Abstract
BACKGROUND
Safety-net hospitals provide essential services to vulnerable patients with complex medical and socioeconomic circumstances. We hypothesized that matched patients at safety-net hospitals and non–safety-net hospitals would have comparable outcomes, costs, and readmission rates after isolated surgical aortic valve replacement (AVR) or mitral valve replacement (MVR).
METHODS
The National Readmissions Database was queried to identify patients who underwent isolated AVR (n = 109 744) or MVR (n = 31 475) from 2016 to 2018. Safety-net burden was defined as the percentage of patients who were uninsured or insured with Medicaid, with hospitals in the top quartile designated as safety-net hospitals. After propensity score matching, outcomes for AVR and MVR at safety-net hospitals vs non–safety-net hospitals were compared.
RESULTS
Overall, 17 925 AVRs (16%) and 5516 MVRs (18%) were performed at safety-net hospitals, and these patients had higher comorbidity rates, had lower socioeconomic status, and more frequently required urgent surgery. Observed inhospital mortality was similar between safety-net hospitals and non–safety-net hospitals (AVR 2.2% vs 2.1%, P = .4; MVR 4.8% vs 4.3%, P = .1). After matching, rates of inhospital mortality, major morbidity, and readmission were similar; however, safety-net hospitals had longer length of stay after AVR (7 vs 6 days, P = .001) and higher total cost after AVR ($49 015 vs $42 473, P < .001) and MVR ($59 253 vs $52 392, P < .001).
CONCLUSIONS
Isolated surgical AVR and MVR are both performed at safety-net hospitals with outcomes comparable to those at non–safety-net hospitals, supporting efforts to expand access to these procedures for underserved populations. Investment in care coordination resources to reduce length of stay and curtail cost at safety-net hospitals is warranted.
Safety-net hospitals provide essential services, including cardiac surgical care, to vulnerable patients with complex medical and socioeconomic circumstances, regardless of their ability to pay. Important disparities exist for these patients in terms of the burden of cardiovascular risk factors,1 disease severity at presentation,2 and access to cardiac surgical interventions.3-5 Furthermore, safety-net hospitals have been the subject of scrutiny with respect to quality of cardiac surgical care; several studies suggest that safety-net hospitals lag behind non–safety-net hospitals.6-8
Although previous studies have identified patient-level disparities in terms of outcomes after surgical aortic valve replacement (AVR) or mitral valve replacement (MVR) in the United States,9-12 few have compared outcomes based on hospital safety-net status.13 We hypothesized that, among propensity score matched patients from a nationwide sample, safety-net hospitals and non–safety-net hospitals would have comparable outcomes, cost, and readmission rates after isolated surgical AVR or MVR.
PATIENTS AND METHODS
STUDY POPULATION AND DATA COLLECTION.
A retrospective cohort study was conducted using Nationwide Readmissions Database data. All index admissions of patients aged 18 years or more who underwent surgical AVR or MVR between January 2016 and December 2018 were identified by the corresponding International Classification of Disease, Tenth Revision (ICD-10) codes. The ICD-10 Clinical Modification and Procedure Coding System codes were used to exclude patients with a diagnosis of endocarditis and patients who underwent concomitant cardiac procedures (Supplemental Table 1). Given that only deidentified data were used, this study was deemed exempt from Institutional Review Board approval.
STUDY DEFINITIONS.
Safety-net burden was defined as the percentage of all admissions with the patient’s primary payer designated as uninsured, or insured by Medicaid. In line with previous studies,7 hospitals in the top quartile of safety-net burden were defined as safety-net hospitals and the remaining hospitals as non–safety-net hospitals. Demographic characteristics including age, sex, primary payer, and median household income quartile were abstracted directly from the Nationwide Readmissions Database. Comorbidities were identified by using the corresponding ICD-10 Clinical Modification codes with a custom Python script (Python Language Reference 3.7; Python Software Foundation). The composite Elixhauser comorbidity index, used to quantify comorbidity burden, was calculated with a Python implementation of Healthcare Cost and Utilization Project Software and Tools (hcuppy 0.0.7).
OUTCOMES.
Our primary outcome was inhospital mortality. Our secondary outcomes were major morbidity (acute kidney injury, stroke, and respiratory failure), length of stay (LOS), total cost of hospitalization, and 30- and 90-day readmission. Total cost was calculated by multiplying the total hospital charge by cost-to-charge ratios provided by the Nationwide Readmissions Database.
STATISTICAL ANALYSIS.
Analyses were performed in SAS 9.4 (SAS Institute) and R 4.1 (The R Project for Statistical Computing). In all analyses, we accounted for the complex survey design of the Nationwide Readmissions Database, including clustering, stratification, and discharge weighting. Categoric variables are presented as number (percentage) and continuous variables are presented as median (interquartile range). Univariate comparisons were performed with the χ2 test with Rao and Scott’s correction or the Wilcoxon rank sum test adjusted for complex survey design, as appropriate. A P value of less than .05 was considered statistically significant.
