Summary
Background
Cardiometabolic dysfunction is common in young people with psychosis. Recently, the Psychosis Metabolic Risk Calculator (PsyMetRiC) was developed and externally validated in the UK, predicting up-to six-year risk of metabolic syndrome (MetS) from routinely collected data. The full-model includes age, sex, ethnicity, body-mass index, smoking status, prescription of metabolically-active antipsychotic medication, high-density lipoprotein, and triglyceride concentrations; the partial-model excludes biochemical predictors.
Methods
To move toward a future internationally-useful tool, we externally validated PsyMetRiC in two independent European samples. We used data from the PsyMetab (Lausanne, Switzerland) and PAFIP (Cantabria, Spain) cohorts, including participants aged 16–35y without MetS at baseline who had 1–6y follow-up. Predictive performance was assessed primarily via discrimination (C-statistic), calibration (calibration plots), and decision curve analysis. Site-specific recalibration was considered.
Findings
We included 1024 participants (PsyMetab n=558, male=62%, outcome prevalence=19%, mean follow-up=2.48y; PAFIP n=466, male=65%, outcome prevalence=14%, mean follow-up=2.59y). Discrimination was better in the full- compared with partial-model (PsyMetab=full-model C=0.73, 95% C.I., 0.68–0.79, partial-model C=0.68, 95% C.I., 0.62–0.74; PAFIP=full-model C=0.72, 95% C.I., 0.66–0.78; partial-model C=0.66, 95% C.I., 0.60–0.71). As expected, calibration plots revealed varying degrees of miscalibration, which recovered following site-specific recalibration. PsyMetRiC showed net benefit in both new cohorts, more so after recalibration.
Interpretation
The study provides evidence of PsyMetRiC's generalizability in Western Europe, although further local and international validation studies are required. In future, PsyMetRiC could help clinicians internationally to identify young people with psychosis who are at higher cardiometabolic risk, so interventions can be directed effectively to reduce long-term morbidity and mortality.
Funding
NIHR Cambridge Biomedical Research Centre (BRC-1215-20014); The Wellcome Trust (201486/Z/16/Z); Swiss National Research Foundation (320030-120686, 324730- 144064, and 320030-173211); The Carlos III Health Institute (CM20/00015, FIS00/3095, PI020499, PI050427, and PI060507); IDIVAL (INT/A21/10 and INT/A20/04); The Andalusian Regional Government (A1-0055-2020 and A1-0005-2021); SENY Fundacion Research (2005-0308007); Fundacion Marques de Valdecilla (A/02/07, API07/011); Ministry of Economy and Competitiveness and the European Fund for Regional Development (SAF2016-76046-R and SAF2013-46292-R).
For the Spanish and French translation of the abstract see Supplementary Materials section.
Keywords: Psychosis, Early Intervention, Risk Prediction Algorithm, Metabolic Syndrome, International Validation, PsyMetab, PAFIP
Research in context.
Evidence before this study
Meta-analyses have consistently found strong global associations between cardiometabolic and psychotic disorders. This directly translates to a global shortened life-expectancy of up to 15 years in people with psychotic disorders. In the general population, cardiometabolic risk prediction algorithms are commonly used to encourage personalized treatment decisions with the aim of primary prevention of longer-term cardiometabolic outcomes. However, a recent systematic review and exploratory analysis found that these existing algorithms are unlikely to be suitable for young people with psychosis and may underpredict risk in this group. Therefore, a cardiometabolic risk prediction algorithm tailored for young people with psychosis, the Psychosis Metabolic Risk Calculator (PsyMetRiC) was developed and externally validated in the UK.
Added value of this study
Risk prediction algorithms can only be confirmed to be suitable for populations they have been tested in, and international populations are likely to vary in ethnicity; culture and dietary habits; average population health, healthcare access; social norms, behaviours and attitudes, and legislation. We therefore performed detailed external validation analysis of PsyMetRiC in two independent European samples, from Switzerland and Spain. In doing so, we found that PsyMetRiC maintains its predictive performance and potential clinical usefulness across those borders and can reliably predict the risk of incident metabolic syndrome in young people with psychosis.
Implications of all the available evidence
PsyMetRiC is likely to be generalizable for use in at least some Western European nations. Our findings can pave the way toward a future globally-useful bedside tool to encourage personalized treatment decisions with the aim of improving the long-term physical health of young people with psychosis.
Alt-text: Unlabelled box
Background
People with psychotic disorders such as schizophrenia die on average 10–15 years sooner than the general population,1 predominantly due to a substantial burden of physical comorbidity including type 2 diabetes (T2D), obesity and cardiovascular disease (CVD).2 Crucially, this comorbidity reduces quality of life, is responsible for a considerable proportion of overall treatment costs,3 and it transcends borders: a high prevalence of cardiometabolic disorders has been consistently reported among people with psychotic disorders in Europe,4, 5, 6, 7 The Americas,8,9 Oceania,10 Asia11 and Africa.12
An early marker of cardiometabolic risk is the metabolic syndrome (MetS), which is a clustering of cardiometabolic traits such as disrupted glucose-insulin homeostasis, adiposity, hypertension, and dyslipidaemia. While MetS is a cardiometabolic intermediate, it has consistently shown a high risk of progression to more distal and chronic phenotypes such as type 2 diabetes13 and cardiovascular disease,14 alongside severe disease endpoints such as myocardial infarction,15 cerebrovascular events16 and premature mortality.17 Therefore, the metabolic syndrome is an important marker of past, present, and future cardiometabolic risk. Treatment for MetS usually focuses on addressing the relevant constituent traits either through behavioural or pharmacological interventions.
