Abstract
Background
Many Intensive Care Unit (ICU) survivors suffer from a multi- system disability, termed the post-intensive care syndrome. There is no current national coordination of either rehabilitation pathways or related data collection for them. In the last year, the need for tools to systematically identify the multidisciplinary rehabilitation needs of severely affected COVID-19 survivors has become clear. Such tools offer the opportunity to improve rehabilitation for all critical illness survivors through provision of a personalised Rehabilitation Prescription (RP). The initial development and secondary refinement of such an assessment and data tools is described in the linked paper. We report here the clinical and workforce data that was generated as a result.
Methods
Prospective service evaluation of 26 acute hospitals in England using the Post-ICU Presentation Screen (PICUPS) tool and the RP. The PICUPS tool comprised items in domains of a) Medical and essential care, b) Breathing and nutrition; c) Physical movement and d) Communication, cognition and behaviour.
Results
No difference was seen in total PICUPS scores between patients with or without COVID-19 (77 (IQR 60-92) vs. 84 (IQR 68-97); Mann-Whitney z = −1.46, p = 0.144. A network analysis demonstrated that requirements for physiotherapy, occupational therapy, speech and language therapy, dietetics and clinical psychology were closely related and unaffected by COVID-19 infection status. A greater proportion of COVID-19 patients were referred for inpatient rehabilitation (13% vs. 7%) and community-based rehabilitation (36% vs.15%). The RP informed by the PICUPS tool generally specified a greater need for multi-professional input when compared to rehabilitation plans instituted.
Conclusions
The PICUPS tool is feasible to implement as a screening mechanism for post-intensive care syndrome. No differences are seen in the rehabilitation needs of patients with and without COVID-19 infection. The RP could be the vehicle that drives the professional interventions across the transitions from acute to community care. No single discipline dominates the rehabilitation requirements of these patients, reinforcing the need for a personalised RP for critical illness survivors.
Keywords: Rehabilitation needs, intensive care, COVID-19
Introduction
Survivorship is increasingly considered to be a defining issue for modern critical care. 1 Many who leave intensive care units (ICUs) alive suffer from post intensive care syndrome2,3 to which many factors contribute: rapid acute muscle wasting and associated disability 4 ; cognitive problems relating to impaired short-term memory and executive function; depression, anxiety and post-traumatic stress-disorder 5 ; and dysphonia and dysphagia in those with and without tracheostomies. 6 Impacts are compounded by increased sedentary behaviour, and from psychosocial problems that arise from increased dependency, unemployment and economic deprivation.7,8 Functional capacity can be impaired for more than 5 years. 8
Early multi-disciplinary rehabilitation following major illness or injury is both effective and highly cost efficient.9,10 The UK Rehabilitation Outcomes Collaborative (UKROC), an NHS England-commissioned national clinical registry, systematically collates data on needs, inputs and outcomes for every patient admitted for inpatient specialist rehabilitation in England 11 with, as yet, no equivalent system in the community. The British Society of Rehabilitation Medicine’s (BSRM’s) patient-held Rehabilitation Prescription (RP) for major trauma 12 sets out an individual’s on-going rehabilitation needs and the plan to provide for them. Data are collated nationally through the Trauma Audit and Research Network (TARN). 13 Linked TARN and UKROC data led to a National Clinical Audit quantifying the shortfall in provision of specialist inpatient rehabilitation beds in England and the cost of rectifying it. 14
Despite national guidance being published in 2009, 15 and a wealth of academic output since, there is no national coordination of either rehabilitation pathways or data collection for ICU survivors. Any provision of post-ICU rehabilitation services is determined at Trust level. 16 More specifically, in the last year, the need for tools to systematically identify the multidisciplinary rehabilitation needs of severely affected COVID-19 survivors in a comprehensive way has become clear. Such tools offer the opportunity to improve rehabilitation for all critical illness survivors through provision of a personalised RP. 17
The Intensive Care Society (ICS) and the BSRM convened the National Post-Intensive Care Rehabilitation Collaborative to develop the Post-ICU Presentation Screen (PICUPS) tool as a means to identify the rehabilitation needs not just of post-ICU COVID-19 patients, but of all critical care survivors. 18 This tool was intended to address the first stage of the care pathways following severe illness/injury, as set out by the BSRM, 17 supporting triage and handover of ICU patients stepping down to acute wards and onwards into rehabilitation, informing the immediate care plan whilst signposting to relevant disciplines for further assessment and intervention and thus aiding the development of a personalised RP. It was also intended to support systematic collection of data on rehabilitation needs, and to be completed by any member of the critical care team, not requiring any disciplinary specific knowledge.
