Abstract
The COVID-19 pandemic has exposed gaps and areas of need in health systems worldwide. This work aims to map the evidence on COVID-19-related healthcare needs of adult patients, their family members, and the professionals involved in their care during the first year of the pandemic. We searched the databases MEDLINE, Embase, and Web of Science. Two reviewers independently screened titles and abstracts and assessed full texts for eligibility. Disagreements were resolved by consensus. Descriptive data were extracted and inductive qualitative content analysis was used to generate codes and derive overarching themes. Thirty-six studies met inclusion criteria, with the majority reporting needs from the perspective of professionals (35/36). Professionals’ needs were grouped into three main clusters (basic, occupational, and psycho-socio-emotional needs); patients’ needs into four (basic, healthcare, psycho-socio-emotional, and other support needs); and family members’ needs into two (psycho-socio-emotional and communication needs). Transversal needs across subgroups were also identified and grouped into three main clusters (public safety, information and communication, and coordination and support needs). This evidence map provides valuable insight on COVID-19-related healthcare needs. More research is needed to assess first-person perspectives of patients and their families, examine whether needs differ by country or region, and evaluate how needs have evolved over time.
Keywords: COVID-19, pandemic, needs assessment, healthcare needs, healthcare professionals’ needs, patients’ needs, family members’ needs, evidence map, systematic review
1. Introduction
The first cases of the new coronavirus infectious disease (COVID-19) were reported in late-December 2019 in Wuhan, China [1]. Due to the alarming levels of spread and severity of the disease, the World Health Organization (WHO) declared COVID-19 as a pandemic shortly after, in March 2020 [2]. The pandemic triggered a global health, social, economic, and human crisis that has exposed gaps and areas of need in systems of care [3].
Since its emergence, COVID-19 has tested the resilience and preparedness of the health systems worldwide. They were overall unprepared to respond to a public health emergency such as COVID-19, and due to the unprecedented nature of the novel coronavirus, had insufficient time and resources to adapt, facing the pandemic with limited effective resources available [4,5,6,7,8]. Limited or inadequate medicines, equipment, personnel, and facilities were reported [9,10,11]. Appropriate service delivery was further compounded by ineffective public health policies and initiatives [12], financial instability, and health information and communication challenges [3].
The significant impact on care systems particularly affected the workforce, service users, and their family members. The health workforce, the driving force of health care supply, struggled with high levels of mental and physical distress [13,14]. They faced enormous work overloads, financial instability, increased risks of infection transmission in part due to insufficient personal protective equipment (PPE), and overall exhaustion [13,14,15]. Moreover, healthcare professionals that were redeployed because of staff shortages faced additional challenges by working in unfamiliar settings [16,17]. Introducing public health safety measures, such as social distancing, stay-at-home-orders, or school and childcare closures, further exacerbated difficulties for professionals, as well as impacted patients and their families [18].
The saturation of the health systems led to a decrease in the quality of services [19,20] and person-centered care [21]. Patients encountered barriers to accessing health services [21,22], communication difficulties with healthcare providers [23], and lack of social support, among other difficulties [22,24]. COVID-19 patients have had pronounced healthcare needs, with approximately half of them needing physical, cognitive, and psychological follow-up care post-acute symptoms’ resolution [25,26,27]. On the other hand, non-COVID patients including people with noncommunicable diseases, such as cancer and cardiovascular disease, experienced disrupted care in general due to a health system responding to the acute pandemic situation [18]. In fact, cessation of essential services to non-COVID patients, and postponing or avoiding seeking medical care contributed to higher morbidity and mortality rates [28]. Besides, previous research has demonstrated the pandemic has increased care disparities, making populations at high social risk, such as underrepresented minorities, more vulnerable to COVID-19 [29]. The growing use of telehealth further reinforced health inequities for marginalized populations who have limited access to technology and financial resources [22]. In turn, families of service users have also been deeply impacted by the COVID-19 pandemic as they have also faced communication, financial, and other social challenges, as well as high psychological distress [30].
The early phase of the COVID-19 pandemic was particularly challenging as the health workforce, patients, and their families were subject to the unpreparedness of health systems and a high degree of uncertainty. To date, no structured attempt has been made to summarize the state of research on COVID-19-related healthcare needs during the first year of the pandemic in these population subgroups. Given the magnitude and the profound impact of the COVID-19 pandemic, and the significance of addressing these needs, mapping the evidence during the first year of the pandemic by conducting a systematic search of existing knowledge in the field is warranted.
1.1. Evidence Mapping
Evidence mapping is an emerging method for reviewing and synthetizing evidence in a reproducible and transparent manner [31]. It was first developed and used in the social sciences [32,33], and it has since been widely used in other fields including health sciences (e.g., patient preferences [34], central nervous system injury [35], environmental management [36]). More specifically, evidence mapping is a systematic search of a broad subject area used to identify clusters and gaps in knowledge and/or future research needs that presents results in a user-friendly product, such as a visual or a searchable database [37]. This framework does not require a critical appraisal of included studies but instead aims to assess what type of research has been conducted, what settings have been evaluated, and what methods have been used. Qualitative or quantitative analyses are not always performed; alternatively, the synthesis is limited to a narrative description of the state of knowledge [36]. In sum, evidence mapping is particularly useful as an exploratory, comprehensive evidence synthesis method of a broad topic to provide an overview of the evidence base in an easily digestible format.
1.2. Objectives
The present evidence map (EM) aims to (i) describe key characteristics of research on healthcare-related needs associated with COVID-19 from the perspective of adult patients, their family members, and the professionals involved in their care during the first year of the pandemic, and (ii) identify knowledge clusters and gaps to inform future research, clinical practice, and policymaking. This work will provide us with a thorough overview of research on COVID-19-related healthcare needs in the three subgroups of the population most directly affected by the pandemic. This EM also seeks to inform an ongoing online cross-sectional survey study exploring Spanish healthcare and related needs during the care pathway of people with a history of COVID-19, based on the experience of patients and the professionals involved in their care (direct and indirect service providers), in primary care, hospital, and elderly residential care settings.
2. Materials and Methods
2.1. Protocol Registration and Guideline
A protocol was registered in Open Science Framework (OSF) on 25 January 2021, prior to commencing the screening process (OSF, DOI 10.17605/OSF.IO/3PEYT). Our evidence map adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [38] when possible (Supplementary File, Table S1).
2.2. Literature Search
The final search strategy was developed in collaboration with an expert librarian. We conducted an electronic search of three databases, MEDLINE, Embase, and Web of Science, from 2019 to 14 January 2021, for publications related to our objectives by using Medical Subject Headings (MeSH) and keywords covering COVID-19, needs assessment, and healthcare needs. Searches were adapted to each database as needed (Supplementary File, Table S2).
2.3. Eligibility Criteria
We identified primary work addressing healthcare and related needs associated with COVID-19 from the perspective of adult patients, their family members, and the professionals involved in their care during the first year of the pandemic. For the purposes of our review, “need” is defined as a lack or scarcity of something that is considered essential. A “healthcare need” may be related to treatment, control, management, or prevention, and care or follow-up care [39]. Related healthcare needs may include social care needs or other. Overall, identified needs may be related to the coronavirus disease itself and its consequences, as well as the relationship with relatives and the work or leisure environment, the relationship with professionals, and the relationship with the healthcare system as an entity differentiated from the people who work in it. “Family” is defined as any group of persons who are related biologically, emotionally, or legally such as siblings, parents, spouses, hired caregivers, significant others, and friends (see Omole et al., 2011 for a similar definition of “family” [40]). The terms “family members” and “relatives” are used interchangeably. “Professionals” are defined as any healthcare worker who delivers care and services either directly (e.g., nurses, physicians, psychologists, social workers) or indirectly (e.g., medical waste handlers, managers, security guards, etc.). There were no restrictions on the type of article (e.g., letters), study design, or study setting (country, healthcare, or social context). Table 1 details the inclusion and exclusion criteria.
Table 1.
Inclusion and exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Primary qualitative and/or quantitative work addressing any healthcare-related needs associated with COVID-19 from the perspective of adult patients, their relatives, and the professionals involved in their care. |
|
Two reviewers (MAB, ADD) independently piloted the eligibility criteria on a sample of 50 articles with the aim of achieving 80% agreement. Given a 92% agreement was reached, the eligibility criteria remained unchanged. Two additional reviewers (HVR, ABR) were subsequently trained on the eligibility criteria to provide support during the screening process and obtained at least an 80% agreement.
2.4. Study Selection
Metadata of all identified articles were uploaded to Rayyan, a free web application designed to help authors conduct systematic reviews [41]. Two reviewers (MAB, ADD, HVR, ABR) independently screened titles and abstracts for their potential inclusion against the eligibility criteria, and MAB and ADD subsequently screened the full text of all included articles to determine eligibility. Any disagreement was resolved by consensus.
2.5. Data Extraction
The data extraction form was piloted by three researchers (MAB, ADD, HVR) independently on five of the included articles and refined prior to extraction. Data were subsequently extracted by one reviewer (ADD) and cross-checked by at least one additional reviewer (MAB, HVR). The following data were extracted: (i) article metadata including citation, publication type (e.g., review, letter), and language of publication, (ii) study characteristics including geographical area, study aim, study setting (e.g., hospital, primary care), study design (e.g., qualitative, quantitative) and methods used to identify needs, and point of contact (i.e., data collection dates and pandemic outbreak phase details), and (iii) population characteristics (e.g., sample size, type of population (participants and population whose needs were identified relevant to our objectives), age, gender).
