyses could be exploited in future to better address therapeutic strategies. Further investigations to better characterize this mixed population are needed to understand its role in MBC.
Abstract
Circulating tumor cells’ (CTCs) heterogeneity contributes to counteract their introduction in clinical practice. Through single-cell sequencing we aim at exploring CTC heterogeneity in metastatic breast cancer (MBC) patients. Single CTCs were isolated using DEPArray NxT. After whole genome amplification, libraries were prepared for copy number aberration (CNA) and single nucleotide variant (SNV) analysis and sequenced using Ion GeneStudio S5 and Illumina MiSeq, respectively. CTCs demonstrate distinctive mutational signatures but retain molecular traces of their common origin. CNA profiling identifies frequent aberrations involving critical genes in pathogenesis: gains of 1q (CCND1) and 11q (WNT3A), loss of 22q (CHEK2). The longitudinal single-CTC analysis allows tracking of clonal selection and the emergence of resistance-associated aberrations, such as gain of a region in 12q (CDK4). A group composed of CTCs from different patients sharing common traits emerges. Further analyses identify losses of 15q and enrichment of terms associated with pseudopodium formation as frequent and exclusive events. CTCs from MBC patients are heterogeneous, especially concerning their mutational status. The single-cell analysis allows the identification of aberrations associated with resistance, and is a candidate tool to better address treatment strategy. The translational significance of the group populated by similar CTCs should be elucidated.
Keywords: metastatic breast cancer, circulating tumor cells, copy number aberrations, single nucleotide variants, single cell sequencing, next generation sequencing, liquid biopsy
1. Introduction
Recent updates concerning cancer statistics have reported that, in 2020, breast cancer (BC) ranked as the most commonly diagnosed tumor type worldwide [1]. Despite the high morbidity of BC, survival at 5 and 10 years has higher rates compared to other cancer types, especially in developed countries, where massive screening is successfully applied to detect BC at early stages [2]. However, these rates dramatically drop for patients diagnosed with metastatic BC (MBC), which still represents an incurable disease [3].
Circulating tumor cells (CTCs) consist of a rare population of cells that detach from the tumor mass towards secondary organs, thus being among the main perpetrators of the metastatic spread of epithelial tumors [4]. In MBC, CTC enumeration was proven to be an independent prognostic factor of progression-free survival (PFS) and overall survival (OS), displaying poor prognosis in patients with basal CTC count ≥5 in 7.5 mL of blood [5]. Furthermore, baseline enumeration of CTCs was shown to predict the progression of disease earlier than the standard timing of anatomical assessment using conventional radiological tests in BC patients with limited metastatic dissemination [6]. In recent years, the molecular heterogeneity of CTCs has been deeply investigated, and intra-patient heterogeneity is considered nowadays a matter of fact with manifest clinical implications [7]. Up to now, next-generation sequencing (NGS) is the master technique for the identification of alterations associated with pathogenesis [8,9,10]. Hence, molecular characterization of CTCs through NGS could provide critical information concerning the primary tumor in MBC and represents a fascinating tool to improve precision medicine [11].
In this study, we aimed at exploring the heterogeneity of CTCs from MBC patients through single-cell single nucleotide variant (SNV) and copy number aberration (CNA) analysis. In brief, our findings highlight great levels of intra- and inter-patient CTC heterogeneity, especially concerning their SNVs. Furthermore, the herein reported detection of aberrations involving clinically-relevant genes, even over time, supports the role of CTCs as a “liquid biopsy” to better address therapies in the near future. Finally, we identified a group populated by similar CTCs from different patients that need further analysis to delineate their role in MBC pathogenesis.
2. Materials and Methods
2.1. Patients
Six patients diagnosed with metastatic luminal (estrogen receptor (ER) and progesterone receptor (PgR) positive, Human Epidermal Growth Factor Receptor 2 (HER2) negative) BC were enrolled in this study. Blood withdraws were performed at three timepoints: at baseline (timepoint A), 6–8 weeks after the beginning of treatment (timepoint B) and 2–4 weeks after the last dose of therapy (timepoint C). All subjects gave written informed consent to the conservation and use of the samples for research purposes. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved on 9 November 2018 by the Romagna Ethics Committee (CEROM) of Meldola (IRST174.19).
2.2. CTC Enrichment, Recovery and Whole Genome Amplification (WGA)
CTCs and white blood cells prestained with antibodies to CD45 and pan-CK and DAPI were aspirated from the CellSearch cartridge used for the CTC enumeration, and single cells were isolated using DEPArray NxT (Menarini-Silicon Biosystems SpA, Bologna, Italy). After isolation of cells in PCR-sterile tubes, we performed volume reduction and 1X PBS wash under a sterile hood. Samples were stocked at −20 °C until further analysis.
To obtain evaluable DNA for downstream analysis, we performed WGA using Ampli1 WGA kit (Menarini-Silicon Biosystems SpA, Bologna, Italy) and the quality of amplified DNA was assessed using the Ampli1 QC kit (Menarini-Silicon Biosystems SpA, Bologna, Italy). The PCR product was evaluated through electrophoresis on a 2% agarose gel and visualized using Chemidoc XRS System (Bio-rad, Hercules, CA, USA). Based on the number of visualizable bands for each sample we proceeded with library preparation. WGA products were conserved at −20 °C until further downstream analysis.
2.3. Library Preparation and Sequencing
For CNA analysis, libraries were prepared from samples with at least two out of four bands at the quality control. The preparation of the libraries was performed using the Ampli1 Lowpass kit for Ion Torrent (Menarini-Silicon Biosystems SpA, Bologna, Italy) following the protocol provided by the manufacturer. Final library concentration and quality were assessed by Qubit 4.0 Fluorometer (Thermo Fisher, Waltham, MA, USA) and Bioanalyzer High Sensitivity DNA (Agilent Technologies, Waldbronn, Germany), respectively. Equimolar pools were prepared and loaded into Ion 520 Chips using the Ion Chef System (Thermo Fisher, Waltham, MA, USA). Sequencing was carried out using the Ion Torrent S5 System.
Samples with at least three out of four bands at the quality control were considered eligible for SNV analysis. Libraries were prepared using the Ampli1 OncoSeek Panel (Menarini-Silicon Biosystems SpA, Bologna, Italy) and quantified using the KAPA Library quantification Kit (Roche, Basel, Switzerland). Equimolar pools were loaded on 300-cycles V2 cartridges and sequenced 2 × 151 on MiSeq sequencing system (Illumina Inc., San Diego, CA, USA).
2.4. Bioinformatic and Statistical Analyses
The bioinformatics analyses were performed with customized pipelines. For Ampli1 OncoSeek Panel, raw de-multiplexed reads from the MiSeq sequencer were trimmed of primer sequences and successively aligned to the reference human genome (UCSC-Build37/hg19) using the Burrows–Wheeler algorithm [12], running in paired-end mode. To ensure good call quality and to reduce the number of false positives, samples underwent Base Quality Score Recalibration (BQSR), using the Genome Analysis Toolkit GATK, version 3.2.2 [13]. After BQSR, sequences around regions with insertions and deletions (indels) were realigned locally with GATK. For somatic variant analysis VarScan 2.3.9 [14] was used to search for SNVs and indels. Genomic and functional annotations of detected variants were made by Annovar [15]. Coverage statistics were performed by DepthOfCoverage utility of GATK. BASH and R custom scripts.
For CNA calling, Control-FREEC [16] was used starting from sorted bam files derived by Ion Torrent S5 System and samtools [17], and a quality check of our samples was performed by computing the derivative log ratio spread (DLRS) [18]. Then, we applied two non-parametric tests (Mann–Withney and Kolmogorov-Smirnov) computing p-values in order to assess the statistical significance of each call and filtered out preliminary CNAs having at least one of the two p-values higher than 0.05. From each CNA, we extracted the list of genes spanning the aberration and performed enrichment analysis on Gene Ontology (GO) datasets [19] for each sample with EnrichR [20]. Next, we applied the Genomic Identification of Significant Targets in Cancer (GISTIC) tool [21] in order to identify regions with significant aberrations inside a group of samples. Finally, we performed hierarchical clustering on different groups of samples based on copy numbers inside bins of 1 million bases, computing distance among samples with Euclidean metrics.
