Abstract
The use of polyunsaturated fatty acids in Attention-Deficit/Hyperactivity Disorder (ADHD) and developmental disorders has been gaining interest with preparations containing different dosages and combinations. Gamma-linolenic acid (GLA) is an ω-6 fatty acid of emerging interest with potential roles as an adjuvant anti-inflammatory agent that could be used with ω-3 PUFAs in the treatment of ADHD and associated symptoms. A narrative review was undertaken to examine the potential role(s) of the ω-6 fatty acid GLA. PubMed, Google Scholar, and Scopus were searched to examine the potential role(s) of the ω-6 fatty acid GLA as (1) an antioxidant and anti-inflammatory agent, (2) a synergistic nutrient when combined with ω-3 PUFAs, and (3) a potential etiological factor in ADHD and its treatment. The results show that GLA exerts anti-inflammatory effects by increasing dihomo-gamma-linolenic acid in immune cells. ω-3 PUFAs, such as EPA and DHA, are often co-administered with GLA because these ω-3 PUFAs may prevent the accumulation of serum arachidonic acid in response to GLA administration without limiting the storage of DGLA in immune cells. The administration of ω-3 PUFAs alone might not be sufficient to effectively treat patients with ADHD and developmental disorders. Overall studies point towards a combination of EPA and DHA with GLA in a 9:3:1 ratio appearing to be associated with ADHD symptom improvement. A combination of PUFAs may lead to better outcomes.
Keywords: attention deficit hyperactivity disorder (ADHD), brain function, brain structure, cognition, developmental, difference, gamma-linolenic acid (GLA), hyperactivity, neuro-immune, neuroinflammatory, ω-3 PUFAs, oxidative stress, wellbeing
1. Introduction
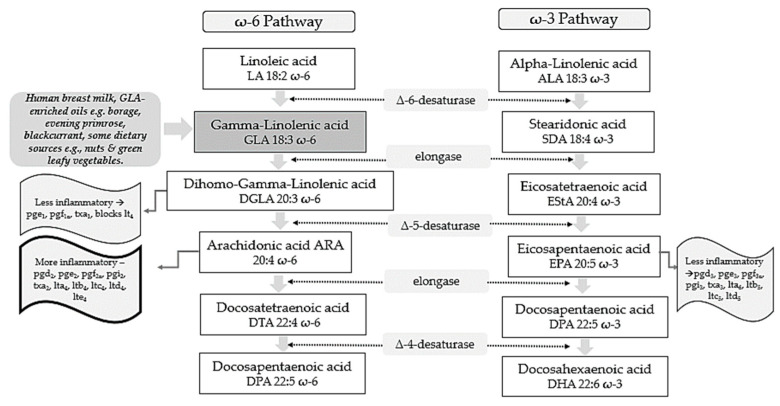
Polyunsaturated fatty acids (PUFAs) include two pathways of fatty acids—ω-3 and ω-6—which are both known to play major biological roles as structural and functional components of cell membranes and have a profound influence on the development of the central nervous system [1]. As shown in Figure 1, linoleic acid (LA) and alpha-linolenic acid (ALA) are precursors of ω-6 and ω-3 families, respectively and are regarded as essential fatty acids (EFAs) as they cannot be synthesized by the human body in amounts needed for health and wellbeing, and thus need to be supplied by diet [2,3]. These parent fatty acids yield arachidonic acid (ARA, ω-6), eicosapentaenoic acid (EPA, ω-3), and docosahexaenoic acid (DHA, ω-3) which regulate body homeostasis and act locally via bioactive signaling lipids called eicosanoids [3].
Figure 1.
ω-6 and ω-3 family pathways. Key: pg, prostaglandin; pgi, prostacyclin; tx, thromboxane; lt, leukotriene.
Studies on evolutionary aspects of human diets indicate that major changes have taken place concerning types and profiles of dietary essential fatty acids obtained [4,5]. Genetically speaking, human beings in modern life live in a nutritional environment that differs from that which gave birth to their genetic pattern back in the evolutionary history of the genus Homo [5]. Whilst the dietary ratio of ω-6 to ω-3 fatty acids was once balanced and 1 to 1, in Western lifestyles this is now around 15–17 to 1 [4]. This is in stark contrast to recommendations from national agencies which advise that an ω-6 to ω-3 ratio of 4:1 is preferable [6]. It has been reported that lowering the ω-6 to ω-3 ratio to such thresholds could reduce enzymatic metabolic competition and facilitate the metabolism of more downstream products from ALA [7].
According to the Diagnostic and Statistical Manual of Mental Disorders V Edition (DSM-V), neurodevelopmental disorders (NDDs) are defined as a group of conditions with onset in the developmental period, inducing deficits that produce impairments of functioning [8,9]. NDDs comprise intellectual disability (ID), communication disorders, autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), neurodevelopmental motor disorders, and specific learning disorders [8].
According to the DSM-V, ADHD diagnosis is based on some age-dependent symptoms of inattention and/or hyperactivity/impulsivity that interfere with functioning of development and should occur for at least 6 months [9]. ADHD is a neurodevelopmental disorder with onset in childhood, however, 50% of subjects continue to experience symptoms throughout adolescence and 30–60% in adulthood [10]. Overall pooled prevalence in the world is 7.2%; it is higher in males than in females, and it is most common in school-aged children [11]. Community prevalence of ADHD globally in children and young people has been reported to be between 2% and 7%, and an average of approximately 5% [12]. Other research reports a higher ADHD prevalence amongst boys, urban young people and those born to mothers with a history of psychiatric hospitalization [13].
These disorders typically manifest early in development, typically before a child begins school, and are characterized by developmental deficits that can impact social, personal, educational, or occupational functioning [9]. The developmental deficits can range from very specific limitations of learning or control of executive functions to global impairments of social skills or intelligence [1]. ADHD and ASD are amongst the most common neurodevelopmental disorders [1]. The impact of ADHD can have extended ramifications on academic performance, social skills, family relationships, and emotional wellbeing [14]. For some, without intervention, long-term outcomes can contribute to antisocial behavior, poor academic performance, non-medicinal drug use/addictive behavior, obesity, and reduced self-esteem [15].
The ω-3 PUFAs EPA and DHA have been considered for their potential roles in the treatment of symptoms in those affected by ADHD [16,17]. In the past, ω-6 PUFAs have been renowned for their generation of pro-inflammatory eicosanoids [3]. Subsequently, the potential benefits of ω-6 gamma linolenic acid (GLA) have been overshadowed. This standpoint changed in the 1980s when the potential anti-inflammatory effects of GLA began to generate more scientific interest [18,19,20]. It is now increasingly recognized that inflammation is a normal and innate part of human defense and tissue healing [21]. Renewed attention is therefore being given to ω-6 fatty acids, as they can regulate phagocytic capacity, cell migration and proliferation, and inflammatory mediator production [22]. This also includes a growing number of randomized controlled trials (RCTs) focusing on ω-6 fatty acids and aspects of cognitive and psychological wellbeing [23,24].
