Abstract
N-myc downstream-regulated gene 2 (NDRG2) is a tumor-suppressor gene that suppresses tumorigenesis and metastasis of tumors and increases sensitivity to anti-cancer drugs. In this review, we summarize information on the clinicopathological characteristics of tumor patients according to NDRG2 expression in various tumor tissues and provide information on the metastasis inhibition-related cell signaling modulation by NDRG2. Loss of NDRG2 expression is a prognostic factor that correlates with TNM grade and tumor metastasis and has an inverse relationship with patient survival in various tumor patients. NDRG2 inhibits cell signaling, such as AKT-, NF-κB-, STAT3-, and TGF-β-mediated signaling, to induce tumor metastasis, and induces activation of GSK-3β which has anti-tumor effects. Although NDRG2 operates as an adaptor protein to mediate the interaction between kinases and phosphatases, which is essential in regulating cell signaling related to tumor metastasis, the molecular mechanism of NDRG2 as an adapter protein does not seem to be fully elucidated. This review aims to assist the research design regarding NDRG2 function as an adaptor protein and suggests NDRG2 as a molecular target to inhibit tumor metastasis and improve the prognosis in tumor patients.
Keywords: NDRG2, metastasis, epithelial–mesenchymal transition, tumor-suppressor
1. Introduction
N-myc downstream-regulated gene 2 (NDRG2) belongs to the NDRG family along with NDRG1, -3, and -4, forms a homologous cluster in several species, and is characterized by an NDR protein domain consisting of an esterase-/lipase-/thioesterase-active-site serine and an α/β-hydrolase fold of approximately 220 amino acids. However, NDRG proteins have no enzymatic activity [1,2,3]. NDRG2 has been proposed as a functional gene in response to cellular stresses in cellular metabolic processes [4,5,6], hypoxia [7], and lipotoxicity [8]. Additionally, the functions of NDRG2 as a tumor suppressor contribute to tumor growth inhibition and anti-metastasis in various tumors. Tumor metastasis is known to be the main cause of death in cancer patients [9]. Metastasis is the process of moving from the primary tumor to other organs due to the limited supply of oxygen and nutrients and the epithelial–mesenchymal transition (EMT) step is a key step for metastasis [10,11,12,13]. In this review, we aim to provide useful information for tumor control studies by summarizing clinicopathological properties in various tumors and presenting the function of NDRG2 as a modulator of cell signaling for EMT.
2. Anti-Tumor Function of NDRG2 Based on Clinicopathological Characteristics of Various Tumor Patients
The expression of NDRG2 seems more reasonable to be suggested as a prognostic marker related to the reduction in pathological symptoms of the tumor rather than a diagnostic marker related to tumor development. NDRG2 expression is regulated at the transcriptional or the post-transcriptional step. Hypermethylation of the NDRG2 promoter region is a representative mechanism of NDRG2 transcriptional repression in various tumors [14,15,16,17,18,19]. Another mechanism regulating NDRG2 expression is mediated by microRNAs (miRNAs); miRNA-181c [20], miR-454 [21], miR-483 [22], miR-650 [23], and et al. NDRG2 expression level is positively correlated with tumor differentiation and overall survivals, but negatively correlated with tumor invasion, tumor recurrence, lymph node metastasis, and TNM staging in various tumor patients (Table 1).
Table 1.
Clinicopathological role of NDRG2 in tumors.
| Tumor | Reported Findings | Refs. |
|---|---|---|
| Astrocytoma |
|
[24,25] |
| Bladder cancer |
|
[26] |
| Breast cancer |
|
[27] |
|
[28] | |
|
[4] | |
| Colorectal cancer |
|
[23] |
|
[29] | |
|
[30] | |
|
[31] | |
| Esophageal cancer |
|
[32,33,34] |
| Gallbladder cancer |
|
[35] |
|
[36] | |
| Gastric cancer |
|
[37] |
|
[38] | |
|
[15] | |
| Glioma |
|
[19] |
|
[39] | |
|
[40] | |
| Liver cancer |
|
[41] |
|
[17] | |
|
[42] | |
|
[20] | |
| Lung cancer |
|
[43] |
| Renal cancer |
|
[44] |
|
[45] |
3. Anti-Metastatic Role of NDRG2
3.1. Epithelial–Mesenchymal Transition (EMT) and NDRG2
Cancers have the potential to metastasize and most cancer patients die from uncontrolled metastasis [46,47]. Therefore, establishing a strategy to control or inhibit tumor metastasis is very important for increasing the survival rate and treatment of tumor patients. Metastasis is a multi-step process initiated by the escape of tumor cells from primary tumor tissue and ending with the colonization of secondary tumors at distant tissues from the primary site. The steps of metastasis can be subdivided into the escape of cancer cells from the primary tumor, intravascular invasion, survival, extravasation, and colonization [48,49,50,51]. EMT is a key mechanism for promoting cancer metastasis, whereby cell types with a mesenchymal phenotype generally become invasive [52]. EMT is regulated by activation of the SNAI, ZEB, and TWIST transcription factor network (EMT-TF) families, which directly repress epithelial marker genes involved in cell adhesion, polarity, and cytoskeletal organization [53]. Various cellular signaling pathways, such as TGF-β signaling and AKT, NF-κB, and STAT3 activation, can induce the expression of EMT-TFs and metastatic effector proteins [54,55,56,57,58,59]. NDRG2 expression correlates inversely with TNM grade and metastasis in tumor patients (Table 1) and inhibits invasion and metastasis of tumor cells by modulating metastatic cell signaling pathways.
3.2. AKT and NDRG2
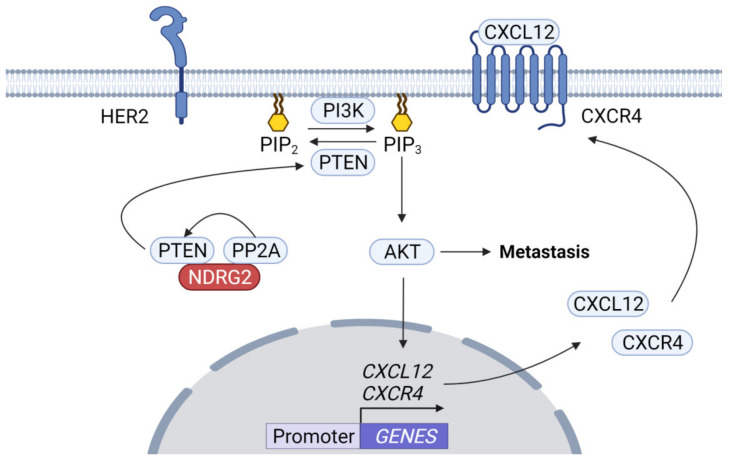
Bone is a common metastasis site in various cancer patients [60,61,62]. The phosphoinositide 3-kinase (PI3K)/AKT signaling pathway has been implicated in bone metastasis in several tumors. pAKT levels are elevated in 81.8% of primary HER2-positive breast cancers with bone metastasis, suggesting that the HER2/CXCR4/AKT pathway plays a role in bone metastasis [57]. The function of the CXCL12/CXCR4 axis in promoting metastasis is mediated in part by AKT activation [63,64]. In addition, bone metastasis is more frequently induced by breast cancer cells with hypoxia-inducing factor 1α (HIF-1α), which responds to hypoxia and is stabilized by AKT, resulting in CXCR4 upregulation [65]. Further, overexpression of AKT1 in prostate cancers upregulates CXCR4 expression and loss of PTEN in the cells enhances AKT-mediated expression of CXCL12 and CXCR4 [66]. Low NDRG2 expression is associated with pAKT and XIAP upregulation, while overexpression of NDRG2 suppresses AKT/XIAP signaling pathway and EMT in esophageal cancer cells [34]. NDRG2 is considered a PTEN-binding protein recruiting protein phosphatase 2A (PP2A) to PTEN, which inhibits PI3K-AKT pathway via PTEN activation by PP2A in adult T-cell leukemia-lymphoma (ATLL) (Figure 1) [67]. Therefore, it is possible NDRG2 inhibits metastasis mediated by AKT activation pathway by acting as a bridge between PP2A and PTEN to inhibit PI3K activation.
