Abstract
Although infection with human papillomavirus (HPV) is associated with nearly all cervical cancers (CC), a small proportion are HPV-negative. Recently, it has become clear that HPV-negative CC represent a distinct disease phenotype compared to HPV-positive disease and exhibit increased mortality. In addition, variations between different HPV types associated with CC have been linked to altered molecular pathology and prognosis. We compared the immune microenvironments of CC caused by HPV α9 species (HPV16-like), HPV α7 species (HPV18-like) and HPV-negative disease. HPV-negative CC appeared distinct from other subtypes, with greatly reduced levels of lymphocyte infiltration compared to either HPV α9 or α7 CC. Besides reduced levels of markers indicative of B, T, and NK lymphocytes, the expression of T-cell effector molecules, activation/exhaustion markers, and T-cell receptor diversity were also significantly lower in HPV-negative CC. Interestingly, HPV-negative CC expressed much higher levels of potential neoantigens than HPV-positive CC. These results identify profound differences between the immune landscape of HPV-positive and HPV-negative CC as well as modest differences between HPV α9 and α7 CC. These differences may contribute to altered patient outcomes between HPV-negative and HPV-positive CC and potentially between CC associated with different HPV types.
Keywords: human papillomavirus, cervical cancer, TCGA, gene expression, immune landscape, immune exhaustion, T-cell function, tumor immunology, neoantigens, TCR repertoire
1. Introduction
Worldwide, cervical cancer (CC) is the fourth most prevalent cancer in women, with over 600,000 new cases and 340,000 deaths in 2020 [1]. CC remains a leading cause of cancer death in younger women in economically disadvantaged countries [1]. Infection with human papillomavirus (HPV) is associated with 85–90% of CC [2,3], with no clear etiology for HPV-negative CC [4]. HPVs are highly transmissible, representing the most common sexually transmitted infection in North America [5]. Of the over 400 known HPV types, 30 preferentially infect the anogenital mucosa, resulting in papillomas (warts) [6,7]. A subset of HPV-induced lesions of the cervix progresses to carcinoma, commonly as a result of damage to the viral genome, leading to random integration into the host genome. This often leads to a constitutively elevated level of expression of the viral E6 and E7 oncogenes in CC [7].
Of the various cancer-causing HPV types, HPV16 is the predominant species, accounting for nearly 60% of all CC [2,3]. HPV16 is a member of the α9 family, which includes the closely related types HPV31, 33, 35, 52, 58, and 67 [6]. Statistically, HPV18 and HPV45 exhibit the second and third highest association with CC, accounting for ~10% and ~5% of cases, respectively [2,3]. HPV18 and 45 are members of the α7 family, which includes closely related types HPV39, 59, 68, 70, 85, and 97 [6]. Patients with HPV-positive CC appear to have a more favorable prognosis than their HPV-negative counterparts [8,9,10,11], and it is clear that HPV-positive and HPV-negative diseases are clinically and pathologically distinct [12,13]. Although somewhat controversial, patient outcomes for HPV16-positive CC appear superior to those that are HPV18-positive [10,14,15,16]. From a tumor virus perspective, these results may not be surprising, given the divergence in sequence and molecular function between the oncogenes encoded by the different HPV types [17].
The aim of this study was to compare the tumor immune landscape between HPV α9, HPV α7, and HPV-negative CC, with the goal of identifying differences that have implications in the diagnosis, prognosis, and treatment of these cancers. Despite the differences in pathology and clinical outcomes between HPV-positive and HPV-negative CC, few studies have directly compared the tumor immune landscapes between these distinct cancers of the cervix [18,19]. Given the tremendous impact that T-cell-targeting immune checkpoint inhibitors have had on cancer treatment [20] and the recent approval of these drugs for some CC [21], we undertook a detailed T-cell-centric analysis of the tumor immune landscape differences between HPV α9 (HPV16-like), HPV α7 (HPV18-like), and HPV-negative CC. Significantly increased T-cell infiltration, T-cell receptor (TCR) repertoire diversity, effector gene expression, activation status, and exhaustion marker expression were observed in both α9 and α7 HPV-positive CC as compared to HPV-negative CC. These observations provide strong evidence that the immune landscape of HPV-negative CC exhibits a distinct immune-cold phenotype compared to the corresponding HPV-positive disease. Intriguingly, HPV-negative CCs express a larger array of potential neoantigens compared to HPV-positive CC, which typically increases the likelihood of T-cell recognition, and is often associated with improved clinical outcomes [22]. These differences in the immune landscape may contribute to increased mortality associated with HPV-negative CC and suggest that it may be less amenable to immunomodulatory interventions such as immune checkpoint inhibitors.
2. Materials and Methods
2.1. Sample Collection and Ethics
All data from The Cancer Genome Atlas (TCGA) were downloaded via the Broad Genome Data Analysis Center’s Firehose server (https://gdac.broadinstitute.org/, accessed on 2 March 2017) or other publicly available sources as noted below; therefore, no ethical approval was needed.
2.2. Analysis of Cellular mRNA Expression
Level 3 mRNA expression data for the TCGA CC dataset was sourced from Broad Genome Data Analysis Center’s Firehose server (https://gdac.broadinstitute.org/, accessed on 2 March 2017), with the datasets manually annotated for HPV status [18,23,24]. For samples infected with multiple HPV types, the genotype with the highest expression was selected [25]. The CC RNA-sequencing dataset is comprised of 278 HPV-positive, 19 HPV-negative, and 3 normal control tissues. Of these, there are 165 HPV16-, 40 HPV18-, 1 HPV30-, 6 HPV31-, 9 HPV33-, 6 HPV35-, 5 HPV39-, 22 HPV45-, 1 HPV51-, 8 HPV52-, 1 HPV56-, 6 HPV58-, 3 HPV59-, 2 HPV68-, 1 HPV69-, 1 HPV70-, and 1 HPV73-positive samples. The correlation of cellular gene mRNA expression and HPV status was performed via sorting the dataset into 200 HPV α9 (HPV16, 31, 33, 35, 52, and 58 types; 200 samples total), HPV α7 (HPV18, 39, 45, 59, 68, and 70 types; 73 samples total) and HPV-negative CC (19 samples total) or normal (non-cancerous; 3 samples total) subsets, with subsequent calculations performed with R’s built-in wilcox.test function with the conf.level parameter set to 0.95. q-Values were calculated for each comparison group with a false discovery rate (FDR) of 10%.
2.3. Analysis of Immune Landscape Features
Selected immune landscape features for the TCGA CC datasets were extracted from Thorsson et al. [26] and similarly analyzed as above via sorting the samples into HPV α9, HPV α7, and HPV-negative CC subsets. As not all data necessary for the calculation of each immune landscape feature were available for all individual TCGA samples, these comparisons include only 196 HPV α9, 72 HPV α7 and 18 HPV-negative CC. HPV integration status was extracted from Qiu et al. [18] and used to compare immune landscape features between CC samples with integrated vs. non-integrated HPV genomes. This work identified 163 integrated and 29 non-integrated HPV α9 CC and 67 integrated and 1 non-integrated HPV α7 CC. Immune landscape comparisons between CC and head and neck cancers utilized TCGA level 3 mRNA expression data sourced from Broad Genome Data Analysis Center’s Firehose server (https://gdac.broadinstitute.org/, accessed on 2 March 2017), that was manually annotated for HPV status as described [27].
2.4. Survival Analysis
Survival analyses utilized the TCGA overall survival (OS) data from Liu et al. [28]. The correlation of survival and cellular gene mRNA expression was performed via sorting the dataset into HPV α9 and α7 subsets. Patients were dichotomized by median expression of CD96, CTLA4, LAG3, PD1, TIGIT, TIM3, CD39, or CD73, with subsequent calculations performed via the coxph and Surv functions, both available via the R survival packages.