Large-scale meta-analyses confirm a globally high prevalence of MetS in young people with psychosis,18 and those trends translate into strong global associations with CVD.19 Therefore, there is an international need for new strategies to address the physical comorbidity of psychotic disorders.
The comorbidity between psychotic and cardiometabolic disorders begins early. Disrupted glucose-insulin homeostasis may pre-date the onset of psychosis,20 and clinically-relevant insulin resistance and dyslipidaemia are detectable from the onset of psychosis in relatively young antipsychotic naïve patients.21,22 Since pharmacological treatments for psychotic disorders can further exacerbate cardiometabolic dysfunction,23 it is crucial that young patients who are most at risk of adverse cardiometabolic outcomes are identified at the outset, so interventions can be directed in an informed manner. Yet, a recent systematic review of cardiometabolic risk prediction algorithms developed either for the general or psychiatric populations reported that none were likely to be suitable for young people with psychotic disorders, and commonly used algorithms substantially underpredict risk in this group.24
Recently, the first cardiometabolic risk prediction algorithm specifically tailored for young people with psychotic disorders, the Psychosis Metabolic Risk Calculator (PsyMetRiC), was developed in the UK.25 When externally validated in another UK sample, PsyMetRiC reliably predicted up-to six-year risk of metabolic syndrome, an age-appropriate precursor to CVD and early mortality.26 PsyMetRiC was designed to be clinically-useful and acceptable to young people, using only commonly recorded data. PsyMetRiC consists of two versions, the full- and partial-models, with the latter excluding biochemical predictors to cover situations where blood tests results are not available. PsyMetRiC demonstrated greater net-benefit than competing strategies across a range of feasible risk-thresholds,25 suggesting it may be clinically useful and aid in the potential to intervene before MetS has developed, reducing the chance of it developing at all.
However, prognostic algorithms can only be confirmed to be suitable for populations they have been tested in. International populations are likely to vary in ethnicity; culture and dietary habits; average population health, healthcare access; social norms, behaviours and attitudes, and legislation. Even large-scale general population-based cardiometabolic risk prediction algorithms show varying performance when tested in different populations.27, 28, 29
Therefore, following TRIPOD reporting guidelines30 (Supplementary Data), we conducted the first study to examine the international transportability of PsyMetRiC. We explored predictive performance in two independent European samples; considered recalibration approaches to create locally-calibrated PsyMetRiC versions; and examined clinical usefulness. Finally, we examined whether prior antipsychotic exposure impacted the predictive performance of PsyMetRiC.
Methods
Data sources
PsyMetab (Switzerland)
We used data from PsyMetab4: an observational prospective study of psychiatric in- and outpatients ongoing since 2007 in the Department of Psychiatry, Lausanne University Hospital, Switzerland and in a private mental health care centre (Les Toises; Lausanne, Switzerland), approved by the Ethics Committee of the Canton of Vaud. Patients were included in both inpatients and outpatient centres located in a region of about 300,000 inhabitants (Lausanne and the surrounding region). Because recruitment was conducted in different centres and institutions, selection bias in the PsyMetab cohort is low.
Briefly, metabolic parameters were collected alongside sociodemographic and lifestyle information at baseline and at 1, 3 and 12 months, and then yearly after the introduction of psychotropic medication. Informed consent was obtained for all participants, which allowed extraction of data collected before 07/08/2021. In addition, the Ethics Committee of the Canton of Vaud granted access to data of participants in the Department of Psychiatry, Lausanne University Hospital collected before 01/01/2016. The total study population featured 2,852 participants. All analyses of PsyMetab data presented herein were conducted locally in Switzerland using R version 4.1.1.31
PAFIP (Spain)
We used data from the Programa Asistencial Fases Iniciales de Psicosis (PAFIP) study,32 an ongoing longitudinal intervention program of first episode non-affective psychosis patients from “Marqués de Valdecilla” University Hospital, Santander, Spain33 since 2001, as approved by the Clinical Research Ethics Committee of Cantabria, Spain. PAFIP is an intensive early intervention service (EIS) aimed at early detection and treatment of first episode non-affective psychosis patients in Cantabria, Northern Spain. Participants or their families provided written informed consent. As a clinical program, PAFIP includes inpatient and outpatient care, and provides specific and personalized clinical attention, cognitive behavioural psychotherapeutic interventions, psychopharmacological treatment for patients, and family interventions during the first 3 years after the program intake.32 The total study population featured 885 participants. All analyses of PAFIP data presented herein were conducted locally in Spain using R version 4.1.2.31
Comparisons between study populations
The UK, Switzerland and Spain are three high-income European countries, and each are highly developed social market economies. While there are similarities between the three countries, there are notable differences also. See Supplementary Methods and Supplementary Table 1 for a detailed comparison of key sociodemographic, economic, and healthcare-related metrics between the overall British, Spanish, and Swiss populations.
