Summary
Background
Differences in survival between groups may reflect avoidable and modifiable inequalities. This study examines the 35-year mortality risk for adults aged 25–44 years in the mid-1980s with disability due to vision, hearing, or motor impairment; physical illness; or mental health problems.
Methods
This Norwegian study was based on data from the Trøndelag Health Study (HUNT1, 1984–86, and HUNT2, 1995–97) linked to tax-registry data for deaths before 15 November 2019. Mortality risk was estimated by Cox regression analysis adjusted for age and sex. Sensitivity analysis included the following possible mediators: education, work, living situation, body mass index, systolic blood pressure and smoking.
Findings
Of the 30,080 HUNT1 participants aged 25–44 years, 5071 (16.9%) reported having disability. During the 35 years of follow-up, 1069 (21.1%) participants with disability and 3107 (12.4%) without disability died. Individuals with any type of disability had 62% higher mortality risk compared to those without a disability, adjusted by age and sex. The highest mortality risks were observed for disability due to severe motor impairment (HR=3.67, 95%CI=2.89–4.67) and severe mental health problems (HR=3.40, 95%CI=2.75–4.23) compared to those without these disabilities. Increased mortality risk was found for all the included disability types. The associations were somewhat mediated, especially by education, work and living situation.
Interpretation
This study shows that among adults aged 25–44 years, the risk of death increases with disability of different types and severity levels, particularly for disability related to mental health problems or motor impairment.
Funding
None.
Keywords: Mortality risk, Disability, Vision impairment, Hearing impairment, Motor impairment, Physical illness, Mental health problems
Research in context.
Evidence before this study
Up until 12 March 2020, literature searches were conducted using PubMed, MEDLINE, EMBASE, PsycINFO, AgeLine, CINAHL, NORART, SweMed and Google Scholar. Several relevant terms were used including ‘disability’, ‘impairment’, ‘adulthood’, ‘ageing’, ‘aging’, ‘mortality’, ‘life expectancy’, ‘survival’, ‘vision’, ‘hearing’, ‘mental health’, ‘mobility’, ‘motor’, ‘physical illness’, and ‘population-based’. The searches were later updated to include publications between 12 March 2020 and 11 April 2022. Most of the retrieved studies included samples of older populations. Few studies had investigated survival associated with long-term disability for adults ages 25-44 years indicating higher mortality risk.
Added value of this study
A novelty of the present study is that it investigates mortality risk among adults of working age who have a disability using a large, population-based dataset with a significantly high participation rate. In addition, it includes variables of social determinants of health and has a follow-up time exceeding three decades. By identifying a markedly elevated mortality risk for adults aged 25–44 years with a disability compared to participant without a disability, the study contributes unique results. A significantly increased mortality risk for adults with disability due to motor impairment, vision impairment, mental health problems or physical illness, even at minor to moderate severity levels, was found, and it was also indicated for adults reporting disability due to hearing impairment. Hence, an added value of this study is that it implies a substantially increased mortality risk in the understudied population of working-age adults with a disability compared to those without a disability.
Implications of all the available evidence
To the best of our knowledge, this is the first population-based study of this size and follow-up time to include adults aged 25–44 years with long-term disability to investigate mortality risk. To avoid premature mortality, all available evidence, including that reported by the present study, underscores a need to raise awareness and increase understanding in research and practice about the potential determinants associated with increased mortality risk among adults of working age with disability.
Alt-text: Unlabelled box
Introduction
Disability involves being partially or fully hindered in participation in society on an equal basis with others as a result of complex interactions between health conditions and contextual factors, both personal and environmental.1 The impact of disability on a person's life may vary in severity and over the life course. As global life expectancy has increased,2 research indicates that the number of years lived with disability before reaching advanced age is also on the rise.3,4 Approximately one billion people have disabilities globally, representing 15% of the world's population.1
Poor health, socioeconomic disadvantages and mortality are closely linked.1,5,6 People with disability may have a higher mortality risk than people without disability because of risk factors related to health, sociodemographic factors and lifestyle.7 In high-income countries offering good-quality medical treatment and health care accessible by all, health needs are expected to trigger the timely and adequate involvement of health and social care services. However, widespread inequities are documented in a European review of social determinants of health,8 and persistent inequalities in health are a disappointment related to Western Europe's ‘welfare states’.9
Topics related to ageing among adults with long-term disabilities often go unrecognised by disability user organisations and researchers,10 and population-based studies on the association between disability in adulthood and survival are few in number.10,11 Working-age adults with disability may face barriers related to education and work,12 finding a partner and taking part in activities that benefit their health.13 These are important social determinants of health associated with life expectancy, although the exact pathways and mechanisms and whether the involved factors are confounders or mediators are unclear.6 Thus far, only a few studies have investigated life expectancy among working-age adults with disability, and these have found increased risk for mortality.5,14, 15, 16, 17 However, apart from a Swedish study on young adults with mild intellectual disability, these studies were conducted in countries without a universal welfare-state model. Thus, inferring these findings to European welfare states may not be valid. Detailed, population-based studies including data on working-age adults with different disability types and severity levels are needed to be able to identify those who are particularly vulnerable to reduced survival.
The objective of this study was to investigate the association between long-term disability and mortality risk for adults of working age using a large and longitudinal Norwegian dataset. This is the first study with more than 35 years of follow-up to examine mortality risk among adults aged 25–44 years with disability due to vision, hearing, or motor impairments; physical illness; or mental health problems according to severity levels. The disability-mortality risk association is investigated adjusted for confounding by age and sex, as well as possible mediation by educational level, work participation, living situation, body mass index (BMI), systolic blood pressure (SBP) and smoking status at baseline. Our hypothesis is that disability in working age is associated with increased mortality risk.
Material and methods
Study population
For the main analysis, data gathered from the study population of the first of four rounds of one of the world's longest-running public health surveys, The Trøndelag Health Study (HUNT) was used.18 The first survey round, HUNT1, was conducted during 1984–86. All adults age 20 years or older in the Norwegian county of Nord-Trøndelag were invited for physical examinations and to complete questionnaires regarding their health, functioning, living situation, education, work, social participation and lifestyle. A total of 77,212 persons participated in HUNT1 (89.4% of those invited).18 The current study sample consists of the 30,080 HUNT1 participants aged 25–44 years at the time of the data collection with non-missing information for our key disability variables (56 were dropped due to missing data). In a sub-analysis restricted to those with non-missing data for all covariates, the sample size was limited to 23,184 (denoting the sample of complete cases). For the sensitivity analysis, data from the second round of HUNT (HUNT2, 1995–97) for the present HUNT1 study population were also included.
