Abstract
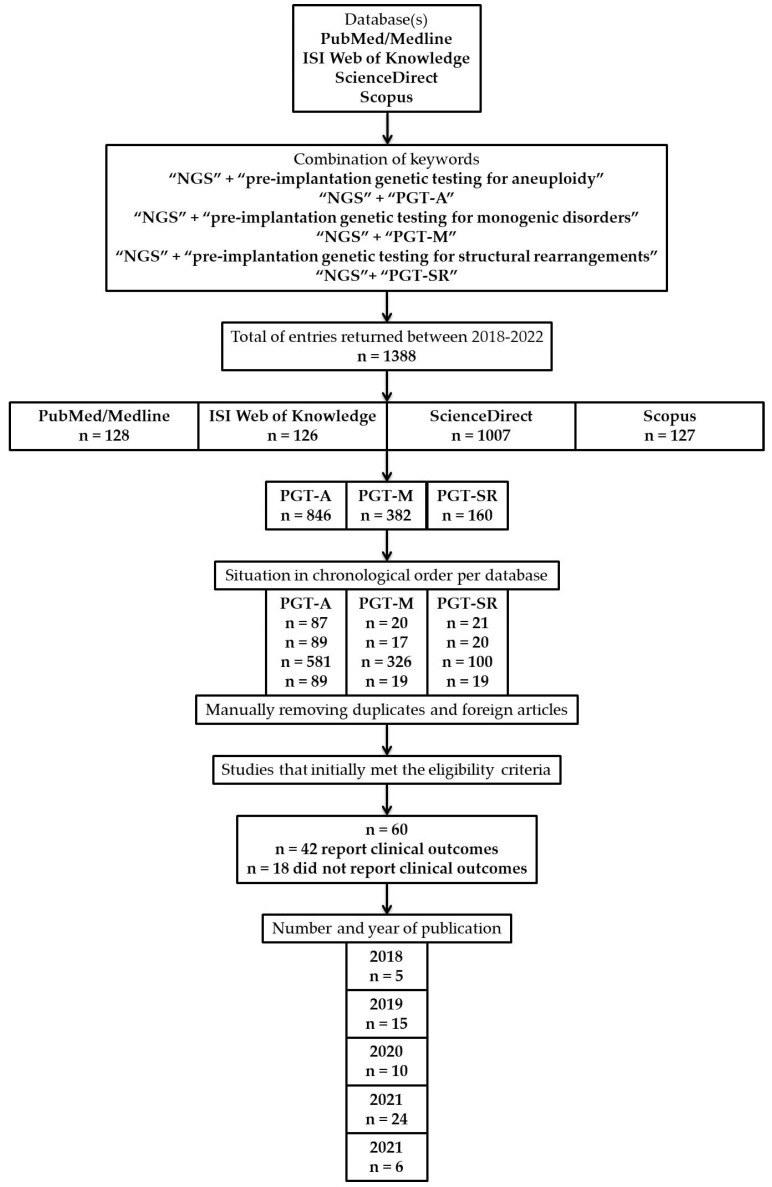
Background: PGT-based NGS revolutionized the field of reproductive medicine, becoming an integrated component within current assisted reproductive technology (ART) protocols. Methods: We searched the literature published in the last half a decade in four databases (PubMed/Medline, ISI Web of Knowledge, ScienceDirect, and Scopus) between 2018 and 2022. Results: A total of 1388 articles were filtered, from which 60 met, initially, the eligibility criteria, but only 42 were included (≥100 patients/couples—62,465 patients and 6628 couples in total) in the present mini-review. In total, forty-two (70.0%) reported reproductive outcomes, while eighteen (30.0%) had distinct objectives. Furthermore, n = 1, 1.66% of the studies focused on PGT, n = 1, 1.66% on pre-implantation genetic testing for monogenic disorders (PGT-M), n = 3, 5.0% on pre-implantation genetic testing for structural rearrangements (PGT-SR) and n = 55, 91.66% on pre-implantation genetic testing for aneuploidies (PGT-A). Conclusions: PGT using NGS proved to be an excellent companion that folds within the current ascending tendency among couples that require specialty care. We strongly encourage future studies to provide a systematic overview expanded at a larger scale on the role of the PGT-NGS.
Keywords: next-generation sequencing, pre-implantation genetic testing, aneuploidy, monogenic disorders, structural rearrangements, in vitro fertilization, assisted reproductive technology
1. Introduction
Although there is a presumption concerning the intrinsic process of human reproduction, this inherited mechanism is still singular and inefficient. Fortunately, the field of reproductive medicine incorporates an ascending trend, comprising methodologies that brought novel insights [1].
Thus, the current method of choice surrounding assisted reproductive technologies (ARTs) is IVF combined with PGT to minimize the risks of genetically abnormal embryo(s) [2]. Retrospectively, PGT evolved from an experimental procedure performed by Handyside et al. [3] more than three decades ago. The authors clarified the usefulness of PCR amplification to detect repetitive Y sequences in determining the sex of the fetus in families with a history as carriers of X-related malformations [3].
Distinct molecular biology techniques are optimized to respond to this constantly growing trend of couples requiring help and emerge as a countermeasure to the rudimentary protocols [4]. The European Society of Human Reproduction and Embryology (ESHRE) recently updated the terminology. Therefore, pre-implantation genetic diagnosis (PGD) and pre-implantation genetic screening (PGS) became PGT [5].
Presently, PGT may target aneuploidies, monogenic disorders, and structural rearrangements [5], PGT focusing on the biopsy of a single or few cells from fertilized embryos obtained in vitro and tested for potential genetic defects. Even though this procedure is complex and requires resources, next-generation sequencing (NGS) revolutionized the field of reproductive medicine [4].
Specialty societies such as PGD International Society (PGDIS), the American Society for Reproductive Medicine (ASRM), and ESHRE PGT Consortium issued a guideline regarding good practice. ESHRE further published an extent covering technical guidance on PGT organization of biopsied embryos and genetic testing [6,7,8,9].
Therefore, the present manuscript aims to highlight the reproductive outcomes of all studies conducted in the last five years (2018–2022) when combining PGT-NGS in circumstances when equal to or more than 100 patients/couples were enrolled.
2. Methodology
The present narrative mini-review follows the standard procedures previously described by Green et al. [10].
2.1. Database Search Strategy
The literature database explored for information until inception (April 2022) was PubMed/Medline, ISI Web of Knowledge, ScienceDirect, and Scopus. Several combinations of keywords such as “NGS” in combination with “pre-implantation genetic testing for aneuploidy—PGT-A”, “pre-implantation genetic testing for monogenic disorders—PGT-M”, and “pre-implantation genetic testing for structural rearrangements—PGT-SR” were employed during the databases tracking.
2.2. Inclusion Criteria
To emphasize the necessity of performing studies on a larger scale and the clinical relevance, we found it suitable to include ≥100 participants and/or couples. Based on the retrieved results, we created a time series (2018–2022) using Microsoft Excel® 2010 that contains the number of studies per year of publication, number, and database searched. Since PGT-NGS is mostly a human-targeted technique, experiences on experimental models, mice, rats, zebrafish (Danio rerio), or other species were not further considered. There were no restrictions concerning diagnosis (private clinics or hospital-based patients), nor in terms of age, sex, religion, and nationality.
2.3. Exclusion Criteria
Case report(s)/series, meta-analyses, review(s), standard or systematic, articles written in another language than English, letters to the Editor, conference posters, work protocols, preprints, and computational simulations have not been considered suitable.
2.4. Study Selection
Three independent authors (B.D., O.-D.I., and T.A.) screened the titles and abstracts of the retrieved result. We completed the assignment of all the relevant literature based on title, abstract, and full content. Any discrepancy was solved by consent with the remaining two authors (N.A., and C.I.).
