Abstract
Background: Studies have demonstrated the link between vitamin-D-related genetic variations and nonskeletal outcomes. We aimed to identify all available data on the association of vitamin-D-related genetic variations with nonalcoholic fatty liver disease (NAFLD). Methods: Potentially eligible studies were identified from Embase and Medline databases from inception to June 2022 using a search strategy that comprised terms for “Vitamin D” and “NAFLD”. Eligible studies must report the association between vitamin D-related genetic variations and presence, severity or response to treatment of NAFLD. Data were extracted from each eligible study. Results: A total of 3495 articles were identified. After a systematic review, twelve studies were included. A total of 26 genetic variations were identified. Presence of NAFLD was associated with variations of GC (rs222054, rs222020, rs10011000, rs7041), VDR (rs2228570, rs11168287, rs10783219, rs4752), CYP24A1 (rs3787557, rs6068816, rs2296241, rs2248359) and CYP27B1 (rs4646536). Severity of NAFLD was associated with variations of GC (rs4588), VDR (rs2228570, rs4334089), CYP2R1 (rs10741657), DHCR7 (rs1544410, rs3829251, rs12785878) and CYP24A1 (rs3787557, rs6068816, rs6097809, rs6127119, rs2248359, rs3787554, rs4809960, rs6022999). Response to calcitriol treatment was associated with variation of VDR (rs10735810). Conclusions: Multiple vitamin D-related genetic variations were associated with NAFLD, indicating the role of vitamin D in the pathogenesis of NAFLD.
Keywords: nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, vitamin D, VDR, CYP27B1, CYP2R1, CYP24A1, GC, DHCR7, genetic variation, polymorphism, systematic review
1. Introduction
Nonalcoholic fatty liver disease (NAFLD) is defined by hepatic fat accumulation in the absence of any secondary causes such as excessive alcohol consumption and hepatic viral diseases [1]. It is a spectrum of diseases that range from fatty acid accumulation in the liver, inflammation of the liver causing nonalcoholic steatohepatitis (NASH), advanced fibrosis, cirrhosis and hepatocellular carcinoma. NAFLD is the most common chronic liver disease in the world and soon to be the most common indication for liver transplantation [1,2]. Previous studies reported a global prevalence of NAFLD as high as one billion individuals, and 25% of these patients progress to NASH [3,4]. NAFLD is known to be a common comorbidity in obesity and metabolic syndrome given its reported prevalence of 65–85% among patients with obesity [5].
Vitamin D is a steroid hormone responsible for regulating calcium and phosphate metabolism. It is also known to exert multitudes of nonskeletal effects given that vitamin D receptor (VDR) is expressed in various types of tissues and cells, including the skin, skeletal muscle, adipose tissue, endocrine pancreas and immune cells, among others [6,7]. Humans get vitamin D from diets (vitamin D2 from yeast and mushrooms and vitamin D3 from animal products) and endogenous synthesis in the skin (vitamin D3 from 7-dehydrocholesterol exposure to UVB). Once entering the circulation, vitamin D (D2 and D3) gets converted into 25-hydroxyvitamin D [25(OH)D], the major circulating form of vitamin D, by the hepatic enzyme 25-hydroxylase. Then, 25(OH)D gets metabolized by the enzyme 25-hydroxyvitamin D-1α-hydroxylase in the kidney into the active form 1,25(OH)2D, which interacts with the intracellular VDR in the target tissues. The 1,25(OH)2D-activated VDR then interacts with the retinoid X receptor (RXR), which selectively recognizes the vitamin D-responsive elements in the promotor sites of the target genes resulting in changes in gene expression [8]. 1,25(OH)2D and 25(OH)D both get catabolized by the enzyme 24-hydroxylase expressed in multiple tissues into inactive carboxylic acids, which are then excreted via the biliary system [6,7].
Genes associated with vitamin D metabolism include (1) DHCR7, encoding 7-dehydrocholesterol reductase, which metabolizes 7-dehydrocholesterol, a substrate of vitamin D [9]; (2) genes encoding the enzyme 25-hydroxylase, which converts vitamin D into the circulating form 25(OH)D, including CYP2R1 (encoding the cytochrome P450 family 2 subfamily R member 1), CYP2J2 (encoding the cytochrome P450 family 2 subfamily J polypeptide 2, known to hydroxylate vitamin D2 better than vitamin D3 [10]), CYP27A1 (encoding the cytochrome P450 family 27 subfamily A member 1) and CYP3A4 (encoding the cytochrome P450 family 3 subfamily A member 4), which converts vitamin D into the circulating form 25(OH)D [11]; (3) CYP27B1, encoding the chrome P450 family 27 subfamily B member 1, or the enzyme 25-hydroxyvitamin D-1α-hydroxylase, which converts 25(OH)D into the active form 1,25(OH)2D; (4) GC, encoding the GC vitamin D-binding protein; (5) VDR, encoding the vitamin D receptor; and (6) CYP24A1, encoding the cytochrome P450 family 24 subfamily A member 1, or the enzyme 24-hydroxylase, which catabolizes 25(OH)D and 1,25(OH)2D into inactive carboxylic acids [9].
Vitamin D deficiency, indicated by low level of serum 25(OH)D of less than 20 ng/mL [12,13] has been shown to be associated with multiple chronic diseases, including cardiovascular disease, diabetes, autoimmune diseases and cancers [6,7,14]. Low level of 25(OH)D is also found to be associated with presence and severity of NAFLD in multiple studies [15,16]. Several underlying mechanisms of the association have been proposed. These include the observation that vitamin D plays a role in modulating the immune system and improving insulin sensitivity [17,18]. However, the causality of this association is still unclarified given that there is limited evidence from clinical trials on the impact of vitamin D supplementation on NAFLD prevention and treatment [19].
