Abstract
Although severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) predominantly infects the respiratory system, several investigations have shown the involvement of the central nervous system (CNS) along the course of the illness, with encephalitis being one of the symptoms. The objective of this systematic review was to evaluate the characteristics (clinical, neuro-radiological aspects, and laboratory features) and outcomes of encephalitis in COVID-19 patients. PubMed, Scopus, and Google Scholar databases were searched from 1 December 2019 until 21 July 2022 to identify case reports and case series published on COVID-19 associated with encephalitis. The quality of the included studies was assessed by the Joanna Briggs Institute critical appraisal checklists. This systematic review included 79 studies, including 91 COVID-19 patients (52.7% male) experiencing encephalitis, where 85.6% were adults (49.3 ± 20.2 years), and 14.4% were children (11.2 ± 7.6 years). RT-PCR was used to confirm 92.2% of the COVID-19 patients. Encephalitis-related symptoms were present in 78.0% of COVID-19 patients at the time of diagnosis. In these encephalitis patients, seizure (29.5%), confusion (23.2%), headache (20.5%), disorientation (15.2%), and altered mental status (11.6%) were the most frequently reported neurologic manifestations. Looking at the MRI, EEG, and CSF findings, 77.6%, 75.5%, and 64.1% of the patients represented abnormal results. SARS-CoV-2-associated or -mediated encephalitis were the most common type observed (59.3%), followed by autoimmune encephalitis (18.7%). Among the included patients, 66.7% were discharged (37.8% improved and 28.9% fully recovered), whereas 20.0% of the reported COVID-19-positive encephalitis patients died. Based on the quality assessment, 87.4% of the studies were of high quality. Although in COVID-19, encephalitis is not a typical phenomenon, SARS-CoV-2 seems like a neuropathogen affecting the brain even when there are no signs of respiratory illness, causing a high rate of disability and fatality.
Keywords: COVID-19, coronavirus, SARS-CoV-2, encephalitis, meningoencephalitis, encephalopathy, systematic review
1. Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus attacks the respiratory system. According to the World Health Organization’s most recent data, over 550 million individuals have been infected, with over 6 million deaths globally [1]. As the coronavirus disease 2019 (COVID-19) pandemic continues, there is growing evidence that this virus also affects the central nervous system (CNS), exhibiting its potential neurotropic and neuroinvasive properties [2,3]. Besides systematic, respiratory, and gastrointestinal symptoms, [4,5,6], neurological manifestations are increasingly recognized in patients with COVID-19, including headache, smell dysfunction, taste disorder, and seizure [7,8,9]. Published data have been suggesting that encephalitis is one of the most fatal neurologic manifestations of COVID-19 involving both adult and pediatric patients [10,11,12]. While the exact mechanism of CNS invasion is still being investigated, possibilities have included both direct viral invasion and indirect damages via inflammatory and autoimmune pathways [13,14].
Encephalitis is an inflammation of the brain parenchyma, exerting serious neurological dysfunction, which is majorly caused by viruses characterized by clinical manifestations such as confusion, reduced or alternative levels of consciousness, fever, headache, seizures, and movement disorder. Diagnosis of encephalitis is usually a combinational approach of laboratory, neuroimaging, and electrophysiologic findings, including blood tests, bronchoalveolar lavage or sputum, urine and stool tests, computed tomography (CT) scan, X-ray, electroencephalogram (EEG), lumbar puncture, and magnetic resonance imaging (MRI) [15,16].
The first case of COVID-19-associated meningoencephalitis was confirmed in a 24-year-old male with severe febrile confusion and generalized tonic-clonic seizure in February 2020 [17]. A recent multicenter retrospective study conducted by the Spanish Society of Neurology reported that encephalitis was present in 2.2% of the COVID-19 patients with neurological symptoms [18]. Previous studies have reported several clinical and laboratory features of SARS-CoV-2-mediated encephalitis. As there has been an escalating number of incidents of encephalitis in COVID-19 patients, with alarming morbidity and mortality rates, this study aimed to systematically evaluate the characteristics (clinical, neuro-radiological aspects, and laboratory features) and outcomes of encephalitis in COVID-19 patients, as well as the possible causative mechanisms of CNS damage.
2. Methods
2.1. Study Guideline
This systematic review (PROSPERO registration number CRD42022354224) implemented the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guideline [19].
2.2. Search Strategies
We used the advanced and expert options of PubMed, Scopus, and Google Scholar databases, searching for journal articles published between 1 December 2019 and 21 July 2022, combining appropriate keywords associated with COVID-19 and encephalitis (Table S1).
2.3. Eligibility Criteria
We considered only case reports or case series published in the English language. In this systematic review, cases with confirmed encephalitis or meningoencephalitis were considered eligible; however, cases reporting only meningitis were excluded.
2.4. Study Screening and Selection
Following the removal of duplicate studies using EndNote X8 software (Clarivate Analytics, Philadelphia, PA, USA), titles, abstracts, and full texts were screened independently by two authors (MAI and SSA) to identify the eligible studies. The reference lists of the included studies were also reviewed to identify any potentially eligible studies. Any disagreements on whether a study should be included or excluded were discussed with the third author (CC) and resolved subsequently.
2.5. Data Extraction
From each study, all the important data and information was retrieved by two authors (MAI and SSA), including study ID (first author’s last name and year of publication), country of origin of the patient, number, age and gender of the patient, SARS-CoV-2 confirmatory test, past medical history, severity of COVID-19, onset of encephalitis from COVID-19 presentation, neurological and psychiatric symptoms, type of suspected or confirmed encephalitis, patients’ outcome, leukocyte types present, opening pressure when performing lumbar puncture, serum blood glucose value, IgG index, brain computerized tomography (CT) scan, magnetic resonance imaging (MRI) and electroencephalogram (EEG) results, white blood cells (WBCs) level, total protein and glucose concentration, status of SARS-CoV-2, and investigation of other pathogens. All the extracted data were verified by another author (CC).
2.6. Quality Assessment
The Joanna Briggs Institute (JBI) critical appraisal checklist for assessing case reports and case series were used to evaluate the methodological quality of the included studies. Two authors (SSA and SK) independently assessed the quality of each of the included studies, and discrepancies were resolved by discussing with the third author (MAI). Studies receiving scores of <50, 50–70, or >70% were classified as low quality (high risk of bias), moderate quality (moderate risk of bias), or high quality (low risk of bias) [9].
3. Results
3.1. Study Selection
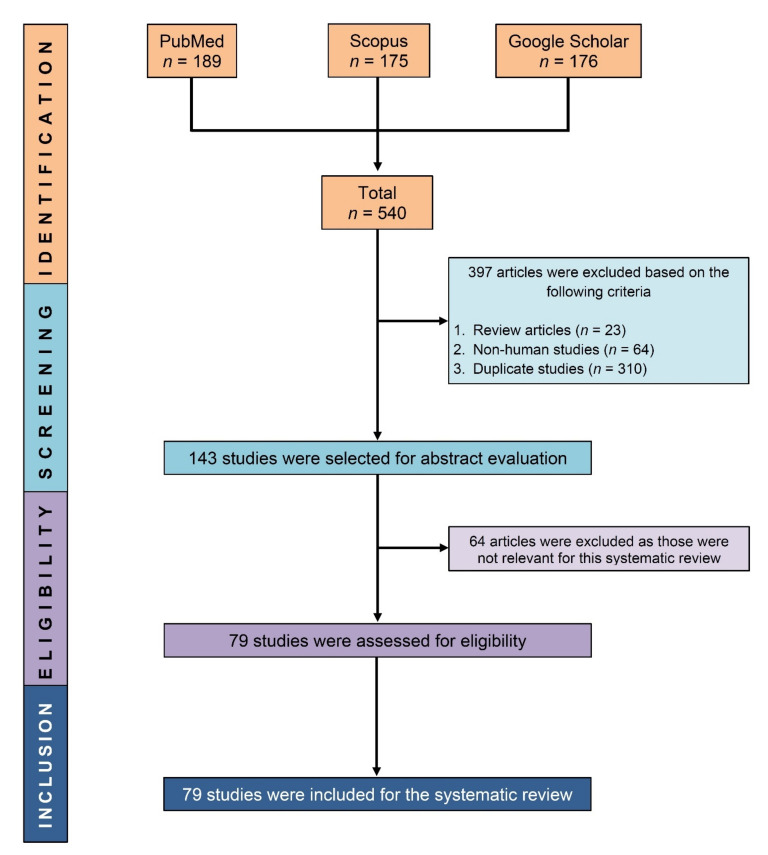
After excluding review articles (n = 23), non-human research (n = 64), and duplicate studies (n = 310) from our initial search results (n = 540), 143 papers were evaluated for eligibility, and 79 studies were eventually included in this systematic review (Figure 1).
Figure 1.
PRISMA flow diagram showing the process of selecting eligible studies.
3.2. General Characteristics of the Included Studies
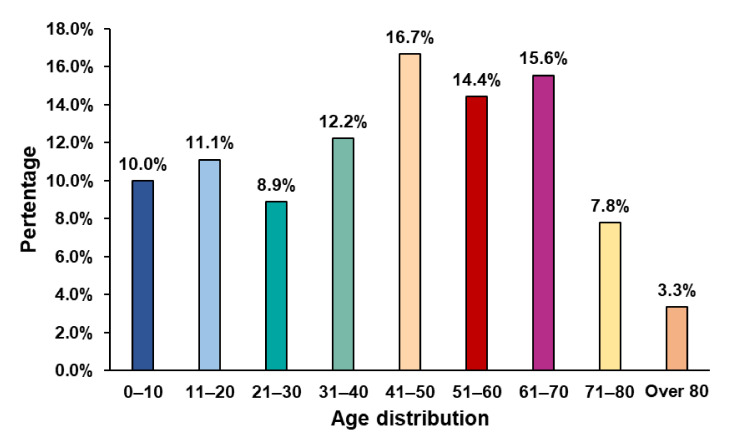
Major characteristics of the included studies are presented in Table 1. In brief, among the included 91 patients, 52.7% were male, 85.6% were adults (aged 49.3 ± 20.2 years), and 14.4% were pediatric patients (aged 11.2 ± 7.6 years), where a majority of the patients’ ages ranged between 41 and 70 years (Figure 2). The majority of the patients’ SARS-CoV-2 (92.2%) were confirmed by using the RT-PCR method.
Table 1.
Major characteristics of the included studies.
| No. | Study ID, Country [references] |
No. of Patient | Age (Years), Gender | Confirmation of SARS-CoV-2 | Past Medical History | Severity of COVID-19 | Onset of Encephalitis from COVID-19 Presentation | Neurological and Psychiatric Symptoms | Type of Suspected or Confirmed Encephalitis | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ahsan 2021, USA [20] |
1 | 7, F | Serology test positive (IgG in serum) | Healthy | Asymptomatic | Post-SARS-CoV-2 infection | 1st admission: status epilepticus, aphasia, encephalopathy; 2nd admission: headache, encephalopathy, slurred speech, altered mental status | Autoimmune encephalitis | Discharged and follow-up confirmed recovery with mild dysarthria |
| 2 | Allahyari 2021, Iran [21] |
1 | 18, F | RT-PCR positive | NR | NR | Initial presentation | Altered mental status, tonic-clonic seizures, confused state, minor meningismus, neck stiffness | Autoimmune encephalitis (SARS-CoV-2-mediated anti-NMDAR encephalitis) | Discharged with full recovery |
| 3 | Andrea 2020, Italy [22] |
1 | 79, F | RT-PCR positive | Rheumatoid arthritis | Mild | Initial presentation | Confusion, somnolence, psychomotor retardation, and cephalea | SARS-CoV-2-mediated encephalitis | Complete recovery in 15 days |
| 4 | Ayatollahi 2020, Canada [23] |
1 | 18, F | RT-PCR positive | NR | Mild | Initial presentation | Drowsiness and confusion, generalized tonic-clonic seizure, impaired orientation to time and place and recent memory | Autoimmune encephalitis | Near complete resolution of the claustrum hyperintensities following 1 month, no seizures following 7 weeks |
| 5 | Ayuningtyas 2022, Indonesia [24] | 1 | 34, F | RT-PCR positive | Obese | Severe | Initial presentation | Reduced consciousness, altered mental status aggressive behavior, seizure, headache | SARS-CoV-2-mediated encephalitis | Discharged with full recovery |
| 6 | Ayuso 2020, Spain [25] |
1 | 72, F | RT-PCR positive | Hypertension, hyperlipidemia, depression, and smoking | NR | Post-SARS-CoV-2 infection (after 8 days of discharge) | 1st admission: delirium; 2nd admission: dizziness, oscillopsia, inattention, disorientation, unsteadiness, myoclonus, and ataxia |
Autoimmune encephalitis (SARS-CoV-2-mediated Bickerstaff encephalitis) | Discharged; after 2 months, very mild unsteadiness was observed |
| 7 | Babar 2020, USA [26] |
1 | 20, F | RT-PCR positive | Obesity and anxiety |
Mild | Initial presentation | Acute altered mental status, confusion, ageusia, insomnia, hypervigilance, obsessive thinking, and urinary incontinence | SARS-CoV-2-mediated encephalitis | Near complete resolution of the neurological symptoms after 12 days of discharge |
| 8 | Benameur 2020, USA [27] |
3 | 31, F | RT-PCR positive | Sickle cell disease | Severe | Initial presentation | Various neurologic manifestations including myoclonus, affected brainstem reflexes, and encephalopathy | SARS-CoV-2-mediated encephalitis | Died |
| 34, M | Hypertension | Initial presentation | NR | |||||||
| 64, M | Hypertension | Initial presentation | Discharged without major neurologic sequelae | |||||||
| 9 | Bernard-Valnet 2020, Switzerland [28] |
2 | 64, F | RT-PCR positive | NR | Mild | Initial presentation | Tonic-clonic seizure, disorientation, strong attention deficit, verbal and motor perseverations and bilateral grasping, hyper-religiosity with mystic delusions, visual hallucinations, and non-convulsive status epilepticus |
SARS-CoV-2-mediated meningoencephalitis | Resolution of her symptoms after 96 h of admission |
| 67, F | RT-PCR positive | NR | Mild | Initial presentation | Intense headache, drowsiness, confusion, motor perseverations, bilateral grasping, and aggressiveness |
SARS-CoV-2-mediated meningoencephalitis | Discharged after 72 h without major neurologic symptoms | |||
| 10 | Bhavsar 2020, USA [29] |
1 | 16, M | RT-PCR positive | Healthy | Mild | Initial presentation | Initially intermittent headache; day 11: confusion, incoherent speech, seizure, and altered mental status, with inconsistent awareness of time and place | SARS-CoV-2-mediated encephalitis | Discharged after day 15 with improved mental status |
| 11 | Bodro 2020, Spain [30] |
2 | 25, M | RT-PCR positive | Healthy | NR | Initial presentation | Headache, left-side paresthesia and ipsilateral paresis, progressing to confusion and agitation | SARS-CoV-2-mediated encephalitis | Fully recovered within 2 days except for amnesia |
| 49, M | RT-PCR positive | Healthy | Mild | Initial presentation | Anomic aphasia, disorientation, confusion, and agitation | Fully recovered within 3 days except for amnesia | ||||
| 12 | Burr 2021, USA [31] |
1 | 23 months, F | RT-PCR positive | Healthy | NR | Initial presentation | Initial: fussiness, poor sleep; day 9: seizure, hyperkinetic movements, and mood lability | Autoimmune encephalitis (SARS-CoV-2-mediated anti-NMDAR encephalitis) | Discharged and fully recovered after 2 weeks |
| 13 | Cao 2020, France [32] |
5 | 49, M | RT-PCR positive | Rheumatoid purpura |
Severe | Initial presentation | Headache and anosmia | SARS-CoV-2-mediated encephalitis | Improvement after 6 days of immunotherapy |
| 56, M | RT-PCR positive | Hypertension | Severe | Initial presentation | Improvement after 2 days of immunotherapy | |||||
| 61, M | RT-PCR positive | Pulmonary sarcoidosis and thrombocytopenia | Severe | Initial presentation | Improvement after 7 days of immunotherapy | |||||
| 37, M | RT-PCR positive | Obesity | Severe | Initial presentation | Died | |||||
| 77, F | RT-PCR positive | Obesity, hypertension and asthma | Severe | Initial presentation | Vegetative state | |||||
| 14 | Casez 2021, France [33] |
1 | 96, F | RT-PCR positive | NR | NR | Initial presentation | At onset: anosmia, dysgeusia; day 3: generalized epileptic seizures, and left hemiparesis | SARS-CoV-2-mediated encephalitis | NR |
| 15 | Chalil 2020, Canada [34] |
1 | 48, F | RT-PCR positive | Healthy | Severe | Initial presentation | Altered mental status | SARS-CoV-2-mediated acute hemorrhagic encephalitis | During the report, she was undergoing rehabilitation |
| 16 | Cheraghali 2021, Iran [35] | 1 | 34 months, child | RT-PCR positive | Healthy | NR | Initial presentation | Tonic-clonic seizures, and loss of consciousness | SARS-CoV-2-mediated encephalitis | Discharged with decerebrate posture |
| 17 | Dahshan 2022, Egypt [36] | 1 | 67, M | RT-PCR positive | Hypertension | NR | Post-SARS-CoV-2 infection (8 days after SARS-CoV-2 infection) | Acute confusion state, behavioral changes, agitation, and one attack of loss of consciousness | Autoimmune encephalitis | Discharged with full recovery |
