Abstract
Background
Perinatal risk factors can vary by immigration status. We examined psychosocial and behavioral perinatal health indicators according to immigration status and immigrant characteristics.
Methods
We conducted a population-based cross-sectional study of 33,754 immigrant and 172,342 non-immigrant childbearing women residents in Manitoba, Canada, aged 15–55 years, who had a live birth and available data from the universal newborn screen completed within 2 weeks postpartum, between January 2000 and December 2017. Immigration characteristics were from the Canadian federal government immigration database. Logistic regressions models were used to obtain Odds Ratios (OR) with 95% confidence intervals (CI) for the associations between immigration characteristics and perinatal health indicators, such as social isolation, relationship distress, partner violence, depression, alcohol, smoking, substance use, and late initiation of prenatal care.
Results
More immigrant women reported being socially isolated (12.3%) than non-immigrants (3.0%) (Adjusted Odds Ratio (aOR): 6.95, 95% CI: 6.57 to 7.36) but exhibited lower odds of depression, relationship distress, partner violence, smoking, alcohol, substance use, and late initiation of prenatal care. In analyses restricted to immigrants, recent immigrants (< 5 years) had higher odds of being socially isolated (aOR: 9.04, 95% CI: 7.48 to 10.94) and late initiation of prenatal care (aOR: 1.50, 95% CI: 1.07 to 2.12) compared to long-term immigrants (10 years or more) but lower odds of relationship distress, depression, alcohol, smoking and substance use. Refugee status was positively associated with relationship distress, depression, and late initiation of prenatal care. Secondary immigrants, whose last country of permanent residence differed from their country of birth, had lower odds of social isolation, relationship distress, and smoking than primary migrants. There were also differences by maternal region of birth.
Conclusion
Immigrant childbearing women had a higher prevalence of social isolation but a lower prevalence of other psychosocial and behavioral perinatal health indicators than non-immigrants. Health care providers may consider the observed heterogeneity in risk to tailor care approaches for immigrant subgroups at higher risk, such as refugees, recent immigrants, and those from certain world regions.
Keywords: Maternity, Perinatal, Postpartum, Immigrant, Canada, Depression, Social isolation, Violence, Health behaviors, Prenatal care
Introduction
Maternal, child, and perinatal outcomes may differ by immigration status [1, 2]. The healthy immigrant effect describes the phenomenon by which immigrants exhibit better health outcomes than the receiving-country population. The phenonmenon, which occurs shortly after arrival [3–5], presumably due to selective migration, has been referred to as an explanation for the favorable outcomes of immigrants. On the other hand, immigrants also exhibit substantial heterogeneity across multiple dimensions of vulnerability [6], and the healthy migrant hypothesis may not apply to specific subgroups, such as refugees [7]. Moreover, mixed results in the literature comparing immigrants and non-immigrants also depend on methodological characteristics, such as different study designs, data sources, population diversity and composition, comparison groups, sample sizes, and differences in variable definitions [8–11].
Disparities in perinatal outcomes may also be due to differences in risk factors between immigrants and non-immigrants. The migration process can be considered a psychosocial stressor [12] that can intersect with immigrant womens’ socioeconomic marginalization and vulnerability in the new country [13]. Pregnancy and the perinatal period are sensitive to environmental influences that can trigger and exacerbate complex health risks associated with perinatal psychosocial changes and adjustments [14]. For instance, poor relationship quality or marital stress related to post-migration and acculturation stress [15] may be risk markers for partner violence [16, 17]. The experience of partner violence or abuse can trigger or worsen depression [10, 18, 19] and increase maternal stress levels, which can strongly influence adopting unhealthy coping behaviors, such as smoking and/or alcohol consumption [20, 21]. Unhealthy behaviors have been reportedly associated with social isolation [22] and delayed prenatal care utilization [22, 23].
Among immigrants, variation in perinatal outcomes and risk factors may be driven by immigrant characteristics [2]. Unlike primary immigrants, who immigrate directly from their country of birth, secondary immigrants (also referred to as two-step or serial migrants) reside in at least one intermediate country before immigrating to their final destination [24, 25]. Secondary (voluntary) immigrants are a highly selected subgroup of immigrants characterized by higher educational credentials and global upward socioeconomic mobility, which are conducive to better health outcomes [26]. However, the secondary migration advantage may not apply to refugees who spent long periods of time in refugee camps in intermediate countries [7]. Several studies have documented the erosion of immigrants’ initial health advantage with increasing duration of residence [4, 27, 28], although some health outcomes such as depression may improve with time since migration [29, 30].
Reports examining multiple psychosocial and behavioral perinatal health indicators among immigrant groups are scarce and limited to non-population-based studies with small sample sizes [1, 31, 32]. A qualitative study examined health behaviors (smoking and alcohol use), social support, and stress during pregnancy among seventeen Southeast Asian immigrant women in Montreal, Canada [33]. Aside from a few population-based studies with reported findings by the duration of residence [34] and nativity [35], there is a lack of studies assessing psychosocial and behavioral perinatal health outcomes among immigrant subgroups defined according to refugee status, secondary migration and maternal birth region.
To advance knowledge on the psychosocial and behavioral perinatal health indicators among childbearing immigrant women, we used population-based provincially funded screening data collected in the home by public health nurses, typically within 2 weeks postpartum, linked to Canadian federal government immigration records. All new permanent residents to Canada, including economic and refugee applicants and their dependents are eligible for the free-of-charge publicly-funded universal health care coverage, which includes physician and hospital services that is provincially administered. Some temporary residents (work permit visas) are also eligible for the provincial health care coverage. A small proportion of refugee claimants (also known as asylum seekers) are not covered by the Manitoba Health Care Insurance Plan but by a federally-funded program (i.e., the Interim Federal Health Program) while awaiting resolution of their case. Our objective was to compare select psychosocial and behavioral perinatal health indicators between immigrants to Manitoba, Canada and non-immigrants overall and according to key immigrant characteristics, such as refugee status, secondary migration, maternal birth region, and duration of residence.
Methods
Study design, settings, and participants
The population-based cross-sectional study was conducted among childbearing women in Manitoba, Canada. We included immigrant and non-immigrant women aged 15–55 years, who had a live birth between January 1, 2000, to December 31, 2017, and had Baby First or Family First Screening data, a universal newborn screen completed within 2 weeks postpartum.
Data sources
Multiple de-identified linkable administrative databases were accessed at the Manitoba Population Research Data Repository that contains multi-sectoral information of all Manitoba residents. Upon registration to the Manitoba Health Insurance Plan, the publicly-funded health care coverage for all residents, all individuals are registered in the Manitoba Health Insurance Registry (MHIR) and assigned a Personal Health Identification Number (PHIN) that is used by health care providers for billing purposes. The MHIR contains personal and sociodemographic information. All health and social services databases are linked to the MHIR at the Ministry of Health. After linkage, the databases are de-identified by stripping personal identifiers such as names and addresses and replacing the PHIN by a scrambled unique identifier (SCRPHIN) that allows tracking of individuals across datasets. These de-identified datasets are then made available for research at the Repository [36]. The primary data sources were the Baby First (2000–2002) and Family First (2003–2017) screening data (BFS/FFS). The BFS/FFS screenings were designed to collect data on biological, social, and demographic risk factors of childbearing women in Manitoba [37]. Using the screening form, visiting public health nurses attempt to assess all families with newborns at home within a week of discharge from the hospital. This universal newborn screen provides valuable information for determining appropriate resources and services for the family and population-level surveillance. Information on immigration characteristics was obtained from the Immigration, Refugees, and Citizenship Canada Permanent Resident (IRCC-PR) database, which provides information on the immigration characteristics of all immigrants who obtained permanent residence in Canada from January 1985 to December 2017. The linkage rate of the IRCC-PR and the MIHR was 96% [38]. Additional linked databases were the Discharge Abstract Database from the Canadian Institute for Health Information (for hospital births), the Midwifery Summary System (for home births), and the Social Allowances Management Information Network (SAMIN) database that was used to determine receipt of Employment and Income Assistance (EIA). Small area Census data was used to assign neighborhood income quintiles and rural residence.
Cohort formation
Birth records from the Discharge Abstract Database and the Midwifery Summary System from January 1, 2000, to December 31, 2017, were used to create a cohort (n = 269,543) of eligible mothers. Cohort included all maternity records, irrespective of the number of offspring or delivery events to a mother over the study period. We reduced multiple records (n = 3369) in the case of twins, triplets, or more to one record per maternity and retained n = 266,174. We also excluded maternity records not linkable to the BFS/FFS dataset 59,219 (22.2%). These were stillbirths or births resulting in neonatal death and births in which the mother did not participate in the screening due to not being contacted or refused. We further excluded births to mothers aged < 15 years or > 55 years (n = 293), those with unknown neighborhood income quintile (n = 541), and unknown urban/rural residence (n = 151) (Fig. 1).
Fig. 1.