Interestingly, variations of genes involved in the vitamin D metabolism pathway described above have been shown to be associated with many conditions, such as coronary artery disease, osteoporosis, diabetes and autoimmune diseases, indicating the interaction between this pathway and health outcomes [20,21,22,23]. Additionally, a number of studies have reported the association between vitamin D-related genetic variations and NAFLD [24,25,26,27,28,29,30,31,32,33,34,35]. The objective of this systematic review was therefore to identify and summarize the results of all available studies that explored the association of vitamin D-related genetic polymorphisms with presence, severity and response to treatment of NAFLD.
2. Methods
2.1. Search Strategy
Two investigators (A.J., N.C.) independently searched records indexed in Embase and Medline from inception to June 2022. The search strategy included terms related to nonalcoholic fatty liver disease, vitamin D and genes involved in the vitamin D metabolic pathway, as shown in Supplemental Material S1. The PRISMA guideline for systematic review was followed, as indicated in Supplemental Material S2. No language restriction was applied.
2.2. Eligibility Criteria
Eligible studies must be observational studies that investigated the association between presence, severity or response to treatment of NAFLD and genetic variations in vitamin D-related genes. These genes include DHCR7, CYP2R1, CYP2J2, CYP27A1, CYP3A4, CYP27B1, GC, VDR and CYP24A1.
Two investigators (A.J., B.P.) independently reviewed the titles and abstracts of retrieved records. Records that clearly did not fulfill the eligibility criteria based on type of article, study design or outcome of interest were excluded at this stage. Then, two investigators (A.J., B.P.) independently evaluated the full text of the remaining records for their final eligibility. The quality of each included study was assessed using the Newcastle–Ottawa quality assessment scale for the case–control study [36], which was performed by two investigators (AJ, BP). Different opinions in the eligibility and quality assessment of the records were resolved by discussion with the senior investigator (N.C.).
2.3. Data Extraction
Data from each eligible record were extracted using the standardized data collection form, which contained the following information: last name of the first author, country of the study, number of participants, evaluation of presence and/or severity of NAFLD, mean age of the participants, percentage of female participants and reported association of vitamin D-related genetic variations with outcomes.
3. Results and Discussion
3.1. Results
3.1.1. Search Results
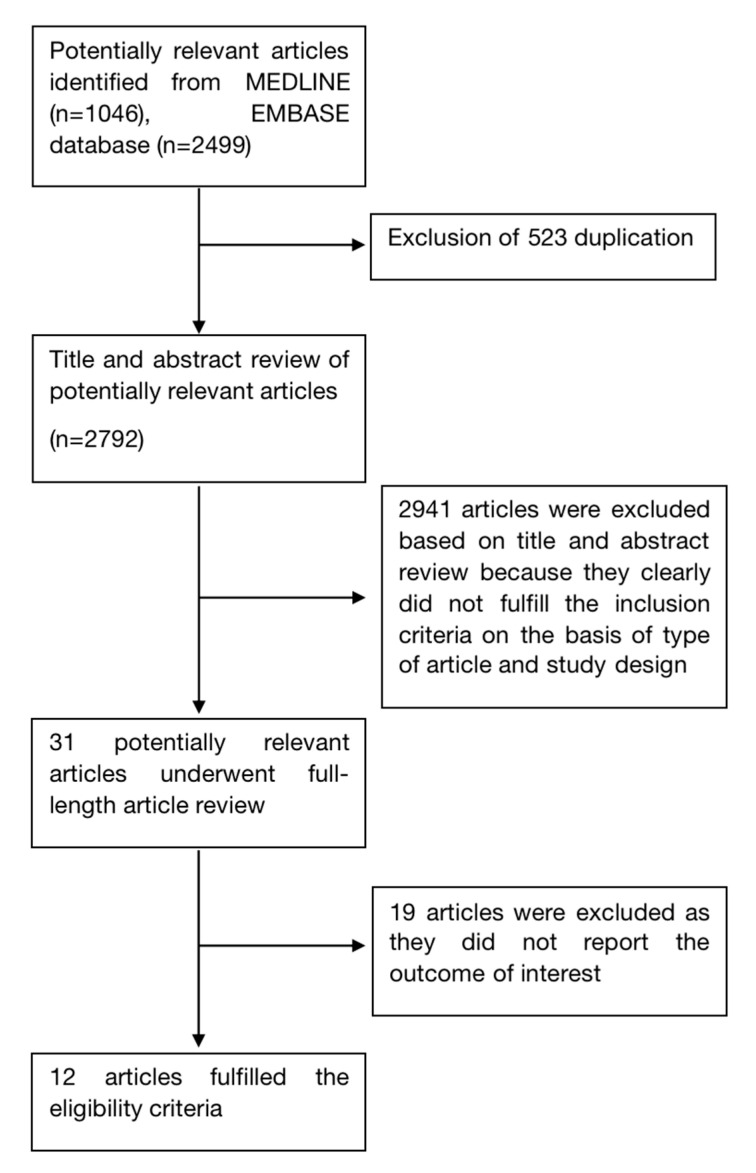
A total of 3495 records were identified from the electronic search. After removal of 523 duplicates, 2972 records underwent title and abstract review. A total of 2941 records were excluded at this stage as they clearly did not fulfill the eligibility criteria based on type of article, study design and outcome of interest, leaving 31 records for full-text review. A total of 19 records were further excluded at this stage since they did not report the outcome of interest. Finally, a total of 12 studies fulfilled the eligibility criteria [24,25,26,27,28,29,30,31,32,33,34,35]. Figure 1 summarizes the literature search and review process of this study.
Figure 1.
Study identification and literature review process.
