Abstract
Purpose
Both mobile (MB) and fixed (FB) bearing implants are routinely used for total knee arthroplasty (TKA). This meta-analysis compared MB versus FB for TKA in terms of implant positioning, joint function, patient reported outcome measures (PROMs), and complications. It was hypothesised that MB performs better than FB implants in primary TKA.
Methods
This meta-analysis was conducted according to the 2020 PRISMA statement. In February 2022, the following databases were accessed: Pubmed, Web of Science, Google Scholar, Embase. All the randomized clinical trials (RCTs) comparing mobile versus fixed bearing for primary TKA were considered.
Results
Data from 74 RCTs (11,116 procedures) were retrieved. The mean follow-up was 58.8 (7.5 to 315.6) months. The MB group demonstrated greater range of motion (ROM) (P = 0.02), Knee Society Score (KSS) score (P < 0.0001), and rate of deep infections (P = 0.02). No difference was found in implant positioning: tibial slope, delta angle, alpha femoral component angle, gamma femoral component angle, beta tibial component angle, tibiofemoral alignment angle, posterior condylar offset, radiolucent lines. No difference was found in duration of the surgical procedure. No difference was found in the following PROMs: Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analogue scale (VAS), function and pain subscales of the KSS score. No difference was found in the rate of anterior knee pain, revision, aseptic loosening, fractures, and deep vein thrombosis.
Conclusion
There is no evidence in support that MB implants promote greater outcomes compared to FB implants in primary TKA.
Level of evidence
Level I.
Keywords: Total knee arthroplasty, Mobile bearing, Fixed bearing
Introduction
Knee osteoarthritis (OA) is common [6, 94]. Knee OA impairs joint function and quality of life, limiting physical activities and patient independency [71, 73, 115]. Total knee arthroplasty (TKA) is advocated for end-stage knee OA [46, 74, 85]. Both mobile (MB) and fixed (FB) bearing implants are available for primary TKA [1, 49]. FB implants were introduced first, and still represent the most common type of TKA [21, 84]. The polyethylene inlay of FB implants is secured on the tibial plateau. On the other hand, MB implants allow rotation of the polyethylene inlay around its longitudinal axis, miming the physiological kinematics of the knee and promoting a wider range of motion [22, 34, 93]. Previous evidence suggested that MB may promote greater outcomes in functional scores and complications [40, 44, 45, 75, 95]. However, the difference was minimal, and whether mobile bearing provide better outcomes remains controversial [5, 16, 38, 46, 63, 82, 96, 100, 103, 111]. Several randomized clinical trials (RCTs), which have not been yet considered in any previous meta-analyses, have recently been recently published [8, 24, 28, 59, 93, 105, 107, 123]. An update of current evidence could clarify whether MB implants promote greater outcomes to FB in TKA in terms of outcome and complication rate. This meta-analysis compared MB versus FB for primary TKA in terms of implant positioning, patient reported outcome measures (PROMs), and complications. It was hypothesised that MB promotes better outcomes than FB implants in primary TKA.
Materials and methods
Eligibility criteria
All the clinical investigations comparing mobile versus fixed bearing for primary TKA were considered. Only randomized clinical trials (RCTs) with level I to II of evidence, according to Oxford Centre of Evidence-Based Medicine [47], were considered. Only articles in English, German, Italian, French, and Spanish were eligible. Only studies published in peer reviewed journals with accessible full-text article were considered. Only studies which clearly stated the number of included procedures with a minimum of 8 months follow-up were considered. Reviews, opinions, letters, and editorials were not considered. Animals, in vitro, biomechanics, computational, and cadaveric studies were not eligible. All studies investigating the efficacy of experimental rehabilitation protocols were also not included. Studies reporting revision surgeries were also excluded from the analysis.
Search strategy
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [89]. The PICODT algorithm was preliminary pointed out:
P (Population): end-stage knee osteoarthritis;
I (Intervention): TKA;
C (Comparison): Mb versus Fb;
O (Outcomes): implant alignment, surgical duration, range of motion, PROMs, complications;
D (Design); RCT;
T (Follow-up): minimum 8 months.
In February 2022, the following databases were accessed: Pubmed, Web of Science, Google Scholar, Embase. The search was limited to RCTs, with no time constrains. The following keywords were used in combination using the Boolean operator AND/OR: knee, osteoarthritis, total, arthroplasty, replacement, prosthesis, implant, mobile bearing, fixed bearing, patient reported outcome measures, PROMs, function, efficacy, complication, revision, reoperation, pain, outcome.
Selection and data collection
Two authors (F.C. and K.E.) independently performed the database search. All the resulting titles were screened and if suitable, the abstract was accessed. The full-text of the abstracts which matched the topic was accessed. A cross reference of the bibliography of the full-text articles were also screened for inclusion. All disagreements between the authors were debated and, if necessary, solved by a third author (NM).
Data items
Two authors (F.C. and K.E.) independently performed data extraction.
The following data at baseline were extracted:
Generalities of the study: name of the first author, year of publication and journal, length of the follow-up, number of patients, percentage of women (%), body mass index (BMI).
The following data at baseline and at last follow-up were extracted:
Range of motion (ROM);
-
PROMs: Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), visual analogue scale (VAS), Knee Society Score (KSS), and relate function (KSFS and pain (KSPS) subscales.
The following data at last follow-up were collected:
Implant alignment: tibial slope, delta angle, alpha femoral component angle, gamma femoral component angle, beta tibial component angle, tibiofemoral alignment angle, posterior condylar offset, radiolucent lines;
Surgical duration;
Complications: anterior knee pain (AKP), revision, aseptic loosening, fractures, deep vein thrombosis (DVT).
Study risk of bias assessment
The risk of bias was valuated using the software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen). The risk of bias was evaluated, based on the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions [27], by the two reviewers (F.C. and K.E.). The following endpoints were evaluated: selection, detection, performance, attrition, reporting, and other bias. To assess the overall risk of publication bias, the funnel plot of the most commonly reported outcome was performed. The funnel plot charted the standard error (SE) of the Log Odd Ratio (LogOR) versus its OR. The degree of asymmetry of the plot is directly proportional to the degree of bias. To assess the risk of bias of each included studies, the risk of bias graph was performed.
Statistical analysis and synthesis methods
The statistical analyses were performed by the main author (F.M.). For descriptive statistics, the IBM SPSS software (version 25) was used. The mean difference and standard deviation were adopted. The T test was performed to assess baseline comparability, with values of P > 0.1 considered satisfactory. For the meta-analyses, the software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen) was used. For continuous data, the inverse variance method with mean difference (MD) effect measure was used. For binary data, the Mantel–Haenszel method with odd ratio (OR) effect measure was used. The confidence interval (CI) was set at 0.95 in all the comparison. Heterogeneity was assessed using 2 and Higgins-I2 tests. If 2 > 0.05, no statistically significant heterogeneity was found. If 2 < 0.05 and Higgins-I2 > 60% high heterogeneity was found. A fixed model effect was used as default. In case of high heterogeneity, a random model was used. Overall values of P < 0.05 were considered statistically significant.
Results
Study selection
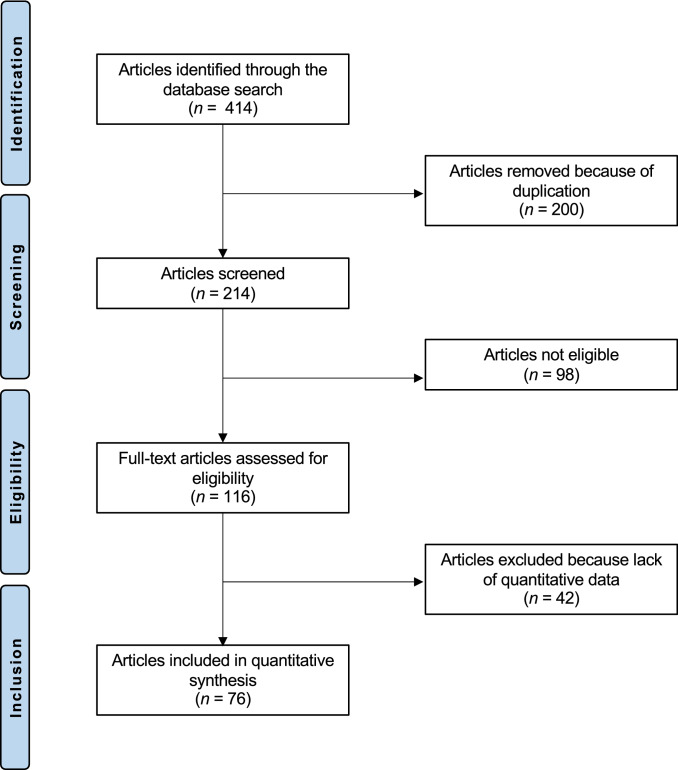
The literature search resulted in 414 articles. After removal of duplicates (N = 200), a further 140 articles were not eligible for the following reasons: study design (N = 78), language limitation (N = 17), short follow-up (N = 19), lacking quantitative data under the endpoints of interest (N = 26). Finally, 74 comparative studies were included. The results of the literature search are shown in Fig. 1.
Fig. 1.
