Abstract
Benign Paroxysmal Positional Vertigo (BPPV), the most common vestibular disorder characterized by recurrent, brief episodes of vertigo, is attributed to the presence of otoconia in the semicircular canals. Two mechanisms contribute to its cause-canalolithiasis (otoconia freely mobile in the semicircular canal) and cupulolithiasis (otoconia adherent to the cupula). Posterior semicircular canal is the most common canal involved. Although the occurrence of BPPV in lateral and superior semicircular canal is rare, with the advancement in diagnostic techniques, their incidence is being reported in the past few years. Various diagnostic tests and therapeutic maneuvers have been described in the management of BPPV. The present report is a comprehensive review of the tests and maneuvers for BPPV written as a guide intended to help the clinicians in the accurate diagnosis and application of a canal-specific treatment maneuver for BPPV. A simplified algorithmic approach (“The Bangalore BPPV Algorithm”) for the management of BPPV is described.
Keywords: Benign Positional Paroxysmal Vertigo (BPPV), Positional tests, Therapeutic maneuvers, Canalolithiasis, Cupulolithiasis
Introduction
Benign Paroxysmal Positional Vertigo (BPPV) is the most common vestibular disorder characterized by recurrent, brief episodes of positional vertigo (spinning sensation produced by the changes in the head position relative to the gravity). It accounts for approximately 20–30% of the referrals to vestibular clinics and approximately 17%-42% of patients with vertigo have BPPV [1].
BPPV is caused by the aberrant stimulation of the vestibular receptors within the semi-circular canals. Two mechanisms, canalolithiasis, in which the otoconia are freely floating within the semicircular canals and cupulolithiasis, where the migrated otoconia become fixed upon the cupula of the semicircular canal, are considered in the pathogenesis of BPPV [2].
Otoconia are calcium carbonate crystals attached to the macula. They are substances with greater specific gravity than the endolymph and are thus subject to movement with changes in the direction of the gravitational force. Once the otoconia enter the semicircular canals, they move in the endolymph when the attitude of the head is changed relative to gravity and cause endolymphatic fluid movement or pressure changes leading to displacement of the cupula. The debris can either fall towards or away from the ampulla, creating ampullopetal or ampullofugal deflection of the cupula. Stimulation of the vestibular nerves as a result of deflection of the cupula is the cause of the vertigo perceived [3].
Posterior Semicircular Canal (PSC) is the most common canal involved accounting for 80–90% cases. Lateral Semicircular Canal (LSC) is involved in 5–15% cases and Superior Semicircular Canal (SSC) in less than 2% cases [4]. Bilateral and multi-canal involvement although significantly rare, have been reported in the literature [5].
Diagnosis
The diagnosis of BPPV rests on the typical elements in the patient’s history and the characteristics of the nystagmus elicited by the diagnostic positional tests.
History
The symptoms are usually described by the patient as a rotational or spinning sensation during changes of head position relative to gravity such as rolling over in bed or tilting the head to look upward [1, 6–14]. Diagnostic suggestions in the history include [15];
Attacks of positional vertigo lasting for about a minute and provoked by turning in bed and with head movements.Prolonged mild unsteadiness or subjective imbalance in between the attacks of vertigo is less well recognized in the literature but commonly encountered in clinical practice.
Alternative complaints may be lightheadedness, dizziness, nausea, palpitations or the feeling of being “off balance”.
Attacks lasting for a longer time (more than a few minutes) are considered atypical and warrant consideration of alternate diagnosis.
An elderly patient with vague complaints of imbalance and dizziness can also have BPPV and therefore deserves positional testing.
Any preferred sleep position of the patient should be asked for, as BPPV sometimes may be on the side which the patient prefers to sleep [16].
Clinical Examination
A complete neuro-otological examination is necessary, considering the possibility of occurrence of more than one vestibular disorder in one patient [17, 18]. While the diagnostic positional tests are described in detail, the other tests are considered out of scope of the current article and hence mentioned under the following five blocks [3].
Oto-neurological Examination: General Examination of the Patient, Clinical and Audiological Examination of the Ear and Examination of Cranial Nerves
Tests for Vestibulo-Ocular-Reflex (VOR): Head Impulse, Nystagmus in primary and eccentric gaze, Test of Skew (HINTS), examination of eye movements (saccades, smooth pursuit and optokinetic), VOR suppression test, and Dynamic Visual Acuity (DVA) (Oscillopsia) test.
Tests for Vestibulo-Spinal Reflex (VSR): Tandem gait, Romberg’s test, Unterberger’s test.
Tests for cerebellar dysfunction.
Diagnostic positional tests.
Diagnostic Positional Tests
Diagnostic positional tests work by moving the head in planes parallel to the individual semicircular canals which result in provocation of symptoms of vertigo and production of a characteristic nystagmus. The features of the nystagmus allow the clinician to identify which semicircular canal is involved.
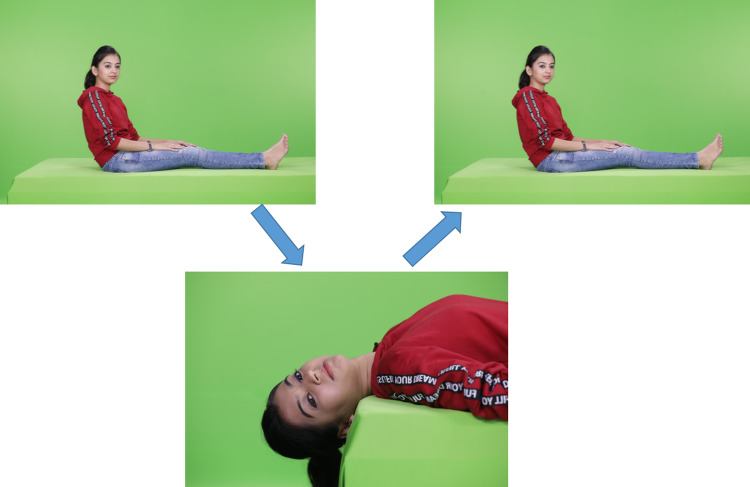
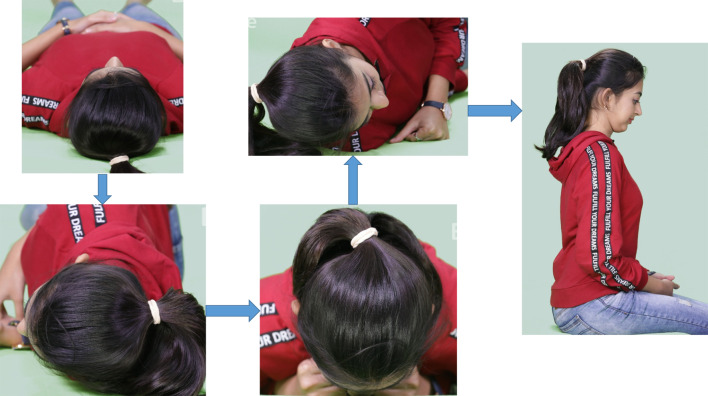
Dix-Hallpike Test (Fig. 1)
Fig. 1.
