Abstract
Objective
Health-related stigma is considered a social determinant of health equity and a hidden burden of disease. This study aimed to assess the level and dimensions of stigma and respective coping mechanisms in COVID-19 survivors.
Methods
A mixed-methods study with sequential explanatory design was conducted at the University Hospital of Ulm, Germany. Stigma was assessed using the Social Impact Scale (SIS) including adult COVID-19 survivors with mild-to-severe disease. Subsequently, 14 participants were sampled with regard to gender, age and severity of disease for in-depth interviews to understand how stigma was experienced and coping strategies were applied. The questionnaire was analysed using descriptive statistics, t-test and analysis of variance. Content analysis was used for qualitative data.
Results
From 61 participants, 58% were men and mean age was 51 years. The quantitative analysis of the SIS indicated an intermediate level of experienced stigma. Participants experienced stigma mainly as ‘social rejection’ (M=14.22, SD=4.91), followed by ‘social isolation’ (M=10.17, SD=4.16) and ‘internalised shame’ (M=8.39, SD=3.32). There was no significant difference in experienced stigma regarding gender, education, occupational status or residual symptoms. However, participants between 30 and 39 years of age experienced higher levels of stigma than other age groups (p=0.034). The qualitative analysis revealed how stigma seemed to arise from misconceptions creating irrational fear of infection, leading to stereotyping, vilification, discrimination and social exclusion of COVID-19 survivors, leaving them feeling vulnerable. Stigma cut through all social levels, from the individual level at the bottom to the institutional and societal level at the top. Social networks protected from experiencing stigma.
Conclusion
COVID-19-related stigma is a relevant burden in the ongoing pandemic. Providing accurate information and exposing misinformation on disease prevention and treatment seems key to end COVID-19-related stigma.
Keywords: COVID-19, mental health, social medicine
Strengths and limitations of this study.
Mixed-methods approach to gain an in-depth understanding of COVID-19-related stigma and applied coping strategies.
Detailed list of quotes for every theme to increase transparency, objectivity and traceability.
Telephone interviews instead of face-to-face interviews because of contact regulations.
Single-centre study design.
Lack of a validated instrument particularly designed to assess stigma in COVID-19 survivors.
Introduction
Health-related stigma is a social phenomenon, which implies a negative attitude towards people with a certain condition.1 2 Stigma occurs in different forms3: It can result from assumed attitudes of others (perceived stigma), discriminatory behaviours (enacted stigma), a shift to a devalued self-perception (internalised stigma) and inequities embedded in policies, institutions and social organisations (structural stigma). Regarding health, stigma is often seen as a hidden burden of disease4 and a social determinant of health and health inequity.5 It generates psychological stress6 and causes affected people to hide their condition with severe consequences for their own health, and in case of infectious diseases, for public health.7 In the context of the COVID-19 (coronavirus disease 2019) pandemic, the risk of stigmatisation has been addressed early8–10 and reports of discrimination against patients and survivors have accumulated.11 Across the globe, people infected with or recovered from SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2) became a target of ostracism, humiliation, harassment and even violence. Studies from Pakistan, Uganda, Malaysia, India, China, Ghana, Iran and Brazil found that COVID-19 survivors and even their families were often rejected from social life or essential services and felt humiliated.12–21 COVID-19 survivors were blamed for the disease13 15 16 and perceived as a source of infection even after being cured,12 16 21 22 some reported finical hardship as a consequence.13 19 23 Stereotyping was common,15 especially blaming the poor, labourers and migrants16 or people of seemingly Asian origin.24–26 Research from Malaysia, Iran and Tunisia found that affected people made efforts to hide the infection.15 20 27 Due to stigma, people with suspected COVID-19 might avoid testing or treatment facilities, leading to poor health outcomes and the further spread of the virus.
So far, most studies were conducted in low-income and middle-income countries and little is known about the phenomenon in high-income countries. Labbé et al24 analysed editorial cartoons from Canadian newspapers and found, among others, a stigmatising attitude towards people from certain geographical areas with high SARS-CoV-2 incidence rates. A recent study from Spain using a survey among the general population could demonstrate that discrimination and internalised stigma increased and decreased with the dynamic of the pandemic.28 To the best of our knowledge, no study so far assessed COVID-19-related stigma in survivors from high-income countries. Therefore, our objective was to evaluate the level and dimensions of experienced stigma and applied coping strategies in COVID-19 survivors during the early pandemic in a high-income setting.
Methods
Sampling and data collection
We conducted a sequential explanatory mixed-method study in the area of Ulm, Germany. Every adult with positive SARS-CoV-2-PCR nasopharyngeal swab was included that presented either at the hospital’s outpatient COVID-19 testing centre, the hospital’s emergency room or that was admitted to the hospital between March and May 2020 (n=150). Exclusion criteria were age <18 years and death during hospitalisation. The ‘Social Impact Scale’ (SIS) questionnaire (quantitative methods), a form assessing residual symptoms and socioeconomic factors and a form on which participants could optionally provide a phone number for the phone interviews were sent to the COVID-19 survivors 3–9 months post infectionem. After the quantitative analysis confirmed experienced stigma in COVID-19 survivors, a phenomenological approach was employed using in-depth interviews (qualitative methods) to explore why and how stigma was experienced and to assess possible coping strategies.
Quantitative methods
The ‘Social Impact Scale’ questionnaire
Experienced stigma was assessed with the 24-item SIS questionnaire designed by Fife and Wright29 for people living with HIV/AIDS or cancer and translated to German by Eichhorn et al with good psychometric properties (Cronbach’s α=0.81–0.89).30 We added seven additional COVID-19-related questions (cf online supplemental material 1), which were evaluated separately. On a 4-point Likert scale, participants rate the given statements (items) from ‘I strongly disagree’ to ‘I strongly agree’ (1 to 4 points) resulting in an overall stigma score. These items are assigned to different dimensions of stigma, namely ‘social rejection’ (nine items), ‘internalised shame’ (five items), ‘social isolation’ (seven items) and ‘financial insecurity’ (three items) and are evaluated separately.
bmjopen-2021-059472supp001.pdf (132.2KB, pdf)
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics V.23. Descriptive analyses included demographic information, post-COVID-19 symptoms, the overall level of stigma and its dimensions. Results are reported in means (M) and standard deviation (SD). Univariate analyses were performed assessing differences in experienced stigma regarding gender, age groups, education, occupational status and residual symptoms using t-test, analysis of variance and correlation where appropriate. Missing data were handled by listwise exclusion. A significance level of p<0.05 was considered significant.
