Abstract
Bacillus licheniformis is used in a broad spectrum of areas, including some probiotic preparations for human and veterinary health. Moreover, B. licheniformis strains are known producers of various bioactive substances with antimicrobial and antibiofilm effects. In searching for new potentially beneficial bacteria for oral health, the inhibitory effect of B. licheniformis strains isolated from canine dental biofilm against pathogenic oral bacteria was evaluated. The antimicrobial effect of neutralized cell-free supernatants (nCFS) was assessed in vitro on polystyrene microtiter plates. Furthermore, molecular and morphological analyses were executed to evaluate the production of bioactive substances. To determine the nature of antimicrobial substance present in nCFS of B. licheniformis A-1-5B-AP, nCFS was exposed to the activity of various enzymes. The nCFS of B. licheniformis A-1-5B-AP significantly (p < 0.0001) reduced the growth of Porphyromonas gulae 3/H, Prevotella intermedia 1/P and Streptococcus mutans ATCC 35668. On the other hand, B. licheniformis A-2-11B-AP only significantly (p < 0.0001) inhibited the growth of P. intermedia 1/P and S. mutans ATCC 35668. However, enzyme-treated nCFS of B. licheniformis A-1-5B-AP did not lose its antimicrobial effect and significantly (p < 0.0001) inhibited the growth of Micrococcus luteus DSM 1790. Further studies are needed for the identification of antimicrobial substances.
Keywords: Bacillus licheniformis, antimicrobial effect, oral pathogens, cell-free supernatant
1. Introduction
In recent years, the use of probiotic bacteria and their bioactive substances to inhibit the growth of oral pathogenic bacteria has gained a growing interest [1,2,3]. So far, most of the investigated probiotic bacteria have been members of intestinal microbiota [2], with emphasis on Lactobacillus and Bifidobacterium being the main studied genera [4,5]. However, it is assumed that probiotics of oral origin would be more effective for adapting to the surfaces of the oral cavity [6].
Probiotic strains belonging to the genus Bacillus have shown to be transient colonizers of the host. Both forms, vegetative and spore, have been used as probiotics. Their antimicrobial effect is a result of the production of different metabolites, such as bacteriocins, biosurfactants (BS) and exopolysaccharides (EPS) [4].
Bacillus licheniformis is a Gram-positive, endospore-producing bacterium that belongs to the Bacillus subtilis group [7,8]. Bacteria of this group are considered to be relatively safe, but certain strains can cause opportunistic infections [9]. In comparison to most bacilli, which are in general aerobic, B. licheniformis is a facultative anaerobe [10] and is commonly found in natural environments such as soil or plants [11,12]. Some strains or their bioactive substances have been included in probiotics for human and veterinary use, and the aquaculture, biomedicine, pharmaceutical and food industries or in environmental applications [13,14]. B. licheniformis could promote animal health by stimulating the immune system, enhancing function of mucosal barriers, inhibiting the colonization of pathogenic bacteria, promoting the proliferation of potentially beneficial microorganisms and maintaining the balance of microbiota [15].
B. licheniformis is able to produce a wide range of antimicrobial substances with inhibitory activity against a broad spectrum of bacteria [9,13], and due to the production of these extracellular substances, B. licheniformis is considered to be an economically interesting microorganism. For example, it is used for the manufacturing of antibiotics and enzymes such as amylases or proteases [8,10,11]. Bacitracin is the first peptide antibiotic derived from cultures of B. licheniformis and has been applied widely in the medical and veterinary area with excellent safety. This antibiotic is a mixture of at least 5 polypeptides, and consists of 3 separate compounds, bacitracin A, B and C. It is active against various species of Gram-positive and a few species of Gram-negative bacteria [16,17]. In addition to that, some strains can produce two-peptide lantibiotic bacteriocin lichenicidin [18]; however, synthesis of bacteriocin-like peptides such as lichenin and bacillocin was also reported [13]. Moreover, B. licheniformis can synthesize EPS of various biological activities, including antibacterial and antioxidant effects [19]. A typical example is levan [20], which is synthesized by an enzyme, levansucrase [21]. Inhibitory effects of B. licheniformis can also be associated with the non-ribosomal synthesis of lipopeptide BS lichenysin [22,23]. These biological properties make B. licheniformis a potential candidate for the development of new probiotics.
Therefore, the aim of present study was to investigate in the vitro inhibitory effect of B. licheniformis strains isolated from canine dental biofilm against canine and human oral pathogens.
2. Materials and Methods
2.1. Identification of Bacterial Strains
Bacterial strains B. licheniformis A-1-5B-AP and B. licheniformis A-2-11B-AP isolated from canine dental biofilms were cultured on blood agar (BA) at 37 °C for 24 h under aerobic conditions and identified based on the 16S rRNA gene and gyrB gene. BA was prepared as Tryptone Soya Agar (HiMedia, Mumbai, India) supplemented with 5% sterile horse blood. For identification by the 16S rRNA gene, DNA was extracted from pure bacterial cultures using DNAzol Direct (Molecular Research Center Inc., Cincinnati, USA) according to the manufacturer’s instructions. For identification by gyrB gene, DNA was isolated using Quick-DNA Fecal/Soil Microbe Miniprep Kit (Zymo Research, Irvine, USA). PCR reaction was performed in a thermocycler (TProfesional Basic, Biometra GmbH, Gôttingen, Germany) using OneTaq 2X Master Mix with standard buffer (New England Biolabs, Foster City, CA, USA) and universal primers (27F, 1492R) for the 16S rRNA gene [24] and Blich-F1: 5′AKACGGAAGTGACGGGAAC3′ and Blich-R1: 5′AGAAACTTTTCRAGCGCTT3′ for gyrB gene according to Huang et al. [25].
The PCR conditions for the 16S rRNA gene consisted of an initial denaturation at 94 °C for 5 min, followed by 30 cycles including denaturation at 94 °C for 1 min, annealing at 55 °C for 1 min and extension at 72 °C for 3 min and final extension at 72 °C for 10 min. The PCR conditions for gyrB gene were 5 min at 95 °C, 30× [1 min at 95 °C, 1 min at 65 °C and 1 min at 72 °C] and 5 min at 72 °C. B. licheniformis DSM 13 (German Collection of Microorganisms and Cell Cultures, Braunschweig, Germany) was used as a positive control. A negative control (RNase-free water) was included in the PCR reactions. The expected product size for the gyrB gene was 613 bp.
PCR products were visualized on a 2% agarose gel under UV light using GelRed [26] (Biotium, Inc., Hayward, CA, USA) and sent for purification and Sanger sequencing at Microsynth (Vienna, Austria). The obtained sequences were processed using Geneious 8.0.5 program (Biomatters, Auckland, New Zealand). Then, they were compared to the NCBI GenBank database using BLASTn [27]. The sequences of the 16S rRNA genes were stored in GenBank database under the accession numbers (AN) MT492074 and MT492090.
