Abstract
Objective
Investigate racial and ethnic differences in infant sleep and examine associations with insurance status and parent-infant bedtime behavioral factors (PIBBF).
Methods
Participants are part of the COVID-19 Mother Baby Outcomes (COMBO) Initiative, Columbia University. Data on infant sleep (night, day and overall sleep duration, night awakenings, latency, infant's sleep as a problem) were collected at 4 months postpartum. Regressions estimated associations between race/ethnicity, insurance status, PIBBF and infants’ sleep.
Results
A total of 296 infants were eligible (34.4% non-Hispanic White [NHW], 10.1% Black/African American [B/AA], 55.4% Hispanic). B/AA and Hispanic mothers were more likely to have Medicaid, bed/room-share, and report later infant bedtime compared to NHW mothers. Infants of B/AA mothers had longer sleep latency compared to NHW. Infants of Hispanic mothers slept less at night (∼70 ± 12 minutes) and more during the day (∼41 ± 12 minutes) and Hispanic mothers were less likely to consider infants’ sleep as a problem compared to NHW (odds ratio 0.4; 95% confidence interval: 0.2-0.7). After adjustment for insurance status and PIBBF, differences by race/ethnicity for night and day sleep duration and perception of infant's sleep as a problem persisted (∼32 ± 14 minutes, 35 ± 15 minutes, and odds ratio 0.4; 95% confidence interval: 0.2-0.8 respectively). Later bedtime was associated with less sleep at night (∼21 ± 4 minutes) and overall (∼17 ± 5 minutes), and longer latency. Infants who did not fall asleep independently had longer sleep latency, and co-sleeping infants had more night awakenings.
Conclusions
Results show racial/ethnic differences in sleep in 4-month-old infants across sleep domains. The findings of our study suggest that PIBBF have an essential role in healthy infant sleep, but they may not be equitably experienced across racial/ethnic groups.
Keywords: Race, Ethnicity, Disparities, Sleep, Infancy, Bedtime behavioral factors
Introduction
Sleep health is an essential component of general health and is associated with numerous mental and physical health outcomes in the general population.1 Increasing evidence indicates that we are in the middle of a sleep crisis, with approximately 70 million American adults who suffer from chronic sleep loss and sleep disorders.2 This crisis also applies to children such that the average child sleep duration has decreased over the last century, with children sleeping ∼1 minute less per year, on average, since 1905,3 and less than half of youth meeting the guideline of 8-10 hours of sleep per night.4 , 5 Additionally, the burden of poor sleep health is not experienced equally across the US population. Adults from racial/ethnic minority backgrounds have been found to experience worse sleep health compared to White adults.6 Similar disparities have been reported among children. Recent systematic reviews have shown that non-Hispanic White (NHW) children are more likely to get the recommended amount of sleep, go to bed earlier, and have more regular sleep schedules compared to children from racially and ethnically minoritized communities.7., 8., 9.
The emergence of sleep disparities has been observed as early as during infancy.10., 11., 12. For the infant, the early postnatal period is characterized by rapid development of sleep and wake patterns, marking a major neurobiological milestone. When infants are born, their circadian rhythm is not yet established, and thus sleep-wake patterns are evenly distributed during the 24-hour period. Around 3 months of life, the circadian rhythm begins to establish, and infants gradually spend more time asleep during the night. In the first 6 months of life there is also a decline in total sleep duration (0-2 months mean sleep duration = 14.6 hours [9.3-20.0], 6 months mean sleep duration = 12.9 [9.4-15.8]).13 As sleep consolidates during the night, night awakenings are still normal in the first 6 months of life, often driven by frequent feedings.14 While in the first year of life a certain degree of heterogeneity in infant sleep duration and frequency of night awakenings is expected, sleep problems have been reported in up to 10%-15% of infants15., 16, 17. and are a source of concern for both parents and pediatricians. Such sleep problems have been reported to negatively affect physical, cognitive, and socioemotional neurodevelopment.18 , 19 In addition to the direct adverse impact of poor sleep on infants and young children, several studies have indicated that when infants and children do not sleep well, their parents report higher levels of parental stress and depression and lower levels of sense of competence and overall quality of life,20 which could further compound the negative impact on infant development.
Several factors are known to influence infants’ sleep health, including maternal mental health,21 sleep environment, bedtime routines,22 and family socioeconomic status (SES).23 , 24 Sadeh et al outlined a socio-ecological model, which views sleep as nested within a broader context (culture, environment, family), and more proximal factors, including intrinsic child characteristics and parenting factors, all shaping the parent-child interactive context, which in turn has a bidirectional relationship with infant sleep.25 Parent-child sleep interactions have been shown to significantly affect sleep: a consistent bedtime routine has been associated with longer nighttime sleep duration, shorter sleep onset latency, and less fragmented sleep.23 Other factors that have been shown to promote better sleep in early childhood include earlier bedtime26 and encouraging children to fall asleep on their own without excessive parental assistance.27 In addition, while there are well-established advantages of breastfeeding for the development of infants, breastfeeding has been found to be associated with more frequent night wakings and with lower percentage of self-soothing. Similarly, a few studies have shown that infants who co-sleep are more likely to have more spontaneous arousals, but results are not conclusive and might differ when co-sleeping is practiced sporadically or habitually.13 A few studies suggest that these factors might differ in various racial/ethnic groups, with mothers from racially and ethnically minoritized communities being more likely to describe disruptions from environmental factors, putting their infant to sleep later, feeding infants to sleep, or exposing infants to television before bedtime, likely influenced by the broader context in which they parent.28 Nonetheless, the potential contribution of these factors to racial/ethnic sleep disparities, particularly during infancy, has not been fully investigated.
In this study, we aimed to examine racial/ethnic differences in sleep duration, latency, and number of night awakenings in infants at 4 months of age, accounting for their insurance status and parent-infant bedtime behavioral factors (PIBBF) (bedtime, how does infant fall asleep, where infant sleeps). In addition, given the complex bidirectional relationship between infant sleep, parenting, and socio-cultural factors,29 , 30 we investigated associations between parent-reported infant sleep patterns and sleep problems and whether this differed by race/ethnicity. Understanding PIBBF as an inextricable contextual factor during infancy, that may underlie sleep health disparities in infancy, may support the much-needed initiatives to develop and test sleep interventions tailored to the needs of minoritized and marginalized families.
Methods
Study design
This study included a subset of data collected from a cohort of participants who participated in the COVID-19 Mother Baby Outcomes (COMBO) Initiative at Columbia University Irving Medical Center (CUIMC) and were born between February 2020 and February 2021 (www.ps.columbia.edu/COMBO). The larger COMBO study is ongoing and aims to comprehensively describe the health and wellbeing of mother-infant dyads during the COVID-19 pandemic. All procedures were approved by the CUIMC Institutional Review Board and informed consent was obtained from all participants.