3. Results
3.1. CTC Isolation in MBC Patients and Quality Assessment
Epithelial CTCs were enriched using the CellSearch system, and single-cell isolation was performed using the DEPArrayNxT platform. Overall, we isolated 124 single pure CTCs from 6 MBC patients (Table 1).
Table 1.
List of patients with clinical parameters and number of single CTCs for each patient and timepoint.
| Patient ID | Therapy | Clinical Response |
Site of Metastasis | Number of CTC Isolated | |||
|---|---|---|---|---|---|---|---|
| Timepoint A | Timepoint B | Timepoint C | Total | ||||
| CH28 | Capecitabine | PR | Bone, Lymph nodes | 5 | 5 | ||
| CH29 | Fulvestrant + Palbociclib | PD | Peritoneum | 17 | 9 | 30 | 56 |
| CH30 | Capecitabine + Vinorelbine | PD | Bone, Liver | 37 | 2 | 39 | |
| CH32 | Capecitabine + Vinorelbine | SD | Bone, Liver, Lung | 15 | 15 | ||
| CH46 | Letrozole + Ribociclib | SD | Bone | 5 | 5 | ||
| CH47 | Letrozole + Ribociclib | N/A | Bone, Lymph nodes | 4 | 4 | ||
| Total | 83 | 9 | 32 | 124 | |||
CTC: circulating tumor cell; PR: partial response; PD: progressive disease; SD: stable disease; N/A: not available.
At QC check, 35 CTCs (28.23%) displayed 4 PCR bands, whereas 24 (19.35%) exhibited 3 bands. Twenty-eight (22.58%) showed medium quality with 2 out of 4 bands. Thirty-seven CTCs were considered not suitable for downstream analysis: 16 (12.90%) and 21 CTCs (16.94%) showed, respectively, 1 and 0 bands. An example of the results obtained after PCR products run on agarose gel electrophoresis is reported in Figure S1 (Supplementary Material File S1). For each patient, we isolated one 10-lymphocyte pool for normalization in downstream analysis. All the lymphocyte pools demonstrated optimal quality for downstream analysis, displaying 4/4 bands at the PCR-based quality control check.
3.2. Single Nucleotide Variant (SNV) Analysis on Single CTCs
To gain information concerning the somatic molecular features of CTCs, 59 CTCs from 4 patients whose amplified DNA showed appropriate quality (at least 3 PCR bands) were tested for a hotspot panel of 60 tumor-related genes. Additional analysis conducted of lymphocyte-pool samples excluded the presence of candidate germinal mutations in all the patients. Overall, called variants were observed in 32 out of 55 evaluable CTCs (58.2%). Regarding CTCs from patient CH28, we obtained poor sequencing quality in terms of coverage statistics, thus the results are unavailable. CTCs from patients CH46 and CH47 were not included in the SNV analysis having less than 3 bands at QC. The list of the alterations found in single CTCs is reported in Table S1.
In patient CH29, variants were called in 15/17 (88%) CTCs. We found three shared variants with unknown clinical significance: ATM S333F (12/15 CTCs; 80%) persistent at all the timepoints, TP53 R210X (3/15 CTCs; 20%) from timepoints A and B, PTEN S287X (2/15 CTCs; 13%) from timepoint B. At time C, we observed in a single CTC the RB1 F755S variant. Despite its clinical significance is still unknown, somatic mutations affecting this locus have been reported as an acquired mechanism of CDK4/6 inhibitors resistance [22].
Concerning patient CH30, while 10 CTCs did not display any alteration affecting the tested genes, we found exclusive exonic variants in 13 out of 23 CTCs (56.5%). Notably, two mutations with clinical significance were observed: the nonsynonymous SNVs PIK3CA N345D [23] (1 CTC from timepoint A) and MLH1 S127L [24] (rs201673334; 1 CTC from timepoint A).
Patient CH32 displayed 4 out of 15 CTCs (26.67%) from timepoint A with called variants. We found in 2 CTCs (50%) the nonsynonymous SNV AKT1 E17K (rs121434592), reported as pathogenic in several cancer types including BC and associated with resistance to therapies [25,26,27]. In addition, two mutations affecting the TP53 locus were identified: a frameshift deletion occurring on the DNA binding domain TP53 S128fs (2/4 CTCs; 50%) and the nonsynonymous SNV TP53 V25F (rs121912654, 1/4 CTC; 25%).
In summary, CTCs harbor alterations associated with pathogenesis and therapy resistance, and the high intra- and inter-patient heterogeneity levels make the translational interpretation of identified variants in CTCs challenging.
3.3. Single Cell Profiling of CTCs
Considering SNV results, we aimed at further exploring the molecular characteristics of CTCs by profiling their CNAs.
A total of 87 single CTCs were sequenced, and the quality was checked by computing the DLRS [18]. 77/87 samples (88.15%) were considered suitable for further bioinformatic analyses (DLRS values < 0.3). Data of CTCs from patient CH28 are unavailable due to quality issues, having a DLRS ≥ 0.3, and the good quality of copy number profile of the leukocyte pools of patient CH28 excluded procedure shortcomings (Supplementary Material File S1, Figure S2). The lack of significative aberrations on lymphocyte pools allowed us to confirm the tumoral nature of identified CNAs. The CNA profile plots of representative CTC are reported in Supplementary Material Figure S4.
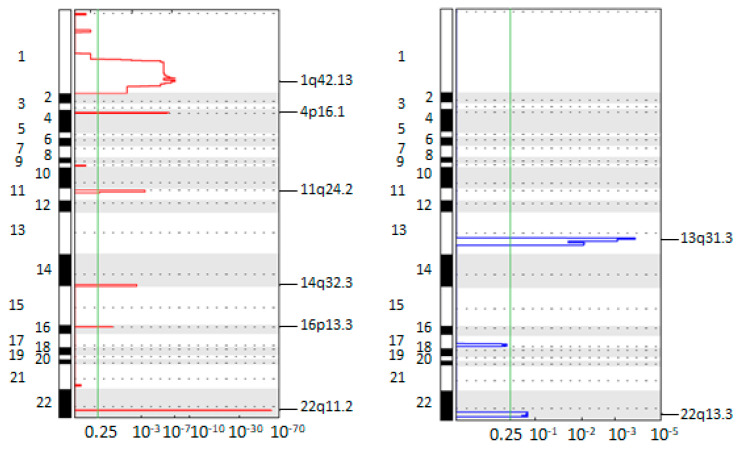
To investigate the frequency and the amplitude of segmented copy number values, we used the GISTIC tool. The plots in Figure 1 report the frequent gains and losses that occurred in all the CTCs (n = 77).
Figure 1.
Genomic Identification of Significant Targets in Cancer (GISTIC) amplification (left, red) and deletion (right, blue) plots on single circulating tumor cells (CTCs) of all the patients. The genome is oriented vertically from top to bottom, and the GISTIC q-values at each locus are plotted from left to right on a log scale. The green line represents the significance threshold (q-value = 0.25).
Overall, this analysis identified frequent amplifications on chromosomes 1q, 4p, 11q, 14q, 16p and 22q. The most frequent amplified region was a 183.70 kb long region on chromosome 22q11.2, containing only the KIAA1671 gene whose product was previously considered as a candidate biomarker for early detection of in situ BC [28]. Of relevance, the gain of 11q24.2 involves the CCND1 gene [29].
Among the most frequent deletions, we found loss on chromosome 13q. Notably, this region hosts the RB1 locus, codifying a crucial tumor-suppressor whose loss is associated with resistance to anti-CDK4/6 therapies in ER-positive BC [28]. In addition, we found the deletion of the tumor suppressor gene CHEK2 in chromosome 22q13.3, a region commonly found loss in BC [30].
Taken together, data from GISTIC analyses identify the presence of aberrations in CTCs associated with breast pathogenesis.
