Abstract
Simple Summary
Aiming to discover potential treatments for GBM, this review connects emerging research on the roles of neurotransmitters in the normal neural and the GBM microenvironments and sheds light on the prospects of their application in the neuropharmacology of GBM. Conventional therapy is blamed for its poor effect, especially in inhibiting tumor recurrence and invasion. Facing this dilemma, we focus on neurotransmitters that modulate GBM initiation, progression and invasion, hoping to provide novel therapy targeting GBM. By analyzing research concerning GBM therapy systematically and scientifically, we discover increasing insights into the regulatory effects of neurotransmitters, some of which have already shown great potential in research in vivo or in vitro. After that, we further summarize the potential drugs in correlation with previously published research. In summary, it is worth expecting that targeting neurotransmitters could be a promising novel pharmacological approach for GBM treatment.
Abstract
For decades, glioblastoma multiforme (GBM), a type of the most lethal brain tumor, has remained a formidable challenge in terms of its treatment. Recently, many novel discoveries have underlined the regulatory roles of neurotransmitters in the microenvironment both physiologically and pathologically. By targeting the receptors synaptically or non-synaptically, neurotransmitters activate multiple signaling pathways. Significantly, many ligands acting on neurotransmitter receptors have shown great potential for inhibiting GBM growth and development, requiring further research. Here, we provide an overview of the most novel advances concerning the role of neurotransmitters in the normal neural and the GBM microenvironments, and discuss potential targeted drugs used for GBM treatment.
Keywords: neurotransmitters, glioblastomas multiforme (GBM), neural microenvironment, GBM microenvironment, targeted therapies, antagonist/agonist
1. Introduction
Glioblastoma (GBM; Grade IV astrocytoma) is among the most aggressive tumors of the central nervous system (CNS) [1], characterized by fast development and an average survival of only 14 months in patients diagnosed with GBM. Currently, treatment strategies for GBM patients are limited. Radiotherapy and chemotherapy with temozolomide (TMZ) following debulking surgery are the standard treatment options [2]. Although the combination of TMZ has been considered a significant improvement in GBM treatment, it just prolongs the survival time of patients by 2 months on average [2,3,4]. Furthermore, according to research published by CA Cancer J Clin in 2020 [5], many patients with recurrent GBM are not admitted into continuous treatment, which basically indicates the failure of the first surgery. Until now, there is no treatment standard for recurrence and no drugs that extend the survival time. Thus, more effective treatment options to change the poor outcomes of GBM patients are urgently needed.
Researchers have been exploring immunotherapy and precision oncology approaches in recent years. Although some of them have revealed great potential when applied in vitro or in vivo, many of them failed in clinical trials due to unknown reasons. The main factors underlying the high invasiveness and recurrence of GBM are rather complex. There have been some suggestions about paying more attention to the tumor microenvironment, including the extracellular matrix (ECM), communication between glioblastoma stem cells (GSCs; or brain tumor initiating cells, BTICs) and glial cells, etc. [6,7,8,9,10]. Neurotransmitters have long been recognized as prominent signaling molecules of neurogenesis and homeostasis in the CNS [11]. It is found that neurotransmitters could make an overall impact on GBM behaviors through reusing signaling pathways in the normal neural microenvironment, thus, providing a possible way to uncover the mystery of GBM biology [12,13].
By summarizing recent results, we identify ten neurotransmitters as key players in GBM behaviors, which could be classified according to their chemical constitution: (1) acetylcholine (Ach); (2) amino acids, such as glutamate (Glu) and gamma-aminobutyric acid (GABA); (3) biogenic amines, such as dopamine, serotonin (5-HT) and norepinephrine (NE); (4) neuropeptides, such as substance P (SP) and neuropeptide Y (NPY); (5) purines, such as adenosine triphosphate (ATP); (6) gases, such as nitric oxide (NO) [14]. Here, we aim to address three critical areas: (i) we investigate the role of neurotransmitters in the normal neural microenvironment and the GBM microenvironment; (ii) we discuss the key molecular pathways associated with the growth and progression of GBM at the cellular level; (iii) we provide an overview of current knowledge regarding the connections between each neurotransmitter and GBM and focus on the development of therapeutic strategies targeting neurotransmitters.
2. Neurotransmitters Function as Necessary Components of Neural Microenvironment and GBM Microenvironment
Traditionally, neurotransmitter signaling is mediated by neurotransmitters released from synapses (‘phasic activation’). However, neurotransmitters diffused from synapses or secreted from non-synapses can cause the activation of target cells as well (‘tonic activation’) [15]. In other words, in addition to being produced by the autonomic nervous system, neurotransmitters can also be released from immunocytes and tumor cells [11]. Meanwhile, numerous non-neurons, such as astrocytes and tumor cells, could react to neurotransmitters via expressing receptors [15,16,17].
It has been demonstrated that neurotransmitters have an impact on adult neurogenesis [15]. Although neurogenesis mainly occurs in the embryonic and early postnatal brain, neural stem cells (NSCs) and neural progenitor cells (NPCs) from the subventricular zone (SVZ) in the lateral ventricles and the subgranular zone (SGZ) in the dentate gyrus of the hippocampus are able to produce new neurons and glial cells in adult brains [18,19]. In these areas, a specific microenvironment, composed of brain microvessels surrounded by neurons and non-neurons, supports the preservation of some characteristics that are recognized as stem cell properties, such as the proliferative and self-renewal capacity of cells. The non-neuron components include NSCs, NPCs, ependymal cells, astrocytes, microglia, macrophages and the ECM [12,19].
By an autocrine or paracrine action, neurotransmitters establish a close link with neurogenesis, especially in the cell proliferation, migration, survival and differentiation of NSCs/NPCs. For example, recent studies have identified the connection between mAChRs and adult hippocampal neurogenesis both in vitro [20] and in vivo [21]. Meanwhile, ACh-nAChRs contribute to the postnatal reactivation of NSCs and adult neurogenesis by maintaining the survival of immature neurons and promoting the proliferation of NSCs in SVZ and SGZ [22]. In the adult brain, the activation of glutamate receptors (GluRs) in NPCs correlates with neurogenesis via inducing cell proliferation, migration, survival and cell differentiation of NPCs [23]. NPY in SVZ and dentate gyrus acts as a regulator of the proliferation, differentiation and migration of NSCs [24].
Furthermore, neurotransmitters act as a universal currency for intercellular communication to connect different types of cells in the neural microenvironment. For instance, GABA mediates the intercellular communication between NPCs in SVZ, playing a role in controlling the migration and cell proliferation of NPCs [25]. ATP has been well-known as energy currency and is involved in various kinds of physiological activities. In general, ATP is released from synaptic vesicles and is able to communicate with glia around the synapse. Glial cells can also release ATP to neurons. In this process, purinergic signaling plays the role of key position in communication between neurons and glial cells [26] (further information in Table 1).
Table 1.
The function of neurotransmitters in CNS and GBM.
| Neurotransmitters | Receptors | Physiological Functions | References | Pathological Functions | References |
|---|---|---|---|---|---|
| Acetylcholine | mAChR M1–M5 nAChR |
|
[20,21,22] |
|
[27,28,29,30,31,32,33,34,35,36] |
| Glutamate | NMDAR AMPAR mGluR I–III |
|
[23,37,38,39] |
|
[40,41,42,43,44,45,46,47,48,49,50] |
| GABA | GABAAR GABABR GABACR |
|
[25,51] |
|
[12,52,53,54] |
| Dopamine | DRD1-DRD5 |
|
[55,56,57] |
|
[58] |
| Serotonin | 5-HTR 1–7 |
|
[59] |
|
[60] |
| Norepinephrine/ Noradrenaline | β-AR |
|
[61] |
|
[62,63,64] |
| Purinergic | P1,P2 |
|
[65] |
|
[66] |
| Neuropeptide Y | Y1, Y2, Y4, Y5 |
|
[24,67] |
|
[68,69] |
| Substance P | NK-1R |
|
[70] |
|
[71,72,73,74,75,76] |
| NO | - |
|
[77] |
|
[78,79,80,81,82,83,84] |
Similar to the neural microenvironment, neurotransmitters act as necessary components of the GBM microenvironment as they infiltrate tumor tissue and exert a regulatory role in the proliferation, migration, apoptosis, autophagy, metabolism, survival, differentiation and angiogenesis of GBM. It is not surprising that GBM cells may retain responsiveness to neurotransmitters [85]. On the one hand, since glioma cells share some markers and molecular characteristics with NSCs [86], it is recognized that glioma may arise from NSCs in SVZ [87]. However, there are also studies suggesting that glioma could originate from astrocytes or oligodendrocyte precursor cells (OPCs) [88], indicating the need for further research. On the other hand, similar to the neurogenesis microenvironment induced by NSCs, a specific microenvironment composed of tumor cells, neurons, stem cells, fibroblasts and vascular and immune cells has been identified in GBM [19,89]. The expression of neurotransmitter receptors has been found on all kinds of cells in the GBM microenvironment [11].
Growing evidence has confirmed the presence of GSCs, a cell subset of tumor cells that exhibit stem cell-like characteristics and express NSC markers [90]. Notably, GSCs have been considered a crucial factor in the invasion, recurrence and chemo-/radio-resistance of GBM [12,91,92]. Unlike NSCs, GSCs are characterized by uncontrolled proliferation and the ability to form a heterogeneous tumor mass through differentiating to heterogeneous cell populations [12,13,93]. Furthermore, GSCs have great potential to develop into TMZ-resistant GBM (TR-GBM) cells, especially under continuous low-dose TMZ stimulation. What should be noticed is that this kind of epigenetic plasticity is reversible, unlike the usual differentiation. It is, therefore, critical to check GSCs’ status before targeting them, to determine whether they are quiescent or proliferative [94]. In addition, the communication between GSCs and the GBM cells also contributes to drug resistance. For instance, GSC-derived PD-L1-containing exosomes have been found to activate Adenosine 5‘-monophosphate (AMP)-activated protein kinase/autophagy-related protein-1 homolog(AMPK/ULK1) pathway, suppress apoptosis and promote protective autophagy, thus, increasing TMZ-resistance in GBM [95]. Through regulating neurotransmitter-associated activities, GSCs will be silenced to some extent and, thus, reducing GBM invasion, recurrence and chemo-/radio-resistance.
3. Neurotransmitters and Their Activation on Intracellular Signaling of GBM
The Cancer Genome Atlas (TCGA) GBM dataset shows the transcriptomic and genomic changes of GBM [96]. Researchers have been exploring the mechanisms of molecular alterations in order to determine core signaling pathways that drive GBM pathogenesis. Researchers identified critical genomic mutations responsible for GBM progression: the PI3K pathway (PIK3CA, PIK3R1, PTEN, EGFR, PDGFRA, and NF1), the Rb pathway (CDK4, CDK6, CCND2, CDKN2A/B, and RB1) and the p53 pathway (MDM2, MDM4, and TP53) [97,98].
Many studies have suggested the role of neurotransmitters in intracellular molecular pathways. Of note, these molecular pathways are hijacked by GBM as well. In general, the most common intracellular signals involved are receptor tyrosine kinase (RTK) pathways [73,99], G protein-coupled receptor (GPCR) pathways [100], apoptosis and autophagy signaling pathways [101] (Figure 1).
Figure 1.
The modulation of neurotransmitters on common molecular pathways. Neurotransmitters mediate the transformation of extracellular ligand signaling into intracellular signaling through multiple kinds of receptors, thus, affecting cell proliferation, migration, metabolism, apoptosis, autophagy, survival, differentiation and angiogenesis. The main intracellular signaling includes RTK pathways, GPCR pathways, apoptosis and autophagy signaling pathways. The activation of RTKs and GPCRs are associated with Ca2+ flux, which has been considered as the initial impulse and critical modulator of GBM signaling. All neurotransmitters can be identified by GPCRs, while ACh, Glu, GABA and ATP secretion activate Ca2+ flux via ionotropic receptors. GPCR mainly consists of three families: (i) Gaq/11 family (including M1/3/5 mAChR, mGluR I, 5−HTR2, P2Y and Y1/2), (ii) Gi/o family (including M2/4 mAChR, mGluR II/III, GABABR, D2−4, P1 and 5−HTR1/5) and (iii) Gs family (including D1/5, NK−1R, 5−HTR4/6/7, β−AR and P1). The mTOR pathway plays a vital role in autophagy induction. NF−kB has been shown to get involved in tumorigenesis, tumor growth and tumor response to drugs as a transcription factor. Apoptosis is mainly related to two mechanisms: (i) the extrinsic pathways initiated by pro-apoptotic ligands and (ii) the intrinsic pathways mediated by mitochondrial permeabilization. Neurotransmitters become involved in the activation of pro−caspase−8/9/10/3.
The neurotransmitters in our studies all have receptors on cell membranes except NO. These receptors can be classified as ionotropic receptors or GPCRs. Ionotropic receptors complete transmembrane signal transduction via ion flux (including Na+, Ca2+ and Cl−), while GPCRs do that by initiating signal cascades mediated by signaling proteins [14]. In addition, we identify a signal network between Calcium (Ca2+), RTKs and GPCRs. ACh, Glu, GABA and ATP secretion activate Ca2+ flux via ionotropic receptors, serving as a Ca2+ entry from the extracellular region to the intracellular region [102]. Moreover, RTKs and GPCRs are also involved in Ca2+ release from the endoplasmic reticulum (ER) [103]. In summary, Ca2+ has been recognized as an initial impulse and critical modulator of GBM signaling involved in GBM invasion and migration. Research has demonstrated the significant role of GPCR-RTK signaling and Ca2+ signaling in non-canonical modes of RTK activation in GBM [104].
RTK signaling pathways are activated by RTKs, including epidermal growth factor receptors (EGFRs), vascular endothelial growth factor receptors (VEGFRs), hepatocyte growth factor receptors (HGFRs) and so on. Previous investigations found that abnormal activation of EGFRs is widely seen in tumor change, related to drug resistance and poor clinical outcome in patients with GBM. Unfortunately, glioblastoma cells are insensitive to EGFR tyrosine kinase inhibitors (EGFR-TKIs), creating a dilemma for drug treatment [105,106,107,108]. However, there is some interesting research exploring the underlying reasons. For instance, EGFR amplification has been identified as an independent predictor of longer survival in older patients diagnosed with GBM [109]. Furthermore, Furnari, F. B. et al. summarized the molecular mechanisms of EGFR amplification and mutations in GBM, and most importantly, revealed the intrinsic EGFR heterogeneity in GBM [110]. These findings deepen the current understanding of EGFR-targeted therapy, which is of great significance in drug design. RTK signaling pathways get involved in the modulation of cell growth, differentiation and reproduction [104,111]. There are two critical pathways altered in GBM, the Ras/MAPK (Ras protein/mitogen-activated protein kinase) and PI3K/AKT/PTEN (phosphatidylinositol 3-hydroxy kinase/protein kinase B/PTEN Phosphohydrolase), resulting in oncogenic changes that ultimately lead to uncontrolled invasion and drug resistance. The PI3K/Akt/PTEN pathway is constitutively active due to PTEN alterations, PIK3CA mutations or Akt amplification in GBM [112]. PTEN has been recognized as one of the chromosome 10 tumor suppressor genes in GBM progression [113]. The relationship between PI3KCA and PTEN has been discussed back in 2005. PIK3CA mutation can encode a protein that antagonizes PTEN in the PI3K/Akt pathway [114]. Researchers have summarized the potential mechanisms for resistance, mainly focusing on targeting RTKs [104,115].
Of note, the mammalian target of rapamycin (mTOR) pathway plays a vital role in autophagy induction [116]. For instance, mTOR can be activated through the protein kinase B (PKB/AKT) or mitogen-activated protein kinase (MAPK) pathway, thereby inhibiting cell autophagy [117]. In addition, studies have revealed that PI3K-PTEN-AKT–mTOR signaling emerges as a type of fundamental signaling pathway in the regulation of cell activities, such as cell proliferation and cell death [111]. Taking ONC201 as an example, as a dopamine receptor D2 (DRD2) antagonist, it inactivates protein kinase B/extracellular-regulated protein kinases (AKT/ERK) signaling in tumor cells [118]. Moreover, LY341495, which is a mGluR2/3 antagonist, inhibits the ERK1/2 and PI3K/AKT/mTOR pathways, thus, reducing cell growth [119].
Further, the chief regulator of cell survival is the NF-κB (nuclear factor-kB) pathway, which has been identified to be activated in over 50% of all cancers, including GBM [120]. It is known that GBM is featured with high heterogeneity [93], drug resistance and a high level of NF-kB [79]. As a transcription factor, NF-kB has been shown to get involved in tumorigenesis, tumor growth and tumor response to drugs [121]. Therefore, NF-kB followed by signaling pathways (such as signal transducer and activator of transcription 3, STAT3) has been considered the main driver in GBM [122]. Furthermore, research has shown that NF-κB is relative to all kinds of different neurotransmitters directly or indirectly, including NO, Glu and so on, thus, occupying a significant position in adjuvant therapy [123,124].
The pathways that mediate apoptosis are divided into external pathways and internal pathways. The external pathway activates pro-caspase-8 and pro-caspase-10 through the connection of pro-apoptotic ligands and death receptors extracellularly, thus, activating caspase-3 to complete cell apoptosis. Instead, the intrinsic pathway is caused by mitochondrial alterations and implicated in intracellular signaling mediated by non-receptors [125]. Strikingly, neurotransmitters have been shown to be involved in the activation of pro-caspase-8/9/10/3 and promote cell apoptosis in GBM cell lines [46,126,127].