| 18 | Dono 2021, Italy [37] |
1 | 81, M | RT-PCR positive | Mild hypertension | NR | Post-SARS-CoV-2 infection (on day 14 during her hospitalization for COVID-19 infection) | Since day 14: mild confusion with fluctuation of the mental status; day 16: myoclonic jerks and non-convulsive status epilepticus with coma |
Suspected autoimmune encephalitis | Died |
| 19 | Duong 2020 and Huang 2020, USA [38,39] |
1 | 41, F | RT-PCR positive | T2DM and obesity | NR | Initial presentation | Seizure, lethargy, disorientation, agitation, and hallucination |
SARS-CoV-2-mediated encephalitis | Mental status improved by hospital day 12 |
| 20 | Durovic 2021, Germany [40] | 1 | 22, M | RT-PCR positive | Healthy | NR | Post-SARS-CoV-2 infection (10 days after SARS-CoV-2 infection) | Severe headache, neck stiffness, general weakness, and a loss of smell and taste | Autoimmune encephalitis | Discharged with full recovery |
| 21 | Efe 2020, Turkey [41] |
1 | 35, F | RT-PCR positive | NR | NR | Initial presentation | Headache, nausea, dizziness, and drug-refractory seizures |
SARS-CoV-2-mediated encephalitis | NR |
| 22 | El Aoud 2021, France [42] |
1 | 60, M | Serology test positive | Dyslipidemia | Mild | Initial presentation | Headache, disturbance of consciousness, and vertigo | SARS-CoV-2-mediated encephalitis | Discharged and recovered after 1 month |
| 23 | Elmouhib 2022, Morocco [43] | 1 | 54, F | RT-PCR positive | Healthy | Severe | Initial presentation | Altered mental state, dyspnea, altered consciousness | SARS-CoV-2-mediated autoimmune limbic encephalitis | Discharged with improved state |
| 24 | Esmaeili 2022, Iran [44] | 1 | 67, M | RT-PCR positive | Healthy | Severe | Initial presentation | Drowsiness, decreased level of consciousness, deep tendon reflexes were brisk, and plantar reflexes were upward |
Acute disseminated encephalitis | Died |
| 25 | Etemadifar 2020, Iran [45] |
1 | 51, M | RT-PCR positive | Hypothyroidism and migraine | Mild | Initial presentation | For 3 days, episodic headache, nausea, and drowsiness, and generalized tonic-clonic seizure | SARS-CoV-2-mediated encephalitis | Died |
| 26 | Ferdosian 2021, Iran [46] | 1 | 7, M | RT-PCR positive | Controlled seizures | Mild | Initial presentation | Loss of consciousness, inability to speak | SARS-CoV-2-mediated encephalitis | Discharged with supportive treatment |
| 27 | Freire-Álvarez 2020, Spain [47] | 1 | 39, M | RT-PCR positive | NR | Mild | Initial presentation | Drowsiness, mental disorientation, inconsistent language disorder, and headache | SARS-CoV-2-mediated encephalitis | Following intravenous immunoglobulins and cytokine blockade with IL-6 receptor antagonist, the patient fully recovered after 30 days from admission |
| 28 | Gaughan 2021, Ireland [48] |
1 | 16, F | RT-PCR positive | Mild learning disability | Asymptomatic | Initial presentation | Visual and auditory hallucinations, cognitive difficulties, and high-frequency tremor |
Autoimmune encephalitis | Discharged; at six months, showed significant improvements |
| 29 | Ghosh 2020, India [49] |
1 | 44, F | RT-PCR positive | Healthy | NR | Initial presentation | For 10 days: hypogeusia, hyposmia; then, confusion, disorientation, cognitive disorders, apraxia; then, tonic-clonic seizure and coma |
SARS-CoV-2-mediated AHNE | Died |
| 30 | Grimaldi 2020, France [50] |
1 | 72, M | RT-PCR positive | Transient global amnesia | Mild | Initial presentation | Since day 17: action tremor, ataxia, dysarthria, and upper limb dysmetria and myoclonus |
Autoimmune encephalitis | Improved and discharged at day 37 |
| 31 | Gunawardhana 2021, Sri Lanka [51] | 1 | 47, F | RT-PCR positive | Uncomplicated T2DM | Mild | Post-SARS-CoV-2 infection (4 weeks after SARS-CoV-2 infection) | Confusion and abnormal behavior, seizures, status epilepticus | SARS-CoV-2-mediated encephalitis | Discharged to home with only minor residual cognitive deficits |
| 32 | Haider 2020, USA [52] |
1 | 66, M | RT-PCR positive | Benign prostatic hypertrophy, fatty liver disease, and hypertension |
NR | Initial presentation | Seizure; impaired orientation to time, place, and person; and persistent confusion | SARS-CoV-2-mediated encephalitis | Two months post-discharge, the patient showed significant improvements following rituximab |
| 33 | Hassan 2021, Pakistan [53] | 1 | 58, M | RT-PCR positive | Hypertension | Severe | Initial presentation | Acute chorea | SARS-CoV-2-mediated encephalitis | Discharged |
| 34 | Hayashi 2020, Japan [54] |
1 | 75, M | RT-PCR positive | Mild Alzheimer’s disease |
Severe | Initial presentation | Left-dominant kinetic tremor in hands, alerted consciousness, dysmetria, ataxia, disorientation, and mild gait disturbance | SARS-CoV-2-mediated encephalitis | Died |
| 35 | Kahwagi 2021, Senegal [55] |
1 | 7, F | RT-PCR positive | NR | Mild | Post-SARS-CoV-2 infection (On day 6 during her hospitalization) |
Initial: headache; day 6: generalized tonic-clonic seizures; day 9: gait and behavioral disturbance, confusional syndrome, osteotendinous, and hyperreflexia | SARS-CoV-2-mediated encephalitis | Complete recovery over the follow-up of 2 months |
| 36 | Kamal 2020, United Arab Emirates [56] |
1 | 31, M | RT-PCR positive | Healthy | Mild | Initial presentation | Day 3, behavioral disturbance; day 5: altered mental state, acute behavioral changes, severe confusion, fluctuations in the level of consciousness, and drowsiness | SARS-CoV-2-mediated encephalitis | Discharged; further follow-up confirmed good condition |
| 37 | Kasturiarachi 2022, USA [57] | 1 | 19, F | RT-PCR positive | Menorrhagia, learning disability, and remote suicidal ideation | NR | Post-SARS-CoV-2 infection (recent infection) | Headaches, vomiting, and psychosis, left gaze deviation and right hemiplegia, unable to follow commands or open her eyes spontaneously, seizures, hyperreflexia in the right upper and lower extremities, no hyperkinetic movements |
Sjogren’s-associated encephalitis | Discharged with improved mental status but needed to be monitored closely as an outpatient |
| 38 | Khoo 2020, UK [58] |
1 | 65, F | RT-PCR positive | Alzheimer’s disease, osteoarthritis, and gastro-esophageal reflex disease |
Mild | Post-SARS-CoV-2 infection (2 weeks after SARS-CoV-2 infection) | Week 2: widespread involuntary movements, diplopia, cognitive decline, speaking difficulties, increasing confusion; at entry: myoclonus, ocular movement disorder, aphasia, and perseveration | Autoimmune encephalitis | Discharged with improved neurological symptoms; back to baseline after 1 month from onset |
| 39 | Kimura 2021, Japan [59] | 1 | 68, F | RT-PCR positive | Hypertension | NR | Post-SARS-CoV-2 infection (2 weeks after SARS-CoV-2 infection) | Her eyes were fixed in position and complete flaccid paralysis with diminished tendon reflexes in all extremities; no pathological reflex | Autoimmune encephalitis (SARS-CoV-2-mediated Bickerstaff encephalitis) | Discharged with residual double vision and bilateral disturbance in abduction |
| 40 | Koh 2022, Republic of Korea [60] | 1 | 20, F | RT-PCR positive | Healthy | Moderate | Initial presentation | Tonic-clonic seizure On her left face and arm, drowsy mentality, personality change, dizziness, and somnolence |
Suspected autoimmune encephalitis | Discharged with near-complete recovery |
| 41 | Kumar 2020, India [61] |
1 | 35, M | RT-PCR positive | Headache | NR | Initial presentation | 10 days before: headache; at entry: coma | SARS-CoV-2-mediated ANE | Died |
| 42 | Kumar 2022, India [62] | 1 | 9 days, neonate | RT-PCR positive | Respiratory distress, hypoxia |
NR | Post-SARS-CoV-2 infection (MRI done after 42 days of illness) | Generalized hypotonia generalized seizures | SARS-CoV-2-mediated encephalitis | Discharged with tachypnoea without hypoxia |
| 43 | Marques 2022, Portugal [63] | 2 | 49, F | RT-PCR positive | Healthy | NR | Post-SARS-CoV-2 infection (6 days after SARS-CoV-2 infection) | Altered mental status, lethargic, not oriented to time and place, could not follow commands, neck rigidity, amnesia | SARS-CoV-2-mediated encephalitis | Two months post discharge, she was doing well, with no neurological signs and symptoms |
| 50, F | RT-PCR positive | Depression | NR | Post-SARS-CoV-2 infection (8 days after SARS-CoV-2 infection) | Restless, sometimes physically aggressive, mutism | Three months post discharge, she was doing well with no neurological signs and symptoms | ||||
| 44 | McAbee 2020, USA [11] |
1 | 11, M | RT-PCR positive | Healthy | Asymptomatic | Initial presentation | Status epilepticus | SARS-CoV-2-mediated encephalitis | Recovered within 6 days |
| 45 | Mekheal 2022, USA [64] | 1 | 88, F | NR | Hypertension | NR | Post-SARS-CoV-2 infection (2 months after SARS-CoV-2 infection) | Right leg weakness, dysarthria, altered mental status | Autoimmune encephalitis | NR |
| 46 | Meshref 2021, Egypt [65] | 1 | 66, F | RT-PCR positive | Chronic bronchitis and ischemic heart disease | NR | Initial presentation | Delirious state, confusion, fluctuant conscious level, and disorientation | SARS-CoV-2-mediated encephalitis | Discharged home with full consciousness, no neurological deficits |
| 47 | Mierzewska-Schmidt 2022, Poland [66] | 1 | 2 months, Boy | RT-PCR positive | Healthy | NR | Initial presentation | Irritability, nystagmus, agitation then apathy | SARS-CoV-2-mediated AHNE | The baby showed signs of brain death |
| 48 | Miqdad 2021, Saudi Arabia [67] | 1 | 36, M | RT-PCR positive | Glucose-6 phosphate dehydrogenase deficiency | NR | Initial presentation | Cognitive impairment and decreased responsiveness | SARS-CoV-2-mediated encephalitis | Discharged home with regular follow-up in the neurology clinic |
| 49 | Monti 2020, Italy [68] |
1 | 50, M | RT-PCR positive | Mild hypertension | Asymptomatic | Initial presentation | Confabulations and delirious ideas; day 4: impaired awareness and status epilepticus | Autoimmune encephalitis | Discharged after 4 months of hospitalization without neurological deficits |
| 50 | Moriguchi 2020, Japan [17] |
1 | 24, M | RT-PCR positive | NR | Mild | Initial presentation | Headache, consciousness disturbance, generalized seizures, and status epilepticus | SARS-CoV-2-mediated encephalitis | NR |
| 51 | Morvan 2020, France [69] |
1 | 56, M | RT-PCR positive | Malnutrition, renal lithiasis with left renal abscess and Mycobacterium abscessus pulmonary infection |
NR | Initial presentation | Coma | SARS-CoV-2-mediated ANE | Died |
| 52 | Mullaguri 2021, USA [70] | 2 | 77, F | RT-PCR positive | Parkinson’s disease, cognitive impairment, and hypertension | Severe | Initial presentation | Oriented to self but not to place or time | SARS-CoV-2-mediated AHNE | Died |
| 68, F | RT-PCR positive | Chronic lymphocytic leukemia and hypertension |
Severe | Post-SARS-CoV-2 infection (5 days after SARS-CoV-2 infection) | Comatose, persistent severe encephalopathy | Died | ||||
| 53 | Natarajan 2020, India [10] |
1 | 13, F | RT-PCR positive | Healthy | Mild | Initial presentation | Headache and generalized tonic-clonic seizure | SARS-CoV-2-mediated encephalitis | Discharged home in a normal neurological state |
| 54 | Oosthuizen 2021, South Africa [71] | 1 | 52, M | RT-PCR positive | Healthy | NR | Initial presentation | Multidirectional gaze-evoked nystagmus, dysarthria, and truncal and appendicular ataxia | SARS-CoV-2 mediated encephalitis | Discharged while walking independently, mild emotional lability persisted |
| 55 | Orsini 2021, Brazil [72] | 1 | 52, M | RT-PCR positive | Healthy | Severe | Initial presentation | Intense agitation, cognitive impairment, tonic-clonic seizure | SARS-CoV-2 mediated encephalitis | Died |
| 56 | Panariello 2020, Ecuador [73] |
1 | 23, M | NR | Healthy | Moderate | Initial presentation | Psychomotor agitation, anxiety, thought disorganization, persecutory delusions, dyskinesias and auditory hallucinations | Autoimmune encephalitis | Clinical condition improved |
| 57 | Picod 2020, France [74] |
1 | 58, F | Serology test positive | Hypertension and chronic kidney disease | Asymptomatic | Post-SARS-CoV-2 infection | Clonic seizure, aphasia, right-side hemiparesis, coma, and myoclonus | SARS-CoV-2-mediated encephalitis | Discharged from intensive care unit on day 17, with mild short-term memory impairment |
| 58 | Pilotto 2020, Italy [75] |
1 | 60, M | RT-PCR positive | Healthy | Mild | Initial presentation | First 5 days: irritability, confusion, and asthenia; day 4–5: cognitive fluctuation, at entry: severe akinetic syndrome, mutism, and inhibited, archaic reflexes | SARS-CoV-2-mediated encephalitis | Discharged with normal neurological features |
| 59 | Pizzanelli 2021, Italy [76] |
1 | 74, F | RT-PCR positive | Mild hypothyroidism | Severe | Initial presentation | Day 13: mild confusion and brief episode of impaired awareness; day 14: generalized tonic-clonic seizure |
SARS-CoV-2-mediated autoimmune limbic encephalitis | Discharged on day 35 |
| 60 | Poursadeghfard 2021, Iran [77] | 1 | 18, F | RT-PCR positive | Healthy | NR | Initial presentation | Blurred vision, drowsy | SARS-CoV-2-mediated encephalitis | NR |
| 61 | Rebeiz 2020, USA [78] |
1 | 30 s, M | RT-PCR positive | History of alcohol abuse | Asymptomatic | Initial presentation | 1st admission: confusion, behavioral changes, psychotic features including hallucinations; 2nd admission: worsened mental status, non-verbal, progressive neurological deterioration, and seizures | SARS-CoV-2-mediated encephalitis | Died |
| 62 | Reddy 2021, USA [79] |
1 | 22, F | RT-PCR positive | Infantile seizures |
Asymptomatic | Initial presentation | 2 days of headache; at entry: acute altered mental status; while hospitalized: status epilepticus |
SARS-CoV-2-mediated encephalitis | Died |
| 63 | Sangare 2020, France [80] |
1 | 56, M | RT-PCR positive | Hypertension | Severe | Initial presentation | Vegetative state | SARS-CoV-2-mediated encephalitis | Discharged after 5.5 months, with mild attention deficit disorder |
| 64 | Sarmast 2022, Pakistan [81] | 1 | 63, F | RT-PCR positive | Hypothyroidism and diabetes mellitus | NR | Initial presentation | Confusion accompanied by restlessness, fearfulness, and visual hallucinations. She was anxious, agitated, and aggressive. Altered level of consciousness, slight tremors of the limbs, and psychomotor restlessness | SARS-CoV-2-mediated encephalitis | Two weeks post discharge, she was doing well, with no neurological signs and symptoms |
| 65 | Sattar 2020, Pakistan [82] |
1 | 44, M | RT-PCR positive | Healthy | Moderate | Initial presentation | Day 20: generalized tonic-clonic seizures and confusion | SARS-CoV-2-mediated encephalitis | Discharged on day 34 with normal neurological state |
