Abstract
We report the case of a 71-year-old woman with a skin ulcer derived from an abscess around the tibia. The abscess resulted in periprosthetic joint infection and osteomyelitis 11 years after total knee arthroplasty. The first symptom was a skin ulcer of the lower leg. Magnetic resonance imaging revealed a circumferential mass around the proximal tibia. A skin biopsy taken around the ulcer showed thrombosis and degenerated collagen. Contrast-enhanced computed tomography showed a circumferential mass around the proximal tibia with ring enhancement. Biopsies of the skin ulcer and circumferential mass showed an abscess caused by Enterococcus faecium and methicillin-resistant Staphylococcus epidermis. We conducted debridement of the abscess, a gastrocnemius flap and split-thickness skin grafting and a 2-stage revision of the total knee component with a hinged prosthesis. Two years later, the infection did not reoccur and the patient can walk without a cane. This case is unique as abscess around proximal tibia caused necrotic skin ulcer and appearance of abscess was fibrous and different from typical bacterial abscesses containing pus or fluid. Contrast-enhanced computed tomography was effective for differentiation of the pathological condition.
Keywords: Skin ulcer, Circumferential abscess, Total knee arthroplasty, Contrast-enhanced computed tomography, Ring enhancement
Introduction
Enterococcus, a gram-positive cocci occurring in chains, is a major pathogen in community. The species that are clinically important and the cause of most infections are Enterococcus faecalis and Enterococcus faecium [1]. Enterobacteria can cause bloodstream infections [2,3].
Periprosthetic infection with Enterobacteria, including Enterococcus, has been reported [4]. Enterococci are the third most common Gram-positive pathogens isolated in prosthetic joint infections [5,6]. In this study, we report a case of periprosthetic joint infection and osteomyelitis with circumferential abscess and a skin ulcer caused by Enterococcus and methicillin-resistant Staphylococcus epidermis (MRSE) after total knee arthroplasty. This case is unique as abscess around proximal tibia caused necrotic skin ulcer and appearance of abscess was fibrous and different from typical bacterial abscesses containing pus or fluid.
Case presentation
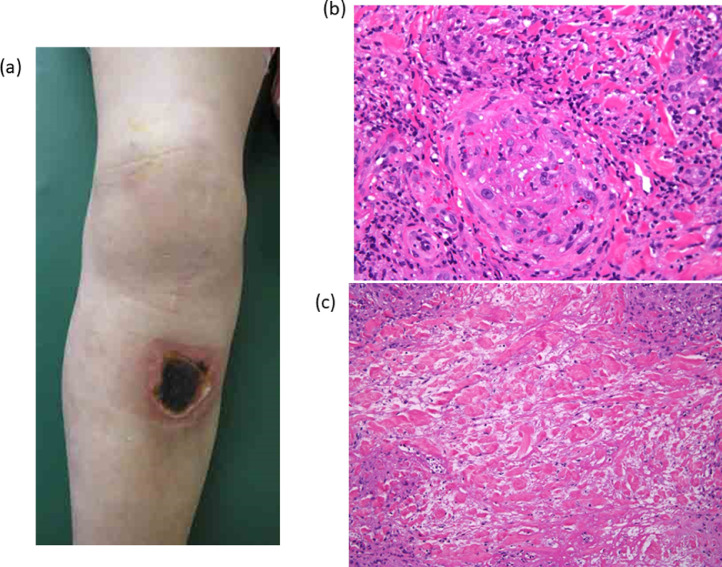
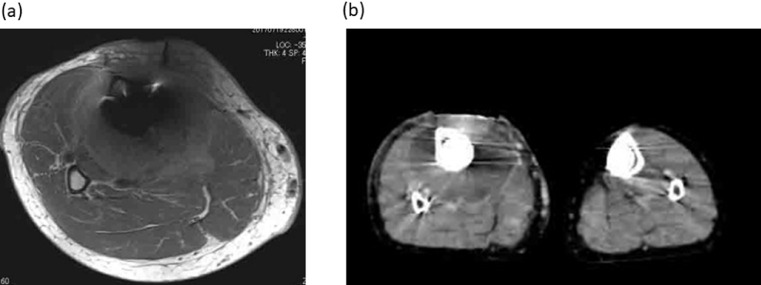
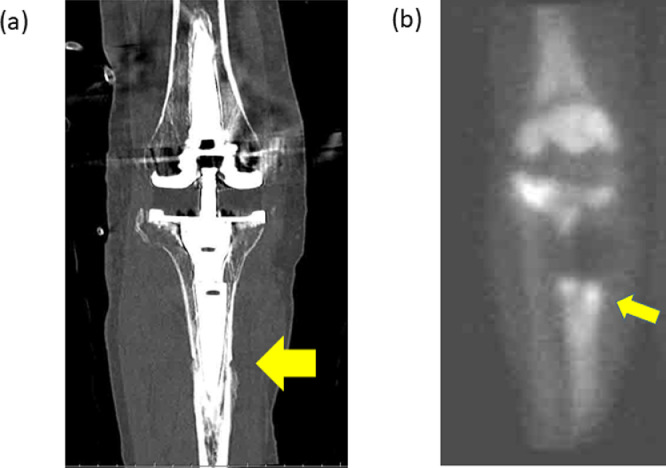
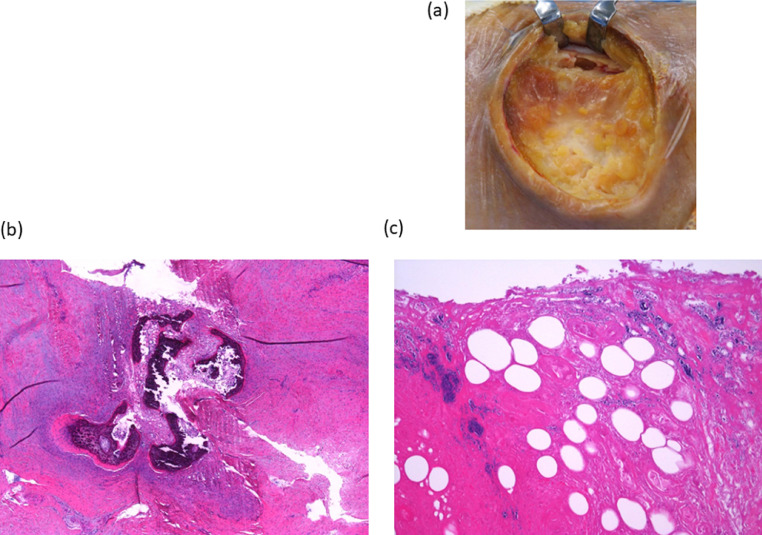
