Summary
Background
Population health has stagnated or is declining in many high-income countries. We analysed whether nationally administered austerity cuts in England were associated with prevalence of multimorbidity (individuals with two or more long-term conditions) and health-related quality of life.
Methods
We conducted an observational, longitudinal study on 147 local authorities in England. We examined associations of changes in spending over time (2009/10-2017/18), in total and by budget line, with (i) prevalence of multimorbidity, 2+ conditions (2011/12-2017/18), and (ii) health-related quality of life (EQ-5D-5L) score (2012/13-2016/17). We estimated linear, log-log regression models, incorporating local authority fixed-effects, time-varying demographic and socio-economic confounders, and time trends.
Findings
All local authorities experienced real spending cuts, varying from 42% (Barking and Dagenham) to 0·3% (Sefton). A 1% cut in per capita total service expenditure was associated with a 0·10% (95% CI 0·03 to 0·16) increase in prevalence of multimorbidity. We found no association (0·003%; 95% CI -0·01 to 0·01) with health-related quality of life. By budget line, after controlling for other spending, a 1% cut in public health expenditure was associated with a 0·15% (95% CI 0·11 to 0·20) increase in prevalence of multimorbidity, and a 1% cut in adult social care expenditure was associated with a 0·01% (95% CI 0·002 to 0·02) decrease in average health-related quality of life.
Interpretation
Fiscal austerity is associated with worse multimorbidity and health-related quality of life. Policymakers should consider the potential health consequences of local government expenditure cuts and knock-on effects for health systems.
Funding
Medical Research Council.
Keywords: Multimorbidity, Health-related quality of life, Austerity, Local government expenditure
Research in context.
Evidence before this study
We searched PubMed, from inception to 14 December 2021, for articles in English examining local government spending and multimorbidity or health-related quality of life. We searched the terms (“local govern*” or “local authorit*” or “local service*”) and (“expend*” or “spend*” or “cuts” or “cut” or “austerity”) and (“multimorbid*” or “long-term” or “chronic” or “health-related quality of life”). We identified relevant studies mostly from the US and UK. The literature concentrated primarily on mortality outcomes. Other outcomes included single condition prevalence, care-related quality of life for users of social care, hospital visits for potentially preventable acute and chronic conditions, and general health status (measured poor to excellent) in the population. Exposures included impacts of total local government service expenditure, or a focus on a single specific budget line. The literature to date generally appears consistent in showing associations of spending cuts with negative outcomes. To our knowledge, however, there has been no study examining effects of local government spending cuts, and multiple budget lines as potential drivers, on the prevalence of multiple long-term conditions, or on the health-related quality of life experienced by the general population living through fiscal austerity.
Added value of this study
We examined whether local government spending per capita in England, 2009/10-2017/18, in total and by budget line, was associated with multimorbidity prevalence, 2011/12-2017/18, and health-related quality of life (EQ-5D-5L) score, 2012/13-2016/17. We exploited the within-local government area fiscal austerity cuts over time. These cuts were largely exogenously determined, imposed by national government, and not primarily influenced by levels of local service needs. We estimated that a 1% cut in per capita total service expenditure was associated with a 0·10% (95% CI 0·03 to 0·16) increase in the prevalence of multimorbidity. We found no association (0·003%; 95% CI -0·01 to 0·01) of total expenditure with health-related quality of life. By budget line, after controlling for other spending, a 1% cut in public health expenditure was associated with a 0·15% (95% CI 0·11 to 0·20) increase in prevalence of multimorbidity, and a 1% cut in adult social care expenditure was associated with a 0·01% (95% CI 0·002 to 0·02) decrease in average health-related quality of life
Implications of all the available evidence
Our findings suggest that cuts to local government spending are associated with increased prevalence of multimorbidity and decreased health-related quality of life. In particular, multimorbidity appears to be associated with per capita public health expenditure, and health-related quality of life with social care expenditure. There were cuts to total local government spending in all localities over the analysis period, like-for-like public health expenditure also experienced real-term cuts, and there was relative stagnation in social care expenditure over this time. This might help explain national trends in these outcomes, and previous findings of associations of austerity cuts with increased mortality rates and other negative outcomes. Decreased population health, and increased co-morbidities, would also likely have compounded the negative effects of the subsequent Covid-19 pandemic. Policymakers should consider the potential health consequences of government service expenditure cuts and potential knock-on effects for health systems. In particular, national policymakers involved in determining grant formulas should aim to incorporate these trade-offs between short- and long-term funding, and to better reflect the additional reliance of some communities, the more deprived, on this public investment.
Alt-text: Unlabelled box
Introduction
Population health has stagnated or is declining in many high-income countries, despite ever-increasing healthcare spending. Trends in England are amongst the worst. Over the last decade there was a steeper slowdown in life expectancy in England and Wales compared to the average in 22 other high-income countries.1
The same is true for quality of life as for quantity. Health-related quality of life in England has been static with a slight downward trend between 2012 and 2017, and with increasing inequalities, particularly deteriorations for younger females and those living in the most deprived areas.2 The prevalence of individuals living in ill-health, with multimorbidity (two or more long-term conditions), is also increasing.3 Multimorbidity is a global research priority, associated with numerous negative patient and health system outcomes.4
While health systems can directly impact disease prevalence and population health outcomes, this is not the only important sector. It has been estimated that only a minority of health outcomes are determined by medical care, while up to 90% have been attributed to the ‘wider (social) determinants of health’,5 a mix of behaviours, social circumstances, environment, education, as well as other constitutional factors, such as genetics.6 Recent health service innovations, therefore, attempt to better address these wider determinants.
However, it is not obvious that expanding or adapting the health system is the only, or optimal, way to address prevention. Most obviously, public health budgets aim explicitly at preventing risk factors, such as smoking and obesity, at the population level. More broadly, local authority service expenditure in England, which encompasses public health, also includes social care, highways and transport, housing, cultural, and environmental spending. All of these could plausibly shape the social environment, and therefore population health.
