Abstract
Background: Music-based intervention has been used as first-line non-pharmacological treatment to improve cognitive function for people with mild cognitive impairment (MCI) or dementia in clinical practice. However, evidence regarding the effect of music-based intervention on general cognitive function as well as subdomains of cognitive functions in these individuals is scarce. Objective: To evaluate the efficacy of music-based interventions on a wide range of cognitive functions in people with MCI or dementia. Method: We searched the effect of various music therapies using randomized controlled trials on cognitive function using several databases. Studies based on any type of dementia or MCI were combined. The effects of music-based intervention on each cognitive function were pooled by meta-analysis. Results: A total of 19 studies involving n = 1024 participants (mean age ranged from 60 to 87 years old) were included. We found statistically significant improvements in MMSE (general cognitive function), the Frontal Assessment Battery (executive function), and the Auditory Verbal Learning Test (episodic memory). Conclusions: This study provides positive evidence to support music-based interventions for improving a wide range of cognitive functions in older adults with MCI and dementia. Therefore, we recommend increased use of music in people’s homes, day care centers and nursing homes. This study was registered with PROSPERO, number 250383.
Keywords: music intervention, music therapy, dementia, MCI, nonpharmacological therapy, cognitive functions
1. Introduction
The number of people with dementia and mild cognitive impairment (MCI) has rapidly increased in recent decades and related challenges have become a global burden [1]. Dementia and MCI are characterized by irreversible impairment of cognitive function, behavioral and psychological symptoms of dementia, and decrease in the activities of daily living (ADL) [2]. Decreased cognitive function is one of the main reasons why the lives of people with dementia become difficult [3]. In people with dementia and MCI, cognitive decline also negatively affects quality of life (QoL), ADL functioning, and communication with relatives and healthcare professionals [4]. Therefore, it is important for cognitive function to be improved in the daily lives of people with dementia and MCI.
Pharmacological and non-pharmacological intervention are two approaches for improving cognitive function. The latest pharmacological approaches indicate the beneficial effects of acetylcholinesterase inhibitors and memantine in people with Alzheimer’s disease [5]. However, the costs and risks associated with utilizing pharmacological therapy have been an issue [5]. Additionally, antidepressants, sedatives, and anti-dementia drugs are commonly used as add-on therapies, but have shown negative impacts on QoL [6]. Due to fewer risks and adverse effects, a non-pharmacological approach using cognitive activities, physical exercise, and art and play therapies has been suggested as a first line treatment strategy for the neuropsychiatric symptoms of dementia [6]. Previous studies have shown that these intervention programs lead to improvements in cognitive function in people with dementia and MCI [7,8]. Thus, non-pharmacological approaches have attracted the attention of aging researchers and caregivers.
Musical skill is a preserved skill in people with dementia [9,10]. Consequently, music-based intervention is a major strategy of the non-pharmacological intervention approach [11]. Music-based intervention is defined as any intervention using “music” (music as a cultural product usually involving some combination of melody, rhythm and harmony cognitively processed by the human brain) to study the therapeutic effect [11]. “Music” is then differentiated from single pitch sound and sound (or aspects of music) transduced into vibrotactile sensation of neuromodulatory and physiological effects [12,13]. The review in this paper focuses exclusively on music-based interventions which were mainly categorized into music therapy by a trained music therapist and music medicine by healthcare or music professionals [11,14]. At the beginning, music therapy was defined as “an intentional use of properties and the potential of music and its impact on the human being” [15]. Recently, the American Music Therapy Association has narrowed this definition to: “Music Therapy is the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy program”(https://www.musictherapy.org/about/musictherapy/, access date: 4 July 2022). It suggests that music therapy involves therapeutic relationships between participants and music therapists. On the other hand, music medicine does not need these relationships.
Music has been widely used in clinical practice throughout history [16]. However, the results of studies on the effectiveness of music-based intervention lack consistency. Some meta analyses focusing on global cognitive function showed that music-based intervention had small to moderate effects on maintaining or improving cognitive function [17,18]. Other meta-analyses showed inconsistent results in that music-based intervention was found to have no effect on impairment [19]. Due to the small number of studies included in the previous meta-analyses and these inconsistent results [18,19,20], it is difficult to conclude whether music-based intervention would have positive effects on cognition in aging populations or not. It still needs to be investigated whether music-based intervention has the potential to improve cognitive function in people with dementia and MCI.
Previous meta-analysis studies mainly focused on the benefits of music-based intervention for general cognitive function measured by the Mini Mental State Examination (MMSE). However, prior evidence suggests that cognitive function has multiple subdomains [21]. In addition, each individual with dementia shows deterioration of cognitive function in a different way. In terms of the subdomains of cognitive function, some show specific deterioration of memory while others show decline in executive function [21]. Therefore, it is essential to investigate whether music-based intervention would have positive effects on each cognitive function subdomain. In this study, we performed a systematic review and meta-analysis to evaluate the effectiveness of music-based intervention on each subdomain of cognitive function in people with dementia and MCI.
2. Materials and Methods
Analysis methods and eligibility criteria were specified in advance and documented in a protocol registered on PROSPERO (International Prospective Register of Systematic Reviews; Record ID = 250383). This systematic review and meta-analysis were conducted in accordance with the PRISMA check-list [22]. Please see Supplementary Materials (Supplemental Table S1).
2.1. Eligibility Criteria
Trials were considered for inclusion in this review if the criteria set out below were met.
Participants: Men and women aged 60+ with a clinical diagnosis of cognitive impairment or dementia. Intervention: Any music-based intervention or community music activity including listening to music, singing, playing an instrument, and music with movement or exercise. The design of the trial must have been such that the independent effects of either exercise, cognitive, or dual-task training on cognition could be analyzed. We delimited our review to exclude interventions focusing on music or sound as vibrotactile stimulation, single frequency sound, or sound for its vibratory effect. Comparison: Any concurrent control group was eligible, including no intervention/usual care, meditation, pharmacological intervention, exercise intervention, late intervention, and painting or other art related activities. Outcome: Any validated cognitive tests reported at the baseline and follow up after exposure to any type of music-based intervention. Study design: Randomized controlled trials that allocated individuals to either an intervention or concurrent control group.
2.2. Search Strategy
We searched scientific articles which were published between January 2000 and April 2021. The following electronic databases were used to search for completed trials: PubMed, CINAHL, PsycINFO, and Google Scholar. For the PubMed search, we checked the “randomized controlled trial” box. For the other searches, we added “randomized controlled trial” as a key word in addition to certain other keywords. For the cognitive function domain, keywords included (“music” OR “sing” OR “song” OR “listen”) AND (“dementia” OR “elderly” OR “Alzheimer’s” OR “cognitive impairment”) AND (“cognitive function” OR “cognition” OR “memory” OR “attention” OR “executive function” OR “processing speed”). All key search terms were combined, where possible, with medical sub-headings (MeSH) and indexed terms to identify potentially relevant studies. Trials on interactive music intervention and listening to music were manually identified from the title and abstract previews of all search records.
2.3. Inclusion and Exclusion Criteria
Based on the previous studies [23,24,25,26], we set the inclusion and exclusion criteria. Randomized controlled trials were included if they met the following inclusion criteria: (1) participants with clinical diagnosis of dementia or cognitive impairment. We also included persons with Alzheimer’s disease, Parkinson’s disease, and mixed dementia; (2) studies that investigated the treatment effect of any type of music-based intervention; (3) studies that reported at least one of the following outcomes: general cognitive function, episodic memory, working memory, attention, processing speed, and executive function; (4) studies that measured the scores of the clinical assessment scales from baseline to endpoint or follow up among the intervention and control groups. Studies were excluded if the study design was not a randomized controlled trial, they compared participants with dementia/MCI and healthy individuals or only included healthy adults, or there were insufficient details from which the study outcomes could be derived.
2.4. Study Outcomes
Based on the previous studies [25,26], cognitive function was categorized into seven different cognitive domains: general cognitive function, episodic memory, working memory, short-term memory, attention, processing speed, and executive function. We used all of the available clinical cognitive assessment scales in each domain from the included studies as our primary outcomes. Examples of the primary outcomes of this study are the change scores in MMSE [27], Severe Impairment Battery (SIB) [28], Montreal Cognitive Assessment (MoCA) [29], Auditory Verbal Learning Test (AVLT) [30], The Word Memory Test (WMT) [31], Trail Making Test A (TMT-A) [32], Digit Symbol Substitution (DSST) [33], Verbal Fluency Test, Trail Making Test B (TMT-B) [32] and Frontal Assessment Battery (FAB) [34]. The MMSE, SBI, and MoCA focused on general cognitive function; the AVLT and WMT focused on episodic memory and shortterm memory, respectively; the TMT-A and DSST focused on processing speed; and the Verbal Fluency Test, TMT-B, and FAB focused on executive function.
Standard mean difference (SMD) with standard deviation (SD) or 95% confidence interval (CI) was used to evaluate the changes in assessment scores between the music-based intervention and control groups. For the TMT-A and TMT-B, since a longer time indicated a lower cognitive function [32], we reversed the score for analysis. A higher score for the MMSE, SBI, MoCA, AVLT, WMT, DSST, FAB, TMT-A, and TMT-B indicated better cognitive function.
