Abstract
In the light of the lack of authorized COVID-19 vaccines adapted to the Omicron variant lineage, the administration of the first and second booster dose is recommended. It remains important to monitor the efficacy of such an approach in order to inform future preventive strategies. The present paper summarizes the research progress on the effectiveness of the first and second booster doses of COVID-19. It also discusses the potential approach in vaccination strategies that could be undertaken to maintain high levels of protection during the waves of SARS-CoV-2 infections. Although this approach can be based, with some shortcomings, on the first-generation vaccines, other vaccination strategies should be explored, including developing multiple antigen-based (multivariant-adapted) booster doses with enhanced durability of immune protection, e.g., through optimization of the half-life of generated antibodies.
Keywords: COVID-19, Omicron, booster, vaccine effectiveness
1. Introduction
The Omicron lineage of SARS-CoV-2 (B.1.1.529) was first detected in November 2021 in Botswana and South Africa [1]. It accumulated over 50 sense mutations in the genome, among which approximately thirty induced amino-acid changes in the spike protein, with ten concerning the receptor-binding domain [2]. Such a high number of mutations led to substantial evasion of naturally-acquired and vaccine-induced immunity, ultimately resulting in increased transmissibility [3,4]. Consequently, within several weeks Omicron variant became a predominant SARS-CoV-2 variant circulating globally [5]. As shown, a key feature of Omicron behind this rapid spread was not an increased viral load than for the preceding Delta variant ([6] or higher affinity to the ACE2 receptor [7], but substantial evasion of naturally-acquired and vaccine-induced neutralizing antibodies [8,9]. This had raised concerns over the efficacy of the authorized vaccines designed in 2020, long before the emergence of Omicron, which were using spike protein without the critical changes found in Omicron [10]. The main vaccines used worldwide included mRNA-based vaccines BNT162b2 (BioNTech/Pfizer, Mainz, Germany/New York, NY, USA) and mRNA-1273 (Moderna Therapeutics, Cambridge, MA, USA), adenoviral vector vaccines AZD1222 (Oxford/AstraZeneca, UK/Sweden) and Ad26.COV2.S (Janssen/Johnson & Johnson, Beerse, Belgium/New Brunswick, NJ, USA) and inactivated vaccine CoronaVac (Sinovac, Beijing, China) [10].
On the other hand, the first-generation vaccines remained effective against other variants, such as Delta, which were also characterized by the mutated spike protein [11,12,13]. However, to maintain high levels of protection, a booster strategy has been implemented [14,15]. This decision was also motivated by the observations of the gradual decrease of the antibody levels within several weeks from the last dose [16,17], which increased the odds of breakthrough infections [18].
Since the Omicron-adapted vaccines remain under clinical development [19,20,21], the administration of a booster dose, and recently also a second booster dose, based on the original version of vaccines (the majority of which are mRNA vaccines) have been thus recommended to curb the globally increasing transmission of Omicron variant. Therefore, it remains important to monitor the effect of booster strategies during the dominance of the Omicron lineage and, if necessary, offer some potential future vaccination strategies. It is imperative given that antibody levels following administration of a booster dose also tend to decrease, usually within 3–4 months, while the Omicron variant is, contrary to Delta lineage, better adapted to reduce the recognition of spike protein by T-cells [22]. The evaluation of booster strategies can be performed by assessment of the vaccine’s efficacy which is measured in a controlled clinical trial (by comparing the outcome in vaccinated individuals to those receiving a placebo and calculation of the relative risk), or by evaluation of the vaccine’s effectiveness, which is measured in the real-world studies and allows us to understand how well the vaccines work to protect communities as a whole.
In the present paper, we update the research progress on the effects of the first and second booster doses of COVID-19 and discuss the potential modifications to vaccination strategies to maintain high levels of protection during the future waves of SARS-CoV-2 infections caused by Omicron variant or novel viral lineage that may emerge.
2. The Increased Omicron-Neutralizing Activity of the Booster (Three Doses) Vaccination
The objective of this section was to review the effect that booster COVID-19 vaccination can have on immune responses in the context of the Omicron variant. Due to the substantial genetic mutation in its spike protein [1], Omicron variants exhibit an increased escape from vaccine-induced neutralizing antibodies. This is because the COVID-19 vaccines authorized in 2020/2021 were based on the spike protein of the SARS-CoV-2 version that emerged in Wuhan, China, in late 2019. Subsequently, they poorly match the Omicron lineage. Neutralization of Omicron could even be undetectable in the selected individuals who completed only the primary vaccination course [23]. However, the mRNA vaccine booster elicited neutralizing protection against the Omicron variant [23,24,25,26,27,28]. The mRNA vaccine BNT162b2 (Pfizer) booster substantially increased the neutralizing antibody titers against two major Omicron sub-lineages (BA.1 and BA.2), whereas the corresponding neutralizing antibody titers were lower six months after the initial vaccination [29]. Similarly, Pedersen et al. documented that the serums of participants receiving the homologous BNT162b2 booster can neutralize both Omicron BA.1 and BA.2 isolates [30]. Nemet et al. also reported a substantially increased geometric Omicron-neutralizing titer in the healthy participants receiving the BNT162b2 booster, compared to the low geometric Omicron-neutralizing titer value (in the participants receiving two-dose BNT162b2 vaccine [31]. In a prospective observational study in older nursing home residents (68–98 years old) in France, the BNT162b2 booster dose increased the mean of Omicron-specific neutralizing titers by nearly 2 fold in the SARS-CoV-2-naïve and COVID-19 recovered residents three-months after administration, respectively. The percentage of residents with detectable Omicron-neutralizing antibodies also substantially increased to >80% [32]. Canaday et al. examined the effect of boosting with BNT162b2 mRNA vaccine on humoral immunity and Omicron-specific neutralizing activity among nursing home residents and healthcare workers in the USA, and it was found that the booster administration increased the proportion of participants with detectable Omicron-neutralizations range to 86%, whereas only 28% of participants after full-dose vaccination had the detectable Omicron-specific neutralization activity [33]. Pajon et al. reported that the geometric mean titer level against Omicron variants after one month of mRNA-1273 booster was 20-fold higher than after a month of the primary vaccination course with two-dose mRNA-1273 but rapidly declined by 85% after six months [34]. The inactivated virus vaccine booster substantially increased the neutralizing antibody responses to Omicron lineage variants in a cohort study on the adaptive responses of CoronaVac booster in the healthcare professional receiving the CoronaVac booster nine months after two-dose CoronaVac vaccination. Over 55% of subjects demonstrated the Omicron-neutralizing activities after the boosting dose-the geometric mean titer increased by 2 fold [35]. Moreover, a third dose of the protein subunit vaccine MVC-COV1901 (Medigen Vaccine Biologics Zhubei, Hsinchu County, Taiwan), containing an adjuvanted stable prefusion spike protein of SARS-CoV-2 (similarly to spike protein encoded by the mRNA vaccines), was reported to improve the neutralizing capacity against Omicron [36]. All these studies highlighted the increased neutralizing activity of booster vaccination against Omicron variant despite being lower than that against wildtype variants, as well as the rapid decline over the following months. Moreover, data from studies in non-human primates indicate that boost administration induces comparable immunity and protection against the Omicron variant shortly after administration, regardless of whether an ancestral spike-matched vaccine or Omicron-matched vaccine was used [37].