In this narrative review, we examine the potential role(s) of the ω-6 fatty acid GLA as (1) an antioxidant and anti-inflammatory agent, (2) a synergistic nutrient when combined with EPA, and (3) a potential etiological factor in ADHD and its treatment.
2. GLA as an Antioxidant and Anti-Inflammatory Molecule
GLA is composed of 18 carbon atoms with three double bonds and belongs to the category of ω-6 PUFAs [25]. GLA is present in human breast milk, a significant source for infants, and can be obtained from certain botanical seed oils and ingested from dietary supplements [25,26]. Natural sources of GLA include the oils of borage (Borago officinalis L., 20–26% GLA), black currant (Ribes nigrum L., 15–18%), and evening primrose (Oenothera biennis L., 8–12%) [25]. Some foods provide GLA in trace amounts, such as nuts and green leafy vegetables [26]. Unfortunately, GLA-rich foods are consumed in low quantities by the average person with the typical dietary intake of GLA being negligible [27].
Metabolically, as shown in Figure 1, GLA is produced in the body by the delta 6-desaturase enzyme acting on the parent fatty acid LA. It is then rapidly elongated to dihomo-gamma-linolenic acid (DGLA) by the enzyme elongase, acetylated, and incorporated into cell membrane phospholipids without resultant changes in ARA [28,29,30]. This has been demonstrated in in vivo metabolic research where GLA supplementation resulted in DGLA accumulation in neutrophil glycerolipids rather than ARA [31]. It has been postulated that this increase in DGLA relative to ARA within inflammatory cells such as neutrophils could diminish ARA metabolite biosynthesis [31]. This presents a plausible mechanism in terms of how dietary GLA could exert its anti-inflammatory effects [31].
Upon cell activation, DGLA is then released as free fatty acids (FAs) by phospholipase A2 and converted to several anti-inflammatory metabolites through competition with ARA for the enzymes cyclooxygenase (COX) and lipoxygenase (LOX) [32]. COX products from DGLA include prostaglandins 1 (PGE1), which can exert vasodilatory and anti-inflammatory actions [33,34]. 15-hydroxyeicosatrienoic acid (15-HETrE) is also the 15-lipoxygenase product of DGLA which can inhibit proinflammatory eicosanoid biosynthesis and exert anti-inflammatory properties [30,35]. The Δ-6-desaturase activity appears to be altered by various factors. For example, desaturase mRNA levels may be influenced by the quantity and composition of dietary carbohydrates, protein, fats, and micronutrients including vitamin A, B12, folate, iron, zinc, and polyphenols [36]. Reduced enzyme activity is also observed in elderly people [27]. Other work suggests that Δ-6-desaturase activity could also be reduced in young children presenting signs of dry skin, desquamation, and thickening of the skin, as well as growth failure [27].
GLA and its metabolites have also been found to influence the expression of several genes, regulating levels of gene products including matrix proteins [26]. Such gene products are thought to have central roles in immune function and programmed cell death (apoptosis) [26]. Critical associations are also proposed between ADHD and the level of oxidative stress which can induce cell membrane damage, changes in inner structure and function of proteins, and DNA structural damage which eventually culminate in ADHD development [37].
3. GLA Synergy with EPA
ARA can also be synthesized from DGLA through Δ-5 desaturase, encoded by fatty acid desaturase 1 (FADS1) within the FADS gene cluster (Figure 1). ARA and its potent eicosanoid products (prostaglandins, thromboxanes, leukotrienes, and lipoxins) play an important role in immune responses and inflammation [38]. Therefore, dietary supplementation with GLA has the capability to both increase levels of DGLA and its several anti-inflammatory metabolites, as well as ARA and its pro-inflammatory metabolic products and this might represent a therapeutic concern [25].
To counterbalance these pathways and make full use of the anti-inflammatory mechanisms of the molecule, the ω-3 long-chain-PUFAs (LC-PUFAs) EPA and DHA are often co-administered with GLA [39]. Humans supplemented with GLA, and EPA have substantially elevated blood EPA levels, but not ARA levels, suggesting that this supplement combination inhibits the development of pro-inflammatory ARA metabolites [39].
Evidence shows that 0.25 g/d EPA + DHA can block GLA-induced elevations in plasma ARA levels, while supplementation with borage + fish oil combinations inhibit leukotriene generation [40,41] and attenuate the expression of pro-inflammatory cytokines genes [42]. Furthermore, studies suggest that botanical oil combinations of borage oil, enriched in GLA, and echium oil (from Echium plantagineum L.) abundant in ω-3 PUFAs (ALA and stearidonic acids; SDA) enhanced the conversion of dietary GLA to DGLA whilst inhibiting the further conversion of DGLA to ARA [43]. Such supplementation strategies maintained the anti-inflammatory capacity of GLA, while increasing EPA, without causing accumulation of ARA.
This has been observed to directly translate into a clinical benefit in various therapeutic areas. For example, when enteral diets were enriched with marine oils containing EPA, DHA, and GLA, cytokine production and neutrophil recruitment in the lung were reduced, resulting in fewer days on ventilation and Intensive Care Unit stay-in patients with acute lung injury or acute respiratory distress syndrome (ARDS) [44]. Other research has observed decreased morbidity and mortality of critically ill patients with severe ARDS [45] and improved quality of life in asthma patients [40]. Positive outcomes of a combined ω-6/ω-3 PUFAs therapy have been observed in patients with rheumatoid and psoriatic arthritis in a RCT, where treatment with ω-3 LC-PUFAs and GLA led to an increase of GLA and DGLA concentrations in plasma lipids, cholesteryl esters, and erythrocyte membranes, indicating a reduction in the production of ARA inflammatory eicosanoids [46].
4. GLA and ADHD Focus
Even though the pathogenetic pathways of NDDs are still not completely clear, growing scientific evidence points to oxidative stress and neuroinflammation as triggers for their genesis, and might be pivotal in their clinical pattern and evolution [47,48]. ω-6 and ω-3 PUFAs and their metabolites are involved in immune-inflammatory and brain structural mechanisms and therefore these molecules may play a role in neurological disorders in which disruption of these mechanisms represent a contributing pathogenetic factor [49,50].
4.1. Pathogenesis and Role of Neuroinflammation
The etiology of ADHD is multifactorial and still not fully understood. Evidence indicates that ADHD is heritable, however, no genes of major effect have been detected so far [51]. Pre- and peri-natal inflammatory factors that can affect the in-utero environment seem to be also involved in the etiology of the disease i.e., infections [52], smoking [53], obesity and poor diet [54], and pollutants to which the mother might be exposed [55,56]. Prenatal exposures to inflammation have also been associated with a volume reduction of cortical areas associated with ADHD [57]. Furthermore, a bilateral decrease in grey matter volume in the cingulate and parietal areas was observed in children with ADHD [57].
The hypothesis that inflammation is part of the pathway to ADHD and more in general to NDDs is consistent. Neuroinflammation influences brain development and subsequent risk of neurodevelopmental disorders through mechanisms such as glial activation [58], increased oxidative stress [59], aberrant neuronal development [60], reduced neurotrophic support [61], and altered neurotransmitter function [62]. Studies have identified associations between ADHD and regulatory genes involved in cell adhesion and inflammation, such as the gene for the interleukin-1 receptor antagonist (IL-1 RA) [63]. Moreover, immune disorders such as eczema [64], asthma, rheumatoid arthritis, type 1 diabetes, and hypothyroidism [65] are associated with greater rates of ADHD diagnosis.
