Abstract
Countries worldwide have deployed mass COVID-19 vaccination drives, but there are people who are hesitant to receive the vaccine. Studies assessing the factors associated with COVID-19 vaccination hesitancy are inconclusive. This study aimed to assess the global prevalence of COVID-19 vaccination hesitancy and determine the potential factors associated with such hesitancy. We performed an organized search for relevant articles in PubMed, Scopus, and Web of Science. Extraction of the required information was performed for each study. A single-arm meta-analysis was performed to determine the global prevalence of COVID-19 vaccination hesitancy; the potential factors related to vaccine hesitancy were analyzed using a Z-test. A total of 56 articles were included in our analysis. We found that the global prevalence of COVID-19 vaccination hesitancy was 25%. Being a woman, being a 50-year-old or younger, being single, being unemployed, living in a household with five or more individuals, having an educational attainment lower than an undergraduate degree, having a non-healthcare-related job and considering COVID-19 vaccines to be unsafe were associated with a higher risk of vaccination hesitancy. In contrast, living with children at home, maintaining physical distancing norms, having ever tested for COVID-19, and having a history of influenza vaccination in the past few years were associated with a lower risk of hesitancy to COVID-19 vaccination. Our study provides valuable information on COVID-19 vaccination hesitancy, and we recommend special interventions in the sub-populations with increased risk to reduce COVID-19 vaccine hesitancy.
Keywords: COVID-19, vaccination, hesitancy, acceptance, prevalence
1. Introduction
Coronavirus disease 2019 (COVID-19) vaccination has been progressing globally since the beginning of 2021. Several types of vaccines, including inactivated, vector-based, messenger ribonucleic acid (mRNA), and protein subunit vaccines, are being administered to recipients [1]. Since the vaccines became available, there have been expectations of the COVID-19 pandemic ending, considering that previous vaccination programs have been effective in managing several infectious diseases such as rubella, mumps, measles, and polio. These vaccination programs have been proven to improve global health and the economy [2,3]. However, the probability of failure of any vaccination program should be assessed. A study reported that the barriers to effective vaccination programs include inconvenient and limited clinic hours for immunization, inadequate access to healthcare, high vaccine administration fees, and vaccine hesitancy [4]. Of these factors, vaccine hesitancy is considered one of the most critical [5]. Individuals who are hesitant to be immunized have a tendency to spread incorrect information about vaccination, which may influence people close to them to reject vaccines as well [6].
Vaccine hesitancy is commonly observed in the case of new vaccines or vaccine candidates [7,8]. This phenomenon was reported in the case of malaria [9], dengue [10], and Ebola [11]. The factors contributing to vaccine hesitancy are complex and may include a lack of awareness regarding disease prevention and socioeconomic status [12,13]. This phenomenon poses a dilemma to vaccine coverage. Moreover, governments—as the highest regulatory authority of any nation—seemingly do not provide special interventions to reduce hesitancy toward vaccination programs. It is observed in the guidelines on COVID-19 vaccination, that the primary recommendation only focused on dose allocation, outreach, delivery, and monitoring; there was no information on how to reduce COVID-19 vaccination hesitancy [14].
Regarding COVID-19 vaccination, several studies have been conducted to assess the prevalence of COVID-19 vaccine hesitancy and its associated predictors [7,8,15]. However, the findings were inconclusive with variability regarding the correlation between COVID-19 vaccine acceptance and the following: sociodemographic factors, vaccine confidence and trust regarding vaccine safety, complacency towards the disease, conspiracy beliefs towards COVID-19 vaccination and willingness to pay for the vaccine [7,16,17,18,19,20,21]. Therefore, a meta-analysis is necessary to determine the potential factors influencing COVID-19 vaccination hesitancy.
2. Materials and Methods
2.1. Study Design
During the period May–June 2022, we conducted a meta-analysis that followed the protocols of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) [22,23]. In line with the purpose of our study, we first performed an organized search of PubMed, Scopus, and Web of Science and, subsequently, collected the required information to calculate the global prevalence of vaccine hesitancy and effect estimates of the potential influencing factors. The PRISMA checklist for this review is provided in (Supplementary Materials). Additionally, data used in this review are available in Figshare (https://doi.org/10.6084/m9.figshare.20055539.v3, accessed on 6 December 2022) [23].
2.2. Eligibility Criteria
We determined the eligibility criteria before conducting the organized search. An article was included in the analysis if the following inclusion criteria were met: (1) whether it assessed the prevalence of COVID-19 vaccination hesitancy or (2) identified potential factors influencing COVID-19 vaccination hesitancy. Reviews, commentaries, letters to the editor, grey literature, and double publications were excluded.
2.3. Search Strategy and Data Extraction
As of 25 May 2022, we performed an organized search of PubMed, Scopus, and Web of Science. Prior to the search for the main outcomes, the potential factors associated with COVID-19 vaccination hesitancy were determined. We used keywords from the following medical subject headings: “vaccine”, “vaccination”, or “immunization”; “COVID-19” or “coronavirus disease 2019”; “hesitancy” or “acceptance”. We limited the organized search to the English language. If we found any duplication, we included the studies with larger sample sizes. Furthermore, we also conducted an organized search of the reference lists of the relevant articles to obtain additional papers. Thereupon, the following information was collected from the selected articles: (1) first author name, (2) year of publication, (3) study design, (4) study period, (5) Newcastle–Ottawa scale (NOS), (6) the prevalence of COVID-19 vaccination hesitancy, and (7) event rate of potential factors associated with COVID-19 vaccination hesitancy. Two independent teams, led by JKF and SAPK, conducted the article search and data extraction. Prior to the systematic search, the kappa statistic was used to measure the agreement between the two investigators. If the kappa statistic was greater than the p-value, agreement was established.
2.4. Assessment of the Methodological Quality
All potential articles for inclusion in the study were assessed for quality using NOS [24]. The quality was considered high, moderate, or low if the score was 7–9, 4–6, or 0–3, respectively. Low-quality articles were excluded from the analysis. Using a pilot form, the two independent teams, led by JKF and SAPK, conducted the NOS assessment, and any discrepancies were resolved through discussion.
2.5. Outcome Measures
The major outcomes were global prevalence and potential influencing factors of COVID-19 vaccination hesitancy. To identify the potential factors associated with vaccine hesitancy, we performed an initial organized search in PubMed, Scopus, and Web of Science. We identified the following potential factors: age group, gender, marital status, educational attainment, religion, employment status, healthcare-related job, socioeconomic status, urbanity, presence of children and elderly people at home, household size, and presence of family members with a medical background. Additionally, wearing masks, hand hygiene, compliance with physical distancing norms, smoking, history of chronic disease, personal history of COVID-19 diagnosis, COVID-19 diagnosis of a family member/friend, hospitalization due to COVID-19 among people in the same social circle, death owing to COVID-19 among people in the same social circle, safety conceptions about COVID-19 vaccines, and history of influenza vaccination in the past few years were also factors of interest.
2.6. Statistical Analysis
Before calculating the global prevalence of COVID-19 vaccination hesitancy and effect estimates of potential predictors of such hesitancy, we conducted an analysis of potential publication bias and heterogeneity among the studies. We analyzed the risk of publication bias using the Egger’s test, with a p-value of <0.05 suggesting the existence of publication bias. Furthermore, we performed an analysis of heterogeneity among studies using the Q test, with a p-value of <0.10 indicating heterogeneity; thus, a random effects model was applied for data analysis—in cases where there was no heterogeneity, a fixed-effects model was used. A single-arm meta-analysis was performed using the dichotomous covariate method to calculate the event rate from each study to discern the global prevalence of COVID-19 vaccination hesitancy. The effect estimate was presented as the event rate. The analysis was performed using the R package (RStudio version 4.1.1, R Studio, Boston, MA, USA). The effect estimates of potential factors associated with COVID-19 vaccination hesitancy were outlined in a forest plot as a pooled odds ratio and 95% confidence interval (OR, 95% CI).