The initial development and secondary refinement of the PICUPS assessment and data tools is described in the linked paper [ref]. These tools are also available on the Intensive Care Society’s web page: https://members.ics.ac.uk/ICS/ICS/GuidelinesAndStandards/Framework_for_assessing_early_rehab_needs_following_ICU.aspx. In brief the PICUPS is a screening tool for rehabilitation needs across disciplines. Thresholds set within the score-range for each item trigger referrals to the various different disciplines for further evaluation using more detailed assessment tools, which PICUPs does not replace. These then inform the RP on step down from acute care to indicate their needs for rehabilitation during their next stage of care and the plans to provide for them (ranging from inpatient rehabilitation to community-based services).
Given the time pressures related to the COVID-19 first wave, the PICUPS and RP minimum dataset have now been incorporated into the UKROC dataset and a dedicated data collection software package is freely available on request from lnwh-tr.ukroc@nhs.net.
The roll out and testing of the PICUPS and RP followed a methodology used in implementation science, where a range of methods are deployed to facilitate spread and adoption of innovations. Both the PICUPS and RP are designed as clinical tools, out of which useful data fall. As a result of extensive ICU community engagement with the tool, and enthusiasm for the RP, a significant amount of clinical data was generated on the rehabilitation needs of patients following ICU Care, which are described in this manuscript.
Methods
The design and data collection for the national pilot are described in Part I.
The aims of presenting this analysis is to provide insights into the type of information that the PICUPS and RP can provide and how this may be used to inform clinical practice and service provision.
Quantitative analysis
Data were extracted and cleaned using Microsoft Excel, and exported to the Statistical Package for Social Sciences (SPSS version 26, IBM Inc) for pilot analysis. Missing data were expected for a number of reasons including the rapidity of development and dissemination. No data were imputed. Although data on age, sex and ethnicity were collected and held locally, they were not collated centrally in this pilot in order to preserve subject anonymity. The clinical data presented here were tested for normality using D’Agustino and Pearson Omnibus, and reported as Median (Interquartile Range). Significance was set at p < 0.008 allowing for multiple testing and all tests were two-tailed.
A network plot of disciplines was created using Pearson correlations (https://igraph.org/r). Each node represents a discipline, and its size is proportional to the frequency of cases requiring that discipline. The width of edges is proportional to the correlation between nodes. No minimum limit of correlation was used. We used the force-directed Fruchterman-Reingold algorithm to determine the layout, which positions correlated nodes closer to one another. 19 COVID-19 status was added as a further node in a sensitivity analysis.
Further methodological details are available in the online supplement (https://journals.sagepub.com/doi/suppl/10.1177/1751143720988708).
Results
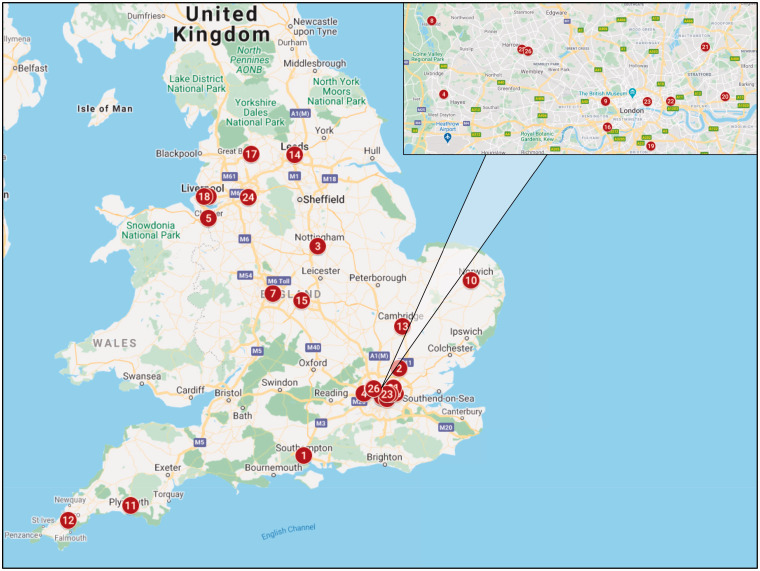
Data were collated from 314 patients from 26 hospitals that were widely distributed around England (Figure 1). Of these, 276 records included at least some information on rehabilitation needs in the RP section (Figure 2 (See Part I: https://journals.sagepub.com/doi/pdf/10.1177/1751143720988715)), and COVID-19 diagnosis was confirmed in 118 of these (42.8%).