3.4. Longitudinal Investigation of CTC CNA Profiles
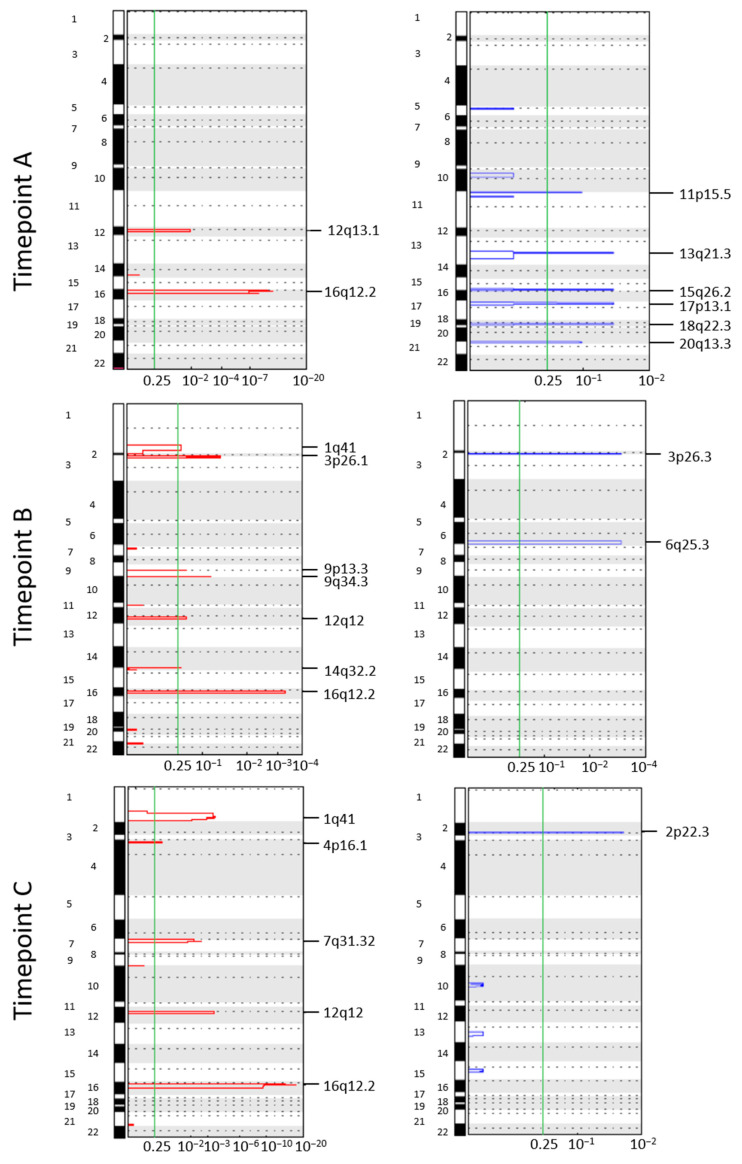
Next, we aimed at identifying patient-specific aberrations in CTCs involved in tumor progression and CTC survival. To this purpose, we applied the GISTIC algorithm to CTCs of patients CH29 and CH30, having CTCs from at least two time points.
Patient CH29 (treated with fulvestrant plus palbociclib) displayed heterogeneous aberration spectra across the time points and gain of chromosome 16q12.2 emerged as a persistent alteration. Gains in regions 1q41 and 12q12 emerged as frequently in gain in time B and persistence in time C, suggesting their occurrence as a result of selection pressure exerted by therapy. Indeed, region 12q12 hosts the CDK4 gene whose overexpression represents one of the main mechanisms of resistance to CDK4/6 inhibitors [31] (Figure 2).
Figure 2.
Genomic Identification of Significant Targets in Cancer (GISTIC) amplification and deletion plots on single circulating tumor cells (CTCs) from patient CH29. Each column represents a different timepoint. The genome is oriented vertically from top to bottom, and the GISTIC q-values at each locus are plotted from left to right on a log scale. The green line represents the significance threshold (q-value = 0.25). A: basal (10 CTCs); B: screening (6–8 weeks after; 5 CTCs); C: end of therapy (13 CTCs).
Concerning patient CH30 (treated with vinorelbine plus capecitabine), frequent aberrations in CTCs from timepoints A and C were gain of chromosome 11q13.2 and chromosome 22q11.2 (Figure 3).
Figure 3.
Genomic Identification of Significant Targets in Cancer (GISTIC) amplification and deletion plots on single circulating tumor cells (CTCs) from patient CH30. Each column represents a different timepoint. The genome is oriented vertically from top to bottom, and the GISTIC q-values at each locus are plotted from left to right on a log scale. The green line represents the significance threshold (q-value = 0.25). A: basal (37 CTCs); C: end of therapy (2 CTCs).
The region 11q13 is a gene-rich region found amplified in 15% of all primary breast tumors [32], and hosts genes known as potential contributors to positive selection for cell proliferation and survival by previous studies, among which the oncogene CCND1 [33].
Collectively, the liquid biopsy of two differently treated MBC patients confirmed CTC heterogeneity in terms of CNA profiling, while some alterations persist along the course of treatment and host genes associated with resistance to anti-tumor agents.
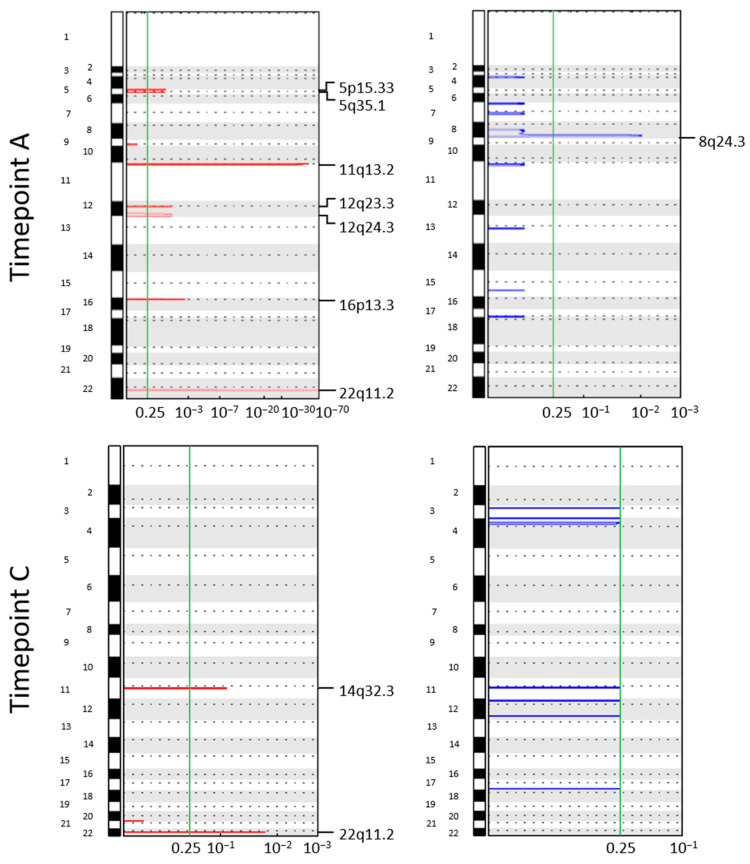
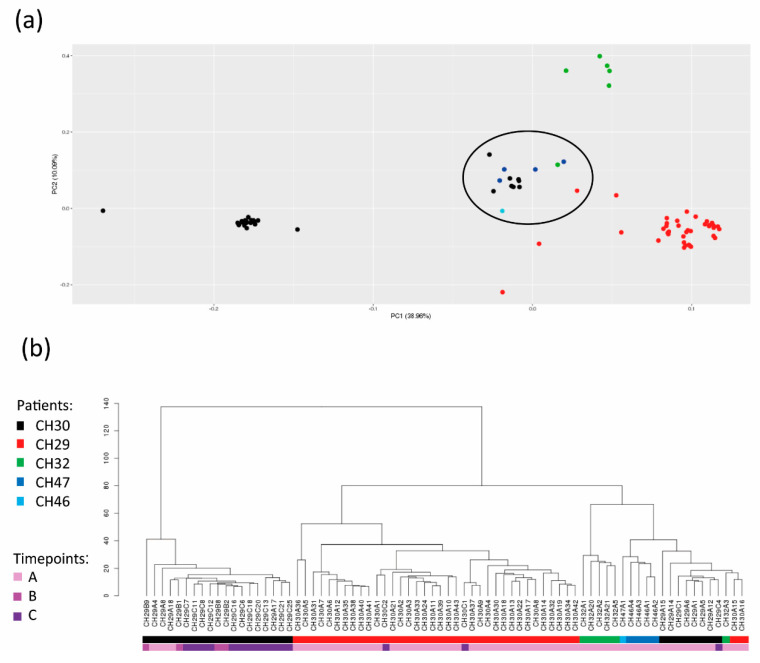
3.5. Identification of a Population of CTCs with Common Traits
Next, in order to better understand the levels of CTC heterogeneity, we integrated single-cell data from all the patients. For this purpose, we performed principal component analysis (PCA) for dimensionality reduction and unsupervised visualization of CNA data (Figure 4a).