Austerity cuts to manage public finances, enacted following the 2008 global financial crisis, were particularly detrimental for public services in England, however.7 This might have contributed to the negative trends observed in population health.
Cuts to overall central funding in England,8 and specifically reductions in spending on services which support older or disabled people,9,10 appear to have negatively influenced mortality. These austerity associations also appear to hold in other international comparisons.11 There have, however, been fewer studies examining other measures of population health, perhaps offering mechanisms for the mortality associations observed. Previous research does suggest a plausibility of this link. In the US, for example, States with a higher ratio of social to healthcare spending had better outcomes for prevalence rates of single long-term conditions, such as obesity and asthma, as well as mortality rates.12 Lower spending has also been linked with an increase in hospital visits for potentially preventable acute and chronic conditions,13 reductions in care-related quality of life for social care users,14 and lower population general health status.15
We aimed to examine whether local authority spending cuts over the austerity period in England, in total and by budget line, were associated with multimorbidity prevalence and health-related quality of life.
Methods
We used nationally representative survey data linked to local authority service expenditure data in England. We exploited variation in expenditure within local authorities due to austerity cuts using longitudinal population-level analyses.
Study setting
Table 1 details the spending areas of local authorities in England.
Table 1.
Local authority selected service expenditure areas in England.
| Local authority service expenditure area | Description (sub-expenditures) |
|---|---|
| Public health | Total spending on public health services, such as sexual health services, public health advice, obesity, physical activity, substance misuse, and smoking and tobacco. |
| Highways and transport | Total spending on transport services, such as highways and roads maintenance, parking services, and public transport. |
| Social care (adult) | Total spending on adult social care services. Services include physical and mental health support, sensory, memory and cognition, and learning disability support, social support, and assistive equipment and technology. |
| Housing (General Fund Revenue Account only) | Total spending on housing services, such as housing strategy, homelessness, housing benefits, housing welfare. |
| Cultural | Total spending on cultural services, such as museums and galleries, arts development and support, recreation and sport, open spaces, library services. |
| Environmental | Total spending on environmental services, such as regulatory services (trading standards, water and food safety, etc.), CCTV, flood defence, waste management. |
| Other local authority spending | Including: Planning and development; Central services; Police; Fire and rescue services; and other unallocated items. |
| Total (minus education) | Total spending by Local Authorities associated with delivering every individual service (sum of above). |
Local authority budgets were predominantly determined by a mix of local revenue from council tax (around a quarter of funding), and, the majority, grants from central government (around three quarters of funding).
The central government funding was made up of both:
-
(i)
a general grant (also known as the ‘Formula Grant’ – encompassing a ‘Revenue Support Grant’ and business rates), which made up roughly a quarter of the financed service expenditure. This funding was fully flexible for local authorities to choose the spending area;16
-
(ii)
specific grants (roughly a half of total service expenditure), which paid directly for services such as running schools and helping vulnerable people with accommodation needs. Some of this funding was ringfenced for specific spending, particularly the funding for schools (34% of the total funding in 2009/10), whereas other specific grants held only the title of a desired spending area but were actually flexible for subsequent spending.16
The 2010 Spending Review set out nationally defined cuts to central government grants. For local government, it projected a 26% decrease in cumulative real growth in central government contributions, and a 14% decrease in local government spending to 2014/15. This meant the extent of cuts by budget line could vary by geography, but required “tough choices on how services [were] delivered within reduced allocations” for all.17
The 2010 Review also set additional rules to disincentivise the raising of local taxes to compensate for these national cuts.16 More deprived areas also had innate lesser ability to raise local taxes to compensate for their additional needs.18 Furthermore, the latest review of the Formula Grant took place in 2013, meaning local authority ‘needs’ estimates within the formula have been held constant since that point,8 despite ever-changing populations. This implies that the overall spending cuts were largely determined by nationally implemented administrative policy rules, rather than in response to any measure of local population needs (see Appendix for further details).
The recent Marmot report further proved this disassociation of funding cuts from need. Between 2009/10 and 2017/18, the most deprived decile of authorities, where need is highest, made an average cut to total service spending per person of 32%, compared to 17% in the least deprived.7 Our identification strategy, therefore, relies on the assumption that austerity cuts were largely exogenously determined, imposed by government and not primarily influenced by levels of service needs.
Once a local authority's budget(s) are determined, they are not able to borrow to finance their day-to-day spending. They therefore have to run a balanced budget, or draw on previous underspend reserves from earlier years.19 Locally-elected officials are then responsible for allocating the available expenditure across spending areas. Their final choices will, therefore, partially reflect the spending rules (for instance, ringfencing and national allocation formulae), their own and their electorates priorities, and their total available budget. Certain spending areas also appear to be more adaptive to prioritisation decisions than others, as evidenced by the extent of variation in spending in relation to the average budget cuts in a locality. For example, central and other spending areas show wide variation, whereas social care and environmental spending were relatively protected and, particularly social care, show less variation across places.20
Plausible mechanisms
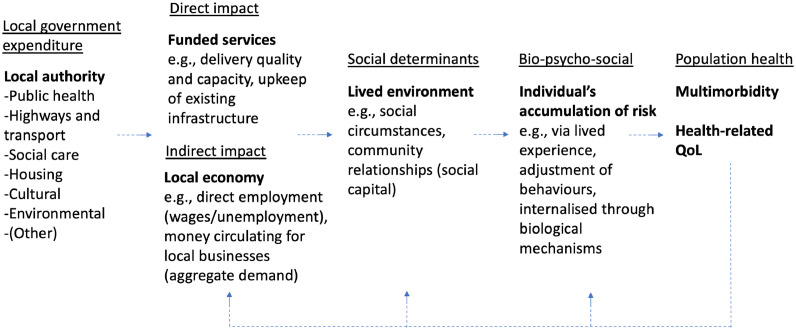
Figure 1 outlines the plausible mechanisms for local government service expenditure to impact population health outcomes, including multimorbidity and health-related quality of life. Changes in service expenditure are likely to have two more immediate impacts, (i) direct impacts on the funded services, potentially affecting quality and/or capacity of services delivered, as well as upkeep and maintenance of existing infrastructure (for example, green spaces); and, (ii) indirect impacts, through both the direct employment of local people to deliver these services (which could impact wages, and/or the employment rate), and more widely through the flows of income through the local economy, affecting (aggregate) demand and so also those employed by other local businesses and the wider population. This, in turn, can affect the lived environment, social circumstances and wider community relations (for instance, social capital and inequality). These experiences can be internalised by individuals through a variety of routes, including psychologically, through changes in behaviours, and through biological mechanisms. Finally, these act to impact individual, and so measurable population, health outcomes. There is likely to be an increasing lag period between left and right of the logic model, although some outcomes are likely to be affected quicker than others (see below). There is also, in the longer-term, likely to be some positive feedback as population health ultimately acts to further affect the same pathway (although, this is likely to be over a number of years, longer than we are able to measure in this study).
