Abstract
Sustainability interventions were implemented at the Royal Brisbane and Women’s Hospital (RBWH) following identification of inhaled anaesthetic gases as a target for reducing medical carbon emissions. This quality improvement study assessed and evaluated the impact of sustainability interventions on the environmental and financial cost of inhaled anaesthetic gas use in order to guide future initiatives and research in reducing carbon emissions from healthcare practice.
Ethical exemption was granted from the RBWH Research Ethics Committee (EX/2021/QRBW/76078). Usage (bottles) and expenditure for desflurane and sevoflurane from January 2016 to December 2021 were obtained. Global warming potential and carbon dioxide equivalent (CO2e) were used to report environmental impact of volatile agents. Methods to estimate this were performed in Excel based on Campbell and Pierce methodology. An Environmental Protection Agency greenhouse gas equivalency calculator was used to convert CO2e to equivalent petrol carbon emissions and kilometres travelled by a typical passenger vehicle.
The total number of bottles of sevoflurane and desflurane purchased between January 2016 and December 2021 decreased by 34.76% from 1991 to 1299. The number of desflurane bottles purchased decreased by 95.63% from 800 to 35 bottles. The number of sevoflurane bottles purchased increased by 6.13% from 1191 bottles to 1264 bottles. This was achieved by implementing quality improvement interventions such as staff education of desflurane-sparing practices, distribution of posters and progressive removal of desflurane from operating theatres. Total carbon emission from volatile anaesthetics equalled 2326 tonnes CO2e. Combined desflurane and sevoflurane emissions decreased by 87.88%. In 2016, desflurane made up 92.39% of the annual CO2e, which steadily decreased to 33.36% in 2021. Combined sevoflurane and desflurane usage costs decreased by 58.33%.
Substantial reductions in carbon emissions from volatile anaesthetics demonstrate the significant degree to which environmentally sustainable practices have been implemented. Applying desflurane-sparing practice can heavily limit anaesthetic drug expenditure and contribution to environmental waste. This is important given the global health sector’s challenge to optimise patient outcomes in the face of global climate change crisis.
Keywords: Anaesthesia, Quality improvement, Healthcare quality improvement, Education
What is already known on this topic
Limiting the use of volatile anaesthetics can reduce the carbon footprint of healthcare and the adverse effects of occupational exposure. Recent trends of inhaled anaesthetic use and implementation of volatile-sparing strategies have not been well documented.
What this study adds
This study highlights that advocacy and education coupled with targeted systemic changes can heavily limit anaesthetic drug expenditure and contribution to environmental waste.
How this study might affect research, practice or policy
This study provides evidence that reduction of greenhouse gas emissions can be achieved with environmentally conscious anaesthetic practices, through incorporating sustainable practices at both an individual and organisational level.
Problem
Inhaled anaesthetic agents (IAAs)—specifically sevoflurane and desflurane—are potent ‘greenhouse gases’ that carry significant global warming potential (GWP) by trapping heat. Each volatile gas respectively carries 130 and 2540 times the GWP of carbon dioxide (CO2) over 100 years (GWP100). Recent literature also recognises that occupational exposure poses a potential health hazard to healthcare personnel, with associated genetic damage and oxidative stress.1 2
In supporting the ‘triple bottom line’ of sustainability in accounting for people, place and finance when considering the global impact of technology,3 use of alternatives to IAAS may therefore represent a potential target for reducing the carbon footprint of anaesthesia. Alternatives such as total intravenous anaesthesia (TIVA) and regional anaesthesia can be used, particularly as a substitution for desflurane given its colossal GWP.4 5
To quantify our contribution to greenhouse gas emissions and to implement changes, we undertook a quality assurance project to minimise the health impact of climate change and promote environmental sustainability practices in the anaesthetic workplace.6 This quality improvement (QI) project aimed to reduce hospital greenhouse gas emissions and evaluate the effectiveness of sustainability measures implemented by staff of the Department of Anaesthesia and Perioperative Medicine at the Royal Brisbane and Women’s Hospital (RBWH). Inhaled anaesthesia greenhouse gas emissions and expenditure, specifically sevoflurane and desflurane, between January 2016 and December 2021, were analysed in order to guide future initiatives and research in reducing consumption and optimising environmental and economic benefits.
Background
Climate change poses an existential threat to global health.4 7 8 The WHO has declared climate change a defining issue of the 21st century, potentially contributing to an estimated 8.9 million deaths worldwide.9 Evaluation of carbon footprint in potential hotspots allows for a targeted approach to reducing CO2 emissions contributing to pollution and climate change.
