Purpose of review
HIV-1 controller individuals represents a model that can be useful for the development of novel vaccines and therapies. Initial studies pointed to the involvement of improved adaptive immunity, however, new emerging evidence suggests the contribution of innate cells to effective antiviral responses in spontaneous controllers. Therefore, understanding the alterations on innate cell subsets might be crucial to develop new effective therapeutic strategies.
Recent findings
Among different innate immune cells, dendritic cell (DC) and natural killer (NK) cell are essential for effective antiviral responses. DC from controllers display improved innate detection of HIV-1 transcripts, higher induction of interferons, higher antigen presenting capacities and increased metabolism and higher capacities to induce polyfunctional CD8+ T-cell responses. Such properties have been mimicked by Toll-like receptor ligands and applied to DC-based immunotherapies in humans and in animal models. NK cells from controllers display higher expression of activating receptors promoting increased antibody-dependent cellular cytotoxicity (ADCC) and natural cytotoxicity activities. Neutralizing antibodies in combination with interleukin-15 superagonist or interferon-α can increase ADCC and cytotoxicity in NK cells from HIV-1 progressors.
Summary
Mimicking DC and NK cell innate profiles in controllers has become a promising strategy to step forward a novel efficient immunotherapy against the HIV-1 infection.
Keywords: controllers, dendritic cell, HIV-1, innate immunity, natural killer cell
INTRODUCTION
Spontaneous immune control of HIV-1 infection occurs in rare and heterogenous populations of infected individuals, which are capable of controlling viral replication in plasma to low (viremic controllers; VC) or undetectable (elite controllers; EC) and represents a proof-of-concept that can be useful for the development of future vaccines and therapies. Initial studies pointed to the involvement of improved adaptive immunity activated by protective polymorphic Human Leukocyte Antigen (HLA)-B alleles, effective cytotoxic and polyfunctional CD8+ T cells capable of eliminating infected cells, and intrinsic resistance of CD4+ T cells to HIV-1 [1–7]. However, during the last few years, new emerging evidence suggests the contribution of innate immune cells to immune control in HIV-1 controllers. Innate immune cells comprise a heterogeneous group of cell subsets, such as myeloid cells and natural killer (NK) cells, that are critical to induce antiviral responses [8,9].
Box 1.
no caption available
INNATE IMMUNE RESPONSE IN NATURAL HIV-1 CONTROLLERS
Myeloid cells possess multiple pattern recognition receptors (PRRs), including Toll-like receptors (TLR), RIG-I-like receptors (RLR), C type lectin receptors (CLR), intracellular DNA and RNA sensors and inflammasome components that are capable of recognizing conserved pathogen-associated molecular patterns (PAMPs) [10,11]. Recognition of PAMPs by these PRRs activates a complex network of signaling pathways leading to the production of pro-inflammatory cytokines and type I and III interferons (IFNs), finally stimulation of other innate cells and modulating the adaptive immune response [12]. Progressive HIV-1 infection leads to immune dysfunction affecting both the adaptive but also the innate fraction, even in the presence of antiretroviral treatment [13,14]. However, different innate responses mediated by myeloid cells and NK cells have been detected in HIV-1 controllers [15]. In addition, HIV-1 controllers have been considered a model to develop new effective immunotherapies and vaccines to prevent or eradicate HIV-1 infection. Here, we will review the most recent advances on the understanding of altered molecular and cellular mechanisms of innate immune responses in HIV-1 controllers, specially focusing on dendritic cells and NK cells and how they can be modulated to mimic HIV-1 controllers for new preventive and therapeutic strategies.