Figure 1.
Logic model for plausible effects of local government expenditure on population health.
Within each expenditure area there are also multiple sub-expenditures (see examples from Table 1). Each of these is likely to have:
-
(i)
varying degrees of direct and indirect impacts,
-
(ii)
potentially varying, or unpredictable, directions of effect on population health outcomes (for example, increased spending on public transport might reduce physical activity, but have a positive impact on pollution),
-
(iii)
varying time lags between the expenditure and outcomes,
-
(iv)
and sometimes varying effects for different population sub-groups (for example, publicly funded social care is based on needs-assessment limiting who is likely to benefit from any direct effects)
This complex system shows there are several plausible mechanisms. It also emphasises the need to control for the potential impacts of other expenditure areas when examining any one ex-post, as they are likely (or, at least have potential) to impact shared outcomes. The mechanisms of the impact of cuts on health are also difficult (perhaps impossible) to capture using current data. The model does, however, allow us to speculate on two things, as service expenditure cuts acting through the direct impact route should act almost immediately on funded services: 1) we would expect any impacts on outcomes might primarily act on psychological stress/mental health conditions and behaviours in the shorter-term; 2) we would also expect specific populations to be more affected than others by service expenditure cuts in the shorter-term, particularly the most deprived populations who might not have the income to replace the services privately, and those who already have a chronic condition and generally higher public service needs (those who are close to the tipping point of developing further conditions, who potentially experience a change in circumstances that sends them over the edge).
Data
We included data for 147 of all 152 upper-tier local authorities. Two (City of London, and Isles of Scilly) were excluded from the analysis as outliers due to their small population size (2-9000, at least three times smaller than the next smallest), and three (Bournemouth, Poole, Dorset) excluded because of boundary changes over the analysis period which made data inconsistent.
Our outcome variables measured: i) prevalence of multimorbidity; and, ii) health-related quality of life. We obtained both measures by aggregating anonymised individual-level data from the GP Patient Survey (GPPS), a large repeated cross-sectional postal survey administered to a random sample of registered patients from all GP practices in England (over 400,000 respondents per wave – see Appendix).21
Multimorbidity was defined as a binary indicator for presence of two or more from a count of 15 specific self-reported long-term conditions (see Appendix) + “another long-term condition” (max, n=16). Health-related quality of life was measured by the EQ-5D-5L index, measured on a scale between -0·59 to 1, where 1 indicates perfect health, 0 a state equivalent to death, and negative values indicate a state worse than death.22 Data on EQ-5D-5L was only included in the GPPS survey from 2012/13-2016/17.
Survey weights that account for the sampling design and the impact of non-response bias ensure GPPS is representative of the population of adult patients registered with a GP (largely representative of the entire adult population).23 We incorporated these weights when aggregating population averages of each outcome measure, percentage multimorbid and average health-related quality of life score, by local authority.
Our key exposure was gross expenditure per capita for each upper-tier local authority from the Place-based Longitudinal Data Resource.24 We used total service expenditure (minus education, excluded because the expenditure line has been gradually withdrawn from local authority budgets over time, at different rates in different localities – see Appendix); and service expenditure for seven budget lines: highways and transport; adult social care; public health; housing; cultural; environmental; other – all other budget lines.
We converted all service expenditure to 2017 prices using the ONS consumer price index (CPI),25 and used data from 2009/10-2017/18 to enable analysis of two-year lagged spending on outcomes (see Robustness checks). For analysis of individual budget lines, public health expenditure was only assigned to local authorities from 2013/14, so these analyses instead incorporated spending data from 2013/14-2017/18.
We took the logarithm of each of the outcome and service expenditure variables so that analyses could be interpreted as elasticities, i.e., a log-log model, where a % change in the outcome can be interpreted in relation to a 1% change in per capita expenditure.
We included additional time-varying confounders from the NOMIS dataset26 to account for changes in the demographics and economic circumstances of each local authority over time. We included five variables, annual: % resident population aged 16-64; % resident population aged 65+; % White UK ethnicity; % 16-64 who were economically inactive; average gross disposable household income per capita (see Appendix).
No ethics approval was necessary for analysis of anonymised data.
Analysis
We first geographically mapped per capita total service expenditure differences between 2017/18 and 2009/10 and service expenditure over time by budget line, to illustrate the extent of variation within the data.
We then ran linear, log-log regression models as our primary analyses (see Appendix), attempting to maximise sample size and statistical power. We first ran the model, for each outcome separately, incorporating total service expenditure as the only exposure variable. Secondly, we included all individual budget lines as unique exposure variables within the same model. This allowed us to observe which specific spending line, controlling for others, appeared to be driving the previous result. For all models, we also included a local authority fixed-effect, which controlled for all observable/unobservable fixed differences between areas over time. We further adjusted for selected time-varying co-variates (above) and a linear trend to control for the overall national expected trend in outcomes. We used robust standard errors (equivalent to clustered by local authority with fixed-effects), and ran all analyses using STATA v16.27
Robustness checks
We re-ran our analyses with several alternative specifications:
-
(i)
Added a one-year lag of the service expenditure exposure variable(s). This aimed to additionally control for the effects of previous service expenditure by local authorities on the outcomes, since any effects might be delayed.
