Abstract
We describe a large outbreak of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) involving an acute-care hospital emergency department during December 2020 and January 2021, in which 27 healthcare personnel worked while infectious, resulting in multiple opportunities for SARS-CoV-2 transmission to patients and other healthcare personnel. We provide recommendations for improving infection prevention and control.
On December 30, 2020, as healthcare personnel (HCP) coronavirus disease 2019 (COVID-19) vaccination was being initiated in the United States, the infection prevention team of an acute-care hospital (hospital A) in Santa Clara County, California recognized a cluster of 22 emergency department (ED) HCP who worked on December 25 and then tested positive for SARS-CoV-2 after becoming symptomatic. The hospital notified Santa Clara County Public Health Department (SCCPHD) and California Department of Public Health (CDPH) on January 3, 2021. CDPH, SCCPHD, and hospital A requested assistance from the Centers for Disease Control and Prevention (CDC) to investigate potential routes of transmission, to identify infection prevention and control (IPC) gaps, and to recommend strategies to mitigate future risks.
Methods
A probable case was defined as a positive SARS-CoV-2 test by polymerase chain reaction (PCR) occurring in (1) hospital A HCP assigned to the ED (referred to as ED HCP), (2) HCP (referred to as ED-linked HCP) or patient (referred to as ED patient) who spent at least 15 minutes in the ED in the 14-day period prior to infection (symptom onset date or positive SARS-CoV-2 test specimen collection date, if asymptomatic), or (3) HCP or patient with an epidemiologic link to a confirmed case (eg, present on the same unit at the same time) provided the timing of the infection fell between and including December 11, 2020, and January 9, 2021. Notably, this date range represents a full incubation period (14 days) before and after December 25. Confirmed cases met the probable case criteria and had a SARS-CoV-2 isolate that matched the outbreak sequence; that is, they differed by ≤3 single nucleotide polymorphisms (SNPs) according to whole-genome sequencing (WGS).
We reviewed California Reportable Disease Information Exchange (CalREDIE), California Connected system (CalCONNECT), and testing records of hospital A to identify SARS-CoV-2 infections among HCP and ED patients. Prior to the identification of this cluster, hospital A had been offering voluntary weekly PCR testing to asymptomatic HCP with low uptake. Following outbreak identification, hospital A offered PCR testing every 3 days between January 1 and February 28 to all HCP who were in the ED on December 25. All hospital HCP, including ED HCP who did not work on December 25, were encouraged to undergo testing for SARS-CoV-2. All patients admitted for inpatient treatment were tested for SARS-CoV-2 on admission, and those who were in the ED between December 25 and December 30 additionally received serial testing every 3 days during their hospitalization. Patients who presented to the ED on December 25 between 9:00 a.m. and 7:00 p.m. and were not admitted were offered SARS-CoV-2 testing after identification of the outbreak. The Santa Clara County public health laboratory performed WGS.
Using staffing rosters, we determined dates when infected ED HCP had worked between December 11 and January 9 and were infectious, defined as during 2 days prior to symptom onset and within 10 days after symptom onset.
The hospital IPC team conducted a survey between January 5 and January 11 of all ED and ED-linked HCP who had worked on December 25. The survey assessed potential exposures during their December 25 shift, previous exposures during December, observations on shifts between December 18 and December 25, and COVID-19 vaccination status. A team of federal, state health department, and county health department staff including infection preventionists, an industrial hygienist, medical officers, and epidemiologists conducted 2 onsite observations of clinical and nonclinical work areas and interviewed unit managers, infection preventionist, occupational health manager, facilities manager, and the facility’s management team. We used these results to describe IPC and industrial hygiene policies and practices for COVID-19 prevention in hospital A, including entry screening, physical distancing, personal protective equipment use, case investigation, contact tracing, work restriction, airflow, and ventilation.
This activity was reviewed by the CDC and was conducted consistent with applicable federal law and CDC policy (eg, 45 CFR part 46, 21 CFR part 56; 42 USC §241(d); 5 USC §552a; 44 USC §3501 et seq).
