Abstract
Background. Recurrent therapeutic failures reported for the treatment of methicillin-resistant Staphylococcus aureus (MRSA) infective endocarditis (IE) with vancomycin may be due to poor bactericidal activity. Alternative antibacterial approaches using bacteriophages may overcome this limitation. Objectives. An experimental rat model of MRSA IE (EE) was used to examine the efficacy of vancomycin combined with a 1:1 bacteriophage (phage) cocktail composed of Herelleviridae vB_SauH_2002 and Routreeviridae 66. Methods. Six hours after inoculation with ca. 5 log10 colony forming units (CFU) of MRSA strain AW7, animals were treated with either: (i) saline, (ii) an equimolar two-phage cocktail (bolus of 1 mL followed by a 0.3 mL/h continuous infusion of 10 log10 plaque forming units (PFU)/mL phage suspension), (iii) vancomycin (at a dose mimicking the kinetics in humans of 0.5 g b.i.d.), or (iv) a combination of both. Bacterial loads in vegetations, and phage loads in vegetations, liver, kidney, spleen, and blood, were measured outcomes. Results. Phage cocktail alone was unable to control the growth of strain AW7 in cardiac vegetations. However, when combined with subtherapeutic doses of vancomycin, a statistically significant decrease of ∆4.05 ± 0.94 log10 CFU/g at 24 h compared to placebo was detected (p < 0.001). The administration of vancomycin was found to significantly impact on the local concentrations of phages in the vegetations and in the organs examined. Conclusions. Lytic bacteriophages as an adjunct treatment to the standard of care antibiotics could potentially improve the management of MRSA IE. Further studies are needed to investigate the impact of antibiotics on phage replication in vivo.
Keywords: bacteriophage, phage therapy, infective endocarditis, MRSA, vancomycin
1. Introduction
Staphylococcus aureus (S. aureus) endocarditis continues to be associated with substantial morbidity and mortality rates [1], especially when caused by methicillin-resistant strains (MRSA) [2]. Current guidelines recommend the use of vancomycin for MRSA infective endocarditis (IE), while daptomycin is a reasonable alternative [3]. However, minimal penetration into vegetation [4], a slow bactericidal effect [5], and potentially severe side effects such as nephrotoxicity challenge this dosing scheme. Clinical failures associated with the administration of vancomycin have included renal failure [6] and the emergence of vancomycin-intermediate S. aureus (VISA) clones [7]. Thus, alternative and/or adjunct treatments for MRSA IE are needed.
The therapeutic use of bacterial viruses called bacteriophages (phages), referred to as phage therapy, has been successfully applied to cases involving bacterial infections for nearly a century in several Eastern European countries [8]. Since the early 2000s, phage therapy has undergone greater investigation in Western societies, including for the treatment of S. aureus IE [9,10]. Renewed interest for this forgotten cure is principally in response to a growing threat of antibiotic resistance [11]. Recently, however, a few randomized clinical trials have repeatedly failed to report phage therapy efficacy [12].
In sharp contrast to most experimental settings, phages have mainly been evaluated in conjunction with antibiotics [13]. However, the use of antibiotics may represent a double-edged sword if it reduces the number of bacteria needed for phages to replicate. Recently, we reported a synergistic bactericidal effect of a novel anti-S. aureus two-phage cocktail in combination with beta-lactam and flucloxacillin, for the treatment of methicillin-susceptible S. aureus (MSSA) experimental infective endocarditis (EE). However, the same study also observed that in the presence of flucloxacillin, the pharmacokinetic (PK) profile of the phages was significantly altered in vivo [14]. Here, we further investigate whether the same phage cocktail will synergize with the glycopeptide vancomycin, for the treatment of MRSA EE. We also evaluate to what extent vancomycin affects the PK profile of phages in this well-established rat model of EE [15,16].
2. Materials and Methods
2.1. Bacterial Strains, Bacterial Genomic DNA, and Bacteriophages
MRSA strain AW7 [17] was isolated from a patient in Switzerland with bacteremia and has been used to establish EE [18] and pneumonia [19,20,21]. We adapted a protocol from Bae et al. [22] to obtain purified S. aureus genomic DNA (described in Supplemental Material). Herelleviridae (formerly Myoviridae) phage vB_SauH_2002 was isolated from sewage water [14]. The genome of vB_SauH_2002 is composed of a circular double stranded DNA (dsDNA) of 145,076 bp in length (Genbank accession no. MW528836). Routreeviridae (formerly Podoviridae) phage 66 was purchased from the National Collection of Types Cultures of Public Health England (catalogue #8289). Its genome is composed of a linear dsDNA of 18,199 bp in length (Genbank accession no. NC_007046). These two phages were produced on MSSA Laus102 strain [23], and the concentration of each phage solution was adjusted to 10 log10 PFU/mL. Details regarding the growth conditions and reagents are provided in Supplemental Material.
2.2. In Vitro Activities of Phages and Vancomycin against Planktonic Cultures and Biofilms
The lytic activity of each single phage and their combination as a 1:1 cocktail was evaluated in diluted drop tests, turbidity assays, or time-kill assays on planktonic AW7 cultures in the presence or absence of vancomycin at 1× and 10× minimum inhibitory concentration (MIC) [24]. A detailed description of the methods used is provided in the Supplemental Material section.