3. Results
3.1. Selection of Studies
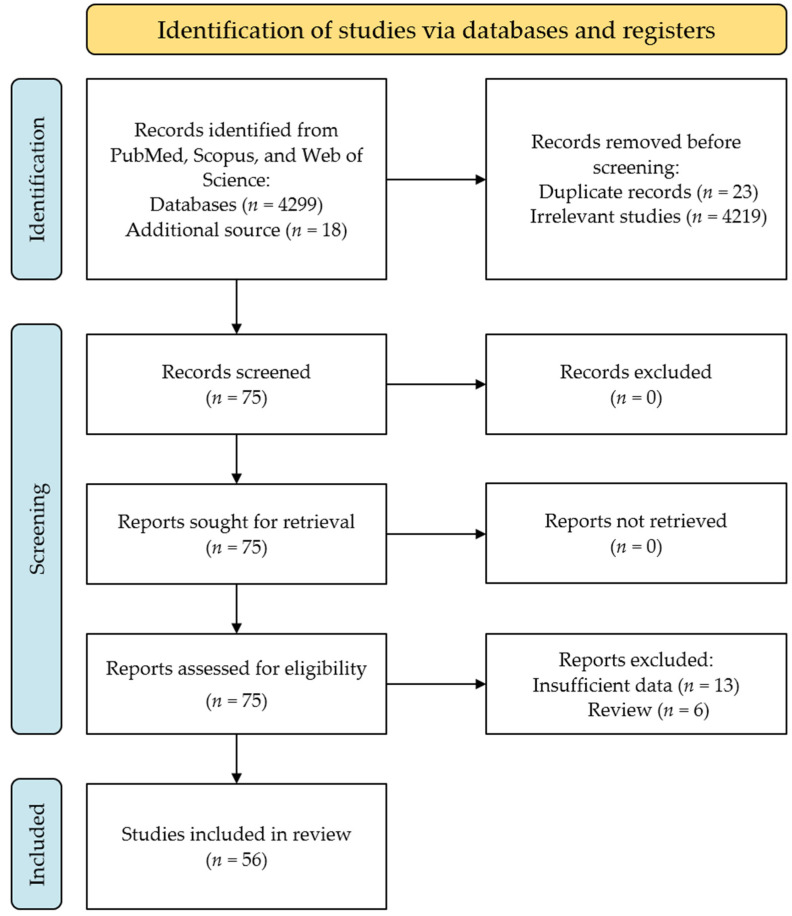
We retrieved 4299 potential papers from the databases mentioned and 18 from the reference lists of related articles. Of these, 23 papers were excluded owing to duplication and 4219 papers with irrelevant subjects. Thus, 75 articles were included in the full-text review. Subsequently, six reviews and thirteen articles were excluded because of insufficient data. Eventually, a total of 56 articles were included in the final analysis to calculate the global prevalence and potential influencing factors in COVID-19 vaccination hesitancy [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79]. The plotting of article selection in our study is presented in (Figure 1), and the characteristics of the included articles are listed in (Table 1).
Figure 1.
A flowchart of article selection in this review.
Table 1.
Baseline characteristics of articles included in our analysis [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
| Author and Year | Country | Sample Size | Study Period | Population | Funding | NOS 1 |
|---|---|---|---|---|---|---|
| Aemro et al., 2021 [25] | Ethiopia | 418 | May–June 2021 | Healthcare workers | No funding | 5 |
| Ali et al., 2021 [26] | Bangladesh | 1134 | January 2021 | General population | No funding | 6 |
| Barry et al., 2021 [27] | Saudi Arabia | 1512 | November 2020 | Healthcare workers | No funding | 6 |
| Bell et al., 2020 [28] | England | 1252 | April–May 2020 | General population | London School of Hygiene and Tropical Medicine | 6 |
| Chen et al., 2021 [29] | China | 2531 | January 2021 | General population | NA | 7 |
| Chudasama et al., 2022 [30] | Multinational | 275 | April–July 2021 | Healthcare workers | NA | 6 |
| Detoc et al., 2020 [31] | France | 3259 | March–April 2020 | General population | NA | 5 |
| Dong et al., 2020 [32] | China | 1236 | June–July 2020 | General population | Chinese University of Hong Kong | 6 |
| Dror et al., 2020 [33] | Israel | 1661 | 2020–2022 | Healthcare workers | NA | 5 |
| Faasse et al., 2020 [34] | Australia | 2232 | March 2020 | General population | UNSW Science Goldstar (2020) | 5 |
| Fisher et al., 2020 [35] | US | 991 | April 2020 | General population | Agency for Healthcare Research and Quality | 7 |
| Goodwin et al., 2022 [36] | Multinational | 3059 | December 2020–January 2021 | General population | Ariel University, JSPS KAKENSHI, Hungaria National Excellence Program | 6 |
| Habib et al., 2022 [37] | Saudi Arabia | 1445 | August–October 2021 | Students | King Saud University | 7 |
| Bou Hamdan et al., 2021 [38] | Lebanon | 758 | May–June 2021 | Students | No funding | 7 |
| Harapan et al., 2020 [39] | Indonesia | 1359 | March–April 2020 | General population | No funding | 6 |
| Horiuchi et al., 2021 [40] | Japan | 1200 | May–June 2021 | General population | No funding | 7 |
| Hossain et al., 2021 [41] | Bangladesh | 1497 | February 2021 | General population | No funding | 6 |
| Huang et al., 2022 [42] | China | 4227 | January–March 2021 | General population | National Health Commission of the People’s Republic of China | 7 |
| Ikiisik et al., 2021 [43] | Turkey | 384 | December 2020 | General population | NA | 7 |
| Jabessa et al., 2022 [44] | Ethiopia | 350 | August–September 2021 | General population | No funding | 6 |
| Jain et al., 2021 [45] | India | 1068 | February–March 2021 | Students | No funding | 6 |
| Kelekar et al., 2021 [46] | US | 408 | September–December 2020 | Students | NA | 6 |
| Khubchandani et al., 2021 [47] | US | 1878 | June 2020 | General population | No funding | 8 |
| Koh et al., 2022 [48] | Singapore | 528 | May–June 2021 | Healthcare workers | No funding | 6 |
| Kumar et al., 2021 [49] | Qatar | 1414 | October–November 2020 | Healthcare workers | Qatar National Library | 5 |
| Lazarus et al., 2020 [50] | Multinational | 13,426 | June 2020 | General population | City University of New York | 6 |
| Lee et al., 2022 [51] | South Korea | 1016 | January 2021 | General population | No funding | 6 |
| Li et al., 2022 [52] | China | 721 | June 2021 | Students | Xuzhou Medical University | 7 |
| Liddell et al., 2021 [53] | Australia | 437 | June 2021 | General population | UNSW Sydney/Australian Red Cross | 6 |
| Lucia et al., 2021 [54] | US | 167 | NA | Students | No funding | 5 |
| Malik et al., 2020 [55] | US | 672 | May 2020 | General population | Yale Institute for Global Health | 8 |
| Marzo et al., 2022 [56] | Multinational | 5260 | February–May 2021 | General population | No funding | 7 |
| Mascarenhas et al., 2021 [57] | US | 245 | 2020 | Students | No funding | 6 |
| Mohammed et al., 2021 [58] | Ethiopia | 614 | March–July 2021 | Healthcare workers | No funding | 7 |
| Mose et al., 2022 [59] | Ethiopia | 420 | March 2021 | Students | No funding | 6 |
| Nery et al., 2022 [60] | Brazil | 2537 | November 2020–January 2021 | General population | Brazilian Ministry of Health | 8 |
| Neumann-Böhme et al., 2020 [61] | Multinational | 7664 | April 2020 | General population | European Union’s Horizon 2020 research and innovation programme | 6 |
| Ousseine et al., 2022 [62] | France | 15,427 | February–April 2021 | General population | National Agency for Research on AIDS and Viral Hepatitis (ANRS) | 6 |
| Patwary et al., 2021 [19] | Bangladesh | 543 | July–August 2021 | General population | No funding | 6 |
| Qunaibi et al., 2021 [63] | Multinational | 36,220 | January 2021 | General population | No funding | 7 |
| Raja et al., 2022 [64] | Sudan | 217 | June–July 2021 | Students | No funding | 5 |
| Reiter et al., 2020 [65] | US | 2006 | May 2020 | General population | National Center for Advancing Translational Sciences | 7 |
| Rodríguez-Blanco et al., 2021 [66] | Spain | 2494 | November–December 2020 | General population | No funding | 6 |
| Saied et al., 2021 [67] | Egypt | 2133 | January 2021 | Students | NA | 7 |
| Salali et al., 2020 [68] | Multinational | 5024 | May 2020 | General population | No funding | 6 |
| Schwarzinger et al., 2021 [69] | France | 1942 | July 2020 | General population | French Public Health Agency | 7 |
| Shah et al., 2021 [70] | India | 274 | February 2021 | Students | NA | 7 |
| Singh et al., 2021 [71] | Hong Kong | 245 | May 2021 | General population | Tung Foundation | 7 |
| Tao et al., 2021 [72] | China | 1392 | November 2020 | General population | National Key Research and Development Project of China | 7 |
| Tlale et al., 2022 [73] | Botswana | 4952 | February 2021 | General population | No funding | 6 |
| Wang et al., 2020 [74] | Hong Kong | 806 | February–March 2020 | Healthcare workers | No funding | 6 |
| Ward et al., 2020 [75] | France | 5018 | April 2020 | General population | Agence Nationale de la Recheche and the CNRS | 8 |
| Wong et al., 2020 [76] | Malaysia | 1159 | April 2020 | General population | Ministry of Education Malaysia | 8 |
| Wu et al., 2021 [77] | China | 29,925 | August 2021 | General population | National Social Science Fund of China | 7 |
| Xu et al., 2021 [78] | China | 5247 | January 2021 | Healthcare workers | Health Commission of Chongqing municipal, China | 6 |
| Yassin et al., 2022 [79] | Sudan | 365 | April 2021 | Healthcare workers | NA | 6 |