2.5. Data Extraction
Two investigators (E.I. and R.N.) independently assessed the relevance of the search results and abstracted the demographic details of individual trials into a data extraction Excel form, including year of publication, study location, number of participants included, mean age, number and percentage of female participants, stages of dementia, recruitment site, type of music-based intervention, control group intervention, treatment period and duration, and all clinical assessment scales.
2.6. Risk of Bias Assessment
E.I. and R.N. independently assessed the quality of each study according to the methodology section of the Consolidated Standards of Reporting Trials (CONSORT) statement [35]. A 14-point scale was designed for the evaluation of study quality including (1) random allocation, (2) treatment allocation concealed, (3) groups/subjects similar at baseline regarding important prognostic values, (4) eligibility criteria specified, (5) blinded outcome assessor, (6) blinded care provider, (7) blinded patients/people, (8) point estimates and measures of variability presented for the primary outcome measures, (9) intention-to-treat analysis, (10) details of random allocation methods, (11) adequate description of the control/comparison group, (12) between-group statistical comparison, (13) reporting dropouts, and (14) reporting CONSORT statement.
The potential risk of bias [36] for included trials was checked using the Cochrane Risk of Bias assessment tool with the following domains: (1) random sequence generation of intervention and control groups, (2) the method of concealment of allocation, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) the completeness of outcome data, and (6) selective outcome reporting.
2.7. Data Synthesis and Statistical Analysis
Standard mean difference (SMD) and standard deviation (SD) or 95% confidence interval (CI) were used to evaluate the range of scores on the assessment scales between the music-based intervention and control groups. Cognitive outcomes were grouped based on the cognitive domain measured (e.g., general cognitive function, episodic memory, working memory, short-term memory, attention, processing speed, and executive function). In addition, we separately conducted meta-analyses on whether each cognitive domain included more than one study with MCI or dementia and music-based intervention by music therapist or not.
Changes from baseline values were used to conduct meta-analyses as they allowed for the comparison of more trials. When only pre- and post-data were presented, changes from baseline scores were calculated by deducting the baseline score from the follow-up score. Standard error (SE) scores were converted to standard deviation (SD) scores using the following equation [37]:
| SD = SE × √N |
Changes from baseline standard deviation (SD) were calculated using the following correlation coefficient equation:
| SDE/change = √SD2E/baseline + SD2E/final − (2 × 0.5 × SDE/baseline × SDE/final) |
All meta-analyses were performed to combine the effect sizes using meta packages in R [38]. If a study reported multiple change scores of cognitive tests in the same cognitive domain, then we used multilevel meta-analysis using metafor package in R [39]. Statistical heterogeneity among the trials was assessed, and a p value of <0.05 was regarded as statistically significant. A higher score reflecting better cognitive function was represented by a positive effect estimate. A lower score reflecting poorer task performance was represented by a negative effect estimate. A random-effects model was chosen due to the expected heterogeneity between trial protocols. Heterogeneity was measured using Higgins I2 statistic [40] and an I2 threshold of >40% was set to detect heterogeneity. Forest plots were used to graphically present the combined results.
3. Results
3.1. Literature Search and Study Selection
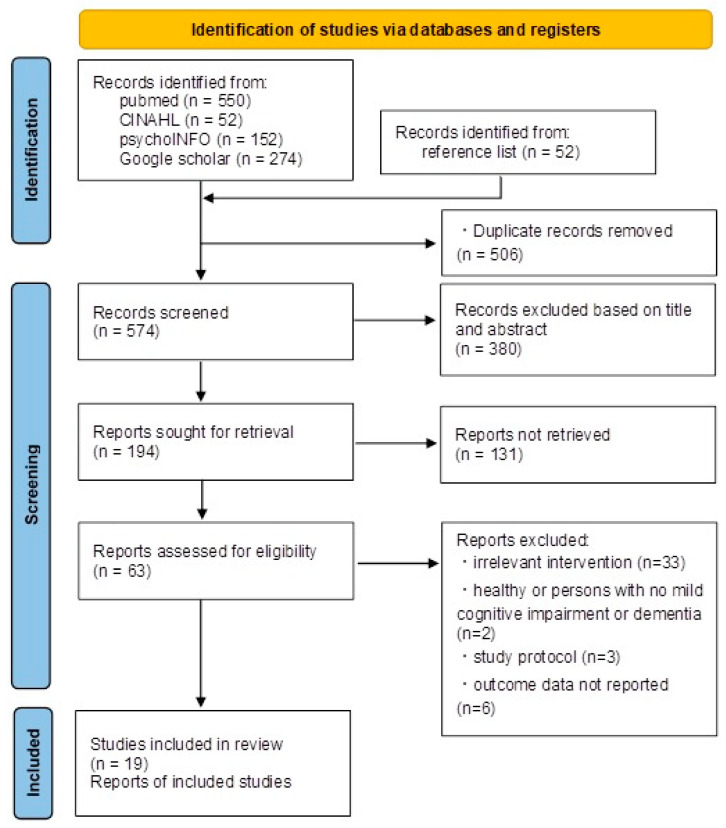
A total of 522 abstracts were identified from the databases and an additional 52 potential studies were further extracted from the bibliographies of review articles. All 574 titles and abstracts were screened and the full texts of 194 studies were further evaluated for relevance. A total of 44 studies about cognitive function were excluded for the following reasons: 33 had irrelevant intervention or study groups, nine did not specify what would be required for there to be adequate data for analysis (such as a lack of standard deviation), and two compared participants with dementia and healthy controls or included only healthy adults. The definitive analysis included 19 trials for cognitive function involving participants with dementia all over the world, published between 2000 and 2021. The study selection process is presented in the PRISMA flow chart (Figure 1).
Figure 1.
PRISMA flow chart.
3.2. Characteristics of Included Studies
The 19 eligible trials were comprised of n = 1024 participants with a clinical diagnosis of MCI and any stage of dementia. Included RCTs were conducted in Asia (eight studies; Japan, Korea, China, and Singapore), Europe (eight studies; Italy, France, Sweden, and Belgium), and US (three studies). The sample sizes ranged from 26 to 298 (11 studies including 10–50 people; 5 studies including 51–100 people, 1 study including 101–200 people, and 2 studies including 201–300 people), the mean age ranged from 60.0 to 87.1 years, and the percentage of females ranged from 50.0% to 100% (Table 1). Regarding the severity of dementia, three studies claimed that they recruited participants with MCI [41,42,43], six studies claimed that they recruited participants with mild-to-moderate dementia [44,45,46,47,48,49], two included participants with severe dementia [50,51], and eight included participants with dementia of any severity level [45,52,53,54,55,56,57,58,59].
Table 1.
Characteristics of included randomized controlled trials.
