Abstract
Introduction:
Depression and anxiety among tuberculosis (TB) patients can adversely affect TB treatment adherence and completion.
Aim:
We studied whether integrating mental health services into existing TB treatment programs would reduce symptoms of depression and anxiety and improve treatment completion among patients with drug-susceptible TB.
Methods:
Integrated practice units (IPUs) for TB and mental health were established within six existing TB treatment facilities in Karachi, Pakistan. Patients were screened for depression and anxiety and, if symptomatic, offered a mental health intervention consisting of at least four counseling sessions. We measured changes in reported levels of depression and anxiety symptoms from baseline following completion of counseling sessions, and rates of TB treatment completion.
Results:
Between February 2017 and June 2018, 3500 TB patients were screened for depression and anxiety. 1057 (30.2%) symptomatic patients received a baseline adherence session. 1012 enrolled for a mental health intervention received at least 1 counseling session. 522 (51.5%) reported no symptoms after four to six sessions. Symptomatic patients who completed at least four counseling sessions had higher rates of TB treatment completion than those who did not (92.9% vs 75.1%; p < 0.0001).
Conclusion:
Mental health interventions integrated within TB programs can help reduce symptoms of depression and anxiety and improve TB treatment completion.
Keywords: Mental health intervention, task-shifting, drug-susceptible tuberculosis, depression, anxiety
Introduction
Tuberculosis (TB) continues to be a leading cause of morbidity and mortality in the world, 1 with the highest number of deaths from infectious diseases attributable to TB. 2 The World Health Organization (WHO) estimates approximately 10 million new TB cases in 2018, of which, only 70% initiated treatment. 2 Literature suggests that TB patients may be vulnerable to developing mental health disorders such as depression and anxiety,3,4 and that there may be a high level of comorbidity.5,6 Studies conducted in Pakistan, Ethiopia, and Nigeria have placed prevalence estimates for comorbid TB and depression/anxiety between 46% and 54%.7–9
Depression in TB patients comes with substantial risks, such as non-compliance, prolonged treatment, and an increased risk of developing drug resistance, all of which contribute to poorer health outcomes.10,11 In an Ethiopian study, TB patients with untreated probable depression had significantly higher treatment default and death rates and lower treatment success rates compared to those without probable depression. 12 Left untreated, depression may lead to increased negative treatment outcomes, decreased quality of life,13,14 greater disability, treatment default and mortality. 12
Poor medication adherence is also frequently found in cases where physical illnesses and mental disorders are present.12,15 This is a major concern as non-adherence to TB treatment can lead to an increased risk of treatment failure, drug resistance, continued transmission of disease, prolonged treatment, and mortality.10–12,15 A longitudinal study in Peru suggests that patients with major depressive episodes at baseline had 3.5 times the risk of defaulting from treatment or death compared to those without such episodes. 15
Studies suggest that psychological interventions for treatment compliance can lead to better management of depression and assist with TB management, 16 and reduce lost to follow-up. 17 Furthermore, early detection of mental health disorders is necessary for treatment adherence, 18 minimizing stigma, 19 and preventing relapse. 7
The burden of TB disease tends to be concentrated in low resource settings.2,20 Pakistan (population of approximately 207.8 million 21 ) is currently ranked as the fifth highest TB burden country with an estimated incidence of 265 cases per 100,000 population. 2 WHO 22 estimates for Pakistan suggest a 4.2% prevalence of depression (resulting in 7.1% of years lived with disability) and a 3.5% prevalence of anxiety (3.1% of years lived with disability). Studies in Pakistan have found the prevalence of depression and anxiety in TB patients to range between 37% and 53%.23–25
Based on the existing evidence regarding the impact of mental health on TB treatment outcomes and the high prevalence of comorbidity in Pakistan, we aimed to integrate mental health services within existing TB treatment programs. The primary objective of this study was to evaluate whether integration of a mental health intervention in TB treatment sites improved symptoms of depression and anxiety and treatment completion rates among drug-susceptible tuberculosis (DS-TB) patients.
Methods
Between February 2017 and June 2018, we conducted a prospective interventional study with patients seeking care for DS-TB across six public and private hospital settings in Karachi, Pakistan.
Study setting
Study sites in Karachi included one private tertiary care hospital, three public sector tertiary care hospitals, and two private sector diagnostic and treatment centers. Standard TB treatment is free across all three facility types. The public sector hospitals and private diagnostic centers charge nominal fees for some tests and consultations while the private tertiary care hospital is completely free.
