Abstract
Methamphetamine use is surging globally as a cause of morbidity and mortality. Treatment is typically sought in early abstinence, when craving and depressive symptoms are intense, contributing to relapse and poor outcomes. To advance an understanding of this problem and identify therapeutic targets, we conducted a retrospective analysis of brain structure in 89 adults with Methamphetamine Use Disorder who were in early abstinence and 89 healthy controls. Unlike most prior research, the participants did not significantly differ in age, sex, and recent use of alcohol and tobacco (p-values ≥ 0.400). We analyzed thickness across the entire cerebral cortex by fitting a general linear model to identify differences between groups. Follow-up regressions were performed to determine whether cortical thickness in regions showing group differences was related to craving, measured on a visual analog scale, or to the Beck Depression Inventory score. Participants in early methamphetamine abstinence (M ± SD = 22.1 ± 25.6 days) exhibited thinner cortex in clusters within bilateral frontal, parietal, temporal, insular, and right cingulate cortices relative to controls (p-values < 0.001, corrected for multiple comparisons). Unlike craving (β = 0.007, p = 0.947), depressive symptoms were positively correlated with cortical thickness across clusters (β = 0.239, p = 0.030) and with thickness in the anterior cingulate cluster (β = 0.246, p = 0.027) in the methamphetamine-dependent group. Inasmuch as anterior cingulate pathology predicts response to antidepressants for Major Depressive Disorder, cingulate structure may also identify patients with Methamphetamine Use Disorder who can benefit from antidepressant medication.
Keywords: anterior cingulate cortex, brain structure, cortical thickness, depressive symptoms, gray matter, Methamphetamine Use Disorder
INTRODUCTION
Methamphetamine use and its role in overdose deaths are escalating.1–3 Because early relapse characterizes Methamphetamine Use Disorder and thwarts therapeutic success,4 it is paramount to understand the biological bases of problems in early abstinence. Spontaneous craving for methamphetamine decreases during the first month,5,6 but cue-induced craving rises before declining at 3 months of abstinence.5 Depressive symptoms pose further challenges as they predict low treatment attendance and continued methamphetamine use.7
The U.S. Food and Drug Administration has not approved any medication for Methamphetamine Use Disorder, and non-pharmacological interventions remain the mainstay of treatment. Cognitive behavioral therapy reduces craving, depressive symptoms, and methamphetamine use,8,9 as does exercise training, which also reduces stimulant use.8,10–12 However, cognitive deficits interfere with therapy13–16 and predict poor treatment outcomes across substance use disorders.17
Novel approaches that consider problems in early abstinence, when patients typically seek treatment, are needed. Structural brain correlates of depressive symptoms promise to provide therapeutic targets and improve treatment matching inasmuch as numerous studies relate gray matter to the therapeutic response of patients with Major Depressive Disorder.18,19 Anatomical neuroimaging studies, including some from our laboratory,20,21 have compared participants with Methamphetamine Use Disorder and healthy controls. Participants ranging in abstinence from hours to several months had deficits relative to controls in gray-matter volumes of orbitofrontal, dorsolateral prefrontal, and superior temporal cortices22 and gray-matter densities of the left middle frontal gyrus and bilateral insula.23 When the abstinence period lasted 4 to 7 days, participants with Methamphetamine Use Disorder exhibited smaller gray-matter volumes in cingulate, limbic, and paralimbic cortices of the right hemisphere21 and smaller gray-matter volumes in the right inferior temporal, left superior temporal, right supramarginal, and left precentral gyri.20
Cortical deficits appear to reverse and even show compensatory increases. Gray-matter volume in the left superior temporal gyrus increased between 1 and 4 weeks of abstinence from methamphetamine,20 and volumes of orbitofrontal and parietal cortices were positively related to the duration of abstinence, which ranged from 12 to 400 days, in men.24 Participants who were abstinent from methamphetamine for 6 months or more exhibited higher gray-matter density in the right middle frontal gyrus than those abstinent for shorter periods, but both groups had lower gray-matter density in this region than healthy controls.25
Prior studies of early methamphetamine abstinence were of small sample sizes, and case and control groups were generally not matched on sex or use of substances other than methamphetamine. The largest study compared 61 participants with Methamphetamine Use Disorder (54 smoked tobacco) with 44 controls (17 smoked) and excluded individuals with an abstinence period of less than 2 weeks.23 This and another study22 grouped individuals over several months of abstinence from methamphetamine when compensatory changes in brain structure may occur.23–25 Moreover, studies measured cortical volume, a composite of thickness and surface area, which are independent and should be considered separately.26 Indeed, individuals ranging in methamphetamine abstinence from hours to decades exhibited smaller gray-matter volumes in bilateral frontal and right insular cortices, and thickness deficits in bilateral frontal and rostral anterior cingulate cortices, but no abnormalities in surface areas compared with healthy controls.27
Here we studied 89 individuals with Methamphetamine Use Disorder in early abstinence (M ± SD = 22.1 ± 25.6 days) and 89 healthy controls who were similar in age, sex, and recent use of alcohol and tobacco. Groups were compared on the entire cerebrum to identify regional differences in cortical thickness, a measure associated with lower false positive rates in surface-based analysis than volume and surface area.28 We hypothesized that thickness deficits in early methamphetamine abstinence would be related to craving and depressive symptoms, thereby revealing possible targets for intervention.
MATERIALS AND METHODS
Study Design
This cross-sectional investigation pooled data from studies that were approved by the institutional review board of the University of California at Los Angeles. Some of these data were used in other analyses.20,29–36 Participants were recruited with online and print advertisements. They provided written informed consent after a detailed explanation of the respective studies and received monetary compensation. Eligibility was ascertained by interview, physical examination, and laboratory tests. Participants were excluded for major medical illnesses and psychiatric conditions warranting treatment other than Methamphetamine or Nicotine Dependence, which were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).37 Given the correspondence of DSM-IV Stimulant Dependence with DSM-5 Stimulant Use Disorder,38,39 we refer to methamphetamine-dependent participants as having Methamphetamine Use Disorder. They had urine tests positive for methamphetamine at study entry but negative tests for methamphetamine, amphetamines, cocaine, opiates, benzodiazepines, and alcohol at behavioral and neuroimaging assessments. Healthy controls tested negative for all substances listed above at baseline and times of assessment.