| Study and Year | Country | Recruitment Site | No. of Participants | Mean Age | Female | Severity of Dementia | Type of Music-Based Intervention | Control Type | Intervention Period | Intervention Frequency |
Time for Each Intervention | Study Outcomes | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ceccato 2012 [55] |
Italy | Support center | 51 | 86.3 | 40 (78.4%) | Non-specific | STAM (music with movement, clapping hands) | Control | 12 weeks | Twice a week | 40 min | MMSE | 10 |
| Yu-ling 2018 [49] |
USA | Dementia outpatient unit at a medical center | 28 | 77.3 | 14 (50%) | Mild to moderate | Musical dual task (sing or play instrument while walking) | Control | 8 weeks | Once a week | 60 min | MMSE, TMT-A | 12 |
| Doi 2017 [41] |
Japan | National center for geriatrics and gerontology | 201 | 76 | 104 (51.7%) | MCI | Play instrument (percussion) | Dance, control | 40 weeks | Once a week | 60 min | MMSE, TMT-A, TMT-B, Story and word memory | 11 |
| Don Mei Li 2016 [56] |
China | Long term care facility | 40 | 82.4 | 28 (70%) | Non-specific | Folk recreation (singing) | Control | 16 weeks | 3 times a week | 40–50 min | TMT-A | 8 |
| Giovagnoli 2017 [44] |
Italy | One nursing center | 39 | 73.6 | 24 (61.5%) | Mild to moderate | Play instrument | Active control (cognitive training, neuroeducation) | 12 weeks | Twice a week | 45 min | TMT, DSST | 9 |
| Giovagnoli 2018 [52] |
Italy | One center | 45 | 73.2 | 31 (68.9%) | Non-specific | Music (playing music) and drugs | Drugs only | 24 weeks | Twice a week | 40 min | SBI, MMSE | 13 |
| Innes 2017 [58] |
USA | Community | 60 | 60.6 | 56 (93.3%) | Non-specific | Listening to music | Meditation | 12 weeks | Daily | 12 min | TMT-A, TMT-B, DSST, | 12 |
| Innes 2018 [47] |
USA | Community | 53 | 60 | 46 (86.8%) | Non-specific | Listening to music | Meditation | 12 weeks | Daily | 30–45 min | TMT-A, TMT-B | 11 |
| Kim 2020 [48] |
Korea | Adult day care center | 35 | 79.3 | 26 (74.3%) | Mild AD | Recollection based occupational music-based intervention (singing, listening) | Control | 24 weeks | 5 sessions a week | 60 min | MMSE | 9 |
| Lyu 2018 [50] |
China | Geriatric hospital | 298 | 69.7 | 173 (58.1%) | Mild to severe AD | Singing | Lyric reading, control | 12 weeks | Twice a day, twice a week | 30–40 min, | Verbal fluency, AVLT, MMSE. | 10 |
| Mahendran 2018 [45] |
Singapore | Community living | 68 | 71.1 | 38 (55.9%) | Mild neurocognitive decline | Music reminiscence (listening) | Art therapy, control | 12 weeks | Once a week | 65 min (including 15 min break) | AVLT | 11 |
| Miyazaki 2020a [42] |
Japan | Residential care facilities | 26 | 81.5 | 20 (76.9%) | MCI | Singing (karaoke) | Active control | 12 weeks | Once a week | 120 min | MoCA, FAB | 12 |
| Miyazaki 2020b [51] |
Japan | Nursing home | 46 | 87 | 40 (87.0%) | Non-specific | Play instrument (Drum) | Control | 12 weeks | Twice a week | 30 min | MMSE, FAB | 9 |
| Narme 2013 [53] |
France | Nursing home | 37 | 87.1 | 32 (86.5%) | Alzheimer’s with mixed dementia | Play instrument (Percussion) | Cooking | 4 weeks | Twice a week | 60 min | SBI | 8 |
| Pohl 2020 [59] |
Sweden | Community dwelling individuals diagnosed with PD | 46 | 70 | 32 (69.6%) | PD | Training with music based intervention | Control | 12 weeks | Twice a week | 60 min | MoCA, PDQ39 | 11 |
| Pongan 2017 [46] |
France | University hospital | 59 | 79.5 | 39 (66.1%) | Mild Alzheimer’s disease | Singing | Painting | 12 weeks | Once a week | 120 min | TMT-A, FAB, | 13 |
| Raglio 2015 [60] |
Italy | Nursing home and day care centers | 120 | 81.7 | 94 (78.3%) | Moderate to severe dementia | Active music therapy, listening to music | Control | 10 weeks | Twice a week | 30 min | MMSE | 11 |
| Shimizu 2018 [43] |
Japan | Community dwelling individuals participating in the dementia care class | 45 | 74.6 | 38 (84.4%) | MCI | Music with movement | Active control (movement without music) | 12 weeks | Once a week | 60 min | FAB | 10 |
| Van de Winckel 2002 [54] |
Belgium | Public hospital | 25 | 81.7 | 25 (100%) | Non-specific | Exercise with music | Active control (one to one conversation) | 12 weeks | Once a day | 30 min | MMSE, ADS 6 | 9 |
| Total | 1024 |
Note: MMSE scores: 0~11 severe dementia, 12~17 moderate dementia, 18~23 mild dementia, 23~30 no dementia.
Regarding the type of therapy investigated, four studies investigated singing therapy [42,46,50,53], eight studies investigated music listening therapy [41,45,47,48,50,52,56,58], three studies investigated playing instruments [47,51,53], and five studies investigated music with movement therapy [43,44,53,54,59]. In five studies, the certificated music therapist provided the music sessions [44,49,52,55,60].
A total of 13 studies included comparisons with a usual care group [41,42,43,45,48,49,50,51,52,55,56,57,59] and nine studies included comparisons with an active control group [41,44,45,46,47,50,53,54,58]. The active control intervention included various therapies such as meditation [52], other art related therapies [42,45,46,47,50], or exercise [41,43], and in the blank control group, the participants received the usual care [41,42,43,45,48,49,50,51,52,55,56,57,59]. Regarding the intervention durations of the included studies, the average intervention period was 14.2 (SD = 7.5) weeks, and the average time was 51.5 (SD = 28.0) minutes (Table 1).
The included studies used a wide range of cognitive function measures and the domains are shown in Table 2.
Table 2.
Description of clinical assessment scale in different domains.
| Outcome | Test | Number of Studies | Number of Studies Compared with Control Group | Number of Studies Compared with Active Control Group |
|---|---|---|---|---|
| General cognitive function | MMSE | 8 | 5 | 3 |
| MoCA | 2 | 1 | 1 | |
| Episodic memory | AVLT | 2 | 2 | 2 |
| Working memory | 0 | - | - | |
| Short-term memory | 1 | - | - | |
| Attention | 0 | - | - | |
| Processing speed | TMT-A | 6 | 2 | 6 |
| DSST | 1 | 0 | 1 | |
| Executive function | Verbal fluency | 2 | 2 | 2 |
| TMT-B | 4 | 0 | 4 | |
| FAB | 5 | 2 | 3 |
3.3. General Cognitive Function
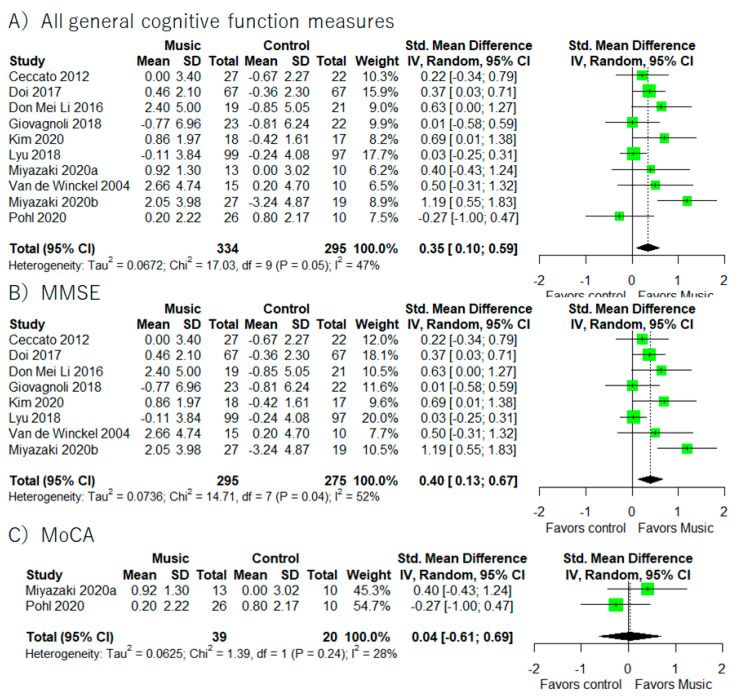
A total of 10 studies provided the results regarding general cognitive function (Figure 2) [41,42,44,50,51,54,55,56,58,59]. Of those 10 studies, eight provided results for the MMSE [41,44,50,51,54,55,56,58], two for the MoCA [42,59], and one for the SIB [52]. Meta-analysis using all studies (Figure 2) revealed that music-based intervention had a positive effect on general cognitive function (I2 = 47.1%, SMD = 0.35, 95% CI 0.10 to 0.59). In addition, meta-analysis on studies using only the MMSE as the outcome measure showed a significant improvement in MMSE score (I2 = 52.4%, SMD = 0.40, 95% CI 0.13 to 0.67).
Figure 2.
Trial level data, effect estimates, and forest plot for all general cognitive functions’ measures (A), MMSE (B), and MoCA (C). The area of green square is proportional to the study’s weight in the meta-analysis.
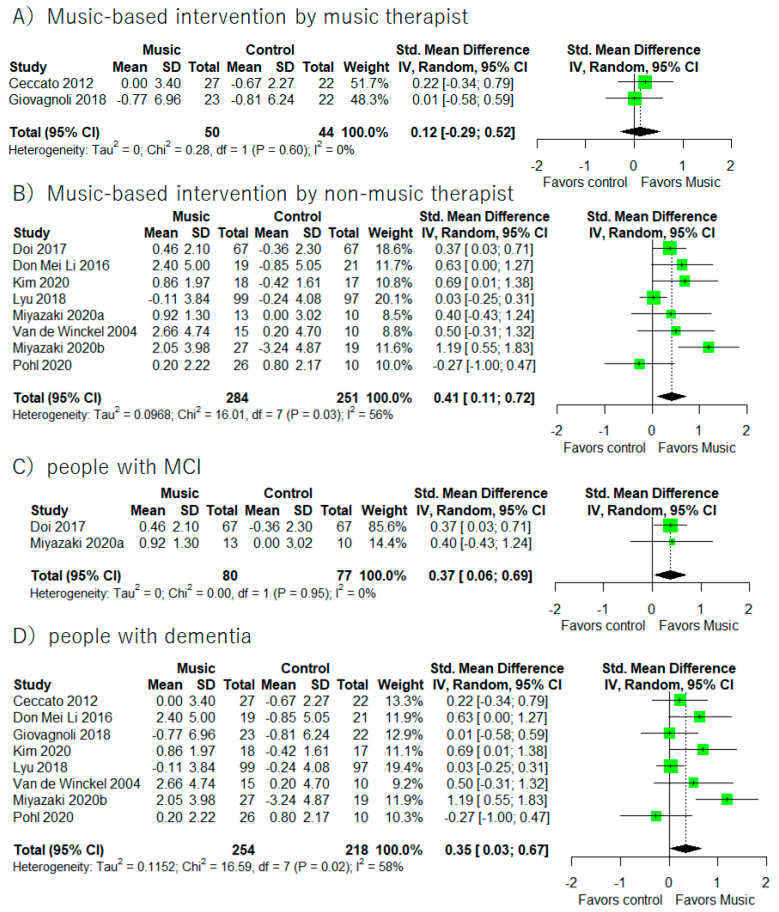
Supplementary Meta-analyses (Figure 3) revealed that music-based intervention improved general cognitive functions in people with MCI (I2 = 0%, SMD = 0.37, 95% CI 0.06 to 0.69) and dementia (I2 = 58%, SMD = 0.35, 95% CI 0.03 to 0.67). Moreover, music-based intervention by non-music therapists showed significant improvements in general cognitive functions (I2 = 56.3%, SMD = 0.41, 95% CI 0.11 to 0.72).
