Abstract
Purpose:
A novel, selective, next-generation transforming growth factor beta (TGFβ) receptor type-1 small molecule inhibitor, LY3200882, demonstrated promising preclinical data. This first-in-human trial evaluated safety, tolerability, recommended phase II dose (RP2D), pharmacokinetics, pharmacodynamics, and preliminary antitumor activity of LY3200882 as monotherapy or with other anticancer agents in patients with advanced cancer.
Patients and Methods:
This phase I multicenter study of oral LY3200882 (NCT02937272) comprised dose escalation, monotherapy expansion in grade 4 glioma, and combination therapy in solid tumors (LY3200882 and PD-L1 inhibitor LY3300054), pancreatic cancer (LY3200882, gemcitabine, and nab-paclitaxel), and head and neck squamous cell cancer (LY3200882, cisplatin, and radiation).
Results:
Overall, 139 patients with advanced cancer were treated. The majority (93.5%) of patients experienced ≥1 treatment-emergent adverse events (TEAE), with 39.6% LY3200882-related. Grade 3 LY3200882-related toxicities were only observed in combination therapy arms. One patient in the pancreatic cancer arm experienced cardiovascular toxicity. The LY3200882 monotherapy RP2Ds were established in two schedules: 50 mg twice a day 2-weeks-on/2-weeks-off and 35 mg twice a day 3-weeks-on/1-week-off. Four patients with grade 4 glioma had durable Revised Assessment in Neuro Oncology (RANO) partial responses (PR) with LY3200882 monotherapy (n = 3) or LY3200882-LY3300054 combination therapy (n = 1). In treatment-naïve patients with advanced pancreatic cancer, 6 of 12 patients achieved Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 PR and 3 of 12 patients demonstrated stable disease, for an overall 75% disease-control rate with the combination of LY3200882, gemcitabine, and nab-paclitaxel.
Conclusions:
LY3200882 as monotherapy and combination therapy was safe and well tolerated with preliminary antitumor activity observed in pancreatic cancer. Further studies to evaluate the efficacy of LY3200882 with gemcitabine and nab-paclitaxel in advanced pancreatic cancer are warranted.
Translational Relevance.
This phase I multicenter trial provides novel insights into the safety, pharmacokinetics (PK), pharmacodynamics (PD), and antitumor activity of LY3200882 as monotherapy and with standard therapies as combination therapy across cancer types. The results indicate that LY3200882, a novel, potent and selective, next-generation, small molecule inhibitor of transforming growth factor beta (TGFβ) receptor 1, is safe and well tolerated, has a robust PK-PD profile, and is associated with early signals of monotherapy antitumor activity in grade 4 glioma. Interestingly, LY3200882 demonstrated promising antitumor activity when given with gemcitabine and nab-paclitaxel chemotherapy in treatment-naïve patients with advanced pancreatic cancer. This study provides supporting clinical evidence to further investigate the efficacy of LY3200882 with gemcitabine and nab-paclitaxel in patients with advanced pancreatic cancer, an area of urgent clinical need.
Introduction
Transforming growth factor beta (TGFβ) is a multifunctional cytokine involved in cell growth, differentiation, migration, and survival. It is pivotal for embryogenesis and maintaining tissue homeostasis (1–3). Nonetheless, TGFβ demonstrates paradoxical activity in cancer (2). During early stages of cancer, TGFβ inhibits tumor progression through increased apoptosis, decreased cell proliferation, and reduced expression of growth factors, whereas, during late stages, TGFβ enhances tumor progression by promoting epithelial–mesenchymal transition and tumor angiogenesis, invasion, and metastasis (4, 5). Moreover, during tumor progression, TGFβ suppresses immune surveillance by either diminishing the antitumor functions of CD8+, CD4+, and dendritic cells, or by inhibiting natural killer cells from producing IFNγ (6), which suggests potential for immunomodulatory therapeutic options. Additionally, cancer-associated fibroblasts (CAF) express high levels of TGFβ that suppresses and prevents infiltration of CD8+ T cells into the tumor (7, 8). The CAFs are involved in the remodeling of the extracellular matrix during tumorigenesis and cause a stromal-rich immunosuppressive environment, a common feature of cold tumors such as pancreatic cancer and colorectal cancer (7, 8). Combining TGFβ blockade with immune potentiators such as checkpoint inhibitors may induce antitumor killing in stromal-rich tumors generally not responsive to checkpoint inhibitors alone (9).
Deregulation of TGFβ signaling is observed in multiple cancers, including pancreatic cancer, grade 4 glioma, and squamous cell carcinoma of the head and neck (HNSCC; refs. 10–13). In glioma, TGFβ is overexpressed compared with normal brain tissue, indicating a role in the development of these tumors. TGFβ enhances the production of platelet-derived cell growth factor, thereby inducing cell proliferation (14). Further, TGFβ type 1 produced by glioma-infiltrating macrophages enhances the invasive properties of cancer cells (14). Among several tumor types, TGFβ has a particularly relevant role in pancreatic cancer with the signal transduction pathway commonly mutated in this disease, as confirmed in recent whole-genome or exome sequencing analyses (15). In HNSCC, increased expression promotes cell proliferation and inhibits apoptosis (16). Apart from enhancing tumorigenesis, abnormal TGFβ signaling may promote radioresistance and immune evasion, thereby leading to poor prognosis and cancer recurrence (10, 12). Moreover, preclinical studies have demonstrated reduced DNA damage, increased clonogenic cell death, and tumor-growth delay when TGFβ was inhibited before radiotherapy (17).
The therapeutic efficacy of the pharmacologic inhibition of the TGFβ canonical Smad-dependent pathway in preclinical models of pancreatic cancer was demonstrated by using galunisertib (LY2109761, Eli Lilly and Company), a selective small molecule inhibitor of TGFβ receptor type-1 (TGFβR1; ref. 18). The results of the preclinical studies prompted the clinical investigation of the inhibition of TGFβ signaling in combination with chemo- or immunotherapeutic agents as a treatment strategy for patients with pancreatic cancer, and indicated an improvement in overall survival (OS) in combination with gemcitabine in this subset of patients (18–20).
This study introduces, for the first time, LY3200882, a novel, selective, next-generation small molecule inhibitor of TGFβR1. LY3200882 is an adenosine triphosphate–competitive inhibitor of the serine-threonine kinase domain of TGFβR1. It has a different chemical structure than galunisertib and was designed to be more potent and selective for TGFβR1 (21). Preclinical studies demonstrated LY3200882 to be superior to galunisertib from pharmacokinetic (PK), pharmacodynamic (PD), and toxicology perspectives (Data on file). LY3200882 induced durable tumor regression in orthotopic syngenic 4T1-luciferase–positive preclinical tumor models of triple-negative breast cancer in vitro and in vivo (17). LY3200882 also demonstrated immunomodulatory effects through the induction of T-cell proliferation (21). Furthermore, the combination of the antiprogrammed death ligand-1 (PD-L1) inhibitor LY3300054 and LY3200882 demonstrated antitumor activity in syngeneic CT26 models (21). Given these immunomodulatory effects observed in preclinical studies, we hypothesized that LY3200882 induces antitumor killing as monotherapy or with the PD-L1 inhibitor LY3300054 in indications such as gliomas that have been generally refractory to immune checkpoint blockade. Additionally, considering the pleotropic role TGFβ exhibits in cell signaling, we set out to test whether combination treatment with standard cytotoxic chemotherapy agents in pancreatic cancer and HNSCC will improve response rates. This first-in-human phase I trial was conducted to determine the safety, tolerability, recommended phase II dose (RP2D), PK, PD, and preliminary antitumor activity of LY3200882 as monotherapy or with other anticancer agents as combination therapy for the treatment of patients with advanced cancer.