Study design and data collection
Integrated practice units (IPUs) offering mental health services were set up within existing TB treatment facilities; the IPUs were designed to embed mental health screening and counseling services into the existing treatment flow at each facility. The IPU used a task-shifting approach to service delivery, utilizing lay health counselors for the provision of mental health services. Counselors completed a 6 to 8-day in-person training on basic counseling skills delivered by a clinical psychologist. The training was divided between lectures and practical components such as role-playing exercises. Training content covered the basics of TB and mental health disorders, basic cognitive behavioral therapeutic techniques, core communication skills, and ethical considerations required for counseling.
The study was open to all patients seeking care for DS-TB at the study sites. Consecutive patients initiating DS-TB treatment at the study sites were given a baseline TB treatment adherence and supportive counseling session, consisting of information about TB, TB treatment side effects, the importance of treatment adherence, addressing the stigma associated with TB, and the link between TB and mental health. Mental health screening was offered using the Aga Khan University Anxiety and Depression Scale (AKUADS); a 25-item indigenously developed, Urdu language screening tool measuring depression and anxiety, and validated with the local population. The discriminatory properties of the scale are as follows: sensitivity is 66%, specificity is 79%, positive predictive value is 83%, and negative predictive value is 60%.26,27 The AKUADS defines a score of <21 as normal, while scores of 21–40, 41–60, and 61–75 are mild, moderate, and severe depression/anxiety, respectively. Exclusion criteria for mental health screening included not speaking Urdu, being too unwell at the time of screening, having hearing or speech impairments, and not planning on re-visiting the facility.
Patients scoring ⩾21 were considered symptomatic for depression/anxiety and offered a mental health intervention consisting of four to six mental health counseling sessions, or more based on necessity. Sessions were aligned with TB treatment appointments, which typically occurred monthly for the duration of TB treatment (approximately 6–8 months). Counseling sessions aimed to identify problems causing patients mental distress (i.e. the stigma they were facing from family or friends) and to work with the patient to formulate solutions and coping strategies to help alleviate or better manage distress (i.e. equipping them with the knowledge required to combat stigma, and teaching them how to have a positive dialogue regarding their problems and feelings with their friends and family).
Patients were reassessed using the AKUADS at the fourth counseling session. Patients who were still symptomatic on the scale were offered additional counseling sessions and reassessed on the AKUADS again at subsequent sessions. We considered individuals as having received a complete mental health intervention if they completed at least four counseling sessions and had a score of <21 on the AKUADS on their last assessment, and a partial mental health intervention if they received less than four counseling sessions.
Data were collected from medical records at all study sites, including demographic characteristics (age, gender, education level, and type of facility), AKUADS score at baseline and final reassessment, and TB treatment outcomes. The major outcomes of interest were the AKUADS score after intervention completion and a successful TB treatment outcome. A successful TB treatment combined the two standard outcomes of cured (the patient’s culture or smear test returned negative post-treatment) and treatment completion (the patient has completed treatment without evidence of failure, but there is no record of a sputum smear or culture results post-treatment). 28
Statistical analyses
Demographic characteristics were compared between individuals who were symptomatic and asymptomatic for depression/anxiety at baseline using chi-square tests for categorical variables and t-tests for continuous variables, and across facility types using chi-square tests for categorical variables and analysis of variance (ANOVA) tests for continuous variables.
Differences in AKUADS scores pre- and post-mental health intervention were assessed using the Wilcoxon signed-rank test. Analysis was restricted to patients who completed the intervention and had AKUADS rescreening scores available.