2.5. Limitations of the Study
We concentrated on a mini-review rather than a quantitative meta-analysis due to the scarcity and heterogeneity of existing evidence.
3. Results
In Figure 1 can be found a flowchart of the present study design.
Figure 1.
A flowchart of the present study design, strategy, results, and studies that met the eligibility criteria.
A total of sixty manuscripts in the present manuscript were eligible, from which 75% (n = 45) were retrospective studies, 13.33% (n = 8) prospective studies, 6.66% (n = 4) retrospective observational studies, 3.33% (n = 2) randomized controlled trials (RCTs) and 1.66% (n = 1) observational study. Only n = 42 articles reported reproductive/clinical outcomes, the remaining n = 18 being used as informatic support since they differed by objective and results. Due to the plethora of conditions introduced by the authors that define the study design of articles included in this manuscript, we focus on specific data. Therefore, the main parameters of interest are: implantation, pregnancy, clinical pregnancy, ongoing pregnancy, miscarriage, spontaneous pregnancy loss, late pregnancy loss, biochemical pregnancy and ectopic pregnancy. Thus, based on these considerations, we stratified these studies (with or without indications for PGT, respectively, depending on the allocation per groups) according to the demographic information and assignment in numerical order (Table 1 and Table 2).
Table 1.
Stratification of studies based on the number of patients/couples grouped without indications for PGT.
| No. of Patients or Couples | Reproductive Outcomes | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Implantation | Pregnancy | Clinical Pregnancy | Ongoing Pregnancy | Miscarriage/ Early Pregnancy Loss |
Spontaneous Pregnancy Loss | Late Pregnancy Loss | Biochemical Pregnancy | Ectopic Pregnancy | ||
| NO ALLOCATION PER GROUPS | ||||||||||
|
270
patients |
63.10% (n = 53)
vs. 46.67% (n = 30) |
[11] | ||||||||
|
314
patients |
66.2% (n = 235) | 52.4% (n = 186) | 5.6% (n = 20) | 2.3% (n = 8) | 7.6% (n = 27) | 0.6% (n = 2) | [12] | |||
|
330
patients |
60% (n = 215) vs.
40% (n = 8) |
18% (n = 65)
vs. 40% (n = 8) |
[13] | |||||||
|
460
patients |
69.7% (n = 159) vs.
57.2 (n = 63) |
[14] | ||||||||
| 31649 patients | 62% | [15] | ||||||||
|
100
couples |
65.38% (n = 34) | n = 8 | 2.94% (n = 1) | 69.23% (n = 36) | [16] | |||||
| WITH ALLOCATION PER GROUPS | ||||||||||
|
166
patients |
29.0% (n = 9)
vs. 45.7% (n = 64) vs. 24.0% (n = 6) |
29.0% (n = 9)
vs. 40.7% (n = 57) vs. 16% (n = 4) |
30.9% (n = 4)
vs. 21.9% (n = 16) vs. 42.8% (n = 3) |
0% (n = 0)
vs. 0% (n = 0) vs. 0% (n = 0) |
[17] | |||||
|
228
patients |
65.4% (n = 53) vs.
67.4% (n = 99) |
13.2% (n = 7)
vs. 15.2% (n = 15) |
14.8% (n = 9)
vs. 15.4% (n = 18) |
[18] | ||||||
|
260
patients |
67.8% (n = 124)
vs. 63.6% (n = 49) |
75.4% (n = 138) vs.
70.1% (n = 54) |
57.9% (n = 106)
vs. 58.4% (n = 45) |
[19] | ||||||
|
275
patients |
*
31.5% vs. 28.8% ** 16.40% vs. 20.50% |
[20] | ||||||||
|
364
patients |
***
64.29% (n = 63) vs. 50.38% (n = 134) **** 64.12% (n = 84) vs. 51.60% (n = 226) |
***
3.17% (n = 2) vs. 11.94% (n = 16) **** 4.76% (n = 4) vs. 12.39% (n = 28) |
***
6.12% (n = 6) vs. 11.26% (n = 17) **** 8.70% (n = 8) vs. 9.96% (n = 25) |
[21] | ||||||
|
525
patients |
68.0% (n = 221)
vs. 55.5% (n = 111) |
13.1% (n = 29)
vs. 11.7% (n = 13) |
16.9% (n = 45)
vs. 20.1% (n = 28) |
[22] | ||||||
| 1152 patients |
3.2%
vs. 6.8% |
4.2%
vs. 3.9% |
1.1%
vs. 0.4% |
[23] | ||||||
|
142
couples |
45.77% (n = 65)
vs. 29.41% (n = 5) |
59.15% (n = 84) vs.
47.10% (n = 8) |
42.96% (n = 61) vs.
17.65% (n = 3) |
6.15% (n = 4)
vs. 40.0% (n = 2) |
13.38% (n = 19)
vs. 17.65% (n = 3) |
[24] | ||||
|
150
couples |
3.4% (n = 1)
vs. 14.7% (n = 8) |
6.9% (n = 2)
vs. 1.8% (n = 1) |
[25] | |||||||
|
180
couples |
n = 9
vs. n = 2 vs. n = 2 |
[26] | ||||||||
|
779
couples |
*****
67.9% (n = 106) vs. 69.6% (n = 117) vs. 75.6% (n = 68) ****** 86.8% (n = 33) vs. 78.4% (n = 29) vs. 46.4% (n = 13) |
*****
51.2% (n = 66) vs. 47.4% (n = 65) vs. 62.2% (n = 51) ****** 44.7% (n = 17) vs. 64.7% (n = 22) vs. 69.2% (n = 18) |
[27] | |||||||
| 1418 couples |
50.5% (n = 341) vs.
41.7% (n = 228) |
15.5% (n = 54)
vs. 22.8% (n = 52) |
[28] | |||||||
*—Chromosome translocation patients, **—aneuploidy patients, ***—FET with or without aneuploidy screening in the first ET attempt, ****—FET with or without aneuploidy screening in all transfer attempts, *****—<40 y, ******—≥40 y.
Table 2.
Stratification of studies based on the number of patients/couples with indications for PGT.
| No. of Patients or Couples |
Reproductive Outcomes | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Implantation | Pregnancy | Clinical Pregnancy | Ongoing Pregnancy | Miscarriage/ Early Pregnancy Loss |
Spontaneous Pregnancy Loss | Late Pregnancy Loss | Biochemical Pregnancy | Ectopic Pregnancy | ||
| NO ALLOCATION PER GROUPS | ||||||||||
| 296 patients |
85.7% (n = 12)
vs. 84.0% (n = 84) vs. 80.0% (n = 44) vs. 80.0% (n = 8) |
7.1% (n = 1)
vs. 6% (n = 6) vs. 5.4% (n = 3) vs. 10% (n = 1) |
[29] | |||||||
| 783 patients |
12.0% (n = 29)
vs. 11.0% (n = 15) vs. 12.7% (n = 8) |
10.7% (n = 29)
vs. 12.3% (n = 19) vs. 13.7% (n = 10) |
[30] | |||||||
| 1531 patients | 44.4% (n = 8) | 38.9% (n = 7) | [31] | |||||||
| WITH ALLOCATION PER GROUPS | ||||||||||
| 206 patients |
64.71% (n = 22) vs.
65.71% (n = 23) |
n = 1
vs. n = 3 |
[32] | |||||||
|
108 patients
|
51.8% (n = 43)
vs. 52% (n = 13) |
47% (n = 39)
vs. 52% (n = 13) |
47% (n = 39)
vs. 36% (n = 9) |
5.1% (n = 2)
vs. 30.7% (n = 4) |
[33] | |||||
| 108 patients |
79.4% (n = 50)
vs. 66.7% (n = 16) vs. 25.0% (n = 5) |
76.2% (n = 48) vs.
62.5% (n = 15) vs. 25.0% (n = 5) |
68.3% (n = 43) vs.