2.2. Preparation of Neutralized Cell-Free Supernatants
B. licheniformis A-1-5B-AP, A-2-11B-AP and DSM 13 were inoculated on Brain Heart Infusion (BHI) agar (HiMedia, Mumbai, India) and grown at 37 °C for 24 h under aerobic conditions. A standardized suspension of the individual strains was prepared by resuspending the solitary colonies in 3 mL of saline solution, and turbidity was then adjusted to 1–1.1 McFarland at 565 nm wavelength (DEN-1 McFarland densitometer, Biosan, Riga, Latvia). After that, 0.5 mL suspension was inoculated into 50 mL BHI broth (HiMedia, Mumbai, India) and incubated on a shaker aerobically for 24 h at 37 °C and 119 rpm (SKO-D XL, Agrolab, Pischelsdorf, Austria). BHI broth inoculated with saline solution was used as a control. Subsequently, the inoculated BHI broth were centrifuged for 40 min at 4 °C and 4500 rpm (ROTINA 420R, Hettich, Tuttlingen, Germany). The obtained cell-free supernatant (CFS) was neutralized with 10 M NaOH to pH 7 and filtered through a microbiological filter with a pore size of 0.22 μm (Minasart; Biotech, Göttingen, Germany).
2.3. Antimicrobial Effect of B. licheniformis Strains
The oral pathogenic strains Porphyromonas gulae 3/H, Prevotella intermedia 1/P and Streptococcus mutans ATCC 35668 were used to test the antimicrobial effect of neutralized CFS (nCFS) of B. licheniformis strains. P. gulae 3/H and P. intermedia 1/P (periodontal disease associated bacteria) were isolated from canine dental biofilm and grown on BA at 37 °C for 72 h under anaerobic conditions (BBL GasPakTM Plus, Becton, Dickinson and Co., Franklin Lakes, NJ, USA). S. mutans was selected as human oral pathogen causing dental caries. S. mutans ATCC 35668 was acquired from the Faculty of Natural Sciences of Comenius University in Bratislava. It was inoculated on BA plates and incubated aerobically for 24 h at 37 °C.
For the testing of canine oral pathogens, 110 µL of a standardized suspension of pathogenic strains P. gulae 3/H and P. intermedia 1/P (1–1.1 McFarland) were pipetted into 11 mL tubes, and the tubes were filled to 11 mL with individual nCFS enriched with yeast extract (5 g/L; Condalab, Madrid, Spain), cysteine (1 g/L; Sigma-Aldrich, St. Louis, MO, USA), hemin (5 mg/L; Sigma-Aldrich, St. Louis, MO, USA) and vitamin K1 (1mg/L; Sigma-Aldrich, St. Louis, MO, USA). BHI broth was enriched with yeast extract before autoclaving, while cysteine, hemin and vitamin K1 were filtered and added afterwards. Individual enriched nCFS with saline solution were used as a negative control. An enriched BHI broth with pathogenic strains without nCFS was used as a positive control. To prevent oxygen access, the tubes were parafilm-coated and cultured for 72 h at 37 °C. After cultivation, the volume of each tube was homogenized and pipetted into the wells of a polystyrene microtiter plate (Greiner Bio-One GmbH, Frickenhausen, Germany) at 200 µL per well.
For human oral pathogen S. mutans ATCC 35668, individual nCFS were pipetted into the wells of a polystyrene microtiter plate at 180 µL per well. Subsequently, 20 µL of a standardized suspension of S. mutans ATCC 35668 (1–1.1 McFarland) were pipetted into the medium and nCFS. BHI broth and individual nCFS with saline solution were used as a negative control. BHI broth with S. mutans ATCC 35668 without nCFS was used as a positive control. Microtiter plates were cultured for 24 h at 37 °C.
To evaluate the growth of pathogenic strains in the presence of individual nCFS, absorbance at 570 nm was measured (Synergy 4 Multi-Mode Microplate Reader, BioTek, Winnoski, VT, USA). Individual strains were tested in at least three independent experiments and the results are interpreted as the arithmetic mean of the measured values ± the standard deviation.
2.4. Bacitracin Susceptibility Test of Oral Pathogens
Disk diffusion test was used to evaluate the susceptibility of Micrococcus luteus DSM 1790 and oral pathogens, namely P. intermedia 1/P and S. mutans ATCC 35668 to bacitracin. M. luteus DSM 1790 was purchased from Leibniz Institute DSMZ (German Collection of Microorganisms and Cell Cultures, Braunschweig, Germany). Turbidity of standardized suspension of individual bacterial strains was adjusted to 0.5 McFarland and inoculated onto BA plate [28]. A disk containing 10 units of bacitracin B (HiMedia, Mumbai, India) was placed on top of the inoculated agar plate, which was then incubated at 37 °C for 24, 48 and 72 h in case of M. luteus DSM 1790, S. mutans ATCC 35668 and P. intermedia 1/P, respectively. P. intermedia 1/P was cultivated under anaerobic conditions. After incubation, the inoculated plates were examined for inhibition zones. Growth inhibition zone diameter was measured in millimeters for all bacterial strains.
2.5. Evaluation of the Ability to Produce Bioactive Substances
The ability to produce bioactive substances was assessed based on molecular and morphological analyses. Production of EPS was evaluated phenotypically. B. licheniformis strains were inoculated on modified BHI agar with high sucrose content (100 g/L) and cultured aerobically at 37 °C for 24 h. The phenotypic manifestation of EPS production was assessed visually by forming viscous fiber or mucoid growth called as “ropy” and “nonropy” manifestation, respectively. A screening test was used to monitor the production of BS in B. licheniformis strains. The oil spreading test was performed according to Morikawa et al. [29]. Firstly, 20 mL of distilled water were added to the Petri dish and 20 μL of crude oil was dripped onto the water surface, followed by 10 μL of nCFS of tested strains. BHI broth without surfactant was used as a negative control and Tween 80 was used as a positive control.
B. licheniformis strains were tested by PCR for the presence of lsRN gene encoding the enzyme levansucrase, which is involved in the synthesis of levan EPS; the bli04127 gene, which represents the structural gene of Bliα lichenicidin peptide; and lchAA gene encoding lichenysin synthetase. DNA isolated by Quick-DNA Fecal/Soil Microbe Miniprep Kit, OneTaq 2X Master Mix with standard buffer, RNase-free water and primers were used for PCR. Primers and PCR reaction conditions are listed in Table 1. B. licheniformis DSM 13 was used as a positive control and RNase-free water was used as a negative control. PCR products were visualized on a 2% agarose gel under UV light using GelRed and submitted for purification and Sanger sequencing to Microsynth. The obtained sequences were processed using the Geneious program. Subsequently, they were compared to the NCBI GenBank database using BLASTn. The sequences of the lsRN, bli04127 and lchAA genes were stored in GenBank database under AN ON081292, ON081293, ON649684 and ON649685.
Table 1.