Participants were between the ages of 26 and 54. The lower end of the age range represents a time after cortical thinning starts decelerating in young adulthood.40,41 T1-weighted brain images were collected using a magnetization-prepared rapid acquisition gradient echo sequence on a 1.5-T Sonata (field of view: 256 × 256 mm2, 160 sagittal slices, resolution: 1 mm3), a 3-T Trio (field of view: 256 × 256 mm2, 176 sagittal slices, resolution: 1 mm3), or a 3-T Prisma scanner (field of view: 300 × 320 mm2, 208 sagittal slices, resolution: 0.8 mm3; all Siemens, Erlangen, Germany). We used the recon-all pipeline of FreeSurfer 6.0.0 (surfer.nmr.mgh.harvard.edu) and constructed 3D models of cortical surface to measure local cortical thickness.42 For group analysis, the data were resampled into a common space and smoothed with a 10-mm full-width half-maximum kernel.
Among 488 participants with brain images, data from 297 met FreeSurfer quality control criteria as determined by the automated tool Qoala-T.43 Cortical thickness data from 287 participants (89 with Methamphetamine Use Disorder and 198 healthy controls) could be harmonized using ComBat, a method that adjusts for differences in scanner type and scan protocol while preserving biological associations.44 ComBat thereby reduces spurious findings and increases the power and reproducibility of statistical tests.44 This also holds when participant characteristics are not randomly distributed across scanners and protocols as demonstrated by harmonizing two datasets with different age groups to conduct a life-span study.44
We applied the case-control algorithm of SPSS 27 (IBM, Armonk, NY, USA) to match 89 of the 198 healthy controls to the 89 participants with Methamphetamine Use Disorder on sex, years of formal education, and whether they smoked cigarettes. Of the 178 participants for final analysis, a subsample of 32 was also matched on cannabis use status, depressive symptoms, and scanner for image acquisition. Evaluation with the ENIGMA Cortical Quality Control Protocol 2.0 (enigma.usc.edu) revealed frontal or temporal pole underestimations in 3 participants from the Methamphetamine Use Disorder group and 2 from the control group. The analyses reported included these participants as their exclusion did not change any results.
Analytic Strategy
Analyses of group differences in demographics and use of addictive substances other than methamphetamine were conducted in SPSS, using a significance level of 0.05 (two-tailed). Categorical variables were assessed with Pearson’s chi-square and Fisher’s exact tests. Continuous variables were examined with Mann-Whitney U and Kruskal-Wallis tests after determining that the data were not normally distributed by evaluating histograms, normal quantile-quantile plots, and tests of normality (Kolmogorov-Smirnov, Shapiro-Wilk).
We conducted a general linear model vertex-wise analysis over the whole cerebrum, using FreeSurfer software to identify group differences in cortical thickness. Cohen’s d was calculated from the age-adjusted model as a measure of effect size (0.2 = small, 0.5 = medium, 0.8 = large). 45 Vertices were considered significant at p < 0.001, with a cluster correction set at p < 0.05 to account for multiple comparisons.28
Follow-up regressions were performed in SPSS, using a significance level of 0.05 (two-sided). Regressions were controlled for age40 in keeping with the vertex-wise analysis. The average thickness across clusters with significant group differences, weighted by cluster size, was used as the dependent variable. We first assessed whether this measure was related to participant characteristics exhibiting at least trend-level group differences. We then analyzed how the weighted average thickness across clusters was related to sex, methamphetamine use (lifetime years, days in the past 30), and aspects of early abstinence (duration, craving, depressive symptoms). In case of significant effects, we conducted subsequent regressions on clusters in regions of interest. Correlation coefficients are reported to quantify the relationship between variables that were significantly linked to cortical thickness.
RESULTS
Description of the Study Sample (Table 1)
Table 1:
Participant Characteristics
| Healthy Control | Methamphetamine Use Disorder | Group Difference | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 34.9 ± 6.9 | 36.0 ± 7.5 | U = 4249.5, z = 0.842, p = 0.400 |
| Women/Men | 34/55 | 34/55 | None |
| Education (years) | 13.3 ± 1.8 | 12.4 ± 2.0 | U = 2800.5, z = −3.483, p < 0.001* |
| Employed | 53 | 15 | X2 (1) = 36.032, p < 0.001* |
| Ethnicity/Race | X2 (4) = 26.256, p < 0.001* | ||
| African American | 22 | 6 | + |
| Asian/Pacific Islander | 6 | 5 | − |
| Caucasian | 44 | 31 | + |
| Hispanic | 12 | 27 | + |
| Other | 5 | 20 | + |
| Any Use in Past 30 Days | |||
| Alcohol | 57 | 58 | X2 (1) = 0.069, p = 0.792 |
| Tobacco (cigarettes) | 73 | 73 | None |
| Cannabis | 26 | 38 | X2 (1) = 3.513, p = 0.061 |
| Methamphetamine Use | |||
| Age of first use | 23.2 ± 7.8# | ||
| Lifetime years | 9.8 ± 6.6# | ||
| Days in the past 30 | 16.1 ± 10.7† | ||
| Preferred route of administration F | |||
| Smoking | 57 | ||
| Intravenous | 18 | ||
| Intranasal | 11 | ||
| Oral | 1 | ||
| None | 1 | ||
| At Brain Scan | |||
| Days abstinent | 22.1 ± 25.6† | ||
| Craving | 21.4 ± 26.2# | ||
| BDI | 3.1 ± 5.5 | 8.7 ± 8.6# | U = 4993.0, z = 5.851, p < 0.001* |
| Scanner | Χ2 (2) = 29.469, p < 0.001* | ||
| 1.5-T Sonata | 23 | 18 | – |
| 3-T Trio | 9 | 41 | + |
| 3-T Prisma | 57 | 30 | + |
Values of variables are the number of participants in the relevant group or group M ± SD. Craving for methamphetamine was measured on a visual analog scale from 0 (none) to 100 (extreme). The Beck Depression Inventory (BDI) distinguishes no or minimal (< 10), mild to moderate (10–18), moderate to severe (19–29), and severe depressive symptoms (30–63).61 U (Mann-Whitney U test), X2 (Pearson’s chi-square test),
significant group difference at p < 0.05, significant (+) or non-significant (−) at p < 0.05 in Bonferroni-adjusted post hoc analyses
significantly or
non-significantly different at p < 0.05 across scanners in Kruskal-Wallis tests (specific p-values given in text)
non-significantly different across scanners in Fisher’s exact test (X2 (8) = 3.526, p = 0.981)
The sample consisted of 89 adults with Methamphetamine Use Disorder and 89 healthy controls who were matched 1:1 on sex and cigarette smoking status. Healthy controls were also selected based on educational attainment, but participants with Methamphetamine Use Disorder had fewer years of formal education and were more often unemployed than controls (p-values < 0.05). Hispanics were overrepresented whereas African Americans and Caucasians were underrepresented in the Methamphetamine Use Disorder group (p-values < 0.05 in Bonferroni-adjusted pairwise comparisons). The groups were comparable in age and whether they consumed alcohol in the past 30 days (p-values ≥ 0.400). Cannabis use in the past 30 days was numerically more frequent in participants with Methamphetamine Use Disorder (p = 0.061), who reported more depressive symptoms than controls (p < 0.05). Other variables related to early abstinence and methamphetamine use are listed in Table 1.