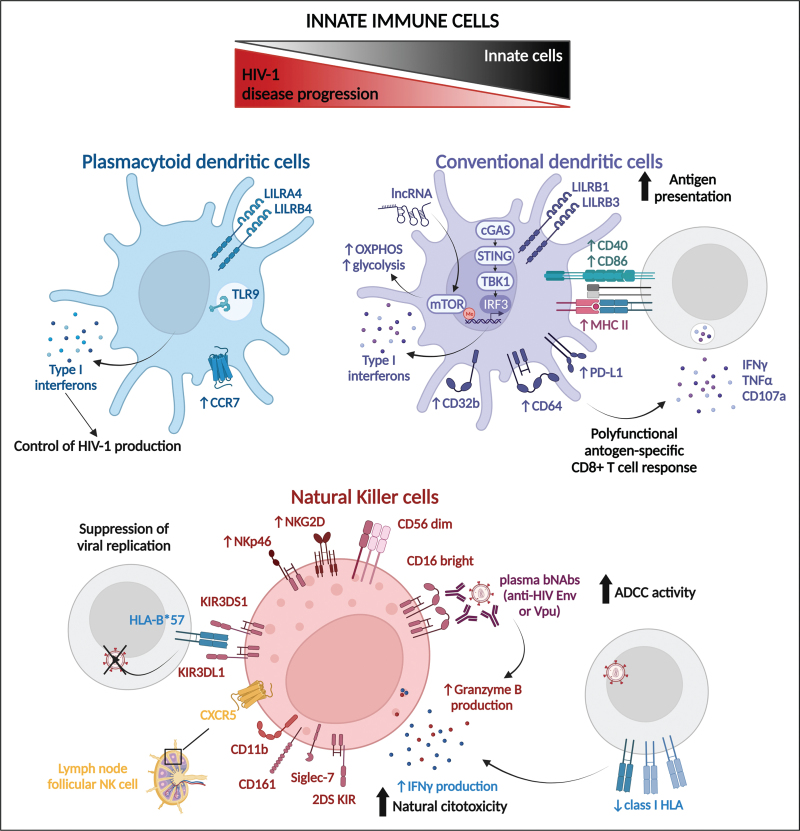
Role of dendritic cells
Dendritic cells (DCs) are professional antigen presenting cells which mediate both activation and polarization of T lymphocytes, therefore playing a critical role in specific adaptive immunity [10,16–18]. DCs can be subdivided into conventional (cDC) and plasmacytoid (pDC) dendritic cells, according to their function. cDC comprise CD1c+ and CD141+ subsets, which display different abilities to stimulate CD4+ and CD8+ T cells, respectively. A reduction of cDC frequencies present in blood correlate with HIV-1 disease progression, however, frequencies are preserved in EC even in comparison to people living with HIV-1 (PLWH) on antiretroviral treatment [11,19]. Interestingly, circulating cDC from EC display higher capacities of antigen presentation associated with higher expression of activating immunomodulatory receptors such as Leukocyte Immunoglobulin-Like Receptor subfamily B (LILRB1) and LILRB3 [20]. Previous studies reported that improved detection of HIV-1 transcripts by the Cyclic GMP-AMP Synthase pathway in cDC which might contribute to activation of CD8+ T cells in HIV-1 controllers [5,21]. Subsequent transcriptional studies at the single-cell level identified an activation state of circulating cDC from EC characterized by high interferon gene expression signatures regulated by TANK-Binding Kinase 1, co-expression of high levels of CD64 and Programmed Death-Ligand 1 (PD-L1) and superior functional capacities to activate polyfunctional HIV-1-specific CD8+ T cell responses [6]. Of note, LN CD1c+ cDC expressing PD-L1+ were also shown to modulate HIV-1 transcription in CD4+ T cells in lymph node of treated aviremic HIV-infected individuals [22], which may be also relevant for immune control, but their role in lymphoid tissue from EC has not been investigated in detail. Interestingly, a recent study identified the upregulation of a long coding RNA in DC from peripheral blood as the key element associated to the immunometabolic induction after TLR3 stimulation, suggesting that differences from EC to normal progressors could be influenced by epigenetic changes leading to trained DCs [23▪▪,24]. In addition, a mass cytometry analysis identified a subpopulation of circulating CD1c+ cDC highly enriched in EC that was characterized by co-expression of high levels of HLA-DR and the inhibitory Fc receptor CD32b [19]. Interestingly, CD1c+cDC from peripheral blood can also promote effective humoral responses against HIV-1 and the induction of broadly neutralizing antibodies in viremic controllers (VC) thanks to higher abilities to secrete IL-6 and IL-12 [17]. Therefore, improved host-restriction of HIV-1 replication and increased innate activation of CD1c+ cDC, which seems to be associated with improved activation of protective CD8+ T-cell responses (Fig. 1). In contrast, although peripheral blood CD141+ cDC were initially reported to be more resistant to HIV-1 infection [25], their potential contribution to natural control of HIV-1 has not been explored.
FIGURE 1.
Schematic representation of main features of innate cells from HIV-1 controllers. Graphical representation of the main phenotypical characteristics and functional responses identified on plasmacytoid dendritic cells (in blue), conventional dendritic cells (purple) and natural killer cells (red) from HIV-1 controllers.
