Abstract
Aim:
To identify drug-related death trends associated with synthetic cannabinoid receptor agonists (SCRAs) reported to the National Programme on Substance Abuse Deaths (NPSAD) from England.
Design:
Case reports from NPSAD (England) where a SCRA was detected in post-mortem tissue(s) and/or implicated in the death were extracted, analyzed, and compared against non-SCRA-related deaths that occurred over the same time period (2012–2019).
Findings:
One hundred sixty-five death SCRA-related reports were extracted, with 18 different SCRAs detected. Following the first death in 2012, a subsequent sharp increase in reporting is evident. Acute SCRA use was the underlying cause of death in the majority of cases (75.8%) with cardiorespiratory complications the most frequently cited underlying physiological cause (13.4%). SCRA users were predominantly found dead (68.6%), with a large proportion of those witnessed becoming unresponsive described as suddenly collapsing (81.6%). Psychoactive polydrug use was detected in 90.3% of cases, with alcohol the most commonly co-detected (50.3%), followed by opioids (42.2%), benzodiazepines/Z-drugs (32.1%), stimulants (32.1%, [28.5% cocaine]), and cannabis (24.8%).
Compared to all non-SCRA-related NPSAD deaths occurring over the same time period, SCRA-related decedents were more predominantly male (90.3% vs. 72.0%; p<0.01), and lived in more deprived areas (p<0.01). While a comparatively significant proportion of decedents were homeless (19.4% vs. 4.1%), living in a hostel (13.3% vs. 2.3%) or in prison (4.9% vs. 0.2%) at time of death (all p<0.01), the greatest majority of SCRA-related decedents were living in private residential accommodations (57.6%).
Conclusions:
This is the largest dataset regarding SCRA-related mortalities reported to date. Reporting of SCRA-related deaths in England have increased considerably, with polydrug use a specific concern. Lack of effective deterrents to SCRA use under current UK legislation, compounded by limited knowledge regarding the physiological impacts of SCRA consumption and their interaction with other co-administered substances are contributory factors to the occurrence of SCRA-related mortalities in an increasingly deprived demographic.
Keywords: synthetic cannabinoid receptor agonist, spice, cannabinoid, drug-related death, substance abuse, novel psychoactive substance
Introduction
Synthetic cannabinoid receptor agonists (SCRAs) interact with endogenous cannabinoid receptors, the receptors that mediate the effects of the major active ingredient in cannabis, delta-9-tetrahydrocannabinol (THC).1 Acting as full agonists at the CB1 receptor, SCRAs possess greater potency in comparison to THC, which acts as a partial agonist at CB1/2 receptors.1–3
Commercial production of SCRAs targeting recreational users commenced in the United Kingdom in the mid-2000s.4,5 Marketed openly as “legal highs,” they were aimed at a niche middle class demographic of experimental users (“psychonauts”) interested in exploring recreational drug diversity.6 Although users preferred cannabis to SCRAs,7,8 the appeal of “legal high” SCRA use included that they were legal, did not appear on standard drug tests, and were readily available.9–14 Indeed, following the control of many SCRA compounds as Class B substances under the Misuse of Drugs Act (MDA) 1971 or their banning by the Psychoactive Substances Act (PSA) 2016, there was a subsequent decline in recreational use of SCRAs in the general population.15,16
However, significant use prevalence in some vulnerable subgroups, particularly homeless, and prison populations persisted,6,12–14,16–18 due to their widespread availability and difficulty in detecting analytically. SCRAs also appeal to these users as the strong intoxication they induce is cited to provide release from unbearable situations by enabling detachment from reality.16,19–21
The SCRA dose effect is unpredictable: the same dose can induce profound intoxication in some subjects, while remaining imperceivable in others.22,23 Repeated administrations may therefore induce sudden and unexpected intoxication, increasing risk of accidental overdose. Clinical features of illicit SCRA use is variable, ranging from an agitated delirium with hallucinations to a reduced level of consciousness, with cardiovascular features such as tachycardia and arrhythmias, vomiting, and dizziness.24 In recent years, increasing numbers of SCRA-related deaths have been reported globally.6,25–27 While there is considerable regional variation in detected SCRAs types in post-mortem tissue, a common mechanism in precipitating cardiovascular complications leading to death is evident.
In this article, we contribute to the growing evidence of the dangers of SCRA use by describing trends in SCRA-related deaths that have occurred in England. In addition to analysis of cause(s) of death and toxicological evidence, we also consider the evolving sociodemographics of SCRA-related decedents.
Methods
National Programme on Substance Abuse Deaths
National Programme on Substance Abuse Deaths (NPSAD) regularly receives voluntary reports from 88.0% of English coroners on deaths related to psychoactive drugs (Table 1).28 A death is referred to a Coroner if it has an unknown cause, is violent or unnatural, sudden, and unexplained, occurred during an operation or before the person came out of an anesthetic, or was potentially caused by an industrial disease or poisoning.29 Toxicology tests are requested, dependent upon individual case circumstances at the discretion of the Coroner.
Table 1.
Data Points Collected by National Programme on Substance Abuse Deaths
| Mandatory | Optional |
|---|---|
| Gender | Ethnicity |
| Date of birth | Living arrangementsa |
| Date of death | Employment status |
| Cause(s) of death | Usual addressa |
| Manner of death | Place of death |
| Toxicology reportb | Narrative of circumstances of death |
| Inquest conclusion date | Past social and medical histories |
| Coronial jurisdiction | Prescribing status |
Usual address and living arrangements were also available for all SCRA-related cases.
In some cases, toxicology reports are not available, for example, in cases where a prolonged hospital stay preceded death. Toxicology reports were available for all SCRA-related cases.
SCRA, synthetic cannabinoid receptor agonist.
The King's College London Biomedical & Health Sciences, Dentistry, Medicine and Natural & Mathematical Sciences Research Ethics Subcommittee confirmed (November 2020) that NPSAD does not require REC review as all subjects are deceased.