2.6. Data Coding and Synthesis
We conducted inductive qualitative content analysis. Qualitative content analysis is a descriptive and interpretative, iterative process in which codes are generated and counted and patterns in the data are examined [42,43]. Codes were generated based on careful readings of the data, according to the types of needs identified. Data coding was piloted by three authors (MAB, ADD, HVR) independently on five of the included articles to develop and refine the coding framework. Data coding was completed using the NVivo qualitative research data analysis software for Mac (Release 1.4.1, © QSR International Pty Ltd.). The full text of all included articles was first read to determine eligibility and re-read for the purpose of assigning codes. Articles were re-read more times as needed to review and refine the codes individually and during the process of consensus, and to group conceptually similar codes into overarching themes. The first ten articles were independently coded by two reviewers (MAB, ADD), after which codes and emerging themes were discussed to obtain consensus and further refine the coding framework. The remaining data were subsequently coded by one reviewer (ADD) and cross-checked by a second reviewer (MAB). All codes and emerging themes were iteratively discussed and refined until consensus was reached. Data were narratively synthetized and tables and figures were created to summarize and visually depict the data.
3. Results
3.1. Literature Search and Selection Process
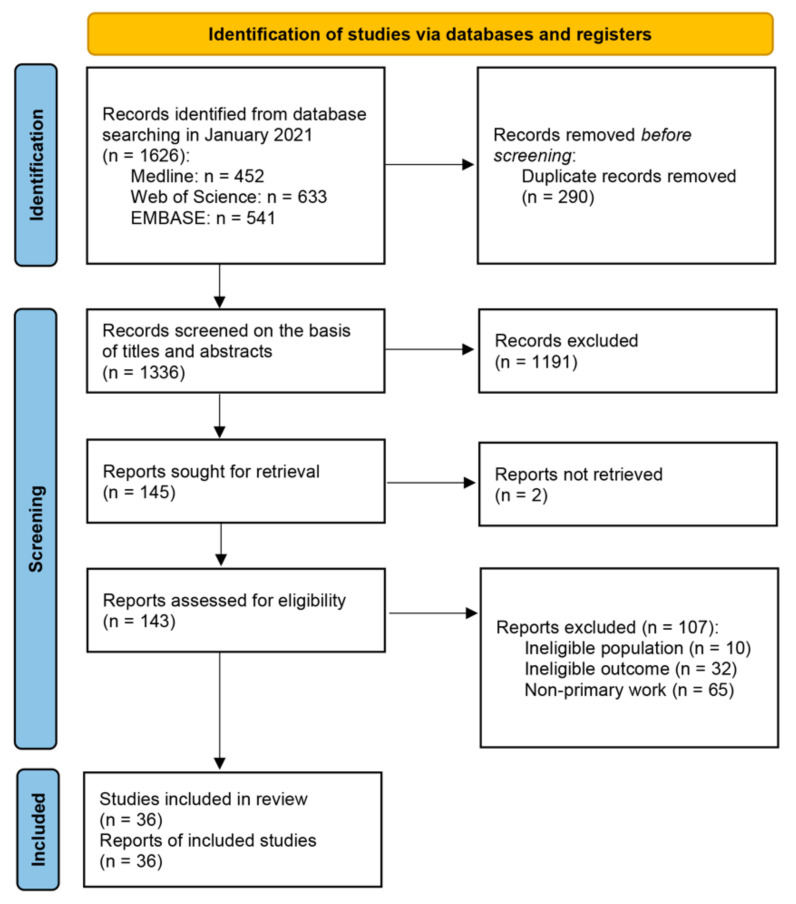
A total of 1626 records were identified from database searching. After removing duplicates, 1336 titles and abstracts were screened, of which 145 remained. A total of 143 full texts were retrieved and assessed for eligibility, of which 36 studies met inclusion criteria (Figure 1). The excluded studies and reasons for exclusion can be found in Supplementary File, Table S3.
Figure 1.
PRISMA flowchart. From: Page et al., (2021) [44].
3.2. Key Characteristics of the Included Studies
The majority of the included studies were published as original research (78%). Studies were conducted in multiple geographical locations: Asia (33%) was the most represented location, followed by Europe (28%), and North America (22%), while only a few studies were performed in Australia (6%), Africa (3%), or represented multiple countries (8%). Healthcare needs were most frequently assessed within hospital settings (44%), followed by studies encompassing professionals in multiple settings (39%). Most of the studies used either qualitative or quantitative methodology for data collection, and fewer studies used mixed methodologies. The majority of needs were identified by professionals, while only one study directly incorporated patient perspectives [45]. No study assessed the first-person perspectives of patients’ relatives. All studies were published in English. Table 2 summarizes the key characteristics of the studies included in this evidence map. Further details of the included studies are presented in Supplementary File, Table S4.
Table 2.
Summary of key characteristics of included studies.
| Variable | n (%) | |
|---|---|---|
| Type of publication | ||
| Original research | 28 (78%) | |
| Brief report | 3 (8%) | |
| Perspective | 2 (6%) | |
| Letter to the editor/commentary | 2 (6%) | |
| Review | 1 (3%) | |
| Geographical location | ||
| Asia | 12 (33%) | |
| Europe | 10 (28%) | |
| North America | 8 (22%) | |
| Multi-country | 3 (8%) | |
| Australia | 2 (6%) | |
| Africa | 1 (3%) | |
| Healthcare setting | ||
| Hospitals | 16 (44%) | |
| Multiple settings | 14 (39%) | |
| Elderly residential care | 2 (6%) | |
| Primary care | 2 (6%) | |
| Community-based | 1 (3%) | |
| Unspecified | 1 (3%) | |
| Study design | ||
| Quantitative | 14 (39%) | |
| Qualitative | 14 (39%) | |
| Mixed | 8 (22%) | |
| Needs identified by | ||
| Professionals | 35 (97%) | |
| Patients | 1 (3%) | |
3.3. Type of Needs and Evidence Clusters
Professionals’ needs were reported by both patients (n = 1) and professionals (n = 34), and so were the unmet needs of patients (patients: n = 1; professionals: n = 12). Family members’ needs were reported by professionals only (n = 13). A set of public health disease prevention needs that affect the health of the population as a whole including professionals, patients, and family members, referred to as transversal needs, were also identified. Transversal needs were reported by both patients (n = 1) and professionals (n = 15). Table 3 presents the main evidence clusters and most frequently reported needs by and across study subgroups. A more detailed description of the type of needs identified in the included studies by and across study subgroups can be found in Supplementary Files, Tables S5–S8.
Table 3.
Main evidence clusters and most frequently reported needs by and across study subgroups.
| Professionals | Patients | Family Members | Transversal Needs | |
|---|---|---|---|---|
| Total No. of Studies | 35/36 (97%) | 13/36 (36%) | 13/36 (36%) | 16/36 (44%) |
| Evidence clusters | Basic needs (n = 16) Occupational needs (n = 34) Psycho-socio-emotional needs (n = 28) |
Basic needs (n = 2) Healthcare needs (n = 11) Psycho-socio-emotional needs (n = 9) Other support needs (n = 8) |
Psycho-socio-emotional needs (n = 8) Communication needs (n = 7) |
Public safety needs (n = 9) Information and communication needs (n = 16) Other needs: Coordination and support (n = 6) |
| Most frequently reported needs |
General or other psychological health resources or support (n = 25) Adequate supply of appropriate personal protective equipment (n = 22) Other information, resources, and procedures to reduce risk of acquiring COVID-19 (n = 24) |
Access to emotional support (n = 5) Family communication and social interaction (n = 6) Access to mental health professionals (n = 6) Access to social support (including social welfare and childcare) (n = 5) |
Communication and social interaction between family and patients or residents (n = 5) Access to psycho-emotional support (n = 5) |
General education and awareness campaigns (n = 11) Clarifying fake news and misinformation (n = 6) Reducing social stigma (n= 6) |
3.3.1. Professionals’ Needs during the First Year of COVID-19
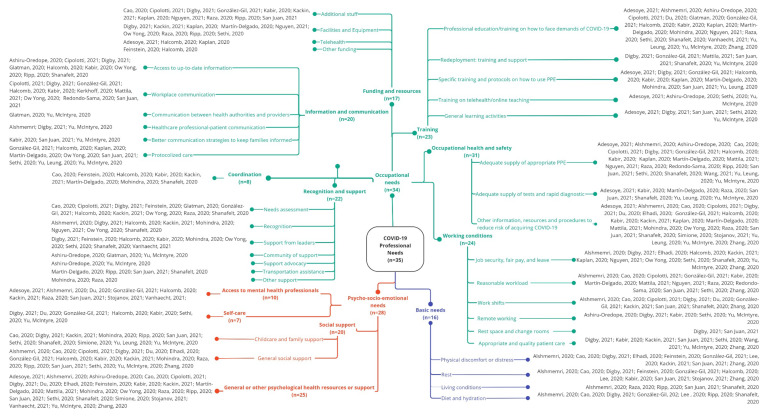
Professionals’ needs were grouped into three main clusters: basic, occupational, and psycho-socio-emotional (Figure 2).
Figure 2.
Healthcare professionals’ needs during the first year of the COVID-19 pandemic [5,13,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77].
3.3.1.1. Basic Needs
Sixteen studies (n = 16) reported basic needs, related to physical discomfort or distress, rest, living conditions, and diet and hydration [5,13,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Across the included studies, healthcare professionals highlighted the need to decrease bodily discomfort and physical distress (e.g., tiredness, excessive sweating, headache, breathing difficulties, etc.), mainly caused by prolonged wearing of PPE [5,13,46,47,48,49,50,51,52,53]. A need for adequate rest in order to remain physically and mentally healthy (both during and after shifts) and be able to provide high-quality care was also reported [5,13,46,47,49,50,51,53,57,58,59]. Many physical and mental challenges of working continuously were noted, which were further exacerbated by sleeping difficulties. Elevated workloads, high patient–professional ratios, and shifts that did not allow for disconnection or rest contributed to these challenges. Healthcare professionals also pointed out the need for lodging support, to adequately self-isolate after the work shift to avoid infecting others, for professionals working long shifts and who do not live close to the health center, and during sick leave [5,13,54,55,56]. Further, healthcare providers stressed the need to have time and access to healthy meals and hydration during and after shifts, especially when wearing PPE and working long shifts [13,46,47,50,51,55,56].