3. Results
3.1. HPV-Positive and HPV-Negative CC Exhibit Strong Differences in Lymphocyte Infiltration
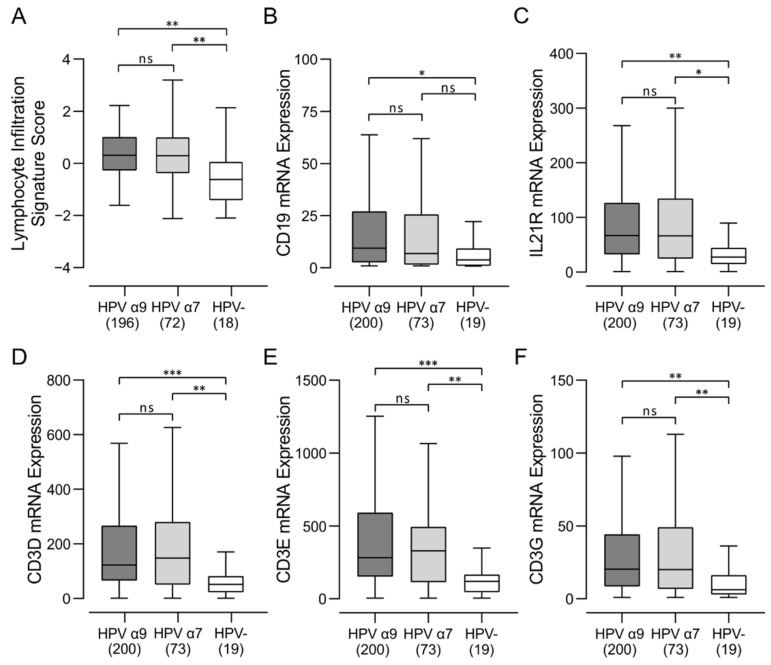
Recent breakthroughs in cancer immunotherapy have clearly demonstrated the critical role of various immune mechanisms in controlling many different types of malignancies. The number, localization, and phenotypes of tumor-infiltrating lymphocytes (TILs) provides insight into the tumor immune landscape and may help predict response to immunotherapy [29]. We first started to explore the differences in the immune landscape between HPV-positive and HPV-negative CC by analyzing the TCGA Illumina HiSeq mRNA expression data from the CC cohort using a previously described Lymphocyte Infiltration Signature Score [26]. Samples from this cohort were divided into HPV α9 (HPV16-like; 196 samples), HPV α7 (HPV18-like; 72 samples) and HPV-negative CC (18 samples). Both groups of HPV-positive samples exhibited dramatically greater scores for lymphocyte infiltration compared to HPV-negative samples, indicative of substantial differences in the presence of TILs between HPV-positive CC compared to HPV-negative CC regardless of HPV type (Figure 1A). In this respect, HPV-negative CC appear to represent an immune-cold microenvironment, with characteristics of an immune-excluded tumor [30]. However, this mRNA based signature provides no spatial context for the localization of the lymphocytes within and around the tumor, which plays a critical role in immune effects against the tumor [29].
Figure 1.
Analysis of tumor infiltrating lymphocytes and subsets in HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancer. (A) Comparison of Lymphocyte Infiltration Signature Score between HPV α9, HPV α7, and HPV-negative cervical cancers. Values were extracted from Thorsson et al. [26] and HPV status annotated manually; (B–F) expression of marker genes related to B-cell (CD19, IL21R) and T-cell (CD3D, CD3E, CD3G) infiltration. Numbers in brackets refer to the number of samples included in each analysis. *** p ≤ 0.001, ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
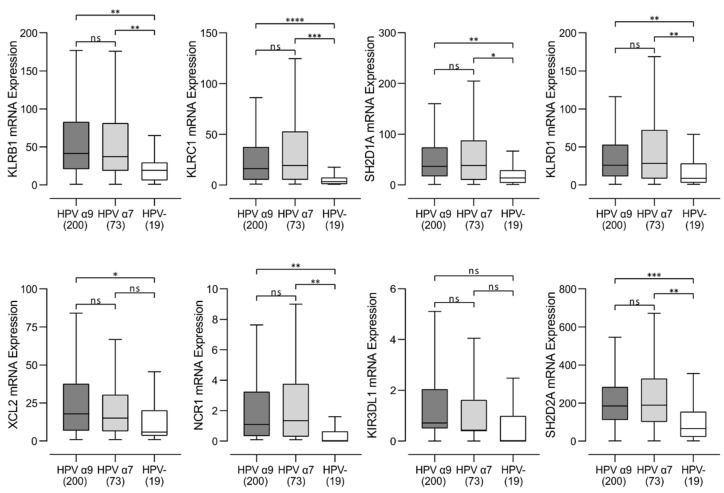
3.2. Higher Levels of B, T, and NK Lymphocytes Are Present in HPV-Positive CC
We next assessed the relative proportions of B, T, and NK lymphocytes in these CC samples, based on relative expression of mRNAs encoding lineage defining marker genes. We used the levels of CD19 and IL21R mRNA as measures of B-cell infiltration and CD3D, CD3E, and CD3G for T-cell infiltration and numerous markers for NK cells (Figure 1B–F and Figure 2). Values for normalized mRNA expression levels were available for 200 HPV α9, 73 HPV α7, and 19 HPV-negative CC. Higher levels of these markers of B, T, and NK cells were typically observed in HPV-positive CC compared to HPV-negative CC, regardless of HPV type.
Figure 2.
Transcript levels of NK cell marker genes in HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancer. Normalized RNA-seq data was extracted from The Cancer Genome Atlas (TCGA) database for cervical cancer cohort. Numbers in brackets refer to the number of samples included in each analysis. **** p ≤ 0.0001, *** p ≤ 0.001, ** p ≤ 0.01, * p = 0.05, ns (not significant).
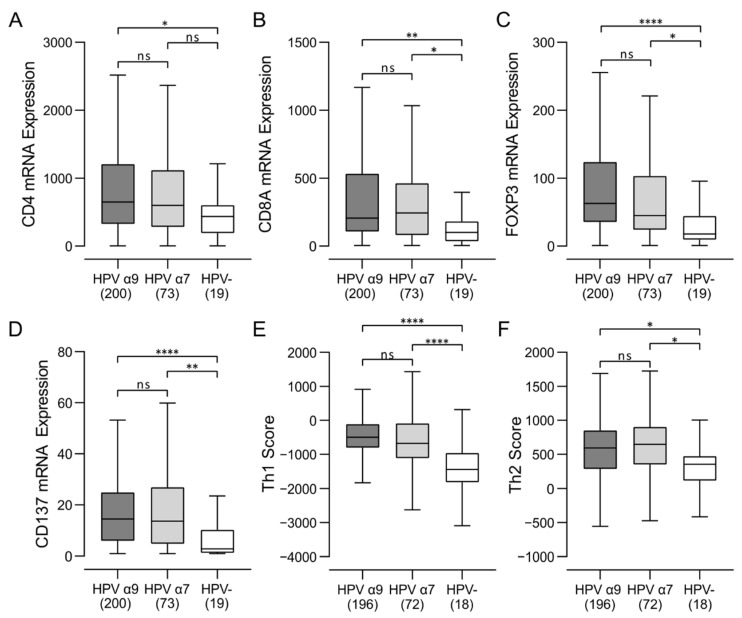
3.3. Higher Levels of CD4+, CD8+ T Cells, and T Regulatory Cells Were Present in HPV-Positive CC
We next assessed the relative proportion of CD4+, CD8+ T cells and T regulatory cells (Tregs) in these samples, based on relative expression of the lineage defining CD4, CD8A, and FOXP3 marker genes, respectively (Figure 3). HPV-positive samples showed significantly increased expression of all three genes versus HPV-negative CC, confirming that enhanced infiltration by CD4+ T helper cells, CD8+ cytotoxic T cells, and Tregs are a common feature of HPV-positive CC as compared to HPV-negative samples. CD4+ T helper signatures suggest that all CC is biased towards a humoral Th2, rather than cell-mediated Th1 response, although both are upregulated in HPV-positive samples compared to HPV-negative CC. Furthermore, CD137 (4-1BB), an activation-induced costimulatory molecule present primarily on CD8+ T cells, was expressed at significantly higher levels in HPV-positive CC as compared to HPV-negative CC, suggesting a higher overall level of T-cell activation in HPV-positive CC (Figure 3).
