Background
Subsurface radiofrequency (RF) treatments produce skin contraction by causing coagulation of the underlying subcutaneous fat. This method is marketed to fill a treatment gap for patients who do not wish to have surgery. A systematic review of this subject has not been previously published.
Methods
An electronic search was performed using PubMed to identify the literature describing subsurface RF treatments.
Results
Thirty articles were evaluated. An InMode device was used in 23 studies, and a Thermi device was used in 6 studies, with or without liposuction. Treatment areas included the face, neck, body, breasts, and labia. Most studies relied on patient satisfaction scores and physician review of photographs. The most frequent complications were induration and nodules. Most patients experienced prolonged swelling and numbness. Several studies reported marginal mandibular neuropraxias. The skin response after treatment of the abdomen was poor, and seromas were common. The incidence of burns improved after modification of the InMode device. Breast treatment did not appear to be effective in treating ptosis. Patient satisfaction scores were modest. Most studies (77%) were published by authors with a known conflict of interest. In some studies, the photographs did not accurately depict the treatment result. Institutional review board approval and disclosure of off-label regulatory status were often missing.
Discussion
Thermal treatment of the subcutaneous tissue introduces extra risks without a compensatory benefit. Comparisons in terms of safety, cost, recovery time, results, and complications do not favor energy-based devices. A treatment gap may be fictitious; properly informed patients may be treated with existing surgical procedures at all ages.
Conclusions
Little evidence supports the efficacy and safety of subcutaneous RF treatments as an improvement over results that may be obtained using traditional surgical methods such as submental lipectomy, liposuction, and abdominoplasty. Photographic integrity is often lacking. Financial conflict of interest is pervasive. Marketing precedes the science. Plastic surgeons need to be aware of these serious limitations and the off-label regulatory status of these devices, before purchasing expensive equipment and recommending subsurface RF treatments to patients.
Key Words: radiofrequency, subsurface, InMode, Thermi, RFAL, radiofrequency-assisted liposuction
For more than 2 decades, energy devices, including laser, ultrasound, cryotherapy, and radiofrequency (RF), have figured prominently at plastic surgery meetings, particularly the sections on innovations. Nonsurgical or minimally invasive methods are presumed to be the way of the future. However, the marketing has frequently preceded the science.1 Reliable evidence supporting the efficacy and safety of many of these devices is still lacking.
Radiofrequency treatments produce an electric current that generates heat through resistance in the dermis and subcutaneous tissue.2 Originally, surface RF treatments (eg, Thermage RF; Solta Medical, Pleasanton, CA) were used in an effort to create skin tightening.2 This method was introduced as a nonsurgical facelift.3 However, clinical experience revealed minimal efficacy.3–8 In some cases, facial fat atrophy occurred, requiring remedial fat grafting.7 The threshold for burning the skin (>42°C) is much lower than the threshold for contraction of subdermal and subcutaneous collagen (60°C).9
In 2009, Paul and Mulholland9 introduced a subsurface RF device designed to heat the adipose tissue and tighten the overlying skin. The subcutaneous tissue is heated to 65°C while limiting the epidermal temperature to 40°C.9 Subsurface RF devices (BodyTite, ThermiTight) are sold by 2 manufacturers in the United States (InMode, Lake Forest, CA and Thermi, Irving, TX). A “treatment gap” is proposed, and these devices are marketed to fill that gap.10,11 Candidates have conditions that are deemed not severe enough to justify excisional surgery but not mild enough for most nonsurgical treatments,11 such as RF microneedling.
A systematic review of studies reporting subsurface RF treatments has not been previously published. This study was undertaken to explore the evidence, evaluate problems such as conflict of interest, and, in doing so, better inform patients and plastic surgeons who may consider purchasing these devices and offering these treatments to their patients.
METHODS
An electronic literature review was performed to identify publications that evaluate aesthetic applications of subsurface RF treatments. The search terms “radiofrequency,” “InMode,” and “ThermiTight” were entered into the PubMed search engine. The search included all articles published in English starting in 2009, the year of the original publication,9 to September 2021. Only studies that included subcutaneous application of thermal energy using subsurface probes were reviewed. Acne treatments were excluded. Preliminary studies using Renuvion (previously called J-Plasma) RF-helium plasma devices (Apyx Medical, Clearwater, FL) were not evaluated.
RESULTS
Thirty unique articles evaluating subsurface RF treatments were identified (Table 1).9,11–39 In 23 studies (77%), an InMode product was used. A Thermi product was used in 6 studies (20%). One Korean study used a similar monopolar device.26 Two recent articles published in 2019 and 2020 report the same findings in the same 247-patient population.11,40 Data from the first published study were tabulated.11 No prospective randomized studies that include a control group have been published. Data heterogeneity precluded a meta-analysis. Most authors (67%) also used liposuction in some or all patients. The median number of study patients was 25 (range, 9–745). The most common treatment areas were the neck (57%), trunk (37%), upper arms (37%), and face (33%). Local anesthesia was used in 9 studies, and general anesthesia in 8 studies. Three studies used local anesthesia in some patients and general anesthesia in others. The tissues were routinely tumesced. Five studies used oral sedation. Intravenous anesthesia was used in 3 studies.
TABLE 1.
Published Studies of Subsurface Radiofrequency Treatments
| No. | Study (Year) | No. Patients | Device | Anesthesia | Area | Liposuction | Complications | Measuring Device | Financial Conflict |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Paul and Mulholland9 (2009) | 20 | BodyTite | General, tumescent | Trunk, inner thighs, arms, male breasts | Yes | None reported | None | Invasix assisted in thermal measurements. M.P. served as chief of the medical advisory board and received fees and stock options. |
| 2 | Blugerman et al12 (2010) | 23 | BodyTite | General, tumescent | Abdomen, flanks | Yes | None reported | Measurements on skin surface (moles, umbilicus, incision sites) using a flexible ruler | G.B. and D.S. were gifted the device and received study-related expenses. M.P. was a consultant and chief of the medial advisory board, received a stipend, and held stock options in Invasix. |
| 3 | Divaris et al13 (2011) | 53 | BodyTite | General, superwet | Abdomen, flanks, outer thighs, arms | Yes | None reported | Measurements between 2 points and circumference | None reported. M.P. has conflicts disclosed in other contemporaneous studies. |
| 4 | Ahn et al14 (2011) | 42 | FaceTite | Oral or IV sedation, tumescent, nerve blocks | Face, neck | Yes | None reported | 5-Point patient satisfaction scores, punch biopsies | None reported. R.S.M. and M.P. have conflicts disclosed in other contemporaneous studies. |
| 5 | Ion et al15 (2011) | 50 | BodyTite | General, tumescent | Abdomen, flanks, buttocks, thighs, posterior neck | Yes | 2 Burns | None | None reported |