Regarding the cohort regions specifically, Cantabria has a population of 535,131 inhabitants, of whom 180,717 live in the capital city, Santander. Of the employed population, 60% work in services, 32% in industry, and 8% in the primary sector. These data are similar to the rest of Spain.34 Likewise, unemployment rate trends in Cantabria over the last 40 years is representative of Spain in general, and the gross domestic product per capita in Cantabria ($25,180) is similar to wider Spain ($30,090). Although immigration rates are rising across Spain, Spanish natives still make up around 90% of the population. In Cantabria, it is estimated that around 95% of the population is White European, yet the ethnic makeup of PAFIP is similar to other Spanish psychosis cohorts.35 The sex and age distribution in PAFIP cohort is similar to that reported in other Spanish cohorts.36 No national study of the incidence of psychosis has been conducted to date in Spain,37 but the global annual incidence for psychosis in Cantabria is 1·38/10,000 person years.33 This is similar to the median values reported in other Spanish cities.36
The Lausanne region of Switzerland has a population of around 300,000, with around 140,000 living in the city itself. Of the employed population, 79% work in services, 19% in industry, and 2% in the primary sector. Migrants make up 30% of the population of the Lausanne region, slightly lower than the national prevalence (38%). The incidence of psychosis in the Lausanne region has not been reported, but the incidence of psychosis across Switzerland is in line with other developed nations.38,39 Cardiometabolic parameters of PsyMetab have been compared to the CoLaus general population cohort, finding a similar prevalence of MetS and obesity.4 In addition, national statistics from the Swiss Federal Statistical Office suggest that the prevalence of obesity in PsyMetab is similar to the Swiss general population.40 Furthermore, cardiovascular risk in PsyMetab as estimated using the Framingham Risk Score is in line with other psychiatric populations.4 Finally, the median socio-economic status in PsyMetab41 is similar to the general Swiss population,42 suggesting that the cohort is representative of the Swiss population.
Inclusion and exclusion criteria
Following the methodology from the original PsyMetRiC study,25 in both samples we excluded participants who: were aged <16y or >35y at the time of baseline assessment; had <1 year follow-up data available; met the outcome criteria at baseline; or had missing data on all predictor or outcome constituent variables. We also excluded participants who did not have a diagnosis of a psychosis-spectrum disorder at baseline (ICD-10 codes F06·0-2, F20-F31, F32·3, F33·3, F53·1 as defined in the original PsyMetRiC study25). See Supplementary Table 2 for the diagnostic classification of included participants. See Supplementary Figure 1 for a flow-chart of included participants in the study from both samples.
Outcome
As per the original PsyMetRiC study,25 we used the harmonized definition43 of MetS as a binary outcome: ethnicity-specific waist circumference ≥94 cm in males and ≥80 cm in females for Caucasians; ≥90 cm in males and ≥80 cm in females for other ethnic groups, or body mass index (BMI) >29.9; alongside two of: triglycerides ≥1.70mmol/L; high-density lipoprotein (HDL) <1.03mmol/L (males) or <1.29mmol/L (females); systolic blood pressure >130 mmHg; fasting plasma glucose (FPG) >5.60mmol/L. In each sample, where multiple follow-ups were available for each participant, we used the latest follow-up available between 1 and 6 years after baseline with the least amount of missing data (Statistical Analysis).
The PsyMetRiC algorithms
PsyMetRiC consists of two forced-entry multivariable penalized logistic regression equations: the full-model and the partial-model. Predictors were included on a balance of clinical knowledge, prior research, and likely clinical usefulness/patient acceptability. See the original PsyMetRiC study25 for further details. The partial-model was developed to cover eventualities where biochemical results may not be available. The PsyMetRiC algorithm coefficients are presented in Table 1. See the original PsyMetRiC study25 for further details. See Supplementary Table 3 for the associations of individual PsyMetRiC predictors with MetS in the PsyMetab and PAFIP samples.
Table 1.
Original PsyMetRiC Algorithm Coefficients After Shrinkage for Optimism.
| PsyMetRiC Predictor | Full-Model | Partial-Model |
|---|---|---|
| Intercept | −6.439813 | −6.973829 |
| Age in years (continuous) | 0.006233226 | 0.00633115 |
| Black/African-Caribbean Ethnicity (yes/no) | 0.004258861 | 0.07548129 |
| Asian / Other Ethnicity (yes/no) | 0.211217746 | 0.29285950 |
| Male Sex (yes/no) | 0.222300765 | 0.31460036 |
| Body Mass Index (BMI) (kg/m2) (continuous) | 0.141186241 | 0.16912161 |
| Current Smoking Status (smoker, non-smoker) | 0.153691193 | 0.24751854 |
| Prescribed a Metabolically-Active Antipsychotica (yes/no) | 0.497552758 | 0.60013558 |
| High-Density Lipoprotein (HDL) (mmol/L) (continuous) | −0.399013329 | b |
| Triglycerides (mmol/L) (continuous) | 0.343528440 | b |
See Supplementary Table 4.
Predictor not included in model.