Figure 4.
Intertumoral heterogeneity of circulating tumor cells (CTCs). (a) Principal component analysis (PCA) plot was generated using all the CTCs of all the patients. Each dot corresponds to a single CTC of each patient with a colour-based code. Black: patient CH29; Red: patient CH30; Green: patient CH32; Blue: patient CH46; Cyan: patient CH47. The black circle highlights the crossed-patient CTC set. (b) Hierarchical clustering tree.
Based on our results, single CTCs from the same patient have the tendency to group together, although a subpopulation of mixed CTCs from different patients was present (crossed-patient CTC set). The existence of a crossed-patient CTC set was confirmed by the hierarchical clustering tree (Figure 4b). The crossed-patient CTC set was populated by 15 cells, and each patient had at least one CTC grouping within this set.
Next, we applied GISTIC 2.0 and term enrichment analyses to explore the molecular and functional features of the crossed-patient CTC set (Table S2), and the results were compared with those obtained from the entire CTC case series using the same tools (Table S3).
The most frequent private aberrations in the crossed-patient CTC set were gain in region 9q34.3 (813 kb) and a great loss borne by 15q (71.80 Mb), which is frequently reported in the literature in association with tumor progression and metastasis in BC [34,35,36,37] (Supplementary Figure S3). In Table 2, we reported the genes included within 15q with a tumor-suppressor role in BC.
Table 2.
List of tumor suppressor genes comprised within the region 15q.
| Gene | Gene Product | Genomic Location |
References |
|---|---|---|---|
| BLM | Bloom Syndrome RecQ Like Helicase | 15q26.1 | [38] |
| ONECUT1 | One Cut Homeobox 1 | 15q21.3 | [39] |
| PML | Promyelocytic Leukemia Protein | 15q22 | [40] |
| THBS1 | Thrombospondin-1 | 15q15 | [41] |
| TP53BP1 | Tumor Protein P53 Binding Protein 1 | 15q15-q21 | [42] |
| ANP32A | Acidic Nuclear Phosphoprotein 32 Family Member A | 15q23 | [43] |
| ALDH1A2 | Aldehyde Dehydrogenase 1 Family Member A2 | 15q21.3 | [44] |
| CCNDBP1 | Cyclin D1 Binding Protein 1 | 15q14-q15 | [45] |
| BMF | Bcl2 Modifying Factor | 15q14 | [46] |
| ST20 | Suppressor Of Tumorigenicity 20 | 15q25.1 | [47] |
| MIR211 | Hsa-Mir-211 | 15q13.3 | [48] |
| MIR7-2 | Hsa-Mir-7 | 15q26.1 | [49] |
| MIR9-3 | Hsa-Mir-9 | 15q26.1 | [50,51] |
| MIR422A | Hsa-Mir-422a | 15q22.31 | [52] |
The results of the enrichment analyses showed that the most enriched term in GO Biological Process was “positive regulation of transforming growth factor beta production (GO:0071636)” in 14/15 CTCs (93.3%). However, this term is not considered privately enriched in the crossed-patient CTC set, as it was also found enriched less frequently in CTCs from the entire case series (51/77 CTCs; 66.2%). The “pseudopodium (GO:0031143)” (GO Cellular Component database) was another frequent enriched term in the crossed-patient CTC set (9/15 CTCs; 60%), while it was less enriched in the entire case series (18/77 CTCs; 23.4%).
Our data infer the existence of a crossed-patient CTC set with specific molecular and functional characteristics. Our findings sketch various levels of heterogeneity: (I) CTCs tend to group in a patient-specific manner, and (II) some CTCs are similar to each other while belonging to different patients. Hence, despite a context of evident heterogeneity, our data reveal the existence of a hidden similarity among CTCs.
4. Discussion
In recent years, CTCs have been deeply investigated due to their pivotal role in the metastatic cascade, but their high heterogeneity still contributes to counteract their introduction in clinical practice [7,53]. In fact, as a consequence of the dynamic changes in the bloodstream, CTCs can converge in distinct subpopulations with specific genomic and phenotypic features [54]. Up to now, CTC enumeration remains the only FDA-approved CTC-based assay in clinical practice with prognostic purpose [55], but the heterogeneous genetic features characterizing this cell population could no longer be neglected as they dramatically influence disease manifestation and outcome [56]. Hence, the identification of novel approaches to further exploit data from CTCs for translational purposes beyond CTC enumeration is imperative. The aim of this study is to explore the molecular landscape of CTCs in MBC patients. For this purpose, we exploited single-cell resolution NGS to assess CTC mutational status and CNA profile. However, this study has some flaws. Firstly, the limited number of patients makes challenging to achieve robust statistical data. However, this weakness is mitigated by high-quality single-cell data illustrated in this article, especially with whole-genome CNA profiling. Moreover, the availability of primary tumor and metastatic specimens would have been helpful to integrate the mutational profiling, and to better delineate the clonal selection of CTCs based on their CNAs.
Our results confirm that single-cell analysis of CTCs represents an accurate approach to unmasking genetic heterogeneity. In our study, testing single CTCs for a panel of 60 cancer-relevant genes revealed a great intra-patient degree of variant heterogeneity, supporting the existence of distinct self-specific mutational signatures for each CTC. Our study is not the first to describe the detection of mutational heterogeneity in single CTCs from MBC patients [11,57,58,59,60].
At the same time, while no mutations were common among patients, we detected a limited number of alterations shared among CTCs within the same patient even at different time points. This finding, as observed by other researchers [11], highlights that the presence of shared molecular alterations reflects the common clonal origin of tumor cells in the bloodstream [61]. Overall, due to the high degree of heterogeneity, the translational significance of candidate alterations is still not univocal. One key example is represented by the AKT E17K variant which is reported as pathogenic and associated with resistance to therapies in BC [62] but was retrieved in 50% of CTCs at timepoint A in patient CH32. Finally, we found a limited number of CTCs with called SNVs. This result may be imputable to the tested panel, which includes a limited number of genes and covers hotspot mutations. Hence, we cannot exclude the presence of alterations occurring on other genes not included in this analysis.
Concerning chromosomal aberration analysis, while confirming the heterogeneous portrait of CNAs in CTCs, we described the emergence of frequent alterations involving genes with a critical role in MBC in agreement with the literature. This workflow was previously successfully exploited by our group for the longitudinal characterization of single CTCs from early BC [7] and oesophageal cancer patients [63]. Herein, we found that gain of the region 22q11.2 emerged as the most frequent aberration in CTCs. This short aberration includes a unique gene, KIAA1671, which codifies for an uncharacterized protein involved in mitosis and chromosome segregation [64]. Although its role is still unexplored, KIAA1671 seems to contribute to BC pathogenesis, since autoantibodies against the codified protein were detected in serum from BC patients [28]. Moreover, emerging frequent aberrations included several gains (1q, 4p, 11q, 14q and 16p) and losses (13q and 22q), among which aberrations already described in BC and often hosting clinically-relevant genes. One example is represented by WNT3A (1q42), whose protein product encompasses a wide range of roles, from oncogenesis to developmental processes. In vitro studies have demonstrated a role for WNT3A in BC proliferation [65] and resistance to tamoxifen treatment [66]. CCND1 (11q13) amplification is frequent in BC and associated with progression and resistance [29,67]. The encoding product, Cyclin D1, is an oncogenic protein with a pivotal role in G1 to S phase transition during the cell cycle [33,68]. A high copy number of CCND1 was previously found to identify a subset of ER-positive patients with poorer prognosis [69]. Beyond its role in cell cycle regulation, Cyclin D1 harbours also non-canonical cdk-independent functions, among which the ability to interact with the hormone binding domain of ER. As a consequence, ER-mediated transcripts are upregulated even in absence of the canonical ligand [70]. On the other hand, Checkpoint Kinase 2, codified by the CHEK2 (22q12.1) gene, acts as a tumor-suppressor in BC where gene loss is not infrequent [71,72].