3.1.2. Characteristics of Studies Reporting the Association between Vitamin D-Related Genetic Variations and Presence and/or Severity of NAFLD
A total of 12 studies consisting of at least 18,012 participants combined reported the outcome of interest [24,25,26,27,28,29,30,31,32,33,34,35]. These studies were conducted from 2010 to 2022. Four studies (two from the same population) are from China [30,31,32,35], three studies from the same group are from the United Kingdom [26,27,28], and the rest are from Australia [24], Germany, Iran [33], Japan [25] and the United States [34]. The average age of participants varied from 13.8 to 55.0 years and the percentage of females varied from 16.7 to 60.0%. Five studies investigated the association between vitamin D-related genetic variations and presence of NAFLD [24,26,30,34,35], six studies explored the relationship between the genetic variations and severity of NAFLD [26,27,28,29,34] and one study explored the influence of VDR genetic variation on response to calcitriol treatment [33]. Evaluations of NAFLD were performed by liver ultrasound in five studies [24,31,32,33,35], liver biopsy in four studies [25,26,27,28] and abdominal computed tomography in one study [34]. Eight of the twelve studies were of high quality based on a Newcastle–Ottawa score of more than 7 [24,25,29,30,31,32,34,35]. Five studies performed multivariate analysis to adjust for potential confounders [25,29,30,31,35]. The characteristics of all included studies were summarized in Table 1.
Table 1.
Main characteristics of studies investigating the association between vitamin D-related genetic variations and nonalcoholic fatty liver disease included in the systematic review.
| Study | Young [34] | Adams [24] | Gibson [27] |
| Country | USA | Australia | UK |
| Year of publication | 2010 | 2012 | 2014 |
| Total number of participants | 1180 | 928 | 78 |
| Recruitment of participants | Cases were patients with NAFLD recruited from families in San Antonio, San Luis Valley, and Los Angeles, USA who had CT measured of liver and visceral fat Controls were patients without NAFLD recruited from the same sites during the same period |
Cases were patients with NAFLD recruited from the Western Australian Pregnancy Cohort (Raine) Study in Perth, Western Australia from 1989 to 1992 Controls were patients without NAFLD recruited from the same sources during the same period |
Cases were NAFLD patients with increased fibrosis of liver (F2–F4) or increased NAS score recruited from medical records from the King’s College Hospital Pediatric Liver Clinic, UK Controls were NAFLD patients without increased fibrosis of liver (F2–F4) or increased NAS score recruited from the same source during the same period |
| Evaluation of NAFLD | CT measure of the liver and visceral fat | Liver ultrasound at age 17 | Liver biopsy |
| Average age of participants (years) | 48.7 | Cases: 17.0 Controls: 17.0 |
N/A |
| Percentage of female participants | 62.4 | Cases: 60.3 Controls: 45.9 |
N/A |
| Variables adjusted in multivariate analysis | N/A | N/A | N/A |
| Newcastle–Ottawa score | Selection: 4 Comparability: 0 Exposure: 3 |
Selection: 4 Comparability: 0 Exposure: 3 |
Selection: 3 Comparability: 0 Exposure: 3 |
| Study | Gibson [26] | Gibson [28] | Jamka [29] |
| Country | UK | UK | Germany |
| Year of publication | 2015 | 2018 | 2018 |
| Total number of participants | 103 | 103 | 241 |
| Recruitment of participants | Participants were patients with NAFLD recruited from medical records from the King’s College Hospital Pediatric Liver Clinic, UK, from March 2001 to July 2013 | Participants were patients with NAFLD recruited from medical records from the King’s College Hospital Pediatric Liver Clinic, UK, from March 2001 to July 2013 | Participants were patients with chronic liver diseases recruited from the Department of Medicine II, Saarland University Medical Center, Homburg, Germany |
| Evaluation of NAFLD | Liver biopsy | Liver biopsy | Fibroscan |
| Average age of participants (years) | 13.8 | 13.8 | 55.0 |
| Percentage of female participants | 34.0 | 34.0 | 43.1 |
| Variables adjusted in multivariate analysis | N/A | N/A | Age, season |
| Newcastle–Ottawa score | Selection: 3 Comparability: 0 Exposure: 3 |
Selection: 3 Comparability: 0 Exposure: 3 |
Selection: 3 Comparability: 1 Exposure: 3 |
| Study | Wang [32] | Arai [25] | Wang [31] |
| Country | China | Japan | China |
| Year of publication | 2018 | 2019 | 2021 |
| Total number of participants | 9182 | 229 | 3025 |
| Recruitment of participants | Cases were patients with NAFLD recruited from adult Chinese citizens from 23 sites in Shanghai, Zhejiang, Jiangsu, Anhui, and Jiangxi provinces from 2014 to 2016 Controls were patients without NAFLD recruited from the same sites during the same period |