-
(ii)
Added a two-year lag of the service expenditure variable(s) to allow for any potential longer delays.
-
(iii)
Simultaneously included one- and two-year lags of service expenditure.
-
(iv)
Added a one-year lag of the outcome variable. This allowed us to control for all unobservable co-variates that determined that specific outcome in the previous year.
-
(v)
Simultaneously included the one-year lag of the outcome and one-year lag of service expenditure.
-
(vi)
Relaxed the assumption of a shared linear time trend and allowed the trends to vary by local authority.
-
(vii)
Relaxed assumption of linearity and added a quadratic time-squared term.
-
(viii)
While it is impossible to simultaneously and non-parametrically adjust for both unit-specific and time-specific unobserved confounders,28 we further relaxed the linear time trend assumption and instead included a flexible time fixed-effect.
While EQ-5D-5L is a validated measure of population health, there is no gold-standard measure of multimorbidity prevalence. We therefore constructed alternative multimorbidity outcomes and re-ran all the above models. These were: the average count of long-term conditions per capita; prevalence of three or more from the 16 self-reported conditions; four or more; and, finally, presence of both a mental and physical long-term condition. These aimed to capture a range of conceptualisations of multimorbidity, from broader to more restrictive/potentially complex definitions. We additionally examined the different domains of the EQ-5D-5L score individually. Finally, we conducted exploratory (due to small sample size) subgroup analyses for both of the main outcomes, stratified by quintile of average local authority index of multiple deprivation (2010).29 These alternative definitions also allowed us to begin to explore our hypothesised mechanisms (see Figure 1).
Role of the funding source
The funders had no role in study design, data collection, analysis, or interpretation of the results, nor in writing the report and decision to submit for publication.
Results
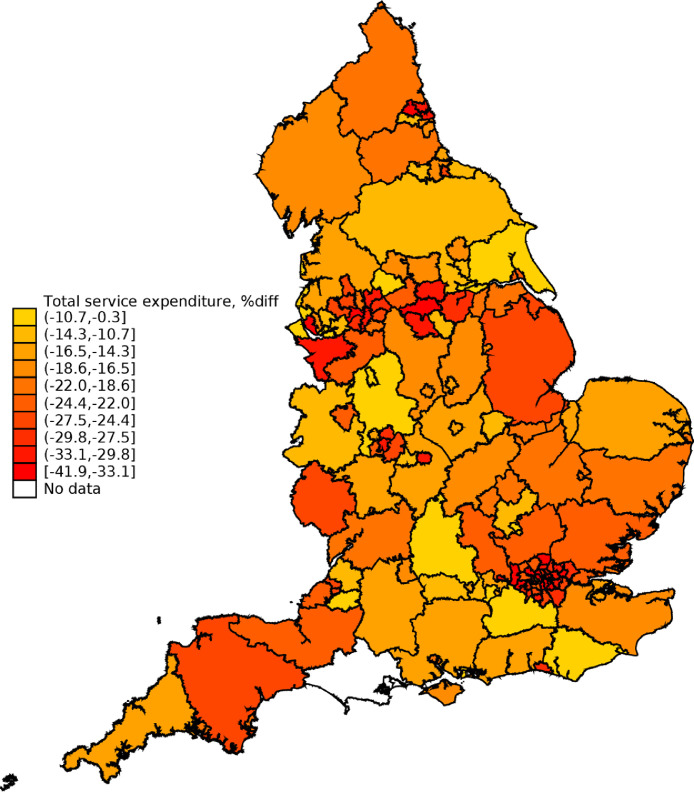
Between 2009/10 and 2017/18, every upper-tier local authority experienced cuts to per capita total service expenditure in real terms. These cuts varied substantially across geography, however, from a nearly 42% cut in Barking and Dagenham and in Westminster, to only a 0·3% cut in Sefton (see Figure 2), with a mean cut of 22%.
Figure 2.
Variation in total per capita service expenditure, geographical and over time (% difference, 2017/18 minus 2009/10). Darker red indicates larger levels of per capita expenditure cuts over the period.
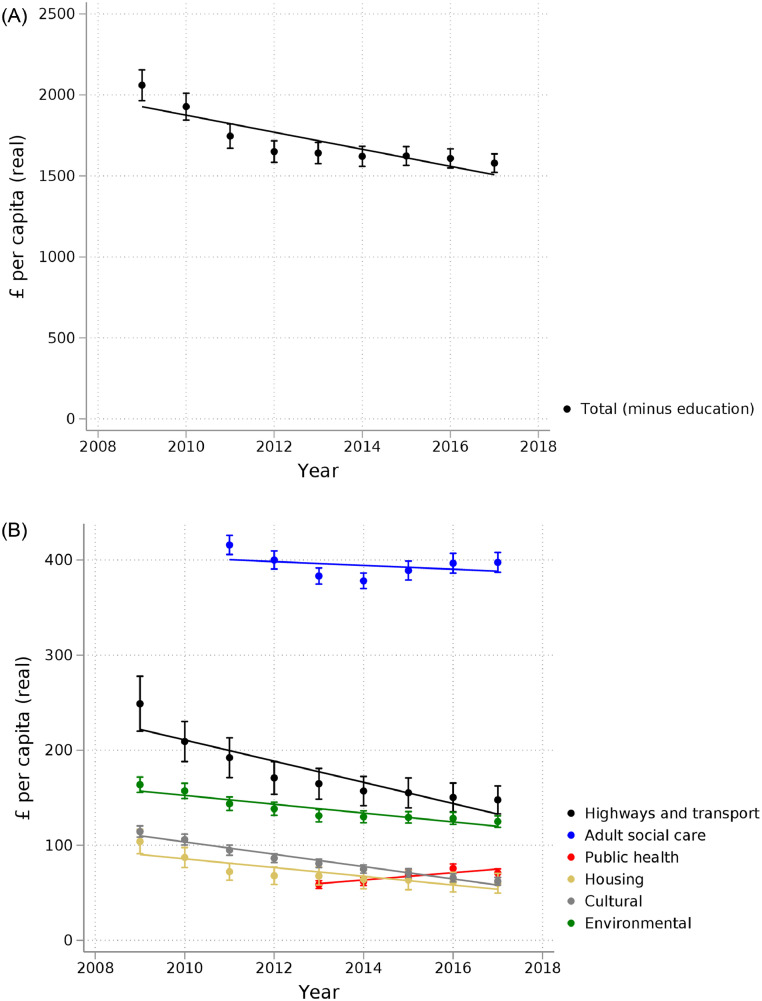
Spending on all specific budget lines decreased (see Figure 3), except for public health (due to the transfer of children's (0-5) services to this budget from 2014/15)30. However, public health nevertheless made up a very small proportion of total local authority spending, on average roughly 4% over the period. Adult social care spending was relatively flat over the period, first decreasing then increasing slightly from 2014/15, making up on average nearly a quarter (23%) of total local authority spending (see Appendix for proportions, and descriptive statistics for all other study variables, including corresponding geographical and time-trends for the main outcomes, and values by local authority used for Figure 2).