Synergy between both antibacterial treatments was defined as an additional ≥ 2 log10 CFU/mL reduction in bacterial load compared to the effect of the best single treatment [25].
2.3. Murine Model of EE
Female Wistar rats (Charles River, L’Abresle, France) weighing 180–200 g were used in this study. Animals were kept in specific pathogen-free rooms (12 h light/dark conditions, 23 ± 1 °C, water, and food ad libitum). The experiments involving animals were performed according to Swiss Animal Protection Law guidelines, and were approved by the Cantonal Committee on Animal Experiments of the State of Vaud (approval N° VD 879.10). Animals were anesthetized with an intraperitoneal administration of ketamine (Ketalar®, 75 mg/kg) and xylazine (Xylasol®, 0.5 mg/kg). An intraperitonal administration of buprenorphin (Temgesic®, 0.15 mg/kg) just prior to surgery served as an analgesic.
Induction of infection. Catheter-induced sterile aortic vegetations were produced in rats as previously described [16]. Antibacterial drug administration was performed according to a dosing schedule that mimics the kinetics of human intravenous (IV) antibiotic therapy [26,27]. For this purpose, an IV line was placed via the jugular vein into the superior vena cava and connected to a programmable infusion pump (Pump 44; Harvard Apparatus, Inc., South Natick, MA, USA) [26]. Bacterial inocula were prepared from dilutions of mid-exponential phase cultures of MRSA strain AW7 (optical density at 600 nm (OD600 nm) = 0.6, ~8 log10 CFU/mL). Twenty-four hours after surgery, each animal received 500 µL inoculum through the IV route (5.11 ± 0.48 log10 CFU, corresponding to 10 times the 90% infectious dose [26]). Inoculum size was confirmed by counting isolated colonies on trypticase soy agar plates (TSA; BD DifcoTM, Becton Dickinson, Sparks, MD, USA). Three uninfected animals were used for PK studies. Additional information related to the EE model used is provided in Supplemental Materials.
Power calculation. We hypothesized that 100% and 30% of the placebo and phage cocktail/vancomycin-treated rats would exhibit infected vegetations at 24 h, respectively. These estimates, along with an α = 0.05 and power (1−β) = 0.8, indicated that a sample size of at least eight animals per group was needed [28].
2.4. Treatment Protocol
Six hours after bacterial challenge, a subset of animals was euthanized to assess the concentrations of bacteria present in vegetations at the onset of treatment. The remaining animals were subsequently treated with either: (i) mock therapy (saline); (ii) a phage cocktail (10 log10 PFU/mL, equimolar concentrations of each phage) injected as a 1 mL bolus, followed by continuous infusion at 0.3 mL/h for up to 48 h; (iii) a subtherapeutic IV dose of vancomycin mimicking human kinetic treatment of 0.5 g given every 12 h for up to 48 h [29]; or (iv) a combination of both treatments (Supplemental Figure S1). Programmable infusion pumps were used to deliver the treatments. Concentrations of bacteria in vegetations were assessed again 24 h and 48 h after the onset of treatment in the remaining rats that were euthanized. Concentrations were determined from colony counts of TSA plates. Details regarding the exact numbers of animals used in each group are reported in the Supplemental Material section.
2.5. Outcomes
Primary outcomes included bacterial loads within cardiac vegetations at 24 h and 48 h after onset of treatment. Secondary outcomes included phage concentrations at 24 h and 48 h in cardiac vegetations, blood, spleen, liver, and kidneys. Selection of phage-resistant clones from the cardiac vegetations obtained under phage/vancomycin combinations were examined at 48 h. Methods used to assess all outcomes are described in Supplemental Material.
2.6. Statistical Analysis
Data obtained from time-kill assays and from the in vivo model of IE were compared using two-way analysis of variance (ANOVA) with Tukey’s multiple comparisons test. The Mann–Whitney test was used to compare PK data from healthy and MRSA-infected animals. All statistical analyses were performed with GraphPad Prism software (version 9.0.0, La Jolla, CA, USA). Statistical test results were considered significant when p ≤ 0.05 were obtained. Mean values are reported with standard deviation (SD).