Case identification
A retrospective study design identified all SCRA-related cases reported from England by searching the entire NPSAD database (records received from 1997 to April 1, 2020) in the post-mortem drug fields for the numerical code assigned to the “synthetic cannabinoid” drug class.
Non-SCRA-related cases where death had occurred from 2012 onward, the year in which the first reported SCRA-related death occurred, were subsequently extracted to perform demographic comparisons with SCRA-related cases (records received January 1, 2012, to April 1, 2020) by identifying cases where the “synthetic cannabinoid” drug class coding was absent from the post-mortem drug fields.
Data analysis
Software
Data analysis and statistics (Student's t-test and Chi square) were performed using IBM® SPSS™ Statistics for Windows version 25 and Microsoft Excel 365.
2019 Projection
The average time between death and coronial inquest conclusion where an SCRA was present is ∼7 months. Further deaths occurring in 2019 are therefore anticipated to be reported to NPSAD. Based on jurisdiction reporting trends, the number of SCRA-related deaths expected to be received by NPSAD has been projected.
Cause of death
Circumstances that lead to death are categorized on the death certificate issued by the coroner, as follows:
Cause 1a: The immediate cause of death (and underlying if no 1b or 1c cited)
Cause 1b: Any disease/circumstance underlying Cause 1a
Cause 1c: Any disease/circumstance underlying Cause 1b
Cause 2: Any disease/circumstance that did not cause the death, but contributed in some way.
It is not a requirement for a Cause 1b, 1c, or 2 to be cited for all deaths.29 Immediate and underlying cause of death were identified using these criteria.
Presence at post-mortem indicates a person died with a drug in their system. Implicated drugs are those determined by the coroner and consulting pathologists as directly involved in causing the death.
Toxicological significance scores
A toxicological significance score for each SCRA-related case, in accordance to the methodology proposed by Elliott et al.,30 was assigned dependent upon the cited cause(s) of death and toxicological interpretation provided by the consulting pathologist.
Deprivation scores
The English Indices of Deprivation 2019 was used to obtain deprivation data.31
Results
One hundred sixty-five people died in England and were reported to NPSAD where an SCRA was detected in post-mortem tissue(s) and/or implicated in the death by April 1, 2020. It is clear that SCRA-related fatalities have been increasingly reported to NPSAD in recent years (Fig. 1). When normalized against total NPSAD reporting in England over the same time period, a proportional rise in the occurrence of SCRA-related deaths remains evident (data not shown).
FIG. 1.
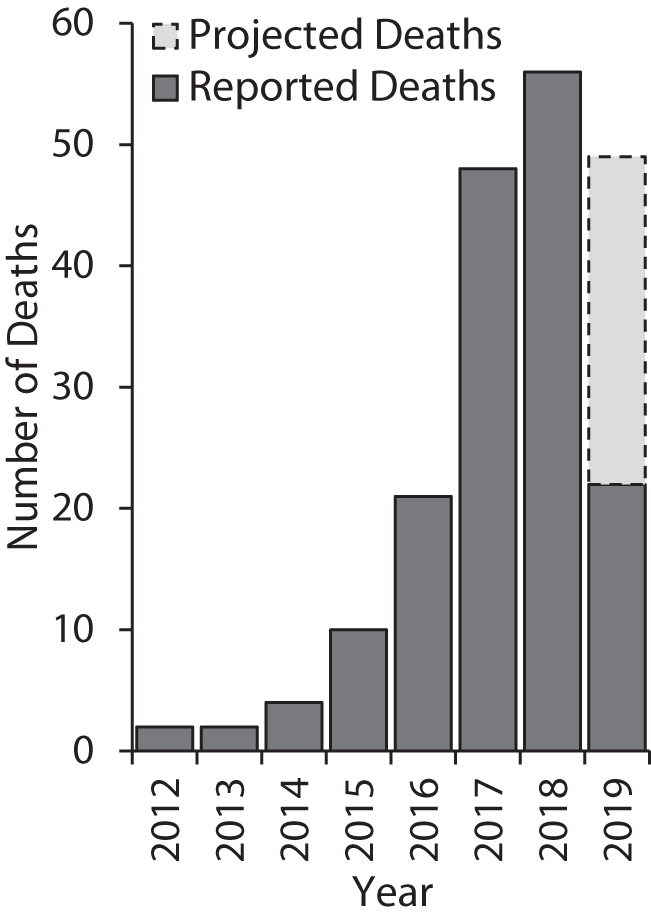
Deaths reported to NPSAD from England by April 1, 2020, where an SCRA was detected at post-mortem and/or implicated in causing the death. NPSAD, National Programme on Substance Abuse Deaths; SCRA, synthetic cannabinoid receptor agonist.
Types of SCRA detected
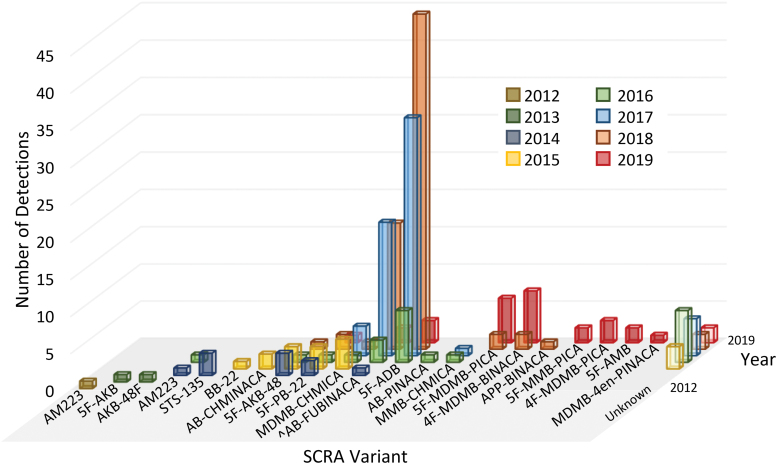
Eighteen different SCRAs were detected in submitted toxicology reports (Table 2). Multiple new SCRAs were detected almost every year since 2012, and there is a shifting pattern over time as to the most commonly detected SCRAs (Fig. 2).
