Abstract
A survey was conducted to identify the prevalence of occupational burnout amongst health care professionals caring for COVID-19 patients in the Intensive Care Unit (ICU) of a Welsh hospital. The response rate was 79%. Nurses and other staff reassigned to work in the ICU had higher levels of burnout. Working in Personal Protective Equipment was most distressing, followed by direct patient care. There were positive outcomes including learning opportunities, professional development and job satisfaction. The impact of the pandemic on staff burnout may have been mitigated by acknowledging the contribution of staff, improving communication and encouraging them to access support.
Keywords: Coronavirus disease, health care professionals, occupational burnout, intensive care unit
Introduction
The global pandemic caused by Coronavirus Disease 2019 (COVID-19) has increased the workload on front line health care professionals (HCPs) leading to exhaustion. Chronic staff shortages, coupled with increased demand for acute medical care has led to stretching of existing resources. 1 , 2 Intensive Care Unit (ICU) professionals are at higher risk of occupational burnout which could affect their performance at work, leading to absenteeism, loss of work days 3 and burnout contagion. 4 During the first wave of COVID-19, many HCPs were reallocated to work on COVID wards and ICU to accommodate the increased demand in these areas.
Aims
To identify the prevalence of burnout and the contributing factors amongst HCPs caring for COVID-19 patients admitted to ICU.
Methodology
This study was conducted in August 2020 at Nevill Hall Hospital, a Welsh district general hospital, where ICU bed capacity was increased from 8 to 23 to accommodate the rapid influx of patients. A 15 question survey was distributed by email and WhatsApp to 194 people including ICU and anaesthetic consultants, trainees and non-consultant doctors, Advanced Critical Care Practitioners (ACCPs), ICU nurses, Operating Department Practitioners (ODPs), and non-ICU nurses (scrub nurses, recovery nurses and theatre assistants).
Results
The response rate was 79% (Table 1). 76% found working in Personal Protective Equipment (PPE) stressful, followed by providing patient care (30%), working outside their normal roles (30%), inadequate rest (26%), family problems (25%), difficulty with colleagues (20%) and increased workload (16%).
Table 1.
Survey participants and response rate.
| Total | Responded | Response rate | |
|---|---|---|---|
| Consultants | 22 | 13 | 59% |
| Non consultant doctors | 32 | 20 | 62% |
| ICU nurses | 49 | 47 | 96% |
| Non ICU nurses | 68 | 50 | 73% |
| ODPS | 23 | 23 | 100% |
| Total | 194 | 153 | 79% |
ICU: intensive care unit; ODPS: operating department practitioners.
People reassigned to work in ICU reported difficulty working in an unfamiliar environment, lack of empathy from management and lack of physical rest space due to social distancing. ICU nurses reported difficulties coping with patient deaths, communicating with patient families, supporting non-ICU staff and shortages of experienced nurses and doctors. Doctors revealed struggles with the increased workload, reduced downtime and multiple changes to their roles and responsibilities in a short time frame.
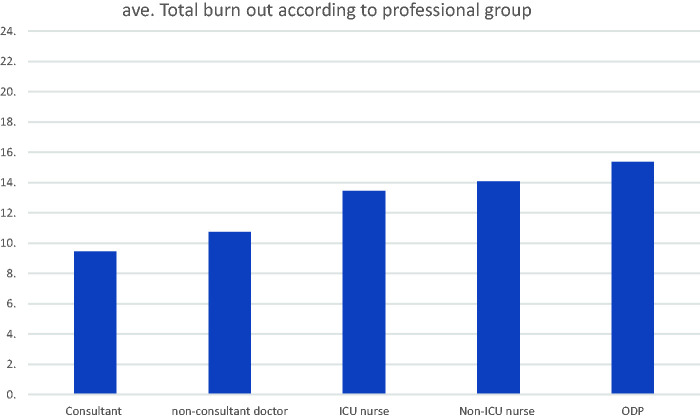
The survey probed into specific symptoms of burnout including tiredness, new headache, depression, helplessness and insomnia. A score was awarded based on its presence either constantly (4), frequently (2), occasionally (1) or never (0) and the average burnout score in each group was calculated (range 0 to 24). ODPs scored highest (15), followed by non-ICU nurses (14) and ICU nurses (13). Consultant doctors scored the lowest (Figure 1).
