Abstract
Background
Surgical education strongly involves the use of mentorship to improve the confidence and efficiency of trainees. Social distancing due to the COVID-19 pandemic may serve as a catalyst to promote the use of telementoring and other remote learning opportunities in medical education.
Methods
A comprehensive literature review was performed using the electronic databases PubMed, Embase, Web of Science, Scopus, and the Cochrane Library with respect to telementoring in the surgical field.
Results
The overall consensus of telementoring experience among all 25 studies was generally positive, citing “positive experience,” “increased confidence,” and “increased surgical skill.” Using over 15 different technologies, a total of 12 simulations, 149 tasks, and 491 surgeries were conducted via telementoring. Eight mentor-mentee relationships were identified, with the most common relationship being surgeon-to-surgeon in 12 studies.
Conclusions
The implementation of telementoring has been shown to be effective in improving surgical skills and learner experiences while overcoming financial and geographical barriers.
Keywords: Mentoring, Surgery, Surgical training, Virtual, Technology, Medical education
1. Introduction
With the recent outbreak of COVID-19, many safety measures have been implemented to avoid the use of the traditional in-person approach to teaching. To overcome this obstacle, programs have been adopting the practice of telementoring, an alternative method of enhancing medical education remotely. Telementoring is “a relationship, facilitated by telecommunication technology, in which an expert (Mentor) provides guidance to a less experienced learner (Mentee) from a remote location.“1 The employment of mentorship programs for health professionals has been widely accepted as beneficial for the growth and development of both the mentor and mentee.2 While mentors are able to impart knowledge and become more aware of their own professional skills, mentees have reported increased confidence, job satisfaction, productivity, career advancement, and much more.3 Thus, the adoption of telementoring programs can overcome the geographical restrictions in place due to COVID-19, while continuing to foster these mentor-mentee relationships in the healthcare field.
The use of telementoring has proven numerous benefits towards the development of surgeons. Telementoring can be used to increase access to geographically isolated areas while providing adequate surgical training and education.4 Surgeons in rural areas of developing countries can be successfully mentored at the accessibility of the mentoring physician's country.5 These systems have provided a practical and cost-effective alternative mentoring tool that overcomes the cost of on-site mentoring programs that require travel costs and time off from work for physicians.6 With the recent advances in technology, telementoring has also grown from audio and video feedback systems to include the use of robotic arms, augmented reality, or live on-screen demonstrations using cursors (telestrations). Such advances have been promising for the continuing advancement of medical education in the surgical field, especially with the abrupt restrictions implemented with the onset of COVID-19.
The purpose of this scoping review was to identify various modalities of telementoring and to evaluate their impact on surgical education. These findings can inform medical educators and surgeons on how to best develop and implement telementoring systems with the goal of enhancing the quality of clinical medical education.
2. Methods
An expert searcher conducted a comprehensive review of the literature in telementoring within the surgical field published between January 2010 and September 2020. Databases searched included PubMed, Embase, Web of Science, Scopus, and the Cochrane library. Subject headings/index terms were utilized in combination with free-text words or natural language terms representing telementoring and surgical education. Examples of those terms include (“telementoring OR tele-mentoring OR ementor OR e-mentor”) AND (“Specialties, Surgical"[Mesh] OR surgery OR surgical OR orthopedic OR orthoped*“). See a comprehensive search strategy in the Appendix. Search results were imported to Covidence software for screening. Studies were included if they were published in English focusing on the use of telementoring in the surgical field across the spectrum of medical education. Studies were excluded if they were not primary research studies, the mentoring was not primarily virtual, a full-text article was not available, or if they were not pertaining to telementoring in surgery. Review articles, case reports, commentaries, editorials, published conference abstracts, and letters were excluded. Title/abstract and full-text studies were independently screened by 2 reviewers (AL and MP). A standardized data abstraction form was developed and utilized. Data extracted included the year of publication, country, setting, mentee participants, mentor participants, sample size, type of intervention, purpose of study, study design, technology used, data collection method, surgical task, and subspecialty. We determined the style of mentoring relationships by utilizing the classifications described in a study by Burgess et al.3 These styles include the classic model, ‘trans’ model, networking model, reverse mentoring, group mentoring, spot mentoring, virtual mentoring, and shadowing.3 The data extraction was conducted in duplicates and independently by AL and MP. Any disagreements from full-text screening and data extraction were resolved through discussion with MM serving as a tie-breaker. We conducted a qualitative scoping review due to wide variations in the selected studies in terms of study design, type of intervention, technology used, evaluation techniques, and outcomes.
We applied the four levels of evaluation model by Kirkpatrick to analyze the types of outcomes measured in each study.7 As is outlined in his book “The Four Levels of Evaluation”, Level 1 is a measurement of the learner's attitude toward the training, Level 2 is a measurement of the learning of the skill or knowledge itself, Level 3 is a measurement of whether the participant has changed their behavior and will apply what they learn going forward, and Level 4 is a measurement of direct results, in this case, changing patient outcomes and satisfaction post-mentoring.
3. Results
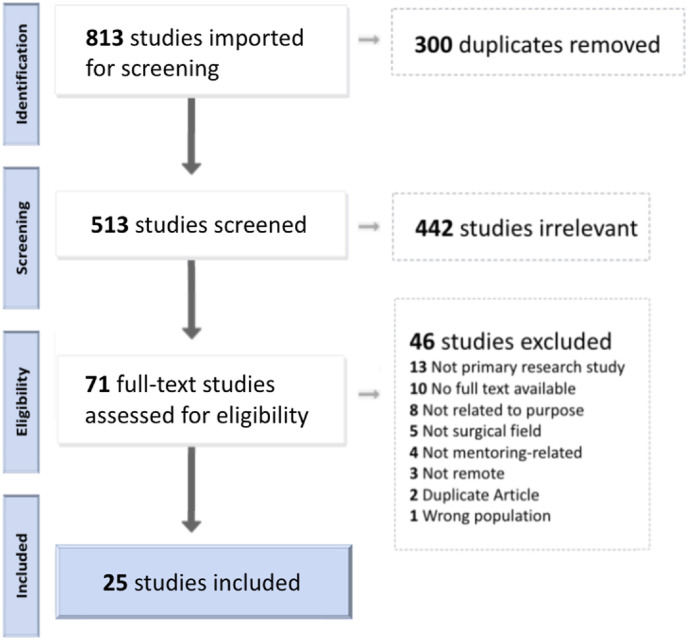
Out of 813 studies, we selected 25 studies for the review after removing duplicates and screening articles against inclusion/exclusion criteria set a priori. The PRISMA flow diagram of study selection is shown in Fig. 1 .