Higher levels of antibodies against basal ganglia [66] and dopamine transporter [67] have been detected in subjects with ADHD. Furthermore, ADHD patients have reported increased cerebrospinal fluid levels of pro-inflammatory cytokine tumor necrosis factor β (TNF- β) and lower amounts of anti-inflammatory cytokine IL-4 [68]. This translates into an overall vulnerability of central nervous system (CNS) structures. Under normal conditions the blood–brain barrier (BBB) separates the peripheral immune system, preventing peripheral immune cells from entering the CNS. However, injuries, inflammatory diseases, and psychological stress may compromise the BBB, consequently, peripheral activated monocytes and T-lymphocytes may penetrate the brain, thereby inducing microglial activation, neuroinflammation, and neurotoxic responses [69].
A lack of dopamine in ADHD pathogenesis has been supported by the evidence that medications like methylphenidate and amphetamines, which increase the levels of dopamine in the synaptic cleft, can temporarily improve symptoms [70]. However, up to 30% of ADHD patients do not respond to this treatment, while only about 50% show signs of improvement [71]. Recent studies have provided evidence for the role of the monoamine serotonin (5-HT), synthesized from the essential amino acid tryptophan in a few areas of the brain such as the dorsal raphe nucleus, and which is an important regulator of behavioral inhibition [72]. Children with ADHD may have lower blood levels of 5-HT [73], which might contribute to the symptoms of ADHD [74]. Therefore, alternative pharmacological treatments for ADHD include selective-serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tri-cyclic-antidepressants (TCA) all of which target the 5-HT system [75].
Relevantly, some ω-3 PUFAs and some ω-6 PUFAs such as GLA are directly involved in the synthesis, release, and re-uptake of neurotransmitters [76], Subsequently, an ω-3 PUFAs deficiency or an imbalance between ω-6 and ω-3 PUFAs may lead to impaired neurological functioning and behavioral disturbances similar to those which characterize ADHD [76].
4.2. Combined ω-6 and ω-3 PUFA Supplementation
As previously described, ADHD is a multifactorial condition, which depends on genetic and environmental factors [77,78]. Dietary deficiencies and imbalances have been attributed to the etiology of ADHD and are viewed as a plausible adjunctive therapy [79,80]. In particular, ω-3 PUFAs are well-recognized nutrients for being central to proper brain development and function [81].
The human brain is comprised of around 60% of lipids and essential PUFAs play a key role in its structure and functions [82]. Postmortem measurements of the cortex have shown that DHA concentrations in a healthy brain accrues and increase until 18 years-old [83]. Subsequently, ω-3 PUFAs shortfalls in the early life course are thought to have lasting impacts on the central nervous system, including reduced neuron size [83]. Neuron membranes need high amounts of ω-3 and ω-6 PUFAs, especially DHA and ARA, whose presence affects their fluidity, neurotransmission, and permeability, as well as membrane-bound proteins [81].
Over the last decade, several systematic reviews and meta-analysis publications have focused on the roles of ω-6 and ω-3 PUFA supplementation as adjunctive therapy for ADHD [84,85,86]. Derbyshire et al. (2017) undertook a systematic review of 16 RCTs finding that four studies [87,88,89,90] used supplements containing a 9:3:1 ratio of EPA/DHA/GLA which improved erythrocyte levels and showed promise as adjunctive therapy to traditional medications, lowering the dose and improving compliance with medications such as methylphenidate (MPH) [84]. Puri et al. (2014) conducted a meta-regression analysis of RCTs finding that longer study duration, GLA, and the interaction between GLA and EPA were statistically significantly linked to reductions in inattention in children with ADHD [86]. Gillies et al. (2012) reviewed 13 trials focusing on ω-3/ω-6 supplementation in children and teenagers with ADHD concluding that some data did show an improvement in attention and behavior symptoms [85]. It was, however, concluded that small sample sizes, variability of selection criteria, follow-up times, and the form and dosage of the supplement could have impacted on results [85].
A growing number of trials have also been published. A PubMed search limited to the last 10 years and focusing on studies in childhood and adulthood yielded the following main publications. Döpfner et al. (2021) found that a 4-month intervention with ω-6/ω-3 fatty acids in preschool children at risk of ADHD had some positive effects on symptoms although larger studies are warranted [91]. Chang et al. (2019) undertook a longer 12-week double-blind RCT, finding that EPA supplementation taken by 6–18-year-olds significantly improved blood erythrocyte levels and emotional symptoms, particularly amongst those with low EPA levels at baseline [92]. Interestingly, Barragán et al. (2017) found that children with ADHD treated with methylphenidate (MPH) required lower doses of the prescription medicine when given ω-3/ω-6 PUFAs supplements in a dosage of 558 mg EPA, 174 mg DHA, and 60 mg GLA (9:3:1 ratio) for 12 months, and experienced fewer medication-related side effects, implying that ω-3/ω-6 PUFAs may act as a useful adjunctive therapy to MPH, helping to improve tolerability, dosing, and adherence [87]. A placebo-controlled RCT recruiting 76 males (aged 12–16 years) with ADHD found that 12-weeks of supplementation with an ω-3/ω-6 PUFA supplement improved EPA, DHA, and total ω-3 fatty acid levels although no distinct benefits were found for psychological outcomes [88]. Johnson et al. (2012) randomized 75 children (aged 8 to 18 years) to 3 months of ω-3/ω-6 (Equazen eye q) or a placebo and found that responders (those with more than a 25% reduction in ADHD symptoms) had a significantly greater increase in ω-3 plasma levels and a reduced ω-6:ω-3 ratio at 3 and 6-months follow-up [89].
5. Discussion
Taken together ADHD is a prevalent condition, often persisting into adulthood that if left without intervention could become a risk factor for educational underachievement, unemployment, mental health disorders, and criminality [12]. Certain dietary factors but particularly supplementation with PUFAs appear to have mediatory effects on behavior in children with ADHD [93]. Unfortunately, habitual intakes of these fatty acids appear to be lacking from dietary sources. For example, it has been reported that in the United Kingdom only around 7.3% of children, 12.8% of teenagers, and 15.6% of young adults meet oily fish recommendation, one of the main dietary sources of ω-3 fatty acids [94]. As mentioned, GLA-rich foods are also only consumed in low quantities with the typical dietary intake of GLA being negligible [24]. It is, however, recognized that ongoing dietary intake studies are needed as it is difficult to accurately assess intakes of fatty acids and habitual intakes can be susceptible to under-reporting and plasma fatty acids are not always regarded as being accurate markers of food intake [95]. From a metabolic perspective, deficiencies of LA, ALA, ARA, EPA, and DHA can indicate malnutrition and deficiency of certain minerals, trace elements and vitamins which are important co-factors for the appropriate activity of desaturases [96]. Consequently, it is reasonable to assume that GLA, DGLA, AA, EPA, and DHA deficiencies can also be attributed to lower desaturases and elongase activities [96].
