Abstract
To determine whether variables such as Age, Gender, Demographic background of the patient and Pre-operative usage of hearing aids affect the outcomes of pediatric cochlear implant surgery when modified; in terms of speech and hearing gain. A hospital based retrospective-prospective type of cohort study was conducted over a period of 5 years at a Tertiary care Teaching hospital and referral centre covering a population of about 68.9 million. Candidates selected were 1–5 years of age with bilateral congenital severe-profound sensori-neural hearing loss. 50 patients were selected and were operated using VERIA technique of Cochlear Implant Surgery. Intraoperative testing of electrode functioning was done in all patients using NRT technique. The switching on of implant was done after 1 month, following which patients underwent 100 sessions of auditory verbal therapy and training. Outcomes were evaluated in terms of hearing and speech gain by using Revised CAP scores, ITMAIS scores and PEACH scores in the loco-regional language. Those implanted at a younger age and with at least 3 months of hearing aid usage pre-operatively had better outcomes measures. There was no effect on outcomes when the gender and demographic origin of the patient were compared. Candidates implanted before 3 years age give better results and they should be encouraged to use hearing aid regularly and continuously before the surgery and should be advised trial and fitting as soon as CI planning begins. Also, gender and demographic background should not be considered when planning CI as these have no significant effect on outcomes.
Keywords: Cochlear implants, Deaf and mute, CAP, PEACH, IT-MAIS
Introduction
A recent WHO estimate suggests that world-wide approximately 466 million people (or 6.1% of the world’s population) are living with disabling hearing loss as in 2018. This estimate is projected to rise to 630 million by 2030 and to over 900 million by 2050. Approximately 90% of people with moderate to profound hearing impairment reside in low- and middle-income countries [1]. (Tables 1, 2, 3, 4 and 5).
Table 1.
IT-MAIS and PEACH scores comparison with age
| Age (years) | IT-MAIS score | Peach score |
|---|---|---|
| ≤3 | 34.93 + 2.15 | 45.26 + 4.69 |
| >3.1 | 31.42 + 4.54 | 38.65 + 9.59 |
| p value | 0.005 | 0.014 |
The above table shows a statistically significant difference is present between the 2 scores with better scores in the candidates implanted before 3 years of age
Table 2.
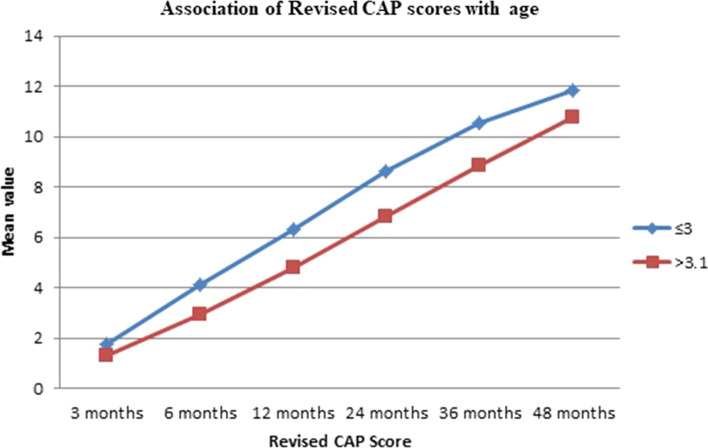
Association of Revised CAP score with age
| Age (years) | 3 months | 6 months | 12 months | 24 months | 36 months | 48 months |
|---|---|---|---|---|---|---|
| ≤3 | 1.73 + 1.16 | 4.13 + 0.83 | 6.33 + 0.61 | 8.6 + 0.63 | 10.53 + 0.63 | 11.86 + 0.35 |
| >3.1 | 1.28 + 1.04 | 2.91 + 1.26 | 4.8 + 1.34 | 6.8 + 1.41 | 8.88 + 1.40 | 10.77 + 1.06 |
| p value | 0.185 | 0.001 | 0.0001 | <0.0001 | <0.0001 | 0.0003 |
The above table shows the relation between Revised CAP scores and their age association in those less than or more than 3 years of age. It indicates better scores for younger age groups at each of the monthly evaluation interval with a significant p value for all intervals except for at 3 months which is the score at earliest measuring time interval
Table 3.