Qualitative methods
Sampling and data collection
From those participants consenting to an in-depth interview, we purposefully sampled a broad range with high and low perceived stigma based on the questionnaire, different severity of disease, gender, age and education to gain diverse accounts of the phenomenon. Data were analysed using MAXQDA Plus 2020. The analysis began after the 5th interview and data saturation was reached after the 11th. Three additional interviews were conducted to ensure no new themes emerged, resulting in a total number of 14 interviews. The interviews were held in German, being the native language of the participants, and followed an interview guide (cf online supplemental material 2). However, the interviewer (LP) aimed for an open discussion, allowing the interviewee to determine which topics to focus on. Due to contact regulations, the interviews were conducted by phone and recorded.
Analysis and trustworthiness
After transcription, the analysis was conducted in English, that is, English codes were applied to the German transcripts. Translating the transcripts to English was avoided in order to remain close to the source data and avoid a loss of information. LP used content analysis to develop a preliminary coding scheme from emerging codes and themes (inductive ‘bottom-up’ approach). Coding is the first step in qualitative analysis in which phrases are linked and shapes an idea31–33; thus coding implies computing meaning.34 Subsequently, the interpretation of these rather explicit and descriptive codes generates more latent and subtle subthemes that give a deeper understanding of the phenomenon.35–37 As a final step, overarching themes evolve, which allowed organising the data into a comprehensive framework. To ensure reliability, the coding scheme was subsequently applied to the interviews by SB and BG (deductive ‘top-down’ approach). Deviant codes were discussed within the research team and adjusted (peer-check), resulting in a refined coding scheme. To increase transparency, additional tables with key quotes for each code are attached (cf online supplemental material 3 and 4). Using mixed methods allows for methodological triangulation, that is, assessing the phenomenon from different perspectives.
Patient and public involvement
This research was inspired by patients’ narratives from our post-COVID-19 outpatient department. During follow-up visits, patients moved from physical disorders to social consequences they experienced after having COVID-19, which often involved stigma. The interview guide was informed by those narratives. As mentioned earlier, the interview was designed as an open discussion allowing the participants to prioritise topics and report their experiences freely. However, patients were not involved in designing or recruiting. We aim to offer a lay summary in German on our website to inform participants about the results.
Results
Quantitative results
Descriptive results
In total, 61 questionnaires were analysed which equals a response rate of 41%. The socioeconomic characteristics and residual symptoms are displayed in table 1.
Table 1.
Socioeconomic characteristics and residual symptoms
| Variable | Results (%) | Residual symptoms | N | % | |
| Age | M=51 years (SD=14.6, minimum=18, maximum=78) | Dyspnoea on exertion | 11 | 20.4 | |
| Gender | Male | 58 | Fatigue | 6 | 12.2 |
| Female | 42 | Paraesthesia | 5 | 10.2 | |
| Education | No formal education | 0 | Cough | 4 | 8.2 |
| Lower secondary education, no graduation | 11.5 | Sore throat | 4 | 8.2 | |
| Lower secondary education, graduation | 9.8 | Cephalgia | 4 | 8.2 | |
| Intermediate secondary education | 26.2 | Palpitations | 4 | 8.2 | |
| Upper secondary education | 18.8 | Rhinorrhoea | 3 | 6.1 | |
| High school graduation | 34.4 | Loss of smell and taste | 3 | 6.1 | |
| Occupation | Regularly employed | 70.3 | Diarrhoea | 2 | 4.1 |
| Unemployed/receiving pension | 15.6 | Myalgia | 2 | 4.1 | |
| Student/trainee | 6.3 | Xerophthalmia | 2 | 4.1 | |
| People informed about infection | Close family members | 98.4 | Sleeping disorder | 2 | 4.1 |
| Friends | 95.3 | Loss of hair | 2 | 4.1 | |
| Acquaintances | 81.3 | Lack of attention | 2 | 4.1 | |
| Distant relatives | 78.1 | Mucus | 1 | 2.0 | |
| Close coworkers | 76.6 | Dyspnoea without exertion | 0 | 0 | |
| Neighbours | 73.4 | Fever | 0 | 0 | |
| Superiors | 71.9 | Hearing loss | 0 | 0 | |
| Distant coworkers | 50.0 | Loss of vision | 0 | 0 | |
The Social Impact Scale
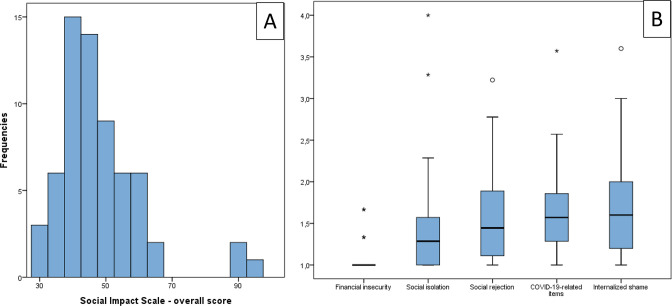
Each of the 31 items (24 SIS items and 7 COVID-19-realted items) was rated with 1–4 points, resulting in a possible total score of 31–124. The total stigma score in our cohort ranged from 31 to 97 with a mean of 48.1 (SD=13.1), and a median of 45.0 (cf figure 1A). Analysing the dimensions of stigma based on the 24 SIS items, ‘internalised shame’ (M=1.68, SD=0.66) and ‘social rejection’ (M=1.58, SD=0.55) showed the highest levels of stigma, followed by ‘social isolation’ (M=1.45, SD=0.59). ‘Financial insecurity’ (M=1.17, SD=0.46) played a minor role (cf figure 1B). The overall mean per item was 1.55 (SD=0.42). Adapted to the original questionnaire,29 we calculated aggregate means: ‘social rejection’ showed the highest aggregate mean (M=14.22, SD=4.91), followed by ‘social isolation’ (M=10.17, SD=4.16) and ‘internalised shame’ (M=8.39, SD=3.32) and, ultimately, financial insecurity (M=3.51, SD=1.38). The data were evenly distributed. Items of special interest are summarised in table 2.
Figure 1.
(A) Social Impact Scale, overall score. (B) Dimensions of stigma. High numbers equal high level of experienced stigma.
Table 2.