PROPENSITY SCORE MATCHED ANALYSIS.
A propensity score matched analysis was performed to compare outcomes between safety-net hospitals and non-safety-net hospitals after adjusting for differences in baseline characteristics. Cohorts were matched by age, sex, insurance status, household income quartile, prosthesis type, elective admission status, and Elixhauser comorbidities. Greedy nearest-neighbor matching through the PSMATCH function in SAS 9.4 was used to create pairs in a 1:1 ratio between safety-net hospitals and non-safety-net hospitals with a caliper of 0.005 standard deviation of the logit. Quality of match was assessed with overall propensity score balance, individual standard mean differences of the covariates, and statistical insignificance of the covariates after matching. An average standard mean difference of 0.10 was considered acceptable. After matching, univariate comparisons were performed with the tests described in preceding text.
RESULTS
PATIENTS UNDERGOING AVR AT SAFETY-NET VS NON–SAFETY-NET HOSPITALS.
Preoperative Characteristics.
A weighted total of 109 744 patients (64.0% male) underwent isolated surgical AVR in the United States between 2016 and 2018 (17 925 [16.3%] at safety-net hospitals; 91 819 [83.7%] at non–safety-net hospitals; Figure 1A). In terms of differences in baseline characteristics between the two cohorts, patients who underwent AVR at safety-net hospitals were younger (median age 66 vs 67 years), more often in the lowest household income quartile (27.5% vs 21.1%), less often in the highest household income quartile (20.0% vs 23.3%), and more likely to undergo nonelective surgery (25.2% vs 18.5%) than patients at non–safety-net hospitals (all P < .001; Table 1). In addition, patients at safety-net hospitals had a higher burden of comorbidities, including anemia (15.8% vs 12.2%, P < .001), congestive heart failure (38.2% vs 34.6%, P < .001), and diabetes mellitus (14.3% vs 12.8%, P < .001), whereas patients at non–safety-net hospitals had higher rates of hypertension (48.5% vs 47.5%, P = .01) and obesity (27.4% vs 25.9%, P < .001). Last, patients at safety-net hospitals were more likely to receive a mechanical valve than patients at non–safety-net hospitals.
FIGURE.
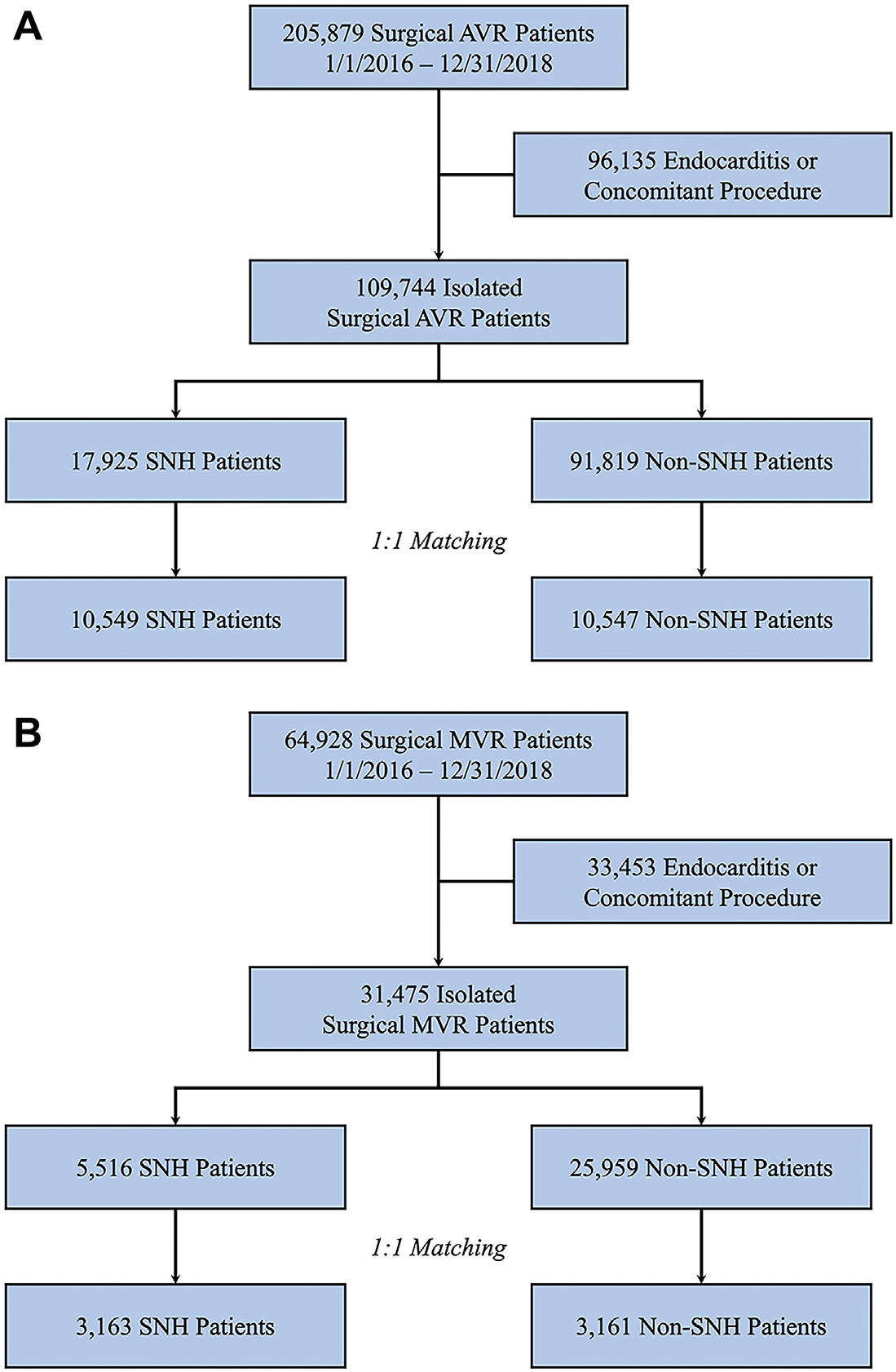
Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) diagrams for (A) aortic valve replacement (AVR) and (B) mitral valve replacement (MVR) at safety-net hospitals (SNH) and non–safety-net hospitals.