Figure 1.
AKT inhibition by the NDRG2–PP2A complex. HER2 activates PI3K/AKT signaling. PTEN is a dual protein/lipid phosphatase using phosphatidylinositol, 3,4,5 triphosphate (PIP3), a product of PI3K, as a substrate. An increase in PIP3 recruits AKT to the membrane, which is activated by other PIP3-dependent kinases. NDRG2 acts as a bridge mediating the interaction between PP2A and PTEN, thus the NDRG2–PP2A complex recruits PTEN and triggers its activation. PTEN can inhibit AKT activity by inducing dephosphorylation of PIP3, thereby inhibiting AKT-dependent tumor cell metastasis.
3.3. Nuclear Factor-κB (NF-κB) and NDRG2
NF-κB is a key transcription factor contributing to pathogenesis of inflammation and cancer [68]. NF-κB forms a complex with IκB in the cytoplasm, and when IκBα is ubiquitinated and subsequently degraded by the 26S proteasome, NF-κB is released and migrates to the nucleus to act as a transcription factor. Specifically, NF-κB activation is a potential mechanism explaining the relationship between inflammation and tumors [69]. Metastatic breast cancer cells overexpress the chemokine receptor CXCR4, and metastatic tissues express a large amount of CXCL12, a ligand of CXCR4 [48]. Further, NF-κB activation induces expression of matrix metalloproteinases, urokinase-type plasminogen activators, and cytokines in metastatic breast cancer cell lines [58]. NF-κB p65 (RelA) is constitutively activated in gastric cancer, which correlated with cancer invasion-associated clinicopathological features, lymphoid invasion, depth of invasion, and peritoneal metastasis [70]. Activation of NF-κB induces osteolytic bone metastasis by inducing CSF2 (GM-CSF) expression [71]. Loss of NDRG2 expression is associated with tumor metastasis by inducing EMT via NF-κB activation [72]. NDRG2 attenuated NF-κB activation in PMA-treated human breast cancer cell (MDA-MB-231), which suppresses migration and invasion by inhibiting COX-2 expression [73]. Furthermore, NDRG2 suppresses tumor invasion by attenuating matrix metalloproteinase 9 (MMP9) expression via NF-κB inhibition [74].
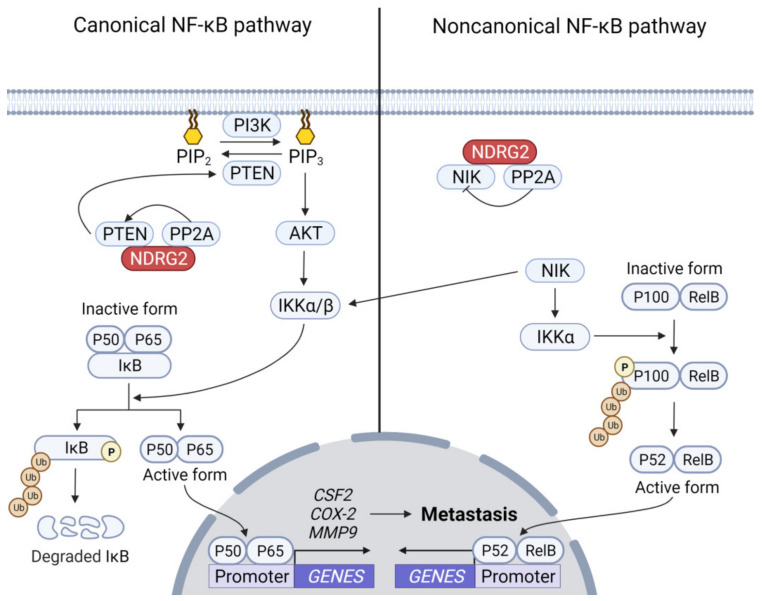
Although NDRG2 expression likely inhibits NF-κB-mediated tumor metastasis, how NDRG2 inhibits NF-κB activity remains unclear. Recently, Ichikawa et al. proposed NDRG2 inhibits NF-κB in canonical and non-canonical pathways [75]. In the canonical pathway, the PI3K-AKT signaling pathway enhances the activation of canonical NF-κB [76,77] and NDRG2-mediated PTEN activation may inhibit canonical NF-κB by attenuating the PI3K-AKT activation pathway. In the non-canonical NF-κB pathway, activated NF-κB-inducing kinase (NIK) phosphorylates IKKα, which leads to phosphorylation of p100 to partially degrade p52 formation. RelB-bound p52 translocates into the nucleus to induce target genes (Figure 2) [78,79,80]. NDRG2 inhibits non-canonical NF-κB by interacting with NIK, followed by dephosphorylation of NIK via the NDRG2–PP2A complex.
Figure 2.
Inhibition of NF-κB-dependent tumor cell metastasis by NDRG2. The PI3K/AKT/IKKα/NF-κB pathway contributes to tumor cell metastasis by inducing related genes, such as CSF2, COX-2, and MMP9. IKKα is also a substrate of NIK. NDRG2 inhibits the canonical NF-κB pathway via AKT inhibition to inhibit IKKα activation. Activated NIK induces phosphorylation of IKKα, which phosphorylates p100 to process p100 to p52 in a proteasome-dependent manner. The NDRG2–PP2A complex dephosphorylates NIK to inhibit the non-canonical NF-κB pathway.
3.4. Signal Transducer and Activator of Transcription 3 (STAT3) and NDRG2
Activation of STAT proteins is typically induced by Janus-Kinase (JAK) family proteins which are receptor-associated tyrosine kinases [81]. Activation of STAT3 occurs in a variety of tumors and aberrant STAT3 activation is associated with tumorigenesis and invasion promotion [82,83,84,85]. Metastatic spread of tumor cells requires cell motility, extracellular matrix infiltration, and angiogenesis. STAT3 activation contributes to enhancement of integrin 6 expression that promotes tumor cell motility, acquisition of invasive traits such as MUC1, Bcl6, cathepsins, and UPA, and increases expression of MMPs [86,87,88]. Furthermore, expression of E-cadherin, a representative anti-metastatic phenotype, is inhibited by STAT3 activation. STAT3 regulates ZEB1 expression, which can participate in STAT3-induced cell invasion and E-cadherin downregulation in colorectal cancer [89]. TWIST, an EMT-TF, is transcriptionally induced by STAT3 activation and plays a role as a transcriptional repressor of E-cadherin [59,90]. STAT3 also contributes to angiogenesis through the action of a transcription factor inducing vascular endothelial growth factor (VEGF) expression [91,92]. In unstimulated cells, STAT3 is regulated by negative regulators, protein inhibitors of activated STATs (PIAS), members of the cytokine signaling inhibitor (SOCS) family, protein tyrosine phosphatases (SHP1, SHP2, PTPN1, PTPN2 PTPRD, and PTPRT), and ubiquitin enzymes, to remain inactive in the cytoplasm [93,94]. SOCS expression can be induced by STAT3 activation, after which SOCS becomes a STAT3 regulator [95]. Overexpression of NDRG2 can inhibit STAT3 activation by inducing SOCS1 [96] and inhibition of STAT3 by NDRG2 suppresses EMT by reducing SNAIL expression (Figure 3) [97]. The transcription factor MYB activates STAT3 and AKT pathways by inhibiting NDRG2 expression via miR-130a expression in salivary adenoid cystic carcinoma [98]. Although NDRG2 regulates on STAT3 and SOCS1 induction in NDRG2-expressed cells, which is considered a mechanism for NDRG2-mediated STAT3 inhibition, the molecular mechanism is still unclear. Further analysis into the molecular mechanisms is needed, such as (1) how does NDRG2 induce SOCS1 expression, and (2) can NDRG2 play a role as a bridge to allow JAKs or STAT3 to interact with protein tyrosine phosphatases?