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart.
What follows is synthesized evidence from the selected studies, presented in 6 segments: 1) characteristics of selected studies; 2) style of mentor-mentee relationship; 3) technology used; 4) number of surgeries or tasks performed; 5) data collection methods; and 6) outcomes described. The summary of key findings from each study is shown in Table 1 .
Table 1.
Description of studies included in the scoping review.
| Author | Country | Setting | Technology Used | Mentee Participants | Intervention | Measures of Outcome | Outcomes | Level of Evaluation |
|---|---|---|---|---|---|---|---|---|
| Andersen et al., 201621 | USA | Simulation Lab | System for Telementoring with Augmented Reality (STAR) | 20 Premedical & Medical Students | 2 tasks with multiple sets each | Placement error of incisions, number of focus shifts, and task completion time |
|
2 |
| Zakrison et al., 201711 | USA | Online Communication | Email, FaceTime, Skype, GoToMeeting | 65 Resident, Fellow, & Junior Faculty | N/A | Surveys |
|
1, 3 |
| Ponce et al., 201426 | USA | Clinical, Operating Room | Stryker Endoscopic tower | 6 Residents | 15 surgeries | Length of surgery and satisfaction surveys |
|
1, 2 |
| Ereso et al., 201027 | USA | Simulation Lab | Mounted Canon VB-50i | 8 Residents | 24 surgeries | Operative Performance Scale and surveys |
|
1,2 |
| Chou et al., 201923 | Australia | Clinical | 1 Surgeon | 85 surgeries | Sink modification of the Clavien-Dindo classification system, Harris Hip score, Harris Pain Score, Yasunaga classification of Hip congruency, and Tonnis classification of Pre- and postoperative grading of osteoarthritis |
|
2, 4 | |
| Forgione et al., 201528 | Italy, Russia | Clinical, Operating Room | OR1 Smartconnect | 1 Surgeon | 2 surgeries | Surgical complications |
|
2, 3, 4 |
| Vera et al., 201433 | USA | Simulation Lab | Augmented Reality Telementoring (ART) | 19 Medical Students | 10 suturing tasks each | Speed of placement, placement errors, Wright's cumulative average model of the learning curve slope, and surveys |
|
1,2 |
| Treter et al., 201332 | USA | Clinical, Operating Room | Video | 2 Surgeons | 2 surgeries | Surgical complications and length of surgery |
|
2, 4 |
| Snyderman et al., 201610 | USA, Slovenia | Clinical, Operating Room | VisitOR1 | 1 Skull-based Surgical Team | 10 procedures | Telesurgery Evaluation Form, Surgical complications, the extent of tumor resection, length of surgery, and satisfaction survey |
|
1, 2, 3, 4 |
| Shin et al., 201524 | USA | Clinical, Operating Room | da Vinci Connect | 11 Residents | 55 surgeries | Global Evaluative Assessment of Robotic Skill (GEARS) form and an evaluation of the mentoring interface |
|
1, 2, 4 |
| Ponsky et al., 201415 | USA | Clinical, Operating Room | Skype, VisitOR1 | 4 Surgeons | 6 surgeries | Surgical complications and length of surgery |
|
2, 4 |
| Okrainec et al., 201037 | Canada, Botswana | Simulation Lab | Skype | 13 Surgeons & 3 Junior Trainees | 5 FLS tasks each | Simulator scores for each task and Fundamentals of Laparoscopic Surgery (FLS) score |
|
2 |
| Nguyen et al., 201720 | USA, Canada (two surgeons in Guatemala and Argentina) | Clinical, Operating Room | VisitOR1 | 15 Surgical Fellows & Surgeons | 30+ surgeries with a minimum of 2 surgeries per mentee | Surgical complications and survey on quality of telecommunication and effectiveness of mentoring by both mentee and mentor |
|
1, 2, 3, 4 |
| Mizota et al., 201716 | Japan | Simulation Lab | Go Pro HERO3+, Google Hangouts | 20 Residents | 91 remote sessions | Survey, task completion time, and knot error points, and duration of coaching |
|
1,2 |
| Miller et al., 201117 | USA, Australia | Clinical, Operating Room | Skype | 1 Surgeon | 3 surgeries | Surgical complications and length of surgery |
|
2, 3, 4 |
| Kirkpatrick et al., 201518 | Canada | Simulation Lab | Skype | 12 Med techs | 1 simulation task | Performance on incision fluid loss and time, retraction fluid loss and time, direction fluid loss and time, identification fluid loss and time, packing fluid loss and time, number of sponges, skin incision closure percentage, and survey of participants confidence levels |
|
1, 2 |
| Hinata et al., 201425 | Japan | Clinical, Operating Room | da Vinci S | 4 Surgeons | 120 surgeries with 30 surgeries per surgeon | Operating time, blood loss, transfusion %, complication %, continence rate at 3 month post-op, and surgical margin % |
|
2, 4 |
| Fuertes-Guir et al., 201619 | Spain | Clinical, Operating Room | Adobe Connect | 2+ Surgeons | 36 patients | Operating time, length of hospital stay, conversions, post-op outcomes |
|
2, 4 |
| Dawe et al., 201831 | Canada | Simulation Lab | Reacts Lite | 4 Non-Surgeon Medical Officers | 3 tasks per mentee | Task-specific scores determining success, comfort and pre- and post-operative willingness survey |
|
1, 2 |
| Datta et al., 201536 | USA, Paraguay, Brazil, Germany | Clinical, Operating Room | Google Glass | 2 Surgeons | 10 surgeries | Lichtenstein-Specific Operative Performance Rating Scale (OPRS) and post-training survey |
|
1, 2, 3 |
| Burckett-St Laurent et al., 201613 | Canada | Simulation Lab | Skype | 19 Anesthetists | 19 tasks | 22 item procedural checklist and 9 item Global Rating Scale (GRS) and post-training survey questionnaire |
|
1, 2 |
| Budrionis et al., 201630 | Norway | Simulation Lab | Laprotrain Endoscopic Trainer | 8 Telemedicine & E-Health Students | 6 tasks per mentee | Localization error distance, duration of task, quality of mentoring communication, user satisfaction survey |
|
1, 2 |
| Bruns et al., 20168 | USA, France | Clinical, Operating Room | VisitOR1 | 2 Surgeons | 2 surgeries | Surgical complications and length of surgery |
|
1, 2, 3, 4 |
| Andersen et al., 201722 | USA | Simulation Lab | System for Telementoring with Augmented Reality (STAR) | 20 Premedical & Medical Students | 2 tasks per mentee | Placement error, focus shifts, and time of task completion |
|
2 |
| Glick et al., 202012 | Israel | Simulation Lab | HoloLens AR glasses | 13 Medical Students | 13 tasks | Surveys, placement accuracy, placement time, and nine procedure-specific parameter assessments |
|
1, 2 |
3.1. Characteristics of selected studies
