Abstract
Background:
In Germany, the number of calls for Emergency Medical Services (EMS) are increasing, while the number of general practitioners and hospitals are decreasing, resulting in a growing demand and workload for emergency physicians and paramedics. Furthermore, an aging population with increasingly complex medical histories, present emergencies in which a more detailed assessment and therapies are urgently needed. Therefore, common EMS systems need to find solutions to handle these problems.
Methods:
We used a user-focused five-step approach to define a technological solution: Research of current systems, definition of goals and requirements, development of concept, test series and evaluation, evaluation of costs and benefits.
Results:
Development of a holistic telemedical concept to connect in-hospital clinical emergency physicians and paramedics on the scene, by implementing and connecting systems that are already partially being used in common EMS in Germany. By using live audio and video communication, including vital signs between the two, a system can be established by keeping costs low, affordable and at the same time protecting patient data in line with General Data Protection Regulation.
Conclusion:
Implementing technologies in a practical specialty like Emergency Medicine with a user-focused approach demonstrates that the hurdle for integration into established routines can improve current processes. Evaluation of costs and usability is a main driver to define success of such concepts and can improve if such systems can be developed to be used in larger networks.
Keywords: eHealth, telemedicine, emergency medicine, emergency medical service communication systems, pre-hospital emergency care
Introduction
In Germany, the demand for Emergency Medical Services (EMS) is steadily growing.1 –4 Numbers of professionals, medical resources, and equipment are increasing and public service investments are being adjusted to the growing demand.5 –7 But as the amount of emergency medical professionals available on the job market is diminishing, the demand for such services is still high.8 –11
As a result, currently used strategies and options, which commonly are used for increases in demand in the emergency healthcare sectors, are now turning into exhausted sources.7,12,13
Therefore, new options need to be discussed.
Technology, especially in healthcare, is rapidly becoming more available. However, at the same time, is leading to an increase in costs that is inconsistent with the growth in patient benefits and outcomes. We, therefore, sought out available technological solutions for EMS and based on these results developed a more available and easier-to-apply system to ease the demand.14,15
EMS in Germany
Patients evaluated by paramedics are mainly transferred to emergency departments (EDs), as EMS is historically and structurally organized to be part of the clinical healthcare sector. This system was developed to treat patients in life-threatening situations; therefore, a transport to an ED would be necessary.16 –18
However, the amount of non-urgent emergency responses is increasing. Patients are being transported to hospitals, despite the fact that they could be treated in other primary care facilities, such as a general practitioners (GPs) or specialist doctor’s offices. Increasingly, this has led to an overcrowding and overuse of current capacities, especially by younger patients. Such problems are not only reported in Germany, but also in many other countries.19 –21
In addition to the aforementioned, Germany has an Emergency Physician (EP)–based EMS system, in which in life-threatening situations, an EP-staffed vehicle is sent to the site of emergency in addition to an ambulance.22 –24 As the demand for these EPs is increasing and the current system continues to rely on response times of an average of about 10 min for ambulances and about 15 min for the arrival of an EP, varying due to differing federal state regulations, more options are needed to maintain an appropriate standard of care in the near future.24 –27
Telemedicine in EMS in Germany
To manage this increase in demand, technology in the form of telemedicine has been used and implemented in a few regions.
As a technology, telemedicine is a branch of e-health and defined by the World Health Organization (WHO) as the delivery of healthcare services by using communication networks to connect geographically distributed users with another. It, therefore, could overcome various barriers to medical access, address issues like shortages or uneven distribution of human and structural medical resources.28,29
Telemedicine in Emergency Medicine has been shown to be effective in EDs early since 1999 30 and has also been internationally implemented into daily use in urban and rural regions.31,32 Some systems, like for example, in Houston, TX (“Project ETHAN Houston”; Emergency Telehealth and Navigation) have served more than 10,000 calls by now and provide a long track record.33 –35
In Germany, the project “Telenotarzt Aachen” (TNA Aachen) in the state of North Rhine Westphalia currently has the longest track record and supplies the biggest area with a telemedical system.9,36 –38 Other regions in Germany, such as the federal state of Bavaria or Mecklenburg Western Pomerania are following this model, but are currently in an earlier stage of development.37,39
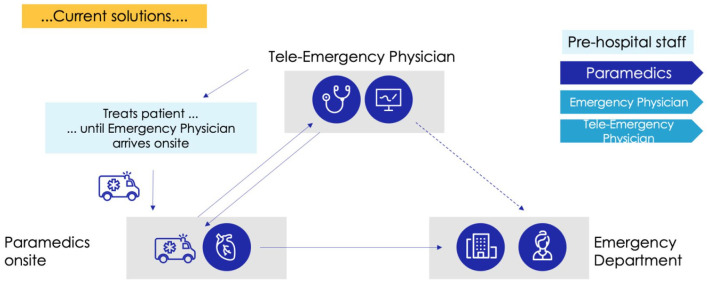
Therefore, these two telemedical systems stand out representatively and rely on the following concept: A remotely located EP, placed at a central dispatch or control center for emergency calls, provides virtual support and advice for paramedics at the site of emergency. In these systems, the telemedical EP (TEP) supports EMS (Figure 1). This has proven to result in increased turn-around times by supporting triage in non-urgent calls (ETHAN Houston) and in giving adequate medical advice directly to paramedics (TNA Aachen).33,36,40
Figure 1.
Currently implemented telemedicine models in German EMS.
Challenges of telemedicine in EMS
This shows that telemedicine can be implemented and adapted to many international structures of emergency medicine, but still is not widely adapted and used. 41
This may have many reasons but typically large scale technological structures can present a high hurdle for implementation and the goal to reduce current cost has often not been met.31,38,42 –44
In Germany, the costs of such systems have been evaluated and have shown to be very high, particularly in the phase of implementation. However, in rural areas, they present an alternative to investing in new ambulances and EP-vehicle stations and further staff.39,45,46
Of course, there are further limitations such as clinical use, reimbursement, legal or social issues:
Clinically, evaluation of a patient from distance, can result in a varying quality of patient–physician relationship, inappropriate care or even fragmenting care by involving too many or multiple different providers.47–49
Reimbursement-wise, depending on national healthcare structure and its financing, there also seems to be a restriction of availability. While increasingly more private insurers have to cover telehealth costs by law, Medicare only provides care if areas are understaffed for healthcare professionals in the United States.50,51 But in countries with a single-payer health insurance (like Canada), or organizations that not only pay but also provide healthcare, seem to be large adopters of telemedicine.52,53
Legally there are many different aspects that range from state licensure and practice to credentialing and professional liability as well as protection of patient confidentiality.