Disability
The definition and operationalisation of disability assessed in HUNT align well with the WHO's International Classification of Functioning, Disability and Health (ICF) framework, defining disability as a result of an interaction between the person and the society.1 In HUNT, disability was self-reported and based on the initial yes/no question: ‘Do you suffer from any long-term illness or injury of a physical or psychological nature that impairs your functioning in your everyday life?’ (long-term here means that it has lasted or will last for at least one year). Participants responding ‘yes’ were further asked to describe the type of impairment or condition causing the disability, and they could report more than one if they had two or more. The alternative response categories were motor impairment, vision impairment, hearing impairment, physical illness or mental health problems. The participants were also asked about the severity (slight, moderate, severe) of the reported impairment or condition.19 In the analyses, the slight and moderate severity categories were collapsed and designated ‘moderate’. Participants reporting no disability on the initial disability question were coded ‘None’ for all sub-types of disability. Those with missing responses for disability type sub-items but valid responses to the initial disability question were coded as ‘Other’ for that sub-item.
Covariates
In addition to age and sex, the sociodemographic and health variables educational level, work participation, living situation, body mass index (BMI), systolic blood pressure (SBP) and smoking status at baseline were included in the present study. Age, sex, educational level, work participation, living situation and smoking status at baseline were self-reported, whereas systolic blood pressure, height and weight were objectively measured. Educational level was grouped as compulsory (<10 years), secondary (10–12 years) or tertiary (13+ years). Work participation was grouped as full-time paid work, part-time paid work, housework, and not working. Living situation was binary as living alone or living with someone. Smoking status at baseline was grouped as never, former, and current. Two SBP assessments per respondent were performed by trained nurses or technicians using a mercury sphygmomanometer; the respondent was assessed in a sitting position after having rested a minimum of 5 minutes. The mean value of the two measurements was used for the analyses. BMI was defined as weight in kilograms divided by the height in meters squared (kg/m2) and categorised as four groups, <18.5, 18.5–24.9, 25–29.9, and 30+.
Mortality
Using unique personal identification numbers, the HUNT data were linked with data from the Tax Administration of Norway, a national registry providing data on emigration and death. Participants were followed from their initial individual date of participation in HUNT1 (between 1984 and 1986) until emigration, death, or 15 November 2019, whichever occurred first.
Consent
All participants in HUNT received information about the HUNT-study and signed consent forms. The Norwegian Data Inspectorate and the Regional Committee for Medical and Health Research Ethics (REC, reference number 45034), HUNT study (reference number 2019/15992), and the Norwegian Centre for Research Data (reference number 230227) approved this study.
Main analysis
Stata version 16 was used for all statistical analyses estimating the 35-year mortality risk for HUNT1 participants with disability compared to those without disability. For the analysis investigating mortality risk for the different types of disabilities studied and the severity level, the reference group comprised those without any of these disabilities. Mortality rates were calculated as the number of deaths by person-years (py). PY takes into account both the number of people in the study and the amount of time each person spends in the study. Age and sex were standardised to adjust for the potential confounding effect of the relationship by using the full study population in five-year age bands by sex as the standard population. Survival according to disability status was modelled using the Kaplan-Meyer survival curve for illustrative purposes. In the main analyses, mortality hazard ratios (HRs) according to disability status were estimated by Cox regression using the age attained as the time scale. A set of Cox models was fitted to investigate possible confounding and mediating effects. First, models adjusted for the confounders of sex and age were fitted for the full sample (Model 1a) and for the sample of complete cases (Model 1b). Model fit comparisons were conducted using the likelihood ratio test. Moreover, flexible parametric survival models were used to model the probability of surviving to a specified age and to investigate deviations from the proportional hazards (PHs) assumption.20 The significance of the differences in the survival curves between disability groups was estimated using post-hoc predictions from the flexible parametric regression model. The PH assumption was formally tested using the likelihood ratio test and by comparing the flexible model assuming PH with the flexible model without this assumption. In the flexible model, restricted cubic splines with four boundary knots were used to model baseline survival and three knots were used for time-dependent effects. Significant interactions with age and sex were included in the model.
Sensitivity analysis
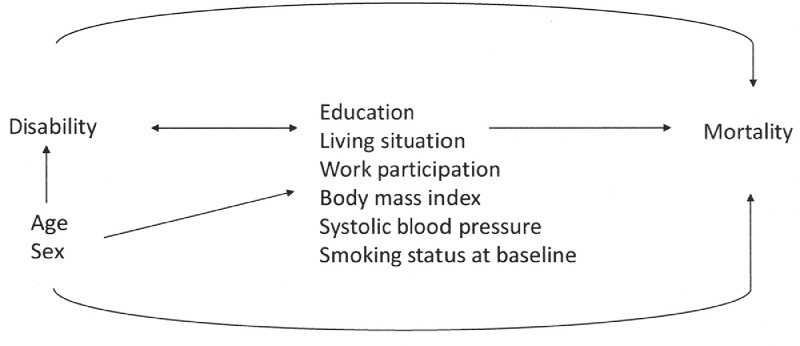
Regarding potential pathways and mechanisms involved in the association between disability and mortality, it was presumed prior to the analysis that age and sex are confounding factors and that education, work participation, living situation, body mass index (BMI), systolic blood pressure (SBP) and smoking status at baseline could be possible mediating factors (illustrated in Figure 1). A mediator is a factor that may interact with an exposure, and the interaction is assumed to have potential direct or indirect effects on an investigated outcome.21 Whereas the main analysis is adjusted for the confounders of age and sex, the other variables are considered either confounders or mediators and are included in the sensitivity analysis. The rationale is that age and sex may independently affect both the disability as well as the mortality risk, whereas the other factors are also thought to be potential mediators. Thus, it is assumed that disability status may affect these variables and, in turn, affect mortality risk.
Figure 1.
Direct acyclic graph (DAG) showing the assumed causal relationship between disability status at baseline and mortality risk. The included covariates are age and sex (confounders), education level, work participation, living situation, body mass index (BMI), systolic blood pressure (SBP) and smoking status at baseline (mediators).
Additional sensitivity analyses were performed that included variables from HUNT2 (1995–97) in order to investigate whether changes in disability status from HUNT1 to HUNT2 would affect mortality risk during the 35 years of follow-up, or if mortality risk would be affected if follow-up was set from HUNT2. The assessment of disability status and the included covariates for HUNT2 were identical to those for HUNT1; 11 years after HUNT1. HUNT2 was conducted with a 70% participation rate. A variable with six groups, using both time points, was created for assessing disability status based on the yes/no question at both time points with three possible categories for HUNT1 and HUNT2 (yes = Y, no = N, missing = -). The groups included in the analysis of the mortality risk associated with changes in disability status between HUNT1 and HUNT2 were as follows: NN, YN, NY, YY, N-, and Y-, with NN as the reference group.
Role of the funding source
This study received no external funding.