The proportion of patients experiencing a successful TB treatment outcome was compared across those who did and did not receive the mental health intervention and, among those who did receive the intervention, those who received less than four versus four or more counseling sessions, using chi-square tests. Among symptomatic individuals, we also assessed whether there was a statistically significant increase in the percent of individuals who completed treatment as more counseling sessions were completed using the Cochran–Armitage test for trend p < 0.0001. We restricted this analysis only to those who had a TB treatment outcome available. Individuals who were symptomatic but had refused the mental health intervention were also excluded from the analysis. Non-parametric tests, specifically the Wilcoxon rank sum test, were used where the data were not normally distributed. Statistical analysis was conducted using the SAS V9.4. 29
Results
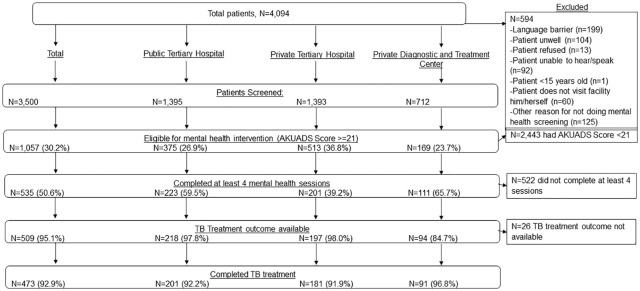
Between February 2017 and June 2018, 4094 consecutive patients initiated DS-TB treatment at the chosen study sites. 594 (14.5%) patients did not undergo mental health screening at baseline for several reasons, including a language barrier (199, 33.5%), being too ill to undergo screening (104, 17.5%), and having a hearing or speech impairment (93, 15%). Figure 1 outlines complete reasons for not undergoing screening and the flow of patients through the study.
Figure 1.
Description of patient flow, enrollment, and completion.
The remaining 3500 (85.5%) were screened for depression and anxiety using the AKUADS. Among the screened, 1057 (30.2%) were symptomatic and offered the intervention. 45 (4.3%) patients refused the intervention after the baseline counseling session while 1012 (95.7%) were given the intervention, of which 535 (50.6%) completed it. TB treatment outcomes were available for 978 (96.6%) patients who were symptomatic at baseline.
Of the patients screened, 1797 (51.4%) were men and 1703 (48.6%) were women, with a mean age of 34.8 years (standard deviation (SD) = 15.7 years). The cohort symptomatic for depression/anxiety was significantly younger with a mean age of 33.1 (p-value < 0.001), consisted of more women (p-value < 0.001), and sought care more frequently in the private tertiary care hospitals, which provided free services (p-value < 0.001). Table 1 presents additional patient characteristics.
Table 1.
Description of patient characteristics, by being symptomatic (AKUADS score ⩾21) or not (AKUADS score <21) and type of health facility.
| Characteristic | Total screened (n = 3500) | Symptomatic (n = 1057) | Not symptomatic (n = 2443) | p-value | Public tertiary care hospital (n = 1395) | Private tertiary care hospital (n = 1393) | Private diagnostic and treatment centers (n = 712) | p-value |
|---|---|---|---|---|---|---|---|---|
| Age, mean (SD) (n = 3499) | 34.8 (15.7) | 33.1 (14.3) | 35.5 (16.2) | <0.0001 a | 33.5 (15.3) | 33.8 (15.3) | 39.2 (16.6) | <0.0001 b |
| Male sex, n (%) (n = 3499) | 1797 (51.4) | 416 (39.4) | 1381 (56.5) | <0.0001 | 675 (48.4) | 759 (54.5) | 363 (51.1) | 0.0055 |
| Education level, n (%) (n = 3478) | 0.1893 | <0.0001 | ||||||
| Primary education | 923 (26.5) | 251 (23.9) | 672 (27.7) | 305 (22.1) | 396 (28.5) | 222 (31.3) | ||
| High school education | 1311 (37.7) | 403 (38.3) | 908 (37.4) | 539 (39.1) | 508 (36.6) | 264 (37.2) | ||
| More than high school education | 107 (3.1) | 33 (3.1) | 74 (3.1) | 46 (3.3) | 44 (3.2) | 17 (2.4) | ||
| Religious education | 140 (4.0) | 44 (4.2) | 96 (4.0) | 37 (2.7) | 68 (4.9) | 35 (4.9) | ||
| No formal education | 997 (28.7) | 321 (30.5) | 676 (27.9) | 453 (32.8) | 373 (26.9) | 171 (24.1) | ||
| Public tertiary care hospital, n (%) | 1395 (39.9) | 375 (35.5) | 1020 (41.8) | <0.0001 | ||||
| Private tertiary care hospital, n (%) | 1393 (39.8) | 513 (48.5) | 880 (36.0) | |||||
| Private diagnostic and treatment centers, n (%) | 712 (20.3) | 169 (16.0) | 543 (22.2) | |||||
AKUADS: Aga Khan University Anxiety and Depression Scale.
Individuals who were symptomatic, as indicated at baseline by an AKUADS score ⩾21, were offered the mental health intervention.
Chi-square tests used unless otherwise noted.
t-test.