Cases were NAFLD patients with advanced fibrosis of liver (F3–F4) recruited from families in San Antonio, San Luis Valley, and Los Angeles Controls were NAFLD patients without advanced fibrosis of liver (F3–F4) recruited from the same sites during the same period |
Cases were patients with NAFLD recruited from a community in Nanjing, Jiangsu, China from July to September 2018 Controls were patients without NAFLD recruited from the same source during the same period |
| Evaluation of NAFLD | Liver ultrasound | Liver biopsy | Liver ultrasound |
| Average age of participants (years) | 54.0 | 55.0 | Cases: 40.4 Controls: 39.7 |
| Percentage of female participants | 64.0 | 46.7 | Cases: 15.5 Controls: 18.1 |
| Variables adjusted in multivariate analysis | N/A | Age, body mass index, total cholesterol, serum 25(OH)D3 | Age, sex, visceral obesity, ALT, GGT, hypertension, hypertriglyceridemia, hyperglycemia, low HDL-C, unfavorable alleles |
| Newcastle–Ottawa score | Selection: 4 Comparability: 0 Exposure: 3 |
Selection: 3 Comparability: 2 Exposure: 3 |
Selection: 3 Comparability: 2 Exposure: 3 |
| Study | Yaghooti [33] | Zhang [35] | Wang [30] |
| Country | Iran | China | China |
| Year of publication | 2021 | 2021 | 2022 |
| Total number of participants | 128 | 3023 | N/A |
| Recruitment of participants | Participants were patients with fatty liver recruited from patients referred to the Ahvaz Golestan Hospital, Iran, from 2017 to 2018 | Cases were patients with NAFLD recruited from a community in Nanjing, Jiangsu, China, from July to September 2018 Controls were patients without NAFLD recruited from the same source during the same period |
Cases were patients with NAFLD recruited from Chinese population Controls were patients without NAFLD recruited from the same source during the same period |
| Evaluation of NAFLD | Liver ultrasound | Liver ultrasound | N/A |
| Average age of participants (years) | N/A | Cases: 40.5 Controls: 39.9 |
N/A |
| Percentage of female participants | N/A | Cases: 15.4 Controls: 17.5 |
N/A |
| Variables adjusted in multivariate analysis | N/A | Age, visceral obesity, hypertension, hypertriglyceridemia, low HDL-C, ALT, exercise | Age, gender, overweight, abdominal obesity, hypertension, hypertriglyceridemia, hyperglycemia |
| Newcastle–Ottawa score | Selection: 3 Comparability: 0 Exposure: 3 |
Selection: 4 Comparability: 2 Exposure: 3 |
Selection: 3 Comparability: 2 Exposure: 3 |
Abbreviations: 25(OH)D3: 25-hydroxyvitamin D3; ALT: Alanine aminotransferase; CT: Computed tomography; GGT: Gamma-glutamyl transferase; HDL-C: High-density lipoprotein-cholesterol; N/A: Not available; NAFLD: Nonalcoholic fatty liver disease; NAS: Nonalcoholic fatty liver disease activity score; UK: United Kingdom; USA: United States of America.
3.1.3. Association between Vitamin D-Related Polymorphism and Presence, Severity and Response to Treatment of Nonalcoholic Fatty Liver Disease
Among the 12 included studies, a total of 26 genetic variations of six genes were identified to be associated with presence, severity or response to treatment of NAFLD, including GC, VDR, CYP27B1, CYP2R1, DHCR7 and CYP24A1. As shown in Table 2, the presence of NAFLD was associated with variations of the genes GC (rs222054, rs222020, rs10011000, rs7041), VDR (rs2228570, rs11168287, rs10783219, rs4752), CYP24A1 (rs3787557, rs6068816, rs2296241, rs2248359) and CYP27B1 (rs4646536) [24,26,30,31,32,34]. Liver density based on abdominal computed tomography was associated with variations of the genes VDR (rs4334089) and CYP24A1 (rs3787557, rs6068816, rs6097809, rs6127119, rs2248359, rs3787554, rs4809960, rs6022999) [34]. Histological steatosis was associated with variations of the genes DHCR7 (rs3829251) and VDR (rs2228570) [28,29]. In addition, another DHCR7 variation (rs12785878) was found to be associated with histological steatosis in one study [28] but not in the other [29]. Inflammation and fibrosis based on NAFLD activity score were associated with mutations in the genes DHCR7 (rs12785878), GC (rs4588), VDR (rs2228570) and CYP2R1 (rs10741657) [28]. Advanced fibrosis based on NAFLD activity score was associated with VDR (rs1544410) genetic variation [25]. Overall NAFLD activity score was associated with CYP2R1 (rs10741657) [27]. Finally, response to calcitriol treatment indicated by the degree of decrease in alkaline phosphatase was associated with VDR (rs10735810) genetic variation [33].
Table 2.
Association between vitamin D-related genetic variations and presence, severity and response to treatment of nonalcoholic.