Items of special interest from the questionnaire
| Items with the highest experienced stigma: | M |
| ‘I feel others are concerned they could catch my illness.’ | 2.52 |
| ‘I feel guilty because I accidentally might have infected others.’* | 2.03 |
| ‘I feel others think I am to blame for my illness.’ | 2.00 |
| ‘Due to my illness others seem to feel awkward and tense when they are around me.’ | 1.97 |
| ‘I feel institutions and professionals (health authority, healthcare workers) treated me unfairly.’* | 1.81 |
| Items with the lowest experienced stigma: | M |
| ‘I have experienced financial hardship that has affected my relationship with others.’ | 1.08 |
| ‘Some family members have rejected me because of my illness.’ | 1.11 |
| ‘My job security has been affected by my illness.’ | 1.15 |
*Additional COVID-19-related questions.
There was no difference in experienced stigma comparing gender (t59 = 0.437, p=0.664), educational level (F4 = 0.687, p=0.604), occupational status (F3 = 0.995, p=0.404) or residual symptoms (composite score of symptoms) (r46 = −0.250, p=0.093). However, there was a significant difference in age: participants between 30 and 39 years of age experienced higher levels of stigma than other age groups (F6 = 2.499, p=0.034).
Qualitative results
Before conducting the interviews, participants were selected to balance gender, age groups, educational background and severity of disease (cf table 3). Gender distribution and mean age were equivalent to the quantitative results. Participants from the ends of the age range, with different educational level and severity of disease were purposefully sampled.
Table 3.
Characteristics of interviewees and length of interviews
| Gender (N) | Male: 8 | Female: 6 | ||
| Age in years | Mean: 51.8 | Median: 52 | Min: 23 | Max: 77 |
| ISCED* 2011 level of education | Mean: 3.7 | Median: 3 | Min: 2 | Max: 7 |
| Severity of disease (N)† | Ambulatory mild disease: 4 | Hospitalised, moderate disease: 6 | Hospitalised, severe disease: 4 | |
| Length of interview in minutes | Mean: 48 | Median: 41 | Min: 18 | Max: 76 |
*International Standard Classification of Education ranging from 0 (early childhood education) to 8 (doctorate or equivalent).
†According to the WHO classification.59
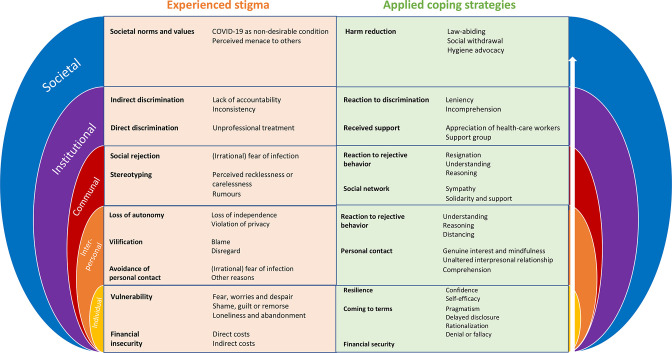
The analytical process revealed how COVID-19 survivors experienced stigma as a multilayered phenomenon: The descriptive codes and latent subthemes generated overarching themes that represent the societal layer in which stigma was experienced and coping strategies were applied. The following section will guide the reader through each layer, starting with the individual layer and continuing to the immediate and then wider environment. The number of times respective codes were applied throughout the interviews is indicated by (n). To keep this report concise, only one exemplary quote for every code is presented. However, we invite the reader to consult the online supplemental materials 3 and 4, which offer additional quotes.
Theme 1: the individual layer
Vulnerability was identified as key subtheme contributing to or resulting from internalised or perceived stigma. Different codes added to increased vulnerability:
Fear, worries and despair (n=11): ‘I was thinking «why me???»… and «I hope this ends well…».’ (female (f), 50–59 year-old (y/o)); most participants were worried about the outcome, especially elderly patients and those referred to the hospital.
Shame, guilt or remorse (n=14): ‘Of course you feel bad knowing you infected others.’ (f, 20–29 y/o); although infecting others happened unwittingly in all cases, participants often felt as active ‘spreader’. This caused feelings of shame and remorse.
Loneliness and abandonment (n=14): ‘Being on my own was the hardest part.’ (male (m), 60–69 y/o); this feeling often rose from the isolation faced in home-quarantine or single hospital rooms, but also from a perceived lack of reliable information regarding the disease.
On the other hand, resilience as coping strategy mitigated the experienced stigma, resulting from:
Confidence (n=5): ‘I knew I was getting medication; I was sure that would help, otherwise they wouldn’t give it to me. I wasn’t worried I would die.’ (m, 60–69 y/o); the elderly putting faith in modern medicine or the young relying on their body’s defences felt confident they would be spared from adverse outcomes.
Self-efficacy (n=2): ‘In the beginning it was very hard for me. But as soon as I managed to structure my day, time just flew by.’ (m, 30–39 y/o); self-efficacy reflects a person’s assumed control over a situation and was identified as a rare but resourceful coping strategy.
Additionally, participants indicated different ways of coming to terms with the undergone infection:
Pragmatism (n=2): ‘I had it [COVID-19], that’s all there is. Now I am cured and immune.’ (f, 70–79 y/o); some refused to dwell in the past and did not make a big deal about having had COVID-19. Interestingly, this also occurred in one participant that had been hospitalised for a few days.
Delayed disclosure (n=3): ‘In the beginning, I didn’t want to share with anyone. Afterwards, we talked about it.’ (f, 70–79 y/o); participants from different age groups and with different severity of disease admitted that they needed some time to process before they were able to confide in someone else.
Rationalisation (n=2): ‘When I was there, it wasn’t known to be a hotspot!’ (m, 50–59 y/o); some participants offered a rationale to justify how they got infected. They emphasised that they did not deliberately put themselves and thereby others at risk.
Denial or fallacy (n=1): ‘Maybe I didn’t have it [COVID-19]. I even know couples, where one had it and the other didn’t.’ (m, 50–59 y/o). One participant doubted the established diagnosis.
Financial insecurity concerned comparatively few self-employed participants. This applied to both direct and indirect costs, the latter resulting from a loss of income:
Direct costs (n=2): ‘If I hadn’t had any savings, it would have been problematic.’ (m, 40–49 y/o);
Indirect costs (n=1): ‘I have to earn my money with physical labour. When I can’t work, I don’t earn money…’ (m, 50–59 y/o).