Figure 3.
Analysis of T-cell populations in HPV-positive and HPV-negative cervical cancers. (A–C) Expression of marker genes related to CD4+ helper (CD4), CD8+ cytotoxic (CD8A), and Treg (FOXP3) cells; (D) expression of CD137 (TNFRSF9/4-1BB), an activation-induced costimulatory molecule present primarily on CD8+ T cells. (E,F) Comparison of CD4+ helper Th1 and Th2 Signature Score between HPV α9, HPV α7, and HPV-negative (HPV-) cervical cancers. Numbers in brackets refer to the number of samples included in each analysis. **** p ≤ 0.0001, ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
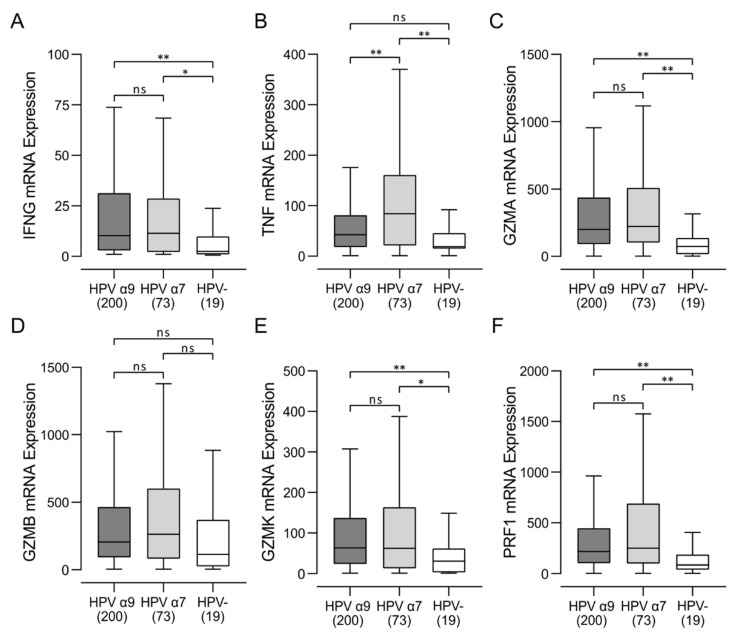
3.4. HPV-Positive CC Expressed Higher Levels of Multiple T-Cell Effector Molecules Than HPV-Negative CC with Characteristics of a T-Cell-Inflamed Phenotype
Activated cytotoxic CD8+ T cells produce various effector molecules, including IFN-γ and TNF. Although expression of IFN-γ and TNF mRNAs in these samples was low, it was detected at significantly higher levels in HPV-positive versus HPV-negative CC (Figure 4). HPV-positive CC tumors also expressed significantly higher levels of cytotoxic mediators, including granzyme A (GZMA), granzyme B (GZMB), granzyme K (GZMK), and perforin (PRF1) compared to HPV-negative CC (Figure 4). Taken together, these results indicate that CD8+ T cells are not only present at higher levels in HPV-positive CC but are concomitantly more active and actively produce effector molecules such as IFN-γ, TNF, granzymes, and perforin.
Figure 4.
Transcript levels of lymphocyte effector molecules in HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancers. (A–F) Expression of marker genes related to activated cytotoxic CD8+ T cells, including IFN-γ (IFNG), TNF-α (TNF), granzyme A (GZMA), granzyme B (GZMB), granzyme K (GZMK), and perforin (PRF1). Numbers in brackets refer to the number of samples included in each analysis. ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
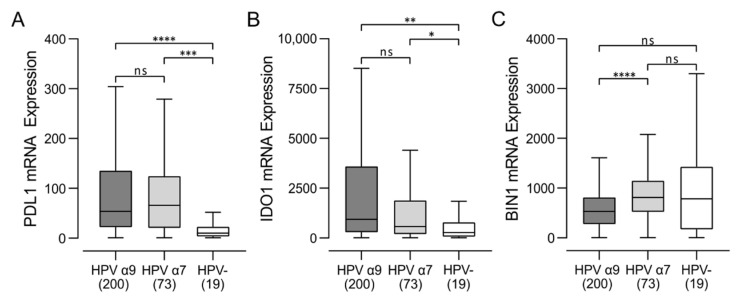
Increased T-cell infiltration and higher levels of effector gene expression in HPV-positive CC indicates that these tumors exhibit many characteristics of T-cell-inflamed tumors [30]. Indeed, HPV-positive CC express high levels of the immune regulatory genes including PDL1 and IDO (Figure 5), another distinctive characteristic of the T-cell-inflamed tumor phenotype. We noted that expression of BIN1, a negative regulator of IDO1 expression [31], was significantly downregulated in HPV α9 CC, which express the highest levels of IDO1 (Figure 5). Overall, these data indicate that HPV-positive CC, in treatment-naïve patients, exhibits characteristics resembling a T-cell-inflamed phenotype compared to their HPV-negative counterparts (Figure 3 and Figure 4).
Figure 5.
Transcript levels of tumor-derived interferon-responsive immunomodulatory genes in cervical cancer. Normalized RNA-seq data for genes associated with tumor cell mediated immunomodulation, including (A) PDL1 (CD274), (B) IDO1, and (C) its negative regulator BIN1, were compared between HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancers. Numbers in brackets refer to the number of samples included in each analysis. **** p ≤ 0.0001, *** p ≤ 0.001, ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
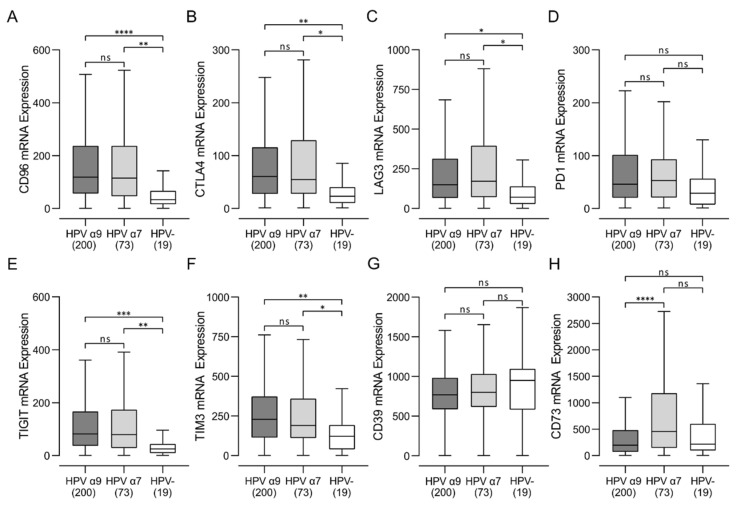
3.5. HPV-Positive CC Express High Levels of Multiple Immune Checkpoint Markers
Once activated, T cells upregulate expression of multiple cell surface receptors that negatively regulate their proliferation and moderate their level of activation [32]. These immune checkpoint/exhaustion markers include CD96, CTLA4, LAG3, PD1, TIGIT, and TIM3, and a high expression level of these markers is another distinctive characteristic of T-cell-inflamed tumors [30]. These gene products are also important targets for immune checkpoint inhibitors that are approved, or under development. Notably, all these checkpoint genes, except for PD1, were significantly upregulated in HPV-positive CC compared with HPV-negative CC (Figure 6). Although a trend of increased PD1 expression was also present for HPV-positive versus HPV-negative CC, this was not statistically significant. Taken together, HPV-positive CC displays a markedly increased T-cell exhaustion signature from HPV-negative CC, indicative of sustained CD8+ T-cell activation reminiscent of a T-cell-inflamed phenotype. In contrast HPV-negative CC appear dramatically less immune-infiltrated, with a T-cell-excluded microenvironment.