| 6 | Paul et al16 (2011) | 24 | BodyTite | General, tumescent | Abdomen, flanks | Yes | 1 Seroma | Measurements on skin surface (moles, umbilicus, incisions) using a flexible ruler | M.P. served as a consultant and medical advisor for Invasix and received stock options. R.S.M. received consulting fees and technology. |
| 7 | Hurwitz and Smith17 (2012) | 17 | BodyTite with cannula | Oral sedation, superwet | Arms, abdomen, thighs | Yes | 2 Seromas, 4 patients with induration, 1 burn, 1 nodule | Patient 1–5 ratings, circumferences | Use of BodyTite and surgeon reimbursement. D.J.H. was a paid investigator for InMode, held stock options, and accepted $5000 in fees for lectures. |
| 8 | Theodorou et al18 (2012) | 97 | BodyTite | Oral sedation, tumescent | Thighs, trunk, knees, arms, neck | Yes | 14.6% (infections, seromas, 9 burns, end hits) | Patient surveys, physician assessment of photos | Consultant fees |
| 9 | Duncan19 (2012) | 12 | BodyTite | General, superwet | Upper arms | Yes | 1 Scar deformity | Measurements on photographs, skin laxity measured with calipers | Free use of device. InMode consultant |
| 10 | Blugerman et al20 (2013) | 59 | BodyTite | IV anesthesia, tumescent | Male breasts | Yes | None for radiofrequency treatment | Patient satisfaction on a 1–10 scale | G.B., D.S., and R.S.M. were gifted the device. R.S.M. is a paid consultant. |
| 11 | Theodorou and Chia21 (2013) | 40 | BodyTite | Oral sedation, tumescent | Upper arms | Yes | 1 Burn, 1 seroma | Patient surveys and physician evaluation of photographs | Authors are consultants. Patients reimbursed by Invasix |
| 12 | Duncan22 (2013) | 12 | BodyTite | General, superwet | Abdomen | Yes | Nodules in 2 patients persisting >1 y | Measurements on photographs | Free use of device. InMode consultant disclosed in other studies |
| 13 | Key23 (2014) | 35 | Thermi-Tight | Local, tumescent | Submental, jowls | No | None reported | Photographic assessment | None reported |
| 14 | Chia et al24 (2015) | 10 | BodyTite | General, tumescent | Upper arms | Yes | None reported | Skin measurements, fluorescent ink tattoos, patient satisfaction | C.T.C. and S.J.T. are consultants. Invasix paid for transportation and lodging and reimbursed patients. |
| 15 | Kang et al25 (2015) | 13 | FaceTite | Local, tumescent | Neck | No | Erythema, edema, focal hardness | Physician review of photographs, patient 4-point ratings | None reported |
| 16 | Kim et al26 (2016) | 20 | Apolex (monopolar), with cannula | Local | Submental, lower face | Yes | 2 Patients with paresthesias | Patient surveys, physician assessment of photos, Cutometer | Commercial funding for study |
| 17 | Wu et al27 (2016) | 12 | Thermi-RF | Local | Upper arms | No | Erythema (4%), contour irregularity (4%), bruising (13%) | Patient surveys, skin laxity grading, arm measurements | D.C.W. received financial support. |
| 18 | Keramidas and Rodopoulou28 (2016) | 55 | NeckTite and FaceTite | Local plus sedation (58%), general (27%), local (15%), superwet | Neck and jowls | Yes | Burns (3.6%), persistent hardness (9%), marginal mandibular neuropraxia (2%) | Patient 1–5 ratings, physician 1–5 ratings of photographs | None reported |
| 19 | Dendle et al29 (2016) | 35 | Thermi-RF | Local | Submental, jawline | No | Nodules (18.5%), 2 marginal mandibular neuropathies, 1 burn | Patient 1–5 ratings | None reported. D.C.W. received financial support for a contemporaneous study. Device loaned by Thermi Aesthetics |
| 20 | Jones et al30 (2017) | 10 | Thermi-Tight | Ketorolac, tumescent | Neck | No | None reported | Neck Laxity Grade, patient assessments | D.C.W. is a consultant for Thermi Aesthetics. D.C.W. and M.P.G. received research support and discounted equipment. |
| 21 | Sanan et al31 (2019) | 12 | Thermi-Tight | Local, tumescent | Face and neck | No | 1 Facial abscess, 1 incisional pain | Patient 1–5 ratings, review of photographs | None reported |
| 22 | Dayan et al11 (2019) | 247 | FaceTite and RF microneedling | Local (97%) or general (3%) | Neck and jowls | No | Prolonged swelling (4.8%), hardened areas (3.2%), 3 neuropraxias (1.2%) | Baker Face Neck score, patient satisfaction | All authors are InMode consultants. |
| 23 | Dayan et al32 (2020) | 10 | AccuTite | Oral sedation, local, tumescent | Labia minora and majora | No | None reported | Measurement of labial protrusion, patient satisfaction, 1–10 scale | All authors are InMode consultants. |
| 24 | Chia et al33 (2020) | 300 | BodyTite | Oral sedation, tumescent | Face, neck, trunk, breasts, upper arms, thighs, knees | Yes | 0.7%, 2 Burns, 1 marginal mandibular branch neuropraxia | None | C.T.C. and S.J.T. are consultants for InMode and stockholders. |
| 25 | Dayan et al34 (2020) | 25 | AccuTite, BodyTite, FaceTite | Local, tumescent | Face, neck, arms, thighs, abdomen | Yes | None reported | Perfusion and lymphatic imaging | All authors are consultants and/or investigators with InMode. |
| 26 | Cohen et al35 (2020) | 10 | InMode (FaceTite) | Local, tumescent | Face and neck | No | Edema in 1 patient | Ultrasound echogenicity, physician 1–5 rating, patient satisfaction | None reported. E.D. has reported conflicts in other contemporaneous publications. |
| 27 | Cook et al36 (2021) | 745 | BodyTite FaceTite, AccuTite | Local (67.5%) or general (32.5%), and tumescent | Neck, trunk, arms, knees, breasts. | Yes | Swelling (9%), nodules (8.5%), hyperpigmentation (0.5%), contour irregularity (1%), burns in 2 patients | Patient satisfaction | J.N.P. and B.E.D. are paid research investigators and speakers for InMode and have stock options. |
| 28 | Han et al37 (2021) | 227 | FaceTite | IV sedation, tumescent | Lower face and neck | Yes | 2 Patients with hardness, 1 depression deformity (fat grafted) | Physician review of photographs, patient questionnaires | None reported |
| 29 | Demesh et al38 (2021) | 9 | AccuTite and RF microneedling | Nitrous oxide, tumescent | Lower face and neck | No | None reported | Investigator and patient assessments using 5-point scale | None reported |
| 30 | Turer et al39 (2021) | 72 | Thermi-RF | Local, tumescent | Neck | No | Pharyngeal inflammation in 1 patient | Skin area measurements, physician evaluation of photographs, Cutometer, patient and physician questionnaires | B.E.D. owned shares in ThermiGen, was a consultant, and received honoraria from ThermiGen. |
IV, intravenous.
Treatment times ranged from 45 minutes for the face and neck28 to 102 minutes, on average, for multiple areas.33 Breasts required 60 to 90 minutes.36 The average treatment time for the “Embrace” protocol, combining FaceTite with topical RF (Morpheus8, InMode), was 58 minutes.40 Many investigators used forward-looking infrared imaging to monitor the surface temperature,9,16,23,31,39 especially when using the Thermi device.
Variable posttreatment protocols were described. Turer et al39 applied paper tape on the neck covered by foam and a Velcro chin strap, worn for 3 to 6 days. Patients were instructed not to shower for 1 week. A garment was worn intermittently while at home and at night for the next 3 weeks. Strenuous activity was prohibited for 4 weeks. After treating the abdomen with the BodyTite device, Hurwitz and Smith17 instructed patients to apply compression foam for 5 to 7 days and then shower. Elastic garments were recommended for 3 weeks. Induration was treated with massage and low-level laser treatments.17
Eleven studies (37%) reported no complications. Cook et al36 reported adverse events in 19% of patients; half of these cases were prolonged swelling. Keramidas and Rodopoulou28 reported hardness of the subcutaneous tissue of the neck in 9% of patients, requiring daily massage for 3 months.