Patients and Methods
Study design
The study was a first-in-human, multicenter, nonrandomized, open-label, phase I study of oral LY3200882 (NCT02937272). The primary objectives of the study were to assess the safety and tolerability and to establish a RP2D of LY3200882 monotherapy and with other anticancer agents as combination therapy in patients with advanced or metastatic cancers. The secondary objectives included evaluation of PK (5- to 50-mg range), PD, and preliminary antitumor activity of LY3200882 as monotherapy or in combination with other anticancer agents. The study was comprised of three parts: LY3200882 monotherapy dose escalation in patients with advanced or metastatic cancer (part A), monotherapy dose expansion in patients with grade 4 glioma (part B), and LY3200882 combination therapies in advanced cancers including grade 4 glioma, pancreatic cancer, and HNSCC (part C; Supplementary Fig. S1).
Dose escalation was assessed using two dosing schedules. In schedule A, LY3200882 was administered orally twice daily for 2 weeks followed by a treatment break for 2 weeks with a 2-weeks-on/2-weeks-off dose schedule (2w/2w). In schedule B, LY3200882 was administered orally twice a day for 3 weeks followed by a treatment break for 1 week with a 3-weeks-on/1-week-off dose schedule (3w/1w). During dose escalation, each treatment arm and dose level group comprised at least 3 patients who were evaluable for dose-limiting toxicity assessment. A 3+3 dose-escalation trial design was utilized and guided by safety, tolerability, and PK data (21). In the dose-expansion monotherapy arm, safety, tolerability, PD, and preliminary efficacy of the RP2D of LY3200882 were evaluated in patients with isocitrate dehydrogenase (IDH) 1- or 2–mutant or IDH wild-type (WT) grade 4 glioma.
In the combination dose-escalation arm, the safety, tolerability, PD, and preliminary antitumor activity of the RP2D of LY3200882 were determined in combination with the PD-L1 inhibitor LY3300054 in patients with advanced solid tumors (Combination arm C1), in combination with gemcitabine and nab-paclitaxel in treatment-naïve patients with pancreatic cancer (Combination arm C2), and in combination with cisplatin and radiation therapy in treatment-naïve patients with HNSCC (Combination arm C3). Details of each dose-schedule regimen and route of administration are provided in Supplementary Table S1. After completing the monotherapy arm of the trial, the study was terminated early due to a lack of substantial efficacy in patients with advanced glioblastoma. Hence the subsequent combination arms of the trial were not fully enrolled and evaluated.
Patients and methods
Inclusion criteria
Patients at least 18 years of age, with adequate organ function, an estimated life expectancy of ≥12 weeks, and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1 (22) were eligible for the study. In the monotherapy dose-escalation arm, patients with histologic or cytologic evidence of advanced or metastatic cancer who failed to benefit from standard therapies were included. In the monotherapy dose-expansion arm, eligible patients had a known histologically-confirmed diagnosis of either recurrent IDH mutant or IDH WT grade 4 glioma (23, 24). In the combination arms, patients were required to have a confirmed diagnosis of advanced cancers (arm C1), metastatic pancreatic cancer (arm C2), or locoregionally advanced HNSCC (arm C3). Patients enrolled in arms C2 and C3 were treatment naïve.
Exclusion criteria
All patients with elevated cardiac enzymes, moderate or severe cardiovascular disease, secondary malignancy, diffuse leptomeningeal disease, esophageal or gastric varices with high bleeding risk, acute leukemia, or a history of hypersensitivity to study drug components were excluded. Patients who had received radiotherapy within 2 weeks of enrollment or any systemic treatment within the past 28 days were also excluded from the study. Further, patients with active or suspected autoimmune disease and those receiving systemic steroids were excluded from receiving the combination of LY3200882 and LY3300054.
This study was conducted in accordance with the International Conference on Harmonisation requirements for Good Clinical Practice and with the consensus ethics principles derived from the International Ethics Guidelines, outlined in the Declaration of Helsinki and Council for International Organizations of Medical Sciences (25). All patients provided written informed consent before study enrollment.
Study assessments
Patients who received at least 1 dose of LY3200882 or any of the combination drugs were evaluated for safety, tolerability, PK, PD, and preliminary efficacy profiles. Safety was determined by the NCI Common Terminology Criteria for Adverse Events (CTCAE) v 4.03 (26). Additionally, investigators assessed whether adverse events (AE) were study-treatment related or caused by other factors. Plasma samples for PK analyses were assayed using a validated liquid chromatography/tandem mass spectrometry method (Covance Bioanalytical Service). Maximum observed concentration (Cmax), time of Cmax (tmax), AUC, apparent clearance (CL/F), and volume of distribution (V/F) were estimated. Langerhans cell (LC; langerin-specific clone 12D6) quantification was performed using an IHC assay using skin biopsy samples collected at baseline and on treatment as a PD surrogate marker for the TGFβ pathway (NeoGenomics Laboratories Inc). Overall response rate [(ORR); complete response (CR)/partial response (PR)], OS, and progression-free survival (PFS) were assessed by Response Evaluation Criteria in Solid Tumors (RECIST) v 1.1 for solid tumors and Revised Assessment in Neuro Oncology (RANO) criteria for gliomas (23). Disease assessment was performed using CT or MRI at baseline and between days 22 to 28 of every other cycle until confirmed progressive disease or patient withdrawal from the study.
Statistical analyses
All patients who received any dose of the study treatment were included in the safety and efficacy analyses. Clinical data including demographics, baseline characteristics, safety, and efficacy was analyzed using SAS 9.4 software (SAS Institute Inc.). For safety analyses, the frequency and percentage of patients with AEs were presented for each arm of the study. PK parameter estimates were analyzed using noncompartmental procedures with Phoenix WinNolin v64 build 8.1 software (Certara) and log-transformed Cmax and AUC estimates were assessed using a power model with dose as a fixed effect. Best overall response per RECIST v1.1 with confirmation on CR and PR were represented by frequency. PFS and OS were analyzed using the Kaplan–Meier method. PFS was defined as the time from the date of first study treatment to the first date of documented progression or death due to any cause. For patients who were not known to have died or progressed as of the cut-off dates, PFS times were censored at the date of the last progression-free disease assessment before the date of any subsequent anticancer therapy. OS was defined as the time from the date of first study treatment to the date of death from any cause. For each patient who was not known to have died as of the cut-off date, OS data were censored for that analysis at the date of last contact before the data inclusion cut-off date.
Results
Patient disposition and demographic characteristics
Overall, 180 patients were enrolled, of which 139 (77.2%) patients were nonrandomly assigned to study treatment and received at least 1 dose of the study drug. At the time of data cut-off (March 2020), 131 (94.2%) patients had discontinued trial treatment with most patients discontinuing the study because of progressive disease. A total of 62 patients received escalating doses of LY3200882 as monotherapy for 2w/2w (n = 30) and 3w/1w (n = 32) over a 28-day cycle in the dose-escalation arm. In the dose-expansion arm, 40 patients with grade 4 glioma (IDH WT grade 4 glioma or glioblastoma, n = 25; IDH mutant n = 15) were treated with the RP2D-selected 50 mg twice a day for the 2w/2w schedule. A total of 28 patients with advanced cancer, pancreatic cancer, or HNSCC in the combination arms were treated with the RP2D and other anticancer agents. Patient disposition is summarized in Supplementary Fig. S1.