Modern IAAs include hydrofluorocarbons sevoflurane and desflurane, the chlorofluorocarbon isoflurane and nitrous oxide. These undergo minimal in vivo metabolism, and are released virtually unchanged (≥95%) into the troposphere—the lowest layer of the atmosphere in which the greenhouse gas effect occurs.10 Sevoflurane and desflurane are known to remain in the troposphere for 1.1 years and 14 years, respectively.11
For context, consumption of one bottle of sevoflurane (250 mL) during anaesthesia is the CO2 equivalent of driving 196 km in an average petrol fuel passenger car, compared with the desflurane (240 mL) CO2 equivalent of driving 3539 km.7 11 As detailed by Sherman et al, these figures do not account for the additional environmental impact of electrical energy consumed by desflurane vaporisers to heat the anaesthetic agent.10
Studies conducted in the USA, UK, Canada and Australia have described the disproportionate contribution of desflurane to carbon emissions compared with other inhaled anaesthetics.12–15 Weinberg et al found that desflurane accounted for 77% of total annual inhaled anaesthesia greenhouse gases in the Victorian public hospital system while sevoflurane and isoflurane contributed much smaller proportions of 17% and 2%, respectively.13
Despite the known adverse environmental impact of IAAs being comprehensively described, implementation of mitigation strategies has been slow. A growing body of literature recommends that use of desflurane should be restricted to cases where there is a significant patient benefit to limit the greenhouse effect of anaesthesia. Several studies suggest that actual benefits of desflurane are small and can be readily replaced with other anaesthetic agents that are more environmentally friendly.16–18 Chronic occupational exposure to unscavenged waste anaesthetic gases (WAGs) has also been reported to cause potential adverse effects.
Previous studies have investigated the impact of similar sustainability measures in Victorian, Australian and international hospitals, comparing environmental and financial impacts with significant improvements in carbon footprint.14 19 20 However, recent trends of IAA emission rates in Australia remain undocumented.
To our knowledge, this study is the first in Australia to evaluate the effectiveness of sustainability using analysis of environmental and financial cost of IAAs.
Measurement
Patients and the public were not involved in this study. Outcomes were obtained through annual audits of bottles purchased and expenditure of desflurane and sevoflurane between January 2016 and December 2021. Data were obtained from the Department of Pharmacy detailing the number of bottles distributed to the operating theatre suite and the corresponding expenditure. These purchase data were used as a surrogate measure of usage. GWP100 and CO2 equivalent (CO2e) conversions were used to report the environmental impact of the volatile agents. Methods to estimate this were performed using data analysis software based on Campbell and Pierce1 methodology.
To determine the CO2e of a volatile anaesthetic bottle, mass (kg) is multiplied by GWP of each gas. GWP100 of sevoflurane and desflurane is 130 and 2540, respectively. A bottle of desflurane (240 mL) has a CO2e of 886 kg and sevoflurane (250 mL) has a CO2e of 49 kg. An Environmental Protection Agency greenhouse gas equivalency calculator was used to convert CO2e to equivalent petrol carbon emissions and kilometres travelled by a typical passenger vehicle.21
Design
This QI activity was undertaken at the RBWH in Brisbane, Australia, between January 2016 and December 2021. RBWH is a major tertiary referral hospital and part of the Metro North Hospital and Health Service. It is the largest teaching and research hospital in Queensland and uses 22 operating theatres with anaesthesia and perioperative medicine for all surgical and interventional procedures. With over 28 000 surgeries and more than 10 000 interventional procedures per year, this department is an ideal target for implementation of anaesthetic sustainability improvements to reduce carbon emissions.
QI interventions were implemented and overseen by the department director and staff specialists. No formal staff training was required. Presentations on awareness of environmental impact of IAAs were given to staff. Implementation was achieved by senior staff specialist anaesthetists raising awareness of the environmental impact of IAAs and voluntarily augmenting their practice to avoid desflurane. Registrar and resident doctors from other hospitals on rotation through RBWH were educated by senior staff specialists about avoiding the use of desflurane where possible. This is primarily administered on an individual-individual basis during supervised theatre time. Education is encouraged to include the following topics: environmental impact of IAA, avoiding use of desflurane, alternatives to IAA including regional anaesthesia and TIVA, low-flow anaesthesia and end-tidal (ET) control mode. Information on the topic was further disseminated via email and newsletters to all departmental staff. Posters and infographics were displayed in break rooms and high-traffic areas. An example of a displayed infographic can be seen below (figure 1). The anaesthetic machines were configurated to recirculate sampling gas. From April 2021, desflurane vaporisers from individual operating theatres were progressively removed. The department made a formal pledge to be desflurane free by 2022.