Participants
All mother-infant dyads participating in the COMBO Initiative received prenatal care and delivered at the CUIMC-affiliated NewYork-Presbyterian Morgan Stanley Children's Hospital or NewYork-Presbyterian Allen Pavilion Hospital since the onset of the pandemic (first New York City laboring woman diagnosed March 13, 2020 at Morgan Stanley Children's Hospital). All dyads with a documented SARS-CoV-2 infection during pregnancy according to the electronic health record were invited to participate and were enrolled during pregnancy or in the first few months postpartum. For each exposed dyad, 1-3 unexposed dyads, defined as the absence of electronic health record documentation of maternal SARS-CoV-2 infection during pregnancy and at delivery, were matched based on infant sex, gestational age (GA) in 2-week windows, mode of delivery, and date of birth within approximately a 2-week window. Participants included in this study gave birth between February 2020 and February 2021 and premature infants were excluded.
Measures
All data were collected from chart review and surveys that were administered through the CUIMC REDCap system (version 10.6.2) and participants were offered the option to complete the surveys in English or Spanish.
Socio-demographics
Demographic data included infant sex, GA, and maternal age at delivery. As part of hospital intake records, mothers self-reported their ethnic background as “non-Hispanic,” “Hispanic,” or “decline to answer” and were also asked to specify their racial background choosing from categories recommended by the National Institutes of Health as “White,” “Black or African American,” “Asian,” “American Indian or Alaskan Native,” “Native Hawaiian or other Pacific Islander,” and/or “Other combinations not described.” For the analyses presented in this manuscript, we combined race and ethnicity variables to obtain one single race/ethnicity variable as follows: non-Hispanic White (NHW), Black or African American (B/AA) and Hispanic (H), Asian, American Indian or Alaskan Native, Native Hawaiian or other Pacific Islander, and Other combinations not described. Additionally, mothers were asked about their breastfeeding practices (mostly/exclusively breastfeeding, partially breastfeeding or utilizing mostly/exclusively formula). Insurance type was used as a proxy for income level based on the low to very low income based eligibility for Medicaid insurance vs. the middle to higher income levels associated with commercial healthcare insurance coverage.31
Sleep health
We collected maternal reported sleep health data when the child was 4 months old using the Brief Infant Sleep Questionnaire (BISQ), test-retest correlations r > 0.82.32 Sleep variables extracted from the BISQ included sleep duration (daytime: “How much time does your baby spend in sleep during the day (between 7 in the morning and 7 in the evening)?”; nighttime: “How much time does your baby spend in sleep during the night (between 7 in the evening and 7 in the morning)?”, and 24 hour, calculated as the sum of nighttime and daytime duration), number of night awakenings, sleep latency, and maternal perception of their infants having sleep problems. Perception of infant sleep as a problem was defined as a categorical variable based on the following question: “Do you consider your baby's sleep as a problem?” If the parent answered either “A very serious problem” or “A small problem” a value of 1 was assigned. Otherwise, if the parent replied “Not a problem at all” a value of 0 was assigned.
Parental bedtime practices
Data from the BISQ also included bedtime routine practices: bedtime, sleeping arrangement (Independent in a crib in a separate room, room sharing, bed sharing) and how the infant fell asleep (“While feeding/being rocked/being held/In bed near parent,” “In bed alone”).
Statistical analyses
Sleep health variables included duration (daytime, nighttime, 24 hours), latency, number of night awakenings, and maternal perception of sleep problems. Data missingness was N = 14 for nighttime sleep duration, N = 22 for daytime and total sleep duration, N = 19 for sleep latency, and N = 1 for number of night awakenings. We tested for normal distribution of continuous variables. Skewed variables (sleep latency, bedtime) were discretized and transformed from continuous to ordinal. Outliers for sleep duration were determined based on the sample distributions, utilizing the 5th and 95th percentiles as cutoffs. The cutoff values for nighttime sleep were 300-720 minutes, for daytime sleep 90-480 minutes, and for 24-hour sleep 512-1020 minutes. These values were in line with normative values for infants in the 3-6 months range published in previous research.13 Similarly, values of sleep latency higher than 120 minutes were considered outliers. Data was excluded at the level of the sleep variable and not at the participant level.
Descriptive statistics were calculated for socio-demographic and sleep health variables. Bivariate statistics were used to examine differences in socio-demographic and sleep health variables by race/ethnicity. Then, a series of multiple linear regression models were used to examine the association between sleep measures (nighttime, daytime and total sleep duration, sleep latency, number of night awakenings) and race/ethnicity, based on the conceptual framework proposed by Sadeh et al.25 In the first round of models, we controlled for intrinsic infant characteristics. Thus, based on existing literature on differences by sex for infant sleep33 and to account for the rapid sleep cycling changes that occur around 4 months of age, the models were adjusted by sex and infant's age at assessment (Model 1). Next, we additionally adjusted for insurance status, as a measure of SES, to account for the broader contextual environments in which families live and that can affect the parent-child interaction (Model 2). We then added PIBBF (sleep environment, bedtime, how the baby falls asleep, and breastfeeding) to the model (Model 3). We then ran the same 3 models to predict maternal perception of infant sleep as a problem, with an additional fourth model adjusting for infant sleep variables (Model 4). All analyses were completed using R 4.0.4.
Results
Of the 374 infants eligible for this sub-study of the COMBO Initiative, 5 were excluded because mothers did not fill out the sleep questionnaire, 44 because mothers declined to report their race/ethnicity, and 29 infants were excluded from the analyses because they identified with race/ethnic groups whose sample size was too small to be included in the analyses (“Asian” [n = 15], “American Indian or Alaskan Native” [n = 1], “Native Hawaiian or other Pacific Islander” [n = 1], “Other combinations not described” [n = 12]). Regarding the identification of outliers, 26 outliers were eliminated for 24 hour sleep duration, 18 for day sleep duration, 11 for night sleep duration, and 13 for sleep latency.
In Tables 1 and 2 , we summarize socio-demographic factors and PIBBF (Table 1) and sleep health (Table 2) of the overall sample and by race/ethnicity.
Table 1.