3. Results
3.1. In Vitro Activity of vB_SauH_2002/Phage 66 Cocktail on MRSA AW7
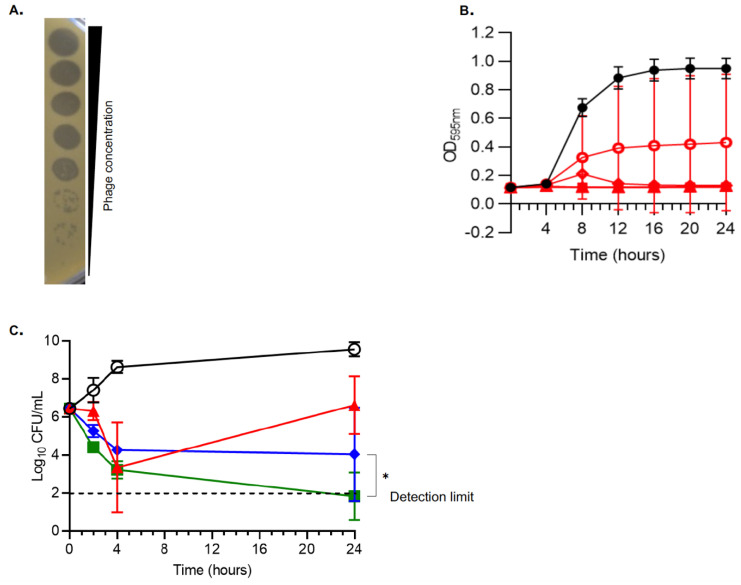
A phage cocktail (with a non-diluted phage titer of 10 log10 PFU/mL) composed of an equimolar mixture of Herelleviridae vB_SauH_2002 and Routreeviridae 66 formed clear plaques on a lawn of MRSA strain AW7 in a diluted drop test assay (Figure 1A). In turbidity assays, a multiplicity of infection (MOI) of at least 0.1 was needed to prevent the growth of strain AW7 over 24 h (Figure 1B). In time-kill assays, the phage cocktail at an MOI of 1 was highly bactericidal at 4 h (∆3.09 ± 0.80 log10 CFU/mL vs. onset of treatment; p < 0.01). However, regrowth was observed at 24 h (Figure 1C), and was prevented with the addition of 2xMIC vancomycin. Phage/vancomycin treatment also exhibited synergistic activity compared to vancomycin alone and achieved an additional ∆2.21 ± 0.75 log10 CFU/mL reduction at 24 h (Figure 1C, p < 0.05).
Figure 1.
In vitro activity of the phage cocktail against MRSA AW7. (A) Diluted drop tests; (B) Turbidity assays; (C). Time-kill assays in absence and presence of vancomycin. (A) The phage cocktail was serially 10-fold diluted from top to bottom (starting concentration was 1010 PFU/mL). (B) Control without phages (closed black circles); phages at MOI = 0.01 (open red circles), MOI = 0.1 (open red diamonds), MOI = 1 (open red triangles), MOI = 10 (closed red squares), and MOI = 100 (closed red triangles). (C) Time-kill assays were performed by challenging MRSA AW7 with saline (open black circles); phage cocktail at MOI = 1 (closed red triangles), vancomycin at 2×MIC (closed blue diamonds), or a combination of both treatments (closed green squares). Means (±SD) of three independent experiments performed in triplicate are shown in panels B and C. One-way ANOVA with Tukey correction for multiple comparison statistical tests were performed to compare either areas under the curves of curves obtained at MOI = 0.1 (Figure 1B) or 24 h time-points (Figure 1C). CFU, colony forming unit; MIC, minimum inhibitory concentration; MOI, multiplicity of infection; PFU, plaque forming unit. * p < 0.05.
3.2. Subtherapeutic Doses of Vancomycin Synergize with the Phage Cocktail In Vivo
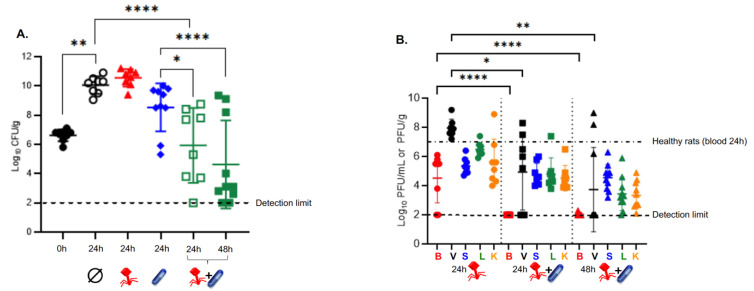
Without treatment, bacterial loads within cardiac vegetations rose from 6.55 ± 0.59 log10 CFU/g at the onset of therapy (i.e., 6 h post-inoculation) to 9.99 ± 0.70 log10 CFU/g after 24 h (Figure 2A, p < 0.01). Administration of either the phage cocktail or subtherapeutic doses of vancomycin failed to control bacterial growth within the vegetations at 24 h (10.55 ± 0.60 log10 CFU/g vs. 8.53 ± 1.65 log10 CFU/g, respectively), compared to the placebo (9.99 ± 0.70 log10 CFU/g) (p = 0.99 and p = 0.59, respectively). When the phage cocktail was administered in combination with subtherapeutic doses of vancomycin, a significant decrease in bacterial load was observed within cardiac vegetations at 24 h compared to placebo (∆4.05 ± 0.94 log10 CFU/g, p < 0.001). This decrease in bacterial load was also superior to that achieved with a subtherapeutic dose of vancomycin alone (5.93 ± 2.56 log10 CFU/g vs. 8.53 ± 1.65 log10 CFU/g, respectively; p < 0.05). Furthermore, phage and vancomycin exhibited synergistic activity to produce a ∆2.60 ± 1.0 log10 CFU/g decrease in bacteria load compared to antibiotic alone. The latter combination remained bacteriostatic at 24 h compared to the onset of therapy (5.93 ± 2.56 log10 CFU/g vs. 6.55 ± 0.59 log10 CFU/g, respectively; p = 0.27). Maximal bacterial killing was achieved when the phage/vancomycin combination was administered for 48 h (∆1.98 ± 0.67 log10 CFU/g decrease compared to the onset of treatment; p = 0.051) (Figure 2A).