1 NOS: Newcastle–Ottawa scale; all selected studies were based on a cross-sectional design.
3.2. Global Prevalence of COVID-19 Vaccination Hesitancy
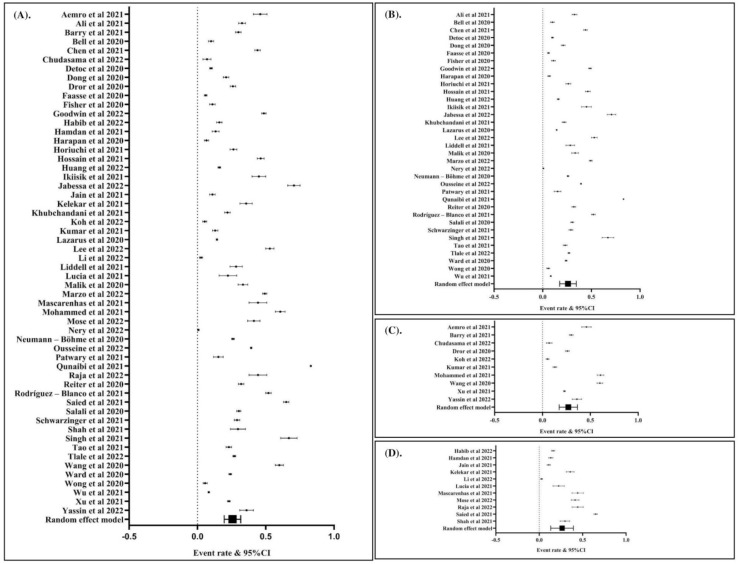
To calculate the global prevalence of COVID-19 vaccination hesitancy, we included a total of 56 articles. Data analysis using the random effects model revealed that the global prevalence was 25% (event rate: 0.25; 95% CI: 0.19, 0.32; p Egger’s: 1.2710; p heterogeneity: <0.0001; p < 0.0001). The global prevalence of COVID-19 vaccination hesitancy is presented in (Figure 2A). In sub-group analysis, we found that the prevalence of COVID-19 vaccination hesitancy in the general population (Figure 2B), healthcare workers (Figure 2C), and students (Figure 2D) was 25%, 26%, and 25%, respectively.
Figure 2.
The global prevalence of hesitancy to COVID-19 vaccination (event rate: 0.25; 95% CI: 0.20, 0.32; p Egger: 1.2580; p heterogeneity: <0.0001; p: <0.0001) (A). The prevalence of hesitancy to COVID-19 vaccination among general population (event rate: 0.25; 95% CI: 0.18, 0.34; p Egger: 1.3090; p heterogeneity: <0.0001; p: <0.0001) (B). The prevalence of hesitancy to COVID-19 vaccination among healthcare workers (event rate: 0.26; 95% CI: 0.18, 0.37; p Egger: 0.7670; p heterogeneity: <0.0001; p: <0.0001) (C). The prevalence of hesitancy to COVID-19 vaccination among students (event rate: 0.25; 95% CI: 0.14, 0.40; p Egger: 1.2090; p heterogeneity: <0.0001; p: 0.0030) (D). The studies included are provided in the reference list [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
3.3. Potential Factors Associated with COVID-19 Vaccination Hesitancy
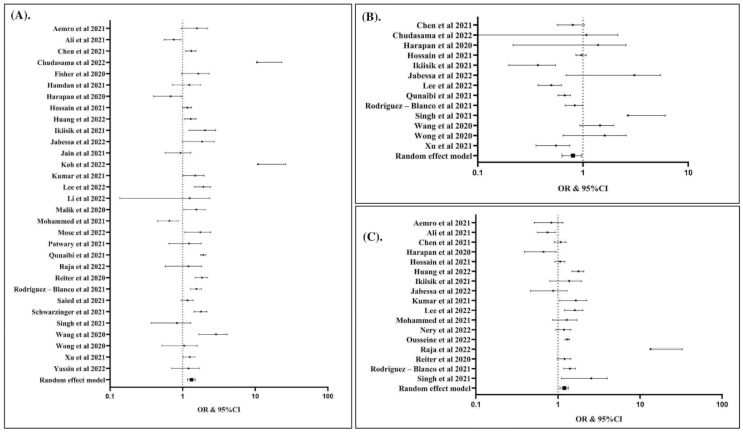
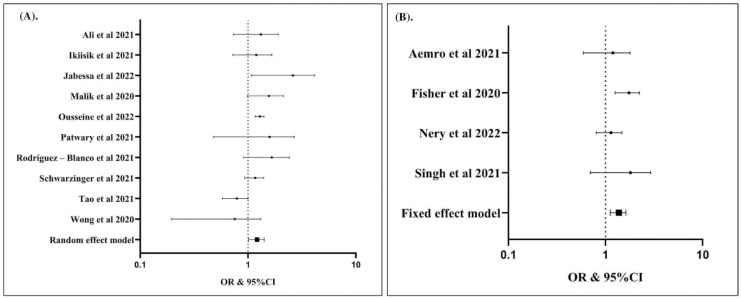
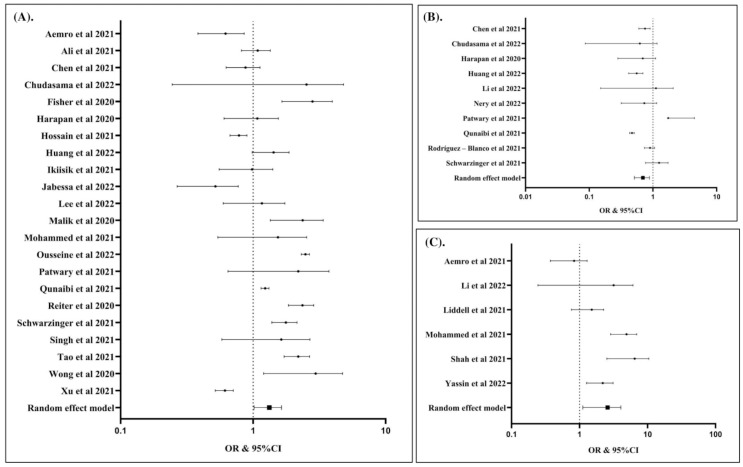
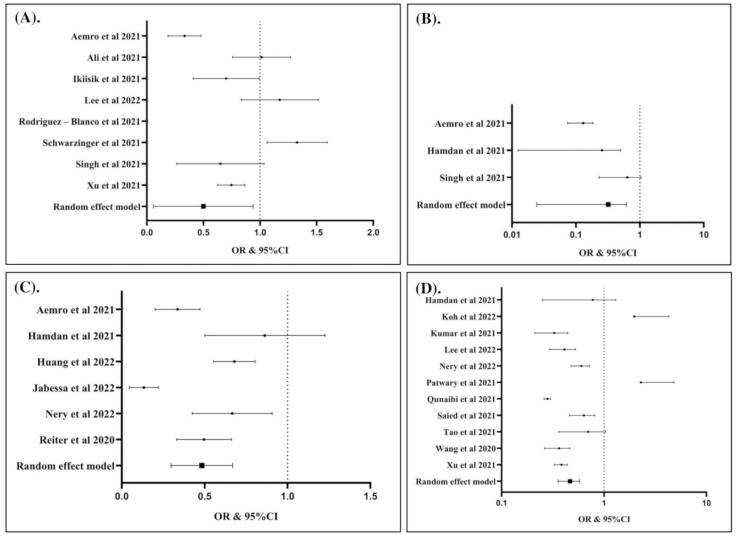
The potential factors associated with COVID-19 vaccination hesitancy are summarized in (Table 2) and presented in (Figure 3, Figure 4, Figure 5 and Figure 6). Our analysis revealed that out of 25 factors, 12 of them were associated with COVID-19 vaccine hesitancy. The following factors were associated with a higher risk of vaccination hesitancy: being a woman (compared to man) (Figure 3A), being ≤50 years old (compared to those older than 50 years (Figure 3B), being single (compared to married individuals) (Figure 3C), being unemployed (compared to employed) (Figure 4A), living in a household with five or more individuals (compared to living in smaller households) (Figure 4B), having an educational attainment lower than an undergraduate degree (compared to those with an undergraduate degree or higher) (Figure 5A), having a non-healthcare-related job (compared to having a healthcare-related job) (Figure 5B), and considering COVID-19 vaccines to be unsafe (compared to those who consider COVID-19 vaccines to be safe) (Figure 5C).
Table 2.