Table 2.
Year During Which Each Synthetic Cannabinoid Receptor Agonist Type Was First Detected in Cases Reported to National Programme on Substance Abuse Deaths from England
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|
| AM2201 | 5F-AKB | 5F-PB-22 | BB-22 | 5F-ADB | 5F-MDMB-PICA | 5F-MMB-PICA | |
| AM223 | AKB-48F | 5F-AKB-48 | AB-CHMINACA | AB-PINACA | 4F-MDMB-BINACA | 4F-MDMB-PICA | |
| AKB-48 | MDMB-CHMICA | MMB-CHMICA | APP-BINACA | 5F-AMB | |||
| STS-135 | MDMB-4en-PINACA | ||||||
| AB-FUBINACAa |
AMB- and EMB-FUBINACA have not been separately classified from AB-FUBINACA as detectors have limited capability in differentiating between these compounds.62
FIG. 2.
SCRA types detected at post-mortem and/or implicated in causing death in cases reported to NPSAD from England. 5F-ADB and AB-FUBINACA detections have dominated in recent years, representing 40.6% and 18.9% of total detections, respectively. 2019 Data are for reported only (i.e., not projected) detections. Note that total detections sum to greater than the total number of SCRA-related cases as in some cases, multiple SCRA variants were detected: a total of 217 SCRA detections were made across the 165 reported cases. ^AB-FUBINACA also includes figures for AMB- and EMB-FUBINACA and their metabolites as detectors have limited capability in differentiating between these compounds.62 Color images are available online.
Cause of death
While physiological system failures were cited as the immediate cause of death in 32.7% of cases (n=54/165; 23.6% of which were cardiorespiratory), acute drug use was most often cited by the coroner as the underlying cause, with SCRA use cited in majority of cases (Table 3). When taking into account all causes of death (Causes 1a–c and Cause 2), a toxicological significance score of 3,30 which denotes that the SCRA was cited as a cause of death or likely to have contributed to toxicity/death, even in the presence of other drugs, was applicable in 85.5% of cases (n=141/165). A toxicology significance score of 2, which denotes that the SCRA may have contributed to toxicity/death, but other drugs present may be more toxicologically significant, was applicable in 27.9% of cases (n=23/165), with the remaining case assigned a score of 1, denoting an alternative cause of death (in this case, a traumatic external environmental factor). Qualitative analysis of cases with narratives provided (n=121/165) revealed that SCRA users were found dead in 68.6% of cases (n=83/121). Where the decedent was witnessed becoming unresponsive (31.4% of cases; n=38/121), the majority were described as having suddenly collapsed (81.6%; n=31/38).
Table 3.
Immediate and Underlying Causes of Death Listed on Death Certificates of Synthetic Cannabinoid Receptor Agonist-Related Decedents in Cases Reported to National Programme on Substance Abuse Deaths from England
| Cause | Immediate cause |
Underlying cause |
|---|---|---|
| % of Decedents (n) | % of Decedents (n) | |
| Acute drug use | 67.3 (111) | 87.9 (145) |
| Implicating SCRA(s) | 57.6 (95) | 75.8 (125) |
| Not implicating SCRA(s) | 9.7 (16) | 12.1 (20) |
| Physiological system | 32.7 (54) | 12.1 (20) |
| Cardiac | 10.3 (17) | 7.3 (12) |
| Respiratory | 13.3 (22) | 6.1 (10) |
| Neurological | 9.1 (15) | 3.6 (6) |
| Hepatic | 1.2 (2) | 1.8 (3) |
| Mental health | 0.6 (1) | 0.6 (1) |
| Gastrointestinal | 0.6 (1) | — |
| Trauma | — | — |
| Other | 3.0 (5) | 3.0 (5) |
As more than one immediate and/or underlying cause of death was cited in some cases, these will add to greater than the total number of deaths.
A single SCRA was detected by toxicology in 126 cases, with multiple SCRA co-administration detected in 39 cases: the most common combination was 5F-ADB and AB-FUBINACA (n=24/165). Alcohol was the most commonly co-detected substance (50.3% of cases; n=83/165; cases where alcohol was attributed to likely post-mortem production by the pathologist [≤10 mg/dL]32 were excluded). In 80.1% of these cases (n=67/83), the blood alcohol of decedents was over 50 mg/dL, with 48.2% at a blood alcohol level between 50 and 199 mg/dL (n=40/83), and 31.3% over 200 mg/dL (n=27/83). Polydrug use of legal prescription and/or illicit substances was detected in 90.3% of cases (n=149/165). An increasing trend in polydrug administration is evident, with the average number of co-administered substances in 2012–2016 (mean 3.6) significantly lower compared with 2018 (mean 5.6; p<0.01) and 2019 (mean 5.7; p<0.01). In 42.2% of cases (n=70/165), SCRA(s) were detected with at least one opioid, and in 32.1% of cases (n=53/165) with at least one benzodiazepine/Z-drug, with an overlap of 42 cases where both opioid(s) and benzodiazepine/Z-drug(s) were co-detected (25.5% of cases). Excluding SCRAs themselves, there were 124 detections of other illicit substances from 84 decedents (49.7% of cases); most notably, 53 decedents (32.1% of cases) had co-administered stimulants (47 of which included cocaine [28.5% of cases]) and 41 cannabis (24.8% of cases). A high proportion of decedents was known to use drugs (57.0%; n=94/165). Medications available by UK prescription were detected in 64.8% of cases (n=107/165). Where prescribing history was provided, 54.9% of cases (n=50/91) were prescribed drugs that are directly psychoactive. Antidepressants were the most commonly prescribed (41.8%; n=38/91) followed by opioids (18.7%; n=17/91), antipsychotics (15.4%; n=14/91), gabapentinoids (12.1%; n=11/91), and benzodiazepines/Z-drugs (9.9%; n=9/91).