In addition, longitudinal analyses on single cells from MBC patients with CTCs in at least two timepoints allowed us to track the clonal selection of CTCs during treatment, supporting the power of CTC CNA profiling as an informative approach in patient monitoring [7,53,73]. For instance, being 16q12.2 in gain in all the timepoints in patient CH29, we consider this aberration as evidence of a resistant clone that escapes the selective pressure exerted by treatment with fulvestrant and palbociclib. The presence within this region of loci codifying for protein with a central role in EMT and cell migration, among which AMFR and genes encoding metallothioneins [74,75], gives a further demonstration. In addition, the occurrence of CTC clones harboring gain 12q12 clearly reflects the selection exerted by palbociclib, since the amplification of the CDK4 gene represents one master mechanism of resistance of this agent [31]. Analogously, the presence of therapy-resistant clones was illustrated also in patient CH30, whose CTCs harbored gains in 11q13.2 and 22q11.2 before chemotherapy started, and persisted at the end of therapy. Again, critical genes are hosted within these regions, among which CCND1.
Last, besides marked inter-patient CTC heterogeneity, in-depth analyses revealed the emergence of a mixed group populated by CTCs with common genomic traits, being more similar to each other compared to other cells from the same patient. Interestingly, we noted that losses occurring on the long arm of chromosome 15 were frequent and appeared exclusive to the mixed group. Interestingly, copy number losses of 15q might have a profound effect on the expression of the multitude of tumor suppressor genes hosted. Therefore, the involvement of aberrations occurring in 15q in several cancer types, among which bladder [76], head-and-neck [36], and breast tumors [34,77], is not new. In addition, through enrichment analyses we found that the mixed population had the term associated with pseudopodium generation was enriched. Pseudopodia are actin-dependent cell protrusions implied in mesenchymal tumor cell migration, and inhibition of the protein involved has been proposed as a potential strategy for metastasis blockade [78,79]. To the best of our knowledge, this is the first description of a further mixed population, but understanding the exact significance of this crossed-patient CTC set is nearly impossible within our analyses. However, since the enrolled patients had undergone breast surgery before the diagnosis of metastasis, we cannot exclude that this condition could be derived from the different sources of CTCs, i.e., occult niches and metastasis. Further analyses on a higher number of cases and CTCs and on the metastatic site and primary tumor would be helpful to address this topic.
5. Conclusions
Through single cell analysis, we found that MBC CTCs display self-specific mutational signatures but might retain molecular traces of their clonal origin. Moreover, single-cell CNA profiling brings out the presence of frequent aberrations implying genes involved in breast tumorigenesis, while longitudinal analyses allow us to track the clonal selection of CTCs during treatment. Moreover, despite the great heterogeneity, a group of CTCs from different patients sharing common genomic traits emerged, displaying losses on 15q and enrichment of terms associated with pseudopodium generation as frequent events. Collectively, our findings demonstrate that single-cell molecular analyses could be exploited in the future to better address therapeutic strategies. Further investigations to better characterize this mixed population are needed to understand its role in MBC.
Acknowledgments
This work was partly supported thanks to the contribution of Ricerca Corrente by the Italian Ministry of Health within the research lines “Innovative therapies, phase I-III clinical trials and therapeutic strategy trials based on preclinical models, onco-immunological mechanisms and nanovectors” and “Precision, gender and ethnicity-based medicine and geroscience: genetic-molecular mechanisms in the development, characterization and treatment of tumors”. Giulia Gallerani is currently working at Department of Experimental, Diagnostic and Specialty Medicine (DIMES), University of Bologna, Bologna, Italy.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cancers14163925/s1, Figure S1. DNA integrity testing in sorted cells; Figure S2. Genomic copy number aberration profiles of two representative single circulating tumor cells (CTCs) and one lymphocyte pool from patient CH28; Figure S3. Genomic Identification of Significant Targets in Cancer (GISTIC) amplification and deletion plots on single circulating tumor cells (CTCs) from the crossed-patients CTC set; Figure S4. Copy Number aberration (CNA) plot of the most representative circulating tumor cells (CTCs) for each patient; Table S1. List of the variants detected in single circulating tumor cells (CTCs) of patients in the different timepoints; Table S2. enrichment analysis of crossed-patient CTC set; Table S3. enrichment analysis of all the investigated CTCs.
Author Contributions
Conceptualization, T.R. and G.G.; methodology, T.R., P.F. and G.G.; formal analysis, D.A. and M.T.; investigation, T.R., E.R. and G.G.; resources, A.R., M.P., R.M. and G.M.; data curation, T.R. and G.G.; writing—original draft preparation, T.R.; writing—review and editing, F.F. and G.G.; project administration, T.R. and G.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Romagna Ethics Committee (CEROM) of Meldola (Protocol code IRST174.19; 9 November 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.DeSantis C.E., Ma J., Gaudet M.M., Newman L.A., Miller K.D., Goding Sauer A., Jemal A., Siegel R.L. Breast Cancer Statistics, 2019. CA Cancer J. Clin. 2019;69:438–451. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 3.Wang R., Zhu Y., Liu X., Liao X., He J., Niu L. The Clinicopathological Features and Survival Outcomes of Patients with Different Metastatic Sites in Stage IV Breast Cancer. BMC Cancer. 2019;19:1091. doi: 10.1186/s12885-019-6311-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alix-Panabières C., Pantel K. Circulating Tumor Cells: Liquid Biopsy of Cancer. Clin. Chem. 2013;59:110–118. doi: 10.1373/clinchem.2012.194258. [DOI] [PubMed] [Google Scholar]
- 5.Giordano A., Cristofanilli M. CTCs in Metastatic Breast Cancer. Recent Results Cancer Res. 2012;195:193–201. doi: 10.1007/978-3-642-28160-0_18. [DOI] [PubMed] [Google Scholar]