Dendle et al29 reported that the most common adverse effects after Thermi treatments of the face and neck were tenderness (63%), edema (89%), bruising (52%), numbness (82%), and nodules or induration (19%). The most frequently reported complication reported among all studies was hardening of the subcutaneous tissue, producing induration and nodules.11,17,22,25,28,29,36,37 These areas frequently took months to soften. Seromas requiring serial drainage commonly occurred after treating the abdomen with the BodyTite device. Some operators routinely inserted a drain when treating the abdomen and left it in place for up to 14 days.18,41 Hurwitz and Wright42 retreated the abdomen in 25% of cases and routinely treated loose skin with Morpheus8 RF microneedling. Seven cases of neuropraxia of the marginal mandibular nerve were reported among the 30 studies.11,28,29,33
Most articles reported subjective methods of evaluation, such as patient satisfaction scores (67%) or physician evaluation of before-and-after photographs (43%). Paul and Mulholland9 measured distances between 2 surface landmarks, such as moles or the umbilicus, using a flexible ruler. These authors reported a linear contraction varying from 12.7% to 47% 6 months after RF-assisted liposuction. The authors noted that the soft tissue contraction would be much greater, calculated as the square of linear contraction. A 47% linear contraction would theoretically produce a 72% reduction in surface area (1–0.53 × 0.53). Measurements on photographs from other studies reveal lesser degrees of skin contraction (Fig. 1).
FIGURE 1.
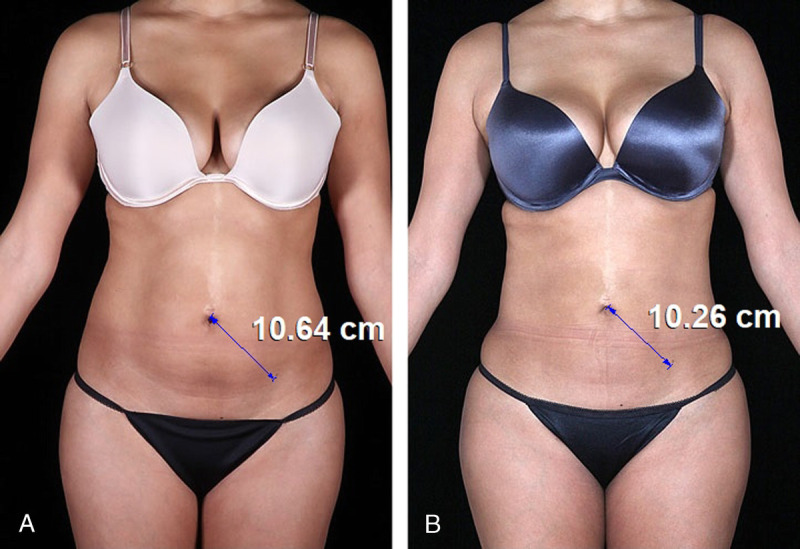
A, B, This 30-year-old woman is shown before and 1 year after BodyTite-assisted liposuction of her abdomen and flanks. Measurements are made using the Canfield 7.4.1 Mirror imaging software (Canfield Scientific, Fairfield, NJ). The distance between the pigmented skin lesion of the left lower abdomen and the umbilicus has decreased 0.38 cm (3.6%). The calculated reduction in surface area is 7.6%. A hip width of 34 cm was used for calibration (although this measurement does not affect percent change). Adapted from Theodorou et al.18
Duncan22 used tattooed markers to facilitate surface measurements. This investigator studied 12 patients in whom RF-assisted liposuction was used on one side of the abdomen and not on the other, finding a greater reduction in surface area measurements (36%) for patients receiving RF assistance compared with liposuction alone (8%) at 1 year follow-up. However, in some cases, the skin “buckled” in the heated areas, causing greater skin laxity on the heated side. Other investigators also reported inadequate skin tightening after subsurface RF treatment, leaving skin redundancy and wrinkling.15–17 Hurwitz and Smith17 attributed this progressive wrinkling to contracture of the subcutaneous tissue beyond the shrinkage capability of the overlying skin.
In 2015, Chia et al24 compared RF-assisted liposuction of one upper arm with unassisted liposuction of the other upper arm. The authors reported a 13% surface area reduction for RF-assisted liposuction versus an 8% reduction for the control arm at 1 year. The differences between treatments were not statistically significant.
A recent retrospective study by Cook et al36 reported a large experience (n = 745) using the InMode device on multiple areas, including the neck, trunk, arms, and breasts (Fig. 2). Another study published almost simultaneously reported a prospective study of patients treated with the Thermi product. Major improvements in the jawline and neck were demonstrated in photographs.39 Photographs from other studies showed less dramatic results (Fig. 3).
FIGURE 2.
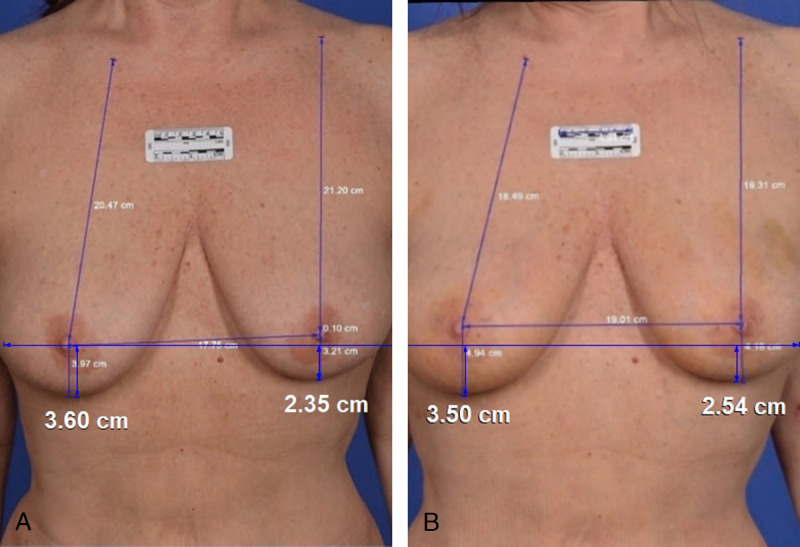
A, B, This 61-year-old woman is seen before and 3 months after a FaceTite treatment of her breasts. The patient still has bruising and swelling. The published photographs have been matched for size and orientation using the Canfield 7.4.1 imaging software. Measurements of the lower pole level are similar. Adapted from Cook et al.36
FIGURE 3.

A, B, Pretreatment and 1-month posttreatment photographs of this 53-year-old woman have been matched for size and orientation. The authors report that she was treated with FaceTite. The submental fullness is corrected, although the patient has persistent skin laxity. Adapted from Cook et al.36
Some studies using the BodyTite device on the abdomen included photographs of patients who also had abdominoplasties or a surgical diastasis repair.11,14,15,17 One patient had a “mini neck-lift” in addition to a FaceTite treatment.14
Most articles (77%) were published by authors with known financial conflicts. In 5 studies, no financial conflicts were reported,13,14,22,29,35 but at least 1 of the authors was known to have a conflict that was reported in another contemporaneous study. Many of the authors were paid consultants. Some also held ownership positions in the form of stock options. Two authors also served as chairmen of the medical advisory board of InMode (formerly Invasix).9,12,32–34
Investigators were often allowed to keep their InMode BodyTite devices (US $205,000)10 after their study without paying for the device.12,16,20 Duncan22 reported that she voluntarily returned her InMode device after using it at no charge for her study. Key23 was the only author to report no financial conflicts and the fact that he purchased his RF equipment.