Figure 3.
Inhibition of STAT3 activation pathway by NDRG2. JAK is activated upon cytokine or growth factors, resulting in dimerization through phosphorylation and nuclear translocation of STAT3 to induce transcription of metastasis-related genes, such as ZEB1, TWIST, SNAIL, and VEGF. Cytokine signaling inhibitory factor (SOCS) protein is a representative negative regulator on JAK. NDRG2 induces SOCS1 expression through an unknown mechanism (dash line) and SOCS1 inhibits STAT3-mediated tumor cell metastasis by inhibiting JAK activation.
3.5. TGF-β and NDRG2
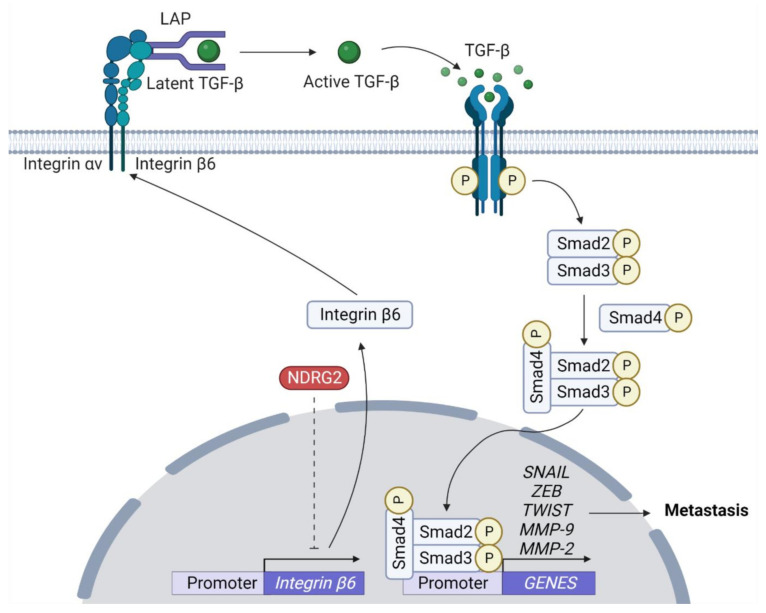
Although TGF-β plays a tumor-suppressor function, in the later stages of cancer progression, cancer cells remain responsive to TGF-β but become resistant to the cell proliferation inhibitory effects by TGF-β. Here, TGF-β acts directly on the cancer cells, leading to EMT through induction of E-cadherin transcriptional repressors, such as SNAIL, ZEB, and TWIST [99,100]. TGF-β binds to the receptor and induces formation of a complex with Smad2, Smad3, and Smad4, which regulates the expression of various target genes [101]. Further, TGF-β-induced EMT is closely related to proteolytic activity of MMPs [102]. Among the MMP family, MMP2 plays an important role in basement membrane remodeling by degrading collagen I, IV, V, plasminogen, and laminin-5 [103,104,105]. Further, NDRG2 can antagonize TGF-β-mediated liver cancer cell invasion by downregulating expression of MMP2 and laminin 332 pathway components [41]. Meanwhile, integrin complexes, integrin αν and integrin β6, induce conversion from latent TGF-β into its active form [106]. In a mouse breast cancer cell model, overexpression of NDRG2 disrupts TGF-β-mediated gene expression and inhibits conversion from latent TGF-β by reducing of integrin β6 expression, which inhibits tumor cell invasion (Figure 4) [28]. Despite growing cell biological and clinical evidence on the relationship between NDRG2 expression and inhibition of TGF-β-mediated tumor metastasis, its molecular mechanism is yet to be identified.
Figure 4.
NDRG2-mediated inhibition of TGF-β signaling. αvβ6 activates TGF-β by binding to tripeptide Arg-Gly-Asp (RGD) motif of the latency-associated peptide (LAP). When integrins bind to the RGD motif of LAP, their binding to the actin cytoskeleton triggers a conformational change that releases active TGF-β. TGF-β via SMAD signaling can induce expression of EMT-TFs, such as SNAIL, TWIST, and ZEB, and MMP2. NDRG2 inhibits the conversion of latent TGF-β to active TGF-β by inhibiting expression of integrin β6 through an unknown mechanism (dash line).
3.6. GSK-3β and NDRG2
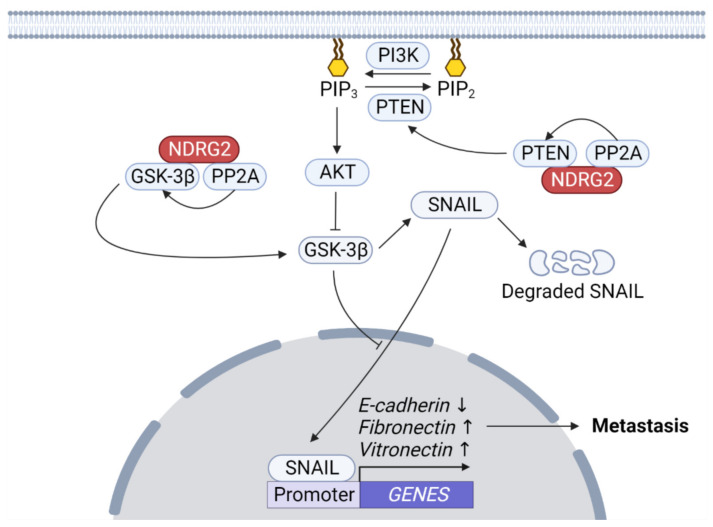
Overexpression of constitutively active GSK-3β mutants increases chemosensitivity, cell cycle arrest, and decreases tumorigenicity [107,108]. GSK-3 can inhibit the Wnt/β-catenin pathway by phosphorylating β-catenin, leading to ubiquitin/proteasome-dependent degradation of β-catenin that serves as a transactivator for TCF/LEFs. Therefore, GSK-3 acts as a tumor suppressor by inhibiting β-catenin-mediated tumorigenic characteristics including EMT [109,110]. AKT induces inactivation of GSK-3β, which in turn inhibits SNAIL phosphorylation, leading to SNAIL translocation into the nucleus and its stabilization leading to EMT [111,112]. Phosphoinositide 3-kinase (PI3K)-mediated AKT activation signaling is inhibited by phosphatase and tensin homolog (PTEN) which dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate [113]. The GSK-3β mechanism activation resulting in EMT inhibition in NDRG2-overexpressed cells can be considered as follows: (1) NDRG2 as a PTEN-binding protein recruits PP2A to PTEN, which activates PTEN and inhibits PI3K-AKT signaling [67]; (2) NDRG2 forms a complex with PP2A and GSK-3β, then induces the activation of GSK-3β by removing inhibitory phosphorylation of GSK-3 β by PP2A (Figure 5) [114].
Figure 5.
NDRG2–PP2A-mediated GSK-3β activation. AKT induces inhibitory phosphorylation of glycogen synthase kinase-3 beta (GSK-3β). The NDRG2–PP2A complex recruits PTEN, which dephosphorylates PIP3 to inhibit AKT activation. Further, the NDRG2–PP2A complex releases the inhibitory phosphate of GSK-3β to activate it. Active GSK-3β phosphorylates SNAIL to induce β-Trcp-mediated ubiquitination and degradation, which controls its subcellular localization. GSK-3β activation downregulates EMT phenotypes, such as E-cadherin upregulation and fibronectin and vitronectin downregulation.
4. Conclusions and Outlook
Although expression of NDRG2 is not abolished in all carcinomas and tumor tissues, low expression of NDRG2 is closely related to poor prognosis, such as increased metastasis, higher TNM stage, and reduced survival. specifically, metastasis of tumor cells can worsen patient prognosis. Therefore, tumor metastasis inhibition may be a therapeutic strategy to improve prognosis and improve patient survival rate. Studies on NDRG2-mediated inhibition of tumor metastasis can provide useful scientific information on development of tumor therapeutics.