All of these aspects are relevant and must be evaluated for the position of the healthcare professional, the healthcare facility, and a possible service facility.47,54
Even within a country, borders between federal states, can limit the use.
In the US state of Texas, telemedical services can only be provided if an in-person visit has previously been performed, 55 while in Germany only the state of North Rhine-Westphalia requires tele-emergency physicians to have passed a specialist course on Tele-emergency Medicine, which can only be attended once specific requirements have been fulfilled. 56
These regulation and credentialing steps can be seen to improve the quality of telemedical service, but also decrease the accessibility as a result of increasing requirements for providers.
Therefore, certain populations and providers could be excluded, which in regard for already underserved communities can result in a further lack of accessibility to healthcare structures.57,58 Especially the already existing lack of access to telecommunication technologies in older and rural populations can further increase the burden.29,59
We, therefore, want to promote a different model of Telemedicine in EMS: A low-cost concept.
By not only supporting and developing a consultation-based telemedical service for paramedics or emergency medical providers, but by actually connecting patients with physicians, we want to develop a system that allows real-time and live teleconsultation between patients and remote physicians. This way, patients can be connected directly with the physician that will provide treatment in the following process. At the same time, structurally independent working levels of care (depending on the level of urgency) can be integrated into a real-time telemedical communication network.
Simultaneously, already available and daily used technologies on ambulances, primary care clinics, or EDs will be used for this telemedical concept.
Methods
We first defined a timeline for development:
The timeline consisted of the following five points:
Research of holistic telemedical systems currently used in emergency medicine.
Definition of goals and quality requirements.
Conception of a holistic concept.
Testing and evaluation—from demonstration to realistic environments.
Evaluation of costs and potential benefits.
Research of holistic telemedical systems used in emergency medicine
Research was performed by an interdisciplinary group of emergency physicians, paramedics, medical informatics, and experts in data protection and safety at the Technische Hochschule Mittelhessen.
A literature review via MEDLINE, Cochrane Database, EMBASE, ENDPIECE, and Google Scholar for telemedical concepts and applications in EMS that were used in a holistic manner and multiple conditions of patients was performed. Requirements that these systems had to meet to be considered as “holistic” were to transfer patient’s vital data live and provide a live bi-directional (= synchronous) communication similarly to videoconferencing between an emergency physician and a paramedic. Excluded were systems that, were not implemented into routine daily use, only used one-directional communication, did not use live transfer of vital data or live videoconferencing or were only used for one type of condition or clinical specialty like “Stroke,” “Trauma,” “Heart failure,” or “Dermatology.” Excluded were articles that were not available in English or German or institutional access was not available.
The results were then categorized in the same group if they were applied in the same region or used the same technology.
The following search terms were used: “Telemedicine,” “Tele-Emergency Physician,” “Emergency Medical Services,” “EMS,” “Communication,” “low-cost,” “efficiency,” as well as the German terms “Telemedizin,” “Telenotarzt,” “Rettungsdienst,” “Notarzt,” “Kommunikation,” “Kosten,” and “Effektivität.”
1. Definition of goals and quality requirements.
After evaluation of the literature results, we defined quality requirements as a must for a holistic telemedical EMS concept. We also defined these as goals our concept must achieve.
2. Conception of a holistic concept.
A holistic telemedical system was assembled to be used for every common medical scenario in any preclinical setting and had to meet our quality requirements.
The parts were assembled and tested in a demonstration environment in which technical usability could be evaluated.
3. Testing and Evaluating from demonstration to realistic environments.
After testing technical usability in a demonstration environment, the system was tested in ambulances and local EDs.
An emergency medical scenario was defined in which this system was to be tested.
The scenario was a scripted myocardial infarction and was acted by a team of two paramedics, EPs from local EDs and medical professionals acting as a patient. Patient treatment was according to local German EMS algorithms and coherent with current medical standards. 60
Paramedics were supported telemedically by EPs during this scenario in which, according to local algorithms, an EP would have to be called by paramedics and then the EP would have to arrive telemedically on scene.
After receiving written consent by each of the participants, the scenarios were simulated and documented by picture and video to reproduce this approach and evaluate the use of technology.
The participants were directly asked to review this system and give advice to further improve this concept.
Evaluation of costs
Evaluation of costs was performed by summing up and comparing to the average reimbursement of an EP-staffed vehicle deployment in the region of Giessen.
Breakeven points per ambulance were calculated and compared to possible cost savings reported in earlier researched literature.
Breakeven was defined as the amount of calls for EP-staffed vehicles needed to be saved to equal the investment costs for such a telemedical concept per ambulance.