Figure 1.
Geographic distribution of participating centres.
1: University of Southampton NHS Trust; 2: The Princess Alexandra Hospital; 3: Queens Medical Centre, Nottingham; 4: The Hillingdon Hospital; 5: Countess of Chester Hospital; 6: Liverpool Heart and Chest Hospital; 7: Queen Elizabeth Hospital Birmingham; 8: Harefield Hospital; 9: St Marys Hospital London; 10: Norfolk & Norwich University Hospital; 11: University Hospitals Plymouth NHS Trust; 12: Royal Cornwall Hospital NHS Trust; 13: Addenbrookes Hospital Cambridge; 14: Leeds Teaching Hospitals; 15: University Hospitals Coventry & Warwick; 16: Harefield Hospital, London; 17: East Lancashire Hospitals NHS Trust; 18: Royal Liverpool University; 19: Kings College Hospital; 20: Barts Health (Newham Hospital); 21: Barts Health (Whipps Cross Hospital); 22: Barts Health (Royal London Hospital); 23: Barts Health (St Bartholomew's Hospital); 24: Wythenshawe Hospital Manchester; 25: London Northwest University Healthcare NHS Trust (Northwick Park); 26: London Northwest University Healthcare NHS Trust (RHRU).
Figure 2.
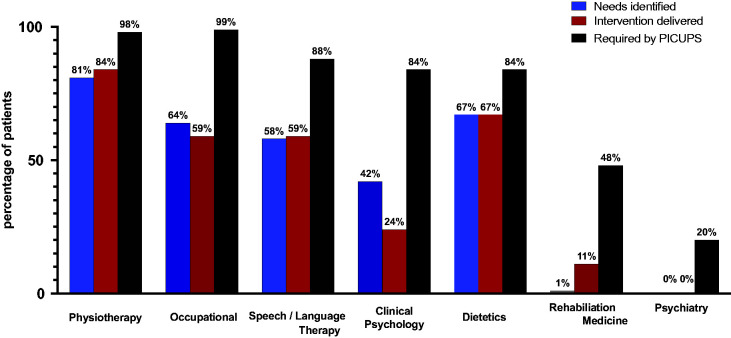
Total PICUPS scores and subscales compared between patients with (red) and without (blue) COVID-19. Data are Median (Interquartile Range). Significance was set at p < 0.008 for a Mann Whitney U test allowing for multiple tests; * indicates significant between group differences.
Workforce needs and the effect of COVID-19 diagnoses
One hundred and thirty-nine patients had at least one complete PICUPS score, of whom 56 (40.3%) had COVID-19 and 83 (59.7%) did not. No difference was seen in total PICUPS scores between patients with or without COVID-19 (77 (IQR 60–92) vs. 84 (IQR 68–97); Mann-Whitney z = −1.46, p = 0.144, Figure 2). The PICUPS Physical and Psychosocial scales were also not different between groups when analysed according to the three subscales identified by factor analysis in Part I (https://journals.sagepub.com/doi/suppl/10.1177/1751143720988708). The PICUPS Respiratory subscale was higher in non-COVID-19 patients (31 (IQR 27–34) vs. 29 (IQR 24–32); p = 0.006), from a total possible score range 0-35 (Table 1, Figure 2).
Table 1.