- 6.Giuliano M., Giordano A., Jackson S., De Giorgi U., Mego M., Cohen E.N., Gao H., Anfossi S., Handy B.C., Ueno N.T., et al. Circulating Tumor Cells as Early Predictors of Metastatic Spread in Breast Cancer Patients with Limited Metastatic Dissemination. Breast Cancer Res. 2014;16:440. doi: 10.1186/s13058-014-0440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossi T., Gallerani G., Angeli D., Cocchi C., Bandini E., Fici P., Gaudio M., Martinelli G., Rocca A., Maltoni R., et al. Single-Cell NGS-Based Analysis of Copy Number Alterations Reveals New Insights in Circulating Tumor Cells Persistence in Early-Stage Breast Cancer. Cancers. 2020;12:2490. doi: 10.3390/cancers12092490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruno S., Bochicchio M.T., Franchini E., Padella A., Marconi G., Ghelli Luserna di Rorà A., Venturi C., Raffini M., Prisinzano G., Ferrari A., et al. Identification of Two DNMT3A Mutations Compromising Protein Stability and Methylation Capacity in Acute Myeloid Leukemia. J. Oncol. 2019;2019:5985923. doi: 10.1155/2019/5985923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sturgill E.G., Misch A., Lachs R., Jones C.C., Schlauch D., Jones S.F., Shastry M., Yardley D.A., Burris H.A., Spigel D.R., et al. Next-Generation Sequencing of Patients with Breast Cancer in Community Oncology Clinics. JCO Precis. Oncol. 2021;5:1297–1311. doi: 10.1200/PO.20.00469. [DOI] [PubMed] [Google Scholar]
- 10.Goodman A.M., Choi M., Wieduwilt M., Mulroney C., Costello C., Frampton G., Miller V., Kurzrock R. Next-Generation Sequencing Reveals Potentially Actionable Alterations in the Majority of Patients with Lymphoid Malignancies. JCO Precis. Oncol. 2017;1:1–13. doi: 10.1200/PO.16.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paoletti C., Cani A.K., Larios J.M., Hovelson D.H., Aung K., Darga E.P., Cannell E.M., Baratta P.J., Liu C.J., Chu D., et al. Comprehensive Mutation and Copy Number Profiling in Archived Circulating Breast Cancer Tumor Cells Documents Heterogeneous Resistance Mechanisms. Cancer Res. 2018;78:1110–1122. doi: 10.1158/0008-5472.CAN-17-2686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li H., Durbin R. Fast and Accurate Short Read Alignment with Burrows-Wheeler Transform. Bioinformatics. 2009;25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenna A., Hanna M., Banks E., Sivachenko A., Cibulskis K., Kernytsky A., Garimella K., Altshuler D., Gabriel S., Daly M., et al. The Genome Analysis Toolkit: A MapReduce Framework for Analyzing next-Generation DNA Sequencing Data. Genome Res. 2010;20:1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koboldt D.C., Zhang Q., Larson D.E., Shen D., McLellan M.D., Lin L., Miller C.A., Mardis E.R., Ding L., Wilson R.K. VarScan 2: Somatic Mutation and Copy Number Alteration Discovery in Cancer by Exome Sequencing. Genome Res. 2012;22:568–576. doi: 10.1101/gr.129684.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang K., Li M., Hakonarson H. ANNOVAR: Functional Annotation of Genetic Variants from High-Throughput Sequencing Data. Nucleic Acids Res. 2010;38:e164. doi: 10.1093/nar/gkq603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boeva V., Popova T., Bleakley K., Chiche P., Cappo J., Schleiermacher G., Janoueix-Lerosey I., Delattre O., Barillot E. Control-FREEC: A Tool for Assessing Copy Number and Allelic Content Using next-Generation Sequencing Data. Bioinformatics. 2012;28:423–425. doi: 10.1093/bioinformatics/btr670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danecek P., Bonfield J.K., Liddle J., Marshall J., Ohan V., Pollard M.O., Whitwham A., Keane T., McCarthy S.A., Davies R.M., et al. Twelve Years of SAMtools and BCFtools. Gigascience. 2021;10:giab008. doi: 10.1093/gigascience/giab008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Möhlendick B., Bartenhagen C., Behrens B., Honisch E., Raba K., Knoefel W.T., Stoecklein N.H. A Robust Method to Analyze Copy Number Alterations of Less than 100 Kb in Single Cells Using Oligonucleotide Array CGH. PLoS ONE. 2013;8:e67031. doi: 10.1371/journal.pone.0067031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashburner M., Ball C.A., Blake J.A., Botstein D., Butler H., Cherry J.M., Davis A.P., Dolinski K., Dwight S.S., Eppig J.T., et al. Gene Ontology: Tool for the Unification of Biology. Nat. Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuleshov M.V., Jones M.R., Rouillard A.D., Fernandez N.F., Duan Q., Wang Z., Koplev S., Jenkins S.L., Jagodnik K.M., Lachmann A., et al. Enrichr: A Comprehensive Gene Set Enrichment Analysis Web Server 2016 Update. Nucleic Acids Res. 2016;44:W90–W97. doi: 10.1093/nar/gkw377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mermel C.H., Schumacher S.E., Hill B., Meyerson M.L., Beroukhim R., Getz G. GISTIC2.0 Facilitates Sensitive and Confident Localization of the Targets of Focal Somatic Copy-Number Alteration in Human Cancers. Genome Biol. 2011;12:R41. doi: 10.1186/gb-2011-12-4-r41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Condorelli R., Spring L., O’Shaughnessy J., Lacroix L., Bailleux C., Scott V., Dubois J., Nagy R.J., Lanman R.B., Iafrate A.J., et al. Polyclonal RB1 Mutations and Acquired Resistance to CDK 4/6 Inhibitors in Patients with Metastatic Breast Cancer. Ann. Oncol. 2018;29:640–645. doi: 10.1093/annonc/mdx784. [DOI] [PubMed] [Google Scholar]
- 23.Gymnopoulos M., Elsliger M.-A., Vogt P.K. Rare Cancer-Specific Mutations in PIK3CA Show Gain of Function. Proc. Natl. Acad. Sci. USA. 2007;104:5569–5574. doi: 10.1073/pnas.0701005104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Luca F., Rotunno G., Salvianti F., Galardi F., Pestrin M., Gabellini S., Simi L., Mancini I., Vannucchi A.M., Pazzagli M., et al. Mutational Analysis of Single Circulating Tumor Cells by next Generation Sequencing in Metastatic Breast Cancer. Oncotarget. 2016;7:26107–26119. doi: 10.18632/oncotarget.8431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao S.P., Kiliti A.J., Zhang K., Vasani N., Mao N., Jordan E., Wise H.C., Shrestha Bhattarai T., Hu W., Dorso M., et al. AKT1 E17K Inhibits Cancer Cell Migration by Abrogating β-Catenin Signaling. Mol. Cancer Res. 2021;19:573–584. doi: 10.1158/1541-7786.MCR-20-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudolph M., Anzeneder T., Schulz A., Beckmann G., Byrne A.T., Jeffers M., Pena C., Politz O., Köchert K., Vonk R., et al. AKT1 E17K Mutation Profiling in Breast Cancer: Prevalence, Concurrent Oncogenic Alterations, and Blood-Based Detection. BMC Cancer. 2016;16:622. doi: 10.1186/s12885-016-2626-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Y., Huang L., Dong Y., Tao C., Zhang R., Shao H., Shen H. Effect of AKT1 (p. E17K) Hotspot Mutation on Malignant Tumorigenesis and Prognosis. Front. Cell Dev. Biol. 2020;8:573599. doi: 10.3389/fcell.2020.573599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernández-Madrid F., Tang N., Alansari H., Granda J.L., Tait L., Amirikia K.C., Moroianu M., Wang X., Karvonen R.L. Autoantibodies to Annexin XI-A and Other Autoantigens in the Diagnosis of Breast Cancer. Cancer Res. 2004;64:5089–5096. doi: 10.1158/0008-5472.CAN-03-0932. [DOI] [PubMed] [Google Scholar]
- 29.Elsheikh S., Green A.R., Aleskandarany M.A., Grainge M., Paish C.E., Lambros M.B.K., Reis-Filho J.S., Ellis I.O. CCND1 Amplification and Cyclin D1 Expression in Breast Cancer and Their Relation with Proteomic Subgroups and Patient Outcome. Breast Cancer Res. Treat. 2008;109:325–335. doi: 10.1007/s10549-007-9659-8. [DOI] [PubMed] [Google Scholar]
