Abstract
Objectives
This study examines the relationship between COVID-19 disclosure stigma and COVID-19 testing hesitancy and assesses their changes between November 2020 and 2021.
Study design
This was a longitudinal cohort.
Methods
A total of 355 participants completed four study waves between November 2020 and November 2021. Factor analyses and Cronbach's alpha assessed the factor structure and internal consistency of the COVID-19 Disclosure Stigma scale. Paired t-tests and McNemar's Chi-squared test assessed change between the study waves. Multivariable logistic regression models examined the relationship between COVID-19 disclosure stigma and testing hesitancy at four study waves.
Results
COVID-19 disclosure stigma declined significantly between the last study waves (P = 0.030). The greatest disclosure concern was reporting a positive test to close contacts (range: 19%–21%) followed by disclosure to friends (range: 10%–15%) and family (range: 4%–10%). Over the course of the four study waves, COVID-19 testing hesitancy when symptomatic ranged from 23% to 30%. Older age, female gender, and having received a COVID-19 vaccine were associated with decreased odds of testing hesitancy. Greater COVID-19 disclosure stigma and more conservative political ideology showed a consistent relationship with increased odds of COVID-19 testing hesitancy.
Conclusions
Study findings suggest that many people anticipate feeling stigmatized when disclosing positive test results, especially to close contacts. A substantial percentage of study participants reported hesitancy to be tested when symptomatic. This study identifies a need for interventions that normalize COVID-19 testing (e.g. engaging leaders with conservative followings), provide strategies for disclosing positive results, and allow anonymous notification of potential COVID-19 exposure.
Keywords: COVID-19 disclosure stigma, COVID-19 testing hesitancy, Stigma, Coronavirus
Introduction
Testing for infection by SARS-CoV-2 (COVID-19 testing) is a critical tool for identifying and mitigating the spread of COVID-19. Initially, testing in the United States was highly limited in the months following the country's first confirmed case of COVID-19 in late January 2020.1 , 2 The rate of testing increased dramatically in the first 8 months of the pandemic, from about 2 million tests per week in late April 2020 to approximately 2 million tests per day by late November 2020.1 Starting in 2020, COVID-19 tests were available for free via programs offered by many health departments and purchase at many stores with pharmacies. Beginning in 2022, COVID-19 home test kits could be ordered from the US government at no cost. Even after the introduction of vaccinations for SARS-CoV-2, which effectively reduce cases of severe illness, COVID-19 testing remains an integral means of reducing the spread of the virus and helping to guide treatment.3 For example, prompt testing of symptomatic individuals is critical, as COVID-19 antivirals are most effective when administered within the first few days.4 Yet, although there has been a plethora of research focused on vaccine hesitancy, research on COVID-19 testing hesitancy has been limited. Understanding COVID-19 testing hesitancy and barriers to testing can inform COVID-19 prevention and pandemic control programs.
Stigma is one such barrier to COVID-19 testing uptake. Stigma refers to a set of interrelated social processes, which differentiate persons characterized as ‘normal’ from the ‘abnormal,’ based on a given attribute and negative stereotypes.5 , 6 It is common for stigma to be associated with infectious diseases, as it has been linked to HIV, hepatitis C, syphilis, tuberculosis, Ebola, and H1N1.7 Stigma toward other pandemic diseases (e.g. HIV/AIDS) has been identified as a predictor of not testing.8 In the context of COVID-19, stigma toward COVID-19 has manifested in different ways to disproportionately target a variety of sociodemographic groups, including persons of Asian descent,9 people who are more likely to contract and spread COVID-19 (e.g. healthcare workers),10 people of low socio-economic status engaged in essential work,11 as well as people who have tested positive for COVID-19.12
In this article, we focus on the stigma associated with people who have tested positive for COVID-19. We view stigma as a multilevel construct that works along gradients of power, with stigma operating at the intrapersonal level by affecting one's self-perception as well as at the interpersonal level by shaping relationships.13 , 14 During the COVID-19 pandemic, misinformation, as well as other social and structural processes, have facilitated the spread of stigmatization of people infected with COVID-19.12 Misinformation has driven fear and anxiety over becoming infected, which, along with an individual's fear of infecting others, can lead to social exclusion or isolation. For example, a study of Jordanian adults found that perceived discrimination at work was associated with COVID-19 testing hesitancy.15 Structural infection control measures, such as quarantine, physically exclude individuals and can further fuel stigma on an intrapersonal and interpersonal level.16 Furthermore, terms used in the media and public discourse such as ‘super spreader’ and ‘transmitting the virus’ assign blame for infection to the individual.16
Disclosure is highly intertwined with stigma17 and central to COVID-19 prevention and mitigation strategies. When a health condition is stigmatized, disclosure concern increases. Moreover, similar to stigma, disclosure can shape social relationships—disclosing an illness such as COVID-19 can significantly alter interpersonal relationships and support from their social network17 as those infected may be viewed as careless for acquiring COVID-19 and endangering others through COVID-19 transmission. Given the importance of disclosing one's positive COVID-19 status in mitigating the spread of COVID-19, we focus specifically on individuals' comfort in disclosing positive results to close contacts. For testing to be effective, the contacts of people who test positive for COVID-19 need to be notified, tested, and isolate if they test positive. As many locales do not have contact tracing programs, personal disclosure is an important method for contacts to be notified of exposure and potential infections. In addition, where contact tracing is used, personal disclosure may be quicker than public health officials notifying contacts. In this study, we use novel items addressing three theory-informed and practice-relevant domains (i.e. friends, family, and other close contacts) to capture COVID-19 disclosure stigma.