Figure 2.
Treatment of EE with the phage cocktail in the presence or absence of a subtherapeutic dose of vancomycin. (A) Bacterial loads in cardiac vegetations measured at 6 h post infection (i.e., 0 h or onset of treatment) in the control rats (closed black circles, n = 8) and 24 h after the onset of treatment in rats given a mock therapy (saline, open black circles, n = 8), the phage cocktail alone for 24 h (closed red triangles, n = 8), a low dose of vancomycin alone for 24 h (closed blue diamonds, n = 10), or the phage cocktail in combination with vancomycin for 24 h (open green squares, n = 8) and 48 h (closed green squares, n = 10). Each symbol represents one animal. (B) In vivo phage pharmacokinetics. Phage concentrations in blood (red), cardiac vegetations (black), spleen (blue), liver (green), and kidneys (orange) from rats 24 h after initiation of treatments with either the phage cocktail alone (left; n = 8) or the phage cocktail and vancomycin combination (middle; n = 8), and 48 h after initiation of treatment with the phage cocktail and vancomycin combination (right; n = 10). The black dotted-dashed line represents the mean concentration of phages at 24 h in the blood of healthy rats treated with the phage cocktail (alone) (n = 3). Means (±SD) are reported. * p < 0.05; ** p < 0.01; **** p < 0.0001; one-way ANOVA with Tukey’s multiple comparisons test.
3.3. Subtherapeutic Doses of Vancomycin Impair the PK Profile of Phage In Vivo
The mean phage concentration determined from the blood of infected rats after a 24-h IV infusion of the phage cocktail did not statistically differ from that determined from the blood of healthy rats (4.53 ± 1.70 log10 PFU/mL vs. 6.90 ± 0.41 log10 PFU/mL, respectively; p = 0.47) (Figure 2B). In contrast, subtherapeutic doses of vancomycin strongly affected the PK profiles of phages in the blood and across the organs tested. For example, there were very few phages recovered from the blood in 1 out of 10 rats 48 h after phage-vancomycin combined therapy (2.02 ± 0.08 log10 PFU/mL vs. 4.53 ± 1.70 log10 PFU/mL for phages alone in infected animals, respectively; p < 0.0001). Furthermore, glycopeptide treatment decreased phage availability within cardiac vegetations by ∆3.03 ± 1.16 log10 PFU/g at 24 h, and by ∆4.33 ± 1.10log10 PFU/g at 48 h (p < 0.05 and p < 0.01, respectively) (Figure 2B).
3.4. The Phage 66-Resistance Phenotype Observed In Vivo Is Not Linked to Genetic Determinants
The best treatment regimen (i.e., phage/vancomycin for 48 h) in this study was not able to completely eradicate bacteria from cardiac vegetations. Therefore, we next investigated the possible role of resistance selection in the persistence of infection. None of the 53 single clones recovered from vegetations of the experimental rats treated with the combination therapy for 48 h displayed increased MIC for vancomycin (data not shown). Six clones out of 53 were still susceptible to phage vB_SauH_2002, developed resistance to phage 66, and were still susceptible to the phage cocktail (SRS pattern, respectively; Supplemental Table S1 and Supplemental Figure S2B). Using clone 17C4-SSS as a reference genome (SSS meaning susceptible to vB_SauH_2002, phage 66, and the cocktail), comparative genomics identified several non-synonymous mutations in five representative SSS clones and the six SRS clones. These mutations are mainly limited to single nucleotide polymorphisms (SNP) or small indels within coding genes and in intergenic regions, with only few leading to frameshifts (Supplemental Tables S2 and S3). Interestingly, all but one mutation were identified in both the SSS and the SRS clones, and were mainly located in genes coding for transposases of the IS4 family (Supplemental Tables S2 and S3). Of note, the SNP leading to Gly18Cys was the only mutation detected in one SRS clone (i.e., clone C11) but not in the SSS clones. The SNP impacts gene 993, which codes for an IS4 transposase (Supplemental Tables S2 and S3, highlighted in red). However, this same transposase was also found to be impacted by two other non-synonymous mutations (leading to Val41Gly and Gly20Asp) present in both the SSS and other SRS clones (Supplemental Tables S2 and S3).
3.5. Despite Efficient Infection, Phage 66 Is Not Able to Control the In Vitro Growth of Planktonic MRSA AW7 Cells
Since phage 66 was found to be more prone to resistance development than phage vB_SauH_2002, we further characterized its in vitro bactericidal activity against MRSA AW7. In double layer assays, phage 66 formed PFU on a lawn of MRSA AW7. Moreover, the PFU were more turbid than the PFU observed for phage vB_SauH_2002 alone, or for the phage cocktail (Supplemental Figure S2A). Interestingly, the PFUs were devoid of surrounding halos, which were previously reported on MSSA Laus102 [14]. Finally, compared to phage vB_SauH_2002, which was able to control the growth of planktonic MRSA AW7 cells in vitro for 24 h at an MOI = 0.1 (Supplemental Figure S3A), phage 66 was ineffective, even at MOI = 100 (Supplemental Figure S3B).