Figure 1.
A range of posters and educational material was developed for display in break rooms and high traffic areas. In this example, an Environmental Protection Agency greenhouse gas equivalency calculator was used to convert CO2e of IAAs to equivalent petrol carbon emissions and kilometres travelled by a typical passenger vehicle. (2) This information was then applied to the local context to more clearly demonstrate the impact of IAAs. Posters also provided suggestions for reducing use of desflurane. ET, end-tidal; TIVA, total intravenous anaesthesia.
Strategy
QI interventions took place between 2016 and 2021 at RBWH.
Behavioural changes:
Raised awareness of the environmental impact of volatile anaesthetics.
Face-to-face departmental meetings.
Poster designed and distributed.
Journal club presentations on scientific evidence.
Encouraged regional anaesthesia and TIVA.
Encouraging use of low fresh gas flows (FGFs) with IAA.
Encouraging use of ET control mode to deliver volatile anaesthetic agents.
Regular updates on achievements (CO2 reduction, financial savings).
Director of department support.
System changes:
Gradual removal of desflurane vaporisers from individual operating theatres.
Upgraded intravenous pump fleet and anaesthetic machines.
Automated control of circuit anaesthetic concentrations (ET control mode).
Configuring anaesthetic machines to recirculate sampling gas.
Anaesthetic machines default to low FGFs with volatile anaesthetics.
Annual usage and expenditure data of IAA were reviewed by the department director and Department of Anaesthesia and Perioperative Pharmacy Group. QI strategies were progressively implemented in the order above.
Results
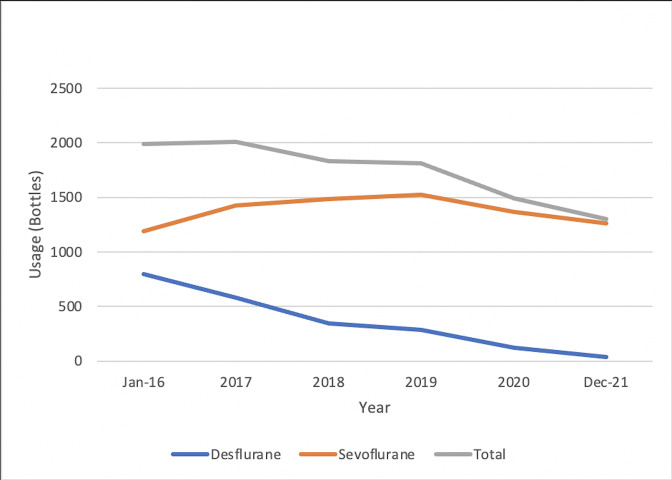
The quantity of desflurane and sevoflurane bottles purchased during a 6-year period from January 2016 to December 2021 was assessed. The number of sevoflurane bottles was initially 1191, with a slight increase to 1525 bottles in 2019 before decreasing to 1264 by the end of 2021. Overall, this represents a slight increase of 6.13%. Bottles of desflurane purchased decreased from 800 to 35, which represents a reduction of 95.63%. The total number of volatile bottles purchased decreased from 1991 to 1299. This represents a 34.76% total reduction of sevoflurane and desflurane bottles purchased (figure 2).
Figure 2.
Number of desflurane and sevoflurane bottles purchased from pharmacy data.
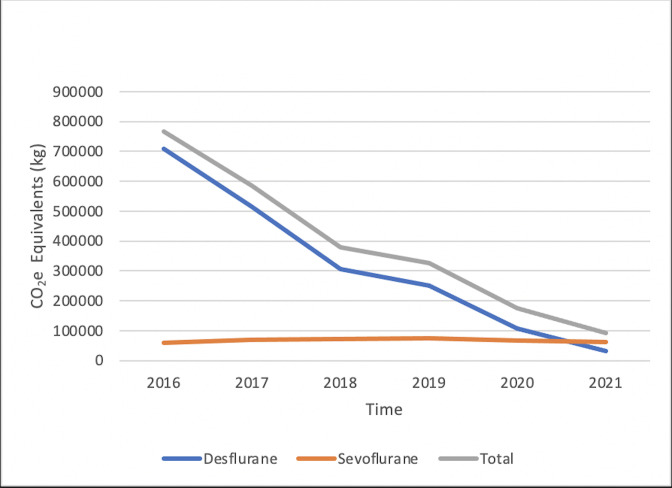
Based on the number of sevoflurane and desflurane bottles purchased from January 2016 to December 2021, the department’s total carbon emission was equivalent to 2325.74 tonnes of CO2e. Individually, sevoflurane emissions were 58.36 tonnes CO2e in 2016 compared with 61.94 tonnes CO2e in 2021. This demonstrates a 6.13% increase in carbon footprint for sevoflurane. Desflurane carbon emissions equalled 708.8 tonnes CO2e in 2016 and decreased to 31.01 tonnes CO2e in 2021. This demonstrates a 95.63% reduction of carbon footprint for desflurane. Combined desflurane and sevoflurane emissions decreased from 767.16 tonnes CO2e to 92.95 tonnes CO2e, representing a reduction of 87.88% (figure 3).