62.5% (n = 15) vs. 10.0% (n = 2) |
[34] | ||||||
| 155 patients | 80% (n = 68) | 66% (n = 56) | [35] | |||||||
| 283 patients | 52.3% (n = 148) | [36] | ||||||||
| 554 patients | 63.9% (n = 186) | 19.3% (n = 36) | [37] | |||||||
| 661 patients |
50.0% (n = 137) vs.
45.7% (n = 143) |
9.9% (n = 27)
vs. 9.6% (n = 30) |
10.6% (n = 29)
vs. 8.3% (n = 26) |
[38] | ||||||
| 974 patients |
69.9%
vs. 64.9% |
n = 472
vs. n = 94 |
n = 21
vs. n = 6 |
[39] | ||||||
| 1051 patients | 14.5% (n = 100) | n = 68 | n = 11 | [40] | ||||||
| 1513 patients |
51.34% (n = 306) vs.
49.56% (n = 227) |
10.07% (n = 60) vs.
6.33% (n = 29) |
9.56% (n = 57)
vs. 10.48% (n = 48) |
[41] | ||||||
| 648 couples |
64.7% (n = 202)
vs. 0% (n = 0) vs. 68.8% (n = 11) vs. 30.8% (n = 12) |
73.1%
vs. 23.5% |
7.4% (n = 23)
vs. 23.5% (n = 24 vs. 12.5% (n = 2) vs. 5.1% (n = 2) |
9% (n = 28)
vs. 16.7% (n = 17) vs. 12.5% (n = 2) vs. 12.8% (n = 5) |
1.0% (n = 3) vs.
0% (n = 0) vs. 0% (n = 0) vs. 0% (n = 0) |
[42] | ||||
We also tried to retrieve information related to the sequencer by strictly using article-related data and the supplementary materials section.
- (1)
- (2)
Following the allocation of the articles that met the eligibility criteria, we extracted several strong points:
-
(1)
The body mass index (BMI) and obesity influence the chances of implantation and amplify the risk of miscarriage [40,46], also dependent on the couple’s age [27], cesarean section (C-section) [22], and ovarian reserve [23], rather than correlated with previous unsuccessful pregnancies [36];
-
(2)
While age exerts a detrimental effect, it is mitigated through SNP-based PGT-A [39], and the embryos’ morphology possesses a significant threat with greater impact [11,37,47], but contradicted on several occasions [21,29,38]; Embryo morphokinetic [11,34,37] and inner cell mass (ICM) morphology constitute an optimal predictor of sustained implantation [48];
-
(3)
Mitochondrial DNA (mtDNA) copy numbers are higher in day 5 blastocysts of older women than day 6 blastocysts, further associated with a low chance of ongoing pregnancies [14,24]; The content of mtDNA is unable to predict the miscarriage risk [12] and additionally refuted when comparing the outcome differences between them [19] despite the cryo-storage [49];
-
(4)
Despite the sensitivity of platforms, errors still might occur, and their optimization is mandatory; PGT-NGS significantly improves the clinical outcomes in mosaic embryos [28,41,50], FAST-SeqS being a reliable and scalable PGT-A method [15];
-
(5)
Mosaic embryos have poor reproductive potential but retain the ability to result in live births [13,33], further sustaining that TE biopsy did not add detectable adverse effects [42] but as a supplement for the management of recurrent implantation failure (RIF) [45]; However, zona pellucida opening combined with TE biopsy increases the risk of mosaicism [32], TE mosaicism deriving after TE and ICM differentiation [30], while re-biopsy may rescue those with developmental potential [31];
-
(6)
Routine endometrial receptivity (ERA) is not supported in patients undergoing first autologous transfer, estradiol (E2) variation before progesterone (P4) initiation without influencing the transfer’s outcome; Estrogen is inversely associated with gestational age [18,51];
-
(7)
NGS-based PGT-A ensures good prognosis in patients [35,52] that suffer or are affected by distinct genetic abnormalities such as SMF [43], with structural rearrangements carriers [16,25,26], Turner syndrome [17], and iRPL [44];
-
(8)
Public coverage of ART should be strongly encouraged [20].
Although the true potential of the PGT has yet to be elucidated and fully transposed into current protocols, there is still controversy regarding this topic. Fortunately, there are currently 16 RCTs underway, from which six are observational (n = 3790 estimated participants) (NCT04734769, NCT04878991, NCT04976920, NCT04732013, NCT04711239, NCT03520933) and 10 are interventional (n = 3414 estimated participants) (NCT04414748, NCT04856696, NCT04000152, NCT03900780, NCT05009745, NCT04577560, NCT04485910, NCT04989348, NCT04654741, NCT03530254) (accessed on 4/12/2022) that may offer insight on this matter. Among the observational studies, (n = 1) is multicenter, (n = 3) reports the experience from a single center, whereas in the remaining (n = 2) no center is attributed. Analogous observations are also valid for those interventionals since (n = 2) are multicenter, while (n = 8) are from a single-center.
3.1. Pre-Implantation Genetic Testing for Monogenic Diseases
Unfortunately, between the pre-established timeframe, we could identify only one article aiming to assess the role of aneuploidy in PGT-M in young women. From 364 patients enrolled and subsequently divided into two unequal groups (n = 98/n = 266), a total of 569 frozen embryo transfer (FET) cycles (n = 131/n = 438) resulted from 385 oocytes. The aneuploidy screening significantly improved ongoing pregnancy/live birth rates following the first frozen embryo cycles and reduced the associated time for achieving a pregnancy [21].
3.2. Pre-Implantation Genetic Testing for Structural Rearrangements
From 1857 blastocysts following 528 cycles in 403 couples enrolled, 216 blastocysts were transferred through FET. There is some controversy regarding the results obtained since there is a significantly higher rate of balanced reciprocal translocation in women than in their counterparts. Additionally, it marks an improvement in transferable blastocysts rate in couples treated with gonadotropin-releasing hormone antagonist (GnRHa) compared with agonist groups [16]. Another study refutes this possible association among the assessed parameters [53]. Similar observations are outlined in a report of unbalanced chromosomal abnormalities, independently of the maternal age and gonadotropin dosage [26]. The risk of unbalanced rearrangement in paracentric and pericentric carriers is in a sex-associated pattern correlated with the ratio of inverted segment size [25].
3.3. Pre-Implantation Genetic Testing for Aneuploidy
The prevalence of de-novo segmental aneuploidies is relatively low [54]. Recent evidence brought us closer to resolving the true value of PGT-A [52] despite the necessity of future studies [42]. Four chromosomes (15, 16, 21, and 22) [55] are frequently reported, and identified in abnormalities [56]. SNP-based PGT-A possesses the ability to mitigate the negative effects of maternal age on IVF outcomes [39].
One way to expand this field of research is to optimize the work protocols and increase the accessibility to the general population through distinct national programs. Public coverage of ART procedures could represent a viable option compared with privately funded institutions [20], while different biopsy protocols of the TE may impact the mosaic blastocyst rate [32]. The transfer at the blastocyst stage is preferred, the long-term cryo-storage for more than 36 months remaining a safe alternative that ensures a good prognosis [35,49].
Several parameters modulate the quality of blastocysts by variances of mtDNA content. Interestingly, the associated level did not differ between non- and pregnant women [12], with a mean copy number of 0.0016 ± 0.0012 per genome. Variants of mtDNA can be found in both coding and non-coding regions, affecting the rate of reproductive outcomes, but independently on the maternal age and day of the biopsy [24]. The mtDNA, euploidy rate, and clinical pregnancy rate are superior for D5 compared with D6 blastocysts [14,24], with comparable results in rates between GnRHa and human chorionic gonadotropin (hCG) [57].