3.3.1.2. Occupational Needs
A wide range of occupational needs were identified in thirty-four studies (n = 34) [5,13,45,46,47,48,49,50,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77], which were grouped into the following seven sub-themes: funding and resources, coordination, information and communication, recognition and support, training, occupational health and safety, and working conditions.
Funding and Resources (n = 17)
An overall need for financial support and additional resources for health services was identified. Professionals highlighted the need for sufficient and adequately trained staff, including the need for additional nurses, doctors, Intensive Care Unit (ICU) workers, mental health staff, and other non-healthcare support staff. This need was related to increased patient volumes, unwillingness to provide services that would place professionals at higher risk of contagion, and sick leave as a high rate of sick leave was observed when more patients with COVID-19 began to emerge [5,46,47,50,52,54,55,58,66,72,73]. Additionally, adequate facilities, equipment (other than PPE), and resource management to meet changing demands were needed, including dedicated staff areas and single rooms, dedicated patient areas for quarantine, dedicated air-conditioning and circulation systems, and sufficient supplies, medications, and beds [47,52,54,55,60,61,62,72,73]. In regard to telehealth services, the following needs were identified: government support, and support establishing services across settings including specific funding to facilitate the transition and reserve in-person visits for patients needing physical attention [57,63,73]. Other financial support and resources for health services were identified, such as the ability for professionals to provide and bill for services different from the regular services, and overall financial support through public–private donations [49,57].
Coordination (n = 8)
A need to improve coordination activities was identified. Professionals perceived a lack of task coordination and hoped there could be a more specific task division, as redeployment processes and changes in the working units made it difficult to work with different and changing team members. A clear chain of command in the management and execution of plans, in-person consultation with physicians, and empowerment to delegate tasks and defer less important and time-sensitive activities were also identified as needs [46,49,52,56,57,58,60,71].
Information and Communication (n = 20)
Professionals highlighted the need for support concerning the provision of concise, timely, up-to-date, and clear information about the pandemic, so they did not have to research everything themselves (e.g., patient management, infection control protocols, local information, noncontradictory information, etc.) [47,55,56,57,58,61,64,65,66,68]. The need for improved intra- and inter-professional communication was also reported by both patients and professionals, including improved communication between colleagues, team members, and the different services [5,45,47,50,57,58,61,66,67,68]. Accordingly, professionals requested more time to meet with supervisors and colleagues, and staff meetings to discuss as a group the best plan moving forward. There was also a need to improve communication between health authorities and providers to better respond to the emergency situation [65,69], and a need to improve healthcare professional-patient communication, especially when telehealth was used as a substitute for most face-to-face clinic appointments [13,47,69]. Better communication strategies between health authorities, health providers, and families were needed in order to keep families fully informed, particularly when it involved patients in the ICU or when patients were dying [5,58,69]. Finally, the need for standardized, implementable protocols to govern clinical care and logistic planning was noted. Professionals reported the need for additional guidance, such as having access to a go-to person for any clarification on procedures and protocols related to COVID-19 [5,50,57,60,61,62,69,70,73].
Recognition and Support (n = 22)
Healthcare professionals emphasized the importance of listening to their perspectives and experiences to identify and rapidly address their needs via tangible actions [46,47,49,50,52,54,56,57,61,65,66]. Professionals wanted to be consulted or be actively involved in decision-making processes, and be regularly updated on the issues that affected them. Moreover, recognition of the vital role played by all professionals during the pandemic emerged as an important unmet need, including frontline and backline professionals [13,47,52,56,57,61,71,72]. The genuine expression of gratitude by the general population is powerful, but professionals stated that this recognition should also come from patients, colleagues, supervisors, managers, organizations, and insurance companies, in the form of real-time support, visible leadership within the workplace and within the profession, and actionable plans [47,49,56,57,58,61,62,71,74]. Accordingly, it was deemed necessary to establish COVID-19 communities of support [64,65,69]. The need for support advocacy for professionals’ safety, education, and delivery of care from national and international healthcare associations was also identified [64,69]. Other support needs such as transportation assistance [5,55,56,60], and overall support from the state, the community, and family, particularly for women, were highlighted [54,71].
Training (n = 23)
Training-related needs were one of the main occupational needs identified by healthcare professionals. They perceived a need to receive professional education and training on how to face the demands and complexity of COVID-19 to support the provision of high-quality care to patients during the first year of the pandemic (symptoms, transmission pathway, screening procedures, treatment, patient management, counseling skills, working with vulnerable populations, infection control, etc.) [13,50,53,54,56,57,58,60,62,63,64,65,66,69,70,71,72,73,74,75]. Healthcare professionals also needed to receive specific training on how, when, and where to wear PPEs as they reported fear of not using it properly because of the lack of adequate instructions or practice and frequently changing requirements [5,47,50,57,58,60,63,70,71,73]. We also identified the need for sufficient training and support in preparation for redeployment and during the onboarding process to work in clinical areas that were outside professionals’ usual scope of practice [5,47,50,56,67,69]. Similarly, the transition to online services was a huge challenge for some professionals and for organizations in general, and receiving specific training on telehealth and online teaching was stated as a possible way to overcome this challenge [62,63,64,69]. Some issues identified as barriers to providing virtual care included a lack of familiarity with the different technological systems and the logistics of scheduling and billing for virtual visits. Finally, some studies highlighted the need to minimize COVID-19’s impact on general learning activities including medical education and research, as doctors in training faced uncertainty regarding examinations and courses that had been paused, which in turn could impact the trainees’ preparedness for independent practice [5,47,62,63,69].
Occupational Health and Safety (n = 31)
The need for an adequate and timely supply of appropriate PPE, at low or no cost, and ways to preserve existing PPE was one of the most frequently reported needs from the perspective of healthcare professionals (e.g., N95 masks, face shields, alcohol, and different gowns for different departments and healthcare settings) [5,13,46,47,50,54,55,56,57,58,60,62,63,64,66,67,68,69,70,72,73,76]. The unavailability and substandard quality of PPE were indeed one of the major causes of professionals’ frustration and distress. An adequate supply of tests, access to testing through occupational health, and rapid diagnosis for all staff, when necessary, was also needed to ensure the health and safety of professionals [5,54,56,58,60,63,69,70]. Moreover, based on professionals’ constant fear of self-infection (especially those at high risk because of age or health conditions) or spreading the virus to their families, friends, and patients, the need for up-to-date information, resources, and procedures aimed to reduce the risk of becoming infected or being a portal for disease transmission was noted (e.g., accommodation, insurance for all, designated floors, negative pressure airborne infection isolation rooms, etc.) [5,13,46,47,48,50,52,53,54,56,57,58,59,60,61,63,66,67,69,70,71,73,75,77].
Working Conditions (n = 24)
Ethical dilemmas emerged due to worsening working conditions. Job security, fair pay and sick leave arose as one of the main needs of healthcare professionals in this subtheme [13,47,48,52,53,56,57,61,62,69,72,73]. They stated the importance of having financial stability and support and a clear understanding of the human resources policies. Reasonable workloads [5,13,46,50,53,54,58,60,62,66,67,68,72] and suitable work shifts [5,13,46,47,50,52,53,56,66,75] were also identified as two important concerns to healthcare workers during the first year of COVID-19. Healthcare workers expressed concerns about the emotional impact of working continuously under challenging circumstances, with frequent changes to processes and procedures, and being unable to provide high-quality care, as the workload increased substantially as staff became ill. They reported decreased concentration after working long hours, in part due to high patient-professional ratios and night shifts that did not allow them to disconnect or rest, amplifying the need to hire additional staff. Access to rest spaces, change rooms, and lunchrooms were also needed to alleviate the strenuous working conditions [5,47].
Professionals who transitioned to work remotely expressed the need to implement high-quality telehealth services, and for organizations and professionals to adjust to the specific conditions of remote working [47,58,62,64,69]. Remote working was a positive experience for some, with fewer interruptions, less commuting time, and more flexibility. In other cases, the home environment was unsuitable for working remotely due to poor internet connection, noisy or distracting housemates (including children), or inadequate space and facilities. Decreased quality of care was also reported for patients without COVID-19, especially those with chronic conditions, during end-of-life care, for care home residents, and for clinical rehabilitation services. Accordingly, healthcare professionals stated the need to provide appropriate and high-quality care even during the peak of the pandemic [5,47,52,53,58,62,69,76].
3.3.1.3. Psycho-Socio-Emotional Needs
Twenty-eight studies (n = 28) reported psycho-socio-emotional needs from the perspective of professionals. These were grouped into the following four subthemes: Access to mental health professionals, self-care strategies, social support, and general or other psychological health resources or support [5,13,46,47,48,49,50,52,53,54,55,56,57,58,59,60,61,62,63,64,66,67,69,70,71,74,75,77].
Access to Mental Health Professionals (n = 10)
Psychological health was highlighted as a major concern during the first year of the pandemic. In a time of extreme work hours, uncertainty, and intense exposure to critically ill patients, professionals voiced the need to have access to mental health professionals [5,13,50,52,54,57,59,63,74,75]. Therapeutic options needed varied and included individual or group sessions, in-person or online, and short- (e.g., channel or helpline) or long-term support provided by psychologists and therapists in related fields.
Self-Care (n = 7)
Self-care is a “multidimensional, multifaceted process of purposeful engagement in strategies that promote healthy functioning and enhance well-being” [78]. Across the included studies, a need for organizations to encourage professionals’ self-care and for professionals to engage in self-care in order to enhance wellbeing was identified (e.g., limiting exposure to media, psycho-education, expressing feelings, meditation, yoga or other relaxation techniques, exercise, singing, writing or other recreational activities) (Although social support is also perceived as a self-care practice, it was coded separately given emphasis and frequency noted) [47,50,52,57,62,69,75].