Figure 3.
Annual greenhouse gas contribution of desflurane and sevoflurane in CO2e. CO2e, carbon dioxide equivalent.
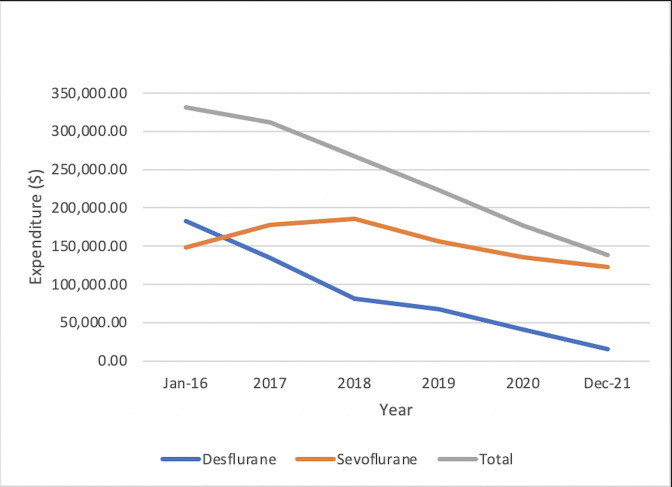
Expenditure for sevoflurane slightly increased between 2016 and 2018 before overall decreasing from $A148 167.73 in 2016 to $A122 906.1 in 2021. Expenditure for desflurane steadily decreased from $A182 992.30 in 2016 to $A15 085.62 in 2021. The expenditure for sevoflurane and desflurane combined decreased from $A331 160.04 in 2016 to $A137 991.72 in 2021, which represents a reduction in cost of 58.33%. This reduction was achieved despite the 88.45% increase in average cost per bottle of desflurane in 2021 (figure 4).
Figure 4.
Annual expenditure of desflurane and sevoflurane in Australian dollar.
Lessons and limitations
Limitations to this study include the fact that data on individual interventions are not available, hence we are unable to gauge the specific degree of contribution each QI activity had on overall carbon footprint reduction. More data points regarding individual clinician use of IAAs, duration of anaesthetic and duration of desflurane use would be useful in future.
For example, while FGF rates collection was not part of the methodology of this study, it seems reasonable that post-education gas flow rates are lower than previously given the significant reduction in desflurane consumption.19 22 A 2014 New Zealand study found that even without specific initiatives, FGF used in one institution’s anaesthetic department decreased by 35% over 4 years.23 This study therefore lends support to the proposal by Kennedy and French23 that there is an ongoing trend towards the use of lower FGFs in volatile anaesthetics. Improvements in equipment and monitoring are likely additional contributing factors. Future studies could collect information on FGF rates used in individual cases.
Direct utilisation of volatile gases was not able to be obtained, hence pharmacy purchasing data are used as a surrogate. Utilisation of volatile and corresponding carbon emissions is therefore likely to be overestimated.
Nitrous oxide is another source of IAA carbon emissions that contributes significantly to global warming and ozone depletion. While non-medical sources are responsible for most nitrous oxide emissions, nitrous oxide is commonly used as an adjunct to other gases. Studies show that addition of 60% FGF of 2 L/min nitrous oxide to 1-MAC hour of sevoflurane can increase the global warming impact of the compound by a ratio of 5.9.12 However, consumption of nitrous oxide was not assessed as part of this study as majority of medical use originates from the maternal ward at RBWH.
Given that a reduction in IAAs would necessitate replacement with other forms of anaesthesia, collection of data on alternatives such as regional anaesthesia or TIVA would provide a more informed and holistic comparison of anaesthetic trends in future studies.