Results
Research of holistic telemedical systems used in emergency medicine
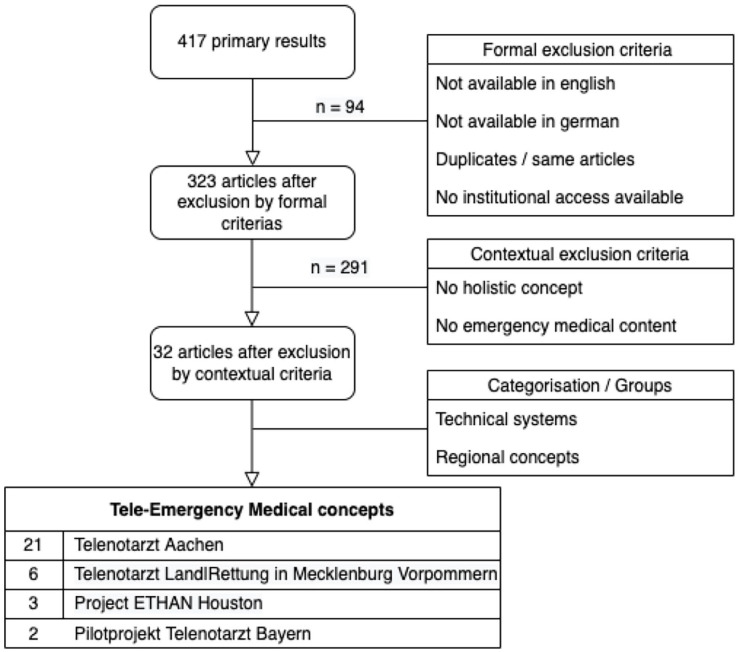
A total of 417 primary search results were screened. By using the earlier defined criteria, 94 articles were excluded for formal criteria, as well as 291 for contextual-related criteria. Therefore, 32 articles met the requirements and were categorized.
Holistic telemedical systems that were most widely implemented were Telenotarzt Aachen in Northrhine Westphalia, Germany (21 Publication), followed by Telenotarzt Land|Rettung in Mecklenburg-Western Pomerania, Germany (six Publications), ETHAN Houston in Texas, United States (three publications) and Pilotprojekt Telenotarzt Bayern in Bavaria, Germany (two Publications.)
Ethan provided evidence that turnaround times were improved and patients were transferred with a more cost-effective system, resulting in possible savings for the healthcare system.33,35,61
While TNA Aachen as well as Telenotarzt Land|Rettung showed that such a system improved staff efficiency, reduced EP contact times and could be implemented in a physician-based emergency medical system.36,40,62,63
Both systems showed that a telemedical system for EMS can be implemented no matter how local EMS Structures have historically been developed (physician based in Germany vs paramedic based in the United States) and can be used to facilitate and improve emergency medical care.
Both showed that a larger financial investment of US$1,500,000 (ETHAN Houston) or 1,049,466 € (Telenotarzt Model Aachen) is needed on a yearly basis. This is needed, as special technologies have to be bought to implement telemedical infrastructure such as fully equipped telemedical ambulances and new positions of TEPs at a control center have to be established and maintained.39,61
Cost efficiency was shown in the US Model as each year an annual benefit of US$928,000 could be calculated. 61 In Germany, this level of efficiency has not been reached yet, as regions that use this model are smaller in size and the number of averaged daily calls for EP are rather low at about 2.5 per day.37,46,64 But to increase efficiency, current efforts are being used to increase the range per telemedically supported control center. 65
Definition of goals and quality requirements
Therefore, we concluded that the following requirements and goals have to be met to develop a holistic telemedical system:
While patient safety and data security are the most important requirements, we concluded that a low-cost concept was needed and possible: costs for many technical components are low, many components are standardized and interconnectable, and technologies that are already being used in German ambulances like Toughbooks for mobile documentation or electrocardiograms (ECGs) can already transfer vital data or only need a software update or a technical modification/adapter to do so.
Also lowering costs compared to currently used systems, would increase usability and availability of telemedicine, while at the same time committing to the highest level of patient safety and data security according to General Data Protection Regulation (GDPR) and national healthcare regulations (Table 1).
Table 1.
Quality requirements and goals for a low-cost telemedical EMS concept.
| Quality requirement and goals |
|---|
| Patient safety (most important point) |
| Data security (second most important) |
| Low acquisition cost |
| Cost-efficiency |
| Standard components |
| Simple installation |
| Simple usability |
| Available web application |
| Worldwide usability |
EMS: Emergency Medical Services.
Conception of a holistic concept
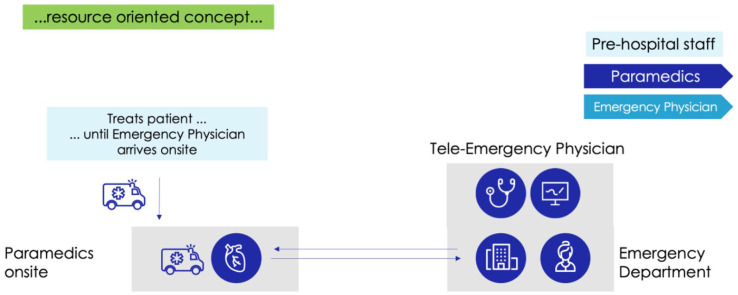
We defined these requirements and developed the following concept that also requires a TEP, but divided the physical role from the technical: instead of physically placing one EP at a regional control center, we placed the role of the TEP at local EDs and other providers of out-of-hospital or primary care.
By placing the role of the EP in local ED (or other structures in which non-urgent patients can be treated), patients can be connected early to EDs and EPs, while EMS can assist at the scene and, if needed, transfer the patients to the facility the consulted TEP is located at.
Patients could, therefore, be screened, triaged earlier and, if needed, monitored during transport. This early connection to the ED allows an earlier integration of each patient into the processes of the local emergency medical facility.
Especially in critically ill patients, who would be transferred anyhow to ED, the receiving physician would have the possibility to connect earlier with incoming paramedics and prepare the ED or order further examinations from the incoming ambulance. This would allow the patient-receiving EPs to support paramedics (teleconsultation), while at the same time talk and see the patient to develop a primary diagnosis, check severity (telediagnosis and triage), and monitor the patient (telemonitor).
While allowing the ED to prepare needed resources, inform other clinical facilities for the patient’s arrival, if needed. Equally, patients that do not need urgent care, can be screened early on scene and be referred and connected to primary care facilities.
By not only connecting the clinical sector like ED with EMS, but by also integrating primary care facilities and specialist offices into an emergency medical network and overriding structural borders created by legislature, patients could be transferred to the appropriate medical care facility and overuse of ED could, therefore, be prevented, while using technology to improve current processes and distribution of available resources. (see Figures 2 –4)
Figure 2.