On the other hand, pDC are very effective secreting high levels of type I IFNs and are critical to induce immune responses to viral infections [11,19]. Reduced frequencies of pDC present in blood also correlates with HIV-1 disease progression and in in PLWH on antiretroviral treatment, and are also enriched in EC [11,19,26]. Furthermore, a specific pDC subpopulation co-expressing high levels of LILRA4 and LILRB4 negatively correlating with blood viral load was enriched in EC compared to progressor individuals with primary HIV-1 infection, in agreement with previous in vitro experiments that showed that pDC from EC displayed higher abilities to inhibit HIV-1 production by infected cells [19,27]. Interestingly, a recent study described higher proportions of pDC expressing the tissue homing marker CCR7 in blood of EC [26]. Moreover, a rhesus macaque model showed a negative correlation between frequencies of pDC and percentage of pDC synthesizing IFN-α, and the percentage of NK cells, CD4+ T cells and CD8+ T cells expressing interleukin (IL)-17 [28]. To summarize, DC, and particularly CD1c+ cDC, may play an essential role in the HIV-1 control in EC as they modulate the specific adaptive immune response towards a more effective phenotype (Fig. 1).
Natural killer cells
NK cells are crucial due to their cytotoxic capacity of elimination of virus-infected cells as well as their ability to modulate immune responses through cytokine production [29]. Different NK cell subsets are defined according to their CD56 and CD16 expression. CD56 dim CD16 bright NKs are characterized by high cytotoxic capacities mediating antibody-dependent cellular cytotoxicity (ADCC). On the other hand, the CD56 bright CD16 dim NK cell subpopulation is responsible for immunomodulatory functions [30,31]. Finally, CD56 negative NK cells have been linked to memory-like NK cells responses but in HIV-1 infection this subset is characterized by dysfunctional cytotoxic activity and positively correlates with disease progression [32]. In fact, lack of expression of NKG2C, a marker associated with memory NK, has been associated with lower HIV-1 viral load set point [33]. In addition, recent studies in rhesus macaques described the existence of adaptive NK cells against the Simian Immunodeficiency Virus (SIV), pointing to the possibility to generate HIV-specific trained NK cells as a therapy [21,34]. Therefore, the role of adaptive memory-like NK cells in natural control of HIV-1 remains unclear. A recent study comparing distribution of the distinct NK cell subpopulations in EC versus viremic, PLWH on Antiretroviral therapy (ART) and HIV-negative controls, described similar proportions of cytotoxic CD56 dim CD16+ subpopulation in EC and HIV-negative individuals, whereas viremic PLWH displayed lower proportions of this NK cell subset. Within this population, a subpopulation characterized by CD11b+ CD57− CD161+ Siglec-7+, was significantly enriched in EC, and displayed higher expression of IFN-γ after IL-12/IL-18 stimulation and also higher ADCC activity in vitro to a target cell line [35]. In this regard, a study identified higher levels of plasma HIV-1 Env-specific and Vpu epitope-specific antibodies in EC compared to viremic individuals, which were capable of mediating activation and granzyme B production in an NK cell line, suggesting higher effectiveness of ADCC mediated by Env and Vpu epitope [36]. And another study identified that plasma HIV-1 gp140 antibodies present in long-term nonprogressors PLWH increased ADDC activity of NK cells from HIV-1-negative donors against reactivated latently HIV-infected cells [37]. Furthermore, NK cells express both activating and inhibitory receptors, and the proportion of ligands of one or another on the target cell determines the fate of the NK cell response. Inhibitory receptors repress cytotoxic activity of NK cells against target cells. However, downregulation of the class I HLA in the target cell can activate cytotoxic function in NK cells. In this regard, killer immunoglobulin-like receptors (KIRs) are expressed on the surface of NK cells and can regulate activating or inhibitory signals through binding to class I HLA molecules. One study identified higher expression of HLA-C C2, which has been associated to control of viremia and slower disease progression, and their 2DS KIR receptor ligands in peripheral blood from EC but not long term nonprogressors [38]. In addition, two different studies identified higher expression of NKG2D on circulating NK cells from EC, compared to PLWH, and less downregulation of NKG2D ligands by HIV-1 Nef, which leads to increased susceptibility of CD4+ infected cells to ADCC [39,40▪]. On the contrary, higher expression NKp46 activating receptor has been reported in circulating NK cells from EC [21]. Finally, interaction between protective HLA-B∗57 and KIR3DL1 and KIR3DS1 in EC can suppress viral replication [21,41▪]. HLA-B∗57 has also been reported to play a role in viral control by CD8+ T cells, and although no evidence of synergy has yet been found, it highlights the importance of NK cells responses on EC to maintain viral control. Furthermore, lymph node CXCR5+ NK cells from this macaque model, which correlated with plasma viral load, exhibited higher expression of Fcγ receptors, pointing to higher ADCC functionality not only in blood but also in tissue, in combination with enhances IL-12 and IL-15 signaling [42▪▪]. In conclusion, NK cells seem to play a significant role restraining HIV-1 progression in controllers independently of protective adaptive immune responses (Fig. 1).