TABLE 1.
Preoperative Characteristics of Patients Who Underwent Isolated Surgical Aortic Valve Replacement at Safety-Net vs Non–Safety-Net Hospitals
| Unmatched (n = 109 744) | Matched (n = 20 074) | |||||
|---|---|---|---|---|---|---|
| Variable | Safety-Net Hospitals (n = 17 925) |
Non–Safety-Net Hospitals (n = 91 819) |
P Value |
Safety-Net Hospitals (n = 10 537) |
Non–Safety-Net Hospitals (n = 10 537) |
SMD |
| Age, y | 66 (58-73) | 67 (59-74) | <.001 | 66 (58-73) | 66 (57-73) | −0.001 |
| Male | 11 467 (64.0) | 58 805 (64.0) | .9 | 6739 (64.0) | 6550 (62.2) | −0.037 |
| Elixhauser score | 10 (2-19) | 10 (2-18) | .03 | 10 (2-19) | 10 (2-19) | …b |
| Anemia | 2834 (15.8) | 11 186 (12.2) | <.001 | 1,626 (15.4) | 1687 (16.0) | −0.006 |
| Chronic kidney disease | 2375 (13.3) | 12 160 (13.2) | 1 | 1362 (12.9) | 1446 (13.7) | −0.024 |
| COPD | 3644 (20.3) | 18 315 (20.0) | .2 | 2142 (20.3) | 2234 (21.2) | −0.022 |
| Coagulopathy | 5814 (32.4) | 31 566 (34.4) | <.001 | 3416 (32.4) | 3604 (34.2) | −0.038 |
| Congestive heart failure | 6845 (38.2) | 31 722 (34.6) | <.001 | 3981 (37.8) | 4099 (38.9) | −0.023 |
| Diabetes mellitus | 2560 (14.3) | 11 731 (12.8) | <.001 | 1505 (14.3) | 1573 (14.9) | −0.019 |
| Drug abuse | 426 (2.4) | 1055 (1.2) | <.001 | 228 (2.2) | 231 (2.2) | −0.002 |
| Hypertension | 8506 (47.5) | 44 540 (48.5) | .01 | 5039 (47.8) | 4863 (46.2) | 0.033 |
| Obesity | 4645 (25.9) | 25 139 (27.4) | <.001 | 2712 (25.7) | 2910 (27.6) | −0.042 |
| Peripheral arterial disease | 4747 (26.5) | 24 496 (26.7) | .6 | 2752 (26.1) | 2860 (27.1) | −0.023 |
| Household incomea | <.001 | |||||
| Quartile 1 | 4854 (27.5) | 19 102 (21.1) | 2703 (26.1) | 2699 (26.0) | 0.001 | |
| Quartile 2 | 4906 (27.8) | 25 175 (27.8) | 2819 (27.2) | 2854 (27.5) | −0.008 | |
| Quartile 3 | 4369 (24.8) | 25 133 (27.8) | 2653 (25.6) | 2638 (25.4) | 0.003 | |
| Quartile 4 | 3522 (20.0) | 21 048 (23.3) | 2190 (21.1) | 2185 (21.1) | 0.001 | |
| Bioprosthetic | 13 441 (75.0) | 72 750 (79.2) | <.001 | 7898 (75.0) | 7826 (74.3) | −0.016 |
| Mechanical valve | 4498 (25.1) | 19 119 (20.8) | <.001 | 2639 (25.0) | 2711 (25.7) | 0.017 |
| Nonelective | 4515 (25.2) | 16 958 (18.5) | <.001 | 2631 (25.0) | 2683 (25.5) | 0.409 |
Indexed to patient’s zip code
Cohorts matched by each individual Elixhauser comorbidity but not composite score. Values are median (interquartile range) or n (%). COPD, chronic obstructive pulmonary disease; SMD, standardized mean difference.