Out of 25 studies selected, 13 studies were case series, 10 studies were randomized controlled trials, with 2 studies following other study designs. Among all studies included, 9 were conducted within the USA; 5 were conducted at sites in the USA and other countries; 9 were in another country; 2 were between other countries outside the USA. For example, in Bruns et al., two experienced fellowship-trained minimally invasive pediatric surgeons in Akron, OH, and Denver, CO were connected with mentee pediatric surgeons in Paris, France.8 Okrainec and colleagues showed that through the use of telementoring, there was an improvement in surgical skills in resource-restricted countries, achieving a 100% technical skills pass rate.9 This training platform provided a cost-effective method of teaching in developing countries and could be used to teach laparoscopic skills anywhere in the world with internet access. This study along with many others implied that telementoring can offer proficient teaching of medical and surgical skills in countries that lack training opportunities. Snyderman et al. expressed the importance of the geographical location of the mentee group if the benefit is to provide skills and expertise to an area that is in need, stating that it is “desirable to select centers that are geographically positioned to become regional centers of excellence.“10 In this way, those learning centers would be able to disseminate the knowledge appropriately throughout their region, and “become teachers for the next generation of surgeons.“10
The setting of the telementoring experience also varied between studies. Thirteen out of the 25 studies took place in clinical settings, while 11 were conducted within simulation labs. Clinical settings included the operating room as well as pre-operative and post-operative consultations. Simulation labs often included learning sessions with suturing skill tasks, laparoscopic surgical tasks, and surgical tasks on animal models. Zakrison et al. utilized only online communication via various modalities that revolved around fostering academic and personal growth in young acute care surgeons.11 This study was not deemed to specifically take place in either the clinical setting or simulation lab.
3.2. Types of mentoring participants
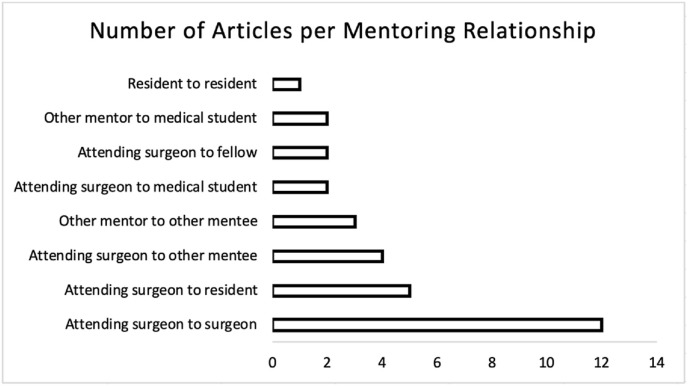
Although various forms of mentor-mentee relationships were found within the 25 selected studies, some trends were noticed. Surgeon mentors were the most common, seen in 20 of the 25 studies. Eight mentor-mentee relationships were identified: surgeon to surgeon in 12 studies, surgeon to resident in 5 studies, and surgeon to medical student in 2 studies. For example, the study by Glick and colleagues investigated telementoring of medical students by physicians who previously served as Israel Defense Forces battalion combat surgeons.12 Another example is Snyderman et al. who described telementoring between a more experienced surgical team from the University of Pittsburgh providing mentoring to a similarly focused team from the University of Maribor in Slovenia.10 Some studies involved multiple mentor-mentee relationships. Fig. 2 depicts the types of mentoring relationships and the number of studies that implemented that style of mentorship.
Fig. 2.
Types of mentoring relationships.
The studies in our scoping review exemplified more than one style of mentoring based on the model of mentoring styles classified by Burgess et al.3 Virtual mentoring encompasses all 25 studies that we selected, and under the umbrella of virtual mentoring, the most commonly utilized mentoring style was the classic model. The classic model is seen between a more experienced mentor and a less experienced mentee within the same field with a “formal approach, well planned, with a specific setting.“3
A wide array of mentoring relationships was highlighted in the selected studies. In a study by Burckett-St. Laurent et al., training was provided for telementoring including four online simulation sessions and one offline lecture.13 In contrast, the study by Vera et al. involved mentees and mentors in either a traditional mentoring or a telementoring experience for only 1 h, during which both groups were assessed on their laparoscopic skills and the efficiency of the mentoring.14
3.3. Type of technology used in telementoring
Out of 25 included studies, over 15 different technologies were utilized to facilitate telementoring, with the most common being video call software, used by 11 studies. Screen sharing software was utilized in 6 studies, robotic cameras in 5 studies, and augmented reality in 4 studies. The screen-sharing software was often utilized for laparoscopic surgeries or robotic surgeries, particularly helpful if the screen was the primary visual source of the mentee surgeon. Various telementoring software programs were used in the included studies: video or conference call software (e.g., Skype, FaceTime, Google Hangouts, Adobe Connect),9 , 11 , 13 , 15, 16, 17, 18, 19 VisitOR1 , 8 , 10 , 15 , 20 System for Telementoring with Augmented Reality (STAR),21 , 22 Email,11 , 23 and da Vinci Connect.24 , 25 Other technologies were employed as well, including Stryker Endoscopic Tower,26 Canon VB-50i,27 OR1 Smartconnect,28 GoPro Hero 3+,16 Google Glass,29 Laprotrain Endoscopic Trainer,30 HoloLens AR Glasses,12 Reacts Lite,31 an augmented reality telementoring (ART) platform,14 and an unspecified video-sharing system.32 A few studies utilized multiple technologies for telementoring.11 , 15 For example, Mizota and colleagues utilized both Google Hangouts and a wearable camera (GoPro Hero3+) to transmit the images and facilitate the telementoring.16
In addition to the traditional telementoring video and audio communication, multiple studies also utilized on-screen annotations. Budrionis et al. studied the impact of on-screen telestrations on the efficacy of telementoring education for laparoscopic tasks.30 The results of their study showed a decreased duration of assigned tasks, increased quality of mentoring, and an overall positive attitude of the participants in the group with on-screen annotations.30 The study suggests that various modalities, such as on-screen annotations, can be added or subtracted from the traditional telementoring format depending on the needs of the specific task or surgery. In a study by Fuertes-Guiró et al., on-screen annotations were also utilized to help “specify specific anatomical points where action should be taken” and “minimize doubts in the operating room.“19 A full breakdown of characteristics for each study can be found in Table 1.