Social Support (n = 20)
Many staff members had to distance themselves from family and friends due to work (e.g., long work hours, self-imposed or ordered quarantines) or their loved ones’ fears of becoming infected. In a context where the usual social networks and leisure activities used by healthcare workers to de-stress were restricted, the need for other forms of social support and social connection was highlighted (e.g., vent emotions with supportive people, informal peer support groups, virtual educational activities, video chat with family and friends) [5,13,46,47,48,50,52,53,54,55,57,58,62,66,69,71,75]. Healthcare professionals also highlighted the need for childcare and family support, including financial support, as work hours and demands increased and schools and daycare closures occurred [5,46,47,52,55,56,62,69,70,71,77].
General Psychological Health Support or Other Psychological Health Resources (n = 25)
During the first year of COVID-19, a mental health crisis began to emerge in healthcare workers. Healthcare professionals worldwide experienced high levels of stress, anxiety, and depression, which directly affected patient care and professionals’ personal and family wellbeing. Hence, most of the included studies deemed the need for other resources and general psychological health support to help healthcare workers cope with emotional symptoms and anticipate mental health needs [5,13,46,47,48,49,52,53,54,55,56,58,59,60,61,62,63,64,66,67,69,71,74,75,77].
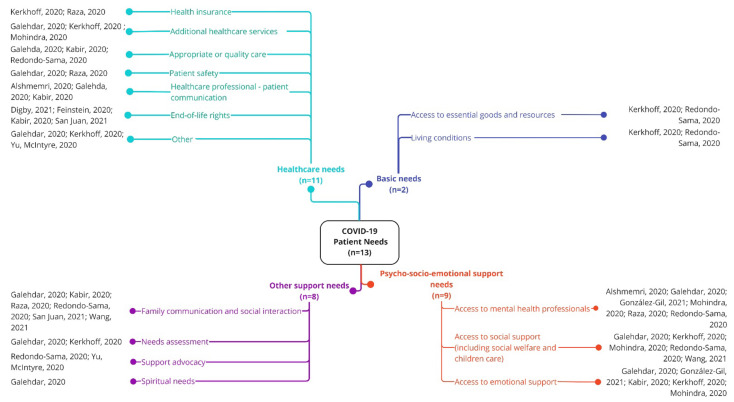
3.3.2. Patients’ Needs during the First Year of COVID-19
Patients’ needs were grouped into four main clusters: basic, healthcare, psycho-socio-emotional, and other support needs (Figure 3).
Figure 3.
Patients’ needs during the first year of the COVID-19 pandemic [5,13,24,45,47,49,50,54,58,68,69,71,76].
3.3.2.1. Basic Needs
Basic needs, including access to essential goods and resources, and lodging support, were identified in two studies (n = 2) [45,68]. As the pandemic spread, patients required support for urgent and regular home deliveries of essential supplies during isolation (e.g., food, PPE, cleaning supplies, hygiene products, supportive care medication) [45,68]. Additionally, patient’s identified the need to access information and services in their preferred language [45]. Finally, a need for lodging support for patient’s to safely isolate also emerged, related to shared living spaces or homelessness [45,68].
3.3.2.2. Healthcare Needs
Patients’ healthcare needs were highlighted in eleven studies (n = 11) [5,13,24,45,47,49,54,58,68,69,71]. The need for support obtaining healthcare coverage was essential in those countries without public health services [45,54]. A deep concern emerged because of the unrealistic charges per day COVID-19 patients needed to afford. The need to improve the quality of care for all people during the pandemic was highlighted, in particular for vulnerable populations such as low-income families, patients with underlying conditions, care home residents, elderly, and homeless people [24,58,68]. Accordingly, some studies pointed out the need to receive additional short- and long-term quality healthcare services, such as nutritional, counseling, and rehabilitative care [24,45,71]. Patient safety was another concern, as in some cases, the isolation wards lacked the necessary facilities and equipment. Patients must always come first, and to ensure patient safety, adhering to internationally recognized standard procedures and patient safety strategies is needed [24,54]. Further, the need to improve professional-patient communication was noted [13,24,58]. Building strong connections with patients and providing emotional support could alleviate negative feelings related to isolation, physical problems, and the lack of a definitive treatment. During the first year of COVID-19, the idea that patients could die alone was particularly distressing. In this respect, four studies in different countries highlighted the need to preserve patient rights during end-of-life care and immediately after death [5,47,49,58]. Finally, the need to address other healthcare needs arose, including hospital environmental familiarization, the need for patients to be fully informed of their health status, the need to facilitate low-barrier testing for close contacts, and the need for up-to-date and clear information on COVID-19 and rehabilitation [24,45,69].
3.3.2.3. Psycho-Socio-Emotional Needs
Psycho-socio-emotional needs for patients with COVID-19 were identified in nine studies (n = 9) [13,24,45,50,54,58,68,71,76]. As COVID-19 patients might suffer from many mental health concerns (e.g., death anxiety, social stigma, hopelessness, separation anxiety) during and after the disease, the need for access to mental health professionals was noted [13,24,50,54,68,71]. Additionally, the need for low-barrier social support services, including childcare and social welfare of the patient and their family, to mitigate economic concerns was identified [24,45,68,71,76]. Furthermore, emotional support for COVID-19 patients was highlighted as a primary requirement, including more informal support (e.g., general affection, peer support groups) and also the need to implement screening programs to identify patients in need of psychological counseling [24,45,50,58,71].
3.3.2.4. Other Support Needs
Finally, eight studies (n = 8) identified other support needs for COVID-19 patients during the first year of the pandemic [5,24,45,54,58,68,69,76]. First, continuous communication and social interaction with family and friends was stated as one important unmet need [5,24,54,58,68,76]. As humans are social beings, special attention should be paid to patients isolated due to COVID-19 to decrease feelings of homesickness and loneliness during this period. Accordingly, allowing patients to communicate with their families and relatives during isolation and hospitalization was highlighted. Patients’ perspectives are key to providing comprehensive patient care. For this reason, patients’ needs should be continuously assessed, identified, and addressed [24,45]. Given the uncertainties and the changes to healthcare and community resources resulting from policies aimed to manage the pandemic, all patients with COVID-19, but especially vulnerable patients, such as older patients and people with disabilities, would benefit from support advocacy [68,69]. Finally, one study highlighted spiritual care is needed to provide comprehensive care as it gives patients mental peace [24].
3.3.3. Family Members’ Needs during the First Year of COVID-19
Family members’ needs were grouped into two main clusters: psycho-socio-emotional and communication (Figure 4).
Figure 4.
Family members’ needs during the first year of the COVID-19 pandemic [5,24,47,49,50,54,58,66,68,69,71,75,76].
3.3.3.1. Psycho-Socio-Emotional Needs
Psycho-socio-emotional needs of patients’ relatives were identified in eight studies (n = 8) [5,47,49,50,66,68,71,75]. It was noted that family members of COVID-19 patients needed psychological and/or emotional support during and after the patient’s acute illness, including during the mourning process [49,50,66,68,75]. Some studies also highlighted the need of providing social support to family members, including financial support to mitigate economic concerns, and childcare assistance while infected patients were hospitalized [50,68,71]. Finally, the need for families to accompany dying patients whenever possible was stressed [5,47,49].
3.3.3.2. Communication Needs
Seven studies (n = 7) included communication needs [5,54,58,68,69,76]. As during the first year of the pandemic visits were mostly forbidden, there was a need for better communication between health authorities, health professionals, and families to keep families informed [5,58,69]. Families often had to hear difficult-to-understand information about their relatives’ health status over the telephone, rather than in person, and this lack of face-to-face communication made interacting with families of dying patients even more challenging. Moreover, the need for continuous communication (e.g., regular updates of the patients/relatives’ health status) and interaction between family and patients/residents was noted [5,24,54,68,76].
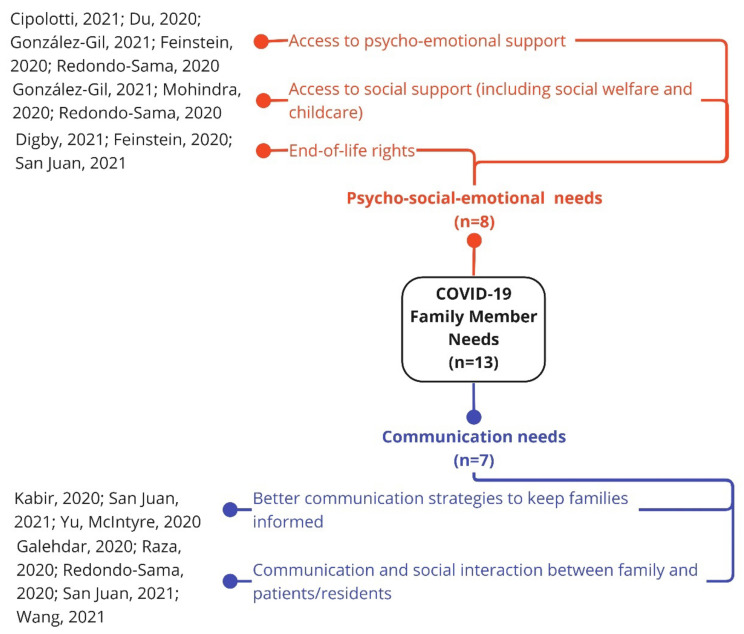
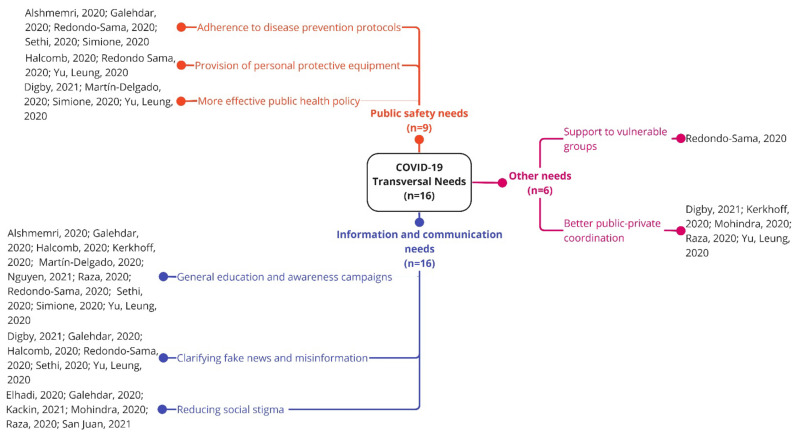
3.3.4. Transversal Needs during the First Year of COVID-19
Transversal needs were grouped into three main clusters: public safety needs, information and communication needs, and other needs (Figure 5).