The potential factors associated with the hesitancy to COVID-19 vaccination.
| Covariates | Hesitancy/Total (n [%]) | NS | p Egger | p Het | OR | 95% CI | p |
|---|---|---|---|---|---|---|---|
| Age group (years) | |||||||
| ≤30 | 6568/14,356 [45.8] | 16 | 0.2320 | <0.0001 | 1.14 | 0.98–1.32 | 0.0870 |
| 31–40 | 5097/11,335 [45.0] | 16 | 0.2360 | <0.0001 | 1.09 | 0.94–1.26 | 0.2630 |
| 41–50 | 3034/6536 [46.4] | 15 | 0.2730 | <0.0001 | 0.88 | 0.74–1.06 | 0.1760 |
| >50 | 2034/4677 [43.5] | 13 | 0.2980 | <0.0001 | 0.79 | 0.64–0.98 | 0.0290 |
| Sex | |||||||
| Male | 8934/22,362 [40.0] | 31 | 0.2840 | <0.0001 | 0.76 | 0.67–0.85 | <0.0001 |
| Female | 11,170/28,707 [38.9] | 31 | 0.2840 | <0.0001 | 1.32 | 1.17–1.49 | <0.0001 |
| Marital status | |||||||
| Married | 6888/20,496 [33.6] | 17 | 0.1950 | <0.0001 | 0.84 | 0.75–0.95 | 0.0040 |
| Single | 7173/18,764 [38.2] | 17 | 0.1950 | <0.0001 | 1.19 | 1.06–1.34 | 0.0040 |
| Educational attainment | |||||||
| <BSC | 12,130/22,950 [52.9] | 22 | 0.5260 | <0.0001 | 1.30 | 1.03–1.65 | 0.0300 |
| ≥BSC | 17,532/41,182 [42.6] | 22 | 0.5260 | <0.0001 | 0.77 | 0.61–0.97 | 0.0300 |
| Religion | |||||||
| Christian | 1053/2124 [49.6] | 5 | <0.0001 | 0.4380 | 1.17 | 1.01–1.35 | 0.0340 |
| Muslim | 1265/3961 [31.9] | 6 | 0.5110 | <0.0001 | 1.39 | 0.85–2.26 | 0.1860 |
| Hindu | 16/129 [12.4] | 2 | 1.5700 | 0.0710 | 0.28 | 0.02–3.40 | 0.3150 |
| Employment | |||||||
| Not working | 1704/4455 [38.2] | 10 | 0.1790 | 0.0090 | 1.20 | 1.02–1.42 | 0.0300 |
| Working | 5883/16,413 [35.8] | 10 | 0.1790 | 0.0090 | 0.83 | 0.71–0.98 | 0.0300 |
| Healthcare-related job | 2886/8313 [34.7] | 10 | 0.3340 | <0.0001 | 0.68 | 0.52–0.89 | 0.0040 |
| Socioeconomic status | |||||||
| Low income | 1320/2939 [44.9] | 7 | 0.4840 | <0.0001 | 1.31 | 0.88–1.94 | 0.1790 |
| Middle income | 1217/3220 [37.8] | 7 | 1.2050 | <0.0001 | 0.61 | 0.25–1.52 | 0.2900 |
| High income | 1427/2515 [56.7] | 7 | 1.2860 | <0.0001 | 1.28 | 0.49–3.38 | 0.6140 |
| Urbanicity | |||||||
| Urban | 9192/28,583 [32.2] | 15 | 0.4500 | <0.0001 | 0.92 | 0.72–1.18 | 0.5070 |
| Rural | 3128/8338 [37.5] | 15 | 0.4500 | <0.0001 | 1.09 | 0.85–1.39 | 0.5070 |
| Children at home | 1207/4595 [26.3] | 8 | 1.4040 | <0.0001 | 0.37 | 0.14–0.99 | 0.0490 |
| Aged people at home | 456/1542 [29.6] | 5 | 0.2760 | 0.0140 | 1.07 | 0.78–1.45 | 0.6920 |
| Household number (n) | |||||||
| ≤2 | 930/3192 [29.1] | 5 | 0.3900 | <0.0001 | 0.94 | 0.64–1.36 | 0.7270 |
| 3–4 | 564/2067 [27.3] | 5 | 0.2290 | 0.0110 | 0.89 | 0.69–1.14 | 0.3510 |
| ≥5 | 278/712 [39.0] | 4 | 0.1680 | 0.1620 | 1.36 | 1.13–1.63 | 0.0010 |
| Family members with medical backgrounds | 464/1382 [33.6] | 2 | 0.0410 | 0.3170 | 0.92 | 0.78–1.07 | 0.2770 |
| Wearing masks all the time | 1523/6606 [23.1] | 6 | 0.5570 | <0.0001 | 0.61 | 0.36–1.05 | 0.0720 |
| Constantly washing hands | 1209/4974 [24.3] | 4 | 0.8900 | <0.0001 | 0.45 | 0.18–1.16 | 0.0980 |
| Keep physical distancing | 213/745 [28.6] | 3 | 0.8370 | 0.0010 | 0.23 | 0.08–0.65 | 0.0050 |
| Smoker | 665/2236 [29.7] | 5 | 0.0590 | 0.3360 | 1.13 | 0.99–1.29 | 0.0610 |
| History of chronic disease(s) | 3828/8197 [46.7] | 17 | 0.1840 | <0.0001 | 0.91 | 0.80–1.03 | 0.1420 |
| Ever tested for COVID-19 | 670/4430 [15.1] | 6 | 0.4340 | <0.0001 | 0.46 | 0.31–0.68 | <0.0001 |
| Personal history of COVID-19 diagnosis | 4114/7733 [53.2] | 15 | 0.6090 | <0.0001 | 0.94 | 0.66–1.33 | 0.7150 |
| Family member/friend ever diagnosed with COVID-19 | 1192/3759 [31.7] | 7 | 0.2960 | <0.0001 | 0.83 | 0.63–1.09 | 0.1730 |
| Hospitalization due to COVID-19 among people in the same social circle | 69/621 [11.1] | 2 | <0.0001 | 0.9770 | 0.57 | 0.37–0.88 | 0.0110 |
| Death due to COVID-19 among people in the same social circle | 63/537 [11.7] | 3 | <0.0001 | 0.9450 | 0.73 | 0.49–1.08 | 0.1160 |
| COVID-19 vaccines are not safe | 628/1595 [39.4] | 6 | 0.7000 | <0.0001 | 2.24 | 1.21–4.14 | 0.0100 |
| Influenza vaccination in the past few years | 3481/10,687 [32.6] | 11 | 0.3460 | <0.0001 | 0.46 | 0.36–0.58 | <0.0001 |
OR: odds ratio; CI: confidence interval; NS: number of studies; p Het: p heterogeneity; BSC: Bachelor of Science.
Figure 3.
Female was associated with increased risk of hesitancy to COVID-19 vaccination compared to male (OR: 1.32; 95% CI: 1.17, 1.49; p Egger: 0.2840; p heterogeneity: <0.0001; p: <0.0001) (A). Individuals with age > 50 years was associated with lower risk of hesitancy to COVID-19 vaccination compared to individuals with age ≤ 50 years (OR: 0.79; 95% CI: 0.64, 0.98; p Egger: 0.2980; p Het: <0.0001; p: 0.0290) (B). Single individuals had higher risk of hesitancy to COVID-19 vaccination than married individuals (OR: 1.19; 95% CI: 1.06, 1.34; p Egger: 0.1950; p heterogeneity: <0.0001; p: 0.0040) (C). The studies included are provided in the reference list [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
Figure 4.
Unemployed individuals were associated with increased risk of hesitancy to COVID-19 vaccination compared to working individuals (OR: 1.20; 95% CI: 1.02, 1.42; p Egger: 0.1790; p heterogeneity: 0.0090; p: 0.0300) (A); individuals with household number ≥ 5 individuals had higher risk of hesitancy to COVID-19 vaccination (OR: 1.36; 95% CI: 1.13, 1.63; p Egger: 0.1680; p heterogeneity: 0.1620; p: 0.0010) (B). The studies included are provided in the reference list [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
Figure 5.
Individuals with the education levels < BSC had higher risk of hesitancy to COVID-19 vaccination than ≥ BSC (OR: 1.30; 95% CI: 1.03, 1.65; p Egger: 0.5260; p heterogeneity: <0.0001; p: 0.0300) (A); individuals having the healthcare-related job had lower risk of hesitancy to COVID-19 vaccination (OR: 0.68; 95% CI: 0.52, 0.89; p Egger: 0.3340; p heterogeneity: <0.0001; p: 0.0040) (B); Individuals considering that COVID-19 vaccines are not safe had higher risk of hesitancy to COVID-19 vaccination (OR: 2.24; 95% CI: 1.21, 4.14; p Egger: 0.7000; p heterogeneity: <0.0001; p: 0.0100) (C). The studies included are provided in the reference list [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
Figure 6.
Individuals living with children in the home had lower risk of hesitancy to COVID-19 vaccination (OR: 0.37; 95% CI: 0.14, 0.99; p Egger: 1.4040; p heterogeneity: <0.0001; p: 0.0490) (A); individuals keeping physical distancing had lower risk of hesitancy to COVID-19 vaccination (OR: 0.23; 95% CI: 0.08, 0.65; p Egger: 0.8370; p heterogeneity: 0.0010; p: 0.0050 (B); individuals with history of COVID-19 test were associated with lower risk of hesitancy to COVID-19 vaccination (OR: 0.46; 95% CI: 0.31, 0.68; p Egger: 0.4340; p heterogeneity: <0.0001; p: <0.0001) (C); individuals with history of influenza vaccination in the past few years had lower risk of hesitancy to COVID-19 vaccination (OR: 0.46; 95% CI: 0.36, 0.58; p Egger: 0.3460; p heterogeneity: <0.0001; p: <0.0001) (D). The studies included are provided in the reference list [19,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79].