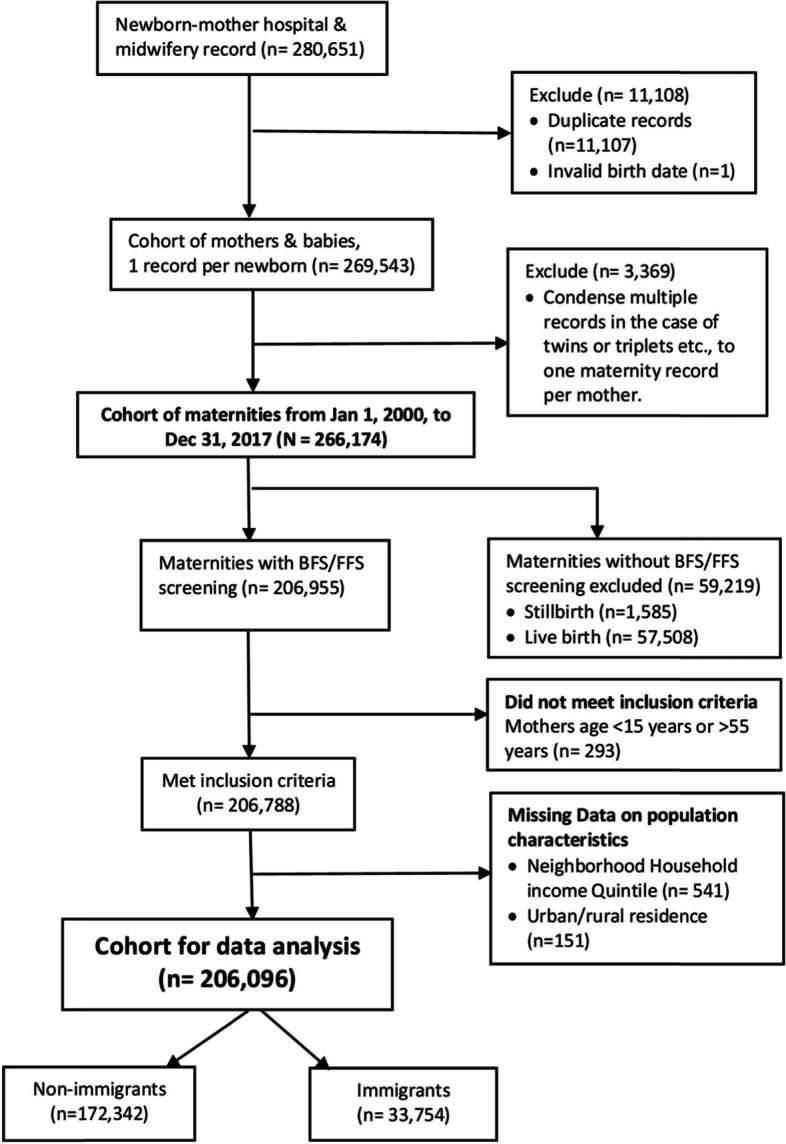
Flow chart cohort selection
Dependent variables
Psychosocial and behavioral Outcomes were nurse-recorded information collected during the BFS/FFS. Outcomes examined are maternal depression, defined as self-reported depression, during pregnancy up until the postpartum interview (yes, no); social isolation, defined as lack of social support or isolation related to culture, language, or geography (yes, no); relationship distress, defined as self-reported distress or conflict between parenting partners (e.g., separations, frequent arguments) (yes, no); partner violence, defined as self-reported current or history of violence between parenting partners (yes, no); alcohol use during pregnancy, defined as self-reported consumption of alcoholic beverages during pregnancy (yes, no); smoking during pregnancy, defined as self-reported smoking during pregnancy (yes, no); substance use during pregnancy, defined as self-reported illicit drug or substance use during pregnancy (yes, no); and late initiation of prenatal care, defined as prenatal care (PNC) that begins after the first trimester of pregnancy (more than 13 weeks gestation) (yes, no). Due to varying number of missing values in the dependent variables, the sample size varied by outcome.
Explanatory variables
International immigrants were identified by having a record in the IRCC-PR database. Women not in the IRCC-PR database and not having a record in the registry indicating that they came from another country were classified as Non-immigrant (Canadian-born). Since the IRCC-PR database began in 1985, a very small portion of immigrants who obtained permanent residence before 1985, when immigration was less common, may have been misclassified as non-immigrants.
Secondary immigrants were defined as immigrants to Canada whose last country of permanent residence differed from their country of birth. Those whose countries of birth and last permanent residency were the same were classified as primary immigrants.
Refugees were protected persons in Canada or dependants abroad of a protected person in Canada. They include all refugee categories (i.e., Syrian, Government-Assisted Refugees, Privately Sponsored Refugees, and Blended Visa Office-Referred refugees).
Birth region was based on the country where the woman was born. Countries were grouped into world regions of birth based on the United Nations classification [39] and regrouped where sample sizes are small as Southeast Asia, South & Rest of Asia, Western Europe, Eastern Europe, Rest of Europe, West Africa, East Africa, Rest of Africa, North America & Oceania, Latin America & the Caribbean.
Duration of residence was estimated as the length of time from the date of obtaining permanent residence in Canada to the birth of the child and grouped into < 5 years, 5–9 years, and ≥ 10 years. Some immigrants may have held temporary resident status and had birth events before obtaining permanent residence.
Covariates
Measured covariates included sociodemographic variables such as mothers’ age (in years) at the birth of the index child (below 20, 20–24, 25–29, 30–34, 35–39, 40–55), low education defined as reported mothers low education or completed <12th grade (yes, no) and lone mother (yes, no) from the BFS/FFS data, urban/rural residence, neighborhood income quintile (Q1- lowest, Q2, Q3, Q4, Q5- highest) from Census data, and receipt of EIA 1 year before birth to 2 weeks after (yes, no) from the SAMIN data. Family factor variables were family size, i.e., the number of dependents < 18 years in the same family as index child (none, at least one) from the MHIR. In analyses restricted to immigrants, knowledge of official Canadian languages (English/French, none) was obtaimed from the IRCC-PR database.
Statistical analysis
There were missing values in the dependent variables. Individuals with missing values in the dependent variables were excluded based on the assumption that missingness would not strongly bias comparisons between immigrants and non-immigrants [40]. Hence, the final sample size varied for each outcome. There was no percentage thresholds for missing exclusions. Instead, we compared the propotion of missings between immigrants and non-immigrants using standardized differences, with values < 0.1 indicating significant differences. For selected covariates with missing values, we created a dummy value ‘unknown’ to reduce sample size loss [41].
Participants’ characteristics were described using frequencies, percentages, means, and standard deviations. Logistic regression was used to estimate unadjusted (OR) and adjusted odds ratios (aORs) with 95% confidence intervals (CI) for the associations between immigration status and the dependent variables. Because in the BFS/FFS dataset 52% of the maternities were to women who had more than one maternity in the study period, their outcomes are correlated and may affect the associations because of their repeated measurements in the dataset, which violates the assumption of independence of observations [42]. Generalized Estimating Equations (GEE) were therefore used to account for the clustering of maternities within women [43].
In the analyses restricted to immigrants, we used internal comparison subgroups. Primary immigrants were used as the reference group to assess associations by secondary migration, based on studies that found higher rates of psychological distress among secondary immigrants [44]. Similarly, non-refugees were the reference group for analysis that examined associations by refugee status based on higher rates of psychosocial risk factors among women of refugee background [45]. Western Europeans were the reference group for associations by birth region based on their low rates of adverse birth outcomes among European-born women [2, 46], and for being more ethnically alike to the mainstream Canadian-born population. Given that the association of duration of residence and adverse birth outcomes produced mixed results [28], we used 10 or more years of residence as the reference group because of the documented convergence of health status of immigrants with that of the non-immigrant population. Cell counts of less than six were deemed unreportable and suppressed following Manitoba privacy regulations. All analyses were conducted using SAS V9.4 (SAS Institute Inc., Cary, NC).
Results
Table 1 describes the population characteristics of 172,342 non-immigrant and 33,754 international immigrant cohorts. Immigrant women were slightly older, their average age in the early thirties, and only about 4% were lone mothers compared to 12% among non-immigrants. About 79.3% had higher education or had completed more than high school education, and the majority (78.6%) lived in an urban area. Immigrants were overrepresented (29.9%) in the lowest neighborhood income quintile, but only 4% received employment and income assistance, compared to 16% among non-immigrants. Excluding the index child, 61% of families had one or more other dependent(s) less than 18 years. Most immigrant participants originated from Asia, while for other regions, the proportion ranged from 3.3% for West Africa to 8.6% for Eastern Europe.
Table 1.