Existing research on the relationship between COVID-19 testing and COVID-19 stigma in the United States is limited. One study by Earnshaw et al. assessed COVID-19 stigma and testing intentions early in the COVID-19 pandemic (April 2020) and identified a significant association between anticipated stigma and COVID-19 testing intentions.18 In addition to looking only at a specific timepoint soon after the advent of the pandemic, the authors also note that their measure of testing (i.e. if participants would seek a test if one were to be ‘ordered’ by their doctor) may have resulted in an inflated likelihood of self-reported test-seeking; thus, they call for future work to focus on testing intention when symptomatic.18 An additional limitation of the current body of literature on COVID-19 stigma is that COVID-19 is presented as a relatively fixed entity.19 , 20 However, stigma, including stigma associated with testing positive for COVID-19, may have changed over time.21 For example, the announcement of various celebrities and politicians who have tested positive for COVID-19 may impact perceptions of the disease and normalize diagnosis.22 Moreover, increased access to home testing may have altered levels of COVID-19 stigma.23 In addition, as vaccines are now readily available that greatly reduce the probability of severe COVID-19, hospitalization, and death, SARS-CoV-2 may not be perceived as so threatening, which may alter the level of stigma surrounding testing and of being infected. The present study, therefore, examines COVID-19 disclosure stigma within the continually changing dynamics of the COVID-19 pandemic by assessing it at multiple time points and examining the relationship between COVID-19 disclosure stigma and COVID-19 testing hesitancy over time. A subanalysis also includes vaccination status in models of vaccine hesitancy. It is important to look at vaccination status because those who are not vaccinated are at the highest risk of severe infection and should be quickly tested for potential treatment with antivirals.
Methods
Recruitment and sampling
This study used participants from the COVID-19 and Well-Being Study. The COVID-19 and Well-Being Study is an online longitudinal cohort study that began in March 2020 that aimed to examine individual-, social-, and societal-level fluctuations related to COVID-19 amid the rapidly changing landscape of the pandemic. Study periods occurred every few months and aimed to capture changes in COVID-19–related information, behaviors, and health status. Participants were initially recruited through Amazon's Mechanical Turk (MTurk), a platform that is frequently used by health researchers, as it allows for the study of real-time dynamics of large groups.24 Study populations recruited through MTurk are not nationally representative but have been documented to perform better than other convenience samples on several key dimensions and have demonstrated good reliability.25 , 26 The study protocols followed MTurk's best practices, including ensuring confidentiality, using unique completion codes, integrating attention checks throughout the survey, repeating study-specific qualification questions, and removing ineligible participants.27 , 28 Eligibility for recruitment into the longitudinal cohort included being age 18 years or older, living in the United States, being able to speak and read English, having heard of the coronavirus or COVID-19, and providing written informed consent. To enhance reliability, eligible participants also had to pass attention and validity checks embedded in the survey.29
At baseline, 809 people were eligible for the study and asked to participate in each subsequent survey wave. This analysis uses survey waves when information on COVID-19 stigma was collected and includes survey waves 4 (November 2020), 5 (March 2021), 6 (June 2021), and 7 (November 2021). Participants were notified through the MTurk platform when a new survey was deployed. Participants received a reminder message to complete the survey approximately every 2 days during the survey window or until they completed the survey. To assess change over time, only participants who participated in all four waves were included in the present analysis. In total, 361 people participated in all four waves. Three participants were excluded from the present analysis due to missing data on the COVID-19 stigma questions or testing intentions. An additional three participants who did not identify as male or female were excluded due to small sample size, providing a final sample size of 355 participants. Participants were compensated $4.25 for completing each of the online surveys at waves 4, 5, 6, and 7, which is equivalent to approximately $12 per hour. The study protocols were approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Measures
Three items assessed COVID-19 disclosure stigma. These items were designed to target disclosure stigma within the three interpersonal relationship domains of friends, family, and close contacts.
These three domains are frequently included in stigma-related scales seeking to measure secrecy and disclosure around stigmatized health conditions (e.g. mental illness,30, 31, 32 HIV33). The three items were as follows: ‘If I had a positive coronavirus test, I would feel very uncomfortable telling my friends,’ ‘If I had a positive coronavirus test, I would feel very uncomfortable telling my family,’ and ‘If I had a positive coronavirus test, I would feel very uncomfortable telling people that I had recently been in close contact with.’ Although often the ‘close contacts’ domain may be asked about in other scales using terms such as ‘community members’ or ‘coworkers,’ we use the language of ‘people that I had recently been in close contact with’ to better align with COVID-19 prevention efforts and common COVID-19–related messaging. The participants responded on a 1- to 5-point Likert scale of ‘strongly disagree,’ ‘disagree,’ ‘neither agree or disagree,’ ‘agree,’ and ‘strongly agree.’ The sum of the three items at each study wave formed the stigma scale score (range: 5–15), with higher scores representing greater disclosure stigma.