Demographics
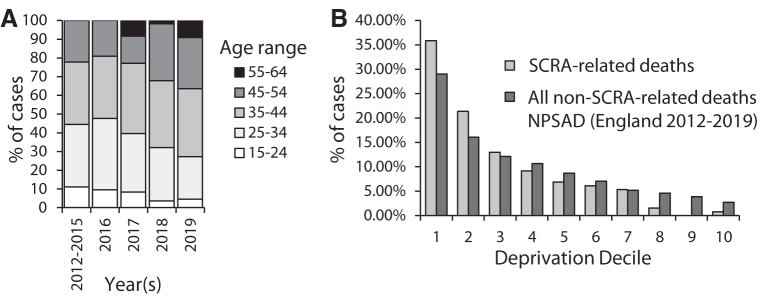
The proportion of male SCRA-related decedents is significantly higher than that observed for all non-SCRA-related deaths reported to NPSAD from England over the same time period (p<0.01) (Table 4), concording with the proportion reported (88%) in a recent global systematic review.25 While the age of SCRA-related decedents is not significantly different to the non-SCRA-related deaths, those who died in 2012–2015 (mean age 34.5±10.3) when compared to those who died in 2018–2019 (mean age 40.0±8.9) were significantly younger (p<0.05) (Fig. 3A).
Table 4.
Age, Gender, and Usual Living Circumstances of Synthetic Cannabinoid Receptor Agonist-Related Decedents in Cases Reported to National Programme on Substance Abuse Deaths from England
| Age and gender | % SCRA-related deaths (n) | % All non-SCRA-related NPSAD cases (England 2012–2019) |
|---|---|---|
| Men | 90.3 (149) | 72.0 |
| Women | 9.7 (16) | 28.0 |
| Mean age (±SD) | 38.41±9.40 | 40.11±13.73 |
| Usual living circumstances | ||
| Private residential | 57.6 (95) | 80.9 |
| Hostel | 13.3 (22) | 2.3 |
| Homeless | 19.4 (32) | 4.1 |
| Prison | 4.9 (8) | 0.2 |
| Unknown | — | 11.3 |
| Othera | 4.9 (8) | 1.3 |
Complementary data for all non-SCRA-related cases submitted to NPSAD from England within the same time period have been provided for comparison.
Rehab, hospital, hotel, nursing home, boat, caravan, shed, workplace.
NPSAD, National Programme on Substance Abuse Deaths; SD, standard deviation.
FIG. 3.
(A) Percentage of cases by age range per year of SCRA-related decedents reported to NPSAD from England. Decedent numbers for 2012–2015 have been summed due to low figures for these years. (B) Deprivation decile by postcode of usual address of SCRA-related decedents and all non-SCRA-related decedents reported to NPSAD from England 2012–2019. A ranking within the first decile represents the most deprived areas in England, while a ranking within the tenth decile represents the least deprived areas. These rankings are based upon assessment of income, employment, education, health and disability, crime, barriers to housing and services, and living environment statistics.30 Homeless decedents were excluded from this analysis by default due to lack of a usual address (n=32), as were those whose usual address was outside England (n=2).
The proportion of SCRA-related decedents living in private housing accommodation is significantly lower than for the non-SCRA-related deaths reported (p<0.01), while the proportions of those living in a hostel or prison, or homeless are significantly higher (all p<0.01) (Table 4). The usual address of SCRA-related decedents was on average located in one of the most deprived areas of England (decile score 1–3) (Fig. 3B). Furthermore, when compared to the usual addresses of decedents for the non-SCRA-related deaths, SCRA-related decedents were significantly more likely to have been living in the more deprived areas (p<0.01) (Fig. 3B). Just 18.5% of SCRA-related deaths occurring in 2012–2015 were of people living in the least deprived areas of England (deciles 6–10; n=5/27), despite those who died in this time period accounting for only 10.9% of total SCRA-related deaths (n=18/165).
Discussion
SCRAs have consistently ranked as one of the largest groups of novel psychoactive substances on the European drug market.5 While SCRA use prevalence among the general population has declined in recent years,33 the number of SCRA-related deaths reported from England to NPSAD has concomitantly risen, in line with estimated SCRA use prevalence.34 This dataset is the largest reported to date, exceeding the total number of cases included in a recent global systematic review.25
Heterogeneous in harm
The Welsh Emerging Drugs and Identification of Novel Substances (WEDINOS) laboratory, the UK's only year-round drug submission and testing facility, detected illicit SCRAs in 6.25% of submissions received from January 2017 to December 201935; 43.2% were 5F-ADB, 22.8% 4F-MDMB-BINACA, and 18.9% AB-FUBINACA. While the proportions of deaths where 5F-ADB and AB-FUBINACA were detected in cases reported to NPSAD are reflected by their frequency of WEDINOS detections, the proportion of deaths in which 4F-MDMB-BINACA was detected is markedly lower (4.1% of SCRA-related death reports). It has been suggested that some SCRAs possess lower toxicities, potentially accounting for discrepancies between their use prevalence estimations and incidences of mortality.36 Indeed, while 30% of test purchases were positive for the SCRA cumyl-PEGACLONE in a recent German study, only one case was reported where cumyl-PEGACLONE was implicated in causing death, and even then, this was in combination with other SCRAs (5F-ADB and 5F-MDMB-P7AICA) and underlying health conditions.37 Cumyl-PEGACLONE was first detected in the United Kingdom in 2016,38 but no death involving Cumyl-PEGACLONE was reported to NPSAD at the time of writing. Some SCRA users possess “inverted expertise” demonstrating awareness of such trends, often earlier and to a greater extent than the support services trying to help them.39 Engaging SCRA users to combine their knowledge with available data is required to provide an up-to-date evidence base for health care professionals to provide effective treatments and interventions.
Isolated use is an SCRA-specific risk
Underlying cause of death was majority attributed to acute drug abuse by coroners, with SCRAs implicated in most cases. As a large proportion of SCRA users become unresponsive in isolation,16,25 contrary to other recreational drug taking behaviors,40 unwitnessed overdose represents a significant SCRA-specific risk. Greater awareness of the risk of lone SCRA use is therefore needed among both SCRA users and their associates.