The interactions with the ECM are also one of the neurobiological roots maintained by GBM [85]. Neurotransmitter signaling, including Ach [27], Glu [47], NE [62,128] and SP [76], plays a prominent role in the regulation of invasion behavior of GBM via acting on matrix metalloproteinases (MMPs) (Figure 2). MMPs, which are a group of proteolytic enzymes containing Zn2+ secreted by cancer cells, have the ability for dissolving various kinds of ECM that includes fibronectin, Fibrinogen, chondroitin sulfate proteoglycans (CSPGs), laminin, heparan sulfate proteoglycans (HSPGs), collagens and tenascin-C [129,130]. Furthermore, studies have revealed that GBM cells prefer to migrate to a more rigid microenvironment, resulting in the impairment of tissue morphology and promoting tumor growth and development [130]. The hardness of the microenvironment is determined by the composition of ECM: both the enhanced matrix crosslink in the ECM and the anchoring of integrin-focal adhesion complexes (FAK) between cells and the ECM have provided the desired properties to allow tumor invasion [49].
Figure 2.
The role of neurotransmitters in regulating infiltrative capacity of GBM. Neurotransmitters, such as ACh, Glu, NE and SP, regulate invasion behavior of GBM by affecting the activation of matrix metalloproteinases (MMPs). MMPs are a group of proteolytic enzymes secreted by cancer cells and have the ability for dissolving various kinds of extracellular matrix (ECM). The ECM, containing various kinds of molecules, is mainly localized to three compartments: the basement membrane (basal lamina), the perineuronal nets and the neural interstitial matrix. MMPs influence the lesion’s microenvironment during remyelination by cleaving CSPGs, laminins and ECM receptors such as integrins. GBM cells prefer to migrate to a more rigid microenvironment, resulting in the impairment of tissue morphology and promoting tumor growth and development. The hardness of the microenvironment is in relation to the composition of the ECM: both the enhanced matrix crosslink in the ECM and the anchoring of integrin-focal adhesion complexes (FAK) between cells and the ECM have provided the desired properties to allow tumor invasion. Tumor-associated microglia and macrophages (TAMs) participate in immunomodulation and MMP secretion.
Overall, at the cellular level, neurotransmitters in GBM retain the ability to transform ligand binding on the cell membrane into intracellular signaling. Elucidating common pathways associated with neurotransmitters helps in understanding the next part and facilitates the better use of neurotransmitters as a tool for treating tumors.
4. The Influence of Neurotransmitters on GBM and Potential Therapeutic Targets
Since the potent infiltrative capability of GBM makes it impossible to cure the tumor only by surgical resection, radiotherapy and chemotherapy after surgery are crucial [131]. As mentioned before, current drugs for chemotherapy are insufficient and have low-effectiveness. In this regard, the growing understanding of how neurotransmitters influence the initiation and advance of GBM has led to the development and evaluation of potential drugs targeting neurotransmitters and their receptors. In the following text, we review the existing advancement, provide a list of related experiments in Table 2 and display the targets of neurotransmitter-related drugs in Figure 3, attempting to provide a reference for future drug selection. (Due to the downregulation of GABA receptors in GBM and the lack of experiments to prove the role of Y2 receptors in GBM, we did not show these two neurotransmitters (GABA and NPY) and their receptors in Figure 3. Detailed discussion can be found in Section 4.3 and Section 4.8.1).
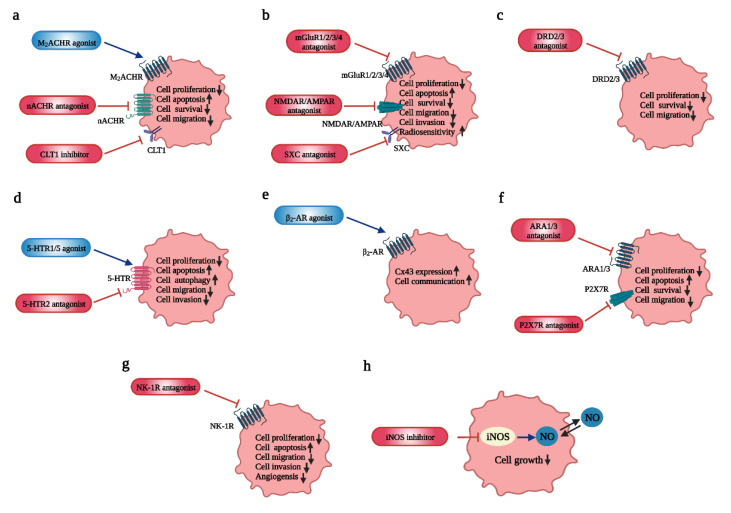
Figure 3.
Potential targets of neurotransmitter-related drugs in GBM. Different neurotransmitters and their potential targets for GBM treatment. (a) ACh and M2AChR, nAChR, CTL1. (b) Glu and mGluR1/2/3/4, NMDAR/AMPAR, SXC. (c) DA and DRD2/3. (d) 5-HT and 5-HTR1/2/5. (e) NE and β2-AR. (f) ATP and ARA1/3, P2X7R. (g) SP and NK-1R. (h) NO and iNOS inhibitor.
Of note, drugs inhibit tumor growth mainly by interfering in the balance of cell proliferation, apoptosis and autophagy, thus, serving active participation in the response of tumor cells. For example, the mutation of mitochondria DNA (mt-DNA) causes the functional disorder of mitochondria and the activation of intracellular signaling pathways, including AKT, Ras and ERK pathways, as well as the activation of hypoxia-inducible factor 1α (HIF-1α) and NF-κB, thus, regulating the expression of nuclear genes associated with drug resistance [132]. Furthermore, research has found that fluoxetine induces transmembrane Ca2+ influx and causes mitochondrial Ca2+ overload, thereby triggering apoptosis [133].
Table 2.
Potential effects of drugs targeting neurotransmitters in treating GBM.
| Drugs | Targets | Approved by FDA? | Effects | Type of Study | References |
|---|---|---|---|---|---|
| Basic Studies | |||||
| Arecaidine propargyl ester (APE) | M2 mAChR agonist | NO |
|
in vitro (GBM line U251MG and GBM line U87MG, GSC line GB7 and GSC line GB8) | [134,135] |
| Iper-8-naphthalimide(N-8-Iper) | M2 mAChR agonist | NO |
|
in vitro (GSC line GB7); in vitro (GSC line GB7 and GSC line G166) | [31,136] |
| Iper-6-phthalimide(P-6-Iper) | M2 mAChR agonist | NO | no appreciable effects on GSCs growth | in vitro (GSC line GB7) | [31] |
| Atracurium Besylate | nAChR antagonist | YES |
|
in vitro (GSC line HSR-GBM1, GSC line HSR040622 and GSC line HSR040821) | [32] |
| StN-2(MG624) | α7 and α9 nAChR antagonist | NO |
|
in vitro (GBM cell line U87) | [137] |
| StN-4 | α7 and α9/10 nAChR antagonist (silent agonist) | NO |
|
in vitro (human U87MG and GBM5 cells) | [138] |
| StN-8 | α7 and α9/10 nAChR antagonist | NO |
|
in vitro (human U87MG and GBM5 cells) | [138] |
| 3-(2,4-dimethoxybenzylidene) anabaseine (GTS-21) | α7 nAChR antagonist | NO | inhibit cell proliferation in a dose- and time-dependent manner in an α7-nAChR-dependent/α7-nAChR-independent manner | in vitro (GBM cell line A172, U87 and G28, and patient-derived glioblastoma cells) | [35] |
| Kynurenic acid (KYNA) | α7 nAChR and all iGluR antagonist | NO |
|
in vitro (GBM cell line T98G) | [139] |
| Amb4269951 | Choline Transporter-Like Protein 1(CTL1) inhibitor | NO |
|
in vitro (GBM cell line U251MG) and in vivo (mice xenograft models) | [126] |
| Dizocilpine (MK801) | NMDAR (N-methyl-D-aspartate receptor) antagonist | NO |
|
in vitro (GBM cell line LN18, GBM cell line U251MG and patient-derived glioblastoma cells) | [140] |
| Memantine | NMDAR antagonist | YES | induce cytotoxicity of GBM in a dose-dependent fashion | in vitro (human GBM cell line T98G and U87MG) | [141] |
| MP1-MP2 | NMDAR antagonist | NO | induce significant cell death by apoptosis | in vitro (human GBM cell line U87MG) | [142] |
| Ifenprodil | NMDAR GluN2B antagonist | YES | more potent than MK801 in inhibiting cell migration and survival, as well as in the sensitivity to radiation | in vitro (cell lines) | [40] |
| Perampanel (PER) | AMPAR antagonist | YES |
|
in vitro (GBM cell line U87, U138 and A172; GBM cell line HROG02, HROG05, HROG15 and HROG24) | [143,144] |
| GYKI 52466 | AMPAR GluR1 antagonist | NO | diminish cell death induced by cancer in peritumor brain | in vitro (rat F98 glioma-implanted brain slice cultures) | [145] |
| Fluoxetine | AMPAR GluR1 antagonist | YES |
|
in vitro (GBM cell line U87 and Hs683 and rat glioma cell line C6) and in vivo (experimental animal models) | [41] |
| Riluzole | mGluR1 antagonist | YES |
|
in vitro (GBM cell line U87, patient-derived glioblastoma cells) and in vivo (U87 cell xenograft model) | [127,146] |
| BAY36-7620 | mGluR1 antagonist | NO |
|
in vitro (GBM cell line U87) and in vivo (U87 cell xenograft model) | [127] |
| CPCCOEt | mGluR1 antagonist | NO |
|
in vitro (GBM cell line A172 and U87) | [147] |
| JNJ16259685 | mGluR1 antagonist | NO |
|
in vitro (GBM cell line A172 and U87) | [147] |
| (2S)-α-ethylglutamate (EGlu) | mGluR2/3 antagonist | NO | cell proliferation inhibition in a time-dependent fashion | in vitro (GBM cell line U87) | [119] |
| MTPG | mGluR2/3 antagonist | NO | cell proliferation inhibition in a time-dependent fashion | in vitro (GBM cell line U87) | [119] |
| LY341495 | mGluR2/3 antagonist | NO |
|
in vitro (GBM cell line U87) | [119] |
| Sulfasalazine (SSZ) | xc−cystine/glutamate transporter antagonist | YES |
|
in vitro (rat glioma cell F98, human glioma cell U251, primary astrocytes and neurons, and rat organotypic brain slices) | [148] |
| VU0155041 | mGluR4 antagonist | NO |
|
in vitro (GBM cell line LN229) | [46] |
| Quetiapine | DRD2 antagonist | YES |
|
in vitro (patient-derived HK-157, HK-308, HK-374, and HK-382 GBM lines) and in vivo (the GL261 orthotopic mouse models of GBM, and HK-374 patient-derived orthotopic xenografts) | [149] |
| Perphenazine | DRD2/3 and 5-HT antagonist | NO |
|
in vivo | [150] |
| Valerenic acid | HTR5A agonist | NO |
|
in vitro (U251 MG human glioblastoma cell lines) | [60] |
| Brexpiprazole | DRD2 and 5-HT1A agonist, 5HT2A antagonist | YES | increase the sensitivity of GSCs to osimertinib through the downregulation of survivin expression | in vitro (GSCs:A172GS, GS-Y01, GS-NCC01, and GS-Y) | [151,152] |
| Clenbuterol hydrochloride | β2-AR agonist | NO | upregulate Cx43 expression that promotes cell communication | in vitro (OECs) | [153] |
| AZ10606120 | P2X7R antagonist | NO |
|
in vitro (U251 MG cells) | [154,155] |
| Paris saponin H (PSH) | ARA1 and ARA3 inhibitor | NO |
|
in vitro (U251 cells) | [156] |
| 1400W, S-MIU | iNOS inhibitor | NO | inhibit the cell growth of astrocytes and U87 cell line with EGFRvIII expression | in vivo (U87 cell line, rat model) | [157,158] |
| Clinical Studies | |||||
| Memantine | NMDAR antagonist | YES | in safe combinations with TMZ in newly diagnosed GBM with a 21-month median survival and a 2-year survival rate of 43% | Phase I, randomized, (newly diagnosed, n = 85) | [159] |
| Talampanel (LY300164) | AMPAR antagonist | NO |
|
Phase II, single-agent (recurrent, n = 22) Phase II, single-arm (newly diagnosed, n = 72) Phase II, randomized, (newly diagnosed, n = 365) |
[160,161,162] |
| ONC201 | DRD2 antagonist | NO |
|
in vitro (U87MG, U251MG, U373MG, Hs683, SF-295, A172 and LN-18 cell lines) and in vivo (patient-derived GBM cell lines and orthotopic xenograft mouse models) Phase II, non-Randomized, (recurrent, n = 140) |
[163,164,165] |
| Chlorpromazine | DRD2 antagonist | YES |
|
in vitro (cell lines T98G, U-251 MG and U-87 MG) Phase II, recruiting, (newly diagnosed, n = 41) |
[166] |
| Escitalopram oxalate | SSRI (selective serotonin reuptake inhibitors) | YES |
|
in vitro (U87MG cells GBM8401 cells) Phase II, Randomized, (newly diagnosed, n = 100) |
[167] |
4.1. Acetylcholine (ACh): Regulates GBM Proliferation, Survival and Invasion
GBM may be able to synthesize ACh, which can be used as an autocrine and paracrine signaling to modulate tumor proliferation, survival and invasion [27]. The activation of AChRs, for instance, promotes the invasion of GBM via an MMP-9 activity mediated by intracellular Ca2+ increase [27]. Recent studies have indicated that M2 mAChRs exhibit inhibitory effects on the cell proliferation and survival in GBM cell lines and GSC lines. Specifically, M2 mAChRs induce apoptosis and cell cycle arrest of GBM cells, whereas they hamper the cell cycle and inhibit cell proliferation mediated by Notch-1/EGFR pathways in GSC lines [28,29,30,31]. In an elegant study, M3 mAChRs (CHRM3) appear to be implicated in the decrease of patient survival [27]. As for nAChRs, the expression of α1nAChRs (encoded by CHRNA1) and α9nAChRs (encoded by CHRNA9) is elevated and is related to reduced patient survival [27]. It is found that these two receptors correlate with the maintenance of self-renewal of GSCs in an ex-vivo experiment [32]. In GBM cell lines, the activation of α7nAChRs and α9nAChRs has shown the inhibition of cell apoptosis (via EGFR/AKT pathways) and promotion of cell proliferation (via EGFR/ERK pathways) [33,34]. What is more, the increase in α7nAChRs in GBM cells, vessel endothelium and tumor-associated macrophages of GBM have been identified, inducing the inhibition of cell proliferation [35]. The activation of AChRs (mainly α7 nAChRs) on astrocytes and microglia may also prevent excessive neuroinflammation, which causes damage to neurons and glial cells [36]. Up to now, few studies have linked the “brain cholinergic anti-inflammatory pathway” with GBM, which deserves further research.
The various relationships between GBM and AChRs, especially M2 mAChRs and α7/α9 nAChRs, support AChRs as a promising target for developing innovative antitumor therapies. N-8-Iper is the most potent agonist among the selective M2 mAChR agonists in Table 2, with approximately 100 times the potency of ACh [31]. The upregulation of some certain receptors in tumor cells is conducive to the tumor-specific action of selective ligands, without toxicity to normal cells. Since many experiments and public databases (such as accession number GSE16805) have proved that the expression of α9 nAChRs is higher in GBM [27,32,34] (no expression in normal mammalian brain [168,169,170], α9 nAChRs may be a powerful promising target. Atracurium Besylate (nAChR antagonist) [32], MG624 (α7 and α9 nAChR antagonist) [137] and StN-4/StN-8 (α7 and α9/10 nAChR antagonist) [138] have shown significant inhibitory effect on the viability of GBM/GSC cell lines. However, it has been reported that some of their anti-tumoral effects are nAChR-independent, which increases the difficulty of elaborating their mechanisms in GBM and needs additional investigations [35,138]. Strikingly, targeted drugs for AChRs combined with chemotherapeutic agents represent a new prospective treatment for GBM. For instance, the combination of N-8-Iper and doxorubicin, cisplatin or temozolomide shows a stronger impairment of the growth of GSC lines than that with the single treatment. This may be related to the decrease in the ATP-binding cassette (ABC) efflux pumps mediated by the M2 receptor, reducing the excretion of chemotherapeutic drugs [136].
It is shown that the choline metabolism increases in many tumors and the transporting system of choline, which has been recognized as an important rate-limiting step, which could be a promising target in GBM therapy [27]. Although the potential effect of Amb4269951, a Choline Transporter-Like Protein 1(CTL1) inhibitor, has been distinguished in vitro and in vivo [126], little is known about the choline transport system in GBM [171].
Notably, the blood–brain barrier (BBB) that prevents brain tumors from being infiltrated by drugs is an obstruction to be reckoned with for drug consideration. Studies have identified that nAChRs could be implicated in drug delivery through receptor-mediated transcytosis (RMT), providing a promising way for the intracranial transportation of drugs that avoids the BBB [172]. Taken together, future research should further identify potent selective AChR agonists/antagonists to develop targeted drug-screening strategies for GBM treatment.
4.2. Glutamate (Glu): Modulates GBM Growth and Progression, as Well as Increases Radiosensitivity
Recent studies have demonstrated the regulation of both synaptic and non-synaptic glutamate on embryonic neurogenesis and the migration of neurons and astrocytes. To our knowledge, these physiological processes are absent in adult brains, but could be found in glioma [39].