A 71-year-old woman underwent staged bilateral TKA for bilateral knee osteoarthritis 14 years before being treated at our facility. Because of severe instability of the knee, a semi-constrained knee prosthesis with a stem was used for surgery (Fig. 1). Following the procedure, the patient experienced no complications and could walk without a cane during the postoperative period. Eleven years after the primary operation, a necrotic ulcer with reddening of the circumjacent skin developed on the anterior aspect of the right lower leg (Fig. 2A). The patient felt no pain, and the laboratory data indicated no inflammation. A skin biopsy taken around the ulcer showed thrombosis and degenerated collagen (Figs. 2B and C). However, no organism was detected in the bacteriological examination. Magnetic resonance imaging (MRI) revealed a circumferential mass around the proximal tibia (Fig. 3A). Diffusion-weighted MRI showed the patchy mass like legion with metal artifact. Contrast-enhanced computed tomography showed a circumferential mass around the proximal tibia with ring enhancement (Fig. 3B). Plain computed tomography showed a small bone defect in the lateral proximal area and around the middle of the tibia stem (Fig. 4A). High uptake in the same area was confirmed by bone scintigraphy (Fig. 4B). We suspected circumferential abscess formation around the proximal tibia and subsequent osteomyelitis of the tibia. In the operating theater, biopsies were conducted from the proximal tibia and circumferential abscess. The overall circumferential abscess was fibrous and different from typical bacterial abscesses, which contain pus or fluid (Fig. 5A). Bacteriological examination revealed no bacteria in the proximal tibia and E faecium and MRSE in the circumferential abscess. Histological examination showed inflammatory changes, including invasion of neutrophil cells, in the proximal tibia and degenerated collagen with scarce cells in the circumferential abscess (Figs. 5B and C). We diagnosed the circumferential abscess around the proximal tibia caused by E faecium and MRSE. Debridement of the abscess was conducted by expanding the edge of the skin ulcer and the skin defect and subcutaneous tissue were successfully covered by a gastrocnemius flap and split-thickness skin grafting. Four months later, E faecium was detected in the joint fluid. The patient underwent surgery for removal of the femur and tibial components and placement of a cement articulating spacer with vancomycin and amikacin sulfate. E faecium was also detected in the resected tibial bone. Three months later, we performed a 2-stage revision of the total knee component with a hinged prosthesis (Figs. 6A and B). Two years after the revision total knee replacement, the infection did not reoccur and the patient could walk without a cane (Fig. 6C).