Most patients enrolled in the dose-escalation arm were heavily pretreated with a median of 3 (0–8) prior systemic lines, whereas patients in the expansion arm with grade 4 glioma were treated with a median of 1 (1–5) prior systemic therapy. Patients in the combination arms were treated with a median of 1 (0–7) prior systemic therapy (Table 1). Patients with advanced cancer treated in combination with LY3300054 were treated with a median of 2 (1–7) prior systemic therapies. Patients with pancreatic cancer treated in combination with gemcitabine and nab-paclitaxel and patients with HNSCC treated in combination with cisplatin and radiation therapy were treatment naïve.
Table 1.
Baseline demographics and participant characteristics.
| LY3200882 in a 2w/2w schedule | LY3200882 in a 3w/1w schedule | Grade 4 glioma treated with RP2D dose from dose-expansion arm in a 2w/2w schedule | Advanced cancer treated with LY3200882 +PD-L1 inhibitor LY3300054 | Pancreatic cancer with LY3200882 +gemcitabine +nab-paclitaxel | HNSCC treated with LY3200882 +cisplatin +radiation therapy | Japanese cohort | |
|---|---|---|---|---|---|---|---|
| Parameter | Dose-escalation arm; schedule A (N = 30) | Dose-escalation arm; schedule B (N = 32) | Dose-expansion arm (N = 40) | Combination arm C1 (N = 13) | Combination arm C2 (N = 12) | Combination arm C3 (N = 3) | (N = 9) |
| Sex, n (%) | |||||||
| Male | 19 (63.3) | 26 (81.3) | 24 (60.0) | 8 (61.5) | 10 (58.3) | 3 (100.0) | 5 (55.6) |
| Female | 11 (36.7) | 6 (18.8) | 16 (40.0) | 5 (38.5) | 5 (41.7) | 0 (0.0) | 4 (44.4) |
| Age, years | |||||||
| Mean (SD) | 49.8 (11.5) | 49.8 (13.9) | 48.3 (12.8) | 53.2 (16.7) | 54.7 (12.6) | 51.7 (7.6) | 56.8 (12.1) |
| Baseline ECOG performance statusa, n (%) | |||||||
| 0 | 8 (26.7) | 4 (12.5) | 15 (37.5) | 3 (23.1) | 7 (58.3) | 1 (33.3) | 9 (100.0) |
| 1 | 22 (73.3) | 27 (84.4) | 25 (62.5) | 10 (76.9) | 5 (41.7) | 2 (66.7) | 0 (0.0) |
| Initial pathologic diagnosis | |||||||
| Grade 4 gliomab | 6 (20.0) | 7 (21.9) | 25 (62.5) | 2 (7.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pancreatic cancer | 3 (10.0) | 3 (9.4) | 0 (0.0) | 0 (0.0) | 12 (100.0) | 0 (0.0) | 1 (11.1) |
| HNSCCc | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 0 (0.0) |
| Prior lines of therapy, n (%) | |||||||
| ≥1 prior surgery | 25 (83.3) | 27 (84.4) | 37 (92.5) | 10 (76.9) | 5 (41.7) | 0 (0.0) | 4 (44.4) |
| ≥1 prior radiotherapy | 25 (83.3) | 25 (78.1) | 40 (100.0) | 10 (76.9) | 0 (0.0) | 1 (33.3) | 3 (33.3) |
| ≥1 prior systemic therapy | 29 (96.7) | 31 (96.9) | 40 (100.0) | 13 (100.0) | 2 (16.7) | 0 (0.0) | 9 (100.0) |
| Patients with >2 regimens | 6 (20.0) | 6 (18.8) | 7 (17.5) | 4 (30.8) | 0 (0.0) | 0 (0.0) | 1 (11.1) |
| Patients with ≥3 regimens | 22 (73.3) | 20 (62.5) | 9 (22.5) | 6 (46.2) | 0 (0.0) | 0 (0.0) | 7 (77.8) |
Abbreviations: 2w/2w, 2-weeks-on/2-weeks-off schedule; 3w/1w, 3-weeks-on/1-week-off schedule; ECOG, Eastern Cooperative Oncology Group; HNSCC, head and neck squamous cell carcinoma; N, total population; n, total number of patients in the subset; RP2D, recommended phase II dose; SD, standard deviation; US, United States.
aECOG: 0, fully active, able to carry on all predisease performance without restriction; 1, restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e.g., light housework, office work.
bGrade glioma included patients with glioblastoma, glioblastoma multiforme, IDH WT, and IDH mutant.
c1 patient from this arm had supraglottis edidermoid carcinoma.
Safety outcomes
Overall, 130 (93.5%) patients experienced ≥ 1 treatment-emergent adverse event (TEAE), with 49 (35.3%) patients experiencing grade 3 or greater TEAEs (all causality). Most AEs were either grade 1 or 2 (64.7%) with grade 3 myelosuppression only observed in combination with cytotoxic chemotherapy in patients with pancreatic cancer or HNSCC (Table 2). The most common TEAEs experienced by ≥15% patients included headache, nausea, anemia, and fatigue (Supplementary Table S2). A total of 55 (39.6%) patients experienced TEAEs that were study-treatment related. The most frequent study-related TEAEs included headache, fatigue, and increased alanine aminotransferase. No LY3200882-related cardiovascular AEs and dose-limiting toxicities were observed with LY3200882 monotherapy.
Table 2.
Summary of study treatment-related AEs with >5% frequency.
| LY3200882 in a 2w/2w schedule | LY3200882 in a 3w/1w schedule | Grade 4 glioma treated with RP2D dose from dose-expansion arm in a 2w/2w schedule | Advanced cancer treated with LY3200882 +PD-L1 inhibitor LY3300054 | Pancreatic cancer with LY3200882 +gemcitabine +nab-paclitaxel | HNSCC treated with LY3200882 +cisplatin +radiation therapy | Japanese cohort | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dose-escalation arm; schedule A (N = 30) | Dose-escalation arm; schedule B (N = 32) | Dose-expansion arm (N = 40) | Combination arm C1 (N = 13) | Combination arm C2 (N = 12) | Combination arm C3 (N = 3) | (N = 9) | ||||||||
| Preferred term | Any grade | Grade ≥3 | Any grade | Grade ≥3 | Any grade | Grade ≥3 | Any grade | Grade ≥3 | Any grade | Grade ≥3 | Any grade | Grade ≥3 | Any Grade | Grade ≥3 |
| Subjects with ≥1 TEAE related to study treatment, n (%) | 10 (33) | 0 (0) | 10 (31) | 0 (0) | 10 (25) | 0 (0) | 7 (54) | 0 (0) | 12 (100) | 6 (50) | 3 (100) | 2 (67) | 3 (33) | 0 (0) |
| Fatigue | 0 (0) | 0 (0) | 1 (3) | 0 (0) | 4 (10) | 0 (0) | 1 (8) | 0 (0) | 5 (42) | 0 (0) | 1 (33) | 0 (0) | 0 (0) | 0 (0) |
| Anemia | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 6 (50) | 1 (8) | 3 (100) | 0 (0) | 1 (11) | 0 (0) |
| ALT increased | 0 (0) | 0 (0) | 2 (6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 4 (33) | 1 (8) | 0 (0) | 0 (0) | 1 (11) | 0 (0) |
| Nausea | 1 (3) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (17) | 0 (0) | 2 (67) | 1 (33) | 1 (11) | 0 (0) |
Abbreviations: 2w/2w, 2-weeks-on/2-weeks-off schedule; 3w/1w, 3-weeks-on/1-week-off schedule; ALT, alanine aminotransferase; HNSCC, head and neck squamous cell carcinoma; N, total population; n, total number of patients in the subset; RP2D, recommended phase II dose; TEAE, treatment-emergent adverse event.