However, most participants were either employed or received pension and hence costs were covered by their health insurance, implying financial security (n=8): ‘I was on sick leave and got my loan as usual.’ (f, 20–29 y/o);
Theme 2: the interpersonal layer
Used to a certain level of self-determination and a scope of action, most participants were hit hard by the loss of autonomy:
Loss of independence (n=5): ‘We were all isolated, other people had to take care of us.’ (f, 20–29 y/o); Quarantine or being bed-ridden meant depending on others, which was a new situation for many participants.
Violation of privacy (n=4): ‘I live in a small village and within 2 hours, everyone knew about it [COVID-19].’ (f, 20–29 y/o); transgression of personal boundaries or unauthorised passing of personal information left some participants, young and elderly, feeling powerless.
Almost every participant suffered some form of vilification as perceived or enacted stigma:
Blame (n=9): ‘Some people said it is my own fault that I got infected.’ (m, 50–59 y/o). Some patients were made responsible for catching SARS-CoV-2 or blamed for unknowingly infecting others. This reflects a shift in perspective from passively acquiring a disease to actively spreading it. This change from victim to perpetrator was described as particularly hurtful when people had been severely ill from COVID-19.
Disregard (n=4): ‘They [acquaintances] did not really care about what had happened to me.’ (f, 20–29 y/o); lack of concern or misconceptions about what participants were going through left some participants frustrated or angry. This was reported by patients with mild symptoms as well as those hospitalised.
As mentioned earlier, loneliness and abandonment left participants feeling vulnerable. Additional avoidance of personal contact by others when participants were no longer contagious was hence particularly upsetting and by far the most frequently reported form of enacted stigma:
(Irrational) fear of infection (n=27) was presumably the most important driver for the reported behaviour of others: ‘Many people withdrew from me for a long time… I think they were still afraid of getting infected.’ (f, 70–79 y/o).
Participants reported different ways in dealing with the rejective behaviour of others:
Understanding (n=10); most participants could at least partly comprehend and therefore excuse this behaviour: ‘I could totally understand their [friends] behaviour. No one knew exactly how long people can transmit COVID-19.’ (f, 20–29 y/o).
Reasoning (n=2); others tended to argue: ‘When they [friends] took a step back, I told them there was no reason, they could hug me, I am no longer contagious.’ (m, 50–59 y/o).
Distancing (n=2) oneself and avoiding emotional involvement and further frustration: ‘When I heard about what others said, I just distanced myself from that.’ (m, 50–59 y/o).
Consequently, personal contact was much appreciated by all participants and proved one of the most powerful coping strategies:
Genuine interest and mindfulness (n=7) regarding the participants’ well-being were key elements: ‘It’s very important that there are people who care about you and want to know how you are doing. My mum called every day to check on me, that felt good.’ (m, 30–39 y/o).
Unaltered interpersonal relationship (n=4), that is, discovering that ‘nothing had changed’ made participants feel relieved: ‘With my friends, it is the same way as it has been before.’ (m, 30–38 y/o).
Comprehension (n=4): ‘I talked to a friend, and she could totally relate.’ (f, 20–29 y/o). When sharing their stories induced sympathy and comprehension, participants felt that their emotions were acknowledged and legitimate.
Theme 3: the communal layer
The lines between the interpersonal and communal layers are particularly blurry. Thus, codes and subthemes emerging are often similar, yet referring to a different social group. While the interpersonal layer focuses on close personal relationships, the following section refers to more distant contacts or anonymous settings.
Social rejection plays an important role in enacted stigma. Again, a potential driver identified was:
(irrational) fear of infection (n=6): ‘When I did my groceries and kept a 2–3 metres distance, people still told me to go further away… they even changed the side of the street when they saw me.’ (f, 20–29 y/o).
Additionally, stereotyping as perceived stigma was indicated by younger people:
Perceived recklessness or carelessness (n=4): ‘Now you [referring to the interviewer] are probably going to say «how on earth could you go skiing, and how could you go there [place where she got infected]?!?», but back then it wasn’t that obvious…’ (f, 20–29 y/o);
Rumours (n=2): ‘In town, everyone acted like they knew better why I was infected.’ (f, 20–29 y/o).
The reaction to experienced stigma on the communal level included:
Understanding (n=3): ‘I tried to understand their reaction [people at work] and asked myself, how I would have reacted in their place? And honestly, I would keep my distance too. That is probably human.’ (m, 30–39 y/o).
Reasoning (n=2): ‘I told them [people in a grocery store] I am no longer contagious and that they don’t need to keep a 10-metre distance. I fact, I am less dangerous than other people.’ (f, 20–29 y/o).
Resignation (n=3), that is, accepting adverse behaviour without arguing: ‘I didn’t really bother. Couldn’t change it anyway. […] You have to take it the way it is.’ (m, 40–49 y/o).
Social network and inclusion turned out as a valuable resource against experienced stigma:
Sympathy (n=7): ‘So many people called during my absence to make sure I am okay, and they were so happy to hear from me when I called them back.’ (m, 60–69 y/o). For many participants, it was important that others cared about them and felt for them.
Solidarity and support (n=7) from friends or neighbours helped many participants to persevere the isolation and let them rest assured that they would receive help if needed: ‘Many people from our village offered help and asked if they could get us anything. I was surprised by their willingness to help.’ (f, 50–59 y/o).
Theme 4: the institutional layer
Institutional stigma referred to stigma faced in contact with health authorities, hospital staff, general practitioners and paramedics. Actions directed towards individual participants were labelled direct discrimination, a form of enacted stigma. They resulted mainly from
Unprofessional treatment (n=4), which means inappropriate reactions from healthcare workers: ‘Since I was the second patient in that other hospital, they had a lot of «respect» of me and avoided coming close to me… that was even worse for me than the [rejecting] behaviour of other people.’ (f, 20–29 y/o).
Structural stigma was also based on regulations affecting patients infected with COVID-19 in general which was labelled indirect discrimination. Two codes were identified:
Lack of accountability (n=10): In many participant’s views, health authorities and other institutions failed to take responsibility or lacked transparency; ‘They [health authorities] gave us a number where we could call, but no one ever answered the phone.’ (f, 20–29 y/o).
Inconsistency (n=4): Due to contradictory information, participants lost trust in health officials and felt increasingly insecure: ‘They [the health authority] told me on the phone my quarantine ended on Thursday. Then I got the letter from them saying I needed to stay in quarantine for another 2 weeks.’ (m, 50–59 y/o).