As a large tertiary hospital, generalisability of findings is broad due to the variety and volume of surgeries that the hospital provides and therefore the application of desflurane-sparing practices can be applied to. The sustainability interventions implemented were straightforward and applicable to other major and regional institutions. Yearly re-auditing of IAAs is recommended to re-evaluate practice patterns over time, and a multi-institutional audit would allow for comprehensive analysis of practice trends state-wide and nationally. A de-identified questionnaire could also be sent to staff to gauge departmental sentiment towards IAAs.
Conclusions
Annual desflurane use decreased drastically at RBWH. Bottles of desflurane used decreased from 800 bottles in 2016 to 35 bottles in 2021. Comparatively, a multicentre audit of 65 Victorian public hospitals in 2014 reported that bottles of desflurane increased by 726 per year (288 in 2005 to 1164 in 2011).9 While the Victorian study is not directly comparable due to the different time frame, lack of overlapping years and absence of data on specific initiatives, our study suggests an evolution in practice towards desflurane-sparing techniques.
Desflurane has by far the highest impact on the RBWH Department of Anaesthesia and Perioperative Medicine emissions. Out of a total 2326 tonnes of CO2e generated in the last 6 years, 83% of the department’s volatile-related greenhouse gas emissions can be attributed to desflurane. For context, this is equivalent to a passenger car driving more than 9.4 million km, or 235 times around the earth.21 This is despite the fact that the department, as of 2021, used approximately 36 times more sevoflurane than desflurane annually (figure 2). This proportion of greenhouse gas emissions is similar to those found in previous Australasian studies. A review of 65 Victorian public hospitals in 2014 reported that desflurane contributed 77% of overall carbon emissions over a period of 7 years.13 While isoflurane was no longer being used in the majority of Victorian public hospitals, sevoflurane and desflurane remained as the primary volatile agents, used respectively at a ratio of 2.2 to 1. This supports the fact that desflurane use has a GWP that is exponentially greater than sevoflurane.24
Our data also confirm the potential for significant cost savings by reducing the use of desflurane.5 25 26 The department has made substantial savings by reducing the proportion of desflurane spending from over $180 000 down to $15 085.62 annually.
Low FGF
Low-flow anaesthesia has been found to consume less inhaled anaesthetic, reduce cost, and waste and environmental impact, with improved patient safety compared with using high FGF.27 The principle of this revolves around a lower FGF equating to higher fractions of gases recirculated within a system, leading to less wastage. Ryan and Nielsen16 propose achieving ideal FGF rates at 2 L/min with sevoflurane, and 0.5 L/min with desflurane. More recent studies have shown that using FGF <1 L/min with sevoflurane is safe, despite recommendations against this on product information sheets due to concern for compound A production.28 Gordon24 further emphasises the importance of low-flow anaesthesia as any FGF that exceeds the patient’s needs and the system requirements will be delivered essentially unchanged into the atmosphere.
Kennedy and French reported that even a small absolute change in flow rate (1.95 to 1.27 L/min), resulted in potential annual savings of more than US$130 000.19 23 This further emphasises that small degrees of change spread across many cases can add up to a significant reduction in IAA consumption and cost.
Avoiding unnecessary flushing of the circuit also prevents excess occupational exposure through WAGs. This, along with scavenging systems, hazard awareness training, regular monitoring and maintenance of anaesthesia delivery equipment, may reduce risk of adverse effects of chronic workplace exposure.1 5
Total intravenous anaesthesia
Another such intervention, TIVA, has been reported in multiple publications to be environmentally more favourable than IAAs in life cycle assessments.5 10 The greenhouse gas emissions that result from using desflurane are approximately 2600 times the emissions that result from using propofol.24 Despite sevoflurane proving to be far less detrimental, it still results in approximately 135 times greater emissions than propofol. A first principles study by Sherman et al10 found that when accounting for the entire life cycle, including natural resource extraction, manufacturing, transportation, usage and even disposal of medical waste that is generated from propofol infusions like syringes and tubing, the GWPs of inhaled anaesthetics are four orders-of-magnitude greater than a MAC-equivalent quantity of propofol. Importantly, propofol may offer an advantage over desflurane with respect to postoperative nausea and vomiting and time to discharge after ambulatory surgery.29 30
ET control mode
Modern technology on anaesthetic machines allows for manual or automated control of ET gas concentrations.31 Machines capable of regulating the gas mixture and FGF of oxygen, nitrogen dioxide and volatile anaesthetic agents simplify the management of volatile agents in delivering selected ET concentrations.10 31 32
Studies have shown that automated ET control modes can minimise the quantity of IAA used to maintain a selected ET concentration.6 10 33 Tay et al31 illustrate how automated control reduced costs by 27% and decreased greenhouse gas emissions by 44%, with these changes mainly facilitated by a proportional reduction in desflurane use.
