Abstract
Heart failure with preserved ejection fraction (HFpEF) represents the most common HF phenotype of patients aged > 65 years, with an incidence and a prevalence that are constantly growing. The HFpEF cardinal symptom is exercise intolerance (EI), defined as the impaired ability to perform physical activity and to reach the predicted age-related level of exercise duration in the absence of symptoms—such as fatigue or dyspnea—and is associated with a poor quality of life, a higher number of hospitalizations, and poor outcomes. The evidence of the protective effect between exercise and adverse cardiovascular outcomes is numerous and long-established. Regular exercise is known to reduce cardiovascular events and overall mortality both in apparently healthy individuals and in patients with established cardiovascular disease, representing a cornerstone in the prevention and treatment of many cardio-metabolic conditions. Several studies have investigated the role of exercise in HFpEF patients. The present review aims to dwell upon the effects of exercise on HFpEF. For this purpose, the relevant data from a literature search (PubMed, EMBASE, and Medline) were reviewed. The analysis of these studies underlines the fact that exercise training programs improve the cardiorespiratory performance of HFpEF patients in terms of the increase in peak oxygen uptake, the 6 min walk test distance, and the ventilatory threshold; on the other hand, diastolic or systolic functions are generally unchanged or only partially modified by exercise, suggesting that multiple mechanisms contribute to the improvement of exercise tolerance in HFpEF patients. In conclusion, considering that exercise training programs are able to improve the cardiorespiratory performance of HFpEF patients, the prescription of exercise training programs should be encouraged in stable HFpEF patients, and further research is needed to better elucidate the pathophysiological mechanisms underpinning the beneficial effects described.
Keywords: exercise intolerance, heart failure, exercise, heart failure with preserved ejection fraction, cardiopulmonary exercise test, peak VO2
1. Introduction
Heart failure with preserved ejection fraction (HFpEF) is defined as a clinical syndrome characterized by typical symptoms (e.g., breathlessness and fatigue) and signs (e.g., peripheral oedema and lung crackles), evidence of cardiac structural and/or functional abnormalities—consistent with the presence of left ventricle diastolic dysfunction/raised left ventricle filling pressures—and left ventricular ejection fraction (LVEF) ≥ 50% [1,2].
Notably, HFpEF represents the most common HF phenotype of patients aged > 65 years [3], with a constantly growing incidence and prevalence [4] due to the ageing of the general population and the increasing prevalence of conditions associated with HFpEF development (i.e., obesity, metabolic syndrome, and diabetes mellitus) [5,6,7].
Nowadays, HFpEF represents a major cause of morbidity and mortality. It is a complex syndrome characterized by multi-organ involvement; it is typical in older, female patients and is frequently correlated with obesity, hypertension, ischemic heart disease, diabetes mellitus, and atrial fibrillation [8,9,10,11], and it may present with a wide range of clinical pictures, ranging from asymptomatic or mild disease to life-threatening conditions [1].
The diagnosis of HFpEF is challenging, and in recent years, functional testing (i.e., to detect hemodynamic abnormalities during exercise) has been clearly proven as important in HFpEF diagnosis [12]. Indeed, there is an intimate link between the (expected) hemodynamical changes during exercise and the abnormalities described in HFpEF, with some not present at rest and detectable only during exercise [12]
Finally, exercise intolerance (i.e., the impaired ability to perform physical activity and to reach the predicted age-related level of exercise duration in the presence of symptoms—such as fatigue or dyspnea) is a typical feature of HFpEF and is associated with a poor quality of life, a higher incidence of hospitalization, and poor outcomes [13].
Taking these premises into account and shedding light upon the intimate link between exercise and HFpEF, the present review aims to dwell upon the effects of exercise on HFpEF. For this purpose, the relevant data from a literature search (PubMed, EMBASE, and Medline) were reviewed. After a brief introductive paragraph on the general benefits of exercise on cardiovascular performance, with an excursus on the role of exercise on primary and secondary prevention, the available evidence regarding the effect of exercise in HFpEF is revised; finally, the future perspectives with regard to the role of exercise in the management and treatment of HFpEF are discussed.
2. Cardiovascular Benefits of Exercise
The evidence of an inverse relationship between exercise and adverse cardiovascular outcomes is numerous and long-established [14,15]. Indeed, regular exercise is known to reduce cardiovascular events and overall mortality in both apparently healthy individuals and patients with established cardiovascular disease, representing a cornerstone in the prevention and treatment of many cardio-metabolic conditions [16,17].
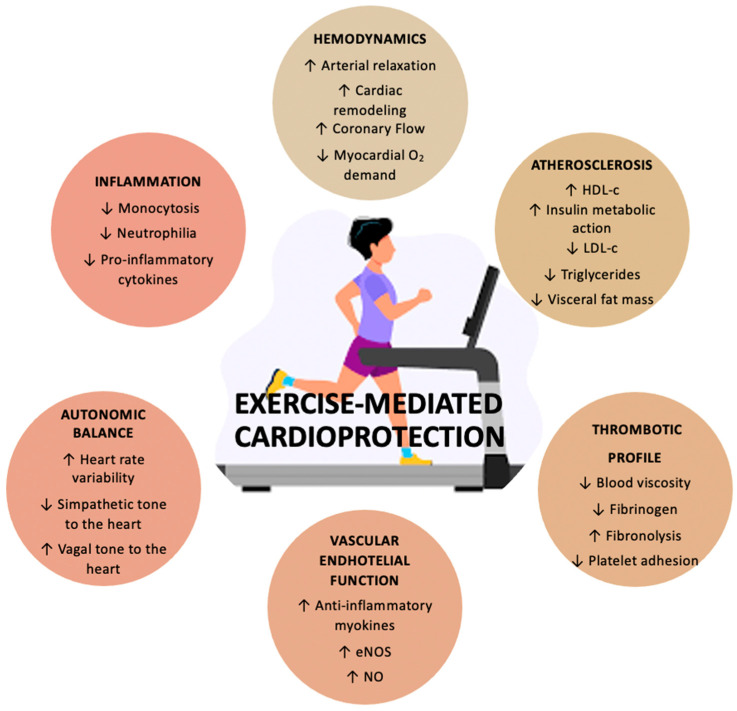
Specifically, physical activity promotes cardiovascular health through two main mechanisms: firstly by attenuating the negative effect of many established risk factors for cardiovascular disease (e.g., cholesterol, and insulin sensitivity) and secondly by exerting direct beneficial effects [18]. (Figure 1)
Figure 1.
Exercise mediated protective effects on the cardiovascular system. Abbreviations: eNOS: endothelial nitric oxide synthase; NO: nitric oxide; HDL-c: high density lipoprotein cholesterol; LDL-c: low density lipoprotein cholesterol.
2.1. Effects on Cardiovascular Risk Factors
Regular training is associated with the reduction in cardiovascular risk factors, such as Body Mass Index (BMI), LDL cholesterol, blood pressure, and sleep apnea, and with the increase in HDL cholesterol and insulin sensitivity.
Exercise is known to be a powerful intervention for weight loss, particularly when combined with a balanced diet [19]. In turn, even a modest reduction in body weight (5–10%) ameliorates lipid disorders and other cardiovascular risk factors that generally coexist in dyslipidaemic patients [20]. Specifically, a meta-analysis that included 182 participants, using a random-effects model, showed a decrease in BMI in patients with sleep apnea receiving exercise prescriptions.
With regard to dyslipidemia, Kraus et al. explored the effects of the amount and the intensity of exercise on the lipid profile in overweight and obese dyslipidaemic patients, showing that high-amount–high-intensity exercise significantly reduced LDL concentrations. This effect was also confirmed for the HDL variables [21]; indeed, 25–30 km of brisk walking per week or the equivalent aerobic physical activities increased HDL levels by 3–6 mg/dL. Finally, in 509 T2DM patients, targeted metabolomics on lipidomics suggested that HDL subclasses appear sensitive to light intensities, whereas only the high category of physical activity intensity was consistently associated with VLDL subclasses [22].
With regard to blood pressure, a recent meta-analysis of data from 1207 hypertensive patients showed a significant reduction in systolic (−10 mmHg) and diastolic (−5.5 mmHg) blood pressure in subjects following aerobic training programs [23], with High-Intensity Interval Training (HIIT) also showing a significant reduction in older patients [24]; in addition, it has recently been shown that physical activity and exercise added to the usual care may further reduce BP in patients with resistant hypertension [25]; similar results have been observed in T2DM patients [26]. Similarly, strength training, by resulting in skeletal muscle hypertrophy, can lead to increased tissue responsiveness to insulin in terms of glucose storage and utilization. Thus, aerobic exercise, resistance training, or their combination can improve insulin sensitivity, leading to a reduced risk of developing T2DM in patients with impaired fasting glucose and reduced blood HbA1c concentrations (0.7%) in diabetic patients [27].
2.2. Direct Cardiovascular Effects
Regarding the direct effects of exercise on cardiovascular diseases (CVD), regular exercise exerts multiple positive effects on the structure and function of the heart and peripheral vasculature. Firstly, regular training is associated with higher nitric oxide bioavailability [28]. Ashor et al. reported the significant enhancement of endothelial function with aerobic, resistance, and combined modalities of exercises; for every increase of 2 metabolic equivalents (MET) in exercise intensity, a 1% improvement in flow-mediated dilation was observed [29]. Exercise also promotes vascular remodeling, which consists of increased diameter and dilatation capacity of the coronary and peripheral arteries and decreased vascular wall thickness and the development of coronary collateral vessels [30,31]. In addition, regular physical activity influences the atherosclerotic plaque structure by modifying the composition and amount of collagen and elastin in animal models [32]. Notably, other mechanisms by which exercise results in direct cardiovascular benefits involve the autonomic nervous system via a decrease in catecholamine levels, ß-adrenergic receptor concentration, angiotensin 2, and increased nitric oxide bioavailability, with a consequent protection against fatal arrhythmias. Life-threatening arrhythmias—rare in HFpEF—can also be prevented by cardiac preconditioning mechanisms [33]. Finally, among the direct cardioprotective mechanisms mediated by physical exercise, anti-thrombotic and anti-inflammatory properties play a crucial role and are mainly sustained by muscle-derived myokines [34].