Flow chart of the literature search
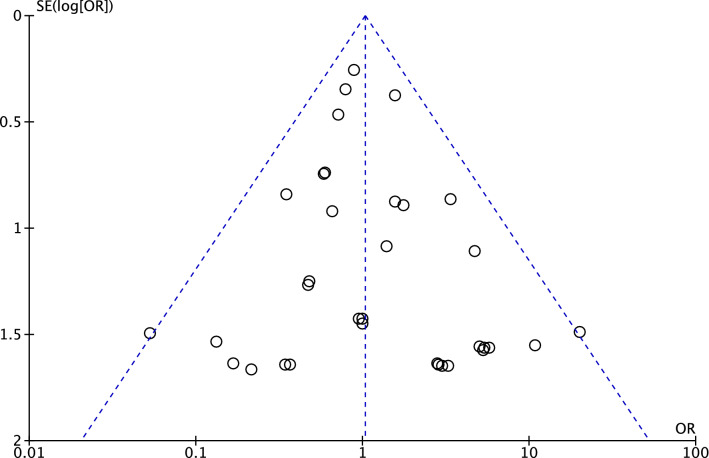
Risk of publication bias
The funnel plot of the most commonly reported outcome (revision) was performed to assess the risk of publication bias. The plot evidenced very good symmetry, with optimal distribution of the estimated effects of the included studies. The Egger’s test score was P = 0.6, attesting a low risk of publication bias (Fig. 2).
Fig. 2.
Funnel plot
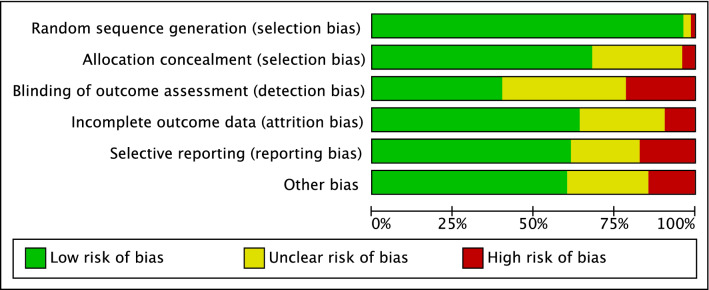
Study risk of bias assessment
Given the randomized design of the included studies, the risk of selection bias was low. The risk of detection bias was low to moderate, as was the risk of attrition and reporting biases. The risk of other bias was also low to moderate. Concluding, the quality of the methodological assessment was good. The Cochrane risk of bias graph is shown in Fig. 3.
Fig. 3.
Methodological quality assessment
Study characteristics and results of individual studies
Data from 11,116 procedures were retrieved. 69% (7670 of 11,116 patients) were women. The mean follow-up was 58.8 (7.5 to 315.6) months. The mean age was 67.5 ± 5.9 years, the mean BMI was 28.6 ± 2.3 kg/m2. Comparability was found at baseline concerning the mean age, mean BMI, female, ROM, KSS, OKS, KSS pain, WOMAC, VAS, and KSS function. Generalities and patient baseline of the included studies are shown in greater detail in Table 1, the baseline comparability between the two groups at baseline in Table 2.
Table 1.
Generalities and patient baseline of the included studies
| Author, year | Journal | Follow-up (months) | Bearing | Procedures (n) | Mean age | Mean BMI | Women (%) |
|---|---|---|---|---|---|---|---|
| Abdel et al., 2018 [2] | Bone Joint J | 120.1 | APE FB | 50 | 67 | ||
| Metal backed FB | 66 | 67 | |||||
| MB | 53 | 67 | |||||
| Aggarwal et al., 2013 [4] | J Arthroplasty | 66 | MB | 29 | 60 | 27.4 | 83 |
| FB | 27 | 54.6 | 25.3 | 85 | |||
| Aglietti et al., 2005 [5] | J Arthroplasty | 36 | MB | 103 | 71 | 27.5 | 86 |
| FB | 107 | 69.5 | 27.5 | 81 | |||
| Amaro et al., 2016 [7] | Knee Surg Sports Tramatol Arthrosoc | 24 | FB | 32 | 66.2 | 29.8 | 69 |
| MB | 32 | 65.2 | 31.1 | 75 | |||
| Amaro et al., 2019 [8] | J Knee Surg | 24 | FB | 32 | 66.2 | 29.8 | 69 |
| MB | 32 | 65.2 | 31.1 | 75 | |||
| Artz et al., 2015 [9] | J Arthroplasty | 24 | FB | 102 | 61.6 | 47 | |
| MB | 104 | 61.7 | 55 | ||||
| Bailey et al., 2014 [10] | Knee Surg Sports Tramatol Arthrosoc | 24 | MB | 161 | 69.2 | 30.4 | 69 |
| FB | 170 | 70.1 | 31.6 | 70 | |||
| Baktir et al., 2016 [11] | Acta Orthop Traumatol Turc | 72 | MB | 47 | 64.9 | 33.3 | 87 |
| FB | 46 | 64.7 | 32.2 | 89 | |||
| Ball et al., 2011 [12] | J Arthroplasty | 48 | MB | 51 | 64.9 | 31.0 | 56 |
| FB | 42 | 64.0 | 31.0 | 56 | |||
| Beard et al., 2007 [13] | Knee | 36 | MB | 33 | 73.1 | 60 | |
| FB | 33 | 73.1 | 60 | ||||
| Bhan et al., 2005 [14] | J Bone Joint Surg | 54 | FB | 32 | 63 | 69 | |
| MB | 32 | 63 | 69 | ||||
| Breeman et al., 2013 [17] | Bone Joint J | 60 | MB | 276 | 69 | 29.5 | 16 |
| FB | 263 | 69 | 30.3 | 59 | |||
| Breugrem et al., 2008 [18] | Clin Orthop Relat Res | 12 | FB | 53 | 68.9 | 29.1 | 64 |
| MB | 47 | 71.2 | 28.4 | 65 | |||
| Breugem et al., 2012 [19] | Knee Surg Sports Traumatol Arthrosc | 94.8 | FB | 40 | 80 | 65 | |
| MB | 29 | 78 | 65 | ||||
| Chaudhry et al., 2018 [23] | J Orthop Traumatol | 90 | FB | 60 | 57.6 | 25.1 | 72 |
| MB | 50 | 58.7 | 25.7 | 71 | |||
| Choi et al., 2010 [25] | J Bone Joint Surg | 24 | MB | 85 | 70.1 | 26.6 | 93 |
| FB | 85 | 71.1 | 26.5 | 97 | |||
| Feczko et al., 2017 [31] | BMC Musculoskelet Disord | 60 | FB | 48 | 30.1 | ||
| MB | 42 | 28.7 | |||||
| Ferguson et al., 2014 [32] | Knee | 24 | MB | 163 | 69.8 | 29.7 | 53 |
| FB | 163 | 70.2 | 31.1 | 53 | |||
| Fransen et al., 2015 [33] | J Arthroplasty | 72 | MB | 77 | 65.7 | 30.2 | 68 |
| FB | 69 | 63.8 | 30.2 | 72 | |||
| Garling et al., 2005 [35] | Acta Orthop | 24 | MB | 21 | 66 | 27.0 | 50 |
| FB | 21 | ||||||
| Gioe et al., 2009 [36] | J Bone Joint Surg | 24 | MB | 176 | 71.79 | 31.9 | 2 |
| FB | 136 | 72.62 | 31.5 | 4 | |||
| Hansson et al., 2005 [38] | Knee | 24 | MB | 25 | 74 | 48 | |
| FB | 27 | 75 | 52 | ||||
| Hanusch et al., 2010 [39] | Int Orthop | 24 | FB | 55 | 69.4 | 29.9 | 40 |
| MB | 50 | 70 | 29.7 | 60 | |||
| Harrington et al., 2009 [41] | J Arthroplasty | 24 | FB | 72 | 63.3 | 34.2 | 69 |
| MB | 68 | 63.7 | 34.2 | 59 | |||
| Hasegawa et al., 2008 [42] | Knee Surg Sports Traumatol Arthrosc | 40 | MB | 25 | 73 | 25.2 | 88 |
| FB | 25 | 73 | 25.2 | 88 | |||
| Henricson et al., 2006 [43] | Clin Orthop Relat Res | 24 | MB | 26 | 72 | ||
| FB | 26 | 72 | |||||
| Jacobs et al., 2011 [48] | Knee Surg Sports Traumatol Arthrosc | 12 | MB | 46 | 67.6 | 71 | |
| FB | 46 | 66.7 | 70 | ||||
| Jolles et al., 2012 [50] | J Bone Joint Surg | 60 | MB | 26 | 67.1 | 29.6 | 68 |
| FB | 29 | 70.2 | 27.9 | 48 | |||
| Kalisvaart et al., 2012 [51] | J Bone Joint Surg | 60 | FB (polyethylene) | 75 | 67 | 32.1 | 69 |
| FB (modular-metal-backed) | 76 | 67.1 | 30.5 | 70 | |||
| MB | 76 | 67.4 | 33.1 | 70 | |||
| Kim et al., 2007 [56] | J Bone Joint Surg | 67.2 | MB | 174 | 67 | 26.7 | 64 |
| FB | 174 | 67 | 26.7 | 64 | |||
| Kim et al., 2007 [64] | J Bone Joint Surg | 158.4 | FB | 146 | 69.8 | 27.5 | 94 |
| MB | 146 | 69.8 | 27.5 | 94 | |||