Additionally, the Omicron-neutralizing activity of the heterologous booster vaccination was also studied. In a subject-blinded, randomized-controlled trial to assess the immunogenicity and safety of heterologous booster COVID-19 vaccination compared with a homologous booster regimen in Singapore, heterologous mRNA-1273 booster vaccination (following a primary course of vaccination with BNT162b2) induced a more robust neutralizing response against the Omicron variant in older individuals compared with homologous BNT62b2 [38]. Wang et al. showed that both the homologous inactivated whole-virion vaccine BBIBP-CorV (Sinopharm, Beijing, China) booster and the heterologous booster with protein subunit vaccine ZF2001 (Anhui Zhifei Longcom Biopharmaceuticals, Hefei, China) considerably increased neutralization titers for Omicron variant [39]. In a phase 4, a non-inferiority, single-blind, randomized study in Brazil, the Omicron-neutralizing capacity was found to substantially increase in the serum samples of the participants who received the primary vaccination regimen of the inactivated virus vaccine CoronaVac and further received a third homologous dose of CoronaVac. However, those who received a third heterologous dose of Ad26.COV2.S, BNT162b2, or AZD1222 had a higher neutralizing response than those who received the homologous booster [40]. Therefore, heterologous immunization with inactivated vaccine followed by mRNA-booster elicits strong immunity against the SARS-CoV-2 Omicron variant [41]. For the population receiving CoronaVac as the primary vaccine, the heterologous booster with other types of vaccines (e.g., mRNA vaccine) can be considered [42]. The summary of reviewed studies in this section is provided in Table 1.
Table 1.
Summary of studies evaluating the Omicron-neutralizing activity of the first COVID-19 vaccine booster.
| Reference | Design | Findings |
|---|---|---|
| [33] |
|
|
| [34] |
|
|
| [35] |
|
|
| [38] |
|
|
| [39] |
|
|
| [40] |
|
|
3. The Increased Effectiveness of the Booster Vaccination (Three Doses) against the Omicron Variant
This section aimed to review the effectiveness of booster COVID-19 vaccination, based on non-Omicron adapted vaccines, in protection against the Omicron variant of SARS-CoV-2. The increased vaccine effectiveness of the booster against Omicron-associated infection has been widely reported. In a prospective observational study including data of 11,690 adults across 21 hospitals in the USA, the effectiveness of mRNA vaccination (BNT162b2 and mRNA-1273) to prevent Delta variant-associated hospitalization was 85% and 94% for two doses and three doses (booster), respectively, whereas the effectiveness of the mRNA vaccination against Omicron variant was 65% and 86% for two doses and booster, respectively [43]. Tartof et al. showed that the nine-month effectiveness of two doses of the BNT162b2 vaccine against hospital admission due to Omicron infection was 41% while against emergency department admission was 31%. However, after three doses, the effectiveness of BNT162b2 against hospital admission due to the Omicron variant was 85% at <3 months but declined to 55% after ≥3 months [44]. In a test-negative case-control design research in England, the increased vaccine effectiveness (67.2%, at 2-4 weeks) of the BNT162b2 (Pfizer) booster dose against the Omicron variant was observed among patients who received full-dose BNT162b2 vaccination, and the vaccine effectiveness declined to 45.7% at ≥10 weeks [45]. Likewise, in a large, test-negative case-control study in California, USA, the increased vaccine effectiveness (71.6%) of the mRNA-1273 vaccine booster against Omicron infection was observed in participants at 14–60 days after the booster. However, the booster vaccine effectiveness decreased to 47.4% at >60 days [46]. Šmíd et al. showed that the vaccine effectiveness of a recent booster in the Czech Republic increased to 56% against Omicron infection and increased to 87% against Omicron hospitalization, whereas the vaccine effectiveness of the primary course of vaccination against Omicron hospitalization was 45% [47]. Ferdinands et al. showed that during the Omicron period, the booster vaccine effectiveness against COVID-19-associated emergency department/urgent care visits and hospitalizations increased to 87% and 91%, respectively, during the first two months after the booster, but declined to 66% and 78%, respectively, by the fourth month after the booster [48]. Butt et al. showed that vaccine effectiveness of booster vaccination relative to primary vaccination series (relative vaccine effectiveness) was 19%, 52%, and 83% for confirmed infection, hospitalization, admission to intensive care unit, or death, respectively. Despite the relatively low vaccine effectiveness of mRNA booster vaccine dose against the Omicron infection, the booster administration provides substantial protection from hospitalization and performs well in preventing the most severe/critical forms of the disease [49]. Modes et al. showed that the likelihoods of both intensive care unit admission and death during the Omicron-predominant period were lowest among adults who had received a booster dose, highlighting the importance of booster vaccination [50]. Additionally, Plumb et al. also reported that during the Omicron-predominant period, the estimated vaccine effectiveness against reinfection-associated hospitalization increased to 68% after a booster dose from 35% after two-dose primary vaccination [51].
Although the primary course of vaccination was based on various vaccines, the booster strategies were mostly based on mRNA vaccinations [10]. As a result, some individuals were receiving heterologous booster vaccines making it necessary to understand the safety, immunogenicity, and efficacy of such an approach [52,53,54,55]. In relation to the Omicron variant, Accorsi et al. showed that all three studied booster regimens (Ad26.COV2.S/Ad26.COV2.S, Ad26.COV2.S/mRNA, and mRNA/mRNA/mRNA) protected against symptomatic infection, while the highest vaccine effectiveness occurred in the regimens (Ad26.COV2.S/mRNA and mRNA/mRNA/mRNA) that included a booster dose of an mRNA vaccine [56]. The lowest vaccine effectiveness was observed with the homologous Ad26.COV2.S/Ad26.COV2.S booster [56]. In the retrospective cohort studies in Qatar, Abu–Raddad et al. reported decreased cumulative incidences (2.4% and 1.0%) of symptomatic Omicron infection in the homologous BNT162b2 and mRNA-1273 booster cohort, respectively, compared to those (4.5% and 1.9%) of corresponding non-booster cohorts [57]. The effectiveness of the BNT162b2 and mRNA-1273 booster against symptomatic Omicron infection was estimated to be 49.4% and 47.3%, respectively [57]. In a test-negative design using consolidated national administrative data in Malaysia, Suah et al. compared the effectiveness of homologous and heterologous BNT162b2, CoronaVac, and AZD1222 booster vaccination against Delta and Omicron infection (heterologous booster vaccinations: (i) 2 × CoronaVac + 1 × BNT162b, (ii) 2 × CoronaVac + 1 × AZD122, and (iii) 2 × AZD122 + 1 × BNT162b), boosting was associated with the higher adjusted marginal effectiveness values, and a BNT162b2 booster was recommended for the subjects receiving the primary regimen with inactivated and vectored vaccines [58]. Analyzing 80,287 emergency department/urgent care visits and 25,244 hospitalizations among adults across 10 US states during the Omicron predominance period (16 December 2021–7 March 2022), Natarajan et al. reported that the effectiveness of heterologous booster practice (1 × Ad26.COV2.S/1 × mRNA dose) against emergency department/urgent care visits and hospitalization (79% and 78%, respectively) were higher than those (54% and 67%, respectively) of the homologous Ad26.COV2.S booster vaccination (2 × Ad26.COV2.S). However, they were lower than those of 3 × mRNA doses (83% and 90%, respectively). Therefore, the vaccinees receiving Janssen primary vaccine should preferentially receive the mRNA vaccine booster to improve the protection against Omicron [59]. All these studies demonstrated the increased vaccine effectiveness of the existing vaccine booster against the Omicron variant, especially the heterologous booster vaccination, compared to primary vaccination with the non-mRNA vaccine. Therefore, the mRNA vaccine booster was recommended for the individuals who previously received the non-mRNA primary vaccination.
All in all, the administration of a booster dose of the first-generation COVID-19 vaccines increases the protection level against Omicron infection and hospitalization. However, this protection declined compared to that against other SARS-CoV-2 variants. As shown through clinical trials and real-world observations, the efficacy of the primary course of vaccination against variants circulating in 2020 and the first half of 2021 was higher than the efficacy against Omicron lineage after a booster administration [11,18,60,61,62,63,64,65]. Moreover, the level of protection from infection and hospitalization tends to decrease three-four months after administration [44,48,65,66]. As recently summarized by Higdon et al., the effectiveness of booster vaccination against Omicron one month after its administration was higher for all outcomes compared to the effectiveness of the primary vaccine course against the same variant. However, as estimated using random-effects meta-regression, effectiveness against symptomatic infection decreased by 24% within the first four months and by 5% in relation to protection from hospitalization, with further decrease projected by six months [44]. The summary of reviewed studies in this section is provided in Table 2.