COVID-19 testing hesitancy was assessed by asking participants, ‘If you had symptoms of coronavirus, how likely is it that you would get tested for coronavirus?’ Responses included ‘extremely unlikely,’ ‘unlikely,’ ‘neutral,’ ‘likely,’ and ‘extremely likely.’ To assess COVID-19 testing hesitancy, a dichotomous variable was created to compare those not likely to get a COVID-19 test when symptomatic (responses of ‘extremely unlikely,’ ‘unlikely,’ and ‘neutral’) to those likely to be tested (responses of ‘extremely likely’ and ‘likely’). Demographics were assessed at baseline data collection (March 2020), and variables included age, race/ethnicity, sex, family income, education, and political orientation. Age was assessed as a continuous variable. The respondents' race/ethnicity included ‘White,’ ‘non-Hispanic Black,’ ‘Hispanic,’ ‘Asian,’ ‘Mixed,’ or ‘Other.’ Due to small sample size, ‘Hispanic,’ ‘Asian,’ ‘Mixed,’ and ‘Other’ were collapsed into ‘Other.’ Sex of the respondents was based on their reported sex assigned at birth. Household income was dichotomized, based on the median, at 60,000 USD or less vs more than 60,000 USD per year. Education was also dichotomized based on the median, at some college degree or less vs bachelor's degree or higher. As the response to COVID-19 in the United States has become politically oriented, participants were also asked about their political orientation on a scale from ‘very liberal,’ ‘liberal,’ ‘slightly liberal,’ ‘moderate,’ ‘slightly conservative,’ ‘conservative,’ to ‘very conservative,’ with higher scores representing more conservative orientations. Two people did not identify their political ideology and were coded as moderate.
A supplementary analysis also adjusted for vaccination status. This analysis focused on waves 5, 6, and 7 because vaccines were not available at the time of prior survey waves. Vaccination status was assessed at each of these three waves and compared participants who had received at least one dose of a COVID-19 vaccine to participants who had received no doses. A second supplemental analysis assessed the independent effect of each of the COVID-19 disclosure stigma items on COVID-19 testing hesitancy.
Analyses
We used descriptive statistics to assess COVID-19 disclosure stigma and testing hesitancy when having symptoms of COVID-19 at each study wave. A factor analysis and Cronbach's alpha were used to assess the factor structure and internal consistency of the COVID-19 Disclosure Stigma scale. Paired t-tests assessed change in mean COVID-19 disclosure stigma, and McNemar's Chi-squared test assessed change in COVID-19 testing hesitancy between study waves.
Unadjusted logistic regression models examined the relationship between COVID-19 disclosure stigma and testing hesitancy at each study wave. To assess the independent association between COVID-19 disclosure stigma and testing hesitancy, multivariable models for each of the four study waves were analyzed, adjusting for demographic variables. In the logistic regression models, COVID-19 disclosure stigma was converted to a z-score. A first supplemental analysis used multivariable logistic regression models to examine the relationship between COVID-19 disclosure stigma and hesitancy, adjusting for demographics as well as COVID-19 vaccination status. The second supplementary analysis examined each COVID-19 disclosure stigma item separately to assess the independent effect of each measure using bivariate and multivariable models. All analyses were performed using STATA 17 (StataCorp).34
Results
Table 1 shows the demographic characteristics of the study population. The mean age of study participants was 42.22 years (SD 11.94). About half of the sample (55.49%) was female, and 82.82% were White. The political ideology of participants was diverse, with 51.27% identifying as liberal, 22.25% as moderate, and 26.48% as conservative. More than half (59.72%) of participants had received a bachelor's degree or higher, and 47.04% reported a household income >$60,000. At wave 5, 13.52% of participants reported receiving at least one dose of the COVID-19 vaccine. This increased to 69.86% at wave 6 and 77.18% at wave 7.
Table 1.
Demographics (N = 355).
| Variable | N (%) or mean (SD) |
|---|---|
| Age, mean (SD) | 42.22 (11.94) |
| Sex | |
| Male | 158 (44.51%) |
| Female | 197 (55.49%) |
| Race | |
| White | 294 (82.82%) |
| Black | 21 (5.92%) |
| Other | 40 (11.27%) |
| Education | |
| Some college or less | 143 (40.28%) |
| Bachelor degree or higher | 212 (59.72%) |
| Income | |
| $60K or less | 188 (52.96%) |
| >$60K | 167 (47.04%) |
| Political orientation,a mean (SD) | 3.42 (1.75) |
| Received COVID-19 vaccine, Wave 5 | 48 (13.52) |
| Received COVID-19 vaccine, Wave 6 | 248 (69.86) |
| Received COVID-19 vaccine, Wave 7 | 274 (77.18) |
Political orientation: (1) very liberal, (2) liberal, (3) slightly liberal, (4) moderate, (5) slightly conservative, (6) conservative, and (7) very conservative.