Figure 3.
Trial level data, effect estimates, and forest plot in supplementary meta-analyses for music-based intervention by music therapist (A), music-based intervention by non-music therapist (B), people with MCI (C), and people with dementia (D). The area of green square is proportional to the study’s weight in the meta-analysis.
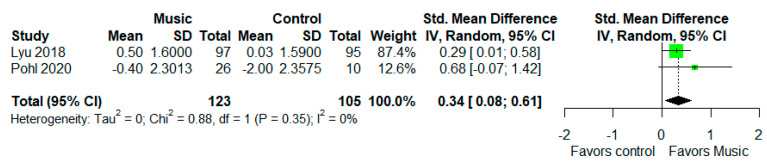
3.4. Episodic Memory
The AVLT was used as a measure for episodic memory in two measures (Figure 4) [45,50]. Meta-analysis revealed that music-based intervention improved AVLT performance (I2 = 0%, SMD = 0.34, 95% CI 0.08 to 0.61).
Figure 4.
Trial level data, effect estimates, and forest plot for the effects of music-based intervention on the AVLT. The area of green square is proportional to the study’s weight in the meta-analysis.
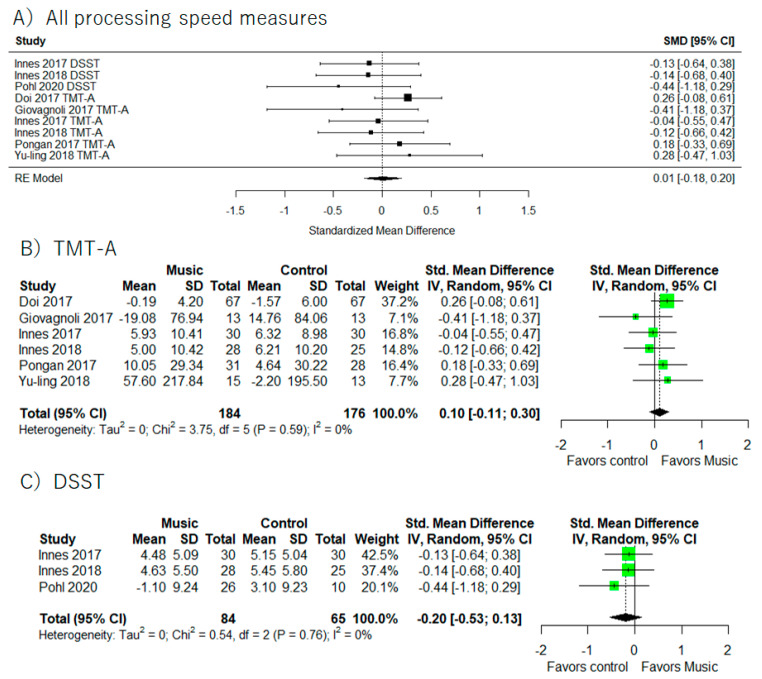
3.5. Processing Speed
Processing speed results were provided in seven studies (Figure 5) [41,44,46,47,49,58,59] (I2 = 8.5%, SMD = 0.01, 95% CI −0.18 to 0.20). There were no statistically significant relations between music-based intervention and cognitive function. We also did not find any significant results in each cognitive test (TMT-A and DSST).
Figure 5.
Trial level data, effect estimates, and forest plot for the effects of music-based intervention on all processing speed measure (A), TMT-A (B), and DSST (C). The area of green square is proportional to the study’s weight in the meta-analysis.
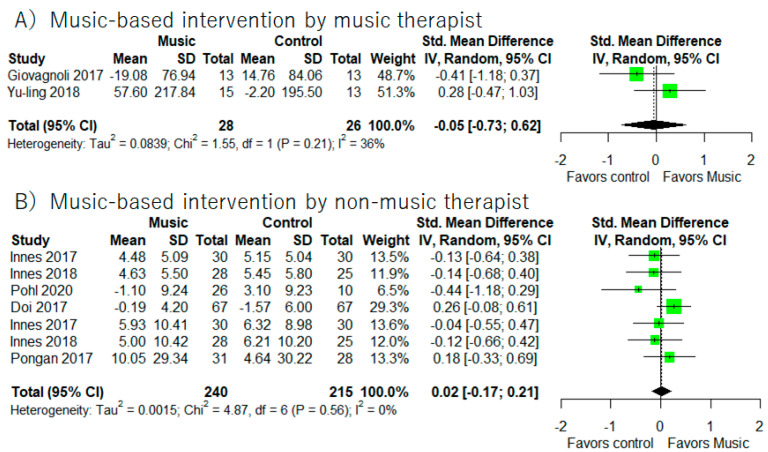
In addition, supplemental meta-analyses (Figure 6) did not show significant improvements of processing speed based on participants (MCI or dementia) and music-based intervention by the music therapist or not.
Figure 6.
Trial level data, effect estimates, and forest plot in supplementary meta-analyses for music-based intervention by music therapist (A), music-based intervention by non-music therapist (B). The area of green square is proportional to the study’s weight in the meta-analysis.
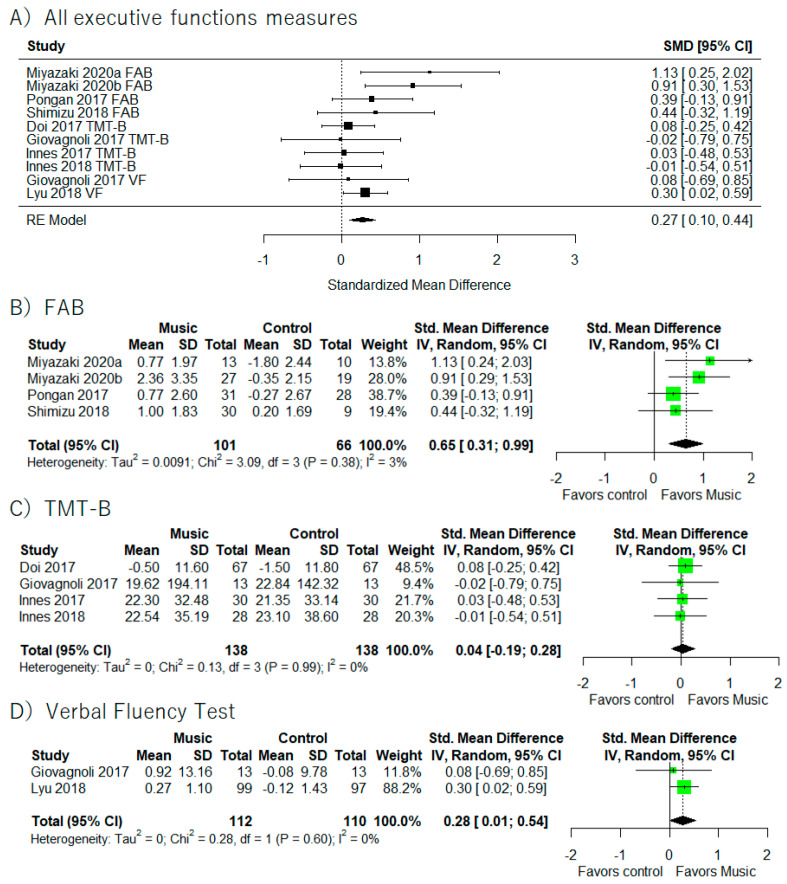
3.6. Executive Function
A total of nine studies provided executive function results (Figure 7) [41,42,43,44,46,47,50,51,58]. Of those nine studies, four provided results for the FAB [42,43,46,51], two studies used the Verbal Fluency Test [44,50], and four used the TMT-B [41,44,47,58]. Meta-analysis using all studies revealed that music-based intervention generally improved executive function (I2 = 8.51%, SMD = 0.27, 95% CI 0.10 to 0.44). In addition, meta-analysis including studies that only used the FAB as the outcome measure showed the beneficial effects of music-based intervention on FAB performance (I2 = 3.1%, SMD = 0.65, 95% CI 0.31 to 0.99) and Verbal Fluency Test (I2 = 0%, SMD = 0.28, 95% CI 0.01 to 0.54).
Figure 7.
Trial level data, effect estimates, and forest plot for the effects of music-based intervention on all executive functions’ measures (A), TMT-B (B), FAB (C), and Verbal Fluency Test (D). The area of green square is proportional to the study’s weight in the meta-analysis.