In contrast, living with children at home (compared to having no child at home) (Figure 6A), maintaining physical distancing norms (compared to not following such norms) (Figure 6B), having ever tested for COVID-19 (compared to having never tested for COVID-19) (Figure 6C), and having a history of influenza vaccination in the past few years (compared to not having been vaccinated for influenza in the past few years) (Figure 6D) were associated with a lower risk of hesitancy to COVID-19 vaccination.
3.4. Source of Heterogeneity and Potential Publication Bias
Heterogeneity was not found for six variables (Christian religion, household size ≥ 5 individuals, family members with a medical background, smoking, hospitalization due to COVID-19 among people in the same social circle, and death owing to COVID-19 among people in the same social circle). Therefore, we used a fixed-effects model. Conversely, other variables were assessed using a random effects model. The Egger’s test was used to assess potential bias among the studies. Our pooled analyses revealed a risk of publication bias for the following covariates: the Christian religion, family members with a medical background, hospitalization due to COVID-19 among people in the same social circle, and death owing to COVID-19 among people in the same social circle (Table 2).
4. Discussion
Our study estimated the global prevalence of COVID-19 vaccination hesitancy at 25%. The current findings are consistent with those of previous meta-analyses, which estimated the prevalence of vaccine hesitancy in the general population at 26–42% [15,80,81,82,83]. In special populations, previous meta-analyses revealed that the hesitancy for COVID-19 vaccination was estimated at 24%, 27%, and 26% in multiple sclerosis patients, older people, and healthcare students, respectively [84,85,86]. Furthermore, hesitancy to receive a COVID-19 booster was reported at 21% in the general population [87]. Moreover, high rates of COVID-19 vaccine hesitancy were reported among the ethnic minorities in the UK [88]. Our estimate was in the range of extant literature. However, our study had a larger sample size, which might have provided a more accurate calculation. Moreover, in sub-group analysis, we also identified that the prevalence of COVID-19 vaccination hesitancy was 25%, 26%, and 25% in the general population, healthcare workers, and students, respectively. This study also identified the potential predictors of COVID-19 vaccine hesitancy, thereby providing more comprehensive evidence on this phenomenon.
The current study noted that the potential factors associated with COVID-19 vaccination hesitancy can be contextualized in terms of awareness, knowledge, and socioeconomic status. In the context of awareness of COVID-19 vaccination, we found that older people (>50 years), those living with children at home, individuals who have ever tested for COVID-19, and those with a history of influenza vaccination had a lower risk of COVID-19 vaccination hesitancy. In contrast, several factors, such as single marital status and unemployment, were associated with an increased risk of hesitancy toward COVID-19 vaccination.
The precise underlying factors contributing to COVID-19 vaccination hesitancy could not be defined clearly. However, some presumptions may explain these findings. Older individuals are more likely to suffer from one or more chronic diseases compared to younger people. In our previous investigation, we found that advanced age and comorbidity were associated with an increased risk of severity in COVID-19 patients [89]. Therefore, the possibility of an increased risk of severe COVID-19 might influence the awareness of such individuals and contribute to a lower risk of COVID-19 vaccination hesitancy in this group due to low levels of complacency [90].
Similarly, individuals living with children at home might be afraid of transmitting the virus to their children should they be infected with COVID-19. Therefore, it is reasonable that this group is less hesitant to receive COVID-19 vaccination. Interestingly, a similar impact was not observed in individuals living with elderly people at home. This ironic finding is supported by previous studies, which found that living with children was a crucial determinant of health-related behavior [91], whereas this was not the case for individuals living with elderly people [92].
Furthermore, individuals who have ever tested for COVID-19 and had a history of influenza vaccination might have had good practice in disease prevention. Disease screening and vaccination history have been shown to affect health behavior, which can possibly explain why this group is less averse to COVID-19 vaccination. Moreover, married individuals might engage in protective behavior toward their spouse; couples have mutual concern and might have a better life expectancy than single individuals. A previous study found that married individuals had better health behavior and a lower risk of mortality than single individuals [93]. Thus, single individuals might be more averse than married individuals to COVID-19 vaccination. This reason, in the context of poor health behavior, might also explain vaccine hesitancy in unemployed individuals.
Our study also found that individuals with lower educational levels and those who consider COVID-19 vaccines to be unsafe had a higher risk of COVID-19 vaccination hesitancy. In contrast, individuals with healthcare-related jobs had a lower risk of COVID-19 vaccination hesitancy. The association between higher educational levels, knowledge of disease prevention, and vaccine acceptance or hesitancy has been widely investigated [16,94,95,96]. Individuals with higher educational levels and healthcare-related jobs might have adequate information on the global pandemic and consider vaccination to be a great step toward ending the pandemic, which can explain why this group had a lower risk of vaccine hesitancy. Our current findings are supported by previous studies in the context of dengue, Ebola, and monkeypox vaccines. Those studies also showed that knowledge of disease prevention and good health practices had a significant impact on the acceptance of vaccine candidates [97,98,99,100,101].
Although we could not elucidate the role of socioeconomic status in COVID-19 vaccination hesitancy in this study, we found that some factors related to socioeconomic status, such as unemployment and household size (≥5 individuals), were associated with COVID-19 vaccination hesitancy. Socioeconomic status has been proven to affect health-related behavior [102]. Individuals with a low socioeconomic status might lack knowledge of the pandemic and the role of vaccination in the pandemic. Moreover, individuals with a low socioeconomic status might also lack social interaction; therefore, they might lack adequate knowledge concerning disease prevention, which could contribute to COVID-19 vaccination hesitancy. Previous meta-analyses in this context did not assess the role of socioeconomic status in COVID-19 vaccination hesitancy. However, in other settings, such as in the case of dengue vaccines, socioeconomic status was found to affect vaccination acceptance [100].
To the best of our knowledge, this meta-analysis is the first comprehensive study to assess COVID-19 vaccination hesitancy worldwide. In sub-group analysis, our study identified similar prevalence rates of hesitancy to COVID-19 vaccination in the general population, healthcare workers, and students; suggesting that interventions to reduce the risk of COVID-19 vaccination hesitancy in those populations do not need to be differentiated. In addition to reporting the global prevalence, we also identified the potential factors associated with hesitancy to receive COVID-19 vaccination. Although the COVID-19 vaccination program targets the global population, some people have been hesitant to receive the vaccine. Our study identified the factors associated with such hesitancy, thereby shedding light on the populations that require special attention in order for the vaccination program to be successful. We recommend customized interventions and education for these special populations. A study suggested that customized effective, ethical, and evidence-based communication may be able to increase the acceptance of the COVID-19 vaccination [103]. This customized intervention was suggested to provide by community leaders and healthcare practitioners to establish the trust of COVID-19 vaccination [88]. Moreover, a recent study also reported that providing the population with reliable information regarding the COVID-19 pandemic and the COVID-19 vaccination was associated with the increased rate of vaccination acceptance among the Israeli parents [104]. On the other hand, while we have provided the valuable information on the factors associated with the risk COVID-19 vaccine hesitancy, it should be realized that the main factor driving individuals to be able to receive the vaccinations is the proven effectiveness and safety of vaccines in well-documented long-term studies. However, among those exhibiting COVID-19 vaccination hesitancy, there are people who outright refuse vaccination. Therefore, further studies should be performed with a focus on this group.
There are some potential limitations of our study. First, a meta-analysis is a methodological approach conducted by calculating the crude effect of the related factors to determine the evidence. However, the impact of potential confounding factors is difficult to evaluate. In the current study, potential confounding factors such as the types of COVID-19 vaccine, government regulations, source of information regarding COVID-19 vaccination, and environmental factors were not included; therefore, our findings should be interpreted carefully. We reported that considering the COVID-19 vaccine to be unsafe was one of the factors associated with increased risk of COVID-19 vaccination hesitancy. Considering that the different types of COVID-19 vaccine have different side effects; the factors of the type of vaccine might also govern the final findings. Moreover, the government regulations in several countries have implemented COVID-19 vaccination as a condition of administration, and the regulations in each country may have differences; thereby, this circumstance may also affect the final findings of this study. Therefore, we reiterate the importance of the basic tenet in studying the phenomenon of vaccine hesitancy, which is the time, context, place, and type specificity. All these peculiarities need to be considered in the efforts aiming to fathom the determinants of vaccine hesitancy [105]. Second, our study involved a multi-national population, and the knowledge of disease prevention among people with similar socioeconomic status and educational level might vary in each region. Third, all the papers included in our study had an observational research design. Therefore, further studies including randomized controlled trials are required in order to obtain better levels of evidence.
5. Conclusions
Our study estimated the global prevalence of COVID-19 vaccination hesitancy at 25%. It also recommended special interventions to minimize COVID-19 vaccination hesitancy among unmarried individuals, women, people with low educational levels, the unemployed, people living in households with five or more individuals, and those who believe COVID-19 vaccines to be unsafe.
Acknowledgments
We thank Lembaga Pengelola Dana Pendidikan (LPDP) Republic of Indonesia for supporting this project.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10081356/s1, Supplementary S1: PRISMA 2020 Checklist.