3.4. Types of interventions
Depending on the study, participants within a mentor-mentee relationship performed surgeries, surgical tasks, or worked with simulators all under telementoring guidance. In total, of the 25 studies we reviewed, 12 simulations, 149 tasks, and 491 surgeries were conducted through the use of telementoring technology.
In Ereso et al., general surgery residents with no formal subspecialty training beyond 3 clinical years were instructed to participate in 3 scenarios designed to simulate the performance of a subspecialty operative procedure, including a cardiac operation of suture repair of right ventricular injury, an orthopedic operation of external fixation of open tibial fracture, and a neurosurgical operation of craniectomy for a traumatic subdural hematoma.27 The subspecialty task was performed in order to demonstrate the “feasibility of the technology in transferring subspecialty skills by the proctor to the operating resident.“27 Table 2 shows a full breakdown of the specific tasks performed in each study, as well as the surgical subspecialty of the task or surgery.
Table 2.
Surgical subspecialty and surgical task.
| Author | Subspecialty | Task |
|---|---|---|
| Andersen et al., 201621 | Non-specified surgical training | Port placement, abdominal incision |
| Zakrison et al., 201711 | N/A | N/A |
| Ponce et al., 201426 | Orthopedics | Arthroscopic shoulder surgery (rotator cuff repair, and shoulder instability procedures) |
| Ereso et al., 201027 | General surgery (performing scenarios in Cardiac, Orthopedic, Neurosurgery) | Penetrating right ventricular injury requiring suture repair, an open tibial fracture requiring external fixation, and a traumatic subdural hematoma requiring craniotomy |
| Chou et al., 201923 | Orthopedics | Periacetabular osteotomy (PAO) |
| Forgione et al., 201528 | Colorectal surgery | Laparoscopic colonic resections |
| Vera et al., 201433 | Non-specified surgical training | Laparoscopic suturing and knot-tying tasks |
| Treter et al., 201332 | Endocrine surgery | Posterior retroperitoneoscopic adrenalectomy (PRA) |
| Snyderman et al., 201610 | Otolaryngology | Endoscopic endonasal surgeries of the skull base |
| Shin et al., 201524 | Urology | Prostatectomy and kidney cases (radical or partial nephrectomy) |
| Ponsky et al., 201415 | Pediatric surgery | Thoracic surgery left lower lobe resection, gastric stimulator placement, laparoscopic inguinal hernia repair |
| Okrainec et al., 201037 | Non-specified surgical training | Laparoscopic suturing and knot-tying tasks |
| Nguyen et al., 201720 | Bariatric surgery | Laparoscopic sleeve gastrectomy |
| Mizota et al., 201716 | General surgery, thoracic surgery | Suturing tasks (needle-holding, needle-driving, knot-tying) |
| Miller et al., 201117 | Endocrine surgery | Posterior retroperitoneoscopic adrenalectomy (PRA) |
| Kirkpatrick et al., 201518 | Trauma | Laparotomy with midline incision into the peritoneal cavity followed by sponge packing of an exsanguinating liver hemorrhage |
| Hinata et al., 201425 | Urology | Robotic surgery prostatectomy |
| Fuertes-Guir et al., 201619 | Bariatric surgery | Laparoscopic bariatric surgery (Roux-en-Y gastric bypass and sleeve gastrectomy) |
| Dawe et al., 201831 | Non-specified surgical training | ED thoracotomy, surgical airway, chest tube insertion |
| Datta et al., 201536 | General surgery | Lichtenstein hernioplasty |
| Burckett-St Laurent et al., 201613 | Anesthesiology | Ultrasound-guided supraclavicular brachial plexus block (SCB) |
| Budrionis et al., 201630 | Non-specified surgical training | 4 localizations and 2 cutting exercises using a laparoscopic simulator |
| Bruns et al., 20168 | Pediatric surgery | Laparoscopic appendectomy; thoracoscopic total thymectomy |
| Andersen et al., 201722 | Military medicine | Adhesive placement and abdominal incision |
| Glick et al., 202012 | Military medicine | Chest thoracotomy |
3.5. Measures of outcome from telementoring
A mixture of telementoring evaluation techniques was detailed across the included studies. Of the 25 studies, 11 studies assessed the effectiveness of the telementoring experience via measurements of surgical performance based on task accuracy, speed, surgical outcomes, etc. Task completion time14 , 21 , 22 , 30 and length of surgery were also measured.8 , 15 , 17 , 19 , 25 , 26 , 32 Two studies only surveyed participants (both mentors and mentees) to determine the effectiveness. The most common method, used by 12 studies, was to evaluate both the surgical performance and surveys of participants. Other surgical telementoring outcomes were measured with more specific scales, including the Global Rating Scale of Operative Performance,27 Sink modification of the Clavien-Dindo classification system, Harris Hip Score, Harris Pain Score, Yasunaga system for hip congruency, Tonnis Classification for Pre- and postoperative grading of osteoarthritis,23 Global Evaluative Assessment of Robotic Skill (GEARS) form,24 Fundamentals of Laparoscopic Surgery (FLS) score,9 Lichtenstein-Specific Operative Performance Rating Scale (OPRS),29 and a Telesurgery Evaluation Form.10
Using Kirkpatrick's Four Levels of Evaluation Model7 we found that out of the 25 studies, 60% used a Level 1 evaluation, 96% had a Level 2 evaluation, 28% had a Level 3 evaluation, and 44% had a Level 4 evaluation. The outcomes and level of evaluation of each study can be found in Table 1.