At first, many participants’ reaction to this discriminatory behaviour was:
Incomprehension (n=8): ‘I really felt mocked by the health authorities.’ (f, 20–29 y/o); but eventually, in retrospect, they often reacted understandingly and forgivingly, which was labelled
Leniency (n=8): ‘I guess they [the health authorities] were just overwhelmed.’ (m, 50–59 y/o).
Additionally, receiving professional support was much appreciated:
Appreciation of healthcare workers (n=4): ‘He [family doctor] called every day to make sure I was okay. That felt good.’ (f, 70–79 y/o).
Support group (n=2): ‘Is there a self-help group for COVID-19 survivors?’ (m, 50–59 y/o).
Theme 5: the societal layer
This layer characterised societal norms and values which are partly internalised by participants.
First, COVID-19 was seen as a non-desirable condition (n=5) and something usually ‘others’ catch: ‘I was surprised. I never thought we would get it.’ (f, 50–59 y/o).
Second, even if unaware of carrying an infectious virus, participants perceived themselves as a menace to others (n=10) and public health in general. This was the most sensitive subject during the interview:
Question: ‘Do you happen to know if you accidentally infected somebody?’
Answer: ‘I don’t want to talk about that.’ (m, 50–59 y/o).
This led to different reactions, which we subsumed as harm reduction:
Law-abiding (n=5): Participants emphasised that they stuck to the regulations and thereby avoided spreading the disease: ‘When we came back [from a hotspot] we stayed at home. So when we finally knew we had it [COVID-19], at least I didn’t feel guilty, because I knew I didn’t infect anyone else.’ (f, 20–29 y/o).
Social withdrawal (n=3): Others reduced social contacts even after COVID-19 was over, often to avoid rejective behaviour: ‘When my quarantine ended, I didn’t ask people to meet. I was afraid they would react… in a strange way.’ (f, 20–29 y/o).
Hygiene advocacy (n=3): Others propagated hygiene practices as effort to control the disease: ‘I tell everyone they should wear their face masks.’ (f, 70–79 y/o).
Discussion
The social impact of COVID-19 in relation to other stigmatising conditions
Regarding the quantitative results, the overall level of experienced stigma was lower in our cohort compared with people living with HIV/AIDS or cancer in the USA29 or Germany30 (cf table 4). HIV/AIDS is known as a highly stigmatising infection,38 explaining the high level of experienced stigma throughout all dimensions. Comparing our results to people with cancer, ‘social rejection’ and ‘internalised shame’ were similar29 or slightly higher30 in people with COVID-19. We assume that the perceived risk of infecting others with SARS-CoV-2 compared with a non-communicable disease like cancer increases feelings of shame and rejection. In contrast to chronic conditions such as HIV/AIDS and cancer, stigma towards COVID-19 survivors might decrease over time.
Table 4.
Experienced stigma in people living with cancer, HIV/AIDS or after COVID-19
| HIV/AIDS29 (aggregate means) | Cancer29 (aggregate means) | COVID-19 (aggregate means) | Cancer30 (means) | COVID-19 (means) | |
| Social rejection | 19.95 | 14.87 | 14.22 | 1.42 | 1.58 |
| Internalised shame | 13.74 | 8.45 | 8.39 | 1.51 | 1.68 |
| Social isolation | 17.85 | 14.64 | 10.17 | 1.71 | 1.45 |
| Financial insecurity | 8.12 | 5.73 | 3.51 | 1.68 | 1.17 |
| Total score | 59.66 | 43.69 | 36.29 | 1.59 | 1.55 |
Experienced stigma and applied coping strategies from the inner to the outer societal level
On an individual level, factors such as personality, social resources and economic situation, can either enhance or mitigate the impact of stigma. In our cohort, COVID-19-related stigma did usually not culminate in financial hardship, in contrast to other, mainly low-income and middle-income countries.13 16 39 Some participants suffered from a loss of income while being ill, but none reported loss of livelihood or job insecurity.
A sudden illness like COVID-19 resulting in fear of death or infecting others, loneliness and shame generates a feeling of vulnerability, which serves as a breeding ground for experiencing stigma. Vice versa, stigma seems to increase vulnerability, both in this and other studies.6 21 40 41 Hence, COVID-19-related stigma leads to psychological stress and adds to the burden of disease.13 23 40 Loss of autonomy, specifically the violation of privacy, was also observed in other settings.13 39 42 Participants reported that rumours of someone being infected travelled quickly and confidentiality was often breached, even in healthcare facilities. This poses a serious risk for people to hide their condition and refrain from test-seeking or healthcare-seeking, favouring the further spread of the virus.16 In contrast, the individual’s resilience was a valuable source for coping, reflected either by self-confidence or trust in others. In other studies, faith in God strengthened the resilience in COVID-19 survivors.23 43 ‘Coming to terms with the disease’ was described as a way of accepting and adapting, which was similarly found by Gopichandran and Subramaniam39 using the terms ‘understanding disease characteristics, risk acceptance and self-isolation’ and by Bhandari et al43 as ‘accepting reality’. Sharing experiences, often delayed, which is not uncommon after trauma, rationalisation to justify former behaviour and, in one case, denial were other coping strategies observed, similarly to the ‘rationalisation and sharing problems’ Bhandari et al43 described.
On an interpersonal or communal level, stigma was often experienced as vilification including blame, social rejection and stereotyping. Similarly, Gopichandran and Subramaniam39 noticed an exclusion from essential services such as grocery stores and water taps. Jiang et al11 found that 5% of respondents lived in communities that rejected people with COVID-19. Imran et al13 reported social rejection of whole families if one member fell ill. Amir (2020)12 described how patients were treated as outcasts, given bad names and blamed for spreading the disease. Our data suggests that triggers for discriminating of COVID-19 survivors were a general fear of getting infected and noticing presumably irresponsible behaviour of others, often based on misconceptions regarding modes of transmission. Since the virus was perceived as lethal, social rejection seemed reasonable to keep supposedly infectious people at a distance.12 13 16 25 42 In some studies, stigmatising attitudes were linked to experienced vulnerability, poor education and conflicting information in the media,17 22 24 44 pointing out the necessity of careful communication and precise information about COVID-19.28 On the other hand, a strong, solidary social network and sound relationships were valuable resources to cope with stigma.23 39 43 45 This might work in both directions: For those not infected, COVID-19 is not reduced to a faceless, dangerous virus, but connected to a human being.46 This can induce a comprehensive and mindful attitude that prevents stigmatisation and supports those infected. ‘Humanising’ COVID-19 has been insinuated as a way to end stigma, either by involving celebrities or sharing narratives from affected people.15 17 47
Stigma experienced on an institutional level included both direct and indirect discrimination. The former resulted from inappropriate treatment by professionals, such as negligence of patients or compelling them to leave the hospital. Difficulties in accessing healthcare, poor services and negligence were also found in other settings.18 39 40 Indirect discrimination referred to a lack of accountability when health authorities were presumably too overwhelmed to take over responsibility. These experiences elicited either incomprehension or leniency in participants and show the necessity for institutions to be transparent25 and give consistent instructions to preserve people’s confidence and compliance.