Dix-Hallpike Test demonstrated for the right side
This is a test performed by the clinician where the patient is moved through a set of specified head positions to elicit the nystagmus that is characteristic of PSC-BPPV (up-beating, torsional nystagmus with upper poles of both the eyes (iris) beating towards the affected side). The test involves the patient sitting on a bed with legs outstretched. The examiner stands beside the patient.
Step 1: The patient’s head is turned 45° towards one side (in the yaw plane).
Step 2: The patient is made to lie down rapidly, with the examiner holding the head (still turned at an angle of 45°) in such a way that it is extended by about 20° beyond the edge of the bed. In this position, the characteristics of the nystagmus are noted (Tables 1, 2). This is performed initially on the right side and if the result is negative, the test is repeated on the left side. This completes the Dix-Hallpike test.
Table 1.
Diagnostic tests for BPPV
| Canal | Optimal test |
|---|---|
| Posterior semicircular canal | Dix-Hallpike Test |
| Lateral semicircular canal | Pagnini-McClure Test |
| Superior semicircular canal | Supine Straight Head Extension Test |
Table 2.
Characteristics of the nystagmus to be noted during clinical examination
| Nystagmus | Description |
|---|---|
| Latency | Recorded in seconds. No latency indicates cupulolithiasis |
| Intensity | Measured by the peak Slow Phase Velocity (SPV) in Videonystagmography or by subjective rating on direct clinical examination |
| Direction | Up/Down-beating: With reference to patient’s forehead |
| Horizontal: With reference to patient’s right or left | |
| Torsional: With reference to the beating direction of upper pole of the iris | |
| Progression | Crescendo-decrescendo/constant intensity/decrescendo |
| Duration | Lasting for less than 1 min: Canalolithiasis |
| Lasting for greater than 1 min: Cupulolithiasis | |
| Fatigability | Fatigable: If the nystagmus dies down on maintaining the same position.Non-fatigable indicates cupulolithiasis or central causes |
| Reversal | Any reversal of nystagmus in the same position and in the reversal of provoking position is to be noted |
| Habituation | Less intense nystagmus seen on repetition of the test is described as nystagmus showing habituation. More intense nystagmus indicates facilitation of response (seen in migraine) |
It is recommended to wait for a full minute before declaring that the patient does not have nystagmus. When nystagmus is present, it is important to wait until the nystagmus completely disappears. Frenzel/Micheal goggles or Video-Nystagmo-Graphy (VNG) may be used for optimal visualization and recording of nystagmus. The test is to be avoided in certain situations like cervical spondylosis, severe kyphoscoliosis, limited cervical range of motion, spinal cord injuries, cervical radiculopathies, low back aches and morbid obesity [8, 9, 19]. A side-lying test can be performed as an alternative in these conditions. In this, first the patient’s head is turned 45º away from the side to be tested. Then the patient is briskly laid on the side being tested, during which the nystagmus is recorded. Next, the patient is made to sit slowly with the head in the same position [12].
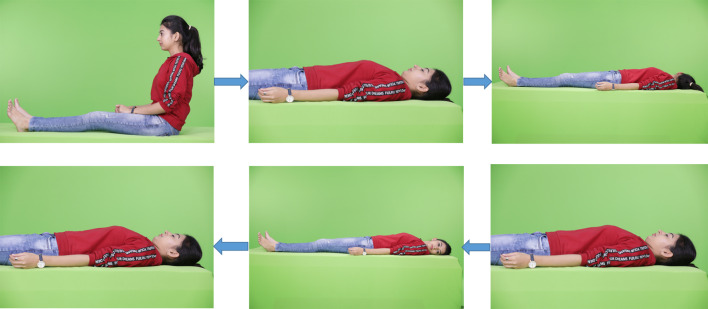
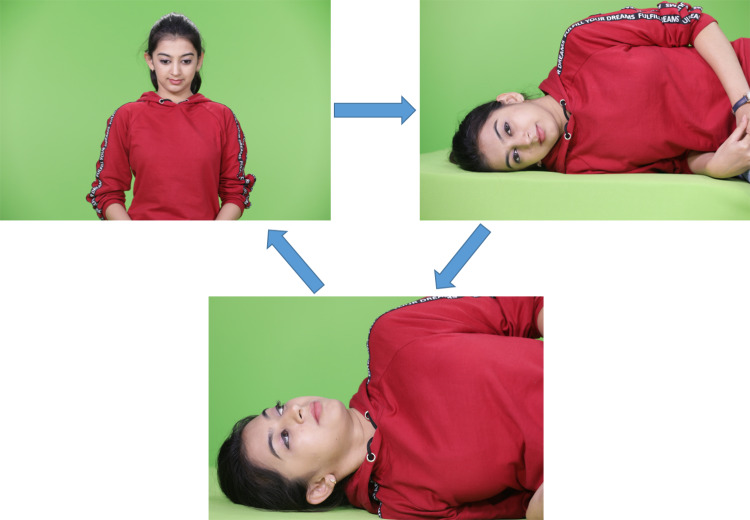
Pagnini-McClure Test (Barany test) (Fig. 2)
Fig. 2.