ANOVA.
The median score and interquartile range (IQR) for individuals screened at baseline were 26 (IQR = 23–31) and the scores at the end of the intervention were reduced to 10 (IQR = 7–14). We observe a statistically significant reduction in the AKUADS score for patients receiving the mental health intervention across all three treatment facility types (p-value < 0.0001), with an average decrease of 16 points in score (see Table 2).
Table 2.
AKUADS pre- and post-measurements for all individuals who had a score available at or after visit four, broken down by type of facility.
| Site | Median pre-intervention measurement (AKUADS) | Median post-intervention measurement (AKUADS) | p-value |
|---|---|---|---|
| Total population (n = 522) | 26 (23–31) | 10 (7–14) | <0.0001 |
| Public tertiary care hospitals (n = 211) | 27 (24–33) | 11 (7–19) | <0.0001 |
| Private tertiary care hospital (n = 201) | 26 (23–30) | 9 (6–11) | <0.0001 |
| Private diagnostics and treatment centers (N = 110) | 27 (24–30) | 11 (7–14) | <0.0001 |
AKUADS: Aga Khan University Anxiety and Depression Scale.
All values reported are median (interquartile range (IQR)). All p-values are calculated using the Wilcoxon signed-rank test.
Differences in successful TB treatment outcomes were assessed for patients with available outcomes (n = 3377). Symptomatic TB patients who received the intervention were able to achieve similar successful treatment outcome rates as individuals who were non-symptomatic at baseline (p = 0.2198). Of those who received the mental health intervention, 75.1% completed less than four sessions while 92.9% received four or more sessions with successful TB treatment outcomes (p < 0.0001). This trend persisted across each type of treatment facility (see Table 3).
Table 3.
TB treatment completion among individuals with treatment outcomes available, broken down by mental health intervention participation and facility type.
| Intervention | Patients with TB treatment outcomes available a | Patients who completed TB treatment b | p-value |
|---|---|---|---|
| Total (n = 3455) | |||
| Did not receive intervention, N = 2443 | 2399 (98.2) | 2063 (86.0) | 0.2198 |
| Received intervention N = 1012 | 978 (96.6) | 825 (84.4) | |
| <4 sessions, N = 477 | 469 (98.3) | 352 (75.1) | <0.0001 |
| ⩾4 sessions, N = 535 | 509 (95.1) | 473 (92.9) | |
| Public tertiary care hospitals (n = 1381) | |||
| Did not receive intervention, N = 1020 | 1004 (98.4) | 861 (85.8) | 0.3240 |
| Received intervention, N = 361 | 354 (98.1) | 311 (87.9) | |
| <4 sessions, N = 138 | 136 (98.6) | 110 (80.9) | 0.0015 |
| ⩾4 sessions, N = 223 | 218 (97.8) | 201 (92.2) | |
| Private tertiary care hospitals (n = 1366) | |||
| Did not receive intervention, N = 880 | 870 (98.9) | 711 (81.7) | 0.5924 |
| Received intervention, N = 486 | 478 (98.4) | 384 (80.3) | |
| <4 sessions, N = 285 | 281 (98.6) | 203 (72.2) | <0.0001 |
| ⩾4 sessions, N = 201 | 197 (98.0) | 181 (91.9) | |
| Private diagnostic and treatment centers (n = 708) | |||
| Did not receive intervention, N = 543 | 525 (96.7) | 491 (93.5) | 0.0798 |
| Received intervention, N = 165 | 146 (88.5) | 130 (89.0) | |
| <4 sessions, N = 54 | 52 (96.3) | 39 (75.0) | <0.0001 |
| ⩾4 sessions, N = 111 | 94 (84.7) | 91 (96.8) | |
TB: tuberculosis.
Denominator to calculate percentage is the total number of individuals in each group, per column 1.
Denominator to calculate percentage is the total number of individuals with treatment outcomes available, per column 2.
All p-values are calculated using chi-square tests.
Difference in percentage of individuals completing TB treatment per counseling session completed was assessed for 978 symptomatic individuals with available TB treatment outcomes. The trend indicates that there was a significant increase in treatment completion with each subsequent session (p < 0.001). Table 4 presents additional details.
Table 4.