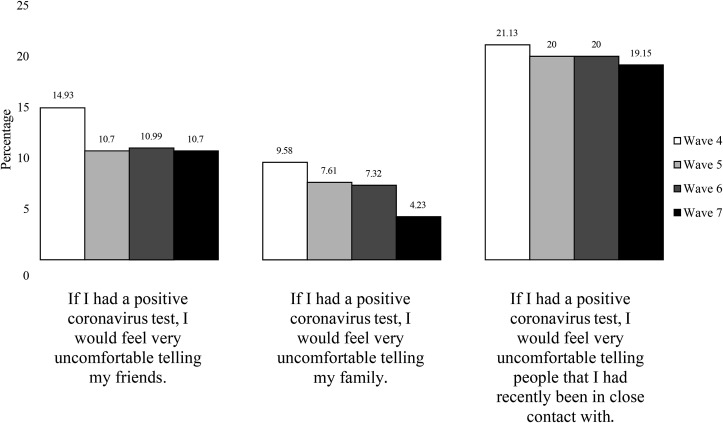
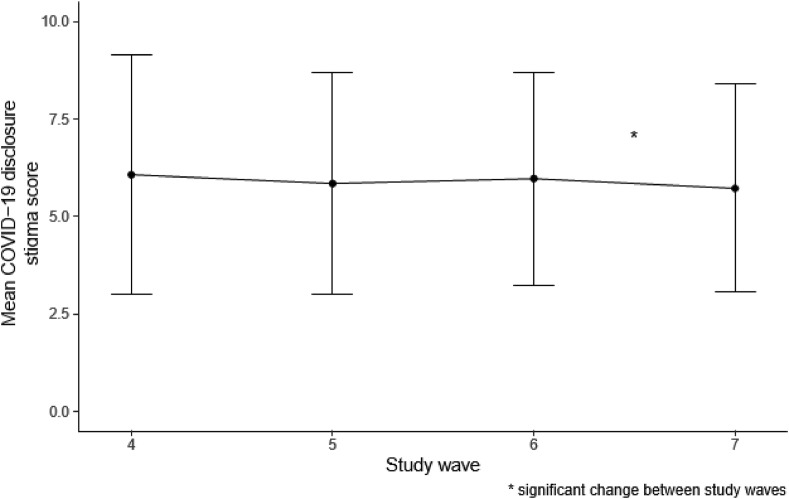
Across the four study waves, participants reported the greatest disclosure stigma in reporting a positive test to close contacts (Fig. 1 , 21.13% in wave 4–19.15% in wave 7) followed by disclosure stigma around telling friends (14.93% in wave 4–10.70% in wave 7). The least disclosure stigma was in reporting positive results to family (9.58% in wave 4–4.23% in wave 7). The COVID-19 Disclosure Stigma Scale indicated a one factor structure at each study wave and high internal consistency (α wave 4 = 0.85; α wave 5 = 0.82; α wave 6 = 0.79; α wave 7 = 0.80; Table 2 ). Scores on the COVID-19 Disclosure Stigma Scale did not significantly change between wave 4 and 5, nor between wave 5 and wave 6 (Fig. 2 ). However, there was a significant decline in COVID-19 disclosure stigma between waves 6 and 7 (P = 0.030).
Fig. 1.
Frequency of endorsing COVID-19 disclosure stigma items across study waves.
Table 2.
Factor structure of COVID-19 Disclosure Stigma scale.
| COVID-19 Disclosure Stigma Scale Items | Study wave 4 |
Study wave 5 |
Study wave 6 |
Study wave 7 |
||||
|---|---|---|---|---|---|---|---|---|
| Eigen-value | Factor loading | Eigen-value | Factor loading | Eigen-value | Factor loading | Eigen-value | Factor loading | |
| If I had a positive coronavirus test, I would feel very uncomfortable telling my friends. | 1.90 | 0.80 | 1.67 | 0.75 | 1.57 | 0.73 | 1.65 | 0.79 |
| If I had a positive coronavirus test, I would feel very uncomfortable telling my family. | −0.10 | 0.83 | −0.14 | 0.76 | −0.13 | 0.75 | −0.11 | 0.73 |
| If I had a positive coronavirus test, I would feel very uncomfortable telling people that I had recently been in close contact with. | −0.15 | 0.74 | −0.16 | 0.74 | −0.17 | 0.69 | −0.18 | 0.70 |
| Cronbach Alpha | α = 0.85 | α = 0.82 | α = 0.79 | α = 0.80 | ||||
Fig. 2.
Mean COVID-19 disclosure stigma scores by survey wave.
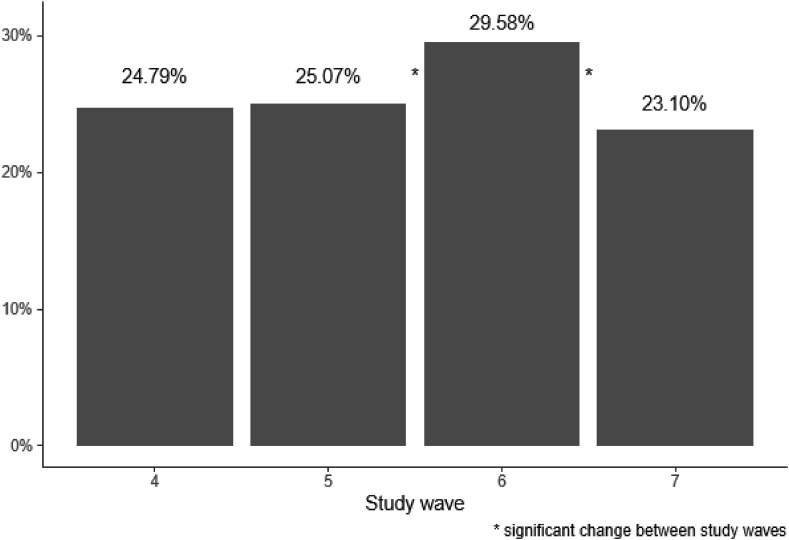
Over the four study waves, COVID-19 testing hesitancy when symptomatic ranged from 23.10% to 29.58% (Fig. 3 ). A statistically significant increase in COVID-19 testing hesitancy was evident between waves 5 and 6 (P = 0.044) followed by a significant decrease between waves 6 and 7 (P = 0.005).