Results
Descriptive statistics
A total of 5071 (16.9%) of the 30,080 HUNT1 participants aged 25–44 years reported having a disability at baseline. As shown in Table 1, the prevalence was slightly higher among men (18.0%) than among women (15.7%). The most prevalent disability type was due to physical illness (6.8%) and the least prevalent was disability due to hearing impairment (2.6%).
Table 1.
Descriptive statistics of the study population, ages 25–44 years at baseline (Number of respondents = 30,080).
| Number of respondents (%) |
Number of deaths |
Person years (py) |
Mortality rate per 100 000 py |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Disability status | Total | Women | Men | Women | Men | Women | Men | Women | Men |
| No | 25009 (83.1) | 12678 (84.3) | 12331 (82.0) | 1286 | 1821 | 427518 | 409006 | 300.8 | 445.2 |
| Yes | 5071 (16.9) | 2359 (15.7) | 2712 (18.0) | 428 | 641 | 77326 | 86228 | 553.5 | 743.4 |
| Disability sub-type and severity | |||||||||
| Vision impairment | |||||||||
| None | 28928 (96.2) | 14424 (95.9) | 14504 (96.4) | 1608 | 2326 | 484814 | 478231 | 331.7 | 486.4 |
| Moderate | 1028 (3.4) | 546 (3.6) | 482 (3.2) | 94 | 108 | 17835 | 15389 | 527.1 | 701.8 |
| Severe | 124 (0.4) | 67 (0.4) | 57 (0.4) | 12 | 28 | 2196 | 1614 | 546.6 | 1734.7 |
| Hearing impairment | |||||||||
| None | 29305 (97.4) | 14790 (98.4) | 14515 (96.5) | 1678 | 2350 | 496725 | 478240 | 337.8 | 491.4 |
| Moderate | 643 (2.1) | 202 (1.3) | 441 (2.9) | 30 | 89 | 6632 | 14228 | 452.3 | 625.5 |
| Severe | 132 (0.4) | 45 (0.3) | 87 (0.6) | 6 | 23 | 1487 | 2766 | 403.6 | 831.7 |
| Motor impairment | |||||||||
| None | 28940 (96.2) | 14582 (97.0) | 14358 (95.4) | 1603 | 2306 | 490399 | 473569 | 326.9 | 486.9 |
| Moderate | 986 (3.3) | 377 (2.5) | 609 (4.0) | 75 | 124 | 12182 | 19481 | 615.7 | 636.5 |
| Severe | 154 (0.5) | 78 (0.5) | 76 (0.5) | 36 | 32 | 2263 | 2184 | 1590.8 | 1465.4 |
| Physical illness | |||||||||
| None | 28041 (93.2) | 14080 (93.6) | 13961 (92.8) | 1528 | 2203 | 473799 | 460972 | 322.5 | 477.9 |
| Moderate | 1724 (5.7) | 800 (5.3) | 924 (6.1) | 138 | 196 | 26125 | 29774 | 528.2 | 658.3 |
| Severe | 315 (1.0) | 157 (1.0) | 158 (1.1) | 48 | 63 | 4920 | 4488 | 975.5 | 1403.8 |
| Mental health problems | |||||||||
| None | 29024 (96.5) | 14452 (96.1) | 14572 (96.9) | 1571 | 2304 | 486055 | 480886 | 323.2 | 479.1 |
| Moderate | 841 (2.8) | 464 (3.1) | 377 (2.5) | 98 | 119 | 15117 | 11632 | 648.3 | 1023.0 |
| Severe | 215 (0.7) | 121 (0.8) | 94 (0.6) | 45 | 39 | 3671 | 2716 | 1225.8 | 1435.8 |
| Other* | 101 (0.4) | 48 (0.4) | 53 (0.4) | 14 | 12 | 1577 | 1742 | 887.9 | 688.9 |
| Disability by age | |||||||||
| Age in years, any disabilities | |||||||||
| 25–29 | 919 | 386 | 533 | 29 | 50 | 13138 | 17999 | 220.7 | 277.8 |
| 30–34 | 1172 | 529 | 643 | 71 | 122 | 17605 | 20818 | 403.3 | 586.0 |
| 35–39 | 1475 | 711 | 764 | 141 | 184 | 23103 | 24166 | 610.3 | 761.4 |
| 40–44 | 1505 | 733 | 772 | 187 | 285 | 23480 | 23245 | 796.4 | 1226.1 |
| Age in years, no disabilities | |||||||||
| 25–29 | 7030 | 3538 | 3492 | 137 | 195 | 107982 | 100566 | 126.9 | 180.6 |
| 30–34 | 7919 | 3984 | 3935 | 257 | 366 | 117354 | 110672 | 219.0 | 311.9 |
| 35–39 | 8299 | 4104 | 4195 | 387 | 557 | 114058 | 113523 | 339.3 | 488.3 |
| 40–44 | 6832 | 3411 | 3421 | 505 | 703 | 88124 | 84245 | 573.1 | 797.7 |
Of the participants in HUNT1 with a disability, 10.8% had attained a tertiary educational level, whereas the equivalent figure for those without a disability was 17.9% (Table 2). Only 4.6% of the participants without a disability did not work in contrast to 17.5% of those with a disability. For both groups, 4% were living alone. Those with a disability had a higher prevalence of smoking at baseline (current smoker 46.3% vs 39.7%) and of overweight and obesity (38.7% vs 34.0%) compared to those without a disability; SBP was similar across disability status.
Table 2.
Confounders and mediators at baseline at Trøndelag Health Study, survey round 1 (HUNT1).
| Total | Disability status at HUNT1 |
||
|---|---|---|---|
| Number of respondents (%) | No disability, number of respondents (%) |
Any disability, number of respondents (%) |
|
| Education | |||
| Compulsory | 8555 (36.4) | 6734 (34.4) | 1821 (46.4) |
| Secondary | 11015 (46.9) | 9338 (47.7) | 1677 (42.8) |
| Tertiary | 3921 (16.7) | 3497 (17.9) | 424 (10.8) |
| Work | |||
| Full-time | 17686 (58.9) | 15093 (60.4) | 2593 (51.2) |
| Part-time | 6672 (22.2) | 5667 (22.7) | 1005 (19.8) |
| Housework | 3665 (12.2) | 3085 (12.3) | 580 (11.5) |
| Not working | 2027 (6.7) | 1141 (4.6) | 886 (17.5) |
| Living situation | |||
| Lives with someone | 28925 (96.2) | 24045 (96.1) | 4880 (96.2) |
| Lives alone | 1155 (3.8) | 964 (3.9) | 191 (3.8) |
| Smoking status at baseline | |||
| Never | 8562 (36.2) | 7334 (37.2) | 1228 (30.9) |
| Former | 5456 (23.0) | 4548 (23.1) | 908 (22.8) |
| Current | 9665 (40.8) | 7825 (39.7) | 1840 (46.3) |
| BMI, kg/m2 | |||
| <18.5 | 435 (1.5) | 345 (1.4) | 90 (1.8) |
| 18.5–24.99 | 18766 (63.8) | 15830 (64.6) | 2936 (59.5) |
| 25–29.99 | 8450 (28.7) | 6968 (28.4) | 1482 (30.0) |
| 30+ | 1779 (6.0) | 1352 (5.5) | 427 (8.7) |
| SBP, mmHg, mean (SD) | n = 29420 | 126.6 (14.7) | 126.7 (14.7) |
Note: Abbreviations: BMI=Body mass index (kg/m2), SBP=Systolic blood pressure (mmHg).