Given this, these fatty acids must be provided from alternative sources. This is particularly relevant to those with conditions such as ADHD who may have different physiological requirements for these PUFAs. For example, LaChance et al. (2016) found that children and young people with ADHD had elevated ratios of blood ω-6/ω-3 and ARA/EPA fatty acids suggesting an underlying metabolic disturbance in essential fatty acid levels in these individuals [97]. Common genetic variations within the fatty acid desaturase (FADS) gene cluster can also affect the rate of conversion of 18 C-PUFAs, including GLA, to LC-PUFAs [98]. This raises questions about whether gene-PUFA interactions may mean that “one size fits all” dietary recommendations and supplementation strategies may not be appropriate for all populations or indeed individuals within specific populations [25].
As discussed in the present publication, the pathogenetic mechanisms of NDDs including ADHD are not yet fully understood but clinical evidence points to oxidative stress and inflammation as potential triggering factors [37,65,72]. Since ω-3 and ω-6 PUFAs are involved in immune-inflammatory and brain structural mechanisms, these molecules may play a role in neurological disorders in which disruption of these pathways represents a contributing pathogenetic factor [29,49,82]. The anti-inflammatory functions of GLA, an ω-6 PUFA, are still to be fully understood but there is some evidence that ω-3 and ω-6 PUFAs may work better when combined. The most appropriate dosage ratio to express their therapeutic potential, however, is yet to be derived.
There is a growing body of studies indicating that specific combinations of PUFAs may be of benefit to ADHD management, potentially acting as an adjunctive to conventional medicines, possibly even lowering the dosage needed from these [81,84,87]. In particular, a growing number of publications demonstrate that the combination of EPA and DHA with the addition of GLA in a 9:3:1 ratio is associated with slightly better outcomes in terms of improvement in ADHD symptoms [87,88,89,90]. Subsequently, an emerging evidence base indicates that the presence of GLA in ADHD symptom treatment strategies might represent an added value. Furthermore, it is plausible that the administration of ω-3 PUFAs alone might not be sufficient to effectively treat patients with ADHD and developmental disorders and a combination of PUFAs may subsequently lead to better outcomes. Other work has found that ω-3 combined with ω-6 fatty acids, including GLA, may reduce ASD symptoms in children born preterm showing early ASD signs [99].
It is, however, recognized that ongoing research is needed. As mentioned, wide variability in sample sizes, selection criteria, intervention timeframes, and the form and dosage of supplement makes comparing results between studies challenging and could have skewed results [85]. The n-6 PUFA (GLA) evaluation techniques should be properly stated in research papers, and procedures should be uniform from clinical trials to facilitate cross-study comparisons.
In general, when interventions were shorter than 12-weeks duration and used lower supplement dosages findings are less highly regarded [100]. Erythrocytes only tend to survive in the body for 120 days, thus short supplementation trials may not be sufficient to detect changes in LC-PUFA compositions [88]. Furthermore, the turnover of PUFAs in the brain is thought to be slower in children meaning that longer periods of supplementation and/or higher doses are likely to be needed [100].
Finally, it is important to consider that there is growing interest in natural and sustainable vegan and vegetarian dietary sources of n-3 PUFAs [101]. For example, plant-based oils, marine fish oils and algal oils, which all contain various level of n-3 PUFAs may all have roles to play in improving ADHD symptoms. Validated methodologies are needed to develop and build research in this area.
6. Conclusions
In summary, PUFAs have been gaining attention in terms of their role in the etiology, treatment, and management of NDDs including ADHD. The evidence for ω-3 PUFAs is well documented but the role(s) of GLA are less well known. The present narrative review has explained that GLA appears to have anti-inflammatory properties that could be used with ω-3 PUFAs in the treatment of ADHD and associated symptoms. In particular, a combination of EPA and DHA with the addition of GLA in a 9:3:1 ratio appears to be associated with improvements in ADHD symptoms. It is possible that ω-3 long-chain PUFAs may prevent the accumulation of serum ARA in response to GLA. While evidence broadly supports these findings, ongoing research is needed in the form of mechanistic studies and rigorous clinical trials.
Author Contributions
J.D., R.C. and M.M. compiled the first draft of the manuscript. J.D., R.C., M.M. and E.D. edited, proof-read and conducted a second draft of the manuscript. J.D., R.C., M.M. and E.D. reviewed the final draft. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
J.D.H is Managing Director of Springfield Nutraceuticals Belgium, a nutraceutical company that also sells omega 3 supplements. The other authors have no conflicts of interest to declare that are relevant to the content of this article.
Funding Statement
The research submission process and open access fees were sponsored by Springfield Nutraceuticals Belgium BV.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tesei A., Crippa A., Ceccarelli S.B., Mauri M., Molteni M., Agostoni C., Nobile M. The potential relevance of docosahexaenoic acid and eicosapentaenoic acid to the etiopathogenesis of childhood neuropsychiatric disorders. Eur. Child Adolesc. Psychiatry. 2017;26:1011–1030. doi: 10.1007/s00787-016-0932-4. [DOI] [PubMed] [Google Scholar]
- 2.Di Pasquale M.G. The essentials of essential fatty acids. J. Diet Suppl. 2009;6:143–161. doi: 10.1080/19390210902861841. [DOI] [PubMed] [Google Scholar]
- 3.Saini R.K., Keum Y.S. Omega-3 and omega-6 polyunsaturated fatty acids: Dietary sources, metabolism, and significance—A review. Life Sci. 2018;203:255–267. doi: 10.1016/j.lfs.2018.04.049. [DOI] [PubMed] [Google Scholar]
- 4.Simopoulos A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed. Pharmacother. 2002;56:365–379. doi: 10.1016/S0753-3322(02)00253-6. [DOI] [PubMed] [Google Scholar]