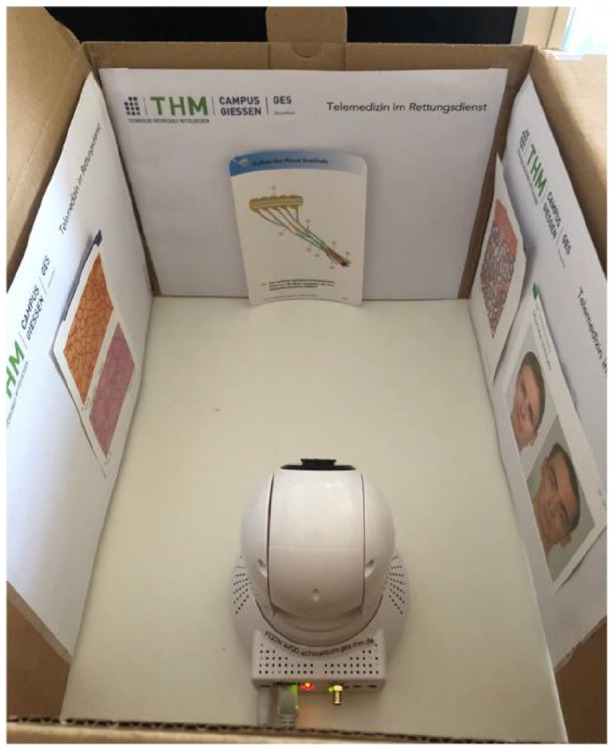
Demonstration environment for technical usability.
Figure 3.
Literature review and categorization of results.
Figure 4.
Resource-oriented concept for EMS in Giessen.
This approach integrates technology into already established and validated process structures of local emergency medicine, by transferring the patient’s essential information from the scene to the appropriate care facility. This would reduce the need to implement an additional out-of-hospital EP in a dispatch center and would strengthen local structures of medical care.
Therefore, extra cost-intensive positions that can only support and give advice in out-of-hospital care of patients could be saved, while a more patient- and process-focused concept of telemedicine could be implemented.
Technically our concept involves two systems:
A mobile and stationary system for communication and one system for the transfer of vital data.
Stationary communication system
Consists of five parts: Camera, microphone, loudspeaker, router including sim card, and an uninterruptible power source (UPS; compare Table 2).
Table 2.
Stationary communication system.
| Components | Model | Manufacturer |
|---|---|---|
| Camera | Lupus LE 200 WLAN | Lupus Electronics |
| Microphone | König CMP-MIC9 – Flexible mini Mikrofon 3.5 mm |
König |
| Loudspeaker | Leto Compact 2.0 Speaker Set Black | Leto |
| Router | Teltonika RUT 950 | Teltonika |
| Sim card | Standard Sim | Deutsche Telekom |
| Uninterruptible power supply (UPS) | APC Back UPS PRO USV 900VA BR900G-GR |
APC |
Mobile communication system
Consists of three parts: Durable tablet, sim card, video conference solution (compare Table 3).
Table 3.
Mobile communication system.
| Components | Model | Manufacturer |
|---|---|---|
| Tablet | FZ-G1 Toughbook | Panasonic |
| Sim card | Standard Sim | Deutsche Telekom |
| Videoconference solution | Cisco Jabber | Cisco |
Vital data system
Consists of three parts: ECG, telemedical ECG software, sim card (compare Table 4).
Table 4.
Vital data system.
| Components | Model | Manufacturer |
|---|---|---|
| ECG with telemetric capability | C3 with oxygen saturation, 12 lead ECG, blood pressure measurement, temperature, CO2 measurement, defibrillator |
Corpuls |
| Telemedical Software | Corpuls.web Live Application | Corpuls |
| Sim card | Standard Sim | Deutsche Telekom |
ECG: electrocardiography.
Tele-emergency physician work environment in the ED
Consists of five parts: personal computer, screens, webcam, headset, Internet browser (compare Table 5).
Table 5.
Tele-emergency physician work environment in the ED.
| Components | Model | Manufacturer |
|---|---|---|
| Personal computer | HP Prodesk | HP |
| Two screens | LA 1956 Screen 1: Communication (Cisco Jabber/Lupus Camera) Screen 2: Vital data (corpuls.web Live) |
HP |
| Webcam | Logitech C270 HD Webcam 720p | Logitech |
| Headset | Sennheiser PC8 USB | Sennheiser |
| Internet Browser | Standard Webbrowser (Internet Explorer,
Chrome) (for logging into vital data and communication system) |
Microsoft |
ED: emergency department.
Testing and evaluation—from demonstration to realistic environments
The technically assembled concept was first tested in a demonstration environment. From EDs, it could be reached via standard web browsers, so that camera functions could be used.
This system was then integrated to ambulances. The following simulations showed that an integration into local processes as well as treatment of patients was possible, while adherence to local EMS protocols and guidelines was maintained. Allowing EP from the ED to treat patients which they would later receive (Figure 5).
Figure 5.

TEP view on the patient during the scenario.
While reviewing the simulations with the participants, it was concluded that most of the treatment that was done by the TEP was performed at the scene of incident.
Monitoring of transport was also performed, but the process of transport would often require more of an observational, then interactive role of a TEP. It was concluded that this could allow a possibility of parallel observation and treatment of more than one patient by one TEP if necessary (Figure 6).
Figure 6.

Paramedics consulting with the TEP on the patient’s clinical status.
Also, the early engagement of an EP shortened unnecessary waiting periods at EDs, due to the fact that administrative processes and triage were carried out by paramedics on scene and confirmed by TEP. This allowed the processes of patient admission to EDs to be more streamlined and could simplify the management of patient flows.
Also, participants concluded that further standardized testing was required as this was a test of concept focused on feasibility of a novel technology constellation for EMS and EDs.
Evaluation of costs and potential benefits
Overall investment
The overall investment for such a solution was at 85.182.47 €, without discounts that counties, hospitals or other public service organizations are individually eligible for.
The primary costs would consist of maintaining servers for videoconferencing and the telemedical software solution. In our exemplary German model, this would be provided and serviced for by the local emergency medical government authorities and would cost 80.960.11 €, providing 50 licenses for participants and hospitals
A participating hospital would have to invest into the missing parts. In our model, we used available PCs in EDs and only had to provide a headset and webcam at a cost of 58,73 €.