Figure 1.
Burnout score according to professional group.
Other symptoms highlighted were nightmares, work-related anxiety, irritability, panic attacks, diarrhoea, joint pains, plantar fasciitis and lock-jaw. Dehydration secondary to PPE use and reduced fluid intake to minimise toilet visits was reported. Many felt that their contributions were not acknowledged by management.
Despite an onsite clinical psychology service being embedded to support staff, only 12% had accessed it. Many had sought the support of family, friends, GPs, Unions and religious leaders. Suggestions for improvement included regular debriefing, improving communication whilst in PPE, continuous presence of doctors, fairer distribution of workload and provision of recuperation spaces.
When asked about their thoughts on subsequent waves, 35% felt they were prepared, 46% felt anxious, 10% felt stressed and 7% said they would struggle to cope with another wave. 40% felt they had fully recovered from the stress of the first wave.
Some positive outcomes of working during the pandemic were new learning opportunities, professional development, increased job satisfaction, confidence and camaraderie, and pride in serving during the pandemic.
Discussion
Occupational burnout develops via two pathways: excessive job demands leading to exhaustion, insufficient job resources leading to disengagement. 5 Before pandemic, high burnout scores were reported in 30–50% of HCPs in acute care specialities, with 2–3x higher suicide rates. 6 A 2019 NHS Employers report found that stress accounts for over 30% of sickness absence in the NHS, costing £300–400 million per year. Due to unprecedented working conditions and increased workload during the pandemic, these figures are expected to rise. 7
To safeguard the welfare of staff, wellbeing needs to be explicitly prioritised. Although managers were busy addressing organisational issues, better communication and their physical presence along with a greater appreciation of sacrifices made by staff would have elevated morale. A transformational style of leadership could be used as the model to address these issues. 8
Conclusion
This study identified the presence of burnout symptoms amongst HCPs working in Welsh ICU during the COVID-19 pandemic. Working in PPE is challenging and unavoidable, hence encouraging refreshment breaks is essential to mitigate exhaustion. Acknowledging the contribution of staff, encouraging them to seek support from peers and psychologists will hopefully enable them to cope with the challenges that future spikes will present.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gayathri Chinnappa Srinivas https://orcid.org/0000-0002-8527-3328
References
- 1.Baska M. NHS workforce figures show sector still struggling with chronic staffing shortage. People management, www.peoplemanagement.co.uk/news/articles/nhs-chronic-staffing-shortage (2019, accessed 5 April 2021).
- 2.Propper C, Stoye G, Zaranko B. The wider impacts of the coronavirus pandemic on the NHS. The Institute for Fiscal Studies. IFS Briefing Note BN280, www.ifs.org.uk/publications/14798 (2020, accessed 5 April 2021). [DOI] [PMC free article] [PubMed]
- 3.Vincent L, Brindley P, Highfield J, et al. A national survey of burnout in UK intensive care staff. J Intensive Care Soc 2019; 20: 363–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs 2005; 51: 276–287. [DOI] [PubMed] [Google Scholar]
- 5.Dall'Ora C, Ball J, Reinius M, et al. Burnout in nursing: a theoretical review. Hum Resour Health 2020; 18: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brindley PG, Olusanya S, Wong A, et al. Psychological ‘burnout’ in healthcare professionals: updating our understanding, and not making it worse. J Intensive Care Soc 2019; 20: 358–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meredith N. Levels of stress and burnout of NHS staff during Covid-19 to be examined. University of Surrey Press release, www.surrey.ac.uk/news/levels-stress-and-burnout-nhs-staff-during-covid-19-be-examined (2020, accessed 5 April 2021).
- 8.Doody O, Doody CM. Transformational leadership in nursing practice. Br J Nurs 2012; 21: 1212–1214. [DOI] [PubMed] [Google Scholar]