Multiple effects of GluRs have been found in GBM: (i) the phosphorylation of transcription factor CREB followed by NMDAR activation is responsible for the promotion of GBM survival and migration, as well as the increase in radiosensitivity through inhibiting the repairment of the DNA double-strand break (DSB) [40]; (ii) AMPARs mediate the Ca2+-dependent activation of the AKT/PKB signaling pathway, stimulating tumor growth and invasion [41,42,43,44]; (iii) different subtypes of mGluRs induce opposite effects on GBM. Studies have exhibited that more expression of mGluR3 implicates a higher malignancy of tumors and a higher fatality [45], consistent with the result of D’Alessandro, G., et al., who reported the inhibition of GBM proliferation caused by the block of mGluR2/3 [42]. Instead, mGluR4 may inhibit cell proliferation and induce apoptosis by (i) decreasing cyclin D1 expression and increasing pro-caspase-8/9/3, (ii) or regulating the expression of Bcl-2/Bax, (iii) or reducing Gli-1 expression that emerges as a transcription factor of Sonic Hedgehog (SHH) signaling [46]. Significantly, both NMDARs and APAMRs show an influence on the extracellular matrix. For one thing, NMDARs are implicated in the activation of MMP2 [47]. For another, the high expression of GluR1 may promote the expression of integrins (β1 integrins mainly) on the glioma cell membrane, which, in turn, increases the adhesion to the ECM and drives migration along perivascular and subpial spaces [48].
Accumulating evidence suggests that glutamate is an important regulator of cellular activities in both the neural and GBM microenvironment: high concentrations of glutamate in extracellular space leads to not only the excitotoxic cell death of neurons, but also the promotion of tumor growth, migration and invasion [44,49,50]. As a result, it is necessary to elucidate how the regulation of glutamate levels performs in the neural and GBM microenvironments.
Currently, the active participation of neurons, astrocytes and microglia has been identified. It is well-established that tripartite synapses composed of synaptic neurons and astrocytes produce the glutamate cycle. In the tripartite synapse, glutamate released to the synaptic cleft not only acts on postsynaptic neurons, but also diffuses around astrocytes, rendering an activation of GluRs on astrocytes and a glutamate uptake. Subsequently, astrocytes secrete glutamate to the presynaptic neuron, resulting in the glutamate cycle [173,174]. It is shown that glutamate uptake and release also occur in microglial cells [175]. Overall, glial cells uptake glutamate through glutamate transporters (EAAT) and glutamine synthetase (GS), and glutamate release may be related to the activation of glutamate-cystine antiporters, Best1 channels and Cx43 hemichannels [175]. Furthermore, microglia can also inhibit the glutamate release of glioma cells via transferring miR-124 (a tumor suppressor) to astrocytes and tumor cells by releasing Small Extracellular Vesicles (SEVs) [176]. Compared to the normal neural microenvironment, the release and conduction process of glutamate in the GBM microenvironment are altered and cause a high level of extracellular glutamate [49], which may be mediated by the following mechanisms: (i) a 100-fold excess spontaneous secretion of glutamate compared to normal levels (>100 µM), induced by the upregulation of the cystine/glutamate antiporter xc-(System xc-, SXC) and an instantaneous intracellular Ca2+ increase caused by P2X7, which is activated by high levels of ATP in the extracellular matrix; (ii) reduced reuptake of glutamate due to the decrease in excitatory amino acid transporter (EAAT2) expression; (iii) the failure of astrocytes to clear glutamate in the extracellular milieu [40,49,177,178].
The inhibitory effects of iGluR antagonists and mGluR blockers on GBM growth have been reported both in vivo experiments and in vitro experiments (Table 2). Indeed, since the interference of mGluRs in rapid excitatory impulse transmission seems much smaller than that of iGluRs, the mGluR might be a more appropriate target that exhibits less untoward reaction in patients [179]. Furthermore, the silence of mGluR1 genes has been shown to evidently reduce glioma proliferation [147].
Remarkably, diverse derivatives of memantine could be potential antitumor agents for GBM therapy as well. For example, the synthesized memantine-derived compounds MP1-10, especially MP1 and MP2, have been improved to suppress cell proliferation of T98G and U87-MG in a dose-dependent fashion. Nevertheless, further biological studies show that only MP1 exhibit appropriate solubility and enzyme stability in gastric fluids and intestinal secretions, which is appropriate for further in vivo pharmacokinetic research [142]. In addition, nitromemantine, which is the second-generation memantine derivatives, not only attenuates NMDAR signaling directly, but also carries NO to the regions with overactive NMDAR, causing high concentrations of NO and superior tumoricidal effects than memantine. However, further verifications on animal models are needed [177].
Combinatorial treatment with TMZ and other drugs, such as riluzole [180], Kynurenic acid (KYNA) [139], perampanel [143] and talampanel [49], has been a promising strategy for GBM therapies as it shows conspicuous advantages in decreasing chemoresistance, enhancing radiosensitivity and improving the survival of patients. Further study also provides a new perspective on medicine combination. For example, combinatorial treatment with fasudil and glutamate exhibits more significant inhibitory effects on cell activity and more synergist effects on lactic dehydrogenase-C4 (LDH) levels than fasudil monotherapy. Fasudil is a Rho-associated coiled-coil containing a kinase (ROCK) inhibitor that has been utilized as a common drug for clinical treatment of subarachnoid hemorrhage (SAH). In an experiment conducted on primary human GBM cells, fasudil has been found to elevate the sensitivity of GBM cells to glutamate excitotoxicity through increasing NMDAR GluN2B expression [181]. Nevertheless, whether this combination treatment is equally effective in animal models remains unknown.
Sulfasalazine (SSZ/SAS), emerged as an SXC inhibitor correlating with the release of glutamate and the intracellular transportation of cysteine, resulting in the decreased production of glutathione, thus, impairing the GBM tolerance to oxidative stress [148]. However, although SSZ has exhibited a good effect without any toxicity in experiment rodents, serious side effects on patients with GBM have been shown in two clinical trials, characterized by significant toxicity for neuronal function, bone-marrow and the hematological system (mainly leukopenia and neutropenia) [182]. Indeed, the increase in extracellular glutamate levels and synaptic damage in rat hippocampal cultures given SXC inhibitors (including sorafenib and erastin) have been identified [183]. Additionally, propofol, involved in the regulation of Ca2+ permeable AMPA receptor (CPAR)-SXC pathways, could suppress the proliferation, invasion and migration of C6 glioma cells significantly [184]. More evidence of propofol’s validity in GBM needs to be found in the future. To sum up, current knowledge of the role of glutamate in tumor proliferation, survival, migration, invasion and radiosensitivity advances our understanding of the biology and therapies of GBM. Selective ligands of GluRs and the xc−cystine/glutamate transporter that have reliable safety, high bioactivation in vivo and BBB penetrability may be potential therapeutic strategies for GBM.
4.3. Gamma-Aminobutyric Acid (GABA): Inhibits GBM Growth
The activation of GABAAR in low-grade glioma could inhibit cell growth by depolarizing the membrane through increasing intracellular Cl− caused by Na+–K+–2Cl− co-transporter NKCC1. Nevertheless, the decreased numbers of mRNA encoding GABAR subunits and loss of GABAAR in GBM may indicate the relationship between the number of functional GABAAR and the grade of the glioma [12,52,53]. It also means that GBM may counteract the attenuation of GABA on cell proliferation by decreasing the expression of GABAAR [54]. Notably, there are conflicting findings regarding whether GABA can decrease the proliferation of GSCs. Recently, the functional expression of GABAAR and a significant increase in the number of tumor cells while applying bicuculline, a GABAAR antagonist, have been identified in tumor cells from GBM patients. It is also reported that GABA selectively acts on cells with stem cell-like properties, maintaining the quiescence of GSCs and allowing GSCs to enter cell cycles again after surgical resection of tumor bulks [185]. On the contrary, El-Habr’s studies show that GABA has no inhibitory effects on GSCs [186].
Although GABA may inhibit GBM proliferation, its existence has not been confirmed in experiments so far [187]. The human glioblastoma stem cell line, U3047MG, has been recommended by Babateen, O., et al. as the model that may be suitable for exploring the potential effects of GABA on GBM in the future, due to its abundant expression of GABAR subunits and some functional channels [53].
Because of the lack of GABAR in GBM and its inability to respond to agonists/antagonists, researchers have recently focused on RNA editing and GABA metabolism. RNA editing refers to the process of post-transcription alteration of the RNA sequence via base switching/insertion/deletion, playing a distinguished role in maintaining tissue homeostasis. Recent studies have revealed that the reduction of GABRA3 editing, which is implicated in the editing of α3-GABAR, would promote tumor invasion [188]. Identifying altered RNA editing events in GBM may help to develop alternative gene-therapy options.
GABA, associated with the synthesis of succinate via activating GABA transaminase and succinic semialdehyde dehydrogenase (SSADH), has been recognized as an essential substrate of the TCA cycle and a positive regulator of GBM proliferation [189]. It is likely that GABA oxidation and SSADH activity establish new ways to target GBM [189]. However, specific SSADH inhibitors have not been detected yet. Moreover, the level of GHB (the by-product of GABA catabolism), which could be elevated by the reduction in SSADH expression or the compensation of GHB, is implicated in transforming the glioma from a highly malignant state into a phenotype that is more differentiated and less aggressive [186]. Up to now, GHB has been exploited for multiple pathological symptoms, such as narcolepsy and alcohol withdrawal. Significantly, studies have identified its good properties to pass through the BBB, indicating that it could be an additional therapeutic target in GBM [186]. To date, the GABA metabolism may be a more potent target than GABAR when discovering novel therapies for GBM.
4.4. Dopamine: Inhibits GBM Invasiveness and Migration
In general, there appear to be two main mechanisms in dopamine treatment for GBM: inhibiting tumor angiogenesis through the VEGF pathway and inducing cell autophagy mediated by the mTOR pathway or via the Beclin1 (BECN1)-dependent pathway [190,191,192]. Studies have suggested that dopamine inhibits tumor migration by reducing stress-mediated angiogenesis [58]. Surprisingly, the mechanism of how dopamine reduces angiogenesis is still under investigation, which may be a huge breakthrough [193,194,195]. Immune alterations are mainly responsible for stress-induced tumor invasion. The concept of tumor vasculature normalization was put forward by Jain et al. in 2005 [196]. Tumor associated-macrophage (TAM) polarization had been suggested as a potential target for inducing tumor vasculature normalization [197]. Research conducted on C6 glioma-bearing rats [198] proved that low dopamine modulates TAM polarization, induces vascular normalization and, thus, suppresses glioma growth. Dopamine reprograms M2-polarized macrophages by downregulating the VEGF/VEGFR2 signaling, thus, switching M2-polarized macrophages to an M1 phenotype. Furthermore, dopamine has been shown to modulate the microglial cell inflammatory response induced by IL-1b, IL-6 and inducible nitric oxide synthase (iNOS) [199,200,201]. Dopamine acting on immune-competent cells has revealed great influence on glioma development and progression. On the one hand, dopamine inhibits tumor angiogenesis. On the other hand, dopamine communicates with the immune system and participates in inflammatory activities. In addition, dopamine has been suggested as an important modulator in autophagy and apoptosis [57,202].
Moreover, DRD2 antagonists have great potential in treating GBM. ONC201 appears to act as a selective DRD2 antagonist. It may not be as strong as other DRD2 antagonists, but it performs better when it comes to clinical use for its wide anticancer effect [118]. DRD5 modulates DRD2 signaling negatively and, thus, weakens the ONC201 drug effect [203]. Moreover, ONC201 enhances radiation and the TMZ effect in GBM cell lines [163]. Chlorpromazine synergizes with TMZ in reducing the viability and cloning efficiency of GBM cells and inducing cell death [166]. A previously published article has shown that perphenazine is excellent in blocking DRD3. It can inhibit SVZ cell growth which is supported by DRD3 activation [204].
Surprisingly, DRD2 and DRD3 agonists were demonstrated to induce autophagy through the BECN1-dependent signaling pathway. This research applies dopamine as an important regulator in autophagy [192]. As mentioned before, cell proliferation is controlled by mTOR and its inactivation induces autophagy. Significantly, an uncontrolled proliferation that results from a decline in apoptosis is responsible for radiotherapy resistance to GBM treatment. Additionally, clinical use of rapamycin can upregulate drug sensitivity in glioblastoma for its inhibition of mTOR signaling [191]. In conclusion, dopamine is promising for further research.
4.5. Serotonin (5-HT): Involved in Cell Apoptosis, Autophagy and Chemotherapy Reinforcement
Serotonin activates multiple subtypes of receptors and induces different kinds of responses, as well as GBM heterogeneity [93], thus, requiring further research [190]. For example, current understanding of 5-HT-targeted drugs mostly concentrates on HTR5A and HTR7A. HTR5A was found downregulated in GBM compared to low-grade gliomas including astrocytoma, oligoastrocytoma and oligodendroglioma [60]. It was well-established that valerenic acid, a potential agonist of HTR5A, could trigger autophagy and apoptosis and, thus, induce the death of GBM cells [60]. In U373 GBM cells, interleukin-6 can be induced by serotonin activating on 5-HT7 receptors [205]. In turn, interleukin-6 contributes to supporting GBM progression via the autocrine pathway [206]. Generally, targeting 5-HT receptors is a type of potential way of treating GBM, functioning as reinforcement to chemotherapy [207,208,209].
GSCs represent one of the mechanisms responsible for the high chemoresistance of GBM that is associated with a poor prognosis [95]. In this regard, co-treatment involving 5-HT may be a potent approach to improve chemosensitivity of GSCs. For instance, brexpiprazole is able to amplify GBM response to TMZ by regulating serotonin and dopamine. Furthermore, the combination of brafiprazole and orcetinib is more effective in inhibiting GBM progression by downregulating the expression of surviving, and no significant side effect was confirmed [151].
Researchers have indicated that selective serotonin reuptake inhibitors (SSRIs) are toxic to some tumors and own a potential drug effect on GBM. SSRIs are applied in depression treatment at first and they have surprising outcomes in particular patients who suffer from depression caused by GBM. Following studies discovered that SSRIs suppress GBM cell proliferation in different ways. What is worth mentioning is that some FDA-approved antidepressants already reached favorable outcomes in clinical trials [208,210]. Considered as a more superior SSRI, escitalopram oxalate exhibits favorable tolerability. However, the understanding of the mechanism of how escitalopram oxalate suppresses GBM is still limited, which needs more research to investigate the potential use in GBM [167]. Researchers have been testing the idea of drug repurposing and evaluating drugs, and SSRIs are one of the most promising kinds.
4.6. Norepinephrine/Noradrenaline (NE/NA): Inhibits GBM Invasiveness and Migration, as Well as Modulates Tumorigenesis
In the past few decades, β-AR agonists have been indicated as one of the central modulators of tumor initiation and progression by triggering the cyclic adenosine monophosphate/protein kinase A (cAMP/PKA) and MAPK signaling. Although the precise mechanism is still unknown, it is becoming clearer as research advances [63,64]. He, J.J., et al. showed that activating β-ARs could upregulate MMP-2 and MMP-9 levels and trigger the ERK1/2 pathway, promoting U251 cell growth [128].
The level of Cx43 and gap junction intercellular communication form a transit system, which is able to amplify drug effects from a single cell to the whole tumor. Studies have demonstrated that β2-AR agonists upregulate the Cx43 protein levels in the GBM cell lines and promote cytotoxic effects [211,212].
Research conducted in astrocyte cells derived from human glioblastoma indicates that clenbuterol hydrochloride, a β2-AR agonist, upregulates the Cx43 expression level. In contrast, ICI 118551, a β2-AR antagonist reverses this activity. Moreover, both drugs have similar effects on co-culture systems. This new finding sheds light on a new approach to sensitizer design, which is to upregulate Cx43 expression levels by activating β2-AR [153].
As we discuss, activating β-ARs may result in anti-tumor effect (upregulate Cx43 protein levels) or pro-tumor effect (upregulate MMP-2 and MMP-9 levels). More research in this field would be of great help.
4.7. Purinergic: Involved in Tumorigenesis, GBM Invasion, Migration
Commonly, the expression of adenosine (P1) and nucleotide (P2) receptors is found not only on neurons, but also on glial cells. As a major regulator in presynaptic activities, P1 receptors serve as critical elements in the crosstalk among tumor cells, astrocytes and microglia, influencing tumor-related astrocyte phenotypic differentiation [66]. On the one hand, P2X ionotropic receptors participate in synaptic remodeling and rapid synaptic transmission. P2Y receptors, on the other hand, are implicated in presynaptic modulation, which includes inducing long-term (nutritional) signaling in the cell life circle. P1 and P2 receptors are both related to communication between neurons and glia cells, which modulate neuronal activities involved in inflammatory reaction, myelination, tumorigenesis and neurodegeneration [213].
Several articles published recently indicate that the elimination of extracellular ATP and the increase in adenosine directly not only affect tumor progression, invasion and angiogenesis, but also induce the migration, adhesion and homing between cancer cells, activating the immune system [214]. Activating P2X7R triggers various effects including cell growth, death and immune cell activation, depending on different kinds of microenvironment and expression levels [215,216]. P2X7R is associated with insensitivity to ATP cytotoxicity, which has been proven in research conducted in vitro by Morrone FB [217]. Research also revealed that in glioma treatment, a higher P2X7R level represents a better outcome in radiotherapy and a longer survival time. Data analysis on P2X7R articles suggests its promising future applied in predicting radiotherapy outcomes and survival probability [218]. The application of BBG (a P2X7R inhibitor) remarkably suppresses the growth of C6 tumors. However, in the U251 glioblastoma cell line, the result is just the opposite. [155]. This comparison suggests that more research is needed concerning the drug design of P2X7R.