Figure 5.
Transversal needs during the first year of the COVID-19 pandemic [5,13,24,45,47,48,52,54,57,60,62,68,70,71,72,77].
3.3.4.1. Public Safety Needs
Public safety needs were identified in nine studies (n = 9). Needs in this cluster elucidated the importance for the general public to adhere to disease prevention protocols [13,24,62,68,77], need for the government and/or health authorities to provide professionals and the general population with PPE to minimize the spread of the virus [57,68,70], and overall need for more effective public health policies to contain the outbreak (e.g., border control and/or quarantine measures for returning residents and travelers, follow up of asymptomatic cases, more restrictive containment measures) [47,60,70,77].
3.3.4.2. Information and Communication Needs
Information and communication transversal needs were identified in sixteen studies (n = 16). To avoid spreading the virus, culturally tailored health-related and COVID-19 education and awareness should be improved in the general public (e.g., principles of disease prevention, awareness of risks, symptoms and linkage to care, instructions about where to get tested) [13,24,45,54,57,60,62,68,70,72]. Additionally, fake news and misinformation should be rapidly clarified [24,47,57,62,68,70]. Moreover, efforts should be undertaken to reduce social stigma [5,24,48,52,54,71]. Social stigma was one of the causes of patients’ anxiety as they feared social rejection, and a major cause of suppression of travel history and incompliance with transmission prevention strategies.
3.3.4.3. Other Needs
Other needs related to coordination and support were identified in six studies (n = 6). More specifically, the need for coordinated care between the public and private sectors was noted [45,47,54,70,71], as well as the need to provide support to vulnerable groups to minimize the spread of the virus, including the provision of basic needs (food, housing, access to shower, etc.) [68].
4. Discussion
Early on in the pandemic, COVID-19 caused serious repercussions to daily life that were felt across the globe, raising social, economic, political, and global safety concerns. As a first step towards identifying health systems’ limitations to subsequently improve their resilience and preparedness for future global crises, it is important to explore how COVID-19 first affected healthcare workers, patients, and families. To the best of our knowledge, this is the first study to map knowledge clusters and gaps regarding healthcare and related needs of adult patients, their family, and the professionals involved in their care during the first year of the COVID-19 pandemic.
4.1. Evidence Clusters
The impact of this pandemic on the physical and mental health of healthcare professionals has been highlighted in several reports since the initial outbreak. A plethora of studies examined the prevalence of mental health symptoms in healthcare professionals facing the pandemic on the front line, reporting moderate and high levels of stress, anxiety, depression, sleep disturbance, and burnout [79,80,81]. In the aftermath of the COVID-19 outbreak, healthcare professionals had to work under extreme pressure and needed to balance conflicting demands related to their own physical and mental health as well as those of colleagues, patients, and family members [54]. The evidence suggests that professionals’ occupational and psycho-socio-emotional needs are intertwined, as clinical well-being is heavily influenced by organizational factors of well-being. Different studies have pointed out several work-related risk factors that may lead to increased occupational stress and emotional exhaustion, including access to or prolonged use of PPE, increased work pressure, lack of social support from colleagues and supervisors, and prolonged work hours [82,83]. A perceived risk or fear of COVID-19 can also contribute to mental health problems [84]. The lack of PPE and the subsequent fear of becoming a portal of transmission were two of the most common causes of frustration and distress in the included studies, which makes this especially relevant. Even when PPE was available, healthcare workers voiced the need for specific training on how, when, and where to wear PPE. Accordingly, recent studies with frontline healthcare workers have suggested that access to high-quality PPE and in-person training on how to use them, should be the minimum standard to prevent transmission and ensure safety. Greater confidence in using PPE also correlates with an improved workplace culture [85]. Our results suggest that mental health support strategies and easy-to-implement, flexible, and effective mental health interventions for healthcare professionals should be incorporated into pandemic preparedness plans, while improving working conditions and developing mechanisms to increase occupational safety in these high-risk clinical settings. To date, most interventions have mainly focused on the individual level, but proactive organizational approaches are also needed and could be less stigmatizing [83], especially when the threshold for healthcare professionals to seek help might be higher compared to other population groups [67]. Finally, to develop effective approaches to support healthcare providers, it is essential for providers to be involved in the decision-making process.
In regard to patients, ensuring that all patients have access to essential goods, services, lodging support and information should be an aspect included in preparedness plans. Several articles highlight the need to improve the healthcare service quality (e.g., improve hospital facilities and equipment) in order to guarantee that all patients receive high-quality care. This stresses the importance of providing universal access to health services to ensure that all patients get adequate treatment. Improving communication between patients and healthcare professionals is another key aspect that needs to be considered: the current healthcare environment affords little time with each patient, and this can impede effective patient-professional communication. Patient-centered interviewing, caring communication skills, and shared decision making are strategies known to improve patient-professional communication [86]. Given the serious nature of the COVID-19 outbreak, it is not surprising that a high proportion of patients experienced depression, anxiety, and post-traumatic symptoms [81,87]. Therefore, early detection and appropriate treatment of mental health symptoms are required in patients with COVID-19, both during and after acute symptom resolution, in order to reintegrate with society and family life [88].
COVID-19 has also had a profound impact on patients’ relatives. Deleterious effects on the quality of life of the survivors’ family members have been reported, with partners being most impacted. According to Shat et al. [89], many family members reported being worried and frustrated, and experienced sadness and difficulties in caring for their loved ones. Similarly, Kentish-Barnes et al. [90] found that having a loved one who died or was close to death and reporting poor communication with the healthcare professionals are risk factors for psychological burden. In line with other work, we identified several psycho-socio-emotional and communication needs. The establishment of family-centered services to provide support to patients with COVID-19 and their family members is therefore a key consideration in the future management of this pandemic and possibly other serious threats.
4.2. Evidence Gaps
Some important evidence gaps have been highlighted in our work. First, more studies focusing on first-person perspectives from patients and family members are needed. However, based on the needs identified, moving forward, organizations should plan to implement comprehensive strategies of care that include specific family-centered guidelines for crisis management and respect the voices of patients and their families [90]. Our results indicated the need for low-cost and low-barrier access to support for patients and families, including: basic needs (lodging support, access to essential goods, and access to information and services in patients’ preferred language), healthcare coverage, mental health and social support services, and other. Similarly, more effective public health initiatives are needed, particularly targeting vulnerable populations. As stated by Chua et al. [91], preparedness for future pandemics and global health crisis requires adopting more inclusive responses that protect all individuals, including the elderly, low-income, homeless, and disabled people. Health literacy is key to empowering individuals and their communities and can be used as a tool to promote public safety during health emergencies.
Furthermore, addressing the barriers to implementing organizational changes to support wellbeing is needed, as addressing the wellbeing of healthcare professionals requires a whole system participatory approach [5]. Our work demonstrated organizational factors such as shift planning, workload, communication within the workplace, visible leadership, involvement in decision-making processes, etc., need to be addressed in addition to providing psycho-socio-emotional support.
We identified a further research gap in a lack of studies performed beyond Asia, Europe, and North America, especially in low-income countries. A more comprehensive understanding of the healthcare and social needs arising from the first COVID-19 outbreaks worldwide will require more insights from Africa and other underrepresented regions, such as Oceania and South and Central America.
Finally, as we only focused on the first year of the COVID-19 pandemic, more research is required to assess how needs evolved over time and which unforeseen needs arose as the outbreak progressed (e.g., rehabilitation needs, vaccination-related issues). The identified needs will need to be prioritized and addressed.
4.3. Implications for Practice
A wide variety of improvement opportunities emerged from this study. Policymakers, managerial staff, and clinicians can learn from this mapping exercise by promoting better preparedness and resilience at multiple levels. Researchers, on the other hand, should test and evaluate the effectiveness of interventions tailored to meet the identified needs, at different levels:
Macro-level Interventions
Promote channels of information and official communication on a regular basis that is up-to-date, concise and clear; facilitate staff hiring processes or streamline external subcontracting of services.
Meso-level Interventions
Setting up coordination teams to channel and structure training and information needs, so that high-quality care can be delivered while ensuring that decision making involves multiple stakeholders. Develop an emergency response plan adapted to pandemics, including specific actions, roles, and responsibilities defined with a multisectoral approach and integration of primary and residential care. These plans should include adequate facilities (e.g., isolation rooms), resource management protocols and other easy-to-implement protocols; material resources, support, and training for professionals; and accompaniment of patients at home. Attention to the mental health of professionals and patients should be ensured, favoring access to mental health professionals, evidence-based self-care practices and social support, including peer teams (similar to already tested strategies for second victims of adverse events) or self-help groups adapted to pandemic status and local idiosyncrasy/culture.
Clinical level Interventions
Emphasis on person and kin-centered care, facilitating clear and reliable communication with patients and families, establishing liaison professionals or volunteers, and streamlining the use of new technologies to maintain connections and social relationships. Establishment of specific end of life care channels to ensure support and care for COVID and non-COVID pathologies.