2.3. Clinical Context
Exercise-related health benefits are reported in both primary and secondary prevention, including for patients with CAD or heart failure [35].
Numerous studies performed in primary-prevention patients have shown beneficial effects in CVD prevention regardless of age, gender, or ethnicity [36]. In a prospective cohort analysis among 4207 subjects, increased physical activity was inversely associated with coronary heart disease, stroke, and total cardiovascular disease, even in older patients. Risk reduction was related to the intensity and duration of exercise [37]. Manson et al. prospectively examined the incidence of cardiovascular events among postmenopausal women by physical activity, showing that walking and vigorous exercise were associated with a significant reduction in events, independently of ethnic group, age, and BMI [38]. The PRIME study collected data from 9758 patients and demonstrated that leisure-time physical activity energy expenditure was associated with a lower risk of major cardiovascular events [39]. Moreover, the ARIC study demonstrated that subjects who maintained guideline-recommended levels of physical activity over time had the lowest heart failure risk, and increasing physical activity over a 6-year interval was also associated with further risk reduction [40].
The positive effects of physical activity are also reported in secondary prevention, independently of age and disease severity. Cardiac rehabilitation (CR) reduces mortality, hospitalizations, and care use and improves cardiorespiratory fitness, quality of life, and mental health and is therefore strongly recommended in the international guidelines to patients with coronary artery disease [41,42,43,44,45]. The guidelines [35,46] suggest continuous aerobic exercise for at least 20–30 min 3 days/week (preferably 45–60 min 6–7 days/week) at 50–80% of VO2max. Resistance exercise two to three times/week should be added to the aerobic exercise. It consists of 8–10 exercises at an intensity of 30–70% of the 1 repetition maximum (1RM) for upper body exercises and 40–80% of 1RM for lower body exercises, with 12–15 repetitions in at least 1 set. The first meta-analyses of exercise-based CR was carried out over 30 years ago, demonstrating 20% to 25% reductions in CVD and all-cause mortality from ten randomized controlled trials in 4347 patients [47]. More recently, the meta-analysis by Lawler et al. of 34 randomized controlled trials summarized cardiovascular outcomes in post-MI patients who performed CR. The patients randomized to CR had a lower risk of reinfarction, cardiac mortality, and all-cause mortality, regardless of the study periods, the duration of CR, or the time beyond active intervention. In addition, CR had positive consequences on cardiovascular risk factors such as smoking habits, BMI, blood pressure, and lipid profile [48].
2.4. Effect of Exercise in Prevention of HFpEF
Physical activity prevents HFpEF through two main mechanisms: firstly by (i.e., indirect effects) attenuating the negative effect of many established risk factors for HFpEF (e.g., cholesterol, obesity, insulin sensitivity) and secondly (i.e., direct effects) by exerting beneficial effects on heart structure and cardiovascular performance (e.g., cardiac remodeling and cardiopulmonary performance) [49].
It has been well established that all the risk factors described above (see Section 2.1) predispose to HFpEF. Therefore, the ability of exercise to positively impact on these risk factors indirectly determines a decreased risk of HFpEF [49]. Specifically, a recent investigation investigating the association between exercise, body mass index, and HF in a cohort of more than 50,000 patients demonstrated that, among HF subtypes, the cumulative incidence of HFpEF was significantly lower across the higher physical activities categories; on the other hand, the association between higher levels of physical exercise and the cumulative risk of HFrEF was modest and not statistically significant [50]. A possible explanation for this can be found in the results of a study involving more than 20,000 subjects, showing that, after adjustment for HF risk factors (i.e., age, blood pressure, diabetes mellitus, body mass index, smoking status, and total cholesterol), a 1-unit greater fitness level in metabolic equivalents reached in midlife was associated with a lower risk of heart failure hospitalization after the age of 65, but with only a modest effect on the risk of coronary diseases [51]. These data further support the findings of a meta-analysis that revised twelve prospective cohort studies, including more than 370,000 subjects, demonstrating a dose-dependent inverse association between physical activity and the risk of HF [52].
However, low fitness and physical inactivity also negatively impact through direct effects on the HFpEF risk [49]; specifically, it has been shown that low fitness is associated with a higher prevalence of cardiac remodeling and diastolic dysfunction [53], suggesting that exercise may lower heart failure risk through its effect on favorable cardiac remodeling and the prevention of diastolic dysfunction; as a result, inactivity is correlated with diastolic dysfunction, determining a higher risk of HFpEF [49,53].
3. Evidence of Exercise in HFpEF
The HFpEF cardinal symptom is exercise intolerance (EI), manifested by dyspnea and fatigue during exertion, in some cases so limiting it forces patients into a sedentary lifestyle, further aggravating the clinical conditions [54,55]. Different systems contribute to EI in HF patients, influencing their treatment and prognosis [13]. Symptoms of EI and dyspnea were typically attributed to diastolic dysfunction, but multiple studies identified different cardiac abnormalities, including chronotropic incompetence and altered increase in systolic output in the context of increased left ventricular stiffness [56]. Moreover, recent findings highlighted the involvement of peripheral factors (such as vascular system, endothelium, adipose tissue, and skeletal muscle) in the pathophysiology of HFpEF, contributing to a significantly impaired ventricular–arterial coupling response to exercise [57,58,59,60,61].
In the following paragraphs, the clinical evidence available in HFpEF patients regarding the effect of exercise on different endpoints—evaluated with different techniques—will be discussed.
3.1. Cardiopulmonary Exercise Test
Historically, most studies evaluated exercise intolerance (primary endpoint to assess clinical status and the effects of therapeutic interventions in patients with HFpEF) through the cardiopulmonary exercise test (CPET); this method allows the contextual assessment of ventilatory, hemodynamic, and metabolic parameters [62,63,64]. Specifically, this technique quantifies EI by measuring the reduction in the peak oxygen consumption (VO2) (VO2 peak). The VO2 peak depends on peak cardiac output (Q peak) and the arteriovenous oxygen difference ((A-V) O2) peak, conforming to the Fick principle (VO2 peak = Q peak × A-V O2 peak) [62].
Several investigators identified peak VO2 as the primary outcome for assessing the effect of exercise in HFpEF (Table 1).. Kitzman DW et al. enrolled 53 elderly patients with HFpEF (EF ≥ 50% and no significant coronary, valvular, or pulmonary disease). In this study, the patients who performed supervised exercise training (3 days per week for 16 weeks) significantly increased VO2 peak exercise by 2.7 mL/Kg/min compared to the baseline, together with power output and exercise time compared to the control group (all p < 0.001) [65]. On the other hand, there were no changes in the peak respiratory exchange ratio between the groups. Similar findings were supported by the same groups in a later investigation, in which 32 HFpEF subjects performed endurance exercise training for 16 weeks [66]; as a result, the VO2 peak, the peak power output, and the ventilatory aerobic threshold (p = 0.01) were significantly higher in an active group than in the control group. A modest increase in the VO2 peak was observed by Fujimoto N in 11 HFpEF patients after 1 year of ET [67]. In the Prospective Aerobic Reconditioning Intervention Study (PARIS) study, in which 40 stable HFpEF patients were enrolled, an increase in peak VO2 of 3 mL/Kg/min was observed after 4 months of ET; specifically, an improvement of 16% was directly due to ET (as shown by differences in peak arterial–venous oxygen differences) [68]. An increase in the VO2 peak was also observed by Maldonado-Martin S in a population of 23 older patients performing cycling and walking at 50% to 70% of peak oxygen uptake intensity for 3 days/week for 16 weeks [69]. The VO2 peak was also considered as the primary endpoint in the multicenter trial performed by Edelmann F, in which 64 HFpEF patients were enrolled and 2:1 randomized to supervised endurance/resistance training, in addition to the usual care or to the usual care alone [70]. The exercise consisted of endurance by cycling 2 times weekly for 4 weeks and of resistance 3 times weekly from 5 inward training sessions (32 sessions). The authors found an increase in the VO2 peak of 2.6 mL/kg/min in the training group compared with a slight decrease of 0.7 mL/kg/min in the control group. Similar findings were reached by Brubaker PH, who demonstrated the enhancement of physical function in patients with HFpEF after 48 sessions of endurance exercise training, with an increase in the VO2 peak [71], and by Fu TC, investigating 30 HFpEF patients with aerobic interval training for 30 min/day, 3 days/week for 12 weeks on a cycle ergometer, reaching a significant post-interventional improvement of the VO2 peak (p < 0.05) [72]. Added to these data, the combination of caloric restriction and aerobic exercise training was related to exercise capacity, with a significant increase in the VO2 peak [73]. Finally, Smart NA determined the functional capacity responses of HFpEF patients to exercise training: in the exercise group, there was an incremental change in the VO2 peak (24.6%, p = 0.02) and a reduction in the V(E)/VCO2 slope (12.7%, p = 0.02) [74].
Table 1.