Rhizoma Paridis (RP; the rhizome of Paris) has been proven to suppress tumor growth. Research published previously demonstrated that saponins extracted from RP has wide anti-cancer effects, such as mediating apoptosis and interfering the cell cycle, activating the immune response and inhibiting migration with angiogenesis. Paris saponin H (PSH), a steroid saponin molecule of RP, is similar to Paris Saponin II, Polyphyllin D and Polyphyllin VII. Paris Saponin II inhibits angiogenesis by downregulating VEGF and disturbing signaling involving VEGFR2 [219]. Polyphyllin D and Polyphyllin VII are associated with cell cycle arrest and apoptosis procedures [220,221]. Research conducted on mice has proven that total steroidal saponins can activate the receptors of adenosine, and some saponins (such as 8-cyclopentyl1, 3-(N)-xanthine, 3-dipropyl-2 and N6-cyclohexyladenosine) are capable of blocking the A1/A3 adenosine receptor [156].
We notice the complexity in transforming basic trials of purinergic activities into practical applications. However, it is worth exploring to achieve a deeper understanding.
4.8. Neuropeptide
4.8.1. Neuropeptide Y (NPY): Stimulates Tumor Growth and Progression
NPY, secreted by hippocampal interneurons, is a type of abundant neurotransmitter in CNS [222,223]. It has been confirmed that NPY has multiple effects related to cancer biology, such as stimulating tumor-associated angiogenesis, cell proliferation, migration and chemoresistance, as well as regulating the differentiation of stem cells [68]. NPY may have special effects on GBM. An elegant study shows that NPY could not be seen in many brain tumors but could be found in nerve fibers of most kinds of glioma. Furthermore, the expression of Y2 receptors on GBM cells is upregulated and distributed extensively [69]. More research in vitro and in vivo is needed to confirm the regulation of NPY on GBM. In addition, leptin is well-known to inhibit NPY neurons in the arcuate nucleus of the hypothalamus [224]. However, since the exact molecular mechanism remains unclear, there is still a long way to go before leptin could be put forth into clinical development.
Recent studies have tried to utilize NPY in cancer imaging and therapy, focusing on breast cancer first [222]. hY1R-preferring agonists, especially [F7, P34]-NPY, have shown great potency in imaging tumor sites in patients with breast cancer, thanks to the high frequency and density of Y1 receptors on breast tumor cells, as well as the discrepancy of the receptor subtypes between breast carcinomas (Y1 receptors) and non-neoplastic breast (Y2 receptors) [225,226]. Another novel advancement is peptide-drug conjugates (PDC), which serve as a new carrier promising to deliver antitumor drugs to tumors selectively without damaging healthy tissues. Consistently, this kind of conjugate is dependent on the specific expression of cell surface receptors as well [227]. In GBM, the high frequency and density of Y2 receptors may also create a condition in favor of selective GBM targeting [69,227]. Nevertheless, the high expression of Y2 receptors is compared with other human tumors, and there is insufficient evidence to support the difference in NPY receptor subtypes between GBM and normal brain tissues. Further investigation is required.
4.8.2. Substance P (SP): Induces GBM Proliferation, Invasiveness and Migration
SP, which is a neuropeptide released by neuronal and non-neuronal cells, belongs to the family of tachykinins [228]. The overexpression of NK-1Rs can be found both on the tumor cell membranes and in the neovasculature of the GBM microenvironment, and results in a worse survival time and prognosis for GBM patients [71,72]. Activating NK-1Rs leads to the phosphorylation of AKT and ERK1/2, the activation of c-myc and activator protein-1 (AP-1) and the promotion of DNA synthesis [100,229]. As a result, this type of receptor emerges as having critical participation in the proliferation, invasion and migration of GBM, via inducing anti-apoptotic effects, favoring angiogenesis and triggering inflammation correlated with tumor progression [73,74,75]. NK-1Rs have also been confirmed to have a direct impact on the migration of GBM via upregulating MMP-2 and MT1-MMP [76]. In addition, the pathological transformation of the original signal transduction pathway in astrocytes may correlate with the upregulation of NK-1R [230].
Of note, the effects of NK-1R antagonists on cell growth and apoptosis have been identified and summarized recently [73]. In addition, an innovative co-treatment with NK1R antagonists and CaMKII inhibitors has shown synergistic inhibition on the growth of GSCs and their derivatives both in vitro and in vivo [231]. Further experiments on animal models in the future will make efforts to translate this combination therapy to the clinic.
Therapeutics that deliver radiation at toxic levels to the site of the disease by a radiolabeled molecule are known as targeted radionuclide therapy. Due to the high and specific expression of NK-1Rs on GBM cells, injecting SP analogues labeled with β−-/α- emitting isotopes locally represents a novel therapy for GBM, especially in tumor recurrence [71,232]. It is proved that α particles (225Ac, 213Bi, 211At) are more effective and specific than β− particles (131I, 90Y, 177Lu) [71]. The experiment in GBM cell lines and the GSC line has demonstrated the inhibition of 225Ac-1,4,7,10-Tetraazacyclododecane-1-Glutaric Acid-4,7,10-Triacetic Acid (DOTAGA/DOTA) -SP on the viability, proliferation and apoptosis of tumor cells [233]. In addition, several clinical studies have indicated that targeted radiopeptide therapy is safe and well-tolerated, concerning 90Y-DOTA-SP [71,234], 213Bi-DOTA-SP [71,235,236,237], 225Ac-DOTA-SP [232] and 211At-DOTA-SP [238]. Taken together, it is expected that SP analogues and NK-1R antagonists could be feasible for controlling GBM in the future.
4.9. NO: Involved in GBM Proliferation and Migration and Cell Apoptosis
NO is produced by three subtypes of nitric oxide synthase (NOS), including neuronal NOS (nNOS), inducible NOS (iNOS) and endothelial NOS (eNOS) [239]. An immunohistochemistry check for NOS expression reveals that, in contrast to healthy human brains, NOSs are overexpressed in gliomas and vary in different types and levels of this kind of tumor. In total, systematic analysis shows the upregulation of NOSs in glioma cells and the peritumor microenvironment, suggesting that NO production is complex and contains various sources [81].
Scholars have held different opinions on the role of NO in cancer biology, namely whether it functions as a tumor promoter or inhibitor [84]. This discussion could be attributed to different research backgrounds, such as the tumorigenesis stage, NO expression level, the NOS subtype and its location and various kinds of neoplastic cells and their differentiation status [81]. Among all these variables, the concentration may matter most. Some suggest that a moderate concentration (100–350 μmol/L) reduces cell proliferation and genomic instability, while some of the literature shows that a high concentration (500–1000 μmol/L) causes cell reproduction decline, apoptosis upregulation, irreversible DNA impairment and Ataxia telangiectasia mutated/Ataxia telangiectasia and Rad3-related protein (ATM/ATR)-dependent p53 phosphorylation induced by downstream signaling pathways [78,79,80,81,82,83].
EGFRvIII/STAT3 pathway is critical signaling downstream in glioblastoma and gets involved in GBM cell proliferation, migration and progression. In addition, STAT3 activates iNOS via binding to the promoter of iNOS genes. Therefore, inhibiting iNOS pharmacologically and genetically can suppress invasiveness and reproduction of GBM cells. 1400W and S-MIU are selective iNOS inhibitors [72,73,74,75] that reduce cell proliferation of astrocytes and U87 cell lines with EGFRvIII expression [84].
As mentioned before, NF-KB is involved in malignance formation through regulating downstream pathways. There is research conducted in C6 glioma cells indicating that NF-kB modulation is significant to Nos2 regulation. NF-KB activation is associated with a nondegradable form of IjBa, which interferes with NF-KB signaling and LPS, as well as the expression of cytokine-stimulated iNOS [240].
Reviewing back, the key point in understanding the role of NO has been summarized down to the NO concentration, the redox environment and the exposure time [239]. Considerably, more work will need to be done to identify the effect of NO.
5. Conclusions and Future Directions
As shown above, the influence of neurotransmitters on GBM is complicated: different transmitters activate different pathways, and even the same transmitter can cause the opposite effect due to the diversity of receptor subtypes and environments. For example, as mentioned before, the role of NO in tumor biology can be pro- or anti-tumor activities, which may be caused by multiple factors, including the level of NO/NOS in the peritumor microenvironment, the NOS type, the tumor stage and the degree of the differentiation of the tumor, as well as the tumor subtypes that express NOS preferentially [81]. Therefore, while testing new drugs, it is of great significance to design tailored clinical trials according to the characteristics of each neurotransmitter [5].
In addition to assisting in synaptic transmission, neurotransmitters act on a wide variety of cells in the GBM microenvironment, including neurons, tumor cells, glial cells and vascular endothelial cells, thus, mediating a broad regulatory effect on the survival, progression, recurrence and chemo-/radio-resistance of GBM. Hence, it can be expected that targeting neurotransmitters could be a promising novel pharmacological approach for GBM treatment. For one thing, taking into account drugs associated with neurotransmitters provides us with an abundant drug box. For another, the capability of GBM cells to alter the expression levels of neurotransmitter receptors allows them to be distinguished from non-tumor cells in the microenvironment and specifically targeted by drugs, thus, reducing side effects [227].
Specifically, therapeutic options associated with neurotransmitters may include: (i) activating/silencing numerous neurotransmitters receptors or regulating the number of receptors via gene expression. Notably, in pursuit of high efficiency and low toxicity, receptors that are differently expressed in tumor cells are considered to be more suitable as molecular targets, such as α9nAChRs, NK-1Rs and Y2Rs; (ii) providing a novel molecular marker when evaluating therapeutic strategies and the prognosis of patients, such as α9nAChRs that are up-regulated in GBM and predict a negative prognosis [241]. In addition, Yuri Belotti et al. have identified a subset of ten neurotransmitter receptors genes (DRD1, HTR1E, HTR3B, GABRA1, GABRA4, GABRB2, GABRG2, GRIN1, GRM7 and ADRA1B) that correlates with the unfavorable prognosis of GBM [242]; (iii) regulating the metabolism of neurotransmitters (synthesis, storage, release and inactivation), such as Amb4269951, SSZ, Escitalopram oxalate, 1400W and S-MIU; (iv) utilizing neurotransmitters or their receptor as drug carriers, such as nAChR-mediated transcytosis and PDC; (v) applying with other types of drugs (such as TMZ) to amplify efficacy or reduce chemoresistance. In order to increase the accuracy of targeted therapies and lower side effects, more analysis of differential gene expression between GBM and normal cells is needed.
Although the drugs mentioned in our research are mainly applied in vitro, there are several drugs in our studies that have progressed to phase I/II clinical trials, which include memantine [159], talampanel [160,161,162], ONC201 [164,165], chlorpromazine [166] and escitalopram oxalate [167]. Furthermore, experiments in mouse models also show good results [41,127,149,150,157,158]. Hence, we hold an optimistic perception that, with further research, drugs targeting neurotransmitters may be applied in GBM treatment. In order to reduce the duration and cost of drug development, we suggest that future work could give priority to the repurposing of FDA-approved drugs [208,243]. In general, those compounds consist of small molecule inhibitors and chemically modified derivatives of drugs, with high bioactivation in vivo and concerning blood-brain barrier (BBB) penetrability [244], such as psychotropic, antiepileptic, antidepressive and antihypertensive drugs [159].
Furthermore, different molecular subtypes of GBM may be sensitive to different neurotransmitters since they contain different mutations. For example, the activation of M2 receptors is likely involved in the mediation of Notch-1/EGFR pathways in p53 wild-type GB7 cells, which could not be seen in p53-deficient GB8 cells. Instead, M2 receptors on p53-deficient GB8 cells may induce a cytotoxicity effect mediated by oxidative stress and apoptosis [13,134]. As such, the effect of targeting M2 receptors for treatment correlates with the genotype of patients and the molecular subtypes of GBM [13]. To achieve favorable efficacy, it is vital to detect the genotype of the patients and the molecular subtypes of GBM when considering drug options. Future studies should explore targeted drugs combined with genomics and proteomics analysis, in order to accomplish precision medicine and improve the prognosis of GBM patients [245].
Author Contributions
Q.H. (Qiqi Huang) and L.C. wrote the paper, made the tables and designed the figures; J.L. designed and made the figures; Q.H. (Qiongzhen Huang) carefully read and provided helpful discussions and insightful comments; H.S. supervised the review and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This research was funded by the Guangdong Basic and Applied Basic Research Foundation (2020A1515010038), the Presidential Foundation of Zhujiang Hospital of Southern Medical University (No. yzjj2018rc03) and National Undergraduate Training Program for Innovation and Entrepreneurship (202112121004).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Janjua T.I., Rewatkar P., Ahmed-Cox A., Saeed I., Mansfeld F.M., Kulshreshtha R., Kumeria T., Ziegler D.S., Kavallaris M., Mazzieri R., et al. Frontiers in the treatment of glioblastoma: Past, present and emerging. Adv. Drug Deliv. Rev. 2021;171:108–138. doi: 10.1016/j.addr.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Hottinger A.F., Stupp R., Homicsko K. Standards of care and novel approaches in the management of glioblastoma multiforme. Chin. J. Cancer. 2014;33:32–39. doi: 10.5732/cjc.013.10207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wardak Z., Choe K.S. Molecular pathways and potential therapeutic targets in glioblastoma multiforme. Expert Rev. Antican. 2013;13:1307–1318. doi: 10.1586/14737140.2013.852472. [DOI] [PubMed] [Google Scholar]
- 4.Linz U. Commentary on Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial (Lancet Oncol. 2009;10:459–466) Cancer. 2010;116:1844–1846. doi: 10.1002/cncr.24950. [DOI] [PubMed] [Google Scholar]
- 5.Tan A.C., Ashley D.M., López G.Y., Malinzak M., Friedman H.S., Khasraw M. Management of glioblastoma: State of the art and future directions. CA Cancer J. Clin. 2020;70:299–312. doi: 10.3322/caac.21613. [DOI] [PubMed] [Google Scholar]
- 6.Radin D.P., Tsirka S.E. Interactions between Tumor Cells, Neurons, and Microglia in the Glioma Microenvironment. Int. J. Mol. Sci. 2020;21:8476. doi: 10.3390/ijms21228476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quail D.F., Joyce J.A. The Microenvironmental Landscape of Brain Tumors. Cancer Cell. 2017;31:326–341. doi: 10.1016/j.ccell.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johung T., Monje M. Neuronal activity in the glioma microenvironment. Curr. Opin. Neurobiol. 2017;47:156–161. doi: 10.1016/j.conb.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arneth B. Tumor Microenvironment. Medicina. 2019;56:15. doi: 10.3390/medicina56010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Monje M., Borniger J.C., D’Silva N.J., Deneen B., Dirks P.B., Fattahi F., Frenette P.S., Garzia L., Gutmann D.H., Hanahan D., et al. Roadmap for the Emerging Field of Cancer Neuroscience. Cell. 2020;181:219–222. doi: 10.1016/j.cell.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang S.H., Hu L.P., Wang X., Li J., Zhang Z.G. Neurotransmitters: Emerging targets in cancer. Oncogene. 2020;39:503–515. doi: 10.1038/s41388-019-1006-0. [DOI] [PubMed] [Google Scholar]