Mortality
The mean follow-up time for HUNT1 participants was 33.2 years; the median was 34.6 years and the maximum 35.8 years. During the total follow-up time of 1,000,078 person-years (py), 4176 died. Of these, 398 deaths occurred before HUNT2 (prior to 1 January 1995). The maximum attained age at the end of the follow-up period was 80.7 years.
Mortality by overall disability status at HUNT1
Those reporting long-term disability at HUNT1 had an elevated mortality rate compared to individuals without a disability, both for men and women (Table 3, Figure 2). The age- and sex-adjusted HR for disability compared to no disability was 1.62 (95% confidence interval (CI 1.51, 1.74) in the full sample (Table 3, Model 1a) and 1.58 (95% CI 1.46, 1.72) in the sample of complete cases with non-missing values for all covariates (Model 1b). In the sensitivity analysis, further adjustment for possible mediating factors for educational level, work participation and living situation (Model 2) attenuated the HR to 1.39 (95% CI 1.28, 1.52), while adjustment for health-related variables (Model 3) attenuated the HR slightly less. In the fully adjusted model, the HR was 1.34 (95% CI 1.24, 1.47).
Table 3.
Mortality hazard ratios (HR) with 95% confidence intervals (CIs) by disability type. Adjustments for confounders and mediators. Cox regression.
| Main analysis. Full sample, n = 30,080 HR (95% CI) |
Sensitivity analyses. Complete cases sample, n = 23,184 HR (95% CI) |
||||
|---|---|---|---|---|---|
| Disability | Model 1a Adjusted for age and sex |
Model 1b Adjusted for age and sex |
Model 2 Adjusted for age, sex, education, work and living situation |
Model 3 Adjusted for age, sex, smoking status at baseline, BMI, SBP |
Model 4 Fully adjusted |
| Any disability | |||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 1.62 (1.51, 1.74) | 1.58 (1.46, 1.72) | 1.39 (1.28, 1.52) | 1.47 (1.36, 1.60) | 1.34 (1.24, 1.47) |
| Disability type | |||||
| Hearing impairment | |||||
| None | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.12 (0.94, 1.35) | 1.23 (1.001, 1.51) | 1.14 (0.93, 1.40) | 1.18 (0.96, 1.45) | 1.12 (0.91, 1.38) |
| Severe | 1.39 (0.96, 2.00) | 1.40 (0.91, 2.14) | 1.25 (0.82, 1.93) | 1.42 (0.93, 2.19) | 1.34 (0.87, 2.06) |
| Vision impairment | |||||
| None | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.46 (1.27, 1.68) | 1.45 (1.22, 1.71) | 1.31 (1.11, 1.56) | 1.33 (1.12, 1.58) | 1.24 (1.04, 1.46) |
| Severe | 2.77 (2.03, 3.78) | 2.51 (1.69, 3.72) | 2.19 (1.48, 3.25) | 2.54 (1.72, 3.77) | 2.36 (1.59, 3.50) |
| Motor impairment | |||||
| None | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.36 (1.18, 1.56) | 1.34 (1.13, 1.58) | 1.18 (0.99, 1.39) | 1.27 (1.08, 1.51) | 1.15 (0.97, 1.37) |
| Severe | 3.67 (2.89, 4.67) | 2.77 (1.95, 3.94) | 2.03 (1.42, 2.91) | 2.33 (1.64, 3.33) | 1.82 (1.27, 2.60) |
| Physical illness | |||||
| None | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.37 (1.22, 1.53) | 1.31 (1.15, 1.50) | 1.18 (1.03, 1.35) | 1.26 (1.11, 1.44) | 1.18 (1.03, 1.34) |
| Severe | 2.82 (2.33, 3.40) | 2.49 (1.96, 3.16) | 1.74 (1.36, 2.23) | 2.10 (1.65, 2.67) | 1.62 (1.27, 2.07) |
| Mental health problems | |||||
| None | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Moderate | 1.99 (1.74, 2.29) | 2.00 (1.71, 2.35) | 1.70 (1.44, 2.00) | 1.70 (1.45, 1.99) | 1.50 (1.27, 1.77) |
| Severe | 3.40 (2.75, 4.23) | 3.50 (2.70, 4.50) | 2.29 (1.75, 2.99) | 3.17 (2.45, 4.11) | 2.36 (1.80, 3.08) |
| Other disability⁎⁎ | |||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 2.02 (1.38, 2.98) | 2.14 (1.34, 3.40) | 1.85 (1.16, 2.94) | 2.13 (1.34, 3.39) | 1.96 (1.23, 3.12) |
Table 3, note: Abbreviations: n = Number of respondents, BMI=Body Mass Index (kg/m2), HUNT=Trøndelag Health Study, SBP=Systolic Blood Pressure (mmHg). In the study population (N = 30,080), there were 4176 deaths during follow-up from 1984–2019. Of these deaths, 398 occurred during 1984–1994 (before HUNT2), 164 during 1995–97 (during HUNT2), 712 during 1998–2005 (between HUNT2 and 3), 420 during 2006–08 (during HUNT3), 1610 during 2009–2016 (between HUNT3 and HUNT4), and 872 during HUNT4.
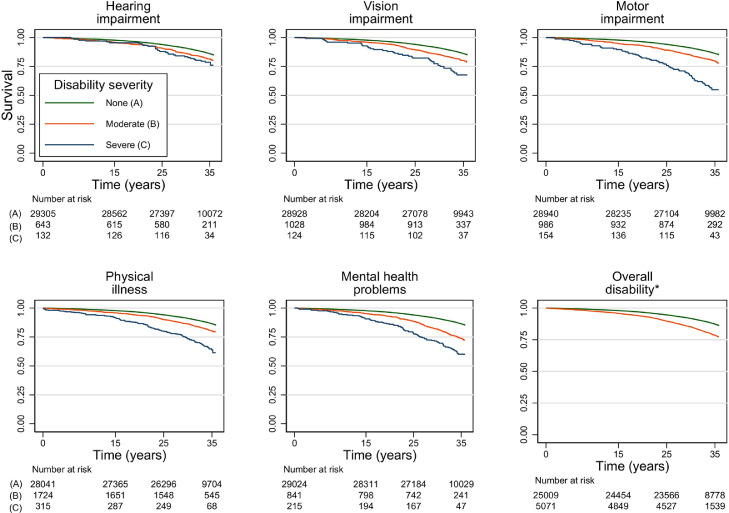
Figure 2.