Author Contributions
Conceptualization, J.K.F. and G.S.; methodology, J.K.F., Y.J.S., M.A. (Muhammad Anshory), L.W., S.A.P.K., M.I., K.K., M.F., F.P., B.H., I.D.P., L.A., L.M., F.S.I., W.O.E., K.W.N., O.W., S.E., U.H., L.R., H.L., R.A. (Rinto Ariwibowo), R.A. (Riska Andistyani), R.F., M.H., F.A.D.N., F.T. and F.O.L.; software, J.K.F.; validation, J.K.F., M.S., G.S., Y.J.S., M.A. (Muhammad Anshory), L.W., S.A.P.K., M.I., K.K., M.F., F.P., B.H., I.D.P., L.A., L.M., F.S.I., W.O.E., K.W.N., O.W., S.E., U.H., L.R., H.L., R.A. (Rinto Ariwibowo), R.A. (Riska Andistyani), R.F., M.H., F.A.D.N., F.T., F.O.L., H.I.K., A.A.R., S.A., A.A.M., M.G., M.A.H., M.A. (Mubarak Alfaresi), R.A.A., N.A.A., A.N.A., K.D. and H.H.; formal analysis, J.K.F.; investigation, J.K.F., Y.J.S., M.A. (Mubarak Alfaresi), L.W., S.A.P.K., M.I., K.K., M.F., F.P., B.H., I.D.P., L.A., L.M., F.S.I., W.O.E., K.W.N., O.W., S.E., U.H., L.R., H.L., R.A. (Rinto Ariwibowo), R.A. (Riska Andistyani), R.F., M.H., F.A.D.N., F.T. and F.O.L.; re-sources, M.S., H.I.K., A.A.R., S.A., A.A.M., M.G., M.A.H., M.A. (Mubarak Alfaresi), R.A.A., N.A.A., A.N.A., K.D. and H.H.; data curation, J.K.F., Y.J.S., M.A. (Muhammad Anshory), L.W., S.A.P.K., M.I., K.K., M.F., F.P., B.H., I.D.P., L.A., L.M., F.S.I., W.O.E., K.W.N., O.W., S.E., U.H., L.R., H.L., R.A. (Rinto Ariwibowo), R.A. (Riska Andistyani), R.F., M.H., F.A.D.N., F.T. and F.O.L.; writing—original draft preparation, J.K.F., Y.J.S., M.A. (Muhammad Anshory), L.W., S.A.P.K., M.I., K.K., M.F., F.P., B.H., I.D.P., L.A., L.M., F.S.I., W.O.E., K.W.N., O.W., S.E., U.H., L.R., H.L., R.A. (Rinto Ariwibowo), R.A. (Riska Andistyani), R.F., M.H., F.A.D.N., F.T. and F.O.L.; writing—review and editing, J.K.F., M.S., G.S., A.A.R., S.A., A.A.M., M.G., M.A.H., M.A. (Mubarak Alfaresi), R.A.A., N.A.A., A.N.A., K.D. and H.H.; visualization, J.K.F.; supervision, G.S., A.A.R., S.A., A.A.M., M.G., M.A.H., M.A. (Muhammad Anshory), R.A.A., N.A.A., A.N.A., K.D. and H.H.; project administration, J.K.F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data underlying the results are available at the Supplementary Files (https://doi.org/10.6084/m9.figshare.20055539.v3). Accessed on 11 June 2022.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kashte S., Gulbake A., El-Amin S.F., III, Gupta A. COVID-19 vaccines: Rapid development, implications, challenges and future prospects. Hum. Cell. 2021;34:711–733. doi: 10.1007/s13577-021-00512-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenwood B. The contribution of vaccination to global health: Past, present and future. Philos. Trans. R. Soc. Lond B Biol. Sci. 2014;369:20130433. doi: 10.1098/rstb.2013.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salo H., Kilpi T. National vaccination program—A success story of public health and economy. Duodecim. 2017;133:977–983. [PubMed] [Google Scholar]
- 4.Anderson E.L. Recommended solutions to the barriers to immunization in children and adults. Mo. Med. 2014;111:344–348. [PMC free article] [PubMed] [Google Scholar]
- 5.Shen S.C., Dubey V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can. Fam. Physician. 2019;65:175–181. [PMC free article] [PubMed] [Google Scholar]
- 6.Pugliese-Garcia M., Heyerdahl L.W., Mwamba C., Nkwemu S., Chilengi R., Demolis R., Guillermet E., Sharma A. Factors influencing vaccine acceptance and hesitancy in three informal settlements in Lusaka, Zambia. Vaccine. 2018;36:5617–5624. doi: 10.1016/j.vaccine.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sallam M., Al-Sanafi M., Sallam M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022;15:21–45. doi: 10.2147/JMDH.S347669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aide P., Bassat Q., Alonso P.L. Towards an effective malaria vaccine. Arch. Dis. Child. 2007;92:476–479. doi: 10.1136/adc.2005.092551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fatima K., Syed N.I. Dengvaxia controversy: Impact on vaccine hesitancy. J. Glob. Health. 2018;8:010312. doi: 10.7189/jogh.08.020312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mesch G.S., Schwirian K.P. Vaccination hesitancy: Fear, trust, and exposure expectancy of an Ebola outbreak. Heliyon. 2019;5:e02016. doi: 10.1016/j.heliyon.2019.e02016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voo J.Y.H., Lean Q.Y., Ming L.C., Md Hanafiah N.H., Al-Worafi Y.M., Ibrahim B. Vaccine Knowledge, Awareness and Hesitancy: A Cross Sectional Survey among Parents Residing at Sandakan District, Sabah. Vaccines. 2021;9:1348. doi: 10.3390/vaccines9111348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmid P., Rauber D., Betsch C., Lidolt G., Denker M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE. 2017;12:e0170550. doi: 10.1371/journal.pone.0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beste L.A., Chen A., Geyer J., Wilson M., Schuttner L., Wheat C., Rojas J., Nelson K., Reddy A. Best Practices for an Equitable Covid-19 Vaccination Program. NEJM Catal. Innov. Care Deliv. 2021;2 doi: 10.1056/CAT.21.0238. [DOI] [Google Scholar]
- 15.Norhayati M.N., Che Yusof R., Azman Y.M. Systematic Review and Meta-Analysis of COVID-19 Vaccination Acceptance. Front. Med. 2022;8:783982. doi: 10.3389/fmed.2021.783982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sallam M., Dababseh D., Eid H., Hasan H., Taim D., Al-Mahzoum K., Al-Haidar A., Yaseen A., Ababneh N.A., Assaf A., et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health. 2021;18:2407. doi: 10.3390/ijerph18052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosiello D.F., Anwar S., Yufika A., Adam R.Y., Ismaeil M.I.H., Ismail A.Y., Dahman N.B.H., Hafsi M., Ferjani M., Sami F.S., et al. Acceptance of COVID-19 vaccination at different hypothetical efficacy and safety levels in ten countries in Asia, Africa, and South America. Narra J. 2021;1:e55. doi: 10.52225/narra.v1i3.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sallam M., Anwar S., Yufika A., Fahriani M., Husnah M., Kusuma H.I., Raad R., Khiri N.M.E., Abdalla R.Y.A., Adam R.Y., et al. Willingness-to-pay for COVID-19 vaccine in ten low-middle-income countries in Asia, Africa and South America: A cross-sectional study. Narra J. 2022;2:e74. doi: 10.52225/narra.v2i1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patwary M.M., Bardhan M., Disha A.S., Hasan M., Haque M.Z., Sultana R., Hossain M.R., Browning M., Alam M.A., Sallam M. Determinants of COVID-19 Vaccine Acceptance among the Adult Population of Bangladesh Using the Health Belief Model and the Theory of Planned Behavior Model. Vaccines. 2021;9:1393. doi: 10.3390/vaccines9121393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Del Riccio M., Boccalini S., Rigon L., Biamonte M.A., Albora G., Giorgetti D., Bonanni P., Bechini A. Factors Influencing SARS-CoV-2 Vaccine Acceptance and Hesitancy in a Population-Based Sample in Italy. Vaccines. 2021;9:633. doi: 10.3390/vaccines9060633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montalti M., Di Valerio Z., Rallo F., Squillace L., Costantino C., Tomasello F., Mauro G.L., Stillo M., Perrone P., Resi D., et al. Attitudes toward the SARS-CoV-2 and Influenza Vaccination in the Metropolitan Cities of Bologna and Palermo, Italy. Vaccines. 2021;9:1200. doi: 10.3390/vaccines9101200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fajar J.K. Supplementary files: Global prevalence and potential influencing factors of COVID-19 vaccination hesitancy: A meta-analysis. Figshare. 2022;1:1. doi: 10.6084/m9.figshare.20055539.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 25.Aemro A., Amare N.S., Shetie B., Chekol B., Wassie M. Determinants of COVID-19 vaccine hesitancy among health care workers in Amhara region referral hospitals, Northwest Ethiopia: A cross-sectional study. Epidemiol. Infect. 2021;149:e225. doi: 10.1017/S0950268821002259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ali M., Hossain A. What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ Open. 2021;11:e050303. doi: 10.1136/bmjopen-2021-050303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barry M., Temsah M.H., Alhuzaimi A., Alamro N., Al-Eyadhy A., Aljamaan F., Saddik B., Alhaboob A., Alsohime F., Alhasan K., et al. COVID-19 vaccine confidence and hesitancy among health care workers: A cross-sectional survey from a MERS-CoV experienced nation. PLoS ONE. 2021;16:e0244415. doi: 10.1371/journal.pone.0244415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020;38:7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen H., Li X., Gao J., Liu X., Mao Y., Wang R., Zheng P., Xiao Q., Jia Y., Fu H., et al. Health Belief Model Perspective on the Control of COVID-19 Vaccine Hesitancy and the Promotion of Vaccination in China: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021;23:e29329. doi: 10.2196/29329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chudasama R.V., Khunti K., Ekezie W.C., Pareek M., Zaccardi F., Gillies C.L., Seidu S., Davies M.J., Chudasama Y.V. COVID-19 vaccine uptake and hesitancy opinions from frontline health care and social care workers: Survey data from 37 countries. Diabetes Metab. Syndr. 