| 66 | Sharma 2022, USA [83] | 3 | 43, M | RT-PCR positive | Healthy | Mild | Initial presentation | Bitemporal headache, tonic-clonic seizures, | Self-limiting hemorrhagic encephalitis | Discharged with occasional headaches |
| 43, M | RT-PCR positive | Healthy | Severe | Post-SARS-CoV-2 infection (5 days after SARS-CoV-2 infection) | Non-verbal, and had an episode of rapid eye fluttering and gaze deviation, acute respiratory distress syndrome |
Self-limiting leukoencephalopathy | Discharged but complained about recurrent headaches | |||
| 52, M | RT-PCR positive | Diabetes, hypertension, and hyperlipidemia | Severe | Post-SARS-CoV-2 infection (3 weeks after SARS-CoV-2 infection) | Bifrontal headache, blurred vision, left- and right-sided ptosis, ischemic third and sixth nerve palsy |
SARS-CoV-2-mediated encephalitis | Discharged with assistance. No light perception in the left eye with complete ophthalmoplegia, intact vision in the right eye with ptosis | |||
| 67 | Sofijanova 2020, Republic of Macedonia [84] |
1 | 9 months, infant | RT-PCR positive | NR | Severe | Initial presentation | Tonic-clonic seizures, disturbed consciousness, shortness of breath, weakened reaction to painful stimuli | NR | NR |
| 68 | Svedung Wettervik 2020, Sweden [85] |
1 | 40′s, F | RT-PCR positive | Healthy | Severe | Initial presentation | Coma | SARS-CoV-2-mediated AHLE | After TPE treatment for 5 days, patient showed clinical and biochemical improvements |
| 69 | Tee 2022, Malaysia [86] | 1 | 69, M | RT-PCR positive | Hypertension and atrial fibrillation | NR | Initial presentation | Altered behavior | SARS-CoV-2-mediated encephalitis | Subsequently remained well, with no neurological sequelae |
| 70 | Urso 2022, Italy [87] | 1 | 5, F | RT-PCR positive | Healthy | NR | Initial presentation | Neck swelling, right latero-cervical and painful lymphadenopathy, altered mental status, and drowsiness |
SARS-CoV-2-mediated encephalitis | Discharged when COVID-19 test came back negative |
| 71 | Valadez-Calderon 2022, Mexico [88] | 1 | 28, M | NR | No history of chronic disease |
Mild | Post-SARS-CoV-2 infection (2 weeks after SARS-CoV-2 infection) | Incoherent speech, somnolence, auditory hallucinations, suicidal ideation, and generalized tonic-clonic seizures |
Autoimmune encephalitis (anti-NMDAR and anti-glutamic acid decarboxylase 65 co-expression) | Discharged home, but after six weeks-follow-up, he continues physical rehabilitation and presents neurological sequelae related to mood changes, irritability, and agitation episodes |
| 72 | Vandervorst 2020, Belgium [89] |
1 | 29, M | RT-PCR positive | Healthy | Moderate | Initial presentation | Confusion, disorientation in time and space, immediate and short-term memory deficits, concentration and attention difficulties, anxiety, paranoid delusions, followed by dysgeusia and anosmia |
Suspected SARS-CoV-2-associated encephalitis | Improved during hospitalization |
| 73 | Woldie 2020, Canada [90] |
1 | 24, M | RT-PCR positive | AIHA | Severe | Post-SARS-CoV-2 infection (one week later at his follow-up appointment) | Persistent headache, decreased level of consciousness, and seizure activity. | SARS-CoV-2-mediated ANE | Died |
| 74 | Ye 2020, China [91] |
1 | NR, M | RT-PCR positive | NR | Moderate | Initial presentation | Confusion, altered consciousness | SARS-CoV-2 associated encephalitis | Discharged with cleared consciousness |
| 75 | Zambreanu 2020, UK [92] |
1 | 66, F | RT-PCR positive | NR | Mild | Initial presentation | Confusion, seizure, disoriented to time and place, amnestic and mild word-finding difficulties |
Limbic encephalitis | Neurological recovery |
| 76 | Zandifar 2020, Iran [93] |
2 | 49, M | Not performed | NR | Severe | Initial presentation | Seizures; disorientation to place, time, and persons; and decrease of consciousness | Suspected SARS-CoV-2 associated encephalitis | Died |
| 39, M | RT-PCR positive | Moderate | Disoriented, agitated headache, tonic seizure, decreased consciousness and non-responsive verbal or painful commands | SARS-CoV-2 associated encephalitis | ||||||
| 77 | Zanin 2021, Italy [12] |
1 | 47, M | RT-PCR positive | Healthy | Mild | Initial presentation | Intense headache, epileptic seizures | SARS-CoV-2 associated encephalitis | Died |
| 78 | Zuhorn 2020, Germany [94] |
1 | 54, M | RT-PCR positive | Arterial hypertension, obesity (BMI 34 kg/m2), obstructive sleep apnea syndrome | Moderate | Initial presentation | Aggressiveness, Disorientation, and stupor |
Parainfectious encephalitis | Recovered and was discharged with only mild cognitive impairment |
Abbreviations: NR: not reported, M: male, F: female, T2DM: type 2 diabetes mellitus, AHLE: acute hemorrhagic leukoencephalitis, AIHA: autoimmune hemolytic anemia (AIHA), TPA: tissue plasminogen activator, AHNE: acute hemorrhagic necrotizing encephalitis, ANE: acute necrotizing encephalitis.
Figure 2.
Age distribution of COVID-19 patients with encephalitis.
A majority of the studies were reported on European (37.2%), followed by Asian (30.8%) and North American (23.1%), COVID-19 patients. Of these patients, 31.9 were healthy, without any past medical history of illness. Among the reported levels of severity of the COVID-19 patients, 11.7%, 38.3%, 11.7%, and 38.3% of the patients were denoted as asymptomatic, mild, moderate, and severe, respectively. Interestingly, the onset of encephalitis-associated symptoms was manifested in 78.0% of the COVID-19 patients as an initial presentation. Seizure (29.5%), confusion (23.2%), headache (20.5%), disorientation (15.2%), and altered mental status (11.6%) were the most frequently reported neurologic manifestations. Among the types of diagnosed encephalitis, a majority were confirmed to be SARS-CoV-2-associated or -mediated encephalitis (59.3%), followed by autoimmune encephalitis (18.7%). Among the included patients, 66.7% were discharged (37.8% improved, 28.9% fully recovered, and 12.2% patients were discharged without reporting their outcomes), whereas 20.0% of the reported COVID-19-positive encephalitis patients died. Looking at the MRI, EEG, and CT scan findings, 77.6%, 75.5%, and 64.1% of the patients presented with abnormal results, respectively. All the diagnostic features of the COVID-19 patients with encephalitis are presented in Table 2 and S2.
Table 2.
Diagnostic features of encephalitis in patients with COVID-19.
| No. | Study ID | Neuroimaging | Neurophysiology | Serum Analysis | CSF Analysis | Other Pathogen Investigation | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Brain CT Scan Result | Brain MRI Result | EEG Result | WBC | Total Protein (mg/dL) | Glucose (mg/dL) | SARS-CoV-2 | Other Explorations | ||||
| 1 | Ahsan 2021 | NR | Axial T2 showed left perirolandic cortex and posterior parietal lobe cerebral edema, and axial DWI showed restricted diffusion. | Cerebral slowing with left focal slowing | MOG IgG positive | Elevated | 48 | 46 | NR | OCB positive | Bacterial or viral pathogens were negative |
| 2 | Allahyari 2021 | Generalized brain edema | Generalized brain edema | NR | CRP 2+ | Elevated | 241 | 55 | Positive | Anti-NMDAR Positive, HSV 1 and HSV 2 DNA negative | NR |
| 3 | Andrea 2020 | Presented with non-specific diffuse cortical atrophy |
NR | Triphasic waves were observed | Normal CRP and LDH, severe hyponatremia |
Normal | 61 | 49 | Negative | None | HSV negative |
| 4 | Ayatollahi 2020 | Normal | 1st admittance: normal; 2nd admittance: signal hyperintensities on FLAIR and T2-weighted sequences in the claustrum bilaterally | 1st admittance: slow wave activity; 2nd admittance: moderate bilateral non-epileptiform abnormalities | Thrombocytopenia, normal RBC, WBC and hemoglobin, CRP. ANA, aPL, aCL, anti-dsDNA, and ANCA were negative | Elevated | 30 | 41 | Negative | None | HSV negative |
| 5 | Ayuningtyas 2022 | NR | No lesion or intracerebral or intracerebellar pathological enhancement was found | NR | Increased CRP level, and increased D-dimer level | Elevated | 108 | 63 | Positive | No Bacteria and AFB | Anti-HIV, HbSAg, anti-HCV, HSV, and CMV negative |
| 6 | Ayuso 2020 | Normal | 2nd admittance: hyperintense lesions in the caudal vermis and right flocculus, and contrast enhancement was observed in the floor of the fourth ventricle |
Normal | Normal | Normal | 41 | 70 | NR | OCB, anti-Hu, anti-Yo, anti-Ri, anti-CV2, anti-Ma2, and anti-amphiphysin abs were negative |
Anti-GD1 was positive. HIV, VZV, EBV, CMV, and Mycoplasma
Pneumoniae were negative |
| 7 | Babar 2020 | Normal | Normal | Generalized slowing |
Elevated CRP, ferritin, TPO ab, and D-dimer. Negative anti-NMDAR ab, anti-GAD ab, VGKC ab, ANA, ANCA, IgM anti-β2-GPI ab, anti-DNase B ab, anti-streptolysin ab, IL-1 β, IL-6, IL-10, IL-2, C3, and C4 | Normal | 18 | 74 | Negative | None | Gram bacteria negative |
| 8 | Benameur 2020 | NR | Cerebral hemispheric restricted diffusion and cerebral edema | NR | Increased levels of anti-S1 IgM; anti-E IgM, IL-6, IL-8, IL-10, IP-10, and TNF-α | Elevated | >200 | 40 | Negative | None | Influenza A virus positive, influenza B virus negative |
| NR | Splenium lesion and FLAIR recovery | Diffuse slowing | Normal | 37 | 111 | Negative | None | Bacterial or viral pathogens were negative | |||
| NR | Equivocal fluid-attenuated inversion recovery, FLAIR abnormality in the right temporal lobe | NR | Normal | 21 | 88 | Negative | None | Bacterial or viral pathogens were negative | |||
| 9 | Bernard-Valnet 2020 | NR | Normal | Nonconvulsive, focal status epilepticus, slowed theta background rhythm |
NR | Mild elevated | 46.6 | NR | Negative | None | Bacterial or viral pathogens were negative |
| NR | Normal | NR | NR | Mild elevated | 46.1 | NR | Negative | None | |||
| 10 | Bhavsar 2020 | Normal | NR | Slow background without epileptiform discharges or seizures | Normal CBC, CRP and ESR, negative autoimmune encephalopathy antibody panel, hyponatremia | Elevated | 173 | 35 | Negative | None | Bacterial or viral pathogens were negative |
| 11 | Bodro 2020 | Normal | Normal | NR | Elevated D-dimer | Elevated | 105.5 | 80 | Negative | Elevated IL-1β, IL-6, ACE |
Bacterial or viral pathogens were negative |
| Normal | Normal | NR | Elevated CRP, ferritin, LDH, and D-dimer, mild platelet reduction | Elevated | 115.5 | 54 | Negative | Elevated IL-6, ACE |
NR | ||
| 12 | Burr 2021 | NR | Normal | NR | Normal CRP and ESR and positive NMDAR-IgG positivity | NR | 25 | 56 | Negative | None | Bacterial or viral pathogens were negative |
| 13 | Cao 2020 | NR | Bilateral hyperintense lesions in the deep and periventricular supratentorial white matter, either punctiform and slightly diffuse (cases 1–3) or diffuse and confluent (cases 4 and 5), associated with lesions in the pons for two patients (cases 1 and 2) |
Unspecific slow-wave activity | Elevated IL-6 | normal | 32 | NR | Negative | Normal IL-6 | NR |
| Normal IL-6 | 26 | Negative | Normal IL-6 | ||||||||
| Elevated IL-6 | 115 | Negative | Elevated IL-6 | ||||||||
| Elevated IL-6 | 18 | Negative | None | ||||||||
| Elevated IL-6 | 18 | Negative | Normal IL-6 | ||||||||
| 14 | Casez 2021 | NR | Hyperintensity of the olfactory tracts on T2 fluid-attenuated inversion recovery, and diffusion-weighted imaging | NR | NR | 8 WBC | Normal | NR | Negative | None | NR |
| 15 | Chalil 2020 | Extensive bilateral parietal and occipital intraparenchymal hemorrhage and extensive edema causing hydrocephalus |
Cortical gadolinium enhancement with hyper-intense T2 and FLAIR signal surrounding the hemorrhages |
Mild diffuse slowing | Elevated D-dimer, CRP, and ferritin | Elevated | NR | NR | Negative | Elevated CSF IgG ratio | Negative for VZV, HSV, and ENV |
| 16 | Cheraghali 2021 | NR | Symmetric, cortical, and juxtacortical high T1 and T2 signal abnormality, in bilateral parieto-occipital lobes | NR | Elevated level of blood sugar, AST, ALT, ESR, LDH, and positive CRP test |
Normal | 15 | 100 | Positive | Negative for bacterial growth | HSV 1 and HSV 2 negative |
| 17 | Dahshan 2022 | Normal | Normal | NR | NR | Normal | Normal | Normal | NR | HSV 1 and HSV 2 negative | NR |
| 18 | Dono 2021 | NR | Axial T2 fluid-attenuated inversion recovery (T2-FLAIR) and axial diffusion-weighted imaging showed hyperintense lesions of the bilateral parietal cortex, left temporal cortex, and right cingulate cortex |
Epileptiform abnormalities, continuous sharp waves and spike-and-slow-wave complexes |
Slight lymphocytopenia, elevated D-dimer, normal CRP | Elevated | 47 | 78 | Negative | OCB positive | HSV, EBV, CMV, and VZV were negative |
| 19 | Duong 2020 and Huang 2020 | Normal | NR | Generalized slowing with no epileptic discharges |
Normal | Elevated | 100 | 120 | Positive | None | Negative for bacterial culture and HSV 1 |
| 20 | Durovic 2021 | NR | Multiple disseminated pathological T2 and FLAIR hyperintensities | NR | Lyme borreliosis and HIV was negative, MOG antibody positive | Elevated | 39.9 | 64 | Negative | HSV 1 and HSV 2 negative | Complete recovery over the follow-up of 2 months |
| 21 | Efe 2020 | NR | Hyperintense signal in the left temporal lobe in T2 and T2 FLAIR |
NR | NR | NR | NR | NR | NR | None | NR |
| 22 | El Aoud 2021 | Normal | Focal hyperintense signal in the splenium of the corpus callosum on T2 FLAIR and diffusion-weighted images | Slow oscillations without epileptiform features |
Lymphophenia, elevated CRP and ferritin, hypoalbuminemia, ANA, and ANCA were negative |
normal | 49 | 55 | NR | None | Mycoplasma pneumoniae, syphilis, HIV, influenza A and B were negative |
| 23 | Elmouhib 2022 | Normal | High-signal intensity lesion on DWI, T2 FLAIR in the temporal lobes, without diffusion restriction on apparent diffusion coefficient map | NR | CRP at 200 mg/L with a negative PCT at 0.05 μg/L, ferritin at 2300 μg/L | Normal | 100 | 63 | NR | NR | NR |
| 24 | Esmaeili 2022 | NR | Extensive high signal lesions in T2W and FLAIR sequences on bilateral cerebral hemispheres, para-ventricular and subcortical white matter, middle cerebellar peduncles, centrum semi vale, corpus callosum, basal ganglia, thalami, midbrain, and pons. Post-contrast MRI showed sparse enhancements on midpart of the midbrain and left parietal lobe | NR | Elevated CRP and ESR, prothrombin time and partial thromboplastin time were normal | Normal | Normal | Normal | Negative | EBV, HSV, CMV, VZV negative | NR |
| 25 | Etemadifar 2020 | Generalized brain edema and signs of brain herniation | Generalized brain edema, downward herniation of cerebellar tonsils and brain stem, and FLAIR hyperintensities in bilateral cerebral cortices and corpus striatum |
Normal | Leukocytosis, lymphopenia, elevated D-dimer | NR | NR | NR | NR | None | NR |
| 26 | Ferdosian 2021 | NR | Diffuse brain edema | NR | CPK: 42, LDH: 554, CRP: weakly +, ESR: 6. COVID-19 PCR was negative |
Normal | 30 | 57 | Positive | HSV, Enterovirus negative | NR |