Intervention opportunities by health care professionals to treat SCRA toxicity are consequentially limited. This is further exacerbated by misidentification of SCRA users presenting with drug toxicity: a recent study found only 55.5% of patients presenting with SCRA intoxication had detectable SCRAs on analytical testing, suggesting that clinicians often misattribute effects of other drugs or medical conditions to SCRA use.41 Tools to identify individuals presenting with SCRA toxicity are needed to best provide treatment.
Lack of effective UK legislation
The shifting pattern in detected SCRAs cannot be attributed to prohibitive UK legislations: neither MDA amendments introduced in 2009, 2013, and 2016 controlling some SCRAs nor their generic ban under PSA (2016) correlate with changes in the most commonly detected SCRAs year-on-year. Rather, it is likely due to legislative changes in China, where a large proportion of SCRAs are thought to be manufactured.18 The control of eight SCRAs, including 5F-ADB and AB-FUBINACA, by the State Council of China in August 2018 correlates with the shift away from these SCRAs being the most dominantly detected by both NPSAD and WEDINOS,35 and toward newer generation SCRAs such as 4F-MDMB-BINACA and 5F-MDMB-PICA. A similar situation has been reported in Germany, where implementation of their law on NPS (the NpSG: Neue-psychoaktive-Stoffe-Gesetz), a prohibitive policy based upon the structural features of SCRAs, had limited effect on the availability of 5F-ADB and its use, whereas introduction of the 5F-ADB ban in China did indeed correlate with a reduction in 5F-ADB availability and use prevalence in Germany.42 SCRA-related deaths in England are not projected to dramatically decrease, indicating need for alternate interventions. A ban citing commonly used names for SCRA preparations (e.g., “Spice” and “Mamba”) as opposed to specific SCRA molecular structural variants may prove more effective, as was observed in Australia.43
From “herbal highs” to the “heroin of cannabis”
The reputation of SCRAs has evolved: online “psychonaut” discussion forums that originally encouraged SCRA use now act as deterrents.44 This is reflected in the evolving demographic presented in this study, with those dying in 2012–2015 younger and, on average, living in less deprived areas than those who died from 2016 onward. This demographic shift may indicate effectiveness of the 2016 PSA in deterring SCRA use in younger individuals living in less deprived areas.15,16
It is well documented that SCRAs are increasingly problematic in homeless and prison populations.4,14,21,45 However, these data indicate that a greater proportion of decedents were living in private residential accommodation at the time of death, although in socioeconomically deprived areas. This needs serious consideration in the design of targeted strategies addressing SCRA use, which currently focus on homeless and prison populations.46,47 Furthermore, as almost half of the decedents were known to misuse drugs, health care and other supporting professionals should be routinely inquiring about SCRAs in polysubstance users and informing them about SCRA-specific risks.
Knowledge of SCRA-disease/drug interactions is scarce
Cardiorespiratory complications were cited as immediate causes of death in a marked proportion of cases, complementing findings in a recent systematic review,25 and correlating with circumstance of sudden collapse. While SCRA cardiotoxicity is an established concern,24,48 the mechanisms of SCRA-mediated cardiorespiratory failure are poorly understood.49,50 Furthermore, the cardiorespiratory effects of SCRAs in combination with other cardiotoxic (e.g., stimulant) and/or cardiorespiratory depressant (e.g., opiate) substances are poorly characterized and represent an urgent area of enquiry. Such research is required to recommend effective interventions, for example, as to whether cardiac QT interval monitoring in SCRA users attending drug services should be undertaken, as is suggested for those prescribed methadone, who also use crack cocaine.51
While the number of substances detected by toxicology in SCRA-related decedents increased from 2012 to 2019, evidence for SCRA drug-drug interactions remains scarce. Studies indicate that some SCRA types interact with cytochrome P450 pathways, which may alter the pharmacodynamics of other co-administered substances, leading to adverse events.52–61 However, these studies used older SCRA types, which differ substantially in terms of molecular structure to those currently prevalently used.35 Indeed, only 4 SCRAs for which this metabolism data are available were detected in cases reported to NPSAD (AB-CHIMINACA, AKB-48, AM2201, and STS-135), and account for just 9 of the 217 SCRA detections. This noticeable absence of in vivo human investigations of SCRA pharmacodynamics is likely due, in part, to insufficient toxicity data making human administration studies unfeasible and the absence of on-site toxicology in clinical settings in the UK limiting observational data linking patient presentations to specific SCRAs. This is in contrast to other cannabinoid-based drugs, including illicit cannabis, for which drug interaction data are easily accessible.62 Further research into potential SCRA drug-drug interactions is needed to better understand potential adverse events and advise SCRA users of harmful interactions that may occur with co-administered illicit or prescription medications.
SCRA users display high rates of polydrug use,10 concording with patterns observed in other illicit drug users.40 However, the proportion of SCRA-related decedents who were known to use drugs reported to NPSAD is near twofold of that reported in a recent global systematic review.25 Furthermore, the proportions of decedents reported to NPSAD co-administering opioids, benzodiazepines/Z-drugs, stimulants, and alcohol consistently outstrip those observed in the review.25 Of particular concern is the mortality rate associated with opioid-SCRA co-administration, as this is 10-fold higher than the rate reported in living users.63 Whether this represents an increased mortality risk associated with opioid-SCRA co-intoxication is unclear. A need for understanding risks conferred by patterns of substance misuse, including SCRAs, appears to be important in the UK context.