Difference in TB treatment completion by number of counseling sessions attended among symptomatic individuals with treatment outcomes available.
| Number of counseling sessions | Patients with available TB treatment outcomes (n = 978) | Patients who completed TB treatment (n = 825) | Patients who completed TB treatment (%) |
|---|---|---|---|
| 1 | 229 | 168 | 73.4% |
| 2 | 153 | 115 | 75.2% |
| 3 | 87 | 69 | 79.3% |
| 4 | 413 | 383 | 92.7% |
| 5 | 52 | 48 | 92.3% |
| 6–9 a | 44 | 42 | 95.5% |
TB: tuberculosis.
Cochran–Armitage test for trend to assess whether there was a statistically significant increase in the percent of individuals who completed treatment as more sessions were completed, p < 0.0001.
Sessions 6–9 have been grouped together as only four individuals received >6 sessions.
Discussion
Individuals symptomatic for depression and/or anxiety who completed a mental health intervention (four or more sessions) had a higher rate of successful TB treatment outcomes compared to those who did not complete the mental health intervention. This finding was significant across all three facility types indicating that integrating mental health interventions into TB treatment sites can be an effective way to increase adherence and successful treatment outcomes among individuals with depression and/or anxiety across different service provider settings.
These findings support other studies that have found mental health interventions helpful in ensuring TB treatment adherence. A systematic review 30 reported that psycho-emotional support interventions can positively impact TB treatment outcomes. In addition, a pilot intervention in Nepal 19 found that patients in the two intervention groups (counseling and counseling with financial support) had a higher rate of positive treatment outcomes compared to those in the control group (no support). Moreover, a cluster randomized controlled trial conducted in Ethiopia found that individuals who received psychological counseling with TB adherence education had significantly better medication adherence in comparison to those who only received the directly observed therapy intervention. 18
We also observed a trend of increased treatment compliance among symptomatic individuals with each subsequent counseling session, with the greatest increase in completion occurring at session number four. Moreover, we found symptomatic individuals who received the mental health intervention were able to complete TB treatment at a similar rate to non-symptomatic individuals. Symptomatic individuals tend to be at a greater risk of not completing treatment; 31 thus, similar treatment completion rates between the two, combined with the findings of the trend analysis, suggest that receiving a complete or partial mental health intervention could lead to improvement in treatment outcomes among patients with reported depression and anxiety. However, it is important to note that this cannot be measured directly, as due to ethical reasons the study had no control group of symptomatic individuals who were not offered the intervention.
The results of this study also add to the evidence base for the effectiveness of mental health service provision using the lay health model. Research shows that contextually sensitive psychological treatment regimens delivered by appropriately trained lay health counselors tend to be effective in terms of reducing overall disability. 32 Mental health interventions based on lay health worker models tend to warrant a significant reduction in depression rates when rescreened at end-line. 32 A randomized control trial 33 in a lower-middle class community in Karachi, Pakistan, found out that eight counseling sessions provided by lay health workers can significantly reduce levels of anxiety and depression. These findings support our conclusion, whereby individuals exposed to the mental health intervention had significantly reduced depression and/or anxiety compared to baseline.
Limitations
This study has several programmatic limitations. In the absence of a control group of symptomatic patients against whom another group of symptomatic patients receiving the mental health intervention could be compared, the impact of the intervention remains unobserved. We chose to forgo the control group because there is considerable evidence regarding the benefits of providing mental health services to patients with physical illnesses, and we decided it would be unethical to not provide it when needed. However, other studies support the argument that patients without mental health support are less likely to adhere to the TB treatment which decreases the possibility that, without the control group, our findings are not significant.
As the study was open to all DS-TB patients seeking care at our study facilities, we did not have a predetermined sample size. Given the large number of study participants, the chance that our findings are not representative is greatly reduced.
This study excluded individuals who were not fluent in Urdu and those with hearing and speech impairments as providing the intervention to these groups would have required additional resources in terms of translated tools and competency over regional and sign language. Individuals with hearing and speech impairments could potentially be more vulnerable to developing depression and may require additional mental health support.
Furthermore, our findings cannot be generalized to multidrug-resistant tuberculosis (MDR-TB) and hospitalized patients. The treatment course of these patients is longer and disease severity is frequently greater than in patients with DS-TB. It is possible that this intervention would not be as effective or that these patients may need additional support.
This study also does not have a qualitative component and thus does not document patient-level insight regarding their experiences with mental distress and how the intervention may have helped them cope and better adhere to treatment. Resource and time constraints limited us from incorporating such a component and this can be the focus of future studies.