Figure 3.
Trends in average upper-tier local authority service expenditure per capita (£, real prices, 2017 equivalent), total expenditure (above) and selected budget lines (below). Vertical bars indicate 95% confidence intervals, with a fitted trend for each series.
Table 2 shows the results for adjusted regression analyses of total local authority service expenditure on outcomes. A 1% increase in per capita total service expenditure was associated with a 0·10% (95% CI 0·03 to 0·16) decrease in the prevalence of multimorbidity. In other words, since the models were linear, a 1% cut to funding would have been associated with a corresponding 0·10% increase in multimorbidity. We found no association (0·003%; 95% CI -0·01 to 0·01) of total service expenditure with health-related quality of life.
Table 2.
Adjusted# total expenditure regression results on log-log models.
| (1) | (2) | |
|---|---|---|
| (Logged) | Multimorbidity (2+) | EQ-5D-5L |
| Total expenditure per capita | -0·0950⁎⁎ | 0·0031 |
| 95% Confidence Interval (p-value) |
-0.1597 to -0.0303 (0·004) |
-0.0065 to 0.0128 (0.525) |
| Observations | 1029 | 735 |
| Adjusted R-squared | 0·116 | 0·095 |
Both models adjusted for Aged 16 – 64 (%), Aged 65+ (%), White UK national (%), Economically inactive - aged 16-64 (%), Gross Disposable Household Income (GDHI) per head (£), local authority fixed effects, a linear time trend, with robust standard errors (S.E.); *p<0.05; **p<0.01; ***p<0.001.
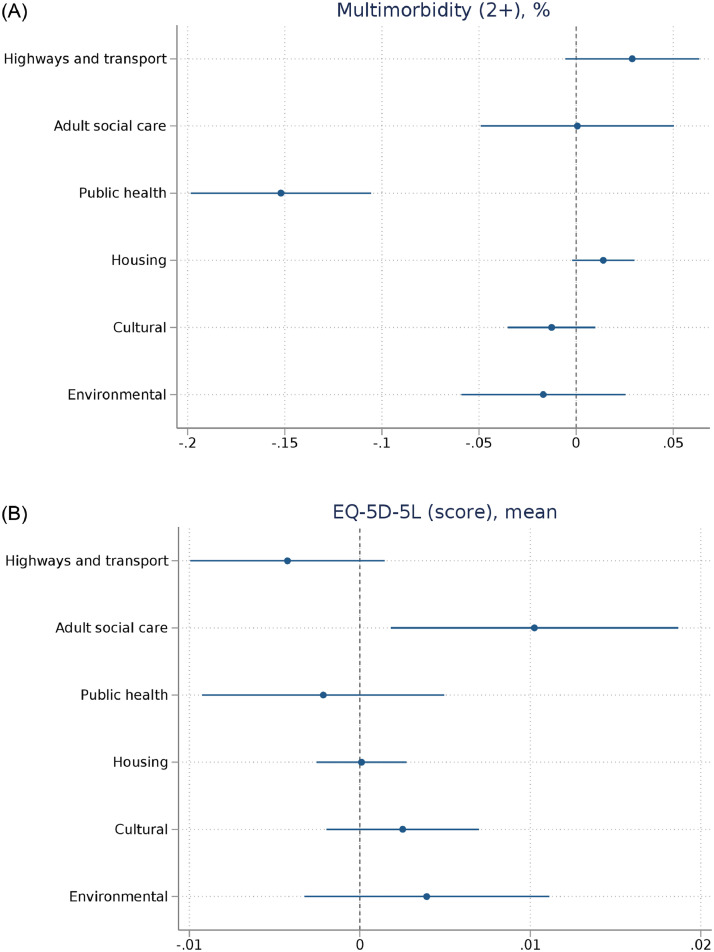
Figure 4 shows the corresponding coefficients from the analyses incorporating individual budget lines. After controlling for other spending lines, a 1% increase in public health expenditure was associated with a statistically significant 0·15% (95% CI 0·11 to 0·20) decrease in the prevalence of multimorbidity. After controlling for other spending lines, a 1% increase in adult social care expenditure was associated with a statistically significant 0·01% (95% CI 0·002 to 0·02) increase in average E5-5D-5L score, health-related quality of life. Consequently, cuts to public health and adult social care would be associated with an increase in multimorbidity and a decrease in health-related quality of life, respectively. Other budget lines were not statistically significantly associated with either outcome in the primary analyses.
Figure 4.
Budget lines coefficient plots. Adjusted# log-log models.