| Outcome | Gene | Locus | Finding |
|---|---|---|---|
| Presence of NAFLD | GC | rs222054 |
|
| GC | rs222020 |
|
|
| GC | rs10011000 |
|
|
| GC | rs7041 |
|
|
| GC | rs2282679 | ||
| GC | rs222020 |
|
|
| GC | rs4588 |
|
|
| GC | rs1155563 |
|
|
| GC | rs16847024 |
|
|
| GC | rs3733359 |
|
|
| VDR | rs2228570 |
|
|
| VDR | rs11168287 |
|
|
| VDR | rs10783219 |
|
|
| VDR | rs4752 |
|
|
| CYP24A1 | rs3787557 |
|
|
| CYP24A1 | rs6068816 |
|
|
| CYP24A1 | rs2296241 |
|
|
| CYP24A1 | rs2248359 |
|
|
| CYP24A1 | rs6013897 |
|
|
| CYP27B1 | rs4646536 |
|
|
| CYP2R1 | rs10741657 | ||
| DHCR7 | rs12785878 |
|
|
| Liver density a | VDR | rs4334089 |
|
| CYP24A1 | rs3787555 |
|
|
| CYP24A1 | rs6068816 |
|
|
| CYP24A1 | rs6097809 |
|
|
| CYP24A1 | rs6127119 |
|
|
| CYP24A1 | rs2248359 |
|
|
| CYP24A1 | rs3787554 |
|
|
| CYP24A1 | rs4809960 |
|
|
| CYP24A1 | rs6022999 |
|
|
| CYP27B1 | N/A |
|
|
| CYP2R1 | N/A |
|
|
| Steatosis b | DHCR7 | rs12785878 | |
| DHCR7 | rs3829251 |
|
|
| GC | rs7041 |
|
|
| VDR | rs2228570 |
|
|
| VDR | rs79754353 |
|
|
| CYP2R1 | rs10741657 |
|
|
| Inflammation and fibrosis c | DHCR7 | rs12785878 |
|
| GC | rs4588 |
|
|
| VDR | rs2228570 |
|
|
| CYP2R1 | rs10741657 |
|
|
| Advanced fibrosis d | DHCR7 | rs7944926 |
|
| DHCR7 | rs12785878 |
|
|
| GC | rs2282679 |
|
|
| VDR | rs1544410 |
|
|
| VDR | rs2228750 |
|
|
| VDR | rs7975232 |
|
|
| VDR | rs731236 |
|
|
| CYP27B1 | rs10877012 |
|
|
| CYP2R1 | rs1993116 |
|
|
| CYP2R1 | rs10741657 |
|
|
| NAFLD activity score e | CYP2R1 | rs10741657 |
|
| NAFLD histological severity f | GC | rs2282679 |
|
| CYP2R1 | rs10741657 |
|
|
| Response to calcitriol treatment | VDR | rs10735810 |
|
a Liver density was examined using a variance components approach based on computed tomography measure of the liver and visceral fat. b Steatosis was assessed based on histology using the NAFLD activity score (Gibson et al., 2018 [28]) and controlled attenuation parameter from transient elastography (Jamka et al., 2018 [29]). c Inflammation and fibrosis were assessed using the NAFLD activity score (Gibson et al., 2018 [28]). d Histopathological evaluation was performed by experienced pathologists blinded to clinical and laboratory data of the patients. Liver fibrosis was semi-quantitatively evaluated using the NASH Clinical Research Network scoring system. e The NAFLD activity score included a summation of numerical scores for steatosis (0–3), hepatocyte ballooning (1–2) and lobular inflammation (0–3) (Gibson et al., 2018 [28]). f Biopsies were scored by a liver histopathologist according to the Kleiner–Brunt system. Abbreviations: AA: African American; ALP: Alkaline phosphatase; HA: Hispanic American; N/A: Not applicable; NAFLD: Nonalcoholic fatty liver disease; NASH: Nonalcoholic steatohepatitis.
3.2. Discussion
This is the first systematic review that explored the relationship between vitamin D-related genetic variations and NAFLD. Our systematic review revealed the association of presence, severity and response to treatment of NAFLD with variations of several genes in the vitamin D metabolic pathway, which include DHCR7, CYP2R1, CYP24A1, CYP27B1, GC and VDR. These findings support the notion that the vitamin D signaling pathway may play a significant role in the pathogenesis of NAFLD.
In fact, 1,25(OH)2D, the active form of vitamin D is known to have anti-inflammatory and antifibrogenic effects by inhibiting proinflammatory cytokines production (i.e., interleukin-1, interleukin-6 and tumor necrosis factor-alpha), enhancing anti-inflammatory cytokines production (i.e., interleukin-10 and adiponectin) and suppressing the function hepatic stellate cells [17,37,38]. These actions could therefore slow down the process of liver inflammation and fibrosis. In addition, 1,25(OH)2D was shown to enhance insulin receptor expression, thereby mitigating insulin resistance, which is known to be a major component of NAFLD pathogenesis [39,40].
It is worth noting that multiple observational studies revealed the association between low level of serum 25(OH)D and increased risk and severity of NAFLD [15]. Nevertheless, the causality and clinical significance of this association remain undetermined given that the association could be due to confounding effects (i.e., limited physical activity and high body mass index) as well as reverse causation since hepatic steatosis is shown to be associated with decreased activity of the 25-hydroxylase, which can result in decreased circulating 25(OH)D [15,16]. A few randomized controlled trials have shown that vitamin D supplementation can improve hepatic steatosis and insulin resistance and decrease biomarkers of inflammation in adults with NAFLD [41]. However, a mendelian randomization study by Wang et al. demonstrated no causal association between serum 25(OH)D concentration and presence of NAFLD [32].
Alteration of any steps of vitamin D metabolism could possibly affect levels and functions of vitamin D. For example, previous genome-wide association studies reported variations in the DHCR7(rs12785878), GC (rs2282679), CYP2R1(rs10741657), VDR (rs2228570, rs1544410, rs7975232, rs731236) and CYP24A1 (rs17216707) genes were associated with serum 25(OH)D level [42,43]. Another meta-analysis found that genetic variations of the GC (rs2282679, rs4588, rs1155563, rs7041) and CYP2R1 genes (rs10741657, rs10766197, rs2060793) were associated with vitamin D levels in more than 50% of the respective studies [44]. Therefore, variations in genes related to vitamin D metabolism may eventually affect the risks of NAFLD from multiple possible pathophysiologies mentioned above. It has been shown in an animal model that mice lacking VDR in the liver had increased hepatic steatosis and insulin resistance, as well as diminished the protective effect of vitamin D supplementation on NAFLD [45]. Mechanistic experiments demonstrated that the VDR interaction may improve lipid metabolism by interacting with the hepatocyte nuclear factor 4 α (HNF4α) [45]. Based on this observation, it is possible that genetic variations in the VDR may affect VDR expression in the liver, thereby modifying the risk of NAFLD. Data on animal models associated with other genes in the vitamin D metabolic pathway are, however, lacking.