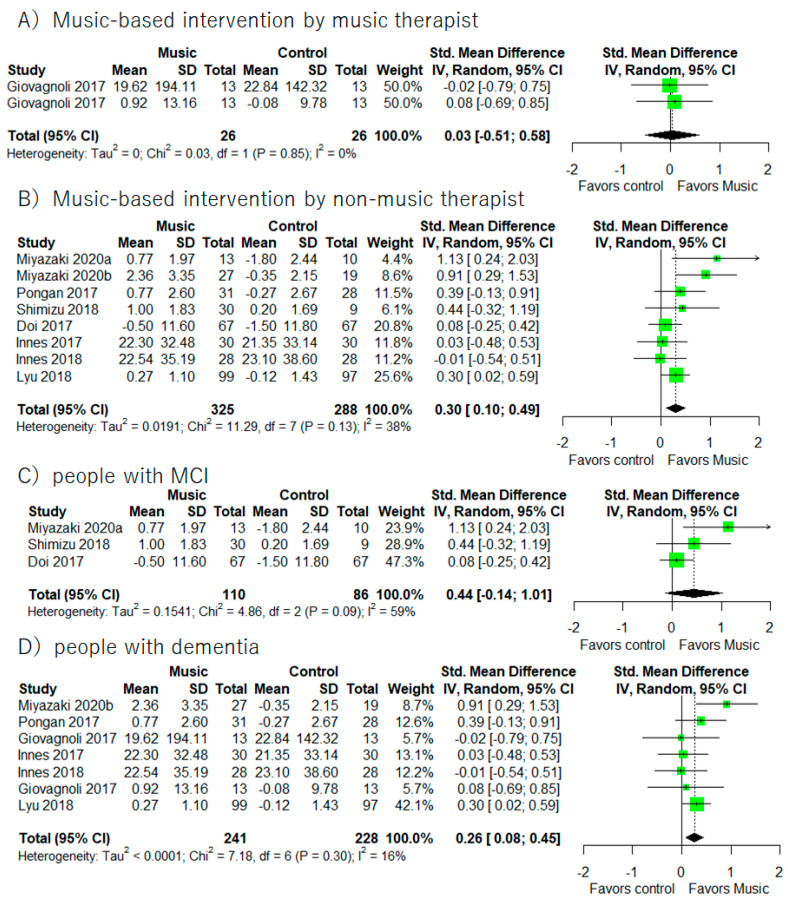
Supplementary meta-analyses (Figure 8) revealed that music-based intervention by non-music therapist improved executive functions (I2 = 38%, SMD = 0.30, 95% CI 0.10 to 0.49). In addition, music-based intervention improved executive functions in people with dementia (I2 = 16%, SMD = 0.26, 95% CI 0.08 to 0.45).
Figure 8.
Trial level data, effect estimates, and forest plot in supplementary meta-analyses for music-based intervention by music therapist (A), music-based intervention by non-music therapist (B), people with MCI (C), and people with dementia (D). The area of green square is proportional to the study’s weight in the meta-analysis.
3.7. Working Memory/Short Term Memory/Attention
There were no specific studies that provided details regarding working memory, short-term memory, or attention.
3.8. Quality Assessment
An assessment of the methodological quality of the included studies is presented in Table 3. The quality assessment score ranged from 8 to 13, with an average of 10.47 (SD = 1.50). All included studies had sufficient methodological quality. The scores of item 5 (blinded outcome assessor), 9 (intention-to-treat analysis), and 14 (reporting CONSORT statement) were low. However, all studies fulfilled the methodological qualities of item 1 (random allocation), 4 (eligibility criteria specified), and 11 (adequate description of the control/comparison group).
Table 3.
Quality assessment scores of included studies using modified Delphi list.
| Lead Author, Year, Country | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Q14 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ceccato 2012 [55] | Y | Y | Y | Y | ? | ? | Y | Y | N | Y | Y | Y | Y | N | 10 |
| Yu-ling 2018 [49] |
Y | Y | N | Y | Y | ? | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Doi 2017 [41] | Y | Y | Y | Y | Y | ? | Y | Y | Y | Y | Y | N | Y | N | 11 |
| Don Mei Li 2016 [56] | Y | Y | Y | Y | ? | ? | Y | Y | N | N | Y | N | Y | N | 8 |
| Giovagnoli 2017 [44] | Y | Y | Y | Y | ? | N | ? | Y | N | Y | Y | Y | Y | N | 9 |
| Giovagnoli 2018 [52] | Y | Y | Y | Y | Y | ? | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Innes 2017 [58] | Y | Y | Y | Y | ? | Y | Y | Y | Y | Y | Y | Y | Y | N | 12 |
| Innes 2018 [47] | Y | Y | Y | Y | Y | ? | Y | Y | N | Y | Y | Y | Y | N | 11 |
| Kim 2020 [48] | Y | Y | Y | Y | ? | ? | Y | Y | N | N | Y | Y | Y | N | 9 |
| Lyu 2018 [50] | Y | Y | Y | Y | Y | N | N | Y | N | Y | Y | Y | Y | N | 10 |
| Mahendran 2018 [45] | Y | Y | Y | Y | ? | N | Y | Y | Y | N | Y | Y | Y | Y | 11 |
| Miyazaki 2020a [42] | Y | Y | Y | Y | Y | Y | Y | ? | N | Y | Y | Y | Y | Y | 12 |
| Miyazaki 2020b [51] | Y | N | Y | Y | N | N | N | Y | N | Y | Y | Y | Y | Y | 9 |
| Narme 2013 [53] | Y | Y | Y | Y | ? | ? | ? | Y | N | N | Y | Y | Y | N | 8 |
| Pohl 2020 [59] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | Y | Y | Y | 11 |
| Pongan 2017 [46] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ? | 13 |
| Raglio 2015 [60] | Y | Y | Y | Y | ? | ? | Y | Y | Y | Y | Y | Y | Y | N | 11 |
| Shimizu 2018 [43] | Y | Y | Y | Y | N | ? | Y | Y | N | Y | Y | Y | Y | N | 10 |
| Van de Winckel 2002 [54] | Y | Y | Y | Y | ? | ? | Y | Y | N | N | Y | Y | Y | N | 9 |
| Total score across studies | 19 | 18 | 18 | 19 | 7 | 3 | 15 | 18 | 7 | 14 | 19 | 17 | 19 | 6 | - |
Note: (Q1) Random allocation, (Q2) treatment allocation concealed, (Q3) groups/subjects similar at baseline regarding important prognostic values, (Q4) eligibility criteria specified, (Q5) blinded outcome assessor, (Q6) blinded care provider, (Q7) blinded patient, (Q8) point estimates and measures of variability presented for the primary outcome measures, (Q9) intention-to-treat analysis, (Q10) details of random allocation methods, (Q11) adequate description of the control/comparison group, (Q12) between-group statistical comparison, (Q13) reporting dropouts, (Q14) reporting CONSORT statement. Y means that previous studies met the criteria of each item. N means that previous studies did not met the criteria of each item. ? means that previous studies did not mention the item.
4. Discussion
We performed a systematic review and meta-analysis to examine the effect of music-based intervention on each subdomain of cognitive function for people with dementia and MCI. We found that music-based intervention improved cognitive function assessed by the MMSE total score. Further, the intervention improved both the executive function and the episodic memory performance. These results are of key importance for patients, clinicians and stakeholders because these cognitive functions are associated with ADL and QoL in people with MCI and dementia [61,62,63].
The first main finding is that music-based intervention increased general cognitive function in people with dementia and MCI. This finding is in line with prior meta-analysis studies [17,18]. However, the results regarding the effects of music-based intervention are still controversial. Some meta-analysis studies have reported no positive effect of musical therapy on general cognitive function [19,20]. The reason for this dissociation is the number of included studies in past meta-analysis studies. For example, the number of included studies in the previous meta-analyses was eight [18], seven [19], and eight [20]. However, the current meta-analysis included 19 studies. Therefore, our meta-analysis provides more validated results.
It is important to note that most of the previous studies ignored the differences between cognitive tests. For example, the MMSE and the MoCA are mainly used to measure general cognitive function, but the sub-components of each test are different [64]. The MMSE emphasizes orientation and language activities while the MoCA emphasizes executive function and visual task domains [65]. Supporting this difference between the MMSE and the MoCA, in this meta-analysis we found that music-based intervention significantly improved MMSE scores but not MoCA scores. This result indicates that it would be better to consider this difference and separately perform meta-analysis for each test. However, we found only two studies using the MoCA [42,59]. Thus, it will be necessary to perform further meta-analysis in the near future.
Considering the types of interventions is important for an understanding of the beneficial effect of music-based intervention on cognitive function. Music-based intervention as a whole could conceptually be divided into receptive intervention type, which required the participants to listen to music, and active intervention type, which required the participants to play musical instruments, to sing songs, or to move with music. In this study, we found eight receptive interventions [41,45,47,48,50,52,56,58] and 11 active interventions [42,43,44,46,47,50,51,53,54,59]. Among the eight studies that measured MMSE scores [41,44,50,51,54,55,56,58], five studies involved receptive music activities [41,44,55,56,58] and three involved active music activities [50,51,54]. Of the eight studies, seven using the MMSE showed increases in MMSE performance [41,50,51,54,55,56,58]. These results indicate that any type of music-based intervention would have beneficial effects on general cognitive function.