| 27 | Freire-Álvarez 2020 | Normal | Extensive involvement of the brain, including cortical and subcortical right frontal regions, right thalamus, bilateral temporal lobes and cerebral peduncles, with no leptomeningeal enhancement |
NR | Elevated ferritin, IL-6, and D-dimer | Elevated | 198 | 48 | Negative | None | CMV, HSV 1 and 2, human HHV 6, HPeV, and VZV negative |
| 28 | Gaughan 2021 | NR | Two tiny punctate T2/FLAIR hyper-intensities in the centrum semiovale bilaterally | Delta slowing | Autoimmune antibody panel negative | NR | 43 | 52.2 | Negative | Autoimmune antibody panel negative | HSV and VZV negative |
| 29 | Ghosh 2020 | NR | Non-enhancing altered intensity lesions in the left high fronto-parietal and right posterior parietal areas with peri-lesional edema; isolated cortical venous thrombosis | NR | All blood parameters normal | Elevated | 60 | 70 | Negative | Elevated IgG index, and OCB negative | Bacterial or viral pathogens were negative |
| 30 | Grimaldi 2020 | NR | Normal | Symmetric diffuse background slowing |
Elevated fibrinogen and CRP, IgG autoantibodies extremely high | Normal | 49 | NR | Negative | OCB negative and IgG autoantibodies | NR |
| 31 | Gunawardhana 2021 | Bi-frontal white matter oedema | T2 FLAIR hyperintensities in the periventricular white matter, mainly clustered around frontal and occipital horns. FLAIR hyperintensities were also noted in the splenium, basal ganglia, and ventral pons |
Low wave discharges consistent with encephalitis | Hemoglobin, liver function tests, creatinine and electrolytes were within normal limits, inflammatory markers (ESR, CRP) were mildly elevated | Elevated | Normal | Normal | SARS-CoV-2 IgM and IgG antibodies are positive SARS-CoV-2 RNA negative | HSV 1 and HSV 2, Japanese encephalitis, VZV were negative | NR |
| 32 | Haider 2020 | Normal | Small acute/subacute lacunar infarcts and a patchy area of T2 bright signals in the cortical and periventricular regions, consistent with cerebritis | Global cerebral dysfunction and severe toxic metabolic encephalopathy | Autoimmune antibody panel negative | Normal | 77 | 86 | Negative | None | Bacterial or viral pathogens were negative |
| 33 | Hassan 2021 | NR | Mild periventricular ischemic changes | NR | Increased CRP, D-dimer, and serum ferritin | Normal | NR | NR | Positive | HSV, OCBs were negative | NR |
| 34 | Hayashi 2020 | NR | Abnormal hyperintensity in the splenium of corpus callosum on diffusion-weighted image | NR | Elevated CRP, lymphopenia | NR | NR | NR | NR | None | NR |
| 35 | Kahwagi 2021 | NR | Normal | Overall slowing of the pattern with the presence of diffuse pseudoperiodic complexes predominating in fronto-temporal area | Elevated CRP | Normal | 76 | NR | NR | None | NR |
| 36 | Kamal 2020 | Multiple hypodensities in the external capsules bilaterally, the insular cortex, and the deep periventricular white matter of the frontal lobes bilaterally |
Abnormal signal intensity in the temporal lobe cortex bilaterally in a rather symmetrical fashion. In addition, the involvement of the parasagittal frontal lobes bilaterally was evident as well, displaying bright signals on T2-fluid-attenuated inversion recovery and T2-weighted images with corresponding diffusion restriction |
Did not display any significant epileptic discharges, possibly due to the masking effect of lorazepam |
Elevated D-dimer | Normal | 55 | 67 | Positive | Normal LA, RF, ANA and aCL |
Mycobacterium Tuberculosis, Gram bacteria, HSV, HHV, and VZV were negative |
| 37 | Kasturiarachi 2022 | NR | Contrast-enhancing lesion in the left occipital, temporal, and frontal lobes, the vermis folia, and tectal plate colliculi; hyperperfusion on arterial spin labeling in the left hemisphere | Left hemispheric poly spike and waves | Elevated LDH, reticulocyte count and bilirubin, schistocytes, and low haptoglobin. Positive ANA, high anti-SSA (anti-Ro) and anti-SSB (anti-La) antibodies, and significantly elevated COVID-19 antibody | NR | NR | NR | Negative | Meningitis/encephalitis panel negative | NR |
| 38 | Khoo 2020 | NR | Normal | Normal | Elevated CRP and D-dimer | Normal | Normal | Normal | Negative | Anti-NMDAR ab and A panel of antineuronal abs and OCB were negative |
NR |
| 39 | Kimura 2021 | NR | No significant abnormalities | No evidence of seizure activity nor response to photic and sound stimuli |
Seropositive for anti–SARS-CoV-2 antibodies |
Normal | 20 | 164 | Negative | OCBs positive |
Campylobacter jejuni, Haemophilus influenzae, Mycoplasma pneumoniae, cytomegalovirus, and EBV negative |
| 40 | Koh 2022 | Patchy ground-glass opacities on bilateral lung fields, compatible with COVID-19 pneumonia |
Diffuse cortical high signal intensities, especially on bilateral insula with increased arterial spin labeling signals |
Repeated high-amplitude polymorphic delta activities from the right frontotemporal area evolving to generalized 1–2 Hz spike-wave discharges, suggesting an impending focal status epilepticus |
IL-6 was mildly elevated to 21.7 pg/mL, CRP level normal |
Elevated | NR | NR | Negative | Elevated IL-6 | HSV, VZV, enterovirus, tuberculosis, EBV, toxoplasmosis, and syphilis negative |
| 41 | Kumar 2020 | Hypodensities in both thalami and left caudate nucleus; left parasellar-middle cranial fossa mass | Left parasellar-middle cranial fossa mass (MRI was performed about 2 weeks earlier than CT) |
NR | Leukocytosis | Normal | Elevated | NR | NR | None | HSV and VZV were negative |
| 42 | Kumar 2022 | NR | Subcortical volume loss (right occipital and left parieto occipital) with cystic changes, tiny hemorrhages at the caudothalamic groove with loss of myelination at the posterior limb of internal capsule | Normal | COVID Ig G And Ig M antibodies were positive | Normal | Normal | Normal | NR | NR | NR |
| 43 | Marques 2022 | Normal | Did not show any pathological changes | Moderate encephalopathy | Elevated LDH and d-dimers | Elevated | 82 | 59 | Negative | HSV, VZV, cytomegalovirus negative | HSV, HIV, VZV negative |
| Normal | Did not show any pathological changes | Mild encephalopathy, without epileptiform activity | HSV 1–2, HIV, and VZV Negative | Normal | 16 | 93 | Negative | HSV, VZV, cytomegalovirus negative | NR | ||
| 44 | McAbee 2020 | Negative | NR | Frontal intermittent delta activity |
NR | Mild elevated | 97 | 92 | NR | None | NR |
| 45 | Mekheal 2022 | Without contrast, an old left cerebellar infarct, with no evidence of acute infarct or hemorrhage |
Old infarct, acute infarct involving the left cerebellum, as well as an effacement of the left temporal horn and edema within the left pons, midbrain, left temporal lobe, and surrounding the basal ganglia |
Moderate-severe diffuse encephalopathy without epileptiform discharges or seizures | Elevated ESR, CRP, and D-dimer, serum COVID-19 IgG antibody positive | Elevated | 145 | 75 | Negative | Meningitis/encephalitis panel by PCR were negative, including all microbial cultures | NR |
| 46 | Meshref 2021 | Right temporal hypo-dense area | Ill-defined area of faint low signal intensity lesion in T1, hyperintense in T2. FLAIR images showed partial restriction in DWI with no significant enhancement post IV gadolinium contrast injection, involving the right cerebral hemisphere, mainly at the temporal area, suggesting encephalitis |
NR | NR | NR | Normal | Normal | NR | No bacterial growth, herpes virus was negative | NR |
| 47 | Mierzewska-Schmidt 2022 | NR | Diffuse areas of oedema associated with numerous symmetrical changes with punctate hemorrhages in basal ganglia, thalami, brainstem, and cerebral gray matter | NR | Low Hb 9.3 g/dL and Platelet count 183 × 103/μL, CRP 7.4 mg/L, D-dimers 0.97 | Elevated | 660.00 | < 10 | Positive | Elevated lactic acid, meningoencephalitis PCR panel was negative | All bacterial cultures were negative |
| 48 | Miqdad 2021 | Unremarkable | Normal | Different abnormalities suggestive of encephalitis | CRP, D-dimer, and procalcitonin were high | Elevated | 832 | 2.59 | NR | HSV PCR and gram stain negative | NR |
| 49 | Monti 2020 | NR | Normal | Abnormal | Elevated levels of IL-6 | Elevated | NR | NR | NR | OCB and anti-NMDAR ab positive, with elevated levels of IL-6 and IL-8 | Bacterial or viral pathogens were negative |
| 50 | Moriguchi 2020 | Normal | Diffusion -weighted images showed hyperintensity along the wall of inferior horn of right lateral ventricle. FLAIR images showed hyperintense signal changes in the right mesial temporal lobe and hippocampus with slight hippocampal atrophy |
NR | Elevated levels of WBC and CRP | Mild elevated | NR | NR | Positive | NR | HSV and VZV were negative |
| 51 | Morvan 2020 | Acute hydrocephalus with diffuse cerebral edema, spontaneous bilateral thalamic hyperdensities, with discrete contrast enhancement and spontaneous hyperdensity in subarachnoidal spaces. |
Hypersignal of both thalami brainstem and cerebellum with some hemorrhagic component on T2 sequences |
NR | Elevated levels of CRP, fibrinogen, and D-dimer Low Hb, high AST, low factor V, high troponin, high creatinine, very low kaliemia |
Normal | 79 | NR | Negative | None | HIV negative |
| 52 | Mullaguri 2021 | Axial sections of the brain showed punctate hemorrhages in the right frontal and left frontal and parietal areas |
Axial section showed hyperintensities in bilateral centrum semiovale areas. MRI of the brain showing innumerable punctate microhemorrhages in the cerebellar peduncles and subcortical regions of bilateral hemispheres, including bilateral basal ganglia and internal capsules | NR | Hyponatremia (132 mMol/L), significant elevations in D-dimer, LDH, ferritin, CRP, and CK |
NR | NR | NR | NR | NR | NR |
| 53 | Natarajan 2020 | NR | Normal | Normal | NR | Elevated | 86 | 77 | Negative | None | HSV, CMV, and VZV were negative |
| 54 | Oosthuizen 2021 | Central midbrain hypodensity |
Features consistent with brainstem encephalitis | Normal | Elevated ESR | Elevated | 37 | 65 | Positive | Immunoglobulin G index 0.62, SARS-CoV-2 antibody negative | Tests for infections and malignancy negative |
| 55 | Orsini 2021 | NR | Normal | Normal | NR | Normal | 60 | 53 | Positive | Bacterial culture negative | NR |
| 56 | Panariello 2020 | Normal | NR | Theta activity at 6 Hz | Elevated CRP and D-dimer with negative ANA, ANCA, anti-ENA, aCL, and anti-β2-GPI abs | NR | 65.4 | 70 | Negative | Elevated IL-6 and anti-NMDAR ab | HSV, EBV, CMV, VZV, and enterovirus were negative |
| 57 | Picod 2020 | Normal | Bilateral lesions (hypersignal or enhancement of meninges, cortical and subcortical regions spread over the insula, the cingula, the medial part of occipital areas, and the internal part of the left-side temporal lobe) | Diffuse intermittent periodic activity | Moderately elevated IL-6 | Normal | 28 | NR | Negative | Elevated IL-6 and OCB negative | HSV negative |
| 58 | Pilotto 2020 | Normal | Normal | Generalized slowing, with decreased reactivity to acoustic stimuli |
Elevated D-dimer, a wide immunological screening of immune-mediated encephalitis was negative |
Mild elevated | 69.6 | NR | Negative | Slightly elevated IL-6, strongly elevated IL-8, TNF-α and β2M | Neurotropic viruses negative |
| 59 | Pizzanelli 2021 | Normal | Bilateral symmetrical mesial temporal lobes T2/FLAIR/DWI hyperintensities, with mild hippocampal thickening | Autoimmune panel for encephalitis negative | Elevated CRP and fibrinogen | Normal | 104 | 67 | Negative | OCB and autoimmune panel for encephalitis negative | Neurotropic viruses negative |
| 60 | Poursadeghfard 2021 | NR | FLAIR increased signal intensity in the cortical and subcortical regions of both mesial temporal lobe as well as both side hippocampal tails, with relative symmetrical appearance without evidence of significant enhancement or restricted DWI compatible with viral or autoimmune encephalitis | NR | NR | NR | NR | NR | NR | NR | Cat-scratch disease, toxoplasmosis, syphilis, Lyme disease, brucellosis, HIV, VZV, HSV, CMV, EBV, and hepatitis B and C were negative |
| 61 | Rebeiz 2020 | A questionable subarachnoid hemorrhage within the mesial parietal region and nonspecific hypoattenuation in the splenium of the corpus callosum |
1st MRI: DWI and FLAIR hyperintensity of the splenium of corpus callosum; 2nd MRI (after readmission): new abnormal T2/FLAIR hyperintense and restricted diffusion involving the left thalamus, right parasagittal frontal cortex, and bilateral genu of the corpus callosum |
Generalized slowing | VES 27; Normal IL-6 and CRP |
Elevated | 297 | 56 | Negative | None | Neurotropic viruses negative |
| 62 | Reddy 2021 | 4 days after admission: severe diffuse cerebral edema with cerebellar tonsillar herniation |
No acute intracranial process |
NR | NR | Normal | 108 | 88 | NR | None | Bacterial or viral pathogens were negative |
| 63 | Sangare 2020 | NR | Multiple small hemorrhagic lesions in the pontine tegmentum, bilateral subinsular region |
Poorly reactive delta slow waves | NR | Normal | Normal | Normal | NR | None | NR |
| 64 | Sarmast 2022 | Unremarkable | Hyperintense signals in frontoparietal and parietotemporal lobes on FLAIR/T2 sequence | NR | Mildly elevated CRP, elevated LDH, CPK, ferritin, and D-dimer | Normal | 66 | 81 | Negative | VZV PCR, HSV 1–2 PCR, CMV PCR, bacterial antigen negative | Negative for HSV 1–2, HIV, enterovirus, and VZV virus |
| 65 | Sattar 2020 | Day 20: few scattered foci of white matter hypo-attenuation |
Day 25: abnormal medial cortical signals in the bilateral frontal lobe region | NR | Autoimmune antibody panel negative | Mild elevated | 39 | 75 | Positive | CSF color pinkish | Bacterial or viral pathogens were negative |
| 66 | Sharma 2022 | left temporal hypodensity |
Intense focal edema within the left hippocampus with mild restricted diffusion, postcontrast enhancement, and hemorrhage seen on susceptibility-weighted imaging | Normal | Creatinine of 1.3 mg/dL, CRP of 42.4 mg/L, ESR of 95 mm/h, CK 858 IU/L, D-Dimer of 1821 FEU, fibrinogen of 644 mg/dL, ferritin of 1352.9 ng/mL, LD of 392 IU/L, prothrombin time (PT/INR) of 1.3/15 |
Elevated | 44 | 59 | NR | Gram stain, bacterial culture, and meningitis/ encephalitis panel were negative. VZV PCR, cryptococcal antigen, culture, AFB smear and culture, and CMV PCR were negative. VZV IgG elevated |
NR |
| Small right temporal hyperdensity (0.6 cm diameter) suggestive of a hemorrhage with normal vasculature |
Right anterior temporal lobe intraparenchymal hemorrhage; additional multiple scattered foci of susceptibility artifact particularly in the gray–white junctions and corpus callosum; and sulcal FLAIR hyperintensity in the right frontal, biparietal, and left temporal lobes |
NR | Elevated IL-6, fibrinogen, and thrombocytopenia | Elevated | 118 | 28 | NR | Meningitis/encephalitis panel, AFB smear and culture, cryptococcal antigen, and VZV PCR, CMV PCR, CSF cytology were negative | NR | ||
| 1st admission: stenosis of the cavernous segment of the right ICA. 2nd admission: unremarkable |