Statistical analysis
Sample preparation and estimation of analytic precision
Biochemical values were converted to mmol/L where necessary. We assessed for the presence of predictor multi-collinearity in both samples by measuring the variance inflation factor (Supplementary Methods). Recently developed criteria44 to estimate analytic precision given the fixed sample sizes (Supplementary Methods) were applied. Briefly, the expected SEs for the C-statistic were 0.028 (PsyMetab) and 0.029 (PAFIP). The expected SEs for the calibration slope and calibration-in-the-large were 0.14 & 0.13 (PsyMetab), and 0.15 & 0.13 (PAFIP) respectively. Multiple imputation using chained equations was considered for missing data (Supplementary Methods). For numerical-based analyses, estimates were pooled using Rubin's rules. For plot-based analyses, plots were generated in each imputed dataset and checked for similarity, with one randomly selected plot per analysis presented in the main manuscript and all remaining plots presented in the Supplementary Data. Comparisons between the original PsyMetRiC development sample, PsyMetab and PAFIP samples for key sociodemographic, lifestyle and biochemical characteristics were performed using ANOVA (for means) and the chi-square equality of proportions test (for proportions).
Primary external validation analysis
The algorithms were applied to both samples independently. The distribution of predicted outcome probabilities was inspected using histograms. Algorithm performance was primarily assessed with measures of discrimination (concordance (C-) statistic), and calibration (calibration plots) (Supplementary Methods). We also recorded the Nagelkerke-Cox-Snell-Maddala-Magee r2 index, the calibration intercept (ideally close to 0), calibration slope (ideally close to 1), and the Brier score (ideally close to 0, with scores >0.25 indicating poor performance).
Recalibration and generation of site-specific PsyMetRiC versions
Given the challenges of external validation in international samples, we expected differences in calibration performance compared with the original PsyMetRiC study, which was developed in the UK. We considered a logistic calibration approach in instances where we identified miscalibration (i.e., unfavourable agreement between the observed proportion and predicted probability) on visual inspection of calibration plots. Logistic calibration takes into account differences in baseline risk that may exist between populations by re-estimating the intercept term, and also re-estimates the slope term. Therefore, logistic calibration assumes similar relative effects of the predictors but allows for larger or smaller absolute effects of the predictors.45 By completing this step, we obtained site-specific versions of PsyMetRiC (PsyMetRiC-CH and PsyMetRiC-ES) (Supplementary Methods). For all results in our analysis, as is customary in prediction modelling research, we present performance estimates accompanied by 95% CIs (derived from an alpha-value of 0.05 as commonly used in inferential statistics). However, in instances where recalibration of PsyMetRiC was conducted, as an additional sensitivity analysis we also present estimates accompanied by an adjusted confidence interval threshold. For example, where analysis was performed before and after logistic recalibration, we divided the “alpha-level” by 2 (0.05/2=0.025) and so present estimates alongside 99% confidence intervals.
Clinical usefulness
Decision curve analysis46 was used to assess clinical usefulness by estimating net benefit across a range of feasible thresholds (i.e., the risk score at which an intervention would be deemed necessary) (Supplementary Methods). We considered a risk threshold upper-bound of 0.30, which represents around a one-in-three chance of developing MetS should nothing change, because it is unlikely that risk thresholds greater than that would be tolerated without intervention. Net benefit incorporates the consequences of the decisions made on the basis of an algorithm, and is therefore preferable to related measures such as sensitivity and specificity.47 We reported the net benefit and standardized net benefit (net benefit / outcome prevalence, i.e., the additional percentage of cases that could be intervened on with use of PsyMetRiC with no increase in false-positives) across a range of reasonable risk thresholds. We drew a decision curve plot to visualise and compare the net benefit of the original vs the site-specific PsyMetRiC versions in each sample, compared with intervening in all or intervening in none. Classical decision theory proposes that at a chosen risk-threshold, the choice with the greatest net-benefit should be preferred.47
Sensitivity analyses
We performed a missing sample comparison to assess the potential impact of missing data on our results. We also examined whether nil or previous use of antipsychotic medications may affect predictive performance by repeating the analysis after excluding participants who were not antipsychotic naïve at the baseline assessment.
Data visualisation
An online data visualisation website for PsyMetRiC was created to accompany the original study (https://psymetric.shinyapps.io/psymetric). The website was updated with site-specific PsyMetRiC versions obtained through recalibration analysis. We also prepared two simulated case scenarios presented as decision trees to visualise the impact of modifiable and non-modifiable risk factors in young people with psychosis, as calculated from the recalibrated site-specific PsyMetRiC full- and partial-models (Supplementary Figure 10).
Role of the funding sources
The funding sources had no role in the study design, data collection, analysis, interpretation or writing of the manuscript.
Results
Samples
After applying inclusion criteria, we included n=558 from the PsyMetab cohort, and n=466 from the PAFIP cohort (Table 2). The PsyMetab and PAFIP samples differed from each other and from the original UK PsyMetRiC development sample on most sociodemographic, lifestyle and biochemical characteristics (Table 2).
Table 2.
Sociodemographic characteristics of the original psymetric development sample and included external validation samples.