One patient with pancreatic cancer receiving LY3200882 (35 mg twice a day with the 3w/1w schedule) with gemcitabine and nab-paclitaxel experienced stage C (American College of Cardiology/American Heart Association guideline) cardiac insufficiency. At screening, the patient had a left ventricular ejection fraction (LVEF) of 70% with an unremarkable echocardiogram (ECHO) showing no kinetic or morphologic abnormalities. Patient had a history of hypertension, which was well controlled with angiotensin-converting enzyme inhibitors and beta blockers. The patient's third month on study ECHO showed that LVEF decreased to 57%, but the patient remained asymptomatic with no elevation in cardiac enzymes and the study treatment was continued. On cycle 7, day 1, patient presented with bilateral edema and dyspnea with elevated blood levels of brain natriuretic peptide (BNP; 212 pg/mL), and evidence of subclavian vein thrombosis. A subsequent ECHO revealed LVEF at 50% with total hypokinesia of the apex and the interventricular septum. Study treatment was discontinued, and high-dose diuretics and anticoagulants started. Within a week, bilateral edema was completely resolved, and dyspnea improved with BNP levels reduced to 48 pg/mL. Cardiac imaging around this time revealed myocardial inflammation. Patient was not rechallenged with gemcitabine/abraxane or other cytotoxic chemotherapy regimen. PK analysis from blood samples taken during study treatment did not reveal higher exposure levels of LY3200882 than the population median.
A total of 24 (17.3%) patients experienced at least 1 serious AE (SAE), with 3 (2.2%) patients experiencing SAEs related to study drug. The study drug–related SAEs comprised grade 2 diarrhea, grade 4 neutropenia, and grade 2 weight loss, which were observed only in the combination expansion arms. A total of 63 (45.3%) deaths were reported in the study; none were deemed to be related to study treatment.
PK
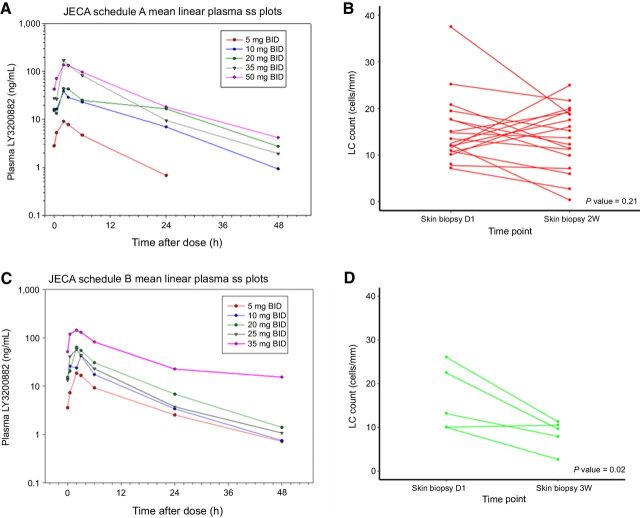
The PK profile of LY3200882 was linear with dose and time, and peak concentration was reached at 2 hours after administration (Fig. 1). The AUC increased in a dose-dependent manner in the 5- to 50-mg dose range investigated (Supplementary Fig. S2, Panel A). Furthermore, PK parameters such as CL/F, V/F, and half-life (t1/2) were constant over time (Supplementary Fig. S2, Panel B), indicating that the LY3200882 PK was independent of the schedule of administration. After reaching maximum LY3200882 concentration, the PK disposition was characterized by a mean CL/F, V/F, and associated t1/2 of 57.3 L/hour, 559 L, and 6.7 hours, respectively. The highest RP2D selected was 50 mg twice a day 2w/2w (schedule A), which achieved the highest exposure among doses tested, and was below the no-observed-adverse-effect level (NOAEL) for cardiotoxicity (3.4 mg X hours/L) determined from nonclinical toxicology studies. Based on the short t1/2, steady state of the drug would be achieved after 2 doses with a 1.4-fold accumulation ratio. These data suggest that LY3200882 is neither an inhibitor nor an inducer of its own metabolism.
Figure 1.
LY3200882 PK concentration versus time profiles at steady state (ss) for the different dosing regimens (panels A and C) and corresponding LC density skin-biopsy data posttreatment (panels B and D). A, PK profiles for arms treated by 50 mg 2w/2w. B, Positive LC count at day 1 and day 14 of patients in the dose-escalation arm treated using the 50 mg 2w/2w. C, PK profiles for arms treated with 3w/1w. D, Positive LC count at day 1 and day 21 of patients in dose-escalation arm treated with 35 mg 3w/1w. BID, twice a day; h, hour; ss, steady state; W, weeks.
PD
Skin LC density was used as a novel surrogate PD biomarker for TGFβ pathway inhibition in this study. Skin biopsies were collected from a subset of patients at baseline before initiating treatment and at day 14 or day 21 for the 2w/2w or 3w/1w dose schedules, respectively. Skin LCs decreased significantly in skin biopsies with LY3200882 monotherapy at 35 mg for 3w/1w (n = 5; P = 0.02), but not in patients treated with LY3200882 monotherapy at 25 mg 3w/1w (n = 7; P = 0.82; Supplementary Fig. S3) or 50 mg 2w/2w (n = 18; P = 0.21; Fig. 1).
Antitumor outcomes
Assessment of the tumor response of LY3200882 indicated that 41 of 139 (29.5%) patients demonstrated either RECIST v1.1 or RANO CR, PR, or stable disease (SD).
LY3200882 monotherapy
Dose-escalation arm (n = 62):
Two patients with grade 4 glioma, of which 1 with IDH WT treated on the 2w/2w schedule and 1 patient with IDH 1–mutant on the 3w/1w schedule, achieved PR according to RANO criteria. The duration of response for the 2 patients was 19 months and 3.9 months on the 2w/2w and 3w/1w schedule, respectively.
The ORR of LY3200882 monotherapy was 3% (2/62) for both schedules combined. The disease control rate (DCR; CR/PR/SD) was 23% (7/30) with the 2w/2w schedule and 25% (8/32) with the 3w/1w schedule (Table 3). The median PFS for patients with advanced cancers treated with the 50 mg twice a day 2w/2w (n = 17) was 1.8 months [95% confidence interval (CI), 0.9–2.0] and for patients on the 35 mg twice a day 3w/1w dose schedule (n = 8) was 1.7 months (95% CI, 0.8–2.6). The median OS for the 17 patients treated with LY3200882 50 mg twice a day 2w/2w schedule was 6.1 months (95% CI, 1.2–11.4), while the median OS of 8 patients treated with 35 mg twice a day 3w/1w schedule of LY3200882 was 4.0 months [95% CI 2.6–Nonevaluable (NE)].
Table 3.