1st admission: mild periventricular white matter disease. 2nd admission: multiple punctate foci of restricted diffusion in the bilateral frontal, parietal, occipital, and temporal lobes, mild meningeal enhancement of the anterior and middle cranial fossa, and opacification of multiple ethmoid and mastoid air cells | NR | 1st admission; creatinine of 1.4 mg/dL, ESR 111 mm/h, CRP 43.5 mg/L, and HbA1c 12.6%. 2nd admission: fibrinogen of >1000 mg/dL, ferritin of 743 ng/mL, ESR of >130 mm/h, CRP of 313 mg/L, PT/INR of 19/1.6, procalcitonin of 1.24 ng/mL, and antithrombin-3 activity of 62% |
Elevated | 82 | 78 | NR | Borrelia burgdorferi IgM/IgG titer (0.09 LIV, 0.09 LIV), negative CSF ACE, VDRL, and cryptococcal antigen, EBV PCR positive |
AIDP, myasthenia gravis, or vasculitis, secondary infections, mycoplasma IgM, anti-cardiolipin antibodies, B-2 glycoprotein, anti-Xa essay, HIV antibodies, hepatitis panel, serum cryoglobulin PAVAL, autoimmune encephalitis panel were negative |
||
| 67 | Sofijanova 2020 | Enlargement of the lateral ventricles, intraventricular masses, pronounced internal hydrocephalus. | NR | NR | Normal | NR | 202.7 | 91.4 | NR | None | NR |
| 68 | Svedung Wettervik 2020 | White matter brain edema with compressed convexity sulci |
Increased white matter intensity on flair images, microhemorrhages with involvement of basal ganglia on susceptibility-weighted imaging | Pronounced, generalized slowing over both hemispheres, no electrographic epileptic activity |
Mild increased IL-6 | Elevated | NR | 86.4 | Negative | Elevated levels of IL-6 | Negative for bacteria and neurotropic viruses |
| 69 | Tee 2022 | Noncontrast brain CT revealed an old right lenticular infarct | Performed 1 month later, normal findings | Performed 3 weeks later, normal findings |
NR | Elevated | 116 | NR | Positive | NR | NR |
| 70 | Urso 2022 | NR | CNS involvement, suggestive of encephalitis | A slow base rhythm (theta-delta) together with synchronous bilateral potentials formed by slow waves with predominance on the right side. | NR | Normal | 27 | Normal | Negative | No bacterial or tuberculous infection | HSV1, varicella-zoster, EBV, and CMV were negative |
| 71 | Valadez- Calderon 2022, Mexico | NR | Hyperintensities in the bilateral anterior cingulate cortex and temporal lobes | Subcortical dysfunction in frontal, temporal, and occipital regions |
Normal | Normal | Normal | Normal | Negative | NR | NR |
| 72 | Vandervorst 2020 | Normal | Asymmetric FLAIR hyperintensity of the left medial temporal cortex associated with mild gyral expansion | General excess of beta-rhythm |
NR | Normal | Normal | Normal | Negative | None | Negative for enterovirus and HSV |
| 73 | Woldie 2020 | Non-specific symmetric cerebral enhancement |
T2/FLAIR hyper intensity on the medial aspect of each temporal lobe, bilateral basal ganglia, and medial thalami consistent with severe acute necrotizing encephalitis | NR | Elevated LDH | NR | NR | NR | NR | NR | Positive for Cryptococcus neoformans |
| 74 | Ye 2020 | Normal | NR | NR | Low WBC and lymphocytes | Normal | 27 | 56.5 | negative | None | Negative for bacterial or tuberculous infection |
| 75 | Zambreanu 2020 | Normal | Non-enhancing, symmetrical T2 and FLAIR hyperintensities in mesial temporal lobes and medial thalami and to a lesser extent upper pons, as well as scattered subcortical white matter hyperintensities |
NR | Elevated CRP, lymphopenia | Normal | 100 | 63 | Negative | Autoimmune antibody panel negative | Negative for streptococci, meningococcus, haemophilus, listeria, Escherichia coli, HSV 1 and 2, HHV6, enteroviruses, parechovirus, CMV, VZV, and Cryptococcus |
| 76 | Zandifar 2020 | Diffuse brain parenchymal edema and reduced lateral ventricles | NR | NR | Leukocytosis and lymphopenia | Mild elevated | 70 | 30 | Negative | None | NR |
| NR | Leukocytosis and lymphopenia and LDH elevated |
Mild elevated | 74 | 33 | Positive | ||||||
| 77 | Zanin 2021 | Increasing vasogenic oedema in the right temporo-fronto-parietal region with extension to the capsular region, to the cerebral peduncle and in the ipsilateral mesencephalic region. Severe compressive effect on the right lateral ventricle |
Severe vasogenic oedema of the white matter with 10 mm shift of the midline and compression of the right lateral ventricle; DWI: extensive cortical marked restriction | NR | Increased CRP and WBC with lymphopenia | NR | NR | NR | NR | None | NR |
| 78 | Zuhorn 2020 | NR | Signal alterations within the claustrum/external capsule region, showed reduced diffusion | NR | LDH, D-dimer, myoglobin, IL-6 and CRP, IgA and IgG positive for SARS-CoV-2 | Mild elevated | 39.6 | 57 | Negative | None | Negative for HSV, VZV, cytomegaly and Epstein Barr virus |
Abbreviation: NR: not reported, AFB: acid-fast bacilli, CT: computed tomography, WBC: white blood cells, RBC: red blood cell, MOG: myelin oligodendrocyte glycoprotein, AST: aspartate aminotransferase, ALT: alanine aminotransferase, HSV: herpes simplex virus, CRP: C-reactive protein, LDH: lactate dehydrogenase, FLAIR: fluid-attenuated inversion recovery, ANA: antinuclear antibody, aCL: anticardiolipin antibody, dsDNA: double-stranded DNA, ANCA: antineutrophil cytoplasmic antibodies, NMDAR: N-methyl-D-aspartate receptor, GAD: glutamic acid decarboxylase, VGKC: voltage gated potassium channel, IL: interleukin, GPI: glycoprotein I, ab: antibody, TPO: thyroid peroxidase, IP: induced protein, CBC: complete blood count, ESR: erythrocyte sedimentation rate, CPK: creatine phosphokinase, CK: creatine kinase, VZV: varicella-zoster virus, ENV: erythrocytic necrosis virus, EBV: Epstein–Barr virus, CMV: cytomegalovirus, OCB: oligoclonal band, DWI: diffusion-weighted imaging, HIV: human immunodeficiency virus, HHV: human herpes virus, HPeV: human parechovirus, LA: lupus anticoagulant, RF: rheumatoid factor, ENA: extractable nuclear antigens, β2M: β2-microglubulin. Normal protein level: 15–45 mg/dL, normal glucose level: 40–70 mg/dL.
3.3. Evidence-Based Analyses
3.3.1. Infant to Children with COVID-19
Seizures were frequently present, and prognosis was often poor. Neurologic involvement in a term neonate with prenatal exposure to SARS-CoV-2 was described for the first time in 2022 [62]. The main and first symptoms of this baby’s infection were respiratory distress and ground glass pneumonia. She manifested seizure thereafter, and neurological deficit only at 49 days of disease following extubating and respiratory improvement. The neurological deficit corresponded to documented MRI lesions. Only IG therapy showed some benefit. A fatal case of acute hemorrhagic necrotizing encephalitis (AHNE) affected a 2-month-old boy, who presented with fever and general symptoms, but had cardiac arrest followed by brain death within a few days [66]. Another young patient was a 9-month-old infant [84]. The initial symptoms were fever and profuse vomiting for two days. Then, he manifested convulsive seizure and consciousness alteration. CT scan indicated severe hydrocephalus, and a high protein titer in the CSF suggested aseptic meningoencephalitis (Table 1). Despite antibiotic, antiviral, anticonvulsant, and anti-edematous medication, the child had a cardiac arrest and had to be resuscitated and intubated. Due to migrating to another country, the rest of the history of the infant remained unclear. A 34-month boy also had a poor prognosis [35]. He manifested with fever, seizure, and upward gaze, with progressive worsening, and was admitted to intensive care unit due to recurrent seizures and consciousness compromission. His brain MRI documented scattered foci of altered signal together with hemorrhagic foci. Therapy based on antibiotics, antiviral, and antiepileptic drug (AED) failed; he had a mild improvement after dexamethasone, hydroxychloroquine, and intravenous immunoglobulins (IVIG). He was finally in a vegetative state. Six more children—three girls, one aged 23 months [31] and two others aged 7 years [20,55], and two boys aged 7 and 11 years [11,46]—were described with febrile and manifesting epileptic seizures. Ahsan’s and McAbee’s [11,20] cases were with status epilepticus. Burr’s [31] child also showed neurological deficits with language disorders and involuntary movements. Neurological impairment occurred up to nine days after the onset of symptoms; an MRI of the brain revealed no abnormalities. Anti-NMDAR receptor antibodies were detected both in serum and CSF [31]. In this case, the initial treatment with IV methylprednisolone was unsuccessful; therefore, IV immunoglobulin (IVIG) was given instead. The case described by Ahsan et al. [20] tells a similar story, with status epilepticus and aphasia following sporadic self-limited seizures in the prior week and neurologic worsening one week later. This girl’s MRI documented alteration in the perirolandic and posterior area of the parietal lobe, with cortical edema. Following the investigation of various autoantibodies, anti-myelin oligodendrocyte glycoprotein (MOG) antibodies were detected. Following that, IVIG therapy was given, and the child improved over the following five days before being sent home; mild dysarthria persisted at follow-up. In addition, the boy described by Ferdosian et al. [46] had fever and aphasia, with consciousness alteration, for three days, and a history of recurrent seizures in the last five months. His MRI documented diffuse brain edema and CSF contained SARS-CoV-2 RNA. He improved initially with therapy with antibiotics, antiviral, and AED, but did not improve after therapy with IVIG, remdesivir, and AED.
The child described by McAbee et al. [11], who developed status epilepticus and fever after two days of generalized weakness, achieved a better prognosis. He was treated with anti-epileptic drugs (AED), and recovery was completed in six days. A girl, described by Kahwagi et al. [55], was the only child manifesting respiratory symptoms. She had a cough, headache, and fever for six days, followed on day six by multiple generalized tonic-clonic seizures. Her MRI was unremarkable. She experienced gait and behavioral issues, confusional syndrome, and osteotendinous hyperreflexia on day nine. Her EEG background displayed slowness and superimposed pseudoperiodic complexes. This girl was treated with only AED; her seizures diminished, and behavior disorders disappeared over the next two months. Finally, a five-year-old girl manifested with respiratory symptoms, low-grade fever, and neck edema with lymphadenopathy [87]. In a few days, she became lethargic; her EEG was characterized by slow-wave rhythm, and brain oedema with altered signal of splenium of corpus callosum and subcortical parietal lobes was detected in brain MR. She improved and was discharged after two weeks, after having been treated with antibiotics, antivirals, and steroids.
3.3.2. Adolescents with COVID-19
Seven teenagers suffered from encephalitis attributed to COVID-19 infection. Other than respiratory symptoms, headache, seizures, mood, and conscious level alteration were the main neurologic manifestations. Natarajan et al. [10] reported the case of a 13-year-old girl with a fluctuant history of fever, headache, tonic seizures, and status epilepticus. Although she did not manifest respiratory symptoms, her chest CT scan revealed patchy peripheral ground glass opacities. She was treated with levetiracetam and ceftriaxone, and improved in 48 h. Ground glass opacities in the lungs were also detected in the 16-year-old boy mentioned by Bhavsar et al. [29]. This boy suffered from pharyngitis, headaches, fever, and generalized weakness. On day 11, his neurologic status worsened, with progressive somnolence, confusion, incoherent speech, and walking. After that, he had seizures that required benzodiazepine and AED. Laboratory investigations revealed plasmatic and urinary alterations consistent with the syndrome of inappropriate antidiuretic hormone secretion (SIADH), and his EEG had a slow background. He was treated with antibiotics, and improvement of hyponatremia was accomplished, although he exhibited persistent neurologic disfunction. After one week, he developed an infrapopliteal deep venous thrombosis, and therapy with low-molecular-weight heparin was started. He was discharged to his home on day 15.
An 18-year-old girl was also infected with ground glass pneumonia [21]. She also manifested with seizures and mood disorders. A brain edema and the presence of anti-NMDA receptor antibodies were causative alterations. Steroids and IVIG determined a good prognosis. Two girls with learning disabilities worsened both intellectually/psychically and with neurological deficit. The 19-year-old described by Kasturiachi et al. [57] had progressive encephalopathy, epileptic EEG alteration without seizures, and multiple MR brain lesions. This case was complicated due to coexisting thrombotic thrombocytopenic purpura and other serologic poliautoimmunity; however, her prognosis was good after therapies with plasmapheresis, steroids, and rituximab.
A controversial case of a 16-year-old girl have been described by Gaughan et al. [48]. She had a history of mild learning needs; she complained of sore throat, fever, and psychotic behavior. After five days of IVIG therapy, the condition worsened, presenting mutism, little to no motor activity, incontinence, and being fed via nasogastric tube. Chest X-ray, MRI, and CSF were unremarkable. Two weeks later, following IVIG therapy, anti-GAD antibodies and extractable nuclear antigen appeared in the serum, transitorily. Repeated EEG showed slow activity. The girl improved 4 weeks after initial presentation and was discharged on day 48. The follow-up visit after six months revealed that she is still experiencing memory difficulties and fatigue.
Another 18-year-old girl, whose case has been described by Ayatollahi et al. [23], had fever, fatigue, malaise, and loss of appetite for a week, which progressed to drowsiness and confusion, and finally urinary retention and repeated generalized tonic-clonic seizure. Both CT brain scans and MRI were normal. In the following days, she had new seizures and fluctuating mood alterations, which were resistant to several therapies. Later on, a new MRI showed altered signals in the claustrum, external capsules, and some areas of the adjacent anterior insular cortex. Thereafter, therapy with intravenous methylprednisolone was started, and after three days, she was discharged in good condition. At follow-up, after one month, MRI showed nearly complete resolution of the previously described signal alterations. Seizures did not recur, although the memory deficit persisted. The last young girl mainly had retinal involvement, with subsequent encephalitis of the temporal lobes. Apart from fever, body pain, headache, and nausea with vomiting, the only neurologic symptom was drowsiness, and the prognosis was good [77].