POTENTIAL IMPLICATIONS FOR NOVEL HIV-1 CURE STRATEGIES
Previous tested immunotherapies against HIV-1 did not efficiently prevent viral rebound after treatment interruption [43,44], pointing to the need to module and fine-tune innate immune cells contributing to antiviral responses such as DCs and NK cells to mimic antiviral immunity in controllers [15,21,45,46]. Due to the important contribution of innate responses in natural viral control in EC, recent strategies have tried to mimic the enhanced antiviral function of DC and NK cell states in preventive and therapeutic purposes by either inducing an EC-like trained immunity state or by other alternative strategies [47]. DC have been used as a tool to induce cytotoxic CD8+ T cells for immunotherapeutic approaches in cancer and vaccines to approach HIV-1 prevention and eradication [48].
Some strategies have focused on inducing high levels of IFN-pathways by using TLR or intracellular sensor agonist [49,50]. For example, TLR7 has been the most extensively used agonist as it could lead to the production of IFN-α through IRF7 activation or other pro-inflammatory cytokines through nuclear factor (NF)-κB activation [51]. In a SHIV-infected monkey study by Borducchi et al.[52] delayed viral rebound was described when bNAbs were administered together with a TLR7 agonist. Although another nonhuman primate vaccine model using the TLR7 agonist did not prevent viral rebound despite inducing immune responses against the vaccine [53]. Studies using a TLR 7/8 agonist in combination with HIV-1 Env peptides in a nonhuman primate model described increased magnitude and durability of the HIV-1-specific antibody response [54]. However, these previous studies administered the TLR agonist systemically instead of targeting DCs. Stunnenberg et al.[55▪] used a TLR7/8 agonist in combination with abortive HIV-1 RNA in order to stimulate DCs. This led to enhanced adaptive responsiveness through T helper 1 responses and increased IFN-γ production by CD8+ T cells in vitro. In addition, a TLR7 agonist, in combination with a TLR9 agonist, improved antigen presentation and increased lymph node homing markers on pDC in an HCV model [56].
Moreover, additional TLR agonists have also shown promising results. An HIV-1 Env vaccine directed to the CD40 receptor of antigen presenting cells and in combination with a TLR9 adjuvant in a humanized mouse model, displayed higher immunoglobulin G (IgG) production together with more structured architecture in the spleen, containing both B and Tfh-like cells expressing PD-1 and BCL-6 [57]. Cheng et al.[58] also directed the vaccination against CD40+ cells using poly (I:C) as TLR3 agonist and a combination of peptides from HIV-1 Gag, Nef and Pol, and described less HIV-1 reservoir in lymphoid tissue and delayed viral rebound. Furthermore, the use of the TLR3 agonist in combination with a STING agonist and HIV-1 Gag peptides to activate DC ex vivo potentiate the acquisition of EC-like functional profiles and their ability to increase polyfunctional HIV-1-specific CD8+ T cell responses in lymphoid tissues in humanized BLT mice and reduced depletion of CD4+ T cells after infection with HIV-1 [59]. In addition, TLR3 also increased responsiveness of CD141+ cDC against the Simian Immunodeficiency Virus in a rhesus macaque model [60].
In the context of chronic HIV-1 infection, antigen presentation by unstimulated DC has not been effective and therefore strategies boosting innate cells specifically using adjuvants directed to TLRs have been developed [49,50]. Consistent with previous studies, exhausted CD8+ T cells might remain dysfunctional after DC-vaccination and functional restoration might require additional modulation such as the use of checkpoint receptor blockade. In this sense, in vitro restoration of polyfunctional HIV-1-specific CD8+ T cell from PLWH on ART after treatment with autologous DC primed with TLR3 agonist in and STING agonist is determined by treatment duration and the co-expression of different PD1, TIGIT and TIM3 checkpoint receptors and reduced mitochondrial respiration and glycolysis. In this study, authors were able to improve response to autologous DCs by combining with checkpoint receptor blockade and a glycolysis promoting drug [61]. Finally, a recent study in nonhuman primates using TLR4 agonist formulated with saponin described higher induction of responses in the lymph nodes due to its capacity to enter draining lymph nodes [62].