Characteristics of the maternities with BFS/FFS records in Manitoba, Canada, 2000–2017 (n = 206,096)
| Non-immigrant 172,342 (83.62%) |
International immigrant 33,754 (16.38%) |
|
|---|---|---|
| Sociodemographic characteristics | ||
| Mother’s age at birth of index child – mean (SD)a | 28.20 (5.61) | 30.48 (5.33) |
| Mother’s age at birth of index child – Category | ||
| Below 20 years | 11,437 (6.64) | 537 (1.59) |
| 20–24 years | 34,745 (20.16) | 4145 (12.28) |
| 25–29 years | 53,935 (31.30) | 9786 (28.99) |
| 30–34 years | 48,852 (28.35) | 11,489 (34.04) |
| 35–39 years | 19,958 (11.58) | 6243 (18.50) |
| 40–55 years | 3415 (1.98) | 1554 (4.60) |
| Lone mother | ||
| Yes | 20,116 (11.67) | 1280 (3.79) |
| No | 145,045 (84.16) | 31,854 (94.37) |
| Unknown | 7181 (4.17) | 620 (1.84) |
| Low educationb | ||
| Yes | 31,974 (18.55) | 3362 (9.96) |
| No | 118,781 (68.92) | 26,766 (79.30) |
| Unknown | 21,587 (12.53) | 3626 (10.74) |
| Neighborhood Income Quintile | ||
| Q1 (lowest) | 35,783 (20.76) | 10,089 (29.89) |
| Q2 | 35,820 (20.78) | 6887 (20.40) |
| Q3 | 34,772 (20.18) | 6453 (19.11) |
| Q4 | 3598 (20.08) | 5822 (17.25) |
| Q5 (Highest) | 31,369 (18.20) | 4503 (13.34) |
| Urban/ Rural residence | ||
| Rural | 72,881 (42.29) | 7224 (21.40) |
| Urban | 99,461 (57.71) | 26,530 (78.60) |
| Received Employment & Income Assistance one year before birth to 2 weeks after | ||
| Yes | 27,104 (15.73) | 1402 (4.15) |
| No | 145,238 (84.27) | 32,352 (95.85) |
| Family factor characteristics | ||
| Family size (Number of dependents < 18 years in the same family as index child) | ||
| None | 73,876 (42.87) | 13,080 (38.75) |
| At least one | 98,466 (57.13) | 20,674 (61.25) |
| Immigrant characteristics | ||
| International Immigrant | ||
| Primary | – | 27,362 (81.11) |
| Secondary | – | 6374 (18.89) |
| Refugee | ||
| Yes | – | 4123 (12.22) |
| No | – | 29,613 (87.78) |
| Knowledge of official Canadian languages (English or French) | ||
| Yes | – | 22,074 (65.43) |
| No | – | 11,662 (34.57) |
| Duration of residence | ||
| < 5 years | – | 18,497 (54.83) |
| 5-9 years | – | 8782 (26.03) |
| 10 above years | – | 6457 (19.14) |
| Maternal Birth Region | ||
| Southeast Asia | – | 9622 (28.51) |
| South Asia & Rest of Asia | – | 10,303 (30.52) |
| Eastern Europe | 2907 (8.61) | |
| Western Europe | – | 1356 (4.02) |
| Rest of Europe | – | 1293 (3.83) |
| East Africa | – | 1958 (5.80) |
| West Africa | – | 1097 (3.25) |
| Rest of Africa | – | 1422 (4.21) |
| North America & Oceania | – | 1207 (3.58) |
| Latin America & Caribbean | – | 2589 (7.67) |
Frequencies expressed as n (%) unless otherwise specified
aSD Standard Deviation
bLow education = reported mothers’ low education or completed <12th grade
Table 2 presents the different outcome prevalences and the unadjusted and adjusted odds ratios comparing international immigrants to non-immigrants. Missing data in the dependent variables ranged from 4.6% for smoking during pregnancy to 32.4% for partner violence. Only social isolation was more prevalent among immigrants, and the association became stronger after adjustment. Conversely, immigrants had a lower prevalence of the other indicators before and after adjusting for sociodemographic and family factors.
Table 2.
Prevalence and odds ratio estimates of perinatal health indicators between immigrant and non-immigrant childbearing women in Manitoba, Canada
| International Immigrants | Non-immigrants | International immigrants versus Non-immigrants |
||||
|---|---|---|---|---|---|---|
| N | n (%) | N | n (%) | OR (95% CI)a | aOR (95% CI)b | |
| Psychosocial indicators | ||||||
| Depression, Mood & Anxiety Disorder (n = 181,189)c | 29,256 | 1522 (5.20) | 151,933 | 28,022 (18.44) | 0.24 (0.23, 0.26) | 0.26 (0.25, 0.29) |
| Social isolation (n = 161,666)c | 29,428 | 3605 (12.25) | 132,238 | 4013 (3.03) | 4.46 (4.24, 4.69) | 6.95 (6.57, 7.36) |
| Relationship distress (n = 182,438)c | 29,971 | 642 (2.14) | 152,467 | 9155 (6.00) | 0.34 (0.31, 0.37) | 0.72 (0.66, 0.78) |
| Partner violence (n = 139,234)c | 24,686 | 126 (0.51) | 114,548 | 2716 (2.37) | 0.21 (0.18, 0.25) | 0.51 (0.42, 0.62) |
| Behavioral indicators | ||||||
| Alcohol use during pregnancy (n = 164,723)c | 29,983 | 868 (2.89) | 134,740 | 19,069 (14.15) | 0.18 (0.17, 0.19) | 0.23 (0.21, 0.25) |
| Smoking during pregnancy (n = 196,623)c | 32,547 | 584 (1.79) | 164,076 | 32,123 (19.58) | 0.08 (0.07, 0.08) | 0.11 (0.10, 0.12) |
| Substance use during pregnancy (n = 163,898)c | 29,867 | 66 (0.22) | 134,031 | 6377 (4.76) | 0.04 (0.03, 0.06) | 0.09 (0.07, 0.11) |
| Late initiation of prenatal care > 13 weeks (n = 194,202)c | 32,261 | 301 (0.93) | 161,941 | 3544 (2.19) | 0.42 (0.37, 0.48) | 0.84 (0.74, 0.95) |
Frequencies expressed as n (%)
aOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models
baOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models, adjusted for Maternal age, lone mother, low education, neighborhood income quintile, urban residence, family size, and employment & income assistance
Bold values = Significant association (p < 0.05)
cTotal excludes missing values for outcomes where (n=)
Frequencies missing for outcomes: (Depression, mood & anxiety disorder n = 24,907; social isolation n = 44,430; Relationship distress n = 23,658; Partner violence n = 66,862; Alcohol use during pregnancy n = 41,373; Smoking during pregnancy n = 9473; Substance use during pregnancy n = 42,198; Late initiation of prenatal care > 13 weeks n = 11,894)
Tables 3 and 4 present odds ratio estimates restricted to international immigrant childbearing women. Secondary compared to primary immigrants had a higher prevalence of social isolation, but this association reversed after adjustment (Table 3). Being a secondary immigrant was also negatively associated with relationship distress. Refugees were more likely to experience relationship distress, depression, mood, and anxiety disorder than non-refugees. The high likelihood of social isolation became marginally significant, while partner violence became non-significant in the adjusted analysis. Compared to Western Europe, women from all birth regions were more likely to experience social isolation, except women from North America and Oceania, who had a lower prevalence, although not statistically significant. Only women from West Africa had a high likelihood of relationship distress in both unadjusted and adjusted analyses. Women from African regions were more likely to experience partner violence. The association was attenuated and non-significant in the adjusted analysis but remained high among women from West Africa. Those from North & South Europe, North America & Oceania, Latin America & the Caribbean were more likely to have depression, mood & anxiety disorder. Recent immigrants had nine times the odds of being socially isolated than those with ten or more years of residence but lower odds of relationship distress and depression than long-term immigrants.
Table 3.