Figure 6.
Analysis of immune checkpoint markers in HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancers. (A–F) Expression of marker genes related to T-cell exhaustion markers, including CD96, CTLA4, LAG3, PD1 (PDCD1), TIGIT, and TIM3 (HAVCR2). (G,H) Expression of marker genes related to immunosuppressive purinergic signals including CD39 (ENTPD1) and CD73 (NT5E). Numbers in brackets refer to the number of samples included in each analysis. **** p ≤ 0.0001, *** p ≤ 0.001, ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
We also examined the expression of the immunosuppressive molecule CD39 (ENTPD1) and its companion molecule CD73 (NT5E) in this cohort of patients. CD39 and CD73 encode enzymes that help calibrate the duration, magnitude, and chemical nature of purinergic signals delivered to immune cells. Together they control the shift from an ATP-driven proinflammatory environment to an adenosine-induced anti-inflammatory milieu [33]. Although their expression in Treg lymphocytes is induced by TCR activation [33], they can also be expressed by tumor cells and myeloid cells [34]. While CD73 showed significantly higher RNA expression levels in HPV α7-positive CC tumors compared to HPV α9 and HPV-negative CC samples, CD39 was not differentially expressed (Figure 6).
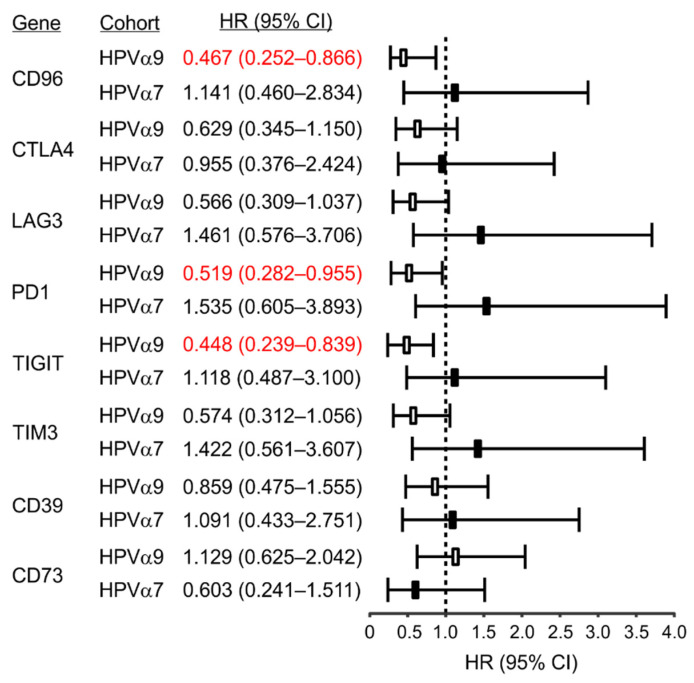
Intriguingly, high expression of each of the five exhaustion factors, but not CD39 or CD73, was associated with a trend in reduced mortality in HPV α9 CC, which was significant for CD96, PD1, and TIGIT (Figure 7; see Figure S1). This correlation with survival further supports a critical role of T-cell activation in HPV α9 CC resolution. In contrast, no significant associations between exhaustion markers and survival were seen for HPV α7. While not significant, high expression of these markers trended towards increased mortality in HPV α7 CC (Figure 7). No correlations were performed for HPV-negative CC as the sample size was too small for statistical analysis.
Figure 7.
Correlation of immune checkpoint markers with patient mortality in HPV-positive (HPV α9 and HPV α7) cervical cancer. Hazard ratios (HR) and 95% confidence intervals (CI) related to immune checkpoint/T-cell exhaustion marker expression for CD96, CTLA4, LAG3, PD1 (PDCD1), TIGIT, TIM3 (HAVCR2), and genes related to immunosuppressive purinergic signals, including CD39 (ENTPD1) and CD73 (NT5E), were calculated. Numbers indicated in red are statistically significant.
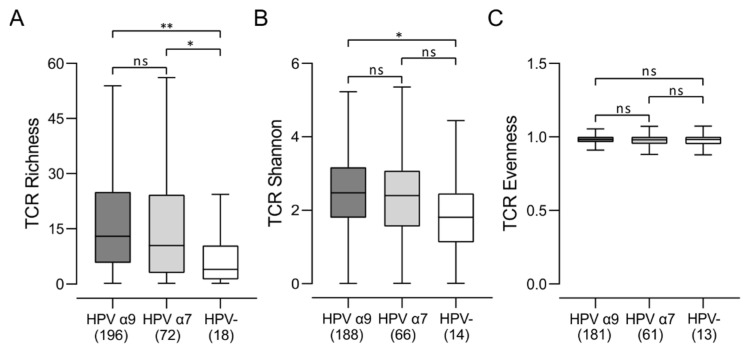
3.6. Comparison of the T-Cell Receptor Repertoire between HPV-Positive and HPV-Negative CC
There is increasing evidence that analysis of TCR repertoire using deep sequencing approaches can serve as a biomarker of immune response in cancer patients [35]. We next compared the characteristics of the TCR repertoire between HPV-positive CC and HPV-negative CC (Figure 8). In terms of unique TCR sequences in the TCR repertoire (richness), both HPV α9 and HPV α7 CC groups showed an increased number of T-cell clones, as compared to HPV-negative CC. Measurements of clonal diversity weighted by the abundance of each complementarity-determining region 3 (CDR3; Shannon entropy) [36] revealed greater diversity in HPV α9 vs. HPV-negative CC, with a similar trend observed for HPV α7 CC. The distribution spectrum of these sequences, reflecting the relative abundance of individual T-cell clones (evenness), showed no significant differences between either group of HPV-positive CC or HPV-negative CC. These results indicate that the TCR repertoire in HPV-positive CC is significantly wider and more diverse than HPV-negative CC.
Figure 8.
Comparison of the T-cell receptor (TCR) repertoire between HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancers. (A) Comparison of unique TCR sequences in the TCR repertoire (richness); (B) comparison of clonal diversity weighted by the abundance of each complementarity-determining region 3 (Shannon entropy); (C) comparison of the distribution spectrum of TCR sequences, reflecting the relative abundance of individual T-cell clones (evenness). Numbers in brackets refer to the number of samples included in each analysis. ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
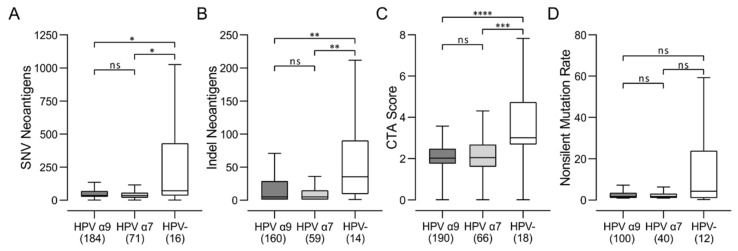
3.7. HPV-Negative CC Express High Levels of Potential Neoantigens
HPV-positive CC maintain expression of various viral proteins, particularly those encoded by the E6 and E7 oncogenes [7]. These viral proteins are recognized as foreign antigens by the human immune system, likely enhancing T-cell responses in HPV-positive CC [37]. Epitope spreading from one dominant viral antigen to another, or to cell-derived tumor-associated antigens, may enhance tumor cell clearance [38]. T-cell recognition of HPV-negative CC, which by definition do not express any foreign viral antigens, will depend on neoantigens derived from mutated cellular genes or aberrant expression of cancer testis antigens (CTAs), which are immunogenic, highly cancer-specific proteins normally only expressed in immune-privileged testis germ cells [39,40]. We compared the levels of potential neoantigens between HPV α9, HPV α7, and HPV-negative CC (Figure 9). HPV-negative CC are predicted to express higher levels of single-nucleotide variant (SNV) neoantigens, insertion–deletion (indel) neoantigens, and neoantigens related to CTA score compared to their HPV-positive counterparts. There was also a trend towards higher nonsilent mutation rates, although this was not significant (Figure 9D). Thus, HPV-negative CC exhibit a higher calculated level of neoantigens than HPV-positive CC and have at least the theoretical potential to be readily recognized by the adaptive immune system via these neoantigens.