Conclusion
Controlling TB is a public health priority and the effectiveness of TB programs is contingent on treatment adherence. This study suggests that integrating mental health screening and counseling services into existing TB facilities improves symptoms of depression and anxiety, and increases treatment completion rates. Our findings contribute to the growing body of evidence of the effectiveness of using lay health counselors for mental health service provision in existing programs, strengthening the case for these types of approaches to be adopted to help bridge the treatment gap for mental health.
Acknowledgments
The authors acknowledge Saira Khowaja for her support in securing permissions for implementation at the chosen sites and Sana Sajun for her technical input during the conceptualization of this study.
Footnotes
Author contributions: A.P. contributed to the conceptualized the study, developed the model and guidelines, and oversaw the implementation of the study. H.S. managed the study implementation, data collection and compilation, and the compilation of the manuscript. S.A. assisted with the implementation, data collection and compilation, as well as with the compilation of the manuscript. M.B.B. conducted the data analysis. N.R.M. contributed to the writing of the manuscript. A.J.K. provided strategic guidance and supervision to the study. All authors worked on the manuscript and approved submission of the manuscript for publishing. Authorship was determined using the ICMJE guidelines. All authors also reviewed the manuscript critically and approved the final content.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Harvard Medical School Center for Global Health Delivery—Dubai (grant no. 027562-746846-0207).
Disclaimer: The views expressed in the submitted article are our own and not an official position of the institution or funder.
Ethical approval: Permission to conduct the study and develop the IPUs was granted by the Institutional Review Boards at Harvard University (IRB16-1334) and Interactive Research and Development (IRD_IRB_2016_05_002). Verbal consent for screening and providing counseling was obtained by the lay health counselor and documented on the mental health application, as not all participants could read and write. Data were de-identified prior to analysis and nobody outside the team had access to these data.
ORCID iD: Aneeta Pasha  https://orcid.org/0000-0002-2699-4301
https://orcid.org/0000-0002-2699-4301
References
- 1. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388(10053): 1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Global tuberculosis report (WHO/CDS/TB/2019.15). Geneva: World Health Organization, 2019. [Google Scholar]
- 3. Avong YK, Isaakidis P, Hinderaker SG, et al. Doing no harm? Adverse events in a nation-wide cohort of patients with multidrug-resistant tuberculosis in Nigeria. PLoS ONE 2015; 10(3): e0120161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu S, Zhang Y, Sun F, et al. Adverse events associated with the treatment of multidrug-resistant tuberculosis: a systematic review and meta-analysis. Am J Ther 2016; 23(2): e521–e530. [DOI] [PubMed] [Google Scholar]
- 5. Sweetland AC, Kritski A, Oquendo MA, et al. Addressing the tuberculosis–depression syndemic to end the tuberculosis epidemic. Int J Tuberc Lung Dis 2017; 21(8): 852–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walker IF, Baral SC, Wei X, et al. Multidrug-resistant tuberculosis treatment programmes insufficiently consider comorbid mental disorders. Int J Tuberc Lung Dis 2017; 21(6): 603–609. [DOI] [PubMed] [Google Scholar]
- 7. Ahmed MM, Mazhar M, Zaidi A. Depression in tuberculosis patients and its relationship to socio demographic factors. J Rawalpindi Med Coll 2016; 20(4): 296–299. [Google Scholar]
- 8. Ambaw F, Mayston R, Hanlon C, et al. Burden and presentation of depression among newly diagnosed individuals with TB in primary care settings in Ethiopia. BMC Psychiatry 2017; 17(1): 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ige OM, Lasebikan VO. Prevalence of depression in tuberculosis patients in comparison with non-tuberculosis family contacts visiting the DOTS clinic in a Nigerian tertiary care hospital and its correlation with disease pattern. Ment Health Fam Med 2011; 8(4): 235–241. [PMC free article] [PubMed] [Google Scholar]
- 10. Peddireddy V. Quality of life, psychological interventions and treatment outcome in tuberculosis patients: the Indian scenario. Front Psychol 2016; 7: 1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sulheri MA, Dogar IA, Sohail H, et al. Prevalence of depression among tuberculosis patients. Ann Punjab Med Coll 2010; 4(2): 133–137. [Google Scholar]