Pagnini-McClure Test
LSC-BPPV was first described by McClure in 1985 [19, 20]. It is the second most common type of BPPV. It tends to resolve more quickly and often spontaneously when compared to PSC-BPPV and may also occur following successful repositioning of PSC-BPPV, when the mobile otoconia that have now reached the utricular sac find their way to the LSC causing canal conversion (although this appears alarming at first, the conversion is easy to treat with maneuvers meant for LSC-BPPV) [8, 21]. The characteristic nystagmus in LSC-BPPV is provoked by supine bilateral head turns (in the yaw plane) (though inappropriately referred to as Supine Roll Test) [19]. Two nystagmus findings reflect two distinct types of LSC-BBPV. Geotropic and Apogeotropic LSC-BPPV. In geotropic form, an intense horizontal nystagmus (beating towards the undermost ear) is produced when the patient is turned towards the affected side. As it beats towards the earth, it is called as geotropic form of LSC-BPPV. When the patient is turned towards the healthy side, horizontal nystagmus is again produced beating towards the undermost ear (again geotropic but the direction of nystagmus has now changed). The side with the strongest nystagmus (more in severity) is the affected side. Apogeotropic variant of LSC-BPPV reported later by Pagnini et al.is characterized by a shorter latency, prolonged duration horizontal nystagmus, but the direction beats away from the undermost ear [20]. Geotropic LSC-BPPV is thought to be caused by otoconial debris moving under the influence of gravity (canalolithiasis) within the long arm of the LSC, stimulating utriculopetal endolymph flow in supine position with the affected ear down. Apogeotropic LSC-BPPV is caused either by the adherence of otoconia to the cupula of the lateral canal (cupulolithiasis) or by the presence of otoconia close to the ampulla [22]. The debris moving in the canal but closer to the ampulla can show mixed characteristics appearing as apogeotropic on Pagnini-McClure test and geotropic (nystagmus beats towards the affected ear) on bowing the head forward in seating position. Spontaneous conversions between geotropic and apogeotropic varieties are common and should not cause alarm.
The Pagnini-McClure test starts with the patient lying down in supine position. The examiner stands at the head end of the table and turns the patient’s head in yaw plane 90º to each side. Examiner then looks for the nystagmus on each side which can be geotropic or apogeotropic. The side of the BPPV is determined by the strength of the nystagmus. In geotropic form, the side with the strongest nystagmus is the affected ear whereas in apogeotropic form, the side opposite the strongest nystagmus is the affected ear.
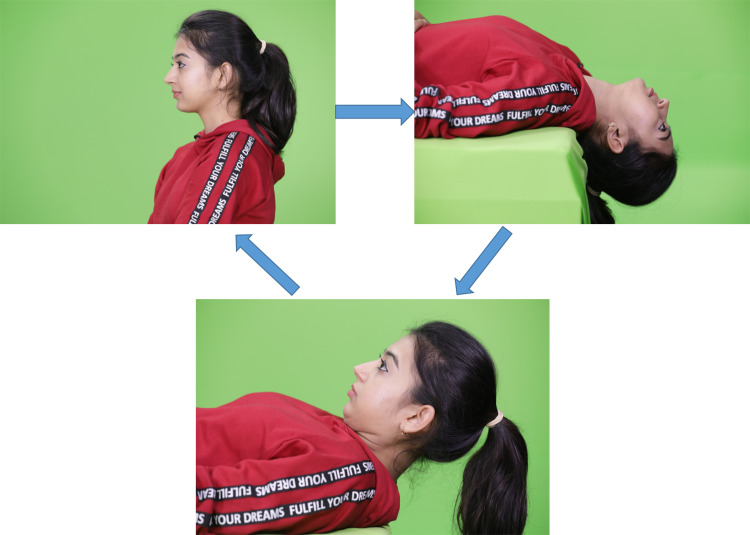
Supine Straight Head Extension Test (Fig. 3)
Fig. 3.
Supine Straight Head Extension Test
Honrubia et al.first described the possibility of SSC-BPPV in patients with down-beating nystagmus during the supine straight head extension test [23]. Bertholon et al.observed that most of the patients with positional down-beating nystagmus had no radiological pathology and hence they were assumed to be due to SSC-BPPV [24]. The test involves extension of the neck of the patient to at least 30º (or to the extent that the patient’s neck safely allows, as previously determined in the sitting position by the patient’s active head extension range) beyond the table in supine straight position while the examiner observes for the nystagmus standing at the head end of the table. Appearance of a down-beating, torsional or often vertical nystagmus is indicative of SSC-BPPV. Side of the BPPV is decided based on the direction of the down-beating nystagmus. If the upper pole of the eyes (iris) beat towards the right, it is considered as right SSC-BPPV. As the occurrence of SSC-BPPV is rare, its division into canalolithiasis and cupulolithiasis forms has currently not been described in the literature and is hence not discussed here.
To summarize, the above three tests, Dix-Hallpike, Pagnini-McClure and Supine Straight Head Extension Tests are helpful in diagnosis of the canal, the side and the type of otolith dysfunction involved (canalolithiasis/ cupulolithiasis). However, it is notable that the type of test does not decide the canal involved, but the characteristic nystagmus does.
Therapeutic Maneuvers
The development of therapeutic treatment maneuvers for BPPV is probably the most important breakthrough in the field of neurotology and arguably in the entire field of medicine. The aim of physical therapy is to eliminate the episodes of positional vertigo by dislodging the otoconial debris from the semicircular canals and placing them back into the utricle. Since the development of the classic Canalolith Repositioning Maneuver (CRM), numerous therapeutic procedures have been described by various authors. The present report is a review of the commonly performed treatment maneuvers for BPPV written as a ready comprehensive guide intended to assist the clinicians in the management of BPPV.
Cawthrone, in 1944, first introduced head and body exercises as a treatment for vertigo, rationale of which was based on central nervous system compensation for peripheral labyrinthine dysfunction [25]. Although this cannot address BPPV, it is likely to have sown the seed of thinking towards physical maneuvers as an approach to managing vertigo. Brandt and Daroff in 1980 provided a mechanical means to promote loosening and dispersal of otolith debris from the cupula [26]. While these exercises were based on habituation and adaptation, the maneuvers discussed below work on “liberating” the otoconia from the cupular attachment or move the free-floating otoconia out of the involved canal, back into the utricular sac.
Epley’s Maneuver (PSC-Canalolithiasis) (Fig. 4)
Fig. 4.
Epley's Maneuver for Right Posterior Semicircular Canal-Canalolithiasis
Designed and instituted in 1979 by Epley, this maneuver has been the most widely accepted treatment of choice for PSC-Canalolithiasis [27, 28].
Step 1: The patient is placed in the upright position with the head turned 45° (in the yaw plane) towards the affected ear (the ear that was positive on the Dix-Hallpike testing). The patient is rapidly laid back to the supine head-hanging 20° position (with the head turned 45º) which is maintained for one minute or until the nystagmus stops.
Step 2: The head is turned 90° towards the other (unaffected) side and held for about one minute or until the nystagmus stops, whichever is longer.
Step 3: The head is turned a further 90° which necessitates the patient’s body to turn from the supine position to the lateral decubitus position making the patient’s head nearly in the facedown position (“shoulder pointing to the roof, eyes looking at the floor”). This is also held for one minute or until the vertigo stops, whichever is longer.