Although NDRG2 is a protein without enzymatic activity, it is involved in many cellular signaling pathways. We propose the role of NDRG2 bridging in mediating interactions between different proteins is crucial in modulating NDRG2-mediated cellular signaling. As an adapter protein, NDRG2 is already known to mediate AKT inhibition, NF-κB inhibition, and GSK3 activation by mediating PP2A/PTEN, PP2A/NIK and PP2A/GSK3 interactions, respectively. However, to clarify the molecular mechanism of NDRG2 related to the anti-tumor phenotype, further analysis of the interactions between kinase and NDRG2 located upstream of cell signaling, as well as interaction between NDRG2 and various phosphatases, such as serine/threonine phosphatases and tyrosine phosphatases, is needed. In particular, although a direct inhibitory mechanism for receptor tyrosine kinases (RTK) by NDRG2 has not been reported so far, we suggest research on the NDRG2–tyrosine phosphatase complex is necessary as a regulatory mechanism for RTK.
Author Contributions
Manuscript was designed, written, and reviewed by K.D.K., K.W.L. and S.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the BioGreen21 Agri-Tech Innovation Program (PJ015731), Rural Development Administration, Korea, and the National Research Foundation of Korea (NRF) grant (2021R1A2C1004847 and 2021R1A5A8029490) funded by the Korean government (MSIT).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Melotte V., Qu X., Ongenaert M., van Criekinge W., de Bruine A.P., Baldwin H.S., van Engeland M. The N-myc downstream regulated gene (NDRG) family: Diverse functions, multiple applications. FASEB J. 2010;24:4153–4166. doi: 10.1096/fj.09-151464. [DOI] [PubMed] [Google Scholar]
- 2.Shaw E., McCue L.A., Lawrence C.E., Dordick J.S. Identification of a novel class in the alpha/beta hydrolase fold superfamily: The N-myc differentiation-related proteins. Proteins. 2002;47:163–168. doi: 10.1002/prot.10083. [DOI] [PubMed] [Google Scholar]
- 3.Qu X., Zhai Y., Wei H., Zhang C., Xing G., Yu Y., He F. Characterization and expression of three novel differentiation-related genes belong to the human NDRG gene family. Mol. Cell. Biochem. 2002;229:35–44. doi: 10.1023/A:1017934810825. [DOI] [PubMed] [Google Scholar]
- 4.Ma J., Liu W., Guo H., Li S., Cao W., Du X., Lei S., Hou W., Xiong L., Yao L., et al. N-myc downstream-regulated gene 2 expression is associated with glucose transport and correlated with prognosis in breast carcinoma. Breast Cancer Res. 2014;16:R27. doi: 10.1186/bcr3628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y., Yang J., Li S., Zhang J., Zheng J., Hou W., Zhao H., Guo Y., Liu X., Dou K., et al. N-myc downstream-regulated gene 2, a novel estrogen-targeted gene, is involved in the regulation of Na+/K+-ATPase. J. Biol. Chem. 2011;286:32289–32299. doi: 10.1074/jbc.M111.247825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Y., Liu C., Hou W., Li Y., Ma J., Lin K., Situ Z., Xiong L., Li S., Yao L. Retrograde ductal administration of the adenovirus-mediated NDRG2 gene leads to improved sialaden hypofunction in estrogen-deficient rats. Mol. Ther. 2014;22:908–918. doi: 10.1038/mt.2013.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ma Y.L., Zhang L.X., Liu G.L., Fan Y., Peng Y., Hou W.G. N-Myc Downstream-Regulated Gene 2 (Ndrg2) Is Involved in Ischemia-Hypoxia-Induced Astrocyte Apoptosis: A Novel Target for Stroke Therapy. Mol. Neurobiol. 2017;54:3286–3299. doi: 10.1007/s12035-016-9814-5. [DOI] [PubMed] [Google Scholar]
- 8.Shen L., Liu X., Hou W., Yang G., Wu Y., Zhang R., Li X., Che H., Lu Z., Zhang Y., et al. NDRG2 is highly expressed in pancreatic beta cells and involved in protection against lipotoxicity. Cell. Mol. Life Sci. 2010;67:1371–1381. doi: 10.1007/s00018-010-0258-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wan L., Pantel K., Kang Y. Tumor metastasis: Moving new biological insights into the clinic. Nat. Med. 2013;19:1450–1464. doi: 10.1038/nm.3391. [DOI] [PubMed] [Google Scholar]
- 10.Valastyan S., Weinberg R.A. Tumor metastasis: Molecular insights and evolving paradigms. Cell. 2011;147:275–292. doi: 10.1016/j.cell.2011.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thiery J.P., Acloque H., Huang R.Y., Nieto M.A. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871–890. doi: 10.1016/j.cell.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Savagner P. Leaving the neighborhood: Molecular mechanisms involved during epithelial-mesenchymal transition. Bioessays. 2001;23:912–923. doi: 10.1002/bies.1132. [DOI] [PubMed] [Google Scholar]
- 13.Kalluri R., Weinberg R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009;119:1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lusis E.A., Watson M.A., Chicoine M.R., Lyman M., Roerig P., Reifenberger G., Gutmann D.H., Perry A. Integrative genomic analysis identifies NDRG2 as a candidate tumor suppressor gene frequently inactivated in clinically aggressive meningioma. Cancer Res. 2005;65:7121–7126. doi: 10.1158/0008-5472.CAN-05-0043. [DOI] [PubMed] [Google Scholar]
- 15.Ling Z.Q., Ge M.H., Lu X.X., Han J., Wu Y.C., Liu X., Zhu X., Hong L.L. Ndrg2 promoter hypermethylation triggered by helicobacter pylori infection correlates with poor patients survival in human gastric carcinoma. Oncotarget. 2015;6:8210–8225. doi: 10.18632/oncotarget.3601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeschke J., Van Neste L., Glockner S.C., Dhir M., Calmon M.F., Deregowski V., Van Criekinge W., Vlassenbroeck I., Koch A., Chan T.A., et al. Biomarkers for detection and prognosis of breast cancer identified by a functional hypermethylome screen. Epigenetics. 2012;7:701–709. doi: 10.4161/epi.20445. [DOI] [PubMed] [Google Scholar]
- 17.Godeke J., Luxenburger E., Trippel F., Becker K., Haberle B., Muller-Hocker J., von Schweinitz D., Kappler R. Low expression of N-myc downstream-regulated gene 2 (NDRG2) correlates with poor prognosis in hepatoblastoma. Hepatol. Int. 2016;10:370–376. doi: 10.1007/s12072-015-9686-1. [DOI] [PubMed] [Google Scholar]
- 18.Tepel M., Roerig P., Wolter M., Gutmann D.H., Perry A., Reifenberger G., Riemenschneider M.J. Frequent promoter hypermethylation and transcriptional downregulation of the NDRG2 gene at 14q11.2 in primary glioblastoma. Int. J. Cancer. 2008;123:2080–2086. doi: 10.1002/ijc.23705. [DOI] [PubMed] [Google Scholar]