Automated ET control improves compliance and participation in low-flow anaesthesia. All anaesthetic machines currently in use at the author’s hospital (RBWH) are capable of this function.
Removal of desflurane from individual operating theatres
Currently, RBWH has removed desflurane from anaesthetic machines and placed bottles elsewhere outside the operating room to limit accessibility. Anecdotally, limiting the accessibility of a drug or having barriers to access dramatically decrease use.
When considering whether desflurane could be permanently removed from the hospital formulary, one of the disincentives cited in literature is the preference for desflurane use in the context of obesity and long-duration anaesthesia to facilitate rapid recovery.34 Evidence indicates it can reduce extubation time compared with sevoflurane.35–37 Despite faster initial recovery with desflurane, studies have not demonstrated significant differences in later recovery periods or a reduction in postoperative respiratory complications.38 39 Evidence is lacking with respect to cost-effective utilisation of operating room time.40 This has prompted authors to comment that, in the face of imminent environmental collapse, the marginal benefits of desflurane compared with sevoflurane in any instance are far outweighed by the very significant environmental impact of desflurane.3 5 6 41
As global momentum builds against desflurane, predictions are that desflurane will no longer be used in Australian hospitals within the next decade or earlier.42 Already in other developed nations, a growing number of institutions are successfully implementing desflurane reduction, with an American study citing 27% of hospitals having eliminated desflurane entirely from their formularies.43 44 In Melbourne, The Alfred and Western Health have taken similar approaches by removing desflurane from their hospital formulary and anaesthetic trolley, respectively.42 45
Conclusion
Despite the continually decreasing trend of volatile usage within the department at RBWH, there is still room for further reductions in use. As ‘greening’ initiatives are not just the responsibility of one person or discipline,8 advocacy of climate change issues within and between departments should continue to be undertaken to incorporate sustainable practices at an organisational level.
This substantial 87.88% reduction in aggregate greenhouse gas contributions reflects an encouraging trend towards more environmentally conscious anaesthetic practices at RBWH. This highlights that the simple, yet safe, interventions when clinically appropriate can have a significantly positive outcome with regard to pollution and global health.
Acknowledgments
We would like to thank Liam Busuttin for his help in providing pharmacy purchasing data.
Footnotes
Contributors: KW is corresponding author and guarantor of this work. KW conceived the idea for the study. KW, GE and YW implemented interventions. KW, KLC and GE performed statistical analysis. YW designed educational material. KW, KLC and GE drafted and reviewed the paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
An ethical exemption was granted from the Royal Brisbane and Women’s Hospital Human Research Ethics Committee (EX/2021/QRBW/76078).
References
- 1.Varughese S, Ahmed R. Environmental and occupational considerations of anesthesia: a narrative review and update. Anesth Analg 2021;133:826–35. 10.1213/ANE.0000000000005504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neghab M, Kargar-Shouroki F, Mozdarani H, et al. Association between genotoxic properties of inhalation anesthetics and oxidative stress biomarkers. Toxicol Ind Health 2020;36:454–66. 10.1177/0748233720935696 [DOI] [PubMed] [Google Scholar]
- 3.Freeman S. Desflurane - balancing environmental costs and cognitive benefits. Anaesthesia 2019;74:948. 10.1111/anae.14728 [DOI] [PubMed] [Google Scholar]
- 4.Campbell M, Pierce JMT, Tom JM. Atmospheric science, anaesthesia, and the environment. BJA Educ 2015;15:173–9. 10.1093/bjaceaccp/mku033 [DOI] [Google Scholar]
- 5.McGain F, Muret J, Lawson C, et al. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020;125:680–92. 10.1016/j.bja.2020.06.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ANZCA . PS64: statement on environmental sustainability in anaesthesia and pain medicine practice Australian and New Zealand College of Anaesthetists; 2019. [DOI] [PubMed] [Google Scholar]
- 7.Malik A, Lenzen M, McAlister S, et al. The carbon footprint of Australian health care. Lancet Planet Health 2018;2:e27–35. 10.1016/S2542-5196(17)30180-8 [DOI] [PubMed] [Google Scholar]
- 8.Wyssusek KH, Keys MT, van Zundert AAJ. Operating room greening initiatives - the old, the new, and the way forward: A narrative review. Waste Manag Res 2019;37:3–19. 10.1177/0734242X18793937 [DOI] [PubMed] [Google Scholar]
- 9.Organization WH . Climate change; 2021.