The second main finding is that we demonstrated the positive effect of music-based intervention on executive function. In addition, we found that music-based intervention led to improvements in FAB and Verbal Fluency Test scores. Considering the types of interventions, three studies used receptive music activities [41,47,58] and six studies used active music activities [42,43,44,46,50,51]. Of the six studies included, the four studies using active music activities reported significant improvements in the performance of executive function [42,46,50,51]. Moreover, all four studies that measured the FAB used active music activities [42,43,46,51]. This suggests that active music-based intervention would have positive effects on executive function. This may be because active music intervention is more likely to promote socialization, engagement, verbal processing, or motor planning compared with receptive music intervention [66]. Since active music intervention has been utilized more often than receptive music intervention, future studies should investigate the effect of active music-based intervention on cognitive function.
The third and final main finding is that music-based intervention led to an improvement in episodic memory. In this meta-analysis, we included two studies [45,50], both of which used the AVLT as a measurement for episodic memory. The AVLT is an auditory verbal learning test using words [67]. The interventions asked the participants to sing and listen to their favorite songs, which were popular in their twenties and thirties, or listen to music and recall their experiences related to the music (reminiscence). The intervention required participants to understand the lyrics (semantic memory) and explicitly and implicitly recall past episodes (episodic memory) during music-based intervention. Therefore, this type of music-based intervention may facilitate episodic memory performance. Due to the small number of available studies, future studies are required that include other memory function measurements to clarify the effect of music-based intervention on episodic memory.
It would be too early to conclude that music-based intervention is not effective in processing speed performance. In this meta-analysis we found only five studies that investigated processing speed [41,44,46,47,58]. In addition, typical music-based intervention does not require the cognitive process related to processing speed [68]. Future studies should include episodic memory or processing speed components during music-based intervention.
It should be important to consider whether the intervention period of the included studies was sufficient to evaluate improvements in cognitive function. Previous systematic review and meta-analysis for non-pharmacological interventions such as cognitive training, exercise, nutrition revealed that previous studies used the similar intervention periods (from 4 to 12 weeks) [25,69,70,71,72]. The short-term intervention was able to improve cognitive functions in older adults with and without dementia. This indicated that the intervention period among the included studies was sufficient time to investigate the improvements in cognitive functions. However, whether an intervention period would affect the beneficial effect of music-based intervention on cognitive function is an important consideration. Further studies should investigate effects of shorter- and longer-term music-based intervention.
It is important to note results from supplementary meta-analyses based on MCI/dementia differences and the music-based intervention with the music therapist/the non-music-therapist (Please see Figure 3, Figure 6, and Figure 8). Music-based intervention improved general cognitive functions in both people with MCI and dementia. On the other hand, music-based intervention improved executive functions in people with dementia. Moreover, music-based intervention by the non-music therapist improved general cognitive functions and executive functions in people with MCI and dementia. However, we did not find any significant improvements from music-based intervention by the music therapist. There would be some consideration points. The main point is the small number of studies included for the supplementary analyses. We found only three studies with MCI and five studies with music therapists. The second point is the countries where the RCT was conducted. All studies with MCI were conducted in Japan. Looking at music-based intervention by a music therapist, four studies were conducted in Italy and one study was in USA. Therefore, we were unable to exclude the possibility of a cultural bias. In the future, there should be more studies to investigate whether benefits from music-based intervention would differ between people with MCI and dementia and between music-based intervention by a music therapist or not.
In the current meta-analysis, we did not include music-based interventions transduced into vibrotactile stimulation or single frequency sound. The music interventions we reviewed are those with sound perceived culturally as music and which we can naturally hear (20 Hz–20 kHz). Although vibrotactile aspects of sound and vibratory dimensions of music are frequently present as potentially therapeutic effects, they are less studied. A recent scoping review reported that vibration intervention had positive effects on cognitive functions [73]. In the future study, we should consider beneficial effects of music-based intervention using vibration on cognitive functions.
This study has several limitations. First, clinical heterogeneity between studies, such as severity of dementia, could not be avoided. Second, although we separately analyzed the clinical cognitive function assessment scales, some of the outcome domains had only one study. Third, some of the included studies had a small sample size. Due to the small number of included studies and the wide variety of participant characteristics, we were unable to conduct a stratified analysis. Fourth, the placebo effect in music intervention studies should have been mentioned. Participants did not know the purpose of the music intervention because they were blinded in 15 of the 19 included studies (see Table 1). However, almost all studies used passive control groups. In this case, participants in the music intervention group would think that they receive a beneficial intervention/treatment. Therefore, a placebo effect might occur because they would expect that their cognitive function would be improved. To reduce the placebo effect, the future study should use an active control intervention group. Finally, we did not consider a kinesthetic and physical aspect in the music-based intervention program. To exclude an effect of physical activity, in the future, we should compare similar physical activities groups with and without music.
5. Conclusions
This meta-analysis illustrates that music-based intervention can improve general cognitive function, executive function, and episodic memory performance in older adults with MCI and dementia. Music-based intervention, compared with other non-pharmacological interventions, is more implementable and less costly with little chance of adverse effects. Therefore, music-based intervention appears to be a suitable intervention to apply more frequently in the clinical field.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10081462/s1, Table S1: PRISMA checklist.
Author Contributions
Conceptualization, E.I. and R.N.; methodology, R.N.; formal analysis, E.I. and R.N.; investigation, E.I. and R.N.; data curation, E.I. and R.N.; writing—original draft preparation, E.I. and R.N.; writing—review and editing, E.I., R.N., J.D., C.-H.C. and B.S.H.; visualization, E.I. and R.N.; project administration, R.N.; funding acquisition, R.N. and J.D., E.I. and R.N. contributed equally to this work and share first authorship. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This study was supported by a grant from the Tohoku University-Université de Lorraine Joint Research Fund 2020. We were also supported by JSPS KAKENHI Grant Numbers 19H01760 and 22H01088 (Grant-in-Aid for Scientific Research (B). R.N. is supported by the JSPS Leading Initiative for Excellent Young Researchers (LEADER) program. None of the funding sources had any involvement in the study design, collection, analysis, interpretation of data, or writing of the paper.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nichols E., Steinmetz J.D., Vollset S.E., Fukutaki K., Chalek J., Abd-Allah F., Abdoli A., Abualhasan A., Abu-Gharbieh E., Akram T.T., et al. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7:e105–e125. doi: 10.1016/S2468-2667(21)00249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agüero-Torres H., Fratiglioni L., Guo Z., Viitanen M., Von Strauss E., Winblad B. Dementia Is the Major Cause of Functional Dependence in the Elderly: 3- Year Follow-up Data from a Population-Based Study. Am. J. Public Health. 1998;88:1452–1456. doi: 10.2105/AJPH.88.10.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clemmensen F.K., Hoffmann K., Siersma V., Sobol N., Beyer N., Andersen B.B., Vogel A., Lolk A., Gottrup H., Høgh P., et al. The Role of Physical and Cognitive Function in Performance of Activities of Daily Living in Patients with Mild-to-Moderate Alzheimer’s Disease—A Cross-Sectional Study. BMC Geriatr. 2020;20:513. doi: 10.1186/s12877-020-01926-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kallio E.L., Öhman H., Hietanen M., Soini H., Strandberg T.E., Kautiainen H., Pitkälä K.H. Effects of Cognitive Training on Cognition and Quality of Life of Older Persons with Dementia. J. Am. Geriatr. Soc. 2018;66:664–670. doi: 10.1111/jgs.15196. [DOI] [PubMed] [Google Scholar]