DISCUSSION
Financial Conflict of Interest
Financial conflict of interest is a major problem in medicine today. One entire issue of the Journal of the American Medical Association was dedicated to this subject.43 Publications on this topic have also appeared in the plastic surgery literature in recent years.44–46 The dollar amount of a conflict of interest does not need to be substantial to be effective.47 Even small gestures, such as paying for meals, build a sense of reciprocity.
The full extent of this financial conflict is often undisclosed to the reader. Such conflicts include direct payments to doctors, providing expensive equipment for studies at no charge (the doctors just keep the equipment), referral fees, payments for speaking and traveling, and funding for clinical trials. An author may also serve as an officer of the company or hold an ownership interest.45
Authors are often listed in the disclosure paragraph of publications as consultants. These physicians are recruited and heavily reimbursed to conduct studies that are published in plastic surgery journals. Plastic surgeons' services are not simply to provide advice to the company (the true role of a consultant), which would be at a much lower hourly fair market price.45
In response to this problem, the “Sunshine Act,” part of the Affordable Care Act, was passed by Congress to provide transparency to the public regarding payments their doctors receive from industry. Medical device companies are required to disclose these payments.48 Surprisingly, there is no record on the Propublica “Dollars for Docs” website of InMode payments to its numerous paid consultants.49
Photographic Integrity
Plastic surgeons and patients rely heavily on photographs. Photographic integrity is therefore essential.1 A 2019 publication claimed to show the results of InMode BodyTite treatments in combination with RF microneedling using the Fractora (InMode) device, later replaced by the Morpheus8 device.11 The study included photographs of 1 patient who also underwent an undisclosed abdominoplasty (Fig. 4).50 In a set of facial photographs contained in the same article, the mandibular border was lightened to soften the appearance of jowls. A third patient appears to have had undisclosed liposuction of the back.
FIGURE 4.

A, B, Pretreatment and 6-month posttreatment photographs of this 47-year-old woman have been matched for size and orientation. The authors report that this patient was treated with bipolar radiofrequency and radiofrequency microneedling treatment of the anterior abdomen. The postoperative photograph shows telltale signs of an abdominoplasty, with a conspicuous oblique scar on the right flank, a periumbilical scar, and downward displacement of pigmented skin lesions. Adapted from Dayan et al11 and reprinted from Swanson.50
A 2015 study24 determined that the percent change in linear measurements on the treated skin of the upper arms exceeded the percent change in area measurements, which is geometrically impossible.51 These patients also received liposuction, which can produce skin tightening on its own (Fig. 5), without energy treatment.24 Photographs of patients who were not actually in the study were published.51
FIGURE 5.
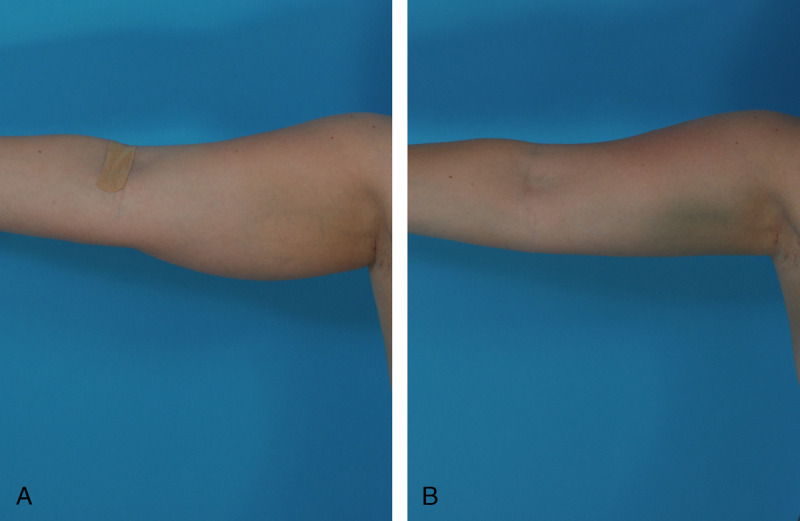
A, B, This 28-year-old woman underwent liposuction of her lower body, arms, and axillae, performed by the author. She is seen before and 3 months after surgery. The arm volume has been reduced, and the skin has contracted.
In a recently published study, the photographs showing “typical” 6-month results of a single Thermi treatment without liposuction are extraordinary.39 Two patients appear to have a full correction of submental adiposity and a major improvement in skin laxity of the lower face and neck—a result rivaling a facelift. Thermi funded the study featuring these excellent results and even provided writing assistance.39 Remarkably, this corporate sponsor held “final responsibility for the study design, collection, analysis, and interpretation of data; and the writing and the decision to submit the manuscript for publication.”39
One set of photographs did not depict a study patient.22 The photographs were provided by another surgeon. The patient is standing more upright in the postoperative photograph, and the lower part of the abdomen is concealed by panties who are pulled up much more than they were preoperatively. Another article also covered the lower abdomen in a postoperative photograph.9
Published photographs were frequently not properly standardized.29,32,33,39,40 In the postoperative photograph, the patient's image was often smaller28,33 or the chin was lifted,29,39 or both.33 In a study using FaceTite and AccuTite devices to treat hypertrophic labia, the labia minora were spread open in the before photograph and brought together in the after photograph.32
Patient Satisfaction
Many studies reported high levels of patient satisfaction.12–14,32 Others reported more modest patient satisfaction scores.28,29,37,39 Sixty-eight percent of the patients in the industry-sponsored study by Turer et al39 expressed satisfaction, and almost the same percentage (67%) of patients would recommend the treatment. Similarly, Dendle et al29 reported that 64% of their patients were satisfied after a Thermi treatment. Han et al37 reported that 21% of patients considered their results from FaceTite-assisted liposuction to be poor or thought that there was no change. Another study using this InMode product reported that 15% of patients were unhappy.28
RealSelf.com52 is a highly popular online plastic surgery forum that features patient reviews of plastic surgeons and procedures. This site avoids the influence of industry sponsorship and can help gauge patient satisfaction among a large number of online reviewers. Patient-rated “Worth It” scores for BodyTite and ThermiTight are 76% and 70%, respectively (Table 2).
TABLE 2.