The subsample consisted of 16 adults with Methamphetamine Use Disorder and 16 healthy controls who were matched 1:1 on image acquisition (per group: 4 scanned on 1.5-T Sonata, 6 on 3-T Trio, and 6 on 3-T Prisma), sex (4 women per group), and any tobacco or cannabis use in the past 30 days (13 and 4, respectively, per group). Years of education (Mann-Whitney U = 104.5, z = −1.022, p = 0.381) and the Beck Depression Inventory score (Mann-Whitney U = 149.5, z = 0.843, p = 0.423) were comparable across case (years: 12.2 ± 1.2, score: 2.8 ± 3.6) and control groups of the subsample (years: 12.4 ± 1.2, score: 2.4 ± 3.6).
Cortical Thickness and Participant Characteristics
The vertex-wise analysis of thickness across the entire cerebral cortex revealed group differences for 17 clusters, all of which displayed less thickness in individuals with Methamphetamine Use Disorder relative to controls (p-values < 0.001, corrected for multiple comparisons; Table 2, Figure 1). These deficits were not attributable to group differences in image acquisition or participant characteristics as indicated by no main effects of scanning (p-values of dummy variables ≥ 0.275), ethnicity (p-values of dummy variables ≥ 0.192), education (p = 0.704), employment (p = 0.997), cannabis use (p = 0.553), or depressive symptoms (p = 0.248) on the weighted average thickness across the 17 clusters. Group (β = −0.548, p < 0.001) and age (β = −0.281, p < 0.001) showed main effects in this regression (R2 = 0.41, F (12, 148) = 8.48, p < 0.001), with the Methamphetamine Use Disorder group and older age being associated with reduced cortical thickness. Age and group status were not significantly correlated (rS = 0.063, p = 0.401).
Table 2:
Cortical Thickness: Methamphetamine Use Disorder < Healthy Control
| Size (mm2) | MNI305 (X, Y, Z) | HC (M ± SE) | MUD (M ± SE) | −lg(p) | Cohen’s d | |
|---|---|---|---|---|---|---|
| Left Hemisphere | ||||||
| Frontal Lobe | ||||||
| Orbital gyri | 417 | −42.6, 37.3, −13.9 | 2.77 ± .015 | 2.64 ± .014 | 6.3568 | 0.79 |
| 140 | −16.9, 33.9, −21.7 | 2.55 ± .022 | 2.42 ± .019 | 4.8242 | 0.67 | |
| Frontomarginal g., s. | 805 | −27.0, 57.3, −8.9 | 2.71 ± .019 | 2.57 ± .016 | 6.7319 | 0.82 |
| Temporal Lobe | ||||||
| Fusiform g. | 232 | −38.5, −62.5, −17.4 | 2.73 ± .019 | 2.61 ± .017 | 4.4877 | 0.64 |
| Insula | ||||||
| Inferior circular s. | 234 | −46.5, −5.9, −16.3 | 3.09 ± .021 | 2.93 ± .019 | 5.8533 | 0.75 |
| Subcentral G. and Sulci | 148 | −44.0, −20.4, 16.6 | 2.83 ± .023 | 2.69 ± .022 | 4.0309 | 0.60 |
| Right Hemisphere | ||||||
| Frontal Lobe | ||||||
| Orbital gyri | 454 | 15.4, 16.6, −22.5 | 2.79 ± .021 | 2.63 ± .016 | 7.1616 | 0.85 |
| 229 | 39.6, 25.4, −11.7 | 2.98 ± .021 | 2.83 ± .021 | 6.2791 | 0.78 | |
| Superior frontal g. | 397 | 9.3, 61.2, 6.7 | 2.70 ± .018 | 2.57 ± .015 | 4.2660 | 0.62 |
| Frontomarginal g., s. | 423 | 36.0, 55.1, −7.2 | 2.59 ± .018 | 2.48 ± .014 | 4.4753 | 0.64 |