Results
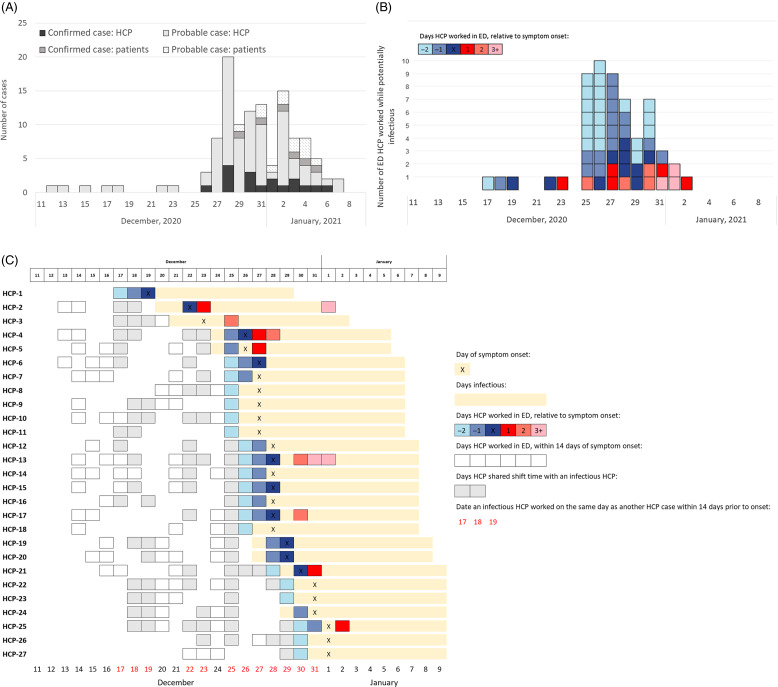
We identified 17 confirmed cases and 82 probable cases among HCP and 6 confirmed cases and 12 probable cases among patients (Fig. 1A). COVID-19 symptoms were reported by 86 (87%) of 99 HCP cases, and 1 individual who worked in the ED died due to COVID-19. Among all 311 ED HCP, 53 (17%) were cases; clinical and nonclinical HCP were similarly affected. Isolates from 19 HCP and 6 patients were sequenced, and with the exception of isolates from 2 HCP, all were ϵ (epsilon or B.1.427) variant and within 3 SNPs. This variant sequence had not been observed in an outbreak among community cases at the time of this investigation.
Fig. 1.
Distribution of SARS-CoV-2 cases in the Emergency Department (ED) of hospital A, December 11, 2020–January 9, 2021. (A) SARS-CoV-2 cases in the ED of hospital A from December 11, 2020, to January 9, 2021 (N = 99 HCP and 18 patients). (B) Distribution of ED HCP cases by date of working in the ED while infectious with SARS-CoV-2 (N = 27). (C) ED HCP cases by days worked in the ED, relative to their COVID-19 symptom-onset date (N = 27).
Between December 27 and January 9, 98% of 146 ED and ED-linked HCP who worked on December 25 were tested for SARS-CoV-2, compared to 69% of 237 ED HCP who did not work on December 25, and 44% of 2,438 other HCP. Our review of HCP location, timing, and staffing data did not reveal any single HCP, patient, or particular event that was linked to the majority of HCP and patient cases.
In total, 27 ED HCP worked while potentially infectious: 2 days before symptom onset (n = 20), 1 day before symptom onset (n = 15), on the same day as symptom onset (n = 10), 1 day after symptom onset (n = 5), 2 days after (n = 4), or 3–10 days after symptom onset (n = 3) (Fig. 1B and 1C). Also, 9 or more infectious HCP worked on each day from December 25 to December 27. We identified 12 calendar days (54 person days, defined as any day when a potentially infectious HCP worked, regardless of shift length) between December 11 and January 9 when at least 1 infectious HCP worked in the ED on the same day as a future HCP or patient who became infected within 14 days. In addition, 6 ED HCP tested positive for SARS-CoV-2 between December 4 and December 10 (not included in case definition), at least 1 of whom worked while infectious during this period.