Postoperative Outcomes.
In terms of unadjusted outcomes after AVR, we observed similar rates of inhospital mortality at safety-net hospitals and non–safety-net hospitals (2.2% vs 2.1%, P = .4); however, there were several differences in the incidence of major morbidity (Table 2). The rates of acute kidney injury (16.6% vs 16.0%, P = .04) and stroke (2.2% vs 1.9%, P = .003) were higher at safety-net hospitals, whereas the rate of respiratory failure (10.9% vs 9.4%, P < .001) was higher at non–safety-net hospitals. In addition, patients at safety-net hospitals had longer LOS (median 7 vs 6 days, P < .001), incurred higher total cost (mean $49 091 vs $41 746, P < .001), and had a higher rate of readmission within 90 days (15.4% vs 14.6%, P = .01).
TABLE 2.
Postoperative Outcomes of Patients After Isolated Surgical Aortic Valve Replacement at Safety-Net vs Non–Safety-Net Hospitals
| Unmatched (n = 109 744) | Matched (n = 20 074) | |||||
|---|---|---|---|---|---|---|
| Variable | Safety-Net Hospitals (n = 17 925) |
Non–Safety-Net Hospitals (n = 91 819) |
P Value |
Safety-Net Hospitals (n = 10 537) |
Non–Safety-Net Hospitals (n = 10 537) |
P Value |
| Inhospital mortality | 388 (2.2) | 1899 (2.1) | .4 | 223 (2.1) | 252 (2.4) | .2 |
| Acute kidney injury | 2979 (16.6) | 14 679 (16) | .04 | 1725 (16.4) | 1787 (17.0) | .3 |
| Stroke | 392 (2.2) | 1706 (1.9) | .003 | 216 (2.1) | 257 (2.4) | .1 |
| Respiratory failure | 1682 (9.4) | 10 017 (10.9) | <.001 | 982 (9.3) | 1186 (11.3) | <.001 |
| Length of stay, d | 7 (5-10) | 6 (5-9) | <.001 | 7 (5-10) | 6 (5-10) | .001 |
| Total cost, $ | 49 091 (38 614-65 523) | 41 746 (32 213-57 805) | <.001 | 49 015 (38 570-65 198) | 42 473 (32 786-59 409) | <.001 |
| Readmission within 30 days | 1979 (11.0) | 9858 (10.7) | .2 | 1136 (10.8) | 1,189 (11.3) | .2 |
| Readmission within 90 days | 2762 (15.4) | 13 425 (14.6) | .01 | 1596 (15.2) | 1,646 (15.6) | .3 |
| Discharged homea | 14 896 (83.1) | 76 241 (83) | .8 | 8759 (83.1) | 8,653 (82.1) | .1 |
With or without home health care. Values are n (%) or median (interquartile range).
After propensity score matching to create 10 537 matched pairs, there were no significant differences between cohorts in the rates of inhospital mortality, acute kidney injury, stroke, or readmission within 30 or 90 days (Table 2); however, the higher rate of respiratory failure (11.3% vs 9.3%, P < .001) observed at non–safety-net hospitals persisted, along with the longer LOS (median 7 vs 6 days; P = .001) and higher total cost (median $49 015 vs $42 473; P < .001) observed at safety-net hospitals.
PATIENTS UNDERGOING MVR AT SAFETY-NET VS NON–SAFETY-NET HOSPITALS.
Preoperative Characteristics.
A weighted total of 31 475 patients (40.6% male) underwent isolated surgical MVR in the United States between 2016 and 2018 (5516 [17.5%] at safety-net hospitals and 25 959 [82.5%] at non–safety-net hospitals; Figure 1B). Again, patients who underwent MVR at safety-net hospitals were younger (median age 64 vs 67 years), more often in the lowest household income quartile (33.1% vs 26.1%), less often in the highest household income quartile (16.7% vs 20.5%), and more likely to undergo nonelective surgery (33.4% vs 28.1%) than patients at non–safety-net hospitals (all P < .001; Table 3). The overall burden of comorbidities was similar between groups; however, patients at safety-net hospitals had higher rates of anemia (20.7% vs 17.0%, P < .001) and diabetes mellitus (11.6% vs 8.6%, P < .001), whereas patients at non–safety-net hospitals had higher rates of chronic kidney disease (20.6% vs 18.7%, P = .002), obesity (22.4% vs 20.2%, P < .001), and peripheral arterial disease (9.4% vs 8.0%, P = .001). Last, patients at safety-net hospitals were more likely to receive a mechanical valve than patients at non–safety-net hospitals.