4.4. Strengths and Limitations
A major strength of this study is that we used a broad-based search strategy and selection criteria, with no restrictions on the type of article, study design, or setting. Moreover, the qualitative content analysis employed allows for rich description while able to summarize the evidence via frequency count. However, this evidence map also presents some limitations. Our findings only included published peer-reviewed work, which has been limited by the pressing needs caused by COVID-19, leaving out potentially non-published but relevant work. A search for backward and forward citations was not performed, nor did we include gray literature. A quality analysis of the included studies was not conducted, although this is not a requirement for evidence maps. In addition, some of the needs and gaps identified during the first year of the pandemic have already largely been addressed, such as the need for an adequate supply of appropriate PPE for professionals [92]. Nevertheless, this information will be useful in facilitating the preparation of health systems for future pandemics. Other identified needs and gaps, however, are still current and pressing, such as the need to improve access to mental health professionals; efforts should be undertaken to prioritize and address them. While our focus was on the early phases of the COVID-19 pandemic, further research should focus on more recent needs (e.g., those related to vaccination and long-term consequences of COVID-19). Moreover, the generalizability of the results is limited as some geographical areas such as Africa, Oceania, and South and Central America are underrepresented. Finally, most of the reviewed evidence was based on healthcare professionals’ viewpoints, with only one study directly incorporating patient experiences and none addressing family members’ first-person perspectives.
5. Conclusions
This evidence map provides valuable insight on healthcare-related needs associated with COVID-19 from the perspective of patients and professionals based on the first year of the pandemic, by: describing key COVID-19-related healthcare needs, identifying knowledge clusters and gaps, and highlighting improvement opportunities that may facilitate multilevel preparedness and resilience. This work elucidated the need for more first-person perspectives from patients and family members. Altogether, our results indicate COVID-19 amplified the need to provide person and kin-centered care, and for health systems to better prepare for public health emergencies, and better support the workforce through organizational approaches to wellbeing. Given the profound multifaceted impact of the pandemic, addressing current healthcare-related needs should be prioritized. Further research is needed to identify which of the identified needs are more relevant, develop initiatives to address those needs, and detect barriers to implementation. Additional research is also warranted to assess whether needs differ by country or region, and to evaluate how needs have evolved over time given the magnitude and dynamic nature of the COVID-19 pandemic.
Acknowledgments
We are appreciative of all the healthcare workers for the work and care provided during the COVID-19 pandemic. The authors would also like to thank Leticia Rodríguez-Rodríguez for her support in conducting the literature search and Ana Blanco Rubio with her assistance during the screening process.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph191610332/s1, Table S1: PRISMA checklist; Table S2: Search strategy used in the consulted databases; Table S3: List of excluded studies and reasons for exclusion; Table S4: Descriptive summary of included studies; Table S5: Description of the type of needs identified for professionals; Table S6: Description of the type of needs identified for patients; Table S7: Description of the type of needs identified for family members; Table S8: Description of the identified transversal needs.
Author Contributions
Conceptualization, C.O., L.P.-P., A.I.G.-G., M.A.B. and A.D.-D.; methodology, M.A.B.; formal analysis, M.A.B. and A.D.-D.; investigation, M.A.B., A.D.-D. and H.V.-R.; resources, C.O. and L.P.-P.; data curation, M.A.B. and A.D.-D.; writing—original draft preparation, M.A.B. and L.S. (introduction), M.A.B. (methods and conclusion), A.D.-D. (results), M.A.B., A.D.-D., C.O. and H.V.-R. (discussion); writing—review and editing, all authors; visualization, M.A.B., A.D.-D. and L.S.; supervision, C.O., L.P.-P. and A.I.G.-G.; project administration, M.A.B. and A.D.-D.; funding acquisition, C.O., L.P.-P. and A.I.G.-G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Hospital Universitario 12 de Octubre (No.: 20/608).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was funded by the Foundation for Biosanitary Research and Innovation in Primary Care (FIIBAP) and the Regional Ministry of Health of the Community of Madrid through non-refundable grants from the credits awarded to the Community of Madrid by the Spanish Government Fund COVID-19, included in Order HAC/667/2020.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O., Ippolito G., Mchugh T.D., Memish Z.A., Drosten C., et al. The Continuing 2019-NCoV Epidemic Threat of Novel Coronaviruses to Global Health—The Latest 2019 Novel Coronavirus Outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Announces COVID-19 Outbreak a Pandemic. [(accessed on 21 April 2022)]. Available online: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic.
- 3.Legido-Quigley H., Mateos-García J.T., Campos V.R., Gea-Sánchez M., Muntaner C., McKee M. The Resilience of the Spanish Health System against the COVID-19 Pandemic. Lancet Public Health. 2020;5:e251–e252. doi: 10.1016/S2468-2667(20)30060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Litewka S.G., Heitman E. Latin American Healthcare Systems in Times of Pandemic. Dev. World Bioeth. 2020;20:69–73. doi: 10.1111/dewb.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Juan V.N.S., Aceituno D., Djellouli N., Sumray K., Regenold N., Syversen A., Symmons S.M., Dowrick A., Mitchinson L., Singleton G., et al. Mental Health and Well-Being of Healthcare Workers during the COVID-19 Pandemic in the UK: Contrasting Guidelines with Experiences in Practice. BJPsych Open. 2021;7:E15. doi: 10.1192/bjo.2020.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rana B.K. COVID-19 Response in South-East Asia: Promoting Healthcare Quality through Political Engagement. IJQHC Commun. 2022;1:lyab009. doi: 10.1093/ijcoms/lyab009. [DOI] [Google Scholar]
- 7.McMahon M., Nadigel J., Thompson E., Glazier R.H. Informing Canada’s Health System Response to COVID-19: Priorities for Health Services and Policy Research. Healthc. Policy. 2020;16:112–124. doi: 10.12927/hcpol.2020.26249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bramucci A., Prante F., Truger A. Decades of Tight Fiscal Policy Have Left the Health Care System in Italy Ill-Prepared to Fight the COVID-19 Outbreak. Intereconomics. 2020;2020:147–152. doi: 10.1007/s10272-020-0886-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vasileiou E. Fighting a War without Weapons? Lessons from the COVID-19 Outbreak. World Med. Health Policy. 2021;13:383–390. doi: 10.1002/wmh3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alqahtani F., Khan A., Alowais J., Alaama T., Jokhdar H. Bed Surge Capacity in Saudi Hospitals during the COVID-19 Pandemic. Disaster Med. Public Health Prep. 2021;19:1–7. doi: 10.1017/dmp.2021.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu H., Intrator O., Bowblis J.R. Shortages of Staff in Nursing Homes during the COVID-19 Pandemic: What Are the Driving Factors? J. Am. Med. Dir. Assoc. 2020;21:1371–1377. doi: 10.1016/j.jamda.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lupu D., Tiganasu R. COVID-19 and the Efficiency of Health Systems in Europe. Health Econ. Rev. 2022;12:14. doi: 10.1186/s13561-022-00358-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alshmemri M.S., Ramaiah P. Nurses Experiences and Challenges during COVID 19: Mixed Method Approach. J. Pharm. Res. Int. 2020;32:81–87. doi: 10.9734/jpri/2020/v32i3130920. [DOI] [Google Scholar]
- 14.Ramaci T., Barattucci M., Ledda C., Rapisarda V. Social Stigma during COVID-19 and Its Impact on HCWs Outcomes. Sustainability. 2020;12:3834. doi: 10.3390/su12093834. [DOI] [Google Scholar]
- 15.Norful A.A., Rosenfeld A., Schroeder K., Travers J.L., Aliyu S. Primary Drivers and Psychological Manifestations of Stress in Frontline Healthcare Workforce during the Initial COVID-19 Outbreak in the United States. Gen. Hosp. Psychiatry. 2021;69:20–26. doi: 10.1016/j.genhosppsych.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martinez M., Stewart N.H., Koza A.L., Dhaon S., Shoushtari C., Arora V.M. The Effect of Redeployment during the COVID-19 Pandemic on Development of Anxiety, Depression, and Insomnia in Healthcare Workers. J. Gen. Intern. Med. 2022;37:1003–1005. doi: 10.1007/s11606-021-07253-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ballantyne H., Achour N. The Challenges of Nurse Redeployment and Opportunities for Leadership during COVID-19 Pandemic. Disaster Med. Public Health Prep. 2022;14:1–7. doi: 10.1017/dmp.2022.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang A.Y., Cullen M.R., Harrington R.A., Barry M. The Impact of Novel Coronavirus COVID-19 on Noncommunicable Disease Patients and Health Systems: A Review. J. Intern. Med. 2021;289:450–462. doi: 10.1111/joim.13184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Golinelli D., Sanmarchi F., Capodici A., Gribaudo G., Altini M., Rosa S., Esposito F., Fantini M.P., Lenzi J. Variations of the Quality of Care during the COVID-19 Pandemic Affected the Mortality Rate of Non-COVID-19 Patients with Hip Fracture. PLoS ONE. 2022;17:e0263944. doi: 10.1371/journal.pone.0263944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tuczyńska M., Staszewski R., Matthews-Kozanecka M., Żok A., Baum E. Quality of the Healthcare Services during COVID-19 Pandemic in Selected European Countries. Front. Public Health. 