Limitations
As detection methods for SCRAs have advanced64,65 and SCRA toxicology testing requests have become more frequent,17 part of the increase in NPSAD reporting is potentially an artifact of improved SCRA detection. However, as standard toxicology screens to do not include SCRAs,66 and there are limitations in detecting SCRAs,64,67 SCRA-related deaths are likely underdetected. Advancements in SCRA detection methods are therefore needed to address the current shortcomings in SCRA toxicological analysis. Furthermore, as NPSAD receives voluntary reports and coronial investigations are not carried out for all deaths, the figures presented in this study almost certainly underrepresent the true number of SCRA-related deaths occurring in England. Greater awareness of the limitations in SCRA-related death reporting is also needed, at both local authority and national drug policy levels, in order for appropriate measures to address the true scale of SCRA-related mortality to be identified and implemented to achieve SCRA-related harm reduction.
How SCRAs cause death is also unclear, especially given their high rate of polydrug co-administration.10 Coroners have limited information on SCRA toxicity upon which to base conclusions,66 and may be implicating SCRAs due to their notoriety.4,8,14
Conclusions
Despite a reduction in overall use prevalence,15,16 deaths attributable to SCRA consumption prevail in deprived demographics. Lack of effective deterrents to SCRA use under current UK legislation, compounded by limited knowledge as to the physiological impacts of SCRA consumption and their interaction with other co-administered substances, can be identified as likely contributory factors to instances of SCRA-related mortality. New legislative, health care, and substance use service approaches are required to reduce SCRA-related harms in the broader deprived demographic identified in this study. Increasing pre-clinical research and effective clinical assessment and engagement of SCRA users will substantiate the knowledge base required to achieve these aims.
Acknowledgments
The authors would like to thank Christine Goodair for her ongoing advice and support as NPSAD Programme Manager. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Abbreviations Used
- MDA
Misuse of Drugs Act
- NPSAD
National Programme on Substance Abuse Deaths
- PSA
Psychoactive Substances Act
- SCRA
synthetic cannabinoid receptor agonist
- SD
standard deviation
- THC
delta-9-tetrahydrocannabinol
- WEDINOS
Welsh Emerging Drugs and Identification of Novel Substances
Author Disclosure Statement
No competing financial interests exist.
Funding Information
All work was funded as part of the usual employment of the authors in their respective institutions. No special funding sources are reported.
Cite this article as: Yoganathan P, Claridge H, Chester L, Englund A, Kalk NJ, Copeland CS (2022) Synthetic cannabinoid-related deaths in England, 2012–2019, Cannabis and Cannabinoid Research 7:4, 516–525, DOI: 10.1089/can.2020.0161.
References
- 1. Akram H, Mokrysz C, Curran HV. What are the psychological effects of using synthetic cannabinoids? A systematic review. J Psychopharmacol. 2019;33:271–283. [DOI] [PubMed] [Google Scholar]
- 2. Atwood BK, Lee D, Straiker A, et al. CP47,497-C8 and JWH073, commonly found in ‘Spice’ herbal blends, are potent and efficacious CB(1) cannabinoid receptor agonists. Eur J Pharmacol. 2011;659:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ligresti A, De Petrocellis L, Di Marzo V. From phytocannabinoids to cannabinoid receptors and endocannabinoids: pleiotropic physiological and pathological roles through complex pharmacology. Physiol Rev. 2016;96:1593–1659. [DOI] [PubMed] [Google Scholar]
- 4. White CM. The pharmacologic and clinical effects of illicit synthetic cannabinoids. J Clin Pharmacol. 2017;57:297–304. [DOI] [PubMed] [Google Scholar]
- 5. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). Fentanils and synthetic cannabinoids: driving greater complexity into the drug situation. An update from the EU Early Warning System. European Union: Luxembourg, 2018. [Google Scholar]
- 6. Peacock A, Bruno R, Gisev N, et al. New psychoactive substances: challenges for drug surveillance, control, and public health responses. Lancet. 2019;394:1668–1684. [DOI] [PubMed] [Google Scholar]
- 7. Smith KE, Staton M. Synthetic cannabinoid use among a sample of individuals enrolled in community-based recovery programs: are synthetic cannabinoids actually preferred to other drugs? Subst Abus. 2019;40:160–169. [DOI] [PubMed] [Google Scholar]
- 8. Castaneto MS, Gorelick DA, Desrosiers NA, et al. Synthetic cannabinoids: epidemiology, pharmacodynamics, and clinical implications. Drug Alcohol Depend. 2014;144:12–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mathews EM, Jeffries E, Hsieh C, et al. Synthetic cannabinoid use among college students. Addict Behav. 2019;93:219–224. [DOI] [PubMed] [Google Scholar]
- 10. Bonar EE, Ashrafioun L, Ilgen MA. Synthetic cannabinoid use among patients in residential substance use disorder treatment: prevalence, motives, and correlates. Drug Alcohol Depend. 2014;143:268–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gunderson EW, Haughey HM, Ait-Daoud N, et al. A survey of synthetic cannabinoid consumption by current cannabis users. Subst Abus. 2014;35:184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brunt TM, Atkinson AM, Nefau T, et al. Online test purchased new psychoactive substances in 5 different European countries: a snapshot study of chemical composition and price. Int J Drug Policy. 2017;44:105–114. [DOI] [PubMed] [Google Scholar]
- 13. Scourfield A, Flick C, Ross J, et al. Synthetic cannabinoid availability on darknet drug markets—changes during 2016–2017. Toxicol Commun. 2019;3:7–15. [Google Scholar]
- 14. Weinstein AM, Rosca P, Fattore L, et al. Synthetic cathinone and cannabinoid designer drugs pose a major risk for public health. Front Psychiatry. 2017;8:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Crime Survey for England and Wales (CSEW). Drugs Misuse: findings from the 2018/19 Crime Survey for England and Wales. Statistical Bulletin: 21/19. Home Office: London, 2019. [Google Scholar]
- 16. Blackman S, Bradley R. From niche to stigma-Headshops to prison: exploring the rise and fall of synthetic cannabinoid use among young adults. Int J Drug Policy. 2017;40:70–77. [DOI] [PubMed] [Google Scholar]