| Characteristic | Original PsyMetRiC Development Sample (UK) | PsyMetab External Validation Sample (Switzerland) | PAFIP External Validation Sample (Spain) | Between-Group Differencesd |
|---|---|---|---|---|
| Sample before Inclusion/Exclusion Criteria Applieda, N. | 1504 | 2852 | 885 | - |
| Included sample sizea, N. (%) | 651 (43.28) | 558 (19.57) | 466 (52.66) | - |
| Age in Years, mean (SD) | 24.52 (4.91) | 25·92 (5.32) | 25·51 (4.99) | F=12.22, p<0.0001 |
| White European/NR Ethnicity, N. (%) | 360 (55.3) | 446 (79.93) | 435 (93.34) | χ=219.67, p<0.0001 |
| Black/African-Caribbean Ethnicity, N. (%) | 109 (16.74) | 68 (12.19) | 15 (3.22) | χ=49.38, p<0.0001 |
| Asian/Other Ethnicity, N. (%) | 181 (27.80) | 44 (7.48) | 16 (3.43) | χ=159.67, p<0.0001 |
| Male Sex, N. (%) | 440 (67.59) | 345 (61.83) | 303 (65.16) | χ=4.38, p=0.112 |
| HDL at baseline, mmol/L, mean (SD) | 1.88 (0.57) | 1.33 (0.36) | 1.32 (0.34) | F=303.57, p<0.0001 |
| Triglycerides at baseline, mmol/L, mean (SD) | 1.39 (1.06) | 1.16 (0.70) | 0.88 (0.40) | F=54.89, p<0.0001 |
| BMI at baseline, kg/m2, mean (SD) | 23.63 (5.43) | 23.60 (5.00) | 22.50 (3.36) | F=9.14, p<0.0001 |
| FPG at baseline (mmol/L), mean (SD) | 5.19 (1.28) | 4.95 (0.82) | 4.69 (0.55) | F=36.11, p<0.0001 |
| Systolic BP at baseline (mmHg), mean (SD) | 120.65 (11.68) | 121.32 (14.00) | 119.86 (14.10) | F=1.56, p=0.211 |
| Prescribed a More-Metabolically-Active Antipsychoticb, N. (%) | 455 (69.89) | 413 (74.01) | 234 (50.21) | χ=71.87, p<0.0001 |
| Smoking at baseline, N. (%) | 315 (48.39) | 362 (64.87) | 279 (59.90) | χ=35.40, p<0.0001 |
| Follow-up time, years, mean (SD) | 1.86 (1.32) | 2.48 (1.40) | 2.59 (0.73) | F=61.47, p<0.0001 |
| Antipsychotic Naïve at baseline, N. (%) | NR | 361 (64.70) | 433 (92.92) | χ=114.53, p<0.0001 |
| Metabolic Syndrome at baseline, N. (%)c | 49 (6.58) | 36 (6.06) | 31 (6.24) | χ=0.53, p=0.766 |
| Metabolic Syndrome at Follow-up, N. (%) | 109 (16.74) | 103 (18.54) | 66 (14.16) | χ=3.40, p=0.183 |
HDL=high-density lipoprotein; BMI=body mass index; FPG=fasting plasma glucose; BP=blood pressure; NR=Not recorded; d.f.=degrees of freedom.
See Supplementary Figure 1 for a flow-chart of included participants in the study.
Definitions of Metabolically-active antipsychotics are listed in Supplementary Table 1.
Corresponds to percentage of sample before those participants were excluded.
Analysis of means was conducted using one-way ANOVA. Analysis of proportions was conducted using the chi-square equality of proportions test.
Primary external validation analysis
PsyMetab, Switzerland
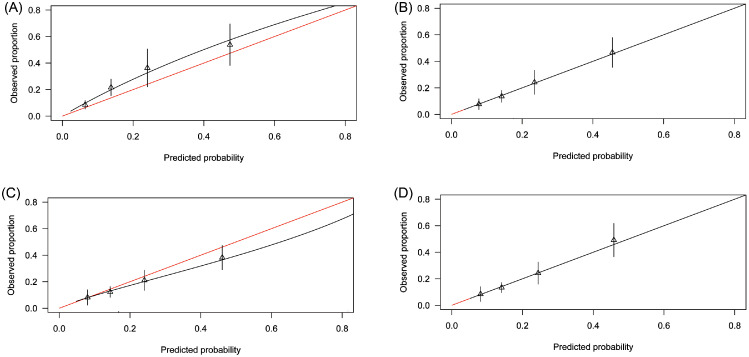
The shape of the distribution of predicted probabilities was similar to the original PsyMetRiC study (Supplementary Figure 2). Predictive performance statistics are reported in Table 3. Calibration plots for the full-model were similar across imputed datasets (Figure 1; Supplementary Figure 3) and show a systematic minor degree of risk underprediction. For the partial-model, calibration plots were similar across imputed datasets and show a minor degree of risk overprediction at higher predicted probabilities (Figure 1; Supplementary Figure 3).
Table 3.
Predictive performance statistics of the PsyMetRiC full- and partial models before and after logistic calibration in PsyMetab and PAFIP.