Total PICUPS scores and subscales compared between patients with (red) and without (blue) COVID-19. Data are Median (Interquartile Range). Significance was set at p < 0.008 for a Mann Whitney U test allowing for multiple tests.
| Item | COVID-19 | Non-COVID-19 | z-score | P |
|---|---|---|---|---|
| N | 56 | 69 | ||
| PICUPS-basic | 51 (39–59) | 52 (45–58) | –0.93 | 0.353 |
| PICUPS-plus | 28 (19–36) | 31 (22–41) | –1.92 | 0.055 |
| PICUPS total | 77 (60–92) | 84 (68–97) | –1.46 | 0.144 |
| PICUPS Subscales | ||||
| Physical | 33 (22–44) | 35 (24–50) | –1.10 | 0.270 |
| Respiratory | 29 (24–32) | 31 (27–34) | –2.77 | 0.006 a |
| Psychosocial | 17 (13–18) | 17 (14–19) | 0.93 | 0.353 |
aSignificant between group differences.
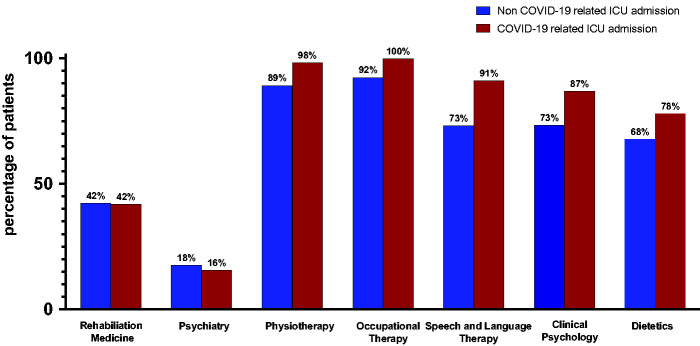
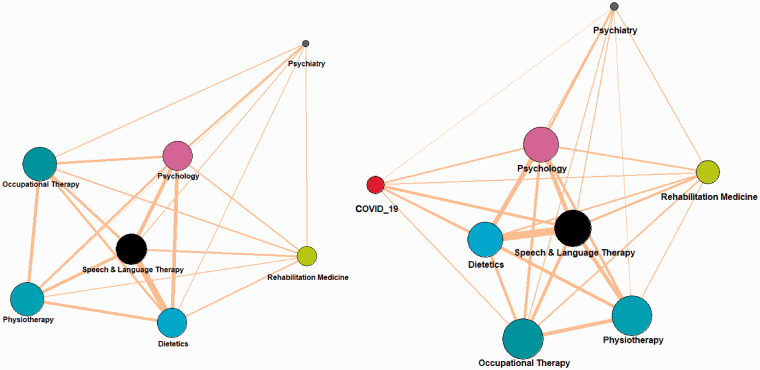
Differences were seen between groups in median workforce requirements (5 disciplines (IQR 5–6) versus 5 disciplines (IQR 4–6); p = 0.002; n = 221, Figure 3). Network analysis demonstrated that requirements for physiotherapy, occupational therapy, speech and language therapy, dietetics and clinical psychology were closely related (Figure 4(a)). The linkage of discipline needs did not differ between COVID-19 and non-COVID-19 patients (Figure 4(b)).
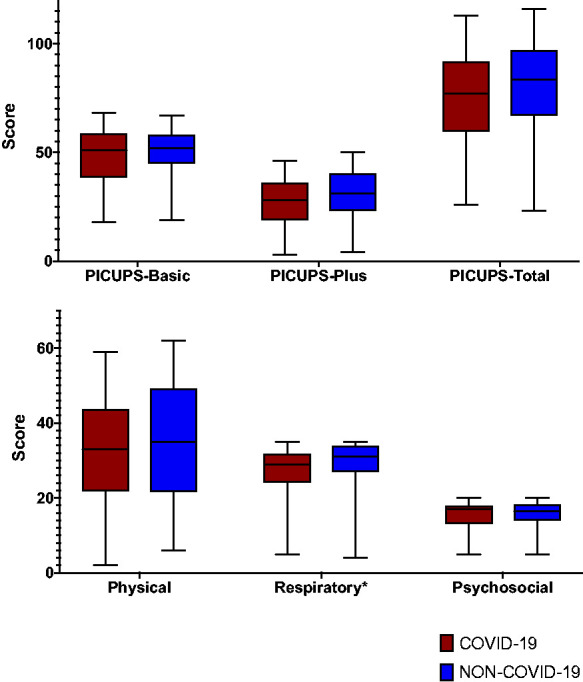
Figure 3.