Taken together, the relationship between vitamin D and pathogenesis and progression of NAFLD remains unclarified and may be complex. The observation that genetic variations of vitamin D-related genes were associated with presence, severity and response to treatment of NAFLD provides additional insights, as it may indicate interindividual differences in responsiveness to vitamin D. This can be supported by the observation by Barchetta et al. [46] in patients with NASH that vitamin D receptor expression on cholangiocytes was negatively correlated with steatosis severity, lobular inflammation and NAFLD score. Furthermore, the concept of individual responsiveness to vitamin D has been introduced based on findings from clinical trials that revealed differences in the degree of genome-wide expression in peripheral blood mononuclear cells as well as metabolomic profiles in response to vitamin D supplementation [47,48,49]. Future studies are warranted to further explain the impact of vitamin D-related genetic variations on metabolic outcomes.
The results of this systematic review may have some research implications as the reported genetic variations associated with NAFLD may be used as a reference for future animal models to further elucidate the link between vitamin D and NAFLD pathogenesis. In addition, these variations may be considered novel markers for determining individuals at risk for developing NAFLD. However, there are certain limitations of this systematic review that should be acknowledged. Most of the included studies are small in sample size, and many of them did not adjust for confounders as only five studies were performed in a large-scale cohort [24,31,32,34,35], and four studies conducted robust multivariate analysis [25,30,31,35]. Notably, none of the included studies considered calcium supplementation, a potential confounder that could affect NAFLD pathogenesis, in their multivariate analyses [50]. More importantly, none of the reported significant genetic variations were confirmed to be associated with outcomes in more than one study. All these could have jeopardized the reliability of the findings. Further studies are required to verify the findings of these studies.
4. Conclusions
This systematic review identified 26 vitamin D-related genetic variations in the DHCR7, CYP2R1, CYP24A1, CYP27B1, GC, and VDR genes to be associated with presence, severity or response to treatment of NAFLD. However, the confidence of these findings was relatively limited awaiting confirmation by future studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms23169122/s1. Ref. [51] is cited in Supplementary Materials.
Author Contributions
Conceptualization, A.J. and N.C.; methodology, A.J., P.S., B.P. and N.C.; investigation, A.J., P.S., B.P. and N.C.; data curation, A.J. and B.P.; original draft preparation, A.J. and N.C.; writing—review and editing, A.J. and N.C.; visualization, N.C.; supervision, N.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Puri P., Sanyal A.J. Nonalcoholic fatty liver disease: Definitions, risk factors, and workup. Clin. Liver Dis. 2012;1:99–103. doi: 10.1002/cld.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banini B.A., Sanyal A.J. Nonalcoholic Fatty Liver Disease: Epidemiology, Pathogenesis, Natural History, Diagnosis, and Current Treatment Options. Clin. Med. Insights Ther. 2016;8:75–84. doi: 10.4137/CMT.S18885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loomba R., Sanyal A.J. The global NAFLD epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013;10:686–690. doi: 10.1038/nrgastro.2013.171. [DOI] [PubMed] [Google Scholar]
- 4.Perumpail B.J., Khan M.A., Yoo E.R., Cholankeril G., Kim D., Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J. Gastroenterol. 2017;23:8263–8276. doi: 10.3748/wjg.v23.i47.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fabbrini E., Sullivan S., Klein S. Obesity and nonalcoholic fatty liver disease: Biochemical, metabolic, and clinical implications. Hepatology. 2010;51:679–689. doi: 10.1002/hep.23280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charoenngam N., Shirvani A., Holick M.F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma. 2019;10:1082–1093. doi: 10.1016/j.jcot.2019.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holick M.F. Vitamin D Deficiency. New Engl. J. Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 8.Carlberg C., Campbell M.J. Vitamin D receptor signaling mechanisms: Integrated actions of a well-defined transcription factor. Steroids. 2013;78:127–136. doi: 10.1016/j.steroids.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bikle D.D. Vitamin D: Newer Concepts of Its Metabolism and Function at the Basic and Clinical Level. J. Endocr. Soc. 2020;4:bvz038. doi: 10.1210/jendso/bvz038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aiba I., Yamasaki T., Shinki T., Izumi S., Yamamoto K., Yamada S., Terato H., Ide H., Ohyama Y. Characterization of rat and human CYP2J enzymes as Vitamin D 25-hydroxylases. Steroids. 2006;71:849–856. doi: 10.1016/j.steroids.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Zhu J.G., Ochalek J.T., Kaufmann M., Jones G., Deluca H.F. CYP2R1 is a major, but not exclusive, contributor to 25-hydroxyvitamin D production in vivo. Proc. Natl. Acad. Sci. USA. 2013;110:15650–15655. doi: 10.1073/pnas.1315006110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holick M.F., Binkley N.C., Bischoff-Ferrari H.A., Gordon C.M., Hanley D.A., Heaney R.P., Murad M.H., Weaver C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 13.Ross A.C., Manson J.E., Abrams S.A., Aloia J.F., Brannon P.M., Clinton S.K., Durazo-Arvizu R.A., Gallagher J.C., Gallo R.L., Jones G., et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J. Clin. Endocrinol. Metab. 2011;96:53–58. doi: 10.1210/jc.2010-2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hossein-nezhad A., Holick M.F. Vitamin D for health: A global perspective. Mayo Clin. Proc. 2013;88:720–755. doi: 10.1016/j.mayocp.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eliades M., Spyrou E., Agrawal N., Lazo M., Brancati F.L., Potter J.J., Koteish A.A., Clark J.M., Guallar E., Hernaez R. Meta-analysis: Vitamin D and non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2013;38:246–254. doi: 10.1111/apt.12377. [DOI] [PubMed] [Google Scholar]