Step 4: The patient is brought into the upright sitting position with “chin to chest”. Some clinicians also recommend a gentle jump from the examination couch to the floor that may push the crystals finally into the utricle. (“Leap of faith” jump).
A modification of Epley’s maneuver was tested by J C Li in 60 patients. It involves simultaneous application of a mastoid oscillator during the various positions of the Epley’s maneuver. A hand-held, low intensity vibrator is used as mastoid bone oscillator. Mastoid vibration helps in movement of the otoconia within the semicircular canal or detachment of otoconia adhered to the canal wall and improves the success rate of Epley’s maneuver to 97% [29]. Mastoid vibration can also be useful at the time of Dix-Hallpike test, when the patient’s history suggests BPPV on a particular side but there is no objective nystagmus on examination. Use of a mastoid oscillator in such a case may help in conversion of the subjective vertigo to objective nystagmus, which is beneficial for the accurate diagnosis of BPPV.
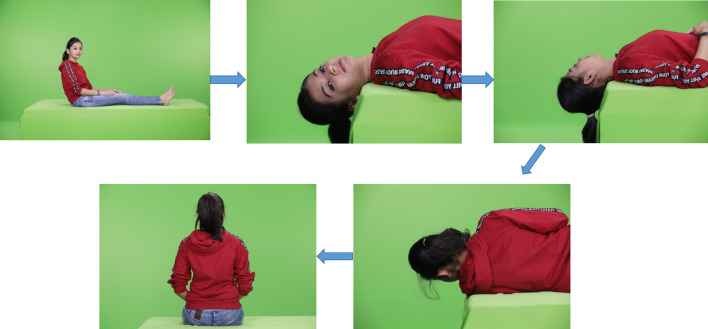
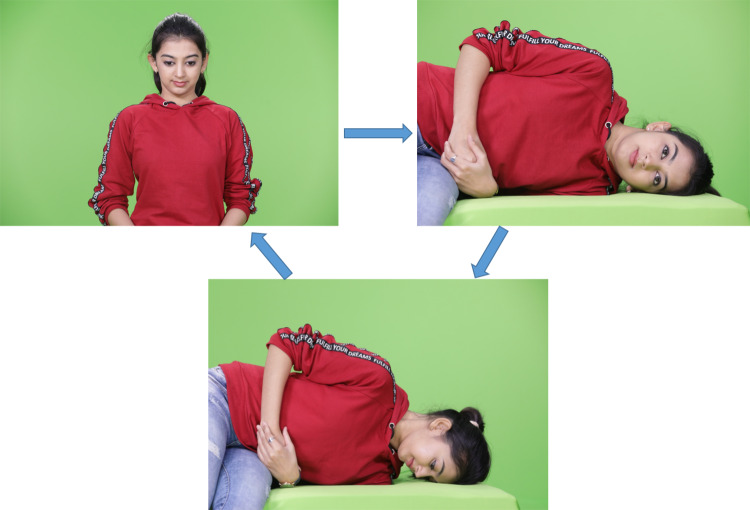
Semont’s Maneuver (PSC-Cupulolithiasis and Canalolithiasis) (Fig. 5)
Fig. 5.
Semont's Liberatory Maneuver for Right Posterior Semicircular Canal-Canalolithiasis/Cupululithiasis
The maneuver (also called liberatory maneuver) utilizes the inertial and gravity forces to liberate the otoconia from the cupula and place them back into the utricular sac [30]. It is the recommended maneuver for PSC-Cupulolithiasis, but can also be used for canalolithiasis.
Step 1: The patient sits on a table with the head turned 45º away from the affected side (in the yaw plane).
Step 2: The patient is then quickly put into the side-lying position, towards the affected side, with the head turned up (nose up).
Step 3: The patient is quickly moved through a rapid 180º arc to the opposite side-lying position with the head facing down, during which the head remains in the same position (nose dive).
Step 4: The patient is then brought back up to the sitting position slowly. Each position is maintained for about 30 s or until the nystagmus stops, whichever is longer.
Both Semont’s and Epley’s maneuvers are equally effective in the treatment of PSC-Canalolithiasis [31, 32].
Lempert’s Barbeque-Roll Maneuver (Geotropic LSC-BPPV) (Fig. 6)
Fig. 6.
Lempert's Barbeque-Roll Maneuver for Geotropic Right Lateral Semicirucular Canal BPPV
The maneuver is employed for geotropic form of LSC-BPPV and is performed after the diagnosis of LSC-Canalolithiasis has been made by Pagnini-McClure test. First described in 1996 by Lempert, the maneuver starts with the patient in supine position. Then, the patient rolls his/her head (or full body) to the unaffected side. Rolling is continued in the same direction until his/her head is completely prone. The maneuver can either be ended here (270° roll) or completed until the final roll (full 360°) and then the patient sits [33]. Some authors describe a staggered barbeque roll maneuver where the head is first turned 90º for 30 s followed by the body at every step.
Each position is held for 30 s or until the nystagmus stops, whichever is longer.
Gufoni Maneuver (Geotropic LSC-BPPV) (Fig. 7)
Fig. 7.
Gufoni Maneuver for Geotropic Right Lateral Semiciruclar Canal BPPV
The maneuver was first developed by Gufoni in 1998, the article published in English by Appiani et al.in 2001 [34]. Either Gufoni or Lempert’s maneuver can be used for the treatment of geotropic LSC-BPPV.
Step 1: The patient is taken from the sitting position to the straight side-lying position on the unaffected side for about 30 s.
Step 2: Then the patient’s head is quickly turned 45°-60° towards the ground and held in this position for about 1 min.
Step 3: The patient then sits up with the head held toward the shoulder on the unaffected side until the body is fully upright and then the head is straightened.
Response rate with the Lempert’s maneuver has been reported to be between 50 and 100%. Casani et al.reported an efficacy of 93% with Gufoni maneuver, while a study by Kim et al. showed 69% results with Gufoni maneuver and 61% results with Lempert’s Barbeque-roll maneuver [35, 36].