Robustness checks
The associations of total service expenditure and multimorbidity remained statistically significant for six of the eight robustness checks (consistently negative estimates, but not statistically significant when a lagged dependent variable was included alone, and with time fixed-effects). Similarly, for health-related quality of life the robustness estimates remained positive but not statistically significant.
For the models by budget line, the association of public health spending and multimorbidity prevalence remained statistically significant in five of the eight robustness checks. It was no longer statistically significant in both models with two-year time lags (where sample size and power reduced), nor in the model with time fixed-effects (where there is less variation to exploit). All models, nevertheless, gave a consistent negative estimate, where magnitude was also smaller in the non-statistically significant models (plus the model including polynomial of time). Adult social care likewise remained statistically significantly associated with health-related quality of life in five of the eight robustness checks. It was also no longer statistically significant in the two models incorporating two-year lags, nor in the model incorporating local authority-specific time trends. However, direction of the estimates and magnitude remained consistent across all models.
The analyses using alternative multimorbidity outcome indicators suggested total service expenditure was only statistically significantly associated with less complex conceptualisations (two or more, as above, and average count of conditions per capita, but not other definitions). All definitions were, though, highly consistent in their indication of associations with public health expenditure. In particular, the coefficient for mental-physical multimorbidity was nearly twice as large as for two or more conditions, suggesting mental health conditions were a potential driver of results. The coefficients for more complex multimorbidity (three/four or more condition definitions) were also slightly larger than for two or more, suggesting these more complex patients might be closer to tipping points. Finally, the breakdown by deprivation suggested the least deprived quintile might drive the association with total service expenditure (environmental spending appeared to drive this result for the least deprived). However, as expected, the public health association appeared to be driven by the most deprived quintile (see Appendix).
The mobility and pain and discomfort EQ-5D-5L domains appeared to drive the adult social care spend and health-related quality of life results. The breakdown by deprivation was not as clear for health-related quality of life, although a more deprived quintile again appeared to drive results. There was also a suggestion that environmental and cultural service spending might have a beneficial association with health-related quality of life for the most deprived quintile (see Appendix).
Discussion
Our findings suggest that cuts to total local government spending are associated with increased prevalence of multimorbidity. Our estimates suggest that the average cut to total service spending of 22% between 2009/10 and 2017/18 was associated with an average increase of 2.2 percentage points in prevalence of multimorbidity. In particular, multimorbidity appears to be associated with per capita public health expenditure, and health-related quality of life with social care expenditure.
These findings fit with previous studies reporting associations of austerity cuts with health outcomes, as measured by mortality.8, 9, 10, 11 An increase in (multiple) long-term conditions could act as a plausible mechanism, increasing the mortality risk in the population. Our results also agree with previous findings that increased local government spending is associated with other measures of population health, including lower prevalence of individual long-term conditions,12 higher levels of general health,15 fewer preventable hospital visits,13 and higher quality of life for specific sub-populations.14 We build on these findings by showing cuts are not only associated with decreased quantity of life, but also decreased health-related quality of life for the general population who survive.
Although we showed that total public health expenditure increased slightly over the period of analysis, more detailed within-budget spending data has shown that like-for-like public health expenditure actually fell in real-terms from 2014/15. Some public health spending was particularly affected by these cuts, for example, health at work programmes (-47%), the NHS health check programme (-24%), and smoking and tobacco (-24%).30 We might have expected cuts to the NHS health check programme, a health check-up for adults aged 40-74 which might affect diagnosis rate, to have decreased the multimorbidity rate in the short-term. However, it only makes up about 1.5% of public health expenditure, so likely to have had a negligible overall effect. In total, then, these like-for-like austerity cuts to public health budgets might have influenced the increase in multimorbidity prevalence observed over the analysis period,3 ultimately leaving the population more vulnerable to the negative effects of Covid-19 most recently.31
The relative stagnation in social care expenditure we showed might also help explain the similarly flat trend in health-related quality of life previously identified at national level.2 However, this expenditure line is not likely to be the only factor driving trends nationally since social care is only required and used by a relatively small proportion of the total population.
Strengths of this study include the ability to use nationally representative data, to incorporate previously unanalysed, but important, population health outcomes, and to examine associations beyond total service expenditure, also incorporating multiple budget lines simultaneously.
However, we were also partially limited by the data. Our population health measures came from survey responses, which might be subject to response bias. Although, we incorporated the survey weights to attempt to adjust for this, and did not rely on the precise level estimates but rather the changes in consistent survey questions over time to examine associations. Due to legislative changes over the analysis period, we were not able to include education expenditure. The transfer of public health expenditure from the NHS to local authorities from 2013 also limited the follow-up time for the analyses by individual budget line, in order to include this important service expenditure area.
We were also limited in our ability to draw on conventional causal methods, currently lacking to examine multiple policies affecting shared outcomes in tandem, instead relying on the exogenous changes to funding that does not appear to be related to population need.7 Instead, we incorporated fixed-effects to further strip out time-invariant differences across areas, and controlled for time-varying confounders. In robustness checks, we also incorporated several alternative specifications, including lagged dependent variables to further address reverse causality and deal with state dependence in outcomes for areas distinct from time-invariant effects. Our results are also in the opposite direction to those we would expect if reverse causality (endogeneity) were a major issue, where we would expect higher levels of spending to be associated with increased need, that is, associated with higher prevalence of multimorbidity and lower health-related quality of life. If endogeneity instead acted in the same direction as our findings, alternative non-causal explanations for our findings would be more likely.
This is an ecological study, which might also bring questions about the ecological fallacy, that population-level findings might not represent individual-level ones. However, arguably both our exposure (service expenditure) and outcomes (prevalence and average score) are population-level ones, not necessarily reducible to purely individual-level characteristics, although acting through individuals.32 For example, our logic model hypothesises indirect (spillover) effects that would not necessarily be captured by individual-level analysis or policy intervention. However, there might be certain services that have a greater proportion of direct, rather than indirect, effects. For example, social care service expenditure would be expected to have a much greater direct effect on those cared for by these services.