Correlation between revised CAP scores according to age
| Revised CAP score at months | R value | P value |
|---|---|---|
| 3 | −0.158 | 0.271 |
| 6 | −0.372 | 0.007 |
| 12 | −0.514 | 0.0001 |
| 24 | −0.613 | <0.0001 |
| 36 | −0.57 | <0.0001 |
| 48 | −0.514 | 0.0001 |
The above table shows the correlation between age and revised CAP scores at monthly evaluation intervals. A statistically significant relation between younger age and higher scores is seen to be present
Table 4.
IT MAIS scores comparison with hearing aid usage
| Hearing aid usage pre op | IT-MAIS scores of the particular group (mean + SD) | IT-MAIS scores of all the rest implantees (mean + SD) | p value |
|---|---|---|---|
| Not used | 31 + 5 | 33 + 4 | 0.119 |
| <3 months | 29 + 3 | 34 + 4 | 0.0006 |
| >3 months | 35 + 3 | 30 + 4 | <0.0001 |
The above table depicts that the scores of IT-MAIS were better when the patients had used hearing aids pre-operatively with the condition that the usage was consistent and for 3 months at least. In the rest 2 categories that is no usage and less than 3 months or inconsistent usage the scores were less than the remaining group of candidates
Table 5.
PEACH scores comparison with hearing aid usage
| Hearing aid usage pre op | PEACH scores of the particular group (mean + SD) | PEACH scores of all the rest implantees (mean + SD) | P value |
|---|---|---|---|
| Not used | 38 + 7 | 41 + 9 | 0.254 |
| <3 months | 36 + 8 | 42 + 9 | 0.027 |
| >3 months | 44 + 9 | 37 + 8 | 0.002 |
The above table depicts that the PEACH scores were better when the patients had used hearing aids pre-operatively with the condition that the usage was consistent and for 3 months at least. In the rest 2 categories that is no usage and less than 3 months or inconsistent usage the scores were less than the remaining group of candidates
For many, hearing aids provide a viable solution, but if one experiences significant hearing loss, hearing aids may offer little or no benefit. This is where cochlear implants (CI) come into role.
A cochlear implant is a hearing prosthesis designed to restore or provide a level of auditory sensation to adults and children who have severe to profound bilateral sensori-neural hearing impairment and who get limited benefit from hearing aids [2].
Cochlear implants provide an effective alternative to hearing aids because they don’t use amplification; instead they bypass the damaged part of the ear and use electrical stimulation to enable hearing.
It is a highly advanced medical device and is the only technology capable of functionally restoring one of the five senses.
Children with profound sensori-neural hearing loss are at significant risk for serious speech and language delays that can impact their communication, academics, and social development. There is accumulating evidence that insufficient auditory stimulation during critical periods of a child’s development will lead to linguistic and communicative deficits. Therefore, profoundly deaf children who derive little or no benefit from conventional hearing aids should be implanted early in life. Use of a cochlear implant has been associated with stronger outcomes in speech perception, speech production, language, and reading compared with children using conventional hearing aids. However, the variability in these results among children is high, and many factors seem to contribute to the successful use of cochlear implants; some children with CIs acquire language skills within normal limits while other children remain far below average.
Previous studies have identified a number of factors that appear to be directly related to spoken language development in children using CIs. These factors include the age at which the hearing loss is identified, the age at which cochlear implantation occurs, the amount of normal hearing experience a child has had prior to losing hearing, usage of hearing aids before implantation, gender variability, socio-economic background, the nature of interpersonal communication to which the child is exposed and associated co morbidities - infectious or syndromic if present.
Tracking of the progress of the implanted candidates post-surgery in terms of auditory and speech gain is done using various scoring systems. Used in this study are the Revised Category of Auditory Performance (CAP) score, Infant–Toddler Meaningful Auditory Integration Scale (IT-MAIS) and Parent’s Evaluation of Aural/Oral Performance of Children (PEACH) score.