3.3.3. Adults with COVID-19
Initial Presentation with Neurological and Respiratory Symptoms
Most cases manifested respiratory symptoms as an early manifestation of SARS-CoV-2 infection. Six cases also manifested neurological symptoms from the beginning of their clinical history [26,27,42,49,69,93]. Several cases developed neurological impairment following respiratory symptoms. The latency between the onset of the infection with respiratory manifestations and the onset of neurological complications varied between 3 days and 41 days [12,24,27,28,30,32,34,36,37,43,45,51,56,58,64,65,70,76,80,81,82,83,85,86,89,90,91,93,94]. Overall, 13 patients were intubated and mechanically ventilated due to respiratory distress; in these cases, the detection of neurological impairment happened when sedation was interrupted, with latency ranging between 4 and 38 days depending on the case [27,32,34,76,80,82,85,93]. In patients whose respiratory distress was less evident, neurological manifestation appeared after a few days in most cases [27,28,30,37,45,56,58,65,89,91,93,94]. In some cases, the latency ranged from over two weeks to 60 days [12,24,27,64,90]. Three patients began their illness with symptoms other than respiratory and developed neurological impairments between 5 and 17 days after the onset of the initial symptoms [22,47,50]. Their clinical presentations consisted of fatigue and malaise for two weeks in one case [47]; progressive diffuse arthralgia and sore throat, followed by fever [50]; and gastrointestinal manifestations in the third case [22]. An onset with neurological presentation was described in a number of reports [17,25,30,33,38,39,41,44,52,53,54,56,59,60,61,68,71,72,73,74,75,78,79,92]. Respiratory complications came later and were symptomatic in three cases [61,75,78]. Even though several patients did not have subjective respiratory difficulties or changes in arterial oxygen saturation, most of them had lung alterations on thorax CT and/or chest X-ray, which were typical of COVID-19 interstitial pneumonia, primarily as ground glass opacities and areas of parenchymal consolidation.
Neurological and Psychiatric Manifestations
Sleep disturbances, progressive altered mental status, psychiatric behavioural symptoms, and hallucination have been described by some authors [22,26,37,47,51,52,56,58,63,72,73,75,78,81,86,89,94]; most of these cases are associated with EEG representations [22,26,37,63,74,75], and some with brain neuroimaging alteration [51,52,56,78,81,94]. Neurological deficit referred to language deficit, cognitive deficits, akinetic syndrome with mutism, signs of cortical impairment, seizures, stroke, cerebellar signs, chorea, paralysis, coma, and signs of brain death [17,25,33,36,37,38,39,47,49,51,52,53,58,59,60,64,65,71,72,74,76,78,79,89,92].
Few cases presented with severe epileptic manifestations. Epileptic manifestations occurred from the first phase of infection, evolving into status epilepticus in some patients. Two of these patients died. The first developed intracranial hypertension with diffuse cerebral edema, and cerebellar herniation occurred [79]. The second case manifested a tonic-clonic seizure, followed by cardiac arrest, and was successfully resuscitated, intubated, and transferred to the intensive care unit. In this case, CT and MRI also showed brain edema and cerebellar herniation [45]. A third patient developed status epilepticus that required the patient to be intubated and mechanically ventilated. Chest CT showed interstitial pneumonia. He had an opening high pressure when lumbar puncture was performed, and SARS-CoV-2 RNA was detected in his CSF, while MRI revealed ventriculitis and encephalitis, mainly in the right mesial lobe and hippocampus [17]. The last case reported early onset of drug-refractory epilepsy; MRI and spectroscopy were suggestive for high-grade glioma; after lobectomy, histopathologic diagnosis was of encephalitis [41]. A late-onset status epilepticus with intracranial hypertension ion caused the death of another patient [12]. In this case, the disease had a two-phase evolution. He had a first respiratory phase, with recovery in 2–3 weeks. After 41 days, the fever reappeared, together with severe headache and vomiting. A brain CT scan and MRI showed unilateral hemispheric vasogenic edema with shift of the medial cerebral structures.
Particular Case of COVID-Linked Encephalitis
Some cases were marked by identification of specific neural antibodies. Three patients suffered from NMDA encephalitis [68,73,88]. Clinical manifestations were psychotic symptoms and seizures only. All of them improved with immuno-therapies, including IV methylprednisolone, IVIG, therapeutic plasma exchange. Only in the case described by Valadez-Calderon et al. [88], in which anti-NMDAR and anti-GAD65 antibodies were co-expressed, were EEG (slow rhythm) and MRI (MR signal alteration anterior cingulated cortex and temporal lobes bilaterally) both altered.
One patient developed an MOG antibody-associated encephalitis. He had minor clinical manifestations, but mulptiple MRI signal alterations: T2 and FLAIR, mainly with cortical distribution. This patient also improved after IV steroids [40]. Bickerstaff brainstem encephalitis involved three patients: two women and a man. Their main manifestation was truncal and cerebellar disfunction. In the case with anti-GD1 IgG antibodies [25], MRI images were altered (alterations in the caudal vermis and right flocculus of the cerebellum, and contrast enhancement in the floor of the IV ventricle). Improvement and resolution of symptoms were obtained with IV methylprednisolone. In the case with anti-gangliosides (GQ1b, GT1a, and GM1/GT1a), both EEG and MRI were normal. The patient improved after therapy with IV steroids, IVIG, but mainly after plasma exchange. The third case had serum onconeural antibodies against amphiphysin, and MR of brainstem encephalitis; this man also improved after steroidal therapy [59].
Another case of autoimmune encephalitis was described by Grimaldi et al. [50]. This man presented with progressive diffuse arthralgia and sore throat and interstitial pneumonia, and after 17 days, progressive action tremor, cerebellar syndrome, and diffuse myoclonus. EEG showed diffuse slowing, and MRI was normal, but PET with F-FDG showed putaminal, cerebellum, and diffuse cortical hypometabolism, confirmed by whole-brain voxel-based SPM quantification. Antibodies against the nuclei of Purkinje cell, striatal neurons, and hippocampal neurons were found in both serum and CSF. The patient was then treated with IVIG without clinical improvement. He improved after therapy with IV methylprednisolone and clonazepam.
Other particular cases of encephalitis were described. Three case reports described limbic encephalitis [43,76,92]. All of these patients had severe pneumonia, seizures or consciousness alteration, and anti-typical MRI alterations. All of them improved after having been treated with steroids, only in one case with IVIG added. A 67-year-old woman had an acute disseminated encephalitis (ADEM), with drowsiness; she had bilateral pneumonia and respiratory distress, was treated with IV steroids and IVIG, and unfortunately died after 4 weeks [44]. Two cases of mild encephalitis with reversible splenial lesion syndrome (RESLES) were described [42,54]. Both of them had interstitial pneumonia. The first patient [42] was afebrile, and presented a short loss of consciousness, cough, and headache. CSF and brain CT scan were normal, so he was discharged from the hospital. Nine days later, he manifested persistent headache, vertigo and intermittent disturbance of consciousness, myalgia, tiredness and persistent bibasilar rales, psychomotor slowing, and vestibular syndrome. MRI documented a signal alteration on the splenium of the corpus callosum. He was treated with analgesics and antibiotics. The patient improved gradually over the next few days. At one-month follow-up, lung complications were reduced, and MRI normalized. The second patient [54] showed marked dysmetria and mild ataxic gate. MRI documented abnormal alteration of the splenium of the corpus callosum, with a suspicion of RESLES. After a few hours, they manifested fever and hypoxemia. Treated with antiviral, antibiotics, and steroids, they neurologically improved but died at day 12 due to respiratory failure. Seven cases had AHNE [49,69,70,90]. This is a severe condition with poor prognosis. Neurological manifestations appeared after several days but were abrupt. Only four cases had pulmonary compromission [69,70,90]. All seven adults with AHNE died within 3 weeks.
Managing Severe Cases
Severe respiratory impairment was the main feature of some cases and required intubation. Benameur et al. [27] described three cases that manifested neurological complications after sedation was discontinued. In one case, cerebral edema with intracranial hypertensive signs was detected with MRI and CSF examination, consistent with encephalomyelitis and superimposed hypoxic ischemia. This woman died when life support was withdrawn. In the second case, profound encephalopathy with multifocal myoclonus was detected, and the patient was neurologically comatose. At lumbar puncture, there was a high opening pressure, suggesting intracranial hypertension. MRI disclosed a signal alteration at the splenium of the corpus callosum. The third case also had a profound encephalopathy without brainstem reflexes. He was treated with hydroxychloroquine, which caused myoclonus that disappeared at the cessation of this therapy. MRI showed signal alteration involving the temporal lobe. In this last case, the IgG anti-S1 receptor-bindle domain was present in serum, and a mild IgM level for SARS-CoV-2 S1 was found in CSF. In these cases, inflammatory molecules have been dosed in CSF, and in one case (the third), IL-8, IL-10, IP-10, and TNFα were increased. In the case series by Cao et al. [32], all five patients were intubated due to acute respiratory distress syndrome. When sedation was withdrawn, one patient was comatose, and the other four were in an unresponsive wakefulness syndrome (vegetative state). Four of them had high IL-6 level in serum, and one patient also had a slight increase of IL-6 in CSF. MRI showed several lesions in supratentorial deep white matter, in the pons, with several multiple small haemorrhagic lesions. Three out of five patients rapidly improved after therapy with intravenous steroids and therapeutic plasma exchange; one patient died. In addition, in the case by Svedung Wettervik et al. [85], the patient was comatose at the wake-up test after intubation. She had brain edema, and microhemorrhages with basal ganglia involvement, in line with acute hemorrhagic leukoencephalitis. An external ventricular drain was positioned, and CSF had fluctuating pressures, with a large amount of white and red cells. IL-6 was high in both plasma and CSF. This patient underwent therapeutic plasma exchange, after which she improved both clinically and in neuroimaging. Chalil et al.’s case developed respiratory distress two weeks from onset [34]. She was intubated, and severe lung complications were observed in chest CT. Therapy was hydroxychloroquine and tocilizumab. Due to the detection of very high D-dimer and ferritin levels, increased CRP, and severe hypoxemia, full anticoagulation started. Extensive bilateral parieto-occipital intraparenchymal hemorrage were observed with intraventricular extension and acute hydrocephalus. On day 15, brainstem reflexes were absent. Heparin was stopped, and external ventricular drain positioned. The authors interpreted this case as a post-infectious acute necrotizing hemorrhagic encephalopathy, due to thalamic involvement, suggested as typical for acute necrotizing hemorragic encephalopathy [34]. The patient was finally extubated, but severe neurologic deficit persisted.
The most prescribed drugs were antibiotics and antiviral agents. Quite often, hydroxychloroquine and high-dose methylprednisolone have been used. Until 2021, therapeutical plasmapheresis and immunosuppressive drugs were rarely prescribed. After the first period of the COVID-19 pandemic, immunomodulating agents, in particular IVIG and tocilizumab, plasmapheresis, and convalescent’s serum, have been used more often, with good response [21,51,59,60,70,81,83,88], except for the most severe cases, like in ANHE.
3.4. Quality Assessment
Among the included studies in this systematic review, based on the JBI critical appraisal tools assessing case reports and case series, 87.3% of the studies were of high quality, followed by 11.4% moderate- and 1.3% low-quality studies (Tables S3 and S4).
4. Discussion
In this systematic review, we comprehensively investigated the clinical and laboratory features, as well as the outcomes of COVID-19 patients with encephalitis. COVID-19 encephalitis can present before, together, or after respiratory manifestation of the illness. The most frequent neurological manifestations of encephalitis are seizure, confusion, headache, disorientation, status epilepticus, and altered mental status, and the degree of the condition is dependent mostly upon the severity of COVID-19 infection, entity of respiratory damage, and entity of neuronal damage and its site [91,95]. Severity of respiratory impairment and neuronal damage are the factors that seem to determine the worst prognosis. The knowledge of possible para- or post-infectious SARS-CoV-2 encephalitis, and of possible inflammatory or immune mechanisms of neuronal damage, can drive research for better therapies to improve outcomes [27,96].
In most cases, preforming a lumbar puncture can suggest the presence of encephalitic involvement. Brain CT scan in an emergency can be useful only in those cases that manifest with very acute neurological compromission, and can reveal brain edema, endocranial hypertension, massive necrosis, and or hemorrhagic lesions. A rapid intervention, acting to reduce intracranial hypertension, can help give the patient a chance to survive and receive the proper therapeutical efforts [97,98]. In those cases with psychiatric or epileptic presentation, CT scan can be unremarkable. MRI is also useful to detect small lesions, which can sometimes be transitory. In some cases, the only way to reveal neuronal disfunction is to use a neurological functional test, such as PET [99,100]. EEG is mostly aspecific, with slow background activity. Sometime EEG can also reveal epileptic activity of the non-convulsive type [101].
In the case of COVID-19, confirmed or suspected, it is important to consider possible neurological involvement. The clinician should consider any behavioral changes or alterations of consciousness. These can be due to hypoxic damage, hematochemical alteration, or circulatory problems, or they can be COVID-19-related. However, it can be a manifestation of neuronal involvement. The precocity of a specific intervention is essential to preserve neurons, and in case of any suspicion, proper tests and exams should be performed. Sometimes, neurological damage progresses slowly or tardively, and neuro-clinical symptoms can appear several day or weeks after the onset of the first symptoms. In these cases, an autoimmune mechanism of damage can be supposed, and this should drive the therapeutical approach [102,103].
Although the exact pathogenesis of the SARS-CoV-2 virus’s access to the CNS and triggering of various neurological manifestations is still under investigation, researchers have suggested a few mechanisms. SARS-CoV-2 can exert neurological manifestations by two main mechanisms. The first mechanism is the direct CNS infection, where SARS-CoV-2 gain access to the CNS from the peripheral nervous system, as RNA of the SARS-CoV-2 virus has been detected in the CSF of the COVID-19 patients. As in mature human olfactory nerves, ACE2 has not been reported, and ACE2 is most likely present at low levels in neurons [104,105]. SARS-CoV-2 possibly uses other facilitator(s) to access the CNS. One of the plausible routes for SARS-CoV-2 entry in the CNS could be that upon nasal infection, SARS-CoV-2 enters the CNS through the olfactory bulb, facilitated by neuropilin-1 (retrograde axonal transport), the only part of the CNS not protected by dura, causing inflammation and demyelination [106,107,108]. The second mechanism involves the disruption of the blood–brain barrier via SARS-CoV-2-ACE2 receptor-mediated vascular damage following viraemia. In this inflammation-mediated autoimmune-associated mechanism, both innate and adaptive immune systems play a role via upregulated inflammatory mediators exerting cytokine storm syndrome, which may result in acute hemorrhagic necrotizing encephalitis via perivascular demyelination [109,110,111].
Neurological symptoms seem to be the initial sign of illness in certain cases of COVID-19. A few cases, however, had already developed antibodies against SARS-CoV-2, suggesting a previous asymptomatic or pauci-symptomatic COVID-19 disease. That is why it is important, in case of neurological manifestation, to perform both the nasopharyngeal swab for SARS-CoV-2 and the serum test for antibodies against the virus. It is speculated that SARS-CoV-2-mediated encephalitis may present inflammatory injury, edema, and alterations in consciousness in patients with COVID-19 [91,96]. Although viral encephalitis confirmation requires virus isolation in the CSF, due to transient dissemination of SARS-CoV-2 virus and low CSF titre, it becomes extremely difficult to confirm viral encephalitis in COVID-19 [91]. For the management of encephalitis in COVID-19, we observed that IVIG therapy, plasma exchange, and corticosteroids may be useful in the treatment of COVID-19-related encephalitis.
There are some notable strengths of our study. First, this is the first systematic analysis based on the published case reports and series that was represented in a comprehensive way. Second, the search strategy was strong, as we used multiple databases with robust search strategies. Third, from our quality assessment, a majority of the studies were of high quality; therefore, the outcome of this systematic review is reliable, and it is based on high-methodological-quality studies. Nevertheless, there are some notable limitations. First, due to the study pattern, we could not analyze the data through a meta-analysis approach. Second, due to exploring the clinical, laboratory, and neuro-imaging data in a comprehensive way, we only included case reports and case series, and we did not consider any observational studies. Third, we could not retrieve our data of interest from all of the studies, which leads to incomplete data for some of the cases. However, since there is presently very little published information on encephalitis in COVID-19 patients, our analysis provided a strong early insight into the clinical, laboratory, and neuro-imaging characteristics of encephalitis in COVID-19 patients.
In the future, larger sample sizes would aid in determining if the neurological aspects, particularly the relationship with encephalitis, are purely coincidental, or whether there are phenotypes and associations particular to SARS-CoV-2.