EMS provider
The investment for the EMS provider calculates at 4.163,63 €, if a new durable tablet would be needed, like in our tested scenario.
Cost per ambulance
If the overall investment is calculated per ambulance, an investment of 3.197,58 € per ambulance has to be made. This includes the licenses per ambulance for vital data and videoconferencing, as well as costs for the stationary and mobile system, while using available Tablets and ECGs.
Cost of EP staffed vehicle
The average cost for deployment of an EP staffed vehicle is at 471,67 € in regions around Giessen.
Breakeven point
Comparing the investment costs per ambulance with the cost per deployment of an EP staffed vehicle, a breakeven point would be reached at 7.04 (5.52 including discounts) saved EP-vehicle deployments.
Discussion
According to a universal definition by WHO, technology in healthcare is supposed to support medical professionals, increase the efficiency of treatment and patient satisfaction. 66 By using a user-focused approach like ours to develop a telemedical concept by integrating local structures and defining a clear goal, technology could, therefore, be integrated in a resource-limited setting.
While every local emergency medical structure not only differs geographically, but also in regional and especially in local medical and structural processes, telemedical technologies need to consider these individual characteristics and be adaptable, to allow a sensible and adequate use for all involved.
Currently used systems require a yearly 6 to 7 figure investment (US$1.500.000 for “ETHAN Houston” or 1.049.466 € for “Telenotarzt Model Aachen”) for providing such a service and seem to be a very high obstacle that many healthcare infrastructures cannot overcome.39,61 Therefore, the step of not creating further high-cost structures, should be seen as a vital step to develop novel approaches and could also result in a wider use of telemedical solutions in emergency medicine.32,41 Especially underfunded and underdeveloped emergency medical systems might benefit from this.
By implementing low-cost concepts and later scaling these in size, more participants and facilities can take part and connect virtually in an emergency medical network. This could offer more specialized treatment options directly at the site of need, resulting in an interprofessional medical network, based on established structures.
Limitations
Generally, results from novel systems, need to provide further real-world and long-term evidence, as we can only provide a conceptual and prototype-like structure on how telemedicine could be implemented in a low-cost, local, and practical manner within a certain region.
As EMS systems also are very variable in design, function, and administration, this provides a more challenging surrounding for the adoption of telehealth in the prehospital settings and has, therefore, lagged far behind hospital settings.
Another limiting factor is the introduction in clinical routines of EDs. As physicians and nurses already have many different responsibilities, the role of a telemedical physician service needs to be designated. It could be discussed if this role could initially be performed by a triage nurse as a first-level contact and if necessary, a physician within the ED could then be consulted.
Further research could focus on such questions of integrating clinical with pre-clinical processes and, therefore, understand how these new “online” pathways connect and interact with “offline” clinical pathways. This could then define, which qualifications, trainings, and knowledge would be needed to introduce such a decentralized telemedical service.
Also local regulations, reimbursement models and differences in legislative structures can result and will need different approaches. By using a practical “goal-in-mind” approach by involving users and authorities in each step of the development process, these could be overcome.
Further research would need to evaluate cost and efficiencies of such concepts, as the calculations presented can only be understood as a prototypical evaluation, that would also need to evaluate running costs and long-term benefits.
In the field of developing community EMS networks, more research is needed as more patients could benefit from such intraoperative systems. Therefore, such systems would need to provide further evidence by reaching essential time marks and clinically relevant outcomes including safety and cost-efficiency in larger multicentered trials.42,43
Conclusion
In this practical approach, we showed that telemedicine in EMS can move a step further than just be an additional structure and extra-cost driver. It can be a more supportive and integrated process allowing real-time treatment of patients, while saving already limited resources, staff and funds, by adding technology to established processes.
By using a practical approach and involving everyday users in each step, concepts like these can, therefore, build on already available structural and technical resources and integrate these in the developmental process more easily. Therefore, hurdles for initial implementation and long-term use could possibly be lowered, especially in areas with less available funds for often pricy healthcare technologies.
Acknowledgments
The authors are grateful to the paramedics, emergency physicians, and experts in the field of Emergency Medicine including local administrators in the region of Giessen and their continuous support. We are also grateful for the contributions made by students, staff, and administration of the University of Applied Sciences THM Giessen
Footnotes
Author contribution(s): Seán F O’Sullivan: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Henning Schneider: Conceptualization; Formal analysis; Funding acquisition; Methodology; Project administration; Resources; Supervision; Writing – review & editing.
Availability of data and materials: The authors confirm they have permission to re-use all the data and costs included. Further data/materials to support the findings of this study are available from the corresponding author upon request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research did not receive specific funding, but was performed as part of the employment of the authors at the Technische Hochschule Mittelhessen Fachbereich Gesundheit.
Ethical approval: Need for an ethical approval was waived by the IRB Ethik-Kommission des Fachbereichs Medizin der Justus Liebig Universität Gießen, Germany—number AZ 111/18, as this is technological research about a digitalized medical process including its development, efficiencies, and limitations compared to other telemedical systems.
Consent for publication: Written informed consent for the publication of these images and details was obtained from the participants.
ORCID iD: Seán F O’Sullivan  https://orcid.org/0000-0002-3696-4632
https://orcid.org/0000-0002-3696-4632
References
- 1. Christ M, Dodt C, Geldner G, et al. Presence and future of emergency medicine in Germany. Anästhesiol Intensivmed Notfallmed Schmerzther 2010; 45(10): 666–671. [DOI] [PubMed] [Google Scholar]
- 2. Gries A, Bernhard M, Helm M, et al. Future of emergency medicine in Germany 2.0. Anaesthesist 2017; 66(5): 307–317. [DOI] [PubMed] [Google Scholar]
- 3. Sieber F, Kotulla R, Urban B, et al. Entwicklung der Frequenz und des Spektrums von Rettungsdiensteinsätzen in Deutschland. Notf Rett 2020; 23(7): 490–496. [Google Scholar]
- 4. Ärzteblatt DÄG Redaktion Deutsches. Notarzteinsätze steigen jährlich um fünf bis sieben Prozent. Deutsches Ärzteblatt, 29 June 2017, https://www.aerzteblatt.de/nachrichten/76670/Notarzteinsaetze-steigen-jaehrlich-um-fuenf-bis-sieben-Prozent (accessed 10 January 2021).