2022;10:870314. doi: 10.3389/fpubh.2022.870314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curnow E., Tyagi V., Salisbury L., Stuart K., Melville-Jóhannesson B., Nicol K., McCormack B., Dewing J., Magowan R., Sagan O., et al. Person-Centered Healthcare Practice in a Pandemic Context: An Exploration of People’s Experience of Seeking Healthcare Support. Front. Rehabil. Sci. 2021;2:726210. doi: 10.3389/fresc.2021.726210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sandhu S., Lemmon M.E., Eisenson H., Crowder C., Bettger J.P. Addressing the Social Determinants of Health during the COVID-19 Pandemic: Ensuring Equity, Quality, and Sustainability. Fam. Community Health. 2021;44:78–80. doi: 10.1097/FCH.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 23.Wittenberg E., Goldsmith J.V., Chen C., Prince-Paul M., Johnson R.R. Opportunities to Improve COVID-19 Provider Communication Resources: A Systematic Review. Patient Educ. Couns. 2021;104:438–451. doi: 10.1016/j.pec.2020.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galehdar N., Toulabi T., Kamran A., Heydari H. Exploring Nurses’ Perception about the Care Needs of Patients with COVID-19: A Qualitative Study. BMC Nurs. 2020;19:119. doi: 10.1186/s12912-020-00516-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen C., Haupert S.R., Zimmermann L., Shi X., Fritsche L.G., Mukherjee B. Global Prevalence of Post COVID-19 Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022 doi: 10.1093/infdis/jiac136. ahead of print . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Groff D., Sun A., Ssentongo A.E., Ba D.M., Parsons N., Poudel G.R., Lekoubou A., Oh J.S., Ericson J.E., Ssentongo P., et al. Short-Term and Long-Term Rates of Postacute Sequelae of SARS-CoV-2 Infection: A Systematic Review. JAMA Netw. Open. 2021;4:e2128568. doi: 10.1001/jamanetworkopen.2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Brien H., Tracey M.J., Ottewill C., O’Brien M.E., Morgan R.K., Costello R.W., Gunaratnam C., Ryan D., McElvaney N.G., McConkey S.J., et al. An Integrated Multidisciplinary Model of COVID-19 Recovery Care. Ir. J. Med. Sci. 2020;190:461–468. doi: 10.1007/s11845-020-02354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Masroor S. Collateral Damage of COVID-19 Pandemic: Delayed Medical Care. J. Card. Surg. 2020;35:1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323:1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 30.Tanoue Y., Nomura S., Yoneoka D., Kawashima T., Eguchi A., Shi S., Harada N., Miyata H. Mental Health of Family, Friends, and Co-Workers of COVID-19 Patients in Japan. Psychiatry Res. 2020;291:113067. doi: 10.1016/j.psychres.2020.113067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collaboration for Environmental Evidence . Collaboration for Environmental Evidence Guidelines for Systematic Review and Evidence Synthesis in Environmental Management. Version 4.2. Centre for Evidence-Based Conservation Bangor University; Wales, UK: 2013. [Google Scholar]
- 32.Bates S., Clapton J., Coren E. Systematic Maps to Support the Evidence Base in Social Care. Evid. Policy A J. Res. Debate Pract. 2007;3:539–551. doi: 10.1332/174426407782516484. [DOI] [Google Scholar]
- 33.Clapton J., Rutter D., Sharif N. SCIE Systematic Mapping Guidance. SCIE; London, UK: 2009. [Google Scholar]
- 34.Gonzalez A.I.G., Schmucker C., Nothacker J., Motschall E., Nguyen T.S., Brueckle M.-S., Blom J., van den Akker M., Röttger K., Wegwarth O., et al. Health-Related Preferences of Older Patients with Multimorbidity: An Evidence Map. BMJ Open. 2019;9:e034485. doi: 10.1136/bmjopen-2019-034485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bragge P., Clavisi O., Turner T., Tavender E., Collie A., Gruen R.L. The Global Evidence Mapping Initiative: Scoping Research in Broad Topic Areas. BMC Med. Res. Methodol. 2011;11:92. doi: 10.1186/1471-2288-11-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haddaway N.R., Bernes C., Jonsson B.-G., Hedlund K. The Benefits of Systematic Mapping to Evidence-Based Environmental Management. Ambio. 2016;45:613–620. doi: 10.1007/s13280-016-0773-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miake-Lye I.M., Hempel S., Shanman R., Shekelle P.G. What Is an Evidence Map? A Systematic Review of Published Evidence Maps and Their Definitions, Methods, and Products. Syst. Rev. 2016;5:28. doi: 10.1186/s13643-016-0204-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., Weeks L., et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 39.Department of Health and Social Care . National Framework for NHS Continuing Healthcare and NHS-Funded Nursing Care. Volume 187 Department of Health and Social Care; London, UK: 2022. [Google Scholar]
- 40.Omole F.S., Sow C.M., Fresh E., Babalola D., Strothers H. Interacting with Patients’ Family Members during the Office Visit. Am. Fam. Physician. 2011;84:780–784. [PubMed] [Google Scholar]
- 41.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—A Web and Mobile App for Systematic Reviews. [(accessed on 30 June 2022)]. Available online: https://www.rayyan.ai/ [DOI] [PMC free article] [PubMed]
- 42.Morgan D.L. Qualitative Content Analysis: A Guide to Paths Not Taken. Qual. Health Res. 1993;3:112–121. doi: 10.1177/104973239300300107. [DOI] [PubMed] [Google Scholar]
- 43.Elo S., Kyngäs H. The Qualitative Content Analysis Process. J. Adv. Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 44.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kerkhoff A.D., Sachdev D., Mizany S., Rojas S., Gandhi M., Peng J., Black D., Jones D., Rojas S., Jacobo J., et al. Evaluation of a Novel Community-Based COVID-19 “Test-to-Care” Model for Low-Income Populations. PLoS ONE. 2020;15:e0239400. doi: 10.1371/journal.pone.0239400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao J., Wei J., Zhu H., Duan Y., Geng W., Hong X., Jiang J., Zhao X., Zhu B. A Study of Basic Needs and Psychological Wellbeing of Medical Workers in the Fever Clinic of a Tertiary General Hospital in Beijing during the COVID-19 Outbreak. Psychother. Psychosom. 2020;89:252–254. doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Digby R., Winton-Brown T., Finlayson F., Dobson H., Bucknall T. Hospital Staff Well-Being during the First Wave of COVID-19: Staff Perspectives. Int. J. Ment. Health Nurs. 2021;30:440–450. doi: 10.1111/inm.12804. [DOI] [PubMed] [Google Scholar]
- 48.Elhadi M., Msherghi A., Elgzairi M., Alhashimi A., Bouhuwaish A., Biala M., Abuelmeda S., Khel S., Khaled A., Alsoufi A., et al. Burnout Syndrome among Hospital Healthcare Workers during the COVID-19 Pandemic and Civil War: A Cross-Sectional Study. Front. Psychiatry. 2020;11:579563. doi: 10.3389/fpsyt.2020.579563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feinstein R.E., Kotara S., Jones B., Shanor D., Nemeroff C.B. A Health Care Workers Mental Health Crisis Line in the Age of COVID-19. Depress. Anxiety. 2020;37:822–826. doi: 10.1002/da.23073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.González-Gil M.T., González-Blázquez C., Parro-Moreno A.I., Pedraz-Marcos A., Palmar-Santos A., Otero-García L., Navarta-Sánchez M.V., Alcolea-Cosín M.T., Argüello-López M.T., Canalejas-Pérez C., et al. Nurses’ Perceptions and Demands Regarding COVID-19 Care Delivery in Critical Care Units and Hospital Emergency Services. Intensive Crit. Care Nurs. 2021;62:102966. doi: 10.1016/j.iccn.2020.102966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee J., Venugopal V., Latha P.K., Alhadad S.B., Leow C.H.W., de Goh N.Y., Tan E., Kjellstrom T., Morabito M., Lee J.K.W. Heat Stress and Thermal Perception amongst Healthcare Workers during the COVID-19 Pandemic in India and Singapore. Int. J. Environ. Res. Public Health. 2020;17:8100. doi: 10.3390/ijerph17218100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kackin O., Ciydem E., Aci O.S., Kutlu F.Y. Experiences and Psychosocial Problems of Nurses Caring for Patients Diagnosed with COVID-19 in Turkey: A Qualitative Study. Int. J. Soc. Psychiatry. 2021;67:158–167. doi: 10.1177/0020764020942788. [DOI] [PubMed] [Google Scholar]
- 53.Zhang Y., Wang C., Pan W., Zheng J., Gao J., Huang X., Cai S., Zhai Y., Latour J.M., Zhu C. Stress, Burnout, and Coping Strategies of Frontline Nurses during the COVID-19 Epidemic in Wuhan and Shanghai, China. Front. Psychiatry. 2020;11:1154. doi: 10.3389/fpsyt.2020.565520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Raza A., Matloob S., Rahim N.F.A., Halim H.A., Khattak A., Ahmed N.H., Nayab D.-E., Hakeem A., Zubair M. Factors Impeding Health-Care Professionals to Effectively Treat Coronavirus Disease 2019 Patients in Pakistan: A Qualitative Investigation. Front. Psychol. 2020;11:572450. doi: 10.3389/fpsyg.2020.572450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ripp J., Peccoralo L., Charney D. Attending to the Emotional Well-Being of the Health Care Workforce in a New York City Health System during the COVID-19 Pandemic. Acad. Med. 2020;95:1136–1139. doi: 10.1097/ACM.0000000000003414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shanafelt T., Ripp J., Trockel M. Understanding and Addressing Sources of Anxiety among Health Care Professionals during the COVID-19 Pandemic. JAMA J. Am. Med. Assoc. 2020;323:2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 57.Halcomb E., Williams A., Ashley C., McInnes S., Stephen C., Calma K., James S. The Support Needs of Australian Primary Health Care Nurses during the COVID-19 Pandemic. J. Nurs. Manag. 2020;28:1553–1560. doi: 10.1111/jonm.13108. [DOI] [PubMed] [Google Scholar]