- 5.Simopoulos A.P. Importance of the ratio of omega-6/omega-3 essential fatty acids: Evolutionary aspects. World Rev. Nutr. Diet. 2003;92:1–22. doi: 10.1159/000073788. [DOI] [PubMed] [Google Scholar]
- 6.Holub B. Clinical nutrition: 4. Omega-3 fatty acids in cardiovascular care. JAMC. 2002;166:608–615. [PMC free article] [PubMed] [Google Scholar]
- 7.Ander B., Dupasquier C., Prociuk M., Pierce G. Polyunsaturated fatty acids and their effects on cardiovascular disease. Exp. Clin. Cardiol. 2003;8:164–172. [PMC free article] [PubMed] [Google Scholar]
- 8.Morris-Rosendahl D.J., Crocq M.A. Neurodevelopmental disorders-the history and future of a diagnostic concept. Dialogues Clin. NeuroSci. 2020;22:65–72. doi: 10.31887/DCNS.2020.22.1/macrocq. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DSM . Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 10.Ahmed R., Borst J.M., Yong C.W., Aslani P. Do parents of children with attention-deficit/hyperactivity disorder (ADHD) receive adequate information about the disorder and its treatments? A qualitative investigation. Patient Prefer. Adherence. 2014;8:661–670. doi: 10.2147/PPA.S60164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas R., Sanders S., Doust J., Beller E., Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 2015;135:e994–e1001. doi: 10.1542/peds.2014-3482. [DOI] [PubMed] [Google Scholar]
- 12.Sayal K., Prasad V., Daley D., Ford T., Coghill D. ADHD in children and young people: Prevalence, care pathways, and service provision. Lancet Psychiatry. 2018;5:175–186. doi: 10.1016/S2215-0366(17)30167-0. [DOI] [PubMed] [Google Scholar]
- 13.Mohammadi M.R., Zarafshan H., Khaleghi A., Ahmadi N., Hooshyari Z., Mostafavi S.A., Ahmadi A., Alavi S.S., Shakiba A., Salmanian M. Prevalence of ADHD and Its Comorbidities in a Population-Based Sample. J. Atten. Disord. 2021;25:1058–1067. doi: 10.1177/1087054719886372. [DOI] [PubMed] [Google Scholar]
- 14.Steinhoff K.W. Special issues in the diagnosis and treatment of ADHD in adolescents. Postgrad. Med. 2008;120:60–68. doi: 10.3810/pgm.2008.09.1908. [DOI] [PubMed] [Google Scholar]
- 15.Shaw M., Hodgkins P., Caci H., Young S., Kahle J., Woods A.G., Arnold L.E. A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: Effects of treatment and non-treatment. BMC Med. 2012;10:99. doi: 10.1186/1741-7015-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang J.P., Su K.P., Mondelli V., Pariante C.M. Omega-3 Polyunsaturated Fatty Acids in Youths with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis of Clinical Trials and Biological Studies. Neuropsychopharmacology. 2018;43:534–545. doi: 10.1038/npp.2017.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonvicini C., Faraone S.V., Scassellati C. Attention-deficit hyperactivity disorder in adults: A systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol. Psychiatry. 2016;21:872–884. doi: 10.1038/mp.2016.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen T.M., Lerche A., Kassis V., Lorenzen I., Sondergaard J. Treatment of rheumatoid arthritis with prostaglandin E1 precursors cis-linoleic acid and gamma-linolenic acid. Scand J. Rheumatol. 1983;12:85–88. doi: 10.3109/03009748309102890. [DOI] [PubMed] [Google Scholar]
- 19.Horrobin D.F. The role of essential fatty acids and prostaglandins in the premenstrual syndrome. J. Reprod. Med. 1983;28:465–468. [PubMed] [Google Scholar]
- 20.Kunkel S.L., Ogawa H., Ward P.A., Zurier R.B. Suppression of chronic inflammation by evening primrose oil. Prog. Lipid Res. 1981;20:885–888. doi: 10.1016/0163-7827(81)90165-X. [DOI] [PubMed] [Google Scholar]
- 21.Innes J.K., Calder P.C. Omega-6 fatty acids and inflammation. Prostaglandins Leukot. Essent. Fat. Acids. 2018;132:41–48. doi: 10.1016/j.plefa.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Silva J.R., Burger B., Kuhl C.M.C., Candreva T., Dos Anjos M.B.P., Rodrigues H.G. Wound Healing and Omega-6 Fatty Acids: From Inflammation to Repair. Mediat. Inflamm. 2018;2018:2503950. doi: 10.1155/2018/2503950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharif S.N., Darsareh F. Impact of evening primrose oil consumption on psychological symptoms of postmenopausal women: A randomized double-blinded placebo-controlled clinical trial. Menopause. 2020;27:194–198. doi: 10.1097/GME.0000000000001434. [DOI] [PubMed] [Google Scholar]
- 24.Majdinasab N., Namjoyan F., Taghizadeh M., Saki H. The effect of evening primrose oil on fatigue and quality of life in patients with multiple sclerosis. Neuropsychiatr. Dis. Treat. 2018;14:1505–1512. doi: 10.2147/NDT.S149403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sergeant S., Rahbar E., Chilton F.H. Gamma-linolenic acid, Dihommo-gamma linolenic, Eicosanoids and Inflammatory Processes. Eur. J. Pharmacol. 2016;785:77–86. doi: 10.1016/j.ejphar.2016.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kapoor R., Huang Y.S. Gamma linolenic acid: An antiinflammatory omega-6 fatty acid. Curr. Pharm. Biotechnol. 2006;7:531–534. doi: 10.2174/138920106779116874. [DOI] [PubMed] [Google Scholar]
- 27.Dobryniewski J., Szajda S.D., Waszkiewicz N., Zwierz K. Biology of essential fatty acids (EFA) Przegl. Lek. 2007;64:91–99. [PubMed] [Google Scholar]
- 28.Williams C.M., Burdge G. Long-chain n-3 PUFA: Plant v. marine sources. Proc. Nutr. Soc. 2006;65:42–50. doi: 10.1079/PNS2005473. [DOI] [PubMed] [Google Scholar]
- 29.Khan S.A., Ali A., Khan S.A., Zahran S.A., Damanhouri G., Azhar E., Qadri I. Unraveling the complex relationship triad between lipids, obesity, and inflammation. Mediat. Inflamm. 2014;2014:502749. doi: 10.1155/2014/502749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fan Y.Y., Chapkin R.S. Importance of dietary gamma-linolenic acid in human health and nutrition. J. Nutr. 1998;128:1411–1414. doi: 10.1093/jn/128.9.1411. [DOI] [PubMed] [Google Scholar]
- 31.Johnson M.M., Swan D.D., Surette M.E., Stegner J., Chilton T., Fonteh A.N., Chilton F.H. Dietary supplementation with gamma-linolenic acid alters fatty acid content and eicosanoid production in healthy humans. J. Nutr. 1997;127:1435–1444. doi: 10.1093/jn/127.8.1435. [DOI] [PubMed] [Google Scholar]
- 32.Chilton L., Surette M.E., Swan D.D., Fonteh A.N., Johnson M.M., Chilton F.H. Metabolism of gammalinolenic acid in human neutrophils. J. Immunol. 1996;156:2941–2947. [PubMed] [Google Scholar]