Results of trials investigating the effects on peak VO2 of exercise training in HFpEF.
| Peak VO2 mL/kg/min |
ET | Ctr | |||
|---|---|---|---|---|---|
| Baseline | Final | baseline | Final | p § | |
| Kitzman 2010 [78] | 13.8 ± 2.5 | 16.1 ± 2.6 * | 12.8 ± 2.6 | 12.5 ± 3.4 | <0.001 |
| Edelmann 2011 [70] | 16.1 ± 4.9 | 18.7 ± 5.4 * | 16.7 ± 4.7 | 16.0 ± 6.0 | <0.001 |
| Smart 2012 [74] | 12.2 ± 3.6 | 15 ± 4.9 * | 14.1 ± 4.1 | 14.8 ± 4.6 | 0.06 |
| Kitzman 2013 [66] | 14.2 ± 2.8 | 15.8 ± 3.3 | 14.0 ± 3.2 | 13.8 ± 3.1 | 0.0001 |
| Maldonado-Martin 2017 [69] | 13.5 ± 2.3 | 16.0 ± 2.6 * | 12.7 ± 3.2 | 12.6 ± 3.4 | 0.01 |
| Brubaker 2020 [71] | 13.7 ± 2.8 | 15.2±6.3 * | 13.3 ± 3.0 | 13.0–14.0 | 0.001 |
| HIIT | MCT | ||||
| Baseline | final | baseline | Final | p § | |
| Angadi 2015 [75] | 19.2 ± 5.2 | 21.0 ± 5.2 * | 16.9 ± 3.0 | 16.8 ± 4.0 | d: 0.94 vs. −1.63 |
| Donelli da Silveira 2020 [76] | 16.1 ± 3.3 | 19.6 ± 3.5 * | 17.6 ± 3.5 | 19.5 ± 3.7 * | <0.001 |
| Mueller 2021 [77] | 18.9 ± 5.4 | 20.2 ± 6.0 | 18.2 ± 5.1 | 19.8 ± 2.5 | 0.002 |
ET: exercise training; Ctr: control group; HIIT: high-intensity interval training; MCT: moderate continuous training. * p < 0.05 pre-intervention vs. post-intervention in the same group; § p: post-intervention between the groups.
An additional field of interest is the investigation of the different effects of HIIT vs. moderate-intensity aerobic continuous training (MI-ACT) in HFpEF patients. Specifically, Angadi SS showed an increase in the VO2 peak by 9% after HIIT, from 19.2 ± 5.2 to 21.0 ± 5.2 mL/Kg/min, (p = 0.04), but it was unmodified after MI-ACT. The ventilation threshold, VE/VCO2 slope, peak HR, respiratory exchange ratio, VE/VCO2, and rate-pressure product were not changed in either group [75]. Similar findings were observed by Donelli da Silveira S and coworkers in a single-blinded randomized clinical trial; indeed, they found an improvement of VO2 of 22% in an HIIT group, compared with 11% with MI-ACT (p < 0.001) after a 12-week follow-up [76]. In contrast, a recent randomized controlled trial performed by Mueller et al. showed no differences in the VO2 peak between patients assigned to HIIT vs. MCT after 3 months [77].
In addition to peak VO2, other parameters (i.e., minute ventilation/carbon dioxide production (VE/VCO2) slop and ventilatory anaerobic threshold (VAT) have been investigate, as depicted in Table 2 and Table 3.
Table 2.
Results of trials investigating the effects on minute ventilation/carbon dioxide production (VE/VCO2) slope of exercise training in HFpEF.
| VE/VCO2 Slope | ET | Ctr | |||
|---|---|---|---|---|---|
| Baseline | final | baseline | Final | p § | |
| Kitzman 2010 [78] | 34 ± 6 | 35 ± 8 | 33 ± 5 | 34 ± 5 | n.s. |
| Smart 2012 [74] | 33.9 ± 3.3 | 29.6 ± 5.3 | 33.7 ± 3.0 | 33.8 ± 3.2 | n.s. |
| Kitzman 2013 [66] | 31.5 ± 4.4 | 32.2 ± 4.5 | 30.6 ± 3.6 | 30.2 ± 3.3 | n.s. |
| HIIT | MCT | ||||
| Baseline | final | baseline | final | p § | |
| Angadi 2015 [75] | 31.2 ± 11.5 | 31.6 ± 10.3 | 26.5 ± 2.4 | 26.7 ± 3.1 | n.s. |
| Donelli da Silveira2020 [76] | 39.4 ± 6.1 | 35.7 ± 4.7 | 36.8 ± 5.4 | 34.6 ± 5.1 | <0.001 |
| Mueller 2021 [77] | 34.5 ± 7.9 | 35.0 ± 9.8 | 34.2 ± 7.2 | 33.7 ± 6.8 | n.s. |
ET: exercise training; Ctr: control group; HIIT: high-intensity interval training; MCT: moderate continuous training. § p: post-intervention between the groups.
Table 3.
Results of trials investigating the effects on ventilatory anaerobic threshold (VAT) of exercise training in HFpEF.
| Ventilatory Anaerobic Threshold (VAT) | ET | Ctr | |||
|---|---|---|---|---|---|
| Baseline | final | baseline | final | p § | |
|
Kitzman 2010 [78] (mL/min) |
746 ± 149 | 822 ± 180 * | 660 ± 174 | 618 ± 126 | <0.001 |
|
Eldemann 2011 [70] (mL/min/kg) |
10.2 ± 3.0 | 12.7 ± 3.6 * | 10.3 ± 2.5 | 10.0 ± 3.2 | <0.001 |
|
Smart 2012 [74] (mL/min/kg) |
7.8 ± 1.8 | 9.8 ± 2.6 | 9.1 ± 3.8 | 9.2 ± 5.3 | n.s. |
|
Kitzman 2013 [66] (mL/min) |
699 ± 178 | 796 ± 163 * | 734 ± 189 | 702 ± 186 | 0.01 |
|
Maldonado Martin 2017 [69] (mL/min/kg) |
9.3 ± 1.5 | 10.4 ± 1.4 | 8.3 ± 1.3 | 8.3 ± 2.2 | n.s. |
|
Brubaker 2020 [71] (mL/min) |
721 ± 161 | 768.8 ± 846.2 * | 703 ± 184 | 636.5 ± 711.5 | 0.001 |
| HIIT | MCT | ||||
| Baseline | final | baseline | final | p | |
|
Angadi 2015 [75] ml/min/kg |
12.2 ± 4.0 | 13.1 ± 3.5 | 11.1 ± 2.1 | 11.7 ± 2.4 | n.s. |
ET: exercise training; Ctr: control group; HIIT: high-intensity interval training; MCT: moderate continuous training. * p < 0.05 pre-intervention vs. post-intervention in the same group; § p: post-intervention between the groups.
3.2. 6MWT
The effects of training programs on exercise tolerance have also been evaluated by performing the 6MWT in multiple RCTs (Table 4). The walking distance increased after exercise training [69,70,71,78], but no differences were observed when comparing the MCT or HIIT [75].
Table 4.
Results of trials investigating the effects on 6-minute walking distance of exercise training in HFpEF.
| 6MWT Distance (m) | ET | Ctr | |||
|---|---|---|---|---|---|
| baseline | final | baseline | final | p § | |
| Kitzman 2010 [78] | 1494 ± 224 | 1659 ± 173 * | 1412 ± 382 | 1460 ± 411 | 0.002 |
| Edelmann 2011 [70] | 545 ± 86 | 569 ± 88 * | 551 ± 86 | 568 ± 80 | 0.63 |
| Kitzman 2013 [66] | 447 ± 107 | 486 ± 89 | 438 ± 79 | 448 ± 70 | 0.009 |
| Maldonado-Martin 2017 [69] | 455 ± 68 | 506 ± 53 * | 402 ± 142 | 430 ± 125 * | 0.028 |
| Brubaker 2020 [71] | 445 ± 88 | 474.5–504.1 * | 425 ± 117 | 434.4 ± 462.9 | <0.001 |
* p < 0.05 pre-intervention vs. post-intervention in the same group; § p: post-intervention between the groups. ET: exercise training; Ctr: control group.
3.3. Echocardiography
Exercise-induced changes in diastolic function were widely investigated, with discordant evidence: on the one hand, some studies described no alterations in diastolic function, as assessed by the E/e’ medial, e’ medial, left atrial volume index; on the other hand, aerobic interval training reduced E/e’ E’ in HFpEF RCTs [67,68,72]. Alves et al. 2012 have shown in 31 HFpEF patients that exercise training 3 times/week for 6 months improves diastolic disfunction, with an increase in the E/A ratio and a decrease in the E-wave DT [79]. Similarly, Fu at al. reported a decrease in the E/e’ ratio with an enhancement of diastolic function after 12 weeks of aerobic interval training [72]. Moreover, the diastolic dysfunction grade was reduced after 4 weeks—HIIT (4 × 4 min at 85–90% peak heart rate, with a 3 min active recovery) in the study of Angadi [75], as well as in Donelli da Silveira, where the value of E/e’ decreased significantly in MCT and HIIT [76]. In contrast, Mueller analyzed diastolic function in HIIT, M-ACT, and a control group after 12 months and observed no significant differences among the groups [77]. Notably, no studies reported changes in the cardiac chamber dimensions. With regard to systolic function, in trials performed by Smart [74] and Kitzman [78] no significant changes were detected.
Table 5 depicts results of exercise training on echocardiographic parameters.
Table 5.