Summary of confirmed best overall response.
| LY3200882 in a 2w/2w schedule | LY3200882 in a 3w/1w schedule | Grade 4 glioma treated with RP2D dose from dose-expansion arm in a 2w/2w schedule | Advanced cancer treated with LY3200882 +PD-L1 inhibitor LY3300054 | Pancreatic cancer with LY3200882 +gemcitabine +nab-paclitaxel | HNSCC treated with LY3200882 +cisplatin +radiation therapy | Japanese cohort | |
|---|---|---|---|---|---|---|---|
| Dose-escalation arm; schedule A (N = 30) | Dose-escalation arm; schedule B (N = 32) | Dose-expansion arm (N = 40) | Combination arm C1 (N = 13) | Combination arm C2 (N = 12) | Combination arm C3 (N = 3) | (N = 9) | |
| Radiologic efficacy parametersa | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) |
| Best overall response | |||||||
| CR | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33) | 0 (0) |
| PR | 1 (3) | 1 (3) | 1 (3) | 1 (8) | 6 (50) | 0 (0) | 0 (0) |
| SD | 6 (20) | 7 (22) | 6 (15) | 4 (31) | 3 (25) | 2 (67) | 0 (0) |
| Progressive disease | 15 (50) | 20 (63) | 26 (65) | 7 (54) | 3 (25) | 0 (0) | 8 (89) |
| Nonevaluable | 8 (27) | 4 (13) | 7 (18) | 1 (8) | 0 (0) | 0 (0) | 1 (11) |
| ORR (CR/PR) | 1 (3) | 1 (3) | 1 (3) | 1 (8) | 6 (50) | 1 (33) | 0 (0) |
| DCR (CR/PR/SD) | 7 (23) | 8 (25) | 7 (18) | 5 (39) | 9 (75) | 3 (100) | 0 (0) |
Abbreviations: 2w/2w, 2-weeks-on/2-weeks-off dose schedule; 3w/1w, 3-weeks-on/1-week-off dose schedule; CR, complete response; N, total population; n, total number of patients in the subset; PR, partial response; RANO, Revised Assessment in Neuro Oncology; RECIST, Response Evaluation Criteria in Solid Tumors v 1.1; RP2D, recommended phase II dose; SD, stable disease.
aRadiologic assessment using RECIST v1.1 or RANO criteria depending on respective tumor type.
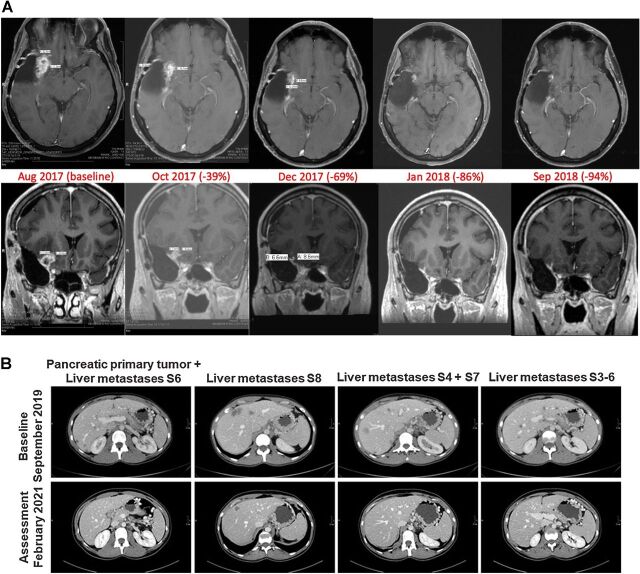
Although no objective response was observed in patients in either group, individual patients showed exceptional clinical benefit. A 53-year-old male diagnosed with IDH WT grade 4 glioma with EGFR P772_V774dupPHV mutation, CDK4 amplification, and methylated MGMT promoter gene enrolled to this study after multiple tumor resections and no clinical benefit with concurrent radiotherapy and chemotherapy, including temozolomide and lomustine. He had a 94% tumor reduction by RANO assessment on LY3200882 monotherapy at 50 mg twice a day (2w/2w schedule), with no clinical toxicities and remained on trial 30.4 months (Fig. 2A). A second patient with IDH 1–mutant grade 4 glioma with EGFRvIII mutation, EGFR amplification, TERT mutation, homozygous deletions of CDKN2A and B, PIK3CA mutation, and CCND2 duplication achieved a RANO PR while on study treatment. The MRI showed a decline in the sum of the perpendicular products of the target lesions from 130 mm2 to 30 mm2 from baseline MRI in December 2018 to follow up in April 2019. The patient remained in PR until October 2019 when study treatment was discontinued due to new brain lesions. The patient received subsequent investigational treatment of a bispecific T-cell engager targeting EGFRVIII, followed by tumor resection, radiotherapy (30 Gy in 10 fractions) and restart of temozolomide; however, no clinical benefit was observed with these therapies. Considering their prior response to treatment, the patient was granted compassionate access use in August 2020 to LY3200882 which was administered as 50 mg twice a day 2w/2w monotherapy, with disease stabilization and patient benefit, and treatment is still ongoing.
Figure 2.
A, MRI images of a 53-year-old male diagnosed with IDH WT grade 4 glioma with EGFR P772_V774dupPHV mutation, CDK4 amplification, and methylated MGMT promoter gene enrolled to this study after multiple tumor resections and no clinical benefit with concurrent radiotherapy and chemotherapy, including temozolomide and lomustine. He had a 94% tumor reduction by RANO assessment on LY3200882 monotherapy at 50 mg twice a day (2w/2w schedule), with no clinical toxicities, and remained on trial approximately 2 years. B, CT scans of patient with pancreatic cancer, after 18 months of treatment with LY3200882+gemcitabine+nab-paclitaxel. A complete response of liver metastases in S6, S4 and 7, and S3–6 was achieved. Primary pancreatic tumor obtained a 40% reduction of its longest diameter. Liver metastasis in S8 achieved a 58% reduction of its longest diameter.
Recurrent IDH mutant and IDH WT grade 4 glioma dose-expansion arm (n = 40):
One patient with IDH WT grade 4 glioma treated with 50 mg twice a day 2w/2w achieved PR according to RANO criteria. The duration of response for this patient was 5.6 months. The ORR and DCR for the dose-expansion arm were 3% (1/40) and 18% (7/40), respectively (Table 3). The median PFS was also similar between both groups of patients: IDH WT glioblastoma 1.6 months (95% CI, 0.9–5.5) and IDH mutant 1.7 months (95% CI, 1.3–1.8). The median OS of 15 patients with recurrent IDH mutant and 25 patients with IDH WT grade 4 glioma was 10.6 months (95% CI, 7.3–NE) and 8.2 months (95% CI, 4.6–9.7), respectively.
LY3200882 in combination with other anticancer agents
LY3200882 and PD-L1 inhibitor LY3300054 (n = 13):
A total of 13 patients with advanced cancer were treated with the combination of LY3200882 and PD-L1 inhibitor LY3300054. One patient with IDH WT grade 4 glioma achieved a PR per RANO for 5.6 months (Table 3). ORR and DCR for the combination therapy arm were 7.7% (1/13) and 39% (5/13), respectively. OS or PFS were not calculated due to the small sample size for this group.