- 19.Skiriute D., Steponaitis G., Vaitkiene P., Mikuciunas M., Skauminas K., Tamasauskas A., Kazlauskas A. Glioma Malignancy-Dependent NDRG2 Gene Methylation and Downregulation Correlates with Poor Patient Outcome. J. Cancer. 2014;5:446–456. doi: 10.7150/jca.9140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang J., Xie C., Pan S., Liang Y., Han J., Lan Y., Sun J., Li K., Sun B., Yang G., et al. N-myc downstream-regulated gene 2 inhibits human cholangiocarcinoma progression and is regulated by leukemia inhibitory factor/MicroRNA-181c negative feedback pathway. Hepatology. 2016;64:1606–1622. doi: 10.1002/hep.28781. [DOI] [PubMed] [Google Scholar]
- 21.Fu Q., Gao Y., Yang F., Mao T., Sun Z., Wang H., Song B., Li X. Suppression of microRNA-454 impedes the proliferation and invasion of prostate cancer cells by promoting N-myc downstream-regulated gene 2 and inhibiting WNT/beta-catenin signaling. Biomed. Pharmacother. 2018;97:120–127. doi: 10.1016/j.biopha.2017.10.115. [DOI] [PubMed] [Google Scholar]
- 22.Sun X., Li K., Wang H., Xia Y., Meng P., Leng X. MiR-483 Promotes Colorectal Cancer Cell Biological Progression by Directly Targeting NDRG2 through Regulation of the PI3K/AKT Signaling Pathway and Epithelial-to-Mesenchymal Transition. J. Healthc. Eng. 2022;2022:4574027. doi: 10.1155/2022/4574027. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Feng L., Xie Y., Zhang H., Wu Y. Down-regulation of NDRG2 gene expression in human colorectal cancer involves promoter methylation and microRNA-650. Biochem. Biophys. Res. Commun. 2011;406:534–538. doi: 10.1016/j.bbrc.2011.02.081. [DOI] [PubMed] [Google Scholar]
- 24.Li L., Wang J., Shen X., Wang L., Li X., Liu Y., Shi M., Zhao G., Deng Y. Expression and prognostic value of NDRG2 in human astrocytomas. J. Neurol. Sci. 2011;308:77–82. doi: 10.1016/j.jns.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Goudarzi P.K., Mehrabi F., Khoshnood R.J., Bagheri A.B., Ahmadi K., Yahaghi E., Abdolhoseinpour H. Expression and prognostic value of the aldehyde dehydrogenase 1 (ALDH1) and N-myc downstream regulated gene 2 (NDRG2) as potential markers in human astrocytomas. Tumour Biol. 2016;37:6261–6265. doi: 10.1007/s13277-015-4491-y. [DOI] [PubMed] [Google Scholar]
- 26.Li R., Yu C., Jiang F., Gao L., Li J., Wang Y., Beckwith N., Yao L., Zhang J., Wu G. Overexpression of N-Myc downstream-regulated gene 2 (NDRG2) regulates the proliferation and invasion of bladder cancer cells in vitro and in vivo. PLoS ONE. 2013;8:e76689. doi: 10.1371/journal.pone.0076689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kloten V., Schlensog M., Eschenbruch J., Gasthaus J., Tiedemann J., Mijnes J., Heide T., Braunschweig T., Knuchel R., Dahl E. Abundant NDRG2 Expression Is Associated with Aggressiveness and Unfavorable Patients’ Outcome in Basal-Like Breast Cancer. PLoS ONE. 2016;11:e0159073. doi: 10.1371/journal.pone.0159073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh S.S., Kim D., Kim D.H., Chang H.H., Sohn K.C., Kim K.H., Jung S.H., Lee B.K., Kim J.H., Kim K.D. NDRG2 correlated with favorable recurrence-free survival inhibits metastasis of mouse breast cancer cells via attenuation of active TGF-beta production. Carcinogenesis. 2012;33:1882–1888. doi: 10.1093/carcin/bgs211. [DOI] [PubMed] [Google Scholar]
- 29.Hong S.N., Kim S.J., Kim E.R., Chang D.K., Kim Y.H. Epigenetic silencing of NDRG2 promotes colorectal cancer proliferation and invasion. J. Gastroenterol. Hepatol. 2016;31:164–171. doi: 10.1111/jgh.13068. [DOI] [PubMed] [Google Scholar]
- 30.Chen W., Peng J., Ou Q., Wen Y., Jiang W., Deng Y., Zhao Y., Wan D., Pan Z., Fang Y. Expression of NDRG2 in Human Colorectal Cancer and its Association with Prognosis. J. Cancer. 2019;10:3373–3380. doi: 10.7150/jca.31382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lorentzen A., Vogel L.K., Lewinsky R.H., Saebo M., Skjelbred C.F., Godiksen S., Hoff G., Tveit K.M., Lothe I.M., Ikdahl T., et al. Expression of NDRG2 is down-regulated in high-risk adenomas and colorectal carcinoma. BMC Cancer. 2007;7:192. doi: 10.1186/1471-2407-7-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi H., Li N., Li S., Chen C., Wang W., Xu C., Zhang J., Jin H., Zhang H., Zhao H., et al. Expression of NDRG2 in esophageal squamous cell carcinoma. Cancer Sci. 2010;101:1292–1299. doi: 10.1111/j.1349-7006.2010.01529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cao W., Yu G., Lu Q., Zhang J. Low expression of N-myc downstream-regulated gene 2 in oesophageal squamous cell carcinoma correlates with a poor prognosis. BMC Cancer. 2013;13:305. doi: 10.1186/1471-2407-13-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang C.L., Zheng X.L., Ye K., Ge H., Sun Y.N., Lu Y.F., Fan Q.X. NDRG2 suppresses proliferation, migration, invasion and epithelial-mesenchymal transition of esophageal cancer cells through regulating the AKT/XIAP signaling pathway. Int. J. Biochem. Cell. Biol. 2018;99:43–51. doi: 10.1016/j.biocel.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 35.Lee D.G., Lee S.H., Kim J.S., Park J., Cho Y.L., Kim K.S., Jo D.Y., Song I.C., Kim N., Yun H.J., et al. Loss of NDRG2 promotes epithelial-mesenchymal transition of gallbladder carcinoma cells through MMP-19-mediated Slug expression. J. Hepatol. 2015;63:1429–1439. doi: 10.1016/j.jhep.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Song S.P., Zhang S.B., Liu R., Yao L., Hao Y.Q., Liao M.M., Zhang Y.D., Li Z.H. NDRG2 down-regulation and CD24 up-regulation promote tumor aggravation and poor survival in patients with gallbladder carcinoma. Med. Oncol. 2012;29:1879–1885. doi: 10.1007/s12032-011-0110-y. [DOI] [PubMed] [Google Scholar]
- 37.Chang X., Li Z., Ma J., Deng P., Zhang S., Zhi Y., Chen J., Dai D. DNA methylation of NDRG2 in gastric cancer and its clinical significance. Dig. Dis. Sci. 2013;58:715–723. doi: 10.1007/s10620-012-2393-z. [DOI] [PubMed] [Google Scholar]
- 38.Choi S.C., Yoon S.R., Park Y.P., Song E.Y., Kim J.W., Kim W.H., Yang Y., Lim J.S., Lee H.G. Expression of NDRG2 is related to tumor progression and survival of gastric cancer patients through Fas-mediated cell death. Exp. Mol. Med. 2007;39:705–714. doi: 10.1038/emm.2007.77. [DOI] [PubMed] [Google Scholar]
- 39.Deng Y., Yao L., Chau L., Ng S.S., Peng Y., Liu X., Au W.S., Wang J., Li F., Ji S., et al. N-Myc downstream-regulated gene 2 (NDRG2) inhibits glioblastoma cell proliferation. Int. J. Cancer. 2003;106:342–347. doi: 10.1002/ijc.11228. [DOI] [PubMed] [Google Scholar]
- 40.Li W., Chu D., Chu X., Meng F., Wei D., Li H., Sun B. Decreased expression of NDRG2 is related to poor overall survival in patients with glioma. J. Clin. Neurosci. 2011;18:1534–1537. doi: 10.1016/j.jocn.2010.12.032. [DOI] [PubMed] [Google Scholar]