RealSelf “Worth It” Scores and Average Price
| Procedure | “Worth It” (%) | Price (US $) | Reviews |
|---|---|---|---|
| Deep plane facelift | 99 | 13,000 | 200 |
| Lower facelift | 96 | 9875 | 1800 |
| Tummy tuck | 95 | 8300 | 33,500 |
| Facelift | 93 | 12,250 | 9200 |
| Breast lift | 93 | 8025 | 3291 |
| Chin liposuction | 91 | 3000 | 1000 |
| Liposuction | 86 | 6250 | 10,800 |
| Fractora RF | 78 | 1275 | 147 |
| FaceTite | 77 | 5100 | 178 |
| BodyTite | 76 | 6650 | 243 |
| Morpheus8 | 73 | 1825 | 160 |
| ThermiSmooth Face | 72 | 1175 | 38 |
| Microneedling RF | 71 | 850 | 56 |
| Thermage | 71 | 2475 | 458 |
| ThermiTight | 70 | 3225 | 184 |
| AccuTite | 44 | 2150 | 11 |
Patient Safety
Radiofrequency (electrical) energy flows from the tip of the internal probe to the external electrode of a bipolar BodyTite device, heating the adipose tissue and the dermis from below.9 The temperature around the tip of the probe reaches 70°C to 80°C.9,33 The external electrode contains a temperature sensor. The device shuts off at a selected temperature. Bell signals indicate when the goal temperature is reached.53 Ultrasound gel is applied liberally to the skin surface.33,34 The Thermi device is monopolar; the current is dispersed into the local adipose tissue and collected by a distant grounding electrode.31 The internal probe includes a temperature sensor. An infrared camera (FLIR Systems, Wilsonville, OR)23,39 monitors the skin temperature.31,53 Some authors keep ice on the field in a sterile glove as a precaution.39
Because the heat is applied to the deep surface of the skin, any burn is full thickness and some burns will require surgical revision.41 Ahn et al14 caution operators not to pass the internal probe too deeply in the face to avoid fat necrosis and a resulting contour depression, or injury to the facial nerve. Unlike most operators, who prefer to stay superficial in the face, Cohen et al35 insert the probe deep to the superficial musculoaponeurotic system.
Introducing a heated probe directly in the vicinity of the marginal mandibular branch of the facial nerve is likely to put this important nerve in jeopardy. The thermal injury is not tissue specific. Nerves close to the probe are likely to be damaged along with fat. When the Thermi study was undertaken from 2016 to 2017,39 a contemporaneous study was conducted to investigate the path of the marginal mandibular nerve among the same patients.54 This study included a nerve stimulator and careful mapping of the nerve, and skin marking.54 This nerve-mapping study and the use of a nerve stimulator are not referenced in the (corporate-sponsored and writing-assisted) clinical study.39 No nerve injuries were reported in either study.39,54
Some authors recommend routinely mapping the marginal mandibular nerve using a nerve stimulator when treating the face and neck.53,55 Several surgeons mark the anticipated course of the marginal mandibular nerve routinely before starting the procedure.33,39,54 Chia et al33 consider this area a “no fly” zone. Dayan et al40 do not treat areas medial to the marionette lines.
The average operating time by treatment area is increased when RF assistance is used.18 When treating awake patients, lidocaine toxicity is a concern. Theodorou et al18 reported that lidocaine doses exceeded 35 mg/kg in 33% of their BodyTite-assisted liposuction cases. These authors called for caution when treating convex areas to avoid end hits and a rapid increase in temperature that can cause a burn.18 Seromas are common.17,18,41,42 These fluid collections likely result from injury to the subcutaneous and subdermal lymphatic system.41 Mulholland41 and Theodorou et al18 insert drains in all patients undergoing RF-assisted abdominal liposuction. The drains remain in place for 5 to 14 days.18
Numbness and dysesthesia are more common when RF assistance is used, resulting from thermal coagulation causing demyelination of the sensory nerves.41 Some patients (5%) do not regain sensation.41 One of the most common injuries after a BodyTite treatment is damage to the medial antebrachial cutaneous nerve of the upper arm, sometimes causing permanent anesthesia.41 Induration is common.25 After thermal treatments, a prolonged thickness and brawny edema of the skin may require many months to resolve.41
In 2020, a case of full-thickness burns, resulting in scars and major skin irregularities, was reported following a BodyTite-assisted liposuction treatment of the thighs in a 51-year-old woman.56 The procedure was performed using a tumescent solution and a target temperature of 40°C. The author also encountered burns in 3 other patients.
Chia et al33 recently published a study using a “second-generation” RF device and reported a significant decrease in complications, including burns. This modification, which was introduced in 2016, adds internal monitoring of temperature and its rate of rise to avoid dangerous temperature spikes.33 The internal electrode cutoff temperature range is 50°C to 70°C, and the external electrode cutoff temperature range is 35°C to 43°C.35 When the predetermined cutoff temperature is reached, RF power automatically switches off.35 Without this modification, complications (ie, fibrous nodules and burns)33,41 may occur before the operator is aware of the excessive heat buildup.33,41
In many studies, it is not clear that proper institutional review board approval was obtained.9,11,16,24,32,33,36,40 The Department of Health and Human Services mandates institutional review board approval for clinical studies in the United States.57 Institutional review board approval is intended to protect patients by properly informing them of the risks of new procedures.
FDA 510(k) Clearance
The InMode BodyTite device received Food and Drug Administration (FDA) clearance in February 2016, based on its being substantially equivalent to an existing device, the ThermiGen Symphony RF System.58 Clearance for this ThermiGen system was based on another device that was cleared because it too was judged to be similar to an existing (predicate) device. According to the FDA records, the earlier devices on which the InMode device was cleared were never actually approved. The indications are identical—use in dermatologic and general surgical procedures for electrocoagulation and hemostasis. The company, including its representatives, is not allowed to market the device for other indications.58
The InMode Quick Reference Guide includes as an indication, “heating of fibrous septa and papillary dermis resulting in collagen contraction and skin tightening.” Any “off label” clinical use that is not FDA-approved requires disclosure. No such disclosures appear in these publications. Inserting a heated probe under the skin of the breasts36 or labia32 to cause tissue necrosis are off-label applications. The thin mucosa and skin of the labia minora would seem too tight a space to accommodate a FaceTite probe. A true subcutaneous plane with adipose tissue may not even exist in these locations. Local numbness and dysesthesias would not be well tolerated.
Manufacturers are required to report adverse events to the FDA.59 InMode consultants have reported “major” complications.18,33 However, there is no record of these adverse events being reported to the FDA, according to the government website.60
Comparison With Surgical Results
Radiofrequency is promoted to patients as a 3-dimensional shrink-wrapping of the “fibroseptal network.”22,24,33,35,37,53 When it was introduced, its advocates promised faster treatment, reduced tissue trauma, improved safety, uniform heating of the skin and the subcutaneous layer, and potential skin contraction.9 A common theme is that advanced expensive technology is scarless, painless, offers a rapid recovery, and is a safer alternative to surgery.42,53 These treatments may be marketed as 1-time procedures, with no surgery, performed in the office under local anesthesia, providing long-lasting results and minimal downtime.53 Radiofrequency treatments are promoted to drive practice volume by recruiting patients who may ultimately return for excisional procedures.53
The publication by Turer et al39 includes a quantitative analysis of neck skin area. Most patients demonstrated a contraction of at least 20 mm2, and the average contraction was 71 mm2 after a Thermi treatment. This is a modest difference. By comparison, the area of a US Forever postage stamp is about 400 mm2.61 Patients treated with a traditional submental lipectomy, especially younger patients, often demonstrate excellent skin contraction (Fig. 6). It is well known that skin contraction can occur in patients without heating the internal tissues (Figs. 5–7).
FIGURE 6.

A, B, This 37-year-old woman is seen before and 3 months after a submental lipectomy and secondary rhinoplasty performed by the author. The neck was treated using a submental incision, liposuction, direct resection of interplatysmal fat, and a medial platysmaplasty. Her profile is enhanced with a good skin response.
FIGURE 7.