Fig. 3.
COVID-19 testing hesitancy by survey wave.
In the logistic regression models (Table 3 ), older age was associated with decreased odds of COVID-19 testing hesitancy in unadjusted waves 5, 6, and 7 models, and these relationships remained significant in each of the adjusted models. Women had decreased COVID-19 testing hesitancy odds compared with males in wave 6 only. Participants reporting a more conservative political ideology had increased odds of COVID-19 testing hesitancy in both the unadjusted and adjusted models for waves 4, 5, and 6. For wave 7, the relationship between political ideology and testing hesitancy was only significant in the adjusted models. Higher COVID-19 stigma showed a consistent relationship with increased odds of COVID-19 testing hesitancy. This relationship was significant in all unadjusted models as well as in the multivariable models for waves 5, 6, and 7.
Table 3.
Unadjusted and adjusted logistic models of COVID-19 testing hesitancy.
| Variable | COVID-19 testing hesitancy—wave 4 |
COVID-19 testing hesitancy—wave 5 |
COVID-19 testing hesitancy—wave 6 |
COVID-19 testing hesitancy—wave 7 |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | |
| Age | 0.98 (0.95, 1.00) | 0.98 (0.95, 1.00) | 0.98 (0.96, 1.00) | 0.97 (0.95, 1.00) | 0.97 (0.95, 0.99) | 0.97 (0.95, 1.00) | 0.96 (0.94, 0.99) | 0.97 (0.94, 0.99) |
| Sex (ref: male) | 0.84 (0.52, 1.36) | 0.95 (0.57, 1.58) | 0.68 (0.42, 1.10) | 0.77 (0.46, 1.28) | 0.51 (0.32, 0.81) | 0.55 (0.34, 0.90) | 0.75 (0.46, 1.23) | 0.85 (0.50, 1.43) |
| Race (ref: white) | ||||||||
| Black | 1.63 (0.63, 4.20) | 1.52 (0.57, 4.06) | 0.73 (0.24, 2.23) | 0.68 (0.21, 2.18) | 1.27 (0.50, 3.26) | 1.23 (0.46, 3.32) | 1.53 (0.57, 4.10) | 1.49 (0.53, 4.17) |
| Other | 1.40 (0.67, 2.89) | 1.27 (0.59, 2.77) | 1.48 (0.73, 3.03) | 1.50 (0.69, 3.25) | 1.53 (0.77, 3.04) | 1.41 (0.66, 2.98) | 2.29 (1.14, 4.61) | 2.03 (0.96, 4.28) |
| Education (ref: some college or less) | 0.85 (0.52, 1.39) | 0.99 (0.58, 1.71) | 0.88 (0.54, 1.42) | 0.81 (0.47, 1.41) | 0.86 (0.54, 1.37) | 0.79 (0.47, 1.34) | 0.94 (0.57, 1.55) | 0.93 (0.53, 1.62) |
| Income (ref: $60,000 or less) | 0.63 (0.39, 1.04) | 0.53 (0.30, 0.91) | 1.14 (0.70, 1.84) | 1.01 (0.58, 1.74) | 1.09 (0.69, 1.72) | 1.03 (0.61, 1.74) | 0.80 (0.48, 1.31) | 0.77 (0.44, 1.34) |
| Political orientation | 1.20 (1.05, 1.38) | 1.28 (1.10, 1.49) | 1.31 (1.14, 1.51) | 1.35 (1.16, 1.57) | 1.27 (1.11, 1.45) | 1.33 (1.14, 1.53) | 1.10 (0.96, 1.27) | 1.17 (1.00, 1.37) |
| COVID-19 Stigma—wave 4 |
1.29 (1.02, 1.64) | 1.23 (0.96, 1.58) | – | – | – | – | – | – |
| COVID-19 Stigma—wave 5 |
– | – | 1.42 (1.13, 1.79) | 1.37 (1.07, 1.74) | – | – | – | – |
| COVID-19 Stigma—wave 6 |
– | – | – | – | 1.46 (1.15, 1.85) | 1.45 (1.13, 1.87) | – | – |
| COVID-19 Stigma—wave 7 |
– | – | – | – | – | – | 1.43 (1.09, 1.87) | 1.38 (1.04, 1.83) |
aOR, adjusted odds ratio; CI, confidence interval.
Bold values represent P-value ≤0.05.
In the first supplemental analysis (Supplemental Table 1), multivariable models also adjusted for COVID-19 vaccination status at waves 5, 6, and 7. COVID-19 disclosure stigma remained significant and independent predictor of vaccination hesitancy at each of the analyzed waves (wave 5: adjusted odds ratio [aOR] = 1.37, 95% confidence interval [CI] = 1.07, 1.74; wave 6: aOR = 1.49, 95% CI = 1.15, 1.95; wave 7: aOR = 1.12, 95% CI = 1.02–1.24).
Participants who had received at least one dose of the COVID-19 vaccine were significantly less likely to report testing hesitancy when symptomatic at wave 6 (aOR: 0.25, 95% CI: 0.15–0.44) and wave 7 (aOR:0.24, 95% CI: 0.13–0.45), but this relationship was not statistically significant in the wave 5 multivariable model.