3.6. Outcomes reported
The overall surveyed consensus of telementoring experience among all 25 studies was generally positive, citing “positive experience,” “increased confidence,” and “increased surgical skill” as a few of the top reactions to their telementoring experience. Survey responses of “positive experience” were seen in 11 studies.8 , 10 , 11 , 13 , 14 , 16 , 20 , 24 , 27 , 30 , 31 Eight studies included the positive feedback of “increased surgical skill” through the use of telementoring.9 , 12, 13, 14 , 21, 22, 23 , 27 Self-reported increased confidence was found in 6 studies.12 , 13 , 18 , 27 , 29 , 31 In only two studies did some respondents mention that the use of telementoring technologies was unnecessary or not used very much.21 , 27
Two studies showed that there were no significant surgical skills differences.18 , 26 One study suggested a shorter coaching time,16 and another study showed a shorter length of postoperative admission.19
No unanimous consensus was found on the length of operation time between studies. A shorter operation time was found in 5 studies.10 , 14 , 19 , 27 , 32 No significant difference in operation time was seen in 3 additional studies.15 , 25 , 26 Only one study noted a longer operation time.21
Studies also looked at how beneficial the application of telementoring can be in real-time operations by measuring “successful” surgeries. These were defined as completed surgeries with no complications, or surgeries with no significant difference in complications between the telementoring group and the non-telementoring groups. Seven studies had surgeries with no complications8 , 10 , 15 , 17 , 28 , 29 , 32 and one study had no significant difference between the groups.25 Only one study had a single intraoperative complication which was handled accordingly.24
Table 1 provides a thorough report of the outcomes with brief descriptions of each of the 25 studies.
4. Discussion
This scoping review summarizes the available published literature on the current use of telementoring within the surgical field. Telementoring provides an alternative form of medical education to overcome geographical barriers in a cost-effective manner. Such practices are gaining more recognition, especially with the recent COVID-19 pandemic and its associated restrictions to in-person training. By identifying and highlighting the use of telementoring in both clinical and non-clinical settings, many recommendations can be considered and implemented to enhance education in the surgical field. This review highlights telementoring in terms of mentoring relationships, future technological advances, and its current challenges.
4.1. Mentoring relationships
The review reveals that surgical mentorship in medical education extends beyond a surgeon to student relationship. The most common type of relationship identified was surgeon to surgeon in 12 studies, followed by surgeon to resident in 5 studies. Surgeon to surgeon mentoring was commonly used for procedures done across the globe such as from the USA to Australia.17 By connecting a more experienced physician for a specific procedure to another less experienced physician, niche procedures may be more feasible for greater populations. The implementation of distant preceptorship can help provide care to patients in those areas lacking a nearby surgical specialist. This reduces the cost not only to the patient who no longer needs to travel to receive specialized surgical care but also to the experienced physician who would have sacrificed travel time otherwise spent. Additionally, telementoring has the potential to address resource-poor areas and their burden of surgical disease. One study explored the applicability of telementoring trans-continentally to deliver safe surgical care to underserved populations.29 The study found applicability in expanding the ability to train and mentor physicians in resource-poor locations using wearable technology, and this has promising insight for the expansion of global surgical education.
Telementoring was also utilized to connect surgeons to medical students. While these studies primarily measured surgical skill performance pre- and post-mentoring, this relationship opens the door to a much wider variety of use for students. Those interested in pursuing a career in the surgical field may be able to increase hands-on learning opportunities e.g. augmented reality. Students who practiced laparoscopic skills using augmented reality were found to have increased surgical skills with a positive mentoring experience.33 Performing these tasks under the supervision of a physician can serve as a gradual introduction into the surgical field, mitigating predisposed fears and fostering a stronger desire to pursue this career path.34 Additionally, students who gained earlier clinical surgical exposure through these technologies reported increased confidence,12 which may help prepare students to excel during their surgical clerkships.
This review found that the majority of studies measured surgical skill improvement or learner attitude; however, one study considered the application of telementoring in a non-clinical setting to foster academic and personal growth in developing surgeons.11 Such mentoring relationships that may be limited due to the number of available mentors or communication challenges were overcome through the EAST Mentoring Program.11 The establishment of a certified program via telementoring may be beneficial for the development of young surgeons to find mentorship opportunities outside of the operating room. Programs such as these that offer career development advice in both academia and personal growth may be a reliable supplement to the in-person mentoring of surgical skills and knowledge.
4.2. Future technological advances
The advancement of audio and visual communication systems has led to a more promising approach to telementoring in real-time. While video calling software was the most common form of technology utilized, other forms were adjunctively used such as robotic cameras or augmented reality systems. Rather than learning through passive observation, learning can instead be enhanced with the localization of more finite details. For example, certain tools can highlight anatomy for the surgeon to identify quickly rather than having to describe its location verbally.26 Such telestration tools enable the mentor to emphasize and make note of specific anatomical points for the surgeon's operative field. One form of technology allowed the mentoring expert surgeon to “virtually touch the tissue” by capturing the image of the mentor's hands over a video input from an endoscopic tower, which then processed a hybrid image to be sent back to the performing surgeon's field of view.35 This form of technology had positive feedback from participants as it allowed for better communication between participants, easier identification of anatomy, and greater potential for recipients to improve surgical skills while receiving supervision.35
Since many telementoring platforms utilize both audio and video streaming services, these surgeries can reach a greater number of people for educational purposes. Datta et al. note that of their 10 streamed surgeries, they had “7939 unique stream views and 26 comments logged by teleproctors among the streamed operations.“36 The use of real-time video streaming services can be a beneficial educational tool utilized by medical students or even practicing surgeons. Videos can also be broadcasted transcontinentally to target a greater audience and to increase learning opportunities worldwide.