NK cells can be activated through cytokines in the environment or directly by some TLR agonists, and its ADCC activity can be promoted by the presence of neutralizing antibodies [63]. Several studies have described that the stimulation of NK cells with IL-15 improves ADCC activity, natural cytotoxicity and IFN-γ production in vitro in PLWH on antiretroviral therapy [64,65]. An in vivo model studying the efficacy of a broadly neutralizing construct specific for both CD4 and HIV-1 gp120 co-receptor binding sites evaluated the ADCC activity comparing mice infected and injected with total PBMCs or mice infected and injected with PBMCs where CD56+ fraction had been depleted. The study described a dramatic increase on the cytotoxic function against infected cells in just 1 day after receiving the treatment. Moreover, efficacy of the construct increased when combined with an IL-15 superagonist [66▪]. A different strategy using IFN-α to prestimulate NK cells described increased NK-mediated clearance of HIV-infected cells by ADDC using either broadly neutralizing targeting gp120 or naturally occurring antibodies. Furthermore, activated NK cells expressing NKp46 and NKG2D increased direct cytotoxicity in this strategy dependently of MHC-I downregulation [67]. Another study used IFN-α to stimulate NK cells in vitro, and described an increase in the cytokine secretion, the polyfunctionality, the degranulation and the cytotoxic potential of NK cells from PLWH, therefore, mimicking the viral suppressive capacity of NK cells from EC. Moreover, IFN-α induced the release of cytokines by NK which in its turn leaded to a global cytokine response of CD8+ T cells from PLWH, meaning that strategies aiming to improve CD8+ T cell function and NK function are not exclusive [68]. Finally, a different strategy to potentiate ADCC from NK cells is the use of nanoparticles conjugated with IgG antibodies specific for HIV-1 gp120 and human CD16. This strategy triggered a potent ADCC cytotoxic response against HIV-infected CD4+ T cells and efficiently reduced latently infected cells after viral reactivation in vitro[69]. In addition, CD155 expression by T cells combined with NKG2D expression on NK cells has been described to increase cytotoxic capacities to eliminate HIV-infected cells in vitro[70]. On the other hand, blockade of the inhibitory checkpoint inhibitory receptor TIGIT on NK cells, which is the ligand of CD155, increases NK cell activity against HIV-1 infected CD4+ T cells in PWH in vitro[71].
CONCLUSION
Together, mimicking DC and NK cell activation states in controllers has become a promising strategy to step forward a novel efficient immunotherapy against the HIV-1 infection.
Acknowledgements
Graphical schematic representations were created with BioRender.com.
Financial support and sponsorship
E.M.G. was supported by the Ramón y Cajal Program (RYC2018-024374-I), the MINECO/FEDER RETOS program (RTI2018-097485-A-I00), Comunidad de Madrid Talento Program (2017-T1/BMD-5396), Gilead becas de investigación (GLD19/00168), by Centro de Investigación Biomédica en Red (CIBERINF) de Enfermedades Infecciosas (CB21/13/00107), La Caixa Banking Foundation (H20-00218) and by REDINCOV grant from Fundació La Marató TV3. M.C.M. was supported by La Caixa Banking Foundation (H20-00218) and Gilead becas de investigación (GLD19/00168).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Salgado M, Swanson MD, Pohlmeyer CW, et al. HLA-B∗57 elite suppressor and chronic progressor HIV-1 isolates replicate vigorously and cause CD4+ T cell depletion in humanized BLT mice. J Virol 2014; 88:3340–3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shasha D, Walker BD. Lessons to be learned from natural control of HIV − future directions, therapeutic, and preventive implications. Front Immunol 2013; 4:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buzon MJ, Yang Y, Ouyang Z, et al. Susceptibility to CD8 T-cell-mediated killing influences the reservoir of latently HIV-1-infected CD4 T cells. J Acquir Immune Defic Syndr 2014; 65:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klingler J, Paul N, Laumond G, et al. Distinct antibody profiles in HLA-B∗57+, HLA-B∗57- HIV controllers and chronic progressors. AIDS 2022; 36:487–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin-Gayo E, Buzon MJ, Ouyang Z, et al. Potent cell-intrinsic immune responses in dendritic cells facilitate HIV-1-specific T cell immunity in HIV-1 elite controllers. PLoS Pathog 2015; 11:e1004930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin-Gayo E, Cole MB, Kolb KE, et al. A reproducibility-based computational framework identifies an inducible, enhanced antiviral state in dendritic cells from HIV-1 elite controllers. Genome Biol 2018; 19:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen S, Deleage C, Darko S, et al. Elite control of HIV is associated with distinct functional and transcriptional signatures in lymphoid tissue CD8+ T cells. Sci Transl Med 2019; 11:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bekkering S, Dominguez-Andres J, Joosten LAB, et al. Trained immunity: reprogramming innate immunity in health and disease. Annu Rev Immunol 2021; 39:667–693. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald KA, Kagan JC. Toll-like receptors and the control of immunity. Cell 2020; 180:1044–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin-Gayo E, Yu XG. Role of dendritic cells in natural immune control of HIV-1 infection. Front Immunol 2019; 10:1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi Y, Su J, Chen R, et al. The role of innate immunity in natural elite controllers of HIV-1 infection. Front Immunol 2022; 13:780922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carty M, Guy C, Bowie AG. Detection of viral infections by innate immunity. Biochem Pharmacol 2021; 183:114316. [DOI] [PubMed] [Google Scholar]