Table 2.
Summary of studies evaluating the effectiveness of the first COVID-19 vaccine booster against the Omicron variant.
| Reference | Design | Findings |
|---|---|---|
| [43] |
|
|
| [44] |
|
|
| [45] |
|
|
| [46] |
|
|
| [47] |
|
|
| [48] |
|
|
| [49] |
|
|
| [56] |
|
|
| [57] |
|
|
| [58] |
|
|
| [59] |
|
|
4. Fourth Dose–What Is the Evidence So Far?
This section’s objective was to review the studies reporting on the effect of administration of an additional booster dose (second booster) of the COVID-19 vaccine not adapted specifically to match Omicron lineage. On 29 March 2022, in response to growing concerns about a rapid decline in the Omicron-neutralizing activity of the booster, the Food and Drug Administration (FDA) authorized a second booster dose of either BNT162b2 or mRNA-1273 vaccines for older persons and immunocompromised individuals who are considered high-risk populations for severe COVID-19. This additional shot is the fourth vaccine dose for immunocompetent people, and for patients with a weakened immune system, it is the fifth due to the three-dose primary vaccination. FDA authorization was followed immediately by a recommendation from the Centers for Disease Control and Prevention to allow eligible persons to receive a second booster dose. Both institutions decided without consulting their vaccine advisory committees, which is an unusual procedure, explaining it as the growing threat of a wave of BA.2 omicron variant infections. A second booster dose of BNT162b2 or mRNA-1273 was recommended for persons 50 years of age and older at least four months after the last shot of any already-approved COVID-19 vaccine. In addition, the BNT162b2 vaccine may be administered on the same schedule to individuals 12 years of age and older following solid organ transplantation or with an equivalent degree of immunodeficiency. Recommendations for the fourth dose of the vaccine were based on published findings from Israel suggesting better protection against the severe course of the disease and no safety issues [67,68]. Israel became the first country worldwide to begin using the fourth dose of the BNT162b2 vaccine in January 2022. According to the regulations, this was offered to health care professionals and adults over 60 years [69].
The effect of additional booster dose administration based on the first-generation COVID-19 vaccines was already a subject of selected real-world studies and prospective, open-label, non-randomized studies (Table 3) [67,68,70]. The latter evaluated both mRNA vaccine formulations, BNT162b2 and mRNA-1273, administered to Israeli medical staff vaccinated with the third dose of BNT162b2 at least four months earlier with IgG antibody levels equal to or lower than 700 BAU/mL [67]. The analysis included 1050 health care workers, 154 persons received the fourth dose of the BNT162b2 vaccine, and another 120 received the mRNA-1273 vaccine one week later. The control group consisted of the age-matched individuals meeting the same eligibility criteria, two for each vaccine recipient. All participants were screened weekly for SARS-CoV-2 infection by PCR testing. Both formulations induced a 9–10-fold increase in IgG antibodies against the SARS-CoV-2 receptor-binding domain and neutralizing antibody titers within two weeks after vaccination. There was also an 8–10-fold increase in live neutralization against the Omicron and other variant strains with titer restoration to the peak after the third dose of BNT162b2n. Compared to controls, the efficacy against SARS-CoV-2 infection compared to controls was 30% and 11% for BNT162b2 and mRNA-1273, respectively. Although sequencing of the infecting virus was not performed, the omicron variant accounted for 100% of the isolates typed during the study period, so it can be assumed that it was responsible for breakthrough infections. The higher protection was documented against symptomatic COVID-19, 43% and 31% for BNT162b2 and mRNA-1273, respectively, compared to controls. However, the authors emphasized that within the wide confidence intervals of the estimates, the vaccine’s effectiveness in protecting against symptomatic disease did not exceed 65%. Therefore, the incidence of breakthrough infections, mostly mild, was high. The study also demonstrated that the fourth dose of mRNA vaccine was safe despite triggering mild systemic and local symptoms in most recipients.
Table 3.
Summary of studies evaluating immunogenicity and efficacy/effectiveness of the second booster of COVID-19 vaccine.
| Reference | Design | Findings |
|---|---|---|
| [67] | Prospective, open-label, non-randomized study Participants–healthcare workers ≥ 18Arms treatment arm
|
Immunogenicity and efficacy
|
| [68] | Retrospective real-world population-based study Participants ≥ 60 yrs
|
Effectiveness
|
| [70] | Retrospective real-world population-based study Participants ≥ 60 yrs
|
Effectiveness–protection assessed 7–30 days and 14–30 days after 4th dose against
|
Although in the study by Regev–Yochay et al. [67], including only healthcare workers, the primary endpoints were immunogenicity of the fourth dose of mRNA vaccines and their safety, and the secondary endpoint was efficacy, the studies published later focused on older adults and evaluated only the clinical effects of administering the fourth dose of BNT162b2 vaccine [68,70].
For the purpose of the analysis conducted by Bar-On et al., data were obtained from the Israeli Ministry of Health database between 10 January through 2 March 2022, covering the period of the dominance of the omicron variant, B.1.1.529. The records of 1,252,331 individuals over 60 years who were eligible for the fourth dose of BNT162b2 were analyzed. The risk of both confirmed SARS-CoV-2 infection and severe COVID-19 was assessed in the patients who received the fourth dose compared to the population after three doses of the vaccine. The incidence of confirmed SARS-CoV-2 infection was lower with the fourth dose by a factor of 2.0 compared to only three doses and by a factor of 1.8 compared to the internal control group consisting of patients 3–5 days after the fourth dose of BNT162b2.
The four-dose group achieved a lower rate of severe COVID-19 by a factor of 3.5 and 2.3 compared to that in the three-dose group and the internal control group, respectively. In addition, protection against confirmed SARS-CoV-2 infection waned with time, whereas the prevention of severe disease was stable over six weeks. However, the analysis did not include other endpoints, such as the risk of hospitalization and death. Another limitation of the study was that it did not consider the impact of comorbidities, which are independent risk factors for severe COVID-19.
The assessment of the efficacy of the fourth dose of the BNT162b2 vaccine, considering the risk of confirmed SARS-CoV-2 infection, symptomatic and severe disease, hospitalization, and death due to COVID-19, was performed by Magen et al. [70]. This observational study from Israel was conducted among individuals aged ≥60 from 3 January through 18 February 2022. Individuals who previously had not been infected with SARS-CoV-2 and received a fourth dose of the vaccine were compared with the population vaccinated with a third dose at least four months earlier by individually selecting subjects based on sociodemographic and clinical variables. Data of 182,122 matched pairs of patients from medical records of the largest Israeli health care organization was included in the analysis. Relative vaccine efficacy assessed 14 to 30 days after the fourth dose for protection against SARS-CoV-2 infection, symptomatic COVID-19, hospitalization, severe disease, and death was 52%, 61%, 72%, 64%, and 76%, respectively. A limitation of this study was that the follow-up time was too short to assess the long-term effect of the fourth dose.
In summary, the existing studies demonstrate that administering the second booster dose increases the protection levels against all outcomes related to the Omicron variant (Table 3). However, it is also clear that this effectiveness is reduced due to antigen mismatch between vaccines and circulating viral variants. This mismatch also increased with the emergence of BA.4 and BA.5 subvariants [71] and will likely continue due to the evolution of SARS-CoV-2. The use of first-generation vaccines, which are readily available, can temporarily improve protection levels–a necessity especially during the predicted future waves of SARS-CoV-2 infections (e.g., during the autumn-winter season in the USA and Europe [72,73]).