Proportion of patients requiring each discipline.
Figure 4.
Network analyses of discipline interdependencies. Panel (a) all patients, (b): with the addition of a COVID-19 infection node. Each node represents a discipline, and its size is proportional to the frequency of cases requiring that discipline. The width of edges is proportional to the correlation between nodes. A force-directed Fruchterman-Reingold algorithm determined the layout, which positions correlated nodes closer to one another.
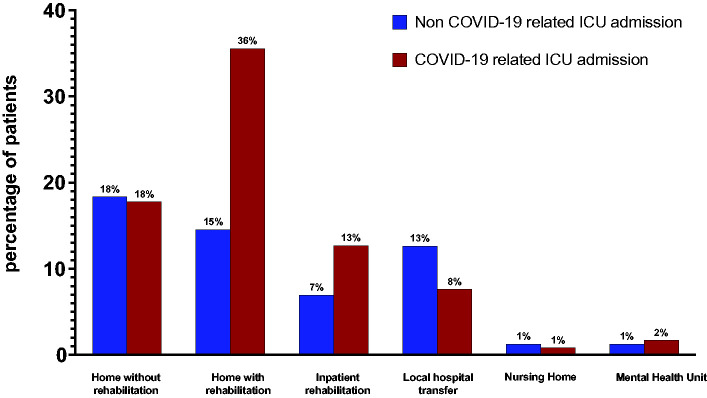
Discharge destination was, however, affected by COVID-19 diagnoses as a greater proportion of COVID-19 patients were referred for inpatient rehabilitation (13% vs. 7%) and community-based rehabilitation (36% vs.15%, Figure 5).
Figure 5.
Discharge destination of patients with and without COVID-19 related admissions.
Rehabilitation prescription
The RP informed by the PICUPS tool generally specified a greater need for multi-professional input when compared to rehabilitation plans instituted. This was seen across all disciplines; Physiotherapy (93% vs. 81%), Occupational Therapy (96% vs. 64%), Speech and Language Therapy (81% vs. 58%), Clinical Psychology (80% vs. 42%) and Dietetics (72% vs. 67%) shown in Figure 6. There was no difference in the pattern of referral required by COVID-19 and Non-COVID-19 patients. The RP required involvement of a consultant in rehabilitation medicine in 48% of patients and a psychiatrist in 20%, but were rarely identified as being required without PICUPS + RP. Delivery of rehabilitation generally matched rehabilitation plans across disciplines except for Clinical Psychology (42% required, 24% delivered), but was universally less that required by the PICUPS and RP.
Figure 6.
Frequency of requirements for involvement of disciplines, by clinical rehabilitation plans (blue = identifed, red = delivered) and as required by the PICUPS (black).
Discussion
We set out originally to develop and test a screening tool for rehabilitation requirements for survivors of critical illness, which would inform a Rehabilitation Prescription. This personalised set of rehabilitation requirements would accompany the patient along their journey of recovery, and reintegration into society. The screening tool was met with significant enthusiasm across a variety of acute settings including District General Hospitals, Trauma Centres and Major Teaching Hospitals (we expected 100–150 scores, but in the end received over 500), this offering the additional opportunity to systematically describe the rehabilitation workforce needs of the critically ill survivor in England. A wide variety of clinicians engaged with the process, and reported the PICUPS to be a useful tool both for clinical practise, multi-disciplinary engagement and for patient care. To our knowledge, this pilot study represents the largest characterisation of the spectrum of rehabilitation needs of intensive care survivors within the context of services and manpower required.