Kaplan–Meier curves. Survival by disability type and severity. All individuals ages 25–44 years at baseline. *For overall disability (panel at bottom right), the categories are disability ‘yes’ (orange) and disability ‘no’ (green).
These survival differences translate into a survival probability of 85.0% (95% CI 83.3, 86.6) for a 30-year-old man with a disability to reach age 65, while the corresponding survival probability for a 30-year-old man without a disability was 91.3% (95% CI 90.7, 91.8) (Table 4). Corresponding probabilities of reaching 65 years of age for 30-year-old women were 89.4% (95% CI 88.0, 90.7) for those with disabilities and 94.0% (95% CI 93.6, 94.5) for those without.
Table 4.
Survival by disability type. Probability in percent (95% CI) of surviving the 35.8 (denoted 35) years follow-up time for 30-year-olds at baseline ((35p30)), by sex and baseline disability status. Probabilities are estimated for a specific age, but the underlying model is based on all ages 25–44 years at baseline. N = 30,080.
| Men | Women | |
|---|---|---|
| Disability | Age 30 years at baseline (35p30) |
Age 30 years at baseline (35p30) |
| Any disability | ||
| No | 91.3 (90.7, 91.8) | 94.0 (93.6, 94.5) |
| Yes | 85.0 (83.3, 86.6)* | 89.4 (88.0, 90.7)* |
| Disability type | ||
| Hearing impairment | ||
| None | 90.4 (89.8, 90.9) | 93.4 (93.0, 93.8) |
| Moderate | 89.5 (87.5, 91.2) | 92.8 (91.3, 94.0) |
| Severe | 87.2 (82.0, 91.0) | 91.2 (87.4, 93.8) |
| Vision impairment | ||
| None | 90.5 (90.0, 91.1) | 93.6 (93.1, 94.0) |
| Moderate | 86.0 (82.5, 88.9)* | 90.4 (87.9, 92.4)* |
| Severe | 74.2 (59.7, 84.2)* | 81.9 (70.8, 89.1) |
| Motor impairment | ||
| None | 90.6 (90.1, 91.2) | 93.6 (93.2, 94.0) |
| Moderate | 86.5 (82.8, 89.4)* | 90.7 (88.0, 92.8)* |
| Severe | 56.9 (43.4, 68.3)* | 68.3 (56.8, 77.3)* |
| Physical illness | ||
| None | 90.6 (90.0, 91.1) | 93.6 (93.2, 94.0) |
| Moderate | 87.6 (86.2, 88.9)* | 91.5 (90.4, 92.5)* |
| Severe | 76.8 (72.6, 80.5)* | 83.8 (80.6, 86.5)* |
| Mental health problems | ||
| None | 90.6 (90.1, 91.0) | 93.7 (93.2, 94.0) |
| Moderate | 82.4 (80.0, 84.6)* | 87.9 (86.2, 89.5)* |
| Severe | 72.5 (66.8, 77.4)* | 80.8 (76.5, 84.3)* |
| Other disability⁎⁎ | ||
| No | 91.3 (90.7, 91.8) | 94.0 (93.6, 94.4) |
| Yes | 82.6 (75.3, 87.8)* | 87.9 (82.6, 91.6)* |
Table 4, note: Probabilities were predicted from flexible parametric survival models (baseline hazard curve is estimated with 4 knots) including the covariates age, sex, disability and significant two-way interaction terms (there were no significant three-way interaction terms) including the entire age range 25–44 years at baseline in HUNT1. Included covariates were time-dependent (no knots).
Significant (p < 0.05) different probability from reference category ‘No disability’ (or ‘None’ for disability types). Significance level was estimated using post-hoc predictions, of differences in survival curves between disability groups, from the flexible parametric regression model.
For ‘Other disability’, severity is not specified, as those with ‘yes’ responses constitute those responding ‘yes’ to the introductory question about having a disability but not one of the five types listed above.
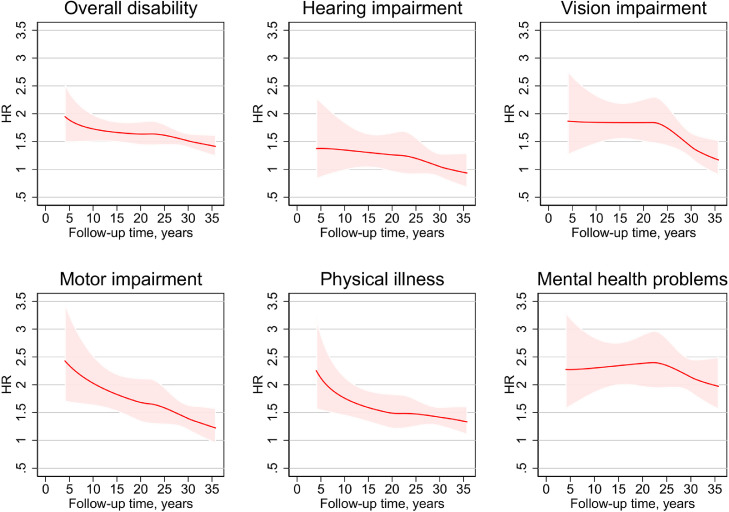
There was a tendency towards smaller HRs with longer follow-up time, but the HRs were above 1.0 throughout the entire follow-up period for most of the disability types except for disability due to a hearing impairment (Figure 3). The model allowing for non-proportional hazard fitted the data significantly better than a PH model (p < 0.01), thus suggesting non-proportional hazards. The Cox model will then give a kind of average HR for the entire follow-up time, which is still informative.
Figure 3.
Non-proportional hazards. Flexible parametric model. First four years of follow-up are not plotted. Ages 25–44 years at HUNT1. Severity levels combined; thus the model is mortality hazard ratio (HR) for those with disability vs no-disability at HUNT1.
Likelihood ratio test testing non-proportional hazards vs proportional hazards: motor impairment (p < 0.01), hearing impairment (p = 0.44), vision impairment (p = 0.05), motor impairment (p = 0.01), physical illness (p < 0.001), mental health problems (p = 0.71).