Primers and PCR conditions.
| Target Sequence (Gene) |
Primer Sequence (5′ to 3′) | PCR Conditions | Product Size (bp) |
Source |
|---|---|---|---|---|
| Levansucrase (lsRN) | TGCTCTAGACGATTCCCGCTTATACAGACTATAGAT | 95 °C 3 min, 24× [95 °C 1 min, 55 °C 30 s, 72 °C 4 min] 72 °C 10 min |
1793 | [30] |
| CGGGATCCTTATTTGTTTACCGTTAGTTCTCCC | ||||
| Lichenicidin (bli04127) | GGAAATGATTCTTTCATGG | 95 °C 5 min, 30× [95 °C 1 min, 55 °C 1 min, 72 °C 1 min] 72 °C 5 min |
215 | [31,32] |
| TTAGTTACAGCTTGGCATG | ||||
| Lichenysin synthetase (lchAA) | GTGCCTGATGTAACGAATG | 94 °C 2 min, 30× [94 °C 15 s, 60 °C 30 s, 72 °C 50 s] 72 °C 5 min |
735 | [33] |
| CACTTCCTGCCATATACC |
2.6. Effect of Enzymes on Antimicrobial Activity
To evaluate the effect of enzymes on antimicrobial substances, nCFS of B. licheniformis A-1-5B-AP were treated with proteinase K (1 mg/mL), lipase (1 mg/mL) and α-amylase (1 mg/mL). The enzymes were activated by incubating the enzyme-treated nCFS at 37 °C for 2 h, and then the enzymes were immediately inactivated at 95 °C for 5 min. Individual enzyme-treated nCFS were pipetted into the wells of a polystyrene microtiter plate at 180 µL per well. Subsequently, 20 µL of a standardized suspension of M. luteus DSM 1790 (1–1.1 McFarland) was pipetted into the medium. Enzyme-treated BHI broth with saline solution and individual enzyme-treated nCFS with saline solution were used as a negative control. BHI broth treated with enzymes with M. luteus DSM 1790 without nCFS was used as a positive control. Microtiter plates were cultured at 37 °C for 24 h. Subsequently, the absorbance at 570 nm was measured. The effect of the enzymes was tested in at least three independent experiments and the results are interpreted as the arithmetic mean of the measured values ± the standard deviation.
2.7. Statistical Analyses
Antimicrobial activity results were evaluated by one-way analysis of variance (ANOVA) with an additional Dunnett’s test in the GraphPad Prism 9.3.1 (GraphPad Inc., San Diego, CA, USA). The growth of M. luteus DSM 1790 in the presence of enzyme-treated nCFS of B. licheniformis A-1-5B-AP was evaluated by unpaired t test. A p-value less than 0.05 (p < 0.05) was considered statistically significant. The antimicrobial activity of our strains B. licheniformis A-1-5B-AP and A-2-11B-AP against selected pathogenic bacteria was compared with the antimicrobial activity of B. licheniformis DSM 13.
3. Results
3.1. Identification of Bacterial Strains
Based on BLASTn analysis for 16S rRNA gene, bacterial isolates A-1-5B-AP and A-2-11B-AP showed high similarity of 99.59% and 99.65%, respectively, with multiple B. licheniformis strains including B. licheniformis DSM 13 (AN: NR118996). PCR reaction with specific primers for gyrB gene was used to confirm the identification of B. licheniformis strains. A PCR product of approximately 600 bp was present in both tested strains and the positive control (B. licheniformis DSM 13). BLASTn analysis confirmed the initial identification.
B. licheniformis A-1-5B-AP had 99.64% similarity with three DNA gyrase subunit B (gyrB) genes of B. licheniformis strains, namely B. licheniformis UTM118 (AN: KF952583), B. licheniformis UTM102 (AN: KF952576) and B. licheniformis C32 (AN: HQ336651). B. licheniformis A-2-11B-AP had 100% similarity with multiple complete genomes and multiple gyrB genes of B. licheniformis strains.
3.2. Antimicrobial Effect of B. licheniformis Strains
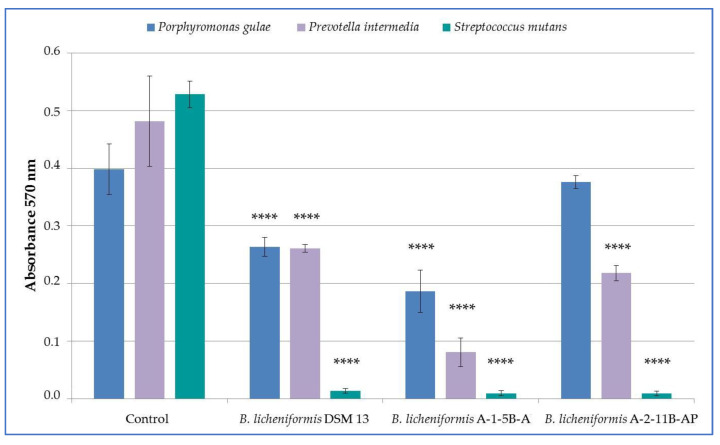
Oral pathogenic strains were used to test the antimicrobial effect of B. licheniformis DSM 13, A-1-5B-AP and A-2-11B-AP. All tested nCFS of B. licheniformis strains had an inhibitory effect on the growth of pathogenic strains of P. gulae 3/H, P. intermedia 1/P and S. mutans ATCC 35668 (Figure 1). The growth of all pathogens tested was significantly inhibited (p < 0.0001) in nCFS of B. licheniformis DSM 13 and A-1-5B-AP compared to control. nCFS of B. licheniformis A-2-11B-AP significantly inhibited the growth of P. intermedia 1/P and S. mutans ATCC 35668 (p < 0.0001) but did not have a significant inhibitory effect on the growth of P. gulae 3/H. In terms of evaluating the percentage of growth inhibition, in P. gulae 3/H it ranged from 5.57 to 53.25%, in P. intermedia 1/P from 45.78 to 83.29%, and in S. mutans ATCC 35668 it was above 97% for all strains tested (Table 2).
Figure 1.
Inhibitory activity of nCFS of Bacillus licheniformis strains against the growth of oral pathogens; data are presented as the arithmetic means ± standard deviation; **** (p < 0.0001)—significant difference compared to the non-treated control.
Table 2.
Inhibition of oral pathogens growth by nCFS of Bacillus licheniformis strains.
| Percentage of Growth Inhibition (%) | |||
|---|---|---|---|
| Bacterial Strains |
B. licheniformis DSM 13 |
B. licheniformis A-1-5B-AP |
B. licheniformis A-2-11B-AP |
| P. gulae 3/H | 33.86 ± 4.12 | 53.25 ± 9.21 | 5.57 ± 2.78 |
| P. intermedia 1/P | 45.78 ± 1.38 | 83.29 ± 5.12 | 54.76 ± 2.78 |
| S. mutans ATCC 35668 | 97.48 ± 0.79 | 98.24 ± 0.82 | 98.30 ± 0.79 |
3.3. Bacitracin Susceptibility Test
In order to exclude the possible inhibitory effect of bacitracin in the nCFS of B. licheniformis strains, pathogenic strains were tested for bacitracin susceptibility. In S. mutans ATCC 35668, a small inhibition zone diameter of 11 mm was present after 24 h incubation. On the other hand, the size of inhibition zone for P. intermedia 1/P was 63 mm. The diameter of the inhibition zone for M. luteus DSM 1790 was 28 mm, thus concluding that sensitivity to the bacitracin of S. mutans ATCC 35668 is intermediate, while P. intermedia 1/P and M. luteus DSM 1790 are sensitive.