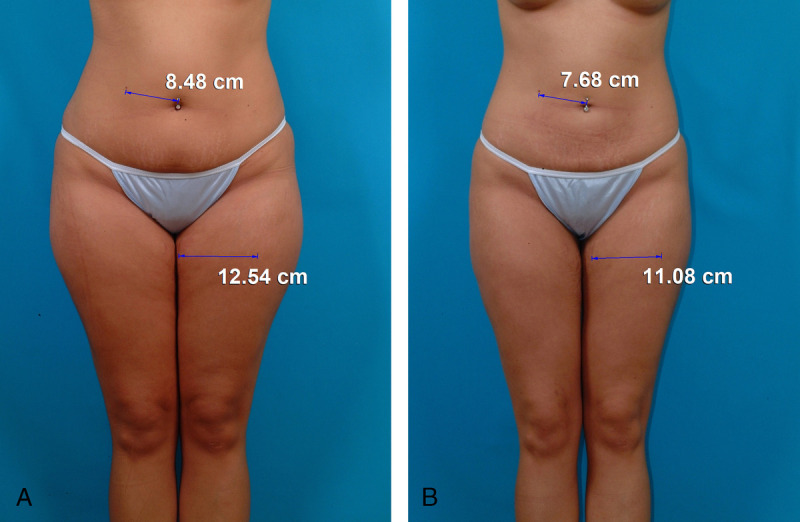
A, B, This 24-year-old woman is shown before and 6 months after lower body liposuction without RF assistance. A single treatment was performed by the author. Superwet infiltration was used. A total intravenous anesthetic was administered. The photographs are matched for size and orientation using the Canfield 7.4.1 Mirror imaging software. Measurements between landmarks on the abdomen—a pigmented lesion and a umbilical piercing—show a 9.4% linear skin contraction. A measurement on the left thigh between a skin lesion and a medial thigh stretch mark reveals an 11.6% linear skin contraction. Decreases in surface area are calculated as the square of linear changes. These reductions are 18.0% and 21.9%, respectively.
A conceptual problem with topical RF treatment is that fat atrophy is not usually desirable in the face. In fact, most aging patients benefit from fat transfer, not fat removal.62 A limitation of energy-based devices is its destructive effect on adipose cells.9 Aspirated fat cannot be transferred to other areas of the body, breast, or face.9 Platysmal bands cannot be treated using these devices and may be unmasked. Subplatysmal fat is best excised surgically.53
Radiofrequency devices are frequently promoted as a “nonexcisional” alternative to a facelift,14,25 even simulating the effect of a facelift.37 Surgery is often described as invasive or excisional. Radiofrequency, unlike ultrasound, which was a previous energy-based treatment, does not specifically target fat. All tissues are coagulated, including vessels, lymphatics, nerves, and connective tissue, causing the tissue to condense.15,35 There is no evidence for a more delicate controlled action like strings on the dermis.40 The liquefied tissue resembles a milkshake as it is aspirated.12
Subsurface RF treatments do require incisions, anesthesia, and frequently a general anesthetic. The procedures are not quick. Downtimes can be prolonged. Subsurface RF treatments are not inexpensive (Table 2). According to RealSelf.com, the average cost of a FaceTite treatment is $5100. BodyTite treatments cost $6650. By comparison, submental liposuction costs $3000. The average cost of liposuction is $6250.52
An alternative is to offer a submental lipectomy (Fig. 6) or a limited-incision deep-plane facelift, which avoids a pulled-back appearance.62 Surgical treatment avoids harm from burning and allows more precise control and dissection of tissues. Fat transfer is now part of the armamentarium of most facelift surgeons.62
Subsurface RF treatments are surprisingly long and tedious. “Burn anxiety” is an issue. Lubricating ointment must be heavily applied. The loud warning bell signals are disquieting. There is no direct visualization of tissue planes. The tissue depth is inflated by the tumescent solution, obscuring landmarks.
A submental lipectomy includes liposuction, direct excision of interplatysmal fat, and a corset platysmaplasty, all done using a single submental incision in 20 to 30 minutes by an experienced plastic surgeon (Fig. 6). The muscle repair treats platysmal bands, which cannot be managed with RF-assisted liposuction.53 No dressings are needed. A chin strap is worn overnight.62 Recovery is quick and discomfort is minimal. Comparisons favor this method (Table 3).
TABLE 3.
Comparison of Submental Lipectomy Versus RFAL
| Variable | Submental Lipectomy* | RFAL |
|---|---|---|
| Efficacy | +++ | ++ |
| Patient satisfaction (RealSelf score) | 91% | 77% |
| Need for temperature monitoring | 0 | Required |
| Risk of burns | 0 | + |
| Risk of nodules | 0 | +++ |
| Risk of facial nerve injury | + | ++ |
| Risk of end hits | 0 | + |
| Skin contraction | ++ | ++ |
| Recovery time | + | +++ |
| Cost of device (US $) | 0 | 205,000 |
| Disposables (US $) | None | 200 |
| Cost of single treatment (US $) | 3000 | 5100 |
| Scarring | + | + |
| Operating time, min | 30 | 45 |
| Anesthesia | Local or general | Local or general |
| Tumescent infusion | Not required | Necessary |
| FDA approval | NA | Off-label |
| Platysma repair | Simultaneous | Second procedure |
| Conflict of interest | 0 | ++++ |
+ indicates lowest magnitude; ++++ indicates highest magnitude.
*Including corset platysmaplasty, performed using submental incision only.
NA, not applicable; RFAL, radiofrequency-assisted liposuction.
Similarly, excellent skin contraction of the abdomen may be achieved after liposuction without RF assistance (Fig. 7). RealSelf “Worth It” scores for surgical procedures are consistently higher (86%–99%) than RF treatments (44%–78%).52 Chin liposuction and deep-plane facelifts score 91% and 99%, respectively (Table 2). According to a patient-reported outcome study, patient satisfaction after a subsuperficial musculoaponeurotic system facelift is 97%, and 94% of patients would recommend the treatment to someone else.62
Patient satisfaction after traditional liposuction tends to be high, with about 90% of patients pleased with their result and 94% reporting that they would do it again.63 Recovery is not difficult. Patients take 5.7 days off work, on average.63 Drains are unnecessary. Seromas are rare.64 The operating time for treatment of the abdomen and flanks is 30 to 60 minutes when performed under intravenous sedation.64 Radiofrequency treatments take longer.18 Retreatments are common.17 Table 4 compares methods.
TABLE 4.
Comparison of Abdominal Liposuction Versus RFAL
| Variable | Abdominal Liposuction* | RFAL |
|---|---|---|
| Efficacy | +++ | +++ |
| Patient satisfaction (RealSelf score) | 86% | 76% |
| Need for temperature monitoring | 0 | Required |
| Risk of burns | 0 | + |
| Risk of end hits | 0 | + |
| Nodules/induration | + | +++ |
| Persistent numbness and dysesthesias | + | +++ |
| Skin contraction | ++ | ++ |
| Skin buckling/laxity | + | +++ |
| Recovery time | + | +++ |
| Cost of device (US $) | 0 | 205,000 |
| Disposables (US $) | None | 200 |
| Cost of single treatment (US $) | 6250 | 6650 |
| With simultaneous abdominoplasty | Yes | No |
| Scarring | + | + |
| Seromas | + | +++ |
| Drains | No | Yes |
| Postoperative massage | Not required | Recommended |
| Postoperative laser/RF treatments | Not required | Recommended |
| Retreatments | + | ++ |
| Operating time, min | 30–60 | >60 |
| Anesthesia | Local or general | Local or general |
| FDA approval | NA | Off-label |
| Conflict of interest | 0 | ++++ |
+ indicates lowest magnitude; ++++ indicates highest magnitude.