| Limbic Lobe | ||||||
| Anterior cingulate g., s. | 173 | 15.1, 40.4, 13.9 | 2.71 ± .015 | 2.59 ± .017 | 6.2876 | 0.78 |
| Middle-posterior cingulate g., s. | 258 | 5.3, −22.1, 39.6 | 2.85 ± .016 | 2.72 ± .014 | 7.0042 | 0.84 |
| Temporal Lobe | ||||||
| Lateral-superior temporal g. | 693 | 63.0, −13.2, −2.0 | 2.91 ± .016 | 2.76 ± .016 | 6.6551 | 0.81 |
| Middle temporal g. | 145 | 64.2, −24.6, −12.7 | 3.07 ± .019 | 2.95 ± .017 | 5.6962 | 0.74 |
| Insula | ||||||
| Inferior circular s. | 147 | 46.0, −15.1, −8.7 | 2.75 ± .020 | 2.61 ± .019 | 4.3889 | 0.63 |
| Parietal Lobe | ||||||
| Precuneus | 146 | 5.0, −61.6, 28.2 | 2.60 ± .016 | 2.51 ± .014 | 4.6405 | 0.65 |
| Occipital Lobe | ||||||
| Occipital pole | 209 | 9.2, −90.7, 14.0 | 1.93 ± .017 | 1.83 ± .016 | 4.3997 | 0.63 |
The vertex-wise analysis of cortical thickness (listed in mm) over the whole cerebrum was controlled for age.40 Vertices were considered significant at p < 0.001, with a cluster correction set at p < 0.05 to account for multiple comparisons.28 Cohen’s d was calculated as a measure of effect size (0.2 = small, 0.5 = medium, 0.8 = large).45 HC (Healthy Control), MUD (Methamphetamine Use Disorder), MNI305 (Montreal Neurological Institute coordinates), g (gyrus), s (sulcus)
Figure 1:
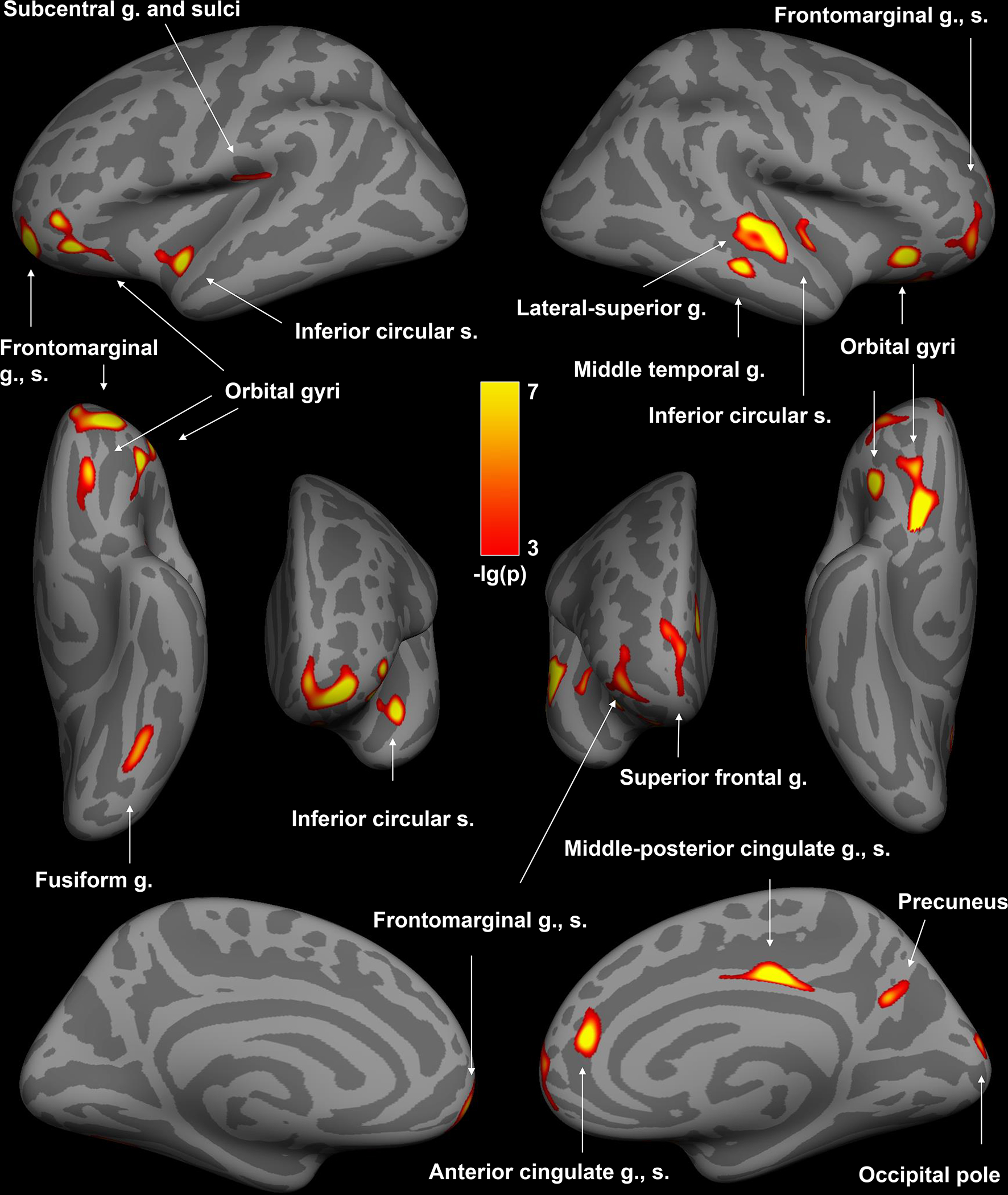
Clusters of thinner cortex in the left and right hemispheres of individuals with Methamphetamine Use Disorder compared with controls. The vertex-wise analysis of thickness across the entire cerebral cortex was controlled for age.40 Vertices were considered significant at p < 0.001, with a cluster correction set at p < 0.05 to account for multiple comparisons.28 Lower p-values are colored brighter. g (gyrus), s (sulcus)
The main effect of group on the weighted average thickness across clusters (β = −0.543, p = 0.005) remained significant in the subsample analysis (R2 = 0.60, F (8, 23) = 4.27, p = 0.003), controlling for age (β = −0.296, p = 0.053), ethnicity (p-values of dummy variables ≥ 0.227), education (p = 0.236), employment (p = 0.959), and depressive symptoms (p = 0.438).
Depressive symptoms (β = 0.239, p = 0.030) and age (β = −0.270, p = 0.014) exerted main effects on the weighted average thickness across clusters in the Methamphetamine Use Disorder group (R2 = 0.15, F (2, 75) = 6.54, p = 0.002). Age and depressive symptoms were not significantly correlated in these participants (rS = −0.056, p = 0.625). We conducted a regression analysis on the cluster in the anterior cingulate because positron emission tomography and functional magnetic resonance imaging studies linked this region to depressive symptoms in Methamphetamine Use Disorder.46,47 Depressive symptoms in early methamphetamine abstinence (β = 0.246, p = 0.027) were also related to cortical thickness in the anterior cingulate cluster (R2 = 0.12, F (2, 75) = 5.26, p = 0.007; Figure 2).