Socio-demographic characteristics and behavioral factors for the overall cohort and by race/ethnicity
| Overall (N = 296) | NHW (N = 102) | B/AA (N = 30) | H (N = 164) | P value | |
|---|---|---|---|---|---|
| Socio-demographic | |||||
| Gestational age (weeks) | 38.6 (1.9) | 38.5 (1.8) | 37.9 (3.1) | 38.8 (1.6) | .05 |
| Age at assessment (weeks) | 18.7 (2.4) | 18.7 (2.3) | 18.7 (3.2) | 18.8 (2.34) | .9 |
| Sex (F/M) | 137/159 | 46/56 | 13/17 | 78/86 | .9 |
| Maternal age (years) | 31.7 (5.5) | 33.4 (4.8) | 32.3 (7.2) | 30.5 (5.2) | .0001 |
| Mode of delivery | .2 | ||||
| Vaginal | 175 (59.1%) | 67 (65.7%) | 17 (56.7%) | 91 (55.5%) | |
| Cesarean | 117 (39.5%) | 33 (32.3%) | 13 (43.3%) | 71 (43.3%) | |
| Medical insurance | <.0001 | ||||
| Commercial | 151 (51.0%) | 90 (88.2%) | 15 (50.0%) | 46 (28.0%) | |
| Medicaid | 144 (48.6%) | 12 (11.8%) | 15 (50.0%) | 117 (71.3%) | |
| Parent-infant bedtime behavioral factors | |||||
| Sleep environment | <.001 | ||||
| Crib in a separate room | 46 (15.7%) | 30 (29.4%) | 4 (13.3%) | 12 (7.5%) | |
| Crib in mother's room | 226 (77.4%) | 68 (66.7%) | 21 (70%) | 137 (85.6%) | |
| Co-sleeping | 20 (6.8%) | 4 (3.9%) | 5 (16.7%) | 11 (6.8%) | |
| How does baby fall asleep | |||||
| While feeding/being rocked/being held/In bed near parent | 240 (81.1%) | 76 (74.5%) | 26 (86.7%) | 138 (84.1%) | .1 |
| In bed alone | 56 (18.9%) | 26 (25.5%) | 4 (13.3%) | 26 (15.8%) | |
| Bedtime | <.001 | ||||
| Up to 7 PM | 46 (15.9%) | 35 (34.3%) | 3 (10.0%) | 8 (5.1%) | |
| 7-8 PM | 61 (21.03%) | 28 (27.4%) | 6 (20.0%) | 27 (17.1%) | |
| 8-10 PM | 121 (41.7%) | 29 (28.4%) | 10 (33.3%) | 82 (51.9%) | |
| 10PM-12 AM | 45 (15.5%) | 8 (7.8%) | 8 (26.7%) | 29 (18.3%) | |
| After 12 AM | 17 (5.9%) | 2 (2.0%) | 3 (10%) | 12 (7.6%) | |
| Breastfeeding | .007 | ||||
| Exclusively breastmilk | 98 (33.1%) | 48 (47.1%) | 11 (36.7%) | 39 (23.8%) | |
| Breastmilk and formula | 94 (31.7%) | 32 (31.4%) | 8 (26.7%) | 54 (32.9%) | |
| Exclusively formula | 104 (35.1%) | 22 (21.6%) | 11 (36.7%) | 71 (43.3%) | |
B/AA, Black/African American; H, Hispanic; NHW, non-Hispanic White.
Table 2.
Sleep variables for the overall cohort and by race/ethnicity
| Overall | NHW (N = 102) | B/AA (N = 30) | H (N = 164) | P value | |
|---|---|---|---|---|---|
| Infant sleep | |||||
| Nighttime sleep duration | 544.9 ± 100.5 | 586.9 ± 80.6 | 547.2 ± 107.8 | 516.5 ± 101.7 | <.001 |
| Daytime sleep duration | 260.1 ± 95.4 | 237.3 ± 80.4 | 251.2 ± 96.0 | 277.2 ± 101.7 | .006 |
| Total sleep duration | 803.7 ± 124.6 | 816.9 ± 94.6 | 794.4 ± 139.4 | 796.3 ± 121.7 | .3 |
| Number of night awakenings | 1.5 ± 1.2 | 1.6 ± 1.3 | 1.5 ± 0.9 | 1.5 ± 1.1 | .4 |
| Sleep latency | .18 | ||||
| 0-15 mins | 72 (27.3%) | 30 (31.2%) | 1 (4.1%) | 41 (28.1%) | |
| 16-30 mins | 106 (40.1%) | 38 (40.4%) | 13 (54.2%) | 55 (37.7%) | |
| 31-60 mins | 51 (19.3%) | 16 (17.0%) | 5 (20.8%) | 30 (20.5%) | |
| 60-120 mins | 35 (13.2%) | 10 (10.6%) | 5 (20.8%) | 20 (13.7%) | |
| Mother considers infant's sleep as a problem (yes) | 80 (27.2%) | 39 (38.2%) | 10 (33.3%) | 31 (18.9%) | .002 |
B/AA, Black/African American; H, Hispanic; NHW, non-Hispanic White.
Of the total of 296 infants included in the analyses: 34.4% mothers identified as NHW, 10.1% as Black or African American and 55.4% as Hispanic. Fifty-one percent had commercial insurance and 48.6% had Medicaid. Average GA at birth was 38.6 weeks (SD = 1.9) with no preterm infants (GA < 37 weeks) included in the analyses, average infant age at assessment was 18.7 weeks (SD = 2.4 weeks), and 46.2% of infants were female. Mothers who self-identified as Hispanic were younger (P = .0001) and B/AA and Hispanic mothers were both significantly more likely to have Medicaid compared to NHW mothers (P < .0001).
Sixteen percent of the infants in the sample slept in their own crib in a separate room, 77.4% in their own crib but in the same room as the mothers and the rest (6.8%) co-slept. B/AA mothers were more likely to co-sleep compared to NHW, and both B/AA and Hispanic were more likely to room share rather than sleep in separate rooms from the infants (P < .0001). Nineteen percent of the infants fell asleep in bed independently, while 81.1% fell asleep being held, rocked, fed or in bed near the parent. Thirty-seven percent of infants went to bed by 8pm. Infants of B/AA and Hispanic mothers were more likley to go to bed after 10 PM (37% and 26%, respectively, compared to 10% of NHW, P < .001). Thirty-three percent of the infants were exclusively breastfed, 31.7% were both breastfed and formula fed and the remaining (35.1%) were exclusively formula fed. Hispanic mothers were more likely to use a combination of formula and breastmilk or exclusively formula, rather than exclusively breastfeeding, compared to NHW mothers (P = .007).
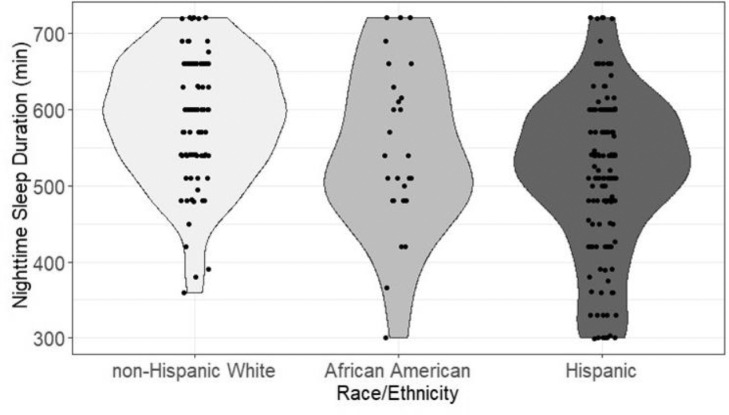
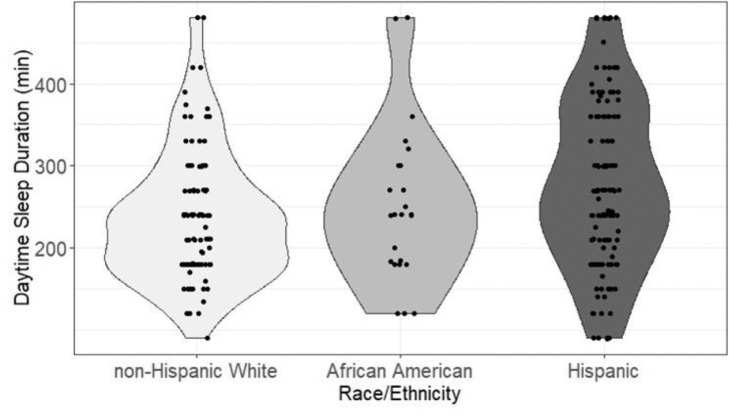
As summarized in Table 2, at 4 months night sleep duration was 544.9 minutes (SD = 100.5), day sleep duration was 260.1 minutes (SD = 95.4), and 24-hour sleep duration was 803.7 (SD = 124.6). Night sleep duration was shorter for B/AA and Hispanic compared to NHW (respectively 547.2.4 ± 107.8, 516.5 ± 101.7, 586.9 ± 80.6 minutes, P < .001). Day sleep duration was longer for Hispanic compared to NHW (respectively 277.2 ± 101.7 and 237.3 ± 73.6 minutes, P = .006). Twenty-four hour sleep duration was on average 803.7 ± 124.6 minutes and it did not differ significantly across racial/ethnic groups. The number of night awakenings was 1.5 (SD = 1.2), with no significant difference by race/ethnicity. Sleep latency was 0-15 minutes for 2% of the infants, 16-30 minutes for 40.1%, 31-60 minutes for 19.3%, and more than 60 minutes for 13.2 with no significant difference by race/ethnicity. Twenty-seven percent of the mothers considered their infant sleep as a problem, and Hispanic mothers were less likely to consider sleep as a problem compared to NHW (respectively 18.9% and 38.1%, P = .002).