The Revised Category of Auditory Performance (CAP) score [3] is described by The Shepherd Centre based on Nottingham CI Program. It assesses the extent of auditory perception, in terms of utility of auditory mechanisms to pursue day to day tasks. The ability to discriminate and understand speech with or without lip reading can also be assessed and the results are categorized accordingly and a score given, taking into account the number of months taken to achieve it. The revision was designed to add more levels into the higher part of the scale, in order to reflect and monitor advanced listening skills targeted for acquisition prior to school, with the implementation of universal newborn hearing screening.
The Infant–Toddler Meaningful Auditory Integration Scale (IT-MAIS) [4, 5] is a modification of the Meaningful Auditory Integration Scale (MAIS) given by Robbins et al. in 1991 [6]. It is a structured interview schedule designed to assess the child’s spontaneous responses to sound in his/her everyday environment. The assessment is based upon information provided by the child’s parent(s) in response to 10 probes each with specific scoring criteria. These 10 probes assess three main areas:
Vocalization behaviour;
Alerting to sounds; and
Deriving meaning from sound.
The Parent’s Evaluation of Aural/Oral Performance of Children (PEACH) [7] was developed to evaluate the effectiveness of amplification for infants and children with hearing impairment by a systematic use of parent’s observations. It was developed as a measure of functional performance in everyday life. It was recognized that parents spend much time with their children in a range of environments and would therefore be the best observers and informants of a child’s aural and oral abilities in daily life [8]. Because the primary goal of amplification is to ensure audibility for a wide range of speech input levels and frequencies [9, 10], the items focus on aural/oral behaviours in speech communication situations in real life.
The advent of universal neonatal hearing screening program and the wide acceptance of cochlear implantation as an effective method of management for profound deafness has significantly lowered the mean age of implantation. But, apart from age many other factors are also responsible for the varied outcomes observed amongst the Cochlear implanted children, some of these have been studied in detail and other are yet to be explored completely and conclusive studies regarding them are still lacking. The age of implantation, use of a pre implantation hearing aid, demographic background of the candidate and gender variations all have an impact, whether major or not on the outcomes of a Cochlear Implant surgery and these are the variables we intend to study here.
Methodology
Design: Hospital based retrospective-prospective type of cohort study.
Study area: Department of Otorhinolaryngology and Head and Neck Surgery, Dr. S.N. Medical College and M.D.M.Hospital, Jodhpur, Rajasthan, India
Sample Size: 50 patients undergoing Cochlear Implantation were included in this study.
Inclusion criteria
1 year of age or older and below 5 years.
Bilateral severe to profound sensori-neural hearing loss.
Insufficient hearing despite consistent hearing aid use to enable the development of functional speech and spoken language.
Patient willing to undergo the procedure after knowing all the aspects of follow up and actual outcomes with regard to expectations.
Exclusion criteria
Absent cochlear nerve.
Absent cochlea
Age above 5 years
Active Infection in ear
Abnormal cochlear anatomy
Patient having any other cardiac anomalies (VSD, ASD, etc.)
Patient having any other CNS disorders
Patients with psychological disorders
Patient not fit for General Anesthesia
The study was carried out by means of information obtained through patients who underwent CI surgery in the service of Otorhinolaryngology department of Dr. S. N. Medical College, Jodhpur, Rajasthan, India. Ethical committee approval was obtained before beginning the study. The patients were analyzed by gender etiology, age at the time of surgery, demographic location and usage of hearing aids preoperatively. The patients were selected for cochlear implantation after thorough evaluation of their type and degree of hearing loss, lack of benefit with hearing aids, radiological determination of the temporal bone–cochlear anatomy for feasibility for implantation, adequate parental motivation for habilitation, obtaining explained consent for the procedure and evaluating the possibility/accessibility of pre- and post-implantation habilitation/therapy and programming centers.