- 33.Du Y., Taylor C.G., Aukema H.M., Zahradka P. Role of oxylipins generated from dietary PUFAs in the modulation of endothelial cell function. Prostaglandins Leukot. Essent. Fat. Acids. 2020;160:102160. doi: 10.1016/j.plefa.2020.102160. [DOI] [PubMed] [Google Scholar]
- 34.Fan Y.Y., Ramos K.S., Chapkin R.S. Dietary gamma-linolenic acid modulates macrophage-vascular smooth muscle cell interactions. Evidence for a macrophage-derived soluble factor that downregulates DNA synthesis in smooth muscle cells. Arter. Thromb. Vasc. Biol. 1995;15:1397–1403. doi: 10.1161/01.ATV.15.9.1397. [DOI] [PubMed] [Google Scholar]
- 35.Heitmann J., Iversen L., Kragballe K., Ziboh V.A. Incorporation of 15-hydroxyeicosatrienoic acid in specific phospholipids of cultured human keratinocytes and psoriatic plaques. Exp. Dermatol. 1995;4:74–78. doi: 10.1111/j.1600-0625.1995.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez-Soto M., Mutch D.M. Diet Regulation of Long-Chain PUFA Synthesis: Role of Macronutrients, Micronutrients, and Polyphenols on Delta-5/Delta-6 Desaturases and Elongases 2/5. Adv. Nutr. 2021;12:980–994. doi: 10.1093/advances/nmaa142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moghadas M., Essa M.M., Ba-Omar T., Al-Shehi A., Qoronfleh M.W., Eltayeb E.A., Guillemin G.J., Manivasagam T., Justin-Thenmozhi A., Al-Bulushi B.S., et al. Antioxidant therapies in attention deficit hyperactivity disorder. Front. BioSci. 2019;24:313–333. doi: 10.2741/4720. [DOI] [PubMed] [Google Scholar]
- 38.Boyce J.A. Eicosanoids in asthma, allergic inflammation, and host defense. Curr. Mol. Med. 2008;8:335–349. doi: 10.2174/156652408785160989. [DOI] [PubMed] [Google Scholar]
- 39.Barham J.B., Edens M.B., Fonteh A.N., Johnson M.M., Easter L., Chilton F.H. Addition of eicosapentaenoic acid to gamma-linolenic acid-supplemented diets prevents serum arachidonic acid accumulation in humans. J. Nutr. 2000;130:1925–1931. doi: 10.1093/jn/130.8.1925. [DOI] [PubMed] [Google Scholar]
- 40.Surette M.E., Stull D., Lindemann J. The impact of a medical food containing gammalinolenic and eicosapentaenoic acids on asthma management and the quality of life of adult asthma patients. Curr. Med. Res. Opin. 2008;24:559–567. doi: 10.1185/030079908X273011. [DOI] [PubMed] [Google Scholar]
- 41.Surette M.E., Koumenis I.L., Edens M.B., Tramposch K.M., Chilton F.H. Inhibition of leukotriene synthesis, pharmacokinetics, and tolerability of a novel dietary fatty acid formulation in healthy adult subjects. Clin. Ther. 2003;25:948–971. doi: 10.1016/S0149-2918(03)80116-9. [DOI] [PubMed] [Google Scholar]
- 42.Weaver K.L., Ivester P., Seeds M., Case L.D., Arm J.P., Chilton F.H. Effect of dietary fatty acids on inflammatory gene expression in healthy humans. J. Biol. Chem. 2009;284:15400–15407. doi: 10.1074/jbc.M109.004861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee T.C., Ivester P., Hester A.G., Sergeant S., Case L.D., Morgan T., Kouba E.O., Chilton F.H. The impact of polyunsaturated fatty acid-based dietary supplements on disease biomarkers in a metabolic syndrome/diabetes population. Lipids Health Dis. 2014;13:196. doi: 10.1186/1476-511X-13-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pontes-Arruda A., Aragao A.M., Albuquerque J.D. Effects of enteral feeding with eicosapentaenoic acid, gamma-linolenic acid, and antioxidants in mechanically ventilated patients with severe sepsis and septic shock. Crit. Care Med. 2006;34:2325–2333. doi: 10.1097/01.CCM.0000234033.65657.B6. [DOI] [PubMed] [Google Scholar]
- 45.Li C., Bo L., Liu W., Lu X., Jin F. Enteral Immunomodulatory Diet (Omega-3 Fatty Acid, gamma-Linolenic Acid and Antioxidant Supplementation) for Acute Lung Injury and Acute Respiratory Distress Syndrome: An Updated Systematic Review and Meta-Analysis. Nutrients. 2015;7:5572–5585. doi: 10.3390/nu7075239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dawczynski C., Hackermeier U., Viehweger M., Stange R., Springer M., Jahreis G. Incorporation of n-3 PUFA and gamma-linolenic acid in blood lipids and red blood cell lipids together with their influence on disease activity in patients with chronic inflammatory arthritis--a randomized controlled human intervention trial. Lipids Health Dis. 2011;10:130. doi: 10.1186/1476-511X-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buss C. Maternal oxidative stress during pregnancy and offspring neurodevelopment. Brain Behav. Immun. 2021;93:6–7. doi: 10.1016/j.bbi.2021.01.007. [DOI] [PubMed] [Google Scholar]
- 48.Han V.X., Patel S., Jones H.F., Dale R.C. Maternal immune activation and neuroinflammation in human neurodevelopmental disorders. Nat. Rev. Neurol. 2021;17:564–579. doi: 10.1038/s41582-021-00530-8. [DOI] [PubMed] [Google Scholar]
- 49.Laye S., Nadjar A., Joffre C., Bazinet R.P. Anti-Inflammatory Effects of Omega-3 Fatty Acids in the Brain: Physiological Mechanisms and Relevance to Pharmacology. Pharmacol. Rev. 2018;70:12–38. doi: 10.1124/pr.117.014092. [DOI] [PubMed] [Google Scholar]
- 50.Caramia G. The essential fatty acids omega-6 and omega-3: From their discovery to their use in therapy. Minerva. Pediatr. 2008;60:219–233. [PubMed] [Google Scholar]
- 51.Brikell I., Kuja-Halkola R., Larsson H. Heritability of attention-deficit hyperactivity disorder in adults. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2015;168:406–413. doi: 10.1002/ajmg.b.32335. [DOI] [PubMed] [Google Scholar]
- 52.Werenberg Dreier J., Nybo Andersen A.M., Hvolby A., Garne E., Kragh Andersen P., Berg-Beckhoff G. Fever and infections in pregnancy and risk of attention deficit/hyperactivity disorder in the offspring. J. Child Psychol. Psychiatry. 2016;57:540–548. doi: 10.1111/jcpp.12480. [DOI] [PubMed] [Google Scholar]
- 53.Silva D., Colvin L., Hagemann E., Bower C. Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133:e14–e22. doi: 10.1542/peds.2013-1434. [DOI] [PubMed] [Google Scholar]
- 54.Sanchez C.E., Barry C., Sabhlok A., Russell K., Majors A., Kollins S.H., Fuemmeler B.F. Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: A meta-analysis. Obes. Rev. 2018;19:464–484. doi: 10.1111/obr.12643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thapar A., Cooper M., Eyre O., Langley K. What have we learnt about the causes of ADHD? J. Child Psychol. Psychiatry. 2013;54:3–16. doi: 10.1111/j.1469-7610.2012.02611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vrijheid M., Casas M., Gascon M., Valvi D., Nieuwenhuijsen M. Environmental pollutants and child health-A review of recent concerns. Int. J. Hyg. Environ. Health. 2016;219:331–342. doi: 10.1016/j.ijheh.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 57.Castellanos F.X., Lee P.P., Sharp W., Jeffries N.O., Greenstein D.K., Clasen L.S., Blumenthal J.D., James R.S., Ebens C.L., Walter J.M., et al. Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA. 2002;288:1740–1748. doi: 10.1001/jama.288.14.1740. [DOI] [PubMed] [Google Scholar]