Mortality by disability type at HUNT1
Table 3 presents the estimated mortality risks associated with disability for HUNT1 due to hearing, vision or motor impairments; physical illness; or mental health problems according to severity levels adjusted for age and sex. In the sensitivity analysis, the estimated mortality risk was estimated adjusted for educational level, work participation, living situation, BMI, SBP and smoking status at baseline compared to individuals without these conditions. The highest mortality risks found in the age- and sex-adjusted analyses were for participants with disability due to severe levels of motor impairment (HR=3.67, 95% CI 2.89, 4.67), severe mental health problems (HR = 3.40 CI 2.75, 4.23), severe physical illness (HR = 2.82 CI 2.33, 3.40), and severe vision impairment (HR = 2.77 CI 2.03, 3.78). The analyses also indicated increased mortality risk associated with disability due to hearing impairment, but the results of the main analyses were not statistically significant (HR=1.39, 95% CI 0.96, 2.00). For all the disability types and severity levels, adjustments in Model 2 for educational level, work participation and living situation attenuated the HRs, while adjustment for health-related variables in Model 3 attenuated the HRs slightly less. The reported HRs above for disability due to severe levels of motor impairment, mental health, physical illness and vision impairment were somewhat attenuated in the fully adjusted models, but HRs remained substantial and significant.
Mortality by overall disability status at HUNT1 and HUNT2
The overall mortality rate (MR) per 1000 py for those having a disability at HUNT1 was 6.5. For those participants changing status from ‘Yes’ at HUNT1 to ‘No’ at HUNT2 (YN), and setting start to follow-up to HUNT2, the MR was 4.9, while those reporting disability at both time points (YY) had a higher MR of 8.1 (Table 5). Those with the highest mortality rate (MR=11.9), however, were in the group reporting disability at HUNT1 and not participating in HUNT2 (Y-). This group also had an increased mortality risk when follow-up time was set from HUNT1 until HUNT2 compared to those reporting no disability at HUNT1 and missing at HUNT2 (N-); MR for Y- was 8.2 vs 4.0 for the group N-. Moreover, changing disability status from ‘No’ to ‘Yes’ (NY) or from ‘No’ to ‘Missing’ (N-) was associated with a significantly increased HR compared to those in the stable ‘No’ (NN) group, in an age- and sex-adjusted model with follow-up time from HUNT2 (Table 5).
Table 5.
Disability status at HUNT1 and HUNT2 and mortality rate (MR) per 1000 person years (py) (N = 30,080).
| Disability status* | Follow-up from HUNT1 to HUNT2 (until 01.01.1995) |
Follow-up from HUNT2 (from 01.01.1995) |
||||||
|---|---|---|---|---|---|---|---|---|
| Number of respondents | Number of deaths | PY (in 1000) |
MR per 1000 PY⁎⁎ |
Number of deaths | PY (in 1000) |
MR per 1000 PY⁎⁎ |
HR (95% CI)⁎⁎⁎ (after HUNT2, 1.1.1995) |
|
| NN | 14366 | 0 | 143 | 0 | 1272 | 347 | 3.6 | 1.0 |
| YN | 1364 | 0 | 14 | 0 | 162 | 33 | 4.9 | 1.27 (1.08, 1.50) |
| NY | 3810 | 0 | 38 | 0 | 574 | 90 | 6.3 | 1.55 (1.41, 1.71) |
| YY | 2127 | 0 | 21 | 0 | 403 | 49 | 8.1 | 1.89 (1.69, 2.11) |
| N- | 6833 | 273 | 67 | 4.0 | 988 | 152 | 6.5 | 1.89 (1.74, 2.06) |
| Y- | 1580 | 125 | 15 | 8.2 | 379 | 33 | 11.9 | 3.20 (2.86, 3.60) |
Disability status at HUNT1 and HUNT2 (No=N, Yes=Y);
Direct standardized using population in five-year age bands by sex as post stratification weights.
HR (95% CI) estimated in Cox regression are adjusted by age (time scale) and sex. Abbreviations: HUNT=Trøndelag Health Study, NN=No disability at either HUNT1 or HUNT2, YN=Disability at HUNT1 and not at HUNT2, NY=No disability at HUNT1 and disability at HUNT2, YY=Disability at both HUNT1 and HUNT2, N-=No disability at HUNT1 and missing at HUNT2, Y-=Disability at HUNT1 and missing at HUNT2.
Discussion
Compared to individuals without a disability and after more than 35 years of follow-up time, this large, population-based study finds a 62% increased mortality risk for adults aged 25–44 years with long-term disability. The analyses were adjusted for age and sex, and mediation was investigated by further adjustment for educational level, work participation, living situation, BMI, SBP and smoking status at baseline. The results of the analyses, including data from the second wave of HUNT (HUNT2) collected 11 years after HUNT1, identify the same pattern of association. Compared to participants without a disability in either HUNT1 or HUNT2, a three fold mortality risk was found for those with disability at HUNT1 who did not participate in HUNT2 (97.5% of these participants were alive at the start of the HUNT2 data collection).
Substantial impacts were also found for the different disability types and severity levels studied, but these were more pronounced at severe levels. Moreover, as illustrated in Figure 3, the results of the flexible parametric model, with non-proportional hazards, indicate a slightly stronger association in the first period after assessment. Compared to participants without the investigated type of disability, the results of the adjusted analysis showed a close to fourfold increased mortality risk associated with a disability due to severe motor impairment, and a close to threefold mortality risk associated with a disability due to severe mental health problems, physical illness, or vision impairment. The results also indicate that disability due to severe hearing impairment was associated with increased mortality risk, but these results of the main analyses were not statistically significant.
The strong associations found between disability due to motor impairment and mortality risk are in accordance with previous research, but this study extended earlier findings by including a younger sample.22, 23, 24, 25 Only one comparable study included participants as young as 40 years of age,24 but the follow-up time was 6 years24 as opposed to more than 35 years in the present study. Hence, the observation that even moderate levels of motor impairment resulted in strong, negative effects on the probability of survival is a novel finding.
Worldwide and in line with these results, disability due to mental health problems has consistently been found to be associated with excessive mortality risk.26 For example, a recent Danish registry-based study found that women and men with mental disorders die seven and ten years earlier, respectively, than the general population.27 The study also identified a variety of causes of death in its sample such as substance abuse and suicide as well as more deaths related to somatic illnesses.27 This complexity underscores that the pathways and mechanisms involved are multifactorial, as also indicated by the present study's results of the sensitivity analysis regarding the reduction in mortality risk when adjusting for social determinants of health. Moreover, studies investigating the mortality risk associated with mental health problems are often based on registry data, which requires a recorded diagnosis made by healthcare personnel. This means that only people who have sought help for their mental health problems are registered. Longitudinal, population-based studies based on self-reported mental health status are rare, and the present research adds to the mostly clinically based comparable studies by using self-reported data on disability due to mental health problems.