Figure 9.
Comparison of the levels of potential neoantigens in HPV-positive (HPV α9 and HPV α7) and HPV-negative (HPV-) cervical cancers. Predicted levels of (A) single-nucleotide variant (SNV) neoantigens; (B) insertion–deletion (indel) neoantigens; (C) cancer testis antigen (CTA) score; and (D) non-silent mutations. Numbers in brackets refer to the number of samples included in each analysis. **** p ≤ 0.0001, *** p ≤ 0.001, ** p ≤ 0.01, * p ≤ 0.05, ns (not significant).
3.8. Comparison of the Immune Landscape between HPV α9-Positive CC with Integrated or Non-Integrated Viral Genomes
While the HPV genome is maintained episomally in a normal infection, integration into the host cell genome is a frequent event in CC [7]. The impact of integration of the viral genome on CC prognosis has been suggested to be negatively correlated with patient outcomes [41], although recent data do not fully support this conclusion [42]. We directly compared all the immune related parameters from this study between HPV α9-positive CC with integrated viral genomes and HPV α9-positive CC with non-integrated viral genomes. No significant differences were observed (Table S2). A similar comparison could not be performed for HPV α7-positive CC as all but one of the 68 samples was integrated [18].
4. Discussion
Despite well-recognized differences between the pathology [12,13] and clinical outcomes [8,9,10,11] between HPV-positive and HPV-negative CC, few if any studies have directly compared the tumor immune microenvironment between these distinct cancers of the cervix. Cancer is a complex disease, and it has become increasingly clear that patient outcomes depend greatly on crosstalk between the tumor and its local immune microenvironment [43]. Given the tremendous impact that immune checkpoint inhibitors targeting T cells have had on cancer treatment and the recent approval of these drugs for PD-L1 positive CC [20], we undertook a detailed T-cell-centric analysis of the tumor immune landscape differences between HPV-positive and HPV-negative CC. As HPV-positive CC is commonly caused by several distinct HPV species, we also compared the tumor immune microenvironments between CC associated with HPV α9 (HPV16-like) and HPV α7 (HPV18-like), the most common HPV species involved in CC. These distinct HPV species exhibit a number of molecular differences [17] and have been associated with different patient outcomes [10,14,15,16]. Notably, immunological differences between HPV α9 and HPV α7 have also not been systematically characterized.
In this study, we report the detailed immune characterization of HPV-positive α9 and α7 CC compared to HPV-negative CC. We performed a mechanistic analysis of the tumor immune microenvironment in treatment-naïve CC using data from the TCGA cohort. However, examination of only the RNA expression levels limits the ability to accurately confirm expression levels on each cell type. We addressed this limitation by using generally accepted immune lineage-specific markers or signatures developed and published by others [26]. We found that both HPV-positive α9 and α7 CC tumors exhibited much higher lymphocyte infiltration than HPV-negative CC (Figure 1). This included higher levels of B, T, and NK lymphocytes (Figure 1 and Figure S1). Both HPV-positive α9 and α7 CC tumors exhibited increased levels of CD4+ helper T cells, CD8+ cytotoxic T cells, and Tregs, with characteristics of a predominant Th2 humoral skewed immune phenotype compared to HPV-negative CC (Figure 3). Interestingly, higher T-cell infiltration into HPV-positive tumors was accompanied with high CD137 (4-1BB) gene transcript levels, suggesting greater T-cell activation. Limited comparable data is available from other studies directly comparing these immune characteristics in CC, but higher lymphocyte infiltration is a well described phenomenon in all HPV-dependent cancers [44], and Tregs specific for HPV antigens have been recovered from CC previously [45]. Previous studies have reported that TILs recovered from CC exhibit prominent Th2 skewing, consistent with the data reported here [46,47].
In agreement with the high CD137 mRNA levels in HPV-positive CC samples, we observed higher T-cell effector production in these CC samples (Figure 4). Indeed, HPV-positive CC expressed significantly higher levels of IFN-γ, TNF, perforin, and granzymes A, B, and K compared to HPV-negative CC samples. Notably, no significant differences in the expression of any of these effectors were observed between HPV α9 and α7 CC. Notably, these values for HPV-positive CC are generally lower than in HPV-positive head and neck squamous cell carcinoma (HNSCC) [48], and a direct comparison of these values is provided in Table S1. Although the mRNA expression data lack spatial data within the tumor, these analyses allow for a preliminary analysis of the immune microenvironments of treatment-naïve CC. The identification of potential biomarkers and targets from this research will guide future endeavors to investigate the potential of these markers more thoroughly.
Given the normalization of TCGA RNA-sequencing data, our calculated values for these T-cell markers and effector genes in HPV-positive CC can be directly compared with those found in HPV-positive HNSCC and represent approximately 25–50% of those values (Table S1). Thus, while these two HPV-dependent cancers exhibit a number of similarities in terms of immune microenvironment, the magnitude of inflammation is generally lower in HPV-positive CC than HPV-positive HNSCC.
Based on these analyses, it became apparent that HPV-positive CC exhibit many characteristics of T-cell-inflamed tumors [30] although at a reduced level to their HPV-positive HNSCC counterparts (Table S1). Indeed, HPV-positive CC express high levels of the immune regulatory genes including IDO and PDL1, indicative of the T-cell-inflamed tumor phenotype (Figure 5). The presence of these immunosuppressive events is generally accompanied by increased expression of multiple T-cell immune checkpoint molecules in a T-cell-inflamed microenvironment, which are also present in HPV-positive, but not HPV-negative CC (Figure 6). Indeed, expression of CD96, CTLA4, LAG3, TIM3, PD1, and TIGIT are all substantially higher in HPV-positive CC, although significant differences were not always present, particularly for comparisons of HPV α7 CC vs. HPV-negative CC (Figure 6). This agrees well with other studies reporting high expression of CD96, PD1, CTLA4, LAG3, PD1, and TIM3 protein in CC in general [49,50,51,52]. Notably, high expression of each of these five exhaustion factors was associated with a trend in reduced mortality in HPV α9 CC, which was significant for CD96, PD1, and TIGIT (Figure 7). This is very similar to what is observed in HPV-positive HNSCC, which is primarily HPV α9 [48]. In contrast, none of the exhaustion markers were associated with reduced mortality when expressed at higher levels in HPV α7 CC. Indeed, they actually trended towards decreased survival, although this was not significant (Figure 7). These data suggest that T-cell exhaustion markers, particularly PD1 and TIGIT, may represent a useful biomarker of survival in HPV α9 CC. The trend toward the opposite clinical association of increased mortality with high exhaustion marker expression in HPV α7 CC requires further investigation in a larger cohort. However, these results suggest that the immune microenvironment is indeed different between HPV α9 and HPV α7 CC. This is also reflected in the significant increase in TNF (Figure 4) and CD73 expression in HPV α7 CC vs. HPV α9 CC (Figure 6). In contrast, no significant differences were observed between HPV α9 CC with integrated HPV versus non-integrated HPV (Table S2).
In terms of the diversity of the TCR repertoire, both HPV α7 and α9 CC exhibit a significantly wider and more diverse T-cell response than HPV-negative CC (Figure 8). HPV-negative CC also clearly show a larger array of potential neoantigens compared to HPV-positive CC, as determined by a number of independent measures, including non-silent mutations, single-nucleotide variant (SNV) neoantigens, insertion–deletion (indel) neoantigens, and CTA score (Figure 9). Thus, HPV-negative CC have at least the theoretical potential to be readily recognized by the adaptive immune system via these neoantigens yet exhibit a relatively small TCR repertoire and limited numbers of TILs. Mechanistically, increased TIL levels and activity can be associated with lower tumor clonal diversity. This may arise as a consequence of immunoediting, where selective pressure by the immune system depletes tumor cell populations expressing target neoantigens [53]. Therefore, the lower level of immune infiltration exhibited by HPV-negative CC, and the corresponding lack of immunoediting, could result in the observed larger array of potential neoantigens compared to HPV-positive CC. Alternatively, this could also be related to the observation that tumor-specific T-cell dysfunction can be driven by persistent antigen exposure [54]. These data provide further evidence that the immune landscape in HPV-negative CC is immunologically cold. As HPV-negative CC exhibits a lower level of lymphocyte infiltration compared to HPV-positive CC (Figure 1, Figure 2 and Figure S1), this could occur via the process of immune exclusion [55].