3.4. Production of Bioactive Substances
The manifestation of EPS production was observed as the qualitative assessment of the phenotypic manifestation in both tested strains of B. licheniformis. B. licheniformis A-1-5B-AP formed a viscous fiber, also known as the “ropy” phenotype (Figure 2). B. licheniformis A-2-11B-AP had a typical mucoid growth with the “non-ropy” phenotype with shiny colonies that are characteristic for EPS production on BHI agar supplemented with 10% sucrose.
Figure 2.
Forming of viscous filament known as ropy phenotype in B. licheniformis A-1-5B-AP.
The oil spreading test was used to detect the production of BS in B. licheniformis strains. Tween 80 was used as a positive control and it created an oil-free clearing zone when dropped on the surface of crude oil. However, both tested strains of B. licheniformis and the negative control showed no clearing zone associated with surfactant activity.
PCR reaction with specific primers was used for the detection of the bli04127 gene responsible for the synthesis of one antimicrobial peptide of the two-peptide lantibiotic lichenicidin. Based on the agarose gel electrophoresis, the PCR products had sizes of approximately 215 bp in both the positive control and B. licheniformis A-2-11B-AP. No PCR products were present in the negative control and B. licheniformis A-1-5B-AP. Following Sanger sequencing, sequences of B. licheniformis A-2-11B-AP and lichenicidin-producing strain B. licheniformis DSM 13 that was used as a positive control showed 100% homology. Based on BLASTn analysis, B. licheniformis A-2-11B-AP showed 100% homology with several complete B. licheniformis genomes, including B. licheniformis DSM 13 (AN: AE017333) and with the lantibiotic gene cluster of B. licheniformis VK21 (AN: GU949560).
B. licheniformis strains are able to produce multiple EPS, including levan, with antibacterial and antibiofilm activity. Levan is synthesized by levansucrase enzyme encoded by the lsRN gene, which was detected by PCR with specific primers BlLs-F and BlLs-R. Regarding agarose gel electrophoresis PCR products of approximately 1800 bp were present in positive control and B. licheniformis A-2-11B-AP. However, no PCR products were present in B. licheniformis A-1-5B-AP and the negative control. Following Sanger sequencing, the sequences of the levan-producing strain B. licheniformis DSM 13 were used as positive control, and B. licheniformis A-2-11B-AP showed 100% homology. Based on BLASTn analysis, B. licheniformis A-2-11B-AP showed 100% homology with several complete B. licheniformis genomes, including B. licheniformis DSM 13 (AN: AE017333) and to the levansucrase gene of B. licheniformis 8-37-0-1 (AN: KF647836).
Most of the B. licheniformis strains are able to synthesize surface-active substances, including lichenysin with antibacterial and antibiofilm activity. PCR with the set of specific primers LicA-F and LicA-R was used for the detection of lichenysin synthetase gene. Using agarose gel electrophoresis, PCR products of 735 bp were present in all strains tested including the positive control. No PCR product was present in the negative control. Based on BLASTn analysis, B. licheniformis A-1-5B-AP showed 99.86% homology with the B. licheniformis lichenysin biosynthesis operon: the lichenysin synthetase A (licA), lichenysin synthetase B (licB), lichenysin synthetase C (licC), and thioesterase (licTE) genes, complete cds (AN: U95370). B. licheniformis A-2-11B-AP showed 100% similarity with multiple complete B. licheniformis genomes and 91.77% identity with the B. licheniformis lichenysin biosynthesis operon: lichenysin synthetase A (licA), lichenysin synthetase B (licB), lichenysin synthetase C (licC) and thioesterase (licTE) genes, complete cds (AN: U95370).
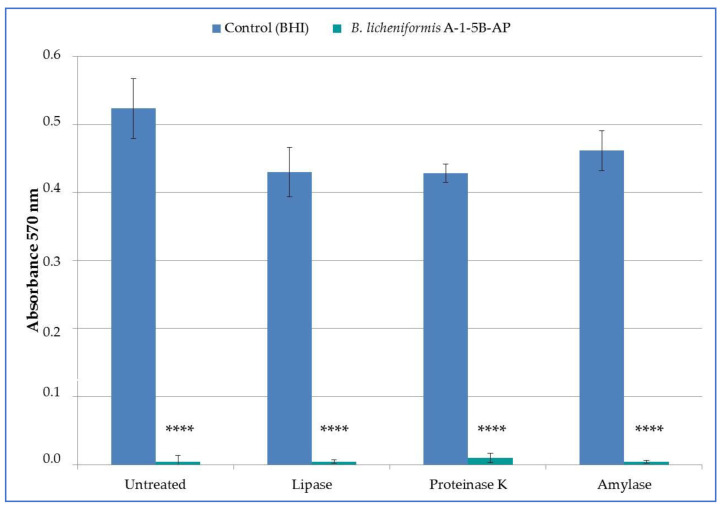
3.5. Effect of Enzymes on Antimicrobial Activity of nCFS B. licheniformis A-1-5B-AP
To determine the nature of antimicrobial substance synthesized by B. licheniformis A-1-5B-AP, nCFS was treated with various enzymes. However, presence of neither enzyme (proteinase K, lipase and α-amylase) affected the antimicrobial activity of nCFS and addition of these enzymes was not accompanied with the loss of the antimicrobial activity of nCFS (Figure 3). All enzyme-treated nCFS significantly (p < 0.0001) inhibited the growth of M. luteus DSM 1790. The percentage of growth inhibition was 99.16 ± 0.48, 98.17 ± 1.33, and 99.22 ± 0.41% for lipase, proteinase K, and α-amylase, respectively.
Figure 3.
Enzymatic treatment of neutralized cell-free supernatants of B. licheniformis A-1-5B-AP and its activity against indicator strain of Micrococcus luteus DSM 1790; data are presented as the arithmetic means ± standard deviation; **** p < 0.0001—significant difference compared to the non-treated control.
4. Discussion
Oral bacteria associated with periodontal diseases and dental caries are receiving considerable attention in order to evaluate the antimicrobial effect of natural substances that could positively affect oral health [34]. To the best of our knowledge, there are currently no studies available describing the inhibitory effect of canine oral strains of B. licheniformis against canine and human oral pathogens. Therefore, the present study evaluated the inhibitory effect of nCFS of B. licheniformis A-1-5B-AP and A-2-11B-AP isolated from canine dental biofilms against selected oral pathogenic strains, namely P. gulae 3/H, P. intermedia 1/P and S. mutans ATCC 35668.
In general, P. gulae and P. intermedia are associated with periodontal disease in dogs [35], while S. mutans plays a major role in the development of dental caries in humans and also promotes formation of oral biofilms [36]. In regard to the periodontal diseases, there is only limited amount of knowledge available about the effectiveness of Bacillus spp. [37], even though members of the genus Bacillus are considered to be relatively good producers of antimicrobial substances. In particular, B. licheniformis has been described as a source of many antimicrobial substances [13]. A mouthwash containing Bacillus subtilis has shown efficacy in reducing periodontal pathogens in humans [38]. In experimental periodontitis in rats, the beneficial effects and possible therapeutic potential of B. subtilis and B. licheniformis were also described [37]. In this study, nCFS of B. licheniformis A-1-5B-AP and DSM 13 strains showed an antimicrobial effect against P. gulae 3/H and P. intermedia 1/P, while nCFS of B. licheniformis A-2-11B-AP significantly inhibited only the growth of P. intermedia 1/P.