| Measure of Predictive Performance | Primary Analysis, Estimate (95% C.I.) |
After Logistic Calibration, Estimate (95% C.I.) |
||
|---|---|---|---|---|
| Full-Model | Partial-Model | Full-Model | Partial-Model | |
| PsyMetab (Switzerland) | ||||
| C-Statistic | 0.73 (0.68, 0.79) | 0.68 (0.62, 0.74) | 0.73 (0.68, 0.79) | 0.68 (0.62, 0.74) |
| r2 | 0.10 (0.06, 0.14) | 0.08 (0.03, 0.13) | 0.12 (0.09, 0,15) | 0.08 (0.04, 0.12) |
| Calibration Intercept | 0.11 (−0.05, 0.26) | 0.12 (0.05, 0.19) | −0.01 (−0.01, −0.01) | −0.01 (−0.01, −0.01) |
| Calibration Slope | 0.77 (0.72, 0.82) | 0.93 (0.86, 1.00) | 1.02 (1.01, 1.04) | 1.03 (1.01, 1.05) |
| Brier Score | 0.13 (0.09, 0.17) | 0.14 (0.08, 0.20) | 0.13 (0.08, 0.16) | 0.14 (0.10, 0.18) |
| PAFIP (Spain) | ||||
| C-Statistic | 0.72 (0.66, 0.78) | 0.66 (0.60, 0.71) | 0.72 (0.66, 0.78) | 0.66 (0.60, 0.71) |
| r2 | 0.10 (0.05, 0.15) | 0.05 (0.02, 0.08) | 0.10 (0.05, 0.15) | 0.05 (0.02, 0.08) |
| Calibration Intercept | 0.24 (0.09, 0.38) | −0.30 (−0.38, −0.22) | 0.01 (0.00, 0.01) | 0.01 (0.00, 0.01) |
| Calibration Slope | 1.09 (0.99, 1.20) | 0.91 (0.80, 1.02) | 1.03 (1.01, 1.05) | 1.04 (1.01, 1.06) |
| Brier Score | 0.13 (0.08, 0.16) | 0.12 (0.09, 0.16) | 0.11 (0.07, 0.16) | 0.12 (0.09, 0.16) |
The C-statistic is a measure of discrimination and estimates the probability that a randomly selected ‘case’ will have a higher predicted probability than a randomly selected non-case. Scores of 1.0 indicate perfect discrimination; scores of >0.70 are generally considered acceptable. The calibration intercept (ideally close to 0) and calibration slope (ideally close to 1) are estimates of model calibration (i.e., the agreement between the observed proportion and predicted risk). The Brier score (ideally close to 0, with scores >0.25 indicating poor performance) is an overall measure of algorithm performance. For comparison, results from the original PsyMetRiC external validation in the UK were: full-model: C=0.75 (95% C.I., 0.69–0.80; r2=0.21 (95% CI., 0.18–0.25); Brier score=0.07 (95% C.I., 0.04–0.10); intercept=-0.05 (95% C.I., −0.08, −0.02); partial-model: C=0.74 (95% C.I., 0.67–0.79); r2=0.17 (95% C.I., 0.14–0.20); Brier score=0.08 (95% C.I., 0.05–0.11); intercept=-0.07 (95% C.I., −0.11, −0.03). See the original PsyMetRiC manuscript for further details.25
Figure 1.
Calibration Plots of PsyMetRiC in PsyMetab (Switzerland). A = Primary Analysis - Full Model; B = After Logistic Calibration – Full Model; C = Primary Analysis – Partial Model; D = After Logistic Calibration – Partial Model.
Calibration plots illustrate agreement between the observed (y axis) and predicted risk (x axis). Perfect agreement would trace the red line. Algorithm calibration is illustrated by the black line. Triangles denote grouped observations for participants at deciles of predicted risk, with 95% C.I.’s indicated by the vertical black lines.
aLogistic calibration takes into account differences in baseline risk that may exist between populations by re-estimating the intercept term, and also re-estimates the slope term thus assuming similar relative effects of the predictors but allowing for a larger or smaller absolute effect of the predictors. See Methods. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
PAFIP, Spain
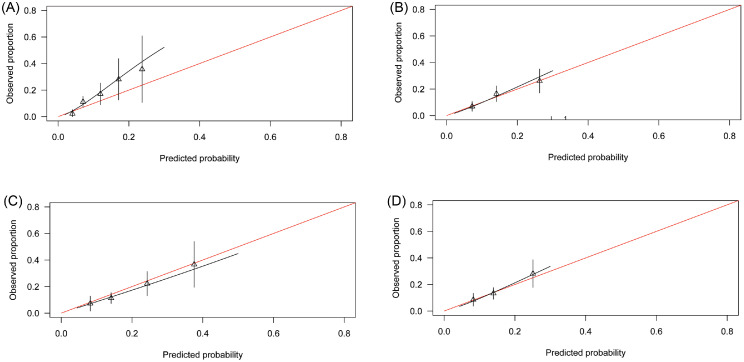
The shape of the distribution of predicted probabilities was similar to the original PsyMetRiC study (Supplementary Figure 4). Performance statistics are shown in Table 3. Calibration plots for the full-model were similar across imputed datasets (Figure 2; Supplementary Figure 5) and show a systematic degree of marked risk underprediction becoming more severe at higher predicted probabilities. For the partial-model, calibration plots were similar across imputed datasets and show good calibration (Figure 2; Supplementary Figure 5).
Figure 2.
Calibration Plots of PsyMetRiC in PAFIP (Spain). A = Primary Analysis - Full Model; B = After Logistic Calibration – Full Model; C = Primary Analysis – Partial Model; D = After Logistic Calibration – Partial Model.
Calibration plots illustrate agreement between the observed (y axis) and predicted risk (x axis). Perfect agreement would trace the red line. Algorithm calibration is illustrated by the black line. Triangles denote grouped observations for participants at deciles of predicted risk, with 95% C.I.’s indicated by the vertical black lines.
aLogistic calibration takes into account differences in baseline risk that may exist between populations by re-estimating the intercept term, and also re-estimates the slope term thus assuming similar relative effects of the predictors but allowing for a larger or smaller absolute effect of the predictors. See Methods. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Algorithm recalibration and generation of site-specific PsyMetRiC versions
PsyMetab (Switzerland)
After logistic calibration (Supplementary Table 5), the shape of the distributions of predicted probabilities were similar to the primary analysis (Supplementary Figure 2). Recalibrated performance statistics are reported in Table 3 and Supplementary Table 6. Calibration plots for both PsyMetRiC versions were similar across imputed datasets (Figure 1; Supplementary Figure 6) and showed excellent calibration.