- 5.Cummings J.L., Tong G., Ballard C. Treatment Combinations for Alzheimer’s Disease: Current and Future Pharmacotherapy Options. J. Alzheimer’s Dis. 2019;67:779–794. doi: 10.3233/JAD-180766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ito E., Berge L.I., Husebo B.S., Nouchi R., Sandvik R.K.N.M. The Negative Impact of Psychotropic Drug Use on Quality of Life in Nursing Home Patients at Different Stages of Dementia: Cross-Sectional Analyses from the COSMOS Trial. J. Am. Med. Dir. Assoc. 2020;21:1623–1628. doi: 10.1016/j.jamda.2020.03.028. [DOI] [PubMed] [Google Scholar]
- 7.Karssemeijer E.G.A., Aaronson J.A., Bossers W.J., Smits T., Olde Rikkert M.G.M., Kessels R.P.C. Positive Effects of Combined Cognitive and Physical Exercise Training on Cognitive Function in Older Adults with Mild Cognitive Impairment or Dementia: A Meta-Analysis. Ageing Res. Rev. 2017;40:75–83. doi: 10.1016/j.arr.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Hill N.T.M., Mowszowski L., Naismith S.L., Chadwick V.L., Valenzuela M., Lampit A. Computerized Cognitive Training in Older Adults with Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Am. J. Psychiatry. 2017;174:329–340. doi: 10.1176/appi.ajp.2016.16030360. [DOI] [PubMed] [Google Scholar]
- 9.Vink A., Hanser S. Music-Based Therapeutic Interventions for People with Dementia: A Mini-Review. Medicines. 2018;5:109. doi: 10.3390/medicines5040109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baird A., Samson S. Music and Dementia. Prog. Brain Res. 2015;2017:207–235. doi: 10.1016/bs.pbr.2014.11.028. [DOI] [PubMed] [Google Scholar]
- 11.Sihvonen A.J., Särkämö T., Leo V., Tervaniemi M., Altenmüller E., Soinila S. Music-Based Interventions in Neurological Rehabilitation. Lancet Neurol. 2017;16:648–660. doi: 10.1016/S1474-4422(17)30168-0. [DOI] [PubMed] [Google Scholar]
- 12.Martorell A.J., Paulson A.L., Suk H.J., Abdurrob F., Drummond G.T., Guan W., Young J.Z., Kim D.N.W., Kritskiy O., Barker S.J., et al. Multi-Sensory Gamma Stimulation Ameliorates Alzheimer’s-Associated Pathology and Improves Cognition. Cell. 2019;177:256–271.e22. doi: 10.1016/j.cell.2019.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clements-Cortes A., Bartel L. Are We Doing More than We Know? Possible Mechanisms of Response to Music Therapy. Front. Med. 2018;5:255. doi: 10.3389/fmed.2018.00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bradt J., Dileo C. Music Interventions for Mechanically Ventilated Patients. Cochrane Database Syst. Rev. 2014;12:CD006902. doi: 10.1002/14651858.CD006902.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munro S., Mount B. Music Therapy in Palliative Care. Can. Med. Assoc. J. 1978;119:1029–1034. doi: 10.1093/med/9780199656097.003.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ray K.D., Mittelman M.S. Music Therapy: A Nonpharmacological Approach to the Care of Agitation and Depressive Symptoms for Nursing Home Residents with Dementia. Dementia. 2017;16:689–710. doi: 10.1177/1471301215613779. [DOI] [PubMed] [Google Scholar]
- 17.Tsoi K.K.F., Chan J.Y.C., Ng Y.-M., Lee M.M.Y., Kwok T.C.Y., Wong S.Y.S. Receptive Music Therapy Is More Effective than Interactive Music Therapy to Relieve Behavioral and Psychological Symptoms of Dementia: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2018;19:568–576.e3. doi: 10.1016/j.jamda.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 18.Moreno-Morales C., Calero R., Moreno-Morales P., Pintado C. Music Therapy in the Treatment of Dementia: A Systematic Review and Meta-Analysis. Front. Med. 2020;7:160. doi: 10.3389/fmed.2020.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fusar-Poli L., Bieleninik Ł., Brondino N., Chen X.J., Gold C. The Effect of Music Therapy on Cognitive Functions in Patients with Dementia: A Systematic Review and Meta-Analysis. Aging Ment. Health. 2018;22:1097–1106. doi: 10.1080/13607863.2017.1348474. [DOI] [PubMed] [Google Scholar]
- 20.van der Steen J.T., Smaling H.J., van der Wouden J.C., Bruinsma M.S., Scholten R.J., Vink A.C. Music-Based Therapeutic Interventions for People with Dementia. Cochrane Database Syst. Rev. 2018;7:CD003477. doi: 10.1002/14651858.CD003477.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harvey P.D. Domains of Cognition and Their Assessment. Dialogues Clin. Neurosci. 2019;21:227–237. doi: 10.31887/DCNS.2019.21.3/pharvey. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hung C.C., Chang C.C., Huang C.W., Nouchi R., Cheng C.H. Gut Microbiota in Patients with Alzheimer’s Disease Spectrum: A Systematic Review and Meta-Analysis. Aging. 2022;14:477–496. doi: 10.18632/aging.203826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sakaki K., Nouchi R., Matsuzaki Y., Saito T., Dinet J., Kawashima R. Benefits of VR Physical Exercise on Cognition in Older Adults with and without Mild Cognitive Decline: A Systematic Review of Randomized Controlled Trials. Healthcare. 2021;9:883. doi: 10.3390/healthcare9070883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nouchi R., Suiko T., Kimura E., Takenaka H., Murakoshi M., Uchiyama A., Aono M., Kawashima R. Effects of Lutein and Astaxanthin Intake on the Improvement of Cognitive Functions among Healthy Adults: A Systematic Review of Randomized Controlled Trials. Nutrients. 2020;12:617. doi: 10.3390/nu12030617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yagi A., Nouchi R., Butler L., Kawashima R. Lutein Has a Positive Impact on Brain Health in Healthy Older Adults: A Systematic Review of Randomized Controlled Trials and Cohort Studies. Nutrients. 2021;13:1746. doi: 10.3390/nu13061746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Folstein M.F., Folstein S.E., McHugh P.R. “Mini-Mental State”. A Practical Method for Grading the Cognitive State of Patients for the Clinician. J. Psychiatr. Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Panisset M., Roudier M., Saxton J., Boller F. Severe Impairment Battery. A Neuropsychological Test for Severely Demented Patients. Arch. Neurol. 1994;51:41–45. doi: 10.1001/archneur.1994.00540130067012. [DOI] [PubMed] [Google Scholar]
- 29.Nasreddine Z.S., Phillips N.A., Bédirian V., Charbonneau S., Whitehead V., Collin I., Cummings J.L., Chertkow H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 30.Rey A. L’examen Psychologique Dans Le Cas d’encephalopathie Traumatique. Arch. De Psychol. 1941;28:286–340. [Google Scholar]
- 31.Green P. Green’s Word Memory Test for Microsoft Windows: User’s Manual. Green’s Publishing; Edmonton, AB, Canada: 2005. [Google Scholar]
- 32.Reitan R.M. Validity of the Trail Making Test as an Indicator of Organic Brain Damage. Percept. Mot. Ski. 1958;8:271–276. doi: 10.2466/pms.1958.8.3.271. [DOI] [Google Scholar]
- 33.McLeod D.R., Griffiths R.R., Bigelow G.E., Yingling J. An Automated Version of the Digit Symbol Substitution Test (DSST) Behav. Res. Methods Instrum. 1982;14:463–466. doi: 10.3758/BF03203313. [DOI] [Google Scholar]
- 34.Dubois B., Slachevsky A., Litvan I., Pillon B. The FAB: A Frontal Assessment Battery at Bedside. Neurology. 2000;55:1621–1626. doi: 10.1212/WNL.55.11.1621. [DOI] [PubMed] [Google Scholar]
- 35.Moher D., Hopewell S., Schulz K.F., Montori V., Gøtzsche P.C., Devereaux P.J., Elbourne D., Egger M., Altman D.G. CONSORT 2010 Explanation and Elaboration: Updated Guidelines for Reporting Parallel Group Randomised Trials. Int. J. Surg. 2012;10:28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 36.Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savović J., Schulz K.F., Weeks L., Sterne J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deeks J.J., Higgins J.P., Altman D.G. Chapter 10: Analysing Data and Undertaking Meta-analyses. In: Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A., editors. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022) John Wiley & Sons, Ltd; Hoboken, NJ, USA: 2022. [(accessed on 10 June 2022)]. pp. 241–284. Available online: www.training.cochrane.org/handbook. [Google Scholar]
- 38.Balduzzi S., Rücker G., Schwarzer G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid. Based Ment. Health. 2019;22:153–160. doi: 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Viechtbauer W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010;36:1–48. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- 40.Higgins J.P.T., Thompson S.G. Quantifying Heterogeneity in a Meta-Analysis. Stat. Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 41.Doi T., Verghese J., Makizako H., Tsutsumimoto K., Hotta R., Nakakubo S., Suzuki T., Shimada H. Effects of Cognitive Leisure Activity on Cognition in Mild Cognitive Impairment: Results of a Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2017;18:686–691. doi: 10.1016/j.jamda.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 42.Miyazaki A., Mori H. Frequent Karaoke Training Improves Frontal Executive Cognitive Skills, Tongue Pressure, and Respiratory Function in Elderly People: Pilot Study from a Randomized Controlled Trial. Int. J. Environ. Res. Public Health. 2020;17:12–14. doi: 10.3390/ijerph17041459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shimizu N., Umemura T., Matsunaga M., Hirai T. Effects of Movement Music Therapy with a Percussion Instrument on Physical and Frontal Lobe Function in Older Adults with Mild Cognitive Impairment: A Randomized Controlled Trial. Aging Ment. Health. 2018;22:1614–1626. doi: 10.1080/13607863.2017.1379048. [DOI] [PubMed] [Google Scholar]