On a societal level, health-related stigma is often associated with certain norms and values. For example, people living with HIV/AIDS are often perceived as ‘dirty’ or ‘immoral’48 and some types of cancer are linked to an unhealthy lifestyle or risk behaviour.49 In contrast to those conditions, COVID-19 is an airborne infection with high transmissibility, meaning that one person infects about three others.50 We noticed that COVID-19 survivors often felt like a source of infection, that is, a menace to others and were ashamed and eager to reduce further harm. The findings indicate a change of perspective from passively ‘catching the virus’—as is commonly used in other infections—to actively ‘spreading the virus’, even if this happened unwittingly. The change equals an unprecedented shift within social norms from ‘victim’ to ‘perpetrator’. This public attitude is also reflected in editorial cartoons blaming certain groups or behaviour for the transmission of COVID-19,24 which does not only add to the psychological stress in affected people, but also to a polarisation within society. As a coping strategy, participants reacted with social withdrawal, a strictly law-abiding or hygiene advocating behaviour.
The experienced stigma and applied coping strategies within the respective social layer are depicted as comprehensive framework in figure 2. Stigma experienced at the individual level is shown at the bottom of the framework, followed by the interpersonal, communal, institutional and finally the societal level.
Figure 2.
Comprehensive framework of experienced stigma and applied coping strategies, stratified by societal layer.
Intersectional stigma
As a social phenomenon, stigma can never be assessed detached from other social conditions, often mirroring power differences between groups. Regarding age, most studies about COVID-19-related stigma suggest a higher prevalence among the elderly or patients with comorbidities, since they are most affected by the disease.25 40 47 However, in our study, young to middle-aged participants reported the highest level of experienced stigma. This might result from the shift from ‘victim’ to ‘perpetrator’ mentioned earlier. Those participants who were seriously ill often received sympathy from their social environment and were seen as ‘victims’. In contrast, young people were often asymptomatic and regarded as ‘super-spreaders’51 and drivers of the pandemic. Similarly, a recent study from Israel found negative age-related stereotypes associated with younger people.52 Reports from illegal parties despite the curfew added to a reckless and careless stereotype of young people.53 We assume stereotyping also caused experienced stigma in participants with travel history54: Those coming back from a skiing trip in a hotspot were seen as a major source of the pandemic and perceived as reckless, putting fun above health. Similarly, the patient’s origin was also connected with stigma in other settings, for example, regarding migrant workers in Delhi, India, residing in Haryana.11 16 25 47 However, since all our participants had the same cultural background, we were not able to assess different ethnicities in our cohort. In contrast to other studies, we did not find any difference in gender13 25 40 55 56 or education55–57 regarding experienced stigma. Previous research identified an association between poverty16 39 or occupational status55 and experienced stigma, assuming a mutual influence: COVID-19 is more easily spread in overcrowded, poorer areas; on the other hand, COVID-19 can lead to a loss of livelihood of those infected. We did not collect data on the economic situation, but used the occupational status as a proxy, which revealed no significant difference between the groups. However, this variable might fail to reflect more subtle socioeconomic differences between participants. Similar to Gopichandran and Subramaniam,39 our qualitative data suggested that experienced stigma differs with residential site: participants in more anonymous urban apartments experienced less stigma than those living in rural areas, where residents know each other and word by mouth travels quickly. On the other hand, participants from rural areas also reported more neighbourly support.
Limitations, reflexivity and possible bias
Regarding the quantitative part, a questionnaire designed for people living with HIV/AIDS or cancer was applied in the absence of one specifically designed for experienced stigma in COVID-19 survivors. Since these conditions differ in many ways, the questionnaire used might fail to reflect certain dimensions of COVID-19-related stigma. Moreover, the response rate to the questionnaire was low, probably due to the sensitive nature of the study and the single-centre study design, resulting in a comparatively low quantitative sample size.
Regarding the qualitative part, the interviews were conducted by phone, so physical appearance and body language did not influence the data, in contrast to face-to-face interviews. This can work in both directions: either participants appreciated the more anonymous atmosphere to share private information, or they would have preferred a more personal and intimate setting. Talking to a medical doctor (LP), participants are used to share physical reports rather than social experiences such as stigma. Participants often had the impression that their narratives were inappropriate or not of interest. Although participants were encouraged to share their stories, an expectation bias cannot be excluded. Since stigma is a sensitive topic, it is easily subjected to a social-desirability bias and hence bearing the risk of the respondents’ inclination towards euphemised answers. Furthermore, a recall bias must be considered due to the retrospective character of the study.
Ultimately, those participants who volunteered to be interviewed were mostly of German origin. The requirement of an advanced level of German and the single-centre study design might have limited the diversity of study participants and caused a selection bias, since the sample is unlikely to represent all cultural groups and ethnicities living in Germany.
Conclusion and implications for stakeholders
Around the globe, stigma is a social phenomenon that cuts through all layers of society. It is intertwined with or aggravated by social factors that can lead to ‘othering’ and discrimination. It can limit access to healthcare and other public services and can therefore be seen as a social determinant of health equity and a hidden burden of disease. Stigma arises from perceived careless behaviour and irrational fear of infection, which emerge from misconceptions about the disease. Information about COVID-19 in social media is often incorrect58 or biased24 and people have difficulties finding reliable sources11 to distinguish between fake and fact. In line with previous research,28 we emphasise the need of providing accurate information and exposing misinformation on disease prevention and treatment to end COVID-19-related stigma.
Supplementary Material
Acknowledgments
We thank Michael Krupka for valuable input and continuous support and Métrey Tiv for reviewing the interview guide.