5. Conclusions
COVID-19 patients with acute characteristic neurological signs such as seizure, confusion, headache, disorientation, status epilepticus, and altered mental status should be evaluated for viral encephalitis immediately, given the present condition of the COVID-19 pandemic. Patients with COVID-19 who are suspected of having encephalitis should have further testing, such as a brain MRI scan, long-term EEG monitoring, and lumbar puncture. The lack of a characteristic CSF profile of viral meningitis/encephalitis, as well as the negative PCR for SARS-CoV-2 virus in CSF, makes the diagnosis of encephalitis caused by the SARS-CoV-2 virus less evident, pointing to a possible autoimmune neuropathogenesis. In the post-acute phase of SARS-CoV-2 infection, it is critical to evaluate the neurological consequences. In this phase, encephalitis should be diagnosed only if there are clinical signs of brain inflammation, such as pleocytosis in the CSF, imaging alterations, focal seizures, or histological alterations. Even if the virus is found in the CSF, encephalitis should not be diagnosed until brain inflammation is present.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells11162575/s1, Table S1: Search strategies, Table S2: Laboratory features of encephalitis patients with SARS-Cov-2 infection, Table S3: Quality assessment of the included case reports, Table S4: Quality assessment of the included case series.
Author Contributions
Conceptualization, M.A.I. and C.C.; methodology, M.A.I., S.S.A., and S.K.; validation, C.C., M.A.I., S.S.A., and F.R.; formal analysis, C.C. and M.A.I.; investigation, M.A.I., C.C., S.S.A., and S.K.; resources, M.A.I., C.C., and F.R.; data curation, C.C., M.A.I., F.R., and S.S.A.; writing—original draft preparation, C.C. and M.A.I. writing—review and editing, M.A.I., C.C., M.A.K., and F.R.; project administration, M.A.I. and F.R.; funding acquisition, M.A.I. and F.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available within the article and Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization WHO COVID-19 Dashboard. 2022. [(accessed on 9 August 2022)]. Available online: https://covid19.who.int.
- 2.Zhou Z., Kang H., Li S., Zhao X. Understanding the neurotropic characteristics of SARS-CoV-2: From neurological manifestations of COVID-19 to potential neurotropic mechanisms. J. Neurol. 2020;267:2179–2184. doi: 10.1007/s00415-020-09929-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 2020;92:552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Islam M.A., Kundu S., Alam S.S., Hossan T., Kamal M.A., Hassan R. Prevalence and characteristics of fever in adult and paediatric patients with coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of 17515 patients. PLoS ONE. 2021;16:e0249788. doi: 10.1371/journal.pone.0249788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yusuf F., Fahriani M., Mamada S.S., Frediansyah A., Abubakar A., Maghfirah D., Fajar J.K., Maliga H.A., Ilmawan M., Bin Emran T., et al. Global prevalence of prolonged gastrointestinal symptoms in COVID-19 survivors and potential pathogenesis: A systematic review and meta-analysis. F1000Research. 2021;10:301. doi: 10.12688/f1000research.52216.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cares-Marambio K., Montenegro-Jiménez Y., Torres-Castro R., Vera-Uribe R., Torralba Y., Alsina-Restoy X., Vasconcello-Castillo L., Vilaró J. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Chronic Respir. Dis. 2021;18:1–12. doi: 10.1177/14799731211002240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saniasiaya J., Islam A., Abdullah B. Prevalence and Characteristics of Taste Disorders in Cases of COVID-19: A Meta-analysis of 29,349 Patients. Otolaryngol. Neck Surg. 2020;165:33–42. doi: 10.1177/0194599820981018. [DOI] [PubMed] [Google Scholar]
- 8.Saniasiaya J., Islam A., Abdullah B. Prevalence of Olfactory Dysfunction in Coronavirus Disease 2019 (COVID-19): A Meta-analysis of 27,492 Patients. Laryngoscope. 2020;131:865–878. doi: 10.1002/lary.29286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Islam A., Alam S.S., Kundu S., Hossan T., Kamal M.A., Cavestro C. Prevalence of Headache in Patients with Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of 14,275 Patients. Front. Neurol. 2020;11:562634. doi: 10.3389/fneur.2020.562634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Natarajan S., Ganesh R., Palaniappan N., Kannan L. SARS-CoV-2 Encephalitis in an Adolescent Girl. Indian Pediatr. 2020;57:1186–1187. doi: 10.1007/s13312-020-2080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McAbee G.N., Brosgol Y., Pavlakis S., Agha R., Gaffoor M. Encephalitis Associated with COVID-19 Infection in an 11-Year-Old Child. Pediatr. Neurol. 2020;109:94. doi: 10.1016/j.pediatrneurol.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zanin L., Saraceno G., Renisi G., Signorini L., Battaglia L., Ferrara M., Rasulo F.A., Panciani P.P., Fontanella M.M. Delayed onset of fatal encephalitis in a COVID-19 positive patient. Int. J. Neurosci. 2021:1–4. doi: 10.1080/00207454.2021.1886095. [DOI] [PubMed] [Google Scholar]
- 13.Espíndola O.M., Brandão C.O., Gomes Y.C.P., Siqueira M., Soares C.N., Lima M.A.S.D., Leite A.C.C.B., Torezani G., Araujo A.Q.C., Silva M.T.T. Cerebrospinal fluid findings in neurological diseases associated with COVID-19 and insights into mechanisms of disease development. Int. J. Infect. Dis. 2020;102:155–162. doi: 10.1016/j.ijid.2020.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bodnar B., Patel K., Ho W., Luo J.J., Hu W. Cellular mechanisms underlying neurological/neuropsychiatric manifestations of COVID-19. J. Med. Virol. 2020;93:1983–1998. doi: 10.1002/jmv.26720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venkatesan A., Geocadin R.G. Diagnosis and management of acute encephalitis: A practical approach. Neurol. Clin. Pract. 2014;4:206–215. doi: 10.1212/CPJ.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ellul M., Solomon T. Acute encephalitis–diagnosis and management. Clin. Med. 2018;18:155. doi: 10.7861/clinmedicine.18-2-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J., Ueno M., Sakata H., Kondo K., Myose N., et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int. J. Infect. Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abildúa A., Atienza S., Monteiro G., Aguirre M., Aguayo L., Álvarez E., García-Azorín D., Montesinos I., Lezama L., Pérez M. Encephalopathy and encephalitis during acute SARS-CoV-2 infection. Spanish Society of Neurology COVID-19 Registry. Neurologia. 2021;36:127–134. doi: 10.1016/j.nrl.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page M.J., E McKenzie J., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Moher D. Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J. Clin. Epidemio. 2021;134:103–112. doi: 10.1016/j.jclinepi.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Ahsan N., Jafarpour S., Santoro J.D. Myelin oligodendrocyte glycoprotein antibody encephalitis following severe acute respiratory syndrome coronavirus 2 in a pediatric patient. Clin. Exp. Pediatr. 2021;64:310–312. doi: 10.3345/cep.2020.01963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allahyari F., Hosseinzadeh R., Nejad J.H., Heiat M., Ranjbar R. A case report of simultaneous autoimmune and COVID-19 encephalitis. J. Neurovirol. 2021;27:504–506. doi: 10.1007/s13365-021-00978-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrea M., Christian M., Lorenzo M., Francesco D., Walter A., Marco M., Andreina B., Maria G.A., Paolo G., Daniela D.G., et al. Unusual Presentation of COVID-19: Encephalitis and Syndrome of Inappropriate Anti-Diuretic Hormone Secretion. Int. J. Clin. Med. 2020;11:559–564. doi: 10.4236/ijcm.2020.1110048. [DOI] [Google Scholar]
- 23.Ayatollahi P., Tarazi A., Wennberg R. Possible autoimmune encephalitis with claustrum sign in case of acute SARS-CoV-2 infection. Can. J. Neurol. Sci. 2021;48:430–432. doi: 10.1017/cjn.2020.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ayuningtyas T., Natadidjaja R.I., Octaviani C., Sahli F., Adlani H. Confirmed severe acute respiratory syndrome coronavirus 2 encephalitis in cerebrospinal fluid: A case report. J. Med Case Rep. 2022;16:1–4. doi: 10.1186/s13256-022-03376-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayuso L.L., Rubio P.T., Rosário R.F.B.D., Arroyo M.L.G., Sierra-Hidalgo F. Bickerstaff encephalitis after COVID-19. J. Neurol. 2020;268:2035–2037. doi: 10.1007/s00415-020-10201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Babar A., Lewandowski U., Capin I., Khariton M., Venkataraman A., Okolo N., Sharma D. SARS-CoV-2 encephalitis in a 20-year old healthy female. Pediatr. Infect. Dis. J. 2020;39:320–321. doi: 10.1097/INF.0000000000002855. [DOI] [PubMed] [Google Scholar]
- 27.Benameur K., Agarwal A., Auld S.C., Butters M.P., Webster A.S., Ozturk T., Howell J.C., Bassit L.C., Velasquez A., Schinazi R.F., et al. Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020. Emerg. Infect. Dis. 2020;26:2016–2021. doi: 10.3201/eid2609.202122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard-Valnet R., Pizzarotti B., Anichini A., Demars Y., Russo E., Schmidhauser M., Cerutti-Sola J., Rossetti A.O., Du Pasquier R. Two patients with acute meningoencephalitis concomitant with SARS-CoV-2 infection. Eur. J. Neurol. 2020;27:43–44. doi: 10.1111/ene.14298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhavsar S.M., Agarwal S., Lewis R., Ganta A., Roshchina Y.S., Clouser K.N., Baer A.Z., Gliksman F., Piwoz J.A. COVID-19 Infection Associated With Encephalitis in an Adolescent. Neurol. Clin. Pract. 2020;11:e189–e192. doi: 10.1212/CPJ.0000000000000911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bodro M., Compta Y., Llansó L., Esteller D., Doncel-Moriano A., Mesa A., Rodríguez A., Sarto J., Martínez-Hernandez E., Vlagea A. Increased CSF levels of IL-1β, IL-6, and ACE in SARS-CoV-2–associated encephalitis. Neurology. 2020;7:1–6. doi: 10.1212/NXI.0000000000000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burr T., Barton C., Doll E., Lakhotia A., Sweeney M. N-Methyl-d-Aspartate Receptor Encephalitis Associated With COVID-19 Infection in a Toddler. Pediatr. Neurol. 2020;114:75–76. doi: 10.1016/j.pediatrneurol.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cao A., Rohaut B., Le Guennec L., Saheb S., Marois C., Altmayer V., Carpentier V.T., Nemlaghi S., Soulie M., Morlon Q., et al. Severe COVID-19-related encephalitis can respond to immunotherapy. Brain. 2020;143:e102. doi: 10.1093/brain/awaa337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Casez O., Willaume G., Grand S., Nemoz B., Lupo J., Kahane P., Brion J.-P. Teaching NeuroImages: SARS-CoV-2–Related Encephalitis: MRI Pattern of Olfactory Tract Involvement. Neurology. 2021;96:645–646. doi: 10.1212/WNL.0000000000011150. [DOI] [PubMed] [Google Scholar]
- 34.Chalil A., Baker C.S., Johnston R.B., Just C., Debicki D.B., Mayich M.S., Bosma K.J., Steven D.A. Acute Hemorrhagic Encephalitis Related to COVID-19. Neurol. Clin. Pract. 2020;11:e147–e151. doi: 10.1212/CPJ.0000000000000900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheraghali F., Tahamtan A., Hosseini S.A., Gharib M.H., Moradi A., Razavi Nikoo H., Tabarraei A. Case report: Detection of SARS-CoV-2 from cerebrospinal fluid in a 34-month-old child with encephalitis. Front. Pediatrics. 2021;9:565778. doi: 10.3389/fped.2021.565778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dahshan A., Abdellatef A.A. Autoimmune encephalitis as a complication of COVID-19 infection: A case report. Egypt. J. Intern. Med. 2022;34:1–3. doi: 10.1186/s43162-022-00119-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dono F., Carrarini C., Russo M., De Angelis M.V., Anzellotti F., Onofrj M., Bonanni L. New-onset refractory status epilepticus (NORSE) in post SARS-CoV-2 autoimmune encephalitis: A case report. Neurol. Sci. 2021;42:35–38. doi: 10.1007/s10072-020-04846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duong L., Xu P., Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020. Brain Behav. Immun. 2020;87:33. doi: 10.1016/j.bbi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang Y.H., Jiang D., Huang J.T. SARS-CoV-2 Detected in Cerebrospinal Fluid by PCR in a Case of COVID-19 Encephalitis. Brain Behav. Immun. 2020;87:149. doi: 10.1016/j.bbi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Durovic E., Bien C., Bien C.G., Isenmann S. MOG antibody-associated encephalitis secondary to Covid-19: Case report. BMC Neurol. 2021;21:1–5. doi: 10.1186/s12883-021-02449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Efe I.E., Aydin O.U., Alabulut A., Çelik O., Aydin K. COVID-19−Associated Encephalitis Mimicking Glial Tumor. World Neurosurg. 2020;140:46–48. doi: 10.1016/j.wneu.2020.05.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El Aoud S., Sorial D., Selmaoui A., Menif I., Lazard M., Hocine M.S., Thomas L. A first case of Mild Encephalitis with Reversible Splenial Lesion (MERS) as a presenting feature of SARS-CoV-2. Rev. Neurol. 2021;177:139–141. doi: 10.1016/j.neurol.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Elmouhib A., Benramdane H., Ahsayen F.Z., El Haddad I.A., El Ghalet A., Laaribi I., Bkiyar H., Nasri S., Skiker I., Housni B. A case of limbic encephalitis associated with severely COVID-19 infection. Ann. Med. Surg. 2022;74:103274. doi: 10.1016/j.amsu.2022.103274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Esmaeili S., Abbasi M.H., Mojtahed M., Emamikhah M., Makiani M.J., Nazarian H., Mirzaasgari Z. Acute disseminated encephalitis (ADEM) as the first presentation of COVID-19; a case report. Ann. Med. Surg. 2022;77:103511. doi: 10.1016/j.amsu.2022.103511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Etemadifar M., Salari M., Murgai A.A., Hajiahmadi S. Fulminant encephalitis as a sole manifestation of COVID-19. Neurol. Sci. 2020;41:3027–3029. doi: 10.1007/s10072-020-04712-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ferdosian F., Mohsenolhoseini Z., Fallah R. Encephalitis Associated With COVID-19 in A 7-year-old Boy: A Case Report. Case Rep. Clin. Pract. 2022;6:246–250. doi: 10.18502/crcp.v6i6.9171. [DOI] [Google Scholar]
- 47.Freire-Álvarez E., Guillén L., Lambert K., Baidez A., García-Quesada M., Andreo M., Alom J., Masiá M., Gutiérrez F. COVID-19-associated encephalitis successfully treated with combination therapy. Clin. Infect. Pract. 2020;7–8:100053. doi: 10.1016/j.clinpr.2020.100053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gaughan M., Connolly S., O’Riordan S., Tubridy N., McGuigan C., Kinsella J.A. Pediatric Parainfectious Encephalitis Associated With COVID-19. Neurology. 2021;96:541–544. doi: 10.1212/WNL.0000000000011476. [DOI] [PubMed] [Google Scholar]