Associations between infant sleep health and race/ethnicity
To examine the role of intrinsic infant characteristics, insurance status and PIBBF in the relationship between sleep health and race/ethnicity, we created 3 models. Results are discussed in the next paragraphs and presented in Table 3. Results from Model 1, adjusted for age at assessment and infant sex, showed that Hispanic mothers reported shorter night sleep duration for their infants, compared to NHW mothers (β = -70.4 ± 12.5, P < .001). Daytime infant sleep as reported by Hispanic mothers was longer than that reported by NHW mothers (β = 41.2 ± 12.5, P < .01). Figs. 1 and 2 show differences in nighttime and daytime sleep duration by race/ethnic group. B/AA mothers reported their infants had longer sleep latency compared to NHW mothers (OR 2.5 95% CI 1.1-5.6, P = .05). In addition, Hispanic mothers were less likely to consider their infant's sleep as a problem compared to NHW (OR 0.4; 95% CI 0.2-0.7, P = .001).
Fig. 1.
Violin plot illustrating the distribution of infant nighttime sleep duration by race/ethnicity.
Fig. 2.
Violin plot illustrating the distribution of infant daytime sleep duration by race/ethnicity.
Results from Model 2 showed that after additional adjustment for insurance status, Hispanic mothers still reported shorter infant night sleep duration, compared to NHW mothers (β = -54.3 ± 15.0, P < .001), longer daytime infant sleep NHW (β = 41.6 ± 14.9, P = .01), and fewer night awakenings (β = -0.3 ± 0.2, P = .05). B/AA mothers still reported their infants had longer sleep latency compared to NHW mothers (OR 2.6; 95% CI 1.2-5.9, P = .05). Hispanic mothers were still less likely to consider their infant's sleep as problem compared to NHW (OR 0.5; 95% CI 0.2-0.9, P = .05).
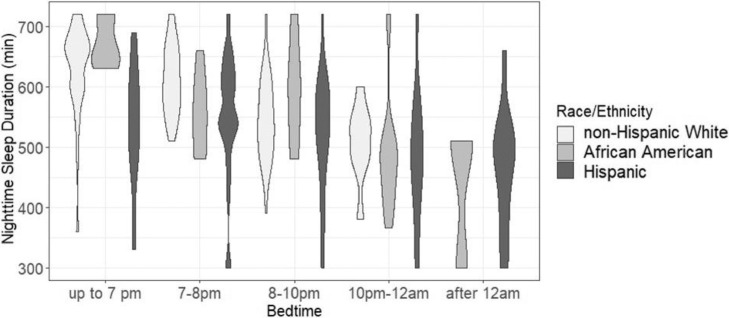
Results from Model 3, additionally adjusted for PIBBF, showed similar differences by race/ethnicity with Hispanic mothers reporting shorter night sleep duration (β = -32.1 ± 14.1, P = .05), longer daytime sleep duration (β = 35.4 ± 15.4, P = .05), and being less likely to consider their infant's sleep as a problem compared to NHW mothers (OR 0.4; 95% CI 0.1-0.9, P = .05). Fig. 3 shows differences in nighttime sleep duration by race/ethnic group, stratified by bedtime.
Fig. 3.
Violin plot illustrating the distribution of infant night sleep duration by race/ethnicity, stratified by bedtime.
Infant sleep and intrinsic infant characteristics
Older age at assessment was associated with shorter sleep duration during the day (Model 3 β = -4.9 ± 2.4, P = .05), shorter sleep latency (Model 3 OR 0.9; 95% CI 0.8-1.0, P = .05), and less night awakenings (Model 2 β = -0.07 ± 0.03, P = .05; Model 3 β = -0.07 ± 0.02, P = .05). Male infants had more awakenings (Model 1 β = 0.5 ± 0.01, P = .001; Model 2 β = 0.4 ± 0.1, P = .01; Model 3 β = 0.4 ± 0.1, P = .01), and their mothers were more likely to perceive their sleep as a problem compared to mothers of females (Model 1 OR 1.8; 95% CI 1.0-3.1, P = .05; Model 2 OR 1.8; 95% CI 1.0-3.1, P = .05; Model 3 OR 1.7; 95% CI 1.0-3.1, P = .05).
Infant sleep and insurance status
Insurance status was significantly associated with night sleep duration, such that mothers with Medicaid reported shorter duration in Model 2 (β = -28.8 ± 13.9, P = .05), but once we accounted for PIBBF the association was no longer significant.
Infant sleep and PIBBF
Regarding the associations of sleep variables with bedtime practices, later bedtime was associated with shorter night sleep duration (Model 3 β = -21.0 ± 4.0, P = .001), shorter total sleep duration (Model 3 β = -17.3 ± 5.4, P = .001), and longer latency (Model 3 OR 1.4; 95% CI 1.1-1.6, P = .001). Parents of infants who fell asleep being fed/rocked/held reported longer sleep latency compared to those who fell asleep in bed independently (Model 3 OR 2.1; 95% CI 1.1-3.9, P = .05). Infants who were exclusively formula fed slept less at night (Model 3 β = 34.8 ± 14.2, P = .05) but had less awakenings (Model 3 β = -0.5 ± 0.2, P = .01), while those who were partially fed with breastmilk and partially with formula had shorter night (Model 3 β = -34.4 ± 13.8, P = .05) and total sleep duration (Model 3 β = 36.8 ± 18.4, P = .05) compared to fully breastfed infants. Lastly, infants from families who practiced co-sleeping or slept in the same room but in separate beds had more awakenings compared to those who slept in their own room (co-sleeping Model 3 β = 0.8 ± 0.3, P = .05, sleep in same room Model 3 β = 0.4 ± 0.2), and infants who co-slept had longer sleep duration during the day (Model 3 β = 61.6 ± 27.8, P = .05) and over 24 hour (Model 3 β = 79.0 ± 34.4, P = .05).
Infant sleep and maternal perceptions of infant sleep as a problem
Number of night awakenings was positively associated with maternal perception of infant sleep as a problem (Model 4 OR 2.2; 95% CI 1.6-3.3, P = .001). Shorter daytime sleep duration and a sleep latency between 30 and 60 minutes were also associated with maternal perception of infant sleep as a problem (Daytime sleep duration: β = -0.005 ± 0.002, P = .01; Latency: β = 1.5 ± 0.6, P = .01).