Patient requirements and workforce needs
The high burden of rehabilitation needs in this post-ICU cohort likely exceeds those generally planned for i.e. a systematic method of screening is likely to be more efficient and focussed on patient need. This is in keeping with other aspects of care of the critically ill, where robust processes, as opposed to individual clinicians’ strategies, are more likely to lead to improvements in patient outcomes. 20 In the setting of post-critical care rehabilitation in the UK, this has been exacerbated by the lack of overarching national strategy. We hope that more systematic use of PICUPS+RP may help to rectify this deficit. The network analysis clearly demonstrates the inter-related nature of the rehabilitation workforce, and that no single specialty should be asked to drive this. Indeed, specialty driven services (as opposed to those driven by the needs of patients) are at risk of confirmation bias and exclusion of other services, both of which are detrimental to patient care.
Recovery from COVID-19 infection
Despite some statistical and numerical differences in rehabilitation need between COVID-19 and non COVID-19 patients, these were not clinically significant. However the COVID patients were more likely to be referred on to Rehabilitation, either as an inpatient or in the community. As time passes and the healthcare community gains experience in dealing with this emergent disease, the commonalities that COVID-19 survivors have with other critical illness survivors are likely to far outweigh the differences. This lesson is being learnt in parallel in the management of Acute Respiratory Distress Syndrome. 21 In terms of rehabilitation of the critically ill patient, the healthcare community has over 2 decades of data and experience to draw on. 22 These data reassure us that the majority of deficits seen in COVID-19 patients are common to all survivors of critical illness. The challenge is to repackage this wealth of knowledge into addressing these deficits in a coordinated fashion. A further challenge will be equity of rehabilitation services. In this study, more COVID-19 survivors were referred for inpatient or community rehabilitation compared to non-COVID-19, despite no discernable differences in needs. This may be the result of many factors, including the success of public awareness campaigns or increased staff awareness of the rehabilitation agenda. 23 Regardless, these data suggest that positive action is required to ensure there is equity of rehabilitation service access for all critical illness survivors, regardless of precipitant diseases.
Strengths and limitations
The rapidity of the development of this pilot led to certain limitations in the dataset. That the PICUPS+RP required greater rehabilitation team input than what was planned clinically may be the result of currently unidentifiable factors: the clinical team may have instituted a plan consistent with the resources available or the PICUPS tool may overestimate the rehabilitation needs of patients. The latter seems less likely as an experienced core therapy team developed thresholds for referrals after careful consideration. Knowledge and motivation have been identified as barriers to rehabilitation planning, and a systematic approach may help overcome this.24,25 Despite the emergency measures for information governance during the pandemic, we remained cautious about any identifiable data. As a result, the disease severity and characteristics of patients were not collated centrally. However the number of sites involved, and the requirement for two different trajectories of recovery ensures that these data are likely to be representative of the national patient population. The rapid engagement to participate in the pilot from the clinical community across the spectrum of critical care services should be noted as suggesting a desire for a consistent approach to improving rehabilitation for these patients. The multi-professional development of the tool and subsequent data collection reflects the strength of the National Post-Intensive Care Collaborative in representing the clinical and academic workforce.
Future directions
At the time of writing, PICUPS and RP development continue to evolve rapidly, along the themes set out as priorities by the Collaborative. Feedback from the pilot has further refined the tool, and most notable is the inclusions of family distress and clearer definitions of terms used. Community engagement continues, with the Welsh Intensive Care Society endorsing the tool, and plans are in place for inclusion of these data points within the Welsh electronic health records. Discussions are ongoing in relation to tool inclusion in discharge summaries in England. The workforce data are being presented to all stakeholders involved in manpower and resource planning for the second wave and the approaching winter. The wide variation in ability to consent to centralised data collection represented a major barrier to workforce planning in the future, and likely signifies the need for it to be mandated by the NHS. Going forwards, NHS Trusts can collect their own local data for clinical purposes at any time, supported by the software developed during this pilot. In view of the above restrictions, and to ensure that all data collection was legally compliant, only de-identified data from the PICUPS and RP has been collated centrally in UKROC to date. However, if future permissions are obtained for the flow of identified data to support tracking of individual patients, the extracts from those local data sources include an option to enable flow of encrypted identifiable data (including retrospective records if appropriate and as permissions allow).