5. Conclusions
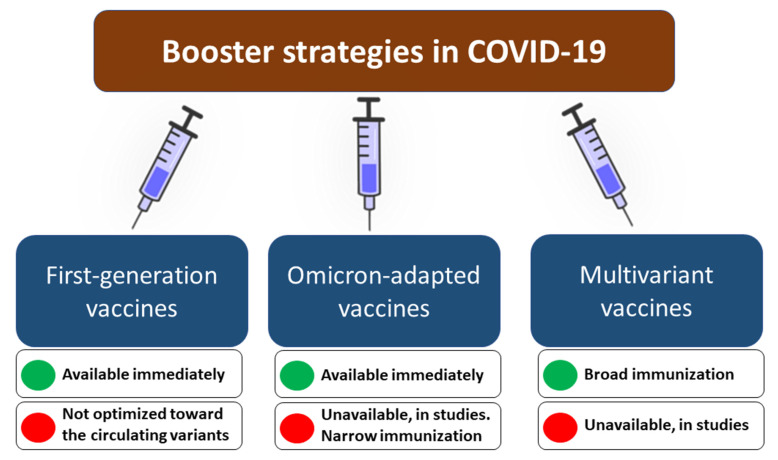
Although the COVID-19 vaccination remains pivotal in decreasing the overall COVID-19 burden and suppressing SARS-CoV-2 evolution [74,75], it is essential to recognize that receiving the primary course vaccination does not protect sufficiently against infection with the Omicron lineage variant. The booster vaccination increases Omicron-neutralizing activity, thereby improving the effectiveness of preventing Omicron-associated infection, symptomatic and severe disease, hospitalization, and death. However, this effect wanes over time due to a gradual decrease in antibody levels three to four months after booster administration, while the vaccine-induced T-cells responses to spike protein of the Omicron variant are lower than to preceding SARS-CoV-2 variants. We outline the potential strategies that could be considered in order to maintain high levels of protection during future waves of SARS-CoV-2 (Figure 1). One should however bear in mind that in any case, the risk/benefit ratio must be analyzed before recommending the booster vaccination [52,76,77,78].
Figure 1.
The potential booster vaccination strategies in COVID-19 to maintain high protection levels during future SARS-CoV-2 infection waves with their advantages and disadvantages.
Offering an additional (second) booster dose of the first generation before the expected wave. This approach has potential limitations in the long-term effectiveness since first-generation vaccines are not adapted to a heavily mutated spike protein of the Omicron variant, while novel sublineages of this variant (i.e., BA4, BA5), with high immune evasion, are emerging [71]. The necessity for repeated vaccinations may be met with increasing unwillingness and hesitancy–the share of individuals vaccinated with subsequent doses may gradually decrease.
Development and use of Omicron-adapted booster dose before the expected wave. This approach would likely increase the specificity of the responses against the Omicron lineage but also does not come without challenges. Firstly, the Omicron variant continues to evolve, and its novel sublineages, characterized by enhanced transmissibility, are characterized by some unique mutations increasing antibody evasion [79,80]. The question remains which variant of spike protein should be selected as an antigen for such a booster vaccine. Furthermore, studies show that despite the Omicron dominance, other SARS-CoV-2 variants, including Delta, remain in cryptic circulation [81]. If one considers the asymmetric cross-immunization in which a person with a history of Omicron infection is four-fold less protected from Delta infection than protection from Omicron in a Delta-immunized individual [82,83], basing booster strategy on the vaccine adapted only to the Omicron variant could bring the potential risk of contracting other SARS-CoV-2 variants.
Development and use of multiple antigen-based (multivariant-adapted) booster dose before the expected wave. This approach would possibly allow inducing a broad immunity against various variants, including Delta, Omicron, Beta, and others. This approach is used against influenza, with trivalent and quadrivalent vaccines targeting three and four strains of the virus, respectively [84]. However, it also comes with some shortcomings. Firstly, the chemical inactivation of SARS-CoV-2 has been shown to induce a transformation of prefusion conformation of spike protein to form resembling postfusion conformation, which is less immunogenic [85]. This challenge can be overcome by developing multivalent subunit vaccines, but their production is longer and more expensive [86]. A more cost- and time-efficient approach would involve the development of multivariant mRNA vaccines. However, these vaccines would require using more than one mRNA molecule to encode different versions of the spike protein. Whether using multiple mRNA molecules in a single-dose vaccine would affect translation efficiency, immunogenicity, and efficacy remain to be understood. There is, however, some evidence that such an approach may provide a broad neutralizing immunity against different SARS-CoV-2 variants, as shown in vivo for mRNA-1273.211 comprising a 1:1 mix of mRNA-1273 (present in the first-generation vaccine developed by Moderna, USA) and mRNA-1273.351 (adapted to Beta variant) [87,88]. More publicly available data is required to understand whether mRNA vaccines adapted to different SARS-CoV-2 variants, including Omicron, are providing efficient protection.
Development of vaccines providing broad immune responses with enhanced durability. The main challenge of currently available COVID-19 vaccines is related to a gradual decrease of antibody levels observed within a few months from dose administration [16]. Although a booster dose temporarily restores antibody levels and strengthens cellular responses [89], the provided protection from different outcomes (including infections and hospital admission) of Omicron infection starts to wane after three-four months from administration [44,48,66]. It becomes more and more evident that vaccine strategies that would increase the durability of protection are necessary. This requires more studies to understand which amino acid substitutions could extend the half-life of antibodies but not decrease their neutralization activities and then design an antigen that would trigger their production. Moreover, some promise is also brought with vaccine candidates based on self-amplifying RNAs (saRNA), which enhance antigen presentation and may therefore mount a robust adaptive immune response against SARS-CoV-2 [90,91]. Further studies are required to understand whether saRNA can enhance the durability of protection.
Acknowledgments
Not applicable.
Author Contributions
Conceptualization, D.Z.-M., P.R. and R.F.; writing—original draft preparation, D.Z.-M., C.H., P.R. and R.F.; writing—review and editing, C.H., P.R. and M.B.; supervision, P.R.; All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Viana R., Moyo S., Amoako D.G., Tegally H., Scheepers C., Althaus C.L., Anyaneji U.J., Bester P.A., Boni M.F., Chand M., et al. Rapid Epidemic Expansion of the SARS-CoV-2 Omicron Variant in Southern Africa. Nature. 2022;603:679–686. doi: 10.1038/s41586-022-04411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ou J., Lan W., Wu X., Zhao T., Duan B., Yang P., Ren Y., Quan L., Zhao W., Seto D., et al. Tracking SARS-CoV-2 Omicron Diverse Spike Gene Mutations Identifies Multiple Inter-Variant Recombination Events. Signal Transduct. Target. Ther. 2022;7:138. doi: 10.1038/s41392-022-00992-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Araf Y., Akter F., Tang Y.-D., Fatemi R., Parvez M.S.A., Zheng C., Hossain M.G. Omicron Variant of SARS-CoV-2: Genomics, Transmissibility, and Responses to Current COVID-19 Vaccines. J. Med. Virol. 2022;94:1825–1832. doi: 10.1002/jmv.27588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCallum M., Czudnochowski N., Rosen L.E., Zepeda S.K., Bowen J.E., Walls A.C., Hauser K., Joshi A., Stewart C., Dillen J.R., et al. Structural Basis of SARS-CoV-2 Omicron Immune Evasion and Receptor Engagement. Science. 2022;375:864–868. doi: 10.1126/science.abn8652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tracking SARS-CoV-2 Variants. [(accessed on 26 June 2022)]. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants.