4. Discussion
We recently developed a promising two-phage cocktail, composed of the Herrelleviridae (formerly Myoviridae) phage vB_SauH_2002, and of the Routreeviridae (formerly Podoviridae) phage 66, for the treatment of MSSA EE [14]. Indeed, both phages not only synergized in vitro against the MSSA strain Laus102, but the phage cocktail also strongly synergizes in vivo in a rat model of EE with the standard of care antibiotic flucloxacillin [14]. While the nature of the receptor of vB_SauH_2002 is unknown, S. aureus Myoviridae commonly uses the anionic WTA backbone as a receptor independently to its glycosylation state [30]. In contrast, the β-O-glycosylation of WTA is required for Podoviridae, and therefore, very likely is required for phage 66 to bind to the bacterial surface [14,31]. Although the two-phage cocktail displayed very close in vitro activity in diluted drop tests and turbidity assays against MRSA strain AW7 as MSSA strain Laus102, it could not control bacterial growth in our in vivo rat model of MRSA EE. It has been demonstrated that predicting in vivo results based on in vitro testing is a difficult task in the context of phage therapy [32]. In the present study, a decrease of ∆3.09 ± 0.80 log10 CFU/mL in 4 h was observed for MRSA AW7. Previously, a decrease of ∆4 log10 CFU/mL in 2 h was observed for MSSA Laus102 [14]. Accordingly, a delayed bactericidal effect in time-kill assays was observed for MRSA AW7 in the present study, and this result is consistent with the total lack of efficacy observed for the phage cocktail alone against AW7 in our in vivo model.
In addition, therapeutic differences observed for the phage/antibiotic combination between MRSA and MSSA isolates in animals with EE may partially be due to the impairment of phage PK profiles using vancomycin. It is generally acknowledged that a virulent phage infection leads to a high phage burst (referred to as auto-dosing), and this is a pre-requisite for the efficacy of phage therapy in vivo [33]. Our results further support this assumption, as the concentration of phages within cardiac vegetations was 2 log10 PFU/g lower in the rats infected with MRSA AW7 compared to the animals infected with MSSA Laus102. Even greater reductions in phage titers (i.e., ranging from ∆3 to ∆4.5 log10PFU/g) were observed across the organs that were evaluated compared to the levels previously measured with MSSA Laus102 [14]. As a result, an MOI of 0.001 achieved within the cardiac vegetations in the MRSA AW7 setting was much lower than the MOI of 100 observed with MSSA Laus102 [14]. This result potentially contributed to the observed lack of efficacy of phages alone against MRSA AW7. Indeed, in the turbidity assays, a lack of AW7 growth control by the phage cocktail was already observed at MOI 0.01. Whether an improvement of the phage PK profile would have resulted in higher in situ MOIs, and subsequently a better bactericidal effect against the MRSA strain, remains to be evaluated. However, the latter could prove challenging to investigate, due to current limitations associated with the production of highly concentrated batches of both phages.
The results of the present study confirm that a combined phage/antibiotic treatment regimen has the potential to outperform single treatment [12]. Yet, a lower efficacy of the phage component against MRSA AW7 eventually translated into a significantly lower therapeutic efficacy of the phage/antibiotic combination against MRSA AW7, compared to MSSA Laus102. Bactericidal activity was not achieved with the phage/vancomycin combination treatment, even after 48 h. In contrast, the phage/flucloxacillin combination previously exhibited strong bactericidal activity, with a ∆5.25 log10 CFU/g decrease in bacteria in vegetations after 24 h [14].
The addition of antibiotic strongly affected the PK profile of the phages tested. We believe that this negative effect of vancomycin is likely explained by the killing of hosts that would have otherwise been used by the phages to replicate. Indeed, a negative impact on the so-called auto-dosing capacity of phages had previously been reported [34]. Moreover, even a subtherapeutic dose of vancomycin dramatically reduced the already very low capacity of the phage to replicate in vivo on MRSA AW7. As a result, the concentration of phage reached at 24 h in the vegetations infected with MRSA AW7 was ca. ∆4 log10 PFU/g lower than the concentration reached following infection with MSSA Laus102 under flucloxacillin therapy [14]. There were also no viable phage particles recovered at 24 h from the blood of the MRSA-infected animals, while 4.52 ± 1.70 PFU/mL was previously detected in the blood of animals treated with a combination of phage and flucloxacillin [14]. It remains to be determined whether this result is due to phage/bacteria interactions and/or a class effect of the antibiotic present. In addition, variables regarding the modes of administration of phage and antibiotic should be evaluated. For example, the sequential administration of treatments, which has only occasionally been studied to date [35], could be investigated.
Based on the present results, careful adjustment/personalization of phage cocktail compositions according to the infecting strain, and their use with or without antibiotics, warrants further study. Indeed, our investigation of the activity of both types of phages revealed major differences in their antibacterial activity, particularly for phage 66. In MRSA AW7, turbid lysis was observed in diluted drop tests, and an absence of depolymerase halos was noted around phage 66 PFUs compared to MSSA Laus102 [14]. Moreover, while phage 66 efficiently prevented the in vitro growth of Laus102 for 16 h at low MOIs [14], it was not able to control AW7 in vitro growth, even at an MOI of 100. These results may have contributed to the unfavorable PK profile for the phage cocktail tested in rats infected with MRSA AW7. In future studies, the concentration of each phage needs to be measured separately.