Footnotes
Contributors: Conceptualisation: LP, BG; Methodology: LP; Data acquisition: LP; Initial analysis: LP; Interpretation of data: LP, SB, CB, BG; Writing—original draft: LP; Visualisation: LP; Writing—review and editing: SB, CB, BG; Final approval: LP, SB, CB, BG; Accountability: LP, SB, CB, BG; Guarantor: LP.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. A part of the data are included in the supplementary material and further data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by ethical board of the University of Ulm No. 315/20. Participants gave informed consent to participate in the study before taking part.
References
- 1.Goffman E. Stigma: notes on the management of spoiled identity. New York: Simon & Schuster, Inc, 1963. [Google Scholar]
- 2.AER B, Pryor JB, Reeder GD. Stigma: advances in theory and research. Basic Appl Soc Psych 2013;35:1–9. [Google Scholar]
- 3.MacLean R. Resources to address stigma related to sexuality, substance use and sexually transmitted and blood-borne infections. Can Commun Dis Rep 2018;44:62–7. 10.14745/ccdr.v44i02a05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO . Undefined and Hidden Burden of Mental Health Problems [Internet]. Geneva, 1999. https://books.google.de/books?id=As33jwEACAAJ [Google Scholar]
- 5.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103:813–21. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campo-Arias A, Pedrozo-Pupo JC, Caballero-Domínguez CC. Relation of perceived discrimination with depression, insomnia and post-traumatic stress in COVID-19 survivors. Psychiatry Res 2022;307:114337. 10.1016/j.psychres.2021.114337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stangl AL, Earnshaw VA, Logie CH, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med 2019;17:31. 10.1186/s12916-019-1271-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UNICEF . COVID-19 & stigma: How to prevent and address social stigma in your community | UNICEF Sudan [Internet]. Available: https://www.unicef.org/sudan/covid-19-stigma-how-prevent-and-address-social-stigma-your-community [Accessed 27 Sep 2021].
- 9.Bruns DP, Kraguljac NV, Bruns TR. COVID-19: facts, cultural considerations, and risk of stigmatization. J Transcult Nurs 2020;31:326–32. 10.1177/1043659620917724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li W, Yang Y, Ng CH, et al. Global imperative to combat stigma associated with the coronavirus disease 2019 pandemic. Psychol Med 2021;51:1957–8. 10.1017/S0033291720001993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang T, Lin L, Zhong Y. COVID-19-related stigma and its’ influencing factors: a rapid nationwide study in China, 2020. Available: https://www.researchsquare.com [Accessed 27 Sep 2021]. [DOI] [PMC free article] [PubMed]
- 12.Amir K. COVID-19 and its related stigma: a qualitative study among survivors in Kampala, Uganda. Stigma Heal, 2021. [Google Scholar]
- 13.Imran N, Afzal H, Aamer I, et al. Scarlett letter: a study based on experience of stigma by COVID-19 patients in quarantine. Pak J Med Sci 2020;36:1471–7. 10.12669/pjms.36.7.3606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dye TD, Alcantara L, Siddiqi S, et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open 2020;10:e046620. 10.1136/bmjopen-2020-046620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chii C, Hospital C, Permaisuri R, et al. Experiences of social stigma among patients tested positive for COVID-19 and their family members: a qualitative study, 2021. Available: https://www.researchsquare.com [Accessed 27 Sep 2021]. [DOI] [PMC free article] [PubMed]
- 16.Bhanot D, Singh T, Verma SK, et al. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2021;8:577018. 10.3389/fpubh.2020.577018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y, Jin J, Zhang X, et al. Reducing Objectification could tackle stigma in the COVID-19 pandemic: evidence from China. Front Psychol 2021;12:664422. 10.3389/fpsyg.2021.664422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh S, Bhutani S, Fatima H. Surviving the stigma: lessons learnt for the prevention of COVID-19 stigma and its mental health impact. MHSI 2020;24:145–9. 10.1108/MHSI-05-2020-0030 [DOI] [Google Scholar]
- 19.Guo M, Kong M, Shi W, et al. Listening to COVID-19 survivors: what they need after early discharge from hospital - a qualitative study. Int J Qual Stud Health Well-being 2022;17:2030001. 10.1080/17482631.2022.2030001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toulabi T, Pour FJ, Veiskramian A, et al. Exploring COVID-19 patients' experiences of psychological distress during the disease course: a qualitative study. BMC Psychiatry 2021;21:625. 10.1186/s12888-021-03626-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sousa ARde, Cerqueira SSB, Santana TdaS, et al. Stigma experienced by men diagnosed with COVID-19. Rev Bras Enferm 2021;75Suppl 1:e20210038. 10.1590/0034-7167-2021-0038 [DOI] [PubMed] [Google Scholar]
- 22.Habib MA, Dayyab FM, Iliyasu G, et al. Knowledge, attitude and practice survey of COVID-19 pandemic in northern Nigeria. PLoS One 2021;16:e0245176. 10.1371/journal.pone.0245176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adom D, Mensah JA, Osei M. The psychological distress and mental health disorders from COVID-19 stigmatization in Ghana. Soc Sci Humanit Open 2021;4:100186. 10.1016/j.ssaho.2021.100186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Labbé F, Pelletier C, Bettinger JA, et al. Stigma and blame related to COVID-19 pandemic: a case-study of editorial cartoons in Canada. Soc Sci Med 2022;296:114803. 10.1016/j.socscimed.2022.114803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roelen K, Ackley C, Boyce P, et al. COVID-19 in LMICs: the need to place stigma front and centre to its response. Eur J Dev Res 2020;32:1592–612. 10.1057/s41287-020-00316-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.He J, He L, Zhou W, et al. Discrimination and social exclusion in the outbreak of COVID-19. Int J Environ Res Public Health 2020;17:2933. 10.3390/ijerph17082933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mlouki I, Zammit N, Ghammem R, et al. Validity and reliability of a modified short version of a stigma scale for use among Tunisian COVID‐19 patients after quarantine: a cross‐sectional study. Heal Sci Reports 2022;5:e520. 10.1002/hsr2.520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ugidos C, López-Gómez A, Castellanos Miguel Ángel, et al. Evolution of intersectional perceived discrimination and internalized stigma during COVID-19 lockdown among the general population in Spain. Int J Soc Psychiatry 2022;68:55–63. 10.1177/0020764020975802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav 2000;41:50–67. 10.2307/2676360 [DOI] [PubMed] [Google Scholar]