Unadjusted and adjusted odds ratio estimates of psychosocial perinatal health indicators among immigrant childbearing women in Manitoba, Canada
| International immigrants n = 33,754 |
Social isolation (n = 29,428)c |
Relationship distress (n = 29,971)c |
Partner violence (n = 24,686)c |
Depression, mood & anxiety disorder (n = 29,256)c |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | |
| Immigrants | ||||||||
| Primary | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Secondary | 1.25 (1.13, 1.37) | 0.76 (0.68, 0.85) | 0.68 (0.54, 0.86) | 0.73 (0.55, 0.97) | 0.87 (0.55, 1.36) | 0.84 (0.50, 1.43) | 0.85 (0.73, 1.00) | 0.98 (0.82, 1.18) |
| Refugees | ||||||||
| Non-refugee | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Refugee | 1.46 (1.32, 1.62) | 1.17 (0.99, 1.38) | 3.70 (3.09, 4.42) | 1.39 (1.02, 1.90) | 3.54 (2.37, 5.28) | 1.02 (0.52, 1.98) | 1.70 (1.46, 1.98) | 1.37 (1.11, 1.70) |
| Maternal birth region | ||||||||
| Western Europe | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Southeast Asia | 2.10 (1.50, 2.95) | 1.76 (1.21, 2.56) | 1.31 (0.79, 2.19) | 1.21 (0.68, 2.16) | 1.48 (0.52, 4.20) | 1.04 (0.35, 3.03) | 0.71 (0.51, 0.98) | 0.71 (0.49, 1.04) |
| South & Rest of Asia | 4.02 (2.88, 5.61) | 3.03 (2.10, 4.36) | 0.83 (0.49, 1.40) | 1.28 (0.73, 2.26) | 1.07 (0.37, 3.08) | 1.12 (0.38, 3.30) | 0.76 (0.55, 1.06) | 0.93 (0.65, 1.34) |
| Eastern Europe | 3.39 (2.38, 4.84) | 2.95 (2.01, 4.33) | 0.68 (0.36, 1.28) | 0.99 (0.50, 1.95) | 1.36 (0.41, 4.49) | 1.54 (0.44, 5.34) | 0.99 (0.69, 1.45) | 1.08 (0.72, 1.61) |
| Rest of Europe | 1.60 (1.06, 2.42) | 2.01 (1.30, 3.10) | 1.11 (0.57, 2.13) | 1.06 (0.53, 2.10) | 1.02 (0.23, 4.57) | 0.85 (0.18, 4.07) | 2.39 (1.65, 3.44) | 2.06 (1.39, 3.07) |
| East Africa | 4.37 (3.07, 6.23) | 2.45 (1.62, 3.69) | 2.67 (1.54, 4.61) | 1.12 (0.57, 2.21) | 3.18 (1.05, 9.58) | 0.86 (0.22, 3.34) | 0.77 (0.51, 1.17) | 0.62 (0.38, 1.00) |
| West Africa | 3.63 (2.50, 5.27) | 2.59 (1.71, 3.92) | 3.43 (1.93, 6.08) | 2.03 (1.02, 4.02) | 4.77 (1.50, 15.16) | 1.92 (0.54, 6.90) | 0.78 (0.48, 1.27) | 0.76 (0.45, 1.30) |
| Rest of Africa | 6.03 (4.21, 8.63) | 3.59 (2.40, 5.38) | 3.60 (2.08, 6.23) | 1.51 (0.77, 2.96) | 3.38 (1.05, 10.91) | 0.75 (0.20, 2.91) | 1.33 (0.90, 1.95) | 1.10 (0.70, 1.73) |
| North America & Oceania | 0.81 (0.50, 1.34) | 0.65 (0.38, 1.09) | 0.76 (0.37, 1.58) | 0.82 (0.38, 1.77) | 1.38 (0.34, 5.52) | 1.25 (0.32, 4.85) | 3.35 (2.32, 4.82) | 3.46 (2.33, 5.14) |
| Latin America & Caribbean | 4.03 (2.84, 5.74) | 3.21 (2.20, 4.69) | 2.57 (1.51, 4.39) | 1.48 (0.83, 2.64) | 1.44 (0.44, 4.70) | 0.63 (0.19, 2.14) | 2.43 (1.73, 3.42) | 2.14 (1.47, 3.11) |
| Duration of residence | ||||||||
| < 5 years | 7.90 (6.61, 9.45) | 9.04 (7.48, 10.94) | 0.53 (0.44, 0.65) | 0.68 (0.53, 0.87) | 0.84 (0.52, 1.36) | 1.22 (0.71, 2.10) | 0.39 (0.34, 0.45) | 0.46 (0.39, 0.53) |
| 5–9 years | 2.42 (1.99, 2.95) | 2.64 (2.15, 3.24) | 0.74 (0.59, 0.91) | 0.84 (0.66, 1.08) | 1.12 (0.67, 1.86) | 1.32 (0.75, 2.32) | 0.58 (0.50, 0.67) | 0.65 (0.56, 0.75) |
| 10 years and more | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
aOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models
baOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models, adjusted for Maternal age, lone mother, low education, neighborhood income quintile, urban residence, family size, employment & income assistance, and knowledge of official Canadian languages
Bold values = Significant association (p < 0.05)
cTotal excludes missing values for outcomes where (n=)
Frequencies missing for outcomes: (Social isolation n = 4326; Relationship distress n = 3783; Partner violence n = 9068; Depression, mood & anxiety disorder n = 4498)
Table 4.
Unadjusted and adjusted odds ratio estimates for behavioral perinatal health indicators among immigrant childbearing women in Manitoba, Canada
| International immigrants n = 33,754 |
Maternal alcohol use during pregnancy (n = 29,983)c |
Maternal smoking during pregnancy (n = 32,547)c |
Maternal substance use during pregnancy (n = 29,867)c |
Late initiation of Prenatal care (n = 32,261)c |
||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | OR (95% CI)a | aOR (95% CI)b | |
| Immigrants | ||||||||
| Primary | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Secondary | 0.77 (0.64, 0.94) | 0.94 (0.75, 1.17) | 0.70 (0.53, 0.93) | 0.71 (0.52, 0.97) | 0.64 (0.31, 1.30) | 0.81 (0.37, 1.78) | 1.63 (1.25, 2.13) | 1.32 (0.97, 1.78) |
| Refugees | ||||||||
| Non-refugee | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
| Refugee | 1.18 (0.96, 1.46) | 0.95 (0.72, 1.25) | 1.98 (1.54, 2.53) | 1.20 (0.85, 1.71) | 2.60 (1.43, 4.76) | 0.94 (0.40, 2.19) | 2.43 (1.86, 3.17) | 1.59 (1.07, 2.36) |
| Maternal birth region | ||||||||
| Western Europe | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | (−) | (−) | 1.0 (Reference) | 1.0 (Reference) |
| Southeast Asia | 0.86 (0.60, 1.23) | 1.02 (0.66, 1.60) | 0.53 (0.34, 0.82) | 0.63 (0.36, 1.11) | (−) | (−) | 1.37 (0.65, 2.92) | 1.88 (0.82, 4.30) |
| South & Rest of Asia | 0.31 (0.21, 0.45) | 0.45 (0.28, 0.71) | 0.28 (0.17, 0.45) | 0.40 (0.23, 0.72) | (−) | (−) | 0.96 (0.45, 2.08) | 1.23 (0.54, 2.82) |
| Eastern Europe | 1.43 (0.98, 2.09) | 1.96 (1.27, 3.04) | 1.02 (0.64, 1.62) | 1.53 (0.89, 2.62) | (−) | (−) | 1.78 (0.79, 4.00) | 1.77 (0.75, 4.17) |
| Rest of Europe | 2.39 (1.58, 3.60) | 2.10 (1.31, 3.39) | 3.62 (2.28, 5.74) | 3.57 (2.10, 6.07) | (−) | (−) | 1.30 (0.51, 3.30) | 1.54 (0.58, 4.07) |
| East Africa | 0.61 (0.38, 0.97) | 0.83 (0.46, 1.49) | 0.61 (0.35, 1.05) | 0.41 (0.20, 0.86) | (−) | (−) | 1.86 (0.81, 4.26) | 1.06 (0.40, 2.76) |
| West Africa | 0.54 (0.29, 1.01) | 0.63 (0.31, 1.27) | 0.26 (0.11, 0.61) | 0.25 (0.09, 0.65) | (−) | (−) | 1.68 (0.67, 4.22) | 1.48 (0.53, 4.15) |
| Rest of Africa | 0.68 (0.41, 1.12) | 0.84 (0.46, 1.51) | 0.53 (0.27, 1.04) | 0.35 (0.14, 0.87) | (−) | (−) | 2.53 (1.10, 5.81) | 1.40 (0.55, 3.60) |
| North America & Oceania | 2.00 (1.31, 3.05) | 2.47 (1.52, 4.02) | 1.48 (0.83, 2.65) | 1.64 (0.85, 3.20) | (−) | (−) | 1.01 (0.37, 2.74) | 1.04 (0.37, 2.93) |
| Latin America & Caribbean | 1.69 (1.15, 2.47) | 1.74 (1.10, 2.74) | 1.51 (0.95, 2.41) | 1.14 (0.66, 1.99) | (−) | (−) | 1.76 (0.78, 3.96) | 1.31 (0.56, 3.05) |
| Duration of residence | ||||||||
| < 5 years | 0.35 (0.30, 0.41) | 0.43 (0.35, 0.52) | 0.33 (0.27, 0.40) | 0.46 (0.36, 0.60) | 0.08 (0.04, 0.17) | 0.07 (0.03, 0.16) | 1.26 (0.93, 1.72) | 1.50 (1.07, 2.12) |
| 5–9 years | 0.42 (0.35, 0.51) | 0.52 (0.42, 0.64) | 0.43 (0.34, 0.54) | 0.58 (0.45, 0.75) | 0.39 (0.23, 0.68) | 0.44 (0.25, 0.78) | 0.86 (0.59, 1.25) | 0.94 (0.64, 1.40) |
| 10 years and more | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) | 1.0 (Reference) |
aOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models
baOR Odds Ratios with 95% CI (Confidence Intervals) are derived from Generalized Estimating Equation models, adjusted for Maternal age, lone mother, low education, neighborhood income quintile, urban residence, family size, employment & income assistance, and knowledge of official Canadian languages
Bold values = Significant association (p < 0.05)
(−) = unreportable (n < 6 for internal comparison group)
cTotal excludes missing values for outcomes where (n=)
Frequencies missing for outcomes: (Alcohol use during pregnancy n = 3771; Smoking during pregnancy n = 1207; Substance use during pregnancy n = 3887; Late initiation of prenatal care > 13 weeks n = 1493)
Only smoking during pregnancy was lower among secondary immigrants than primary immigrants (Table 4). Refugees had higher prevalences of smoking and substance use, but the associations became non-significant after adjustment. Refugees more likely experienced late initiation of PNC compared to non-refugees. Compared to Western Europeans, pregnancy smoking and alcohol consumption were higher among North & South Europe women in the adjusted analysis. Women from Eastern Europe, North America & Oceania, and Latin America & the Caribbean had higher adjusted odds of consuming alcohol but not of smoking. Those from Africa had lower adjusted odds of smoking but not of alcohol consumption, while those from South & Rest of Asia had significantly lower odds of smoking and alcohol use. We did not report odds ratio estimates for substance use by birth regions because the cell count for the internal comparison group (Western Europeans) was less than six. Late initiation of PNC did not exhibit significant variation by region of birth after adjustment. Recent immigrants were less likely to consume alcohol, smoke, or engage in substance use during pregnancy but had 50% higher odds of late initiation of PNC compared to long-term immigrants.