Among 87 ED patients seen between December 25 and December 30 and admitted with a negative SARS-CoV-2 PCR test on admission, 1 (1%) had a positive SARS-CoV-2 test within 2 days, and 4 (5%) had a positive SARS-CoV-2 test within 3–14 days. Among them, 2 were admitted on December 25 and 3 were admitted between December 26 and December 30. Of 69 ED patients seen on December 25 between 9:00 a.m. and 7:00 p.m. who were not admitted and who did not have known SARS-CoV-2 infection on presentation, 13 (21%) tested positive from December 31 through January 5, 35 (49%) tested negative, and 21 (30%) were lost to follow-up. Patients seen in the ED outside this period were not followed.
We identified multiple IPC gaps in hospital A (Table 1). In total, 118 (81%) of 146 HCP who worked in the ED on December 25 responded to the survey. Overall, 72% of HCP had received a first dose of an mRNA vaccine but no HCP had been fully vaccinated. HCP reported working while symptomatic or observing others who worked while symptomatic, citing difficulties in attributing symptoms to COVID-19. HCP noted congregating in the ED break room, work rooms, and other nonclinical areas as well as removing face coverings for meals without physical distancing or barriers. HCP entry screening relied upon an automated temperature check station and a protocol for attesting no COVID-19 symptoms by “badging in” for work. Hospital A’s exposure risk assessments for HCP in early December did not identify all possible workplace exposures. Exposed HCP were permitted to continue working if they remained asymptomatic, in accordance with California executive order no. N-27-20.
Table 1.
Infection Prevention and Control (IPC) and Industrial Hygiene Practices, Observations, and Recommendations, Emergency Department (ED) of Hospital A, December 2020–January 2021
| Domain | Hospital A Policy | Practices and Observations | Recommendations |
|---|---|---|---|
| Infection prevention and control program, hospital administration, and executive leadership support | Facility is part of an integrated system with centralized resources as well as infection prevention staff on site. | 1.5 full time equivalent (FTE) infection preventionist. Resources from the facility’s parent integrated system, such as resources for case investigation, were not utilized during the surge of COVID-19 cases in December 2020, prior to identification of the outbreak. |
• Facility size, scope, services offered, populations cared for, and the type of care settings can be used to conduct a comprehensive needs assessment to determent total IPC FTE needs.
a
• Hospital should allocate sufficient human and material resources to infection prevention to ensure consistent and prompt action to remove or mitigate infection risks and stop transmission of infections. b • Hospital leadership should implement processes and sick leave policies to encourage healthcare personnel (HCP) to stay home when they develop signs or symptoms of acute infectious illness to prevent spreading their infections to patients and other HCP. b |
| Screen and triage everyone entering a healthcare facility for signs and symptoms of COVID-19 | HCP attest to having taken their temperature checked and declining that they have symptoms of COVID-19 by “badging into” the facility. Temperature check was used to screen for fever upon entry to the facility. |
HCP attestation precludes HCP being asked about specific symptoms. Some HCP worked while they had COVID-19 symptoms believing their symptoms were unrelated to COVID-19. One HCP self-reported in a survey: “I thought it was just my asthmatic symptoms.” On the survey, 2 HCP reported that security guards came into work when they were sick and were told to come to work. |
• Establish a process to ensure that everyone (patients, HCP, and visitors) entering the facility is assessed for symptoms of COVID-19 or exposure to others with suspected or confirmed SARS-CoV-2 infection, and that they are practicing source control.
c
• In a setting where HCP attestation is not preventing symptomatic staff from working, facilities could consider active individual screening of HCP on arrival to prevent HCP from working while symptomatic. d • Security personnel and other contractual staff not employed by the healthcare facility, and persons not directly involved in patient care, but who could be exposed to infectious agents that can be transmitted in the healthcare setting, are considered HCP when referring to public health guidance. c • Facilities should follow current local, state, and federal guidance on return to work. e |
| All symptomatic HCP and HCP considered to have high-risk exposures were offered testing. | During the December COVID-19 surge, it sometimes took >3 days to receive results for HCP testing due to surges in COVID-19 cases. | • When HCP are tested for SARS-CoV-2 following an exposure, test results should be available rapidly (ideally within 24 hours), and a clear plan to respond to results should be established. d | |
| Create a process to respond to SARS-CoV-2 exposures among HCP and others | HCP risk assessment tool asked whether HCP had prolonged close contact with persons with SARS-CoV-2 infection, using an exposure definition of 6 feet distance of ≥15 minutes exposure of not wearing recommended personal protective equipment. Facility has a separate case investigation tool for HCP who tested positive for SARS-CoV-2. |
Risk assessment and case investigation tools focused on community exposures. If HCP who tested positive for SARS-CoV-2 could have been exposed in the community, they were classified as a community exposure. |
• Detection of a single instance of SARS-CoV-2 in a HCP who interacts with other HCP or patients should prompt further investigation and actions to mitigate risk.