Infant sleep and the COVID-19 pandemic
In the supplement, we have reported results for models additionally adjusted for time of the pandemic. Results show that none of the infant sleep domains were significantly affected by this variable.
Table 3.
Results from regression analyses
| Night sleep duration | Model 1 | Model 2 | Model 3 | |
|---|---|---|---|---|
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | -39.3 (20.5)+ | -29.4 (20.8) | -6.4 (19.8) | |
| Hispanic | -70.4 (12.5)*** | -54.3 (15.0)*** | -32.1 (14.1) * | |
| Sex | -2.5 (11.6) | 2.1 (11.6) | -2.3 (10.8) | |
| Age at assessment | 3.1 (2.4) | 3.7 (2.4) | 4.0 (2.2) | |
| Insurance status | ||||
| Commercial | Ref | Ref | ||
| Medicaid | -28.8 (13.9)* | -5.8 (13.2) | ||
| Sleep environment | ||||
| Crib in a separate room | Ref | |||
| Crib in mother's room | -16.4 (16.0) | |||
| Co-sleeping | 4.1 (25.8) | |||
| How baby falls asleep | ||||
| In bed alone | Ref | |||
| While feeding/being rocked/being held/in bed near parent | -16.4 (14.0) | |||
| Bedtime | -21.0 (4.0)*** | |||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | |||
| Breastmilk and formula | -34.4 (13.8)* | |||
| Exclusively formula | -34.8 (14.2)* | |||
| Day sleep duration | Model 1 | Model 2 | Model 3 | |
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | -11.3 (21.4) | -11.4 (21.9) | -5.6 (22.5) | |
| Hispanic | 41.2 (12.5)** | 41.6 (14.9)** | 35.4 (15.4) * | |
| Sex | 17.6 (11.7) | 17.9 (0.1) | 23.6 (11.9)* | |
| Age at assessment | -4.0 (2.4)+ | -4.1 (2.4)+ | -4.9 (2.4)* | |
| Insurance status | ||||
| Commercial | Ref | Ref | ||
| Medicaid | -0.3 (14.0) | -4.7 (14.4) | ||
| Sleep environment | ||||
| Crib in a separate room | Ref | |||
| Crib in mother's room | 10.3 (17.1) | |||
| Co-sleeping | 61.6 (27.8)* | |||
| How baby falls asleep | ||||
| In bed alone | Ref | |||
| While feeding/being rocked/being held/in bed near parent | 14.7 (15.7) | |||
| Bedtime | 4.1 (4.6) | |||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | |||
| Breastmilk and formula | -14.9 (15.1) | |||
| Exclusively formula | 5.3 (15.7) | |||
| Total sleep duration | Model 1 | Model 2 | Model 3 | |
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | -24.8 (25.5) | -18.4 (26.2) | -16.4 (26.7) | |
| Hispanic | -19.4 (15.6) | -10.6 (18.6) | -0.5 (18.8) | |
| Sex | 19.2 (14.6) | 17.5 (14.7) | 19.5 (14.5) | |
| Age at assessment | -2.5 (3.0) | -2.0 (3.0) | -2.9 (2.9) | |
| Insurance status | ||||
| Commercial | Ref | Ref | ||
| Medicaid | -17.2 (17.4) | -5.3 (17.7) | ||
| Sleep environment | ||||
| Crib in a separate room | Ref | |||
| Crib in mother's room | 10.2 (20.9) | |||
| Co-sleeping | 79.0 (34.4)* | |||
| How baby falls asleep | ||||
| In bed alone | Ref | |||
| While feeding/being rocked/being held/in bed near parent | -11.3 (19.0) | |||
| Bedtime | -17.3 (5.4)** | |||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | |||
| Breastmilk and formula | -36.8 (18.4)* | |||
| Exclusively formula | -15.3 (18.9) | |||
| Night awakenings | Model 1 | Model 2 | Model 3 | |
|---|---|---|---|---|
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | -0.2 (0.2) | -0.3 (0.2) | -0.3 (0.2) | |
| Hispanic | -0.2 (0.1) | -0.3 (0.2)* | -0.3 (0.2)+ | |
| Sex | 0.5 (0.1)*** | 0.4 (0.1)*** | 0.4 (0.1)** | |
| Age at assessment | -0.07 (0.03)* | - 0.07 (0.03)* | -0.7 (0.02)* | |
| Insurance status | ||||
| Commercial | Ref | Ref | ||
| Medicaid | -0.3 (0.1)+ | -0.3 (0.1)+ | ||
| Sleep environment | ||||
| Crib in a separate room | Ref | |||
| Crib in mother's room | 0.4 (0.2)* | |||
| Co-sleeping | 0.8 (0.3)* | |||
| How baby falls asleep | ||||
| In bed alone | Ref | |||
| While feeding/being rocked/being held/in bed near parent | 0.2 (0.2) | |||
| Bedtime | -0.04 (0.04) | |||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | |||
| Breastmilk and formula | -0.2 (0.2) | |||
| Exclusively formula | -0.5 (0.2)** | |||
| Latency | Model 1 | Model 2 | Model 3 | |
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | 2.5 [1.1-5.6]* | 2.6 [1.2-5.9]* | 1.7 [0.7-3.4] | |
| Hispanic | 1.3 [0.8-2.0] | 1.3 [0.8-2.4] | 1.1 [0.6-2.0] | |
| Sex | 1.1 [0.7-1.7] | 1.1 [0.7-1.7] | 1.0 [0.6-1.6] | |
| Age at assessment | 0.9 [0.8-1.0]+ | 0.9 [0.8-1.0]+ | 0.9 [0.8-1.0]+ | |
| Insurance status | ||||
| Commercial | Ref | Ref | ||
| Medicaid | 0.9 [0.5-1.5] | 0.8 [0.4-1.4] | ||
| Sleep environment | ||||
| Crib in a separate room | Ref | |||
| Crib in mother's room | 0.8 [0.4-1.6] | |||
| Co-sleeping | 1.1 [0.4-3.3] | |||
| How baby falls asleep | ||||
| In bed alone | Ref | |||
| While feeding/being rocked/being held/in bed near parent | 2.1 [1.1-3.9]* | |||
| Bedtime | 1.4 [1.1-1.6]*** | |||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | |||
| Breastmilk and formula | 0.9 [0.5-1.7] | |||
| Exclusively formula | 0.9 [0.5-1.7] | |||
| Infant sleep as a problem | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Race/ethnicity | ||||
| Non-Hispanic White | Ref | Ref | Ref | |
| Black/African American | 0.8 [0.3-1.9] | 0.9 [0.4-2.3] | 0.8 [0.3-2.0] | 0.3 [0.06-1.0]+ |
| Hispanic | 0.4 [0.2-0.7]*** | 0.5 [0.2-0.9]* | 0.4 [0.2-0.8]* | 0.4 [0.1-0.9]* |
| Sex | 1.8 [1.0-3.1]* | 1.8 [1.0-3.1]* | 1.7 [1.0-3.1]* | 2.2 [1.0-4.7]* |
| Age at assessment | 0.9 [0.8-1.0] | 0.9 [0.8-1.1] | 1.0 [0.9-1.1] | 1.0 [0.8-1.1] |
| Insurance status | ||||
| Commercial | Ref | Ref | Ref | |
| Medicaid | 0.6 [0.3-1.2] | 0.5 [0.3-1.1]+ | 0.4 [0.2-1.0]+ | |
| Sleep environment | ||||
| Crib in a separate room | Ref | Ref | ||
| Crib in mother's room | 1.7 [0.7-3.9] | 1.6 [0.6-4.9] | ||