Discussion
Main findings
In our population-based study, immigrants had a higher prevalence of social isolation than non-immigrants but a lower prevalence of other outcomes. Psychosocial and behavioral risks varied by immigrant characteristics; refugee status was strongly associated with relationship distress, depression, and late initiation of PNC; recent immigration with social isolation and late initiation of PNC and certain maternal birth regions with relationship distress, depression, smoking, and/or alcohol use during pregnancy.
Strengths and limitations
A major strength of this study was a novel linkage of the BFS/FFS data with the immigration data. Another strength is the population-based nature of the study, including a large and ethnically diverse sample. However, our study had limitations. First, the BFS/FFS data had varying degrees of missing data in the dependent variables. Missingness in some dependent variables may have affected some comparisons between immigrants and non-immigrants, given that missingness was higher among non-immigrants (23.3% for social isolation, 33.5% for partner violence, 21.8% for alcohol use and 22.2% for substance use) than among immigrants (12.8% for social isolation, 26.9% for partner violence, 11.2% for alcohol use and 11.5% for substance use), with standardized differences larger than 0.1. There were no statistically significant differences in the proportion of missing values according to immigration status for depression (overall 12.1% missing), relationship distress (11.5%), smoking during pregnancy (4.6%) and late initiation of prenatal care (5.8%). On the other hand, social desirability may have underestimated prevalence of some behavioral indicators such as alcohol and substance use during pregnancy. Similarly, individuals experiencing partner violence are less likely to respond to this question for various reasons, including fear of police involvement. However, although some outcomes may be underreported, associations may only be biased if the underreporting was differential according to immigration status. Overall, the potential impact of missingness on the magnitude of associations is uncertain, but the direction may hold for most of the outcomes, given the strong observed associations.
Second, given that the public health nurses complete the BFS/FFS based on their assessment and the information provided by the mother, interviewer bias cannot be ruled out. Although some recall bias may occur, this is likely minimal because of the short time frame between the birth and the completion of the BFS/FFS. Third, excluding women without screening data (i.e., who gave birth to stillborn or children who died in the early neonatal period or had a live birth but did not participate in the screening) implies that our findings may not be generalizable to these cases. Our results apply to permanent residents and cannot be generalized to temporary residents not covered by the provincial health insurance plan, such as asylum seekers. Our measure of duration of residence may underestimate exposure to the Canadian environment among those who became permanent residents after being temporary residents. Fourth, residual confounding due to unmeasured factors or non-detailed measurements, such as the number of cigarettes per day for smoking or frequency and amount of alcohol consumed, may have affected the associations and efficiency of adjustment. Likewise, our data did not distinguish specific forms of partner violence; physical (assault, battery), sexual, verbal abuse, psychological aggression, or control (financial, emotional, coercion) [47]. Last, we could not measure associations for substance use by maternal birth region due to very small sample sizes for certain birth regions.
Regardless of these limitations, our findings contribute to a greater understanding of the complexity of psychosocial and behavioral perinatal health risks of immigrant childbearing women by identifying patterns and subgroups at higher and lower risk, as follows.
Social isolation
The prevalence of social isolation among immigrants in our study (12.3%) was similar to the prevalence reported in a sample of German adults [48]. Culturally relevant support often enjoyed in home countries may be lost after migration-related family separation [49] or not well-established in western countries post-migration [50]. This may explain the high odds among immigrants and across all birth regions [31, 51] except North America & Oceania [52], most of whom are native English speakers, which could explain their lower odds. The result for recent immigrants is unsurprising, given that time is needed to integrate into a new environment and rebuild social networks. Establishing multiple networks over time may improve access to appropriate information that promotes positive health behaviors or minimize stressful situations [53] and possibly explain the drastic reduction after 5 years of residence.
Relationship distress
We found an overall low prevalence among immigrants compared to non-immigrants. A few studies on marital relationships among immigrants are qualitative [15–17] with no comparative results for non-immigrants. Among immigrants, the high odds of experiencing relationship distress for refugees and African immigrant women are consistent with a few qualitative studies [16, 54, 55]. Unlike economic immigrants, refugees’ forced migration may exacerbate disagreements between couples in terms of perceptions and expectations regarding life post-migration. Their disadvantaged social status [56, 57] may create financial hardship, triggering conflict where females depend more on their spouses financially. African men have reportedly shown low involvement and support towards home care or responsibilities [55]. Acculturation stress and gender role reversal [15, 54] can trigger conflict, where women’s new financial power threatens their partner’s authority [58], and women combine home care with work demands. The low prevalence among secondary immigrants is consistent with reported better health outcomes among secondary immigrants who voluntarily transitioned to Canada from an industrialized country compared to primary migrants from non-industrialized birth [24]. A plausible explanation is the selective migration of couples pursuing upward global social mobility [24] that may have gained more economic advantage [26], reducing stressors accompanying their transit [44]. Similarly, selective migration of couples in harmonious relationships may explain the lower odds among recent immigrants.
Partner violence
Consistent with past studies [59–61] is the low prevalence among immigrants, which may be related to differences in the perception of violence. Some immigrant women may not consider some acts violent, may be reluctant to acknowledge or report violence, or overcome structural barriers to navigating help within a complex immigration system [62]. Cultural or social pressures and financial dependency on spouses may cause them to tolerate abuse in silence [47]. The high odds among women from Africa were of significant interest, particularly those from West Africa. This association was very strong but was no longer significant after adjustment, explained partially by control variables and partially by a relatively small subgroup size. We highlight this result based on reported high rates and risk of physical abuse or partner violence among Africans [58, 63]. Normalization of violence may be due to stigma or fear, particularly among women from regions where women have subordinate roles and are disempowered [64].
Depression
Although many studies reported a high prevalence of depression among immigrants compared to non-immigrants [18, 19, 30], our findings align with other studies that found a lower prevalence [65], consistent with the healthy migration hypothesis. Our results further confirmed this hypothesis among recent immigrants, consistent with past studies from the United States [66] and Canada [65]. Conversely, other studies have reported high risk among recent migrants [18, 29] and risk regardless of time since migration [65]. The higher odds of depression among refugees align with previous findings [18, 32]. Unlike economic migrants driven by upscale social mobility and selected for migration, refugees are displaced people who did not seek to migrate and are generally less healthy [7]. Our result also agrees with the reportedly high risk among women from Europe [67], Latin America & the Caribbean [30, 68]. Social support is protective against depression [18, 69], and we found that immigrant women were more socially isolated. Being socially isolated may underlie depression among these birth regions, particularly refugees, due to loss of homeplace practices related to childbirth and support post migration [70].
Alcohol use, smoking & substance/drug use
Our results agree with studies conducted in Canada [22, 23, 34], the United States [35], and France [20] that have shown that immigrants were less likely to engage in unhealthy behavior during pregnancy compared to non-immigrants, which may be related to protective cultural strengths that immigrants bring with them from their countries of origin [71]. We observed similar results among recent immigrants, consistent with a study in the United Kingdom that reported low smoking prevalence that increased for every five-year additional length of stay [72]. The lower odds among secondary immigrants may be due to more health system utilization advantage they likely gained during their transit [26]. Conversely, we found high-risk patterns for consuming alcohol among East Europe, North America & Oceania, and Latin America & the Caribbean, in addition to smoking among North & South Europe, consistent with a Swedish population-based study that found high pregnancy smoking prevalence among immigrant women [73]. Longer historical exposure to cultural acceptance of smoking and alcohol and more gender equality may explain the high prevalence among immigrants from these westernized regions compared to regions where women do not traditionally drink or smoke, as the case is for South & Rest of Asia and Africa.