Dental caries is considered to be one of the most common oral diseases in human population with a relatively high prevalence [39]. It has been shown that some enzymes and antimicrobial compounds produced by some Bacillus spp. inhibit the growth of S. mutans, thereby preventing biofilm formation [36]. Bacillus coagulans in chewable tablet was effective in reducing and inhibiting caries-causing mutans streptococci and lactobacilli levels in plaque and saliva in children [40]. On the other hand, in the study by Rivis et al. [41], the inhibitory effect of the combination of B. subtilis B-5007 and B. licheniformis B-5514 on the growth of the clinical strain S. mutans was not demonstrated. Compared to humans, the occurrence of dental caries in dogs is rare, probably due to the key factors such as differences in the oral microbiota composition, higher pH of saliva or the association with a low-carbohydrate diet. From this point of view, it is assumed that canine oral bacteria could be applied in the control of S. mutans and other cariogenic bacteria in human dental biofilms [42]. In this study, all tested nCFS of B. licheniformis significantly inhibited the growth of S. mutans ATCC 35668, indicating the ability to produce antimicrobial substances. Similarly, in the study by Martins et al. [42], Bacillus sp. isolated from canine dental biofilm showed bacteriocinogenic activity against S. mutans.
Since some strains of B. licheniformis are able to produce bacitracin, a sensitivity test of oral pathogens to bacitracin was also performed. Bacitracin is a non-ribosomally synthesized docapeptide antibiotic produced by certain strains of B. subtilis and B. licheniformis [43]. It has activity mainly against Gram-positive and some Gram-negative bacteria by inhibiting bacterial cell wall biosynthesis [44], and it can also inhibit biofilm formation in cariogenic S. mutans [45]. In the studies of Anumala et al. [46], up to 80% of P. intermedia strains showed sensitivity to bacitracin. In addition, the inhibition of growth and biofilm formation of M. luteus by bacitracin has been demonstrated [47]. Bacitracin B susceptibility testing performed in this study showed that P. intermedia 1/P and M. luteus DSM 1790 strains were also susceptible, which is in agreement with previous claims. However, S. mutans ATCC 35668 showed intermediate sensitivity to bacitracin B, which is in contrast to the result in the study by Kazemi et al. [48], in which the same strain was resistant to 15 μg of bacitracin contained in a disc. It is generally known that S. mutans is resistant to bacitracin, or it contains bacitracin resistance genes. This ability is often used to isolate S. mutans from the entire spectrum of oral microbiota using media containing bacitracin [49,50].
Bacillus spp. are prolific in the production of antimicrobial substances which may give them a selective advantage over other bacterial species [51]. Levan is a fructan-type EPS produced from sucrose via extracellular levansucrases by many bacteria, including B. licheniformis, and its synthesis can occur both under aerobic and anaerobic conditions [52,53]. Levans are involved in many physiological functions, such as the attachment of bacterial cells in their habitat and protection from cold and drought. In addition, levans have a high potential as substances with antibacterial, antibiofilm, antiviral and anticarcinogenic effects [30,54]. BS are amphiphilic compounds produced by microorganisms with significant surface and emulsifying activities [55]. A surface active substance known as lichenysin is produced by B. licheniformis as a secondary metabolite, and its biosynthesis is catalyzed by non-ribosomal peptide synthetases. Its structure is very similar to that of surfactin, a well-known BS produced by B. subtilis. Both compounds can be produced under aerobic or anaerobic conditions [7]. In this study, EPS production was demonstrated phenotypically in both tested strains of B. licheniformis, while in B. licheniformis A-2-11B-AP, a gene encoding levansucrase synthesis was detected by molecular analysis as well. The lichenysin synthetase gene was present in all strains, but the oil spreading test did not demonstrate the presence of this substance in nCFS. Even though the presence of lichenysin synthetase genes in B. licheniformis seems to be very frequent, their production is closely related to environmental conditions, such as the incubation temperature or the type of carbon, nitrogen and phosphate sources present in the culture medium [7].
In our tested strains, the ability to produce lichenicidin was demonstrated only in B. licheniformis A-2-11B-AP; however, its nCFS did not significantly inhibit the growth of P. gulae 3/H compared to nCFS of B. licheniformis A-1-5B-AP. Lichenicidin is a class II dipeptide lantibiotic that was first described in B. licheniformis DSM 13 [56]. Moreover, it has been shown that lichenicidin can be produced by other strains of B. licheniformis, and the structure of its peptides may differ depending on the producing strain [57]. Furthermore, the production of several bacteriocin-like substances with different characteristics and a wide spectrum of activity against pathogenic bacteria, such as lichenin, bacillocin 490 and P40, was also recorded in B. licheniformis strains [58,59].
In contrast to the lichenicidin-producing strains, B. licheniformis A-1-5B-AP showed higher inhibitory activity against all oral pathogens, indicating that this strain is capable of producing a different antimicrobial substance. To elucidate the nature of this antimicrobial substance, nCFS of B. licheniformis A-1-5B-AP was treated with different enzymes, namely proteinase K, lipase and α-amylase, and tested against the indicator strain of M. luteus DSM 1790. However, proteinase K, lipase or α-amylase did not affect the antimicrobial activity present in the nCFS of this strain. Many antimicrobial peptides produced by Bacillus spp. have different resistance to enzyme activity, with stability over a wide range of pH and temperature [60]. The bacteriocin lichenocin 50.2 is completely inactivated by proteinase K and pronase E, and partial inactivation is observed upon treatment with trypsin. BLIS_SXAU06 produced by B. licheniformis SXAU06 can be fully inactivated by pronase E and partially inactivated by trypsin and pepsin, but it is insensitive to proteinase K [61]. Antimicrobial activity of a bacteriocin-like substance JY-1 present in the supernatant of Bacillus spp. JY-1 was not affected by neutral proteinase and proteinase K, but it was partially reduced when treated with trypsin and pepsin [62]. The effect of enzymes including pepsin, trypsin and proteinase K was tested on CFS of B. licheniformis MCC2514 and MCC2512 against M. luteus ATCC9341, and while the antimicrobial compounds found in the supernatants were sensitive to proteinase K, they were resistant to the other protease enzymes tested. Supernatants of these strains were also treated with α-amylase, and showed 50% residual activity [63]. In addition, the possible production of bacitracin could inhibit proteinase K [64] as it is known to be capable of protease inhibition [65].
5. Conclusions
The growth of P. gulae 3/H, P. intermedia 1/P, S. mutans ATCC 35668 and M. luteus DSM 1790 was significantly inhibited by nCFS of B. licheniformis A-1-5B-AP. Based on molecular analysis, the presence of genes associated with the synthesis of lichenysin was detected, although its presence in medium was not confirmed. Furthermore, B. licheniformis A-1-5B-AP was able to produce EPS, which was manifested by the formation of viscous fiber known as the ropy phenotype. Therefore, to determine the nature of the antimicrobial substance produced by B. licheniformis A-1-5B-AP, nCFS was treated with various enzymes. However, there was no loss of antimicrobial activity detected after treatment. Due to the inhibitory activity of B. licheniformis A-1-5B-AP, it has a potential for possible use in the prevention and elimination of not only periodontal pathogens in dogs but also cariogenic S. mutans in humans. Further studies are needed to clarify the identity and characterize the antimicrobial substance present in nCFS of B. licheniformis A-1-5B-AP.