- 17. Ford LT, Berg JD. Analytical evidence to show letters impregnated with novel psychoactive substances are a means of getting drugs to inmates within the UK prison service. Ann Clin Biochem. 2018;55:673–678. [DOI] [PubMed] [Google Scholar]
- 18. Norman C, Walker G, McKirdy B, et al. Detection and quantitation of synthetic cannabinoid receptor agonists in infused papers from prisons in a constantly evolving illicit market. Drug Test Anal. 2020;12:538–554. [DOI] [PubMed] [Google Scholar]
- 19. Ellsworth J. Spice, vulnerability, and victimization: synthetic cannabinoids and interpersonal crime victimization among homeless adults. Subst Abus. 2019;7:1–7. [DOI] [PubMed] [Google Scholar]
- 20. Csák R, Szécsi J, Kassai S, et al. New psychoactive substance use as a survival strategy in rural marginalised communities in Hungary. Int J Drug Policy. 2020;85:102639. [DOI] [PubMed] [Google Scholar]
- 21. Gray P, Ralphs R, Williams L. The use of synthetic cannabinoid receptor agonists (SCRAs) within the homeless population: motivations, harms and the implications for developing an appropriate response. Addict Res Theory. 2020;29:1–10. [Google Scholar]
- 22. Theunissen EL, Hutten N, Mason NL, et al. Neurocognition and subjective experience following acute doses of the synthetic cannabinoid JWH-018: a phase 1, placebo-controlled, pilot study. Br J Pharmacol. 2018;175:18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Theunissen EL, Hutten N, Mason NL, et al. Neurocognition and subjective experience following acute doses of the synthetic cannabinoid JWH-018: responders versus nonresponders. Cannabis Cannabinoid Res. 2019;4:51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Waugh J, Najafi J, Hawkins L, et al. Epidemiology and clinical features of toxicity following recreational use of synthetic cannabinoid receptor agonists: a report from the United Kingdom National Poisons Information Service. Clin Toxicol (Phila). 2016;54:512–518. [DOI] [PubMed] [Google Scholar]
- 25. Giorgetti A, Busardò FP, Tittarelli R, et al. Post-mortem toxicology: a systematic review of death cases involving synthetic cannabinoid receptor agonists. Front Psychiatry. 2020;11:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Darke S, Duflou J, Farrell M, et al. Characteristics and circumstances of synthetic cannabinoid-related death. Clin Toxicol (Phila). 2020;58:368–374. [DOI] [PubMed] [Google Scholar]
- 27. Morrow PL, Stables S, Kesha K, et al. An outbreak of deaths associated with AMB-FUBINACA in Auckland NZ. EClinicalMedicine. 2020;25:100460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Claridge H, Williams BD, Copeland CS. A deadly trend in fentanyl fatalities (England, 1998–2017). Br J Clin Pharmacol. 2020;86:437–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gov.uk. When a death is reported to a coroner. 2020. https://www.gov.uk/after-a-death/when-a-death-is-reported-to-a-coroner Accessed September 7, 2020.
- 30. Elliott S, Sedefov R, Evans-Brown M. Assessing the toxicological significance of new psychoactive substances in fatalities. Drug Test Anal. 2018;10:120–126. [DOI] [PubMed] [Google Scholar]
- 31. Ministry of Housing, Communities & Local Government. English indicies of deprivation 2019. 2019. http://imd-by-postcode.opendatacommunities.org/imd/2019 Accessed September 7, 2020.
- 32. O'Neal CL, Poklis A. Postmortem production of ethanol and factors that influence interpretation: a critical review. Am J Forensic Med Pathol. 1996;17:8–20. [DOI] [PubMed] [Google Scholar]
- 33. Global Drugs Survey 2018. https://www.globaldrugsurvey.com/gds-2018/ Accessed September 7, 2020.
- 34. Webb NE, Wood DM, Greene SL, et al. Change in the new psychoactive substances associated with Emergency Department acute toxicity presentations associated with the introduction of the UK 2016 Psychoactive Substances Act. Clin Toxicol (Phila). 2019;57:36–41. [DOI] [PubMed] [Google Scholar]
- 35. Welsh Emerging Drugs and Identification of Novel Substances (WEDINOS). Welsh Emerging Drugs and Identification of Novel Substances Project. 2020. wedinos.org Accessed September 7, 2020.
- 36. De Luca MA, Fattore L. Therapeutic use of synthetic cannabinoids: still an open issue? Clin Ther. 2018;40:1457–1466. [DOI] [PubMed] [Google Scholar]
- 37. Halter S, Angerer V, Rohrich J, et al. Cumyl-PEGACLONE: a comparatively safe new synthetic cannabinoid receptor agonist entering the NPS market? Drug Test Anal. 2019;11:347–349. [DOI] [PubMed] [Google Scholar]
- 38. Sharp P, Hudson S, Hikin L, et al. The changing pattern of synthetic cannabinoid use within England, April 2014 to March 2018. Med Sci Law. 2019;59:180–186. [DOI] [PubMed] [Google Scholar]
- 39. Gates PJ, Sabioni P, Copeland J, et al. Psychosocial interventions for cannabis use disorder. Cochrane Database Syst Rev. 2016;5:CD005336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hickman M, Carrivick S, Paterson S, et al. London audit of drug-related overdose deaths: characteristics and typology, and implications for prevention and monitoring. Addiction. 2007;102:317–323. [DOI] [PubMed] [Google Scholar]
- 41. Tebo C, Mazer-Amirshahi M, DeGeorge L, et al. Suspected synthetic cannabinoid receptor agonist intoxication: does analysis of samples reflect the presence of suspected agents? Am J Emerg Med. 2019;37:1846–1849. [DOI] [PubMed] [Google Scholar]
- 42. Halter S, Haschimi B, Mogler L, et al. Impact of legislation on NPS markets in Germany—the rise and fall of 5F-ADB. Drug Test Anal. 2020;12:853–856. [DOI] [PubMed] [Google Scholar]
- 43. Cairns R, Brown JA, Gunja N, et al. The impact of Australian legislative changes on synthetic cannabinoid exposures reported to the New South Wales Poisons Information Centre. Int J Drug Policy. 2017;43:74–82. [DOI] [PubMed] [Google Scholar]
- 44. Bilgrei OR. From “herbal highs” to the “heroin of cannabis”: exploring the evolving discourse on synthetic cannabinoid use in a Norwegian Internet drug forum. Int J Drug Policy. 2016;29:1–8. [DOI] [PubMed] [Google Scholar]
- 45. Ralphs R, Williams L, Askew R, et al. Adding Spice to the Porridge: the development of a synthetic cannabinoid market in an English prison. Int J Drug Policy. 2017;40:57–69. [DOI] [PubMed] [Google Scholar]
- 46. Advisory Council on the Misuse of Drugs. Drug related harms in homesless populations and how they can be reduced. Home Office, 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/810284/Drug-related_harms_in_homeless_populations.pdf Accessed September 7, 2020.