- 41.Lee D.C., Kang Y.K., Kim W.H., Jang Y.J., Kim D.J., Park I.Y., Sohn B.H., Sohn H.A., Lee H.G., Lim J.S., et al. Functional and clinical evidence for NDRG2 as a candidate suppressor of liver cancer metastasis. Cancer Res. 2008;68:4210–4220. doi: 10.1158/0008-5472.CAN-07-5040. [DOI] [PubMed] [Google Scholar]
- 42.Zheng J., Li Y., Yang J., Liu Q., Shi M., Zhang R., Shi H., Ren Q., Ma J., Guo H., et al. NDRG2 inhibits hepatocellular carcinoma adhesion, migration and invasion by regulating CD24 expression. BMC Cancer. 2011;11:251. doi: 10.1186/1471-2407-11-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang H., Wang W., Wang X., Cai K., Wu H., Ju Q., Huang Z., Gao X. Reduced N-Myc downstream-regulated gene 2 expression is associated with CD24 upregulation and poor prognosis in patients with lung adenocarcinoma. Med. Oncol. 2012;29:3162–3168. doi: 10.1007/s12032-012-0231-y. [DOI] [PubMed] [Google Scholar]
- 44.Liang Z.L., Kang K., Yoon S., Huang S.M., Lim J.S., Kim J.M., Lim J.S., Lee H.J. NDRG2 is involved in the oncogenic properties of renal cell carcinoma and its loss is a novel independent poor prognostic factor after nephrectomy. Ann. Surg. Oncol. 2012;19:2763–2772. doi: 10.1245/s10434-011-2204-3. [DOI] [PubMed] [Google Scholar]
- 45.Ma J.J., Kong L.M., Liao C.G., Jiang X., Wang Y., Bao T.Y. Suppression of MMP-9 activity by NDRG2 expression inhibits clear cell renal cell carcinoma invasion. Med. Oncol. 2012;29:3306–3313. doi: 10.1007/s12032-012-0265-1. [DOI] [PubMed] [Google Scholar]
- 46.Langley R.R., Fidler I.J. The seed and soil hypothesis revisited--the role of tumor-stroma interactions in metastasis to different organs. Int. J. Cancer. 2011;128:2527–2535. doi: 10.1002/ijc.26031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sleeman J.P., Nazarenko I., Thiele W. Do all roads lead to Rome? Routes to metastasis development. Int. J. Cancer. 2011;128:2511–2526. doi: 10.1002/ijc.26027. [DOI] [PubMed] [Google Scholar]
- 48.Muller A., Homey B., Soto H., Ge N., Catron D., Buchanan M.E., McClanahan T., Murphy E., Yuan W., Wagner S.N., et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 49.Ding Y., Du Y. Clinicopathological significance and prognostic role of chemokine receptor CXCR4 expression in pancreatic ductal adenocarcinoma, a meta-analysis and literature review. Int. J. Surg. 2019;65:32–38. doi: 10.1016/j.ijsu.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Lambert A.W., Pattabiraman D.R., Weinberg R.A. Emerging Biological Principles of Metastasis. Cell. 2017;168:670–691. doi: 10.1016/j.cell.2016.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Majidpoor J., Mortezaee K. Steps in metastasis: An updated review. Med. Oncol. 2021;38:3. doi: 10.1007/s12032-020-01447-w. [DOI] [PubMed] [Google Scholar]
- 52.Pastushenko I., Blanpain C. EMT Transition States during Tumor Progression and Metastasis. Trends Cell. Biol. 2019;29:212–226. doi: 10.1016/j.tcb.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 53.De Craene B., Berx G. Regulatory networks defining EMT during cancer initiation and progression. Nat. Rev. Cancer. 2013;13:97–110. doi: 10.1038/nrc3447. [DOI] [PubMed] [Google Scholar]
- 54.Xu Z., Shen M.X., Ma D.Z., Wang L.Y., Zha X.L. TGF-beta1-promoted epithelial-to-mesenchymal transformation and cell adhesion contribute to TGF-beta1-enhanced cell migration in SMMC-7721 cells. Cell. Res. 2003;13:343–350. doi: 10.1038/sj.cr.7290179. [DOI] [PubMed] [Google Scholar]
- 55.Dong R., Wang Q., He X.L., Chu Y.K., Lu J.G., Ma Q.J. Role of nuclear factor kappa B and reactive oxygen species in the tumor necrosis factor-alpha-induced epithelial-mesenchymal transition of MCF-7 cells. Braz. J. Med. Biol. Res. 2007;40:1071–1078. doi: 10.1590/S0100-879X2007000800007. [DOI] [PubMed] [Google Scholar]
- 56.Matsuoka J., Yashiro M., Doi Y., Fuyuhiro Y., Kato Y., Shinto O., Noda S., Kashiwagi S., Aomatsu N., Hirakawa T., et al. Hypoxia stimulates the EMT of gastric cancer cells through autocrine TGFbeta signaling. PLoS ONE. 2013;8:e62310. doi: 10.1371/journal.pone.0062310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim R., Arihiro K., Emi M., Tanabe K., Osaki A. Potential role of HER-2; in primary breast tumor with bone metastasis. Oncol. Rep. 2006;15:1477–1484. doi: 10.3892/or.15.6.1477. [DOI] [PubMed] [Google Scholar]
- 58.Helbig G., Christopherson K.W., 2nd, Bhat-Nakshatri P., Kumar S., Kishimoto H., Miller K.D., Broxmeyer H.E., Nakshatri H. NF-kappaB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J. Biol. Chem. 2003;278:21631–21638. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- 59.Cheng G.Z., Zhang W.Z., Sun M., Wang Q., Coppola D., Mansour M., Xu L.M., Costanzo C., Cheng J.Q., Wang L.H. Twist is transcriptionally induced by activation of STAT3 and mediates STAT3 oncogenic function. J. Biol. Chem. 2008;283:14665–14673. doi: 10.1074/jbc.M707429200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gerratana L., Fanotto V., Bonotto M., Bolzonello S., Minisini A.M., Fasola G., Puglisi F. Pattern of metastasis and outcome in patients with breast cancer. Clin. Exp. Metastasis. 2015;32:125–133. doi: 10.1007/s10585-015-9697-2. [DOI] [PubMed] [Google Scholar]
- 61.Sternberg C.N., Baskin-Bey E.S., Watson M., Worsfold A., Rider A., Tombal B. Treatment patterns and characteristics of European patients with castration-resistant prostate cancer. BMC Urol. 2013;13:58. doi: 10.1186/1471-2490-13-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Coleman R.E. Metastatic bone disease: Clinical features, pathophysiology and treatment strategies. Cancer Treat. Rev. 2001;27:165–176. doi: 10.1053/ctrv.2000.0210. [DOI] [PubMed] [Google Scholar]
- 63.Wang J., Loberg R., Taichman R.S. The pivotal role of CXCL12 (SDF-1)/CXCR4 axis in bone metastasis. Cancer Metastasis Rev. 2006;25:573–587. doi: 10.1007/s10555-006-9019-x. [DOI] [PubMed] [Google Scholar]
- 64.Cabioglu N., Summy J., Miller C., Parikh N.U., Sahin A.A., Tuzlali S., Pumiglia K., Gallick G.E., Price J.E. CXCL-12/stromal cell-derived factor-1alpha transactivates HER2-neu in breast cancer cells by a novel pathway involving Src kinase activation. Cancer Res. 2005;65:6493–6497. doi: 10.1158/0008-5472.CAN-04-1303. [DOI] [PubMed] [Google Scholar]