Some service expenditure areas might also be more directly driven by need than others, which would introduce some endogeneity. Social care services are again a potential example here, where direct access to the (publicly financed) services is determined by statutory eligibility. However, over the analysis period adult social care expenditure also reflected the overall local authority expenditure picture, where the largest cuts occurred in the most deprived areas,18 those where we would expect need to be highest. As above, the expected direction of endogeneity would also suggest our results were conservative if this was an issue. Nevertheless, as in all observational studies, we cannot rule out the possibility of residual confounding.
Lastly, we were limited to data on service expenditure, where spending alone is not going to give the full picture. There might have been other impacts of the full fiscal austerity package we were not able to capture. What is subsequently done with the money is largely unrecorded, and likely to be variable across geography (including within-local authority variation) where we rely on temporal rather than geographical variation. This is likely to have as much, or more, of an impact on the outcomes we examined. This, and baseline differences in healthcare and local government administration, might also caution generalisability of findings internationally. Although, as above, similar findings are found in other contexts using other population health outcomes. The budget lines we examined are also implemented to accomplish outcomes outside of those we are measuring, for example economic growth and productivity.
These findings have potential implications for any future contemplation of austerity cuts, which might be considered in light of the previously unseen levels of public expenditure, and increased public debt, to combat the Covid-19 pandemic. Recent analysis by the Institute for Fiscal Studies shows that, despite planned increases in real spending power announced in the Chancellor's 2021 Autumn Budget, spending will still be substantially less for local government in 2024/25 than in 2010, and some local authorities might still have to cut additional services over the next few years due to increased financial pressures.33
Policymakers should consider that any suppression of funding for wider local government services might have implications for increasing future healthcare service costs, and decreasing population resilience for future pandemics or other shocks. These population health deteriorations would be difficult to reverse. In particular, national policymakers involved in determining grant formulas should aim to incorporate these trade-offs between short- and long-term funding, and to better reflect the additional reliance of some communities, the more deprived, on this public investment.
Any alternative healthcare-centred strategy will necessarily involve some level of identifying and successfully engaging and treating ‘high-risk’ (however this threshold is defined) individuals. Geoffrey Rose outlined this as the ‘prevention paradox’, “a large number of people exposed to a low risk is likely to produce more cases than a small number of people exposed to a high risk.”34 A population-level ‘mass’ prevention strategy, aiming to shift the whole population's distribution of the risk variable(s) by a small amount, is likely, therefore, to be much more effective than one targeted at high-risk individuals alone. This might be particularly true for prevention of long-term conditions, where the majority of any one individual's potential benefit is small, especially in the short-term.34 Indeed, additional public health expenditure has already been shown to be very productive, more productive than additional healthcare (NHS) expenditure in England.35
Future research should examine further the plausible mechanisms between service expenditure and outcomes we hypothesise, and potential interaction effects between expenditure lines. It should also consider whether more recent attempts to target social determinants directly within healthcare systems can act as a substitute for investment in other public spending areas, or whether there is an optimal service expenditure area for prevention of disease and promoting general population health.
Investment in local government services might have potential to prevent disease accumulation and to increase population wellbeing, forming part of the investment in prevention and in addressing the wider determinants of health. Fiscal austerity could have consequences for both health and health-related quality of life. Policymakers should consider the potential health consequences of government service expenditure cuts and knock-on effects for health systems.
Contributors
JS led the study design, conducted the statistical analysis, and wrote the first draft of the manuscript. JS and MS verified the underlying data, and JS, PB, BG, SWM, NG, AMR, MS had full access. JS, PB, BG, SWM, NG, AMR, MS fed in to the study design, reviewed the methodology and results, and provided critical revisions to the final submitted manuscript.
Data availability statement
The expenditure data used is freely available for download at the Place-based Longitudinal Data Resource (https://pldr.org/dataset), and the time-varying confounders from the ONS NOMIS dataset (https://www.nomisweb.co.uk). The multimorbidity prevalence data cannot be shared publicly because of a data sharing agreement. These were constructed from GP Patient Survey data, available from Ipsos Mori/NHS England (https://gp-patient.co.uk/contact) for researchers who meet the criteria for access.
Declaration of interests
The authors declare no conflicts of interest.
Acknowledgements
The work is part of JS's personal research Fellowship, funded by the Medical Research Council (MRC Grant Ref: MR/T027517/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100436.
Appendix. Supplementary materials
References
- 1.Leon DA, Jdanov DA, Shkolnikov VM. Trends in life expectancy and age-specific mortality in England and Wales, 1970–2016, in comparison with a set of 22 high-income countries: an analysis of vital statistics data. Lancet Public Health. 2019;4(11):e575–ee82. doi: 10.1016/S2468-2667(19)30177-X. [DOI] [PubMed] [Google Scholar]
- 2.Shah V, Stokes J, Sutton M. Inequalities in health-related quality of life: repeated cross-sectional study of trends in general practice survey data. Br J Gen Pract. 2021;71(704):e178–ee84. doi: 10.3399/BJGP.2020.0616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singer L, Green M, Rowe F, Ben-Shlomo Y, Kulu H, Morrissey K. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002-2015. J Comorb. 2019;9 doi: 10.1177/2235042X19872030. 2235042X19872030-2235042X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Academy of Medical Sciences. Multimorbidity: a priority for global health research, 2018.
- 5.World Health Organization. Closing the gap in a generation: health equity through action on the social determinants of health: final report of the commission on social determinants of health. 2008. https://apps.who.int/iris/handle/10665/43943. Accessed 13 April 2022.
- 6.McGovern L, Miller G, Hughes-Cromwick P. Health Affairs. 2014. The relative contribution of multiple determinants to health outcomes. Health Policy Brief, August 21. [Google Scholar]
- 7.Marmot M, Allen J, Boyce T, Goldblatt P, Morrison J. Health equity in England: the marmot review 10 years on. 2020. https://www.health.org.uk/publications/reports/the-marmot-review-10-years-on Accessed 13 April 2022.