Author Contributions
Conceptualization, N.Š.H. and M.M.; methodology, J.K., S.Š. and M.M.; validation, N.Š.H. and M.S..; formal analysis, N.Š.H. and S.Š.; investigation, J.K., N.Š.H., M.S. and R.M.; resources, M.M.; data curation, J.K., N.Š.H. and M.S.; writing—original draft preparation, N.Š.H., S.Š. and M.S.; writing—review and editing, J.K., R.M. and M.M.; visualization, N.Š.H. and M.S.; supervision, M.M.; project administration, M.M.; funding acquisition, M.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Scientific Grand Agency of the Ministry of Education of the Slovak Republic (grant no. VEGA 1/0788/19) and by the Slovak Research and Development Agency (grant no. APVV-16-0203).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zaura E., Twetman S. Critical Appraisal of Oral Pre- and Probiotics for Caries Prevention and Care. Caries Res. 2019;53:514–526. doi: 10.1159/000499037. [DOI] [PubMed] [Google Scholar]
- 2.Zupancic K., Kriksic V., Kovacevic I., Kovacevic D. Influence of Oral Probiotic Streptococcus salivarius K12 on Ear and Oral Cavity Health in Humans: Systematic Review. Probiotics Antimicrob. Proteins. 2017;9:102–110. doi: 10.1007/s12602-017-9261-2. [DOI] [PubMed] [Google Scholar]
- 3.Barzegari A., Kheyrolahzadeh K., Hosseiniyan Khatibi S.M., Sharifi S., Memar M.Y., Zununi Vahed S. The Battle of Probiotics and Their Derivatives against Biofilms. Infect. Drug Resist. 2020;13:659–672. doi: 10.2147/IDR.S232982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee N.K., Kim W.S., Paik H.D. Bacillus strains as human probiotics: Characterization, safety, microbiome, and probiotic carrier. Food Sci. Biotechnol. 2019;28:1297–1305. doi: 10.1007/s10068-019-00691-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romo-Barrera C.M., Castrillón-Rivera L.E., Palma-Ramos A., Castañeda-Sánchez J.I., Luna-Herrera J. Bacillus licheniformis and Bacillus subtilis, Probiotics That Induce the Formation of Macrophage Extracellular Traps. Microorganisms. 2021;9:2027. doi: 10.3390/microorganisms9102027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Busarcevic M., Dalgalarrondo M. Purification and genetic characterisation of the novel bacteriocin LS2 produced by the human oral strain Lactobacillus salivarius BGHO1. Int. J. Antimicrob. Agents. 2012;40:127–134. doi: 10.1016/j.ijantimicag.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Yeak K.Y.C., Perko M., Staring G., Fernandez-Ciruelos B.M., Wells J.M., Abee T., Wells-Bennik M. Lichenysin Production by Bacillus licheniformis Food Isolates and Toxicity to Human Cells. Front. Microbiol. 2022;13:831033. doi: 10.3389/fmicb.2022.831033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee C., Kim J.Y., Song H.S., Kim Y.B., Choi Y.E., Yoon C., Nam Y.D., Roh S.W. Genomic Analysis of Bacillus licheniformis CBA7126 Isolated from a Human Fecal Sample. Front. Pharmacol. 2017;8:724. doi: 10.3389/fphar.2017.00724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nithya V., Muthukumar S.P., Halami P.M. Safety assessment of Bacillus licheniformis Me1 isolated from milk for probiotic application. Int. J. Toxicol. 2012;31:228–237. doi: 10.1177/1091581812443388. [DOI] [PubMed] [Google Scholar]
- 10.Rey M.W., Ramaiya P., Nelson B.A., Brody-Karpin S.D., Zaretsky E.J., Tang M., Lopez de Leon A., Xiang H., Gusti V., Clausen I.G., et al. Complete genome sequence of the industrial bacterium Bacillus licheniformis and comparisons with closely related Bacillus species. Genome Biol. 2004;5:R77. doi: 10.1186/gb-2004-5-10-r77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rehman H.U., Siddique N.N., Aman A., Nawaz M.A., Baloch A.H., Qader S.A.U. Morphological and molecular based identification of pectinase producing Bacillus licheniformis from rotten vegetable. J. Genet. Eng. Biotechnol. 2015;13:139–144. doi: 10.1016/j.jgeb.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veith B., Herzberg C., Steckel S., Feesche J., Maurer K.H., Ehrenreich P., Bäumer S., Henne A., Liesegang H., Merkl R., et al. The complete genome sequence of Bacillus licheniformis DSM13, an organism with great industrial potential. J. Mol. Microbiol. Biotechnol. 2004;7:204–211. doi: 10.1159/000079829. [DOI] [PubMed] [Google Scholar]
- 13.Muras A., Romero M., Mayer C., Otero A. Biotechnological applications of Bacillus licheniformis. Crit. Rev. Biotechnol. 2021;41:609–627. doi: 10.1080/07388551.2021.1873239. [DOI] [PubMed] [Google Scholar]
- 14.Elshaghabee F.M.F., Rokana N., Gulhane R.D., Sharma C., Panwar H. Bacillus as Potential Probiotics: Status, Concerns, and Future Perspectives. Front. Microbiol. 2017;8:1490. doi: 10.3389/fmicb.2017.01490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kan L., Guo F., Liu Y., Pham V.H., Guo Y., Wang Z. Probiotics Bacillus licheniformis Improves Intestinal Health of Subclinical Necrotic Enteritis-Challenged Broilers. Front. Microbiol. 2021;12:623739. doi: 10.3389/fmicb.2021.623739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He L., Chen W., Liu Y. Production and partial characterization of bacteriocin-like pepitdes by Bacillus licheniformis ZJU12. Microbiol. Res. 2006;161:321–326. doi: 10.1016/j.micres.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Stoica R.M., Moscovici M., Tomulescu C., Cășărică A., Băbeanu N., Popa O., Kahraman H.A. Antimicrobial compounds of the genus Bacillus: A review. Rom. Biotechnol. Lett. 2019;24:1111–1119. doi: 10.25083/rbl/24.6/1111.1119. [DOI] [Google Scholar]
- 18.Begley M., Cotter P.D., Hill C., Ross R.P. Identification of a novel two-peptide lantibiotic, lichenicidin, following rational genome mining for LanM proteins. Appl. Environ. Microbiol. 2009;75:5451–5460. doi: 10.1128/AEM.00730-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Petrova P., Arsov A., Ivanov I., Tsigoriyna L., Petrov K. New Exopolysaccharides Produced by Bacillus licheniformis 24 Display Substrate-Dependent Content and Antioxidant Activity. Microorganisms. 2021;9:2127. doi: 10.3390/microorganisms9102127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hertadi R., Umriani Permatasari N., Ratnaningsih E. Box-Wilson Design for Optimization of in vitro Levan Production and Levan Application as Antioxidant and Antibacterial Agents. Iran. Biomed. J. 2021;25:202–212. doi: 10.52547/ibj.25.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Permatasari N.U., Ratnaningsih E., Hertadi R. Molecular cloning and expression of levansucrase gene from Bacillus licheniformis BK1 isolated from Bledug Kuwu Mud Crater. EurAsian J. Biosci. 2019;13:223–230. [Google Scholar]