- 49.Ghosh R., Dubey S., Finsterer J., Chatterjee S., Ray B.K. SARS-CoV-2-Associated Acute Hemorrhagic, Necrotizing Encephalitis (AHNE) Presenting with Cognitive Impairment in a 44-Year-Old Woman without Comorbidities: A Case Report. Am. J. Case Rep. 2020;21:e925641. doi: 10.12659/AJCR.925641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grimaldi S., Lagarde S., Harlé J.-R., Boucraut J., Guedj E. Autoimmune encephalitis concomitant with SARS-CoV-2 infection: Insight from 18F-FDG PET imaging and neuronal autoantibodies. J. Nucl. Med. 2020;61:1726–1729. doi: 10.2967/jnumed.120.249292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gunawardhana C., Nanayakkara G., Gamage D., Withanage I., Bandara M., Siriwimala C., Senaratne N., Chang T. Delayed presentation of postinfectious encephalitis associated with SARS-CoV-2 infection: A case report. Neurol. Sci. 2021;42:3527–3530. doi: 10.1007/s10072-021-05395-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haider A., Siddiqa A., Ali N., Dhallu M. COVID-19 and the Brain: Acute Encephalitis as a Clinical Manifestation. Cureus. 2020;12:e10784. doi: 10.7759/cureus.10784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hassan M., Syed F., Ali L., Rajput H.M., Faisal F., Shahzad W., Badshah M. Chorea as a presentation of SARS-CoV-2 encephalitis: A clinical case report. J. Mov. Disord. 2021;14:245. doi: 10.14802/jmd.20098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hayashi M., Sahashi Y., Baba Y., Okura H., Shimohata T. COVID-19-associated mild encephalitis/encephalopathy with a reversible splenial lesion. J. Neurol. Sci. 2020;415:116941. doi: 10.1016/j.jns.2020.116941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kahwagi J., Diagne R., Fall M., Basse A., Ndiaye M., Diop A. Post infectious encephalitis at Covid19: About one pediatric observation and review of the literature. Rev. Neurol. 2020;177:132–134. doi: 10.1016/j.neurol.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kamal Y.M., Abdelmajid Y., Al Madani A.A.R. Cerebrospinal fluid confirmed COVID-19-associated encephalitis treated successfully. BMJ Case Rep. 2020;13:e237378. doi: 10.1136/bcr-2020-237378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kasturiarachi B.M., Alsbrook D.L., Crook J., Shah N. An Immunologic Storm: A Case of Encephalitis and Thrombotic Thrombocytopenic Purpura With Underlying Likely Sjogren’s Syndrome Induced by a COVID-19 Immune Response. Neurohospitalist. 2022;12:529–535. doi: 10.1177/19418744221079447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Khoo A., McLoughlin B., Cheema S., Weil R.S., Lambert C., Manji H., Zandi M.S., Morrow J.M. Postinfectious brainstem encephalitis associated with SARS-CoV-2. J. Neurol. Neurosurg. Psychiatry. 2020;91:1013–1014. doi: 10.1136/jnnp-2020-323816. [DOI] [PubMed] [Google Scholar]
- 59.Kimura M., Hashiguchi S., Tanaka K., Hagiwara M., Takahashi K., Miyaji Y., Joki H., Doi H., Koga M., Takeuchi H., et al. Case Report: Takotsubo Cardiomyopathy in Bickerstaff Brainstem Encephalitis Triggered by COVID-19. Front. Neurol. 2021;12:822247. doi: 10.3389/fneur.2021.822247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Koh S., Kim Y.S., Kim M.H., Choi Y.H., Choi J.Y., Kim T.-J. Encephalitis with status epilepticus and stroke as complications of non-severe COVID-19 in a young female patient: A case report. BMC Neurol. 2022;22:1–5. doi: 10.1186/s12883-022-02782-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kumar N., Kumar S., Kumar A., Pati B.K., Kumar A., Singh C., Sarfraz A. Acute necrotizing encephalitis as a probable association of covid-19. Indian J. Crit. Care. 2020;24:991–994. doi: 10.5005/jp-journals-10071-23636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kumar V.H., Natarajan C., Siddharth M., Shivabalan S., Gopinath C., Shyam A., Jean M. Post covid pneumonia pulmonary fibrosis and encephalitis in a term neonate with prenatal exposure to SARS CoV-2: A case report. IDCases. 2022;27:e01414. doi: 10.1016/j.idcr.2022.e01414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marques L.M., Marques S.R., Costa O., Freitas E., Machado Á. COVID-19-Associated Encephalitis: Two Case Reports. Cureus. 2022;14:e23243. doi: 10.7759/cureus.23243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mekheal E., Mekheal M., Roman S., Mikhael D., Mekheal N., Manickam R. A Case Report of Autoimmune Encephalitis: Could Post-COVID-19 Autoimmunity Become a Lethal Health Issue? Cureus. 2022;14:e25910. doi: 10.7759/cureus.25910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Meshref M., Hewila I.M., Mageed S.A., Morra M.E. COVID-19 Associated With Encephalitis: Case Report and Review of Literature. Neurologist. 2021;26:268. doi: 10.1097/NRL.0000000000000347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mierzewska-Schmidt M., Baranowski A., Szymanska K., Ciaston M., Kuchar E., PLoSki R., Kosinska J., Pagowska-Klimek I. The case of fatal acute hemorrhagic necrotizing encephalitis in a two-month-old boy with Covid-19. Int. J. Infect. Dis. 2021;116:151–153. doi: 10.1016/j.ijid.2021.12.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Miqdad M.A., Enabi S., Alshurem M., Al-Musawi T., Alamri A. COVID-19–Induced Encephalitis: A Case Report of a Rare Presentation With a Prolonged Electroencephalogram. Cureus. 2021;13:e14476. doi: 10.7759/cureus.14476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Monti G., Giovannini G., Marudi A., Bedin R., Melegari A., Simone A.M., Santangelo M., Pignatti A., Bertellini E., Trenti T., et al. Anti-NMDA receptor encephalitis presenting as new onset refractory status epilepticus in COVID-19. Seizure. 2020;81:18–20. doi: 10.1016/j.seizure.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Morvan A.-C., Kerambrun H. Fatal necrotizing encephalitis associated with COVID-19: A case report. Neurology. 2021;11:214–215. doi: 10.1212/CPJ.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mullaguri N., Sivakumar S., Battineni A., Anand S., Vanderwerf J. COVID-19 Related Acute Hemorrhagic Necrotizing Encephalitis: A Report of Two Cases and Literature Review. Cureus. 2021;13:e14236. doi: 10.7759/cureus.14236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Oosthuizen K., Steyn E.C., Tucker L., Ncube I.V., Hardie D., Marais S. SARS-CoV-2 encephalitis presenting as a clinical cerebellar syndrome: A case report. Neurology. 2021;97:27–29. doi: 10.1212/WNL.0000000000012051. [DOI] [PubMed] [Google Scholar]
- 72.Orsini M., Porto F.H.D.G., Nascimento J.F.D. Neuropsychiatric presentation of Covid-19-related encephalitis: Case report. Psychiatry Res. Commun. 2021;1:100004. doi: 10.1016/j.psycom.2021.100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Panariello A., Bassetti R., Radice A., Rossotti R., Puoti M., Corradin M., Moreno M., Percudani M. Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report. Brain, Behav. Immun. 2020;87:179–181. doi: 10.1016/j.bbi.2020.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Picod A., Dinkelacker V., Savatovsky J., Trouiller P., Guéguen A., Engrand N. SARS-CoV-2-associated encephalitis: Arguments for a post-infectious mechanism. Crit. Care. 2020;24:1–4. doi: 10.1186/s13054-020-03389-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pilotto A., Odolini S., Masciocchi S.S., Comelli A., Volonghi I., Gazzina S., Nocivelli S., Pezzini A., Focà E., Caruso A., et al. Steroid-Responsive Encephalitis in Coronavirus Disease 2019. Ann. Neurol. 2020;88:423–427. doi: 10.1002/ana.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pizzanelli C., Milano C., Canovetti S., Tagliaferri E., Turco F., Verdenelli S., Nesti L., Franchi M., Bonanni E., Menichetti F. Autoimmune limbic encephalitis related to SARS-CoV-2 infection: Case-report and review of the literature. Brain Behav. Immun. Health. 2021;12:1–6. doi: 10.1016/j.bbih.2021.100210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Poursadeghfard M., Sharifian-Dorche M., Nemati A., Mowla A. Simultaneous Encephalitis and Neuroretinitis After COVID-19 in a Young Adult: A Case Report. J. Neurol. Res. 2021;11:102–107. doi: 10.14740/jnr698. [DOI] [Google Scholar]
- 78.Rebeiz T., Lim-Hing K., Khazanehdari S., Rebeiz K. Behavioral Changes Without Respiratory Symptoms as a Presenting Sign of COVID-19 Encephalitis. Cureus. 2020;12:e10469. doi: 10.7759/cureus.10469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reddy R. Status epilepticus in a young woman with suspected SARS-CoV-2 encephalitis. Crit. Care Med. 2021;49:107. doi: 10.1097/01.ccm.0000726856.87504.3e. [DOI] [Google Scholar]
- 80.Sangare A., Dong A., Valente M., Pyatigorskaya N., Cao A., Altmayer V., Zyss J., Lambrecq V., Roux D., Morlon Q., et al. Neuroprognostication of Consciousness Recovery in a Patient with COVID-19 Related Encephalitis: Preliminary Findings from a Multimodal Approach. Brain Sci. 2020;10:845. doi: 10.3390/brainsci10110845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sarmast S.T., Mohamed A.S., Amar Z., Sarwar S., Ahmed Z. A Case of Acute Encephalitis in COVID-19 Patient: A Rare Complication. Cureus. 2021;13:e15636. doi: 10.7759/cureus.15636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sattar S.B.A., Haider M.A., Zia Z., Niazi M., Iqbal Q.Z. Clinical, Radiological, and Molecular Findings of Acute Encephalitis in a COVID-19 Patient: A Rare Case Report. Cureus. 2020;12:e10650. doi: 10.7759/cureus.10650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sharma R., Nalleballe K., Shah V., Haldal S., Spradley T., Hasan L., Mylavarapu K., Vyas K., Kumar M., Onteddu S., et al. Spectrum of Hemorrhagic Encephalitis in COVID-19 Patients: A Case Series and Review. Diagnostics. 2022;12:924. doi: 10.3390/diagnostics12040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sofijanova A., Bojadzieva S., Duma F., Superlishka E., Murtezani A., Jordanova O. Severe Encephalitis in Infant with COVID-19: A Case Report. Open Access Maced. J. Med Sci. 2020;8:514–517. doi: 10.3889/oamjms.2020.5485. [DOI] [Google Scholar]
- 85.Wettervik T.S., Kumlien E., Rostami E., Howells T., von Seth M., Velickaite V., Lewén A., Enblad P. Intracranial Pressure Dynamics and Cerebral Vasomotor Reactivity in Coronavirus Disease 2019 Patient With Acute Encephalitis. Crit. Care Explor. 2020;2:e0197. doi: 10.1097/CCE.0000000000000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tee T.Y., Thabit A.A.M., Khoo C.S., Shahrom H.M., Chan E.Z., Marzukie M.M., Kamaruddin Z.A.C., Thayan R., Chidambaram S.K. Acute encephalitis associated with SARS-CoV-2 confirmed in cerebrospinal fluid: First case in Malaysia. J. Clin. Neurol. 2021;17:490. doi: 10.3988/jcn.2021.17.3.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Urso L., Distefano M.G., Cambula G., Colomba A.I., Nuzzo D., Picone P., Giacomazza D., Sicurella L. The case of encephalitis in a COVID-19 pediatric patient. Neurol. Sci. 2021;43:105–112. doi: 10.1007/s10072-021-05670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Valadez-Calderon J., Navarro A.O., Rodriguez-Chavez E., Vera-Lastra O. Co-expression of anti-NMDAR and anti-GAD65 antibodies. A case of autoimmune encephalitis in a post-COVID-19 patient. Neurologia. 2022;37:503. doi: 10.1016/j.nrl.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Vandervorst F., Guldolf K., Peeters I., Vanderhasselt T., Michiels K., Berends K.J., Van Laethem J., Pipeleers L., Vincken S., Seynaeve L. Encephalitis associated with the SARS-CoV-2 virus: A case report. Interdiscip. Neurosurg. 2020;22:1–3. doi: 10.1016/j.inat.2020.100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Woldie I.L., Brown I.G., Nwadiaro N.F., Patel A., Jarrar M., Quint E., Khokhotva V., Hugel N., Winger M., Briskin A. Autoimmune Hemolytic Anemia in a 24-Year-Old Patient With COVID-19 Complicated by Secondary Cryptococcemia and Acute Necrotizing Encephalitis: A Case Report and Review of Literature. J. Med. Cases. 2020;11:362–365. doi: 10.14740/jmc3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ye M., Ren Y., Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav. Immun. 2020;88:945–946. doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zambreanu L., Lightbody S., Bhandari M., Hoskote C., Kandil H., Houlihan C.F., Lunn M.P. A case of limbic encephalitis associated with asymptomatic COVID-19 infection. J. Neurol. Neurosurg. Psychiatry. 2020;91:1229–1230. doi: 10.1136/jnnp-2020-323839. [DOI] [PubMed] [Google Scholar]
- 93.Zandifar S., Zandifar Z. Acute Viral Encephalitis Associated with SARS-CoV-2. Ann. Clin. Case Rep. 2020;5:1–3. [Google Scholar]
- 94.Zuhorn F., Omaimen H., Ruprecht B., Stellbrink C., Rauch M., Rogalewski A., Klingebiel R., Schäbitz W.-R. Parainfectious encephalitis in COVID-19: “The Claustrum Sign”. J. Neurol. 2020;268:2031–2034. doi: 10.1007/s00415-020-10185-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pilotto A., Masciocchi S., Volonghi I., Crabbio M., Magni E., De Giuli V., Caprioli F., Rifino N., Sessa M., Gennuso M. Clinical presentation and outcomes of SARS-CoV-2 related encephalitis: The ENCOVID multicentre study. J. Infect. Dis. 2020;223:28–37. doi: 10.1093/infdis/jiaa609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liotta E.M., Batra A., Clark J.R., Shlobin N.A., Hoffman S.C., Orban Z.S., Koralnik I.J. Frequent neurologic manifestations and encephalopathy-associated morbidity in Covid-19 patients. Ann. Clin. Transl. Neurol. 2020;7:2221–2230. doi: 10.1002/acn3.51210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Garg R.K., Paliwal V.K., Gupta A. Encephalopathy in patients with COVID-19: A review. J. Med. Virol. 2020;93:206–222. doi: 10.1002/jmv.26207. [DOI] [PubMed] [Google Scholar]
- 99.Kas A., Soret M., Pyatigoskaya N., Habert M.-O., Hesters A., Le Guennec L., Paccoud O., Bombois S., Delorme C. The cerebral network of COVID-19-related encephalopathy: A longitudinal voxel-based 18F-FDG-PET study. Eur. J. Nucl. Med. Mol. Imaging. 2021;48:2543–2557. doi: 10.1007/s00259-020-05178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Guo K., Wei Y., Yuan M., Wei L., Lu J. Identifying the characteristics of brain glucose metabolism using normal 18F-FDG PET database in patients with temporal lobe epilepsy. Neurol. Sci. 2020;41:3219–3226. doi: 10.1007/s10072-020-04426-1. [DOI] [PubMed] [Google Scholar]
- 101.Cani I., Barone V., D’Angelo R., Pisani L., Allegri V., Spinardi L., Malpassi P., Fasano L., Rinaldi R., Fanti S., et al. Frontal encephalopathy related to hyperinflammation in COVID-19. J. Neurol. 2020;268:16–19. doi: 10.1007/s00415-020-10057-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hosseini A.A., Shetty A.K., Sprigg N., Auer D.P., Constantinescu C.S. Delirium as a presenting feature in COVID-19: Neuroinvasive infection or autoimmune encephalopathy? Brain Behav. Immun. 2020;88:68–70. doi: 10.1016/j.bbi.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Umapathi T., Quek W.M.J., Yen J.M., Khin H.S.W., Mah Y.Y., Chan C.Y.J., Ling L.M., Yu W.-Y. Encephalopathy in COVID-19 patients; viral, parainfectious, or both? Eneurologicalsci. 2020;21:100275. doi: 10.1016/j.ensci.2020.100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Harmer D., Gilbert M., Borman R., Clark K.L. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107–110. doi: 10.1016/S0014-5793(02)03640-2. [DOI] [PubMed] [Google Scholar]
- 105.Lersy F., Anheim M., Willaume T., Chammas A., Brisset J.-C., Cotton F., Kremer S. Cerebral vasculitis of medium-sized vessels as a possible mechanism of brain damage in COVID-19 patients. J. Neuroradiol. 2021;48:141–146. doi: 10.1016/j.neurad.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S., van der Meer F., Kallio K., Kaya T., Anastasina M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kumari P., Rothan H.A., Natekar J.P., Stone S., Pathak H., Strate P.G., Arora K., Brinton M.A., Kumar M. Neuroinvasion and encephalitis following intranasal inoculation of SARS-CoV-2 in K18-hACE2 mice. Viruses. 2021;13:132. doi: 10.3390/v13010132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Klingenstein M., Klingenstein S., Neckel P.H., Mack A.F., Wagner A.P., Kleger A., Liebau S., Milazzo A. Evidence of SARS-CoV2 Entry Protein ACE2 in the Human Nose and Olfactory Bulb. Cells Tissues Organs. 2021;209:155–164. doi: 10.1159/000513040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hamming I., Timens W., Bulthuis M.L.C., Lely A.T., Navis G.J., van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chu H., Chan J.F.-W., Yuen T.T.-T., Shuai H., Yuan S., Wang Y., Hu B., Yip C.C.-Y., Tsang J.O.-L., Huang X. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: An observational study. Lancet Microbe. 2020;1:e14–e23. doi: 10.1016/S2666-5247(20)30004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available within the article and Supplementary Materials.