| Kim et al., 2008 [63] | Clin Orthop Relat Res | 24 | FB | 92 | 69.5 | 27.8 | 92 |
| MB | 92 | 69.5 | 27.8 | 92 | |||
| Kim et al., 2009 [57] | J Arthroplasty | 24 | FB | 61 | 48.3 | 26.8 | 74 |
| MB | 61 | 48.3 | 26.8 | 74 | |||
| Kim et al., 2009 [55] | Knee Surg Sports Traumatol Arthrosc | 24 | FB | 66 | 70 | 26.0 | 97 |
| MB | 66 | 70 | 26.0 | 97 | |||
| Kim et al., 2011 [54] | Knee Surg Sports Traumatol Arthrosc | 30 | MB | 37 | 68 | 27.3 | 95 |
| FB | 36 | 66 | 27.1 | 98 | |||
| Kim et al., 2017 [60] | J Arthroplasty | 134.4 | FB | 92 | 61.5 | 26.2 | 82 |
| MB | 92 | 61.5 | 26.2 | 82 | |||
| Kim et al., 2012 [58] | J Bone Joint Surg | 201.6 | MB | 108 | 45 | 25.6 | 77 |
| FB | 108 | 45 | 25.6 | 77 | |||
| Kim et al., 2014 [62] | J Bone Joint Surg | 144 | MB | 444 | 66.5 | 29.6 | 93 |
| FB | 444 | 66.5 | 29.6 | 93 | |||
| Kim et al., 2018 [61] | J Arthroplasty | 156 | MB | 164 | 63 | 28.0 | 87 |
| FB | 164 | 63 | 28.0 | 87 | |||
| Kim et al., 2020 [59] | J Arthroplasty | 315.6 | MB | 291 | 58 | 27.0 | 77 |
| FB | 291 | 58 | 27.0 | 77 | |||
| Killen et al., 2019 [53] | J Clin Orthop Trauma | 144 | FB | 19 | 76.79 | 76 | |
| MB | 28 | 76.57 | 60 | ||||
| Lädermann et al., 2007 [66] | Knee | 36 | FB | 52 | 79 | 29.9 | 77 |
| MB | 50 | 72 | 29.6 | 60 | |||
| Lädermann et al., 2008 [67] | Rev. Chir. Orthop. Reparatrice Appar. Mot | 85.2 | FB | 48 | 69.8 | 29.9 | 77 |
| MB | 44 | 72 | 29.6 | 60 | |||
| Lizaur-Utrilla et al., 2012 [70] | J Arthroplasty | 24 | MB | 61 | 74.6 | 31.3 | 77 |
| FB | 58 | 73.9 | 32.6 | 81 | |||
| Mahoney et al., 2012 [72] | Clin Orthop Relat Res | 24 | MB | 178 | 66 | 31.0 | 67 |
| FB | 183 | 66 | 31.0 | 61 | |||
| Marques et al., 2014 [75] | Knee Surg Sports Traumatol Arthrosc | 48 | FB | 45 | 68.9 | 28.7 | 75 |
| MB | 42 | 69.4 | 30.4 | 70 | |||
| Matsuda et al., 2010 [76] | Knee Surg Sports Traumatol Arthrosc | 70.8 | FB | 31 | 76 | 78 | |
| MB | 30 | 73 | 77 | ||||
| Minoda et al., 2014 [83] | Knee Surg Sports Traumatol Arthrosc | 24 | MB | 46 | 74.3 | 26.3 | 89 |
| FB | 48 | 75.7 | 25.5 | 87 | |||
| Niuewenhuijse et al., 2013 [83] | J Bone Joint Surg | 70 | LPS-Flex MB | 16 | 66.8 | 25.9 | 79 |
| LPS-Flex FB | 12 | 72.2 | 26.5 | 70 | |||
| LPS MB | 14 | 68.7 | 29.0 | 100 | |||
| LPS FB | 19 | 68.5 | 27.6 | 76 | |||
| Nutton et al., 2012 [87] | J Bone Joint Surg | 12 | FB | 40 | 69.8 | 29.8 | 53 |
| MB | 36 | 68.3 | 29.1 | 50 | |||
| Okamoto et al., 2014 [88] | J Arthroplasty | 12 | MB | 20 | 76 | 25.0 | 90 |
| FB | 20 | 78 | 27.0 | 80 | |||
| Park et al., 2018 [91] | Knee Surg Sports Traumatol Arthrosc | 24 | MB | 70 | 69.5 | 26.0 | 93 |
| FB | 70 | 68.9 | 25.6 | 96 | |||
| Pijls et al., 2012 [92] | J Bone Joint Surg | 120 | MB | 21 | 64 | 27.0 | 86 |
| FB | 21 | 66 | 27.0 | 76 | |||
| Poirier et al., 2015 [93] | Orthop Traumatol Surg Res | 108 | FB | 31 | 72 | 58 | |
| MB | 30 | 70 | 53 | ||||
| Powell et al., 2018 [95] | Bone Joint J | 60 | MB | 46 | 65.5 | 29.7 | 44 |
| FB | 39 | 65.5 | 29.7 | 44 | |||
| Price et al., 2003 [96] | J Bone Joint Surg | 12 | FB | 19 | 73.1 | 60 | |
| MB | 21 | 73.1 | 60 | ||||
| Radetzki et al., 2013 [97] | Acta Orthop | 120 | FB | 22 | 65.5 | 24.4 | 60 |
| MB | 17 | 66.5 | 24.1 | 53 | |||
| Rahman et al., 2010 [98] | J Arthroplasty | 43 | MB | 24 | 62.6 | 31.5 | 58 |
| FB | 27 | 62 | 31.4 | 67 | |||
| Roh et al., 2012 [102] | Knee Surg Sports Traumatol Arthrosc | 30 | MB | 42 | 69.8 | 26.5 | 95 |
| MB | 44 | 71 | 26.4 | 93 | |||
| Sappey-Marinier et al., 2019 [104] | Knee Surg Sports Traumatol Arthrosc | 60 | FB | 64 | 71 | 29.0 | 58 |
| MB | 65 | 71 | 30.0 | 60 | |||
| Sappey-Marinier et al., 2020 [105] | Knee Surg Sports Traumatol Arthrosc | 120 | FB | 50 | 71 | 29.0 | 58 |
| MB | 56 | 71 | 30.0 | 60 | |||
| Schotanus et al., 2016 [106] | Knee Surg Sports Traumatol Arthrosc | 24 | MB | 20 | 62.7 | 29 | 48 |
| FB | 22 | 67.3 | 29.4 | 41 | |||
| Schotanus et al., 2017 [107] | Eur J Orthop Surg Traumatol | 24 | MB | 20 | 61.9 | 29.4 | 40 |
| FB | 21 | 67.1 | 29.9 | 43 | |||
| Scuderi et al., 2012 [109] | J Arthroplasty | 48 | MB | 152 | 63.7 | 29.6 | 55 |
| FB | 141 | 63.4 | 29.4 | 62 | |||
| Shemanski et al., 2012 [110] | Knee Surg Sports Traumatol Arthrosc | 72 | FB | 150 | 70 | 68 | |
| MB | 150 | 68 | 60 | ||||
| Tiwari et al., 2019 [113] | Knee Surg Sports Traumatol Arthrosc | 24 | MB | 260 | 69.7 | 26.9 | 94 |
| FB | 133 | 69.7 | 26.7 | 98 | |||
| Tjornild et al., 2015 [114] | Acta Orthop | 24 | FB | 23 | 66 | 30.0 | 46 |
| MB | 23 | 66 | 27.0 | 65 | |||
| Urwin et al., 2014 [116] | Knee | 9 | FB | 8 | 59.3 | 31.9 | 38 |
| MB | 8 | 59.6 | 31.9 | 38 | |||
| Van hammersfeld et al., 2018 [117] | Acta Orthop | 72 | FB | 16 | 68 | 30.1 | 70 |
| MB | 12 | 67.5 | 29.8 | 83 | |||
| Vasdev et al., 2009 [118] | J Orthop Surg | FB | 60 | 63 | 67 | ||
| 42 | MB | 60 | 63 | 50 | |||
| Watanabe et al., 2005 [119] | Int Orthop | 96 | MB | 22 | 59.6 | 96 | |
| Wohlrab et al., 2005 [120] | Z Orthop | 35 | FB | 30 | 65,5 | 24.4 | 62 |
| MB | 30 | 66,5 | 24.1 | 53 | |||
| FB | 22 | 59.6 | 95 | ||||
| Woolson et al., 2011 [121] | J Arthroplasty | 120 | FB | 30 | 77.9 | 29.2 | |
| MB | 31 | 78 | 27.7 | ||||
| Wylde et al., 2008 [122] | J Bone Joint Surg | 24 | FB | 120 | 67.6 | 64 | |
| MB | 108 | 68.9 | 68 |
MB: mobile bearing; FB: fixed bearing
Table 2.