LY3200882, gemcitabine, and nab-paclitaxel (n = 12):
Six (50%) of 12 patients with treatment-naïve advanced pancreatic cancer achieved confirmed RECIST v1.1 PRs, with all but 1 patient demonstrating tumor target-lesion shrinkage, when treated with the combination of LY3200882, gemcitabine, and nab-paclitaxel. One additional patient had an unconfirmed PR. Notably, the ORR and DCR were 50% (6/12) and 75% (9/12), respectively (Table 3; Fig. 3). The median duration of response for patients with pancreatic cancer treated with LY3200882+gemcitabine+nab-paclitaxel was 4.0 months. CA19-9 levels decreased by greater than 50% in 8 of the 12 patients.
Figure 3.
Best overall response of patients with treatment-naïve advanced pancreatic cancer.
An exceptional response was observed in a 36-year-old woman diagnosed with an adenocarcinoma of the tail of the pancreas with multiple and diffuse secondary liver lesions and an ECOG performance status of 1. Molecular profiling was not performed on tumor tissue obtained at diagnosis in this patient and therefore the presence of any oncogenic drivers or other genetic aberrations is unknown. The patient had an early RECIST v1.1 response of PR of both the primary pancreatic and secondary liver lesions; however, because of grade 3 myelotoxicity, the doses of gemcitabine and nab-paclitaxel were reduced. The patient had to be switched to a biweekly schedule for chemotherapy administration, while keeping LY3200882 dose and schedule unchanged. After 18 months of starting study treatment, the patient continues to have a RECIST v1.1 PR, with no cumulative toxicities and an ECOG PS of 0 (Fig. 2B).
LY3200882, cisplatin, and radiotherapy (n = 3):
One patient achieved a RECIST v1.1 CR. The other 2 patients in this group achieved RECIST v1.1 SD. ORR and DCR for the combination therapy arm were 33.3% (1/3) and 100% (3/3), respectively. Because of the small sample size, PFS and OS data were not calculated.
Discussion
This first-in-human phase I study demonstrated the safety and potential efficacy of LY3200882, a next-generation oral TGFβR1 small molecule inhibitor as monotherapy for the treatment of recurrent grade 4 glioma and in combination with other anticancer agents for the treatment of advanced solid tumors, including pancreatic cancer. In the present study, treatment with LY3200882 as both monotherapy and in combination with other antitumor agents was well tolerated with mainly mild to moderate TEAEs. The RP2Ds selected were 50 mg twice a day for the 2w/2w schedule and 35 mg twice a day for the 3w/1w schedule, respectively. In the overall study population that was comprised of a large proportion of patients with relapsed grade 4 glioma, a DCR of 28.1% was observed. Durable RANO PRs were observed in 3 patients treated with LY3200882 monotherapy (2 patients with IDH WT and 1 patient with IDH mutant grade 4 glioma) at 50 mg twice a day 2w/2w and 35 mg twice a day 3w/1w, respectively and 1 patient with IDH WT grade 4 glioma treated with LY3200882 and PD-L1 inhibitor LY3300054 combination. Six of 12 patients with pancreatic cancer treated with LY3200882, gemcitabine, and nab-paclitaxel and 1 patient with HNSCC treated with LY3200882, cisplatin, and radiation therapy had RECIST v1.1 PRs and CR, respectively.
The majority of TEAEs observed with LY3200882 were not considered related to study treatment; TEAEs considered to be treatment-related were mild or moderate in severity, manageable with supportive care, and reversible. Of note, a key concern with the development of TGFβ inhibitors has been the potential for cardiotoxicity based on preclinical toxicology studies (6). Overall, no cardiovascular AEs were observed in patients receiving LY3200882 as monotherapy. We only observed 1 case of treatment-related cardiac toxicity in a patient with pancreatic cancer receiving LY3200882 in combination with gemcitabine and nab-paclitaxel chemotherapy in the form of decreased ejection fraction, hypokinesia of the interventricular septum, and myocardial inflammation leading to discontinuation after 7 cycles. However, it was not clear if the toxicity was related to LY3200882 or to gemcitabine and nab-paclitaxel chemotherapy treatment. Overall, the lack of observed cardiovascular toxicity and general tolerability either as single agent or in combination therapy of LY3200882 is similar to the small molecule TGFβR1 inhibitor galunisertib (19, 27–29). The NOAEL daily AUC threshold values for cardiotoxicity established preclinically in rats and dogs for 2w/2w and 3w/1w schedules were 3.4 and 1.56 mg X h/L, respectively. The AUC achieved following the LY3200882 RP2D of 50 mg twice a day in 2w/2w and 35 mg twice a day in 3w/1w were within the planned daily AUC range and remained below the established NOAEL daily AUC threshold for cardiotoxicity.
Several biomarkers were evaluated in this study to interrogate if we were able to modulate the TGFβ pathway. TGFβ is an important immune regulator and highly expressed in skin LCs (30), and therefore LC assessment was performed as a novel surrogate PD marker in this study since inhibition of TGFβ signaling leads to LC migration out of the epidermis (31). Our study demonstrated a significant decrease in LC cells with the 35 mg 3w/1w dose-schedule regimen of LY3200882, while no significant difference was observed for the 50 mg 2w/2w and 25 mg 3w/1w dose schedules, although general trends downwards were observed. The difference of LC migration between the 2w/2w and 3w/1w schedules may suggest that a more sustained inhibition of TGFβ may be required to achieve a more complete targeted inhibition of the pathway. Alternatively, because of the different dosing interval, the on-treatment skin biopsy for the 2w/2w schedule was performed at 2 weeks and the 3w/1w at 3 weeks. Hence, the observed difference in PD effects may be associated with the time needed for LCs to migrate out of the skin. This temporal difference likely explains the lack of change in cell density observed with the 50 mg twice a day 2w/2w dose schedule despite being treated with a higher dose of LY3200882 compared with the 35 mg twice a day 3w/1w dose schedule. However, the difference between the 35 mg 3w/1w and the 25 mg 3w/1w dose schedules on LC migration suggests a dose-dependent response with a higher dose more effectively blocking the TGFβ pathway. Additionally, phosphorylated SMAD levels were assessed from 9 dose-escalation paired tumor biopsies collected 1 or 2 weeks after the last treatment of cycle 1; however, as these samples represent multiple treatment-dose levels, collection time post last treatment (1 or 2 weeks), and tumor histology, we were not able to collect sufficient data to draw any conclusions.
Of a total of 139 patients, 11 patients achieved radiologic CR/PR and 28 patients had SD with LY3200882-based therapies. A subset of patients with grade 4 glioma (n = 2) had tumor reduction that did not meet response criteria for RANO response but showed SD for durable disease stabilization of over 6 months.
Interestingly, 6 (50%) of 12 patients with treatment-naïve advanced pancreatic cancer demonstrated confirmed RECIST PRs, with all but 1 patient demonstrating tumor target-lesion shrinkage, and an overall DCR of 75% with LY3200882 in combination with gemcitabine and nab-paclitaxel. In addition, 8 of these 12 patients had significant declines in their CA19-9 levels. Although observed in a small sample size (n = 12), these early clinical data compare favorably with the ORR of 23% determined in the registered trial of gemcitabine plus nab-paclitaxel or 31.6% with FOLFIRINOX in patients with treatment-naïve advanced pancreatic cancer (32, 33). The ORR observed with LY3200882 with gemcitabine and nab-paclitaxel in our study was similar to that observed with the ongoing trial evaluating gemcitabine and nab-paclitaxel in combination with a CD40 agonist and nivolumab, also given in first-line pancreatic cancer (34). These data may suggest that targeting the immune axis with T-cell boosters or mechanisms that reverse immune suppression in pancreatic cancer may result in tumor T-cell infiltration and antitumor activity. Unfortunately, because our trial lacked paired biopsies, we were unable to evaluate immune-cell population changes in the tumor. Earlier studies with the first-generation TGFβR1 inhibitor galunisertib with gemcitabine also showed improved ORR (10.8% vs. 3.8%) and DCR (58.7% vs. 51.9%) when compared with single-agent gemcitabine (19, 29).