There is no relationship between BMI and ploidy, but rather upon semen morphology [27] of the embryo with the mention that the live birth rate can be low to the detriment of high miscarriage rate in obese patients [40,46,58] per BMI classification issued by the World Health Organization (WHO). The BMI and serum P4 had an insignificant impact on the copy number. The level of mtDNA is above the mean by comparison with abnormal chromosomal number phenomenon and following TE biopsy [59]. The clinical outcomes are similar between D5 and D6 blastocysts [19].
Relative telomere length of white blood cells (WBC) could offer insight. There is a correlation between telomere shortening once with aging with the rate of aneuploidy [60] and controlled ovarian stimulation (COS) [61]. This argument is antithetical to the actual rates of euploidy, aneuploidy, mosaicism, or blastocyst formation in men stratified by age [62].
The current body of knowledge does not support the routine of ERA [18] and the E2 supplementation before P4 initiation, being discovered an inverse correlation between E2 priming and pregnancy duration [51].
MALBAC-NGS-PGT-A outweighs MDA-SNP-PGT-A in terms of costs and support [28]. Despite the effectiveness of NGS, aCGH, and SNP array-based PGT in the modern era [41], there is a discrepancy in the applicability and results between the sexes, with often minimum conclusions [43] and errors still might occur [50]. Morphokinetic characteristics of embryos are insufficient [34,63], while cell-free DNA in spent blastocyst culture media might be a reasonable non-invasive approach [64]. Therefore, algorithms such as KIDscore D5 and mathematical models to predict the number of transferable blastocysts begin to be relevant in clinical practice. High platforms with over 95% sensitivity and specificity [15] could ease the effort of clinicians to conduct a genetic consultation [65]. PGT-A not only shortens the time of obtaining a pregnancy and the live birth [66], but oocyte donors ≤25 have similar cycle blastocyst euploidy, formation, and oocyte number retrieved as those between 26 and 30 years [67].
Current PGT-A methods can detect amalgams of euploid and aneuploid cells, which is why several teams of authors had it as an objective to evaluate the benefit of embryo selection. Inner cell mass (ICM) remains the most valuable predictor of sustained implantation [48], alongside pronuclear for [68] ploidy at all ages for euploid embryos of good quality at D5 [47], especially in younger patients. Poor quality does not always imply inadequate competence [29], considering that the STAR offered novel directions that marked the IVF practice worldwide [38].
Data suggest that aneuploid embryos and TE factors of miscarriage even after PGT-A, women still might suffer a pregnancy loss [36] or as direction for RIF management [45]. One can only speculate that patients with iRPL may be prone to clinical miscarriages. This argument highlights two scenarios: either these innovative platforms miss defects within chromosomes, especially at the level of IMC that subsequently leads to miscarriage, or the lack of diagnostic tests for RPL [44]. Moreover, there is a marked reduction of implantation and implicitly of ongoing pregnancies and live birth in women that had a C-section [22].
Despite the scarcity of data in the current literature regarding the impact of ovarian reserve and response on the chromosome status, the odds decline for a biopsied blastocyst to be euploid by 24% in the diminished ovarian reverse (DOR) group compared to non-DOR. The euploidy rates are not affected by the patient’s status and no differences between DOR and non-DOR with regard to living births per transfer were observed [23,69].
Recent studies showed that the transfer of mosaic embryos could give rise to healthy pregnancies, but are risks associated, precisely reduced implantation and high miscarriage rate concomitantly with fetal abnormalities. Therefore, they should not be treated as a priority [33]. Interestingly, low-medium mosaicism in TE arises after the differentiation of TE and ICM [30]. Re-biopsy constitutes the approach that may rescue blastocysts with developmental potential [31] if they exhibit direct or reverse cleavage and are morphologically eligible [11] with approximately half of the live birth rates by comparison with those euploids [13,37]. Recipients of donated oocytes subjected to an embryo transfer at blastocyst stage should be opted instead of cleavage stage embryo transfer as recently demonstrated [70], indicated choice in females with Turner Syndrome in cases with or without mosaicism [17], biopsy not adding additional risks to the neonatal outcomes [71].
4. Discussions
We hope this manuscript is a launching pad and may aid different teams of researchers in using it as a support pillar for future large-scale studies and in designing the protocol, possibly, which categories of patients to be enclosed. Although we have tried to cover in both tables as best as possible the reproductive outcomes based on the conditions implied by the authors, several of them had a unique design, while others confirm or refute the previous results of another team. Conclusively, numerous factors may impact reproductive outcomes in a double-edged sword manner, which is why clear inclusion criteria are compulsory to obtain optimal results. Despite the usefulness of predictors to reflect the reproductive potential, risks, and arguably outcome, errors still might occur, relying on sensitivity and specificity of working platforms. Even though national programs should become a priority regardless of the institution, specific interventions have associated risks. In this context, NGS is a groundbreaking research tool with substantial potential in various fields of interest. Thus, the presence of NGS became imperative in all laboratories that conduct ARTs. From our point of view, NGS now stands as the main barrier toward a new stage in our understanding of genetic defects.
Mechanically speaking, NGS is a cluster of novel technologies with a broad spectrum of utility; DNA and RNA sequencing, variants and mutations. It highly surpasses the Sanger sequencing, allowing simultaneous or massively parallel sequencing. Templates equivalent to eight human genomes (25 gigabases) can be sequenced because it does not involve target-specific primers. The foremost advantage by comparison with Sanger is the ability to target multiple sites in a single reaction in contrast to one target per reaction. Platforms designed over the years are 454 pyrosequencing, Illumina, SOLiD, the Polonator, HeliScope Single Molecule Sequencer, Ion Torrent, and PacBio RS. However, NGS involves the fulfillment of five distinct steps; (1) fragmentation, (2) library preparation, (3) massive parallel sequencing, (4) bioinformatic analysis, and (5) interpretation and variant/mutation annotation [72,73,74,75].
Due to its high potential and interest coupled with the recent discoveries, NGS comes tangent with the uprising trend in understanding disease-associated mutations and genetic alterations. The advancements, in particular, target enrichment methods resulted in evidence of variations responsible for dozens of rare genetic diseases; syndromes Schinzel-Giedion, Sensenbrenner, Miller, Kabuki, Fowler, and mutations attributed to hyperphosphatasia mental retardation and neonatal diabetes mellitus [76], but it has certain limitations in studying neurological diseases [77]. The two noninvasive prenatal testing (NIPT) modalities are cell-based/free and assay [78,79]. This technique involves the use of genetic material from maternal blood. Actual options include NGS of cell-free fetal DNA (cffDNA), polymerase-chain-reaction (PCR)-based methods, and microarrays, all attributed to aneuploidy detection and single fetal cell genome analysis. However, certain limitations must be overwhelmed. The possible clinical applications of both qualitative and quantitative NIPT are: qualitative—autosomal dominant and recessive disorders either when the father carries a mutation or compound heterozygosity is present, X-linked and newborn’s preclusion of hemolytic diseases; quantitative—disorders when the mother carriers a mutation or for both parents when they are suspected to be carrying the same mutation [80,81].