Results of trials investigating the effects on echocardiographic parameters of exercise training in HFpEF.
| ECHOCARDIOGRAPHY | ET | Ctr | |||
|---|---|---|---|---|---|
| Baseline | final | baseline | final | p § | |
| Kitzman 2010 [78] | |||||
| EF (%) | 61 ± 5 | 57 ± 8 | 60 ± 10 | 55 ± 8 | ns |
| E/A | 0.90 ± 0.24 | 1.02 ± 0.28 | 1.02 ± 0.38 | 1.12 ± 0.36 | ns |
| DT | 220 ± 55 | 230 ± 40 | 227 ± 52 | 221 ± 52 | ns |
| Edelmann 2011 [70] | |||||
| EF (%) | 67 ± 7 | 66 ± 6 | 66 ± 7 | 67 ± 8 | ns |
| E/e’ | 12.8 ± 3.2 | 10.5 ± 2.5 * | 13.5 ± 4.6 | 14.1 ± 3.9 | 0.01 |
| LAVi mL/m2 | 27.9 ± 7.6 | 24.3 ± 6.5 * | 28.2 ± 8.8 | 28.6 ± 9.2 | 0.01 |
| Smart 2012 [74] | |||||
| EF (%) | 58 ± 13.2 | 61.3 ± 9.5 | 56.7 ±7.7 | 58.7 ±6.4 | ns |
| E/A | 0.87 ± 0.13 | 0.82 ± 0.17 | 0.94 ± 0.39 | 0.82 ± 0.22 | ns |
| DT | 276 ± 50 | 281 ± 54 | 245 ± 44 | 248 ± 36 | ns |
| E/e’ | 20.7 ± 12.8 | 25.1 ± 24 | 15.9 ± 6.8 | 15.9 ± 5.5 | ns |
| Alves 2012 [79] | |||||
| EF (%) | 56.4 | 57.7 * | 55.9 | 55.4 | 0.01 |
| E/A | 0.93 | 1.05 * | 1.01 | 1.04 | 0.01 |
| DT (sec) | 236.7 | 222.7 * | 216.9 | 214.8 | 0.01 |
| EDd (mm) | 51.5 | 51 | 51.7 | 51.9 | ns |
| ESd (mm) | 30.4 | 29.6 | 30.9 | 31.3 | ns |
| Fu 2016 [72] | |||||
| EF (%) | 57.6 ± 1.9 | 57.8 ± 1.7 | 56.5 ± 2.2 | 54.4 ± 3.3 | ns |
| E/A | 1.1 ± 0.2 | 0.9 ± 0.1 | 1.0 ± 0.3 | 0.8 ± 0.2 | ns |
| E/e’ | 21.0 ± 2.2 | 16.1 ± 1.8* | 19.2 ±1.5 | 17.8 ± 1.9 | ns |
| HIIT | MCT | ||||
| Angadi 2015 [75] | |||||
| EF (%) | 65 ± 5 | 63 ± 6 | 66 ± 4 | 61 ± 5 | ns |
| E/A | 1.3 ± 0.5 | 1.2 ± 0.5 | 1.2 ± 0.6 | 1.6 ± 1.1 | ns |
| DT | 194 ± 55 | 225 ± 40 * | 199 ± 71 | 220 ± 43 | ns |
| E/e’ | 14.6 ± 5.6 | 12.7 ± 4.7 | 17.7 ± 6.3 | 16.7 ± 5.2 | ns |
| LAVi (mL/m2) | 35.8 ± 3.0 | 32.4 ± 7.2 | 40.5 ± 9.3 | 46.3 ± 18.1 | ns |
| Donelli da Silveira 2020 [79] | |||||
| EF (%) | 65 ± 5 | 66 ± 4 | 65 ± 5 | 65 ± 5 | ns |
| E/A | 0.99 ± 0.2 | 0.91 0.2 | 1.05 ± 0.3 | 1.08 ± 0.3 | ns |
| DT | 233 ± 33 | 222 ± 27 | 214 ± 33 | 209 ± 37 | ns |
| E/e’ | 14.2 ± 4 | 11.6 ± 3 * | 13.3 ± 3 | 11.1 ± 2 * | ns |
| Mueller 2021 [77] | |||||
| E/e’ | 15.8 ± 3.7 | 14.2 ± 3.9 | 15.9 ± 4.1 | 15.6 ± 4.4 | ns |
| LAVi mL/m2 | 35.4 ± 9.0 | 37.4 ± 10.9 | 37.9 ± 13.0 | 36.6 ± 9.2 | ns |
ET: exercise training; Ctr: control group; EF: ejection fraction; E: mitral peak early wave velocity; A: mitral peak atrial/late wave velocity; LAVi: left atrial volume indexed; DT: deceleration time; e’: early diastolic mitral annular tissue velocity; EDd: end-diastolic diameter; ESd: end-systolic diameter. * p < 0.05 pre-intervention vs. post-intervention in the same group; § p: post-intervention between the groups.
3.4. Circulating Biomarkers
In addition to diastolic dysfunction, the detection of elevated natriuretic peptide levels is crucial in the diagnosis of HFpEF [80,81]. No study reported a significant reduction in BNP or pro-BNP after programs of exercise training for HFpEF patients when compared to the controls. However, Donelli da Silveira et al. demonstrated a reduction in both groups in NT pro-BNP levels when HIIT and MCT were compared [76].
3.5. Quality of Life and Symptoms
Breathlessness and fatigue largely limit the quality of life of HFpEF patients. Exercise intolerance affects daily physical activities and impairs the mental and social quality of life. On this point, exercise training demonstrated the improvement of the quality of life, as assessed by using the Minnesota Living with Heart Failure Questionnaire (MLWHFQ) [66,70,71,72,78,82,83] and the Short Form Health Survey 36 (SF-36) [70,72,78,82], with an effect on the physical, emotional, and vitality domains [66,71].
According to the effect in QoL of different types of exercise training, Donelli da Silveira did not reveal significant differences of HIIT versus MI-ACT [76], while the recent trial by Mueller showed an improvement in the QoL domains in the MCT group compared with the controls, without significant differences between high-intensity interval training and the controls or high-intensity interval training and moderate continuous training [77].
3.6. Autonomic Dysfunction
HFpEF is also associated with autonomic dysfunction, manifesting as sympatho—vagal imbalance, which may result in alterations of heart rate variability (HRV). In this regard, Murad observed an improvement of the standard deviation of all normal RR intervals and of the root mean square of successive differences in normal RR intervals in older HFpEF patients performing 16 weeks of supervised training [84].
3.7. Brachial Artery Flow-Mediated Dilation (FMD)
Among the possible contributors to exercise intolerance in HFpEF patients, endothelial dysfunction and arterial stiffness seem to play a marginal role [67]- Table 6; even if it has been shown that HFpEF patients displayed typical arterial stiffness profiles (evaluated with the arterial velocity pulse index, AVI, and the arterial pressure volume index, API, at rest) when compared to HFrEF, with a significant negative correlation with peak VO2 [85], no changes in brachial artery flow-mediated dilation (FMD) were detected after exercise training in both the HIIT group and the MCT group [66,75]. These findings could be partially justified by the short training duration or the absence of endothelial damage. In addition, it is possible that the training exercise does not affect the vasodilatory function in HFpEF.
Table 6.
Results of trials investigating the effects on brachial artery flow-mediated dilation of exercise training in HFpEF.
| Brachial ArteryFlow-Mediated Dilation (%) | ET | Ctr | |||
|---|---|---|---|---|---|
| baseline | final | baseline | Final | p § | |
| Kitzman 2013 [66] | 4.0 ± 2.0 | 3.8 ± 3.0 | 4.7 ± 3.5 | 4.3 ± 3.5 | ns |
| HIIT | MCT | ||||
| baseline | final | baseline | Final | ||
| Angadi 2015 [75] | 6.9 ± 3.7 | 7.0 ± 4.2 | 8.1 ± 4.1 | 3.4 ± 3.6 | ns |
§p: post-intervention between the groups; ET: exercise training; Ctr: control group.
4. Clinical Impact and Future Perspectives
To date, the treatment of HFpEF is still a challenge for clinicians, and among the RCTs conducted on HFpEF patients, only a few have recently achieved the primary endpoints [86]. In this scenario, the scientific community focused on studying the role of physical activity in increasing exercise tolerance in HFpEF patients. Taken together, the analysis of these studies underlines two important findings: (1) exercise training programs improve the cardiorespiratory function of HFpEF patients, in terms of increase in peak oxygen uptake, the 6 min walk test distance, and the ventilatory threshold, as summarized in Table 1. As a result, it is essential to encourage adequate physical activity in these patients. (2) The diastolic or systolic functions are generally unchanged or only partially modified by the exercise, suggesting that multiple mechanisms contribute to the improvement of exercise tolerance in HFpEF patients. These mechanisms remain unclear, but some authors have suggested that the improvement in the VO2 peak after a structured exercise training in HFpEF patients is the expression of complex peripheral adaptation mechanisms and the consequent increase in oxygen extraction by skeletal muscle [66,87]. As a prototype, after 16 weeks of aerobic interval training, improvements in the VO2 peak were associated with a higher estimated peak arterial–venous oxygen difference and peak heart rate.
These findings reflect the multiple pathophysiological mechanisms determining the reduced exercise and functional capacity in HFpEF patients: cardiac impairment (chronotropic incompetence, reduction in left heart reserve capacity, and elevated filling pressures), vascular dysfunction, pulmonary impairment, and muscle diseases [13].
According to the literature, several studies explored different methods of training; notably, the studies are heterogenous for type, frequency, and intensity of training, including aerobic endurance exercise and resistance training, treadmill, walking, and bicycling. When compared, they did not show a clear superiority of one type over another. However, based on the data available in the literature, in stable HFpEF patients, the guidelines suggest initiating exercise training programs in supervised modalities [1,35,88]. The patients should perform continuous moderate-intensity endurance exercises, lasting from 20 to 60 minutes per session, 3 to 5 days per week, via cycling or treadmill modalities. The time and the frequency should be raised up before the intensity is increased. Once patients demonstrate tolerance for aerobic training levels, resistance training may be initiated.