Early-onset (<50 years) pancreatic cancer accounts for nearly 5% of the total patients with this malignancy. A 2019 transcriptomic analysis comparing the molecular landscape of early-onset and average-age onset pancreatic cancer revealed increased activation of the TGFβ pathway in younger patients who do not respond well to combination chemotherapy regimens. Given these recent data, efforts were made to enrich our patient population with younger patients. The median age of patients with pancreatic cancer in our trial was 56 years, lower than the expected median age for pancreatic cancer, which is around 70 years in the United States and the Western world.
In conclusion, LY3200882 was safe as monotherapy and well tolerated in combination with the PD-L1 inhibitor LY3300054, chemotherapy, and radiotherapy, with most TEAEs considered to be mild, manageable, and reversible. The selected RP2D using the 2w/2w and 3w/1w schedules were identified as 50 mg and 35 mg twice a day, respectively. Dose-limiting toxicities were not observed with either schedule, and the exposure levels of the selected doses were within the planned daily AUC range and below the established NOAEL daily AUC threshold for cardiotoxicity. Notably, promising antitumor activity was observed in patients with treatment-naïve advanced pancreatic cancer with LY3200882 in combination with gemcitabine and nab-paclitaxel. The patients enrolled to this study with pancreatic cancer were younger with a median age of 56 years; it is plausible that this hard-to-treat patient population may benefit from combination treatment including TGFβ inhibitors, warranting further studies to evaluate the efficacy of this combination.
Authors' Disclosures
T.A. Yap reports grants from Eli Lilly during the conduct of the study. T.A. Yap also reports grants from Artios, Constellation, Cyteir, Forbius, GlaxoSmithKline, Genentech, ImmuneSensor, Ipsen, Jounce, Karyopharm, Kyowa, Ribon Therapeutics, Regeneron, Sanofi, Scholar Rock, Tesaro, Vertex Pharmaceuticals, and Novartis; grants and personal fees from AstraZeneca, Bayer, Clovis, EMD Serono, F-Star, Merck, Pfizer, Repare, and Seattle Genetics; and personal fees from Almac, Aduro, Atrin, Axiom, Bristol Myers Squibb, Calithera, Cybrexa, Guidepoint, Ignyta, I-Mab, Janssen, Roche, Rubius, Schrodinger, Varian, and Zai Labs outside the submitted work. M. Vieito reports personal fees from Roche, EMD Serono, and TFS outside the submitted work. S. Kondo reports other support from Eli Lilly during the conduct of the study; S. Kondo also reports personal fees from Chugai, as well as other support from Incyte and Eisai outside the submitted work. V. Atkinson reports personal fees and non-financial support from BMS, as well as personal fees from MSD, NEKTAR, Novartis, Pierre Fabre, Q Biotic, and Roche outside the submitted work. A.F. Carpentier reports grants from Lilly during the conduct of the study; A.F. Carpentier also reports non-financial support from Altevax, as well as personal fees from BMS outside the submitted work. R. Redman reports other support from Merck, Daiichi Sankyo, Pfizer, Iovance, Rgenix, Debiopharm, Immunovaccine Technologies, RAPT Therapeutics, and Bristol Myers Squibb outside the submitted work. A. Cervantes reports grants from Elly Lilly and Company during the conduct of the study. E. Le Rhun reports personal fees from AbbVie, Adastra, Bayer, Leo Pharma, Seattle Genetics, and Tocagen outside the submitted work. S. Ochsenreither reports personal fees from MSD, BMS, AstraZeneca, Merck, and Ipsen outside the submitted work. S. Callies reports other support from Eli Lilly and Company outside the submitted work. M. Man is an employee and stock owner at Eli Lilly and Company. L. Gandhi reports other support from Eli Lilly and Company during the conduct of the study, and was an employee of Eli Lilly and Company during completion of this work. E. Avsar reports other support from Eli Lilly and Company during the conduct of the study, as well as other support from Eli Lilly and Company outside the submitted work; in addition, E. Avsar is a full-time employee of Eli Lilly and Company and works for the pharmaceutical industry as a drug developer. D. Melisi reports grants and personal fees from Incyte Corporation, Evotec, and iOnctura; grants from Shire and Celgene; and personal fees from Baxter outside the submitted work. No disclosures were reported by the other authors.
Supplementary Material
Supplementary Legend
Dosing and administration information
All causality TEAEs
Patient disposition
LY3200882 pharmacokinetics parameters
Line graph of langerhan skin biopsy
Acknowledgments
This work was supported by grants from Eli Lilly and Company. We would like to thank Dan Kaplan for his consulting role on the pharmacodynamic assays and Shuaicheng Freeman Wang for his support. We would like to thank Collin Miles for his extensive contribution to the pharmacokinetics analysis. We would like to thank Shaleen Multani, an employee of Eli Lilly Services India Private Limited for providing writing support. T.A. Yap acknowledges the MD Anderson Cancer Center for support grant P30 CA016672 and the Sheikh Khalifa Bin Zayed Al Nahyan Institute for Personalized Cancer Therapy at the MD Anderson Cancer Center for support grant 1U01 CA180964. Work in the unit of D. Melisi was partially supported by the Associazione Italiana per la Ricerca sul Cancro (AIRC) Investigator Grant no. 23719 and 5 × 1000 Grant no. 12182, by the Italian Ministry of Health Ricerca Finalizzata 2016 GR-2016- 02361134 grant, by the patients' associations “Nastro Viola” and “Voglio il Massimo” donations.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
This article is featured in Highlights of This Issue, p. 6617
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Contributions
T.A. Yap: Conceptualization, investigation, writing–review and editing. M. Vieito: Investigation, writing–review and editing. C. Baldini: Investigation, writing–review and editing. J.M. Sepúlveda-Sánchez: Investigation, writing–review and editing. S. Kondo: Investigation, writing–review and editing. M. Simonelli: Investigation, writing–review and editing. R. Cosman: Investigation, writing–review and editing. A. van der Westhuizen: Investigation, writing–review and editing. V. Atkinson: Investigation, writing–review and editing. A.F. Carpentier: Investigation, writing–review and editing. M. Löhr: Investigation, writing–review and editing. R. Redman: Investigation, writing–review and editing. W. Mason: Investigation, writing–review and editing. A. Cervantes: Investigation, writing–review and editing. E. Le Rhun: Investigation, writing–review and editing. S. Ochsenreither: Investigation, writing–review and editing. L. Warren: Conceptualization, investigation, writing–review and editing. Y. Zhao: Formal analysis, methodology, writing–review and editing. S. Callies: Formal analysis, methodology, writing–review and editing. S.T. Estrem: Formal analysis, methodology, writing–review and editing. M. Man: Formal analysis, methodology, writing–review and editing. L. Gandhi: Conceptualization, writing–review and editing. E. Avsar: Conceptualization, writing–review and editing. D. Melisi: Conceptualization, investigation, writing–review and editing.