Figure 2:
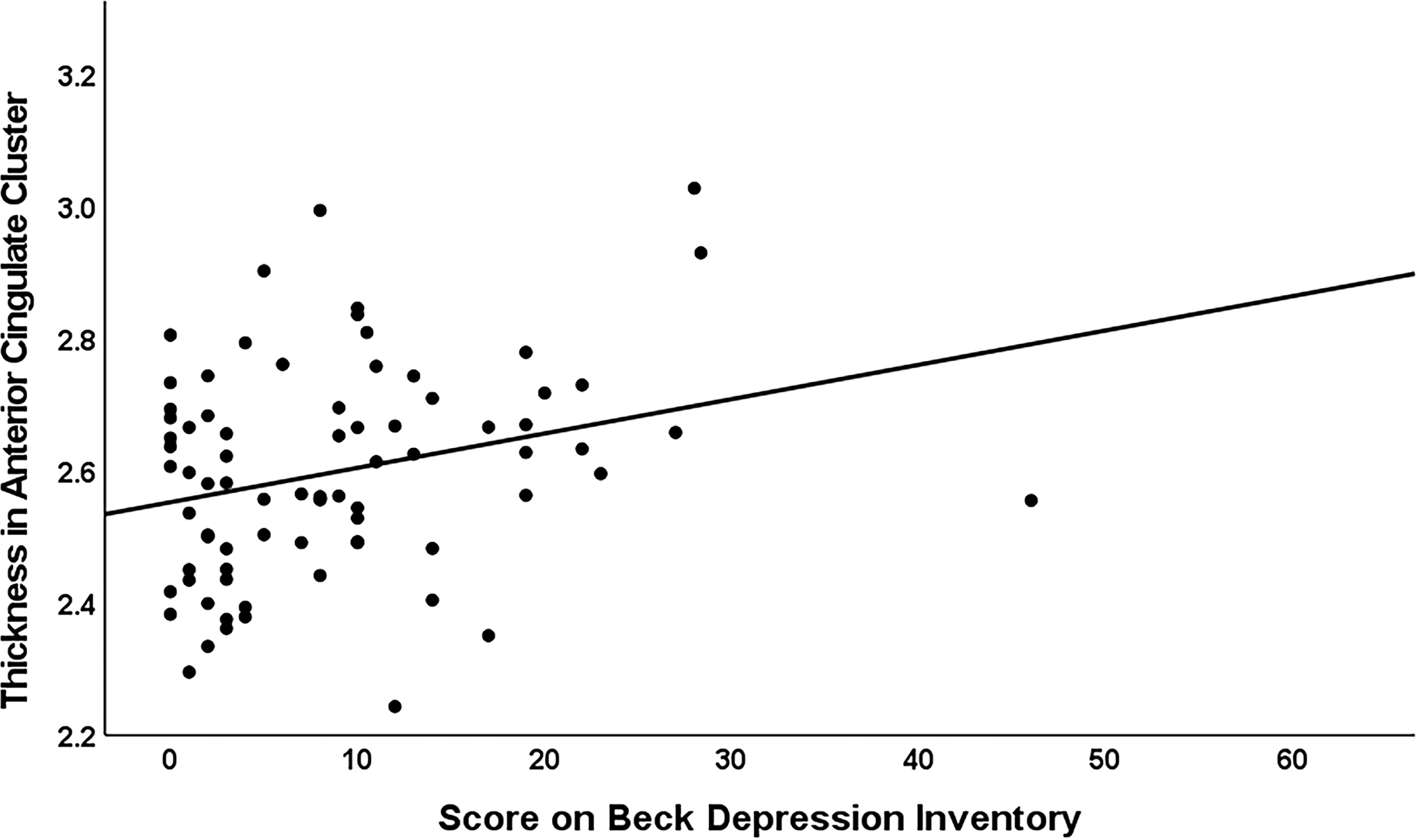
In people who were in early abstinence from chronic methamphetamine use, the age-adjusted regression analysis on the anterior cingulate cluster (R2 = 0.12, F (2, 75) = 5.26, p = 0.007) demonstrated a main effect of depressive symptoms (β = 0.246, p = 0.027) on cortical thickness (displayed in mm). This effect was retained (β = 0.314, p = 0.004) when conducting this regression analysis (R2 = 0.16, F (2, 74) = 7.25, p = 0.001) without the participant who scored 46 on the Beck Depression Inventory (minimal < 10, mild to moderate 10–18, moderate to severe 19–29, severe 30–63).61
Further regressions on data from the Methamphetamine Use Disorder group revealed no main effects on the weighted average thickness across clusters of sex (β = −0.004, p = 0.966), years of methamphetamine use (β = −0.072, p = 0.500), days used in the past 30 (β = 0.068, p = 0.508), days abstinent (β = −0.116, p = 0.333), or craving (β = 0.007, p = 0.947). These variables were in part unevenly distributed across scanners: sex (Pearson’s Χ2 (2) = 4.756, p = 0.093), years of methamphetamine use (Kruskal-Wallis H (2) = 1.303, p = 0.521), days used in the past 30 (Kruskal-Wallis H (2) = 23.855, p < 0.001), days abstinent (Kruskal-Wallis H (2) = 22.099, p < 0.001), craving (Kruskal-Wallis H (2) = 4.869, p = 0.088). Yet, separate regressions for each scanner subgroup did not reveal main effects on the weighted average thickness across clusters of sex (p-values ≥ 0.236), years of methamphetamine use (p-values ≥ 0.242), days used in the past 30 (p-values ≥ 0.210), days abstinent (p-values ≥ 0.190), or craving (p-values ≥ 0.332).
DISCUSSION
Reports on brain structure in early methamphetamine abstinence20–23 are inconsistent, probably due to small sample sizes, different volumetric measurements, and insufficiently controlled confounders. We thus conducted the largest analysis to date of brain structure and the first of cortical thickness across the entire cerebrum in early-abstinent adults with Methamphetamine Use Disorder. Relative to healthy controls, who were comparable in age, sex, and recent use of alcohol and tobacco, they exhibited clusters of thinner cortex in bilateral frontal, parietal, temporal, insular, and right cingulate regions.