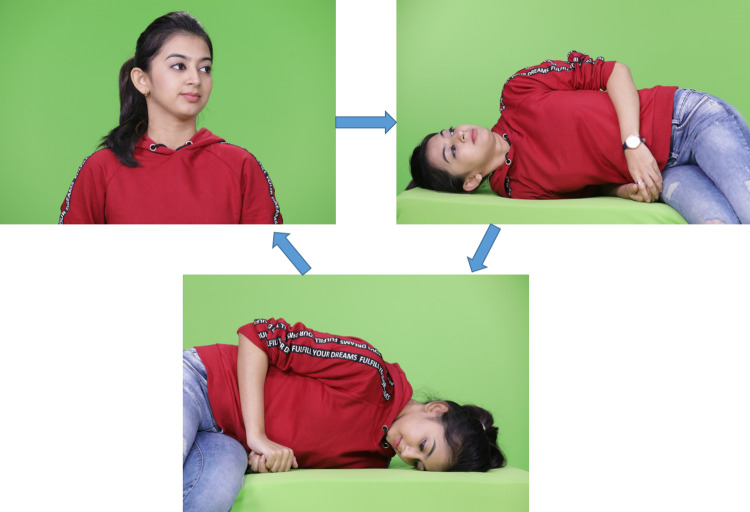
Modified Gufoni or Appiani Maneuver (Apogeotropic LSC-BPPV) (Fig. 8)
Fig. 8.
Appiani Maneuver for Apogeotropic Right Lateral Semicircular Canal BPPV, to convert the apogeotropic form to geotropic form
The maneuver developed by Gufoni for apogeotropic LSC-BPPV was clinically tested by Appiani et al.[37].
Step 1: The patient is taken from the sitting position to the straight side-lying position on the affected side for about 30 s.
Step 2: The head is turned, nose up, 45°-60° and held in that position for about a minute, which would free the debris from the canal side of the cupula (or from being lodged in the anterior arm of the LSC) [20].
Appiani maneuver is used to convert the apogeotropic form of LSC-BPPV into geotropic form, which is subsequently treated with Gufoni maneuver after a waiting period of 30 min [38]. Other tests and maneuvers for LSC-BPPV reported in the literature are mentioned in the Table 3 [39–43].
Table 3.
Other tests and maneuvers for Lateral Semicircular Canal BPPV (LSC-BPPV)
| Other Tests and maneuvers for Lateral Semicircular Canal BPPV |
|---|
| Lying down Test: Horizontal nystagmus seen when the patient is moved to supine straight position facing up (beats away from the affected ear in geotropic and towards the affected ear in apogeotropic LSC-BPPV) |
| Bow and lean Test: On bending forwards in sitting position, the nystagmus beats towards the affected ear in geotropic LSC-BPPV and away from the affected ear in apogeotropic LSC-BPPV |
| Nuti’s Maneuver: Repeated lateral rotation of the head in supine position to move the otoliths from anterior arm of the canal to the posterior arm |
| Vannucchi-Asperella Maneuver: Prolonged forced position maneuver where the patient lies on the affected side for approximately 12 h |
| Zuma’s Maneuver: First, the patient is in the sitting position and then is laid down on the affected side and held in this position for 3 min. Then, the head is rotated 90° toward the ceiling and held in this position for another 3 min. Then, the head is turned 90° toward the unaffected side and held in this position for another 3 min. Finally, the head is tilted slightly forward and then the patient is brought to the sitting position |
Yacovino Maneuver (SSC-BPPV) (Fig. 9)
Fig. 9.
Yacovino Manuver for the treatment of Superior Semicircular Canal BPPV
Considering the rarity of its occurrence, the diagnosis and treatment of SSC-BPPV is challenging. Diagnosis is made by finding of a down-beating nystagmus with a vertical or ideally with a torsional component in a supine straight head extension test. Due to the co-planar orientation of the left posterior canal with the right superior canal, a left Dix-Hallpike test can provoke a right SSC-BPPV. However, a left–right lateralisation is less specific in SSC-BPPV as in the other canal types [24, 44]. Yacovino maneuver can used as an effective maneuver for treatment of SSC-BPPV of either side, the mean success rate of which is reported to be 78.8% [45].
Step 1: Yacovino maneuver is the continuation of straight head extension test where the head is brought down at least 30º below the horizontal triggering a down-beating nystagmus.
Step 2: Once the nystagmus ceases, the patient’s head is quickly moved forward “chin to chest” with vertex near the vertical axis.
Step 3: After another 30 s, head and body are brought into the sitting position [46]. In contrast to other maneuvers for SSC-BPPV, Yacovino maneuver is side-independent and does not require identification of the affected ear.
Few other studies that have demonstrated results of maneuvers for SSC-BPPV are mentioned in the Table 4 [23, 47–49].
Table 4 .
Other maneuvers for Superior Semicircular Canal BPPV (SSC-BPPV)
| Other maneuvers for Superior Semicircular Canal BPPV | |
|---|---|
| Honrubia’s Maneuver | Reverse Epley’s Maneuver |
| Kim’s Maneuver | The head is turned 45º away from the affected ear and then the patient is brought to supine position and lowered to 30º below the horizontal. Next, the head is elevated while lying in a supine position and then returned to a sitting position with the chin tilted downwards. Efficacy of the maneuver was found to be 96.7% |
| Rahko’s Maneuver | The patient lies on the healthy side. The head is first tilted downwards 45º, then moved to 45º up in the supine position, thus accomplishing a 180º flip. Each position is maintained for 30 s and finally the patient sits up |
| Crevit’s Maneuver | Forced prolonged position maneuver: Requires admission of the patient in the hospital. The patient is rapidly moved from sitting to supine position with head extended as far as possible so that the vertex is 60º below the horizontal. Head is supported in this position for 30 min. Then, the head is moved quickly forwards with vertex near the vertical. This is the forced position in which patient is kept for 24 h |
Home Exercises
Home treatments for BPPV are considered in the following conditions [14, 50, 51]:
As an additional vestibular rehabilitation therapy after treatment with repositioning maneuvers.
BPPV resistant to repositioning maneuvers.
For residual complaints of generalized dizziness after repositioning maneuvers.
For those who refuse repositioning maneuvers and who are inaccessible for a complete treatment.
When the side of the BPPV is unclear.
The home maneuvers that can be performed are 1. Epley’s Maneuver 2. Semont’s Maneuver and 3. Brandt-Daroff Exercises. Since the maneuvers are safe and economical, their repeated application in the consequent sessions is recommended for patients who are not symptom free after the first treatment. Modified Epley’s maneuver and modified Semont’s maneuver as described by Radke et al.can also be performed, efficacy of which ranges from 60%-90% [52]. The Brandt and Daroff exercises involve a sequence of rapid lateral head/trunk tilts repeated serially to promote loosening and dispersion of the debris towards the utricle. In this, the patient starts in a sitting position moving quickly to the right side-lying position with head rotated 45° facing upward (nose up). This position is maintained until the vertigo stops and then the patient sits for about 30 s. Then the patient moves rapidly to a left side-lying position with the head rotated 45° facing upward (nose up) [26]. The exercises are repeated in three sessions, three times a day for two weeks. Each session involves five repetitions of the exercise. With the advent of canal-specific maneuvers for BPPV, the use of Brandt-Daroff exercises is limited.