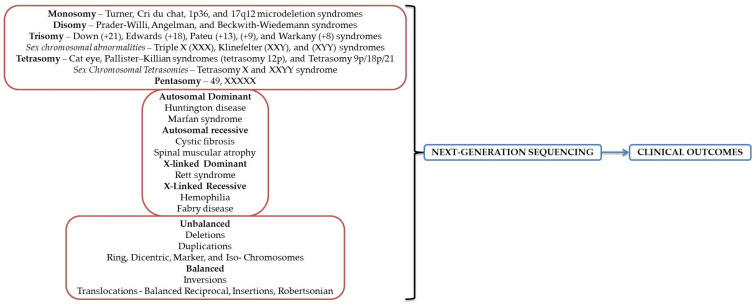
Compared with all NGS platforms developed following the fulfillment of the Human Genome Project (HGP) in 2003, only two are operated in clinical laboratories: Ion Torrent and Illumina systems. The remaining were either phased out due to the time/cost ratio or had limitations that could not be confounded. The principle behind Ion Torrent implies exploiting the emulsion PCR utilizing the aboriginal chemistry of deoxyribonucleoside triphosphate (dNTP) that discharge ions during base incorporation by DNA polymerase and a modified silicon chip detecting the pH modification. Illumina implies a concept on the existing Solexa sequencing-by-synthesis chemistry and use of the small flow cells, decreased imaging period, and rapid sequencing [73]. Illumina might outweigh the Ion Torrent in sequencing applications, but Ion Torrent could compensate Illumina in filling the gaps in the assembly produced. The main limitation of Illumina except the time required per run is the acquirement of variable fragments in length due to a phase shift of the analyzed sequences and consequently a reduced accuracy in the three ends of the segments. Concerning the Ion platforms, the total data output due to a higher error rate and sequence truncation could be improved [76]. Płoski [82] already provided a comprehensive comparison between Illumina and Ion Torrent platforms. A brief description of the NGS utility is presented in Figure 2.
Figure 2.
NGS broad utility in genetic disorders diagnosis.
5. Conclusions
In conclusion, this manuscript may be valuable to other groups in designing the working protocol, the allocation of patients, and the previous outcomes in cases of a more extensive study. NGS-PGT may be improved and suitable to respond to other classes of patients that seek specialty care. Fortunately, experiences on obese patients, at an advanced age, based on their history, or suffering from genetic abnormalities start to gain significant interest. We successfully argue that NGS-based PGT revolutionized this field despite the cases where there are no statistically significant differences between the analyzed groups and parameters evaluated. More specifically, genetic testing increases the chances within all parameters of interest established by us, but the possible involvement of stimulation cycle treatment is still studied. The success is sex- and age-dependent, in some situations proving efficient even in >35 years old women. Although biopsy protocols might impact the embryo’s morphology and morphogenetic, coupled with the health status, algorithms and non-invasive protocols to respond to each hypothetical scenario have been created over the years. Cumulatively, PGT using NGS folds on the constantly increasing trend of couples that seek specialty help. In summary, molecular biology techniques should be viewed as integrative components, reflected by the rates of implantation, clinical and ongoing pregnancy and live birth, accompanied by reduced miscarriage.
Acknowledgments
Not applicable.
Author Contributions
B.D., O.-D.I. and T.A. (Conceptualization, data curation, investigation, formal analysis, methodology, writing—original draft); N.A. and C.I. (conceptualization, methodology, supervision, validation, project administration, writing—review and editing); B.D. (conceptualization, methodology, supervision, validation, project administration). All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Macklon N.S., Geraedts J.P.M., Fauser B.C.J.M. Conception to ongoing pregnancy: The ‘black box’ of early pregnancy loss. Hum. Reprod. Update. 2002;8:333–343. doi: 10.1093/humupd/8.4.333. [DOI] [PubMed] [Google Scholar]
- 2.De Rycke M., Berckmoes V. Preimplantation Genetic Testing for Monogenic Disorders. Genes. 2020;11:871. doi: 10.3390/genes11080871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Handyside A.H., Kontogianni E.H., Hardy K., Winston R.M.L. Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature. 1990;344:768–770. doi: 10.1038/344768a0. [DOI] [PubMed] [Google Scholar]
- 4.Griffin D.K., Ogur C. Chromosomal analysis in IVF: Just how useful is it? Reproduction. 2018;156:F29–F50. doi: 10.1530/REP-17-0683. [DOI] [PubMed] [Google Scholar]
- 5.Zegers-Hochschild F., Adamson G.D., Dyer S., Racowsky C., de Mouzon J., Sokol R., Rienzi L., Sunde A., Schmidt L., Cooke I.D., et al. The International Glossary on Infertility and Fertility Care, 2017 †,‡,§. Hum. Reprod. 2017;32:1786–1801. doi: 10.1093/humrep/dex234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ESHRE PGT Consortium Steering Committee. Carvalho F., Coonen E., Goossens V., Kokkali G., Rubio C., Meijer-Hoogeveen M., Moutou C., Vermeulen N., De Rycke M. ESHRE PGT Consortium good practice recommendations for the organisation of PGT †. Hum. Reprod. Open. 2020;2020:hoaa021. doi: 10.1093/hropen/hoaa021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ESHRE PGT Consortium and SIG-Embryology Biopsy Working Group. Kokkali G., Coticchio G., Bronet F., Celebi C., Cimadomo D., Goossens V., Liss J., Nunes S., Sfontouris I., et al. ESHRE PGT Consortium and SIG Embryology good practice recommendations for polar body and embryo biopsy for PGT †. Hum. Reprod. Open. 2020;2020:hoaa020. doi: 10.1093/hropen/hoaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ESHRE PGT-M Working Group. Carvalho F., Moutou C., Dimitriadou E., Dreesen J., Giménez C., Goossens V., Kakourou G., Vermeulen N., Zuccarello D., et al. ESHRE PGT Consortium good practice recommendations for the detection of monogenic disorders †. Hum. Reprod. Open. 2020;2020:hoaa018. doi: 10.1093/hropen/hoaa018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ESHRE PGT-SR/PGT-A Working Group. Coonen E., Rubio C., Christopikou D., Dimitriadou E., Gontar J., Goossens V., Maurer M., Spinella F., Vermeulen N., et al. ESHRE PGT Consortium good practice recommendations for the detection of structural and numerical chromosomal aberrations. Hum. Reprod. Open. 2020;2020:hoaa017. doi: 10.1093/hropen/hoaa017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green B.N., Johnson C.D., Adams A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006;5:101–117. doi: 10.1016/S0899-3467(07)60142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gazzo E., Peña F., Valdéz F., Chung A., Velit M., Ascenzo M., Escudero E. Blastocyst contractions are strongly related with aneuploidy, lower implantation rates, and slow-cleaving embryos: A time lapse study. JBRA Assist. Reprod. 2020;24:77–81. doi: 10.5935/1518-0557.20190053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Damen A., Elkhatib I., Bayram A., Arnanz A., Abdala A., Samir S., Lawrenz B., De Munck N., Fatemi H.M. Does blastocyst mitochondrial DNA content affect miscarriage rate in patients undergoing single euploid frozen embryo transfer? J. Assist. Reprod. Genet. 2021;38:595–604. doi: 10.1007/s10815-020-02050-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zore T., Kroener L.L., Wang C., Liu L., Buyalos R., Hubert G., Shamonki M. Transfer of embryos with segmental mosaicism is associated with a significant reduction in live-birth rate. Fertil. Steril. 2019;111:69–76. doi: 10.1016/j.fertnstert.2018.08.057. [DOI] [PubMed] [Google Scholar]