- 12.Jung E., Alfonso J., Osswald M., Monyer H., Wick W., Winkler F. Emerging intersections between neuroscience and glioma biology. Nat. Neurosci. 2019;22:1951–1960. doi: 10.1038/s41593-019-0540-y. [DOI] [PubMed] [Google Scholar]
- 13.Cristofaro I., Alessandrini F., Spinello Z., Guerriero C., Fiore M., Caffarelli E., Laneve P., Dini L., Conti L., Tata A.M. Cross Interaction between M2 Muscarinic Receptor and Notch1/EGFR Pathway in Human Glioblastoma Cancer Stem Cells: Effects on Cell Cycle Progression and Survival. Cells. 2020;9:657. doi: 10.3390/cells9030657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hyman S.E. Neurotransmitters. Curr. Biol. 2005;15:R154–R158. doi: 10.1016/j.cub.2005.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Berg D.A., Belnoue L., Song H., Simon A. Neurotransmitter-mediated control of neurogenesis in the adult vertebrate brain. Development. 2013;140:2548–2561. doi: 10.1242/dev.088005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan X., Hasan M.N., Maniar S., Jia W., Sun D. Reactive Astrocytes in Glioblastoma Multiforme. Mol. Neurobiol. 2018;55:6927–6938. doi: 10.1007/s12035-018-0880-8. [DOI] [PubMed] [Google Scholar]
- 17.Wegrzyn D., Freund N., Faissner A., Juckel G. Poly I:C Activated Microglia Disrupt Perineuronal Nets and Modulate Synaptic Balance in Primary Hippocampal Neurons in vitro. Front. Synaptic Neurosci. 2021;13:637549. doi: 10.3389/fnsyn.2021.637549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geribaldi-Doldan N., Hervas-Corpion I., Gomez-Oliva R., Dominguez-Garcia S., Ruiz F.A., Iglesias-Lozano I., Carrascal L., Pardillo-Diaz R., Gil-Salu J.L., Nunez-Abades P., et al. Targeting Protein Kinase C in Glioblastoma Treatment. Biomedicines. 2021;9:381. doi: 10.3390/biomedicines9040381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zarco N., Norton E., Quinones-Hinojosa A., Guerrero-Cazares H. Overlapping migratory mechanisms between neural progenitor cells and brain tumor stem cells. Cell Mol. Life Sci. 2019;76:3553–3570. doi: 10.1007/s00018-019-03149-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Liberto V., Borroto-Escuela D.O., Frinchi M., Verdi V., Fuxe K., Belluardo N., Mudò G. Existence of muscarinic acetylcholine receptor (mAChR) and fibroblast growth factor receptor (FGFR) heteroreceptor complexes and their enhancement of neurite outgrowth in neural hippocampal cultures. Biochim. Biophys. Acta Gen. Subj. 2017;1861:235–245. doi: 10.1016/j.bbagen.2016.10.026. [DOI] [PubMed] [Google Scholar]
- 21.Ramos Costa A.P., Levone B.R., Gururajan A., Moloney G., Hoeller A.A., Lino-de-Oliveira C., Dinan T.G., O’Leary O.F., Monteiro de Lima T.C., Cryan J.F. Enduring effects of muscarinic receptor activation on adult hippocampal neurogenesis, microRNA expression and behaviour. Behav. Brain Res. 2019;362:188–198. doi: 10.1016/j.bbr.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 22.Takahashi T. Multiple Roles for Cholinergic Signaling from the Perspective of Stem Cell Function. Int. J. Mol. Sci. 2021;22:666. doi: 10.3390/ijms22020666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jansson L.C., Åkerman K.E. The role of glutamate and its receptors in the proliferation, migration, differentiation and survival of neural progenitor cells. J. Neural Transm. 2014;121:819–836. doi: 10.1007/s00702-014-1174-6. [DOI] [PubMed] [Google Scholar]
- 24.Malva J.O., Xapelli S., Baptista S., Valero J., Agasse F., Ferreira R., Silva A.P. Multifaces of neuropeptide Y in the brain--neuroprotection, neurogenesis and neuroinflammation. Neuropeptides. 2012;46:299–308. doi: 10.1016/j.npep.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 25.Liu X., Wang Q., Haydar T.F., Bordey A. Nonsynaptic GABA signaling in postnatal subventricular zone controls proliferation of GFAP-expressing progenitors. Nat. Neurosci. 2005;8:1179–1187. doi: 10.1038/nn1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burnstock G. Purinergic signalling and disorders of the central nervous system. Nat. Rev. Drug Discov. 2008;7:575–590. doi: 10.1038/nrd2605. [DOI] [PubMed] [Google Scholar]
- 27.Thompson E.G., Sontheimer H. Acetylcholine Receptor Activation as a Modulator of Glioblastoma Invasion. Cells. 2019;8:1203. doi: 10.3390/cells8101203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferretti M., Fabbiano C., Di Bari M., Ponti D., Calogero A., Tata A.M. M2 muscarinic receptors inhibit cell proliferation in human glioblastoma cell lines. Life Sci. 2012;91:1134–1137. doi: 10.1016/j.lfs.2012.04.033. [DOI] [PubMed] [Google Scholar]
- 29.Ferretti M., Fabbiano C., Di Bari M., Conte C., Castigli E., Sciaccaluga M., Ponti D., Ruggieri P., Raco A., Ricordy R., et al. M2 receptor activation inhibits cell cycle progression and survival in human glioblastoma cells. J. Cell. Mol. Med. 2013;17:552–566. doi: 10.1111/jcmm.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alessandrini F., Cristofaro I., Di Bari M., Zasso J., Conti L., Tata A.M. The activation of M2 muscarinic receptor inhibits cell growth and survival in human glioblastoma cancer stem cells. Int. Immunopharmacol. 2015;29:105–109. doi: 10.1016/j.intimp.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 31.Cristofaro I., Spinello Z., Matera C., Fiore M., Conti L., De Amici M., Dallanoce C., Tata A.M. Activation of M2 muscarinic acetylcholine receptors by a hybrid agonist enhances cytotoxic effects in GB7 glioblastoma cancer stem cells. Neurochem. Int. 2018;118:52–60. doi: 10.1016/j.neuint.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 32.Spina R., Voss D.M., Asnaghi L., Sloan A., Bar E.E. Atracurium Besylate and other neuromuscular blocking agents promote astroglial differentiation and deplete glioblastoma stem cells. Oncotarget. 2016;7:459–472. doi: 10.18632/oncotarget.6314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khalil A.A., Jameson M.J., Broaddus W.C., Lin P.S., Chung T.D. Nicotine enhances proliferation, migration, and radioresistance of human malignant glioma cells through EGFR activation. Brain Tumor Pathol. 2013;30:73–83. doi: 10.1007/s10014-012-0101-5. [DOI] [PubMed] [Google Scholar]
- 34.Pucci S., Fasoli F., Moretti M., Benfante R., Di Lascio S., Viani P., Daga A., Gordon T.J., McIntosh M., Zoli M., et al. Choline and nicotine increase glioblastoma cell proliferation by binding and activating alpha 7-and alpha 9-containing nicotinic receptors. Pharmacol. Res. 2021;163:12. doi: 10.1016/j.phrs.2020.105336. [DOI] [PubMed] [Google Scholar]
- 35.Kolodziej M.A., Gott H., Kopischke B., Bender M.K.F., Weigand M.A., Di Fazio P., Schwarm F.P., Uhle F. Antiproliferative effect of GTS-21 in glioblastoma cells. Oncol. Lett. 2021;22:759. doi: 10.3892/ol.2021.13020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piovesana R., Salazar Intriago M.S., Dini L., Tata A.M. Cholinergic Modulation of Neuroinflammation: Focus on α7 Nicotinic Receptor. Int. J. Mol. Sci. 2021;22:4912. doi: 10.3390/ijms22094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hardingham G.E., Bading H. Synaptic versus extrasynaptic NMDA receptor signalling: Implications for neurodegenerative disorders. Nat. Rev. Neurosci. 2010;11:682–696. doi: 10.1038/nrn2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prickett T.D., Samuels Y. Molecular pathways: Dysregulated glutamatergic signaling pathways in cancer. Clin. Cancer Res. 2012;18:4240–4246. doi: 10.1158/1078-0432.CCR-11-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yohay K., Tyler B., Weaver K.D., Pardo A.C., Gincel D., Blakeley J., Brem H., Rothstein J.D. Efficacy of local polymer-based and systemic delivery of the anti-glutamatergic agents riluzole and memantine in rat glioma models. J. Neurosurg. 2014;120:854–863. doi: 10.3171/2013.12.JNS13641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Müller-Längle A., Lutz H., Hehlgans S., Rödel F., Rau K., Laube B. NMDA Receptor-Mediated Signaling Pathways Enhance Radiation Resistance, Survival and Migration in Glioblastoma Cells-A Potential Target for Adjuvant Radiotherapy. Cancers. 2019;11:503. doi: 10.3390/cancers11040503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu K.H., Yang S.T., Lin Y.K., Lin J.W., Lee Y.H., Wang J.Y., Hu C.J., Lin E.Y., Chen S.M., Then C.K., et al. Fluoxetine, an antidepressant, suppresses glioblastoma by evoking AMPAR-mediated calcium-dependent apoptosis. Oncotarget. 2015;6:5088–5101. doi: 10.18632/oncotarget.3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.D’Alessandro G., Lauro C., Quaglio D., Ghirga F., Botta B., Trettel F., Limatola C. Neuro-Signals from Gut Microbiota: Perspectives for Brain Glioma. Cancers. 2021;13:2810. doi: 10.3390/cancers13112810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Venkataramani V., Tanev D.I., Strahle C., Studier-Fischer A., Fankhauser L., Kessler T., Korber C., Kardorff M., Ratliff M., Xie R., et al. Glutamatergic synaptic input to glioma cells drives brain tumour progression. Nature. 2019;573:532–538. doi: 10.1038/s41586-019-1564-x. [DOI] [PubMed] [Google Scholar]
- 44.Venkatesh H.S., Morishita W., Geraghty A.C., Silverbush D., Gillespie S.M., Arzt M., Tam L.T., Espenel C., Ponnuswami A., Ni L., et al. Electrical and synaptic integration of glioma into neural circuits. Nature. 2019;573:539–545. doi: 10.1038/s41586-019-1563-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mollazadeh H., Mohtashami E., Mousavi S.H., Soukhtanloo M., Vahedi M.M., Hosseini A., Afshari A.R., Sahebkar A. Deciphering the Role of Glutamate Signaling in Glioblastoma Multiforme: Current Therapeutic Modalities and Future Directions. Curr. Pharm. Des. 2020;26:4777–4788. doi: 10.2174/1381612826666200603132456. [DOI] [PubMed] [Google Scholar]
- 46.Zhang Z.C., Zheng X.Y., Luan Y., Liu Y.F., Li X.X., Liu C.X., Lu H.X., Chen X.L., Liu Y. Activity of Metabotropic Glutamate Receptor 4 Suppresses Proliferation and Promotes Apoptosis With Inhibition of Gli-1 in Human Glioblastoma Cells. Front. Neurosci. 2018;12:16. doi: 10.3389/fnins.2018.00320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramaswamy P., Aditi Devi N., Hurmath Fathima K., Dalavaikodihalli Nanjaiah N. Activation of NMDA receptor of glutamate influences MMP-2 activity and proliferation of glioma cells. Neurol. Sci. 2014;35:823–829. doi: 10.1007/s10072-013-1604-5. [DOI] [PubMed] [Google Scholar]
- 48.Piao Y., Lu L., de Groot J. AMPA receptors promote perivascular glioma invasion via beta1 integrin-dependent adhesion to the extracellular matrix. Neuro Oncol. 2009;11:260–273. doi: 10.1215/15228517-2008-094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Corsi L., Mescola A., Alessandrini A. Glutamate Receptors and Glioblastoma Multiforme: An Old ‘‘Route’’ for New Perspectives. Int. J. Mol. Sci. 2019;20:1796. doi: 10.3390/ijms20071796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nguyen H.D., Allaire A., Diamandis P., Bisaillon M., Scott M.S., Richer M. A machine learning analysis of a “normal-like” IDH-WT diffuse glioma transcriptomic subgroup associated with prolonged survival reveals novel immune and neurotransmitter-related actionable targets. BMC Med. 2020;18:280. doi: 10.1186/s12916-020-01748-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Catavero C., Bao H., Song J. Neural mechanisms underlying GABAergic regulation of adult hippocampal neurogenesis. Cell Tissue Res. 2018;371:33–46. doi: 10.1007/s00441-017-2668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smits A., Jin Z., Elsir T., Pedder H., Nistér M., Alafuzoff I., Dimberg A., Edqvist P.H., Pontén F., Aronica E., et al. GABA-A channel subunit expression in human glioma correlates with tumor histology and clinical outcome. PLoS ONE. 2012;7:e37041. doi: 10.1371/journal.pone.0037041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Babateen O., Jin Z., Bhandage A., Korol S.V., Westermark B., Forsberg Nilsson K., Uhrbom L., Smits A., Birnir B. Etomidate, propofol and diazepam potentiate GABA-evoked GABAA currents in a cell line derived from human glioblastoma. Eur. J. Pharmacol. 2015;748:101–107. doi: 10.1016/j.ejphar.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 54.D’Urso P.I., D’Urso O.F., Storelli C., Mallardo M., Gianfreda C.D., Montinaro A., Cimmino A., Pietro C., Marsigliante S. miR-155 is up-regulated in primary and secondary glioblastoma and promotes tumour growth by inhibiting GABA receptors. Int. J. Oncol. 2012;41:228–234. doi: 10.3892/ijo.2012.1420. [DOI] [PubMed] [Google Scholar]
- 55.Herbin M., Simonis C., Revéret L., Hackert R., Libourel P.A., Eugène D., Diaz J., de Waele C., Vidal P.P. Dopamine Modulates Motor Control in a Specific Plane Related to Support. PLoS ONE. 2016;11:e0155058. doi: 10.1371/journal.pone.0155058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yoest K.E., Cummings J.A., Becker J.B. Estradiol, dopamine and motivation. Cent. Nerv. Syst. Agents Med. Chem. 2014;14:83–89. doi: 10.2174/1871524914666141226103135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lan Y.L., Wang X., Xing J.S., Lou J.C., Ma X.C., Zhang B. The potential roles of dopamine in malignant glioma. Acta Neurol. Belg. 2017;117:613–621. doi: 10.1007/s13760-016-0730-2. [DOI] [PubMed] [Google Scholar]
- 58.Moreno-Smith M., Lu C., Shahzad M.M.K., Pena G.N.A., Allen J.K., Stone R.L., Mangala L.S., Han H.D., Kim H.S., Farley D., et al. Dopamine blocks stress-mediated ovarian carcinoma growth. Clin. Cancer Res. 2011;17:3649–3659. doi: 10.1158/1078-0432.CCR-10-2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lauder J.M., Wallace J.A., Wilkie M.B., DiNome A., Krebs H. Roles for serotonin in neurogenesis. Monogr. Neural Sci. 1983;9:3–10. doi: 10.1159/000406871. [DOI] [PubMed] [Google Scholar]
- 60.Lu Q., Ding Y., Li Y., Lu Q. 5-HT receptor agonist Valerenic Acid enhances the innate immunity signal and suppresses glioblastoma cell growth and invasion. Int. J. Biol. Sci. 2020;16:2104–2115. doi: 10.7150/ijbs.44906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weselek G., Keiner S., Fauser M., Wagenführ L., Müller J., Kaltschmidt B., Brandt M.D., Gerlach M., Redecker C., Hermann A., et al. Norepinephrine is a negative regulator of the adult periventricular neural stem cell niche. Stem Cells. 2020;38:1188–1201. doi: 10.1002/stem.3232. [DOI] [PubMed] [Google Scholar]
- 62.Zhong J., Shan W., Zuo Z. Norepinephrine inhibits migration and invasion of human glioblastoma cell cultures possibly via MMP-11 inhibition. Brain Res. 2021;1756:147280. doi: 10.1016/j.brainres.2021.147280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Braadland P.R., Ramberg H., Grytli H.H., Tasken K.A. beta-Adrenergic Receptor Signaling in Prostate Cancer. Front. Oncol. 2014;4:375. doi: 10.3389/fonc.2014.00375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cole S.W., Sood A.K. Molecular pathways: Beta-adrenergic signaling in cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2012;18:1201–1206. doi: 10.1158/1078-0432.CCR-11-0641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Di Virgilio F., Sarti A.C., Falzoni S., De Marchi E., Adinolfi E. Extracellular ATP and P2 purinergic signalling in the tumour microenvironment. Nat. Rev. Cancer. 2018;18:601–618. doi: 10.1038/s41568-018-0037-0. [DOI] [PubMed] [Google Scholar]
- 66.Debom G.N., Rubenich D.S., Braganhol E. Adenosinergic Signaling as a Key Modulator of the Glioma Microenvironment and Reactive Astrocytes. Front. Neurosci. 2021;15:648476. doi: 10.3389/fnins.2021.648476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Silva A.P., Pinheiro P.S., Carvalho A.P., Carvalho C.M., Jakobsen B., Zimmer J., Malva J.O. Activation of neuropeptide Y receptors is neuroprotective against excitotoxicity in organotypic hippocampal slice cultures. FASEB J. 2003;17:1118–1120. doi: 10.1096/fj.02-0885fje. [DOI] [PubMed] [Google Scholar]