Baseline comparability of the two groups
| Endpoint | FB (n = 5517) | MB (n = 5599) | P values |
|---|---|---|---|
| Mean age | 67.5 ± 61 | 67.3 ± 5.6 | n. s |
| Mean BMI | 28.7 ± 2.3 | 28.6 ± 2.3 | n. s |
| Women (%) | 1.7 ± 8.9 | 1.5 ± 6.9 | n. s |
| ROM | 104.9 ± 24.5 | 105.0 ± 24.1 | n. s |
| KSS | 39.7 ± 17.0 | 40.5 ± 17.1 | n. s |
| OKS | 33.1 ± 10.9 | 33.3 ± 10.9 | n. s |
| KSS pain | 25.3 ± 26.5 | 21.1 ± 25.7 | n. s |
| WOMAC | 59.9 ± 8.5 | 59.2 ± 8.3 | n. s |
| VAS | 32.8 ± 36.0 | 32.5 ± 33.0 | n. s |
| KSS function | 43.3 ± 12.8 | 43.5 ± 12.7 | n. s |
No statistically significant difference was detected
MB: mobile bearing; FB: fixed bearing; MD: mean difference; ROM: range of motion; OKS: Oxford Knee Score; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index; VAS: visual analogue scale; KSS: Knee Society Score; n. s.: not significant
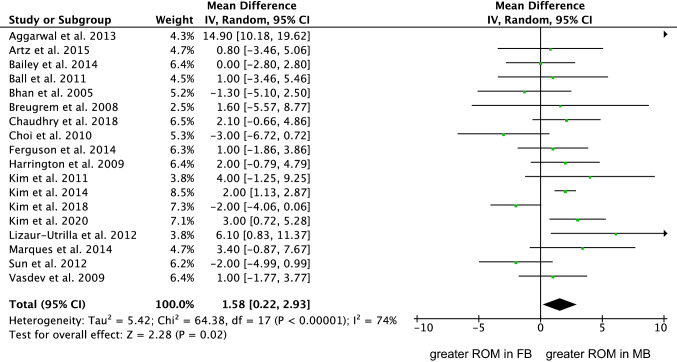
Results of syntheses
Eighteen studies (3827 procedures) were included in the comparison of ROM [4, 9, 10, 12, 14, 18, 23, 25, 41, 54, 59, 60, 62, 70, 75, 118]. The MB group demonstrated greater ROM (MD 1.58; 95% CI 0.22 to 2.93; P = 0.02; Fig. 4).
Fig. 4.
Forest plot of the comparison: ROM (IV: inverse variance; CI: confidence interval). The square represents the effect of each single study. The horizontal line represents the confidence interval of each study. The vertical line “0” represent the no effect threshold. The diamond represents the final effect of the overall analysis
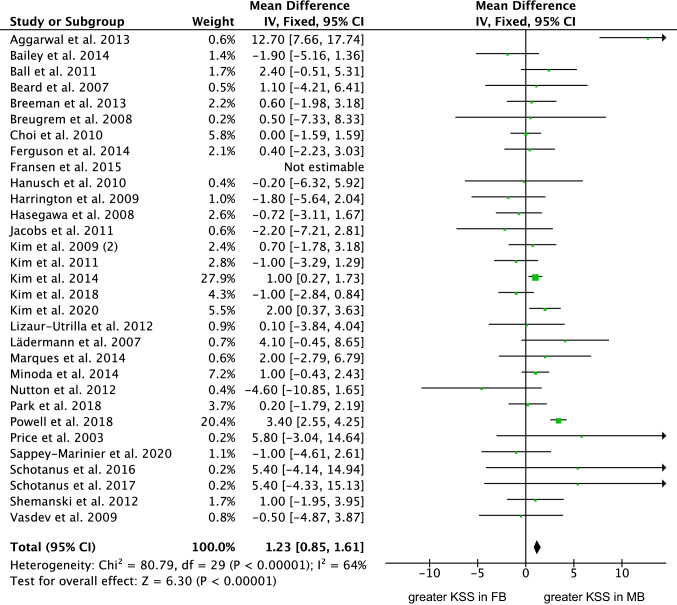
Thirty-one studies (5094 procedures) were included in the comparison of the KSS score [4, 10, 12, 13, 17, 18, 25, 32, 33, 39, 41, 42, 48, 54, 57, 59, 60, 62, 66, 70, 75, 83, 87, 91, 95, 96, 104, 106, 107, 110, 118]. The MB evidenced greater KSS score (MD 1.23; 95% CI 0.85 to 1.61; P < 0.0001; Fig. 5).
Fig. 5.
Forest plot of the comparison: KSS score (IV: inverse variance; CI: confidence interval). The square represents the effect of each single study. The horizontal line represents the confidence interval of each study. The vertical line “0” represent the no effect threshold. The diamond represents the final effect of the overall analysis
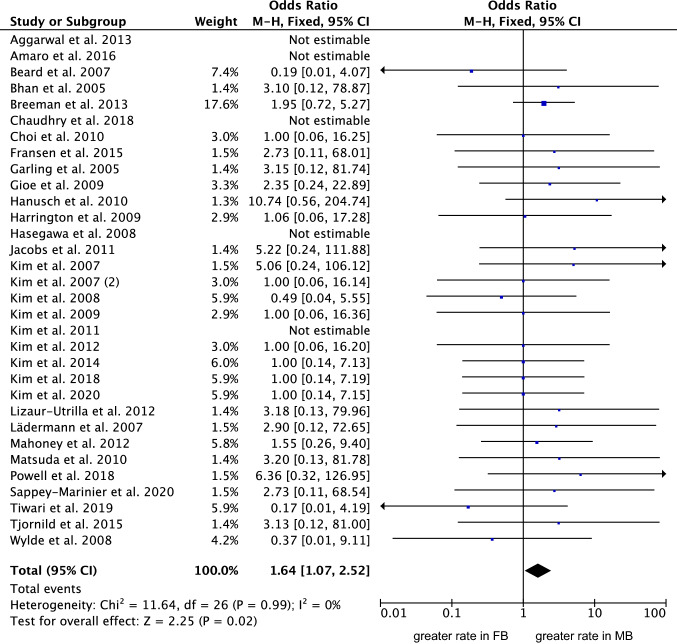
Thirty-two studies (6489 procedures) were included in the comparison of rate of deep infection [4, 7, 13, 14, 17, 23, 25, 33, 35, 36, 39, 41, 42, 55–57, 60–64, 67, 70, 72, 76, 95, 104, 113, 122].The MB group evidenced a greater rate of deep infections (OR 1.64; 95% CI 1.07 to 2.52; P = 0.02; Fig. 6).
Fig. 6.
Forest plot of the comparison: rate of deep infection (M–H: Mantel–Haenszel; CI: confidence interval). The square represents the effect of each single study. The horizontal line represents the confidence interval of each study. The vertical line “0” represent the no effect threshold. The diamond represents the final effect of the overall analysis
No difference was found in implant positioning: tibial slope, delta angle, alpha femoral component angle, gamma femoral component angle, beta tibial component angle, tibiofemoral alignment angle, posterior condylar offset, radiolucent lines. No difference was found in duration of the surgical procedure. No differences were found in the following PROMs: OKS, WOMAC, VAS, function and pain subscales of the KSS score. No difference were found in the rate of the following complications: AKP, revision, aseptic loosening, fractures, DVT.
Discussion
The main finding of the present study was that the MB implants performed in a similar fashion to FB implants for TKA. The analyses evidenced greater KSS, ROM, and rate of the deep infection in MB implants. However, though statistically significant, their clinical relevance is likely limited. Concerning the KSS score, its overall difference between the two implants does not overcome their minimal clinically important difference (MCID), which has been estimated between 6/100 and 9/100 [40, 52, 68, 69, 112]. A formal MCID for the ROM has not yet been estimated. However, given its minimal difference, the clinical relevance of this finding is dubious. Marques et al. [75] conducted a RCT on 99 patients. After 1-year follow-up, a statistically significant increase in ROM and KSS was found in the MB group. After 4-year follow-up no difference was found between the MB and FB group. Kim et al. [59] conducted a RTC on 291 patients, with a follow-up period of 27 years. No differences were found in ROM and KSS between the two groups. Powell et al. [95] analysed 167 patients at 10 years of follow-up, with no statistically significant difference in KSS between MB and FB groups. However, a trend was seen with higher mean scores over the years for the MB group. Given the minimal difference between the two groups in ROM and KSS, the clinical relevance of these findings was dubious. A slight improvement of PROMs was not necessarily associated with a functional advantage [15]. The minimal functional improvement may be explained by greater axial rotation promoted by the MB implants [29, 53, 99]. Amaro et al. [8] evaluating kinematic differences in 64 patients, found that axial rotation was higher in the MB group after 1 year, but disappeared at 2-year follow-up. A histological study showed the development of fibrotic tissue in the synovial membrane and infrapatellar fat pad after a TKA [3]. This produces a hardening effect that may minimize the kinematic differences between the MB and FB groups [8]. MB actively corrects the rotational femoral offset while standing, improving stepping and squatting [46]. However, this difference is not clinically relevant [88]. Moreover, different types of MB implants have different kinematics during stepping and squatting [46], and the final clinical outcome of MB can be influenced by the brand. A long-term study comparing different types of MB and FB implants could be useful to further understand the real benefits of different type of prostheses.
The rate of deep infection was strongly influenced by the study by Breeman et al. [17], which weighted 17.6% on the final effect. Indeed, when conducting the analyses without those data [17], the rate of deep infection is similar between the two groups. Nevertheless, the authors evidenced no difference between the two implants in terms of infections in their study [17]. Indeed, a deep infection was present in 12 of 276 patients in the MB group, and in 6 of 263 patients in the FB group [17]. Some limitations that may have influence our results should be discussed. The authors conducted a multicentre study involving 116 surgeons [17, 99]. Surgeon experience and approaches, implants design and post-operative protocols were not considered.
No differences in radiographic alignment were shown in the present study. Only one study showed a radiographic difference in patellar translation [104]. A tendency to increase patellar translation in the MB group was also evidenced in the present study. In MB implants, the rotation of the tibial component and the variable position of the tibial relative to the femoral implant can affect patellar tracking [90]. However, other meta-analyses comparing patellar translation did not evidence any differences between MB and FB implants [86, 111].