f
• Healthcare facilities should have an established process for notifying the health department about suspected or confirmed cases and plan for responding to these so investigations can be planned jointly between facility (occupational health services and IPC staff) and health department. c |
| Case investigation to be performed on every employee who tests positive for SARS-CoV-2. | Case investigation, risk assessment, and worker restriction performed by unit managers in conjunction with IPC staff. | • Contact tracing should be conducted consistent with applicable laws and regulations. c The best practice is to have a trained occupational health or IPC staff conduct interviews. | |
| During the surge, the facility operated under crisis capacity strategies to mitigate staffing shortages that allowed identified HCP with high-risk exposures to continue to work if they remained asymptomatic and wore N95 respirators during patient care. | Crisis capacity strategies were followed. | • In the event of staffing shortages, consider implementing contingency and crisis capacity strategies in coordination with public health authorities. • Implement contingency capacity strategies to mitigate staffing shortage before implementing crisis capacity strategies. g |
|
| Encourage physical distancing & implement universal source control | Hospital policy included universal indoor masking and room capacity limits based on available space, with 6-foot distancing criteria for eating indoors while unmasked. Education regarding physical distancing and source control was provided to HCP through regular leadership messages and HCP huddles. |
HCP reported observing congregation in ED break room, work rooms, and other nonclinical areas as well as removal of face coverings for meals in these locations without the use of distancing or physical barriers. | • Take steps to minimize high-risk exposures in the workplace, such as physical distancing, limits to the number of people in 1 room, and physical barriers where distancing is not feasible. Regularly assess these prevention practices for consistency and audit HCP adherence.
c
• Provide ongoing education to HCP, reinforcing the concept that exposure to SARS-CoV-2 is not limited to direct patient care. c • HCP should wear well-fitting source control at all times in the healthcare facility, including in breakrooms or other spaces where they might encounter coworkers. c |
| Respiratory protection | Extended use/reuse of N95 during each shift. New N95 every shift. Do not store disposable N95s. |
HCP practiced extended use and reuse of N95 respirators without documented shortage. Disposable N95s were stored in paper bags for reuse. | • Move to conventional strategies when shortages resolve. h |
| Consider performing targeted SARS-CoV-2 testing of patients without signs or symptoms of COVID-19 | Patients are tested for SARS-CoV-2 infection upon admission or if COVID-19 symptoms develop after admission. | No formalized retesting of asymptomatic patients even after prolonged admission. | • Consider SARS-CoV-2 testing of patients without signs or symptoms of COVID-19 to identify asymptomatic or presymptomatic SARS-CoV-2 infections.
c
• To increase detection of patients who might have been in the incubation period at the time of admission, consideration could be given to repeat testing 3–5 days after admission. f |
| Place patients in cohorts on admission based on SARS-CoV-2 test results. | Patients with unknown SARS-CoV-2 infection status and without COVID-19 symptoms were sometimes placed in a shared room in ED. | • Place patients with unknown SARS-CoV-2 infection status in single patient rooms whenever possible, given the availability of such rooms. | |
| Optimize the use of engineering controls and indoor air quality | Airborne infection isolation rooms (AIIRs) maintained at pressure differential of −0.010 inches of water relative to the corridor. | Some AIIRs in the ED (including multiple converted rooms) had positive or neutral pressure differentials to the corridor. AIIRs were maintained at pressure differential of −0.002 inches of water relative to the corridor. |
• Maintain continuous negative air pressure (2.5 Pa [0.01-inch water gauge]) in relation to the air pressure in the corridor; monitor air pressure periodically, preferably daily, with audible manometers or smoke tubes at the door (for existing AII rooms) or with a permanently installed visual monitoring mechanism. Document the results of monitoring.