Operative technique:
All the patients were operated using VERIA technique of Cochlear Implant Surgery under General Anesthesia under complete sterile conditions and with all aseptic precautions. The Veria technique for Cochlear implantation is a non-mastoidectomy technique which is done through the endaural route for the cochleostomy, with a transcanal tunnel drilled in the posterior canal wall. This technique uses a specially designed perforator to make the tunnel in the posterior canal wall [Fig. 1]. Though the conventional technique has been successful it is more time consuming and is prone to various complications especially in children with small facial recess, cochlear malformations and cochlear rotation. This technique is simple, helps in faster healing and earlier fitting of the processor, is precise thereby minimizing trauma to the facial nerve. The surgery can be performed in infants who have not yet developed the mastoid completely [11]. Intraoperative testing of Implant and electrode functioning was also done in all patients using Neural Response Telemetry (NRT) technique. (Figure 2)
Fig. 1. A.

–Specially designed Veria handpiece and B–Veria tunnel (black asterix) created in posterior canal wall leading into middle ear (white star)
Fig. 2.
Line diagram showing association of revised CAP scores with age
Follow up:
The patients were followed up after discharge and the external device fitting and switching on of implant was done after 1 month. Following that these patients underwent 100 sessions of auditory verbal therapy and training with timely evaluation using Revised CAP scores, IT-MAIS scores and PEACH scores in the loco-regional language.
Statistical analysis:
Qualitative data was expressed in the form of proportion and percentages.
Quantitative data were expressed in mean ± SD.
Unpaired t test was used for comparable quantitative variables.
Correlation coefficient was calculated for quantitative variables.
A p-value of < 0.05 was assumed to be statistically significant.
Statistical Package for Social Sciences (SPSS) version 22.0 was used for analysis.
Outcome variable:
Revised CAP scores, IT-MAIS scores and PEACH scores comparison of all the cases with regard to variations according to age, sex, demography and hearing aid usage.
Results
There were a total of 50 candidates with 29 being male and 21 females. 15 of these patients were below the age of 3 years when implanted and the rest were older than 3 years. 26 were from rural demographic background and 24 from urban areas. 25 of these were consistent users of hearing aids pre-operatively for at least 3 months, 14 used inconsistently or used for less than 3 months and 11 did not use the hearing aid at all.
Rest results can be summarized by tables given below.
Discussion
Cochlear implants have transformed the management of severe to profound hearing loss, particularly in the very young and delayed speech and hearing since birth population.
The technology has had the greatest impact in transforming the education of children born with a profound hearing loss who are implanted early. Majority of these children attend mainstream education, using spoken language to communicate.
Careful counselling of parents is crucial to decision-making and to ensure realistic expectations of outcome.
Advances in technology in recent years, in particular the improvement in speech-processing strategies, have led to improved speech perception with CI. In infants, speech perception is of paramount importance for the development of spoken language.
In the past years, data on the post-operative outcomes following cochlear implantation have identified a wide spectrum of variables known to affect post-implantation performance. These variables relate to the device itself, including electrode design, speech processing strategies, and device reliability, as well as individual patient characteristics such as cochleo-vestibular anatomy, presence of associated disabilities, age at implantation, gender of candidate, hearing aid usage and the cause of deafness. Social and educational factors, such as mode of communication, parents/family expectations, demographical background of the patient, post implantation rehabilitation, and socio economic status are additional variables shown to affect post-operative performance.
Despite extensive research examining the post implantation outcomes, the considerable variability in post-operative performance remains incompletely understood. Predictions of post implantation benefits should be individualised and based on comprehensive preoperative assessment, with attention to the complex interplay of the patient and device characteristics. Detailed knowledge of these variables not only improves clinician’s predictive accuracy but may also reveal factors that can be manipulated to achieve optimal performance.
Age at implantation is probably one of the most exhaustively studied variable affecting CI surgery outcomes.
Anderson et al. [12] reviewed data of 37 children who had received their cochlear implants before the age of 2 years and compared to those implanted at a later age using various tests including IT-MAIS scores. Performance of children implanted under the age of 2 years was compared to the performance of 36 children implanted between 2 and 4 years of age and 27 children implanted between 4 and 6 years of age. After one and a half to 2 years of cochlear implant use, children implanted before 2 years of age performed better in terms of auditory listening skills than their peers implanted at a later age.