*Superwet anesthesia, total intravenous anesthesia, abdomen, and flanks.
NA, not applicable; RFAL, radiofrequency-assisted liposuction.
Cook et al36 promote BodyTite as a breast lift alternative. To demonstrate, the authors compare before and after measurements. The procedure requires 30 to 45 minutes per side to perform. The cost is about the same as a mastopexy. Comparison of matched photographs (Fig. 2) reveals minimal benefit.
CONCLUSIONS
Little evidence supports improved efficacy or easier recovery after subcutaneous RF treatments compared with results that may be obtained using traditional methods such as submental lipectomy and liposuction. Controlled studies are lacking. The treatments are not innocuous; complications are common. Investigator conflict of interest taints published studies. Plastic surgeons need to be aware of the limitations of this method and its regulatory status, before purchasing an expensive thermal device and offering RF treatments to patients. Scientific evaluation must take precedence over marketing to ensure that patients receive valid treatment recommendations.
Footnotes
Conflicts of interest and sources of funding: E.S. receives royalties from Springer Nature (Cham, Switzerland).
E.S. is a plastic surgeon in private practice in Leawood, Kansas.
REFERENCES
- 1.Swanson E. Cryolipolysis: the importance of scientific evaluation of a new technique. Aesthet Surg J. 2015;35:NP116–NP119. [DOI] [PubMed] [Google Scholar]
- 2.Fritz K, Salavastru C. Ways of noninvasive facial skin tightening and fat reduction. Facial Plast Surg. 2016;32:276–282. [DOI] [PubMed] [Google Scholar]
- 3.Narins DJ, Narins RS. Non-surgical radiofrequency facelift. J Drugs Dermatol. 2003;2:495–500. [PubMed] [Google Scholar]
- 4.Narins RS Tope WD Pope K, et al. Overtreatment effects associated with a radiofrequency tissue-tightening device: rare, preventable, and correctable with subcision and autologous fat transfer. Dermatol Surg. 2006;32:115–124. [DOI] [PubMed] [Google Scholar]
- 5.Fritz M, Counters JT, Zelickson BD. Radiofrequency treatment for middle and lower face laxity. Arch Facial Plast Surg. 2004;6:370–373. [DOI] [PubMed] [Google Scholar]
- 6.Abraham MT Chiang SK Keller GS, et al. Clinical evaluation of non-ablative radiofrequency facial rejuvenation. J Cosmet Laser Ther. 2004;6:136–144. [DOI] [PubMed] [Google Scholar]
- 7.Alexiades-Armenakas M, Dover JS, Arndt KA. Unipolar versus bipolar radiofrequency treatment of rhytides and laxity using a mobile painless delivery method. Lasers Surg Med. 2008;40:446–453. [DOI] [PubMed] [Google Scholar]
- 8.Araújo AR Soares VP Silva FS, et al. Radiofrequency for the treatment of skin laxity: mith or truth. An Bras Dermatol. 2015;90:707–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paul M, Mulholland RS. A new approach for adipose tissue treatment and body contouring using radiofrequency-assisted liposuction. Aesthetic Plast Surg. 2009;33:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Theodorou SJ, Del Vecchio D, Chia CT. Soft tissue contraction in body contouring with radiofrequency-assisted liposuction: a treatment gap solution. Aesthet Surg J. 2018;38(suppl 2):S74–S83. [DOI] [PubMed] [Google Scholar]
- 11.Dayan E Chia C Burns AJ, et al. Adjustable depth fractional radiofrequency combined with bipolar radiofrequency: a minimally invasive combination treatment for skin laxity. Aesthet Surg J. 2019;39(suppl 3):S112–S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blugerman G, Schavelzon D, Paul MD. A safety and feasibility study of a novel radiofrequency-assisted liposuction technique. Plast Reconstr Surg. 2010;125:998–1006. [DOI] [PubMed] [Google Scholar]
- 13.Divaris M Boisnic S Branchet M-C, et al. A clinical and histological study of radiofrequency-assisted liposuction (RFAL) mediated skin tightening and cellulite improvement — RFAL for skin tightening. J Cosmetics Dermatol Sci Appl. 2011;1:36–42. [Google Scholar]
- 14.Ahn DH Mulholland RS Duncan D, et al. Non-excisional face and neck tightening using a novel subdermal radiofrequency thermo-coagulative device. J Cosmetics Dermatol Sci Appl. 2011;1:141–146. [Google Scholar]
- 15.Ion L, Raveendran SS, Fu B. Body-contouring with radiofrequency-assisted liposuction. J Plast Surg Hand Surg. 2011;45:286–293. [DOI] [PubMed] [Google Scholar]
- 16.Paul M Blugerman G Kreindel M, et al. Three-dimensional radiofrequency tissue tightening: a proposed mechanism and applications for body contouring. Aesthetic Plast Surg. 2011;35:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurwitz D, Smith D. Treatment of overweight patients by radiofrequency-assisted liposuction (RFAL) for aesthetic reshaping and skin tightening. Aesthetic Plast Surg. 2012;36:62–71. [DOI] [PubMed] [Google Scholar]
- 18.Theodorou SJ, Paresi RJ, Chia CT. Radiofrequency assisted liposuction device for body contouring: 97 patients under local anesthesia. Aesthetic Plast Surg. 2012;36:767–779. [DOI] [PubMed] [Google Scholar]
- 19.Duncan DI. Improving outcomes in upper arm liposuction: adding radiofrequency-assisted liposuction to induce skin contraction. Aesthet Surg J. 2012;32:84–95. [DOI] [PubMed] [Google Scholar]
- 20.Blugerman G Schalvezon D Mulholland RS, et al. Gynecomastia treatment using radiofrequency-assisted liposuction (RFAL). Eur J Plast Surg. 2013;36:231–236. [Google Scholar]
- 21.Theodorou S, Chia C. Radiofrequency-assisted liposuction for arm contouring: technique under local anesthesia. Plast Reconstr Surg Glob Open. 2013;1:e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duncan DI. Nonexcisional tissue tightening: creating skin surface area reduction during abdominal liposuction by adding radiofrequency heating. Aesthet Surg J. 2013;33:1154–1166. [DOI] [PubMed] [Google Scholar]
- 23.Key DJ. Integration of thermal imaging with subsurface radiofrequency thermistor heating for the purpose of skin tightening and contour improvement: a retrospective review of clinical efficacy. J Drugs Dermatol. 2014;13:1485–1489. [PubMed] [Google Scholar]
- 24.Chia CT Theodorou SJ Hoyos AE, et al. Radiofrequency-assisted liposuction compared with aggressive superficial, subdermal liposuction of the arms: a bilateral quantitative comparison. Plast Reconstr Surg Glob Open. 2015;3:e459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kang JS Cho SE Nam SM, et al. Nonexcisional, minimally invasive rejuvenation of the neck using radiofrequency tissue tightening (FaceTite™). Arch Aesthetic Plast Surg. 2015;21:91–95. [Google Scholar]
- 26.Kim EJ Kwon HI Yeo UC, et al. Lower face lifting and contouring with a novel internal real-time thermosensing monopolar radiofrequency. Lasers Med Sci. 2016;31:1379–1389. [DOI] [PubMed] [Google Scholar]
- 27.Wu DC Liolios A Mahoney L, et al. Subdermal radiofrequency for skin tightening of the posterior upper arms. Dermatol Surg. 2016;42:1089–1093. [DOI] [PubMed] [Google Scholar]