Taken together, this study provides clear evidence, for the first time, that the immune landscape of HPV-positive CC represents a distinct tumor immune microenvironment from HPV-negative CC, consistent with many characteristics of a T-cell-inflamed phenotype, although the relative levels of these markers are lower than observed in HPV-positive HNSCC (Table S1). Notably, we identified multiple mechanisms that negatively regulate the anti-tumor immune response that are significantly upregulated in the majority of HPV-positive CC cases, several of which are correlated with improved clinical outcome in HPV α9 CC. These exhaustion markers may serve as useful biomarkers for survival in HPV α9 CC, as well as targets for immunotherapies [56]. Many of these negative regulators of the immune response are under investigation in current clinical trials and HPV-positive CC has many immunological features suggesting that it would be amenable to immune checkpoint inhibition therapy.
We also identified differences in NK-cell infiltration and NK-cell-based anti-cancer therapies are emerging as potentially useful for cancer treatment [57]. Like T cells, NK cells can be engineered to express chimeric antigen receptors (CARs) directed against antigens expressed on the surface of tumor cells [58]. These CAR NK cells can be safe and effective [59], and an initial trial using a TCR directed against HPV16 E6 showed some efficacy [60]. Other therapies target NK-cell inhibitory receptors or pathways. For example, monalizumab, an anti-KLRC1 blocking antibody, has been tested in several clinical trials, either as a single agent or in combination with other therapies [61]. The significantly higher expression of KLRC1 in HPV-positive CC compared to HPV-negative CC indicates that this therapy may be a beneficial treatment in HPV-positive CC.
In addition to the changes described above, subtle differences in the immune landscapes between HPV α9 and α7 CC suggest that these cancers may not respond identically to immune checkpoint inhibition. This is potentially important, as a recent large trial of the PD1 monoclonal antibody pembrolizumab did not consider HPV status or HPV type as factors that may contribute to clinical response [62]. Given that pembrolizumab is only approved for treatment of PDL1-positive CC [21], our data suggest that it is likely being used mainly for HPV-positive CC, as HPV-negative CC appear to express much lower levels of PDL1. Ultimately, immune-predictive biomarkers may pave the way for patient stratification for immunotherapy-based treatments currently in progress [63] or promising future combination therapies against multiple T-cell checkpoints [50].
Acknowledgments
A.M.E. was supported in part by an R.G.E. Murray Scholarship. M.S. was supported in part by a F.W. Luney Graduate Entrance Scholarship in Microbiology and Immunology. We thank John Barrett for insightful discussion.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11164825/s1, Figure S1: Impact of expression of selected immune checkpoint markers on patient overall survival. Table S1: Comparison of immune marker scores between cervical cancer and head and neck cancer. Table S2: Comparison of immune marker scores between cervical cancer with integrated or non-integrated HPV α9.
Author Contributions
Conceptualization, A.M.E., M.S., S.F.G., S.M.V. and J.S.M.; methodology and formal analysis A.M.E., S.F.G. and M.S.; data curation, M.S. and J.S.M.; writing—original draft preparation, A.M.E. and J.S.M.; writing—review and editing, M.S., S.F.G. and S.M.V.; supervision, J.S.M.; funding acquisition, J.S.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by a grant from the Canadian Institutes of Health Research (PJT-173496) to J.S.M.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: Globocan Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Guan P., Howell-Jones R., Li N., Bruni L., de Sanjose S., Franceschi S., Clifford G.M. Human papillomavirus types in 115,789 HPV-positive women: A meta-analysis from cervical infection to cancer. Int. J. Cancer. 2012;131:2349–2359. doi: 10.1002/ijc.27485. [DOI] [PubMed] [Google Scholar]
- 3.de Sanjose S., Quint W.G., Alemany L., Geraets D.T., Klaustermeier J.E., Lloveras B., Tous S., Felix A., Bravo L.E., Shin H.R., et al. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11:1048–1056. doi: 10.1016/S1470-2045(10)70230-8. [DOI] [PubMed] [Google Scholar]
- 4.Fernandes A., Viveros-Carreno D., Hoegl J., Avila M., Pareja R. Human papillomavirus-independent cervical cancer. Int. J. Gynecol. Cancer. 2022;32:1–7. doi: 10.1136/ijgc-2021-003014. [DOI] [PubMed] [Google Scholar]
- 5.Weinstock H., Berman S., Cates W., Jr. Sexually transmitted diseases among American youth: Incidence and prevalence estimates, 2000. Perspect. Sex. Reprod. Health. 2004;36:6–10. doi: 10.1363/3600604. [DOI] [PubMed] [Google Scholar]
- 6.Van Doorslaer K., Li Z., Xirasagar S., Maes P., Kaminsky D., Liou D., Sun Q., Kaur R., Huyen Y., McBride A.A. The Papillomavirus Episteme: A major update to the papillomavirus sequence database. Nucleic Acids Res. 2017;45:D499–D506. doi: 10.1093/nar/gkw879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zur Hausen H. Papillomavirus infections—A major cause of human cancers. Biochim. Biophys. Acta. 1996;1288:F55–F78. doi: 10.1016/0304-419X(96)00020-0. [DOI] [PubMed] [Google Scholar]
- 8.Riou G., Favre M., Jeannel D., Bourhis J., Le Doussal V., Orth G. Association between poor prognosis in early-stage invasive cervical carcinomas and non-detection of HPV DNA. Lancet. 1990;335:1171–1174. doi: 10.1016/0140-6736(90)92693-C. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez-Carunchio L., Soveral I., Steenbergen R.D., Torne A., Martinez S., Fuste P., Pahisa J., Marimon L., Ordi J., del Pino M. HPV-negative carcinoma of the uterine cervix: A distinct type of cervical cancer with poor prognosis. BJOG. 2015;122:119–127. doi: 10.1111/1471-0528.13071. [DOI] [PubMed] [Google Scholar]
- 10.Onuki M., Matsumoto K., Tenjimbayashi Y., Tasaka N., Akiyama A., Sakurai M., Minaguchi T., Oki A., Satoh T., Yoshikawa H. Human papillomavirus genotype and prognosis of cervical cancer: Favorable survival of patients with HPV16-positive tumors. Papillomavirus Res. 2018;6:41–45. doi: 10.1016/j.pvr.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lei J., Ploner A., Lagheden C., Eklund C., Nordqvist Kleppe S., Andrae B., Elfstrom K.M., Dillner J., Sparen P., Sundstrom K. High-risk human papillomavirus status and prognosis in invasive cervical cancer: A nationwide cohort study. PLoS Med. 2018;15:e1002666. doi: 10.1371/journal.pmed.1002666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xing B., Guo J., Sheng Y., Wu G., Zhao Y. Human Papillomavirus-Negative Cervical Cancer: A Comprehensive Review. Front. Oncol. 2020;10:606335. doi: 10.3389/fonc.2020.606335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoshida H., Shiraishi K., Kato T. Molecular Pathology of Human Papilloma Virus-Negative Cervical Cancers. Cancers. 2021;13:6351. doi: 10.3390/cancers13246351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hang D., Jia M., Ma H., Zhou J., Feng X., Lyu Z., Yin J., Cui H., Yin Y., Jin G., et al. Independent prognostic role of human papillomavirus genotype in cervical cancer. BMC Infect. Dis. 2017;17:391. doi: 10.1186/s12879-017-2465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwartz S.M., Daling J.R., Shera K.A., Madeleine M.M., McKnight B., Galloway D.A., Porter P.L., McDougall J.K. Human papillomavirus and prognosis of invasive cervical cancer: A population-based study. J. Clin. Oncol. 2001;19:1906–1915. doi: 10.1200/JCO.2001.19.7.1906. [DOI] [PubMed] [Google Scholar]