- 30.Eichhorn S, Mehnert A, Stephan M. [German Version of the Social Impact Scale (SIS-D)--Pilot Testing of an Instrument for Measuring Experienced Stigmatization in a Sample of Cancer Patients]. Psychother Psychosom Med Psychol 2015;65:183–90. 10.1055/s-0034-1398523 [DOI] [PubMed] [Google Scholar]
- 31.Miles MB, Huberman A. An expanded sourcebook: Qualitative data analysis. In: Miles MB, Huberman AM, eds. Sage publications. 2nd edn. London: SAGE Publications, 1994: 56–7. [Google Scholar]
- 32.Richards L, Morse JM, Richards C. README FIRST for a User’s Guide to Qualitative Methods, 2007: 135–8. [Google Scholar]
- 33.Grbich C. Qualitative data analysis : an introduction. SAGE Publications, 2007: 21–2. [Google Scholar]
- 34.Dey I. Grounding grounded theory : guidelines for qualitative inquiry. Academic Press, 1999: 95. [Google Scholar]
- 35.Rossman GB, Rallis SF. An introduction to qualitative research: learning in the field. An Introd to Qual Res Learn F 2020. [Google Scholar]
- 36.Charmaz K. Constructing Grounded theory: a practical guide through qualitative analysis. SAGE Publications, 2006. [Google Scholar]
- 37.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 2004;24:105–12. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 38.Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS 2008;22 Suppl 2:S67–79. 10.1097/01.aids.0000327438.13291.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gopichandran V, Subramaniam S. A qualitative inquiry into stigma among patients with Covid-19 in Chennai, India. Indian J Med Ethics 2021;VI:193–201. 10.20529/IJME.2021.013 [DOI] [PubMed] [Google Scholar]
- 40.Li J, Liang W, Yuan B, et al. Internalized stigmatization, social support, and individual mental health problems in the public health crisis. Int J Environ Res Public Health 2020;17:4507–14. 10.3390/ijerph17124507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sahoo S, Mehra A, Suri V, et al. Lived experiences of the corona survivors (patients admitted in COVID wards): a narrative real-life documented summaries of internalized guilt, shame, stigma, anger. Asian J Psychiatr 2020;53:102187. 10.1016/j.ajp.2020.102187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Son H-M, Choi W-H, Hwang Y-H, et al. The lived experiences of COVID-19 patients in South Korea: a qualitative study. Int J Environ Res Public Health 2021;18:7419. 10.3390/ijerph18147419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhandari S, Khakha DC, Kumar TKA, et al. "I might catch this infection again and this time I will not survive" - A qualitative study on lived-in experiences and coping strategies of COVID-19-positive individuals in India. Indian J Psychiatry 2021;63:560–7. 10.4103/indianjpsychiatry.indianjpsychiatry_196_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moradi Y, Mollazadeh F, Karimi P, et al. Psychological disturbances of survivors throughout COVID-19 crisis: a qualitative study. BMC Psychiatry 2020;20:594. 10.1186/s12888-020-03009-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med 2006;11:353–63. 10.1080/13548500600595327 [DOI] [PubMed] [Google Scholar]
- 46.Logie CH. Lessons learned from HIV can inform our approach to COVID-19 stigma. J Int AIDS Soc 2020;23:e25504. 10.1002/jia2.25504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Asadi-Aliabadi M, Tehrani-Banihashemi A, Moradi-Lakeh M. Stigma in COVID-19: a barrier to seek medical care and family support. Med J Islam Repub Iran 2020;34:98. 10.47176/mjiri.34.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Logie CH, James L, Tharao W, et al. Hiv, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med 2011;8:e1001124. 10.1371/journal.pmed.1001124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: qualitative study. BMJ 2004;328:1470–3. 10.1136/bmj.38111.639734.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.D'Arienzo M, Coniglio A. Assessment of the SARS-CoV-2 basic reproduction number, R0, based on the early phase of COVID-19 outbreak in Italy. Biosaf Health 2020;2:57–9. 10.1016/j.bsheal.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lewis D. Superspreading drives the COVID pandemic - and could help to tame it. Nature 2021;590:544–6. 10.1038/d41586-021-00460-x [DOI] [PubMed] [Google Scholar]
- 52.Werner P, AboJabel H, Tur-Sinai A. Ageism towards older and younger people in the wake of the COVID-19 outbreak. Maturitas 2022;157:1–6. 10.1016/j.maturitas.2021.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Germany: Hamburg police clear neighborhood after thousands show up to party | News | DW | 30.05.2021 [Internet]. Available: https://www.dw.com/en/germany-hamburg-police-clear-neighborhood-after-thousands-show-up-to-party/a-57717566 [Accessed 27 Sep 2021].
- 54.The Guardian . Everyone was drenched in the virus’: was this Austrian ski resort a Covid-19 ground zero? | Coronavirus. Available: https://www.theguardian.com/world/2020/sep/05/everyone-was-drenched-in-the-virus-was-this-austrian-ski-resort-a-covid-19-ground-zero [Accessed 27 Sep 2021].
- 55.Yuan Y, Zhao Y-J, Zhang Q-E, et al. COVID-19-related stigma and its sociodemographic correlates: a comparative study. Global Health 2021;17:54. 10.1186/s12992-021-00705-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dar SA, Khurshid SQ, Wani ZA, et al. Stigma in coronavirus disease-19 survivors in Kashmir, India: a cross-sectional exploratory study. PLoS One 2020;15:e0240152. 10.1371/journal.pone.0240152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Almoayad F, Mahboub S, Amer LB, et al. Stigmatisation of COVID-19 in Riyadh, Saudi Arabia: a cross-sectional study. Sultan Qaboos Univ Med J 2021;21:525–31. 10.18295/squmj.4.2021.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li HO-Y, Bailey A, Huynh D, et al. Youtube as a source of information on COVID-19: a pandemic of misinformation? BMJ Glob Health 2020;5:e002604. 10.1136/bmjgh-2020-002604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Marshall JC, Murthy S, Diaz J, et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis 2020;20:e192–7. 10.1016/S1473-3099(20)30483-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059472supp001.pdf (132.2KB, pdf)
Data Availability Statement
Data are available upon reasonable request. A part of the data are included in the supplementary material and further data are available upon reasonable request.