The MB design has been introduced to better simulate knee kinematics, reducing contact stresses, aseptic loosening, and polyethylene wear [20]. The self-alignment promoted by the MB implants compensates the physiological tibial and the femoral component offset [30]. The latter has been hypothesized to improve the conformity between femoral component and mobile insert during stepping and squatting, thus reducing contact pressure and loosening of polyethylene wear [46]. However, this study was unable to identify differences between the two implants, in contest with previous evidence [59, 62, 105]. Though there is less wear at the femoral condyle interface in MB than in FB implant, the former produce additional wear at the surface of metallic tibial implant, which may explain the similarity in the rate of overall wear [105]. Only one study [37] showed a higher rate of aseptic loosening in the MB group. The risk was higher only in certain models. In the MB implants, the geometry of tibial component is such that the shortening of the keel and the under-face texture increase the risk for micromotion and aseptic loosening [26, 53, 65, 101, 104, 108].
This study certainly has limitations. The analyses were conducted irrespective of the surgical exposure and approach. In the present study, both minimally and standard invasive techniques were included. Surgical exposure may influence outcomes, and minimally invasive surgery performed by experienced surgeon may offer short- and mid-term clinical and functional benefits over the conventional exposure [78]. Moreover, the surgical approach may influence the clinical outcomes. A recent network meta-analysis demonstrated that the mini-subvastus approach outperformed all other approaches (mini-medial parapatellar, midvastus, quadriceps sparring) [77]. Patellar retaining or resurfacing has not been investigated, and may represent a further limitation [80]. Different inlay designs (posterior stabilized, cruciate/bicruciate retaining) were not considered as separate. A previous meta-analysis demonstrated no difference in the outcome between the posterior stabilized versus cruciate retaining [81], while no study which compared MB versus FB using bicruciate retaining implants were included in the present study. The manufacturer of the implants was often biased. MB implants are more sensitive to soft tissue release and optimal gap balancing over flexion and extension. Differently, in FB implants planned resection following the anatomical landmarks (anteroposterior and trans-epicondylar axis) can be performed [79]. Few authors appropriately described the surgical protocol, and further subgroups comparisons were not possible. This may generate bias and increase heterogeneity. The conclusion of the present meta-analysis should be considered with these limitations. Results of the present study indicated that bearing in TKA, whether mobile or fixed, does not influence the clinical outcome.
Conclusion
There is no evidence to support that MP implants promote better outcomes compared to FB implants in primary TKA. The analyses evidenced greater KSS, ROM, and greater rate of the deep infection in MB implants. However, though statistically significant, their clinical relevance is limited. Further clinical trials are required.
Acknowledgements
None.
Author contributions
FM: writing, revising, selection, data collection, data extraction, synthesis methods, study risk of bias assessment, final approval; KE: writing, revising, study selection, data collection, data extraction, study risk of bias assessment, final approval; MP: writing, revising, final approval; FC: writing, revising, final approval; FH: writing, revising, study risk of bias assessment, final approval; JE: writing, revising, final approval; NM: writing, revising, final approval.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial or material support for the research, authorship, and/or publication of this article.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
The authors declare that they have any competing interests for this article.
Ethical approval
This study complies with ethical standards.
Consent to publish
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Filippo Migliorini, Email: migliorini.md@gmail.com.
Nicola Maffulli, Email: n.maffulli@qmul.ac.uk.
Francesco Cuozzo, Email: fra.cuoz@gmail.com.
Marco Pilone, Email: m.pilone97@gmail.com.
Karen Elsner, Email: karenelsner@netcologne.de.
Jörg Eschweiler, Email: joeschweiler@ukaachen.de.
References
- 1.Abdel MP, Tibbo ME, Stuart MJ, Trousdale RT, Hanssen AD, Pagnano MW. Infographic: fixed- versus mobile-bearing total knee arthroplasty at ten years. Bone Joint J. 2018;100-B:923–924. doi: 10.1302/0301-620X.100B7.BJJ-2018-0577. [DOI] [PubMed] [Google Scholar]
- 2.Abdel MP, Tibbo ME, Stuart MJ, Trousdale RT, Hanssen AD, Pagnano MW. A randomized controlled trial of fixed- versus mobile-bearing total knee arthroplasty: a follow-up at a mean of ten years. Bone Joint J. 2018;100-B:925–929. doi: 10.1302/0301-620X.100B7.BJJ-2017-1473.R1. [DOI] [PubMed] [Google Scholar]
- 3.Abdul N, Dixon D, Walker A, Horabin J, Smith N, Weir DJ, et al. Fibrosis is a common outcome following total knee arthroplasty. Sci Rep. 2015;5:16469. doi: 10.1038/srep16469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal AK, Agrawal A. Mobile vs fixed-bearing total knee arthroplasty performed by a single surgeon: a 4- to 6.5-year randomized, prospective, controlled, double-blinded study. J Arthroplasty. 2013;28:1712–1716. doi: 10.1016/j.arth.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Aglietti P, Baldini A, Buzzi R, Lup D, De Luca L. Comparison of mobile-bearing and fixed-bearing total knee arthroplasty: a prospective randomized study. J Arthroplasty. 2005;20:145–153. doi: 10.1016/j.arth.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 6.Ahrar H, Aghili K, Sobhan MR, Mahdinezhad-Yazdi M, Akbarian-Bafghi MJ, Neamatzadeh H. Association of rs2234693 and rs9340799 polymorphisms of estrogen receptor-1 gene with radiographic defined knee osteoarthritis: a meta-analysis. J Orthop. 2019;16:234–240. doi: 10.1016/j.jor.2019.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amaro JT, Arliani GG, Astur DC, Debieux P, Kaleka CC, Cohen M. No difference between fixed- and mobile-bearing total knee arthroplasty in activities of daily living and pain: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:1692–1696. doi: 10.1007/s00167-016-4106-1. [DOI] [PubMed] [Google Scholar]
- 8.Amaro JT, Novaretti JV, Astur DC, Cavalcante ELB, Rodrigues Junior AG, Debieux P, et al. Higher axial tibiofemoral rotation and functional outcomes with mobile-bearing compared with fixed-bearing total knee arthroplasty at 1- but not at 2-year follow-up-a randomized clinical trial. J Knee Surg. 2020;33:474–480. doi: 10.1055/s-0039-1678675. [DOI] [PubMed] [Google Scholar]
- 9.Artz NJ, Hassaballa MA, Robinson JR, Newman JH, Porteous AJ, Murray JR. Patient reported kneeling ability in fixed and mobile bearing knee arthroplasty. J Arthroplasty. 2015;30:2159–2163. doi: 10.1016/j.arth.2015.06.063. [DOI] [PubMed] [Google Scholar]
- 10.Bailey O, Ferguson K, Crawfurd E, James P, May PA, Brown S, et al. No clinical difference between fixed- and mobile-bearing cruciate-retaining total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1653–1659. doi: 10.1007/s00167-014-2877-9. [DOI] [PubMed] [Google Scholar]
- 11.Baktir A, Karaaslan F, Yurdakul E, Karaoglu S. Mobile- versus fixed-bearing total knee arthroplasty: a prospective randomized controlled trial featuring 6–10-year follow-up. Acta Orthop Traumatol Turc. 2016;50:1–9. doi: 10.3944/AOTT.2016.15.0120. [DOI] [PubMed] [Google Scholar]
- 12.Ball ST, Sanchez HB, Mahoney OM, Schmalzried TP. Fixed versus rotating platform total knee arthroplasty: a prospective, randomized, single-blind study. J Arthroplasty. 2011;26:531–536. doi: 10.1016/j.arth.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Beard DJ, Pandit H, Price AJ, Butler-Manuel PA, Dodd CA, Murray DW, et al. Introduction of a new mobile-bearing total knee prosthesis: minimum three year follow-up of an RCT comparing it with a fixed-bearing device. Knee. 2007;14:448–451. doi: 10.1016/j.knee.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Bhan S, Malhotra R, Kiran EK, Shukla S, Bijjawara M. A comparison of fixed-bearing and mobile-bearing total knee arthroplasty at a minimum follow-up of 4.5 years. J Bone Joint Surg Am. 2005;87:2290–2296. doi: 10.2106/JBJS.D.02221. [DOI] [PubMed] [Google Scholar]
- 15.Birnir B, Tierney ML, Lim M, Cox GB, Gage PW. Nature of the 5' residue in the M2 domain affects function of the human alpha 1 beta 1 GABAA receptor. Synapse. 1997;26:324–327. doi: 10.1002/(SICI)1098-2396(199707)26:3<324::AID-SYN13>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 16.Bistolfi A, Massazza G, Lee GC, Deledda D, Berchialla P, Crova M. Comparison of fixed and mobile-bearing total knee arthroplasty at a mean follow-up of 116 months. J Bone Joint Surg Am. 2013;95:e83. doi: 10.2106/JBJS.L.00327. [DOI] [PubMed] [Google Scholar]
- 17.Breeman S, Campbell MK, Dakin H, Fiddian N, Fitzpatrick R, Grant A, et al. Five-year results of a randomised controlled trial comparing mobile and fixed bearings in total knee replacement. Bone Joint J. 2013;95-B:486–492. doi: 10.1302/0301-620X.95B4.29454. [DOI] [PubMed] [Google Scholar]