- 28.Keramidas E, Rodopoulou S. Radiofrequency-assisted liposuction for neck and lower face adipodermal remodeling and contouring. Plast Reconstr Surg Glob Open. 2016;4:e850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dendle J Wu DC Fabi SG, et al. A retrospective evaluation of subsurface monopolar radiofrequency for lifting of the face, neck, and jawline. Dermatol Surg. 2016;42:1261–1265. [DOI] [PubMed] [Google Scholar]
- 30.Jones IT Guiha I Goldman MP, et al. A randomized evaluator-blinded trial comparing subsurface monopolar radiofrequency with microfocused ultrasound for lifting and tightening of the neck. Dermatol Surg. 2017;43:1441–1447. [DOI] [PubMed] [Google Scholar]
- 31.Sanan A Hjelm N Tassone P, et al. Thermistor-controlled subdermal skin tightening for the aging face: clinical outcomes and efficacy. Laryngoscope Investig Otolaryngol. 2019;4:18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dayan E, Ramirez H, Theodorou S. Radiofrequency treatment of labia minora and majora: a minimally invasive approach to vulva restoration. Plast Reconstr Surg Glob Open. 2020;8:e2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chia CT Marte JA Ulvila DD, et al. Second generation radiofrequency body contouring device: safety and efficacy in 300 local anesthesia liposuction cases. Plast Reconstr Surg Glob Open. 2020;8:e3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dayan E Theodorou S Rohrich RJ, et al. Aesthetic applications of radiofrequency: lymphatic and perfusion assessment. Plast Reconstr Surg Glob Open. 2020;8:e3193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen S Dominsky O Artzi O, et al. Deep layer radiofrequency thermo-coagulative technology for cervicofacial contouring: sonographic and clinical results. Plast Reconstr Surg Glob Open. 2020;8:e3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cook J, DiBernardo BE, Pozner JN. Bipolar radiofrequency as an adjunct to face and body contouring: a 745-patient clinical experience. Aesthet Surg J. 2021;41:685–694. [DOI] [PubMed] [Google Scholar]
- 37.Han X Yang M Yin B, et al. The efficacy and safety of subcutaneous radiofrequency after liposuction: a new application for face and neck skin tightening. Aesthet Surg J. 2021;41:NP94–NP100. [DOI] [PubMed] [Google Scholar]
- 38.Demesh D Cristel RT Gandhi ND, et al. The use of radiofrequency-assisted lipolysis with radiofrequency microneedling in premature jowl and neck laxity following facialplasty. J Cosmet Dermatol. 2021;20:93–98. [DOI] [PubMed] [Google Scholar]
- 39.Turer DM, James IB, DiBernardo BE. Temperature-controlled monopolar radiofrequency in the treatment of submental skin laxity: a prospective study. Aesthet Surg J. 2021;41:NP1647–NP1656. [DOI] [PubMed] [Google Scholar]
- 40.Dayan E Rovatti P Aston S, et al. Multimodal radiofrequency application for lower face and neck laxity. Plast Reconstr Surg Glob Open. 2020;8:e2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mulholland RS. BodyTite. Available at: https://www.intechopen.com/books/the-art-of-body-contouring/bodytite-sup-sup-the-science-and-art-of-radiofrequency-assisted-lipocoagulation-rfal-in-body-contour. Accessed June 30, 2021.
- 42.Hurwitz DJ, Wright L. Noninvasive abdominoplasty. Clin Plast Surg. 2020;47:379–388. [DOI] [PubMed] [Google Scholar]
- 43.Conflict of Interest. JAMA . 2017;317:1707–1812. [DOI] [PubMed] [Google Scholar]
- 44.Luce EA. Financial conflicts of interest in plastic surgery: background, potential for bias, disclosure, and transparency. Plast Reconstr Surg. 2015;135:1149–1155. [DOI] [PubMed] [Google Scholar]
- 45.Swanson E, Brown T. A discussion of conflicts of interest in plastic surgery and possible remedies. Plast Reconstr Surg Glob Open. 2018;6:e2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swanson E, Bloom RJ. It is time for plastic surgeons to start picking up the tab. Ann Plast Surg. 2020;85:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DeJong C Aguilar T Tseng CW, et al. Pharmaceutical industry sponsored meals and physician prescribing patterns for Medicare beneficiaries. JAMA Intern Med. 2016;176:1114–1122. [DOI] [PubMed] [Google Scholar]
- 48.Sunshine Act. Available at: https://www.policymed.com/2013/02/physician-payment-sunshine-act-top-50-things-to-know.html. Accessed July 1, 2021.
- 49.Dollars for Docs. Available at: https://projects.propublica.org/docdollars/. Accessed July 1, 2021.
- 50.Swanson E. Concerns regarding photographic representation of the results of radiofrequency treatment. Aesthet Surg J. 2019;39:NP354–NP356. [DOI] [PubMed] [Google Scholar]
- 51.Swanson E. Does radiofrequency assistance improve skin contraction after liposuction? Plast Reconstr Surg Glob Open. 2015;3:e545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Realself. Find the right cosmetic procedure . Available at: https://www.realself.com/procedures. Accessed July 1, 2021.
- 53.Locketz GD, Bloom JD. Percutaneous radiofrequency technologies for the lower face and neck. Facial Plast Surg Clin N Am. 2019;27:305–320. [DOI] [PubMed] [Google Scholar]
- 54.Dibernardo GA DiBernardo BE Wu D, et al. Marginal mandibular nerve mapping prior to nonablative radiofrequency skin tightening. Aesthet Surg J. 2021;41:218–223. [DOI] [PubMed] [Google Scholar]
- 55.Kinney BM Andriessen A DiBernardo BE, et al. Use of a controlled subdermal radio frequency thermistor for treating the aging neck: consensus recommendations. J Cosmet Laser Ther. 2017;19:444–450. [DOI] [PubMed] [Google Scholar]
- 56.Araco A. A case report of deep skin burns following radiofrequency-assisted liposculpting technology of BodyTite. Dermatol Ther. 2020;33:e13683. [DOI] [PubMed] [Google Scholar]
- 57.Guidance for Institutional Review Boards and Clinical Investigators. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions. Accessed July 1, 2021.
- 58.510(k) Premarket Notification. Available at: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K163190. Accessed July 2, 2021.
- 59.Medical Device Reporting for Manufacturers. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/medical-device-reporting-manufacturers. Accessed July 2, 2021.
- 60.MAUDE — Manufacturer and User Facility Device Experience. Available at: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/results.cfm. Accessed July 2, 2021.
- 61.Standard Postage Stamp Size. Available at: https://postagestamps101.com/standard-postage-stamp-size/. Accessed July 1, 2021.
- 62.Swanson E. Outcome analysis in 93 facial rejuvenation patients treated with a deep-plane face lift. Plast Reconstr Surg. 2011;127:823–834. [DOI] [PubMed] [Google Scholar]
- 63.Swanson E. Prospective outcome study of 360 patients treated with liposuction, lipoabdominoplasty, and abdominoplasty. Plast Reconstr Surg. 2012;129:965–978. [DOI] [PubMed] [Google Scholar]
- 64.Swanson E. Prospective clinical study of 551 cases of liposuction and abdominoplasty performed individually and in combination. Plast Reconstr Surg Glob Open. 2013;1:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]