- 68.Abualsaud N., Caprio L., Galli S., Krawczyk E., Alamri L., Zhu S., Gallicano G.I., Kitlinska J. Neuropeptide Y/Y5 Receptor Pathway Stimulates Neuroblastoma Cell Motility Through RhoA Activation. Front. Cell Dev. Biol. 2020;8:627090. doi: 10.3389/fcell.2020.627090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Körner M., Reubi J.C. Neuropeptide Y receptors in primary human brain tumors: Overexpression in high-grade tumors. J. Neuropathol. Exp. Neurol. 2008;67:741–749. doi: 10.1097/NEN.0b013e318180e618. [DOI] [PubMed] [Google Scholar]
- 70.Yang L., Li G., Ye J., Lu D., Chen Z., Xiang A.P., Jiang M.H. Substance P enhances endogenous neurogenesis to improve functional recovery after spinal cord injury. Int. J. Biochem. Cell Biol. 2017;89:110–119. doi: 10.1016/j.biocel.2017.05.030. [DOI] [PubMed] [Google Scholar]
- 71.Kneifel S., Cordier D., Good S., Ionescu M.C., Ghaffari A., Hofer S., Kretzschmar M., Tolnay M., Apostolidis C., Waser B., et al. Local targeting of malignant gliomas by the diffusible peptidic vector 1,4,7,10-tetraazacyclododecane-1-glutaric acid-4,7,10-triacetic acid-substance p. Clin. Cancer Res. 2006;12:3843–3850. doi: 10.1158/1078-0432.CCR-05-2820. [DOI] [PubMed] [Google Scholar]
- 72.Hennig I.M., Laissue J.A., Horisberger U., Reubi J.C. Substance-P receptors in human primary neoplasms: Tumoral and vascular localization. Int. J. Cancer. 1995;61:786–792. doi: 10.1002/ijc.2910610608. [DOI] [PubMed] [Google Scholar]
- 73.Afshari A.R., Motamed-Sanaye A., Sabri H., Soltani A., Karkon-Shayan S., Radvar S., Javid H., Mollazadeh H., Sathyapalan T., Sahebkar A. Neurokinin-1 receptor (NK-1R) antagonists: Potential targets in the treatment of glioblastoma multiforme. Curr. Med. Chem. 2021;28:4877–4892. doi: 10.2174/0929867328666210113165805. [DOI] [PubMed] [Google Scholar]
- 74.Zhang Y.X., Li X.F., Yuan G.Q., Hu H., Song X.Y., Li J.Y., Miao X.K., Zhou T.X., Yang W.L., Zhang X.W., et al. β-Arrestin 1 has an essential role in neurokinin-1 receptor-mediated glioblastoma cell proliferation and G(2)/M phase transition. J. Biol. Chem. 2017;292:8933–8947. doi: 10.1074/jbc.M116.770420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Munoz M.F., Arguelles S., Rosso M., Medina R., Covenas R., Ayala A., Munoz M. The Neurokinin-1 Receptor Is Essential for the Viability of Human Glioma Cells: A Possible Target for Treating Glioblastoma. Biomed. Res. Int. 2022;2022:6291504. doi: 10.1155/2022/6291504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mou L., Kang Y., Zhou Y., Zeng Q., Song H., Wang R. Neurokinin-1 receptor directly mediates glioma cell migration by up-regulation of matrix metalloproteinase-2 (MMP-2) and membrane type 1-matrix metalloproteinase (MT1-MMP) J. Biol. Chem. 2013;288:306–318. doi: 10.1074/jbc.M112.389783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Contestabile A. Regulation of transcription factors by nitric oxide in neurons and in neural-derived tumor cells. Prog. Neurobiol. 2008;84:317–328. doi: 10.1016/j.pneurobio.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 78.Vannini F., Kashfi K., Nath N. The dual role of iNOS in cancer. Redox Biol. 2015;6:334–343. doi: 10.1016/j.redox.2015.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cahill K.E., Morshed R.A., Yamini B. Nuclear factor-κB in glioblastoma: Insights into regulators and targeted therapy. Neuro Oncol. 2016;18:329–339. doi: 10.1093/neuonc/nov265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yakovlev V.A. Role of nitric oxide in the radiation-induced bystander effect. Redox Biol. 2015;6:396–400. doi: 10.1016/j.redox.2015.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tran A.N., Boyd N.H., Walker K., Hjelmeland A.B. NOS Expression and NO Function in Glioma and Implications for Patient Therapies. Antioxid. Redox Signal. 2017;26:986–999. doi: 10.1089/ars.2016.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Badn W., Siesjö P. The dual role of nitric oxide in glioma. Curr. Pharm. Des. 2010;16:428–430. doi: 10.2174/138161210790232158. [DOI] [PubMed] [Google Scholar]
- 83.Shinoda J., Whittle I.R. Nitric oxide and glioma: A target for novel therapy? Br. J. Neurosurg. 2001;15:213–220. doi: 10.1080/02688690120057628. [DOI] [PubMed] [Google Scholar]
- 84.Jahani-Asl A., Bonni A. iNOS: A potential therapeutic target for malignant glioma. Curr. Mol. Med. 2013;13:1241–1249. doi: 10.2174/1566524011313080002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cuddapah V.A., Robel S., Watkins S., Sontheimer H. A neurocentric perspective on glioma invasion. Nat. Rev. Neurosci. 2014;15:455–465. doi: 10.1038/nrn3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Louis D.N., Perry A., Wesseling P., Brat D.J., Cree I.A., Figarella-Branger D., Hawkins C., Ng H.K., Pfister S.M., Reifenberger G., et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A summary. Neuro Oncol. 2021;23:1231–1251. doi: 10.1093/neuonc/noab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lee J.H., Lee J.E., Kahng J.Y., Kim S.H., Park J.S., Yoon S.J., Um J.Y., Kim W.K., Lee J.K., Park J., et al. Human glioblastoma arises from subventricular zone cells with low-level driver mutations. Nature. 2018;560:243–247. doi: 10.1038/s41586-018-0389-3. [DOI] [PubMed] [Google Scholar]
- 88.Yao M., Li S., Wu X., Diao S., Zhang G., He H., Bian L., Lu Y. Cellular origin of glioblastoma and its implication in precision therapy. Cell. Mol. Immunol. 2018;15:737–739. doi: 10.1038/cmi.2017.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Crivii C.B., Bosca A.B., Melincovici C.S., Constantin A.M., Marginean M., Dronca E., Sufletel R., Gonciar D., Bungardean M., Sovrea A. Glioblastoma Microenvironment and Cellular Interactions. Cancers. 2022;14:1092. doi: 10.3390/cancers14041092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Schonberg D.L., Lubelski D., Miller T.E., Rich J.N. Brain tumor stem cells: Molecular characteristics and their impact on therapy. Mol. Asp. Med. 2014;39:82–101. doi: 10.1016/j.mam.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bao S., Wu Q., McLendon R.E., Hao Y., Shi Q., Hjelmeland A.B., Dewhirst M.W., Bigner D.D., Rich J.N. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444:756–760. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 92.Chen J., Li Y., Yu T.S., McKay R.M., Burns D.K., Kernie S.G., Parada L.F. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature. 2012;488:522–526. doi: 10.1038/nature11287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yabo Y.A., Niclou S.P., Golebiewska A. Cancer cell heterogeneity and plasticity: A paradigm shift in glioblastoma. Neuro Oncol. 2021;24:669–682. doi: 10.1093/neuonc/noab269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sachdeva R., Wu M., Johnson K., Kim H., Celebre A., Shahzad U., Graham M.S., Kessler J.A., Chuang J.H., Karamchandani J., et al. BMP signaling mediates glioma stem cell quiescence and confers treatment resistance in glioblastoma. Sci. Rep. 2019;9:14569. doi: 10.1038/s41598-019-51270-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zheng Y., Liu L., Wang Y., Xiao S., Mai R., Zhu Z., Cao Y. Glioblastoma stem cell (GSC)-derived PD-L1-containing exosomes activates AMPK/ULK1 pathway mediated autophagy to increase temozolomide-resistance in glioblastoma. Cell Biosci. 2021;11:63. doi: 10.1186/s13578-021-00575-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature. 2008;455:1061–1068. doi: 10.1038/nature07385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brennan C.W., Verhaak R.G., McKenna A., Campos B., Noushmehr H., Salama S.R., Zheng S., Chakravarty D., Sanborn J.Z., Berman S.H., et al. The somatic genomic landscape of glioblastoma. Cell. 2013;155:462–477. doi: 10.1016/j.cell.2013.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ciriello G., Cerami E., Sander C., Schultz N. Mutual exclusivity analysis identifies oncogenic network modules. Genome Res. 2012;22:398–406. doi: 10.1101/gr.125567.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rutkowska A., Stoczynska-Fidelus E., Janik K., Wlodarczyk A., Rieske P. EGFR(vIII): An Oncogene with Ambiguous Role. J. Oncol. 2019;2019:1092587. doi: 10.1155/2019/1092587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Byrne K.F., Pal A., Curtin J.F., Stephens J.C., Kinsella G.K. G-protein-coupled receptors as therapeutic targets for glioblastoma. Drug Discov. Today. 2021;26:2858–2870. doi: 10.1016/j.drudis.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 101.Carneiro B.A., El-Deiry W.S. Targeting apoptosis in cancer therapy. Nat. Rev. Clin. Oncol. 2020;17:395–417. doi: 10.1038/s41571-020-0341-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.So J.S., Kim H., Han K.S. Mechanisms of Invasion in Glioblastoma: Extracellular Matrix, Ca2+ Signaling, and Glutamate. Front. Cell. Neurosci. 2021;15:663092. doi: 10.3389/fncel.2021.663092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kofuji P., Araque A. G-Protein-Coupled Receptors in Astrocyte-Neuron Communication. Neuroscience. 2021;456:71–84. doi: 10.1016/j.neuroscience.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Tilak M., Holborn J., New L.A., Lalonde J., Jones N. Receptor Tyrosine Kinase Signaling and Targeting in Glioblastoma Multiforme. Int. J. Mol. Sci. 2021;22:1831. doi: 10.3390/ijms22041831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sigismund S., Avanzato D., Lanzetti L. Emerging functions of the EGFR in cancer. Mol. Oncol. 2018;12:3–20. doi: 10.1002/1878-0261.12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Day E.K., Sosale N.G., Xiao A., Zhong Q., Purow B., Lazzara M.J. Glioblastoma Cell Resistance to EGFR and MET Inhibition Can Be Overcome via Blockade of FGFR-SPRY2 Bypass Signaling. Cell Rep. 2020;30:3383–3396.e7. doi: 10.1016/j.celrep.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Guo G., Narayan R.N., Horton L., Patel T.R., Habib A.A. The Role of EGFR-Met Interactions in the Pathogenesis of Glioblastoma and Resistance to Treatment. Curr. Cancer Drug Targets. 2017;17:297–302. doi: 10.2174/1568009616666161215162515. [DOI] [PubMed] [Google Scholar]
- 108.Lee S.Y. Temozolomide resistance in glioblastoma multiforme. Genes Dis. 2016;3:198–210. doi: 10.1016/j.gendis.2016.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Smith J.S., Tachibana I., Passe S.M., Huntley B.K., Borell T.J., Iturria N., O’Fallon J.R., Schaefer P.L., Scheithauer B.W., James C.D., et al. PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J. Natl. Cancer Inst. 2001;93:1246–1256. doi: 10.1093/jnci/93.16.1246. [DOI] [PubMed] [Google Scholar]
- 110.Furnari F.B., Cloughesy T.F., Cavenee W.K., Mischel P.S. Heterogeneity of epidermal growth factor receptor signalling networks in glioblastoma. Nat. Rev. Cancer. 2015;15:302–310. doi: 10.1038/nrc3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Franke T.F., Hornik C.P., Segev L., Shostak G.A., Sugimoto C. PI3K/Akt and apoptosis: Size matters. Oncogene. 2003;22:8983–8998. doi: 10.1038/sj.onc.1207115. [DOI] [PubMed] [Google Scholar]
- 112.Vivanco I., Sawyers C.L. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat. Rev. Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 113.Duerr E.M., Rollbrocker B., Hayashi Y., Peters N., Meyer-Puttlitz B., Louis D.N., Schramm J., Wiestler O.D., Parsons R., Eng C., et al. PTEN mutations in gliomas and glioneuronal tumors. Oncogene. 1998;16:2259–2264. doi: 10.1038/sj.onc.1201756. [DOI] [PubMed] [Google Scholar]
- 114.Hartmann C., Bartels G., Gehlhaar C., Holtkamp N., von Deimling A. PIK3CA mutations in glioblastoma multiforme. Acta Neuropathol. 2005;109:639–642. doi: 10.1007/s00401-005-1000-1. [DOI] [PubMed] [Google Scholar]
- 115.Qin A., Musket A., Musich P.R., Schweitzer J.B., Xie Q. Receptor tyrosine kinases as druggable targets in glioblastoma: Do signaling pathways matter? Neuro-Oncol. Adv. 2021;3:vdab133. doi: 10.1093/noajnl/vdab133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dunlop E.A., Tee A.R. mTOR and autophagy: A dynamic relationship governed by nutrients and energy. Semin. Cell Dev. Biol. 2014;36:121–129. doi: 10.1016/j.semcdb.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 117.Jung C.H., Ro S.H., Cao J., Otto N.M., Kim D.H. mTOR regulation of autophagy. FEBS Lett. 2010;584:1287–1295. doi: 10.1016/j.febslet.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Prabhu V.V., Morrow S., Rahman Kawakibi A., Zhou L., Ralff M., Ray J., Jhaveri A., Ferrarini I., Lee Y., Parker C., et al. ONC201 and imipridones: Anti-cancer compounds with clinical efficacy. Neoplasia. 2020;22:725–744. doi: 10.1016/j.neo.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Arcella A., Carpinelli G., Battaglia G., D’Onofrio M., Santoro F., Ngomba R.T., Bruno V., Casolini P., Giangaspero F., Nicoletti F. Pharmacological blockade of group II metabotropic glutamate receptors reduces the growth of glioma cells in vivo. Neuro Oncol. 2005;7:236–245. doi: 10.1215/S1152851704000961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Taniguchi K., Karin M. NF-κB, inflammation, immunity and cancer: Coming of age. Nat. Rev. Immunol. 2018;18:309–324. doi: 10.1038/nri.2017.142. [DOI] [PubMed] [Google Scholar]
- 121.Zhang Q., Lenardo M.J., Baltimore D. 30 Years of NF-κB: A Blossoming of Relevance to Human Pathobiology. Cell. 2017;168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gray G.K., McFarland B.C., Nozell S.E., Benveniste E.N. NF-κB and STAT3 in glioblastoma: Therapeutic targets coming of age. Expert Rev. Neurother. 2014;14:1293–1306. doi: 10.1586/14737175.2014.964211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Avci N.G., Ebrahimzadeh-Pustchi S., Akay Y.M., Esquenazi Y., Tandon N., Zhu J.J., Akay M. NF-κB inhibitor with Temozolomide results in significant apoptosis in glioblastoma via the NF-κB(p65) and actin cytoskeleton regulatory pathways. Sci. Rep. 2020;10:13352. doi: 10.1038/s41598-020-70392-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Godwin P., Baird A.M., Heavey S., Barr M.P., O’Byrne K.J., Gately K. Targeting nuclear factor-kappa B to overcome resistance to chemotherapy. Front. Oncol. 2013;3:120. doi: 10.3389/fonc.2013.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Igney F.H., Krammer P.H. Death and anti-death: Tumour resistance to apoptosis. Nat. Rev. Cancer. 2002;2:277–288. doi: 10.1038/nrc776. [DOI] [PubMed] [Google Scholar]
- 126.Watanabe S., Nishijima N., Hirai K., Shibata K., Hase A., Yamanaka T., Inazu M. Anticancer Activity of Amb4269951, a Choline Transporter-Like Protein 1 Inhibitor, in Human Glioma Cells. Pharmaceuticals. 2020;13:104. doi: 10.3390/ph13050104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhang C., Yuan X.R., Li H.Y., Zhao Z.J., Liao Y.W., Wang X.Y., Su J., Sang S.S., Liu Q. Anti-cancer effect of metabotropic glutamate receptor 1 inhibition in human glioma U87 cells: Involvement of PI3K/Akt/mTOR pathway. Cell. Physiol. Biochem. 2015;35:419–432. doi: 10.1159/000369707. [DOI] [PubMed] [Google Scholar]
- 128.He J.J., Zhang W.H., Liu S.L., Chen Y.F., Liao C.X., Shen Q.Q., Hu P. Activation of β-adrenergic receptor promotes cellular proliferation in human glioblastoma. Oncol. Lett. 2017;14:3846–3852. doi: 10.3892/ol.2017.6653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lau L.W., Cua R., Keough M.B., Haylock-Jacobs S., Yong V.W. Pathophysiology of the brain extracellular matrix: A new target for remyelination. Nat. Rev. Neurosci. 2013;14:722–729. doi: 10.1038/nrn3550. [DOI] [PubMed] [Google Scholar]
- 130.Najafi M., Farhood B., Mortezaee K. Extracellular matrix (ECM) stiffness and degradation as cancer drivers. J. Cell. Biochem. 2019;120:2782–2790. doi: 10.1002/jcb.27681. [DOI] [PubMed] [Google Scholar]
- 131.Uyar R. Glioblastoma microenvironment: The stromal interactions. Pathol. Res. Pract. 2022;232:153813. doi: 10.1016/j.prp.2022.153813. [DOI] [PubMed] [Google Scholar]
- 132.Ramaiah M.J., Kumar K.R. mTOR-Rictor-EGFR axis in oncogenesis and diagnosis of glioblastoma multiforme. Mol. Biol. Rep. 2021;48:4813–4835. doi: 10.1007/s11033-021-06462-2. [DOI] [PubMed] [Google Scholar]