i
• Educate HCP about facility-specific processes to ensuring functioning AIIRs, with competency confirmation. |
See Bartles R, Dickson A, Babade O: A systematic approach to quantifying infection prevention staffing and coverage needs. 10
See Core infection prevention and control practices for safe healthcare delivery in all settings—recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) 2017. 11
See Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. 2
See Interim guidance on testing healthcare personnel for SARS-CoV-2. 12
See Interim guidance for managing healthcare personnel with SARS-CoV-2 infection or exposure to SARS-CoV-2. 13
See Responding to SARS-CoV-2 infections in acute care facilities. 14
See Strategies to mitigate healthcare personnel staffing shortages. 15
See Strategies for optimizing the supply of N95 respirators. 16
See Guidelines for environmental infection control in health-care facilities. 17
Discussion
A large outbreak of SARS-CoV-2 occurred in the ED of an acute-care hospital. During December 2020, the daily incidence of SARS-CoV-2 infection in Santa Clara County was 68 per 100,000 population, 1 representing potential opportunity for SARS-CoV-2 introduction into a healthcare facility. WGS results were available for 25 cases; 23 of these matched within 3 SNPs, suggesting that a single introduction might have precipitated subsequent transmission events among ED patients and HCP. We were unable to fully evaluate all potential exposures and events that could have contributed to the spread of SARS-CoV-2. However, our investigation did demonstrate that within-facility transmission could have started in early December. During mid-December and early January, we identified 12 calendar days in which a total of 27 HCP worked in the ED while infectious on the same day as a future HCP or patient case who developed symptoms or tested positive for SARS-CoV-2 within 14 days after that exposure. This finding suggests many opportunities for transmission contributing to the later increase in cases. We recommended that there should be a process to ensure identification of everyone entering the facility with COVID-19 symptoms or exposure to others with suspected or confirmed SARS-CoV-2 (Table 1). Detection of a single case of SARS-CoV-2 in an HCP should prompt further actions, such as contact tracing to mitigate risk to other HCP, patients, and visitors. Engineering and administrative controls such as ensuring adequate ventilation in break rooms, limiting room capacity, and adhering to recommended work exclusions are vital to preventing higher-risk exposures between HCP. 2
This study had several limitations. The uptake of SARS-CoV-2 testing at the hospital was incomplete, and the survey was only distributed to HCP who worked on December 25. However, we incorporated data from state surveillance systems to identify all SARS-CoV-2 diagnoses among ED HCP and identified potential transmission chains beyond HCP who worked on December 25. SARS-CoV-2 isolates from before December 26 were not saved and therefore could not be sequenced for comparison with outbreak cases. Similarly, hospital A limited case finding to ED patients seen on December 25, so we were not able to identify SARS-CoV-2 infections among ED patients seen on other days or lost to follow-up. By contrast, patients who were asymptomatic were not tested for SARS-CoV-2 at the time of ED presentation, causing potential misclassification of patient cases. The scope of IPC gaps may have also been underestimated because HCP symptoms and IPC practices were self-reported after the identification of the outbreak. Despite these limitations, observed IPC lapses and the large number of HCP who worked while potentially infectious strongly suggest multiple opportunities for transmission within the ED in December.