2022;16:102361. doi: 10.1016/j.dsx.2021.102361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38:7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dong D., Xu R.H., Wong E.L., Hung C.T., Feng D., Feng Z., Yeoh E.K., Wong S.Y. Public preference for COVID-19 vaccines in China: A discrete choice experiment. Health Expect. 2020;23:1543–1578. doi: 10.1111/hex.13140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., Srouji S., Sela E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020;35:775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Faasse K., Newby J. Public Perceptions of COVID-19 in Australia: Perceived Risk, Knowledge, Health-Protective Behaviors, and Vaccine Intentions. Front. Psychol. 2020;11:551004. doi: 10.3389/fpsyg.2020.551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020;173:964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goodwin R., Ben-Ezra M., Takahashi M., Luu L.N., Borsfay K., Kovacs M., Hou W.K., Hamama-Raz Y., Levin Y. Psychological factors underpinning vaccine willingness in Israel, Japan and Hungary. Sci. Rep. 2022;12:439. doi: 10.1038/s41598-021-03986-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Habib S.S., Alamri M.S., Alkhedr M.M., Alkhorijah M.A., Jabaan R.D., Alanzi M.K. Knowledge and Attitudes of Medical Students toward COVID-19 Vaccine in Saudi Arabia. Vaccines. 2022;10:541. doi: 10.3390/vaccines10040541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamdan M.B., Singh S., Polavarapu M., Jordan T.R., Melhem N.M. COVID-19 vaccine hesitancy among university students in Lebanon. Epidemiol. Infect. 2021;149:e242. doi: 10.1017/S0950268821002314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harapan H., Wagner A.L., Yufika A., Winardi W., Anwar S., Gan A.K., Setiawan A.M., Rajamoorthy Y., Sofyan H., Mudatsir M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Horiuchi S., Sakamoto H., Abe S.K., Shinohara R., Kushima M., Otawa S., Yui H., Akiyama Y., Ooka T., Kojima R., et al. Factors of parental COVID-19 vaccine hesitancy: A cross sectional study in Japan. PLoS ONE. 2021;16:e0261121. doi: 10.1371/journal.pone.0261121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hossain M.B., Alam M.Z., Islam M.S., Sultan S., Faysal M.M., Rima S., Hossain M.A., Mamun A.A. COVID-19 vaccine hesitancy among the adult population in Bangladesh: A nationwide cross-sectional survey. PLoS ONE. 2021;16:e0260821. doi: 10.1371/journal.pone.0260821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang Y., Su X., Xiao W., Wang H., Si M., Wang W., Gu X., Ma L., Li L., Zhang S., et al. COVID-19 vaccine hesitancy among different population groups in China: A national multicenter online survey. BMC Infect. Dis. 2022;22:153. doi: 10.1186/s12879-022-07111-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ikiisik H., Sezerol M.A., Tasci Y., Maral I. COVID-19 vaccine hesitancy: A community-based research in Turkey. Int. J. Clin. Pract. 2021;75:e14336. doi: 10.1111/ijcp.14336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jabessa D., Bekele F. Willingness to receive the COVID-19 vaccine and associated factors among residents of Southwestern Ethiopia: A cross-sectional study. Patient Prefer. Adherence. 2022;16:1177–1185. doi: 10.2147/PPA.S362264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jain J., Saurabh S., Kumar P., Verma M.K., Goel A.D., Gupta M.K., Bhardwaj P., Raghav P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 2021;149:e132. doi: 10.1017/S0950268821001205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kelekar A.K., Lucia V.C., Afonso N.M., Mascarenhas A.K. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J. Am. Dent. Assoc. 2021;152:596–603. doi: 10.1016/j.adaj.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health. 2021;46:270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Koh S.W.C., Liow Y., Loh V.W.K., Liew S.J., Chan Y.H., Young D. COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore. BMC Prim. Care. 2022;23:81. doi: 10.1186/s12875-022-01693-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar R., Alabdulla M., Elhassan N.M., Reagu S.M. Qatar Healthcare Workers’ COVID-19 Vaccine Hesitancy and Attitudes: A National Cross-Sectional Survey. Front. Public Health. 2021;9:727748. doi: 10.3389/fpubh.2021.727748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee M., You M. Direct and Indirect Associations of Media Use With COVID-19 Vaccine Hesitancy in South Korea: Cross-sectional Web-Based Survey. J. Med. Internet Res. 2022;24:e32329. doi: 10.2196/32329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li S., Gao Z., Zhong M., Yu Z., Li J., Bi H. Chinese University Students’ Awareness and Acceptance of the COVID-19 Vaccine: A Cross-Sectional Study. Risk Manag. Healthc. Policy. 2022;15:845–864. doi: 10.2147/RMHP.S360274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liddell B.J., Murphy S., Mau V., Bryant R., O’Donnell M., McMahon T., Nickerson A. Factors associated with COVID-19 vaccine hesitancy amongst refugees in Australia. Eur. J. Psychotraumatol. 2021;12:1997173. doi: 10.1080/20008198.2021.1997173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lucia V.C., Kelekar A., Afonso N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health. 2021;43:445–449. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marzo R.R., Sami W., Alam M.Z., Acharya S., Jermsittiparsert K., Songwathana K., Pham N.T., Respati T., Faller E.M., Baldonado A.M., et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: A cross-sectional study in six Southeast Asian countries. Trop. Med. Health. 2022;50:4. doi: 10.1186/s41182-021-00393-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mascarenhas A.K., Lucia V.C., Kelekar A., Afonso N.M. Dental students’ attitudes and hesitancy toward COVID-19 vaccine. J. Dent. Educ. 2021;85:1504–1510. doi: 10.1002/jdd.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mohammed R., Nguse T.M., Habte B.M., Fentie A.M., Gebretekle G.B. COVID-19 vaccine hesitancy among Ethiopian healthcare workers. PLoS ONE. 2021;16:e0261125. doi: 10.1371/journal.pone.0261125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mose A., Haile K., Timerga A. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS ONE. 2022;17:e0263081. doi: 10.1371/journal.pone.0263081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nery N., Jr., Ticona J.P.A., Cardoso C.W., Prates A., Vieira H.C.A., de Almeida A.S., Souza M., dos Reis O.B., Pellizzaro M., Portilho M.M., et al. COVID-19 vaccine hesitancy and associated factors according to sex: A population-based survey in Salvador, Brazil. PLoS ONE. 2022;17:e0262649. doi: 10.1371/journal.pone.0262649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Neumann-Bohme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., Schreyogg J., Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ousseine Y.M., Vaux S., Vandentorren S., Bonmarin I., Champenois K., Lydie N., Velter A. Predictors of Uncertainty and Unwillingness to Receive the COVID-19 Vaccine in Men Who Have Sex with Men in France. Int. J. Environ. Res. Public Health. 2022;19:5372. doi: 10.3390/ijerph19095372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qunaibi E.A., Helmy M., Basheti I., Sultan I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. Elife. 2021;10:e68038. doi: 10.7554/eLife.68038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Raja S.M., Osman M.E., Musa A.O., Hussien A.A., Yusuf K. COVID-19 vaccine acceptance, hesitancy, and associated factors among medical students in Sudan. PLoS ONE. 2022;17:e0266670. doi: 10.1371/journal.pone.0266670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rodriguez-Blanco N., Montero-Navarro S., Botella-Rico J.M., Felipe-Gomez A.J., Sanchez-Mas J., Tuells J. Willingness to Be Vaccinated against COVID-19 in Spain before the Start of Vaccination: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2021;18:5272. doi: 10.3390/ijerph18105272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Saied S.M., Saied E.M., Kabbash I.A., Abdo S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021;93:4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Salali G.D., Uysal M.S. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 2020;1:1–3. doi: 10.1017/S0033291720004067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shah A.K., Daniel R.A., Kusuma Y.S. Knowledge and Willingness to Accept Vaccine Against SARS-CoV-2 Among Undergraduate Medical Students in Delhi, India. Curr. Health Sci. J. 2021;47:479–484. doi: 10.12865/CHSJ.47.04.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Singh A., Lai A.H.Y., Wang J., Asim S., Chan P.S., Wang Z., Yeoh E.K. Multilevel Determinants of COVID-19 Vaccine Uptake Among South Asian Ethnic Minorities in Hong Kong: Cross-sectional Web-Based Survey. JMIR Public Health Surveill. 2021;7:e31707. doi: 10.2196/31707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tao L., Wang R., Han N., Liu J., Yuan C., Deng L., Han C., Sun F., Liu M., Liu J. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: A multi-center cross-sectional study based on health belief model. Hum. Vaccin Immunother. 2021;17:2378–2388. doi: 10.1080/21645515.2021.1892432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tlale L.B., Gabaitiri L., Totolo L.K., Smith G., Puswane-Katse O., Ramonna E., Mothowaeng B., Tlhakanelo J., Masupe T., Rankgoane-Pono G., et al. Acceptance rate and risk perception towards the COVID-19 vaccine in Botswana. PLoS ONE. 2022;17:e0263375. doi: 10.1371/journal.pone.0263375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang K., Wong E.L.Y., Ho K.F., Cheung A.W.L., Chan E.Y.Y., Yeoh E.K., Wong S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ward J.K., Alleaume C., Peretti-Watel P., Group C. The French public’s attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc. Sci. Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020;16:2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wu J., Li Q., Silver Tarimo C., Wang M., Gu J., Wei W., Ma M., Zhao L., Mu Z., Miao Y. COVID-19 Vaccine Hesitancy Among Chinese Population: A Large-Scale National Study. Front. Immunol. 2021;12:781161. doi: 10.3389/fimmu.2021.781161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xu B., Zhang Y., Chen L., Yu L., Li L., Wang Q. The influence of social network on COVID-19 vaccine hesitancy among healthcare workers: A cross-sectional survey in Chongqing, China. Hum. Vaccine Immunother. 2021;17:5048–5062. doi: 10.1080/21645515.2021.2004837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yassin E.O.M., Faroug H.A.A., Ishaq Z.B.Y., Mustafa M.M.A., Idris M.M.A., Widatallah S.E.K., Abd El-Raheem G.O.H., Suliman M.Y. COVID-19 Vaccination Acceptance among Healthcare Staff in Sudan, 2021. J. Immunol. Res. 2022;2022:3392667. doi: 10.1155/2022/3392667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patwary M.M., Alam M.A., Bardhan M., Disha A.S., Haque M.Z., Billah S.M., Kabir M.P., Browning M., Rahman M.M., Parsa A.D., et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines. 2022;10:427. doi: 10.3390/vaccines10030427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ulbrichtova R., Svihrova V., Svihra J. Prevalence of COVID-19 Vaccination among Medical Students: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2022;19:4072. doi: 10.3390/ijerph19074072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang Q., Yang L., Jin H., Lin L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021;150:106694. doi: 10.1016/j.ypmed.2021.106694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roy D.N., Biswas M., Islam E., Azam M.S. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS ONE. 2022;17:e0265496. doi: 10.1371/journal.pone.0265496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yazdani A., Mirmosayyeb O., Ghaffary E.M., Hashemi M.S., Ghajarzadeh M. COVID-19 vaccines and patients with multiple sclerosis: Willingness, unwillingness and hesitancy: A systematic review and meta-analysis. Neurol. Sci. 2022;43:4085–4094. doi: 10.1007/s10072-022-06051-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Veronese N., Saccaro C., Demurtas J., Smith L., Dominguez L.J., Maggi S., Barbagallo M. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people: A systematic review and meta-analysis. Ageing Res. Rev. 2021;72:101489. doi: 10.1016/j.arr.2021.101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Patwary M.M., Bardhan M., Haque M.Z., Sultana R., Alam M.A., Browning M. COVID-19 Vaccine Acceptance Rate and Its Factors among Healthcare Students: A Systematic Review with Meta-Analysis. Vaccines. 2022;10:806. doi: 10.3390/vaccines10050806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Galanis P., Vraka I., Katsiroumpa A., Siskou O., Konstantakopoulou O., Katsoulas T., Mariolis-Sapsakos T., Kaitelidou D. First COVID-19 Booster Dose in the General Population: A Systematic Review and Meta-Analysis of Willingness and Its Predictors. Vaccines. 2022;10:1097. doi: 10.3390/vaccines10071097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hussain B., Latif A., Timmons S., Nkhoma K., Nellums L.B. Overcoming COVID-19 vaccine hesitancy among ethnic minorities: A systematic review of UK studies. Vaccine. 2022;40:3413–3432. doi: 10.1016/j.vaccine.2022.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mudatsir M., Fajar J.K., Wulandari L., Soegiarto G., Ilmawan M., Purnamasari Y., Mahdi B.A., Jayanto G.D., Suhendra S., Setianingsih Y.A., et al. Predictors of COVID-19 severity: A systematic review and meta-analysis. F1000Research. 2020;9:1107. doi: 10.12688/f1000research.26186.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Al-Sanafi M., Sallam M. Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines. 2021;9:701. doi: 10.3390/vaccines9070701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rattay P., von der Lippe E. Association between Living with Children and the Health and Health Behavior of Women and Men. Are There Differences by Age? Results of the “German Health Update” (GEDA) Study. Int. J. Environ. Res. Public Health. 2020;17:3180. doi: 10.3390/ijerph17093180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.García L.M.R., Navarrro J.M.R. The Impact of Quality of Life on the Health of Older People from a Multidimensional Perspective. J. Aging Res. 2018;2018:4086294. doi: 10.1155/2018/4086294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Robards J., Evandrou M., Falkingham J., Vlachantoni A. Marital status, health and mortality. Maturitas. 2012;73:295–299. doi: 10.1016/j.maturitas.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mohamed N.A., Solehan H.M., Rani M.D.M., Ithnin M., Che Isahak C.I. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS ONE. 2021;16:e0256110. doi: 10.1371/journal.pone.0256110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bari M.S., Hossain M.J., Ahmmed F., Sarker M.M.R., Khandokar L., Chaithy A.P., Aziz F., Mitra S., Emran T.B., Islam M.S., et al. Knowledge, Perception, and Willingness towards Immunization among Bangladeshi Population during COVID-19 Vaccine Rolling Period. Vaccines. 2021;9:1449. doi: 10.3390/vaccines9121449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Theodorea C.F., Widyarman A.S., Dewanto I., Astoeti T.E. COVID-19 Vaccines in Indonesia: Knowledge, Attitudes, and Acceptance Among Dental Professionals. Front. Med. 2021;8:784002. doi: 10.3389/fmed.2021.784002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Harapan H., Fajar J.K., Sasmono R.T., Kuch U. Dengue vaccine acceptance and willingness to pay. Hum. Vaccines Immunother. 2017;13:786–790. doi: 10.1080/21645515.2016.1259045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Harapan H., Anwar S., Bustaman A., Radiansyah A., Angraini P., Fasli R., Salwiyadi S., Bastian R.A., Oktiviyari A., Akmal I., et al. Community Willingness to Participate in a Dengue Study in Aceh Province, Indonesia. PLoS ONE. 2016;11:e0159139. doi: 10.1371/journal.pone.0159139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mudatsir M., Anwar S., Fajar J.K., Yufika A., Ferdian M.N., Salwiyadi S., Imanda A.S., Azhars R., Ilham D., Timur A.U., et al. Willingness-to-pay for a hypothetical Ebola vaccine in Indonesia: A cross-sectional study in Aceh. F1000Research. 2019;8:1441. doi: 10.12688/f1000research.20144.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fajar J.K., Harapan H. Socioeconomic and attitudinal variables associated with acceptance and willingness to pay towards dengue vaccine: A systematic review. Arch. Clin. Infect. Dis. 2017;12:e13914. doi: 10.5812/archcid.13914. [DOI] [Google Scholar]
- 101.Harapan H., Wagner A.L., Yufika A., Setiawan A.M., Anwar S., Wahyuni S., Asrizal F.W., Sufri M.R., Putra R.P., Wijayanti N.P., et al. Acceptance and willingness to pay for a hypothetical vaccine against monkeypox viral infection among frontline physicians: A cross-sectional study in Indonesia. Vaccine. 2020;38:6800–6806. doi: 10.1016/j.vaccine.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pampel F.C., Krueger P.M., Denney J.T. Socioeconomic Disparities in Health Behaviors. Annu Rev. Sociol. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ratzan S.C. “Vaccine Communication in a Pandemic: Improving Vaccine Literacy to Reduce Hesitancy, Restore Trust and Immunize Communities”: Editor’s Introduction. J. Health Commun. 2020;25:745–746. doi: 10.1080/10810730.2021.1884774. [DOI] [PubMed] [Google Scholar]
- 104.Gendler Y., Ofri L. Investigating the Influence of Vaccine Literacy, Vaccine Perception and Vaccine Hesitancy on Israeli Parents’ Acceptance of the COVID-19 Vaccine for Their Children: A Cross-Sectional Study. Vaccines. 2021;9:1391. doi: 10.3390/vaccines9121391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.MacDonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data underlying the results are available at the Supplementary Files (https://doi.org/10.6084/m9.figshare.20055539.v3). Accessed on 11 June 2022.