Further investigations are needed to fully elucidate the pathophysiological mechanisms underpinning the shown beneficial effects of exercise in HFpEF. In addition, the proper role for different types of exercise is not yet understood, nor is the optimal time for exercise training in HFpEF. Moreover, there is a lack of data about long-term adherence and the combination of exercise with other behavioral and lifestyle interventions (e.g., nutrition). Finally, robust studies with a long follow-up are needed to demonstrate the role of exercise training in strong outcomes (i.e., mortality) in HFpEF patients.
Table 7 summarizes the clinical studies investigating the role of exercise training in HFpEF so far.
Table 7.
List of studies investigating the role of exercise training in patients with preserved ejection fraction.
| First Author; Year of Publication (Ref.) | Study Design; Duration (wk) | Type of Exercise | Patient; Age; Women (%) | Principal Outcomes Investigated and Main Findings |
|---|---|---|---|---|
| Kitzman2010 [78] | Randomized, prospective, attention-controlled, single-blind study 16 wk |
1 h ET (warm-up, stimulus, and cool-down phases), 3 times/wk | ET UC |
|
| N = 26 N = 27 | ||||
| 70 ± 6 y 69 ± 5 y | ||||
| 83% 91% | ||||
| Edelmann2011 [70] | Prospective, randomized 2:1 controlled trial 12 wk |
Endurance/resistance training | ET UC |
|
| N = 44 N = 20 | ||||
| 64± 8 y 65 ± 6 y | ||||
| 55% 60% | ||||
| Smart2012 [74] | Randomized, controlled trial 16 wk |
Cycle ergometer exercise training at 60 rpm | ET UC |
|
| N = 12 N = 13 | ||||
| 67 ± 5.8 y 61.9 ± 6.9 y | ||||
| 42% 53% | ||||
| Murad2012 [84] | Randomized, controlled, single-blinded design 16 wk |
1 h ET (warm-up, stimulus, and cool-down phases), 3 times/wk | ET UC |
|
| N = 35 N = 31 | ||||
| 70.1 ± 5.6 y 68.0 ± 4.8 y | ||||
| 63% 64.5% | ||||
| Alves2012 [79] | Randomized controlled trial 24 wk |
Interval training | ET UC |
|
| N = 20 N = 11 | ||||
| Overall | ||||
| 63 ± 11 y | ||||
| 29% | ||||
| Haykowsky2012 [68] | Randomized, single-blind trial 16 wk |
Endurance exercise training | ET UC |
|
| N = 22 N = 18 | ||||
| 70 ± 6 y 68 ± 5 y | ||||
| 82 % 94% | ||||
| Fujimoto2012 [67] | Randomized controlled trial 54 wk |
Endurance exercise training | ET UC |
|
| N = 7 N = 13 | ||||
| 74.9 ± 6 y 70.2 ± 4 y | ||||
| 57% 38% | ||||
| Kitzman2013 [66] | Randomized, controlled, single-blind trial 16 wk |
Walking, arm, and leg ergometry | ET UC |
|
| N = 32 N = 31 | ||||
| 70 ± 7 y 70 ± 7 y | ||||
| 72% 80% | ||||
| Angadi2015 [75] | Randomized comparison trial/pilot study 4 wk |
HIIT vs. MI-ACT | HIIT MCT |
|
| N = 9 N = 6 | ||||
| 69.0 ± 6.1 y 71.5 ± 11.7 y | ||||
| 11% 33% | ||||
| Nolte2015 [83] | Prospective, randomized, controlled trial 12 wk |
Endurance/resistance training | ET UC |
|
| N = 44 N = 20 | ||||
| overall | ||||
| 65 ± 7 y | ||||
| 56% | ||||
| Kitzman2016 [73] | Randomized, attention- controlled, 2 × 2 factorial trail 20 wk |
Walking exercise 3 times/wk | ET Diet group |
|
| N = 26 N = 24 | ||||
| ET + Diet group UC | ||||
| N = 25 N = 25 | ||||
| Overall | ||||
| 67 ± 5 y | ||||
| 81% | ||||
| Fu2016 [72] | Randomized, controlled trial 12 wk |
Aerobic interval training | ET UC |
|
| N = 30 N = 30 | ||||
| 60.5 ± 2.7 y 63.1 ± 2.6 y | ||||
| 33% 40% | ||||
| Maldonado-Martin2017 [69] | Prospective, randomized, single-blinded trial 16 wk |
Cycling and walking at 50% to 70% of VO2 peak intensity | ET UC |
|
| N = 23 N = 24 | ||||
| >65 y | ||||
| 87% | ||||
| Lang2018 [83] | Randomized controlled trial 12 wk |
Home-based comprehensive self-management rehabilitation program | ET UC |
|
| N = 25 N = 25 | ||||
| 71.8 ± 9.9 y 76 ± 6.6 y | ||||
| 64% 44% | ||||
| Donelli da Silveira2020 [76] | Single-blinded, parallel randomized clinical trial 3 d per wk 12 wk |
HIIT vs. MCT | HIIT MCT |
|
| N = 10 N = 9 | ||||
| 60 ± 10 y 60 ± 9 y | ||||
| 70% 56% | ||||
| Brubaker2020 [71] | Randomized controlled trial 16 wk | ≤60 min of moderate-intensity endurance exercise training 3 time/wk | ET UC |
|
| N = 58 N = 58 | ||||
| 70.3 ± 6.7 69.2 ± 6.2 | ||||
| 76% 86% | ||||
| Mueller2021 [77] | Randomized controlled trial 3 mo supervised followed by 9 mo of telemedical monitored home-based training | HIIT vs. MCT vs. UC | HIIT MCT UC |
|
| N = 58 N = 58 N = 60 | ||||
| 70 ± 7 y 70 ± 8 y 69 ±10 y | ||||
| 71% 60% 68% |
Abbreviations: ET, exercise training; wk, weeks; CPET: cardiopulmonary exercise test; 6MWT: 6 min walking test; FMD, flow-mediated dilation; HIIT, high-intensity interval training; IMT, inspiratory muscle training; MET, metabolic equivalent task; MCT: moderate continuous training; MI-ACT, moderate-intensity aerobic continuous training; QoL, quality of life; RMSSD, root mean square of successive differences in normal RR intervals; SDNN, standard deviation of all normal RR intervals; UC, usual care. The blue arrows indicate an improvement after exercise of the variable explored
5. Conclusions
There is an intimate link between exercise and HFpEF, with the inability to perform physical activity being of the principal features impacting of the quality of life and outcome of HFpEF patients, in the presence of symptoms such as fatigue or dyspnea (i.e., exercise intolerance). Considering that exercise training programs are able to improve the cardiorespiratory function of HFpEF patients through multiple mechanisms, even if no role has demonstrated an amelioration in the prognosis, the prescription of exercise training programs in supervised modalities, to improve symptoms, quality of life, and exercise tolerance, should be recommended for stable HFpEF patients.