- 6.Puhach O., Adea K., Hulo N., Sattonnet P., Genecand C., Iten A., Bausch F.J., Kaiser L., Vetter P., Eckerle I., et al. Infectious Viral Load in Unvaccinated and Vaccinated Patients Infected with SARS-CoV-2 WT, Delta and Omicron. bioRxiv. 2022 doi: 10.1101/2022.01.10.22269010. [DOI] [PubMed] [Google Scholar]
- 7.Wu L., Zhou L., Mo M., Liu T., Wu C., Gong C., Lu K., Gong L., Zhu W., Xu Z. SARS-CoV-2 Omicron RBD Shows Weaker Binding Affinity than the Currently Dominant Delta Variant to Human ACE2. Signal Transduct. Target. Ther. 2022;7:8. doi: 10.1038/s41392-021-00863-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arora P., Zhang L., Rocha C., Sidarovich A., Kempf A., Schulz S., Cossmann A., Manger B., Baier E., Tampe B., et al. Comparable Neutralisation Evasion of SARS-CoV-2 Omicron Subvariants BA.1, BA.2, and BA.3. Lancet Infect. Dis. 2022;22:766–767. doi: 10.1016/S1473-3099(22)00224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu L., Iketani S., Guo Y., Chan J.F.-W., Wang M., Liu L., Luo Y., Chu H., Huang Y., Nair M.S., et al. Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2. Nature. 2022;602:676–681. doi: 10.1038/s41586-021-04388-0. [DOI] [PubMed] [Google Scholar]
- 10.Mohamed K., Rzymski P., Islam M.S., Makuku R., Mushtaq A., Khan A., Ivanovska M., Makka S.A., Hashem F., Marquez L., et al. COVID-19 Vaccinations: The Unknowns, Challenges, and Hopes. J. Med. Virol. 2022;94:1336–1349. doi: 10.1002/jmv.27487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sikora D., Rzymski P. COVID-19 Vaccination and Rates of Infections, Hospitalizations, ICU Admissions, and Deaths in the European Economic Area during Autumn 2021 Wave of SARS-CoV-2. Vaccines. 2022;10:437. doi: 10.3390/vaccines10030437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grannis S.J., Rowley E.A., Ong T.C., Stenehjem E., Klein N.P., DeSilva M.B., Naleway A.L., Natarajan K., Thompson M.G. VISION Network Interim Estimates of COVID-19 Vaccine Effectiveness against COVID-19-Associated Emergency Department or Urgent Care Clinic Encounters and Hospitalizations among Adults during SARS-CoV-2 B.1.617.2 (Delta) Variant Predominance—Nine States, June-August 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1291–1293. doi: 10.15585/mmwr.mm7037e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nasreen S., Chung H., He S., Brown K.A., Gubbay J.B., Buchan S.A., Fell D.B., Austin P.C., Schwartz K.L., Sundaram M.E., et al. Effectiveness of COVID-19 Vaccines against Symptomatic SARS-CoV-2 Infection and Severe Outcomes with Variants of Concern in Ontario. Nat. Microbiol. 2022;7:379–385. doi: 10.1038/s41564-021-01053-0. [DOI] [PubMed] [Google Scholar]
- 14.Andrews N., Stowe J., Kirsebom F., Toffa S., Sachdeva R., Gower C., Ramsay M., Lopez Bernal J. Effectiveness of COVID-19 Booster Vaccines against COVID-19-Related Symptoms, Hospitalization and Death in England. Nat. Med. 2022;28:831–837. doi: 10.1038/s41591-022-01699-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rzymski P., Camargo C.A., Jr., Fal A., Flisiak R., Gwenzi W., Kelishadi R., Leemans A., Nieto J.J., Ozen A., Perc M., et al. COVID-19 Vaccine Boosters: The Good, the Bad, and the Ugly. Vaccines. 2021;9:1299. doi: 10.3390/vaccines9111299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shrotri M., Navaratnam A.M.D., Nguyen V., Byrne T., Geismar C., Fragaszy E., Beale S., Fong W.L.E., Patel P., Kovar J., et al. Spike-Antibody Waning after Second Dose of BNT162b2 or ChAdOx1. Lancet. 2021;398:385–387. doi: 10.1016/S0140-6736(21)01642-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yamayoshi S., Yasuhara A., Ito M., Akasaka O., Nakamura M., Nakachi I., Koga M., Mitamura K., Yagi K., Maeda K., et al. Antibody Titers against SARS-CoV-2 Decline, but Do Not Disappear for Several Months. EClinicalMedicine. 2021;32:100734. doi: 10.1016/j.eclinm.2021.100734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rzymski P., Pazgan-Simon M., Kamerys J., Moniuszko-Malinowska A., Sikorska K., Wernik J., Zarębska-Michaluk D., Supronowicz Ł., Sobala-Szczygieł B., Skrzat-Klapaczyńska A., et al. Severe Breakthrough COVID-19 Cases during Six Months of Delta Variant (B.1.617.2) Domination in Poland. Vaccines. 2022;10:557. doi: 10.3390/vaccines10040557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.A Study to Evaluate the Immunogenicity and Safety of Omicron Variant Vaccines in Comparison With MRNA-1273 Booster Vaccine for COVID-19. [(accessed on 26 June 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT05249829.
- 20.Board Members Pfizer and BioNTech Initiate Study to Evaluate Omicron-Based COVID-19 Vaccine in Adults 18 to 55 Years of Age. [(accessed on 26 June 2022)]. Available online: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-initiate-study-evaluate-omicron-based.
- 21.SINOVAC: Supply Vaccines to Eliminate Human Diseases. [(accessed on 26 June 2022)]. Available online: http://www.sinovac.com/news/shownews.php?id=1448&lang=en.
- 22.De Marco L., D’Orso S., Pirronello M., Verdiani A., Termine A., Fabrizio C., Capone A., Sabatini A., Guerrera G., Placido R., et al. Assessment of T-Cell Reactivity to the SARS-CoV-2 Omicron Variant by Immunized Individuals. JAMA Netw. Open. 2022;5:e2210871. doi: 10.1001/jamanetworkopen.2022.10871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garcia-Beltran W.F., St Denis K.J., Hoelzemer A., Lam E.C., Nitido A.D., Sheehan M.L., Berrios C., Ofoman O., Chang C.C., Hauser B.M., et al. MRNA-Based COVID-19 Vaccine Boosters Induce Neutralizing Immunity against SARS-CoV-2 Omicron Variant. Cell. 2022;185:457–466.e4. doi: 10.1016/j.cell.2021.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ariën K.K., Heyndrickx L., Michiels J., Vereecken K., Van Lent K., Coppens S., Willems B., Pannus P., Martens G.A., Van Esbroeck M., et al. Three Doses of BNT162b2 Vaccine Confer Neutralising Antibody Capacity against the SARS-CoV-2 Omicron Variant. NPJ Vaccines. 2022;7:35. doi: 10.1038/s41541-022-00459-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lusvarghi S., Pollett S.D., Neerukonda S.N., Wang W., Wang R., Vassell R., Epsi N.J., Fries A.C., Agan B.K., Lindholm D.A., et al. SARS-CoV-2 BA.1 Variant Is Neutralized by Vaccine Booster-Elicited Serum but Evades Most Convalescent Serum and Therapeutic Antibodies. Sci. Transl. Med. 2022;14:eabn8543. doi: 10.1126/scitranslmed.abn8543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hastert F.D., Hein S., von Rhein C., Benz N.I., Husria Y., Oberle D., Maier T.J., Hildt E., Schnierle B.S. The SARS-CoV-2 Variant Omicron Is Able to Escape Vaccine-Induced Humoral Immune Responses, but Is Counteracted by Booster Vaccination. Vaccines. 2022;10:794. doi: 10.3390/vaccines10050794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Gils M.J., Lavell A., van der Straten K., Appelman B., Bontjer I., Poniman M., Burger J.A., Oomen M., Bouhuijs J.H., van Vught L.A., et al. Antibody Responses against SARS-CoV-2 Variants Induced by Four Different SARS-CoV-2 Vaccines in Health Care Workers in the Netherlands: A Prospective Cohort Study. PLoS Med. 2022;19:e1003991. doi: 10.1371/journal.pmed.1003991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belik M., Jalkanen P., Lundberg R., Reinholm A., Laine L., Väisänen E., Skön M., Tähtinen P.A., Ivaska L., Pakkanen S.H., et al. Comparative Analysis of COVID-19 Vaccine Responses and Third Booster Dose-Induced Neutralizing Antibodies against Delta and Omicron Variants. Nat. Commun. 