TABLE 3.
Preoperative Characteristics of Patients Who Underwent Isolated Surgical Mitral Valve Replacement at Safety-Net vs Non–Safety-Net Hospitals
| Unmatched (n = 31 475) | Matched (n = 6350) | |||||
|---|---|---|---|---|---|---|
| Variable | Safety-Net Hospitals (n = 5516) |
Non–Safety-Net Hospitals (n = 25 959) |
P Value |
Safety-Net Hospitals (n = 3175) |
Non–Safety-Net Hospitals (n = 3175) |
SMD |
| Age, y | 64 (55-73) | 67 (58-75) | <.001 | 64 (55-73) | 64 (55-73) | −0.005 |
| Male | 2201 (39.9) | 10 579 (40.8) | .2 | 1893 (59.6) | 1932 (60.9) | −0.025 |
| Elixhauser score | 14 (6-22) | 14 (6-22) | .2 | 14 (6-22) | 14 (6-22) | …b |
| Anemia | 1144 (20.7) | 4410 (17.0) | <.001 | 651 (20.5) | 633 (19.9) | 0.014 |
| Chronic kidney disease | 1031 (18.7) | 5342 (20.6) | .002 | 596 (18.8) | 614 (19.4) | 0.005 |
| COPD | 1467 (26.6) | 7175 (27.6) | .1 | 595 (18.7) | 589 (18.6) | −0.021 |
| Coagulopathy | 1942 (35.2) | 9646 (37.2) | .006 | 1121 (35.3) | 1116 (35.2) | 0.003 |
| Congestive heart failure | 3476 (63.0) | 16 111 (62.1) | .2 | 2005 (63.2) | 1989 (62.7) | 0.010 |
| Diabetes mellitus | 642 (11.6) | 2232 (8.6) | < .001 | 372 (11.7) | 363 (11.4) | 0.009 |
| Drug abuse | 1638 (29.7) | 7474 (28.8) | .2 | 943 (29.7) | 957 (30.1) | −0.009 |
| Hypertension | 215 (3.9) | 438 (1.7) | <.001 | 95 (3.0) | 90 (2.9) | 0.009 |
| Obesity | 1116 (20.2) | 5823 (22.4) | <.001 | 626 (19.7) | 619 (19.5) | 0.005 |
| Peripheral arterial disease | 443 (8.0) | 2450 (9.4) | .001 | 252 (7.9) | 248 (7.8) | 0.004 |
| Household incomea | <.001 | |||||
| Quartile 1 | 1795 (33.1) | 6680 (26.1) | 979 (31.4) | 971 (31.1) | 0.006 | |
| Quartile 2 | 1454 (26.8) | 7196 (28.2) | 836 (26.8) | 832 (26.7) | 0.003 | |
| Quartile 3 | 1269 (23.4) | 6447 (25.2) | 757 (24.3) | 778 (24.9) | −0.015 | |
| Quartile 4 | 904 (16.7) | 5241 (20.5) | 548 (17.6) | 539 (17.3) | 0.007 | |
| Bioprosthetic valve | 3531 (64.0) | 18 353 (70.7) | <.001 | 2035 (64.1) | 2015 (63.5) | −0.014 |
| Mechanical valve | 1981 (35.9) | 7615 (29.3) | <.001 | 1139 (35.9) | 1160 (35.5) | 0.013 |
| Nonelective | 1839 (33.4) | 7284 (28.1) | < .001 | 1028 (32.4) | 1053 (33.2) | 0.504 |
Indexed to patient’s zip code
Cohorts matched by each individual Elixhauser comorbidity and not composite score. Values are median (interquartile range) or n (%). COPD, chronic obstructive pulmonary disease; SMD, standardized mean difference.
Postoperative Outcomes.
In terms of unadjusted outcomes after MVR at safety-net hospitals and non–safety-net hospitals, respectively, we observed similar rates of inhospital mortality (4.8% vs 4.3%, P = .1), acute kidney injury (25.5% vs 25.8%, P = .7), stroke (2.8% vs 2.4%, P = .2), and readmission within 30 days (16.2% vs 16.1%, P = 1) and 90 days (22.8% vs 23.1%, P = .6); however, non–safety-net hospitals had a higher rate of respiratory failure (14.6% vs 11.6%, P < .001; Table 4). In addition, although patients at safety-net hospitals and non–safety-net hospitals had similar LOS (median 9 vs 9 days; P < .001), patients at safety-net hospitals incurred higher total cost (median $59 524 vs $52 638; P < .001).