Acknowledgments
Not applicable.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Dr Valentina Capone receives a research grant support from CardioPath, Department of Advanced Biomedical Sciences, Federico II University, Naples, Italy.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McDonagh T.A., Metra M., Adamo M., Gardner R.S., Baumbach A., Böhm M., Burri H., Butler J., Čelutkienė J., Chioncel O., et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2022;24:4–131. doi: 10.1002/ejhf.2333. [DOI] [PubMed] [Google Scholar]
- 2.Bozkurt B., Coats A.J.S., Tsutsui H., Abdelhamid C.M., Adamopoulos S., Albert N., Anker S.D., Atherton J., Böhm M., Butler J., et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021;23:352–380. doi: 10.1002/ejhf.2115. [DOI] [PubMed] [Google Scholar]
- 3.Dunlay S.M., Roger V.L., Redfield M.M. Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2017;14:591–602. doi: 10.1038/nrcardio.2017.65. [DOI] [PubMed] [Google Scholar]
- 4.Groenewegen A., Rutten F.H., Mosterd A., Hoes A.W. Epidemiology of heart failure. Eur. J. Heart Fail. 2020;22:1342–1356. doi: 10.1002/ejhf.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho D.H., Yoo B.S. Current Prevalence, Incidence, and Outcomes of Heart Failure with Preserved Ejection Fraction. Heart Fail. Clin. 2021;17:315–326. doi: 10.1016/j.hfc.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Arcopinto M., Schiavo A., Salzano A., Bossone E., D’Assante R., Marsico F., Demelo-Rodriguez P., Baliga R.R., Cittadini A., Marra A.M. Metabolic Syndrome in Heart Failure: Friend or Foe? Heart Fail. Clin. 2019;15:349–358. doi: 10.1016/j.hfc.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Cittadini A., Salzano A., Iacoviello M., Triggiani M., Rengo G., Cacciatore F., Maiello C., Limongelli G., Masarone D., Perticone F., et al. Mutliple hormonal and metabolic deficiency syndrome predicts outcome in heart failure: The T.O.S.CA. Registry. Eur. J. Prev. Cardiol. 2021;28:1691–1700. doi: 10.1093/eurjpc/zwab020. [DOI] [PubMed] [Google Scholar]
- 8.Streng K.W., Nauta J.F., Hillege H.L., Anker S.D., Cleland J.G., Dickstein K., Filippatos G., Lang C.C., Metra M., Ng L.L., et al. Non-cardiac comorbidities in heart failure with reduced, mid-range and preserved ejection fraction. Int. J. Cardiol. 2018;271:132–139. doi: 10.1016/j.ijcard.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Salzano A., Israr M.Z., Yazaki Y., Heaney L.M., Kanagala P., Singh A., Arnold J.R., Gulsin G.S., Squire I.B., McCann G.P., et al. Combined use of trimethylamine N-oxide with BNP for risk stratification in heart failure with preserved ejection fraction: Findings from the DIAMONDHFpEF study. Eur. J. Prev. Cardiol. 2019;27:2159–2162. doi: 10.1177/2047487319870355. [DOI] [PubMed] [Google Scholar]
- 10.Salzano A., Marra A.M., Ferrara F., Arcopinto M., Bobbio E., Valente P., Polizzi R., De Vincentiis C., Matarazzo M., Saldamarco L., et al. Multiple hormone deficiency syndrome in heart failure with preserved ejection fraction. Int. J. Cardiol. 2016;225:1–3. doi: 10.1016/j.ijcard.2016.09.085. [DOI] [PubMed] [Google Scholar]
- 11.Salzano A., D’Assante R., Iacoviello M., Triggiani V., Rengo G., Cacciatore F., Maiello C., Limongelli G., Masarone D., Sciacqua A., et al. Progressive right ventricular dysfunction and exercise impairment in patients with heart failure and diabetes mellitus: Insights from the T.O.S.CA. Registry. Cardiovasc. Diabetol. 2022;21:108. doi: 10.1186/s12933-022-01543-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pieske B., Tschope C., de Boer R.A., Fraser A.G., Anker S.D., Donal E., Edelmann F., Fu M., Guazzi M., Lam C.S.P., et al. How to diagnose heart failure with preserved ejection fraction: The HFA-PEFF diagnostic algorithm: A consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) Eur. Heart J. 2019;40:3297–3317. doi: 10.1093/eurheartj/ehz641. [DOI] [PubMed] [Google Scholar]
- 13.Salzano A., De Luca M., Israr M.Z., Crisci G., Eltayeb M., Debiec R., Ranieri B., D’Assante R., Rega S., D’Agostino A., et al. Exercise Intolerance in Heart Failure with Preserved Ejection Fraction. Heart Fail. Clin. 2021;17:397–413. doi: 10.1016/j.hfc.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Nocon M., Hiemann T., Mueller-Riemenschneider F., Thalau F., Roll S., Willich S.N. Association of physical activity with all-cause and cardiovascular mortality: A systematic review and meta-analysis. Eur. J. Cardiovasc. Prev. Rehabil. 2008;15:239–246. doi: 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- 15.Tikkanen E., Gustafsson S., Ingelsson E. Associations of Fitness, Physical Activity, Strength, and Genetic Risk With Cardiovascular Disease Longitudinal Analyses in the UK Biobank Study. Circulation. 2018;137:2583–2591. doi: 10.1161/CIRCULATIONAHA.117.032432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vanhees L., De Sutter J., Geladas N., Doyle F., Prescott E., Cornelissen V., Kouidi E., Dugmore D., Vanuzzo D., Borjesson M., et al. Importance of characteristics and modalities of physical activity and exercise in defining the benefits to cardiovascular health within the general population: Recommendations from the EACPR (Part I) Eur. J. Prev. Cardiol. 2012;19:670–686. doi: 10.1177/2047487312437059. [DOI] [PubMed] [Google Scholar]
- 17.Giannuzzi P., Mezzani A., Saner H., Björnstad H., Fioretti P., Mendes M., Cohen-Solal A., Dugmore L., Hambrecht R., Hellemans I., et al. Physical activity for primary and secondary prevention. Position paper of the Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology. Eur. J. Cardiovasc. Prev. Rehabil. 2003;10:319–327. doi: 10.1097/01.hjr.0000086303.28200.50. [DOI] [PubMed] [Google Scholar]
- 18.Fiuza-Luces C., Santos-Lozano A., Joyner M., Carrera-Bastos P., Picazo O., Zugaza J.L., Izquierdo M., Ruilope L.M., Lucia A. Exercise benefits in cardiovascular disease: Beyond attenuation of traditional risk factors. Nat. Rev. Cardiol. 2018;15:731–743. doi: 10.1038/s41569-018-0065-1. [DOI] [PubMed] [Google Scholar]
- 19.Shaw K., Gennat H., O’Rourke P., Del Mar C. Exercise for overweight or obesity. Cochrane Database Syst. Rev. 2006;2006:CD003817. doi: 10.1002/14651858.CD003817.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zomer E., Gurusamy K., Leach R., Trimmer C., Lobstein T., Morris S., James W.P.T., Finer N. Interventions that cause weight loss and the impact on cardiovascular risk factors: A systematic review and meta-analysis. Obes. Rev. 2016;17:1001–1011. doi: 10.1111/obr.12433. [DOI] [PubMed] [Google Scholar]
- 21.Kraus W.E., Houmard J.A., Duscha B.D., Knetzger K.J., Wharton M.B., McCartney J.S., Bales C.W., Henes S., Samsa G.P., Otvos J.D., et al. Effects of the amount and intensity of exercise on plasma lipoproteins. N. Engl. J. Med. 2002;347:1483–1492. doi: 10.1056/NEJMoa020194. [DOI] [PubMed] [Google Scholar]
- 22.Henson J., Edwardson C.L., Davies M.J., Gill J.M.R., Heaney L.M., Khunti K., Ng L., Sattar N., Zaccardi F., Yates T. Physical activity and lipidomics in a population at high risk of type 2 diabetes mellitus. J. Sports Sci. 2020;38:1150–1160. doi: 10.1080/02640414.2020.1744836. [DOI] [PubMed] [Google Scholar]
- 23.de Barcelos G.T., Heberle I., Coneglian J.C., Vieira B.A., Delevatti R.S., Gerage A.M. Effects of Aerobic Training Progression on Blood Pressure in Individuals With Hypertension: A Systematic Review With Meta-Analysis and Meta-Regression. Front. Sports Act. Living. 2022;4:719063. doi: 10.3389/fspor.2022.719063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carpes L., Costa R., Schaarschmidt B., Reichert T., Ferrari R. High-intensity interval training reduces blood pressure in older adults: A systematic review and meta-analysis. Exp. Gerontol. 2022;158:111657. doi: 10.1016/j.exger.2021.111657. [DOI] [PubMed] [Google Scholar]
- 25.Dassanayake S., Sole G., Wilkins G., Gray E., Skinner M. Effectiveness of Physical Activity and Exercise on Ambulatory Blood Pressure in Adults with Resistant Hypertension: A Systematic Review and Meta-Analysis. High Blood Press. Cardiovasc. Prev. 2022;29:275–286. doi: 10.1007/s40292-022-00517-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Umpierre D., Ribeiro P.A.B., Kramer C.K., Leitao C.B., Zucatti A.T.N., Azevedo M.J., Gross J.L., Ribeiro J.P., Schaan B.D. Physical Activity Advice Only or Structured Exercise Training and Association With HbA(1c) Levels in Type 2 Diabetes A Systematic Review and Meta-analysis. JAMA J. Am. Med. Assoc. 2011;305:1790–1799. doi: 10.1001/jama.2011.576. [DOI] [PubMed] [Google Scholar]
- 27.Inzucchi S.E., Bergenstal R.M., Buse J.B., Diamant M., Ferrannini E., Nauck M., Peters A.L., Tsapas A., Wender R., Matthews D.R. Management of hyperglycaemia in type 2 diabetes, 2015: A patient-centred approach. Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2015;58:429–442. doi: 10.1007/s00125-014-3460-0. [DOI] [PubMed] [Google Scholar]
- 28.Heaps C.L., Robles J.C., Sarin V., Mattox M.L., Parker J.L. Exercise Training-Induced Adaptations in Mediators of Sustained Endothelium-Dependent Coronary Artery Relaxation in a Porcine Model of Ischemic Heart Disease. Microcirculation. 2014;21:388–400. doi: 10.1111/micc.12116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ashor A.W., Lara J., Siervo M., Celis-Morales C., Oggioni C., Jakovljevic D.G., Mathers J.C. Exercise Modalities and Endothelial Function: A Systematic Review and Dose-Response Meta-Analysis of Randomized Controlled Trials. Sports Med. 2015;45:279–296. doi: 10.1007/s40279-014-0272-9. [DOI] [PubMed] [Google Scholar]