PAFIP (Spain)
After logistic calibration (Supplementary Table 5), the shape of the distributions of predicted probabilities were similar to the primary analysis (Supplementary Figure 4). Recalibrated performance statistics are shown in Table 3 and Supplementary Table 6. Calibration plots for both PsyMetRiC versions were similar across imputed datasets (Figure 2; Supplementary Figure 7) and showed excellent calibration.
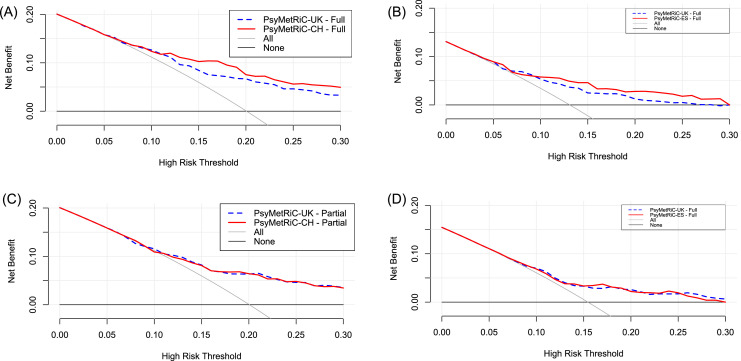
Clinical usefulness
Decision curve analysis (Figure 3, Supplementary Figure 8) showed that in both samples, PsyMetRiC provided universally greater net benefit than competing strategies. In both samples, net benefit was greater with the full-model compared with the partial model. For example, in PsyMetab, if an intervention was considered for participants scoring higher than 0.15, the recalibrated full- and partial-models provided net benefits of 0.09 (95% C.I., 0.05–0.12) and 0.07 (95% C.I., 0.04–0.10) respectively, meaning that an additional 49% of metabolic syndrome cases could be prevented with the full-model, and 38% with the partial-model. In PAFIP, at the same risk-threshold, the recalibrated full- and partial-models provided net benefits of 0.04 (95% C.I., 0.02–0.07) and 0.03 (95% C.I., 0.01–0.06) respectively, meaning that an additional 30% of metabolic syndrome cases could be prevented with the full-model, and 23% with the partial-model (Supplementary Tables 7–10). Recalibration of PsyMetRiC provided minor improvements to net benefit universally, which was more prominent with the full-model (Figure 3, Supplementary Figure 7, Supplementary Tables 7–10).
Figure 3.
Clinical Usefulness of PsyMetRiC in The PsyMetab and PAFIP Samples Before and After Logistic Calibration. A = Full-Model – PsyMetab (Switzerland); B = Full-Model – PAFIP (Spain); C = Partial-Model – PsyMetab (Switzerland); D = Partial-Model – PAFIP (Spain).
The plot reports net benefit (y axis) of PsyMetRiC Full- and Partial-Models (blue dotted line = original PsyMetRiC algorithm applied to the sample; red solid line = recalibrated site-specific version) across a range of risk thresholds (x axis) compared with intervening in all (grey solid line) or intervening in none (black solid line). In Decision Curve Analysis, it is customary to consider only the range of risk-thresholds that may reasonably be considered in clinical practice. Our upper bound of 0.30 represents around a one-in-three chance of developing MetS should nothing change, and it is unlikely that risk thresholds greater would be tolerated. Net harm (i.e., more false positives than true positives exposed to an intervention at a selected risk threshold) is indicated when the decision curve line is plotted at y<0. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Sensitivity analysis
In both cohorts, participants in the excluded sample were more likely to be older (likely due to the exclusion criteria), female, antipsychotic naïve, more likely to smoke, have a longer follow-up time, and have higher concentrations of HDL, triglycerides and FPG at baseline than participants in the included sample (Supplementary Tables 11–12).
We found that 361 (64.70%) participants of PsyMetab and 433 participants (92.92%) of PAFIP had no recorded prior use of antipsychotics at baseline assessment. The sociodemographic characteristics of those participants were similar compared with the main analysis (Supplementary Tables 13-14), but the prevalence of MetS at follow-up was slightly lower (16.90% vs 18.54% in PsyMetab, 13.16% vs 14.16% in PAFIP). Results for discrimination (PsyMetab: full-model C=0.75, 95% C.I., 0.69–0.82; partial-model: C=0.71, 95% C.I., 0.63–0.78; PAFIP: full-model C=0.72, 95% C.I., 0.65–0.79; partial-model: C=0.66, 95% C.I., 0.65–0.74) and calibration (Supplementary Figure 9) were similar in the antipsychotic naïve subsamples compared with the main analytic samples.
Discussion
We tested whether the PsyMetRiC cardiometabolic risk prediction algorithm for young people with psychotic disorders, which was developed in the UK, may be generalizable and clinically useful internationally. To do this, we performed detailed external validation analyses in two independent European samples that differed from one another and from the original PsyMetRiC development sample on a range of key sociodemographic, lifestyle and biochemical characteristics. Our results suggest that PsyMetRiC is likely to be generalisable outside of the UK, to at least some Western European nations.