Prenatal care
Past studies have demonstrated a high likelihood of late initiation of PNC among immigrants compared to non-immigrants [74–77]. Instead, we found a lower likelihood, which partly could be due to selection bias and may mean that immigrants who completed a screening may be more committed to PNC than those who did not. Protective for late initiation of PNC among immigrants to Manitoba perhaps is access to universal health care and the opportunity to choose from several available care providers such as family physicians, obstetricians, and midwives. However, plausible explanations for the high risk among refugees [78] and recent immigrants [74, 79] may be less familiarity with the receiving country’s health care system, language barriers, insufficient support to access services, and discordant expectations between the women and their service providers [13, 79]. It may also be possible that recent immigrants were underrepresented in the screening since a longer duration of residence was associated with lower odds of late initiation of prenatal care.
Conclusion
In this population-based study, we found that compared to non-immigrants, immigrant childbearing women exhibited a higher prevalence of social isolation but a lower prevalence of other psychosocial and behavioral perinatal health indicators. Immigrant subgroups such as refugees, recent immigrants, and certain maternal birth regions exhibited high-risk patterns for multiple indicators.
Findings from this study may help health care providers increase awareness of the heterogeneity of the immigrant population and immigrant subgroups at higher and lower risk for psychosocial and behavioral perinatal health outcomes, and incorporate these considerations in the continuum of care. The high risk for social isolation among recent immigrants, multiple perinatal psychosocial risks among refugee immigrants, and other high-risk patterns in behavioral outcomes among particular birth regions may reflect the lack of awareness of settlement resources, expectation mismatch, or unmet needs across the range of currently available services in the province. Our findings also evidence the limitation of the BFS/FFS as a surveillance tool, particularly concerning high proportion of non-response in some key indicators of risk. Findings from this study call for further research towards exploring and identifying unmet needs across new and existing support programs for immigrant childbearing women. Much attention should focus on the growing diversity of immigrants, particularly recent and refugee immigrants.
Acknowledgments
The authors are grateful to Heather Prior and Wendy Au for their assistance in the data extraction process. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed in the material are those of the authors and not necessarily CIHI. The authors acknowledge the Manitoba Centre for Health Policy (MCHP) for the use of data contained in the Manitoba Population Research Repository under project #2021-018. We acknowledge Manitoba Health, Seniors and Active Living, Immigration, Refugees and Citizenship Canada, and Manitoba Families for the use of their data. The results and conclusions are those of the authors, and no official endorsement by the MCHP, Manitoba Health, IRCC, or other data providers is intended or should be inferred.
Abbreviations
- BFS/FFS
Baby First Screening/ Family First Screening
- IRCC-PR
Immigration, Refugees, and Citizenship Canada Permanent Resident
- SAMIN
Social Allowances Management Information Network
- MHIR
Manitoba Health Insurance Registry
- PNC
Prenatal care
Authors’ contributions
RE formulated the research questions, study design, data cleaning, statistical analysis, interpretation of results, wrote the first draft, and other manuscript iterations. MLU contributed to the funding, research design, interpretation of results, manuscript preparation, supervision, and overall research integrity. MJC provided content expertise on BFS/FFS data. MJC, NN, EW, and MLU contributed to the methodology, interpretation of the findings, revised the manuscript drafts, and approved the final version of the manuscript. The author(s) read and approved the final manuscript.
Authors’ information
NA
Funding
RE was supported by MLU through a fellowship funded by a grant from the Canadian Institutes for Health Research (CIHR) FDN 154280. MLU holds a Canada Research Chair in Applied Population Health.
Availability of data and materials
The datasets generated and analyzed for this study are not publicly available because of Manitoba privacy regulations for highly sensitive personal information data. Access to data at the Manitoba Population Research Data Repository can be granted to those who meet pre-specified criteria for confidential access. Requests to access data for research purposes must be sent to MCHP_Access@cpe.umanitoba.ca. Refer to MCHP policies on data access and use [80].
Declarations
Ethics approval and consent to participate
This study received approval from the University of Manitoba Health Research Ethics Board HS24346 (H2020:446), the Manitoba Health Seniors and Active Living Health Information Privacy Committee HIPC 2020/2021–50 (now Provincial Health Research Privacy Committee), and data use approvals from Immigration, Refugees, and Citizenship Canada (IRCC) and the Department of Families. Informed consent by participants was not required to use this de-identified retrospective data based on the law (Personal Health Information Act) governing access to this information [81].
All methods and procedures in this study were conducted in accordance with the Manitoba Centre for Health Policy’s (MCHP) policies, and results were reported based on the STROBE guidelines.
Consent for publication
NA
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gagnon AJ, Dougherty G, Wahoush O, Saucier J-F, Dennis C-L, Stanger E, Palmer B, Merry L, Stewart DE. International migration to Canada: the post-birth health of mothers and infants by immigration class. Soc Sci Med. 2013;76:197–207. doi: 10.1016/j.socscimed.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Urquia ML, Glazier RH, Blondel B, Zeitlin J, Gissler M, Macfarlane A, Ng E, Heaman M, Stray-Pedersen B, Gagnon AJ, et al. International migration and adverse birth outcomes: role of ethnicity, region of origin and destination. J Epidemiol Community Health. 2010;64(3):243. doi: 10.1136/jech.2008.083535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaushal N, Lu Y. Recent immigration to Canada and the United States: a mixed tale of relative selection. Int Migr Rev. 2015;49(2):479–522. doi: 10.1111/imre.12093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim I-H, Carrasco C, Muntaner C, McKenzie K, Noh S. Ethnicity and postmigration health trajectory in new immigrants to Canada. Am J Public Health. 2013;103(4):e96–e104. doi: 10.2105/AJPH.2012.301185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamilton TG. The healthy immigrant (migrant) effect: in search of a better native-born comparison group. Soc Sci Res. 2015;54:353–365. doi: 10.1016/j.ssresearch.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hossin MZ. International migration and health: it is time to go beyond conventional theoretical frameworks. BMJ Glob Health. 2020;5(2):e001938. doi: 10.1136/bmjgh-2019-001938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wanigaratne S, Cole DC, Bassil K, Hyman I, Moineddin R, Urquia ML. The influence of refugee status and secondary migration on preterm birth. J Epidemiol Community Health. 2016;70(6):622–628. doi: 10.1136/jech-2015-206529. [DOI] [PubMed] [Google Scholar]
- 8.Hyman I, Forte T, Du Mont J, Romans S, Cohen MM. The association between length of stay in Canada and intimate partner violence among immigrant women. Am J Public Health. 2006;96(4):654–659. doi: 10.2105/AJPH.2004.046409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmad F, Ali M, Stewart D. Spousal-abuse among Canadian immigrant women. J Immigr Health. 2005;7:239–246. doi: 10.1007/s10903-005-5120-4. [DOI] [PubMed] [Google Scholar]
- 10.Beydoun HA, Al-Sahab B, Beydoun MA, Tamim H. Intimate partner violence as a risk factor for postpartum depression among Canadian women in the maternity experience survey. Ann Epidemiol. 2010;20(8):575–583. doi: 10.1016/j.annepidem.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miszkurka M, Zunzunegui MV, Goulet L. Immigrant status, antenatal depressive symptoms, and frequency and source of violence: what's the relationship? Arch Women’s Mental Health. 2012;15(5):387–396. doi: 10.1007/s00737-012-0298-7. [DOI] [PubMed] [Google Scholar]