It has been reported that a subset of Laus102 phage 66-resistant variants carry mutations in the tarS coding region of a glycosyltransferase that mediates the beta-O-N-acetylglucosaminylation of wall-teichoic acid (WTA) [14]. However, we did not identify any AW7 phage 66-resistant variants carrying mutations in this region. This was surprising, since tarS mutations, which can result in the removal of beta-O-N-acetylglucosaminylated WTA from the cell wall, have been characterized as a major mechanism of resistance to Podoviridae [36,37]. Furthermore, no specific genetic determinants were found to be associated with the in vivo development of resistance to phage 66 in MRSA AW7. While it is possible that such clones could have been lost during sample processing and/or storage, our observations suggest that resistance to phage 66 is driven by an adaptive phenotypic plasticity in AW7, rather than by genetic mutations. Indeed, it has been demonstrated that variations in bacteriophage activity can occur between different environments, and these are likely to be secondary to different glycosylation patterns of WTA [38,39].
Thus, mechanisms of bacterial resistance to phage may have multiple pathways and components, even within the same bacterial species. Systematic studies of these mechanisms could provide greater insight into possible targets, with the goal of preventing therapeutic failures.
Acknowledgments
We thank Aurélie Marchet, Sabrina Pereira-Pipa, and Nathalie Bonvin for providing outstanding technical assistance.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v14081792/s1, Supplemental Material and Methods, Supplemental Table 1: Phage-resistance patterns of clones recovered in vivo from the vegetations of MRSA AW7-infected rats treated for 48 h with the phage cocktail/vancomycin combination. Supplemental Table 2: Detailed lists of mutations identified in the genomes of representative clones recovered from the vegetations of rats treated for 48 h with the phage cocktail/vancomycin combination. Supplemental Table 3: Summary of unique mutations identified in the genomes of A. SSS and B. SRS clones recovered from the vegetations of rats treated for 48 h with the phage cocktail/vancomycin combination, Supplemental Figure 1: Study design with sampling time points, Supplemental Figure 2: Images of the patterns observed in diluted drop tests for S. aureus AW7 SSS and SRS clones isolated from the cardiac vegetations of rats treated with the phage cocktail/vancomycin combination for 48 h and from which the genome was fully sequenced, Supplemental Figure 3. Activity of phage vB_SauH_2002 and phage 66 against planktonic S. aureus AW7.
Author Contributions
Conceptualization, G.R. Y.-A.Q. and J.E.; methodology, G.R., Y.-A.Q. and J.E.; software: J.S. and G.R.; validation: G.R. and Y.-A.Q.; formal analysis, J.S., G.R. and Y.-A.Q.; investigation, J.S., G.R., and J.E.; resources, G.R. and Y.-A.Q.; data curation, G.R.; writing—original draft preparation, J.S. and G.R.; writing—review and editing, G.R. and Y.-A.Q.; visualization, G.R. and Y.-A.Q.; supervision, G.R.; project administration, Y.-A.Q. and G.R.; funding acquisition, G.R., Y.-A.Q. and J.E. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Swiss National Foundation (grants #320030_176216 and #CR31I3_166124 to Y.-A.Q. and G.R.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Que Y.A., Moreillon P. Infective endocarditis. Nat. Rev. Cardiol. 2011;8:322–336. doi: 10.1038/nrcardio.2011.43. [DOI] [PubMed] [Google Scholar]
- 2.de Kraker M.E., Wolkewitz M., Davey P.G., Grundmann H. Clinical impact of antimicrobial resistance in European hospitals: Excess mortality and length of hospital stay related to methicillin-resistant Staphylococcus aureus bloodstream infections. Antimicrob. Agents Chemother. 2011;55:1598–1605. doi: 10.1128/AAC.01157-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baddour L.M., Baddour L.M., Wilson W.R., Bayer A.S., Fowler V.G., Jr., Tleyjeh I.M., Rybak M.J., Barsic B., Lockhart P.B., Gewitz M.H., et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association. Circulation. 2015;132:1435–1486. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 4.Cremieux A.C., Maziere B., Vallois J.M., Ottaviani M., Azancot A., Raffoul H., Bouvet A., Pocidalo J.J., Carbon C. Evaluation of antibiotic diffusion into cardiac vegetations by quantitative autoradiography. J. Infect Dis. 1989;159:938–944. doi: 10.1093/infdis/159.5.938. [DOI] [PubMed] [Google Scholar]
- 5.Levine D.P., Fromm B.S., Reddy B.R. Slow response to vancomycin or vancomycin plus rifampin in methicillin-resistant Staphylococcus aureus endocarditis. Ann. Intern. Med. 1991;115:674–680. doi: 10.7326/0003-4819-115-9-674. [DOI] [PubMed] [Google Scholar]