TABLE 4.
Postoperative Outcomes of Patients Who Underwent Isolated Surgical Mitral Valve Replacement at Safety-Net vs Non–Safety-Net Hospitals
| Unmatched (n = 31 475) | Matched (n = 6,350) | |||||
|---|---|---|---|---|---|---|
| Variable | Safety-Net Hospitals (n = 5516) |
Non–Safety-Net Hospitals (n = 25 959) |
P Value |
Safety-Net Hospitals (n = 3175) |
Non–Safety-Net Hospitals (n = 3175) |
P Value |
| Inhospital mortality | 265 (4.8) | 1116 (4.3) | .1 | 139 (4.4) | 124 (3.9) | .3 |
| Acute kidney injury | 1407 (25.5) | 6689 (25.8) | .7 | 783 (24.7) | 782 (24.6) | 1 |
| Stroke | 151 (2.8) | 1631 (2.4) | .2 | 89 (2.8) | 88 (2.8) | .9 |
| Respiratory failure | 638 (11.6) | 3782 (14.6) | <.001 | 371 (11.7) | 420 (13.2) | .1 |
| Length of stay, d | 9 (7-16) | 9 (6-16) | <.001 | 9 (7-16) | 9 (6-15) | .1 |
| Total cost, $ | 59 524 (45 252-82 443) | 52 638 (38 813-75 443) | <.001 | 59 253 (45 222-82 286) | 52 392 (38 745-74 034) | <.001 |
| Readmission within 30 days | 891 (16.2) | 4187 (16.1) | 1 | 506 (15.9) | 506 (15.9) | 1 |
| Readmission within 90 days | 1258 (22.8) | 6004 (23.1) | .6 | 728 (22.9) | 725 (22.8) | .9 |
| Discharged homea | 4151 (75.3) | 19 133 (71.3) | .02 | 2419 (76.2) | 2405 (75.8) | .7 |
With or without home health care. Values are n (%) or median (interquartile range).
After propensity score matching to create 3175 matched pairs, there were no significant differences between cohorts in the rates of inhospital mortality, acute kidney injury, stroke, respiratory failure, LOS, or readmission within 30 or 90 days (Table 4). However, the higher total cost observed at safety-net hospitals persisted (median $59 253 vs $52 392; P < .001).
COMMENT
Studies comparing outcomes after cardiac surgery at safety-net hospitals vs non–safety-net hospitals have yielded conflicting results.6-8,13-15 We speculated that differences in outcomes after cardiac surgery may be attributable in part to differences in medical and socioeconomic complexity between patients at safety-net hospitals vs non-safety-net hospitals, as has been previously described.6,13,15,16 In line with our hypothesis, we found that after propensity score matching, inhospital mortality and major morbidity were comparable or better for patients who underwent isolated surgical AVR or MVR at safety-net hospitals vs non–safety-net hospitals. Indeed, non–safety-net hospitals were inferior to safety-net hospitals in the observed rate of postoperative respiratory failure, although this difference did not persist after matching. One possible explanation for this finding is baseline differences between cohorts in the rates of chronic respiratory diseases, which were not included in our analysis or captured in the Nationwide Readmissions Database. Also of note, important predictors of postoperative respiratory failure, including cardiopulmonary bypass time and perioperative transfusions, were not available in the Nationwide Readmissions Database.