2022;13:2476. doi: 10.1038/s41467-022-30162-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yu J., Collier A.-R.Y., Rowe M., Mardas F., Ventura J.D., Wan H., Miller J., Powers O., Chung B., Siamatu M., et al. Neutralization of the SARS-CoV-2 Omicron BA.1 and BA.2 Variants. N. Engl. J. Med. 2022;386:1579–1580. doi: 10.1056/NEJMc2201849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pedersen R.M., Bang L.L., Madsen L.W., Sydenham T.V., Johansen I.S., Jensen T.G., Justesen U.S., Andersen T.E. Serum Neutralization of SARS-CoV-2 Omicron BA.1 and BA.2 after BNT162b2 Booster Vaccination. Emerg. Infect. Dis. 2022;28:1274–1275. doi: 10.3201/eid2806.220503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nemet I., Kliker L., Lustig Y., Zuckerman N., Erster O., Cohen C., Kreiss Y., Alroy-Preis S., Regev-Yochay G., Mendelson E., et al. Third BNT162b2 Vaccination Neutralization of SARS-CoV-2 Omicron Infection. N. Engl. J. Med. 2022;386:492–494. doi: 10.1056/NEJMc2119358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alidjinou E.K., Demaret J., Corroyer-Simovic B., Labreuche J., Goffard A., Trauet J., Lupau D., Miczek S., Vuotto F., Dendooven A., et al. Immunogenicity of BNT162b2 Vaccine Booster against SARS-CoV-2 Delta and Omicron Variants in Nursing Home Residents: A Prospective Observational Study in Older Adults Aged from 68 to 98 Years. Lancet Reg. Health Eur. 2022;17:100385. doi: 10.1016/j.lanepe.2022.100385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Canaday D.H., Oyebanji O.A., White E., Keresztesy D., Payne M., Wilk D., Carias L., Aung H., St Denis K., Sheehan M.L., et al. COVID-19 Vaccine Booster Dose Needed to Achieve Omicron-Specific Neutralisation in Nursing Home Residents. EBioMedicine. 2022;80:104066. doi: 10.1016/j.ebiom.2022.104066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pajon R., Doria-Rose N.A., Shen X., Schmidt S.D., O’Dell S., McDanal C., Feng W., Tong J., Eaton A., Maglinao M., et al. SARS-CoV-2 Omicron Variant Neutralization after MRNA-1273 Booster Vaccination. N. Engl. J. Med. 2022;386:1088–1091. doi: 10.1056/NEJMc2119912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen Y., Chen L., Yin S., Tao Y., Zhu L., Tong X., Mao M., Li M., Wan Y., Ni J., et al. The Third Dose of CoronVac Vaccination Induces Broad and Potent Adaptive Immune Responses That Recognize SARS-CoV-2 Delta and Omicron Variants. Emerg. Microbes Infect. 2022;11:1524–1536. doi: 10.1080/22221751.2022.2081614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hsieh S.-M., Chang S.-C., Cheng H.-Y., Shih S.-R., Lien C.E. Durability and Immunogenicity of Neutralizing Antibodies Response against Omicron Variants after Three Doses of Subunit SARS-CoV-2 Vaccine MVC-COV1901: An Extension to an Open-Label, Dose-Escalation Phase 1 Study. Infect. Dis. Ther. 2022;11:1493–1504. doi: 10.1007/s40121-022-00652-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gagne M., Moliva J.I., Foulds K.E., Andrew S.F., Flynn B.J., Werner A.P., Wagner D.A., Teng I.-T., Lin B.C., Moore C., et al. MRNA-1273 or MRNA-Omicron Boost in Vaccinated Macaques Elicits Similar B Cell Expansion, Neutralizing Responses, and Protection from Omicron. Cell. 2022;185:1556–1571.e18. doi: 10.1016/j.cell.2022.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poh X.Y., Tan C.W., Lee I.R., Chavatte J.-M., Fong S.-W., Prince T., Hartley C., Yeoh A.Y.-Y., Rao S., Chia P.Y., et al. Antibody Response of Heterologous vs Homologous MRNA Vaccine Boosters against the SARS-CoV-2 Omicron Variant: Interim Results from the PRIBIVAC Study, A Randomized Clinical Trial. Clin. Infect. Dis. 2022:345. doi: 10.1093/cid/ciac345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X., Zhao X., Song J., Wu J., Zhu Y., Li M., Cui Y., Chen Y., Yang L., Liu J., et al. Homologous or Heterologous Booster of Inactivated Vaccine Reduces SARS-CoV-2 Omicron Variant Escape from Neutralizing Antibodies. Emerg. Microbes Infect. 2022;11:477–481. doi: 10.1080/22221751.2022.2030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Costa Clemens S.A., Weckx L., Clemens R., Almeida Mendes A.V., Ramos Souza A., Silveira M.B.V., da Guarda S.N.F., de Nobrega M.M., de Moraes Pinto M.I., Gonzalez I.G.S., et al. Heterologous versus Homologous COVID-19 Booster Vaccination in Previous Recipients of Two Doses of CoronaVac COVID-19 Vaccine in Brazil (RHH-001): A Phase 4, Non-Inferiority, Single Blind, Randomised Study. Lancet. 2022;399:521–529. doi: 10.1016/S0140-6736(22)00094-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zuo F., Abolhassani H., Du L., Piralla A., Bertoglio F., de Campos-Mata L., Wan H., Schubert M., Cassaniti I., Wang Y., et al. Heterologous Immunization with Inactivated Vaccine Followed by MRNA-Booster Elicits Strong Immunity against SARS-CoV-2 Omicron Variant. Nat. Commun. 2022;13:2670. doi: 10.1038/s41467-022-30340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng S.M.S., Mok C.K.P., Leung Y.W.Y., Ng S.S., Chan K.C.K., Ko F.W., Chen C., Yiu K., Lam B.H.S., Lau E.H.Y., et al. Neutralizing Antibodies against the SARS-CoV-2 Omicron Variant BA.1 Following Homologous and Heterologous CoronaVac or BNT162b2 Vaccination. Nat. Med. 2022;28:486–489. doi: 10.1038/s41591-022-01704-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lauring A.S., Tenforde M.W., Chappell J.D., Gaglani M., Ginde A.A., McNeal T., Ghamande S., Douin D.J., Talbot H.K., Casey J.D., et al. Clinical Severity of, and Effectiveness of MRNA Vaccines against, COVID-19 from Omicron, Delta, and Alpha SARS-CoV-2 Variants in the United States: Prospective Observational Study. BMJ. 2022;376:e069761. doi: 10.1136/bmj-2021-069761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tartof S.Y., Slezak J.M., Puzniak L., Hong V., Xie F., Ackerson B.K., Valluri S.R., Jodar L., McLaughlin J.M. Durability of BNT162b2 Vaccine against Hospital and Emergency Department Admissions Due to the Omicron and Delta Variants in a Large Health System in the USA: A Test-Negative Case-Control Study. Lancet Respir. Med. 2022;10:689–699. doi: 10.1016/S2213-2600(22)00101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Andrews N., Stowe J., Kirsebom F., Toffa S., Rickeard T., Gallagher E., Gower C., Kall M., Groves N., O’Connell A.