- 13.Martin GE, Frater J. Posttreatment and spontaneous HIV control. Curr Opin HIV AIDS 2018; 13:402–407. [DOI] [PubMed] [Google Scholar]
- 14.Fenwick C, Joo V, Jacquier P, et al. T-cell exhaustion in HIV infection. Immunol Rev 2019; 292:149–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Board NL, Moskovljevic M, Wu F, et al. Engaging innate immunity in HIV-1 cure strategies. Nat Rev Immunol 2021; [Online ahead of print]. [DOI] [PubMed] [Google Scholar]
- 16.O’Keeffe M, Mok WH, Radford KJ. Human dendritic cell subsets and function in health and disease. Cell Mol Life Sci 2015; 72:4309–4325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin-Gayo E, Gao C, Chen HR, et al. Immunological fingerprints of controllers developing neutralizing HIV-1 antibodies. Cell Rep 2020; 30:984.e4–996.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jenabian MA, Patel M, Kema I, et al. Soluble CD40-ligand (sCD40L, sCD154) plays an immunosuppressive role via regulatory T cell expansion in HIV infection. Clin Exp Immunol 2014; 178:102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coindre S, Tchitchek N, Alaoui L, et al. Mass cytometry analysis reveals complex cell-state modifications of blood myeloid cells during HIV infection. Front Immunol 2019; 10:2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang J, Burke PS, Cung TDH, et al. Leukocyte immunoglobulin-like receptors maintain unique antigen-presenting properties of circulating myeloid dendritic cells in HIV-1-infected elite controllers. J Virol 2010; 84:9463–9471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sugawara S, Reeves RK, Jost S. Learning to be elite: lessons from HIV-1 controllers and animal models on trained innate immunity and virus suppression. Front Immunol 2022; 13:858383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banga R, Rebecchini C, Procopio FA, et al. Lymph node migratory dendritic cells modulate HIV-1 transcription through PD-1 engagement. PLoS Pathog 2019; 15:e1007918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪▪.Hartana CA, Rassadkina Y, Gao C, et al. Long noncoding RNA MIR4435-2HG enhances metabolic function of myeloid dendritic cells from HIV-1 elite controllers. J Clin Invest 2021; 131:e146136. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes the role of a long coding RNA in dendritic cells of HIV-1 controllers enhancing their metabolism possibly through trained immunity.
- 24.Fanucchi S, Domínguez-Andrés J, Joosten LAB, et al. The Intersection Of Epigenetics And Metabolism In Trained Immunity. Immunity 2021; 54:32–43. [DOI] [PubMed] [Google Scholar]
- 25.Silvin A, Yu CI, Lahaye X, et al. Constitutive resistance to viral infection in human CD141+ dendritic cells. Sci Immunol 2017; 2:eaai8071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dominguez-Molina B, Ferrando-Martinez S, Tarancon-Diez L, et al. Immune correlates of natural HIV elite control and simultaneous HCV clearance-supercontrollers. Front Immunol 2018; 9:2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Machmach K, Leal M, Gras C, et al. Plasmacytoid dendritic cells reduce HIV production in elite controllers. J Virol 2012; 86:4245–4252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khowawisetsut L, Pattanapanyasat K, Onlamoon N, et al. Relationships between IL-17(+) subsets, Tregs and pDCs that distinguish among SIV infected elite controllers, low, medium and high viral load rhesus macaques. PLoS One 2013; 8:e61264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Björkström NK, Strunz B, Ljunggren HG. Natural killer cells in antiviral immunity. Nat Rev Immunol 2022; 22:112–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cianga VA, Campos Catafal L, Cianga P, et al. Natural killer cell subpopulations and inhibitory receptor dynamics in myelodysplastic syndromes and acute myeloid leukemia. Front Immunol 2021; 12:665541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campbell JJ, Qin S, Unutmaz D, et al. Unique subpopulations of CD56+ NK and NK-T peripheral blood lymphocytes identified by chemokine receptor expression repertoire. J Immunol 2001; 166:6477–6482. [DOI] [PubMed] [Google Scholar]