| Co-sleeping | 1.2 [0.3-4.7] | 1.9 [0.3-11.6] | ||
| How baby falls asleep | ||||
| In bed alone | Ref | Ref | ||
| While feeding/being rocked/being held/in bed near parent | 1.5 [0.7-3.3] | 1.0 [0.4-2.8] | ||
| Bedtime | 1.2 [1.0-1.4] | 1.2 [0.9-1.6] | ||
| Breastfeeding | ||||
| Exclusively breastmilk | Ref | Ref | ||
| Breastmilk and formula | 1.0 [0.5-2.0] | 0.9 [0.4-2.3] | ||
| Exclusively formula | 0.7 [0.3-1.4] | 1.2 [0.4-3.2] | ||
| Nighttime sleep duration | 1.0 [1.0-1.0] | |||
| Day time sleep duration | 0.9 [0.9-1.0]* | |||
| Latency | ||||
| 0-15 mins | Ref | |||
| 16-30 mins | 1.0 [0.4-2.8] | |||
| 31-60 mins | 4.7 [1.6-14.7]** | |||
| 60-120 mins | 1.4 [0.4-4.9] | |||
| Night awakening | 2.2 [1.6-3.3] *** |
Model 1: primary independent variable (IV) race/ethnicity, covariates: infant sex and age at assessment. Model 2: primary IV race/ethnicity, covariates: infant sex, infant age at assessment, and insurance status. Model 3: primary IV race/ethnicity, covariates: infant sex and age at assessment, parent-infant bedtime behavioral factors (sleep environment, how does baby fall asleep, bedtime, and breastfeeding). Model 4: primary IV race/ethnicity, covariates: infant sex and age at assessment, parent-infant bedtime behavioral factors (sleep environment, how does baby fall asleep, bedtime, and breastfeeding), infant sleep variables (nighttime and day time sleep duration, latency, night awakenings) .
* p=0.05, ** p=0.01, *** p=0.001.
Discussion
In this study, we found marked differences in infant sleep duration, latency, and maternal perception of sleep as a problem by race/ethnicity at 4 months of age. We also found that parental bedtime practices were more robustly associated with the variation by race/ethnicity in infant sleep problem perception than insurance status, a proxy for SES.
These findings are consistent with previous literature indicating racial/ethnic differences in sleep duration in infancy.10 , 34 Ash et al found that at 6 months Hispanic infants slept 1 hour less during the night than NHW infants and adjustment by SES only attenuated this difference by 21%. Similarly, in our results Hispanic infants slept ∼70 minutes less at night compared to NHW, and insurance status, our proxy measure for SES, only partly reduced this difference to ∼54 minutes. After additionally adjusting for PIBBF, the difference was ~32 minutes. This is different from what is reported by Ash et al,35 who found that adjustment for parenting behaviors/practices actually reversed the association between ethnicity and sleep duration, so that Hispanic infants slept more than NHW. Nonetheless, the set of parameters used for adjustment between our study and Ash et al only partly overlaps, since they had additional information on country of birth, acculturation income, employment and family structure, and stress.
Yu et al found similar differences in sleep duration at night and showed differences by daytime sleep duration, with Hispanic infants sleeping more, in accordance with our results. In contrast with their findings, we did not find differences for B/AA infants for daytime sleep duration. Similar to Yu et al, overall sleep duration and number of night awakenings did not differ by race/ethnicity, after adjustments. The absence of significant differences in 24-hour sleep duration between NHW and Hispanic infants in our findings and those from Yu et al,34 suggest that the main difference between the two groups lies in the organization of sleep during the 24-hour period, with Hispanic infants sleeping less at night but catching up during the day. Further research is warranted to expand on this in a longitudinal cohort, since a few studies have indicated that later bed/wake times are associated with more obesogenic behaviors and poorer health outcomes.36 , 37 Our results also extend previous knowledge reporting differences by race/ethnicity in sleep latency where we found longer sleep latency in B/AA infants. Nonetheless, this difference was not significant after adjusting for PIBBF. We also confirmed, as reported in previous studies, that maternal perception of infant sleep as a problem is associated with infant sleep, particularly by number of night awakenings,30 but it is also shaped by demographic and cultural variables, as outlined by previous research.29 In our cohort, Hispanic mothers were less likely to report infant sleep as a problem and this association remained significant even after adjustment for insurance status, PIBBFs, and infant sleep. In the context of a social ecological sleep model,38 - 40 SES has been suggested to contribute to children's sleep due to quality of home and neighborhood environments,41 , 39 parental education, family stress,42 or due to parents’ work schedules.43 Using health insurance status as a proxy for SES, we found that low SES only marginally attenuated the association between race/ethnicity disparities in infants’ sleep health. This finding was consistent with other studies of toddlers and of preschoolers,44 wherein SES variables did not significantly account for race/ethnic disparities in early childhood sleep health characteristics. Their findings indicated that parent behaviors related to sleep, such as bedtime routine consistency, were the primary contributing factors, although they might not be completely independent from SES. Later bedtime has also been reported by parents for Hispanic and B/AA toddlers and preschoolers.45 Our current findings extend this knowledge to the infant period.