- 10.Sherman J, Le C, Lamers V, et al. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg 2012;114:1086–90. 10.1213/ANE.0b013e31824f6940 [DOI] [PubMed] [Google Scholar]
- 11.Sulbaek Andersen MP, Sander SP, Nielsen OJ, et al. Inhalation anaesthetics and climate change. Br J Anaesth 2010;105:760–6. 10.1093/bja/aeq259 [DOI] [PubMed] [Google Scholar]
- 12.Facilities TFoESCoEa . Greening the operating room: environmental sustainability for anesthesia practice: American Society of Anesthesiologists. Available: https://www.asahq.org/about-asa/governance-and-committees/asa-committees/committee-on-equipment-and-facilities/environmental-sustainability/greening-the-operating-room
- 13.Weinberg L, Tay S, Aykanat V, et al. Changing patterns in volatile anaesthetic agent consumption over seven years in Victorian public hospitals. Anaesth Intensive Care 2014;42:579–83. 10.1177/0310057X1404200506 [DOI] [PubMed] [Google Scholar]
- 14.de Vos MA R. Bc Anesthesiologists reduce carbon footprint by choosing wisely. BC Medical Journal 2021;63:30–3. [Google Scholar]
- 15.Unit SD . Sustainable Development in Health and Care Report 2018 National Health Service; 2018. https://www.sduhealth.org.uk/policy-strategy/reporting/sustainable-development-in-health-and-care-report-2018.aspx [Google Scholar]
- 16.Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth Analg 2010;111:92–8. 10.1213/ANE.0b013e3181e058d7 [DOI] [PubMed] [Google Scholar]
- 17.Shine KP. Climate effect of inhaled anaesthetics. Br J Anaesth 2010;105:731–3. 10.1093/bja/aeq313 [DOI] [PubMed] [Google Scholar]
- 18.White S. Desflurane - balancing the environmental costs and cognitive benefits. a reply. Anaesthesia 2019;74:949. 10.1111/anae.14731 [DOI] [PubMed] [Google Scholar]
- 19.Kennedy R, French R. An audit of anaesthetic fresh-gas flow rates and volatile anaesthetic use in a teaching hospital. N Z Med J 2003;116:U438. [PubMed] [Google Scholar]
- 20.Weinberg L, Story D, Nam J, et al. Pharmacoeconomics of volatile inhalational anaesthetic agents: an 11-year retrospective analysis. Anaesth Intensive Care 2010;38:849–54. 10.1177/0310057X1003800507 [DOI] [PubMed] [Google Scholar]
- 21.EPA . Greenhouse gas Equivalencies calculator. Washington, DC: United States Environmental Protection Agency, 2021. https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator [Google Scholar]
- 22.McKenzie AJ. Reinforcing a "low flow" anaesthesia policy with feedback can produce a sustained reduction in isoflurane consumption. Anaesth Intensive Care 1998;26:371–6. 10.1177/0310057X9802600405 [DOI] [PubMed] [Google Scholar]
- 23.Kennedy RR, French RA. A ten-year audit of fresh gas flows in a New Zealand Hospital: the influence of the introduction of automated agent delivery and comparisons with other hospitals. Anaesth Intensive Care 2014;42:65–72. 10.1177/0310057X1404200112 [DOI] [PubMed] [Google Scholar]
- 24.Gordon D. Sustainability in the operating room: reducing our impact on the planet. Anesthesiol Clin 2020;38:679–92. 10.1016/j.anclin.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim D, Son J-S, Lee JR, et al. A comparison of desflurane consumption according to fresh gas flow. Korean J Anesthesiol 2014;67:S13–14. 10.4097/kjae.2014.67.S.S13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edmonds A, Stambaugh H, Pettey S, et al. Evidence-based project: cost savings and reduction in environmental release with low-flow anesthesia. Aana J 2021;89:27–33. [PubMed] [Google Scholar]
- 27.Arslan M, Gişi G, Öksüz G, et al. Are high fresh gas flow rates necessary during the wash-in period in low-flow anesthesia? Kaohsiung J Med Sci 2020;36:834–40. 10.1002/kjm2.12251 [DOI] [PubMed] [Google Scholar]
- 28.Kennedy RR, Hendrickx JF, Feldman JM. There are no dragons: low-flow anaesthesia with sevoflurane is safe. Anaesth Intensive Care 2019;47:223–5. 10.1177/0310057X19843304 [DOI] [PubMed] [Google Scholar]