- 16.Jaruvongvanich V., Ahuja W., Sanguankeo A., Wijarnpreecha K., Upala S. Vitamin D and histologic severity of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Dig. Liver Dis. 2017;49:618–622. doi: 10.1016/j.dld.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Charoenngam N., Holick M.F. Immunologic Effects of Vitamin D on Human Health and Disease. Nutrients. 2020;12:2097. doi: 10.3390/nu12072097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Szymczak-Pajor I., Śliwińska A. Analysis of Association between Vitamin D Deficiency and Insulin Resistance. Nutrients. 2019;11:794. doi: 10.3390/nu11040794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hariri M., Zohdi S. Effect of Vitamin D on Non-Alcoholic Fatty Liver Disease: A Systematic Review of Randomized Controlled Clinical Trials. Int. J. Prev. Med. 2019;10:14. doi: 10.4103/ijpvm.IJPVM_499_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feng M., Li H., Chen S.-F., Li W.-F., Zhang F.-B. Polymorphisms in the vitamin D receptor gene and risk of autoimmune thyroid diseases: A meta-analysis. Endocrine. 2013;43:318–326. doi: 10.1007/s12020-012-9812-y. [DOI] [PubMed] [Google Scholar]
- 21.Li L., Wu B., Liu J.-Y., Yang L.-B. Vitamin D Receptor Gene Polymorphisms and Type 2 Diabetes: A Meta-analysis. Arch. Med. Res. 2013;44:235–241. doi: 10.1016/j.arcmed.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Lu S., Guo S., Hu F., Guo Y., Yan L., Ma W., Wang Y., Wei Y., Zhang Z., Wang Z. The Associations Between the Polymorphisms of Vitamin D Receptor and Coronary Artery Disease: A Systematic Review and Meta-Analysis. Medicine. 2016;95:e3467. doi: 10.1097/MD.0000000000003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pakpahan C., Wungu C.D.K., Agustinus A., Darmadi D. Do Vitamin D receptor gene polymorphisms affect bone mass density in men?: A meta-analysis of observational studies. Ageing Res. Rev. 2022;75:101571. doi: 10.1016/j.arr.2022.101571. [DOI] [PubMed] [Google Scholar]
- 24.Adams L.A., White S.W., Marsh J.A., Lye S.J., Connor K.L., Maganga R., Ayonrinde O.T., Olynyk J.K., Mori T.A., Beilin L.J., et al. Association between liver-specific gene polymorphisms and their expression levels with nonalcoholic fatty liver disease. Hepatology. 2013;57:590–600. doi: 10.1002/hep.26184. [DOI] [PubMed] [Google Scholar]
- 25.Arai T., Atsukawa M., Tsubota A., Koeda M., Yoshida Y., Okubo T., Nakagawa A., Itokawa N., Kondo C., Nakatsuka K., et al. Association of vitamin D levels and vitamin D-related gene polymorphisms with liver fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease. Dig. Liver Dis. 2019;51:1036–1042. doi: 10.1016/j.dld.2018.12.022. [DOI] [PubMed] [Google Scholar]
- 26.Gibson P., Fitzpatrick E., Quaglia A., Dhawan A., Wu H., Hart K., Lanham-New S., Moore J.B. Assessment of vitamin D status and genetic variation in vitamin-D related genes: Key findings from a UK paediatric non-alcoholic fatty liver disease population. Proc. Nutr. Soc. 2015;74:OCE1. doi: 10.1017/S0029665115000270. [DOI] [Google Scholar]
- 27.Gibson P.S., Fitzpatrick E., Quaglia A., Dhawan A., Wu H., Hart K., Lanham-New S., Moore J.B. Association of NADSYN1, DHCR7, GC and VDR genotypes with steatosis and liver inflammation in UK paediatric non-alcoholic fatty liver disease patients. Hepatology. 2014;60:967A. doi: 10.1002/hep.27527. [DOI] [Google Scholar]
- 28.Gibson P.S., Quaglia A., Dhawan A., Wu H., Lanham-New S., Hart K.H., Fitzpatrick E., Moore J.B. Vitamin D status and associated genetic polymorphisms in a cohort of UK children with non-alcoholic fatty liver disease. Pediatric. Obes. 2018;13:433–441. doi: 10.1111/ijpo.12293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jamka M., Arslanow A., Bohner A., Krawczyk M., Weber S.N., Grunhage F., Lammert F., Stokes C.S. Effects of Gene Variants Controlling Vitamin D Metabolism and Serum Levels on Hepatic Steatosis. Digestion. 2018;97:298–308. doi: 10.1159/000485180. [DOI] [PubMed] [Google Scholar]