Our analyses showed that PIBBFs were significantly associated with sleep duration, latency, and number of awakenings, and accounted for several of the racial/ethnic differences found in the unadjusted models. A study utilizing a cohort of ∼30,000 infants and toddlers investigated the role of parental behaviors and sleep ecology in explaining variance of sleep patterns, and also found that best predictors of nighttime sleep were related to parental behaviors at bedtime and during the night.46 Consistent with these findings, we found that sleep duration was predominantly explained by parental report of infants’ bedtime. Regarding the effect of sleeping arrangements on infants’ sleep health, our results are in line with the literature, showing more night awakenings for co-sleeping.47 In addition, Sadeh et al found similar results regarding sleep patterns between breastfed vs. formula fed infants, and showed that breastmilk is digested more quickly and therefore infants who are breastfed rather than formula-fed wake up more often to eat as a result.25
Inclusive sampling of multiple racial/ethnic and SES groups is largely missing in the extant literature described above. In this study, we explored parental bedtime practices and SES as potential factors contributing to infant racial/ethnic disparities. In our study, parental behaviors associated with worse sleep outcomes were significantly more common among Hispanic and B/AA mothers, since they were more likely to co-sleep or sleep in the same room rather than in separate rooms from the infants and their infants went to bed later compared to NHW. This information is critical since there has been sparse research adapting sleep interventions for populations disproportionately impacted by poor sleep health. Although some of the social and environmental influences leading to worse sleep may not be readily modifiable (eg, SES, availability of a separate sleep space for children), sleep interventions that address modifiable factors (eg, bedtime, bedtime behaviors), accounting for the need of families experiencing these challenges, would empower them to improve sleep health with potential downstream effects on the overall health of their infants.48 In fact, it has been shown that even a 45 minutes increase in sleep opportunity can lead to significant improvement in children's physical, cognitive, and behavioral health.49 In addition, tailored interventions could optimize real-world uptake and effectiveness.50
Sleep interventions that do not consider the needs of the populations who should benefit from them are destined to fail. In a recent paper, it was reported that, while there were no significant racial/ethnic differences in implementing behavioral sleep intervention, Black non-Hispanic mothers were more likely to report stopping them prior to completion.51 At the same time, one study that focused on ethnically diverse mothers living with economic adversity found that they valued sleep for themselves and their children, which suggests that, if appropriate, interventions would be welcomed.52 Fortunately, there are emerging programs that hold promise to reducing sleep health disparities in early childhood.53
Limitations of this study include the cross-sectional design and the limited available data on socioecological factors, such as parental education, parental stress, number of children in the house, and presence of bedtime routines, that may influence sleep health among infants and help elucidate the underlying mechanisms behind the identified sleep health differences between race/ethnicity groups. As the research evolves in the field of pediatric sleep health disparities, it will be important to follow the suggestions published in the adult literature on best approaches for future research on sleep health disparities.54 Moreover, the reliance of parent-reported sleep health must be considered when interpreting these findings. Research on children's behavior has noted that parental reports may be biased55 and affected by sleep practices, such as co-sleeping,25 and future studies would benefit from objective measures of sleep health. Although data collection for this study occurred during the COVID-19 pandemic, results from our sensitivity analyses did not show an effect of time of the pandemic on infant sleep measures. Nonetheless, we did not have detailed information on COVID-19 infection for the postpartum period, parental stress relative to the pandemic, and income and work changes due to COVID-19, thus we could not account for these factors in our analyses. This study also has several strengths, including a racially/ethnically diverse sample and analyses of several infant sleep domains, a significant addition to the field.
In summary, our study shows racial/ethnic differences in sleep in infants at 4 months of age across several sleep domains. Results highlight the essential role of PIBBF for healthy infant sleep and how these practices are not occurring equally across racial/ethnic groups, potentially due to increased barriers, such as shift-work schedules or sub-optimal home environment, among racial/ethnic minority communities that hinder implementation of optimal bedtime routines. These results highlight important information on the existing health inequities and given the short-term and long-term implications of poor sleep for infant health and neurodevelopment, these results underscore the need to further investigate root causes and mechanisms contributing to these inequities.
Declaration of conflict of interest
DD has received consultation fees from Medela, Inc. The remaining authors have no conflicts to disclose.
Funding
Research reported in this publication was supported by an R01MH126531 to DD and CM and by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under grant number P2CHD058486, awarded to the Columbia Population Research Center. LCS is supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development under grant number K99HD103910. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgments
The authors thank the participants of this study for their generous contribution to this work at the time of high uncertainty and stress.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.sleh.2022.06.010.
Appendix. Supplementary materials
References
- 1.Grandner M.A. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1–22. doi: 10.1016/j.jsmc.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Altevogt B.M., Colten H.R. National Academies Press; 2006. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. [PubMed] [Google Scholar]
- 3.Matricciani L., Olds T., Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012;16(3):203–211. doi: 10.1016/j.smrv.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Patte K.A., Qian W., Leatherdale S.T. Sleep duration trends and trajectories among youth in the COMPASS study. Sleep Health. 2017;3(5):309–316. doi: 10.1016/j.sleh.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Smaldone A., Honig J.C., Byrne M.W. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(suppl 1):S29–S37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 6.Johnson D.A., Jackson C.L., Williams N.J., Alcántara C. Are sleep patterns influenced by race/ethnicity—a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. doi: 10.2147/NSS.S169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crabtree V.M., Korhonen J.B., Montgomery-Downs H.E., Jones V.F., O'Brien L.M., Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Guglielmo D., Gazmararian J.A., Chung J., Rogers A.E., Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health. 2018;4(1):68–80. doi: 10.1016/j.sleh.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith J.P., Hardy S.T., Hale L.E., Gazmararian J.A. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health. 2019;5(1):49–57. doi: 10.1016/j.sleh.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ash T, Davison K.K., Haneuse S., et al. Emergence of racial/ethnic differences in infant sleep duration in the first six months of life. Sleep Med X. 2019;1 doi: 10.1016/j.sleepx.2019.100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nevarez M.D., Rifas-Shiman S.L., Kleinman K.P., Gillman M.W., Taveras E.M. Associations of early life risk factors with infant sleep duration. Acad Pediatr. 2010;10(3):187–193. doi: 10.1016/j.acap.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peña M.-M., Rifas-Shiman S.L., Gillman M.W., Redline S., Taveras E.M. Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep. 2016;39(9):1653–1661. doi: 10.5665/sleep.6086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galland B.C., Taylor B.J., Elder D.E., Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Med Rev. 2012;16(3):213–222. doi: 10.1016/j.smrv.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Pennestri M.-H., Laganière C., Bouvette-Turcot A.-A., et al. Uninterrupted infant sleep, development, and maternal mood. Pediatrics. 2018;142(6):e20174330. doi: 10.1542/peds.2017-4330. [DOI] [PubMed] [Google Scholar]