The Lancet Global Health published a systematic review and meta-analysis on vision impairment and mortality in 2021, which concluded, in agreement with the present study, that mortality was higher in individuals with vision impairment than for those with normal vision or mild vision impairment, and this risk increased with more-severe vision impairment.28 However, prior research has yielded inconsistent results regarding the association between vision impairment and mortality, and limitations related to heterogeneous study designs have been pointed out.29, 30, 31 Furthermore, a majority of the study populations are older than 40 years of age.28 Hence, this study adds unique information concerning the long-term association between disability due to vision impairment and mortality risk in a working-age population.
Disability due to hearing impairment was the only condition that was not statistically significantly associated with increased mortality risk in this study, but the hazard ratios indicate a relationship. This is mainly in line with previous research30,32 but contrary to several other studies that also measured hearing with subjective reports.31,33,34 Most of the studies on this topic detected a weak-to-moderate association between hearing impairment and increased mortality risk.35, 36, 37, 38, 39 While hearing impairment, in and of itself, has not been found to increase mortality risk,40 the association among older adults may be confounded or mediated by factors more strongly and directly related to mortality such as cognitive impairment30 and dementia.41 The results of previous and present findings imply that the association between disability due to hearing impairment and mortality risk may be influenced by different factors over the life course.
Almost threefold increased mortality risk was also found for the heterogeneous group of participants with disability due to severe physical illness. For all the disability types and severity levels included in this study, multiple interrelated factors6,9 may have led to the inequalities in mortality risk we identified. Participants might have been prohibited from engaging in an active life or may have experienced barriers and discrimination related to their disabilities. For these reasons, the sensitivity analyses were adjusted for possible confounding or mediating factors considered important social determinants of health, such as educational level, work participation, living situation, BMI, SBP and smoking status at baseline. The results revealed that the included variables had an impact on participants’ mortality risk. Moreover, they indicated that social determinants of health (education, work participation and living situation) may have a somewhat stronger effect on health than the health-related variables (BMI, SPB and smoking status at baseline) included in this study. However, whether the variables were confounders or mediators in the association between disability and mortality remains unclear.
Strengths and limitations
This study fills the gap in the extant literature by focussing on the understudied group of working-age adults with disabilities. The strengths of this study are the 35-year follow-up period, the large population-based sample, and the ability to investigate the mortality risk associated with long-term disabilities of both moderate and severe levels among working-age adults 25–44 years old, which few studies to date have accomplished. This study's high participation rate is another significant strength; almost 90% of those invited participated in HUNT1. This strength is underscored by the substantially increased mortality risk found for participants with disability at HUNT1 who did not participate in HUNT2. Although the participation rate in HUNT2 was fair at 70%, these results illustrate the importance of high participation rates for the inclusion of vulnerable groups in population-based studies.
An additional strength is the fact that the sample for this regional study can, in many respects, be considered representative of this demographic in all of Norway.42 One exception, however, is that the county does not include any large cities. The results of the present study may be generalisable to other European countries, at least those with fairly similar welfare models and demographics.
Moreover, self-reported disability was used, which may cover a broader range of disability compared to the use of clinical or objective diagnoses. An additional strength is that the underlying question of disability in HUNT is formulated in line with how the WHO defines disability in its ICF model. The benefit of this approach is that we may have been able to include those who do not have a formal diagnosis but have, nevertheless, experienced loss of function that interferes with everyday life.
A general limitation within this field of research is that any comparison of study results is hampered by differing definitions and differences in the operationalisation of disability and impairments and of the sample characteristics. A limitation specific to this study is the failure to include ‘intellectual impairment’ as a response category. In addition, causes of death was not examined.
Conclusion
This large, population-based study with more than 35 years of follow-up identified a considerably increased overall mortality risk for adults 25–44 years of age with long-term disability and for disabilities of different types and severity levels compared to those in the study sample without these disabilities. The highest mortality risks were identified for disability related to severe motor impairment or severe mental health problems.
Contributors
B.E.: Literature search, figures, study design, data interpretation and writing. G.G.T.: Literature search, study design, data interpretation and writing. B.H.S.: Literature search, figures, study design, data analyses, data interpretation and writing. E.M.L.: Literature search, figures, study design, data analyses, data interpretation and writing original draft.
Ethical approval
The Norwegian Data Inspectorate and the Regional Committee for Medical and Health Research Ethics (REC, reference number 45034), HUNT study (reference number 2019/15992), and the Norwegian Centre for Research Data (reference number 230227) approved this study.
Data sharing statement
We are not permitted to share data, but researchers may apply for access to the present data. The lead authors (EML and BHS) affirm that this manuscript is an honest, accurate and transparent account of the study being reported and that no important aspects of the study have been omitted.
Participant involvement
It was not possible to involve HUNT1 participants in the design, conducting, reporting or dissemination plans of the present research.
Dissemination to participants and related patient and public communities
We plan to disseminate all the results to relevant user organisations as soon as the study is published.
Declaration of interests
All authors have completed the ICMJE uniform disclosure form and declare the following: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
The Trøndelag Health Study (HUNT) is a collaboration between the HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU), the Trøndelag County Council, the Central Norway Regional Health Authority, and the Norwegian Institute of Public Health.