The implementation of technological advancements in regard to finances is of great concern, especially in resource-restricted nations. While many studies have seen positive experiences using augmented reality trainers or da Vinci robots, these surgical platforms are not always financially feasible. However, certain studies such as one conducted by Okrainec et al. found several alternative solutions to adjunct telementoring across the nation. Their setup, utilizing two computers to connect to a Fundamentals of Laparoscopic Surgery trainer box with gooseneck camera and external webcam, as well as access to the internet and use of a free video calling software (Skype), found a solution to providing low-cost equipment and software for developing countries.37 The limiting factor of weak internet connectivity saw frequently dropped connections due to bandwidth issues, but lasted a few minutes and did not prevent training from continuing. This mentoring platform allows expert surgeons to provide live feedback and insight to other mentees while overcoming both financially and geographically isolated areas of the world.
4.3. Challenges to telementoring
A common challenge to the implementation of telementoring includes addressing geographically restricted areas with limited access to the internet. As mentioned earlier, many institutions are limited by their financial constraints and may lack a stable internet connection with wireless capabilities. Although there are financially forgiving platforms for audio and video feedback, these solutions require a reliable internet connection to broadcast a live-feed. Okrainec et al. mention a solution to providing internet access to resource-less communities via satellite, but even such would require additional funding.37 Not only is having a stable internet connection vital to broadcast audio and video demonstrations but there is also a reliance on the modality of communication systems that has the potential risk of failure.19 , 38 Such failures have clinical implications such as operative errors and the need for conversion, and institutions may not have backup assistance available on-site.
The ethical and legal considerations are other limitations that must be factored in. Because surgical mentoring can be done intercontinentally, each case needs to be reviewed carefully due to differing medical qualifications among various countries. There needs to be a comprehensive discussion about the technical form of telementoring as well as informed consent including approval of the mentor's contribution.39 Additionally, the patient-physician relationship may be compromised through the use of telementoring. Antoniou et al. state that the traditional relationship between the physician and patient is disturbed with the addition of a remote mentor, and the latter relationship is somewhat undefined.38 One study suggests that there should be a triangulation of information between the patient, mentor, and surgeons so that the patient can provide consent to the encompassing team's contribution to the operation.39 Another alternative solution suggested by Ponsky et al. is that the mentor solely “acts as an informal consultant” and there is no emphasis on the mentor physician-patient relationship.15 They note the essentiality of the performing surgeon's ability to complete the case without the mentor's help, and that the surgeon is only receiving advice on surgical technique or knowledge.
The financial model of telementoring can also be challenging, as expert physicians and their employers are unlikely to be compensated equally for the telementoring experience as they would for their usual surgical operations. There is also an initial cost to set up telementoring at a specific program, which can vary widely in price. Antoniou et al. estimate that the cost of a telementoring system, its software, and complete installation ranges from 50,000 to 85,000 USD, with the addition of annual maintenance fees of approximately 15,000 USD.38 Although there are lower-cost options available, one study found several shortcomings compared to a more expensive telementoring technology. Ponsky et al. indicate that the low-cost solution via store-bought equipment and a Skype connection lacked “interactivity, telestrator capacity, and HIPAA-compliant video encryption.“40 A more expensive telementoring robot was then utilized with telestration capabilities and laser pointing which had much better visualization. However, the more expensive software may also come with certain limitations. Andersen et al. state that the trainee subsystem is not truly a transparent display, which has negative effects on the ability of the mentee to have true visualization of the surgical field and can negatively affect depth perception.21 In a later study, Andersen et al. stated that they required more bandwidth and more robust video streaming solutions.22 While there may be a variety of telementoring technologies that range from free video streaming capabilities to more advanced robotic simulators, institutions should consider the cost-benefit analysis that aligns with their clinical and educational goals.
4.4. Strengths of study
A thorough literature search was conducted by a librarian utilizing various sources of data (PubMed, Embase, Web of Science, Scopus, and Cochrane library) to retrieve published literature for this scoping review. Our search strategy followed the PRISMA Systematic Review guidelines to ensure that this review process is transparent and reproducible. Because retrieved articles were screened by two reviewers independently, this allowed any data extraction disagreements to be resolved through thorough discussion and helped prevent selection bias which could alter the conclusions of the study.
Another strength of this review was the application of Kirkpatrick Level of Evaluation Model. This model added value to all of the telementoring relationships and associated impact on the mentees' skills, attitudes, behaviors, and direct surgical outcomes.7 These outcomes provide substantial evidence demonstrating how beneficial telementoring can be to a training program and its resulting impact on its mentees. Additionally, this review analyzed the various types of mentoring relationships, emphasizing the broad range of mentor-mentee opportunities regardless of one's current level in medical education. These findings suggest strong implications for different institutions in improving undergraduate medical education or enhancing surgical skills for practicing surgeons or surgical trainees.
4.5. Limitations
This review is subjected to several limitations. For one, only studies published in English concerning telementoring in the surgical field were included for the review. Exclusions of articles in other languages and in other specialties may restrict the level and quantity of evidence presented. Additionally, the inclusion of only surgical specialties limits the number of available studies on telementoring. Future analysis should include non-surgical specialties as this can provide different perspectives on the effectiveness of telementoring in medicine. This information could potentially reveal diverse types of mentoring relationships and associated outcomes of telementoring beyond improved surgical skills and positive experiences.
It was also noted that there may be potential bias inherent in 25 studies with small sample sizes of study participants and outcomes; therefore, these conditions may limit the generalizability of study results and may in turn affect the strength of synthesized evidence presented in the review.
Another limitation of the studies included for the review was the level of evaluation performed. For a majority of selected articles, outcome evaluation was limited to Level 1 and Level 2 on the Kirkpatrick Level of Evaluation model.7 Only seven of the 25 studies assessed outcomes at Level 3 (28%) and 11 studies measured outcomes at Level 4 (44%). The assessment of surgical performance (behavioral change) and patient-important outcomes (bottom-line results) in these studies look promising; however, further research would be warranted to investigate long-term impacts of telementoring on surgical skills and patient outcomes with longitudinal studies with a large sample size of participants from multiple institutional sites follow-up assessments.
5. Conclusions
This is a scoping review conducted from a very comprehensive literature search on the topic to date, and our research findings shed further light on telementoring used in surgical medical education. It is our hope that more program educators can explore telementoring as a valuable, scalable tool for mentorship. Telementoring was highlighted in the chosen studies as a growing and effective modality to enhance medical education in the surgical field from within both the simulation setting and the operating room. The results suggest that many forms of technology can be used to overcome the geographical and financial barriers to mentoring across the spectrum of medical education, especially due to the restrictions in place during the COVID-19 pandemic. While this scoping review indicates the feasibility of telementoring programs for learners ranging from attending surgeons to medical students, future studies are needed with larger sample sizes, longitudinal evaluation of patient-oriented outcomes, and rigorous study designs to increase the generalizability of study results. Telementoring used in surgical training for enhanced clinical and educational outcomes appears to be applicable and promising in this field.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Appendix.