Thickness across clusters and thickness of the anterior cingulate cluster were positively correlated with self-report of depressive symptoms in early abstinence, suggesting that gray-matter loss accompanies processes leading to cortical thickening and depressive symptoms. In this regard, methamphetamine causes oxidative stress, excitotoxicity, inflammation, reactive gliosis, and neuroadaptations.48–50 It is conceivable that neuronal loss translates into cortical thinning, whereas glial proliferation following neuronal damage leads to cortical enlargement.48 The proliferation of glial cells has a higher metabolic demand than that of neurons, and cortical enlargement may be related to a higher metabolic rate for glucose.48 Gray-matter volumetric deficits were congruent with metabolic deficits in the right anterior cingulate in overlapping samples of individuals in early abstinence from chronic methamphetamine use,21,47 and depressive symptoms covaried positively with metabolic activity in this region.47 These reports and our data suggest that depressive symptomatology in early abstinence is a behavioral expression of cortical enlargement in regions, such as the right anterior cingulate, where a relative gray-matter deficit is apparent in people with Methamphetamine Use Disorder.
Major Depressive Disorder features gray-matter deficits in the anterior cingulate cortex,51 where enlargements in early stages have also been associated with increased metabolism, inflammation, and neurocompensatory processes.52,53 Greater pretreatment anterior cingulate volume and increase in thickness early in treatment of Major Depressive Disorder predict response to antidepressants.18,19 Leveraging the biomarker potential of the anterior cingulate may improve machine learning algorithms that use pretreatment whole-brain patterns and reach accuracies of 64–89% for antidepressant response prediction in these patients.18 Antidepressants can reduce depressive symptoms and relapse in methamphetamine abstinence as shown for bupropion and mirtazapine in some individuals.54–56 Future studies may examine whether anterior cingulate thickness in those who respond to these medications differs from that in non-responders. Results from such analysis should be interpreted with the understanding that a single medication will likely not be effective for the entire heterogeneous population of people with Methamphetamine Use Disorder.56
The multiple areas of thickness deficits across the cerebral cortex echo the range of cognitive deficits associated with methamphetamine use, including problems with language, attention, memory, psychomotor function, cognitive control, and decision-making.13–16 Some impairments have been linked to structural and functional brain abnormalities in early methamphetamine abstinence.13,14,16 The most consistent correlations are reported for poor cognitive control and decision-making with attenuated activity in prefrontal and anterior cingulate cortices as measured by positron emission tomography and magnetic resonance imaging.16 Both regions exhibit structural deficits in the present work, suggesting that they may underlie these functional abnormalities. The prefrontal and anterior cingulate cortices are therefore promising therapeutic targets, particularly as poor self-control and decision-making have been related to treatment failures.14 Transcranial magnetic and transcranial direct current stimulations of the dorsolateral prefrontal cortex have produced positive effects on executive functions and withdrawal symptoms in people with Methamphetamine Use Disorder.8 The stimulation of the prefrontal cortex can modulate activity in the anterior cingulate, which may partly explain the beneficial effects.57 Technological advances allow for noninvasive direct stimulation of the anterior cingulate, promising more precise therapies of cognitive and affective dysfunctions than is possible by stimulating superficial areas.57
Limitations
The cross-sectional design of this study precludes causal claims regarding the effects of methamphetamine, abstinence from the drug, and depressive symptoms on brain structure. Cortical thickness was not significantly associated with duration of use, recent use, or days of abstinence, but was inversely correlated with cumulative methamphetamine use in other studies,58,59 which suggests a threshold effect for structural change. Cross-sectional investigations spanning longer periods of methamphetamine abstinence than studied here and longitudinal research point towards normalizing effects of abstinence on cortical deficits,20,23–25 indicating that methamphetamine use causes gray-matter loss that is partially recoverable. Deficits may also predate Methamphetamine Use Disorder as less orbitofrontal cortical thickness in adolescents using methamphetamine was associated with a family history of drug use.58 They might also be influenced by differences in alcohol, tobacco, and cannabis use20,60 as quantity of use for these substances was not controlled although the groups did not differ in the percentages of participants who used them. Finally, we conducted a vertex-wise analysis over the whole cerebral cortex to identify methamphetamine-related alterations that might be accessible to available interventions (e.g., transcranial brain stimulation) and thus did not include subcortical structures.
Conclusion
Early abstinence from chronic methamphetamine use features widespread cortical thickness deficits. The severity of depressive symptoms is associated with these deficits, specifically within the right anterior cingulate cortex. Just as anterior cingulate pathology in Major Depressive Disorder predicts response to antidepressants, cingulate structure may also identify patients with Methamphetamine Use Disorder who can benefit from antidepressant medication. Transcranial stimulation of the right anterior cingulate offers another exciting avenue to reduce depressive symptoms and relapse to methamphetamine use. Future research may link the identified thickness deficits to specific cognitive impairments and thereby reveal more targets for improving brain function and therapeutic success.