- 22.Nerurkar A.S. Structural and molecular characteristics of lichenysin and its relationship with surface activity. In: Sen R., editor. Biosurfactants. 1st ed. Volume 1. Springer; New York, NY, USA: 2010. pp. 304–315. [DOI] [PubMed] [Google Scholar]
- 23.Roy A. A Review on the Biosurfactants: Properties, Types and its Applications. J. Fundam. Renew. Energy Appl. 2017;8:1000248. doi: 10.4172/2090-4541.1000248. [DOI] [Google Scholar]
- 24.Jiang H., Dong H., Zhang G., Yu B., Chapman L.R., Fields M.W. Microbial diversity in water and sediment of Lake Chaka, an athalassohaline lake in northwestern China. Appl. Environ. Microbiol. 2006;72:3832–3845. doi: 10.1128/AEM.02869-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang C.H., Chang M.T., Huang L., Chu W.S. Development of a novel PCR assay based on the gyrase B gene for species identification of Bacillus licheniformis. Mol. Cell. Probes. 2012;26:215–217. doi: 10.1016/j.mcp.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Huang Q., Baum L., Fu W.L. Simple and practical staining of DNA with GelRed in agarose gel electrophoresis. Clin. Lab. 2010;56:149–152. [PubMed] [Google Scholar]
- 27.McGinnis S., Madden T.L. BLAST: At the core of a powerful and diverse set of sequence analysis tools. Nucleic Acids Res. 2004;32:W20–W25. doi: 10.1093/nar/gkh435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadanand R.L.N., Raghunath P. Prevalence and antibiotic susceptibility of Streptococcus pyogenes isolated from pyoderma in a tertiary care hospital, Hyderabad, South India. Indian J. Microbiol. Res. 2021;8:274–278. doi: 10.18231/j.ijmr.2021.056. [DOI] [Google Scholar]
- 29.Morikawa M., Hirata Y., Imanaka T. A study on the structure-function relationship of lipopeptide biosurfactants. Biochim. Biophys. Acta. 2000;1488:211–218. doi: 10.1016/S1388-1981(00)00124-4. [DOI] [PubMed] [Google Scholar]
- 30.Nakapong S., Pichyangkura R., Ito K., Iizuka M., Pongsawasdi P. High expression level of levansucrase from Bacillus licheniformis RN-01 and synthesis of levan nanoparticles. Int. J. Biol. Macromol. 2013;54:30–36. doi: 10.1016/j.ijbiomac.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 31.Prieto M.L., O’Sullivan L., Tan S.P., McLoughlin P., Hughes H., O’Connor P.M., Cotter P.D., Lawlor P.G., Gardiner G.E. Assessment of the bacteriocinogenic potential of marine bacteria reveals lichenicidin production by seaweed-derived Bacillus spp. Mar. Drugs. 2012;10:2280–2299. doi: 10.3390/md10102280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bolocan A.S., Pennone V., O’Connor P.M., Coffey A., Nicolau A.I., McAuliffe O., Jordan K. Inhibition of Listeria monocytogenes biofilms by bacteriocin-producing bacteria isolated from mushroom substrate. J. Appl. Microbiol. 2017;122:279–293. doi: 10.1111/jam.13337. [DOI] [PubMed] [Google Scholar]
- 33.Nieminen T., Rintaluoma N., Andersson M., Taimisto A.M., Ali-Vehmas T., Seppälä A., Priha O., Salkinoja-Salonen M. Toxinogenic Bacillus pumilus and Bacillus licheniformis from mastitic milk. Vet. Microbiol. 2007;124:329–339. doi: 10.1016/j.vetmic.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 34.Yang K.M., Kim J.S., Kim H.S., Kim Y.Y., Oh J.K., Jung H.W., Park D.S., Bae K.H. Lactobacillus reuteri AN417 cell-free culture supernatant as a novel antibacterial agent targeting oral pathogenic bacteria. Sci. Rep. 2021;11:1631. doi: 10.1038/s41598-020-80921-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Özavci V., Erbas G., Parin U., Yüksel H.T., Kirkan Ş. Molecular detection of feline and canine periodontal pathogens. Vet. Anim. Sci. 2019;8:100069. doi: 10.1016/j.vas.2019.100069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin Y., Zhou X., Li Y. Strategies for Streptococcus mutans biofilm dispersal through extracellular polymeric substances disruption. Mol. Oral Microbiol. 2022;37:1–8. doi: 10.1111/omi.12355. [DOI] [PubMed] [Google Scholar]
- 37.Messora M.R., Pereira L.J., Foureaux R., Oliveira L.F., Sordi C.G., Alves A.J., Napimoga M.H., Nagata M.J., Ervolino E., Furlaneto F.A. Favourable effects of Bacillus subtilis and Bacillus licheniformis on experimental periodontitis in rats. Arch. Oral Biol. 2016;66:108–119. doi: 10.1016/j.archoralbio.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 38.Alkaya B., Laleman I., Keceli S., Ozcelik O., Cenk Haytac M., Teughels W. Clinical effects of probiotics containing Bacillus species on gingivitis: A pilot randomized controlled trial. J. Periodontal Res. 2017;52:497–504. doi: 10.1111/jre.12415. [DOI] [PubMed] [Google Scholar]
- 39.Cheng L., Zhang L., Yue L., Ling J., Fan M., Yang D., Huang Z., Niu Y., Liu J., Zhao J., et al. Expert consensus on dental caries management. Int. J. Oral Sci. 2022;14:17. doi: 10.1038/s41368-022-00167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ratna Sudha M., Neelamraju J., Surendra Reddy M., Kumar M. Evaluation of the Effect of Probiotic Bacillus coagulans Unique IS2 on Mutans Streptococci and Lactobacilli Levels in Saliva and Plaque: A Double-Blind, Randomized, Placebo-Controlled Study in Children. Int. J. Dent. 2020;2020:8891708. doi: 10.1155/2020/8891708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rivis O., Kryvtsova M., Nikolajchuk V. Antagonistic activity of Bacillus probiotics against bacteria isolates of oral cavity of patients with periodontitis. Vìsn. Dnìpropetr. Unìv. Ser. Bìol. Med. 2013;4:10–13. [Google Scholar]
- 42.Martins K.S., Magalhães L.T.A., de Almeida J.G., Pieri F.A. Antagonism of Bacteria from Dog Dental Plaque against Human Cariogenic Bacteria. BioMed Res. Int. 2018;2018:2780948. doi: 10.1155/2018/2780948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin P., Tan Z., Wang H., Liu W., Miao W. Antimicrobial effect of Bacillus licheniformis HN-5 bacitracin A on rice pathogen Pantoea ananatis. BioControl. 2021;66:249–257. doi: 10.1007/s10526-020-10052-9. [DOI] [Google Scholar]