In a previous study by Ando and colleagues,13 hospitals were divided into quintiles based on safety-net burden, and outcomes after AVR were compared among low-, medium-, and high-burden hospitals. Consistent with the findings of the present study, the investigators found that after adjusting for patient- and hospital-level characteristics through multivariable logistic regression, inhospital mortality and major morbidity were similar at low- and high-burden hospitals. Similar findings have been described for transcatheter aortic valve replacement.17
Interestingly, we found that both LOS (for AVR) and total cost (for AVR and MVR) remained greater for patients who underwent valve replacement surgery at safety-net hospitals after propensity score matching, similar to the findings reported by Ando and colleagues.13 Although an association between longer LOS and higher total cost is intuitive, it remains to be determined how much the differences in LOS (1 day for AVR and 0 days for MVR) contribute to the variation in total cost ($6542 for AVR and $6861 for MVR) observed in our study. In addition, the root cause of greater LOS at safety-net hospitals compared with non–safety-net hospitals warrants further study. One possible explanation is the constraint in coordination of care and limited access to post-hospital facilities (eg, acute rehabilitation, skilled nursing, long-term acute care) for underinsured or uninsured patients.18 As a result, patients at safety-net hospitals may require a protracted hospital course to ensure safe discharge, thereby incurring higher total cost. Implementing enhanced recovery protocols and streamlined care pathways at these centers could help bridge both of these residual gaps between safety-net and non–safety-net hospitals.19 Given the substantial overall cost of valve replacement surgery, targeted strategies to reduce LOS are warranted for safety-net hospitals to facilitate cost containment. In terms of additional cost-containment strategies, we observed no differences in the rates of 30-day and 90-day readmission between safety-net hospitals and non-safety-net hospitals in our matched analysis. This finding is encouraging, given that previous studies have found higher rates of readmission at safety-net hospitals than at non–safety-net hospitals.7,15
An important consideration in interpreting studies such as the present one is that patient- and hospital-level socioeconomic factors are inherently interconnected. Patients at safety-net hospitals, many of whom are uninsured, may be more likely to forgo necessary care and screening20 and, as a result, present with more advanced disease and higher acuity.2,11 Indeed, lower socioeconomic status21-25 and lack of insurance12,26 are independently associated with greater morbidity and mortality after cardiac surgery, and likely exert a synergistic effect on access to cardiac surgical care.3 Additional studies are needed to elucidate the complex relationship between patient- and hospital-level socioeconomic factors, their relative impact on outcomes after cardiac surgery, and where the greatest return on investment may lie for policymakers and other stakeholders aiming to improve the quality of cardiac surgical care for vulnerable populations.
STUDY LIMITATIONS.
Our findings should be interpreted in the context of the limitations inherent to all retrospective studies and administrative databases. Although the Nationwide Readmissions Database provides a large sample size capable of powering a robust propensity score matched analysis, administrative data can be incomplete, and their accuracy relies on nonclinician coding. Consequently, patients with limited access to or use of routine health care services before surgery may be “undercoded” with respect to comorbidities. In addition, we attempted to minimize the influence of baseline covariates by using established comorbidity codes; however, the influence of residual confounding factors cannot be fully excluded. Several potential unmeasured confounders influencing the findings of this study include race and ethnicity, preoperative risk modification, lesion severity, and variation in surgical technique. In addition, although both surgeon and center volume substantially affect outcomes after valve surgery, we were unable to match patients by these volumes. Last, transcatheter therapies have become an integral component of the armamentarium for treating aortic and mitral valve pathologies; however, we elected to exclude these because including them would have complicated our analysis and obfuscated the focus of the present study. Moreover, the introduction of these therapies has altered the landscape of aortic and mitral valve surgery, rendering isolated aortic and mitral valve replacement less common. Although including concomitant cardiac procedures may have enhanced the generalizability of our results, we elected to exclude these procedures as well, given the lack of granularity in the Nationwide Readmissions Database in terms of complex reconstructive techniques, including those often required for patients with infective endocarditis.
CONCLUSION.
After propensity score matching, we found that outcomes of patients who underwent isolated surgical AVR or MVR were comparable at safety-net hospitals and non–safety-net hospitals, supporting efforts to expand access to these procedures for underserved populations. Investment in care coordination resources to reduce length of stay and curtail cost at safety-net hospitals is warranted.
Supplementary Material
Footnotes
Dr Coselli discloses a financial relationship with Terumo Aortic, Medtronic, WL Gore, Lifesciences, Artivion, and CytoSortbents; Dr Preventza with Terumo Aortic and WL Gore.
The Supplemental Table can be viewed in the online version of this article [https://doi.org/10.1016/j.athoracsur.2022.01.049] on http://www.annalsthoracicsurgery.org.
Presented at the Sixty-eighth Annual Meeting of the Southern Thoracic Surgical Association, Atlanta, GA, Nov 3-6, 2021.