- 12.Hwang S-S, Xi J, Cao Y, Feng X, Qiao X. Anticipation of migration and psychological stress and the three gorges dam project, China. Soc Sci Med. 2007;65(5):1012–1024. doi: 10.1016/j.socscimed.2007.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higginbottom GMA, Morgan M, Alexandre M, Chiu Y, Forgeron J, Kocay D, Barolia R. Immigrant women’s experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev. 2015;4(1):13. doi: 10.1186/2046-4053-4-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garcia ER, Yim IS. A systematic review of concepts related to women's empowerment in the perinatal period and their associations with perinatal depressive symptoms and premature birth. BMC Pregnancy Childbirth. 2017;17(Suppl 2):347. doi: 10.1186/s12884-017-1495-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khawaja NG, Milner K. Acculturation stress in south Sudanese refugees: impact on marital relationships. Int J Intercult Relat. 2012;36(5):624–636. doi: 10.1016/j.ijintrel.2012.03.007. [DOI] [Google Scholar]
- 16.Hyman I, Guruge S, Mason R. The impact of migration on marital relationships: a study of Ethiopian immigrants in Toronto. J Comp Fam Stud. 2008;39(2):149–163. doi: 10.3138/jcfs.39.2.149. [DOI] [Google Scholar]
- 17.Hyman I, Mason R, Guruge S, Berman H, Kanagaratnam P, Manuel L. Perceptions of factors contributing to intimate partner violence among Sri Lankan Tamil immigrant women in Canada. Health Care Women Int. 2011;32:779–794. doi: 10.1080/07399332.2011.569220. [DOI] [PubMed] [Google Scholar]
- 18.Dennis CL, Merry L, Gagnon AJ. Postpartum depression risk factors among recent refugee, asylum-seeking, non-refugee immigrant, and Canadian-born women: results from a prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):411–422. doi: 10.1007/s00127-017-1353-5. [DOI] [PubMed] [Google Scholar]
- 19.Daoud N, O’Brien K, O’Campo P, Harney S, Harney E, Bebee K, Bourgeois C, Smylie J. Postpartum depression prevalence and risk factors among indigenous, non-indigenous and immigrant women in Canada. Can J Public Health. 2019;110(4):440–452. doi: 10.17269/s41997-019-00182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melchior M, Chollet A, Glangeaud-Freudenthal N, Saurel-Cubizolles M-J, Dufourg M-N, van der Waerden J, Sutter-Dallay A-L. Tobacco and alcohol use in pregnancy in France: the role of migrant status: the nationally representative ELFE study. Addict Behav. 2015;51:65–71. doi: 10.1016/j.addbeh.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Fanslow J, Silva M, Robinson E, Whitehead A. Violence during pregnancy: associations with pregnancy intendedness, pregnancy-related care, and alcohol and tobacco use among a representative sample of New Zealand women. Aust N Z J Obstet Gynaecol. 2008;48(4):398–404. doi: 10.1111/j.1479-828X.2008.00890.x. [DOI] [PubMed] [Google Scholar]
- 22.Gilbert NL, Nelson CR, Greaves L. Smoking cessation during pregnancy and relapse after childbirth in Canada. J Obstet Gynaecol Can. 2015;37(1):32–39. doi: 10.1016/S1701-2163(15)30360-1. [DOI] [PubMed] [Google Scholar]
- 23.Al-Sahab B, Saqib M, Hauser G, Tamim H. Prevalence of smoking during pregnancy and associated risk factors among Canadian women: a national survey. BMC Pregnancy Childbirth. 2010;10(1):24. doi: 10.1186/1471-2393-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Urquia ML, Frank JW, Glazier RH. From places to flows. International secondary migration and birth outcomes. Soc Sci Med. 2010;71(9):1620–1626. doi: 10.1016/j.socscimed.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Greenwood MJ, Young PA. Geographically indirect immigration to Canada: description and analysis. Int Migr Rev. 1997;31(1):51–71. doi: 10.1177/019791839703100103. [DOI] [PubMed] [Google Scholar]
- 26.Takenaka A. Secondary migration: who re-migrates and why these migrants matter. Migration information source. 2007. [Google Scholar]
- 27.Fuller-Thomson E, Noack AM, George U. Health decline among recent immigrants to Canada: findings from a nationally-representative longitudinal survey. Can J Public Health. 2011;102(4):273–280. doi: 10.1007/BF03404048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Urquia ML, Frank JW, Moineddin R, Glazier RH. Immigrants’ duration of residence and adverse birth outcomes: a population-based study. BJOG. 2010;117(5):591–601. doi: 10.1111/j.1471-0528.2010.02523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Urquia ML, O'Campo PJ, Heaman MI. Revisiting the immigrant paradox in reproductive health: the roles of duration of residence and ethnicity. Soc Sci Med. 2012;74(10):1610–1621. doi: 10.1016/j.socscimed.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 30.Miszkurka M, Goulet L, Zunzunegui MV. Contributions of immigration to depressive symptoms among pregnant women in Canada. Can J Public Health. 2010;101(5):358–364. doi: 10.1007/BF03404853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson AM, Benzies KM, Cairns SL, Fung T, Tough SC. Who is distressed? A comparison of psychosocial stress in pregnancy across seven ethnicities. BMC Pregnancy Childbirth. 2016;16(1):215. doi: 10.1186/s12884-016-1015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stewart DE, Gagnon A, Saucier J-F, Wahoush O, Dougherty G. Postpartum depression symptoms in newcomers. Can J Psychiatry. 2008;53(2):121–124. doi: 10.1177/070674370805300208. [DOI] [PubMed] [Google Scholar]
- 33.Hyman I, Dussault G. Negative consequences of acculturation on health behaviour, social support and stress among pregnant southeast Asian immigrant women in Montreal: an exploratory study. Can J Public Health. 2000;91(5):357–360. doi: 10.1007/BF03404807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kingston D, Heaman M, Chalmers B, Kaczorowski J, O’Brien B, Lee L, Dzakpasu S, O’Campo P. Comparison of maternity experiences of Canadian-born and recent and non-recent immigrant women: findings from the Canadian maternity experiences survey. J Obstet Gynaecol Can. 2011;33(11):1105–1115. doi: 10.1016/S1701-2163(16)35078-2. [DOI] [PubMed] [Google Scholar]
- 35.Elo IT, Culhane JF. Variations in health and health behaviors by nativity among pregnant black women in Philadelphia. Am J Public Health. 2010;100(11):2185–2192. doi: 10.2105/AJPH.2009.174755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Concept: Record Linkage in Manitoba [http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?conceptID=1363#a_references Accessed 7 July 2022].
- 37.Brownell MD, Chartier M, Santos R, Au W, Roos NP, Girard D. Evaluation of a newborn screen for predicting out-of-home placement. Child Maltreat. 2011;16(4):239–249. doi: 10.1177/1077559511422942. [DOI] [PubMed] [Google Scholar]
- 38.Urquia M, Walld R, Wanigaratne S, Eze N, Azimaee M, McDonald JT, Guttmann A. Linking National Immigration Data to provincial repositories: the case of Canada. International journal of population data. Science. 2021;6(1):1412. doi: 10.23889/ijpds.v6i1.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.United Nations: standard country or area codes for statistical use (M49). https://unstats.un.org/unsd/methodology/m49/. Accessed 14 July 2020.
- 40.Hughes RA, Heron J, Sterne JAC, Tilling K. Accounting for missing data in statistical analyses: multiple imputation is not always the answer. Int J Epidemiol. 2019;48(4):1294–1304. doi: 10.1093/ije/dyz032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wirth KE, Tchetgen Tchetgen EJ, Murray M. Adjustment for missing data in complex surveys using doubly robust estimation: application to commercial sexual contact among Indian men. Epidemiology. 2010;21(6):863–871. doi: 10.1097/EDE.0b013e3181f57571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schreiber-Gregory D, Bader K. Logistic and linear regression assumptions: Violation recognition and control. 2018. [Google Scholar]
- 43.Shoukri MM. Analysis of correlated data with SAS and R, fourth edition. Boca Raton: CRC Press, Taylor & Francis Group; 2018. [Google Scholar]
- 44.Montazer S. Disentangling the effects of primary and secondary international migration on psychological distress: the role of mastery. Can J Public Health. 2018;109(3):284–293. doi: 10.17269/s41997-018-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Snow G, Melvin GA, Boyle JA, Gibson-Helm M, East CE, McBride J, et al. Perinatal psychosocial assessment of women of refugee background. Women Birth. 2021;34(3):e302–e308. [DOI] [PubMed]
- 46.Urquia ML, Glazier RH, Mortensen L, Nybo-Andersen A-M, Small R, Davey M-A, Rööst M, Essén B. ROAM ft: severe maternal morbidity associated with maternal birthplace in three high-immigration settings. Eur J Pub Health. 2015;25(4):620–625. doi: 10.1093/eurpub/cku230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Midlarsky E, Venkataramani-Kothari A, Plante M. Domestic violence in the Chinese and south Asian immigrant communities. Ann N Y Acad Sci. 2006;1087(1):279–300. doi: 10.1196/annals.1385.003. [DOI] [PubMed] [Google Scholar]
- 48.Röhr S, Wittmann F, Engel C, Enzenbach C, Witte AV, Villringer A, et al. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc Psychiatry Psychiatr Epidemiol. 2021:1–10. [DOI] [PMC free article] [PubMed]