- 44.Wang Y., Luo Q., Xiao T., Zhu Y., Xiao Y. Impact of Polymyxin Resistance on Virulence and Fitness among Clinically Important Gram-Negative Bacteria. Engineering. 2022;13:178–185. doi: 10.1016/j.eng.2020.11.005. [DOI] [Google Scholar]
- 45.Tran C., Cock I.E., Chen X., Feng Y. Antimicrobial Bacillus: Metabolites and Their Mode of Action. Antibiotics. 2022;11:88. doi: 10.3390/antibiotics11010088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anumala D., Pasupuleti M.K., Nagireddy R.R. Detection and Characterization of Prevotella Intermedia and Its In Vitro Susceptibility to Selected Antimicrobial Agents in Chronic Periodontitis and Acute Myocardial Infarction. Perio J. 2019;3:1–6. doi: 10.26810/perioj.2019.a1. [DOI] [Google Scholar]
- 47.Ahire J.J., Kashikar M.S., Lakshmi S.G., Madempudi R. Identification and characterization of antimicrobial peptide produced by indigenously isolated Bacillus paralicheniformis UBBLi30 strain. 3 Biotech. 2020;10:112. doi: 10.1007/s13205-020-2109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kazemi S., Heidari B., Rassa M. Antibacterial and hemolytic effects of aqueous and organic extracts from different tissues of sea urchin Echinometra mathaei on pathogenic streptococci. Int. Aquat. Res. 2016;8:299–308. doi: 10.1007/s40071-016-0143-0. [DOI] [Google Scholar]
- 49.Nagasawa R., Sato T., Nomura N., Nakamura T., Senpuku H. Potential Risk of Spreading Resistance Genes within Extracellular-DNA-Dependent Biofilms of Streptococcus mutans in Response to Cell Envelope Stress Induced by Sub-MICs of Bacitracin. Appl. Environ. Microbiol. 2020;86:e00770-20. doi: 10.1128/AEM.00770-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zaidi S., Bhardwaj T., Somvanshi P., Khan A.U. Proteomic Characterization and Target Identification Against Streptococcus mutans Under Bacitracin Stress Conditions Using LC-MS and Subtractive Proteomics. Protein J. 2022;41:166–178. doi: 10.1007/s10930-021-10038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bahaddad S.A., Almalki M., Alghamdi O.A., Sohrab S.S., Yasir M., Azhar E.I., Chouayekh H. Bacillus Species as Direct-Fed Microbial Antibiotic Alternatives for Monogastric Production. Probiotics Antimicrob. Proteins. 2022:1–16. doi: 10.1007/s12602-022-09909-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sitthiyotha T., Pichyangkura R., Chunsrivirot S. Molecular dynamics provides insight into how N251A and N251Y mutations in the active site of Bacillus licheniformis RN-01 levansucrase disrupt production of long-chain levan. PLoS ONE. 2018;13:e0204915. doi: 10.1371/journal.pone.0204915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hundschell C.S., Braun A., Wefers D., Vogel R.F., Jakob F. Size-Dependent Variability in Flow and Viscoelastic Behavior of Levan Produced by Gluconobacter albidus TMW 2.1191. Foods. 2020;9:192. doi: 10.3390/foods9020192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ağçeli G.K., Cihangir N. Nano-sized biopolymer levan: Its antimicrobial, anti-biofilm and anti-cancer effects. Carbohydr. Res. 2020;494:108068. doi: 10.1016/j.carres.2020.108068. [DOI] [PubMed] [Google Scholar]
- 55.Gomaa E.Z. Antimicrobial Activity of a Biosurfactant Produced by Bacillus licheniformis Strain M104 Grown on Whey. Braz. Arch. Biol. Technol. 2013;56:259–268. doi: 10.1590/S1516-89132013000200011. [DOI] [Google Scholar]
- 56.Dischinger J., Josten M., Szekat C., Sahl H.G., Bierbaum G. Production of the Novel Two-Peptide Lantibiotic Lichenicidin by Bacillus licheniformis DSM 13. PLoS ONE. 2009;4:e6788. doi: 10.1371/journal.pone.0006788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barbosa J.C., Silva Í.C., Caetano T., Mösker E., Seidel M., Lourenço J., Süssmuth R.D., Santos N.C., Gonçalves S., Mendo S. Assessing the potential of the two-peptide lantibiotic lichenicidin as a new generation antimicrobial. World J. Microbiol. Biotechnol. 2022;38:18. doi: 10.1007/s11274-021-03196-y. [DOI] [PubMed] [Google Scholar]
- 58.Abriouel H., Franz C.M., Ben Omar N., Gálvez A. Diversity and applications of Bacillus bacteriocins. FEMS Microbiol. Rev. 2011;35:201–232. doi: 10.1111/j.1574-6976.2010.00244.x. [DOI] [PubMed] [Google Scholar]
- 59.Karim R., Mahmud M., Hakim M.A. Detection of bacteriocin like substances from normal skin microflora as alternative to conventional antibiotics. Asian J. Agric. Biol. 2019;7:531–537. [Google Scholar]
- 60.Mercado V., Olmos J. Bacteriocin Production by Bacillus Species: Isolation, Characterization, and Application. Probiotics Antimicrob. Proteins. 2022 doi: 10.1007/s12602-022-09966-w. in press . [DOI] [PubMed] [Google Scholar]
- 61.Yu X.J., Han X.T., Li Y.Y., Sun Z., Dong C. Isolation, identification and prokaryotic expression of a bacteriocin-like substance from Bacillus licheniformis. Chin. J. Biotechnol. 2021;37:2453–2462. doi: 10.13345/j.cjb.210181. [DOI] [PubMed] [Google Scholar]
- 62.Zhang Y., Zhou J., Pan L., Dai Z., Liu C., Wang J., Zhou H. Production of Bacteriocin-like Substances by Bacillus spp. JY-1 in Soy Whey. Adv. Biochem. 2019;7:65–70. doi: 10.11648/j.ab.20190703.12. [DOI] [Google Scholar]
- 63.Shobharani P., Padmaja R.J., Halami P.M. Diversity in the antibacterial potential of probiotic cultures Bacillus licheniformis MCC2514 and Bacillus licheniformis MCC2512. Res. Microbiol. 2015;166:546–554. doi: 10.1016/j.resmic.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 64.Zaya N.E., Vaughan E.E., Shah S.K., Castignetti D. Bacitracin: Substantiation and elimination of contaminating proteolytic activity and use as an affinity chromatography ligand to purify a siderophore-degrading enzyme. Curr. Microbiol. 2002;44:71–74. doi: 10.1007/s00284-001-0077-6. [DOI] [PubMed] [Google Scholar]
- 65.Méndez L.R., Arrebola Y., Valdés-Tresanco M.E., Díaz-Guevara L., Bergado G., Sánchez B., Charli J.L., Pascual Alonso I. Bestatin and bacitracin inhibit porcine kidney cortex dipeptidyl peptidase IV activity and reduce human melanoma MeWo cell viability. Int. J. Biol. Macromol. 2020;164:2944–2952. doi: 10.1016/j.ijbiomac.2020.08.157. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.