- 29.Kumar G, Stendall C, Mistry R, et al. A comparison of total intravenous anaesthesia using propofol with sevoflurane or desflurane in ambulatory surgery: systematic review and meta-analysis. Anaesthesia 2014;69:1138–50. 10.1111/anae.12713 [DOI] [PubMed] [Google Scholar]
- 30.Lebenbom-Mansour MH, Pandit SK, Kothary SP, et al. Desflurane versus propofol anesthesia: a comparative analysis in outpatients. Anesth Analg 1993;76:936–41. 10.1213/00000539-199305000-00004 [DOI] [PubMed] [Google Scholar]
- 31.Tay S, Weinberg L, Peyton P, et al. Financial and environmental costs of manual versus automated control of end-tidal gas concentrations. Anaesth Intensive Care 2013;41:95–101. 10.1177/0310057X1304100116 [DOI] [PubMed] [Google Scholar]
- 32.Sulbaek Andersen MP, Nielsen OJ, Wallington TJ, et al. Medical intelligence article: assessing the impact on global climate from general anesthetic gases. Anesth Analg 2012;114:1081–5. 10.1213/ANE.0b013e31824d6150 [DOI] [PubMed] [Google Scholar]
- 33.Feldman JM. Managing fresh gas flow to reduce environmental contamination. Anesth Analg 2012;114:1093–101. 10.1213/ANE.0b013e31824eee0d [DOI] [PubMed] [Google Scholar]
- 34.Sneyd JR. Thiopental to desflurane - an anaesthetic journey. Where are we going next? Br J Anaesth 2017;119:i44–52. 10.1093/bja/aex328 [DOI] [PubMed] [Google Scholar]
- 35.Singh PM, Borle A, McGavin J, et al. Comparison of the recovery profile between desflurane and sevoflurane in patients undergoing bariatric Surgery-a meta-analysis of randomized controlled trials. Obes Surg 2017;27:3031–9. 10.1007/s11695-017-2929-6 [DOI] [PubMed] [Google Scholar]
- 36.Liu F-L, Cherng Y-G, Chen S-Y, et al. Postoperative recovery after anesthesia in morbidly obese patients: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth 2015;62:907–17. 10.1007/s12630-015-0405-0 [DOI] [PubMed] [Google Scholar]
- 37.La Colla L, Albertin A, La Colla G, et al. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth 2007;99:353–8. 10.1093/bja/aem197 [DOI] [PubMed] [Google Scholar]
- 38.Albrecht E, Bayon V, Hirotsu C, et al. Impact of short-acting vs. standard anaesthetic agents on obstructive sleep apnoea: a randomised, controlled, triple-blind trial. Anaesthesia 2021;76:45–53. 10.1111/anae.15236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zucco L, Santer P, Levy N, et al. A comparison of postoperative respiratory complications associated with the use of desflurane and sevoflurane: a single-centre cohort study. Anaesthesia 2021;76:36–44. 10.1111/anae.15203 [DOI] [PubMed] [Google Scholar]
- 40.Werner JG, Castellon-Larios K, Thongrong C, et al. Desflurane allows for a faster emergence when compared to sevoflurane without affecting the baseline cognitive recovery time. Front Med 2015;2:75. 10.3389/fmed.2015.00075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yasny JS, White J. Environmental implications of anesthetic gases. Anesth Prog 2012;59:154–8. 10.2344/0003-3006-59.4.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.ANZCA . The Alfred ditches desflurane. Melbourne: Australian and New Zealand College of Anaesthetists; 2021. https://www.anzca.edu.au/news/top-news/the-alfred-ditches-desflurane [Google Scholar]
- 43.Greenhealth P. The value of sustainability initiatives in surgical suites Reston Practice Greenhealth; 2018. https://practicegreenhealth.org/sites/default/files/upload-files/2018.gor_.report.pdf [Google Scholar]
- 44.Burns C. Drop in NHS use of desflurane cuts CO2 emissions equal to nearly 200 million miles by car. Pharm J 2021. [Google Scholar]
- 45.McGain F. Anaesthetic Gases- greenhouse gas reductions. Melbourne: Global Green and Healthy Hospitals; 2016. https://www.hospitalesporlasaludambiental.net/wp-content/uploads/2016/07/Waste-and-Chemicals-Anaesthetic-Gases-Greenhouse-Gas-Reductions-Western-Health-Australia.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information.