PubMed Search Strategy
(Telementoring OR tele-mentoring OR ementor OR e-mentor OR ((tele OR remote* OR
distance OR web OR video* OR online OR on-line OR virtual) AND mentor*)) AND.
(education, medical [mh] OR schools, medical [mh] OR faculty, medical [mh] OR
“medical education” OR “medical training” OR “medical instruction” OR “medical
teaching” OR “internship and residency” OR “medical school” OR “medical schools” OR
“medical student” OR “medical students” OR “residency and internship” OR “medical
resident” OR “medical residents” OR “medical faculty” OR “clinical faculty”)
AND (“Specialties, Surgical"[Mesh] OR surgery OR surgical OR orthopedic OR orthoped* OR neurosurgery OR neurosurg* OR gynecology OR gynecolog* OR
obstetric* OR ophthalmology OR ophthalmolog* OR otolaryngology OR otolaryngolog*
OR neurotology OR neurotolog* OR traumatology OR traumatolog* OR urology OR urolog*)
References
- 1.Schlachta C.M., Nguyen N.T., Ponsky T., Dunkin B. Project 6 Summit: SAGES telementoring initiative. Surg Endosc. 2016;30(9):3665–3672. doi: 10.1007/s00464-016-4988-5. [DOI] [PubMed] [Google Scholar]
- 2.Warren O.J., Carnall R. Medical leadership: why it's important, what is required, and how we develop it. Postgrad Med. 2011;87(1023):27–32. doi: 10.1136/pgmj.2009.093807. [DOI] [PubMed] [Google Scholar]
- 3.Burgess A., van Diggele C., Mellis C. Mentorship in the health professions: a review. Clin Teach. 2018;15(3):197–202. doi: 10.1111/tct.12756. [DOI] [PubMed] [Google Scholar]
- 4.Augestad K.M., Bellika J.G., Budrionis A., et al. Surgical telementoring in knowledge translation—clinical outcomes and educational benefits: a comprehensive review. Surg Innovat. 2013;20(3):273–281. doi: 10.1177/1553350612465793. [DOI] [PubMed] [Google Scholar]
- 5.Raison N., Khan M.S., Challacombe B. Telemedicine in surgery: what are the opportunities and hurdles to realising the potential? Curr Urol Rep. 2015;16(7):43. doi: 10.1007/s11934-015-0522-x. [DOI] [PubMed] [Google Scholar]
- 6.Antoniou S.A., Antoniou G.A., Franzen J., et al. A comprehensive review of telementoring applications in laparoscopic general surgery. Surg Endosc. 2012;26(8):2111–2116. doi: 10.1007/s00464-012-2175-x. [DOI] [PubMed] [Google Scholar]
- 7.Kirkpatrick Donald. American Society for Training & Development; 2007. The Four Levels of Evaluation. [Google Scholar]
- 8.Bruns N.E., Irtan S., Rothenberg S.S., Bogen E.M., Kotobi H., Ponsky T.A. Trans-atlantic telementoring with pediatric surgeons: technical considerations and lessons learned. J Laparoendosc Adv Surg Tech. 2016;26(1):75–78. doi: 10.1089/lap.2015.0131. [DOI] [PubMed] [Google Scholar]
- 9.Okrainec A., Henao O., Azzie G. Telesimulation: an effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surg Endosc. 2010;24(2):417–422. doi: 10.1007/s00464-009-0572-6. [DOI] [PubMed] [Google Scholar]
- 10.Snyderman C.H., Gardner P.A., Lanisnik B., Ravnik J. Surgical telementoring: a new model for surgical training: surgical Telementoring. Laryngoscope. 2016;126(6):1334–1338. doi: 10.1002/lary.25753. [DOI] [PubMed] [Google Scholar]
- 11.Zakrison T.L., Polk T.M., Dixon R., et al. Paying it forward: four-year analysis of the eastern association for the surgery of trauma mentoring program. J Trauma Acute Care Surg. 2017;83(1):165–169. doi: 10.1097/TA.0000000000001493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glick Y., Avital B., Oppenheimer J., et al. Augmenting prehospital care. BMJ Mil Health. 2021;167(3):158–162. doi: 10.1136/jramc-2019-001320. [DOI] [PubMed] [Google Scholar]
- 13.Burckett-StLaurent D.A., Cunningham M.S., Abbas S., Chan V.W., Okrainec A., Niazi A.U. Teaching ultrasound-guided regional anesthesia remotely: a feasibility study. Acta Anaesthesiol Scand. 2016;60(7):995–1002. doi: 10.1111/aas.12695. [DOI] [PubMed] [Google Scholar]
- 14.Vera A.M., Russo M., Mohsin A., Tsuda S. Augmented reality telementoring (ART) platform: a randomized controlled trial to assess the efficacy of a new surgical education technology. Surg Endosc. 2014;28(12):3467–3472. doi: 10.1007/s00464-014-3625-4. [DOI] [PubMed] [Google Scholar]
- 15.Ponsky T.A., Bobanga I.D., Schwachter M., et al. Transcontinental telementoring with pediatric surgeons: proof of concept and technical considerations. J Laparoendosc Adv Surg Tech. 2014;24(12):892–896. doi: 10.1089/lap.2014.0363. [DOI] [PubMed] [Google Scholar]
- 16.Mizota T., Kurashima Y., Poudel S., Watanabe Y., Shichinohe T., Hirano S. Step-by-step training in basic laparoscopic skills using two-way web conferencing software for remote coaching: a multicenter randomized controlled study. Am J Surg. 2018;216(1):88–92. doi: 10.1016/j.amjsurg.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Miller J.A., Kwon D.S., Dkeidek A., et al. Safe introduction of a new surgical technique: remote telementoring for posterior retroperitoneoscopic adrenalectomy: remote telementoring of PRA. ANZ J Surg. 2012;82(11):813–816. doi: 10.1111/j.1445-2197.2012.06188.x. [DOI] [PubMed] [Google Scholar]