- 30.Wang M., Wang M., Zhang R., Shen C., Zhang L., Ding Y., Tang Z., Wang H., Zhang W., Chen Y., et al. Influences of Vitamin D Levels and Vitamin D-Binding Protein Polymorphisms on Nonalcoholic Fatty Liver Disease Risk in a Chinese Population. Ann. Nutr. Metab. 2022;78:61–72. doi: 10.1159/000522193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang M., Zhang R., Wang M., Zhang L., Ding Y., Tang Z., Wang H., Zhang W., Chen Y., Wang J. Genetic Polymorphism of Vitamin D Family Genes CYP2R1, CYP24A1, and CYP27B1 Are Associated With a High Risk of Non-alcoholic Fatty Liver Disease: A Case-Control Study. Front. Genet. 2021;12:717533. doi: 10.3389/fgene.2021.717533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang N., Chen C., Zhao L., Chen Y., Han B., Xia F., Cheng J., Li Q., Lu Y. Vitamin D and Nonalcoholic Fatty Liver Disease: Bi-directional Mendelian Randomization Analysis. EBioMedicine. 2018;28:187–193. doi: 10.1016/j.ebiom.2017.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yaghooti H., Ghanavati F., Seyedian S.S., Cheraghian B., Mohammadtaghvaei N. The efficacy of calcitriol treatment in non-alcoholic fatty liver patients with different genotypes of vitamin D receptor FokI polymorphism. BMC Pharmacol. Toxicol. 2021;22:18. doi: 10.1186/s40360-021-00485-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Young K.A., Fingerlin T.E., Wagenknecht L.E., Engelman C.D., Haffner S.M., Lorenzo C., Chen Y.D., Sibbel S.P., Norris J.M. Variants in vitamin D genes are associated with liver density and non-alcoholic fatty liver disease (NAFLD) in Hispanics and African Americans: The IRAS Family Study. Diabetologia. 2010;53:S139–S140. doi: 10.1007/s00125-010-1872-z. [DOI] [Google Scholar]
- 35.Zhang R., Wang M., Wang M., Zhang L., Ding Y., Tang Z., Fu Z., Fan H., Zhang W., Wang J. Vitamin D Level and Vitamin D Receptor Genetic Variation Were Involved in the Risk of Non-Alcoholic Fatty Liver Disease: A Case-Control Study. Front. Endocrinol. 2021;12:648844. doi: 10.3389/fendo.2021.648844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luchini C., Stubbs B., Solmi M., Veronese N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J. Meta-Anal. 2017;5:80–84. doi: 10.13105/wjma.v5.i4.80. [DOI] [Google Scholar]
- 37.Keane J.T., Elangovan H., Stokes R.A., Gunton J.E. Vitamin D and the Liver-Correlation or Cause? Nutrients. 2018;10:496. doi: 10.3390/nu10040496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bidulescu A., Morris A.A., Stoyanova N., Meng Y.X., Vaccarino V., Quyyumi A.A., Gibbons G.H. Association between Vitamin D and Adiponectin and Its Relationship with Body Mass Index: The META-Health Study. Front. Public Health. 2014;2:193. doi: 10.3389/fpubh.2014.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sung C.C., Liao M.T., Lu K.C., Wu C.C. Role of vitamin D in insulin resistance. J. Biomed. Biotechnol. 2012;2012:634195. doi: 10.1155/2012/634195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marchesini G., Brizi M., Morselli-Labate A.M., Bianchi G., Bugianesi E., McCullough A.J., Forlani G., Melchionda N. Association of nonalcoholic fatty liver disease with insulin resistance. Am. J. Med. 1999;107:450–455. doi: 10.1016/S0002-9343(99)00271-5. [DOI] [PubMed] [Google Scholar]
- 41.Sharifi N., Amani R. Vitamin D supplementation and non-alcoholic fatty liver disease: A critical and systematic review of clinical trials. Crit. Rev. Food Sci. Nutr. 2019;59:693–703. doi: 10.1080/10408398.2017.1389693. [DOI] [PubMed] [Google Scholar]
- 42.Manousaki D., Mitchell R., Dudding T., Haworth S., Harroud A., Forgetta V., Shah R.L., Luan J.a., Langenberg C., Timpson N.J., et al. Genome-wide Association Study for Vitamin D Levels Reveals 69 Independent Loci. Am. J. Hum. Genet. 2020;106:327–337. doi: 10.1016/j.ajhg.2020.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruiz-Ballesteros A.I., Meza-Meza M.R., Vizmanos-Lamotte B., Parra-Rojas I., de la Cruz-Mosso U. Association of Vitamin D Metabolism Gene Polymorphisms with Autoimmunity: Evidence in Population Genetic Studies. Int. J. Mol. Sci. 2020;21:9626. doi: 10.3390/ijms21249626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krasniqi E., Boshnjaku A., Wagner K.-H., Wessner B. Association between Polymorphisms in Vitamin D Pathway-Related Genes, Vitamin D Status, Muscle Mass and Function: A Systematic Review. Nutrients. 2021;13:3109. doi: 10.3390/nu13093109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang H., Shen Z., Lin Y., Zhang J., Zhang Y., Liu P., Zeng H., Yu M., Chen X., Ning L., et al. Vitamin D receptor targets hepatocyte nuclear factor 4α and mediates protective effects of vitamin D in nonalcoholic fatty liver disease. J. Biol. Chem. 2020;295:3891–3905. doi: 10.1074/jbc.RA119.011487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barchetta I., Carotti S., Labbadia G., Gentilucci U.V., Muda A.O., Angelico F., Silecchia G., Leonetti F., Fraioli A., Picardi A., et al. Liver vitamin D receptor, CYP2R1, and CYP27A1 expression: Relationship with liver histology and vitamin D3 levels in patients with nonalcoholic steatohepatitis or hepatitis C virus. Hepatology. 2012;56:2180–2187. doi: 10.1002/hep.25930. [DOI] [PubMed] [Google Scholar]
- 47.Shirvani A., Kalajian T.A., Song A., Holick M.F. Disassociation of Vitamin D’s Calcemic Activity and Non-calcemic Genomic Activity and Individual Responsiveness: A Randomized Controlled Double-Blind Clinical Trial. Sci. Rep. 2019;9:17685. doi: 10.1038/s41598-019-53864-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shirvani A., Kalajian T.A., Song A., Allen R., Charoenngam N., Lewanczuk R., Holick M.F. Variable Genomic and Metabolomic Responses to Varying Doses of Vitamin D Supplementation. Anticancer Res. 2020;40:535. doi: 10.21873/anticanres.13982. [DOI] [PubMed] [Google Scholar]
- 49.Carlberg C., Haq A. The concept of the personal vitamin D response index. J. Steroid Biochem. Mol. Biol. 2018;175:12–17. doi: 10.1016/j.jsbmb.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 50.Das S., Choudhuri D. Calcium supplementation shows a hepatoprotective effect against high-fat diet by regulating oxidative-induced inflammatory response and lipogenesis activity in male rats. J. Tradit Complement. Med. 2019;10:511–519. doi: 10.1016/j.jtcme.2019.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.