- 14.Wu F.S.-Y., Weng S.-P., Shen M.-S., Ma P.-C., Wu P.-K., Lee N.-C. Suboptimal trophectoderm mitochondrial DNA level is associated with delayed blastocyst development. J. Assist. Reprod. Genet. 2021;38:587–594. doi: 10.1007/s10815-020-02045-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walters-Sen L., Neitzel D., Bristow S.L., Mitchell A., Alouf C.A., Aradhya S., Faulkner N. Experience analysing over 190,000 embryo trophectoderm biopsies using a novel FAST-SeqS preimplantation genetic testing assay. Reprod. Biomed. Online. 2022;44:228–238. doi: 10.1016/j.rbmo.2021.06.022. [DOI] [PubMed] [Google Scholar]
- 16.Cai Y., Ding M., Lin F., Diao Z., Zhang N., Sun H., Zhou J. Evaluation of preimplantation genetic testing based on next-generation sequencing for balanced reciprocal translocation carriers. Reprod. Biomed. Online. 2019;38:669–675. doi: 10.1016/j.rbmo.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 17.Giles J., Meseguer M., Mercader A., Rubio C., Alegre L., Vidal C., Trabalon M., Bosch E. Preimplantation genetic testing for aneuploidy in patients with partial X monosomy using their own oocytes: Is this a suitable indication? Fertil. Steril. 2020;114:346–353. doi: 10.1016/j.fertnstert.2020.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Riestenberg C., Kroener L., Quinn M., Ching K., Ambartsumyan G. Routine endometrial receptivity array in first embryo transfer cycles does not improve live birth rate. Fertil. Steril. 2021;115:1001–1006. doi: 10.1016/j.fertnstert.2020.09.140. [DOI] [PubMed] [Google Scholar]
- 19.Stankewicz T., Ruiz-Alonso M., Soler-Ibañez M., Simón C., Valbuena D. Do clinical outcomes differ for day-5 versus day-6 single embryo transfers controlled for endometrial factor? Reprod. Biomed. Online. 2022;44:478–485. doi: 10.1016/j.rbmo.2021.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Shao Y.-H., Zhang X.Y., Buckett W., Ao A. Impact of in vitro fertilization-preimplantation genetic testing (IVF-PGT) funding policy on clinical outcome: An issue that stems beyond effectiveness of treatment. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019;235:1–5. doi: 10.1016/j.ejogrb.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Hou W., Xu Y., Li R., Song J., Wang J., Zeng Y., Pan J., Zhou C., Xu Y. Role of aneuploidy screening in preimplantation genetic testing for monogenic diseases in young women. Fertil. Steril. 2019;111:928–935. doi: 10.1016/j.fertnstert.2019.01.017. [DOI] [PubMed] [Google Scholar]
- 22.Friedenthal J., Alkon-Meadows T., Hernandez-Nieto C., Gounko D., Lee J.A., Copperman A., Buyuk E. The association between prior cesarean delivery and subsequent in vitro fertilization outcomes in women undergoing autologous, frozen-thawed single euploid embryo transfer. Am. J. Obstet. Gynecol. 2021;225:287.e1–287.e8. doi: 10.1016/j.ajog.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 23.Jaswa E.G., McCulloch C.E., Simbulan R., Cedars M.I., Rosen M.P. Diminished ovarian reserve is associated with reduced euploid rates via preimplantation genetic testing for aneuploidy independently from age: Evidence for concomitant reduction in oocyte quality with quantity. Fertil. Steril. 2021;115:966–973. doi: 10.1016/j.fertnstert.2020.10.051. [DOI] [PubMed] [Google Scholar]
- 24.Lledo B., Ortiz J.A., Morales R., García-Hernández E., Ten J., Bernabeu A., Llácer J., Bernabeu R. Comprehensive mitochondrial DNA analysis and IVF outcome. Hum. Reprod. Open. 2018;2018:hoy023. doi: 10.1093/hropen/hoy023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xie P., Hu L., Tan Y., Gong F., Zhang S., Xiong B., Peng Y., Lu G.X., Lin G. Retrospective analysis of meiotic segregation pattern and interchromosomal effects in blastocysts from inversion preimplantation genetic testing cycles. Fertil. Steril. 2019;112:336–342.e3. doi: 10.1016/j.fertnstert.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 26.Yuan P., Zheng L., Ou S., Zhao H., Li R., Luo H., Tan X., Zhang Q., Wang W. Evaluation of chromosomal abnormalities from preimplantation genetic testing to the reproductive outcomes: A comparison between three different structural rearrangements based on next-generation sequencing. J. Assist. Reprod. Genet. 2021;38:709–718. doi: 10.1007/s10815-020-02053-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li S., Shen Y., Zhu Y., Li H., Jiang W., Yan J., Chen Z.-J. The interaction effect between advanced paternal age and paternal obesity is associated with the low implantation rate in couples with unexplained recurrent pregnancy loss. Gynecol. Obstet. Clin. Med. 2021;1:197–204. doi: 10.1016/j.gocm.2021.10.003. [DOI] [Google Scholar]
- 28.Niu W., Wang L., Xu J., Li Y., Shi H., Li G., Jin H., Song W., Wang F., Sun Y. Improved clinical outcomes of preimplantation genetic testing for aneuploidy using MALBAC-NGS compared with MDA-SNP array. BMC Pregnancy Childbirth. 2020;20:388. doi: 10.1186/s12884-020-03082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Viñals Gonzalez X., Odia R., Naja R., Serhal P., Saab W., Seshadri S., Ben-Nagi J. Euploid blastocysts implant irrespective of their morphology after NGS-(PGT-A) testing in advanced maternal age patients. J. Assist. Reprod. Genet. 2019;36:1623–1629. doi: 10.1007/s10815-019-01496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Capalbo A., Poli M., Rienzi L., Girardi L., Patassini C., Fabiani M., Cimadomo D., Benini F., Farcomeni A., Cuzzi J., et al. Mosaic human preimplantation embryos and their developmental potential in a prospective, non-selection clinical trial. Am. J. Hum. Genet. 2021;108:2238–2247. doi: 10.1016/j.ajhg.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou S., Xie P., Zhang S., Hu L., Luo K., Gong F., Lu G., Lin G. Complex mosaic blastocysts after preimplantation genetic testing: Prevalence and outcomes after re-biopsy and re-vitrification. Reprod. Biomed. Online. 2021;43:215–222. doi: 10.1016/j.rbmo.2021.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Xiong S., Liu W., Wang J., Liu J., Gao Y., Wu L., Zhu J., Hao X., Li J., Liu D., et al. Trophectoderm biopsy protocols may impact the rate of mosaic blastocysts in cycles with pre-implantation genetic testing for aneuploidy. J. Assist. Reprod. Genet. 2021;38:1153–1162. doi: 10.1007/s10815-021-02137-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lin P.-Y., Lee C.-I., Cheng E.-H., Huang C.-C., Lee T.-H., Shih H.-H., Pai Y.-P., Chen Y.-C., Lee M.-S. Clinical Outcomes of Single Mosaic Embryo Transfer: High-Level or Low-Level Mosaic Embryo, Does it Matter? J. Clin. Med. 2020;9:1695. doi: 10.3390/jcm9061695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee C.-I., Chen C.-H., Huang C.-C., Cheng E.-H., Chen H.-H., Ho S.-T., Lin P., Lee M.-S., Lee T.-H. Embryo morphokinetics is potentially associated with clinical outcomes of single-embryo transfers in preimplantation genetic testing for aneuploidy cycles. Reprod. Biomed. Online. 2019;39:569–579. doi: 10.1016/j.rbmo.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 35.Gorodeckaja J., Neumann S., McCollin A., Ottolini C.S., Wang J., Ahuja K., Handyside A., Summers M. High implantation and clinical pregnancy rates with single vitrified-warmed blastocyst transfer and optional aneuploidy testing for all patients. Hum. Fertil. 2020;23:256–267. doi: 10.1080/14647273.2018.1551628. [DOI] [PubMed] [Google Scholar]