Mohan Kameswaran et al. [13] performed a retrospective study involving 100 patients who underwent cochlear implantation. The outcome of cochlear implantation was measured using CAP scores. With early CI in children between 1and 5 years, the outcome was very gratifying. They supported very early implantation to facilitate a series of developmental processes occurring in the critical period of initial language acquisition.
Myung Whan Suh et al. [14] studied 86 pre-lingual deaf children with profound hearing loss and who underwent cochlear implantation before the age of 6 and who had been followed for more than 3 years and concluded that early implantation, within the critical period, was associated with better outcomes and that 2 years of age is the critical time point to perform cochlear implantation in a child.
Kumar Suman et al. [15] conducted a study regarding age of pediatric Cochlear implant patients and evaluated them using PEACH scores in the patient’s native tongue (Parents’ Evaluation of Aural/Oral Performance of Children). Their results revealed that children who received implants before 2 years showed significant higher language ability to function in daily life as compared to those received at 3–4 years.
In consistence with the above studies, in our study we found out similar results. All 3 evaluation parameters- Revised CAP scores, the IT-MAIS scores and PEACH scores had better values for children implanted at a younger age and the difference in scores was also statistically significant.
Thus, younger age seems to be consistently associated with better outcomes. Those implanted after 3 years of age may struggle to catch up and a proportion of children may remain language delayed when compared to their normal hearing peers [16, 17]. The importance of early implantation is due to the fact that there is a sensitive period of around 2–3 years during which the development of the central auditory system shows greatest neural plasticity [18].
There are some studies which indicate that gender might also have a role to play regarding the outcomes of cochlear implanted candidates.
In their records regarding the studies of children with cochlear implants, Geers et al. [19, 20] concluded that female children have been showing better results in language than male children. They compared 181 children implanted before the age of 5 years and found results favouring females with a statistically significant p-value for the scores they used; thus concluding that gender does affect outcomes [9].
Mendes et al. [21] found that no significant differences existed in the results of Cochlear implanted patients when the outcome was evaluated with respect to the gender of the candidate.
Ramos et al. [22] concluded that gender had no significant influence in the development of the linguistic skills in children with severe to profound congenital bilateral sensori–neural deafness after cochlear implantation. They studied 30 children, 12 females and 18 males with severe to profound bilateral sensori-neural hearing loss with cochlear implants. On analysis it was found that in all three linguistic structures studied, semantics, morphosyntax and phonology, the values of the scores obtained for each gender were very similar. They were generally higher in male children than in female children, however, there were no statistically significant differences.
In our study we found that although the scores were marginally higher in the male implanted candidates but these were insignificant statistically. Overall the outcomes were the same in both male and female implantees. This is in contrast with the study of Geers et al. [19] but similar with the studies of Mendes et al. [21] and Ramos et al. [22].
Thus gender seems to play no role in modifying outcomes, although the number of male candidates seems to be higher than females. This is probably due to the sex ratio in this part of our world and decreased awareness and concern regarding the female child which needs to be addressed and corrected upon by spreading more and more education.
The candidates were also compared with respect to their demographic location whether urban or rural. Although, exactly similar studies in this regard were not available as per to our knowledge and research. Still a study by Bush et al. in [23] of 40 children with congenital hearing loss who were considered for cochlear implantation showed that a linear relationship exists between distance to the implant centre and timing of hearing aid amplification and cochlear implantation. Thus concluding to the point that children residing outside of metro areas may be at higher risk of delayed rehabilitative services and cochlear implantation than those residing in urban areas that may be closer in proximity to tertiary care centres
In our study we found that 48% of our patients were of urban demographical background and the rest 52% belonged to rural areas. The IT-MAIS scores of the urban candidates were marginally higher than the rural candidates and vice versa was found for PEACH scores. The CAP scores were better with urban patients at 3, 6, 12 and 24 months of evaluation and with rural patients at 36 and 48 months. But for all these differences in scores, the variations were only marginal and statistically insignificant.