- 18.Breugem SJ, Sierevelt IN, Schafroth MU, Blankevoort L, Schaap GR, van Dijk CN. Less anterior knee pain with a mobile-bearing prosthesis compared with a fixed-bearing prosthesis. Clin Orthop Relat Res. 2008;466:1959–1965. doi: 10.1007/s11999-008-0320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breugem SJ, van Ooij B, Haverkamp D, Sierevelt IN, van Dijk CN. No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc. 2014;22:509–516. doi: 10.1007/s00167-012-2281-2. [DOI] [PubMed] [Google Scholar]
- 20.Buechel FF, Pappas MJ. The New Jersey low-contact-stress knee replacement system: biomechanical rationale and review of the first 123 cemented cases. Arch Orthop Trauma Surg. 1986;105:197–204. doi: 10.1007/BF00435480. [DOI] [PubMed] [Google Scholar]
- 21.Capella M, Dolfin M, Saccia F. Mobile bearing and fixed bearing total knee arthroplasty. Ann Transl Med. 2016;4:127. doi: 10.21037/atm.2015.12.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Castellarin G, Bori E, Innocenti B. Experimental and clinical analysis of the use of asymmetric vs symmetric polyethylene inserts in a mobile bearing total knee arthroplasty. J Orthop. 2021;23:25–30. doi: 10.1016/j.jor.2020.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaudhry A, Goyal VK. Fixed-bearing versus high-flexion RP total knee arthroplasty (TKA): midterm results of a randomized controlled trial. J Orthop Traumatol. 2018;19:2. doi: 10.1186/s10195-018-0493-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen P, Huang L, Zhang D, Zhang X, Ma Y, Wang Q. Mobile bearing versus fixed bearing for total knee arthroplasty: meta-analysis of randomized controlled trials at minimum 10-year follow-up. J Knee Surg. 2022;35:135–144. doi: 10.1055/s-0040-1713356. [DOI] [PubMed] [Google Scholar]
- 25.Choi WC, Lee S, Seong SC, Jung JH, Lee MC. Comparison between standard and high-flexion posterior-stabilized rotating-platform mobile-bearing total knee arthroplasties: a randomized controlled study. J Bone Joint Surg Am. 2010;92:2634–2642. doi: 10.2106/JBJS.I.01122. [DOI] [PubMed] [Google Scholar]
- 26.Crossett L. Evolution of the low contact stress (LCS) complete knee system. Orthopedics. 2006;29:S17–22. [PubMed] [Google Scholar]
- 27.Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. 2019;10:142. doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalyan S, Ozan F, Altun I, Kahraman M, Gunay AE, Ozdemir K. The influence of component rotational malalignment on early clinical outcomes in total knee arthroplasty. Cureus. 2022;14:e22444. doi: 10.7759/cureus.22444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delport HP, Banks SA, De Schepper J, Bellemans J. A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br. 2006;88:1016–1021. doi: 10.1302/0301-620X.88B8.17529. [DOI] [PubMed] [Google Scholar]
- 30.Dennis DA, Komistek RD. Mobile-bearing total knee arthroplasty: design factors in minimizing wear. Clin Orthop Relat Res. 2006;452:70–77. doi: 10.1097/01.blo.0000238776.27316.d6. [DOI] [PubMed] [Google Scholar]
- 31.Feczko PZ, Jutten LM, van Steyn MJ, Deckers P, Emans PJ, Arts JJ. Comparison of fixed and mobile-bearing total knee arthroplasty in terms of patellofemoral pain and function: a prospective, randomised, controlled trial. BMC Musculoskelet Disord. 2017;18:279. doi: 10.1186/s12891-017-1635-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferguson KB, Bailey O, Anthony I, James PJ, Stother IG, M JGB, A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design—outcomes at two year follow-up. Knee. 2014;21:151–155. doi: 10.1016/j.knee.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 33.Fransen BL, Hoozemans MJ, Keijser LC, van Lent ME, Verheyen CC, Burger BJ. Does insert type affect clinical and functional outcome in total knee arthroplasty? A Randomised controlled clinical trial with 5-year follow-up. J Arthroplasty. 2015;30:1931–1937. doi: 10.1016/j.arth.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 34.Fransen BL, van Duijvenbode DC, Hoozemans MJM, Burger BJ. No differences between fixed- and mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25:1757–1777. doi: 10.1007/s00167-016-4195-x. [DOI] [PubMed] [Google Scholar]
- 35.Garling EH, Valstar ER, Nelissen RG. Comparison of micromotion in mobile bearing and posterior stabilized total knee prostheses: a randomized RSA study of 40 knees followed for 2 years. Acta Orthop. 2005;76:353–361. doi: 10.1080/00016470510030823. [DOI] [PubMed] [Google Scholar]
- 36.Gioe TJ, Glynn J, Sembrano J, Suthers K, Santos ER, Singh J. Mobile and fixed-bearing (all-polyethylene tibial component) total knee arthroplasty designs. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:2104–2112. doi: 10.2106/JBJS.H.01442. [DOI] [PubMed] [Google Scholar]
- 37.Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J. 2013;95-B:636–642. doi: 10.1302/0301-620X.95B5.30271. [DOI] [PubMed] [Google Scholar]
- 38.Hansson U, Toksvig-Larsen S, Jorn LP, Ryd L. Mobile vs. fixed meniscal bearing in total knee replacement: a randomised radiostereometric study. Knee. 2005;12:414–418. doi: 10.1016/j.knee.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 39.Hanusch B, Lou TN, Warriner G, Hui A, Gregg P. Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomised controlled trial. Int Orthop. 2010;34:349–354. doi: 10.1007/s00264-009-0901-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hao D, Wang J. Fixed-bearing vs mobile-bearing prostheses for total knee arthroplasty after approximately 10 years of follow-up: a meta-analysis. J Orthop Surg Res. 2021;16:437. doi: 10.1186/s13018-021-02560-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harrington MA, Hopkinson WJ, Hsu P, Manion L. Fixed- vs mobile-bearing total knee arthroplasty: does it make a difference?—a prospective randomized study. J Arthroplasty. 2009;24:24–27. doi: 10.1016/j.arth.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 42.Hasegawa M, Sudo A, Uchida A. Staged bilateral mobile-bearing and fixed-bearing total knee arthroplasty in the same patients: a prospective comparison of a posterior-stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc. 2009;17:237–243. doi: 10.1007/s00167-008-0662-3. [DOI] [PubMed] [Google Scholar]
- 43.Henricson A, Dalen T, Nilsson KG. Mobile bearings do not improve fixation in cemented total knee arthroplasty. Clin Orthop Relat Res. 2006;448:114–121. doi: 10.1097/01.blo.0000224004.40883.ab. [DOI] [PubMed] [Google Scholar]
- 44.Hernigou P, Huys M, Pariat J, Roubineau F, Flouzat Lachaniette CH, Dubory A. Comparison of fixed-bearing and mobile-bearing total knee arthroplasty after high tibial osteotomy. Int Orthop. 2018;42:317–322. doi: 10.1007/s00264-017-3540-0. [DOI] [PubMed] [Google Scholar]
- 45.Hofstede SN, Nouta KA, Jacobs W, van Hooff ML, Wymenga AB, Pijls BG, et al. Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD003130.pub3CD003130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoshi K, Watanabe G, Kurose Y, Tanaka R, Fujii J, Gamada K. Mobile-bearing insert used with total knee arthroplasty does not rotate on the tibial tray during a squatting activity: a cross-sectional study. J Orthop Surg Res. 2020;15:114. doi: 10.1186/s13018-020-1570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Howick J CI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM levels of evidence. Oxford Centre for Evidence-Based Medicine. Available at: https://www.cebm.net/. Accessed May 2022
- 48.Jacobs WC, Christen B, Wymenga AB, Schuster A, van der Schaaf DB, ten Ham A, et al. Functional performance of mobile versus fixed bearing total knee prostheses: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2012;20:1450–1455. doi: 10.1007/s00167-011-1684-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jamshed S, Shah R, Arooj A, Turner A, Plakogiannis C. A novel radiographic technique to assess 180 degrees rotational spin of the Oxford unicompartmental knee mobile bearing. J Orthop. 2020;21:438–443. doi: 10.1016/j.jor.2020.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jolles BM, Grzesiak A, Eudier A, Dejnabadi H, Voracek C, Pichonnaz C, et al. A randomised controlled clinical trial and gait analysis of fixed- and mobile-bearing total knee replacements with a five-year follow-up. J Bone Joint Surg Br. 2012;94:648–655. doi: 10.1302/0301-620X.94B5.27598. [DOI] [PubMed] [Google Scholar]
- 51.Kalisvaart MM, Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD. Randomized clinical trial of rotating-platform and fixed-bearing total knee arthroplasty: no clinically detectable differences at five years. J Bone Joint Surg Am. 2012;94:481–489. doi: 10.2106/JBJS.K.00315. [DOI] [PubMed] [Google Scholar]
- 52.Khow YZ, Liow MHL, Goh GS, Chen JY, Lo NN, Yeo SJ. Defining the minimal clinically important difference for the knee society score following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021 doi: 10.1007/s00167-021-06628-2. [DOI] [PubMed] [Google Scholar]
- 53.Killen CJ, Murphy MP, Hopkinson WJ, Harrington MA, Adams WH, Rees HW. Minimum twelve-year follow-up of fixed- vs mobile-bearing total knee arthroplasty: double blinded randomized trial. J Clin Orthop Trauma. 2020;11:154–159. doi: 10.1016/j.jcot.2019.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim D, Seong SC, Lee MC, Lee S. Comparison of the tibiofemoral rotational alignment after mobile and fixed bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:337–345. doi: 10.1007/s00167-011-1750-3. [DOI] [PubMed] [Google Scholar]