- 32.Cao WJ, Zhang XC, Wan LY, et al. Immune dysfunctions of CD56 neg NK cells are associated with HIV-1 disease progression. Front Immunol 2022; 12:811091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alsulami K, Bolastig N, Dupuy FP, et al. Influence of NKG2C genotypes on HIV susceptibility and viral load set point. J Virol 2021; 95:e0041721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ram DR, Manickam C, Lucar O, et al. Adaptive NK cell responses in HIV/SIV infections: a roadmap to cell-based therapeutics? J Leukoc Biol 2019; 105:1253–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pohlmeyer CW, Gonzalez VD, Irrinki A, et al. Identification of NK cell subpopulations that differentiate HIV-infected subject cohorts with diverse levels of virus control. J Virol 2019; 93:1790–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Madhavi V, Wines BD, Amin J, et al. HIV-1 Env- and Vpu-specific antibody-dependent cellular cytotoxicity responses associated with elite control of HIV. J Virol 2017; 91: e00700-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dhande JR, Bagul RD, Thakar MR. HIV-gp140-specific antibodies generated from indian long-term non-progressors mediate potent ADCC activity and effectively lyse reactivated HIV reservoir. Front Immunol 2022; 13:844610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malnati MS, Ugolotti E, Monti MC, et al. Activating killer immunoglobulin receptors and HLA-C: a successful combination providing HIV-1 control. Sci Rep 2017; 7:42470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alsahafi N, Richard J, Prévost J, et al. Impaired downregulation of NKG2D ligands by nef proteins from elite controllers sensitizes HIV-1-infected cells to antibody-dependent cellular cytotoxicity. J Virol 2017; 91: e00109-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪.Zhang Z, Zhou Y, Lu J, et al. Changes in NK cell subsets and receptor expressions in HIV-1 infected chronic patients and HIV controllers. Front Immunol 2021; 12:792775. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study compares expression of different receptors in NK cell from controllers vs chronic PLWH.
- 41▪.May ME, Pohlmeyer CW, Kwaa AK, et al. Combined effects of HLA-B∗57/5801 elite suppressor CD8+ T cells and NK cells on HIV-1 replication. Front Cell Infect Microbiol 2020; 10:113. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes a nonexclusive protective role of HLA-B∗57 in NK cells and CD8+ T cells.
- 42▪▪.Rahman SA, Billingsley JM, Sharma AA, et al. Lymph node CXCR5+ NK cells associate with control of chronic SHIV infection. JCI Insight 2022; 7:e155601. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes the protective role of CXCR5+ NK cells in lymph node controlling SHIV infection in a macaque model.
- 43.Pantaleo G, Levy Y. Therapeutic vaccines and immunological intervention in HIV infection: a paradigm change. Curr Opin HIV AIDS 2016; 11:576–584. [DOI] [PubMed] [Google Scholar]
- 44.Bekerman E, Hesselgesser J, Carr B, et al. PD-1 blockade and TLR7 activation lack therapeutic benefit in chronic simian immunodeficiency virus-infected Macaques on antiretroviral therapy. Antimicrob Agents Chemother 2019; 63: e01163-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hartana CA, Yu XG. Immunological effector mechanisms in HIV-1 elite controllers. Curr Opin HIV AIDS 2021; 16:243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Walker-Sperling VEK, Cohen VJ, Tarwater PM, Blankson JN. Reactivation kinetics of HIV-1 and susceptibility of reactivated latently infected CD4+ T cells to HIV-1-specific CD8+ T cells. J Virol 2015; 89:9631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sui Y, Berzofsky JA. Myeloid cell-mediated trained innate immunity in mucosal AIDS vaccine development. Front Immunol 2020; 11:315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mohamed H, Miller V, Jennings SR, et al. The evolution of dendritic cell immunotherapy against HIV-1 infection: improvements and outlook. J Immunol Res 2020; 2020:9470102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martinsen JT, Gunst JD, Højen JF, et al. The use of toll-like receptor agonists in HIV-1 cure strategies. Front Immunol 2020; 11:1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hvilsom CT, Søgaard OS. TLR-agonist mediated enhancement of antibody-dependent effector functions as strategy for an HIV-1 cure. Front Immunol 2021; 12:704617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siddiqui MA, Yamashita M. Toll-like receptor (TLR) signaling enables cyclic GMP-AMP synthase (cGAS) sensing of HIV-1 infection in macrophages. mBio 2021; 12:e0281721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borducchi EN, Liu J, Nkolola JP, et al. Antibody and TLR7 agonist delay viral rebound in SHIV-infected monkeys. Nature 2018; 563:360–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bricker KM, Obregon-Perko V, Uddin F, et al. Therapeutic vaccination of SIV-infected, ART-treated infant rhesus macaques using Ad48/MVA in combination with TLR-7 stimulation. PLoS Pathog 2020; 16:e1008954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kasturi SP, Ur Rasheed MA, Havenar-Daughton C, et al. 3M-052, a synthetic TLR-7/8 agonist, induces durable HIV-1 envelope-specific plasma cells and humoral immunity in nonhuman primates. Sci Immunol 2020; 5:eabb1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55▪.Stunnenberg M, van Hamme JL, Zijlstra-Willems EM, et al. Crosstalk between R848 and abortive HIV-1 RNA-induced signaling enhances antiviral immunity. J Leukoc Biol 2022; Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]; This in vitro study describes the enhancement of adaptive responses with the combined use of a TLR7/8 agonist plus abortive HIV-1 RNA.