- 58.Kabir Z.N., Boström A.-M., Konradsen H. In Conversation with a Frontline Worker in a Care Home in Sweden during the COVID-19 Pandemic. J. Cross-Cult. Gerontol. 2020;35:493–500. doi: 10.1007/s10823-020-09415-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stojanov J., Malobabic M., Stanojevic G., Stevic M., Milosevic V., Stojanov A. Quality of Sleep and Health-Related Quality of Life among Health Care Professionals Treating Patients with Coronavirus Disease-19. Int. J. Soc. Psychiatry. 2021;67:175–181. doi: 10.1177/0020764020942800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Martin-Delgado J., Viteri E., Mula A., Serpa P., Pacheco G., Prada D., de Andrade Lourenção D.C., Baptista P.C.P., Ramirez G., Mira J.J. Availability of Personal Protective Equipment and Diagnostic and Treatment Facilities for Healthcare Workers Involved in COVID-19 Care: A Cross-Sectional Study in Brazil, Colombia, and Ecuador. PLoS ONE. 2020;15:e0242185. doi: 10.1371/journal.pone.0242185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yong L.M.O., Xin X., Wee J.M.L., Poopalalingam R., Kwek K.Y.C., Thumboo J. Perception Survey of Crisis and Emergency Risk Communication in an Acute Hospital in the Management of COVID-19 Pandemic in Singapore. BMC Public Health. 2020;20:1919. doi: 10.1186/s12889-020-10047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sethi B.A., Sethi A., Ali S., Aamir H.S. Impact of Coronavirus Disease (COVID-19) Pandemic on Health Professionals. Pak. J. Med. Sci. 2020;36:S6. doi: 10.12669/pjms.36.COVID19-S4.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Adesoye T., Davis C.H., Del Calvo H., Shaikh A.F., Chegireddy V., Chan E.Y., Martinez S., Pei K.Y., Zheng F., Tariq N. Optimization of Surgical Resident Safety and Education during the COVID-19 Pandemic—Lessons Learned. J. Surg. Educ. 2021;78:315–320. doi: 10.1016/j.jsurg.2020.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ashiru-Oredope D., Chan A.H.Y., Olaoye O., Rutter V., Babar Z.-U.-D., Anderson C., Anderson R., Halai M., Matuluko A., Nambatya W., et al. Needs Assessment and Impact of COVID-19 on Pharmacy Professionals in 31 Commonwealth Countries. J. Pharm. Policy Pract. 2020;13:72. doi: 10.1186/s40545-020-00275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Glatman-Freedman A., Bromberg M., Ram A., Lutski M., Bassal R., Michailevich O., Saban M., Frankental D., Dichtiar R., Kruglikov-Moldavsky A., et al. A COVID-19 Call Center for Healthcare Providers: Dealing with Rapidly Evolving Health Policy Guidelines. Isr. J. Health Policy Res. 2020;9:73. doi: 10.1186/s13584-020-00433-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cipolotti L., Chan E., Murphy P., van Harskamp N., Foley J.A. Factors Contributing to the Distress, Concerns, and Needs of UK Neuroscience Health Care Workers during the COVID-19 Pandemic. Psychol. Psychother. Theory Res. Pract. 2021;94:536–543. doi: 10.1111/papt.12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mattila E., Peltokoski J., Neva M.H., Kaunonen M., Helminen M., Parkkila A.K. COVID-19: Anxiety among Hospital Staff and Associated Factors. Ann. Med. 2021;53:237–246. doi: 10.1080/07853890.2020.1862905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Redondo-Sama G., Matulic V., Munté-Pascual A., de Vicente I. Social Work during the COVID-19 Crisis: Responding to Urgent Social Needs. Sustainability. 2020;12:8595. doi: 10.3390/su12208595. [DOI] [Google Scholar]
- 69.Yu J.C., McIntyre M., Dow H., Robinson L., Winston P. Changes to Rehabilitation Service Delivery and the Associated Physician Perspectives during the COVID-19 Pandemic: A Mixed-Methods Needs Assessment Study. Am. J. Phys. Med. Rehabil. 2020;99:775–782. doi: 10.1097/PHM.0000000000001516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu E.Y.T., Leung W.L.H., Wong S.Y.S., Liu K.S.N., Wan E.Y.F. How Are Family Doctors Serving the Hong Kong Community during the COVID-19 Outbreak? A Survey of Hkcfp Members. Hong Kong Med. J. 2020;26:176–183. doi: 10.12809/hkmj208606. [DOI] [PubMed] [Google Scholar]
- 71.Mohindra R., Ravaki R., Suri V., Bhalla A., Singh S.M. Issues Relevant to Mental Health Promotion in Frontline Health Care Providers Managing Quarantined/Isolated COVID19 Patients. Asian J. Psychiatry. 2020;51:102084. doi: 10.1016/j.ajp.2020.102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nguyen E., Owens C.T., Daniels T., Boyle J., Robinson R.F. Pharmacists’ Willingness to Provide Coronavirus Disease (COVID-19) Services and the Needs to Support COVID-19 Testing, Management, and Prevention. J. Community Health. 2021;46:752–757. doi: 10.1007/s10900-020-00946-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kaplan L.J., Kleinpell R., Maves R.C., Doersam J.K., Raman R., Ferraro D.M. Critical Care Clinician Reports on Coronavirus Disease 2019: Results From a National Survey of 4875 ICU Providers. Crit. Care Explor. 2020;2:e0125. doi: 10.1097/CCE.0000000000000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vanhaecht K., Seys D., Bruyneel L., Cox B., Kaesemans G., Cloet M., van den Broeck K., Cools O., De Witte A., Lowet K., et al. COVID-19 Is Having a Destructive Impact on Health-Care Workers’ Mental Well-Being. Int. J. Qual. Health Care. 2021;33:mzaa158. doi: 10.1093/intqhc/mzaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Du J., Mayer G., Hummel S., Oetjen N., Gronewold N., Zafar A., Schultz J.-H. Mental Health Burden in Different Professions during the Final Stage of the COVID-19 Lockdown in China: Cross-Sectional Survey Study. J. Med. Internet Res. 2020;22:e24240. doi: 10.2196/24240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang Z. Use the Environment to Prevent and Control COVID-19 in Senior-Living Facilities: An Analysis of the Guidelines Used in China. Health Environ. Res. Des. J. 2021;14:130–140. doi: 10.1177/1937586720953519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Simione L., Gnagnarella C. Differences Between Health Workers and General Population in Risk Perception, Behaviors, and Psychological Distress Related to COVID-19 Spread in Italy. Front. Psychol. 2020;11:2166. doi: 10.3389/fpsyg.2020.02166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dorociak K.E., Rupert P.A., Bryant F.B., Zahniser E. Development of a Self-Care Assessment for Psychologists. J. Couns. Psychol. 2017;64:325–334. doi: 10.1037/cou0000206. [DOI] [PubMed] [Google Scholar]
- 79.Danet A.D. Psychological Impact of COVID-19 Pandemic in Western Frontline Healthcare Professionals. A Systematic Review. Med. Clínica. 2021;156:449–458. doi: 10.1016/j.medcle.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.García-Iglesias J.J., Gómez-Salgado J., Martín-Pereira J., Fagundo-Rivera J., Ayuso-Murillo D., Martínez-Riera J.R., Ruiz-Frutos C. Impact of SARS-CoV-2 (COVID-19) on the mental health of healthcare professionals: A systematic review. Rev. Esp. Salud. Publica. 2020;94:e202007088. [PubMed] [Google Scholar]
- 81.Abdulla E.K., Velladath S.U., Varghese A., Anju M. Depression and Anxiety Associated with COVID-19 Pandemic among Healthcare Professionals in India—A Systematic Review and Meta-Analysis. Clin. Epidemiol. Glob. Health. 2021;12:100888. doi: 10.1016/j.cegh.2021.100888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fiabane E., Gabanelli P., La Rovere M.T., Tremoli E., Pistarini C., Gorini A. Psychological and Work-Related Factors Associated with Emotional Exhaustion among Healthcare Professionals during the COVID-19 Outbreak in Italian Hospitals. Nurs. Health Sci. 2021;23:670–675. doi: 10.1111/nhs.12871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The Mental Health Impact of the COVID-19 Pandemic on Healthcare Workers, and Interventions to Help Them: A Rapid Systematic Review. Psychiatry Res. 2020;293:113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yıldırım M., Arslan G., Özaslan A. Perceived Risk and Mental Health Problems among Healthcare Professionals during COVID-19 Pandemic: Exploring the Mediating Effects of Resilience and Coronavirus Fear. Int. J. Ment. Health Addict. 2022;20:1035–1045. doi: 10.1007/s11469-020-00424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ayton D., Soh S.-E., Berkovic D., Parker C., Yu K., Honeyman D., Manocha R., MacIntyre R., Ananda-Rajah M. Experiences of Personal Protective Equipment by Australian Healthcare Workers during the COVID-19 Pandemic, 2020: A Cross-Sectional Study. PLoS ONE. 2022;17:e0269484. doi: 10.1371/journal.pone.0269484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Effective Patient–Physician Communication. [(accessed on 30 June 2022)]. Available online: https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2014/02/effective-patient-physician-communication.
- 87.Dong F., Liu H.-L., Dai N., Yang M., Liu J.-P. A Living Systematic Review of the Psychological Problems in People Suffering from COVID-19. J. Affect. Disord. 2021;292:172–188. doi: 10.1016/j.jad.2021.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang H., Xie F., Yang B., Zhao F., Wang C., Chen X. Psychological Experience of COVID-19 Patients: A Systematic Review and Qualitative Meta-Synthesis. Am. J. Infect. Control. 2022;50:809–819. doi: 10.1016/j.ajic.2022.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shah R., Ali F.M., Nixon S.J., Ingram J.R., Salek S.M., Finlay A.Y. Measuring the Impact of COVID-19 on the Quality of Life of the Survivors, Partners and Family Members: A Cross-Sectional International Online Survey. BMJ Open. 2021;11:e047680. doi: 10.1136/bmjopen-2020-047680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kentish-Barnes N., Cohen-Solal Z., Morin L., Souppart V., Pochard F., Azoulay E. Lived Experiences of Family Members of Patients with Severe COVID-19 Who Died in Intensive Care Units in France. JAMA Netw. Open. 2021;4:e2113355. doi: 10.1001/jamanetworkopen.2021.13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chua A.Q., Tan M.M.J., Verma M., Han E.K.L., Hsu L.Y., Cook A.R., Teo Y.Y., Lee V.J., Legido-Quigley H. Health System Resilience in Managing the COVID-19 Pandemic: Lessons from Singapore. BMJ Glob. Health. 2020;5:e003317. doi: 10.1136/bmjgh-2020-003317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Haegdorens F., Franck E., Smith P., Bruyneel A., Monsieurs K.G., Van Bogaert P. Sufficient Personal Protective Equipment Training Can Reduce COVID-19 Related Symptoms in Healthcare Workers: A Prospective Cohort Study. Int. J. Nurs. Stud. 2022;126:104132. doi: 10.1016/j.ijnurstu.2021.104132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.