- 58.Reus G.Z., Fries G.R., Stertz L., Badawy M., Passos I.C., Barichello T., Kapczinski F., Quevedo J. The role of inflammation and microglial activation in the pathophysiology of psychiatric disorders. Neuroscience. 2015;300:141–154. doi: 10.1016/j.neuroscience.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 59.Hassan W., Noreen H., Castro-Gomes V., Mohammadzai I., da Rocha J.B., Landeira-Fernandez J. Association of Oxidative Stress with Psychiatric Disorders. Curr. Pharm. Des. 2016;22:2960–2974. doi: 10.2174/1381612822666160307145931. [DOI] [PubMed] [Google Scholar]
- 60.Belmadani A., Tran P.B., Ren D., Miller R.J. Chemokines regulate the migration of neural progenitors to sites of neuroinflammation. J. NeuroSci. 2006;26:3182–3191. doi: 10.1523/JNEUROSCI.0156-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sen S., Duman R., Sanacora G. Serum brain-derived neurotrophic factor, depression, and antidepressant medications: Meta-analyses and implications. Biol. Psychiatry. 2008;64:527–532. doi: 10.1016/j.biopsych.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kronfol Z., Remick D.G. Cytokines and the brain: Implications for clinical psychiatry. Am. J. Psychiatry. 2000;157:683–694. doi: 10.1176/appi.ajp.157.5.683. [DOI] [PubMed] [Google Scholar]
- 63.Zayats T., Athanasiu L., Sonderby I., Djurovic S., Westlye L.T., Tamnes C.K., Fladby T., Aase H., Zeiner P., Reichborn-Kjennerud T., et al. Genome-wide analysis of attention deficit hyperactivity disorder in Norway. PLoS ONE. 2015;10:e0122501. doi: 10.1371/journal.pone.0122501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lin Y.T., Chen Y.C., Gau S.S., Yeh T.H., Fan H.Y., Hwang Y.Y., Lee Y.L. Associations between allergic diseases and attention deficit hyperactivity/oppositional defiant disorders in children. Pediatr. Res. 2016;80:480–485. doi: 10.1038/pr.2016.111. [DOI] [PubMed] [Google Scholar]
- 65.Instanes J.T., Halmoy A., Engeland A., Haavik J., Furu K., Klungsoyr K. Attention-Deficit/Hyperactivity Disorder in Offspring of Mothers With Inflammatory and Immune System Diseases. Biol. Psychiatry. 2017;81:452–459. doi: 10.1016/j.biopsych.2015.11.024. [DOI] [PubMed] [Google Scholar]
- 66.Toto M., Margari F., Simone M., Craig F., Petruzzelli M.G., Tafuri S., Margari L. Antibasal Ganglia Antibodies and Antistreptolysin O in Noncomorbid ADHD. J. Atten. Disord. 2015;19:965–970. doi: 10.1177/1087054712455505. [DOI] [PubMed] [Google Scholar]
- 67.Giana G., Romano E., Porfirio M.C., D’Ambrosio R., Giovinazzo S., Troianiello M., Barlocci E., Travaglini D., Granstrem O., Pascale E., et al. Detection of auto-antibodies to DAT in the serum: Interactions with DAT genotype and psycho-stimulant therapy for ADHD. J. Neuroimmunol. 2015;278:212–222. doi: 10.1016/j.jneuroim.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 68.Mittleman B.B., Castellanos F.X., Jacobsen L.K., Rapoport J.L., Swedo S.E., Shearer G.M. Cerebrospinal fluid cytokines in pediatric neuropsychiatric disease. J. Immunol. 1997;159:2994–2999. [PubMed] [Google Scholar]
- 69.Wohleb E.S., McKim D.B., Sheridan J.F., Godbout J.P. Monocyte trafficking to the brain with stress and inflammation: A novel axis of immune-to-brain communication that influences mood and behavior. Front. NeuroSci. 2014;8:447. doi: 10.3389/fnins.2014.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Volkow N.D., Wang G.J., Fowler J.S., Ding Y.S. Imaging the effects of methylphenidate on brain dopamine: New model on its therapeutic actions for attention-deficit/hyperactivity disorder. Biol. Psychiatry. 2005;57:1410–1415. doi: 10.1016/j.biopsych.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 71.Arnold L.E., Hurt E., Lofthouse N. Attention-deficit/hyperactivity disorder: Dietary and nutritional treatments. Child Adolesc. Psychiatr. Clin. N. Am. 2013;22:381–402. doi: 10.1016/j.chc.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 72.Dunn G.A., Nigg J.T., Sullivan E.L. Neuroinflammation as a risk factor for attention deficit hyperactivity disorder. Pharmacol. Biochem. Behav. 2019;182:22–34. doi: 10.1016/j.pbb.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spivak B., Vered Y., Yoran-Hegesh R., Averbuch E., Mester R., Graf E., Weizman A. Circulatory levels of catecholamines, serotonin and lipids in attention deficit hyperactivity disorder. Acta Psychiatr. Scand. 1999;99:300–304. doi: 10.1111/j.1600-0447.1999.tb07229.x. [DOI] [PubMed] [Google Scholar]
- 74.Quist J.F., Kennedy J.L. Genetics of childhood disorders: XXIII. ADHD, Part 7: The serotonin system. J. Am. Acad. Child Adolesc. Psychiatry. 2001;40:253–256. doi: 10.1097/00004583-200102000-00022. [DOI] [PubMed] [Google Scholar]
- 75.Park P., Caballero J., Omidian H. Use of serotonin norepinephrine reuptake inhibitors in the treatment of attention-deficit hyperactivity disorder in pediatrics. Ann. Pharmacother. 2014;48:86–92. doi: 10.1177/1060028013506561. [DOI] [PubMed] [Google Scholar]
- 76.Schuchardt J.P., Huss M., Stauss-Grabo M., Hahn A. Significance of long-chain polyunsaturated fatty acids (PUFAs) for the development and behaviour of children. Eur. J. Pediatr. 2010;169:149–164. doi: 10.1007/s00431-009-1035-8. [DOI] [PubMed] [Google Scholar]
- 77.Brikell I., Burton C., Mota N.R., Martin J. Insights into attention-deficit/hyperactivity disorder from recent genetic studies. Psychol. Med. 2021;51:2274–2286. doi: 10.1017/S0033291721000982. [DOI] [PubMed] [Google Scholar]
- 78.Carlsson T., Molander F., Taylor M.J., Jonsson U., Bolte S. Early environmental risk factors for neurodevelopmental disorders—a systematic review of twin and sibling studies. Dev. Psychopathol. 2021;33:1448–1495. doi: 10.1017/S0954579420000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lange K.W. Dietary factors in the etiology and therapy of attention deficit/hyperactivity disorder. Curr. Opin. Clin. Nutr. Metab. Care. 2017;20:464–469. doi: 10.1097/MCO.0000000000000415. [DOI] [PubMed] [Google Scholar]