The RP represents an attractive personalised record of needs and has led to significant engagement with Primary Care through webinars, and has been endorsed by the Royal College of General Practitioners. We strongly endorse the future adoption of the Rehabilitation Prescription as a known and proven person-centred vehicle for critical illness survivors with complex rehabilitation requirements to access the local resources they require. This should be through a standardised and consistent tool/platform where data can be collated at a local level for workforce planning and at national level to inform strategic decisions. The authors await the publication of data from the Faculty of Intensive Care Medicine’s “Life after Critical illness” survey, which we feel our data will compliment, and that significant synergy exists between these pieces of work.
The collaborative have further begun work on related versions of PICUPS including versions to be used in the non-critical care settings and in the community.
Conclusions
The PICUPS tool is feasible to implement as a screening mechanism for post-intensive care syndrome, and highlight rehabilitation needs that may be missed by clinical opinion alone. The Rehabilitation Prescription should be the vehicle that drives the professional interventions across the transitions from acute to community care. No single discipline dominates the rehabilitation requirements of these patients, reinforcing the need for a personalised rehabilitation prescription for critical illness survivors.
This work would not have occurred without the support of the critical care community, and we would specifically like to thank Megan Richardson, Katie Dowling, David McWilliams, Ioan Morgan, Tamara Pendry, Charlotte Pereira, Monica Trivedi, Michela Frankland, Rebecca Vokes, Sarah Linford, Callum Skillen, Wendy Willingham, Vicky Newey, Laura Grimsey, Kate Tantam, Louise Mitchell, Rachel Waddington, Sally Westhead, Jacqui Wakefield, Mandie Thomas, Sean Hanley, Natalie Scott, Lee Bolton and Emmeline Maidment-Fullard.
HM was supported by the National Institute for Health Research Biomedical Research Centre at University College London Hospitals.
Supplementary Material
Acknowledgements
We would like to thank the UK Intensive Care Society, the British Society of Rehabilitation Medicine and the National Emergency Committee for COVID Critical Care, for initiating this process, all the patients and clinical teams who took part in this development and pilot study, and members of the National Post-ICU rehabilitation Collaborative who provided feedback and constructive criticism during development of the PICUPS tool. We are additionally grateful to UK Rehabilitation Outcomes Collaborative for supporting this project. Special thanks are due to Sandy Mather, Alex Day and Asha Abdillahi (ICS) for their work in coordinating the participating pilot centres and to Lynette George, Heather Williams, Margaret Kaminska and Keith Sephton (UKROC) for their work with collation and cleaning of the data.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: LTS is a full time NHS employee but, as part of her NHS activities, she directs the UK Rehabilitation Outcomes Collaborative (UKROC), She has a specific research interest in outcomes evaluation and, together with colleagues (including author RJS) she has published extensively on the development and use of standardised measures, and neither LTS or RJS has any personal financial interest in any of the material mentioned in this article.
Several of the authors have clinical academic posts, and research/development publications of this kind may be used by their employing NHS or University organisation to contribute to departmental returns in evaluations such as the NHS R&D reports or the Research Excellence Framework.
ZP has received honoraria for consultancy from GlaxoSmithKline, Lyric Pharmaceuticals, Faraday Pharmaceuticals and Fresenius-Kabi, and speaker fees from Orion, Baxter, Nutricia and Nestle.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Zudin Puthucheary https://orcid.org/0000-0003-4267-1892
Supplemental material
Supplemental material for this article is available online.