References
- 1. Nickel J, ten Dijke P, Mueller TD. TGFβ family co-receptor function and signaling. Acta Biochim Biophys Sin 2017;50:12–36. [DOI] [PubMed] [Google Scholar]
- 2. Haque S, Morris JC. Transforming growth factor-β: a therapeutic target for cancer. Hum Vaccin Immunother 2017;13:1741–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Colak S, Ten Dijke P. Targeting TGF-beta signaling in cancer. Trends Cancer 2017;3:56–71. [DOI] [PubMed] [Google Scholar]
- 4. Chen Y, Di C, Zhang X, Wang J, Wang F, Yan JF, et al. Transforming growth factor beta signaling pathway: a promising therapeutic target for cancer. J Cell Physiol 2020;235:1903–14. [DOI] [PubMed] [Google Scholar]
- 5. Li Z, Zhang LJ, Zhang HR, Tian GF, Tian J, Mao XL, et al. Tumor-derived transforming growth factor-beta is critical for tumor progression and evasion from immune surveillance. Asian Pac J Cancer Prev 2014;15:5181–6. [DOI] [PubMed] [Google Scholar]
- 6. Akhurst RJ, Hata A. Targeting the TGFbeta signalling pathway in disease. Nat Rev Drug Discov 2012;11:790–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chakravarthy A, Khan L, Bensler NP, Bose P, De Carvalho DD. TGFβ-associated extracellular matrix genes link cancer-associated fibroblasts to immune evasion and immunotherapy failure. Nat Commun 2018;9:4692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tauriello DVF, Palomo-Ponce S, Stork D, Berenguer-Llergo A, Badia-Ramentol J, Iglesias M, et al. TGFβ drives immune evasion in genetically reconstituted colon cancer metastasis. Nature 2018;554:538–43. [DOI] [PubMed] [Google Scholar]
- 9. Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y, et al. TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 2018;554:544–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roy LO, Poirier MB, Fortin D. Differential expression and clinical significance of transforming growth factor-beta isoforms in GBM tumors. Int J Mol Sci 2018;19:1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bian Y, Hall B, Sun ZJ, Molinolo A, Chen W, Gutkind JS, et al. Loss of TGFβ signaling and PTEN promotes head and neck squamous cell carcinoma through cellular senescence evasion and cancer-related inflammation. Oncogene 2012;31:3322–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shen W, Tao GQ, Zhang Y, Cai B, Sun J, Tian ZQ. TGF-beta in pancreatic cancer initiation and progression: two sides of the same coin. Cell Biosci 2017;7:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dituri F, Mancarella S, Cigliano A, Chieti A, Giannelli G. TGFβ as multifaceted orchestrator in HCC progression: signaling, EMT, immune microenvironment, and novel therapeutic perspectives. Semin Liver Dis 2019;39:53–69. [DOI] [PubMed] [Google Scholar]
- 14. Han J, Alvarez-Breckenridge CA, Wang QE, Yu J. TGF-beta signaling and its targeting for glioma treatment. Am J Cancer Res 2015;5:945–55. [PMC free article] [PubMed] [Google Scholar]
- 15. Bailey P, Chang DK, Nones K, Johns AL, Patch AM, Gingras MC, et al. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature 2016;531:47–52. [DOI] [PubMed] [Google Scholar]
- 16. Pang X, Tang YL, Liang XH. Transforming growth factor-β signaling in head and neck squamous cell carcinoma: Insights into cellular responses (Review). Oncol Lett 2018;16:4799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bouquet F, Pal A, Pilones KA, Demaria S, Hann B, Akhurst RJ, et al. TGFbeta1 inhibition increases the radiosensitivity of breast cancer cells in vitro and promotes tumor control by radiation in vivo. Clin Cancer Res 2011;17:6754–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Melisi D, Ishiyama S, Sclabas GM, Fleming JB, Xia Q, Tortora G, et al. LY2109761, a novel transforming growth factor beta receptor type I and type II dual inhibitor, as a therapeutic approach to suppressing pancreatic cancer metastasis. Mol Cancer Ther 2008;7:829–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Melisi D, Garcia-Carbonero R, Macarulla T, Pezet D, Deplanque G, Fuchs M, et al. Galunisertib plus gemcitabine vs. gemcitabine for first-line treatment of patients with unresectable pancreatic cancer. Br J Cancer 2018;119:1208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Melisi D, Oh D-Y, Hollebecque A, Calvo E, Varghese A, Borazanci E, et al. Safety and activity of the TGFβ receptor I kinase inhibitor galunisertib plus the anti-PD-L1 antibody durvalumab in metastatic pancreatic cancer. J Immunother Cancer 2021;9:e002068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pei H, Parthasarathy S, Joseph S, McMillen W, Xu X, Castaneda S, et al. Abstract 955: LY3200882, a novel, highly selective TGFβRI small molecule inhibitor. Cancer Research 2017;77(13_suppl):955. [Google Scholar]
- 22. Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the eastern cooperative oncology group. Am J Clin Oncol 1982;5:649–55. [PubMed] [Google Scholar]
- 23. Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, et al. Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 2010;28:1963–72. [DOI] [PubMed] [Google Scholar]
- 24. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009;10:459–66. [DOI] [PubMed] [Google Scholar]
- 25. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. [DOI] [PubMed] [Google Scholar]
- 26. U.S. Department of Health and Human Services. Common terminology criteria for adverse events (CTCAE) v4.03. 2010. [Accessed 2020 Nov 13]. Available from:https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf.
- 27. Rodon J, Carducci MA, Sepulveda-Sanchez JM, Azaro A, Calvo E, Seoane J, et al. First-in-human dose study of the novel transforming growth factor-beta receptor I kinase inhibitor LY2157299 monohydrate in patients with advanced cancer and glioma. Clin Cancer Res 2015;21:553–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wick A, Desjardins A, Suarez C, Forsyth P, Gueorguieva I, Burkholder T, et al. Phase 1b/2a study of galunisertib, a small molecule inhibitor of transforming growth factor-beta receptor I, in combination with standard temozolomide-based radiochemotherapy in patients with newly diagnosed malignant glioma. Invest New Drugs 2020;38:1570–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ikeda M, Takahashi H, Kondo S, Lahn MMF, Ogasawara K, Benhadji KA, et al. Phase 1b study of galunisertib in combination with gemcitabine in Japanese patients with metastatic or locally advanced pancreatic cancer. Cancer Chemother Pharmacol 2017;79:1169–77. [DOI] [PubMed] [Google Scholar]
- 30. Bobr A, Igyarto BZ, Haley KM, Li MO, Flavell RA, Kaplan DH. Autocrine/paracrine TGFβ1 inhibits Langerhans cell migration. Proc Natl Acad Sci U S A 2012;109:10492–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yap TA. TGF-BR1 inhibitor shows early activity and tolerability in advanced cancers. Targeted Oncology 2018. Proceedings of the 33rd Annual Meeting of the Society for Immunotherapy of Cancer. [Google Scholar]
- 32. Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817–25. [DOI] [PubMed] [Google Scholar]
- 33. Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 2013;369:1691–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. O'Hara MH, O'Reilly EM, Varadhachary G, Wolff RA, Wainberg ZA, Ko AH, et al. CD40 agonistic monoclonal antibody APX005M (sotigalimab) and chemotherapy, with or without nivolumab, for the treatment of metastatic pancreatic adenocarcinoma: an open-label, multicentre, phase 1b study. Lancet Oncol 2021;22:118–31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Legend
Dosing and administration information
All causality TEAEs
Patient disposition
LY3200882 pharmacokinetics parameters
Line graph of langerhan skin biopsy