- 65.Mimeault M., Batra S.K. Hypoxia-inducing factors as master regulators of stemness properties and altered metabolism of cancer- and metastasis-initiating cells. J. Cell. Mol. Med. 2013;17:30–54. doi: 10.1111/jcmm.12004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Conley-LaComb M.K., Saliganan A., Kandagatla P., Chen Y.Q., Cher M.L., Chinni S.R. PTEN loss mediated Akt activation promotes prostate tumor growth and metastasis via CXCL12/CXCR4 signaling. Mol. Cancer. 2013;12:85. doi: 10.1186/1476-4598-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nakahata S., Ichikawa T., Maneesaay P., Saito Y., Nagai K., Tamura T., Manachai N., Yamakawa N., Hamasaki M., Kitabayashi I., et al. Loss of NDRG2 expression activates PI3K-AKT signalling via PTEN phosphorylation in ATLL and other cancers. Nat. Commun. 2014;5:3393. doi: 10.1038/ncomms4393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yang Z., Li C., Wang X., Zhai C., Yi Z., Wang L., Liu B., Du B., Wu H., Guo X., et al. Dauricine induces apoptosis, inhibits proliferation and invasion through inhibiting NF-kappaB signaling pathway in colon cancer cells. J. Cell. Physiol. 2010;225:266–275. doi: 10.1002/jcp.22261. [DOI] [PubMed] [Google Scholar]
- 69.Pikarsky E., Porat R.M., Stein I., Abramovitch R., Amit S., Kasem S., Gutkovich-Pyest E., Urieli-Shoval S., Galun E., Ben-Neriah Y. NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature. 2004;431:461–466. doi: 10.1038/nature02924. [DOI] [PubMed] [Google Scholar]
- 70.Sasaki N., Morisaki T., Hashizume K., Yao T., Tsuneyoshi M., Noshiro H., Nakamura K., Yamanaka T., Uchiyama A., Tanaka M., et al. Nuclear factor-kappaB p65 (RelA) transcription factor is constitutively activated in human gastric carcinoma tissue. Clin. Cancer Res. 2001;7:4136–4142. [PubMed] [Google Scholar]
- 71.Park B.K., Zhang H., Zeng Q., Dai J., Keller E.T., Giordano T., Gu K., Shah V., Pei L., Zarbo R.J., et al. NF-kappaB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat. Med. 2007;13:62–69. doi: 10.1038/nm1519. [DOI] [PubMed] [Google Scholar]
- 72.Tamura T., Ichikawa T., Nakahata S., Kondo Y., Tagawa Y., Yamamoto K., Nagai K., Baba T., Yamaguchi R., Futakuchi M., et al. Loss of NDRG2 Expression Confers Oral Squamous Cell Carcinoma with Enhanced Metastatic Potential. Cancer Res. 2017;77:2363–2374. doi: 10.1158/0008-5472.CAN-16-2114. [DOI] [PubMed] [Google Scholar]
- 73.Kim M.J., Kim H.S., Lee S.H., Yang Y., Lee M.S., Lim J.S. NDRG2 controls COX-2/PGE(2)-mediated breast cancer cell migration and invasion. Mol. Cells. 2014;37:759–765. doi: 10.14348/molcells.2014.0232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim A., Kim M.J., Yang Y., Kim J.W., Yeom Y.I., Lim J.S. Suppression of NF-kappaB activity by NDRG2 expression attenuates the invasive potential of highly malignant tumor cells. Carcinogenesis. 2009;30:927–936. doi: 10.1093/carcin/bgp072. [DOI] [PubMed] [Google Scholar]
- 75.Ichikawa T., Nakahata S., Fujii M., Iha H., Morishita K. Loss of NDRG2 enhanced activation of the NF-kappaB pathway by PTEN and NIK phosphorylation for ATL and other cancer development. Sci. Rep. 2015;5:12841. doi: 10.1038/srep12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ozes O.N., Mayo L.D., Gustin J.A., Pfeffer S.R., Pfeffer L.M., Donner D.B. NF-kappaB activation by tumour necrosis factor requires the Akt serine-threonine kinase. Nature. 1999;401:82–85. doi: 10.1038/43466. [DOI] [PubMed] [Google Scholar]
- 77.Romashkova J.A., Makarov S.S. NF-kappaB is a target of AKT in anti-apoptotic PDGF signalling. Nature. 1999;401:86–90. doi: 10.1038/43474. [DOI] [PubMed] [Google Scholar]
- 78.Sun S.C. The noncanonical NF-kappaB pathway. Immunol. Rev. 2012;246:125–140. doi: 10.1111/j.1600-065X.2011.01088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ling L., Cao Z., Goeddel D.V. NF-kappaB-inducing kinase activates IKK-alpha by phosphorylation of Ser-176. Proc. Natl. Acad. Sci. USA. 1998;95:3792–3797. doi: 10.1073/pnas.95.7.3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xiao G., Fong A., Sun S.C. Induction of p100 processing by NF-kappaB-inducing kinase involves docking IkappaB kinase alpha (IKKalpha) to p100 and IKKalpha-mediated phosphorylation. J. Biol. Chem. 2004;279:30099–30105. doi: 10.1074/jbc.M401428200. [DOI] [PubMed] [Google Scholar]
- 81.Murray P.J. The JAK-STAT signaling pathway: Input and output integration. J. Immunol. 2007;178:2623–2629. doi: 10.4049/jimmunol.178.5.2623. [DOI] [PubMed] [Google Scholar]
- 82.Woss K., Simonovic N., Strobl B., Macho-Maschler S., Muller M. TYK2: An Upstream Kinase of STATs in Cancer. Cancers. 2019;11:1728. doi: 10.3390/cancers11111728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bean J., Brennan C., Shih J.Y., Riely G., Viale A., Wang L., Chitale D., Motoi N., Szoke J., Broderick S., et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc. Natl. Acad. Sci. USA. 2007;104:20932–20937. doi: 10.1073/pnas.0710370104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim D.Y., Cha S.T., Ahn D.H., Kang H.Y., Kwon C.I., Ko K.H., Hwang S.G., Park P.W., Rim K.S., Hong S.P. STAT3 expression in gastric cancer indicates a poor prognosis. J. Gastroenterol. Hepatol. 2009;24:646–651. doi: 10.1111/j.1440-1746.2008.05671.x. [DOI] [PubMed] [Google Scholar]
- 85.Masuda M., Suzui M., Yasumatu R., Nakashima T., Kuratomi Y., Azuma K., Tomita K., Komiyama S., Weinstein I.B. Constitutive activation of signal transducers and activators of transcription 3 correlates with cyclin D1 overexpression and may provide a novel prognostic marker in head and neck squamous cell carcinoma. Cancer Res. 2002;62:3351–3355. [PubMed] [Google Scholar]
- 86.Jianwei Z., Qi L., Quanquan X., Tianen W., Qingwei W. TMPRSS4 Upregulates TWIST1 Expression through STAT3 Activation to Induce Prostate Cancer Cell Migration. Pathol. Oncol. Res. 2018;24:251–257. doi: 10.1007/s12253-017-0237-z. [DOI] [PubMed] [Google Scholar]
- 87.Dauer D.J., Ferraro B., Song L., Yu B., Mora L., Buettner R., Enkemann S., Jove R., Haura E.B. Stat3 regulates genes common to both wound healing and cancer. Oncogene. 2005;24:3397–3408. doi: 10.1038/sj.onc.1208469. [DOI] [PubMed] [Google Scholar]
- 88.Kong L.Y., Abou-Ghazal M.K., Wei J., Chakraborty A., Sun W., Qiao W., Fuller G.N., Fokt I., Grimm E.A., Schmittling R.J., et al. A novel inhibitor of signal transducers and activators of transcription 3 activation is efficacious against established central nervous system melanoma and inhibits regulatory T cells. Clin. Cancer Res. 2008;14:5759–5768. doi: 10.1158/1078-0432.CCR-08-0377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xiong H., Hong J., Du W., Lin Y.W., Ren L.L., Wang Y.C., Su W.Y., Wang J.L., Cui Y., Wang Z.H., et al. Roles of STAT3 and ZEB1 proteins in E-cadherin down-regulation and human colorectal cancer epithelial-mesenchymal transition. J. Biol. Chem. 2012;287:5819–5832. doi: 10.1074/jbc.M111.295964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vesuna F., van Diest P., Chen J.H., Raman V. Twist is a transcriptional repressor of E-cadherin gene expression in breast cancer. Biochem. Biophys. Res. Commun. 2008;367:235–241. doi: 10.1016/j.bbrc.2007.11.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Niu G., Wright K.L., Huang M., Song L., Haura E., Turkson J., Zhang S., Wang T., Sinibaldi D., Coppola D., et al. Constitutive Stat3 activity up-regulates VEGF expression and tumor angiogenesis. Oncogene. 2002;21:2000–2008. doi: 10.1038/sj.onc.1205260. [DOI] [PubMed] [Google Scholar]