Fig. 1.
Plain radiographs of the right knee after the primary total knee arthroplasty.
Fig. 2.
(A) Necrotic ulcer with reddening of the circumjacent skin at the anterior aspect of the right lower leg. Histology of the skin biopsy specimen (H&E staining) showing (B) thrombosis and (C) degenerated collagen.
Fig. 3.
(A) Magnetic resonance imaging showing circumferential mass around the proximal tibia. (B) Contrast-enhanced computed tomography showing a circumferential mass around the proximal tibia with ring enhancement.
Fig. 4.
(A) Plain computed tomography showing a small bone defect in the lateral proximal area and around the middle of the tibia stem component. (B) Bone scintigraphy showing a high uptake in the lateral proximal area and around the middle of the tibia stem component.
Fig. 5.
(A) Fibrous abscess around proximal tibia. (B) Histology of the biopsy specimen from the proximal tibia (H&E staining) showing inflammatory changes including invasion of neutrophils. (C) Histology of the biopsy from the circumferential abscess (H&E staining) showing degenerated collagen with scarce cells.
Fig. 6.
(A,B) X-ray of the right lower limb after revision TKA. (C) Picture of the right lower limb 2 years after revision TKA.
The Hospital Ethics Committee audited and approved the treatment protocol.
Discussion
We report a rare case of a circumferential abscess around the proximal tibia that, subsequently, developed into a periprosthetic knee infection and osteomyelitis of the tibia 11 years after the primary TKA surgery. The patient's first symptom was a small necrotic ulcer with reddening of the circumjacent skin. At this time, no specific pathologic findings were revealed by the skin biopsy, and no organism was detected by bacteriological examination; therefore, no specific diagnosis was made. In MRI, DW1 image showed the patchy mass like legion with metal artifact which indicate abscess or tumor. In imaging of limb with metal implant, artifact from metal prosthesis often results in poor image quality [7]. The field-strength difference between the inside of a metallic implant and in the surrounding tissues, as well as the magnitude of field-strength gradients close to tissue-metal borders can cause artifacts in MRI scans and impair the diagnostic value of MRI for the assessment of peri-implant tissues [8]. In contrast-enhanced computed tomography, also some metallic artifacts were observed, the image showed a circumferential mass around the proximal tibia with ring enhancement which indicate abscess formation. In previous report about diagnosis of deep neck abscesses by contrast-enhanced computed tomography, if fluid collection with ring enhancement was observed, the positive predictive value of deep neck abscess was 85% [9]. By open biopsy the circumferential mass was diagnosed as an abscess caused by E faecium and MRSE. In previous report, E faecium was detected in diseased gall bladders because of biliary calculi or symptomatic cholelithiasis [10]. However, in this patient, no biliary calculi were detected by abdominal ultrasound, and Enterococcus were not detected in the patient's stool culture. Thus, the original focus of the Enterococcus infection in this patient is unknown.
The appearance of circumferential abscess around the proximal tibia in this patient was fibrous and different from typical bacterial abscesses containing pus or fluid. Histological examination showed degenerated collagen in the circumferential abscess. E faecium may have caused the fibrous tissue abscess. The increased virulence of E faecium is accompanied by the production of adhesion proteins, autolysin, and collagenases. Adhesion protein production occurs in E faecium expressing Acm, a gene that enables the production of wall-anchored adhesion proteins attaching to extracellular collagen. Autolysins are proteins enabling cell wall degradation and biofilm formation. The ability to produce these proteins may explain how Enterococci could degrade collagen in the extracellular matrix [11].