ACKNOWLEDGMENTS
This research was supported by grants from the National Institute on Drug Abuse (R01 DA027633) and the National Institutes of Health (K23 DA927734, R21 DA034928 (ACD); R01 DA015179, R01 DA020726, P20 DA022539 (EDL)). Additional funding was provided by UCLA Clinical and Translational Science Institute (UL1TR000124), the Thomas P. and Katherine K. Pike Chair of Addiction Studies (EDL), the Marjorie M. Greene Trust (EDL), and a postdoctoral research grant from the Max Kade Foundation (JP). The funders were not involved in the conceptualization of the study; collection, analysis, and interpretation of data; preparation of the manuscript, or decision to submit it for publication.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.UNODC. World Drug Report 2020, Booklet 2 Drug use and health consequences. Vienna: United Nations publication; 2020. [Google Scholar]
- 2.Han B, Compton WM, Jones CM, Einstein EB, Volkow ND. Methamphetamine Use, Methamphetamine Use Disorder, and Associated Overdose Deaths Among US Adults. JAMA Psychiatry. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential - United States, 2003–2017. MMWR Morb Mortal Wkly Rep. 2019;68(17):388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brecht ML, Herbeck D. Time to relapse following treatment for methamphetamine use: a long-term perspective on patterns and predictors. Drug Alcohol Depend. 2014;139:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang G, Shi J, Chen N, et al. Effects of length of abstinence on decision-making and craving in methamphetamine abusers. PLoS One. 2013;8(7):e68791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zorick T, Nestor L, Miotto K, et al. Withdrawal symptoms in abstinent methamphetamine-dependent subjects. Addiction. 2010;105(10):1809–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glasner-Edwards S, Marinelli-Casey P, Hillhouse M, Ang A, Mooney LJ, Rawson R. Depression among methamphetamine users: association with outcomes from the Methamphetamine Treatment Project at 3-year follow-up. J Nerv Ment Dis. 2009;197(4):225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AshaRani PV, Hombali A, Seow E, Ong WJ, Tan JH, Subramaniam M. Non-pharmacological interventions for methamphetamine use disorder: a systematic review. Drug Alcohol Depend. 2020;212:108060. [DOI] [PubMed] [Google Scholar]
- 9.Stuart AM, Baker AL, Denham AMJ, et al. Psychological treatment for methamphetamine use and associated psychiatric symptom outcomes: A systematic review. J Subst Abuse Treat. 2020;109:61–79. [DOI] [PubMed] [Google Scholar]
- 10.Huang J, Zheng Y, Gao D, Hu M, Yuan T. Effects of Exercise on Depression, Anxiety, Cognitive Control, Craving, Physical Fitness and Quality of Life in Methamphetamine-Dependent Patients. Front Psychiatry. 2019;10:999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rawson RA, Chudzynski J, Mooney L, et al. Impact of an exercise intervention on methamphetamine use outcomes post-residential treatment care. Drug Alcohol Depend. 2015;156:21–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trivedi MH, Greer TL, Rethorst CD, et al. Randomized Controlled Trial Comparing Exercise to Health Education for Stimulant Use Disorder: Results From the CTN-0037 STimulant Reduction Intervention Using Dosed Exercise (STRIDE) Study. J Clin Psychiatry. 2017;78(8):1075–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dean AC, Groman SM, Morales AM, London ED. An evaluation of the evidence that methamphetamine abuse causes cognitive decline in humans. Neuropsychopharmacology. 2013;38(2):259–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.London ED, Kohno M, Morales AM, Ballard ME. Chronic methamphetamine abuse and corticostriatal deficits revealed by neuroimaging. Brain Res. 2015;1628(Pt A):174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Potvin S, Pelletier J, Grot S, Hébert C, Barr AM, Lecomte T. Cognitive deficits in individuals with Methamphetamine Use Disorder: a meta-analysis. Addict Behav. 2018;80:154–160. [DOI] [PubMed] [Google Scholar]
- 16.Sabrini S, Wang GY, Lin JC, Ian JK, Curley LE. Methamphetamine use and cognitive function: a systematic review of neuroimaging research. Drug Alcohol Depend. 2019;194:75–87. [DOI] [PubMed] [Google Scholar]
- 17.Brorson HH, Ajo Arnevik E, Rand-Hendriksen K, Duckert F. Drop-out from addiction treatment: a systematic review of risk factors. Clin Psychol Rev. 2013;33(8):1010–1024. [DOI] [PubMed] [Google Scholar]
- 18.Enneking V, Leehr EJ, Dannlowski U, Redlich R. Brain structural effects of treatments for depression and biomarkers of response: a systematic review of neuroimaging studies. Psychol Med. 2020;50(2):187–209. [DOI] [PubMed] [Google Scholar]
- 19.Fonseka TM, MacQueen GM, Kennedy SH. Neuroimaging biomarkers as predictors of treatment outcome in Major Depressive Disorder. J Affect Disord. 2018;233:21–35. [DOI] [PubMed] [Google Scholar]
- 20.Morales AM, Lee B, Hellemann G, O’Neill J, London ED. Gray-matter volume in methamphetamine dependence: cigarette smoking and changes with abstinence from methamphetamine. Drug Alcohol Depend. 2012;125(3):230–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thompson PM, Hayashi KM, Simon SL, et al. Structural abnormalities in the brains of human subjects who use methamphetamine. J Neurosci. 2004;24(26):6028–6036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakama H, Chang L, Fein G, Shimotsu R, Jiang CS, Ernst T. Methamphetamine users show greater than normal age-related cortical gray matter loss. Addiction. 2011;106(8):1474–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz DL, Mitchell AD, Lahna DL, et al. Global and local morphometric differences in recently abstinent methamphetamine-dependent individuals. NeuroImage. 2010;50(4):1392–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nie L, Ghahremani DG, Mandelkern MA, et al. The relationship between duration of abstinence and gray-matter brain structure in chronic methamphetamine users. Am J Drug Alcohol Abuse. 2021;47(1):65–73. [DOI] [PubMed] [Google Scholar]
- 25.Kim SJ, Lyoo IK, Hwang J, et al. Prefrontal grey-matter changes in short-term and long-term abstinent methamphetamine abusers. Int J Neuropsychopharmacol. 2006;9(2):221–228. [DOI] [PubMed] [Google Scholar]