- 47. United Kingdom Focal Point on Drugs. United Kingdom drug situation 2017. 2017. https://www.gov.uk/government/publications/united-kingdom-drug-situation-focal-point-annual-report Accessed September 7, 2020.
- 48. Hancox JC, Kalk NJ, Henderson G. Synthetic cannabinoids and potential cardiac arrhythmia risk: an important message for drug users. Ther Adv Drug Saf. 2020;11:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Pertwee RG. Receptors and channels targeted by synthetic cannabinoid receptor agonists and antagonists. Curr Med Chem. 2010;17:1360–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Alon MH, Saint-Fleur MO. Synthetic cannabinoid induced acute respiratory depression: case series and literature review. Respir Med Case Rep. 2017;22:137–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mayet S, Gossop M, Lintzeris N, et al. Methadone maintenance, QTc and torsade de pointes: who needs an electrocardiogram and what is the prevalence of QTc prolongation? Drug Alcohol Rev. 2011;30:388–396. [DOI] [PubMed] [Google Scholar]
- 52. Chimalakonda K, Seely K, Bratton S, et al. Cytochrome P450-mediated oxidative metabolism of abused synthetic cannabinoids found in K2/Spice: identification of novel cannabinoid receptor ligands. Drug Met Dispos. 2012;40:2174–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Patton AL, Seely KA, Yarbrough AL, et al. Altered metabolism of synthetic cannabinoid JWH-018 by human cytochrome P450 2C9 and variants. Biochem Biophys Res Commun. 2018;498:597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nielsen LM, Holm NB, Olsen L, et al. Cytochrome P450-mediated metabolism of the synthetic cannabinoids UR-144 and XLR-11. Drug Test Anal. 2016;8:792–800. [DOI] [PubMed] [Google Scholar]
- 55. Ashino T, Hakukawa K, Itoh Y, et al. Inhibitory effect of synthetic cannabinoids on CYP1A activity in mouse liver microsomes. J Toxicol Sci. 2014;39:815–820. [DOI] [PubMed] [Google Scholar]
- 56. Chimalakonda KC, James LP, Radominska-Pandya A, et al. Sulfaphenazole and α-naphthoflavone attenuate the metabolism of the synthetic cannabinoids JWH-018 and AM2201 found in K2/spice. Drug Metab Lett. 2013;7:34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Erratico C, Negreira N, Norouzizadeh H, et al. In vitro and in vivo human metabolism of the synthetic cannabinoid AB-CHMINACA. Drug Test Anal. 2015;7:866–876. [DOI] [PubMed] [Google Scholar]
- 58. Holm NB, Nielsen LM, Linnet K. CYP3A4 mediates oxidative metabolism of the synthetic cannabinoid AKB-48. AAPS J. 2015;17:1237–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Holm NB, Noble C, Linnet K. JWH-018 ω-OH, a shared hydroxy metabolite of the two synthetic cannabinoids JWH-018 and AM-2201, undergoes oxidation by alcohol dehydrogenase and aldehyde dehydrogenase enzymes in vitro forming the carboxylic acid metabolite. Toxicol Lett. 2016;259:35–43. [DOI] [PubMed] [Google Scholar]
- 60. Jones S, Yarbrough AL, Fantegrossi WE, et al. Identifying cytochrome P450s involved in oxidative metabolism of synthetic cannabinoid N-(adamantan-1-yl)-1-(5-fluoropentyl)-1H-indole-3-carboxamide (STS-135). Pharmacol Res Perspect. 2020;8:e00561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kim S, Choi WG, Kwon M, et al. In vitro inhibitory effects of APINACA on human major cytochrome P450, UDP-glucuronosyltransferase enzymes, and drug transporters. Molecules. 2019;24:3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Baxter K, Preston C. Stockley's drug interactions. Pharmaceutical Press, London. [Google Scholar]
- 63. Winstock AR, Barratt MJ. Synthetic cannabis: a comparison of patterns of use and effect profile with natural cannabis in a large global sample. Drug Alcohol Depend. 2013;131:106–111. [DOI] [PubMed] [Google Scholar]
- 64. May B, Naqi HA, Tipping M, et al. Synthetic cannabinoid receptor agonists detection using fluorescence spectral fingerprinting. Anal Chem. 2019;91:12971–12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Segawa H, Fukuoka T, Itoh T, et al. Rapid detection of synthetic cannabinoids in herbal highs using surface-enhanced Raman scattering produced by gold nanoparticle co-aggregation in a wet system. Analyst. 2019;144:6928–6935. [DOI] [PubMed] [Google Scholar]
- 66. Labay LM, Caruso JL, Gilson TP, et al. Synthetic cannabinoid drug use as a cause or contributory cause of death. Forensic Sci Int. 2016;260:31–39. [DOI] [PubMed] [Google Scholar]
- 67. Schaefer N, Kröll A, Körbel C, et al. Time- and temperature-dependent postmortem concentration changes of the (synthetic) cannabinoids JWH-210, RCS-4, as well as Δ9-tetrahydrocannabinol following pulmonary administration to pigs. Arch Toxicol. 2020;94:1585–1599. [DOI] [PMC free article] [PubMed] [Google Scholar]