- 55.Kim TK, Chang CB, Kang YG, Chung BJ, Cho HJ, Seong SC. Early clinical outcomes of floating platform mobile-bearing TKA: longitudinal comparison with fixed-bearing TKA. Knee Surg Sports Traumatol Arthrosc. 2010;18:879–888. doi: 10.1007/s00167-009-0985-8. [DOI] [PubMed] [Google Scholar]
- 56.Kim YH, Kim DY, Kim JS. Simultaneous mobile- and fixed-bearing total knee replacement in the same patients. A prospective comparison of mid-term outcomes using a similar design of prosthesis. J Bone Joint Surg Br. 2007;89:904–910. doi: 10.1302/0301-620X.89B7.18635. [DOI] [PubMed] [Google Scholar]
- 57.Kim YH, Kim JS. Prevalence of osteolysis after simultaneous bilateral fixed- and mobile-bearing total knee arthroplasties in young patients. J Arthroplasty. 2009;24:932–940. doi: 10.1016/j.arth.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 58.Kim YH, Kim JS, Choe JW, Kim HJ. Long-term comparison of fixed-bearing and mobile-bearing total knee replacements in patients younger than fifty-one years of age with osteoarthritis. J Bone Joint Surg Am. 2012;94:866–873. doi: 10.2106/JBJS.K.00884. [DOI] [PubMed] [Google Scholar]
- 59.Kim YH, Park JW, Jang YS. Long-term (Up to 27 years) prospective, randomized study of mobile-bearing and fixed-bearing total knee arthroplasties in patients < 60 years of age with osteoarthritis. J Arthroplasty. 2021;36:1330–1335. doi: 10.1016/j.arth.2020.10.050. [DOI] [PubMed] [Google Scholar]
- 60.Kim YH, Park JW, Kim JS. Comparison of high-flexion fixed-bearing and high-flexion mobile-bearing total knee arthroplasties—a prospective randomized study. J Arthroplasty. 2018;33:130–135. doi: 10.1016/j.arth.2017.07.025. [DOI] [PubMed] [Google Scholar]
- 61.Kim YH, Park JW, Kim JS. The long-term results of simultaneous high-flexion mobile-bearing and fixed-bearing total knee arthroplasties performed in the same patients. J Arthroplasty. 2019;34:501–507. doi: 10.1016/j.arth.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 62.Kim YH, Park JW, Kim JS, Kulkarni SS, Kim YH. Long-term clinical outcomes and survivorship of press-fit condylar sigma fixed-bearing and mobile-bearing total knee prostheses in the same patients. J Bone Joint Surg Am. 2014;96:e168. doi: 10.2106/JBJS.M.01130. [DOI] [PubMed] [Google Scholar]
- 63.Kim YH, Yoon SH, Kim JS. Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res. 2009;467:493–503. doi: 10.1007/s11999-008-0221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kim YH, Yoon SH, Kim JS. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg Br. 2007;89:1317–1323. doi: 10.1302/0301-620X.89B10.19223. [DOI] [PubMed] [Google Scholar]
- 65.Kutzner I, Hallan G, Hol PJ, Furnes O, Gothesen O, Figved W, et al. Early aseptic loosening of a mobile-bearing total knee replacement. Acta Orthop. 2018;89:77–83. doi: 10.1080/17453674.2017.1398012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ladermann A, Lubbeke A, Stern R, Riand N, Fritschy D. Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomised, clinical and radiological study with mid-term results at 7 years. Knee. 2008;15:206–210. doi: 10.1016/j.knee.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 67.Ladermann A, Saudan M, Riand N, Fritschy D. Fixed-bearing versus mobile-bearing total knee arthroplasty: a prospective randomized clinical and radiological study. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:247–251. doi: 10.1016/j.rco.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 68.Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2017;25:3354–3359. doi: 10.1007/s00167-016-4208-9. [DOI] [PubMed] [Google Scholar]
- 69.Lizaur-Utrilla A, Gonzalez-Parreno S, Martinez-Mendez D, Miralles-Munoz FA, Lopez-Prats FA. Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surg Sports Traumatol Arthrosc. 2020;28:1473–1478. doi: 10.1007/s00167-019-05543-x. [DOI] [PubMed] [Google Scholar]
- 70.Lizaur-Utrilla A, Sanz-Reig J, Trigueros-Rentero MA. Greater satisfaction in older patients with a mobile-bearing compared with fixed-bearing total knee arthroplasty. J Arthroplasty. 2012;27:207–212. doi: 10.1016/j.arth.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 71.Maffulli GD, Bridgman S, Maffulli N. Early functional outcome after subvastus or parapatellar approach in knee arthroplasty is comparable. Knee Surg Sports Traumatol Arthrosc. 2012;20:1883–1884. doi: 10.1007/s00167-011-1810-8. [DOI] [PubMed] [Google Scholar]
- 72.Mahoney OM, Kinsey TL, D'Errico TJ, Shen J. The John Insall Award: no functional advantage of a mobile bearing posterior stabilized TKA. Clin Orthop Relat Res. 2012;470:33–44. doi: 10.1007/s11999-011-2114-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Malahias MA, Manolopoulos PP, Mancino F, Jang SJ, Gu A, Giotis D, et al. Safety and outcome of simultaneous bilateral unicompartmental knee arthroplasty: a systematic review. J Orthop. 2021;24:58–64. doi: 10.1016/j.jor.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mannani M, Motififard M, Farajzadegan Z, Nemati A. Length of stay in patients undergoing total knee arthroplasty. J Orthop. 2022;32:121–124. doi: 10.1016/j.jor.2022.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Marques CJ, Daniel S, Sufi-Siavach A, Lampe F. No differences in clinical outcomes between fixed- and mobile-bearing computer-assisted total knee arthroplasties and no correlations between navigation data and clinical scores. Knee Surg Sports Traumatol Arthrosc. 2015;23:1660–1668. doi: 10.1007/s00167-014-3127-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Matsuda S, Mizu-uchi H, Fukagawa S, Miura H, Okazaki K, Matsuda H, et al. Mobile-bearing prosthesis did not improve mid-term clinical results of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010;18:1311–1316. doi: 10.1007/s00167-010-1143-z. [DOI] [PubMed] [Google Scholar]
- 77.Migliorini F, Aretini P, Driessen A, El Mansy Y, Quack V, Tingart M, et al. Better outcomes after mini-subvastus approach for primary total knee arthroplasty: a Bayesian network meta-analysis. Eur J Orthop Surg Traumatol. 2020;30:979–992. doi: 10.1007/s00590-020-02648-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Migliorini F, Eschweiler J, Baroncini A, Tingart M, Maffulli N. Better outcomes after minimally invasive surgeries compared to the standard invasive medial parapatellar approach for total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06306-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Migliorini F, Eschweiler J, Mansy YE, Quack V, Schenker H, Tingart M, et al. Gap balancing versus measured resection for primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg. 2020;140:1245–1253. doi: 10.1007/s00402-020-03478-4. [DOI] [PubMed] [Google Scholar]
- 80.Migliorini F, Eschweiler J, Niewiera M, El Mansy Y, Tingart M, Rath B. Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study. Arch Orthop Trauma Surg. 2019;139:1445–1454. doi: 10.1007/s00402-019-03246-z. [DOI] [PubMed] [Google Scholar]
- 81.Migliorini F, Eschweiler J, Tingart M, Rath B. Posterior-stabilized versus cruciate-retained implants for total knee arthroplasty: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol. 2019;29:937–946. doi: 10.1007/s00590-019-02370-1. [DOI] [PubMed] [Google Scholar]
- 82.Migliorini F, Maffulli N, Cuozzo F, Elsner K, Hildebrand F, Eschweiler J, et al. Mobile bearing versus fixed bearing for unicompartmental arthroplasty in monocompartmental osteoarthritis of the knee: a meta-analysis. J Clin Med. 2022;11:2837. doi: 10.3390/jcm11102837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Minoda Y, Iwaki H, Ikebuchi M, Yoshida T, Mizokawa S, Itokazu M, et al. Mobile-bearing prosthesis and intraoperative gap balancing are not predictors of superior knee flexion: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2015;23:1986–1992. doi: 10.1007/s00167-014-2838-3. [DOI] [PubMed] [Google Scholar]
- 84.Morikawa LH, Combs DB, Andrews SN, Mathews K, Nakasone CK. Component positioning of the first 300 mobile bearing unicompartmental knee arthroplasties. J Orthop. 2021;27:9–12. doi: 10.1016/j.jor.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mortman R, Gioia C, Stake S, Berger PZ, Gu A, Fassihi SC, et al. Linked kinematic knee balancing in unicompartmental knee arthroplasty. J Orthop. 2021;24:182–185. doi: 10.1016/j.jor.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Moskal JT, Capps SG. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res. 2014;472:2185–2193. doi: 10.1007/s11999-014-3539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nutton RW, Wade FA, Coutts FJ, van der Linden ML. Does a mobile-bearing, high-flexion design increase knee flexion after total knee replacement? J Bone Joint Surg Br. 2012;94:1051–1057. doi: 10.1302/0301-620X.94B8.28828. [DOI] [PubMed] [Google Scholar]
- 88.Okamoto N, Nakamura E, Nishioka H, Karasugi T, Okada T, Mizuta H. In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplasty. 2014;29:2393–2396. doi: 10.1016/j.arth.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 89.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ. Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res. 2004;428:221–227. doi: 10.1097/01.blo.0000148892.31464.81. [DOI] [PubMed] [Google Scholar]