SARS-CoV-2 transmission between HCP is a well-known driver of acute-care hospital outbreaks. 3–6 Despite HCP vaccination, breakthrough infections via symptomatic and asymptomatic vaccinated HCP can still contribute to transmission to patients and other HCP. 7 Gaps in physical distancing and source control in non–patient-care areas, delays in testing, and HCP working while infectious have previously been identified as contributing factors. 3,8 Our investigation reinforces the importance of monitoring and ensuring HCP adherence to well-fitting masks for source control and physical distancing, especially in common work and break areas. 9 This aspect may be especially challenging and important during holiday periods when hospital staff are accustomed to engaging in celebratory activities and interacting socially. Early identification of risk and work restriction can prevent further transmission: hospitals should have systems to accurately detect and respond to HCP exposures and should be prepared to notify and follow the recommendations of public health authorities. 2
During surges of SARS-CoV-2, efforts to fully implement vaccination and promote IPC practices are paramount in mitigating within-facility transmission. This outbreak occurred as HCP vaccination was being initiated in the facility. Our findings could additionally inform healthcare facilities’ response to novel emerging respiratory pathogen or an emerging variant that evades vaccine-induced immunity (eg, the SARS-CoV-2 omicron variant).
Acknowledgments
We thank hospital A for sharing data on testing, HCP survey, and staff roster; for providing feedback on the manuscript; and for their care of patients throughout the pandemic. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
References
- 1. COVID-19 cases and deaths. County of Santa Clara Emergency Operations Center website. https://covid19.sccgov.org/dashboard-cases-and-deaths. Published 2021. Accessed September 8, 2021.
- 2. Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Published 2021. Accessed February 15, 2021.
- 3. Schneider S, Piening B, Nouri-Pasovsky PA, Kruger AC, Gastmeier P, Aghdassi SJS. SARS-coronavirus-2 cases in healthcare workers may not regularly originate from patient care: lessons from a university hospital on the underestimated risk of healthcare worker to healthcare worker transmission. Antimicrob Resist Infect Control 2020;9:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borges V, Isidro J, Macedo F, et al. Nosocomial outbreak of SARS-CoV-2 in a “non–COVID-19” hospital ward: virus genome sequencing as a key tool to understand cryptic transmission. Viruses 2021;13:604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lucey M, Macori G, Mullane N, et al. Whole-genome sequencing to track severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission in nosocomial outbreaks. Clin Infect Dis 2021;72:e727–e735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paltansing S, Sikkema RS, de Man SJ, Koopmans MPG, Oude Munnink BB, de Man P. Transmission of SARS-CoV-2 among healthcare workers and patients in a teaching hospital in the Netherlands confirmed by whole-genome sequencing. J Hosp Infect 2021;110:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hetemäki I, Kääriäinen S, Alho P, et al. An outbreak caused by the SARS-CoV-2 delta variant (B.1.617.2) in a secondary care hospital in Finland, May 2021. Euro Surveill 2021;26:2100636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Klompas M, Baker MA, Rhee C, et al. A SARS-CoV-2 cluster in an acute-care hospital. Ann Intern Med 2021;174:794–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richterman A, Meyerowitz EA, Cevik M. Hospital-acquired SARS-CoV-2 infection: lessons for public health. JAMA 2020;324:2155–2156. [DOI] [PubMed] [Google Scholar]
- 10. Bartles R, Dickson A, Babade O. A systematic approach to quantifying infection prevention staffing and coverage needs. Am J Infect Control 2018;46:487–491. [DOI] [PubMed] [Google Scholar]
- 11. Core infection prevention and control practices for safe healthcare delivery in all settings—recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC). Centers for Disease Control and Prevention website. https://www.cdc.gov/hicpac/recommendations/core-practices.html. Published 2017. Accessed May 18, 2022.
- 12. Interim guidance on testing healthcare personnel for SARS-CoV-2. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-healthcare-personnel.html. Published 2021. Accessed April 15, 2021.
- 13. Interim guidance for managing healthcare personnel with SARS-CoV-2 infection or exposure to SARS-CoV-2. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html. Published 2021. Accessed June 10, 2021.
- 14. Responding to SARS-CoV-2 infections in acute care facilities. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/responding-acute-care-facilities.html. Published 2020. Accessed September 8, 2021.
- 15. Strategies to mitigate healthcare personnel staffing shortages. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html. Published 2021. Accessed September 8, 2021.
- 16. Strategies for optimizing the supply of N95 respirators. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/index.html. Published 2021. Accessed April 15, 2021.
- 17. Guidelines for environmental infection control in health-care facilities. Centers for Disease Control and Prevention website. https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf. Published 2003. Accessed May 18, 2022.