- 6.Neely M.N., Youn G., Jones B., Jelliffe R.W., Drusano G.L., Rodvold K.A., Lodise T.P. Are vancomycin trough concentrations adequate for optimal dosing? Antimicrob. Agents Chemother. 2014;58:309–316. doi: 10.1128/AAC.01653-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pfeltz R.F., Wilkinson B.J. The escalating challenge of vancomycin resistance in Staphylococcus aureus. Curr. Drug Targets Infect. Disord. 2004;4:273–294. doi: 10.2174/1568005043340470. [DOI] [PubMed] [Google Scholar]
- 8.Sulakvelidze A., Alavidze Z., Morris J.G., Jr. Bacteriophage therapy. Antimicrob. Agents Chemother. 2001;45:649–659. doi: 10.1128/AAC.45.3.649-659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petrovic Fabijan A., Lin R.C., Ho J., Maddocks S., Ben Zakour N.L., Iredell J.R. Safety of bacteriophage therapy in severe Staphylococcus aureus infection. Nat. Microbiol. 2020;5:465–472. doi: 10.1038/s41564-019-0634-z. [DOI] [PubMed] [Google Scholar]
- 10.Gilbey T., Ho J., Cooley L.A., Fabijan A.P., Iredell J.R. Adjunctive bacteriophage therapy for prosthetic valve endocarditis due to Staphylococcus aureus. Med. J. Aust. 2019;211:142–143.e1. doi: 10.5694/mja2.50274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moelling K., Broecker F., Willy C. A Wake-Up Call: We Need Phage Therapy Now. Viruses. 2018;10:688. doi: 10.3390/v10120688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pirnay J.P., Ferry T., Resch G. Recent progress toward the implementation of phage therapy in Western medicine. FEMS Microbiol. Rev. 2022;46:fuab040. doi: 10.1093/femsre/fuab040. [DOI] [PubMed] [Google Scholar]
- 13.Valente L., Prazak J., Que Y.A., Cameron D.R. Progress and Pitfalls of Bacteriophage Therapy in Critical Care: A Concise Definitive Review. Crit. Care Explor. 2021;3:e0351. doi: 10.1097/CCE.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Save J., Que Y.A., Entenza J.M., Kolenda C., Laurent F., Resch G. Bacteriophages Combined With Subtherapeutic Doses of Flucloxacillin Act Synergistically Against Staphylococcus aureus Experimental Infective Endocarditis. J. Am. Heart Assoc. 2022;11:e023080. doi: 10.1161/JAHA.121.023080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santoro J., Levison M.E. Rat model of experimental endocarditis. Infect. Immun. 1978;19:915–918. doi: 10.1128/iai.19.3.915-918.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heraief E., Glauser M.P., Freedman L.R. Natural history of aortic valve endocarditis in rats. Infect. Immun. 1982;37:127–131. doi: 10.1128/iai.37.1.127-131.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cameron D.R., Ramette A., Prazak J., Entenza J., Haenggi M., Que Y.A., Resch G. Draft Genome Sequence of Methicillin-Resistant Staphylococcus aureus Strain AW7, Isolated from a Patient with Bacteremia. Microbiol. Resour. Announc. 2019;8:e00806–19. doi: 10.1128/MRA.00806-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vouillamoz J., Entenza J.M., Feger C., Glauser M.P., Moreillon P. Quinupristin-dalfopristin combined with beta-lactams for treatment of experimental endocarditis due to Staphylococcus aureus constitutively resistant to macrolide-lincosamide-streptogramin B antibiotics. Antimicrob. Agents Chemother. 2000;44:1789–1795. doi: 10.1128/AAC.44.7.1789-1795.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prazak J., Valente L.G., Iten M., Federer L., Grandgirard D., Soto S., Resch G., Leib S.L., Jakob S.M., Haenggi M., et al. Benefits of aerosolized phages for the treatment of pneumonia due to methicillin-resistant Staphylococcus aureus (MRSA): An experimental study in rats. J. Infect. Dis. 2022;225:1452–1459. doi: 10.1093/infdis/jiab112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valente L.G., Federer L., Iten M., Grandgirard D., Leib S.L., Jakob S.M., Haenggi M., Cameron D.R., Que Y.A., Prazak J. Searching for synergy: Combining systemic daptomycin treatment with localised phage therapy for the treatment of experimental pneumonia due to MRSA. BMC Res. Notes. 2021;14:381. doi: 10.1186/s13104-021-05796-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prazak J., Iten M., Cameron D.R., Save J., Grandgirard D., Resch G., Goepfert C., Leib S.L., Takala J., Jakob S.M., et al. Bacteriophages Improve Outcomes in Experimental Staphylococcus aureus Ventilator-associated Pneumonia. Am. J. Respir. Crit. Care Med. 2019;200:1126–1133. doi: 10.1164/rccm.201812-2372OC. [DOI] [PubMed] [Google Scholar]
- 22.Bae T., Glass E.M., Schneewind O., Missiakas D. Generating a collection of insertion mutations in the Staphylococcus aureus genome using bursa aurealis. Methods Mol. Biol. 2008;416:103–116. doi: 10.1007/978-1-59745-321-9_7. [DOI] [PubMed] [Google Scholar]