-M., et al. Covid-19 Vaccine Effectiveness against the Omicron (B.1.1.529) Variant. N. Engl. J. Med. 2022;386:1532–1546. doi: 10.1056/NEJMoa2119451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tseng H.F., Ackerson B.K., Luo Y., Sy L.S., Talarico C.A., Tian Y., Bruxvoort K.J., Tubert J.E., Florea A., Ku J.H., et al. Effectiveness of MRNA-1273 against SARS-CoV-2 Omicron and Delta Variants. Nat. Med. 2022;28:1063–1071. doi: 10.1038/s41591-022-01753-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Šmíd M., Berec L., Přibylová L., Májek O., Pavlík T., Jarkovský J., Weiner J., Barusová T., Trnka J. Protection by Vaccines and Previous Infection against the Omicron Variant of SARS-CoV-2. J. Infect. Dis. 2022:161. doi: 10.1093/infdis/jiac161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferdinands J.M., Rao S., Dixon B.E., Mitchell P.K., DeSilva M.B., Irving S.A., Lewis N., Natarajan K., Stenehjem E., Grannis S.J., et al. Waning 2-Dose and 3-Dose Effectiveness of MRNA Vaccines against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations among Adults during Periods of Delta and Omicron Variant Predominance—VISION Network, 10 States, August 2021-January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:255–263. doi: 10.15585/mmwr.mm7107e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Butt A.A., Talisa V.B., Shaikh O.S., Omer S.B., Mayr F.B. Relative Vaccine Effectiveness of a SARS-CoV-2 MRNA Vaccine Booster Dose against the Omicron Variant. Clin. Infect. Dis. 2022:328. doi: 10.1093/cid/ciac328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Modes M.E., Directo M.P., Melgar M., Johnson L.R., Yang H., Chaudhary P., Bartolini S., Kho N., Noble P.W., Isonaka S., et al. Clinical Characteristics and Outcomes among Adults Hospitalized with Laboratory-Confirmed SARS-CoV-2 Infection during Periods of B.1.617.2 (Delta) and B.1.1.529 (Omicron) Variant Predominance—One Hospital, California, July 15-September 23, 2021, and December 21, 2021-January 27, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:217–223. doi: 10.15585/mmwr.mm7106e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Plumb I.D., Feldstein L.R., Barkley E., Posner A.B., Bregman H.S., Hagen M.B., Gerhart J.L. Effectiveness of COVID-19 MRNA Vaccination in Preventing COVID-19-Associated Hospitalization among Adults with Previous SARS-CoV-2 Infection—United States, June 2021-February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:549–555. doi: 10.15585/mmwr.mm7115e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rzymski P., Sikora D., Zeyland J., Poniedziałek B., Kiedik D., Falfushynska H., Fal A. Frequency and Nuisance Level of Adverse Events in Individuals Receiving Homologous and Heterologous COVID-19 Booster Vaccine. Vaccines. 2022;10:754. doi: 10.3390/vaccines10050754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Atmar R.L., Lyke K.E., Deming M.E., Jackson L.A., Branche A.R., El Sahly H.M., Rostad C.A., Martin J.M., Johnston C., Rupp R.E., et al. Homologous and Heterologous COVID-19 Booster Vaccinations. N. Engl. J. Med. 2022;386:1046–1057. doi: 10.1056/NEJMoa2116414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mayr F.B., Talisa V.B., Shaikh O., Yende S., Butt A.A. Effectiveness of Homologous or Heterologous COVID-19 Boosters in Veterans. N. Engl. J. Med. 2022;386:1375–1377. doi: 10.1056/NEJMc2200415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nguyen T.T., Quach T.H.T., Tran T.M., Phuoc H.N., Nguyen H.T., Vo T.K., Van Vo G. Reactogenicity and Immunogenicity of Heterologous Prime-Boost Immunization with COVID-19 Vaccine. Biomed. Pharmacother. 2022;147:112650. doi: 10.1016/j.biopha.2022.112650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Accorsi E.K., Britton A., Shang N., Fleming-Dutra K.E., Link-Gelles R., Smith Z.R., Derado G., Miller J., Schrag S.J., Verani J.R. Effectiveness of Homologous and Heterologous COVID-19 Boosters against Omicron. N. Engl. J. Med. 2022;386:2433–2435. doi: 10.1056/NEJMc2203165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Abu-Raddad L.J., Chemaitelly H., Ayoub H.H., AlMukdad S., Yassine H.M., Al-Khatib H.A., Smatti M.K., Tang P., Hasan M.R., Coyle P., et al. Effect of MRNA Vaccine Boosters against SARS-CoV-2 Omicron Infection in Qatar. N. Engl. J. Med. 2022;386:1804–1816. doi: 10.1056/NEJMoa2200797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Suah J.L., Tng B.H., Tok P.S.K., Husin M., Thevananthan T., Peariasamy K.M., Sivasampu S. Real-World Effectiveness of Homologous and Heterologous BNT162b2, CoronaVac, and AZD1222 Booster Vaccination against Delta and Omicron SARS-CoV-2 Infection. Emerg. Microbes Infect. 2022;11:1343–1345. doi: 10.1080/22221751.2022.2072773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Natarajan K., Prasad N., Dascomb K., Irving S.A., Yang D.-H., Gaglani M., Klein N.P., DeSilva M.B., Ong T.C., Grannis S.J., et al. Effectiveness of Homologous and Heterologous COVID-19 Booster Doses Following 1 Ad.26.COV2.S (Janssen [Johnson & Johnson]) Vaccine Dose against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations among Adults—VISION Network, 10 States, December 2021-March 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71:495–502. doi: 10.15585/mmwr.mm7113e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., Perez J.L., Pérez Marc G., Moreira E.D., Zerbini C., et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sadoff J., Gray G., Vandebosch A., Cárdenas V., Shukarev G., Grinsztejn B., Goepfert P.A., Truyers C., Fennema H., Spiessens B., et al. Safety and Efficacy of Single-Dose Ad26.COV2.S Vaccine against COVID-19. N. Engl. J. Med. 2021;384:2187–2201. doi: 10.1056/NEJMoa2101544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Voysey M., Clemens S.A.C., Madhi S.A., Weckx L.Y., Folegatti P.M., Aley P.K., Angus B., Baillie V.L., Barnabas S.L., Bhorat Q.E., et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bajema K.L., Dahl R.M., Prill M.M., Meites E., Rodriguez-Barradas M.C., Marconi V.C., Beenhouwer D.O., Brown S.T., Holodniy M., Lucero-Obusan C., et al. Effectiveness of COVID-19 MRNA Vaccines against COVID-19-Associated Hospitalization—Five Veterans Affairs Medical Centers, United States, February 1-August 6, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70:1294–1299. doi: 10.15585/mmwr.mm7037e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Higdon M.M., Baidya A., Walter K.K., Patel M.K., Issa H., Espié E., Feikin D.R., Knoll M.D. Duration of Effectiveness of Vaccination against COVID-19 Caused by the Omicron Variant. Lancet Infect. Dis. 2022;22:1114–1116. doi: 10.1016/S1473-3099(22)00409-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tartof S.Y., Slezak J.M., Puzniak L., Hong V., Xie F., Ackerson B.K., Valluri S.R., Jodar L., McLaughlin J.M. Immunocompromise and Durability of BNT162b2 Vaccine against Severe Outcomes Due to Omicron and Delta Variants. Lancet Respir. Med. 2022;10:e61–e62. doi: 10.1016/S2213-2600(22)00170-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Regev-Yochay G., Gonen T., Gilboa M., Mandelboim M., Indenbaum V., Amit S., Meltzer L., Asraf K., Cohen C., Fluss R., et al. Efficacy of a Fourth Dose of COVID-19 MRNA Vaccine against Omicron. N. Engl. J. Med. 2022;386:1377–1380. doi: 10.1056/NEJMc2202542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bar-On Y.M., Goldberg Y., Mandel M., Bodenheimer O., Amir O., Freedman L., Alroy-Preis S., Ash N., Huppert A., Milo R. Protection by a Fourth Dose of BNT162b2 against Omicron in Israel. N. Engl. J. Med. 2022;386:1712–1720. doi: 10.1056/NEJMoa2201570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Burki T.K. Fourth Dose of COVID-19 Vaccines in Israel. Lancet Respir. Med. 2022;10:e19. doi: 10.1016/S2213-2600(22)00010-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Magen O., Waxman J.G., Makov-Assif M., Vered R., Dicker D., Hernán M.A., Lipsitch M., Reis B.Y., Balicer R.D., Dagan N. Fourth Dose of BNT162b2 MRNA COVID-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2022;386:1603–1614. doi: 10.1056/NEJMoa2201688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Qu P., Faraone J., Evans J.P., Zou X., Zheng Y.