The findings from analyzing the COVID-19 disclosure items separately (Supplemental Table 2) show that individual items performed differently across study waves. COVID-19 disclosure to friends was significantly associated with COVID-19 testing hesitancy in unadjusted models across study waves but did not retain significance in adjusted models. Both COVID-19 disclosure stigma to family and to close contacts were significant in unadjusted models in two waves, and each retained significance in one of the waves. The lack of significance for individual items in the adjusted model can be explained by the high correlations among the COVID-19 disclosure stigma items (wave 4 r = 0.62–0.73; wave 5 r = 0.59–0.62; wave 6 r = 0.54–0.61, wave 7 r = 0.53–0.64).
Discussion
This study has identified that within this study population, COVID-19 disclosure stigma is prevalent among US adults and is associated with COVID-19 testing hesitancy. These results echo findings from Earnshaw et al. who cross-sectionally identified a relationship between stigma and COVID-19 testing in April 2020 before vaccine availability.18 The focus of this study on COVID-19 disclosure stigma specifically, as well as the replication of the relationship between COVID-19 disclosure stigma and testing hesitancy across multiple time points, provides additional validation of the results. Study findings highlight that public health interventions should focus on reducing COVID-19 disclosure stigma, as COVID-19 testing and disclosure of testing results to close contacts and peers is imperative to mitigate the pandemic.
The significant reduction in COVID-19 disclosure stigma between study waves 6 and 7 (between June and November of 2021) suggests that people may be more willing to disclose a positive COVID-19 test as the pandemic continues. The ongoing trend in COVID-19 disclosure stigma should be monitored, and factors associated with the change identified throughout the pandemic. For example, since the first at-home rapid test was approved by the Food and Drug Administration in November 2020, at least 15 more at-home tests have been approved. This increased accessibility is useful for reducing viral transmission35 and may have made testing positive for COVID-19 less stigmatizing.
This study also illustrated that participants felt the least comfortable disclosing a positive test result to close contacts, with approximately 20% of participants reporting this concern across all study waves (Fig. 1). This finding suggests that public health interventions should provide conversational tools and strategies to aid individuals in disclosing a positive COVID-19 diagnosis to close contacts. Public health communication programs can also help normalize positive diagnoses and the process of disclosing a positive test to peers by highlighting celebrities or political figures who have tested positive and providing conversation starters and communication strategies to aid individuals in disclosing their positive results to peers.
Anonymity around one's disclosure of a positive result could also mitigate stigma and testing hesitancy. Contact tracing provides a potentially anonymous way to notify contacts of COVID-19, but it is not available in many locations, and traditional models of contact tracing may be less effective with highly contagious strains. Hence, it is still imperative to encourage person-to-person disclosure, especially to households and close network members. Innovative technologies, such as websites, apps, or texting services, have been created by public health entities to anonymously notify a contact of exposure without revealing the identity of the person with the positive test. One such example is TellYourContacts.org, which allows you to send an anonymous text or email to someone with whom you have recently been in close contact. The program also provides templates for those who may not know what to say to their close contacts.36
Another key finding from this study was that approximately 25% of participants reported that they would not be tested for COVID-19 if they experienced symptoms, identifying that COVID-19 testing hesitancy is a critical public health concern. Although COVID-19 disclosure stigma was a strong and consistent predictor of testing hesitancy, age and political orientation were also associated with testing intention. Older age was associated with a decreased odds of COVID-19 hesitancy. This association could be due to greater concern about COVID-19 among older populations, a finding identified by Niño et al.37 Individuals identifying with a greater conservative political ideology were more likely to report COVID-19 testing hesitancy if symptomatic. This finding may be due, in part, to perceived social pressure to downplay the seriousness of COVID-19. Vaccine hesitancy may also be higher among more conservative individuals due to misinformation propagated by conservative news sources and political leaders;38 , 39 these same news sources leaders could be engaged in efforts to normalize testing and disclosure.
In later study waves, COVID-19 vaccination status was found to be significantly associated with testing hesitancy. The finding that individuals who have not been vaccinated are also more hesitant to be tested if symptomatic is alarming. Testing for early detection is essential for unvaccinated individuals because they are more likely to develop severe symptoms if they contract COVID-19, and antiviral medications for COVID-19 are most effective if administered soon after infection.4 Future research should assess barriers to testing for unvaccinated individuals. It may be that these individuals would be more willing to be tested with at-home test kits rather than at public testing facilities. This study also identified a significant increase in COVID-19 testing hesitancy between wave 5 (March 2021) and wave 6 (June 2021) and a decrease between waves 6 (June 2021) and 7 (November 2021). This finding aligns with testing uptake trends in the United States.40 The decrease and increase could be associated with lower and higher rates of COVID-19, respectively, during this period. Further research is needed to understand better the factors associated with these trends. For example, sex was only associated with COVID-19 vaccine hesitancy at wave 6, with females reporting significantly reduced vaccine hesitancy compared to males. As COVID-19 positivity rates were experiencing a downward trend at this time, it may be that females’ compared with males’ testing intention is less sensitive to changing rate of community spread.