- 49.Hurtado-de-Mendoza A, Gonzales FA, Serrano A, Kaltman S. Social isolation and perceived barriers to establishing social networks among Latina immigrants. Am J Community Psychol. 2014;53(1):73–82. doi: 10.1007/s10464-013-9619-x. [DOI] [PubMed] [Google Scholar]
- 50.Kim HS, Sherman DK, Taylor SE. Culture and social support. Am Psychol. 2008;63(6):518–526. doi: 10.1037/0003-066X. [DOI] [PubMed] [Google Scholar]
- 51.Hawthorne G. Perceived social isolation in a community sample: its prevalence and correlates with aspects of peoples’ lives. Soc Psychiatry Psychiatr Epidemiol. 2008;43(2):140–150. doi: 10.1007/s00127-007-0279-8. [DOI] [PubMed] [Google Scholar]
- 52.Schumaker JF, Shea JD, Monfries MM, Groth-Marnat G. Loneliness and life satisfaction in Japan and Australia. J Psychol. 1993;127(1):65–71. doi: 10.1080/00223980.1993.9915543. [DOI] [PubMed] [Google Scholar]
- 53.Cacioppo J, Hawkley L. Social isolation and health, with an emphasis on underlying mechanisms. Perspect Biol Med. 2003;46:S39–S52. doi: 10.1353/pbm.2003.0049. [DOI] [PubMed] [Google Scholar]
- 54.Milner K, Khawaja NG. Sudanese refugees in Australia: the impact of acculturation stress. J Pac Rim Psychol. 2010;4(1):19–29. doi: 10.1375/prp.4.1.19. [DOI] [Google Scholar]
- 55.Stewart M, Dennis CL, Kariwo M, Kushner KE, Letourneau N, Makumbe K, Makwarimba E, Shizha E. Challenges faced by refugee new parents from Africa in Canada. J Immigr Minor Health. 2015;17(4):1146–1156. doi: 10.1007/s10903-014-0062-3. [DOI] [PubMed] [Google Scholar]
- 56.Brown-Bowers A, McShane K, Wilson-Mitchell K, Gurevich M. Postpartum depression in refugee and asylum-seeking women in Canada: a critical health psychology perspective. Health (London) 2015;19(3):318–335. doi: 10.1177/1363459314554315. [DOI] [PubMed] [Google Scholar]
- 57.O'Mahony JM, Donnelly TT. How does gender influence immigrant and refugee women's postpartum depression help-seeking experiences? J Psychiatr Ment Health Nurs. 2013;20(8):714–725. doi: 10.1111/jpm.12005. [DOI] [PubMed] [Google Scholar]
- 58.Menjívar C, Salcido O. Immigrant women and domestic violence: common experiences in different countries. Gend Soc. 2002;16(6):898–920. doi: 10.1177/089124302237894. [DOI] [Google Scholar]
- 59.Cohen MM, Maclean H. Violence against Canadian women. BMC Womens Health. 2004;4(1):S22. doi: 10.1186/1472-6874-4-S1-S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Daoud N, Urquia ML, O'Campo P, Heaman M, Janssen PA, Smylie J, Thiessen K. Prevalence of abuse and violence before, during, and after pregnancy in a national sample of Canadian women. Am J Public Health. 2012;102(10):1893–1901. doi: 10.2105/AJPH.2012.300843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kingston D, Heaman M, Urquia M, O’Campo P, Janssen P, Thiessen K, Smylie J. Correlates of abuse around the time of pregnancy: results from a national survey of Canadian women. Matern Child Health J. 2016;20(4):778–789. doi: 10.1007/s10995-015-1908-6. [DOI] [PubMed] [Google Scholar]
- 62.Holtmann C, Rickards T. Domestic/intimate partner violence in the lives of immigrant women: a New Brunswick response. Can J Public Health. 2018;109(3):294–302. doi: 10.17269/s41997-018-0056-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stewart DE, Gagnon AJ, Merry LA, Dennis C-L. Risk factors and health profiles of recent migrant women who experienced violence associated with pregnancy. J Women's Health. 2012;21(10):1100–1106. doi: 10.1089/jwh.2011.3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization . WHO multi-country study on women’s health and domestic violence against women summary report- initial results on prevalence, health outcomes and women’s responses. 2005. [Google Scholar]
- 65.Chow A, Dharma C, Chen E, Mandhane PJ, Turvey SE, Elliott SJ, Becker AB, Subbarao P, Sears MR, Kozyrskyj AL. Trajectories of depressive symptoms and perceived stress from pregnancy to the postnatal period among Canadian women: impact of employment and immigration. Am J Public Health. 2019;109(S3):S197–S204. doi: 10.2105/AJPH.2018.304624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ryan-Ibarra S, Epstein JF, Induni M, Wright MA. Current depression among women in California according to residence in the California-Mexico border region. Rev Panam Salud Publica. 2012;31(5):417–426. doi: 10.1590/S1020-49892012000500010. [DOI] [PubMed] [Google Scholar]
- 67.Levecque K, Van Rossem R. Depression in Europe: does migrant integration have mental health payoffs? A cross-national comparison of 20 European countries. Ethn Health. 2015;20(1):49–65. doi: 10.1080/13557858.2014.883369. [DOI] [PubMed] [Google Scholar]
- 68.Lacey KK, Park J, Briggs AQ, Jackson JS. National origins, social context, timing of migration and the physical and mental health of Caribbeans living in and outside of Canada. Ethn Health. 2019;27(1):223–246. doi: 10.1080/13557858.2019.1634183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.King L, Feeley N, Gold I, Hayton B, Zelkowitz P. The healthy migrant effect and predictors of perinatal depression. Women Birth. 2019;32(3):e341–e350. doi: 10.1016/j.wombi.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 70.O'Mahony J, Donnelly T. Immigrant and refugee women's post-partum depression help-seeking experiences and access to care: a review and analysis of the literature. J Psychiatr Ment Health Nurs. 2010;17(10):917–928. doi: 10.1111/j.1365-2850.2010.01625.x. [DOI] [PubMed] [Google Scholar]
- 71.Urquia ML, Frank JW, Moineddin R, Glazier RH. Does time since immigration modify neighborhood deprivation gradients in preterm birth? A multilevel analysis. J Urban Health. 2011;88(5):959–976. doi: 10.1007/s11524-011-9569-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hawkins SS, Lamb K, Cole TJ, Law C. Influence of moving to the UK on maternal health behaviours: prospective cohort study. BMJ. 2008;336(7652):1052. doi: 10.1136/bmj.39532.688877.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Urquia M, Juárez S, Wall-Wieler E, Hjern A. Smoking during pregnancy among immigrant women with same-origin and Swedish-born partners. Nicotine Tob Res. 2020;23:349–356. doi: 10.1093/ntr/ntaa145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gonthier C, Estellat C, Deneux-Tharaux C, Blondel B, Alfaiate T, Schmitz T, Oury J-F, Mandelbrot L, Luton D, Ravaud P, et al. Association between maternal social deprivation and prenatal care utilization: the PreCARE cohort study. BMC Pregnancy Childbirth. 2017;17(1):126. doi: 10.1186/s12884-017-1310-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cresswell JA, Yu G, Hatherall B, Morris J, Jamal F, Harden A, Renton A. Predictors of the timing of initiation of antenatal care in an ethnically diverse urban cohort in the UK. BMC Pregnancy Childbirth. 2013;13(1):103. doi: 10.1186/1471-2393-13-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Trinh LTT, Rubin G. Late entry to antenatal care in New South Wales, Australia. Reprod Health. 2006;3(1):8. doi: 10.1186/1742-4755-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Choté AA, Koopmans GT, Redekop WK, de Groot CJ, Hoefman RJ, Jaddoe VW, Hofman A, Steegers EA, Mackenbach JP, Trappenburg M, et al. Explaining ethnic differences in late antenatal care entry by predisposing, enabling and need factors in the Netherlands. The generation R study. Matern Child Health J. 2011;15(6):689–699. doi: 10.1007/s10995-010-0619-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kandasamy T, Cherniak R, Shah R, Yudin MH, Spitzer R. Obstetric risks and outcomes of refugee women at a single Centre in Toronto. J Obstet Gynaecol Can. 2014;36(4):296–302. doi: 10.1016/S1701-2163(15)30604-6. [DOI] [PubMed] [Google Scholar]
- 79.Heaman MI, Green CG, Newburn-Cook CV, Elliott LJ, Helewa ME. Social inequalities in use of prenatal care in Manitoba. J Obstet Gynaecol Can. 2007;29(10):806–816. doi: 10.1016/S1701-2163(16)32637-8. [DOI] [PubMed] [Google Scholar]
- 80.Manitoba Center for Health Policy: The Manitoba Population Research Data Repository [https://umanitoba.ca/manitoba-centre-for-health-policy/data-repositoryhttps://umanitoba.ca/faculties/health_sciences/medicine/units/chs/departmental_units/mchp/education/media/4_privacy.pdf Accessed 5 May 2022].
- 81.Manitoba Government: The Personal Health Information Act (PHIA) [https://www.gov.mb.ca/health/phia/index.html Accessed 5 May 2022].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed for this study are not publicly available because of Manitoba privacy regulations for highly sensitive personal information data. Access to data at the Manitoba Population Research Data Repository can be granted to those who meet pre-specified criteria for confidential access. Requests to access data for research purposes must be sent to MCHP_Access@cpe.umanitoba.ca. Refer to MCHP policies on data access and use [80].