- 5. Stadt Frankfurt am Main—Der Magistrat, Amt 37 Branddirektion. Bereichsplan 2018, für den Rettungsdienstbereich Frankfurt am Main. Frankfurt: Amt 37 Branddirektion, 2018, https://frankfurt.de/-/media/frankfurtde/frankfurt-themen/gesundheit/psychische-gesundheit/pdf/bereichsplan-rettungsdienst-frankfurt-2018.ashx (accessed 12 September 2020). [Google Scholar]
- 6. Träger des Rettungsdienst des Main-Taunus Kreises. Bereichsplan MTK, 6. Fortschreibung, 2016 bis 2020, 1. Änderungsanpassung 2018. Report No. 6, 2018, Hofheim am Taunus: Amt für Brandschutz und Rettungswesen (Amt 38), https://www.mtk.org/statics/ds_doc/downloads/Bereichsplan_6_Fortschreibung_Aenderungsanpassung_.pdf (accessed 12 September 2020).
- 7. Ostwald DA, Ehrhard T, Bruntsch F, et al. Fachkräftemangel—Stationärer und ambulanter Bereich bis zum Jahr 2030. Darmstadt: WifOR Institut und PricewaterhouseCoopers AG, 2020, https://www.pwc.de/de/gesundheitswesen-und-pharma/assets/fachkraeftemangel.pdf (accessed 9 December 2020). [Google Scholar]
- 8. Schmiedel R, Behrendt H. Leistungen des Rettungsdienstes 2016/17—Analyse des Leistungsniveaus im Rettungsdienst für die Jahre 2016 und 2017 Bericht zum Forschungsprojekt FE 87.0014/2015 (Performance of the emergency services in 2016/17) (Berichte der Bundesanstalt für Straßenwesen, Reihe M: Mensch und Sicherheit). Bremen: Fachverlag NW in der Carl Ed. Schünemann KG, 2019, http://bast.opus.hbz.nrw.de/frontdoor/index/index/docId/2319#? (accessed 4 February 2021). [Google Scholar]
- 9. Stevanovic A, Beckers SK, Czaplik M, et al. Telemedical support for prehospital emergency medical service (TEMS trial): study protocol for a randomized controlled trial. Trials 2017; 18: 43, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5270339/ (accessed 16 February 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schmiedel R, Behrendt H. Leistungen des Rettungsdienstes 2008/09. Analyse des Leistungsniveaus im Rettungsdienst für die Jahre 2008 und 2009. Bonn: FORPLAN, Dr. Schmiedel GmbH, 2011, https://www.bast.de/BASt_2017/DE/Publikationen/Berichte/unterreihe-m/2011-2010/m217.html (accessed 9 December 2020). [Google Scholar]
- 11. Luiz T, van Lengen RH, Wickenkamp A, et al. [Operational availability of ground-based emergency medical services in Rheinland-Palatinate: state-wide web-based system for collation, display and analysis]. Anaesthesist 2011; 60(5): 421–426. [DOI] [PubMed] [Google Scholar]
- 12. Uppal N, Gondi S. Addressing the EMS workforce shortage: how medical students can help bridge the gap. J Emerg Manag 2019; 17(5): 380–384. [DOI] [PubMed] [Google Scholar]
- 13. Schmidt FM, Wildner M. Übersicht über die Organisation des vertragsärztlichen Bereitschaftsdienstes in Deutschland: Auf welche Basis bauen Krankenhausstrukturgesetz und Versorgungsstärkungsgesetz auf? Gesundheitswesen 2019; 81(07): e133–e140. [DOI] [PubMed] [Google Scholar]
- 14. Baker L, Birnbaum H, Geppert J, et al. The relationship between technology availability and health care spending: attempts to address technology availability and rising costs could end up badly misguided if implications for quality are not considered. Health Aff 2003; 22(Suppl. 1): W3-537–W3-551. [DOI] [PubMed] [Google Scholar]
- 15. Moore L. Measuring quality and effectiveness of prehospital ems. Prehosp Emerg Care 1999; 3(4): 325–331. [DOI] [PubMed] [Google Scholar]
- 16. Wissenschaftliche Dienste des Deutschen Bundestages. Organisation der Notfallversorgung in Deutschland unter besonderer Berücksichtigung des Rettungsdienstes und des Ärztlichen Bereitschaftsdienstes (WD 9: Gesundheit, Familie, Senioren, Frauen und Jugend). Report No. WD 9-3000 – 105/14, 2016. Berlin: Wissenschaftliche Dienste des Deutschen Bundestages, https://www.bundestag.de/resource/blob/408406/0e3ec79bfb78d7dde0c659a2be0927ca/wd-9%E2%80%93105%E2%80%9314–pdf-data.pdf (accessed 14 December 2020). [Google Scholar]
- 17. Sachverständigenrat. Bedarfsgerechte Steuerung der Gesundheitsversorgung—Gutachten 2018. Bonn and Berlin: Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen, 2018, https://www.svr-gesundheit.de/fileadmin/Gutachten/Gutachten_2018/Gutachten_2018.pdf (accessed 14 December 2020). [Google Scholar]
- 18. Schmidt FM, Wildner M. [Overview of the organization of the emergency medical service in Germany: what is the basis for the Hospital Restructuring Act and the Supply Enhancement Act?]. Gesundheitswesen 2019; 81(7): e133–e140. [DOI] [PubMed] [Google Scholar]
- 19. Krämer J, Schreyögg J. Substituting emergency services: primary care vs. hospital care. Health Policy 2019; 123(11): 1053–1060. [DOI] [PubMed] [Google Scholar]
- 20. Derlet RW, Richards JR, Kravitz RL. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 2001; 8(2): 151–155. [DOI] [PubMed] [Google Scholar]
- 21. Di Somma S, Paladino L, Vaughan L, et al. Overcrowding in emergency department: an international issue. Intern Emerg Med 2015; 10(2): 171–175. [DOI] [PubMed] [Google Scholar]
- 22. Bundesärzte Kammer. Indikationskatalog für den Notarzteinsatz. Dtsch Ärztebl 2013; 110(Heft 11): 481–483. [Google Scholar]
- 23. Vorstand BAND e.v. Stellungnahme der BAND zum Indikationskatalog für den Notarzteinsatz: Auf Anfrage des Wissenschaftlichen Beirats der Bundesärztekammer vom 10.04.2019. Notarzt 2019; 35(4): 193–193. [Google Scholar]
- 24. Schulz-Stubner S. Bring the doctor to the patient. . .the German “Notarzt” system. Anesth Analg 2003; 96(3): 912. [DOI] [PubMed] [Google Scholar]
- 25. Mohr M. Hochleistungsmedizin am Boden. Notf Rett 2007; 10(3): 167–170. [Google Scholar]
- 26. Roth K, Baier N, Henschke C, et al. Rechtliche Rahmenbedingungen in der präklinischen Notfallversorgung. Notf Rett 2017; 20(3): 237–250. [Google Scholar]
- 27. Eugene Gerden. EMS around the world: Germany brings the doctors to the action. EMS World, September 2020, https://www.emsworld.com/article/1224765/ems-around-world-germany-brings-doctors-action (accessed 10 January 2021).