- 133.Varalda M., Antona A., Bettio V., Roy K., Vachamaram A., Yellenki V., Massarotti A., Baldanzi G., Capello D. Psychotropic Drugs Show Anticancer Activity by Disrupting Mitochondrial and Lysosomal Function. Front. Oncol. 2020;10:562196. doi: 10.3389/fonc.2020.562196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Di Bari M., Tombolillo V., Alessandrini F., Guerriero C., Fiore M., Asteriti I.A., Castigli E., Sciaccaluga M., Guarguaglini G., Degrassi F., et al. M2 Muscarinic Receptor Activation Impairs Mitotic Progression and Bipolar Mitotic Spindle Formation in Human Glioblastoma Cell Lines. Cells. 2021;10:1727. doi: 10.3390/cells10071727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Cristofaro I., Limongi C., Piscopo P., Crestini A., Guerriero C., Fiore M., Conti L., Confaloni A., Tata A.M. M2 Receptor Activation Counteracts the Glioblastoma Cancer Stem Cell Response to Hypoxia Condition. Int. J. Mol. Sci. 2020;21:1700. doi: 10.3390/ijms21051700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Guerriero C., Matera C., Del Bufalo D., De Amici M., Conti L., Dallanoce C., Tata A.M. The Combined Treatment with Chemotherapeutic Agents and the Dualsteric Muscarinic Agonist Iper-8-Naphthalimide Affects Drug Resistance in Glioblastoma Stem Cells. Cells. 2021;10:1877. doi: 10.3390/cells10081877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bavo F., Pucci S., Fasoli F., Lammi C., Moretti M., Mucchietto V., Lattuada D., Viani P., De Palma C., Budriesi R., et al. Potent Antiglioblastoma Agents by Hybridizing the Onium-Alkyloxy-Stilbene Based Structures of an alpha 7-nAChR, alpha 9-nAChR Antagonist and of a Pro-Oxidant Mitocan. J. Med. Chem. 2018;61:10531–10544. doi: 10.1021/acs.jmedchem.8b01052. [DOI] [PubMed] [Google Scholar]
- 138.Pucci S., Bolchi C., Bavo F., Pallavicini M., De Palma C., Renzi M., Fucile S., Benfante R., Di Lascio S., Lattuada D., et al. Evidence of a dual mechanism of action underlying the anti-proliferative and cytotoxic effects of ammonium-alkyloxy-stilbene-based alpha7- and alpha9-nicotinic ligands on glioblastoma cells. Pharmacol. Res. 2022;175:105959. doi: 10.1016/j.phrs.2021.105959. [DOI] [PubMed] [Google Scholar]
- 139.Walczak K., Deneka-Hannemann S., Jarosz B., Zgrajka W., Stoma F., Trojanowski T., Turski W.A., Rzeski W. Kynurenic acid inhibits proliferation and migration of human glioblastoma T98G cells. Pharmacol. Rep. 2014;66:130–136. doi: 10.1016/j.pharep.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 140.Nandakumar D.N., Ramaswamy P., Prasad C., Srinivas D., Goswami K. Glioblastoma invasion and NMDA receptors: A novel prospect. Physiol. Int. 2019;106:250–260. doi: 10.1556/2060.106.2019.22. [DOI] [PubMed] [Google Scholar]
- 141.Albayrak G., Konac E., Dere U.A., Emmez H. Targeting Cancer Cell Metabolism with Metformin, Dichloroacetate and Memantine in Glioblastoma (GBM) Turk. Neurosurg. 2021;31:233–237. doi: 10.5137/1019-5149.JTN.29176-20.3. [DOI] [PubMed] [Google Scholar]
- 142.Cacciatore I., Fornasari E., Marinelli L., Eusepi P., Ciulla M., Ozdemir O., Tatar A., Turkez H., Di Stefano A. Memantine-derived drugs as potential antitumor agents for the treatment of glioblastoma. Eur. J. Pharm. Sci. 2017;109:402–411. doi: 10.1016/j.ejps.2017.08.030. [DOI] [PubMed] [Google Scholar]
- 143.Salmaggi A., Corno C., Maschio M., Donzelli S., D’Urso A., Perego P., Ciusani E. Synergistic Effect of Perampanel and Temozolomide in Human Glioma Cell Lines. J. Pers. Med. 2021;11:390. doi: 10.3390/jpm11050390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lange F., Weßlau K., Porath K., Hörnschemeyer J., Bergner C., Krause B.J., Mullins C.S., Linnebacher M., Köhling R., Kirschstein T. AMPA receptor antagonist perampanel affects glioblastoma cell growth and glutamate release in vitro. PLoS ONE. 2019;14:e0211644. doi: 10.1371/journal.pone.0211644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Eyüpoglu I.Y., Hahnen E., Heckel A., Siebzehnrübl F.A., Buslei R., Fahlbusch R., Blümcke I. Malignant glioma-induced neuronal cell death in an organotypic glioma invasion model. Technical note. J. Neurosurg. 2005;102:738–744. doi: 10.3171/jns.2005.102.4.0738. [DOI] [PubMed] [Google Scholar]
- 146.Sperling S., Aung T., Martin S., Rohde V., Ninkovic M. Riluzole: A potential therapeutic intervention in human brain tumor stem-like cells. Oncotarget. 2017;8:96697–96709. doi: 10.18632/oncotarget.18043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Dailey C.B., Wroblewska B., Wolfe B.B., Wroblewski J.T. The Role of Metabotropic Glutamate Receptor 1 Dependent Signaling in Glioma Viability. J. Pharmacol. Exp. Ther. 2018;367:59–70. doi: 10.1124/jpet.118.250159. [DOI] [PubMed] [Google Scholar]
- 148.Sehm T., Fan Z., Ghoochani A., Rauh M., Engelhorn T., Minakaki G., Dorfler A., Klucken J., Buchfelder M., Eyupoglu I.Y., et al. Sulfasalazine impacts on ferroptotic cell death and alleviates the tumor microenvironment and glioma-induced brain edema. Oncotarget. 2016;7:36021–36033. doi: 10.18632/oncotarget.8651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Bhat K., Saki M., Cheng F., He L., Zhang L., Ioannidis A., Nathanson D., Tsang J., Bensinger S.J., Nghiemphu P.L., et al. Dopamine Receptor Antagonists, Radiation, and Cholesterol Biosynthesis in Mouse Models of Glioblastoma. J. Natl. Cancer Inst. 2021;113:1094–1104. doi: 10.1093/jnci/djab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kast R.E. Adding perphenazine to increase effectiveness of standard glioblastoma chemoirradiation. J. Buon. 2020;25:1676–1686. [PubMed] [Google Scholar]
- 151.Suzuki S., Yamamoto M., Sanomachi T., Togashi K., Sugai A., Seino S., Yoshioka T., Kitanaka C., Okada M. Brexpiprazole, a Serotonin-Dopamine Activity Modulator, Can Sensitize Glioma Stem Cells to Osimertinib, a Third-Generation EGFR-TKI, via Survivin Reduction. Cancers. 2019;11:947. doi: 10.3390/cancers11070947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Frampton J.E. Brexpiprazole: A Review in Schizophrenia. Drugs. 2019;79:189–200. doi: 10.1007/s40265-019-1052-5. [DOI] [PubMed] [Google Scholar]
- 153.Hosseindoost S., Hashemizadeh S., Gharaylou Z., Dehpour A.R., Javadi S.A.H., Arjmand B., Hadjighassem M. β2-Adrenergic Receptor Stimulation Upregulates Cx43 Expression on Glioblastoma Multiforme and Olfactory Ensheathing Cells. J. Mol. Neurosci. MN. 2020;70:1451–1460. doi: 10.1007/s12031-020-01542-7. [DOI] [PubMed] [Google Scholar]
- 154.Drill M., Powell K.L., Kan L.K., Jones N.C., O’Brien T.J., Hamilton J.A., Monif M. Inhibition of purinergic P2X receptor 7 (P2X7R) decreases granulocyte-macrophage colony-stimulating factor (GM-CSF) expression in U251 glioblastoma cells. Sci. Rep. 2020;10:14844. doi: 10.1038/s41598-020-71887-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Kan L.K., Seneviratne S., Drummond K.J., Williams D.A., O’Brien T.J., Monif M. P2X7 receptor antagonism inhibits tumour growth in human high-grade gliomas. Purinergic Signal. 2020;16:327–336. doi: 10.1007/s11302-020-09705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bi L., Liu Y., Yang Q., Zhou X., Li H., Liu Y., Li J., Lu Y., Tang H. Paris saponin H inhibits the proliferation of glioma cells through the A1 and A3 adenosine receptor-mediated pathway. Int. J. Mol. Med. 2021;47:1. doi: 10.3892/ijmm.2021.4863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Southan G.J., Szabó C., Thiemermann C. Isothioureas: Potent inhibitors of nitric oxide synthases with variable isoform selectivity. Br. J. Pharmacol. 1995;114:510–516. doi: 10.1111/j.1476-5381.1995.tb13256.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jafarian-Tehrani M., Louin G., Royo N.C., Besson V.C., Bohme G.A., Plotkine M., Marchand-Verrecchia C. 1400W, a potent selective inducible NOS inhibitor, improves histopathological outcome following traumatic brain injury in rats. Nitric Oxide Biol. Chem. 2005;12:61–69. doi: 10.1016/j.niox.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 159.Maraka S., Groves M.D., Mammoser A.G., Melguizo-Gavilanes I., Conrad C.A., Tremont-Lukats I.W., Loghin M.E., O’Brien B.J., Puduvalli V.K., Sulman E.P., et al. Phase 1 lead-in to a phase 2 factorial study of temozolomide plus memantine, mefloquine, and metformin as postradiation adjuvant therapy for newly diagnosed glioblastoma. Cancer. 2019;125:424–433. doi: 10.1002/cncr.31811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Iwamoto F.M., Kreisl T.N., Kim L., Duic J.P., Butman J.A., Albert P.S., Fine H.A. Phase 2 trial of talampanel, a glutamate receptor inhibitor, for adults with recurrent malignant gliomas. Cancer. 2010;116:1776–1782. doi: 10.1002/cncr.24957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Grossman S.A., Ye X., Chamberlain M., Mikkelsen T., Batchelor T., Desideri S., Piantadosi S., Fisher J., Fine H.A. Talampanel with standard radiation and temozolomide in patients with newly diagnosed glioblastoma: A multicenter phase II trial. J. Clin. Oncol. 2009;27:4155–4161. doi: 10.1200/JCO.2008.21.6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Grossman S.A., Ye X., Piantadosi S., Desideri S., Nabors L.B., Rosenfeld M., Fisher J. Survival of patients with newly diagnosed glioblastoma treated with radiation and temozolomide in research studies in the United States. Clin. Cancer Res. 2010;16:2443–2449. doi: 10.1158/1078-0432.CCR-09-3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.He L., Bhat K., Ioannidis A., Zhang L., Nguyen N.T., Allen J.E., Nghiemphu P.L., Cloughesy T.F., Liau L.M., Kornblum H.I., et al. Effects of the DRD2/3 antagonist ONC201 and radiation in glioblastoma. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2021;161:140–147. doi: 10.1016/j.radonc.2021.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Arrillaga-Romany I., Odia Y., Prabhu V.V., Tarapore R.S., Merdinger K., Stogniew M., Oster W., Allen J.E., Mehta M., Batchelor T.T., et al. Biological activity of weekly ONC201 in adult recurrent glioblastoma patients. Neuro Oncol. 2020;22:94–102. doi: 10.1093/neuonc/noz164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Chi A.S., Tarapore R.S., Hall M.D., Shonka N., Gardner S., Umemura Y., Sumrall A., Khatib Z., Mueller S., Kline C., et al. Pediatric and adult H3 K27M-mutant diffuse midline glioma treated with the selective DRD2 antagonist ONC201. J. Neuro-Oncol. 2019;145:97–105. doi: 10.1007/s11060-019-03271-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Matteoni S., Matarrese P., Ascione B., Buccarelli M., Ricci-Vitiani L., Pallini R., Villani V., Pace A., Paggi M.G., Abbruzzese C. Anticancer Properties of the Antipsychotic Drug Chlorpromazine and Its Synergism With Temozolomide in Restraining Human Glioblastoma Proliferation In Vitro. Front. Oncol. 2021;11:635472. doi: 10.3389/fonc.2021.635472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Chen V.C., Hsieh Y.H., Chen L.J., Hsu T.C., Tzang B.S. Escitalopram oxalate induces apoptosis in U-87MG cells and autophagy in GBM8401 cells. J. Cell. Mol. Med. 2018;22:1167–1178. doi: 10.1111/jcmm.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Elgoyhen A.B., Johnson D.S., Boulter J., Vetter D.E., Heinemann S. Alpha 9: An acetylcholine receptor with novel pharmacological properties expressed in rat cochlear hair cells. Cell. 1994;79:705–715. doi: 10.1016/0092-8674(94)90555-X. [DOI] [PubMed] [Google Scholar]
- 169.Drescher D.G., Ramakrishnan N.A., Drescher M.J., Chun W., Wang X., Myers S.F., Green G.E., Sadrazodi K., Karadaghy A.A., Poopat N., et al. Cloning and characterization of alpha9 subunits of the nicotinic acetylcholine receptor expressed by saccular hair cells of the rainbow trout (Oncorhynchus mykiss) Neuroscience. 2004;127:737–752. doi: 10.1016/j.neuroscience.2004.05.037. [DOI] [PubMed] [Google Scholar]
- 170.Morley B.J., Li H.S., Hiel H., Drescher D.G., Elgoyhen A.B. Identification of the subunits of the nicotinic cholinergic receptors in the rat cochlea using RT-PCR and in situ hybridization. Brain Res. Mol. Brain Res. 1998;53:78–87. doi: 10.1016/S0169-328X(97)00272-6. [DOI] [PubMed] [Google Scholar]
- 171.Taguchi C., Inazu M., Saiki I., Yara M., Hara N., Yamanaka T., Uchino H. Functional analysis of [methyl-(3)H]choline uptake in glioblastoma cells: Influence of anti-cancer and central nervous system drugs. Biochem. Pharmacol. 2014;88:303–312. doi: 10.1016/j.bcp.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 172.Wei X.L., Zhan C.Y., Shen Q., Fu W., Xie C., Gao J., Peng C.M., Zheng P., Lu W.Y. A D-Peptide Ligand of Nicotine Acetylcholine Receptors for Brain-Targeted Drug Delivery. Angew. Chem. Int. Ed. 2015;54:3023–3027. doi: 10.1002/anie.201411226. [DOI] [PubMed] [Google Scholar]
- 173.Verkhratsky A., Nedergaard M. Physiology of Astroglia. Physiol. Rev. 2018;98:239–389. doi: 10.1152/physrev.00042.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Gras G., Samah B., Hubert A., Léone C., Porcheray F., Rimaniol A.C. EAAT expression by macrophages and microglia: Still more questions than answers. Amino Acids. 2012;42:221–229. doi: 10.1007/s00726-011-0866-6. [DOI] [PubMed] [Google Scholar]
- 175.Osipova E.D., Semyachkina-Glushkovskaya O.V., Morgun A.V., Pisareva N.V., Malinovskaya N.A., Boitsova E.B., Pozhilenkova E.A., Belova O.A., Salmin V.V., Taranushenko T.E., et al. Gliotransmitters and cytokines in the control of blood-brain barrier permeability. Rev. Neurosci. 2018;29:567–591. doi: 10.1515/revneuro-2017-0092. [DOI] [PubMed] [Google Scholar]
- 176.Serpe C., Monaco L., Relucenti M., Iovino L., Familiari P., Scavizzi F., Raspa M., Familiari G., Civiero L., D’Agnano I., et al. Microglia-Derived Small Extracellular Vesicles Reduce Glioma Growth by Modifying Tumor Cell Metabolism and Enhancing Glutamate Clearance through miR-124. Cells. 2021;10:2066. doi: 10.3390/cells10082066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Altinoz M.A., Elmaci I. Targeting nitric oxide and NMDA receptor-associated pathways in treatment of high grade glial tumors. Hypotheses for nitro-memantine and nitrones. Nitric Oxide. 2018;79:68–83. doi: 10.1016/j.niox.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 178.Sontheimer H. A role for glutamate in growth and invasion of primary brain tumors. J. Neurochem. 2008;105:287–295. doi: 10.1111/j.1471-4159.2008.05301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Pereira M.S.L., Klamt F., Thome C.C., Worm P.V., de Oliveira D.L. Metabotropic glutamate receptors as a new therapeutic target for malignant gliomas. Oncotarget. 2017;8:22279–22298. doi: 10.18632/oncotarget.15299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yamada T., Tsuji S., Nakamura S., Egashira Y., Shimazawa M., Nakayama N., Yano H., Iwama T., Hara H. Riluzole enhances the antitumor effects of temozolomide via suppression of MGMT expression in glioblastoma. J. Neurosurg. 2020;134:701–710. doi: 10.3171/2019.12.JNS192682. [DOI] [PubMed] [Google Scholar]
- 181.He M., Luo M., Chen S., Li K., Zheng M., Weng Y., Pi R., Liu A. Combined treatment of fasudil and glutamate decreased the viability of human glioblastoma cells by excitotoxicity through NMDAR in vitro. Int. J. Clin. Exp. Med. 2015;8:18434–18440. [PMC free article] [PubMed] [Google Scholar]
- 182.Verbruggen L., Sprimont L., Bentea E., Janssen P., Gharib A., Deneyer L., De Pauw L., Lara O., Sato H., Nicaise C., et al. Chronic Sulfasalazine Treatment in Mice Induces System xc (-)-Independent Adverse Effects. Front. Pharmacol. 2021;12:625699. doi: 10.3389/fphar.2021.625699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Dahlmanns M., Yakubov E., Chen D.S., Sehm T., Rauh M., Savaskan N., Wrosch J.K. Chemotherapeutic xCT inhibitors sorafenib and erastin unraveled with the synaptic optogenetic function analysis tool. Cell Death Discov. 2017;3:11. doi: 10.1038/cddiscovery.2017.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wang X.Y., Li Y.L., Wang H.Y., Zhu M., Guo D., Wang G.L., Gao Y.T., Yang Z., Li T., Yang C.Y., et al. Propofol inhibits invasion and proliferation of C6 glioma cells by regulating the Ca(2+) permeable AMPA receptor-system x(c)(-) pathway. Toxicol. In Vitro. 2017;44:57–65. doi: 10.1016/j.tiv.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 185.Blanchart A., Fernando R., Häring M., Assaife-Lopes N., Romanov R.A., Andäng M., Harkany T., Ernfors P. Endogenous GAB(AA) receptor activity suppresses glioma growth. Oncogene. 2017;36:777–786. doi: 10.1038/onc.2016.245. [DOI] [PubMed] [Google Scholar]