- 26.Winkler AM, Kochunov P, Blangero J, et al. Cortical thickness or grey matter volume? The importance of selecting the phenotype for imaging genetics studies. NeuroImage. 2010;53(3):1135–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kogachi S, Chang L, Alicata D, Cunningham E, Ernst T. Sex differences in impulsivity and brain morphometry in methamphetamine users. Brain Struct Funct. 2017;222(1):215–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Greve DN, Fischl B. False positive rates in surface-based anatomical analysis. NeuroImage. 2018;171:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dean AC, Morales AM, Hellemann G, London ED. Cognitive deficit in methamphetamine users relative to childhood academic performance: link to cortical thickness. Neuropsychopharmacology. 2018;43(8):1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dean AC, Nurmi EL, Moeller SJ, et al. No effect of attentional bias modification training in methamphetamine users receiving residential treatment. Psychopharmacology (Berl). 2019;236(2):709–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dean AC, Nurmi EL, Morales AM, Cho AK, Seaman LC, London ED. CYP2D6 genotype may moderate measures of brain structure in methamphetamine users. Addict Biol. 2021;26(3):e12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dean AC, Sevak RJ, Monterosso JR, Hellemann G, Sugar CA, London ED. Acute modafinil effects on attention and inhibitory control in methamphetamine-dependent humans. J Stud Alcohol Drugs. 2011;72(6):943–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghahremani DG, Tabibnia G, Monterosso J, Hellemann G, Poldrack RA, London ED. Effect of modafinil on learning and task-related brain activity in methamphetamine-dependent and healthy individuals. Neuropsychopharmacology. 2011;36(5):950–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morales AM, Kohno M, Robertson CL, Dean AC, Mandelkern MA, London ED. Gray-matter volume, midbrain dopamine D2/D3 receptors and drug craving in methamphetamine users. Mol Psychiatry. 2015;20(6):764–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perez Diaz M, Pochon JB, Ghahremani DG, et al. Sex Differences in the Association of Cigarette Craving with Insula Structure. Int J Neuropsychopharmacol. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robertson CL, Ishibashi K, Chudzynski J, et al. Effect of exercise training on striatal dopamine D2/D3 receptors in methamphetamine users during behavioral treatment. Neuropsychopharmacology. 2016;41(6):1629–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association Publishing; 1994. [Google Scholar]
- 38.Gilder DA, Gizer IR, Lau P, Ehlers CL. Item response theory analyses of DSM-IV and DSM-5 stimulant use disorder criteria in an American Indian community sample. Drug Alcohol Depend. 2014;135:29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livne O, Shmulewitz D, Stohl M, Mannes Z, Aharonovich E, Hasin D. Agreement between DSM-5 and DSM-IV measures of substance use disorders in a sample of adult substance users. Drug Alcohol Depend. 2021;227:108958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Storsve AB, Fjell AM, Tamnes CK, et al. Differential longitudinal changes in cortical thickness, surface area and volume across the adult life span: regions of accelerating and decelerating change. J Neurosci. 2014;34(25):8488–8498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tamnes CK, Ostby Y, Fjell AM, Westlye LT, Due-Tønnessen P, Walhovd KB. Brain maturation in adolescence and young adulthood: regional age-related changes in cortical thickness and white matter volume and microstructure. Cereb Cortex. 2010;20(3):534–548. [DOI] [PubMed] [Google Scholar]
- 42.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage. 1999;9(2):179–194. [DOI] [PubMed] [Google Scholar]
- 43.Klapwijk ET, van de Kamp F, van der Meulen M, Peters S, Wierenga LM. Qoala-T: A supervised-learning tool for quality control of FreeSurfer segmented MRI data. NeuroImage. 2019;189:116–129. [DOI] [PubMed] [Google Scholar]
- 44.Fortin JP, Cullen N, Sheline YI, et al. Harmonization of cortical thickness measurements across scanners and sites. NeuroImage. 2018;167:104–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen J A power primer. Psychol Bull. 1992;112(1):155–159. [DOI] [PubMed] [Google Scholar]
- 46.Ghavidel N, Khodagholi F, Ahmadiani A, Khosrowabadi R, Asadi S, Shams J. Frontocingulate Dysfunction Is Associated with Depression and Decreased Serum PON1 in Methamphetamine-Dependent Patients. Neuropsychiatr Dis Treat. 2020;16:489–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.London ED, Simon SL, Berman SM, et al. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Arch Gen Psychiatry. 2004;61(1):73–84. [DOI] [PubMed] [Google Scholar]
- 48.Berman S, O’Neill J, Fears S, Bartzokis G, London ED. Abuse of amphetamines and structural abnormalities in the brain. Ann N Y Acad Sci. 2008;1141:195–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krasnova IN, Cadet JL. Methamphetamine toxicity and messengers of death. Brain Res Rev. 2009;60(2):379–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paulus MP, Stewart JL. Neurobiology, clinical presentation, and treatment of Methamphetamine Use Disorder: a review. JAMA Psychiatry. 2020;77(9):959–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schmaal L, Hibar DP, Sämann PG, et al. Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA Major Depressive Disorder Working Group. Mol Psychiatry. 2017;22(6):900–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li Q, Zhao Y, Chen Z, et al. Meta-analysis of cortical thickness abnormalities in medication-free patients with major depressive disorder. Neuropsychopharmacology. 2020;45(4):703–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Suh JS, Schneider MA, Minuzzi L, et al. Cortical thickness in major depressive disorder: A systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;88:287–302. [DOI] [PubMed] [Google Scholar]
- 54.Chan B, Freeman M, Kondo K, et al. Pharmacotherapy for Methamphetamine/Amphetamine Use Disorder - a systematic review and meta-analysis. Addiction. 2019;114(12):2122–2136. [DOI] [PubMed] [Google Scholar]
- 55.Siefried KJ, Acheson LS, Lintzeris N, Ezard N. Pharmacological treatment of methamphetamine/amphetamine dependence: a systematic review. CNS Drugs. 2020;34(4):337–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soares E, Pereira FC. Pharmacotherapeutic strategies for Methamphetamine Use Disorder: mind the subgroups. Expert Opin Pharmacother. 2019;20(18):2273–2293. [DOI] [PubMed] [Google Scholar]
- 57.Zhao Y, Sallie SN, Cui H, et al. Anterior Cingulate Cortex in Addiction: New Insights for Neuromodulation. Neuromodulation. 2020. [DOI] [PubMed] [Google Scholar]
- 58.Lyoo IK, Yoon S, Kim TS, et al. Predisposition to and effects of methamphetamine use on the adolescent brain. Mol Psychiatry. 2015;20(12):1516–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Okita K, Morales AM, Dean AC, et al. Striatal dopamine D1-type receptor availability: no difference from control but association with cortical thickness in methamphetamine users. Mol Psychiatry. 2018;23(5):1320–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jacobus J, Castro N, Squeglia LM, et al. Adolescent cortical thickness pre- and post marijuana and alcohol initiation. Neurotoxicol Teratol. 2016;57:20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