- 28. Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health 2007; 13(5): 573–590. [DOI] [PubMed] [Google Scholar]
- 29. Wootton R, Geissbuhler A, Jethwani K, et al. Long-running telemedicine networks delivering humanitarian services: experience, performance and scientific output. Bull World Health Organ 2012; 90(5): 341D–347D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brennan JA, Kealy JA, Gerardi LH, et al. Telemedicine in the emergency department: a randomized controlled trial. J Telemed Telecare 1999; 5(1): 18–22. [DOI] [PubMed] [Google Scholar]
- 31. Winburn AS, Brixey JJ, Langabeer J, 2nd, et al. A systematic review of prehospital telehealth utilization. J Telemed Telecare 2018; 24(7): 473–481. [DOI] [PubMed] [Google Scholar]
- 32. Hicks LL, Boles KE, Hudson ST, et al. Using telemedicine to avoid transfer of rural emergency department patients. J Rural Health 2001; 17(3): 220–228. [DOI] [PubMed] [Google Scholar]
- 33. Langabeer JR, 2nd, Gonzalez M, Alqusairi D, et al. Telehealth-enabled emergency medical services program reduces ambulance transport to urban emergency departments. West J Emerg Med 2016; 17(6): 713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Clintonfoundation. ETHAN (Emergency Telehealth and Navigation). Clintonfoundation, https://www.clintonfoundation.org/sites/default/files/chmi_houston_ethan.pdf (2016, accessed 9 January 2021).
- 35. Staff J. Tele-EMS improves productivity and reduces overall costs. JEMS, 4 September 2019, https://www.jems.com/operations/tele-ems-improves-productivity-and-reduces-overall-costs/ (accessed 9 January 2021).
- 36. Bergrath S, Czaplik M, Rossaint R, et al. Implementation phase of a multicentre prehospital telemedicine system to support paramedics: feasibility and possible limitations. Scand J Trauma Resusc Emerg Med 2013; 21: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Koncz V, Kohlmann T, Bielmeier S, et al. Telenotarzt. Unfallchirurg 2019; 122(9): 683–689. [DOI] [PubMed] [Google Scholar]
- 38. Nolting H-D, Zich K. Telemedizinische Prozessinnovationen in den Regelbetrieb. 1. Auflage. Gütersloh: Bertelsmann Stiftung, 2017, https://www.bertelsmann-stiftung.de/fileadmin/files/BSt/Publikationen/GrauePublikationen/VV_Studie_Telemedizin_Lessons_Learned.pdf (accessed 1 June 2019). [Google Scholar]
- 39. Prasser C, Süss R, Hahnenkamp K, et al. Der Telenotarzt als Innovation des Rettungsdienstes im ländlichen Raum—Kosten der Implementierung. Gesundheitsökonomie Qual 2020; 25(3): 150–156, http://www.thieme-connect.de/DOI/DOI?10.1055/a-1080-6792 (accessed 1 May 2020). [Google Scholar]
- 40. Brokmann JC, Rossaint R, Bergrath S, et al. Potenzial und Wirksamkeit eines telemedizinischen Rettungsassistenzsystems. Anaesthesist 2015; 64(6): 438–445. [DOI] [PubMed] [Google Scholar]
- 41. American College of Emergency Physicians (ACEP) Telehealth Section. Review of telehealth literature whitepaper. Irving, TX: ACEP, 2018, https://www.acep.org/globalassets/sites/acep/blocks/section-blocks/telemd/final-whitepaper—sans-definition-8-7-19.pdf (accessed 15 February 2021). [Google Scholar]
- 42. Natafgi N, Shane DM, Ullrich F, et al. Using tele-emergency to avoid patient transfers in rural emergency departments: an assessment of costs and benefits. J Telemed Telecare 2018; 24(3): 193–201. [DOI] [PubMed] [Google Scholar]
- 43. Zachrison KS, Boggs KM, Hayden EM, et al. Understanding barriers to telemedicine implementation in rural emergency departments. Ann Emerg Med 2020; 75(3): 392–399. [DOI] [PubMed] [Google Scholar]
- 44. Rogers H, Madathil KC, Agnisarman S, et al. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed J E Health 2017; 23(9): 707–717. [DOI] [PubMed] [Google Scholar]
- 45. Innovationsausschuss beim Gemeinsamen Bundesausschuss. Beschluss des Innovationsausschusses beim Gemeinsamen Bundesausschuss gemäß § 92b Absatz 3 SGB V zum abgeschlossenen Projekt Telenotarzt Bayern (01NVF16013). Innovationsausschuss Gemeinsamer Bundesausschuss, 2020, https://innovationsfonds.g-ba.de/downloads/projekt-dokumente/35/2020-12-18_Telenotarzt-Bayern.pdf (accessed 1 January 2021).