-M., Carlin C., Bednash J.S., Lozanski G., Mallampalli R.K., Saif L.J., et al. Neutralization of the SARS-CoV-2 Omicron BA.4/5 and BA.2.12.1 Subvariants. N. Engl. J. Med. 2022;386:2526–2528. doi: 10.1056/NEJMc2206725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith T.P., Flaxman S., Gallinat A.S., Kinosian S.P., Stemkovski M., Unwin H.J.T., Watson O.J., Whittaker C., Cattarino L., Dorigatti I., et al. Temperature and Population Density Influence SARS-CoV-2 Transmission in the Absence of Nonpharmaceutical Interventions. Proc. Natl. Acad. Sci. USA. 2021;118:e2019284118. doi: 10.1073/pnas.2019284118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gavenčiak T., Monrad J.T., Leech G., Sharma M., Mindermann S., Brauner J.M., Bhatt S., Kulveit J. Seasonal Variation in SARS-CoV-2 Transmission in Temperate Climates. bioRxiv. 2021 doi: 10.1101/2021.06.10.21258647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yeh T.-Y., Contreras G.P. Full Vaccination against COVID-19 Suppresses SARS-CoV-2 Delta Variant and Spike Gene Mutation Frequencies and Generates Purifying Selection Pressure. bioRxiv. 2021 doi: 10.1101/2021.08.08.21261768. [DOI] [Google Scholar]
- 75.Rzymski P., Szuster-Ciesielska A. The COVID-19 Vaccination Still Matters: Omicron Variant Is a Final Wake-up Call for the Rich to Help the Poor. Vaccines. 2022;10:1070. doi: 10.3390/vaccines10071070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ganesan S., Al Ketbi L.M.B., Al Kaabi N., Al Mansoori M., Al Maskari N.N., Al Shamsi M.S., Alderei A.S., El Eissaee H.N., Al Ketbi R.M., Al Shamsi N.S., et al. Vaccine Side Effects Following COVID-19 Vaccination among the Residents of the UAE-an Observational Study. Front. Public Health. 2022;10:876336. doi: 10.3389/fpubh.2022.876336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rzymski P., Perek B., Flisiak R. Thrombotic Thrombocytopenia after COVID-19 Vaccination: In Search of the Underlying Mechanism. Vaccines. 2021;9:559. doi: 10.3390/vaccines9060559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mushtaq H.A., Khedr A., Koritala T., Bartlett B.N., Jain N.K., Khan S.A. A Review of Adverse Effects of COVID-19 Vaccines. Infez. Med. 2022;30:1–10. doi: 10.53854/liim-3001-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang Q., Guo Y., Iketani S., Li Z., Mohri H., Wang M., Yu J., Bowen A.D., Chang J.Y., Shah J.G., et al. SARS-CoV-2 Omicron BA.2.12.1, BA.4, and BA.5 Subvariants Evolved to Extend Antibody Evasion. bioRxiv. 2022 doi: 10.1101/2022.05.26.493517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cao Y., Yisimayi A., Jian F., Song W., Xiao T., Wang L., Du S., Wang J., Li Q., Chen X., et al. BA.2.12.1, BA.4 and BA.5 Escape Antibodies Elicited by Omicron Infection. Nature. 2022 doi: 10.1038/s41586-022-04980-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yaniv K., Ozer E., Shagan M., Paitan Y., Granek R., Kushmaro A. Managing an Evolving Pandemic: Cryptic Circulation of the Delta Variant during the Omicron Rise. Sci. Total Environ. 2022;836:155599. doi: 10.1016/j.scitotenv.2022.155599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Suryawanshi R.K., Chen I.P., Ma T., Syed A.M., Brazer N., Saldhi P., Simoneau C.R., Ciling A., Khalid M.M., Sreekumar B., et al. Limited Cross-Variant Immunity after Infection with the SARS-CoV-2 Omicron Variant without Vaccination. medRxiv. 2022 doi: 10.1101/2022.01.13.22269243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Laurie M.T., Liu J., Sunshine S., Peng J., Black D., Mitchell A.M., Mann S.A., Pilarowski G., Zorn K.C., Rubio L., et al. SARS-CoV-2 Variant Exposures Elicit Antibody Responses with Differential Cross-Neutralization of Established and Emerging Strains Including Delta and Omicron. J. Infect. Dis. 2022;225:1909–1914. doi: 10.1093/infdis/jiab635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rudenko L., Kiseleva I., Krutikova E., Stepanova E., Rekstin A., Donina S., Pisareva M., Grigorieva E., Kryshen K., Muzhikyan A., et al. Rationale for Vaccination with Trivalent or Quadrivalent Live Attenuated Influenza Vaccines: Protective Vaccine Efficacy in the Ferret Model. PLoS ONE. 2018;13:e0208028. doi: 10.1371/journal.pone.0208028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu C., Mendonça L., Yang Y., Gao Y., Shen C., Liu J., Ni T., Ju B., Liu C., Tang X., et al. The Architecture of Inactivated SARS-CoV-2 with Postfusion Spikes Revealed by Cryo-EM and Cryo-ET. Structure. 2020;28:1218–1224.e4. doi: 10.1016/j.str.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Carpenter C.F., Aljassem A., Stassinopoulos J., Pisacreta G., Hutton D. A Cost-Effectiveness Analysis of an Adjuvanted Subunit Vaccine for the Prevention of Herpes Zoster and Post-Herpetic Neuralgia. Open Forum Infect. Dis. 2019;6:ofz219. doi: 10.1093/ofid/ofz219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wu K., Choi A., Koch M., Elbashir S., Ma L., Lee D., Woods A., Henry C., Palandjian C., Hill A., et al. Variant SARS-CoV-2 MRNA Vaccines Confer Broad Neutralization as Primary or Booster Series in Mice. Vaccine. 2021;39:7394–7400. doi: 10.1016/j.vaccine.2021.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ying B., Whitener B., VanBlargan L.A., Hassan A.O., Shrihari S., Liang C.-Y., Karl C.E., Mackin S., Chen R.E., Kafai N.M., et al. Protective Activity of MRNA Vaccines against Ancestral and Variant SARS-CoV-2 Strains. Sci. Transl. Med. 2022;14:eabm3302. doi: 10.1126/scitranslmed.abm3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Busà R., Sorrentino M.C., Russelli G., Amico G., Miceli V., Miele M., Di Bella M., Timoneri F., Gallo A., Zito G., et al. Specific Anti-SARS-CoV-2 Humoral and Cellular Immune Responses after Booster Dose of BNT162b2 Pfizer-BioNTech MRNA-Based Vaccine: Integrated Study of Adaptive Immune System Components. Front. Immunol. 2022;13:856657. doi: 10.3389/fimmu.2022.856657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Maruggi G., Mallett C.P., Westerbeck J.W., Chen T., Lofano G., Friedrich K., Qu L., Sun J.T., McAuliffe J., Kanitkar A., et al. A Self-Amplifying MRNA SARS-CoV-2 Vaccine Candidate Induces Safe and Robust Protective Immunity in Preclinical Models. Mol. Ther. 2022;30:1897–1912. doi: 10.1016/j.ymthe.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rappaport A.R., Hong S.-J., Scallan C.D., Gitlin L., Akoopie A., Boucher G.R., Egorova M., Espinosa J.A., Fidanza M., Kachura M.A., et al. Low-Dose Self-Amplifying MRNA COVID-19 Vaccine Drives Strong Protective Immunity in Non-Human Primates against SARS-CoV-2 Infection. Nat. Commun. 2022;13:3289. doi: 10.1038/s41467-022-31005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.