- 44.Giovagnoli A.R., Manfredi V., Parente A., Schifano L., Oliveri S., Avanzini G. Cognitive Training in Alzheimer’s Disease: A Controlled Randomized Study. Neurol. Sci. 2017;38:1485–1493. doi: 10.1007/s10072-017-3003-9. [DOI] [PubMed] [Google Scholar]
- 45.Mahendran R., Gandhi M., Moorakonda R.B., Wong J., Kanchi M.M., Fam J., Rawtaer I., Kumar A.P., Feng L., Kua E.H. Art Therapy Is Associated with Sustained Improvement in Cognitive Function in the Elderly with Mild Neurocognitive Disorder: Findings from a Pilot Randomized Controlled Trial for Art Therapy and Music Reminiscence Activity versus Usual Care. Trials. 2018;19:615. doi: 10.1186/s13063-018-2988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pongan E., Tillmann B., Leveque Y., Trombert B., Getenet J.C., Auguste N., Dauphinot V., el Haouari H., Navez M., Dorey J.-M., et al. Can Musical or Painting Interventions Improve Chronic Pain, Mood, Quality of Life, and Cognition in Patients with Mild Alzheimer’s Disease? Evidence from a Randomized Controlled Trial. J. Alzheimer’s Dis. 2017;60:663–677. doi: 10.3233/JAD-170410. [DOI] [PubMed] [Google Scholar]
- 47.Innes K.E., Selfe T.K., Brundage K., Montgomery C., Wen S., Kandati S., Bowles H., Khalsa D.S., Huysmans Z. Effects of Meditation and Music-Listening on Blood Biomarkers of Cellular Aging and Alzheimer’s Disease in Adults with Subjective Cognitive Decline: An Exploratory Randomized Clinical Trial. J. Alzheimer’s Dis. 2018;66:947–970. doi: 10.3233/JAD-180164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim D. The Effects of a Recollection-Based Occupational Therapy Program of Alzheimer’s Disease: A Randomized Controlled Trial. Occup. Ther. Int. 2020;2020:6305727. doi: 10.1155/2020/6305727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yu-ling C., Yu-Cheng P. Musical Dual-Task Training in Patients with Mild-to- Moderate Dementia: A Randomized Controlled Trial. Neuropsychiatr. Dis. Treat. 2018;14:1381–1393. doi: 10.2147/NDT.S159174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lyu J., Zhang J., Mu H., Li W., Champ M., Xiong Q., Gao T., Xie L., Jin W., Yang W., et al. The Effects of Music Therapy on Cognition, Psychiatric Symptoms, and Activities of Daily Living in Patients with Alzheimer’s Disease. J. Alzheimer’s Dis. 2018;64:1347–1358. doi: 10.3233/JAD-180183. [DOI] [PubMed] [Google Scholar]
- 51.Miyazaki A., Okuyama T., Mori H., Sato K., Ichiki M., Nouchi R. Drum Communication Program Intervention in Older Adults With Cognitive Impairment and Dementia at Nursing Home: Preliminary Evidence From Pilot Randomized Controlled Trial. Front. Aging Neurosci. 2020;12:142. doi: 10.3389/fnagi.2020.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giovagnoli A.R., Manfredi V., Schifano L., Paterlini C., Parente A., Tagliavini F. Combining Drug and Music Therapy in Patients with Moderate Alzheimer’s Disease: A Randomized Study. Neurol. Sci. 2018;39:1021–1028. doi: 10.1007/s10072-018-3316-3. [DOI] [PubMed] [Google Scholar]
- 53.Narme P., Clément S., Ehrlé N., Schiaratura L., Vachez S., Courtaigne B., Munsch F., Samson S. Efficacy of Musical Interventions in Dementia: Evidence from a Randomized Controlled Trial. J. Alzheimer’s Dis. 2014;38:359–369. doi: 10.3233/JAD-130893. [DOI] [PubMed] [Google Scholar]
- 54.van de Winckel A., Feys H., de Weerdt W., Dom R. Cognitive and Behavioural Effects of Music-Based Exercises in Patients with Dementia. Clin. Rehabil. 2004;18:253–260. doi: 10.1191/0269215504cr750oa. [DOI] [PubMed] [Google Scholar]
- 55.Ceccato E., Vigato G., Bonetto C., Bevilacqua A., Pizziolo P., Crociani S., Zanfretta E., Pollini L., Caneva P.A., Baldin L., et al. STAM Protocol in Dementia: A Multicenter, Single-Blind, Randomized, and Controlled Trial. Am. J. Alzheimer’s Dis. Other Dement. 2012;27:301–310. doi: 10.1177/1533317512452038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li D.M., Li X.X. The Effect of Folk Recreation Program in Improving Symptoms: A Study of Chinese Elder Dementia Patients. Int. J. Geriatr. Psychiatry. 2017;32:901–908. doi: 10.1002/gps.4543. [DOI] [PubMed] [Google Scholar]
- 57.Chen X., Li D., Xu H., Hu Z. Effect of Traditional Opera on Older Adults with Dementia. Geriatr. Nurs. 2020;41:118–123. doi: 10.1016/j.gerinurse.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 58.Innes K.E., Selfe T.K., Khalsa D.S., Kandati S. Meditation and Music Improve Memory and Cognitive Function in Adults with Subjective Cognitive Decline: A Pilot Randomized Controlled Trial. J. Alzheimer’s Dis. 2017;56:899–916. doi: 10.3233/JAD-160867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pohl P., Wressle E., Lundin F., Enthoven P., Dizdar N. Group-Based Music Intervention in Parkinson’s Disease—Findings from a Mixed-Methods Study. Clin. Rehabil. 2020;34:533–544. doi: 10.1177/0269215520907669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Raglio A., Bellandi D., Baiardi P., Gianotti M., Ubezio M.C., Zanacchi E., Granieri E., Imbriani M., Stramba-Badiale M. Effect of Active Music Therapy and Individualized Listening to Music on Dementia: A Multicenter Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015;63:1534–1539. doi: 10.1111/jgs.13558. [DOI] [PubMed] [Google Scholar]
- 61.Mate K.E., Pond C.D., Magin P.J., Goode S.M., McElduff P., Stocks N.P. Diagnosis and Disclosure of a Memory Problem Is Associated with Quality of Life in Community Based Older Australians with Dementia. Int. Psychogeriatr. 2012;24:1962–1971. doi: 10.1017/S1041610212001111. [DOI] [PubMed] [Google Scholar]
- 62.Davis J.C., Marra C.A., Najafzadeh M., Liu-Ambrose T. The Independent Contribution of Executive Functions to Health Related Quality of Life in Older Women. BMC Geriatr. 2010;10:16. doi: 10.1186/1471-2318-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stites S.D., Harkins K., Rubright J.D., Karlawish J. Relationships Between Cognitive Complaints and Quality of Life in Older Adults With Mild Cognitive Impairment, Mild Alzheimer Disease Dementia, and Normal Cognition. Alzheimer Dis. Assoc. Disord. 2018;32:276–283. doi: 10.1097/WAD.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kang J.M., Cho Y.S., Park S., Lee B.H., Sohn B.K., Choi C.H., Choi J.S., Jeong H.Y., Cho S.J., Lee J.H., et al. Montreal Cognitive Assessment Reflects Cognitive Reserve. BMC Geriatr. 2018;18:261. doi: 10.1186/s12877-018-0951-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Siqueira G.S.A., Hagemann P.D.M.S., Coelho D.D.S., Santos F.H.D., Bertolucci P.H.F., Heyn P.C. Can MoCA and MMSE Be Interchangeable Cognitive Screening Tools? A Systematic Review. Gerontologist. 2019;59:E743–E763. doi: 10.1093/geront/gny126. [DOI] [PubMed] [Google Scholar]
- 66.Gómez-Gallego M., Gómez-Gallego J.C., Gallego-Mellado M., García-García J. Comparative Efficacy of Active Group Music Intervention versus Group Music Listening in Alzheimer’s Disease. Int. J. Environ. Res. Public Health. 2021;18:8067. doi: 10.3390/ijerph18158067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernaeus S.E., Östberg P., Wahlund L.O., Hellström Å. Memory Factors in Rey AVLT: Implications for Early Staging of Cognitive Decline. Scand. J. Psychol. 2014;55:546–553. doi: 10.1111/sjop.12157. [DOI] [PubMed] [Google Scholar]
- 68.Zhang Y., Cai J., An L., Hui F., Ren T., Ma H., Zhao Q. Does Music Therapy Enhance Behavioral and Cognitive Function in Elderly Dementia Patients? A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2017;35:1–11. doi: 10.1016/j.arr.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 69.Alnajjar F., Khalid S., Vogan A.A., Shimoda S., Nouchi R., Kawashima R. Emerging Cognitive Intervention Technologies to Meet the Needs of an Aging Population: A Systematic Review. Front. Aging Neurosci. 2019;11:291. doi: 10.3389/fnagi.2019.00291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kawata N.Y.S., Nouchi R., Oba K., Matsuzaki Y., Kawashima R. Auditory Cognitive Training Improves Brain Plasticity in Healthy Older Adults: Evidence From a Randomized Controlled Trial. Front. Aging Neurosci. 2022;14:826672. doi: 10.3389/fnagi.2022.826672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nouchi R., Hu Q., Saito T., Kawata N.Y.d.S., Nouchi H., Kawashima R. Brain Training and Sulforaphane Intake Interventions Separately Improve Cognitive Performance in Healthy Older Adults, Whereas a Combination of These Interventions Does Not Have More Beneficial Effects: Evidence from a Randomized Controlled Trial. Nutrients. 2021;13:352. doi: 10.3390/nu13020352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nouchi R., Nouchi H., Dinet J., Kawashima R. Cognitive Training with Neurofeedback Using NIRS Improved Cognitive Functions in Young Adults: Evidence from a Randomized Controlled Trial. Brain Sci. 2021;12:5. doi: 10.3390/brainsci12010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hung L., Van E.A., Zee D., Bernardo-Filho M., Da D., De C., Caputo S., Campbell E.A., Kantor J., Kantorová L., et al. Tactile Low Frequency Vibration in Dementia Management: A Scoping Review. Front. Psychol. 2022;1:854794. doi: 10.3389/fpsyg.2022.854794. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.