- 18.Kirkpatrick A.W., Tien H., LaPorta A.T., et al. The marriage of surgical simulation and telementoring for damage-control surgical training of operational first responders: a pilot study. J Trauma Acute Care Surg. 2015;79(5):741–747. doi: 10.1097/TA.0000000000000829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fuertes-Guiró F., Vitali-Erion E., Rodriguez-Franco A. A program of telementoring in laparoscopic bariatric surgery. Minim Invasive Ther Allied Technol. 2016;25(1):8–14. doi: 10.3109/13645706.2015.1083446. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen N.T., Okrainec A., Anvari M., et al. Sleeve gastrectomy telementoring: a SAGES multi-institutional quality improvement initiative. Surg Endosc. 2018;32(2):682–687. doi: 10.1007/s00464-017-5721-8. [DOI] [PubMed] [Google Scholar]
- 21.Andersen D., Popescu V., Cabrera M.E., et al. Medical telementoring using an augmented reality transparent display. Surgery. 2016;159(6):1646–1653. doi: 10.1016/j.surg.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 22.Andersen D., Popescu V., Cabrera M.E., et al. An augmented reality-based approach for surgical telementoring in austere environments. Mil Med. 2017;182(S1):310–315. doi: 10.7205/MILMED-D-16-00051. [DOI] [PubMed] [Google Scholar]
- 23.Chou D.T.S., Solomon L.B., Costi K., Pannach S., Holubowycz O.T., Howie D.W. Structured-mentorship program for periacetabular osteotomy resulted in few complications for a low-volume pelvic surgeon. Clin Orthop. 2019;477(5):1126–1134. doi: 10.1097/CORR.0000000000000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin D.H., Dalag L., Azhar R.A., et al. A novel interface for the telementoring of robotic surgery. BJU Int. 2015;116(2):302–308. doi: 10.1111/bju.12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinata N., Miyake H., Kurahashi T., et al. Novel telementoring system for robot-assisted radical prostatectomy: impact on the learning curve. Urology. 2014;83(5):1088–1092. doi: 10.1016/j.urology.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Ponce B.A., Jennings J.K., Clay T.B., May M.B., Huisingh C., Sheppard E.D. Telementoring: use of augmented reality in orthopaedic education: AAOS exhibit selection. J Bone Jt Surg. 2014;96(10):e84. doi: 10.2106/JBJS.M.00928. [DOI] [PubMed] [Google Scholar]
- 27.Ereso A.Q., Garcia P., Tseng E., et al. Live transference of surgical subspecialty skills using telerobotic proctoring to remote general surgeons. J Am Coll Surg. 2010;211(3):400–411. doi: 10.1016/j.jamcollsurg.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Forgione A., Kislov V., Guraya S.Y., Kasakevich E., Pugliese R. Safe introduction of laparoscopic colorectal surgery even in remote areas of the world: the value of a comprehensive telementoring training program. J Laparoendosc Adv Surg Tech. 2015;25(1):37–42. doi: 10.1089/lap.2014.0191. [DOI] [PubMed] [Google Scholar]
- 29.Datta N., MacQueen I.T., Schroeder A.D., et al. Wearable technology for global surgical teleproctoring. J Surg Educ. 2015;72(6):1290–1295. doi: 10.1016/j.jsurg.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 30.Budrionis A., Hasvold P., Hartvigsen G., Bellika J.G. Assessing the impact of telestration on surgical telementoring: a randomized controlled trial. J Telemed Telecare. 2016;22(1):12–17. doi: 10.1177/1357633X15585071. [DOI] [PubMed] [Google Scholar]
- 31.Dawe P., Kirkpatrick A., Talbot M., et al. Tele-mentored damage-control and emergency trauma surgery: a feasibility study using live-tissue models. Am J Surg. 2018;215(5):927–929. doi: 10.1016/j.amjsurg.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 32.Treter S., Perrier N., Sosa J.A., Telementoring Roman S. A multi-institutional experience with the introduction of a novel surgical approach for adrenalectomy. Ann Surg Oncol. 2013;20(8):2754–2758. doi: 10.1245/s10434-013-2894-9. [DOI] [PubMed] [Google Scholar]
- 33.Vera A.M., Russo M., Mohsin A., Tsuda S. Surg Endosc; 2014. Augmented Reality Telementoring (ART) Platform: A Randomized Controlled Trial to Assess the Efficacy of a New Surgical Education Technology; p. 6. Published online. [DOI] [PubMed] [Google Scholar]
- 34.McKinley S.K., Sell N.M., Saillant N., et al. Enhancing the formal preclinical curriculum to improve medical student perception of surgery. J Surg Educ. 2020;77(4):788–798. doi: 10.1016/j.jsurg.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 35.Ponce B.A., Jennings J.K., Clay T.B., May M.B., Huisingh C., Sheppard E.D. Telementoring: use of augmented reality in. Orthopaedic Education. 2014;96(10):6. doi: 10.2106/JBJS.M.00928. [DOI] [PubMed] [Google Scholar]
- 36.Datta N. Wearable technology for global surgical teleproctoring. J Surg Educ. 2015;72(6):6. doi: 10.1016/j.jsurg.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 37.Okrainec A., Henao O., Azzie G. Telesimulation: an effective method for teaching the fundamentals of laparoscopic surgery in resource-restricted countries. Surg Endosc. 2010;24(2):417–422. doi: 10.1007/s00464-009-0572-6. [DOI] [PubMed] [Google Scholar]
- 38.Antoniou S.A., Antoniou G.A., Franzen J., et al. A comprehensive review of telementoring applications in laparoscopic general surgery. Surg Endosc. Published online. 2012:6. doi: 10.1007/s00464-012-2175-x. [DOI] [PubMed] [Google Scholar]
- 39.Fuertes-Guiro F, Vitali-Erion E, Rodriguez-Franco A. A program of telementoring in laparoscopic bariatric surgery. Minim INVASIVE Ther.:8. [DOI] [PubMed]
- 40.Ponsky TA, Bobanga ID, Schwachter M, et al. Transcontinental Telementoring with Pediatric Surgeons: Proof of Concept and Technical Considerations. :6. [DOI] [PubMed]