- 186.El-Habr E.A., Dubois L.G., Burel-Vandenbos F., Bogeas A., Lipecka J., Turchi L., Lejeune F.X., Coehlo P.L., Yamaki T., Wittmann B.M., et al. A driver role for GABA metabolism in controlling stem and proliferative cell state through GHB production in glioma. Acta Neuropathol. 2017;133:645–660. doi: 10.1007/s00401-016-1659-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Panosyan E.H., Lin H.J., Koster J., Lasky J.L., 3rd In search of druggable targets for GBM amino acid metabolism. BMC Cancer. 2017;17:162. doi: 10.1186/s12885-017-3148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Patil V., Pal J., Mahalingam K., Somasundaram K. Global RNA editome landscape discovers reduced RNA editing in glioma: Loss of editing of gamma-amino butyric acid receptor alpha subunit 3 (GABRA3) favors glioma migration and invasion. PeerJ. 2020;8:e9755. doi: 10.7717/peerj.9755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hujber Z., Horváth G., Petővári G., Krencz I., Dankó T., Mészáros K., Rajnai H., Szoboszlai N., Leenders W.P.J., Jeney A., et al. GABA, glutamine, glutamate oxidation and succinic semialdehyde dehydrogenase expression in human gliomas. J. Exp. Clin. Cancer Res. 2018;37:271. doi: 10.1186/s13046-018-0946-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Caragher S.P., Hall R.R., Ahsan R., Ahmed A.U. Monoamines in glioblastoma: Complex biology with therapeutic potential. Neuro Oncol. 2018;20:1014–1025. doi: 10.1093/neuonc/nox210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Eshleman J.S., Carlson B.L., Mladek A.C., Kastner B.D., Shide K.L., Sarkaria J.N. Inhibition of the mammalian target of rapamycin sensitizes U87 xenografts to fractionated radiation therapy. Cancer Res. 2002;62:7291–7297. [PubMed] [Google Scholar]
- 192.Wang J.D., Cao Y.L., Li Q., Yang Y.P., Jin M., Chen D., Wang F., Wang G.H., Qin Z.H., Hu L.F., et al. A pivotal role of FOS-mediated BECN1/Beclin 1 upregulation in dopamine D2 and D3 receptor agonist-induced autophagy activation. Autophagy. 2015;11:2057–2073. doi: 10.1080/15548627.2015.1100930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Okada H., Mak T.W. Pathways of apoptotic and non-apoptotic death in tumour cells. Nat. Rev. Cancer. 2004;4:592–603. doi: 10.1038/nrc1412. [DOI] [PubMed] [Google Scholar]
- 194.Lefranc F., Brotchi J., Kiss R. Possible future issues in the treatment of glioblastomas: Special emphasis on cell migration and the resistance of migrating glioblastoma cells to apoptosis. J. Clin. Oncol. 2005;23:2411–2422. doi: 10.1200/JCO.2005.03.089. [DOI] [PubMed] [Google Scholar]
- 195.Lefranc F., Facchini V., Kiss R. Proautophagic drugs: A novel means to combat apoptosis-resistant cancers, with a special emphasis on glioblastomas. Oncologist. 2007;12:1395–1403. doi: 10.1634/theoncologist.12-12-1395. [DOI] [PubMed] [Google Scholar]
- 196.Jain R.K. Normalization of Tumor Vasculature: An Emerging Concept in Antiangiogenic Therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 197.Qian B.Z., Pollard J.W. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Qin T., Wang C., Chen X., Duan C., Zhang X., Zhang J., Chai H., Tang T., Chen H., Yue J., et al. Dopamine induces growth inhibition and vascular normalization through reprogramming M2-polarized macrophages in rat C6 glioma. Toxicol. Appl. Pharmacol. 2015;286:112–123. doi: 10.1016/j.taap.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 199.Rahman A., Fazal F. Blocking NF-κB: An inflammatory issue. Proc. Am. Thorac. Soc. 2011;8:497–503. doi: 10.1513/pats.201101-009MW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Trudler D., Weinreb O., Mandel S.A., Youdim M.B., Frenkel D. DJ-1 deficiency triggers microglia sensitivity to dopamine toward a pro-inflammatory phenotype that is attenuated by rasagiline. J. Neurochem. 2014;129:434–447. doi: 10.1111/jnc.12633. [DOI] [PubMed] [Google Scholar]
- 201.Yeung Y.T., McDonald K.L., Grewal T., Munoz L. Interleukins in glioblastoma pathophysiology: Implications for therapy. Br. J. Pharmacol. 2013;168:591–606. doi: 10.1111/bph.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Rubí B., Maechler P. Minireview: New roles for peripheral dopamine on metabolic control and tumor growth: Let’s seek the balance. Endocrinology. 2010;151:5570–5581. doi: 10.1210/en.2010-0745. [DOI] [PubMed] [Google Scholar]
- 203.Prabhu V.V., Madhukar N.S., Gilvary C., Kline C.L.B., Oster S., El-Deiry W.S., Elemento O., Doherty F., VanEngelenburg A., Durrant J., et al. Dopamine Receptor D5 is a Modulator of Tumor Response to Dopamine Receptor D2 Antagonism. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2019;25:2305–2313. doi: 10.1158/1078-0432.CCR-18-2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kast R.E., Ellingson B.M., Marosi C., Halatsch M.E. Glioblastoma treatment using perphenazine to block the subventricular zone’s tumor trophic functions. J. Neuro-Oncol. 2014;116:207–212. doi: 10.1007/s11060-013-1308-y. [DOI] [PubMed] [Google Scholar]
- 205.Lieb K., Biersack L., Waschbisch A., Orlikowski S., Akundi R.S., Candelario-Jalil E., Hull M., Fiebich B.L. Serotonin via 5-HT7 receptors activates p38 mitogen-activated protein kinase and protein kinase C epsilon resulting in interleukin-6 synthesis in human U373 MG astrocytoma cells. J. Neurochem. 2005;93:549–559. doi: 10.1111/j.1471-4159.2005.03079.x. [DOI] [PubMed] [Google Scholar]
- 206.Goswami S., Gupta A., Sharma S.K. Interleukin-6-mediated autocrine growth promotion in human glioblastoma multiforme cell line U87MG. J. Neurochem. 1998;71:1837–1845. doi: 10.1046/j.1471-4159.1998.71051837.x. [DOI] [PubMed] [Google Scholar]
- 207.Kast R.E. Glioblastoma chemotherapy adjunct via potent serotonin receptor-7 inhibition using currently marketed high-affinity antipsychotic medicines. Br. J. Pharmacol. 2010;161:481–487. doi: 10.1111/j.1476-5381.2010.00923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Abadi B., Shahsavani Y., Faramarzpour M., Rezaei N., Rahimi H.R. Antidepressants with anti-tumor potential in treating glioblastoma: A narrative review. Fundam. Clin. Pharmacol. 2021;36:35–48. doi: 10.1111/fcp.12712. [DOI] [PubMed] [Google Scholar]
- 209.Bi J., Khan A., Tang J., Armando A.M., Wu S., Zhang W., Gimple R.C., Reed A., Jing H., Koga T., et al. Targeting glioblastoma signaling and metabolism with a re-purposed brain-penetrant drug. Cell Rep. 2021;37:109957. doi: 10.1016/j.celrep.2021.109957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Petrosyan E., Fares J., Cordero A., Rashidi A., Arrieta V.A., Kanojia D., Lesniak M.S. Repurposing Autophagy Regulators in Brain Tumors. Int. J. Cancer. 2022;151:167–180. doi: 10.1002/ijc.33965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Torrisi F., Alberghina C., Lo Furno D., Zappalà A., Valable S., Li Volti G., Tibullo D., Vicario N., Parenti R. Connexin 43 and Sonic Hedgehog Pathway Interplay in Glioblastoma Cell Proliferation and Migration. Biology. 2021;10:767. doi: 10.3390/biology10080767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.McCutcheon S., Spray D.C. Glioblastoma-Astrocyte Connexin 43 Gap Junctions Promote Tumor Invasion. Mol. Cancer Res. MCR. 2022;20:319–331. doi: 10.1158/1541-7786.MCR-21-0199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Burnstock G. Introduction to Purinergic Signalling in the Brain. Adv. Exp. Med. Biol. 2020;1202:1–12. doi: 10.1007/978-3-030-30651-9_1. [DOI] [PubMed] [Google Scholar]
- 214.Allard B., Longhi M.S., Robson S.C., Stagg J. The ectonucleotidases CD39 and CD73: Novel checkpoint inhibitor targets. Immunol. Rev. 2017;276:121–144. doi: 10.1111/imr.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Braganhol E., Wink M.R., Lenz G., Battastini A.M.O. Purinergic Signaling in Glioma Progression. Adv. Exp. Med. Biol. 2020;1202:87–108. doi: 10.1007/978-3-030-30651-9_5. [DOI] [PubMed] [Google Scholar]
- 216.Di Virgilio F., Dal Ben D., Sarti A.C., Giuliani A.L., Falzoni S. The P2X7 Receptor in Infection and Inflammation. Immunity. 2017;47:15–31. doi: 10.1016/j.immuni.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 217.Morrone F.B., Horn A.P., Stella J., Spiller F., Sarkis J.J., Salbego C.G., Lenz G., Battastini A.M. Increased resistance of glioma cell lines to extracellular ATP cytotoxicity. J. Neuro-Oncol. 2005;71:135–140. doi: 10.1007/s11060-004-1383-1. [DOI] [PubMed] [Google Scholar]
- 218.Gehring M.P., Kipper F., Nicoletti N.F., Sperotto N.D., Zanin R., Tamajusuku A.S., Flores D.G., Meurer L., Roesler R., Filho A.B., et al. P2X7 receptor as predictor gene for glioma radiosensitivity and median survival. Int. J. Biochem. Cell Biol. 2015;68:92–100. doi: 10.1016/j.biocel.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 219.Xiao X., Yang M., Xiao J., Zou J., Huang Q., Yang K., Zhang B., Yang F., Liu S., Wang H., et al. Paris Saponin II suppresses the growth of human ovarian cancer xenografts via modulating VEGF-mediated angiogenesis and tumor cell migration. Cancer Chemother. Pharmacol. 2014;73:807–818. doi: 10.1007/s00280-014-2408-x. [DOI] [PubMed] [Google Scholar]
- 220.Yu Q., Li Q., Lu P., Chen Q. Polyphyllin D induces apoptosis in U87 human glioma cells through the c-Jun NH2-terminal kinase pathway. J. Med. Food. 2014;17:1036–1042. doi: 10.1089/jmf.2013.2957. [DOI] [PubMed] [Google Scholar]
- 221.Pang D., Li C., Yang C., Zou Y., Feng B., Li L., Liu W., Geng Y., Luo Q., Chen Z., et al. Polyphyllin VII Promotes Apoptosis and Autophagic Cell Death via ROS-Inhibited AKT Activity, and Sensitizes Glioma Cells to Temozolomide. Oxidative Med. Cell. Longev. 2019;2019:1805635. doi: 10.1155/2019/1805635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Li J., Tian Y., Wu A. Neuropeptide Y receptors: A promising target for cancer imaging and therapy. Regen Biomater. 2015;2:215–219. doi: 10.1093/rb/rbv013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Zhang Y., Liu C.Y., Chen W.C., Shi Y.C., Wang C.M., Lin S., He H.F. Regulation of neuropeptide Y in body microenvironments and its potential application in therapies: A review. Cell Biosci. 2021;11:151. doi: 10.1186/s13578-021-00657-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Baver S.B., Hope K., Guyot S., Bjørbaek C., Kaczorowski C., O’Connell K.M. Leptin modulates the intrinsic excitability of AgRP/NPY neurons in the arcuate nucleus of the hypothalamus. J. Neurosci. 2014;34:5486–5496. doi: 10.1523/JNEUROSCI.4861-12.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Hofmann S., Maschauer S., Kuwert T., Beck-Sickinger A.G., Prante O. Synthesis and in vitro and in vivo evaluation of an (18)F-labeled neuropeptide Y analogue for imaging of breast cancer by PET. Mol. Pharm. 2015;12:1121–1130. doi: 10.1021/mp500601z. [DOI] [PubMed] [Google Scholar]
- 226.Reubi J.C., Gugger M., Waser B., Schaer J.C. Y(1)-mediated effect of neuropeptide Y in cancer: Breast carcinomas as targets. Cancer Res. 2001;61:4636–4641. [PubMed] [Google Scholar]
- 227.Hoppenz P., Els-Heindl S., Beck-Sickinger A.G. Peptide-Drug Conjugates and Their Targets in Advanced Cancer Therapies. Front. Chem. 2020;8:571. doi: 10.3389/fchem.2020.00571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Duarte L.F., Reyes A., Farias M.A., Riedel C.A., Bueno S.M., Kalergis A.M., Gonzalez P.A. Crosstalk Between Epithelial Cells, Neurons and Immune Mediators in HSV-1 Skin Infection. Front. Immunol. 2021;12:662234. doi: 10.3389/fimmu.2021.662234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Muñoz M., Coveñas R. Glioma and Neurokinin-1 Receptor Antagonists: A New Therapeutic Approach. Anticancer Agents Med. Chem. 2019;19:92–100. doi: 10.2174/1871520618666180420165401. [DOI] [PubMed] [Google Scholar]
- 230.Melani R., Von Itter R., Jing D., Koppensteiner P., Ninan I. Opposing effects of an atypical glycinergic and substance P transmission on interpeduncular nucleus plasticity. Neuropsychopharmacology. 2019;44:1828–1836. doi: 10.1038/s41386-019-0396-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Han J.M., Kim Y.J., Jung H.J. Discovery of a New CaMKII-Targeted Synthetic Lethal Therapy against Glioblastoma Stem-like Cells. Cancers. 2022;14:1315. doi: 10.3390/cancers14051315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Królicki L., Kunikowska J., Bruchertseifer F., Koziara H., Królicki B., Jakuciński M., Pawlak D., Rola R., Morgenstern A., Rosiak E., et al. (225)Ac- and (213)Bi-Substance P Analogues for Glioma Therapy. Semin. Nucl. Med. 2020;50:141–151. doi: 10.1053/j.semnuclmed.2019.11.004. [DOI] [PubMed] [Google Scholar]
- 233.Majkowska-Pilip A., Rius M., Bruchertseifer F., Apostolidis C., Weis M., Bonelli M., Laurenza M., Królicki L., Morgenstern A. In vitro evaluation of (225) Ac-DOTA-substance P for targeted alpha therapy of glioblastoma multiforme. Chem. Biol. Drug Des. 2018;92:1344–1356. doi: 10.1111/cbdd.13199. [DOI] [PubMed] [Google Scholar]
- 234.Kneifel S., Bernhardt P., Uusijärvi H., Good S., Plasswilm L., Buitrago-Téllez C., Müller-Brand J., Mäcke H., Merlo A. Individual voxelwise dosimetry of targeted 90Y-labelled substance P radiotherapy for malignant gliomas. Eur. J. Nucl. Med. Mol. Imaging. 2007;34:1388–1395. doi: 10.1007/s00259-006-0351-8. [DOI] [PubMed] [Google Scholar]
- 235.Cordier D., Forrer F., Kneifel S., Sailer M., Mariani L., Mäcke H., Müller-Brand J., Merlo A. Neoadjuvant targeting of glioblastoma multiforme with radiolabeled DOTAGA-substance P--results from a phase I study. J. Neurooncol. 2010;100:129–136. doi: 10.1007/s11060-010-0153-5. [DOI] [PubMed] [Google Scholar]
- 236.Krolicki L., Bruchertseifer F., Kunikowska J., Koziara H., Królicki B., Jakuciński M., Pawlak D., Apostolidis C., Mirzadeh S., Rola R., et al. Prolonged survival in secondary glioblastoma following local injection of targeted alpha therapy with (213)Bi-substance P analogue. Eur. J. Nucl. Med. Mol. Imaging. 2018;45:1636–1644. doi: 10.1007/s00259-018-4015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Królicki L., Bruchertseifer F., Kunikowska J., Koziara H., Królicki B., Jakuciński M., Pawlak D., Apostolidis C., Mirzadeh S., Rola R., et al. Safety and efficacy of targeted alpha therapy with (213)Bi-DOTA-substance P in recurrent glioblastoma. Eur. J. Nucl. Med. Mol. Imaging. 2019;46:614–622. doi: 10.1007/s00259-018-4225-7. [DOI] [PubMed] [Google Scholar]
- 238.Zalutsky M.R., Reardon D.A., Akabani G., Coleman R.E., Friedman A.H., Friedman H.S., McLendon R.E., Wong T.Z., Bigner D.D. Clinical experience with alpha-particle emitting 211At: Treatment of recurrent brain tumor patients with 211At-labeled chimeric antitenascin monoclonal antibody 81C6. J. Nucl. Med. 2008;49:30–38. doi: 10.2967/jnumed.107.046938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Lam-Himlin D., Espey M.G., Perry G., Smith M.A., Castellani R.J. Malignant glioma progression and nitric oxide. Neurochem. Int. 2006;49:764–768. doi: 10.1016/j.neuint.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 240.Nomura Y. NF-kappaB activation and IkappaB alpha dynamism involved in iNOS and chemokine induction in astroglial cells. Life Sci. 2001;68:1695–1701. doi: 10.1016/S0024-3205(01)00967-5. [DOI] [PubMed] [Google Scholar]
- 241.Pucci S., Zoli M., Clementi F., Gotti C. alpha9-Containing Nicotinic Receptors in Cancer. Front. Cell. Neurosci. 2021;15:805123. doi: 10.3389/fncel.2021.805123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Belotti Y., Tolomeo S., Yu R., Lim W.T., Lim C.T. Prognostic Neurotransmitter Receptors Genes Are Associated with Immune Response, Inflammation and Cancer Hallmarks in Brain Tumors. Cancers. 2022;14:2544. doi: 10.3390/cancers14102544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Kirtonia A., Gala K., Fernandes S.G., Pandya G., Pandey A.K., Sethi G., Khattar E., Garg M. Repurposing of drugs: An attractive pharmacological strategy for cancer therapeutics. Semin. Cancer Biol. 2021;68:258–278. doi: 10.1016/j.semcancer.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 244.Touat M., Idbaih A., Sanson M., Ligon K.L. Glioblastoma targeted therapy: Updated approaches from recent biological insights. Ann. Oncol. 2017;28:1457–1472. doi: 10.1093/annonc/mdx106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.El-Deiry W.S., Goldberg R.M., Lenz H.-J., Shields A.F., Gibney G.T., Tan A.R., Brown J., Eisenberg B., Heath E.I., Phuphanich S., et al. The current state of molecular testing in the treatment of patients with solid tumors, 2019. CA Cancer J. Clin. 2019;69:305–343. doi: 10.3322/caac.21560. [DOI] [PMC free article] [PubMed] [Google Scholar]