- 92.Wei D., Le X., Zheng L., Wang L., Frey J.A., Gao A.C., Peng Z., Huang S., Xiong H.Q., Abbruzzese J.L., et al. Stat3 activation regulates the expression of vascular endothelial growth factor and human pancreatic cancer angiogenesis and metastasis. Oncogene. 2003;22:319–329. doi: 10.1038/sj.onc.1206122. [DOI] [PubMed] [Google Scholar]
- 93.Wu M., Song D., Li H., Yang Y., Ma X., Deng S., Ren C., Shu X. Negative regulators of STAT3 signaling pathway in cancers. Cancer Manag. Res. 2019;11:4957–4969. doi: 10.2147/CMAR.S206175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zou S., Tong Q., Liu B., Huang W., Tian Y., Fu X. Targeting STAT3 in Cancer Immunotherapy. Mol. Cancer. 2020;19:145. doi: 10.1186/s12943-020-01258-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Croker B.A., Kiu H., Nicholson S.E. SOCS regulation of the JAK/STAT signalling pathway. Semin. Cell. Dev. Biol. 2008;19:414–422. doi: 10.1016/j.semcdb.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lee E.B., Kim A., Kang K., Kim H., Lim J.S. NDRG2-mediated Modulation of SOCS3 and STAT3 Activity Inhibits IL-10 Production. Immune Netw. 2010;10:219–229. doi: 10.4110/in.2010.10.6.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kim M.J., Lim J., Yang Y., Lee M.S., Lim J.S. N-myc downstream-regulated gene 2 (NDRG2) suppresses the epithelial-mesenchymal transition (EMT) in breast cancer cells via STAT3/Snail signaling. Cancer Lett. 2014;354:33–42. doi: 10.1016/j.canlet.2014.06.023. [DOI] [PubMed] [Google Scholar]
- 98.Wang Y., Zhang C.Y., Xia R.H., Han J., Sun B., Sun S.Y., Li J. The MYB/miR-130a/NDRG2 axis modulates tumor proliferation and metastatic potential in salivary adenoid cystic carcinoma. Cell. Death Dis. 2018;9:917. doi: 10.1038/s41419-018-0966-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Peinado H., Quintanilla M., Cano A. Transforming growth factor beta-1 induces snail transcription factor in epithelial cell lines: Mechanisms for epithelial mesenchymal transitions. J. Biol. Chem. 2003;278:21113–21123. doi: 10.1074/jbc.M211304200. [DOI] [PubMed] [Google Scholar]
- 100.Lamouille S., Xu J., Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat. Rev. Mol. Cell. Biol. 2014;15:178–196. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Feng X.H., Derynck R. Specificity and versatility in tgf-beta signaling through Smads. Annu. Rev. Cell. Dev. Biol. 2005;21:659–693. doi: 10.1146/annurev.cellbio.21.022404.142018. [DOI] [PubMed] [Google Scholar]
- 102.Padua D., Massague J. Roles of TGFbeta in metastasis. Cell. Res. 2009;19:89–102. doi: 10.1038/cr.2008.316. [DOI] [PubMed] [Google Scholar]
- 103.Prontera C., Mariani B., Rossi C., Poggi A., Rotilio D. Inhibition of gelatinase A (MMP-2) by batimastat and captopril reduces tumor growth and lung metastases in mice bearing Lewis lung carcinoma. Int. J. Cancer. 1999;81:761–766. doi: 10.1002/(SICI)1097-0215(19990531)81:5<761::AID-IJC16>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 104.Stetler-Stevenson W.G. Matrix metalloproteinases in angiogenesis: A moving target for therapeutic intervention. J. Clin. Investig. 1999;103:1237–1241. doi: 10.1172/JCI6870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Giannelli G., Falk-Marzillier J., Schiraldi O., Stetler-Stevenson W.G., Quaranta V. Induction of cell migration by matrix metalloprotease-2 cleavage of laminin-5. Science. 1997;277:225–228. doi: 10.1126/science.277.5323.225. [DOI] [PubMed] [Google Scholar]
- 106.Munger J.S., Huang X., Kawakatsu H., Griffiths M.J., Dalton S.L., Wu J., Pittet J.F., Kaminski N., Garat C., Matthay M.A., et al. The integrin alpha v beta 6 binds and activates latent TGF beta 1: A mechanism for regulating pulmonary inflammation and fibrosis. Cell. 1999;96:319–328. doi: 10.1016/S0092-8674(00)80545-0. [DOI] [PubMed] [Google Scholar]
- 107.Dong J., Peng J., Zhang H., Mondesire W.H., Jian W., Mills G.B., Hung M.C., Meric-Bernstam F. Role of glycogen synthase kinase 3beta in rapamycin-mediated cell cycle regulation and chemosensitivity. Cancer Res. 2005;65:1961–1972. doi: 10.1158/0008-5472.CAN-04-2501. [DOI] [PubMed] [Google Scholar]
- 108.Wang Y., Lam J.B., Lam K.S., Liu J., Lam M.C., Hoo R.L., Wu D., Cooper G.J., Xu A. Adiponectin modulates the glycogen synthase kinase-3beta/beta-catenin signaling pathway and attenuates mammary tumorigenesis of MDA-MB-231 cells in nude mice. Cancer Res. 2006;66:11462–11470. doi: 10.1158/0008-5472.CAN-06-1969. [DOI] [PubMed] [Google Scholar]
- 109.Liu C., Li Y., Semenov M., Han C., Baeg G.H., Tan Y., Zhang Z., Lin X., He X. Control of beta-catenin phosphorylation/degradation by a dual-kinase mechanism. Cell. 2002;108:837–847. doi: 10.1016/S0092-8674(02)00685-2. [DOI] [PubMed] [Google Scholar]
- 110.Webster M.T., Rozycka M., Sara E., Davis E., Smalley M., Young N., Dale T.C., Wooster R. Sequence variants of the axin gene in breast, colon, and other cancers: An analysis of mutations that interfere with GSK3 binding. Genes Chromosomes Cancer. 2000;28:443–453. doi: 10.1002/1098-2264(200008)28:4<443::AID-GCC10>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 111.Zhou B.P., Deng J., Xia W., Xu J., Li Y.M., Gunduz M., Hung M.C. Dual regulation of Snail by GSK-3beta-mediated phosphorylation in control of epithelial-mesenchymal transition. Nat. Cell. Biol. 2004;6:931–940. doi: 10.1038/ncb1173. [DOI] [PubMed] [Google Scholar]
- 112.El Touny L.H., Banerjee P.P. Akt GSK-3 pathway as a target in genistein-induced inhibition of TRAMP prostate cancer progression toward a poorly differentiated phenotype. Carcinogenesis. 2007;28:1710–1717. doi: 10.1093/carcin/bgm103. [DOI] [PubMed] [Google Scholar]
- 113.Maehama T., Dixon J.E. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J. Biol. Chem. 1998;273:13375–13378. doi: 10.1074/jbc.273.22.13375. [DOI] [PubMed] [Google Scholar]
- 114.Park S., Han H.T., Oh S.S., Kim D.H., Jeong J.W., Lee K.W., Kim M., Lim J.S., Cho Y.Y., Hwangbo C., et al. NDRG2 Sensitizes Myeloid Leukemia to Arsenic Trioxide via GSK3beta-NDRG2-PP2A Complex Formation. Cells. 2019;8:495. doi: 10.3390/cells8050495. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.