- 91.Park CH, Kang SG, Bae DK, Song SJ. Mid-term clinical and radiological results do not differ between fixed- and mobile-bearing total knee arthroplasty using titanium-nitride-coated posterior-stabilized prostheses: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27:1165–1173. doi: 10.1007/s00167-018-5095-z. [DOI] [PubMed] [Google Scholar]
- 92.Pijls BG, Valstar ER, Kaptein BL, Nelissen RG. Differences in long-term fixation between mobile-bearing and fixed-bearing knee prostheses at ten to 12 years' follow-up: a single-blinded randomised controlled radiostereometric trial. J Bone Joint Surg Br. 2012;94:1366–1371. doi: 10.1302/0301-620X.94B10.28858. [DOI] [PubMed] [Google Scholar]
- 93.Poirier N, Graf P, Dubrana F. Mobile-bearing versus fixed-bearing total knee implants. Results of a series of 100 randomised cases after 9 years follow-up. Orthop Traumatol Surg Res. 2015;101:S187–192. doi: 10.1016/j.otsr.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 94.Poornima S, Subramanyam K, Khan IA, G S, Hasan Q, Role of SREBP2 gene polymorphism on knee osteoarthritis in the South Indian Hyderabad Population: a hospital based study with G595C variant. J Orthop. 2019;16:293–297. doi: 10.1016/j.jor.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Powell AJ, Crua E, Chong BC, Gordon R, McAuslan A, Pitto RP, et al. A randomized prospective study comparing mobile-bearing against fixed-bearing PFC Sigma cruciate-retaining total knee arthroplasties with ten-year minimum follow-up. Bone Joint J. 2018;100-B:1336–1344. doi: 10.1302/0301-620X.100B10.BJJ-2017-1450.R1. [DOI] [PubMed] [Google Scholar]
- 96.Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, et al. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br. 2003;85:62–67. doi: 10.1302/0301-620X.85B1.13233. [DOI] [PubMed] [Google Scholar]
- 97.Radetzki F, Wienke A, Mendel T, Gutteck N, Delank KS, Wohlrab D. High flex total knee arthroplasty—a prospective, randomized study with results after 10 years. Acta Orthop Belg. 2013;79:536–540. [PubMed] [Google Scholar]
- 98.Rahman WA, Garbuz DS, Masri BA. Randomized controlled trial of radiographic and patient-assessed outcomes following fixed versus rotating platform total knee arthroplasty. J Arthroplasty. 2010;25:1201–1208. doi: 10.1016/j.arth.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 99.Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;418:184–190. doi: 10.1097/00003086-200401000-00030. [DOI] [PubMed] [Google Scholar]
- 100.Riaz O, Aqil A, Sisodia G, Chakrabarty G. P.F.C Sigma((R)) cruciate retaining fixed-bearing versus mobile-bearing knee arthroplasty: a prospective comparative study with minimum 10-year follow-up. Eur J Orthop Surg Traumatol. 2017;27:1145–1149. doi: 10.1007/s00590-017-1920-1. [DOI] [PubMed] [Google Scholar]
- 101.Ries C, Heinichen M, Dietrich F, Jakubowitz E, Sobau C, Heisel C. Short-keeled cemented tibial components show an increased risk for aseptic loosening. Clin Orthop Relat Res. 2013;471:1008–1013. doi: 10.1007/s11999-012-2630-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Roh YW, Jang J, Choi WC, Lee JK, Chun SH, Lee S, et al. Preservation of the posterior cruciate ligament is not helpful in highly conforming mobile-bearing total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2013;21:2850–2859. doi: 10.1007/s00167-012-2265-2. [DOI] [PubMed] [Google Scholar]
- 103.Ruckenstuhl P, Revelant F, Hauer G, Bernhardt GA, Leitner L, Gruber G, et al. No difference in clinical outcome, pain, and range of motion between fixed and mobile bearing Attune total knee arthroplasty: a prospective single-center trial. BMC Musculoskelet Disord. 2022;23:413. doi: 10.1186/s12891-022-05382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sappey-Marinier E, de Abreu FGA, O'Loughlin P, Gaillard R, Neyret P, Lustig S, et al. No difference in patellar position between mobile-bearing and fixed-bearing total knee arthroplasty for medial osteoarthritis: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. 2020;28:1542–1550. doi: 10.1007/s00167-019-05565-5. [DOI] [PubMed] [Google Scholar]
- 105.Sappey-Marinier E, Swan J, Maucort-Boulch D, Batailler C, Malatray M, Neyret P, et al. No significant clinical and radiological differences between fixed versus mobile bearing total knee replacement using the same semi-constrained implant type: a randomized controlled trial with mean 10 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-06346-1. [DOI] [PubMed] [Google Scholar]
- 106.Schotanus MGM, Pilot P, Kaptein BL, Draijer WF, Tilman PBJ, Vos R, et al. No difference in terms of radiostereometric analysis between fixed- and mobile-bearing total knee arthroplasty: a randomized, single-blind, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:2978–2985. doi: 10.1007/s00167-016-4138-6. [DOI] [PubMed] [Google Scholar]
- 107.Schotanus MGM, Pilot P, Vos R, Kort NP. No difference in joint awareness after mobile- and fixed-bearing total knee arthroplasty: 3-year follow-up of a randomized controlled trial. Eur J Orthop Surg Traumatol. 2017;27:1151–1155. doi: 10.1007/s00590-017-1921-0. [DOI] [PubMed] [Google Scholar]
- 108.Scott CE, Biant LC. The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br. 2012;94:1009–1015. doi: 10.1302/0301-620X.94B8.28289. [DOI] [PubMed] [Google Scholar]
- 109.Scuderi GR, Hedden DR, Maltry JA, Traina SM, Sheinkop MB, Hartzband MA. Early clinical results of a high-flexion, posterior-stabilized, mobile-bearing total knee arthroplasty: a US investigational device exemption trial. J Arthroplasty. 2012;27:421–429. doi: 10.1016/j.arth.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 110.Shemshaki H, Dehghani M, Eshaghi MA, Esfahani MF. Fixed versus mobile weight-bearing prosthesis in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:2519–2527. doi: 10.1007/s00167-012-1946-1. [DOI] [PubMed] [Google Scholar]
- 111.Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R. Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty. 2011;26:1205–1213. doi: 10.1016/j.arth.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 112.Song SJ, Lee HW, Bae DK, Park CH. High incidence of tibial component loosening after total knee arthroplasty using ceramic titanium-nitride-coated mobile bearing prosthesis in moderate to severe varus deformity: a matched-pair study between ceramic-coated mobile bearing and fixed bearing prostheses. J Arthroplasty. 2020;35:1003–1008. doi: 10.1016/j.arth.2019.11.034. [DOI] [PubMed] [Google Scholar]
- 113.Tiwari V, Meshram P, Park CK, Bansal V, Kim TK. New mobile-bearing TKA with unique ball and socket post-cam mechanism offers similar function and stability with better prosthesis fit and gap balancing compared to an established fixed-bearing prosthesis. Knee Surg Sports Traumatol Arthrosc. 2019;27:2145–2154. doi: 10.1007/s00167-019-05430-5. [DOI] [PubMed] [Google Scholar]
- 114.Tjornild M, Soballe K, Hansen PM, Holm C, Stilling M. Mobile- vs. fixed-bearing total knee replacement. Acta Orthop. 2015;86:208–214. doi: 10.3109/17453674.2014.968476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tornese D, Robustelli A, Ricci G, Rancoita PMV, Maffulli N, Peretti GM. Predictors of postoperative hospital length of stay after total knee arthroplasty. Singapore Med J. 2021 doi: 10.11622/smedj.2021142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Urwin SG, Kader DF, Caplan N, St Clair Gibson A, Stewart S. Gait analysis of fixed bearing and mobile bearing total knee prostheses during walking: do mobile bearings offer functional advantages? Knee. 2014;21:391–395. doi: 10.1016/j.knee.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 117.Van Hamersveld KT, Marang-Van De Mheen PJ, Van Der Heide HJL, Der Linden-Van V, Der Zwaag HMJ, Valstar ER, Nelissen R. Migration and clinical outcome of mobile-bearing versus fixed-bearing single-radius total knee arthroplasty. Acta Orthop. 2018;89:190–196. doi: 10.1080/17453674.2018.1429108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vasdev A, Kumar S, Chadha G, Mandal SP. Fixed- versus mobile-bearing total knee arthroplasty in Indian patients. J Orthop Surg. 2009;17:179–182. doi: 10.1177/230949900901700211. [DOI] [PubMed] [Google Scholar]
- 119.Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H. Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop. 2005;29:179–181. doi: 10.1007/s00264-005-0646-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wohlrab D, Ditl J, Herrschelmann R, Schietsch U, Hein W, Hube R. Does the NexGen LPS flex mobile knee prosthesis offer advantages compared to the NexGen LPS?—a comparison of clinical and radiological results. Z Orthop Ihre Grenzgeb. 2005;143:567–572. doi: 10.1055/s-2005-836828. [DOI] [PubMed] [Google Scholar]
- 121.Woolson ST, Epstein NJ, Huddleston JI. Long-term comparison of mobile-bearing vs fixed-bearing total knee arthroplasty. J Arthroplasty. 2011;26:1219–1223. doi: 10.1016/j.arth.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 122.Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E. Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br. 2008;90:1172–1179. doi: 10.1302/0301-620X.90B9.21031. [DOI] [PubMed] [Google Scholar]
- 123.Zeng YM, Yan MN, Li HW, Zhang J, Wang Y. Does mobile-bearing have better flexion and axial rotation than fixed-bearing in total knee arthroplasty? A randomised controlled study based on gait. J Orthop Translat. 2020;20:86–93. doi: 10.1016/j.jot.2019.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.