- 30.Haskell W.L., Sims C., Myll J., Bortz W.M., Stgoar F.G., Alderman E.L. Coronary-Artery Size And Dilating Capacity In Ultradistance Runners. Circulation. 1993;87:1076–1082. doi: 10.1161/01.CIR.87.4.1076. [DOI] [PubMed] [Google Scholar]
- 31.Green D.J., Hopman M.T.E., Padilla J., Laughlin M.H., Thijssen D.H.J. Vascular Adaptation To Exercise In Humans: Role Of Hemodynamic Stimuli. Physiol. Rev. 2017;97:495–528. doi: 10.1152/physrev.00014.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shimada K., Mikami Y., Murayama T., Yokode M., Fujita M., Kita T., Kishimoto C. Atherosclerotic plaques induced by marble-burying behavior are stabilized by exercise training in experimental atherosclerosis. Int. J. Cardiol. 2011;151:284–289. doi: 10.1016/j.ijcard.2010.05.057. [DOI] [PubMed] [Google Scholar]
- 33.Oliveira N.L., Ribeiro F., Alves A.J., Teixeira M., Miranda F., Oliveira J. Heart rate variability in myocardial infarction patients: Effects of exercise training. Rev. Port. De Cardiol. 2013;32:687–700. doi: 10.1016/j.repc.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 34.Lavie C.J., Arena R., Swift D.L., Johannsen N.M., Sui X., Lee D.-C., Earnest C.P., Church T.S., O’Keefe J.H., Milani R.V., et al. Exercise and the cardiovascular system: Clinical science and cardiovascular outcomes. Circ Res. 2015;117:207–219. doi: 10.1161/CIRCRESAHA.117.305205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ambrosetti M., Abreu A., Corra U., Davos C.H., Hansen D., Frederix I., Iliou M.C., Pedretti R.F.E., Schmid J.P., Vigorito C., et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021;28:460–495. doi: 10.1177/2047487320913379. [DOI] [PubMed] [Google Scholar]
- 36.Fletcher G.F., Landolfo C., Niebauer J., Ozemek C., Arena R., Lavie C.J. Promoting Physical Activity and Exercise JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018;72:1622–1639. doi: 10.1016/j.jacc.2018.08.2141. [DOI] [PubMed] [Google Scholar]
- 37.Soares-Miranda L., Siscovick D.S., Psaty B.M., Longstreth W.T., Mozaffarian D. Physical Activity and Risk of Coronary Heart Disease and Stroke in Older Adults The Cardiovascular Health Study. Circulation. 2016;133:147–155. doi: 10.1161/CIRCULATIONAHA.115.018323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manson J.E., Greenland P., LaCroix A.Z., Stefanick M.L., Mouton C.P., Oberman A., Perri M.G., Sheps D.S., Pettinger M.B., Siscovick D.S. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N. Engl. J. Med. 2002;347:716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 39.Wagner A., Simon C., Evans A., Ferrieres J., Montaye M., Ducimetiere P., Arveiler D., Grp P.S. Physical activity and coronary event incidence in Northern Ireland and France—The Prospective Epidemiological Study of Myocardial Infarction (PRIME) Circulation. 2002;105:2247–2252. doi: 10.1161/01.CIR.0000016345.58696.4F. [DOI] [PubMed] [Google Scholar]
- 40.Florido R., Kwak L., Lazo M., Nambi V., Ahmed H.M., Hegde S.M., Gerstenblith G., Blumenthal R.S., Ballantyne C.M., Selvin E., et al. Six-Year Changes in Physical Activity and the Risk of Incident Heart Failure ARIC Study. Circulation. 2018;137:2142–2151. doi: 10.1161/CIRCULATIONAHA.117.030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pelliccia A., Sharma S., Gati S., Back M., Borjesson M., Caselli S., Collet J.P., Corrado D., Drezner J.A., Halle M., et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021;42:17–96. doi: 10.1093/eurheartj/ehaa605. [DOI] [PubMed] [Google Scholar]
- 42.Piepoli M.F., Hoes A.W., Agewall S., Albus C., Brotons C., Catapano A.L., Cooney M.T., Corra U., Cosyns B., Deaton C., et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2016;37:2315–2381. doi: 10.1093/eurheartj/ehw106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H., Caforio A.L.P., Crea F., Goudevenos J.A., Halvorsen S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 44.Collet J.P., Thiele H., Barbato E., Barthelemy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021;42:1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 45.Knuuti J., Wijns W., Saraste A., Capodanno D., Barbato E., Funck-Brentano C., Prescott E., Storey R.F., Deaton C., Cuisset T., et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC) Eur. Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 46.Piepoli M.F., Abreu A., Albus C., Ambrosetti M., Brotons C., Catapano A.L., Corra U., Cosyns B., Deaton C., Graham I., et al. Update on cardiovascular prevention in clinical practice: A position paper of the European Association of Preventive Cardiology of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2020;27:181–205. doi: 10.1177/2047487319893035. [DOI] [PubMed] [Google Scholar]
- 47.Oldridge N.B., Guyatt G.H., Fischer M.E., Rimm A.A. Cardiac Rehabilitation After Myocardial-Infarction—Combined Experience Of Randomized Clinical-Trials. JAMA J. Am. Med. Assoc. 1988;260:945–950. doi: 10.1001/jama.1988.03410070073031. [DOI] [PubMed] [Google Scholar]
- 48.Lawler P.R., Filion K.B., Eisenberg M.J. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Am. Heart J. 2011;162:571–584. doi: 10.1016/j.ahj.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 49.Kondamudi N., Haykowsky M., Forman D.E., Berry J.D., Pandey A. Exercise Training for Prevention and Treatment of Heart Failure. Prog. Cardiovasc. Dis. 2017;60:115–120. doi: 10.1016/j.pcad.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 50.Pandey A., LaMonte M., Klein L., Ayers C., Psaty B.M., Eaton C.B., Allen N.B., de Lemos J.A., Carnethon M., Greenland P., et al. Relationship Between Physical Activity, Body Mass Index, and Risk of Heart Failure. J. Am. Coll. Cardiol. 2017;69:1129–1142. doi: 10.1016/j.jacc.2016.11.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berry J.D., Pandey A., Gao A., Leonard D., Farzaneh-Far R., Ayers C., DeFina L., Willis B. Physical fitness and risk for heart failure and coronary artery disease. Circ. Heart Fail. 2013;6:627–634. doi: 10.1161/CIRCHEARTFAILURE.112.000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pandey A., Garg S., Khunger M., Darden D., Ayers C., Kumbhani D.J., Mayo H.G., de Lemos J.A., Berry J.D. Dose-Response Relationship Between Physical Activity and Risk of Heart Failure: A Meta-Analysis. Circulation. 2015;132:1786–1794. doi: 10.1161/CIRCULATIONAHA.115.015853. [DOI] [PubMed] [Google Scholar]
- 53.Brinker S.K., Pandey A., Ayers C.R., Barlow C.E., DeFina L.F., Willis B.L., Radford N.B., Farzaneh-Far R., de Lemos J.A., Drazner M.H., et al. Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function: The Cooper Center Longitudinal Study. JACC Heart Fail. 2014;2:238–246. doi: 10.1016/j.jchf.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pandey A., Shah S.J.J., Butler J., Kellogg D.L., Lewis G.D., Forman D.E., Mentz R.J., Borlaug B.A., Simon M.A., Chirinos J.A., et al. Exercise Intolerance in Older Adults With Heart Failure With Preserved Ejection Fraction JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020;78:1166–1187. doi: 10.1016/j.jacc.2021.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Del Buono M.G., Arena R., Borlaug B.A., Carbone S., Canada J.M., Kirkman D.L., Garten R., Rodriguez-Miguelez P., Guazzi M., Lavie C.J., et al. Exercise Intolerance in Patients With Heart Failure. J. Am. Coll. Cardiol. 2019;73:2209–2225. doi: 10.1016/j.jacc.2019.01.072. [DOI] [PubMed] [Google Scholar]
- 56.Borlaug B.A., Melenovsky V., Russell S.D., Kessler K., Pacak K., Becker L.C., Kass D.A. Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation. 2006;114:2138–2147. doi: 10.1161/CIRCULATIONAHA.106.632745. [DOI] [PubMed] [Google Scholar]
- 57.Borlaug B.A., Olson T.P., Lam C.S.P., Flood K.S., Lerman A., Johnson B.D., Redfield M.M. Global Cardiovascular Reserve Dysfunction in Heart Failure With Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2010;56:845–854. doi: 10.1016/j.jacc.2010.03.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Haykowsky M.J., Kouba E.J., Brubaker P.H., Nicklas B.J., Eggebeen J., Kitzman D.W. Skeletal Muscle Composition and Its Relation to Exercise Intolerance in Older Patients With Heart Failure and Preserved Ejection Fraction. Am. J. Cardiol. 2014;113:1211–1216. doi: 10.1016/j.amjcard.2013.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haykowsky M.J., Brubaker P.H., John J.M., Stewart K.P., Morgan T.M., Kitzman D.W. Determinants of Exercise Intolerance in Elderly Heart Failure Patients With Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2011;58:265–274. doi: 10.1016/j.jacc.2011.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dhakal B.P., Malhotra R., Murphy R.M., Pappagianopoulos P.P., Baggish A.L., Weiner R.B., Houstis N.E., Eisman A.S., Hough S.S., Lewis G.D. Mechanisms of Exercise Intolerance in Heart Failure With Preserved Ejection Fraction The Role of Abnormal Peripheral Oxygen Extraction. Circ. Heart Fail. 2015;8:286–294. doi: 10.1161/CIRCHEARTFAILURE.114.001825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reddy Y.N.V., Andersen M.J., Obokata M., Koepp K.E., Kane G.C., Melenovsky V., Olson T.P., Borlaug B.A. Arterial Stiffening With Exercise in Patients With Heart Failure and Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2017;70:136–148. doi: 10.1016/j.jacc.2017.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guazzi M., Adams V., Conraads V., Halle M., Mezzani A., Vanhees L., Arena R., Fletcher G.F., Forman D.E., Kitzman D.W., et al. Clinical Recommendations for Cardiopulmonary Exercise Testing Data Assessment in Specific Patient Populations. Circulation. 2012;126:2261–2274. doi: 10.1161/CIR.0b013e31826fb946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pane C., Salzano A., Trinchillo A., Del Prete C., Casali C., Marcotulli C., Defazio G., Guardasole V., Vastarella R., Giallauria F., et al. Safety and feasibility of upper limb cardiopulmonary exercise test in Friedreich ataxia. Eur. J. Prev. Cardiol. 2020;29:445–451. doi: 10.1093/eurjpc/zwaa134. [DOI] [PubMed] [Google Scholar]