Demographic location affects the outcomes as access to higher healthcare centres is difficult for persons residing in rural areas, and even if they access it initially for surgery, a vigorous follow up is then required for speech and auditory training which requires repeated visits many times over many years thus posing a difficult task as more travel and more motivation on the part of parents is required, thus affecting outcomes.
In our study, demographical background and its effect on outcomes was not found to be significant, although, this can be justified by the fact that more than usual and very special emphasis was made by our team for proper motivation and counseling of the patient and patient’s relatives pre-operatively and also consistently throughout the duration of hospital stay and post-operative rehabilitation. This helped to overcome factors such as distance to the therapy center and dropout or lost to follow up cases.
Hearing aid usage pre-operatively also affects the CI outcomes. Johanna Grant Nicholas and Ann E. Geers [24] studied the spoken language skills of 76 children who had used a cochlear implant and found the amount of pre-implant intervention with a hearing aid was not related to language outcome at 3.5 years of age.
In our study we concluded that consistent and at least 3 months of usage of hearing aids pre implantation resulted in better outcomes in all 3 scores. Also, no usage and even inconsistent use was associated with poorer outcomes compared to the contrary.
Thus, the usage of pre-implantation hearing aids also helps to improve outcomes but consistent and proper usage is compulsory. It also makes the child acclimatise to having a device fitted over ear and external part of skull and thus helps to improve compliance with CI usage post-implantation.
Conclusion
Thus, the variables affecting performance with a Cochlear implant are diverse, symbiotic and continually evolving with advances in implant technology and ever expanding candidacy criteria. Research into the factors discussed here, as well as their complex interrelationship, affords both clinicians and patients a greater understanding of post implantation performance.
Even within an individual CI recipient, the significance of certain variables may change with time, with increasing patient age, new technology, or increased experience with the implant. Our study, to summarise, indicates better results with younger age and pre-operative consistent hearing aid usage. Also the gender and demography do not seem to affect the outcomes albeit there is proper audiological follow up. Although the confounding effect of these variables needs to be considered and effects on outcomes due to a wide variety of other known and unknown factors cannot be disregarded, this will be an ever on-going research and these studies add up to the pool of data on variables affecting implant outcomes for a larger meta-analysis considering the results over a longer period of time and follow up.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Compliance with Ethical Standards
Conflict of interest
All the authors declare that they have no conflict of Interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shivam Sharma, Email: shivam92@hotmail.com.
Bharti Solanki, Email: drbhartisolanki@gmail.com.
Yogesh Solanki, Email: yogesh_solanki@yahoo.com.
Yogesh Kaurani, Email: kaurani.yogesh@gmail.com.
References
- 1.Addressing the rising prevalence of hearing loss. Geneva: World Health Organization; 2018. Available from: http://www.who.int/pbd/deafness/estimates/en/ Accessed on 02.04.2020
- 2.Waltzmann S, Roland JT. Cochlear Implants. 2. New York: Thieme Publishers; 2006. [Google Scholar]
- 3.http://adipcochlearimplant.in/ADIP_PDF/CAP%20and%20ISD%20scales.pdf as Accessed on 12.05.2020
- 4.https://advancedbionics.com/content/dam/advancedbionics/Documents/Regional/BR/AB_IT-MAIS_Resource.pdf - as Accessed on 12.05.2020
- 5.Zimmerman-Phillips S, Robbins AM, Osberger MJ. Assessing cochlear implant benefit in very young children. Ann Otol Rhinol Laryngol. 2000;109(12):42–43. doi: 10.1177/0003489400109S1217. [DOI] [PubMed] [Google Scholar]
- 6.Robbins AM, Renshaw JJ, Berry SW. Evaluating meaningful auditory integration in profoundly hearing impaired children. Am J Otol. 1991;2(Suppl):144–150. [PubMed] [Google Scholar]