We report a rare case of periprosthetic joint infection and osteomyelitis of the tibia with a circumferential abscess and skin ulcer 11 years after TKA. Contrast-enhanced computed tomography was effective for the diagnosis of circumferential abscess around tibia.
We conducted soft tissue reconstruction and then a 2-stage revision of the knee prosthesis. Curing the infection and functional recovery were achieved 2 years after the final treatment.
Conclusion
We report a rare case of osteomyelitis of the tibia with a circumferential abscess and skin ulcer 11 years after TKA. We first conducted soft tissue reconstruction and then a 2-stage revision of the knee prosthesis. Curing the infection and functional recovery were achieved after the final treatment. Contrast-enhanced computed tomography was the most valuable tool for the diagnosis of circumferential abscess around tibia.
Patient consent
Informed consent for the procedure and publication of data was obtained from the patient and documented.
Footnotes
Competing Interests: There are no conflicts of interest to declare.
References
- 1.Hemapanpairoa J, Changpradub D, Thunyaharn S, Santimaleeworagun W. Does vancomycin resistance increase mortality? Clinical outcomes and predictive factors for mortality in patients with Enterococcus faecium infections. Antibiotics (Basel) 2021;10(2):105. doi: 10.3390/antibiotics10020105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandey S, Raza S, Bhatta CP. The aetiology of the blood stream infections in the patients who presented to a tertiary care teaching hospital in Kathmandu, Napal. J Clin Diagn Res. 2013;7:638–641. doi: 10.7860/JCDR/2013/4752.2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diekema DJ, Hsueh PR, Mendes RE, Pfaller MA, Rolston KV, Sader HS, et al. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother. 2019;63 doi: 10.1128/AAC.00355-19. e00355-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasouli MR, Tripathi MS, Kenyon R, Wetters N, Della Valle CJ, Parvizi J, et al. Low rate of infection control in enterococcal periprosthetic joint infections. Clin Orthop Relat Res. 2012;470:2708–2716. doi: 10.1007/s11999-012-2374-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Renz N, Trebse R, Akgün D, Perka C, Trampuz A, et al. Enterococcal periprosthetic joint infection: clinical and microbiological findings from an 8-year retrospective cohort study. BMC Infect Dis. 2019;19:1083. doi: 10.1186/s12879-019-4691-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thompson O, Rasmussen M, Stefánsdóttir A, Christensson B, Akesson P, et al. A population-based study on the treatment and outcome of enterococcal prosthetic joint infections. A consecutive series of 55 cases. J Bone Jt Infect. 2019;4:285–291. doi: 10.7150/jbji.35683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong N, Zailan I, Tandon A. Imaging update in arthroplasty. J Clin Orthop Trauma. 2021;23 doi: 10.1016/j.jcot.2021.101649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Christoph Germann C, Nanz D, Sutter R. Magnetic resonance imaging around metal at 1.5 Tesla: techniques from basic to advanced and clinical impact. Invest Radiol. 2021;56(11):734–748. doi: 10.1097/RLI.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 9.Freling N, Roele E, Schaefer-Prokop C, Fokkens W. Prediction of deep neck abscesses by contrast-enhanced computerized tomography in 76 clinically suspect consecutive patients. Laryngoscope. 2009;119(9):1745–1752. doi: 10.1002/lary.20606. [DOI] [PubMed] [Google Scholar]
- 10.Manolis EN, Filippou DK, Papadopoulos VP, Kaklamanos L, Katostaras T, Christianakis E, et al. The culture site of the gallbladder affects recovery of bacteria in symptomatic cholelithiasis. J Gastrointestin Liver Dis. 2008;17:179–182. [PubMed] [Google Scholar]
- 11.Belmouhand M, Krohn PS, Svendsen LB, Henriksen A, Hansen CP, Achiam MP, et al. The occurrence of Enterococcus faecium and faecalis is significantly associated with anastomotic leakage after pancreaticoduodenectomy. Scand J Surg. 2018;107:107–113. doi: 10.1177/1457496917731188. [DOI] [PubMed] [Google Scholar]