- 36.Wang A., Kort J., Westphal L. Miscarriage history association with euploid embryo transfer outcomes. Reprod. Biomed. Online. 2019;39:617–623. doi: 10.1016/j.rbmo.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 37.Ozbek I.Y., Mumusoglu S., Polat M., Bozdag G., Sokmensuer L.K., Yarali H. Comparison of single euploid blastocyst transfer cycle outcome derived from embryos with normal or abnormal cleavage patterns. Reprod. Biomed. Online. 2021;42:892–900. doi: 10.1016/j.rbmo.2021.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Munné S., Kaplan B., Frattarelli J.L., Child T., Nakhuda G., Shamma F.N., Silverberg K., Kalista T., Handyside A.H., Katz-Jaffe M., et al. Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: A multicenter randomized clinical trial. Fertil. Steril. 2019;112:1071–1079.e7. doi: 10.1016/j.fertnstert.2019.07.1346. [DOI] [PubMed] [Google Scholar]
- 39.Simon A.L., Kiehl M., Fischer E., Proctor J.G., Bush M.R., Givens C., Rabinowitz M., Demko Z.P. Pregnancy outcomes from more than 1800 in vitro fertilization cycles with the use of 24-chromosome single-nucleotide polymorphism-based preimplantation genetic testing for aneuploidy. Fertil. Steril. 2018;110:113–121. doi: 10.1016/j.fertnstert.2018.03.026. [DOI] [PubMed] [Google Scholar]
- 40.Boynukalin F.K., Abalı R., Gultomruk M., Yarkiner Z., Mutlu A., Bahceci M. Which factors affect the likelihood of miscarriage after single euploid blastocyst transfer? Reprod. Biomed. Online. 2021;42:1187–1195. doi: 10.1016/j.rbmo.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 41.Xiao M., Lei C.-X., Xi Y.-P., Lu Y.-L., Wu J.-P., Li X.-Y., Zhang S., Zhu S.-J., Zhou J., Li X., et al. Next-Generation Sequencing Is More Efficient at Detecting Mosaic Embryos and Improving Pregnancy Outcomes than Single-Nucleotide Polymorphism Array Analysis. J. Mol. Diagn. 2021;23:710–718. doi: 10.1016/j.jmoldx.2021.02.011. [DOI] [PubMed] [Google Scholar]
- 42.Tiegs A.W., Tao X., Zhan Y., Whitehead C., Kim J., Hanson B., Osman E., Kim T.J., Patounakis G., Gutmann J., et al. A multicenter, prospective, blinded, nonselection study evaluating the predictive value of an aneuploid diagnosis using a targeted next-generation sequencing-based preimplantation genetic testing for aneuploidy assay and impact of biopsy. Fertil. Steril. 2021;115:627–637. doi: 10.1016/j.fertnstert.2020.07.052. [DOI] [PubMed] [Google Scholar]
- 43.Xu R., Ding Y., Wang Y., He Y., Sun Y., Lu Y., Yao N. Comparison of preimplantation genetic testing for aneuploidy versus intracytoplasmic sperm injection in severe male infertility. Andrologia. 2021;53:e14065. doi: 10.1111/and.14065. [DOI] [PubMed] [Google Scholar]
- 44.Liu X.-Y., Fan Q., Wang J., Li R., Xu Y., Guo J., Wang Y.-Z., Zeng Y.-H., Ding C.-H., Cai B., et al. Higher chromosomal abnormality rate in blastocysts from young patients with idiopathic recurrent pregnancy loss. Fertil. Steril. 2020;113:853–864. doi: 10.1016/j.fertnstert.2019.11.016. [DOI] [PubMed] [Google Scholar]
- 45.Tong J., Niu Y., Wan A., Zhang T. Next-Generation Sequencing (NGS)-Based Preimplantation Genetic Testing for Aneuploidy (PGT-A) of Trophectoderm Biopsy for Recurrent Implantation Failure (RIF) Patients: A Retrospective Study. Reprod. Sci. 2021;28:1923–1929. doi: 10.1007/s43032-021-00519-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cozzolino M., García-Velasco J.A., Meseguer M., Pellicer A., Bellver J. Female obesity increases the risk of miscarriage of euploid embryos. Fertil. Steril. 2021;115:1495–1502. doi: 10.1016/j.fertnstert.2020.09.139. [DOI] [PubMed] [Google Scholar]
- 47.Awadalla M.S., Vestal N.L., McGinnis L.K., Ahmady A., Paulson R.J. Effect of age and morphology on sustained implantation rate after euploid blastocyst transfer. Reprod. Biomed. Online. 2021;43:395–403. doi: 10.1016/j.rbmo.2021.06.008. [DOI] [PubMed] [Google Scholar]
- 48.Nazem T.G., Sekhon L., Lee J.A., Overbey J., Pan S., Duke M., Briton-Jones C., Whitehouse M., Copperman A.B., Stein D.E. The correlation between morphology and implantation of euploid human blastocysts. Reprod. Biomed. Online. 2019;38:169–176. doi: 10.1016/j.rbmo.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Cimadomo D., Fabozzi G., Dovere L., Maggiulli R., Albricci L., Innocenti F., Soscia D., Giancani A., Vaiarelli A., Guido M., et al. Clinical, obstetric and perinatal outcomes after vitrified-warmed euploid blastocyst transfer are independent of cryo-storage duration. Reprod. Biomed. Online. 2022;44:221–227. doi: 10.1016/j.rbmo.2021.09.027. [DOI] [PubMed] [Google Scholar]
- 50.Friedenthal J., Maxwell S.M., Tiegs A.W., Besser A.G., McCaffrey C., Munné S., Noyes N., Grifo J.A. Clinical error rates of next generation sequencing and array comparative genomic hybridization with single thawed euploid embryo transfer. Eur. J. Med. Genet. 2020;63:103852. doi: 10.1016/j.ejmg.2020.103852. [DOI] [PubMed] [Google Scholar]
- 51.Sekhon L., Feuerstein J., Pan S., Overbey J., Lee J.A., Briton-Jones C., Flisser E., Stein D.E., Mukherjee T., Grunfeld L., et al. Endometrial preparation before the transfer of single, vitrified-warmed, euploid blastocysts: Does the duration of estradiol treatment influence clinical outcome? Fertil. Steril. 2019;111:1177–1185.e3. doi: 10.1016/j.fertnstert.2019.02.024. [DOI] [PubMed] [Google Scholar]
- 52.Li X., Zhu X., Hao Y., Ji D., Zhang Z., Wei Z., Cao Y., Zhou P. Comprehensive assessment of a clinic’s experience of preimplantation genetic testing by a cumulative rate. Taiwan. J. Obstet. Gynecol. 2021;60:225–231. doi: 10.1016/j.tjog.2020.11.034. [DOI] [PubMed] [Google Scholar]
- 53.Tong J., Niu Y., Wan A., Zhang T. Effect of parental origin and predictors for obtaining a euploid embryo in balanced translocation carriers. Reprod. Biomed. Online. 2022;44:72–79. doi: 10.1016/j.rbmo.2021.09.007. [DOI] [PubMed] [Google Scholar]
- 54.Zhou S., Cheng D., Ouyang Q., Xie P., Lu C., Gong F., Hu L., Tan Y., Lu G., Lin G. Prevalence and authenticity of de-novo segmental aneuploidy (>16 Mb) in human blastocysts as detected by next-generation sequencing. Reprod. Biomed. Online. 2018;37:511–520. doi: 10.1016/j.rbmo.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 55.Nair J., Shetty S., Kasi C.I., Thondehalmath N., Ganesh D., Bhat V.R., Mannadia S., Ranganath A., Nayak R., Gunasheela D., et al. Preimplantation genetic testing for aneuploidy (PGT-A)—A single-center experience. J. Assist. Reprod. Genet. 2022;39:729–738. doi: 10.1007/s10815-022-02413-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Y.-L., Yu T.-N., Wang P.-H., Tzeng C.-R., Chen C.-H., Chen C.-H. Could PGT-A pick up true abnormalities that have clinical relevance? Retrospective analysis of 1043 embryos. Taiwan. J. Obstet. Gynecol. 2020;59:496–501. doi: 10.1016/j.tjog.2020.05.005. [DOI] [PubMed] [Google Scholar]