- 23.Resch G., François P., Morisset D., Stojanov M., Bonetti E.J., Schrenzel J., Sakwinska O., Moreillon P. Human-to-bovine jump of Staphylococcus aureus CC8 is associated with the loss of a beta-hemolysin converting prophage and the acquisition of a new staphylococcal cassette chromosome. PLoS ONE. 2013;8:e58187. doi: 10.1371/journal.pone.0058187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CLSI . Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically. 11th ed. Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2018. CLSI Standards M07. [Google Scholar]
- 25.Chin J.N., Jones R.N., Sader H.S., Savage P.B., Rybak M.J. Potential synergy activity of the novel ceragenin, CSA-13, against clinical isolates of Pseudomonas aeruginosa, including multidrug-resistant P.aeruginosa. J. Antimicrob. Chemother. 2008;61:365–370. doi: 10.1093/jac/dkm457. [DOI] [PubMed] [Google Scholar]
- 26.Que Y.A., Entenza J.M., Francioli P., Moreillon P. The impact of penicillinase on cefamandole treatment and prophylaxis of experimental endocarditis due to methicillin-resistant Staphylococcus aureus. J. Infect. Dis. 1998;177:146–154. doi: 10.1086/513805. [DOI] [PubMed] [Google Scholar]
- 27.Moreillon P., Bizzini A., Giddey M., Vouillamoz J., Entenza J.M. Vancomycin-intermediate Staphylococcus aureus selected during vancomycin therapy of experimental endocarditis are not detected by culture-based diagnostic procedures and persist after treatment arrest. J. Antimicrob. Chemother. 2012;67:652–660. doi: 10.1093/jac/dkr521. [DOI] [PubMed] [Google Scholar]
- 28.Dell R.B., Holleran S., Ramakrishnan R. Sample size determination. ILAR J. 2002;43:207–213. doi: 10.1093/ilar.43.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Entenza J.M., Veloso T.R., Vouillamoz J., Giddey M., Moreillon P. Failure of Vancomycin Continuous Infusion against Experimental Endocarditis Due to Vancomycin-Intermediate Staphylococcus aureus. Antimicrob. Agents Chemother. 2011;55:385–387. doi: 10.1128/AAC.00811-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xia G., Corrigan R.M., Winstel V., Goerke C., Gründling A., Peschel A. Wall Teichoic Acid-Dependent Adsorption of Staphylococcal Siphovirus and Myovirus. J. Bacteriol. 2011;193:4006–4009. doi: 10.1128/JB.01412-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li X., Gerlach D., Du X., Larsen J., Stegger M., Kühner P., Peschel A., Xia G., Winstel V. An accessory wall teichoic acid glycosyltransferase protects Staphylococcus aureus from the lytic activity of Podoviridae. Sci. Rep. 2015;5:17219. doi: 10.1038/srep17219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henry M., Lavigne R., Debarbieux L. Predicting In Vivo Efficacy of Therapeutic Bacteriophages Used To Treat Pulmonary Infections. Antimicrob. Agents Chemother. 2013;57:5961–5968. doi: 10.1128/AAC.01596-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abedon S.T. Phage therapy dosing: The problem(s) with multiplicity of infection (MOI) Bacteriophage. 2016;6:e1220348. doi: 10.1080/21597081.2016.1220348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abedon S.T. Phage-Antibiotic Combination Treatments: Antagonistic Impacts of Antibiotics on the Pharmacodynamics of Phage Therapy? Antibiotics. 2019;8:182. doi: 10.3390/antibiotics8040182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Torres-Barceló C., Arias-Sánchez F.I., Vasse M., Ramsayer J., Kaltz O., Hochberg M.E. A Window of Opportunity to Control the Bacterial Pathogen Pseudomonas aeruginosa Combining Antibiotics and Phages. PLoS ONE. 2014;9:e106628. doi: 10.1371/journal.pone.0106628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Uchiyama J., Taniguchi M., Kurokawa K., Takemura-Uchiyama I., Ujihara T., Shimakura H., Sakaguchi Y., Murakami H., Sakaguchi M., Matsuzaki S. Adsorption of Staphylococcus viruses S13′ and S24-1 on Staphylococcus aureus strains with different glycosidic linkage patterns of wall teichoic acids. J. Gen. Virol. 2017;98:2171–2180. doi: 10.1099/jgv.0.000865. [DOI] [PubMed] [Google Scholar]
- 37.Ingmer H., Gerlach D., Wolz C. Temperate Phages of Staphylococcus aureus. Microbiol. Spectr. 2019;7:7–5. doi: 10.1128/microbiolspec.GPP3-0058-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mistretta N., Brossaud M., Telles F., Sanchez V., Talaga P., Rokbi B. Glycosylation of Staphylococcus aureus cell wall teichoic acid is influenced by environmental conditions. Sci. Rep. 2019;9:3212. doi: 10.1038/s41598-019-39929-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Doub J.B., Urish K., Lee M., Fackler J. Impact of Bacterial Phenotypic Variation with Bacteriophage therapy: A Pilot Study with Prosthetic Joint Infection Isolates. Int. J. Infect. Dis. 2022;119:44–46. doi: 10.1016/j.ijid.2022.03.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.