- 16.Ruiz F.J., Inkman M., Rashmi R., Muhammad N., Gabriel N., Miller C.A., McLellan M.D., Goldstein M., Markovina S., Grigsby P.W., et al. HPV transcript expression affects cervical cancer response to chemoradiation. JCI Insight. 2021;6:e138734. doi: 10.1172/jci.insight.138734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basukala O., Banks L. The Not-So-Good, the Bad and the Ugly: HPV E5, E6 and E7 Oncoproteins in the Orchestration of Carcinogenesis. Viruses. 2021;13:1892. doi: 10.3390/v13101892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiu Q., Zhou Q., Luo A., Li X., Li K., Li W., Yu M., Amanullah M., Lu B., Lu W., et al. Integrated analysis of virus and host transcriptomes in cervical cancer in Asian and Western populations. Genomics. 2021;113:1554–1564. doi: 10.1016/j.ygeno.2021.03.029. [DOI] [PubMed] [Google Scholar]
- 19.Chen L., Luan S., Xia B., Liu Y., Gao Y., Yu H., Mu Q., Zhang P., Zhang W., Zhang S., et al. Integrated analysis of HPV-mediated immune alterations in cervical cancer. Gynecol. Oncol. 2018;149:248–255. doi: 10.1016/j.ygyno.2018.01.031. [DOI] [PubMed] [Google Scholar]
- 20.Robert C. A decade of immune-checkpoint inhibitors in cancer therapy. Nat. Commun. 2020;11:3801. doi: 10.1038/s41467-020-17670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borcoman E., Le Tourneau C. Keynote-158 study, FDA granted accelerated approval of pembrolizumab for the treatment of patients with advanced PD-L1-positive cervical cancer. Ann. Transl. Med. 2020;8:1611. doi: 10.21037/atm-20-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jardim D.L., Goodman A., de Melo Gagliato D., Kurzrock R. The Challenges of Tumor Mutational Burden as an Immunotherapy Biomarker. Cancer Cell. 2021;39:154–173. doi: 10.1016/j.ccell.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burk R.D., Chen Z., Saller C., Tarvin K., Carvalho A.L., Scapulatempo-Neto C., Silveira H.C., Fregnani J.H., Creighton C.J., Anderson M.L., et al. Integrated genomic and molecular characterization of cervical cancer. Nature. 2017;543:378–384. doi: 10.1038/nature21386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Banister C.E., Liu C., Pirisi L., Creek K.E., Buckhaults P.J. Identification and characterization of HPV-independent cervical cancers. Oncotarget. 2017;8:13375–13386. doi: 10.18632/oncotarget.14533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brant A.C., Menezes A.N., Felix S.P., Almeida L.M., Moreira M.A.M. Preferential expression of a HPV genotype in invasive cervical carcinomas infected by multiple genotypes. Genomics. 2020;112:2942–2948. doi: 10.1016/j.ygeno.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 26.Thorsson V., Gibbs D.L., Brown S.D., Wolf D., Bortone D.S., Ou Yang T.H., Porta-Pardo E., Gao G.F., Plaisier C.L., Eddy J.A., et al. The Immune Landscape of Cancer. Immunity. 2018;48:812–830.e814. doi: 10.1016/j.immuni.2018.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gameiro S.F., Kolendowski B., Zhang A., Barrett J.W., Nichols A.C., Torchia J., Mymryk J.S. Human papillomavirus dysregulates the cellular apparatus controlling the methylation status of H3K27 in different human cancers to consistently alter gene expression regardless of tissue of origin. Oncotarget. 2017;8:72564–72576. doi: 10.18632/oncotarget.19885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J., Lichtenberg T., Hoadley K.A., Poisson L.M., Lazar A.J., Cherniack A.D., Kovatich A.J., Benz C.C., Levine D.A., Lee A.V., et al. An Integrated TCGA Pan-Cancer Clinical Data Resource to Drive High-Quality Survival Outcome Analytics. Cell. 2018;173:400–416.e411. doi: 10.1016/j.cell.2018.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bai R., Lv Z., Xu D., Cui J. Predictive biomarkers for cancer immunotherapy with immune checkpoint inhibitors. Biomark. Res. 2020;8:34. doi: 10.1186/s40364-020-00209-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gajewski T.F., Corrales L., Williams J., Horton B., Sivan A., Spranger S. Cancer Immunotherapy Targets Based on Understanding the T Cell-Inflamed Versus Non-T Cell-Inflamed Tumor Microenvironment. Adv. Exp. Med. Biol. 2017;1036:19–31. doi: 10.1007/978-3-319-67577-0_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muller A.J., DuHadaway J.B., Donover P.S., Sutanto-Ward E., Prendergast G.C. Inhibition of indoleamine 2,3-dioxygenase, an immunoregulatory target of the cancer suppression gene Bin1, potentiates cancer chemotherapy. Nat. Med. 2005;11:312–319. doi: 10.1038/nm1196. [DOI] [PubMed] [Google Scholar]
- 32.Anderson A.C., Joller N., Kuchroo V.K. Lag-3, Tim-3, and TIGIT: Co-inhibitory Receptors with Specialized Functions in Immune Regulation. Immunity. 2016;44:989–1004. doi: 10.1016/j.immuni.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Antonioli L., Pacher P., Vizi E.S., Hasko G. CD39 and CD73 in immunity and inflammation. Trends Mol. Med. 2013;19:355–367. doi: 10.1016/j.molmed.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Augustin R.C., Leone R.D., Naing A., Fong L., Bao R., Luke J.J. Next steps for clinical translation of adenosine pathway inhibition in cancer immunotherapy. J. Immunother. Cancer. 2022;10:e004089. doi: 10.1136/jitc-2021-004089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kidman J., Principe N., Watson M., Lassmann T., Holt R.A., Nowak A.K., Lesterhuis W.J., Lake R.A., Chee J. Characteristics of TCR Repertoire Associated With Successful Immune Checkpoint Therapy Responses. Front. Immunol. 2020;11:587014. doi: 10.3389/fimmu.2020.587014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosati E., Dowds C.M., Liaskou E., Henriksen E.K.K., Karlsen T.H., Franke A. Overview of methodologies for T-cell receptor repertoire analysis. BMC Biotechnol. 2017;17:61. doi: 10.1186/s12896-017-0379-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zehbe I., Kaufmann A.M., Schmidt M., Hohn H., Maeurer M.J. Human papillomavirus 16 E6-specific CD45RA+ CCR7+ high avidity CD8+ T cells fail to control tumor growth despite interferon-gamma production in patients with cervical cancer. J. Immunother. 2007;30:523–532. doi: 10.1097/CJI.0b013e31803240fa. [DOI] [PubMed] [Google Scholar]