REFERENCES
- 1.Patel SA, Ali MK, Narayan KM, Mehta NK. County-level variation in cardiovascular disease mortality in the United States in 2009-2013: comparative assessment of contributing factors. Am J Epidemiol. 2016;184:933–942. [DOI] [PubMed] [Google Scholar]
- 2.Yeung M, Kerrigan J, Sodhi S, et al. Racial differences in rates of aortic valve replacement in patients with severe aortic stenosis. Am J Cardiol. 2013;112:991–995. [DOI] [PubMed] [Google Scholar]
- 3.Best MJ, McFarland EG, Thakkar SC, Srikumaran U. Racial disparities in the use of surgical procedures in the US. JAMA Surg. 2021;156:274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoenfeld AJ, Sturgeon DJ, Dimick JB, et al. Disparities in rates of surgical intervention among racial and ethnic minorities in Medicare accountable care organizations. Ann Surg. 2019;269:459–464. [DOI] [PubMed] [Google Scholar]
- 5.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–627. [DOI] [PubMed] [Google Scholar]
- 6.Hoyler MM, Tam CW, Thalappillil R, et al. The impact of hospital safety-net burden on mortality and readmission after CABG surgery. J Card Surg. 2020;35:2232–2241. [DOI] [PubMed] [Google Scholar]
- 7.Talutis SD, Chen Q, Wang N, Rosen AK. Comparison of risk-standardized readmission rates of surgical patients at safety-net and non–safety-net hospitals using Agency for Healthcare Research and Quality and American Hospital Association data. JAMA Surg. 2019;154:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wakeam E, Hevelone ND, Maine R, et al. Failure to rescue in safety-net hospitals: availability of hospital resources and differences in performance. JAMA Surg. 2014;149:229–235. [DOI] [PubMed] [Google Scholar]
- 9.Alkhouli M, Alqahtani F, Holmes DR, Berzingi C. Racial disparities in the utilization and outcomes of structural heart disease interventions in the United States. J Am Heart Assoc. 2019;8:e012125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagger JP, Edwards MB, Taylor KM. Influence of socioeconomic status on survival after primary aortic or mitral valve replacement. Heart. 2008;94:182–185. [DOI] [PubMed] [Google Scholar]
- 11.Hoyler MM, Feng TR, Ma X, et al. Insurance status and socioeconomic factors affect early mortality after cardiac valve surgery. J Cardiothorac Vasc Anesth. 2020;34:3234–3242. [DOI] [PubMed] [Google Scholar]
- 12.LaPar DJ, Bhamidipati CM, Walters DM, et al. Primary payer status affects outcomes for cardiac valve operations. J Am Coll Surg. 2011;212:759–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ando T, Adegbala O, Akintoye E, Briasoulis A, Takagi H. The impact of safety-net burden on inhospital outcomes after surgical aortic valve replacement. J Card Surg. 2019;34:1178–1184. [DOI] [PubMed] [Google Scholar]
- 14.Glance LG, Kellermann AL, Osler TM, Li Y, Li W, Dick AW. Impact of risk adjustment for socioeconomic status on risk-adjusted surgical readmission rates. Ann Surg. 2016;263:698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoehn RS, Wima K, Vestal MA, et al. Effect of hospital safety-net burden on cost and outcomes after surgery. JAMA Surg. 2016;151:120–128. [DOI] [PubMed] [Google Scholar]
- 16.Sridhar P, Bhatt M, Qureshi MM, et al. Esophageal cancer presentation, treatment, and outcomes vary with hospital safety-net burden. Ann Thorac Surg. 2019;107:1472–1479. [DOI] [PubMed] [Google Scholar]
- 17.Sheikh MA, Deo SV, Riaz H, et al. Safety-net hospitals versus non-safety centers and clinical outcomes after trans-catheter aortic valve replacement. Catheter Cardiovasc Interv. 2021;97:E425–E430. [DOI] [PubMed] [Google Scholar]
- 18.Tang OY, Rivera Perla KM, Lim RK, Weil RJ, Toms SA. The impact of hospital safety-net status on inpatient outcomes for brain tumor craniotomy: a 10-year nationwide analysis. Neurooncol Adv. 2021;3. vdaa167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams JB, McConnell G, Allender JE, et al. One-year results from the first US-based enhanced recovery after cardiac surgery (ERAS Cardiac) program. J Thorac Cardiovasc Surg. 2019;157:1881–1888. [DOI] [PubMed] [Google Scholar]
- 20.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA. 2000;284:2061–2069. [DOI] [PubMed] [Google Scholar]
- 21.Charles EJ, Mehaffey JH, Hawkins RB, et al. Socioeconomic distressed communities index predicts risk-adjusted mortality after cardiac surgery. Ann Thorac Surg. 2019;107:1706–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coyan GN, Okoye A, Shah A, et al. Effect of neighborhood socioeconomic factors on readmissions and mortality after coronary artery bypass grafting. Ann Thorac Surg. 2021;111:561–567. [DOI] [PubMed] [Google Scholar]
- 23.Koch CG, Li L, Kaplan GA, et al. Socioeconomic position, not race, is linked to death after cardiac surgery. Circ Cardiovasc Qual Outcomes. 2010;3:267–276. [DOI] [PubMed] [Google Scholar]
- 24.Mehaffey JH, Hawkins RB, Charles EJ, et al. Distressed communities are associated with worse outcomes after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2020;160:425–432 e429. [DOI] [PubMed] [Google Scholar]
- 25.Patrick WL, Bojko M, Han JJ, et al. Neighborhood socioeconomic status is associated with differences in operative management and long-term survival after coronary artery bypass grafting. J Thorac Cardiovasc Surg. Published online August 19, 2020. 10.1016/j.jtcvs.2020.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LaPar DJ, Stukenborg GJ, Guyer RA, et al. Primary payer status is associated with mortality and resource utilization for coronary artery bypass grafting. Circulation. 2012;126:S132–S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