- 12. Ambaw F, Mayston R, Hanlon C, et al. Untreated depression and tuberculosis treatment outcomes, quality of life and disability, Ethiopia. Bull World Health Organ 2018; 96(4): 243–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bauer M, Leavens A, Schwartzman K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual Life Res 2013; 22(8): 2213–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Singh SK, Agrawal A, Tiwari KK. Improvement in quality of life in pulmonary tuberculosis patients: a prospective study. Trop Doct 2017; 47(2): 97–100. [DOI] [PubMed] [Google Scholar]
- 15. Ugarte-Gil C, Ruiz P, Zamudio C, et al. Association of major depressive episode with negative outcomes of tuberculosis treatment. PLoS ONE 2013; 8(7): e69514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pachi A, Bratis D, Moussas G, et al. Psychiatric morbidity and other factors affecting treatment adherence in pulmonary tuberculosis patients. Tuberc Res Treat 2013; 2013: 489865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liefooghe R, Suetens C, Meulemans H, et al. A randomised trial of the impact of counselling on treatment adherence of tuberculosis patients in Sialkot, Pakistan. Int J Tuberc Lung Dis 1999; 3(12): 1073–1080. [PubMed] [Google Scholar]
- 18. Tola HH, Shojaeizadeh D, Tol A, et al. Psychological and educational intervention to improve tuberculosis treatment adherence in Ethiopia based on health belief model: a cluster randomized control trial. PLoS ONE 2016; 11(5): e0155147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baral SC, Aryal Y, Bhattrai R, et al. The importance of providing counselling and financial support to patients receiving treatment for multi-drug resistant TB: mixed method qualitative and pilot intervention studies. BMC Public Health 2014; 14(1): 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Horton KC, MacPherson P, Houben RM, et al. Sex differences in tuberculosis burden and notifications in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med 2016; 13(9): e1002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pakistan Bureau of Statistics. Provisional summary results of 6th population and housing census-2017, https://www.pbs.gov.pk/content/provisional-summary-results-6th-population-and-housing-census-2017-0 (accessed 12 December 2019).
- 22. World Health Organization. Depression and other common mental health disorders: global health estimates (WHO/MSD/MER/2017.2). Geneva: World Health Organization, 2017. [Google Scholar]
- 23. Rubeen R, Zareen N, Zameer S, et al. Anxiety and depression in tuberculosis can create impact on quality of life of patient. Acta Med Int 2014; 1(2): 93–98. [Google Scholar]
- 24. Walker IF, Khan AM, Khan AM, et al. Depression among multidrug-resistant tuberculosis patients in Punjab, Pakistan: a large cross-sectional study. Int J Tuberc Lung Dis 2018; 22(7): 773–778. [DOI] [PubMed] [Google Scholar]
- 25. Tariq A, Arshad S, Ejaz M. Frequency of depression in tuberculosis patients and its association with various sociodemographic factors. Pak J Med Health Sci 2018; 12(1): 42–45. [Google Scholar]
- 26. Ali BS, Reza H, Khan MM, et al. Development of an indigenous screening instrument in Pakistan: the Aga Khan University Anxiety and Depression Scale. J Pak Med Assoc 1998; 48(9): 261–265. [PubMed] [Google Scholar]
- 27. Ahmer S, Faruqui RA, Aijaz A. Psychiatric rating scales in Urdu: a systematic review. BMC Psychiatry 2007; 7: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. World Health Organization. Definitions and reporting framework for tuberculosis (WHO/HTM/TB/2013.2). Geneva: World Health Organization, 2013. [Google Scholar]
- 29. Statistical Analysis System (SAS). Statistical Analysis System (Version 9.4). Cary, NC: SAS Institute. [Google Scholar]
- 30. van Hoorn R, Jaramillo E, Collins D, et al. The effects of psycho-emotional and socio-economic support for tuberculosis patients on treatment adherence and treatment outcomes: a systematic review and meta-analysis. PLoS ONE 2016; 11(4): e0154095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Theron G, Peter J, Zijenah L, et al. Psychological distress and its relationship with non-adherence to TB treatment: a multicentre study. BMC Infect Dis 2015; 15(1): 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Patel V, Weobong B, Weiss HA, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet 2017; 389(10065): 176–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ali BS, Rahbar MH, Naeem S, et al. The effectiveness of counselling on anxiety and depression by minimally trained counselors: a randomized controlled trial. Am J Psychother 2003; 57(3): 324–336. [DOI] [PubMed] [Google Scholar]