The present study is one of the first to assess COVID-19 testing hesitancy and COVID-19 disclosure stigma. Future studies should examine additional drivers of these two underexamined constructs. To expand on the present study, researchers should examine barriers to disclosure and how to make it a more normative behavior. Future research should also examine groups at greater risk of experiencing COVID-19 disclosure stigma as well as intervention strategies to mitigate it. For example, research suggests that stigma related to COVID-19 disproportionately impacts racial/ethnic minoritized groups in the United States.41
Study limitations should be noted. The online MTurk sample may not be generalizable to all US adults, although samples from MTurk have been found to outperform other convenience samples.26 This study is not representative of Hispanic and Asian US residents, which are populations that have been uniquely affected by poor COVID-19 outcomes and discrimination, respectively. Furthermore, this study assessed testing intention rather than testing uptake, and intentions may not reflect behaviors when someone is actually symptomatic. Future studies should assess the outcome of acquiring testing when symptomatic as well as examine delays in COVID-19 testing due to disclosure stigma. Qualitative studies are needed to better understand domains of COVID-19 disclosure stigma and can aid in the development of measurement tools. Future studies should assess barriers and facilitators to COVID-19 testing. Underlying health status, insurance status, living conditions, and local COVID-19 rates may be associated with willingness to get tested for COVID-19 when symptomatic and warrant further examination. Factors associated with COVID-19 stigma also warrant additional research. For example, there may be an interaction between COVID-19 stigma and political party.
The dynamics of the ongoing COVID-19 pandemic depend on the emergence of new variants as well as the rapid identification, intervention, and disclosure of positive cases. Although trends in testing hesitancy are declining, approximately one-quarter of respondents reported hesitancy to be tested when symptomatic—particularly people with more conservative political ideology and those with greater COVID-19 disclosure stigma. These findings suggest that current methods of COVID-19 case monitoring are likely not capturing many positive cases, as a substantial portion of US residents are hesitant to be tested when symptomatic. To keep case counts contained and limited, intervention efforts must focus on reducing testing hesitancy and increasing willingness to disclose positive results to peers. Public health interventions that provide strategies for increasing the disclosure of positive results and facilitating anonymous disclosure are needed.
Author statements
Ethical approval
This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Funding
This study was supported by R01 DA040488 and Alliance for a Healthier World. The authors would like to acknowledge the study participants who shared their time and experiences.
Competing interests
The authors have no conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.08.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Alexander M., Unruh L., Koval A., Belanger W. United States response to the COVID-19 pandemic, January–November 2020. Health Econ Policy Law. 2022 Jan;17(1):62–75. doi: 10.1017/S1744133121000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuchat A., CDC COVID-19 Response Team Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020 May 8;69(18):551–556. doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keith T. The White House has a new plan for COVID-19 aimed at getting things back to normal. NPR. 2022 Mar 2 https://www.npr.org/2022/03/02/1083905865/the-white-house-has-a-new-plan-for-covid-19- aimed-at-getting-things-back-to-norm [Internet] [cited 2022 Mar 28]. Available from: [Google Scholar]
- 4.CDC . Centers for Disease Control and Prevention; 2022. COVID-19 and Your Health [Internet]https://www.cdc.gov/coronavirus/2019-ncov/your- health/treatments-for-severe-illness.html [cited 2022 May 11]. Available from: [Google Scholar]
- 5.Goffman E. Prentice-Hall; Englewood Cliffs, N.J.: 1963. Stigma: notes on the management of spoiled identity. [Google Scholar]
- 6.Link B.G., Phelan J.C. Conceptualizing stigma. Annu Rev Sociol. 2001 Aug 1;27(1):363–385. [Google Scholar]
- 7.Saeed F., Mihan R., Mousavi S.Z., Reniers R.L., Bateni F.S., Alikhani R., et al. A narrative review of stigma related to infectious disease outbreaks: what can be learned in the face of the Covid-19 pandemic? Front Psychiatry. 2020 Dec 2;11 doi: 10.3389/fpsyt.2020.565919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Logie C.H. Lessons learned from HIV can inform our approach to COVID-19 stigma. J Int AIDS Soc. 2020 May;23(5) doi: 10.1002/jia2.25504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Misra S., Le P.D., Goldmann E., Yang L.H. Psychological impact of anti-Asian stigma due to the COVID-19 pandemic: a call for research, practice, and policy responses. Psychol Trauma: Theory Res Pract Policy. 2020;12(5):461–464. doi: 10.1037/tra0000821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020 Jul 1;20(7):782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clouston S.A.P., Natale G., Link B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med. 2021 Jan 1;268 doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y., Twersky S., Ignace K., Zhao M., Purandare R., Bennett-Jones B., et al. Constructing and communicating COVID-19 stigma on Twitter: a content analysis of Tweets during the early stage of the COVID-19 outbreak. IJERPH. 2020 Sep 19;17(18):6847. doi: 10.3390/ijerph17186847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cook J.E., Purdie-Vaughns V., Meyer I.H., Busch J.T.A. Intervening within and across levels: a multilevel approach to stigma and public health. Soc Sci Med. 2014 Feb 1;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 14.Richman L.S., Hatzenbuehler M.L. A multilevel analysis of stigma and health: implications for research and policy. Policy Insights Behav Brain Sci. 2014 Oct 1;1(1):213–221. [Google Scholar]