- 30.Castells A., Gusella J.F., Ramesh V., Rustgi A.K. A Region of Deletion on Chromosome 22q13 Is Common to Human Breast and Colorectal Cancers. Cancer Res. 2000;60:2836–2839. [PubMed] [Google Scholar]
- 31.Li Z., Zou W., Zhang J., Zhang Y., Xu Q., Li S., Chen C. Mechanisms of CDK4/6 Inhibitor Resistance in Luminal Breast Cancer. Front. Pharmacol. 2020;11:580251. doi: 10.3389/fphar.2020.580251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karlseder J., Zeillinger R., Schneeberger C., Czerwenka K., Speiser P., Kubista E., Birnbaum D., Gaudray P., Theillet C. Patterns of Dna Amplification at Band Q13 of Chromosome 11 in Human Breast Cancer. Genes Chromosom. Cancer. 1994;9:42–48. doi: 10.1002/gcc.2870090108. [DOI] [PubMed] [Google Scholar]
- 33.Ormandy C.J., Musgrove E.A., Hui R., Daly R.J., Sutherland R.L. Cyclin D1, EMS1 and 11q13 Amplification in Breast Cancer. Breast Cancer Res. Treat. 2003;78:323–335. doi: 10.1023/A:1023033708204. [DOI] [PubMed] [Google Scholar]
- 34.Rhiem K., Klein A., Münch M., Kreutzfeld R., Ramser J., Wardelmann E., Schackert G., von Deimling A., Wiestler O.D., Schmutzler R.K. Chromosomal Region 15q21.1 Is a Frequent Target of Allelic Imbalance in Advanced Breast Carcinomas. Int. J. Cancer. 2003;106:74–77. doi: 10.1002/ijc.11169. [DOI] [PubMed] [Google Scholar]
- 35.Wick W., Petersen I., Schmutzler R.K., Wolfarth B., Lenartz D., Bierhoff E., Hümmerich J., Müller D.J., Stangl A.P., Schramm J., et al. Evidence for a Novel Tumor Suppressor Gene on Chromosome 15 Associated with Progression to a Metastatic Stage in Breast Cancer. Oncogene. 1996;12:973–978. [PubMed] [Google Scholar]
- 36.Poetsch M., Kleist B. Loss of Heterozygosity at 15q21.3 Correlates with Occurrence of Metastases in Head and Neck Cancer. Mod. Pathol. 2006;19:1462–1469. doi: 10.1038/modpathol.3800666. [DOI] [PubMed] [Google Scholar]
- 37.Kee H.J., Shin J.H., Chang J., Chung K.Y., Shin D.H., Kim Y.S., Kim S.K., Kim S.K. Identification of Tumor Suppressor Loci on the Long Arm of Chromosome 15 in Primary Small Cell Lung Cancer. Yonsei Med. J. 2003;44:65. doi: 10.3349/ymj.2003.44.1.65. [DOI] [PubMed] [Google Scholar]
- 38.Kaur E., Agrawal R., Sengupta S. Functions of BLM Helicase in Cells: Is It Acting Like a Double-Edged Sword? Front. Genet. 2021;12:634789. doi: 10.3389/fgene.2021.634789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yuan X.-W., Wang D.-M., Hu Y., Tang Y.-N., Shi W.-W., Guo X.-J., Song J.-G. Hepatocyte Nuclear Factor 6 Suppresses the Migration and Invasive Growth of Lung Cancer Cells through P53 and the Inhibition of Epithelial-Mesenchymal Transition. J. Biol. Chem. 2013;288:31206–31216. doi: 10.1074/jbc.M113.480285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gurrieri C., Capodieci P., Bernardi R., Scaglioni P.P., Nafa K., Rush L.J., Verbel D.A., Cordon-Cardo C., Pandolfi P.P. Loss of the Tumor Suppressor PML in Human Cancers of Multiple Histologic Origins. J. Natl. Cancer Inst. 2004;96:269–279. doi: 10.1093/jnci/djh043. [DOI] [PubMed] [Google Scholar]
- 41.Huang T., Sun L., Yuan X., Qiu H. Thrombospondin-1 Is a Multifaceted Player in Tumor Progression. Oncotarget. 2017;8:84546–84558. doi: 10.18632/oncotarget.19165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li X., Xu B., Moran M.S., Zhao Y., Su P., Haffty B.G., Shao C., Yang Q. 53BP1 Functions as a Tumor Suppressor in Breast Cancer via the Inhibition of NF-ΚB through MiR-146a. Carcinogenesis. 2012;33:2593–2600. doi: 10.1093/carcin/bgs298. [DOI] [PubMed] [Google Scholar]
- 43.Schafer Z.T., Parrish A.B., Wright K.M., Margolis S.S., Marks J.R., Deshmukh M., Kornbluth S. Enhanced Sensitivity to Cytochrome c –Induced Apoptosis Mediated by PHAPI in Breast Cancer Cells. Cancer Res. 2006;66:2210–2218. doi: 10.1158/0008-5472.CAN-05-3923. [DOI] [PubMed] [Google Scholar]
- 44.Wu S., Xue W., Huang X., Yu X., Luo M., Huang Y., Liu Y., Bi Z., Qiu X., Bai S. Distinct Prognostic Values of ALDH1 Isoenzymes in Breast Cancer. Tumor Biol. 2015;36:2421–2426. doi: 10.1007/s13277-014-2852-6. [DOI] [PubMed] [Google Scholar]
- 45.Ma W., Stafford L.J., Li D., Luo J., Li X., Ning G., Liu M. GCIP/CCNDBP1, a Helix–Loop–Helix Protein, Suppresses Tumorigenesis. J. Cell. Biochem. 2007;100:1376–1386. doi: 10.1002/jcb.21140. [DOI] [PubMed] [Google Scholar]
- 46.Oudenaarden C.R.L., van de Ven R.A.H., Derksen P.W.B. Re-Inforcing the Cell Death Army in the Fight against Breast Cancer. J. Cell Sci. 2018;131:jcs212563. doi: 10.1242/jcs.212563. [DOI] [PubMed] [Google Scholar]
- 47.Kim T.E., Kim Y.W., Hwang S.Y., Shin S.M., Shin J.W., Lee Y.H., Shin S.Y., Han K.T., Lee J.M., Namkoong S.E., et al. Candidate Tumor Suppressor, HCCS-1, Is Downregulated in Human Cancers and Induces Apoptosis in Cervical Cancer. Int. J. Cancer. 2002;97:780–786. doi: 10.1002/ijc.10124. [DOI] [PubMed] [Google Scholar]
- 48.Chen L., Zhang Z., Yi Z., Li J. MicroRNA-211-5p Suppresses Tumour Cell Proliferation, Invasion, Migration and Metastasis in Triple-Negative Breast Cancer by Directly Targeting SETBP1. Br. J. Cancer. 2017;117:78–88. doi: 10.1038/bjc.2017.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li M., Pan M., Wang J., You C., Zhao F., Zheng D., Guo M., Xu H., Wu D., Wang L., et al. MiR-7 Reduces Breast Cancer Stem Cell Metastasis via Inhibiting RELA to Decrease ESAM Expression. Mol. Ther.-Oncolytics. 2020;18:70–82. doi: 10.1016/j.omto.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bandini E., Fanini F., Vannini I., Rossi T., Plousiou M., Tumedei M.M., Limarzi F., Maltoni R., Fabbri F., Hrelia S., et al. MiR-9-5p as a Regulator of the Androgen Receptor Pathway in Breast Cancer Cell Lines. Front. Cell Dev. Biol. 2020;8:579160. doi: 10.3389/fcell.2020.579160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barbano R., Pasculli B., Rendina M., Fontana A., Fusilli C., Copetti M., Castellana S., Valori V.M., Morritti M., Graziano P., et al. Stepwise Analysis of MIR9 Loci Identifies MiR-9-5p to Be Involved in Oestrogen Regulated Pathways in Breast Cancer Patients. Sci. Rep. 2017;7:45283. doi: 10.1038/srep45283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zou Y., Chen Y., Yao S., Deng G., Liu D., Yuan X., Liu S., Rao J., Xiong H., Yuan X., et al. MiR-422a Weakened Breast Cancer Stem Cells Properties by Targeting PLP2. Cancer Biol. Ther. 2018;19:436–444. doi: 10.1080/15384047.2018.1433497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Silvestri M., Dugo M., Vismara M., De Cecco L., Lanzoni D., Vingiani A., Folli S., De Santis M.C., de Braud F., Pruneri G., et al. Copy Number Alterations Analysis of Primary Tumor Tissue and Circulating Tumor Cells from Patients with Early-Stage Triple Negative Breast Cancer. Sci. Rep. 2022;12:1470. doi: 10.1038/s41598-022-05502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Menyailo M.E., Tretyakova M.S., Denisov E. V Heterogeneity of Circulating Tumor Cells in Breast Cancer: Identifying Metastatic Seeds. Int. J. Mol. Sci. 2020;21:1696. doi: 10.3390/ijms21051696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cristofanilli M., Budd G.T., Ellis M.J., Stopeck A., Matera J., Miller M.C., Reuben J.M., Doyle G.V., Allard W.J., Terstappen L.W.M.M., et al. Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast Cancer. N. Engl. J. Med. 2004;351:781–791. doi: 10.1056/NEJMoa040766. [DOI] [PubMed] [Google Scholar]