Single applications of the Epley’s or the Semont’s maneuver relieves 80–90% patients, so some patients require repetition of the maneuvers until the positional vertigo resolves [53–55]. The repetition of the maneuvers can either be done by the therapist at the clinic or be taught to the patient to perform at home with the help of a care-giver. The rate of successful treatment of BPPV reaches to 90%-98% after the performance of subsequent repositioning maneuvers [56]. Therefore, for persistent BPPV, repeat repositioning maneuvers can be performed as a preferred treatment and for treatment failures refractory to multiple maneuvers, surgical plugging of the posterior semicircular canal can be considered [19].
Summary and Conclusions
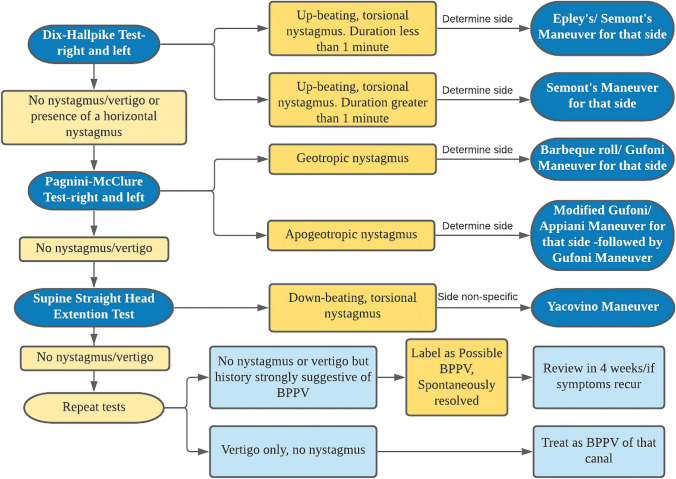
A systematic step-by-step approach to the diagnosis and treatment is essential for the optimum management of BPPV. The diagnosis of BPPV is based on the history and the characteristic nystagmus seen in the positional test. Canal specific treatment with a repositioning maneuver is to be performed (Table 5). A practical algorithmic approach named as “The Bangalore BPPV Algorithm”, being used at our center is described (Fig. 10). Following are the key points to be necessarily considered during the management of BPPV.
Table 5 .
Diagnostic tests, characteristics of the nystagmus and therapeutic maneuvers in the management of BPPV (Described for the right side. Opposite is to be performed for left side BPPV)
| Type of pathology | Diagnostic test | Nystagmus | Therapeutic maneuver |
|---|---|---|---|
| Canalolithiasis of right posterior semicircular canal | Dix- Hallpike Test-right side | Up-beating, right torsional(upper pole of the iris beating to the right) nystagmus lasting for less than 1 min with a latency of onset | Right Epley’s Maneuver/ Right Semont’s Maneuver |
| Cupulolithiasis of right posterior semicircular canal | Dix-Hallpike Test-right side | Up-beating, right torsional nystagmus lasting for more than 1 min | Right Semont’s Maneuver |
| Canalolithiasis of right lateral semicircular canal | Pagnini-McClure Test | Horizontal geotropic nystagmus stronger with right ear down | Lempert’s Barbeque- Roll Maneuver/Gufoni Maneuver |
| Cupulolithiasis of right lateral semicircular canal | Pagnini-McClure Test | Horizontal apogeotropic nystagmus stronger with left ear down without latency | Modified Gufoni/ Appiani Maneuver. Followed by Gufoni Maneuver (after a 30 min waiting period) |
| Right superior semicircular canal BPPV | Supine Straight Head Extension Test/Left Dix-Hallpike Test | Down-beating, torsional or vertical nystagmus | Yacovino Deep Head Hanging Maneuver |
Fig. 10.
"The Bangalore BPPV Algorithm"
Every dizzy patient needs to be tested for the possibility of BPPV.
The canal affected by BPPV is based on the direction of the nystagmus observed but not the positional test employed. For example, on performing Dix-Hallpike test, if the patient shows horizontal nystagmus, it is considered as LSC-BPPV but not PSC-BPPV.
Reversal of the provoking position can cause reversal of the direction of nystagmus. Intense, positionally evoked nystagmus can show reversal of direction even when same position is maintained.
Horizontal nystagmus is described as the direction of the fast phase with respect to the patient’s right and left. Torsional nystagmus is described as the beating direction of the upper pole of the iris with respect to patient’s right and left, and vertical nystagmus is described as the direction with respect to patient’s forehead. Up-beating nystagmus is towards the forehead and down-beating away from the forehead (but not with respect to the earth and sky).
Following types of nystagmus are described in the provoking test for each type of canal involvement. A. Horizontal nystagmus for lateral canals. B. Torsional up-beating nystagmus for posterior canals. C. Torsional down-beating nystagmus for superior canals.
Intractable BPPV unresponsive to repeated repositioning maneuvers can be managed by surgical correction with posterior semicircular canal occlusion or singular nerve resection [57, 58].
Accurate diagnosis of the involved canal and application of an appropriate therapeutic maneuver is essential in the management of BPPV. The treatment maneuvers help in reducing adverse events associated with undiagnosed BPPV, minimize the costs and maximize the quality-of-life of the individuals with BPPV.