- 56.Dominguez-Molina B, Machmach K, Perales C, et al. Toll-like receptor 7 (TLR-7) and TLR-9 agonists improve hepatitis C virus replication and infectivity inhibition by plasmacytoid dendritic cells. J Virol 2018; 92: e01219-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Godot V, Tcherakian C, Gil L, et al. TLR-9 agonist and CD40-targeting vaccination induces HIV-1 envelope-specific B cells with a diversified immunoglobulin repertoire in humanized mice. PLoS Pathog 2020; 16:e1009025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cheng L, Wang Q, Li G, et al. TLR3 agonist and CD40-targeting vaccination induces immune responses and reduces HIV-1 reservoirs. J Clin Invest 2018; 128:4387–4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Calvet-Mirabent M, Claiborne DT, Deruaz M, et al. Poly I:C and STING agonist-primed DC increase lymphoid tissue polyfunctional HIV-1-specific CD8 + T cells and limit CD4 + T-cell loss in BLT mice. Eur J Immunol 2022; 52:447–461. [DOI] [PubMed] [Google Scholar]
- 60.Dutertre CA, Jourdain JP, Rancez M, et al. TLR3-responsive, XCR1+, CD141(BDCA-3)+/CD8α+-equivalent dendritic cells uncovered in healthy and simian immunodeficiency virus-infected rhesus macaques. J Immunol 2014; 192:4697–4708. [DOI] [PubMed] [Google Scholar]
- 61.Calvet-Mirabent M, Sánchez-Cerrillo I, Martín-Cófreces N, et al. Antiretroviral therapy duration and immunometabolic state determine efficacy of ex vivo dendritic cell-based treatment restoring functional HIV-specific CD8+ T cells in people living with HIV. EBioMedicine 2022; 81:104090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Silva M, Kato Y, Melo MB, et al. A particulate saponin/TLR agonist vaccine adjuvant alters lymph flow and modulates adaptive immunity. Sci Immunol 2021; 6:eabf1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Duan S, Liu S. Targeting NK cells for HIV-1 treatment and reservoir clearance. Front Immunol 2022; 13:692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Garrido C, Abad-Fernandez M, Tuyishime M, et al. Interleukin-15-stimulated natural killer cells clear HIV-1-infected cells following latency reversal ex vivo. J Virol 2018; 92: e00235-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Seay K, Church C, Zheng JH, et al. In vivo activation of human NK cells by treatment with an interleukin-15 superagonist potently inhibits acute in vivo HIV-1 infection in humanized mice. J Virol 2015; 89:6264–6274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66▪.Bardhi A, Wu Y, Chen W, et al. Potent in vivo NK cell-mediated elimination of HIV-1-infected cells mobilized by a gp120-bispecific and hexavalent broadly neutralizing fusion protein. J Virol 2017; 91: [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes enhancement of NK cell function mediated by neutralizing HIV antibodies in vivo.
- 67.Tomescu C, Tebas P, Montaner LJ. IFN-α augments natural killer-mediated antibody-dependent cellular cytotoxicity of HIV-1-infected autologous CD4+ T cells regardless of major histocompatibility complex class 1 downregulation. AIDS 2017; 31:613–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kwaa AKR, Talana CAG, Blankson JN. Interferon alpha enhances NK cell function and the suppressive capacity of HIV-specific CD8 + T cells. J Virol 2019; 93: e01541-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Astorga-Gamaza A, Vitali M, Borrajo ML, et al. Antibody cooperative adsorption onto AuNPs and its exploitation to force natural killer cells to kill HIV-infected T cells. Nano Today 2021; 36:101056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davis ZB, Sowrirajan B, Cogswell A, et al. CD155 on HIV-infected cells is not modulated by HIV-1 Vpu and Nef but synergizes with NKG2D ligands to trigger NK cell lysis of autologous primary HIV-infected cells. AIDS Res Hum Retroviruses 2017; 33:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Holder KA, Burt K, Grant MD. TIGIT blockade enhances NK cell activity against autologous HIV-1-infected CD4 + T cells. Clin Transl Immunol 2021; 10:e1348. [DOI] [PMC free article] [PubMed] [Google Scholar]