- 38.Nakagawa M., Greenfield W., Moerman-Herzog A., Coleman H.N. Cross-Reactivity, Epitope Spreading, and De Novo Immune Stimulation Are Possible Mechanisms of Cross-Protection of Nonvaccine Human Papillomavirus (HPV) Types in Recipients of HPV Therapeutic Vaccines. Clin. Vaccine Immunol. 2015;22:679–687. doi: 10.1128/CVI.00149-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fratta E., Coral S., Covre A., Parisi G., Colizzi F., Danielli R., Nicolay H.J., Sigalotti L., Maio M. The biology of cancer testis antigens: Putative function, regulation and therapeutic potential. Mol. Oncol. 2011;5:164–182. doi: 10.1016/j.molonc.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gjerstorff M.F., Andersen M.H., Ditzel H.J. Oncogenic cancer/testis antigens: Prime candidates for immunotherapy. Oncotarget. 2015;6:15772–15787. doi: 10.18632/oncotarget.4694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fleischmann M., Chatzikonstantinou G., Fokas E., Wichmann J., Christiansen H., Strebhardt K., Rodel C., Tselis N., Rodel F. Molecular Markers to Predict Prognosis and Treatment Response in Uterine Cervical Cancer. Cancers. 2021;13:5748. doi: 10.3390/cancers13225748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kamal M., Lameiras S., Deloger M., Morel A., Vacher S., Lecerf C., Dupain C., Jeannot E., Girard E., Baulande S., et al. Human papilloma virus (HPV) integration signature in Cervical Cancer: Identification of MACROD2 gene as HPV hot spot integration site. Br. J. Cancer. 2021;124:777–785. doi: 10.1038/s41416-020-01153-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galon J., Bruni D. Tumor Immunology and Tumor Evolution: Intertwined Histories. Immunity. 2020;52:55–81. doi: 10.1016/j.immuni.2019.12.018. [DOI] [PubMed] [Google Scholar]
- 44.Shamseddine A.A., Burman B., Lee N.Y., Zamarin D., Riaz N. Tumor Immunity and Immunotherapy for HPV-Related Cancers. Cancer Discov. 2021;11:1896–1912. doi: 10.1158/2159-8290.CD-20-1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van der Burg S.H., Piersma S.J., de Jong A., van der Hulst J.M., Kwappenberg K.M., van den Hende M., Welters M.J., Van Rood J.J., Fleuren G.J., Melief C.J., et al. Association of cervical cancer with the presence of CD4+ regulatory T cells specific for human papillomavirus antigens. Proc. Natl. Acad. Sci. USA. 2007;104:12087–12092. doi: 10.1073/pnas.0704672104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sheu B.C., Lin R.H., Lien H.C., Ho H.N., Hsu S.M., Huang S.C. Predominant Th2/Tc2 polarity of tumor-infiltrating lymphocytes in human cervical cancer. J. Immunol. 2001;167:2972–2978. doi: 10.4049/jimmunol.167.5.2972. [DOI] [PubMed] [Google Scholar]
- 47.Bais A.G., Beckmann I., Lindemans J., Ewing P.C., Meijer C.J., Snijders P.J., Helmerhorst T.J. A shift to a peripheral Th2-type cytokine pattern during the carcinogenesis of cervical cancer becomes manifest in CIN III lesions. J. Clin. Pathol. 2005;58:1096–1100. doi: 10.1136/jcp.2004.025072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gameiro S.F., Ghasemi F., Barrett J.W., Koropatnick J., Nichols A.C., Mymryk J.S., Maleki Vareki S. Treatment-naive HPV+ head and neck cancers display a T-cell-inflamed phenotype distinct from their HPV- counterparts that has implications for immunotherapy. Oncoimmunology. 2018;7:e1498439. doi: 10.1080/2162402X.2018.1498439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heeren A.M., Rotman J., Stam A.G.M., Pocorni N., Gassama A.A., Samuels S., Bleeker M.C.G., Mom C.H., Zijlmans H., Kenter G.G., et al. Efficacy of PD-1 blockade in cervical cancer is related to a CD8(+)FoxP3(+)CD25(+) T-cell subset with operational effector functions despite high immune checkpoint levels. J. Immunother. Cancer. 2019;7:43. doi: 10.1186/s40425-019-0526-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y., Wang C., Qiu J., Qu X., Peng J., Lu C., Zhang M., Zhang M., Qi X., Li G., et al. Targeting CD96 overcomes PD-1 blockade resistance by enhancing CD8+ TIL function in cervical cancer. J. Immunother. Cancer. 2022;10:e003667. doi: 10.1136/jitc-2021-003667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Z., Dong D., Zhu Y., Pang N., Ding J. The role of Tim-3/Galectin-9 pathway in T-cell function and prognosis of patients with human papilloma virus-associated cervical carcinoma. FASEB J. 2021;35:e21401. doi: 10.1096/fj.202000528RR. [DOI] [PubMed] [Google Scholar]
- 52.Kassardjian A., Moatamed N.A. Expression of immune checkpoint regulators, cytotoxic T lymphocyte antigen 4 (CTLA-4), and CD137 in cervical carcinoma. Int. J. Clin. Exp. Pathol. 2021;14:1038–1047. [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang A.W., McPherson A., Milne K., Kroeger D.R., Hamilton P.T., Miranda A., Funnell T., Little N., de Souza C.P.E., Laan S., et al. Interfaces of Malignant and Immunologic Clonal Dynamics in Ovarian Cancer. Cell. 2018;173:1755–1769.e1722. doi: 10.1016/j.cell.2018.03.073. [DOI] [PubMed] [Google Scholar]
- 54.Schietinger A., Philip M., Krisnawan V.E., Chiu E.Y., Delrow J.J., Basom R.S., Lauer P., Brockstedt D.G., Knoblaugh S.E., Hammerling G.J., et al. Tumor-Specific T Cell Dysfunction Is a Dynamic Antigen-Driven Differentiation Program Initiated Early during Tumorigenesis. Immunity. 2016;45:389–401. doi: 10.1016/j.immuni.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lanitis E., Dangaj D., Irving M., Coukos G. Mechanisms regulating T-cell infiltration and activity in solid tumors. Ann. Oncol. 2017;28:xii18–xii32. doi: 10.1093/annonc/mdx238. [DOI] [PubMed] [Google Scholar]
- 56.Ferrall L., Lin K.Y., Roden R.B.S., Hung C.F., Wu T.C. Cervical Cancer Immunotherapy: Facts and Hopes. Clin. Cancer Res. 2021;27:4953–4973. doi: 10.1158/1078-0432.CCR-20-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bald T., Krummel M.F., Smyth M.J., Barry K.C. The NK cell-cancer cycle: Advances and new challenges in NK cell-based immunotherapies. Nat. Immunol. 2020;21:835–847. doi: 10.1038/s41590-020-0728-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Imai C., Iwamoto S., Campana D. Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood. 2005;106:376–383. doi: 10.1182/blood-2004-12-4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu E., Marin D., Banerjee P., Macapinlac H.A., Thompson P., Basar R., Nassif Kerbauy L., Overman B., Thall P., Kaplan M., et al. Use of CAR-Transduced Natural Killer Cells in CD19-Positive Lymphoid Tumors. N. Engl. J. Med. 2020;382:545–553. doi: 10.1056/NEJMoa1910607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Doran S.L., Stevanovic S., Adhikary S., Gartner J.J., Jia L., Kwong M.L.M., Faquin W.C., Hewitt S.M., Sherry R.M., Yang J.C., et al. T-Cell Receptor Gene Therapy for Human Papillomavirus-Associated Epithelial Cancers: A First-in-Human, Phase I/II Study. J. Clin. Oncol. 2019;37:2759–2768. doi: 10.1200/JCO.18.02424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.van Hall T., Andre P., Horowitz A., Ruan D.F., Borst L., Zerbib R., Narni-Mancinelli E., van der Burg S.H., Vivier E. Monalizumab: Inhibiting the novel immune checkpoint NKG2A. J. Immunother. Cancer. 2019;7:263. doi: 10.1186/s40425-019-0761-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Colombo N., Dubot C., Lorusso D., Caceres M.V., Hasegawa K., Shapira-Frommer R., Tewari K.S., Salman P., Hoyos Usta E., Yanez E., et al. Pembrolizumab for Persistent, Recurrent, or Metastatic Cervical Cancer. N. Engl. J. Med. 2021;385:1856–1867. doi: 10.1056/NEJMoa2112435. [DOI] [PubMed] [Google Scholar]
- 63.Monk B.J., Enomoto T., Kast W.M., McCormack M., Tan D.S.P., Wu X., Gonzalez-Martin A. Integration of immunotherapy into treatment of cervical cancer: Recent data and ongoing trials. Cancer Treat. Rev. 2022;106:102385. doi: 10.1016/j.ctrv.2022.102385. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.