Funding
The authors have no funding or financial relationships to disclose.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Consent for Publication
Informed consent was taken from the volunteer who participated in the demonstration of the maneuvers, for the publication of the article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J NeurolNeurosurg Psychiatry. 2006;78:710–715. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuknecht HF. Cupulolithiasis. Arch Otolaryngol-Head Neck Surg. 1969;90:765–778. doi: 10.1001/archotol.1969.00770030767020. [DOI] [PubMed] [Google Scholar]
- 3.Kao WT, Parnes LS, Chole RA. Otoconia and otolithic membrane fragments within the posterior semicircular canal in benign paroxysmal positional vertigo. Laryngoscope. 2017;127(3):709–714. doi: 10.1002/lary.26115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169(7):681–693. [PMC free article] [PubMed] [Google Scholar]
- 5.Shim DB, Song CE, Jung EJ, Ko KM, Park JW, Song MH. Benign paroxysmal positional vertigo with simultaneous involvement of multiple semicircular canals. Korean J Audiol. 2014;18:126. doi: 10.7874/kja.2014.18.3.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo. Otolaryngol Head Neck Surg. 2008;139(5_suppl):47–81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Furman JM, Cass SP. Benign paroxysmal positional vertigo. N Engl J Med. 1999;341(21):1590–1596. doi: 10.1056/NEJM199911183412107. [DOI] [PubMed] [Google Scholar]
- 8.Whitney SL, Marchetti GF, Morris LO. Usefulness of the dizziness handicap inventory in the screening for benign paroxysmal positional vertigo. Otology & Neurotology. 2005;26(5):1027–1033. doi: 10.1097/01.mao.0000185066.04834.4e. [DOI] [PubMed] [Google Scholar]
- 9.Dix MR, Hallpike CS. LXXVIII The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann OtolRhinolLaryngol. 1952;61(4):987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- 10.Herdman SJ. Advances in the treatment of vestibular disorders. PhysTher. 1997;77(6):602–618. doi: 10.1093/ptj/77.6.602. [DOI] [PubMed] [Google Scholar]
- 11.Macias JD, Lambert KM, Massingale S, Ellensohn A, Ann FJ. Variables affecting treatment in benign paroxysmal positional vertigo. The Laryngoscope. 2000;110(11):1921–1924. doi: 10.1097/00005537-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 12.Cohen HS. Side-lying as an alternative to the dix-hallpike test of the posterior canal. Otology & Neurotology. 2004;25(2):130–134. doi: 10.1097/00129492-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Haynes DS, Resser JR, Labadie RF, Girasole CR, Kovach BT, Scheker LE, et al. Treatment of benign positional vertigo using the semontmaneuver: efficacy in patients presenting without nystagmus. The Laryngoscope. 2002;112(5):796–801. doi: 10.1097/00005537-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Blatt P, Georgakakis G, Herdman S, Clendaniel R, Tusa R. The effect of the canalith repositioning maneuver on resolving postural instability in patients with benign paroxysmal positional vertigo. Am J Otolaryngol. 2000;21(3):356–363. doi: 10.1016/s0196-0709(00)80045-9. [DOI] [PubMed] [Google Scholar]
- 15.Von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, et al. Benign paroxysmal positional vertigo: diagnostic criteria: consensus document of the committee for the classification of vestibular disorders of the bárány society. VES. 2015;25(3,4):105–117. doi: 10.3233/VES-150553. [DOI] [PubMed] [Google Scholar]
- 16.Shim DB, Kim JH, Park KC, Song MH, Park HJ. Correlation between the head-lying side during sleep and the affected side by benign paroxysmal positional vertigo involving the posterior or horizontal semicircular canal. Laryngoscope. 2012;122(4):873–876. doi: 10.1002/lary.23180. [DOI] [PubMed] [Google Scholar]
- 17.Karlberg M, Hall K, Nicole Q. What inner ear diseases cause benign paroxysmal positional vertigo? ActaOtolaryngol. 2000;120(3):380–385. doi: 10.1080/000164800750000603. [DOI] [PubMed] [Google Scholar]
- 18.Lee N-H, Ban J-H, Lee K-C, Kim SM. Benign paroxysmal positional vertigo secondary to inner ear disease. Otolaryngol Head Neck Surg. 2010;143(3):413–417. doi: 10.1016/j.otohns.2010.06.905. [DOI] [PubMed] [Google Scholar]
- 19.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical practice guideline: benign paroxysmal positional vertigo (update) Otolaryngol Head Neck Surg. 2017;156(3_suppl):47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- 20.McClure JA. Horizontal canal BPV. J Otolaryngol. 1985;14(1):30–35. [PubMed] [Google Scholar]
- 21.Imai T, Ito M, Takeda N, Uno A, Matsunaga T, Sekine K, et al. Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology. 2005;64(5):920–921. doi: 10.1212/01.WNL.0000152890.00170.DA. [DOI] [PubMed] [Google Scholar]
- 22.Fife TD. Recognition and management of horizontal canal benign positional vertigo. Am J Otol. 1998;19(3):345–351. [PubMed] [Google Scholar]
- 23.Honrubia V, Baloh RW, Harris MR, Jacobson KM. Paroxysmal positional vertigo syndrome. Am J Otol. 1999;20(4):465–470. [PubMed] [Google Scholar]
- 24.Bertholon P. Positional down beating nystagmus in 50 patients: cerebellar disorders and possible anterior semicircularcanalithiasis. J NeurolNeurosurg Psychiatry. 2002;72(3):366–372. doi: 10.1136/jnnp.72.3.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cawthorne T. The Physiological Basis for Head Exercises. J Chartered SocPhysiother. 1944;30:106. [Google Scholar]
- 26.Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1980;106(8):484–485. doi: 10.1001/archotol.1980.00790320036009. [DOI] [PubMed] [Google Scholar]
- 27.Epley JM. Thecanalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107(3):399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 28.Epley JM. Human Experience with canalith repositioning maneuvers. Ann N Y AcadSci. 2006;942(1):179–191. doi: 10.1111/j.1749-6632.2001.tb03744.x. [DOI] [PubMed] [Google Scholar]
- 29.Li JC. Mastoid oscillation: a critical factor for success in canalith repositioning procedure. Otolaryngol Head Neck Surg. 1995;112(6):670–675. doi: 10.1016/S0194-59989570174-5. [DOI] [PubMed] [Google Scholar]
- 30.Semont A, Freyss G, Vitte E. Curing the BPPV with a Liberatory Maneuver. In: Barany Society, Pirodda E, editors. Advances in Oto-Rhino-Laryngology [Internet]. S. Karger AG; 1988 [cited 2020 Sep 15]. p. 290–3. [DOI] [PubMed]