- 57.Thorne J., Loza A., Kaye L., Nulsen J., Benadiva C., Grow D., Engmann L. Euploidy rates between cycles triggered with gonadotropin-releasing hormone agonist and human chorionic gonadotropin. Fertil. Steril. 2019;112:258–265. doi: 10.1016/j.fertnstert.2019.03.040. [DOI] [PubMed] [Google Scholar]
- 58.Stovezky Y.R., Romanski P.A., Bortoletto P., Spandorfer S.D. Body mass index is not associated with embryo ploidy in patients undergoing in vitro fertilization with preimplantation genetic testing. Fertil. Steril. 2021;116:388–395. doi: 10.1016/j.fertnstert.2021.02.029. [DOI] [PubMed] [Google Scholar]
- 59.de Los Santos M.J., Diez Juan A., Mifsud A., Mercader A., Meseguer M., Rubio C., Pellicer A. Variables associated with mitochondrial copy number in human blastocysts: What can we learn from trophectoderm biopsies? Fertil. Steril. 2018;109:110–117. doi: 10.1016/j.fertnstert.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 60.Hanson B.M., Tao X., Zhan Y., Kim J.G., Klimczak A.M., Herlihy N.S., Scott R.T., Jr., Seli E. Shorter telomere length of white blood cells is associated with higher rates of aneuploidy among infertile women undergoing in vitro fertilization. Fertil. Steril. 2021;115:957–965. doi: 10.1016/j.fertnstert.2020.09.164. [DOI] [PubMed] [Google Scholar]
- 61.Cascales A., Lledó B., Ortiz J.A., Morales R., Ten J., Llácer J., Bernabeu R. Effect of ovarian stimulation on embryo aneuploidy and mosaicism rate. Syst. Biol. Reprod. Med. 2021;67:42–49. doi: 10.1080/19396368.2020.1850908. [DOI] [PubMed] [Google Scholar]
- 62.Dviri M., Madjunkova S., Koziarz A., Antes R., Abramov R., Mashiach J., Moskovtsev S., Kuznyetsova I., Librach C. Is there a correlation between paternal age and aneuploidy rate? An analysis of 3118 embryos derived from young egg donors. Fertil. Steril. 2020;114:293–300. doi: 10.1016/j.fertnstert.2020.03.034. [DOI] [PubMed] [Google Scholar]
- 63.Zeyad A., Al-Abdulkareem B., Hammadeh M.E. The relationship between preimplantation morphokinetics of human embryos and sex chromosome pattern. Reprod. Biol. 2018;18:385–389. doi: 10.1016/j.repbio.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 64.Rubio C., Navarro-Sánchez L., García-Pascual C.M., Ocali O., Cimadomo D., Venier W., Barroso G., Kopcow L., Bahçeci M., Kulmann M.I.R., et al. Multicenter prospective study of concordance between embryonic cell-free DNA and trophectoderm biopsies from 1301 human blastocysts. Am. J. Obstet. Gynecol. 2020;223:751.e1–751.e13. doi: 10.1016/j.ajog.2020.04.035. [DOI] [PubMed] [Google Scholar]
- 65.Cai Y., Ding M., Zhang Y., Sun Y., Lin F., Diao Z., Zhou J. A mathematical model for predicting the number of transferable blastocysts in next-generation sequencing-based preimplantation genetic testing. Arch. Gynecol. Obstet. 2022;305:241–249. doi: 10.1007/s00404-021-06050-6. [DOI] [PubMed] [Google Scholar]
- 66.Takeuchi K. Pre-implantation genetic testing: Past, present, future. Reprod. Med. Biol. 2020;20:27–40. doi: 10.1002/rmb2.12352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hoyos L.R., Cheng C.Y., Brennan K., Hubert G., Wang B., Buyalos R.P., Quinn M., Shamonki M. Euploid rates among oocyte donors: Is there an optimal age for donation? J. Assist. Reprod. Genet. 2020;37:589–594. doi: 10.1007/s10815-020-01694-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Roos Kulmann M.I., Lumertz Martello C., Bos-Mikich A., Frantz N. Pronuclear and blastocyst morphology are associated age-dependently with embryo ploidy in in vitro fertilization cycles. Hum. Fertil. 2020:369–379. doi: 10.1080/14647273.2020.1808716. [DOI] [PubMed] [Google Scholar]
- 69.Karlıkaya G., Boynukalin F.K., Gultomruk M., Kavrut M., Abalı R., Demir B., Ecemis S., Yarkiner Z., Bahceci M. Euploidy rates of embryos in young patients with good and low prognosis according to the POSEIDON criteria. Reprod. Biomed. Online. 2021;42:733–741. doi: 10.1016/j.rbmo.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 70.Clua E., Rodríguez I., Arroyo G., Racca A., Martínez F., Polyzos N.P. Blastocyst transfer increases cumulative-live-birth-rates and reduces time and cost to livebirth compared with cleavage stage in recipients of donated oocytes. A randomized controlled trial. Reprod. Biomed. Online. 2022;44:995–1004. doi: 10.1016/j.rbmo.2022.01.001. [DOI] [PubMed] [Google Scholar]
- 71.He H., Jing S., Lu C.F., Tan Y.Q., Luo K.L., Zhang S.P., Gong F., Lu G.X., Lin G. Neonatal outcomes of live births after blastocyst biopsy in preimplantation genetic testing cycles: A follow-up of 1721 children. Fertil. Steril. 2019;112:82–88. doi: 10.1016/j.fertnstert.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 72.Frese K.S., Katus H.A., Meder B. Next-generation sequencing: From understanding biology to personalized medicine. Biology. 2013;2:378–398. doi: 10.3390/biology2010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Liu L., Li Y., Li S., Hu N., He Y., Pong R., Lin D., Lu L., Law M. Comparison of Next-Generation Sequencing Systems. J. Biomed. Biotechnol. 2012;2012:251364. doi: 10.1155/2012/251364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mardis E.R. Next-Generation Sequencing Platforms. Annu. Rev. Anal. Chem. 2013;6:287–303. doi: 10.1146/annurev-anchem-062012-092628. [DOI] [PubMed] [Google Scholar]
- 75.Mardis E.R. Next-Generation DNA Sequencing Methods. Annu. Rev. Genomics Hum. Genet. 2008;9:387–402. doi: 10.1146/annurev.genom.9.081307.164359. [DOI] [PubMed] [Google Scholar]
- 76.Gupta A., Gupta U.D. Animal Biotechnology. Academic Press; Cambridge, MA, USA: 2020. Next generation sequencing and its applications; pp. 395–421. [Google Scholar]
- 77.Bras J., Guerreiro R., Hardy J. Use of next-generation sequencing and other whole-genome strategies to dissect neurological disease. Nat. Rev. Neurosci. 2012;13:453–464. doi: 10.1038/nrn3271. [DOI] [PubMed] [Google Scholar]
- 78.Papageorgiou E.A., Patsalis P.C. Non-invasive prenatal diagnosis of aneuploidies: New technologies and clinical applications. Genome Med. 2012;4:46. doi: 10.1186/gm345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Norwitz E.R., Levy B. Noninvasive prenatal testing: The future is now. Rev. Obstet. Gynecol. 2013;6:48–62. [PMC free article] [PubMed] [Google Scholar]
- 80.Cogulu O. Next Generation Sequencing as a Tool for Noninvasive Prenatal Tests. In: Demkow U., Płoski R., editors. Clinical Applications for Next-Generation Sequencing. Academic Press; Cambridge, MA, USA: 2016. pp. 171–188. [Google Scholar]
- 81.Di Resta C., Galbiati S., Carrera P., Ferrari M. Next-generation sequencing approach for the diagnosis of human diseases: Open challenges and new opportunities. Electron. J. IFCC (eJIFCC) 2018;29:4–14. [PMC free article] [PubMed] [Google Scholar]
- 82.Płoski R. Next Generation Sequencing—General Information about the Technology, Possibilities, and Limitations. In: Demkow U., Płoski R., editors. Clinical Applications for Next-Generation Sequencing. Academic Press; Cambridge, MA, USA: 2016. pp. 1–18. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.