- 80.Konikowska K., Regulska-Ilow B., Rozanska D. The influence of components of diet on the symptoms of ADHD in children. Rocz. Panstw. Zakl. Hig. 2012;63:127–134. [PubMed] [Google Scholar]
- 81.Konigs A., Kiliaan A.J. Critical appraisal of omega-3 fatty acids in attention-deficit/hyperactivity disorder treatment. Neuropsychiatr. Dis. Treat. 2016;12:1869–1882. doi: 10.2147/NDT.S68652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chang C.Y., Ke D.S., Chen J.Y. Essential fatty acids and human brain. Acta Neurol. Taiwan. 2009;18:231–241. [PubMed] [Google Scholar]
- 83.Carver J.D., Benford V.J., Han B., Cantor A.B. The relationship between age and the fatty acid composition of cerebral cortex and erythrocytes in human subjects. Brain Res. Bull. 2001;56:79–85. doi: 10.1016/S0361-9230(01)00551-2. [DOI] [PubMed] [Google Scholar]
- 84.Derbyshire E. Do Omega-3/6 Fatty Acids Have a Therapeutic Role in Children and Young People with ADHD? J. Lipids. 2017;2017:6285218. doi: 10.1155/2017/6285218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gillies D., Sinn J., Lad S.S., Leach M.J., Ross M.J. Polyunsaturated fatty acids (PUFA) for attention deficit hyperactivity disorder (ADHD) in children and adolescents. Cochrane Database Syst. Rev. 2012;7:CD007986. doi: 10.1002/14651858.CD007986.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Puri B.K., Martins J.G. Which polyunsaturated fatty acids are active in children with attention-deficit hyperactivity disorder receiving PUFA supplementation? A fatty acid validated meta-regression analysis of randomized controlled trials. Prostaglandins Leukot. Essent. Fat. Acids. 2014;90:179–189. doi: 10.1016/j.plefa.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 87.Barragan E., Breuer D., Dopfner M. Efficacy and Safety of Omega-3/6 Fatty Acids, Methylphenidate, and a Combined Treatment in Children With ADHD. J. Atten. Disord. 2017;21:433–441. doi: 10.1177/1087054713518239. [DOI] [PubMed] [Google Scholar]
- 88.Matsudaira T., Gow R.V., Kelly J., Murphy C., Potts L., Sumich A., Ghebremeskel K., Crawford M.A., Taylor E. Biochemical and Psychological Effects of Omega-3/6 Supplements in Male Adolescents with Attention-Deficit/Hyperactivity Disorder: A Randomized, Placebo-Controlled, Clinical Trial. J. Child Adolesc. Psychopharmacol. 2015;25:775–782. doi: 10.1089/cap.2015.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Johnson M., Mansson J.E., Ostlund S., Fransson G., Areskoug B., Hjalmarsson K., Landgren M., Kadesjo B., Gillberg C. Fatty acids in ADHD: Plasma profiles in a placebo-controlled study of Omega 3/6 fatty acids in children and adolescents. Atten. Defic. Hyperact. Disord. 2012;4:199–204. doi: 10.1007/s12402-012-0084-4. [DOI] [PubMed] [Google Scholar]
- 90.Johnson M., Ostlund S., Fransson G., Kadesjo B., Gillberg C. Omega-3/omega-6 fatty acids for attention deficit hyperactivity disorder: A randomized placebo-controlled trial in children and adolescents. J. Atten. Disord. 2009;12:394–401. doi: 10.1177/1087054708316261. [DOI] [PubMed] [Google Scholar]
- 91.Dopfner M., Dose C., Breuer D., Heintz S., Schiffhauer S., Banaschewski T. Efficacy of Omega-3/Omega-6 Fatty Acids in Preschool Children at Risk of ADHD: A Randomized Placebo-Controlled Trial. J. Atten. Disord. 2021;25:1096–1106. doi: 10.1177/1087054719883023. [DOI] [PubMed] [Google Scholar]
- 92.Chang J.P., Su K.P., Mondelli V., Satyanarayanan S.K., Yang H.T., Chiang Y.J., Chen H.T., Pariante C.M. High-dose eicosapentaenoic acid (EPA) improves attention and vigilance in children and adolescents with attention deficit hyperactivity disorder (ADHD) and low endogenous EPA levels. Transl. Psychiatry. 2019;9:303. doi: 10.1038/s41398-019-0633-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Banaschewski T., Belsham B., Bloch M.H., Ferrin M., Johnson M., Kustow J., Robinson S., Zuddas A. Supplementation with polyunsaturated fatty acids (PUFAs) in the management of attention deficit hyperactivity disorder (ADHD) Nutr. Health. 2018;24:279–284. doi: 10.1177/0260106018772170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Derbyshire E. Oily Fish and Omega-3 s Across the Life Stages: A Focus on Intakes and Future Directions. Front Nutr. 2019;6:165. doi: 10.3389/fnut.2019.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Marchioni D.M., de Oliveira M.F., Carioca A.A.F., Miranda A.A.M., Carvalho A.M., Oki E., Norde M.M., Rogero M.M., Damasceno N.R.T., Fisberg R.M. Plasma fatty acids: Biomarkers of dietary intake? Nutrition. 2019;59:77–82. doi: 10.1016/j.nut.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 96.Das U.N. “Cell Membrane Theory of Senescence” and the Role of Bioactive Lipids in Aging, and Aging Associated Diseases and Their Therapeutic Implications. Biomolecules. 2021;11:241. doi: 10.3390/biom11020241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.LaChance L., McKenzie K., Taylor V.H., Vigod S.N. Omega-6 to Omega-3 Fatty Acid Ratio in Patients with ADHD: A Meta-Analysis. J. Can. Acad. Child Adolesc. Psychiatry. 2016;25:87–96. [PMC free article] [PubMed] [Google Scholar]
- 98.Hester A.G., Murphy R.C., Uhlson C.J., Ivester P., Lee T.C., Sergeant S., Miller L.R., Howard T.D., Mathias R.A., Chilton F.H. Relationship between a common variant in the fatty acid desaturase (FADS) cluster and eicosanoid generation in humans. J. Biol. Chem. 2014;289:22482–22489. doi: 10.1074/jbc.M114.579557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Keim S.A., Boone K.M., Klebanoff M.A., Turner A.N., Rausch J., Nelin M.A., Rogers L.K., Yeates K.O., Nelin L., Sheppard K.W. Effect of Docosahexaenoic Acid Supplementation vs Placebo on Developmental Outcomes of Toddlers Born Preterm: A Randomized Clinical Trial. JAMA Pediatr. 2018;172:1126–1134. doi: 10.1001/jamapediatrics.2018.3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Voigt R.G., Llorente A.M., Jensen C.L., Fraley J.K., Berretta M.C., Heird W.C. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J. Pediatr. 2001;139:189–196. doi: 10.1067/mpd.2001.116050. [DOI] [PubMed] [Google Scholar]
- 101.Saini R.K., Prasad P., Sreedhar R.V., Akhilender Naidu K., Shang X., Keum Y.S. Omega-3 Polyunsaturated Fatty Acids (PUFAs): Emerging Plant and Microbial Sources, Oxidative Stability, Bioavailability, and Health Benefits-A Review. Antioxidants. 2021;10:1627. doi: 10.3390/antiox10101627. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.