- 15.Shahrour G., Jaradat D., Dardas L.A. Barriers related to COVID-19 testing intention. Public Health Nurs. 2021 Nov;38(6):978–983. doi: 10.1111/phn.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das M. Social construction of stigma and its implications – observations from COVID-19. SSRN Journal. 2020 https://www.ssrn.com/abstract=3599764 [Internet] [cited 2022 Apr 15]; Available from: [Google Scholar]
- 17.Chaudoir S.R., Fisher J.D. The disclosure processes model: understanding disclosure decision making and postdisclosure outcomes among people living with a concealable stigmatized identity. Psychol Bull. 2010;136(2):236–256. doi: 10.1037/a0018193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Earnshaw V.A., Brousseau N.M., Hill E.C., Kalichman S.C., Eaton L.A., Fox A.B. Anticipated stigma, stereotypes, and COVID-19 testing. Stigma Health. 2020 Nov;5(4):390–393. [Google Scholar]
- 19.Farrimond H. Stigma mutation: tracking lineage, variation and strength in emerging COVID-19 stigma. Sociol Res Online. 2021 Aug 24 doi: 10.1177/13607804211031580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ramaci T., Barattucci M., Ledda C., Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability. 2020 May 8;12(9):3834. [Google Scholar]
- 21.Earnshaw V.A., Watson R.J., Eaton L.A., Brousseau N.M., Laurenceau J.P., Fox A.B. Integrating time into stigma and health research. Nat Rev Psychol. 2022 Apr;1(4):236–247. doi: 10.1038/s44159-022-00034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myrick J.G., Willoughby J.F. The “celebrity canary in the coal mine for the coronavirus”: an examination of a theoretical model of celebrity illness disclosure effects. Soc Sci Med. 2021 Jun;279 doi: 10.1016/j.socscimed.2021.113963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bevan I., Stage Baxter M., Stagg H.R., Street A. Knowledge, attitudes, and behavior related to COVID-19 testing: a rapid scoping review. Diagnostics. 2021 Sep;11(9):1685. doi: 10.3390/diagnostics11091685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Créquit P., Mansouri G., Benchoufi M., Vivot A., Ravaud P. Mapping of crowdsourcing in health: systematic Review. J Med Internet Res. 2018 May 15;20(5):e187. doi: 10.2196/jmir.9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandler J., Shapiro D. Conducting clinical research using crowdsourced convenience samples. Annu Rev Clin Psychol. 2016 Mar 28;12(1):53–81. doi: 10.1146/annurev-clinpsy-021815-093623. [DOI] [PubMed] [Google Scholar]
- 26.Huff C., Tingley D. “Who are these people?” Evaluating the demographic characteristics and political preferences of MTurk survey respondents. Res Politics. 2015 Jul 1;2(3) [Google Scholar]
- 27.Strickland J.C., Stoops W.W. The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Exp Clin Psychopharmacol. 2019 Feb;27(1):1–18. doi: 10.1037/pha0000235. [DOI] [PubMed] [Google Scholar]
- 28.Young J., Young K.M. Don't get lost in the crowd: best practices for using Amazon's Mechanical Turk in behavioral research. J Midwest Assoc Inf Syst. 2019;2019(2):7–34. [Google Scholar]
- 29.Rouse S.V. A reliability analysis of Mechanical Turk data. Comput Hum Behav. 2015 Feb 1;43:304–307. [Google Scholar]
- 30.Link B.G., Mirotznik J., Cullen F.T. The effectiveness of stigma coping orientations: can negative consequences of mental illness labeling be avoided? J Health Soc Behav. 1991 Sep;32(3):302–320. [PubMed] [Google Scholar]
- 31.Link B.G., Struening E.L., Rahav M., Phelan J.C., Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997 Jun;38(2):177–190. [PubMed] [Google Scholar]
- 32.Moses T. Stigma and self-concept among adolescents receiving mental health treatment. Am J Orthopsychiatry. 2009 Apr;79(2):261–274. doi: 10.1037/a0015696. [DOI] [PubMed] [Google Scholar]
- 33.Berger B.E., Ferrans C.E., Lashley F.R. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001 Dec;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 34.StataCorp . StataCorp LLC; College Station, TX: 2022. Stata statistical software. [Google Scholar]
- 35.Dawson L., Kates J. Rapid home tests for COVID-19: issues with availability and access in the U.S. Issue Brief. 2021 https://www.kff.org/report-section/rapid-home-tests-for-covid-19-issues-with-availability-and- access-in-the-u-s-issue-brief/ [Internet] KFF. [cited 2022 Apr 15]. Available from: [Google Scholar]
- 36.TellYourContacts . 2022. Whom should I notify?TellYourContacts.orghttps://tellyourcontacts.org/why-use-this-site/ [Internet] [cited 2022 Apr 15]. Available from: [Google Scholar]
- 37.Niño M., Harris C., Drawve G., Fitzpatrick K.M. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: evidence from two national data sources. SSM Popul Health. 2021 Mar;13 doi: 10.1016/j.ssmph.2020.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Enders A.M., Uscinski J.E., Klofstad C., Stoler J. The different forms of COVID-19 misinformation and their consequences. Harvard Kennedy Sch Misinformation Rev. 2020;1(8) https://nrs.harvard.edu/URN-3:HUL.INSTREPOS:37366466 Available from: [Google Scholar]
- 39.Romer D., Jamieson K.H. Conspiratorial thinking, selective exposure to conservative media, and response to COVID-19 in the US. Soc Sci Med. 2021 Dec 1;291 doi: 10.1016/j.socscimed.2021.114480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Daily Testing Trends in the US - Johns Hopkins [Internet]. Johns Hopkins Coronavirus Resource Center. [cited 2022 Jul 20]. Available from: https://coronavirus.jhu.edu/testing/individual-states.
- 41.Le P.D., Misra S., Hagen D., Wang S.M., Li T., Brenneke S.G., et al. Coronavirus disease (COVID-19) related discrimination and mental health in five U.S. Southern cities. Stigma Health. 2022 Feb 7 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.