References
- 1.Iwashyna TJ. Survivorship will be the defining challenge of critical care in the 21st century. Ann Intern Med 2010; 153: 204–205. [DOI] [PubMed] [Google Scholar]
- 2.Bein T, Bienvenu OJ, Hopkins RO. Focus on long-term cognitive, psychological and physical impairments after critical illness. Intensive Care Med 2019; 45: 1466–1468. [DOI] [PubMed] [Google Scholar]
- 3.Preiser e. Post-Intensive care syndrome. Lessons from the ICU. Cham: Springer International Publishing, 2020. [Google Scholar]
- 4.Puthucheary ZA, Rawal J, McPhail M, et al. Acute skeletal muscle wasting in critical illness. JAMA 2013; 310: 1591–1600. [DOI] [PubMed] [Google Scholar]
- 5.Pandharipande PP, Girard TD, Jackson JC, et al.; BRAIN-ICU Study Investigators. Long-term cognitive impairment after critical illness. N Engl J Med 2013; 369: 1306–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brodsky MB, Huang M, Shanholtz C, et al. Recovery from dysphagia symptoms after oral endotracheal intubation in acute respiratory distress syndrome survivors. A 5-Year longitudinal study. Ann Am Thorac Soc 2017; 14: 376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamdar BB, Huang M, Dinglas VD, et al. Joblessness and lost earnings after ARDS in a 1-Year national multicenter study. Am J Respir Crit Care Med 2017; 196: 1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herridge MS, Tansey CM, Matte A, et al.; Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011; 364: 1293–1304. [DOI] [PubMed] [Google Scholar]
- 9.Turner-Stokes L, Pick A, Nair A, et al. Multi-disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database Syst Rev 2015; 12: CD004170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner-Stokes L, Williams H, Bill A, et al. Cost-efficiency of specialist inpatient rehabilitation for working-aged adults with complex neurological disabilities: a multicentre cohort analysis of a national clinical data set. BMJ Open 2016; 6: e010238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collaborative TURO. The UK Rehabilitation Outcomes Collaborative, www.kcl.ac.uk/cicelysaunders/research/studies/uk-roc/index (2010, accessed 6 January 2021).
- 12.BSRM, www.bsrm.org.uk/downloads/bsrm-core-standards-for-major-trauma-19.11.2018-clean-for-web.pdf (2018, accessed 6 January 2021).
- 13.NHSE. NHS Standard Contract for Major Trauma service (all ages). D15/S/a London, www.england.nhs.uk/wp-content/uploads/2014/04/d15-major-trauma-0414.pdf (2013, accessed 6 January 2021).
- 14.NCASRI. National Clinical Audit for Specialist Rehailitation following major Trauma: Final report London: Health Quality Improvement Partnership, www.kcl.ac.uk/cicelysaunders/about/rehabilitation/nhs-audit-report-v9-rgb.pdf (2019, accessed 6 January 2021).
- 15.NICECG83 Critical illness rehabilitation: NICE guideline 2009.
- 16.England N. COVID-19 hospital discharge service requirements, www.england.nhs.uk/coronavirus/publication/covid-19-hospital-discharge-service-requirements/ (2020, accessed 6 January 2021).
- 17.Phillips M, Turner-Stokes L, Wade D, et al. Rehabilitation in the wake of COVID-19 – a phoenix from the ashes, www.bsrm.org.uk/downloads/covid-19bsrmissue1-published-27-4-2020.pdf (2020, accessed 6 January 2021).
- 18.ICS and BSRM. Responding to COVID-19 and Beyond: framework for assessing early rehabilitation needs following treatment in intensive care, www.ics.ac.uk/ICS/ICS/GuidelinesAndStandards/Framework_for_assessing_early_rehab_needs_following_ICU.aspx (2020, accessed 6 January 2021).
- 19.Fruchterman TMJ, Reingold EM. Graph drawing by force-directed placement. Software: Pract Exp 1991; 21: 1129–1164. [Google Scholar]
- 20.Weled BJ, Adzhigirey LA, Hodgman TM, et al.; Task Force on Models for Critical Care. Critical care delivery: the importance of process of care and ICU structure to improved outcomes: an update from the American college of critical care medicine task force on models of critical care. Crit Care Med 2015; 43: 1520–1525. [DOI] [PubMed] [Google Scholar]
- 21.Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, et al.; on behalf of the COVID-19 Spanish ICU Network. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med 2020; 46: 2200–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hosey MM, Needham DM. Survivorship after COVID-19 ICU stay. Nat Rev Dis Primers 2020; 6: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tantam K, www.plymouthhospitals.nhs.uk/rehablegend (2018, accessed 6 January 2021).
- 24.Reid JC, McCaskell DS, Kho ME. Therapist perceptions of a rehabilitation research study in the intensive care unit: a trinational survey assessing barriers and facilitators to implementing the CYCLE pilot randomized clinical trial. Pilot Feasibility Stud 2019; 5: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parry SM, Knight LD, Connolly B, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med 2017; 43: 531–542. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.