- 15.Bruni O., Baumgartner E., Sette S., et al. Longitudinal study of sleep behavior in normal infants during the first year of life. J Clin Sleep Med. 2014;10(10):1119–1127. doi: 10.5664/jcsm.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Byars K.C., Yolton K., Rausch J., Lanphear B., Beebe D.W. Prevalence, patterns, and persistence of sleep problems in the first 3 years of life. Pediatrics. 2012;129(2):e276–e284. doi: 10.1542/peds.2011-0372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mersky J.P., Lee C.P., Gilbert R.M., Goyal D. Prevalence and correlates of maternal and infant sleep problems in a low-income US sample. Matern Child Health J. 2020;24(2):196–203. doi: 10.1007/s10995-019-02852-y. [DOI] [PubMed] [Google Scholar]
- 18.Alamian A., Wang L., Hall A.M., Pitts M., Ikekwere J. Infant sleep problems and childhood overweight: effects of three definitions of sleep problems. Prev Med Rep. 2016;4:463–468. doi: 10.1016/j.pmedr.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mindell J.A., Leichman E.S., Composto J., Lee C., Bhullar B., Walters R.M. Development of infant and toddler sleep patterns: real-world data from a mobile application. J Sleep Res. 2016;25(5):508–516. doi: 10.1111/jsr.12414. [DOI] [PubMed] [Google Scholar]
- 20.Sadeh A., Mindell J.A., Owens J. Why care about sleep of infants and their parents? Sleep Med Rev. 2011;15(5):335–337. doi: 10.1016/j.smrv.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Goldberg W.A., Lucas-thompson R.G., Germo G.R., Keller M.A., Poggi E., Sandman C.A. Eye of the beholder ? Maternal mental health and the quality of infant sleep. Soc Sci Med. 2013;79:101–108. doi: 10.1016/j.socscimed.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mindell J.A., Telofski L.S., Wiegand B., Kurtz E.S. A nightly bedtime routine: impact on sleep in young children and maternal mood. Sleep. 2009;32(5):599–606. doi: 10.1093/sleep/32.5.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bathory E., Tomopoulos S. Sleep regulation, physiology and development, sleep duration and patterns, and sleep hygiene in infants, toddlers, and preschool-age children. Curr Probl Pediatr Adolesc Health Care. 2017;47(2):29–42. doi: 10.1016/j.cppeds.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Blair, P.S., Humphreys, J.S., Gringras, P., et al. (2012). Childhood sleep duration and associated demographic characteristics in an English cohort. Sleep 35, no. 3 (2012): 353–360. [DOI] [PMC free article] [PubMed]
- 25.Sadeh A., Tikotzky L., Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Adams E.L., Savage J.S., Master L., Buxton O.M. Time for bed! Earlier sleep onset is associated with longer nighttime sleep duration during infancy. Sleep Med. 2020;73:238–245. doi: 10.1016/j.sleep.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 27.Philbrook L.E., Teti D.M. Bidirectional associations between bedtime parenting and infant sleep: parenting quality, parenting practices, and their interaction. J Fam Psychol. 2016;30(4):431–441. doi: 10.1037/fam0000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ash T, Best J., Khandpur N. Racial/ethnic differences in the contextual factors influencing infant sleep: a qualitative study. Sleep Med Dis Int J. 2020;4(2):48–55. [Google Scholar]
- 29.Mindell J.A., Leichman E.S., Puzino K., Walters R., Bhullar B. Parental concerns about infant and toddler sleep assessed by a mobile app. Behav Sleep Med. 2015;13(5):359–374. doi: 10.1080/15402002.2014.905475. [DOI] [PubMed] [Google Scholar]
- 30.Sadeh A., Mindell J., Rivera L. My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12(5):478–482. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Wild K.T., Betancourt L.M., Brodsky N.L., Hurt H. The effect of socioeconomic status on the language outcome of preterm infants at toddler age. Early Hum Dev. 2013;89(9):743–746. doi: 10.1016/j.earlhumdev.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 32.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6):e570–e577. doi: 10.1542/peds.113.6.e570. [DOI] [PubMed] [Google Scholar]
- 33.Lampl M., Johnson M.L. Infant growth in length follows prolonged sleep and increased naps. Sleep. 2011;34(5):641–650. doi: 10.1093/sleep/34.5.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu X., Quante M., Rueschman M., et al. Emergence of racial/ethnic and socioeconomic differences in objectively measured sleep–wake patterns in early infancy: results of the Rise & SHINE study. Sleep. 2021;44(3):zsaa193. doi: 10.1093/sleep/zsaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ash T, Taveras E.M., Redline S., Haneuse S., Quante M., Davison K. Contextual and parenting factors contribute to shorter sleep among Hispanic/Latinx compared to Non-Hispanic White Infants. Ann Behav Med. 2021;55(5):424–435. doi: 10.1093/abm/kaaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Golley R.K., Maher C.A., Matricciani L., Olds T.S. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37(4):546–551. doi: 10.1038/ijo.2012.212. [DOI] [PubMed] [Google Scholar]
- 37.Olds T.S., Maher C.A., Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34(10):1299–1307. doi: 10.5665/SLEEP.1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bronfenbrenner U. Harvard University Press; 1979. The Ecology of Human Development: Experiments by Nature and Design. [Google Scholar]
- 39.MacKinnon A.L., Tomfohr-Madsen L., Tough S. Neighborhood socio-economic factors and associations with infant sleep health. Behav Sleep Med. 2021;19(4):458–470. doi: 10.1080/15402002.2020.1778478. [DOI] [PubMed] [Google Scholar]
- 40.Owens J., Ordway M. The Social Epidemiology of Sleep. 2019. Sleep among children; pp. 93–120. Oxford University Press. [Google Scholar]
- 41.Doane L.D., Breitenstein R.S., Beekman C., Clifford S., Smith T.J., Lemery-Chalfant K. Early life socioeconomic disparities in children's sleep: the mediating role of the current home environment. J Youth Adolesc. 2019;48(1):56–70. doi: 10.1007/s10964-018-0917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sadeh A., Raviv A., Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000;36(3):291. doi: 10.1037//0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- 43.Lee S., Hale L., Berger L.M., Buxton O.M. Maternal perceived work schedule flexibility predicts child sleep mediated by bedtime routines. J Child Fam Stud. 2019;28(1):245–259. [Google Scholar]
- 44.Patrick K.E., Millet G., Mindell J.A. Sleep differences by race in preschool children: the roles of parenting behaviors and socioeconomic status. Behav Sleep Med. 2016;14(5):467–479. doi: 10.1080/15402002.2015.1017101. [DOI] [PubMed] [Google Scholar]
- 45.Hale L., Berger L.M., LeBourgeois M.K., Brooks-Gunn J. Social and demographic predictors of preschoolers’ bedtime routines. J Dev Behav Pediatr. 2009;30(5):394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mindell J.A., Sadeh A., Kohyama J., How T.H. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11(4):393–399. doi: 10.1016/j.sleep.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 47.Mao A., Burnham M.M., Goodlin-Jones B.L., Gaylor E.E., Anders T.F. A comparison of the sleep-wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry Hum Dev. 2004;35(2):95–105. doi: 10.1007/s10578-004-1879-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williamson A.A., Milaniak I., Watson B., et al. Early childhood sleep intervention in urban primary care: caregiver and clinician perspectives. J Pediatr Psychol. 2020;45(8):933–945. doi: 10.1093/jpepsy/jsaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gruber R., Cassoff J., Frenette S., Wiebe S., Carrier J. Impact of sleep extension and restriction on children's emotional lability and impulsivity. Pediatrics. 2012;130(5):e1155–e1161. doi: 10.1542/peds.2012-0564. [DOI] [PubMed] [Google Scholar]
- 50.Rottapel R.E., Zhou E.S., Spadola C.E., et al. Adapting sleep hygiene for community interventions: a qualitative investigation of sleep hygiene behaviors among racially/ethnically diverse, low-income adults. Sleep Health. 2020;6(2):205–213. doi: 10.1016/j.sleh.2019.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Honaker S.M., Mindell J.A., Slaven J.E., Schwichtenberg A.J. Implementation of infant behavioral sleep intervention in a diverse sample of mothers. Behav Sleep Med. 2021;19(4):547–561. doi: 10.1080/15402002.2020.1817745. [DOI] [PubMed] [Google Scholar]
- 52.Caldwell B.A., Ordway M.R., Sadler L.S., Redeker N.S. Parent perspectives on sleep and sleep habits among young children living with economic adversity. J Pediatr Health Care. 2020;34(1):10–22. doi: 10.1016/j.pedhc.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Bonuck K.A., Blank A., True-Felt B., Chervin R. Promoting sleep health among families of young children in head start: protocol for a social-ecological approach. Prev Chronic Dis. 2016;13:E121. doi: 10.5888/pcd13.160144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Williams N.J., Grandner M.A., Snipes S.A., et al. Racial/ethnic disparities in sleep health and health care: importance of the sociocultural context. Sleep Health. 2015;1(1):28–35. doi: 10.1016/j.sleh.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ordway M.R. Depressed mothers as informants on child behavior: methodological issues. Res Nurs Health. 2011;34(6):520–532. doi: 10.1002/nur.20463. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.