- 64.Saccà F., Puorro G., Marsili A., Antenora A., Pane C., Casali C., Marcotulli C., Defazio G., Liuzzi D., Tatillo C., et al. Long-term effect of epoetin alfa on clinical and biochemical markers in friedreich ataxia. Mov. Disord. 2016;31:734–741. doi: 10.1002/mds.26552. [DOI] [PubMed] [Google Scholar]
- 65.Pandey A., Parashar A., Kumbhani D.J., Agarwal S., Garg J., Kitzman D., Levine B.D., Drazner M., Berry J.D. Exercise Training in Patients With Heart Failure and Preserved Ejection Fraction Meta-Analysis of Randomized Control Trials. Circ. Heart Fail. 2015;8:33–40. doi: 10.1161/CIRCHEARTFAILURE.114.001615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kitzman D.W., Brubaker P.H., Herrington D.M., Morgan T.M., Stewart K.P., Hundley W.G., Abdelhamed A., Haykowsky M.J. Effect of Endurance Exercise Training on Endothelial Function and Arterial Stiffness in Older Patients With Heart Failure and Preserved Ejection Fraction A Randomized, Controlled, Single-Blind Trial. J. Am. Coll. Cardiol. 2013;62:584–592. doi: 10.1016/j.jacc.2013.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fujimoto N., Prasad A., Hastings J.L., Bhella P.S., Shibata S., Palmer D., Levine B.D. Cardiovascular effects of 1 year of progressive endurance exercise training in patients with heart failure with preserved ejection fraction. Am. Heart J. 2012;164:869–877. doi: 10.1016/j.ahj.2012.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Haykowsky M.J., Brubaker P.H., Stewart K.P., Morgan T.M., Eggebeen J., Kitzman D.W. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J. Am. Coll. Cardiol. 2012;60:120–128. doi: 10.1016/j.jacc.2012.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maldonado-Martin S., Brubaker P.H., Eggebeen J., Stewart K.P., Kitzman D.W. Association Between 6-Minute Walk Test Distance and Objective Variables of Functional Capacity After Exercise Training in Elderly Heart Failure Patients With Preserved Ejection Fraction: A Randomized Exercise Trial. Arch. Phys. Med. Rehabil. 2017;98:600–603. doi: 10.1016/j.apmr.2016.08.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Edelmann F., Gelbrich G., Dungen H.D., Frohling S., Wachter R., Stahrenberg R., Binder L., Topper A., Lashki D.J., Schwarz S., et al. Exercise Training Improves Exercise Capacity and Diastolic Function in Patients With Heart Failure With Preserved Ejection Fraction Results of the Ex-DHF (Exercise training in Diastolic Heart Failure) Pilot Study. J. Am. Coll. Cardiol. 2011;58:1780–1791. doi: 10.1016/j.jacc.2011.06.054. [DOI] [PubMed] [Google Scholar]
- 71.Brubaker P.H., Avis T., Rejeski W.J., Mihalko S.E., Tucker W.J., Kitzman D.W. Exercise Training Effects on the Relationship of Physical Function and Health-Related Quality of Life Among Older Heart Failure Patients With Preserved Ejection Fraction. J. Cardiopulm. Rehabil. Prev. 2020;40:427–433. doi: 10.1097/HCR.0000000000000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fu T.C., Yang N.I., Wang C.H., Cherng W.J., Chou S.L., Pan T.L., Wang J.S. Aerobic Interval Training Elicits Different Hemodynamic Adaptations Between Heart Failure Patients with Preserved and Reduced Ejection Fraction. Am. J. Phys. Med. Rehabil. 2016;95:15–27. doi: 10.1097/PHM.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 73.Kitzman D.W., Brubaker P., Morgan T., Haykowsky M., Hundley G., Kraus W.E., Eggebeen J., Nicklas B.J. Effect of Caloric Restriction or Aerobic Exercise Training on Peak Oxygen Consumption and Quality of Life in Obese Older Patients With Heart Failure With Preserved Ejection Fraction A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2016;315:36–46. doi: 10.1001/jama.2015.17346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Smart N.A., Haluska B., Jeffriess L., Leung D. Exercise training in heart failure with preserved systolic function: A randomized controlled trial of the effects on cardiac function and functional capacity. Congest. Heart Fail. 2012;18:295–301. doi: 10.1111/j.1751-7133.2012.00295.x. [DOI] [PubMed] [Google Scholar]
- 75.Angadi S.S., Mookadam F., Lee C.D., Tucker W.J., Haykowsky M.J., Gaesser G.A. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: A pilot study. J. Appl. Physiol. 2015;119:753–758. doi: 10.1152/japplphysiol.00518.2014. [DOI] [PubMed] [Google Scholar]
- 76.da Silveira A.D., de Lima J.B., Piardi D.D., Macedo D.D., Zanini M., Nery R., Laukkanen J.A., Stein R. High-intensity interval training is effective and superior to moderate continuous training in patients with heart failure with preserved ejection fraction: A randomized clinical trial. Eur. J. Prev. Cardiol. 2020;27:1733–1743. doi: 10.1177/2047487319901206. [DOI] [PubMed] [Google Scholar]
- 77.Mueller S., Winzer E.B., Duvinage A., Gevaert A.B., Edelmann F., Haller B., Pieske-Kraigher E., Beckers P., Bobenko A., Hommel J., et al. Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction A Randomized Clinical Trial. JAMA J. Am. Med. Assoc. 2021;325:542–551. doi: 10.1001/jama.2020.26812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kitzman D.W., Brubaker P.H., Morgan T.M., Stewart K.P., Little W.C. Exercise Training in Older Patients With Heart Failure and Preserved Ejection Fraction A Randomized, Controlled, Single-Blind Trial. Circ. Heart Fail. 2010;3:659–667. doi: 10.1161/CIRCHEARTFAILURE.110.958785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Alves A.J., Ribeiro F., Goldhammer E., Rivlin Y., Rosenschein U., Viana J.L., Duarte J.A., Sagiv M., Oliveira J. Exercise Training Improves Diastolic Function in Heart Failure Patients. Med. Sci. Sports Exerc. 2012;44:776–785. doi: 10.1249/MSS.0b013e31823cd16a. [DOI] [PubMed] [Google Scholar]
- 80.Salzano A., D’Assante R., Israr M.Z., Eltayeb M., D’Agostino A., Bernieh D., De Luca M., Rega S., Ranieri B., Mauro C., et al. Biomarkers in Heart Failure: Clinical Insights. Heart Fail. Clin. 2021;17:223–243. doi: 10.1016/j.hfc.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 81.Israr M.Z., Salzano A., Yazaki Y., Voors A.A., Ouwerkerk W., Anker S.D., Cleland J.G., Dickstein K., Metra M., Samani N.J., et al. Implications of serial measurements of natriuretic peptides in heart failure: Insights from BIOSTAT-CHF. Eur. J. Heart Fail. 2020;22:1486–1490. doi: 10.1002/ejhf.1951. [DOI] [PubMed] [Google Scholar]
- 82.Nolte K., Herrmann-Lingen C., Wachter R., Gelbrich G., Dungen H.D., Duvinage A., Hoischen N., von Oehsen K., Schwarz S., Hasenfuss G., et al. Effects of exercise training on different quality of life dimensions in heart failure with preserved ejection fraction: The Ex-DHF-P trial. Eur. J. Prev. Cardiol. 2015;22:582–593. doi: 10.1177/2047487314526071. [DOI] [PubMed] [Google Scholar]
- 83.Lang C.C., Smith K., Wingham J., Eyre V., Greaves C.J., Warren F.C., Green C., Jolly K., Davis R.C., Doherty P.J., et al. A randomised controlled trial of a facilitated home-based rehabilitation intervention in patients with heart failure with preserved ejection fraction and their caregivers: The REACH-HFpEF Pilot Study. BMJ Open. 2018;8:e019649. doi: 10.1136/bmjopen-2017-019649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Murad K., Brubaker P.H., Fitzgerald D.M., Morgan T.M., Goff D.C., Soliman E.Z., Eggebeen J.D., Kitzman D.W. Exercise training improves heart rate variability in older patients with heart failure: A randomized, controlled, single-blinded trial. Congest. Heart Fail. 2012;18:192–197. doi: 10.1111/j.1751-7133.2011.00282.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fujiwara K., Shimada K., Nishitani-Yokoyama M., Kunimoto M., Matsubara T., Matsumori R., Abulimiti A., Aikawa T., Ouchi S., Shimizu M., et al. Arterial Stiffness Index and Exercise Tolerance in Patients Undergoing Cardiac Rehabilitation. Int. Heart J. 2021;62:230–237. doi: 10.1536/ihj.20-418. [DOI] [PubMed] [Google Scholar]
- 86.Anker S.D., Butler J., Filippatos G., Ferreira J.P., Bocchi E., Bohm M., Brunner-La Rocca H.P., Choi D.J., Chopra V., Chuquiure-Valenzuela E., et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021;385:1451–1461. doi: 10.1056/NEJMoa2107038. [DOI] [PubMed] [Google Scholar]
- 87.Tucker W.J., Lijauco C.C., Hearon C.M., Angadi S.S., Nelson M.D., Sarma S., Nanayakkara S., La Gerche A., Haykowsky M.J. Mechanisms of the Improvement in Peak VO2 With Exercise Training in Heart Failure With Reduced or Preserved Ejection Fraction. Heart Lung Circ. 2018;27:9–21. doi: 10.1016/j.hlc.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 88.Maddox T.M., Januzzi J.L., Allen L.A., Breathett K., Butler J., Davis L.L., Fonarow G.C., Ibrahim N.E., Lindenfeld J., Masoudi F.A., et al. 2021 Update to the 2017 ACC Expert Consensus Decision Pathway for Optimization of Heart Failure Treatment: Answers to 10 Pivotal Issues About Heart Failure With Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2021;77:772–810. doi: 10.1016/j.jacc.2020.11.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.