- 7.https://www.grapevineaudiology.com/wp-content/uploads/sites/84/2016/07/PEACH-Questionnaire.pdfas Accessed on 12.05.2020
- 8.Boudreau D. Use of a parent questionnaire in emergent and early literacy assessment of preschool children. Lang Speech Hear Serv Sch. 2005;36(1):33–47. doi: 10.1044/0161-1461(2005/004). [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Audiology. (2003) Pediatric amplification protocol. http://www.audiology.org/NR/rdonlyres/53D26792-E321-41AF-850F-CC253310F9DB/0/pedamp.pdf
- 10.Joint Committee on Infant Hearing Year 2000 position statement: principles and guidelines for early hearing detection and intervention programs. Am J Audiol. 2000;9:9–29. doi: 10.1044/1059-0889(2000/005). [DOI] [PubMed] [Google Scholar]
- 11.Hans JM, Prasad R. Cochlear implant surgery by the veria technique: how and why? experience from 1400 cases. Indian J Otolaryngol Head Neck Surg. 2015;67(2):107–109. doi: 10.1007/s12070-015-0863-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson I, Weichbold V, D’Haese PS, Szuchnik J, Quevedo MS, Martin J, Martin J, Dieler WS, Phillips L. Cochlear implantation in children under the age of two—what do the outcomes show us? Int J Pediatr Otorhinolaryngol. 2004;68:425–431. doi: 10.1016/j.ijporl.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Kameswaran M, Raghunandhan S, Natarajan K, Basheeth N. Clinical audit of outcomes in Cochlear Implantation an Indian experience. Indian J Otolaryngol Head Neck Surg. 2006;58(1):69–73. doi: 10.1007/BF02907745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suh MW, Cho EK, Kim BJ, Chang SO, Kim CS, Oh SH. Long term outcomes of early cochlear implantation in Korea. Clin Exp Otorhinolaryngol. 2009;2(3):120–125. doi: 10.3342/ceo.2009.2.3.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar S, Rout N, Kumar N, Chatterjee I, Selvakumaran H. Performance of indian children with cochlear Implant on PEACH Scale. ISRN Otolaryngol. 2013;2013:565096. doi: 10.1155/2013/565096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nicholas JG, Geers A. Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe to profound hearing loss. J Speech Lang Hear Res. 2007;50:1048–1062. doi: 10.1044/1092-4388(2007/073). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geers A. Speech, language and reading skills after early cochlear implantation. Arch Otolaryngol Head Neck Surg. 2004;130:634–638. doi: 10.1001/archotol.130.5.634. [DOI] [PubMed] [Google Scholar]
- 18.Sharma A, Dorman M, Spahr A. A sensitive period for the development of the central auditory system in children with cochlear implants: implications for age of implantation. Ear Hear. 2002;23:532–539. doi: 10.1097/00003446-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Geers A, Nicholas J, Sedey A. Language skills of children with early cochlear implantation. Ear Hear. 2003;24(1Suppl):46S–58S. doi: 10.1097/01.AUD.0000051689.57380.1B. [DOI] [PubMed] [Google Scholar]
- 20.Geers AE, Nicholas JG, Moog JS. Estimating the influence of cochlear implantation on language development in children. Audiol Med. 2007;5(4):262–273. doi: 10.1080/16513860701659404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mendes JCDP, Pandolfi MM, Carabetta Júnior V, Novo NF, Colombo-Souza P. Fatores associados a alteração da linguagem em crianças pré-escolares. Rev Soc Bras Fonoaudiol. 2012;17(2):177–181. doi: 10.1590/S1516-80342012000200013. [DOI] [Google Scholar]
- 22.Ramos D, Jorge JX, Teixeira A, Ribeiro C, Paiva A. Development of language skills in children with cochlear implants: does the gender have any influence? Rev. CEFAC. 2015;17(2):535–541. doi: 10.1590/1982-021620155214. [DOI] [Google Scholar]
- 23.Bush ML, Burton M, Loan A, Shinn JB. Timing discrepancies of early intervention hearing services in urban and rural cochlear implant recipients. Otol Neurotol. 2013;34(9):1630–1635. doi: 10.1097/MAO.0b013e31829e83ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicholas JG, Geers AE. Effects of early auditory experience on the spoken language of deaf children at 3 years of age. Ear Hear. 2006;27:286–298. doi: 10.1097/01.aud.0000215973.76912.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]