- 8.Alexiou A, Fahy K, Mason K, et al. Local government funding and life expectancy in England: a longitudinal ecological study. Lancet Public Health. 2021;6(9):e641–e6e7. doi: 10.1016/S2468-2667(21)00110-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loopstra R, McKee M, Katikireddi SV, Taylor-Robinson D, Barr B, Stuckler D. Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007-2013. J R Soc Med. 2016;109(3):109–116. doi: 10.1177/0141076816632215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koltai J, McKee M, Stuckler D. Association between disability-related budget reductions and increasing drug-related mortality across local authorities in Great Britain. Soc Sci Med. 2021;284 doi: 10.1016/j.socscimed.2021.114225. [DOI] [PubMed] [Google Scholar]
- 11.Toffolutti V, Suhrcke M. Does austerity really kill? Econ Human Biol. 2019;33:211–223. doi: 10.1016/j.ehb.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Bradley EH, Canavan M, Rogan E, et al. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Aff. 2016;35(5):760–768. doi: 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- 13.McCullough JM, Curwick K. Local health and social services spending to reduce preventable hospitalizations. Popul Health Manag. 2020;23(6):453–458. doi: 10.1089/pop.2019.0195. [DOI] [PubMed] [Google Scholar]
- 14.Longo F, Claxton K, Lomas J, Martin S. Does public long-term care expenditure improve care-related quality of life of service users in England? Health Econ. 2021;30(10):2561–2581. doi: 10.1002/hec.4396. [DOI] [PubMed] [Google Scholar]
- 15.Brown TT, Martinez-Gutierrez MS, Navab B. The impact of changes in county public health expenditures on general health in the population. Health Econ Policy Law. 2014;9(3):251–269. doi: 10.1017/S1744133114000024. [DOI] [PubMed] [Google Scholar]
- 16.Crawford R, Phillips D. Local government spending: where is the axe falling? 2012.
- 17.Treasury HM. 2010. Spending review 2010: The Stationery Office. [Google Scholar]
- 18.Phillips D, Sampson P. Changes in councils’ adult social care and overall service spending in England, 2009–10 to 2017–18. Institute for Fiscal Studies; 2018. Available at: www.ifs.org.uk/publications/13066. Accessed 15 June 2018.
- 19.Institute for Government . 2022. Local Government Funding in England.https://www.instituteforgovernment.org.uk/explainers/local-government-funding-england Accessed 13 April 2022. [Google Scholar]
- 20.Innes D, Tetlow G. Central cuts, local decision-making: changes in local government spending and revenues in England, 2009-10 to 2014-15. 2015. https://ifs.org.uk/uploads/publications/bns/BN166.pdf Accessed 13 April 2022.
- 21.England NHS, Ipsos MORI. 2020. GP Patient Survey.https://www.gp-patient.co.uk/ Accessed 13 April 2022. [Google Scholar]
- 22.EuroQol Group . EQ-5D-5L user guide. 2019. Basic information on how to use the EQ-5D-5L instrument 2019.https://euroqol.org/publications/user-guides/ Accessed 13 April 2022. [Google Scholar]
- 23.C. Baker, Population estimates & GP registers: why the difference, 2016. https://commonslibrary.parliament.uk/population-estimates- gp-registers-why-the-difference/. Accessed 13 April 2022
- 24.University of Liverpool . 2020. Place-based Longitudinal Data Resource.https://pldr.org/dataset Accessed 13 April 2022. [Google Scholar]
- 25.ONS. Dataset: Consumer price inflation time series. 2020. https://www.ons.gov.uk/economy/inflationandpriceindices/datasets/consumerpriceindices. Accessed 13 April 2022.
- 26.ONS. nomis: official labour market statistics. 2021. https://www.nomisweb.co.uk. Accessed 13 April 2022.
- 27.StataCorp . StataCorp LP; College Station, TX: 2020. Stata Statistical Software: Release 16. [Google Scholar]
- 28.Imai K, Kim IS. On the use of two-way fixed effects regression models for causal inference with panel data. Political Anal. 2021;29(3):405–415. [Google Scholar]
- 29.Ministry of Housing Communities & Local Government. Official Statistics: English indices of deprivation 2010. 2011. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2010. Accessed 13 April 2022.
- 30.The King's Fund . 2021. Spending on public health.https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/spending-public-health Accessed 13 April 2022. [Google Scholar]
- 31.Imam Z, Odish F, Gill I, et al. Older age and comorbidity are independent mortality predictors in a large cohort of 1305 COVID-19 patients in Michigan, United States. J Intern Med. 2020;288(4):469–476. doi: 10.1111/joim.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwartz S. The fallacy of the ecological fallacy: the potential misuse of a concept and the consequences. Am J Public Health. 1994;84(5):819–824. doi: 10.2105/ajph.84.5.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.IFS . 2021. Autumn Budget and Spending Review 2021.https://ifs.org.uk/budget-2021 Accessed 13 April 2022. [Google Scholar]
- 34.Rose G. Strategy of prevention: lessons from cardiovascular disease. British Med J (Clinical research ed) 1981;282(6279):1847–1851. doi: 10.1136/bmj.282.6279.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martin S, Lomas J, Claxton K. Is an ounce of prevention worth a pound of cure? A cross-sectional study of the impact of English public health grant on mortality and morbidity. BMJ Open. 2020;10(10) doi: 10.1136/bmjopen-2019-036411. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The expenditure data used is freely available for download at the Place-based Longitudinal Data Resource (https://pldr.org/dataset), and the time-varying confounders from the ONS NOMIS dataset (https://www.nomisweb.co.uk). The multimorbidity prevalence data cannot be shared publicly because of a data sharing agreement. These were constructed from GP Patient Survey data, available from Ipsos Mori/NHS England (https://gp-patient.co.uk/contact) for researchers who meet the criteria for access.