- 46. Bielmeier GS, Groß S, Koncz V, et al. Anlage 1 Ausführlicher Evaluationsbericht gem. Vorlage Nr. 14.1 ANBest IF. Innovationsausschuss Gemeinsamer Bundesausschuss, 2020, https://innovationsfonds.g-ba.de/downloads/projekt-dokumente/29/2020-12-18_Telenotarzt-Bayern_Evaluationsbericht.pdf (accessed 30 December 2020).
- 47. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med 2016; 375(2): 154–161. [DOI] [PubMed] [Google Scholar]
- 48. Wachter R. The digital doctor: hope, hype, and harm at the dawn of medicine’s computer age. 1st ed. New York: McGraw Hill, 2017. [Google Scholar]
- 49. Uscher-Pines L, Mulcahy A, Cowling D, et al. Antibiotic prescribing for acute respiratory infections in direct-to-consumer telemedicine visits. JAMA Intern Med 2015; 175(7): 1234–1235. [DOI] [PubMed] [Google Scholar]
- 50. Thomas L, Capistrant G. State telemedicine gaps analysis coverage &; reimbursement, https://mtelehealth.com/state-telemedicine-gaps-analysis-coverage-reimbursement/ (2016, accessed 22 January 2022).
- 51. Greenstein S, McDevitt R. Evidence of a modest price decline in US broadband services. Inf Econ Policy 2011; 23(2): 200–211. [Google Scholar]
- 52. Brown EM. The Ontario telemedicine network: a case report. Telemed J E Health 2013; 19(5): 373–376. [DOI] [PubMed] [Google Scholar]
- 53. Asch DA. The hidden economics of telemedicine. Ann Intern Med 2015; 163(10): 801–802. [DOI] [PubMed] [Google Scholar]
- 54. Ferorelli D, Nardelli L, Spagnolo L, et al. Medical legal aspects of telemedicine in Italy: application fields, professional liability and focus on care services during the COVID-19 health emergency. J Prim Care Community Health 2020; 11: 2150132720985055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Goodnough A. Texas medical panel votes to limit telemedicine practices in state. The New York Times, 11 April 2015, https://www.nytimes.com/2015/04/11/us/texas-medical-panel-votes-to-limit-telemedicine-practices-in-state.html (accessed 22 January 2022).
- 56. Ärztekammer Nordrhein, Körperschaft des öffentlichen Rechts, Ärztekammer Westfalen-Lippe, Körperschaft des öffentlichen Rechts. Curriculum Qualifikation Telenotarzt der Ärztekammern Nordrhein und Westfalen-Lippe. 1. Auflage. Münster: Ärztekammern Nordrhein und Westfalen-Lippe, 2020, https://www.akademie-wl.de/fileadmin/akademie/dokumente_curricula_artikel/curriculum_qualifikation_telenotarzt_stand_13.08.2020.pdf (accessed 22 January 2022). [Google Scholar]
- 57. Chaet D, Clearfield R, Sabin JE, et al. Ethical practice in telehealth and telemedicine. J Gen Intern Med 2017; 32(10): 1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fox S, Purcell K. Chronic disease and the Internet. Pew Research Center: Internet, Science & Tech, 24 March 2010, https://www.pewresearch.org/internet/2010/03/24/chronic-disease-and-the-internet/ (accessed 22 January 2022).
- 59. Americans Internet access: percent of adults 2000-2015. Pew Research Center: Internet, Science & Tech, 26 June 2015, https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/ (accessed 22 January 2022).
- 60. UAG (ÄLRD) der AG 3 der hess. Expertengruppe zum NotSanG (HMSI). Algorithmen-Notfallversorgung-NotSan.pdf. Darmstadt, https://rettungsdienstschule-gelnhausen.de/algorithmus/Algorithmen-Notfallversorgung-NotSan.pdf (2018, accessed 19 December 2020). [Google Scholar]
- 61. Langabeer JR, 2nd, Champagne-Langabeer T, Alqusairi D, et al. Cost–benefit analysis of telehealth in pre-hospital care. J Telemed Telecare 2017; 23(8): 747–751. [DOI] [PubMed] [Google Scholar]
- 62. Felzen M, Brokmann JC, Beckers SK, et al. Improved technical performance of a multifunctional prehospital telemedicine system between the research phase and the routine use phase—an observational study. J Telemed Telecare 2017; 23(3): 402–409. [DOI] [PubMed] [Google Scholar]
- 63. Bergrath S, Rörtgen D, Rossaint R, et al. Technical and organisational feasibility of a multifunctional telemedicine system in an emergency medical service—an observational study. J Telemed Telecare 2011; 17(7): 371–377. [DOI] [PubMed] [Google Scholar]
- 64. Klaus Graf. Ergebnisbericht gemäß Nr. 14.1 ANBest-IF Projekttitel: Pilotprojekt zur telemedizinischen Unterstützung der Notfallversorgung im Rettungsdienst einer ländlich strukturierten Region. Innovationsausschuss Gemeinsamer Bundesausschuss, 2020, https://innovationsfonds.g-ba.de/downloads/projekt-dokumente/36/2020-12-18_Telenotarzt-Bayern_Ergebnisbericht.pdf (accessed 30 December 2020).
- 65. Ministerium für Arbeit, Gesundheit und Soziales NRW. Telenotarzt—System wird flächendeckend in Nordrhein—Westfalen etabliert—Das Landesportal Wir in NRW, 2020, https://www.land.nrw/pressemitteilung/telenotarzt-system-wird-flaechendeckend-nordrhein-westfalen-etabliert (accessed 19 December 2020).
- 66. World Health Organization. WHO—Global initiative on health technologies. Geneva: World Health Organization, https://apps.who.int/iris/bitstream/handle/10665/70522/WHO_HSS_EHT_DIM_10.12_eng.pdf?sequence=1&isAllowed=y (accessed 12 January 2021). [Google Scholar]