- 56.Riebensahm C., Joosse S.A., Mohme M., Hanssen A., Matschke J., Goy Y., Witzel I., Lamszus K., Kropidlowski J., Petersen C., et al. Clonality of Circulating Tumor Cells in Breast Cancer Brain Metastasis Patients. Breast Cancer Res. 2019;21:101. doi: 10.1186/s13058-019-1184-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fusco N., Malapelle U., Fassan M., Marchiò C., Buglioni S., Zupo S., Criscitiello C., Vigneri P., Dei Tos A.P., Maiorano E., et al. PIK3CA Mutations as a Molecular Target for Hormone Receptor-Positive, HER2-Negative Metastatic Breast Cancer. Front. Oncol. 2021;11:644737. doi: 10.3389/fonc.2021.644737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pestrin M., Salvianti F., Galardi F., de Luca F., Turner N., Malorni L., Pazzagli M., di Leo A., Pinzani P. Heterogeneity of PIK3CA Mutational Status at the Single Cell Level in Circulating Tumor Cells from Metastatic Breast Cancer Patients. Mol. Oncol. 2015;9:749–757. doi: 10.1016/j.molonc.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deng G., Krishnakumar S., Powell A.A., Zhang H., Mindrinos M.N., Telli M.L., Davis R.W., Jeffrey S.S. Single Cell Mutational Analysis of PIK3CA in Circulating Tumor Cells and Metastases in Breast Cancer Reveals Heterogeneity, Discordance, and Mutation Persistence in Cultured Disseminated Tumor Cells from Bone Marrow. BMC Cancer. 2014;14:456. doi: 10.1186/1471-2407-14-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rossi T., Palleschi M., Angeli D., Tebaldi M., Martinelli G., Vannini I., Puccetti M., Limarzi F., Maltoni R., Gallerani G., et al. Case Report: Analysis of Circulating Tumor Cells in a Triple Negative Spindle-Cell Metaplastic Breast Cancer Patient. Front. Med. 2021;8:856. doi: 10.3389/fmed.2021.689895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.D’Oronzo S., Lovero D., Palmirotta R., Stucci L.S., Tucci M., Felici C., Cascardi E., Giardina C., Cafforio P., Silvestris F. Dissection of Major Cancer Gene Variants in Subsets of Circulating Tumor Cells in Advanced Breast Cancer. Sci. Rep. 2019;9:17276. doi: 10.1038/s41598-019-53660-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Araki K., Miyoshi Y. Mechanism of Resistance to Endocrine Therapy in Breast Cancer: The Important Role of PI3K/Akt/MTOR in Estrogen Receptor-Positive, HER2-Negative Breast Cancer. Breast Cancer. 2018;25:392–401. doi: 10.1007/s12282-017-0812-x. [DOI] [PubMed] [Google Scholar]
- 63.Gallerani G., Rossi T., Valgiusti M., Angeli D., Fici P., De Fanti S., Bandini E., Cocchi C., Frassineti G.L., Bonafè M., et al. CNA Profiling of Single CTCs in Locally Advanced Esophageal Cancer Patients during Therapy Highlights Unexplored Molecular Pathways. Cancers. 2021;13:6369. doi: 10.3390/cancers13246369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee M.-C.W., Lopez-Diaz F.J., Khan S.Y., Tariq M.A., Dayn Y., Vaske C.J., Radenbaugh A.J., Kim H.J., Emerson B.M., Pourmand N. Single-Cell Analyses of Transcriptional Heterogeneity during Drug Tolerance Transition in Cancer Cells by RNA Sequencing. Proc. Natl. Acad. Sci. USA. 2014;111:E4726–E4735. doi: 10.1073/pnas.1404656111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.WANG S.-H., LI N., WEI Y., LI Q.-R., YU Z.-P. β-Catenin Deacetylation Is Essential for WNT-Induced Proliferation of Breast Cancer Cells. Mol. Med. Rep. 2014;9:973–978. doi: 10.3892/mmr.2014.1889. [DOI] [PubMed] [Google Scholar]
- 66.Loh Y.N., Hedditch E.L., Baker L.A., Jary E., Ward R.L., Ford C.E. The Wnt Signalling Pathway Is Upregulated in an in Vitro Model of Acquired Tamoxifen Resistant Breast Cancer. BMC Cancer. 2013;13:174. doi: 10.1186/1471-2407-13-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bostner J., Ahnström Waltersson M., Fornander T., Skoog L., Nordenskjöld B., Stål O. Amplification of CCND1 and PAK1 as Predictors of Recurrence and Tamoxifen Resistance in Postmenopausal Breast Cancer. Oncogene. 2007;26:6997–7005. doi: 10.1038/sj.onc.1210506. [DOI] [PubMed] [Google Scholar]
- 68.Butt A.J., McNeil C.M., Musgrove E.A., Sutherland R.L. Downstream Targets of Growth Factor and Oestrogen Signalling and Endocrine Resistance: The Potential Roles of c-Myc, Cyclin D1 and Cyclin E. Endocr.-Relat. Cancer. 2005;12:S47–S59. doi: 10.1677/erc.1.00993. [DOI] [PubMed] [Google Scholar]
- 69.Roy P.G., Pratt N., Purdie C.A., Baker L., Ashfield A., Quinlan P., Thompson A.M. High CCND1 Amplification Identifies a Group of Poor Prognosis Women with Estrogen Receptor Positive Breast Cancer. Int. J. Cancer. 2010;127:355–360. doi: 10.1002/ijc.25034. [DOI] [PubMed] [Google Scholar]
- 70.Tchakarska G., Sola B. The Double Dealing of Cyclin D1. Cell Cycle. 2020;19:163–178. doi: 10.1080/15384101.2019.1706903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Massink M.P.G., Kooi I.E., Martens J.W.M., Waisfisz Q., Meijers-Heijboer H. Genomic Profiling of CHEK2*1100delC-Mutated Breast Carcinomas. BMC Cancer. 2015;15:877. doi: 10.1186/s12885-015-1880-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nevanlinna H., Bartek J. The CHEK2 Gene and Inherited Breast Cancer Susceptibility. Oncogene. 2006;25:5912–5919. doi: 10.1038/sj.onc.1209877. [DOI] [PubMed] [Google Scholar]
- 73.Castro-Giner F., Aceto N. Tracking Cancer Progression: From Circulating Tumor Cells to Metastasis. Genome Med. 2020;12:31. doi: 10.1186/s13073-020-00728-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Denisenko T.V., Gorbunova A.S., Zhivotovsky B. Mitochondrial Involvement in Migration, Invasion and Metastasis. Front. Cell Dev. Biol. 2019;7:355. doi: 10.3389/fcell.2019.00355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Si M., Lang J. The Roles of Metallothioneins in Carcinogenesis. J. Hematol. Oncol. 2018;11:107. doi: 10.1186/s13045-018-0645-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Natrajan R., Louhelainen J., Williams S., Laye J., Knowles M.A. High-Resolution Deletion Mapping of 15q13.2-Q21.1 in Transitional Cell Carcinoma of the Bladder. Cancer Res. 2003;63:7657–7662. [PubMed] [Google Scholar]
- 77.Fang M., Toher J., Morgan M., Davison J., Tannenbaum S., Claffey K. Genomic Differences between Estrogen Receptor (ER)-Positive and ER-Negative Human Breast Carcinoma Identified by Single Nucleotide Polymorphism Array Comparative Genome Hybridization Analysis. Cancer. 2011;117:2024–2034. doi: 10.1002/cncr.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shankar J., Messenberg A., Chan J., Underhill T.M., Foster L.J., Nabi I.R. Pseudopodial Actin Dynamics Control Epithelial-Mesenchymal Transition in Metastatic Cancer Cells. Cancer Res. 2010;70:3780–3790. doi: 10.1158/0008-5472.CAN-09-4439. [DOI] [PubMed] [Google Scholar]
- 79.Choi S., Bhagwat A.M., Al Mismar R., Goswami N., Ben Hamidane H., Sun L., Graumann J. Proteomic Profiling of Human Cancer Pseudopodia for the Identification of Anti-Metastatic Drug Candidates. Sci. Rep. 2018;8:5858. doi: 10.1038/s41598-018-24256-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.