References
- 1.World Health Organization . World Health Organization; Geneve: 2011. World report on disability 2011. [PubMed] [Google Scholar]
- 2.Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cambois E, Blachier A, Robine JM. Aging and health in France: an unexpected expansion of disability in mid-adulthood over recent years. Eur J Public Health. 2013;23(4):575–581. doi: 10.1093/eurpub/cks136. [DOI] [PubMed] [Google Scholar]
- 4.Beller J, Epping J. Disability trends in Europe by age-period-cohort analysis: increasing disability in younger cohorts. Disabil Health J. 2021;14(1) doi: 10.1016/j.dhjo.2020.100948. [DOI] [PubMed] [Google Scholar]
- 5.Park JM, Oh U, Roh BR, Moon Y. Disparities in mortality by disability: an 11-year follow-up study of 1 million individuals. Int J Public Health. 2017;62(9):989–996. doi: 10.1007/s00038-017-0966-5. [DOI] [PubMed] [Google Scholar]
- 6.Dugravot A, Fayosse A, Dumurgier J, et al. Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study. Lancet Public Health. 2020;5(1):e42–e50. doi: 10.1016/S2468-2667(19)30226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Majer IM, Nusselder WJ, Mackenbach JP, Klijs B, van Baal PH. Mortality risk associated with disability: a population-based record linkage study. Am J Public Health. 2011;101(12):e9–e15. doi: 10.2105/AJPH.2011.300361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P. WHO European review of social determinants of health and the health divide. Lancet. 2012;380(9846):1011–1029. doi: 10.1016/S0140-6736(12)61228-8. [DOI] [PubMed] [Google Scholar]
- 9.Mackenbach JP. The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med. 2012;75(4):761–769. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- 10.Hilberink SR, van der Slot WMA, Klem M. Health and participation problems in older adults with long-term disability. Disabil Health J. 2017;10(2):361–366. doi: 10.1016/j.dhjo.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Klingbeil H, Baer HR, Wilson PE. Aging with a disability. Arch Phys Med Rehabil. 2004;85(7 Suppl 3):S68–S73. doi: 10.1016/j.apmr.2004.03.014. quiz S4-5. [DOI] [PubMed] [Google Scholar]
- 12.Jajtner KM, Brucker DL, Mitra S. Midlife work limitations are associated with lower odds of survival and healthy aging. J Gerontol B. 2022;77(4):790–802. doi: 10.1093/geronb/gbab214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 14.Forman-Hoffman VL, Ault KL, Anderson WL, et al. Disability status, mortality, and leading causes of death in the United States community population. Med Care. 2015;53(4):346–354. doi: 10.1097/MLR.0000000000000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prynn JE, Dube A, Mkandawire J, et al. Self-reported disability in relation to mortality in rural Malawi: a longitudinal study of over 16 000 adults. BMJ Open. 2020;10(8) doi: 10.1136/bmjopen-2019-034802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heslop P, Blair PS, Fleming P, Hoghton M, Marriott A, Russ L. The Confidential Inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet. 2014;383(9920):889–895. doi: 10.1016/S0140-6736(13)62026-7. [DOI] [PubMed] [Google Scholar]
- 17.Hirvikoski T, Boman M, Tideman M, Lichtenstein P, Butwicka A. Association of intellectual disability with all-cause and cause-specific mortality in Sweden. JAMA Netw Open. 2021;4(6) doi: 10.1001/jamanetworkopen.2021.13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krokstad S, Langhammer A, Hveem K, et al. Cohort profile: the HUNT Study, Norway. Int J Epidemiol. 2013;42(4):968–977. doi: 10.1093/ije/dys095. [DOI] [PubMed] [Google Scholar]
- 19.NTNU . 2020. HUNT 1 Questionnaires.https://hunt-db.medisin.ntnu.no/hunt-db/variablelist Accessed 22 December 2020. [Google Scholar]
- 20.Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J. 2009;9(2):265–290. [Google Scholar]
- 21.VanderWeele TJ. Mediation analysis: a practitioner's guide. Ann Rev Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- 22.Bergland A, Jørgensen L, Emaus N, Strand BH. Mobility as a predictor of all-cause mortality in older men and women: 11.8 year follow-up in the Tromsø study. BMC Health Serv Res. 2017;17(1):22. doi: 10.1186/s12913-016-1950-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elbaz A, Sabia S, Brunner E, et al. Association of walking speed in late midlife with mortality: results from the Whitehall II cohort study. Age. 2013;35(3):943–952. doi: 10.1007/s11357-012-9387-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keevil VL, Luben R, Hayat S, Sayer AA, Wareham NJ, Khaw KT. Physical capability predicts mortality in late mid-life as well as in old age: findings from a large British cohort study. Arch Gerontol Geriatr. 2018;74:77–82. doi: 10.1016/j.archger.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper R, Strand BH, Hardy R, Patel KV, Kuh D. Physical capability in mid-life and survival over 13 years of follow-up: British birth cohort study. Bmj. 2014;348:g2219. doi: 10.1136/bmj.g2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827–1835. doi: 10.1016/S0140-6736(19)32316-5. [DOI] [PubMed] [Google Scholar]
- 28.Ehrlich JR, Ramke J, Macleod D, et al. Association between vision impairment and mortality: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(4):e418–e430. doi: 10.1016/S2214-109X(20)30549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lopez D, McCaul KA, Hankey GJ, et al. Falls, injuries from falls, health related quality of life and mortality in older adults with vision and hearing impairment–is there a gender difference? Maturitas. 2011;69(4):359–364. doi: 10.1016/j.maturitas.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Mitoku K, Masaki N, Ogata Y, Okamoto K. Vision and hearing impairments, cognitive impairment and mortality among long-term care recipients: a population-based cohort study. BMC Geriatr. 2016;16:112. doi: 10.1186/s12877-016-0286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miyawaki A, Kobayashi Y, Kawachi I. Self-reported hearing/visual loss and mortality in middle-aged and older adults: findings from the Komo-Ise Cohort, Japan. J Epidemiol. 2020;30(2):67–73. doi: 10.2188/jea.JE20180198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schubert CR, Fischer ME, Pinto AA, et al. Sensory impairments and risk of mortality in older adults. J Gerontol A Biol Sci Med Sci. 2017;72(5):710–715. doi: 10.1093/gerona/glw036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Feeny D, Huguet N, McFarland BH, Kaplan MS, Orpana H, Eckstrom E. Hearing, mobility, and pain predict mortality: a longitudinal population-based study. J Clin Epidemiol. 2012;65(7):764–777. doi: 10.1016/j.jclinepi.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Denney JT, Boardman JD. Hearing impairment, household composition, marital status, and mortality among U.S. adults. J Gerontol B. 2021;76(1):201–208. doi: 10.1093/geronb/gbz157. [DOI] [PubMed] [Google Scholar]
- 35.Contrera KJ, Betz J, Genther DJ, Lin FR. Association of hearing impairment and mortality in the national health and nutrition examination survey. JAMA Otolaryngol Head Neck Surg. 2015;141(10):944–946. doi: 10.1001/jamaoto.2015.1762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Genther DJ, Betz J, Pratt S, et al. Association of hearing impairment and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2015;70(1):85–90. doi: 10.1093/gerona/glu094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fisher D, Li CM, Chiu MS, et al. Impairments in hearing and vision impact on mortality in older people: the AGES-Reykjavik study. Age Ageing. 2014;43(1):69–76. doi: 10.1093/ageing/aft122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gopinath B, Schneider J, McMahon CM, Burlutsky G, Leeder SR, Mitchell P. Dual sensory impairment in older adults increases the risk of mortality: a population-based study. PLoS One. 2013;8(3):e55054. doi: 10.1371/journal.pone.0055054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Engdahl B, Idstad M, Skirbekk V. Hearing loss, family status and mortality - findings from the HUNT study, Norway. Soc Sci Med. 2019;220:219–225. doi: 10.1016/j.socscimed.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 40.Hsu AK, McKee M, Williams S, et al. Associations among hearing loss, hospitalization, readmission and mortality in older adults: a systematic review. Geriatr Nurs. 2019;40(4):367–379. doi: 10.1016/j.gerinurse.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 41.Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–446. doi: 10.1016/S0140-6736(20)30367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.NTNU . 2022. HUNT Databank.https://www.ntnu.edu/hunt/databank Accessed 2 May 2022. [Google Scholar]