- 31.Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD003162.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE. Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg. 1993;119(4):450–454. doi: 10.1001/archotol.1993.01880160098015. [DOI] [PubMed] [Google Scholar]
- 33.Lempert T, Tiel-Wilck K. A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope. 1996;106(4):476–478. doi: 10.1097/00005537-199604000-00015. [DOI] [PubMed] [Google Scholar]
- 34.Appiani GC, Catania G, Gagliardi M. A Liberatory Maneuver for the Treatment of Horizontal Canal Paroxysmal Positional Vertigo. Otology and Neurotology. 2001;22(1):66–69. doi: 10.1097/00129492-200101000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Casani AP, Vannucci G, Fattori B, Berrettini S. The treatment of horizontal canal positional vertigo: our experience in 66 cases. The Laryngoscope. 2002;112(1):172–178. doi: 10.1097/00005537-200201000-00030. [DOI] [PubMed] [Google Scholar]
- 36.Kim J-S, Oh S-Y, Lee S-H, Kang J-H, Kim DU, Jeong S-H, et al. Randomized clinical trial for apogeotropic horizontal canal benign paroxysmal positional vertigo. Neurology. 2012;78(3):159–166. doi: 10.1212/WNL.0b013e31823fcd26. [DOI] [PubMed] [Google Scholar]
- 37.Appiani GC, Catania G, Gagliardi M, Cuiuli G. Repositioning Maneuver for the Treatment of the Apogeotropic Variant of Horizontal Canal Benign Paroxysmal Positional Vertigo. Otology Neurotology. 2005;26(2):257–260. doi: 10.1097/00129492-200503000-00022. [DOI] [PubMed] [Google Scholar]
- 38.Vannucchi P, Asprella GL, Gufoni M. The physical treatment of lateral semicircular canal canalolithiasis. Audiologic Med. 2005;3:52–56. [Google Scholar]
- 39.Choung YH, Shin YR, Kahng H, Park K, Choi SJ. 'Bow and lean test' to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. 2006;116(10):1776–1781. doi: 10.1097/01.mlg.0000231291.44818.be. [DOI] [PubMed] [Google Scholar]
- 40.Nuti D, Agus G, Barbieri MT, Passali D. The management of horizontal-canal paroxysmal positional vertigo. ActaOtolaryngol. 1998;118(4):455–460. doi: 10.1080/00016489850154559. [DOI] [PubMed] [Google Scholar]
- 41.Lee JB, Han DH, Choi SJ, Park K, Park HY, Sohn IK, et al. Efficacy of the “bow and lean test” for the management of horizontal canal benign paroxysmal positional vertigo. The Laryngoscope. 2010;120(11):2339–2346. doi: 10.1002/lary.21117. [DOI] [PubMed] [Google Scholar]
- 42.Asprella LG. Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. ActaOtorhinolaryngolItal. 2005;25(5):277–283. [PMC free article] [PubMed] [Google Scholar]
- 43.Zuma e Maia F. New treatment strategy for apogeotropic horizontal canal benign paroxysmal positional vertigo. Audiol Res. 2016;6(2):163. doi: 10.4081/audiores.2016.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bronstein AM. Vestibular reflexes and positional manoeuvres. J NeurolNeurosurg Psychiatry. 2003;74(3):289–293. doi: 10.1136/jnnp.74.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. J ClinNeurol. 2015;11(3):262. doi: 10.3988/jcn.2015.11.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yacovino DA, Hain TC, Gualtieri F. New therapeutic maneuver for anterior canal benign paroxysmal positional vertigo. J Neurol. 2009;256(11):1851–1855. doi: 10.1007/s00415-009-5208-1. [DOI] [PubMed] [Google Scholar]
- 47.Crevits L. Treatment of anterior canal benign paroxysmal positional vertigo by a prolonged forced position procedure. J NeurolNeurosurg Psychiatry. 2004;75(5):779–781. doi: 10.1136/jnnp.2003.025478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rahko T. The test and treatment methods of benign paroxysmal positional vertigo and an addition to the management of vertigo due to the superior vestibular canal (BPPV-SC) ClinOtolaryngol. 2002;27(5):392–395. doi: 10.1046/j.1365-2273.2002.00602.x. [DOI] [PubMed] [Google Scholar]
- 49.Kim YK, Shin JE, Chung JW. The effect of canalith repositioning for anterior semicircular canal canalithiasis. ORL J OtorhinolaryngolRelat Spec. 2005;67(1):56–60. doi: 10.1159/000084336. [DOI] [PubMed] [Google Scholar]
- 50.Han BI, Song HS, Kim JS. Vestibular rehabilitation therapy: review of indications, mechanisms, and key exercises. J ClinNeurol. 2011;7(4):184–196. doi: 10.3988/jcn.2011.7.4.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chang W-C, Yang Y-R, Hsu L-C, Chern C-M, Wang R-Y. Balance improvement in patients with benign paroxysmal positional vertigo. ClinRehabil. 2008;22(4):338–347. doi: 10.1177/0269215507082741. [DOI] [PubMed] [Google Scholar]
- 52.Radtke A, von Brevern M, Tiel-Wilck K, Mainz-Perchalla A, Neuhauser H, Lempert T. Self-treatment of benign paroxysmal positional vertigo: Semontmaneuver vs Epley procedure. Neurology. 2004;63(1):150–152. doi: 10.1212/01.wnl.0000130250.62842.c9. [DOI] [PubMed] [Google Scholar]
- 53.Lynn S, Pool A, Rose D, Brey R, Suman V. Randomized trial of the canalith repositioning procedure. Otolaryngol Head Neck Surg. 1995;113:712–720. doi: 10.1016/S0194-59989570010-2. [DOI] [PubMed] [Google Scholar]
- 54.Asawavichianginda S, Isipradit P, Snidvongs K, Supiyaphun P. Canalith repositioning for benign paroxysmal positional vertigo: a randomized, controlled trial. Ear Nose Throat J. 2000;79:732–737. [PubMed] [Google Scholar]
- 55.Froehling DA, Bowen JM, Mohr DN, et al. Thecanalith repositioning procedure for the treatment of benign paroxysmal positional vertigo: a randomized controlled trial. Mayo ClinProc. 2000;75:695–700. doi: 10.4065/75.7.695. [DOI] [PubMed] [Google Scholar]
- 56.Reinink H, Wegner I, Stegeman I, et al. Rapid systematic review of repeated application of the epleymaneuver for treating posterior BPPV. Otolaryngol Head Neck Surg. 2014;151:399–406. doi: 10.1177/0194599814536530. [DOI] [PubMed] [Google Scholar]
- 57.Parnes LS, McClure JA. Posterior semicircular canal occlusion for intractable benign paroxysmal positional vertigo. Ann OtolRhinolLaryngol. 1990;99(5):330–334. doi: 10.1177/000348949009900502. [DOI] [PubMed] [Google Scholar]
- 58.Kisilevsky V, Bailie NA, Dutt SN, Rutka JA. lessons learned from the surgical management of benign paroxysmal positional vertigo: the university health network experience with posterior semicircular canal occlusion surgery (1988–2006) J Otolaryngol Head Neck Surg. 2009;38(2):212–221. [PubMed] [Google Scholar]