We found that the discrimination performance of PsyMetRiC, as measured by the C-statistic, was similar across both samples, but as expected, slightly reduced compared with the external validation performance in the UK. As in the original PsyMetRiC study,25 we also found that the PsyMetRiC full-model discriminated cases of MetS from non-cases better than the partial-model. The better performance of the full-model which included standard blood biochemical results, reiterates that a comprehensive physical health assessment for young people with psychosis should include blood tests where possible. For example, unmedicated patients with first episode psychosis commonly present with metabolic abnormalities including insulin resistance21 and dyslipidaemia22 even in the presence of a normal BMI.20 The partial-model is unable to capture this metabolic abnormality, whereas the full-model is able, because a raised triglyceride:HDL ratio is indicative of insulin resistance48,49 and is clinically useful given that more sensitive tests, such as the homeostasis model assessment or hyperinsulinaemic-euglycaemic clamp method are not routinely available in clinical practice.
The agreement between observed and predicted risk, i.e., calibration, is equally important to algorithm predictive performance. Precise agreement between the observed and predicted risk estimates is crucial since in the future, PsyMetRiC score cut-offs may be introduced to determine eligibility (or ineligibility) for a particular intervention. For older adults in the general population, a QRISK250 score higher than 0·10 defines the need for clinical intervention, which may include prescription of a statin.51 The clinical usefulness of QRISK2 at different proposed risk thresholds has been assessed.52 An algorithm that is poorly calibrated may therefore lead to the disproportionate withholding of potentially effective interventions in some people who would benefit, and/or vice versa, thus potentially predisposing to patient harm. In our study, we found that the calibration performance of both PsyMetRiC versions was good in the PsyMetab cohort, suggesting that the PsyMetRiC risk estimates were likely to be relatively precise in that sample. However, in the PAFIP sample the full-model showed evidence of miscalibration such that PsyMetRiC underpredicted risk. This pattern of miscalibration was not evident with the partial-model, raising the possibility that the biochemical predictors included in the full-model may be one potential explanation for the miscalibration. Interestingly, the mean concentrations of triglycerides were lower in the PAFIP sample compared with the UK development and PsyMetab samples. This between-sample variability may be one contributing explanation for the miscalibration, because the algorithm coefficient for triglycerides was trained and weighted on the UK sample distribution of triglyceride levels. Therefore, the linear predictors derived from the PsyMetRiC equations may have been smaller than expected in the PAFIP sample because the distribution of triglyceride levels were lower than expected, leading to a pattern of underprediction of risk.
Despite this, calibration performance recovered fully following recalibration, without impacting discrimination performance. Nevertheless, even though our recalibration approach can be considered a relatively minor means of algorithm revision because predictor coefficients were unaltered, any change made to a previously validated algorithm necessitates the need for new external validation. Therefore, both site-specific PsyMetRiC versions (PsyMetRiC-CH and PsyMetRiC-ES) now require external validation in unseen samples from Switzerland and Spain respectively, to ensure that the site-specific versions are generalizable to the Swiss and Spanish populations, respectively.
We found that the predictive performance of PsyMetRiC did not differ depending on whether participants were antipsychotic naïve at baseline or not. This is an important finding because it was not possible in the original PsyMetRiC study25 to discern whether patients were antipsychotic naïve at baseline. That previous antipsychotic exposure had a negligible effect on algorithm predictive performance increases the likely usefulness of PsyMetRiC for psychosis early intervention services, whose newly enrolled patients might equally be referred from a general/family practitioner (and so may be antipsychotic naïve) or from a psychiatric inpatient unit (and so may have been previously exposed to an antipsychotic).
With decision curve analysis we showed that in both samples, both PsyMetRiC versions are likely to be clinically useful, and could lead to improved detection of future MetS cases in young people with psychotic disorders. In future, these individuals could be considered for targeted intervention strategies with the aim of primary prevention of more distal cardiometabolic outcomes like T2D and CVD, thus reducing long-term morbidity and mortality in this group. Decision curve analysis also showed in both samples that the full-model improved net benefit to a greater extent than the partial-model, and also that the recalibrated site-specific versions improved net benefit even further with the full-model. Yet, given that the site-specific versions require additional external validation, our results suggest that the original PsyMetRiC algorithms could be used unamended and still be clinically useful.
Despite the encouraging findings, PsyMetRiC now requires revision to further improve its accuracy, alongside further testing in UK and international samples. Regarding revision, there are several aspects of PsyMetRiC that can be improved. First, the severity of the metabolic adverse effects of different antipsychotics exists as a continuum rather than a dichotomy.23 A future revision of PsyMetRiC should seek to include antipsychotics modelled individually. Relatedly, each algorithm predictor is determined at baseline and so the potential impact of future antipsychotic switching due to adverse effects (which may or may not be cardiometabolic) and/or poor efficacy cannot be known. While our defined population consists of individuals early in the course of a psychotic disorder and the mean follow-up time of 2–3 years reduces the likelihood of multiple switches, more complex modelling strategies in sufficiently powered samples will be required to fully address this issue.
A second aspect of the PsyMetRiC algorithm that could be improved is the granularity of the ethnicity predictor. At present due to sample size limitations ethnicity is captured in three categories, yet this is likely to be an oversimplification. For example, there are clear differences in cardiometabolic risk among different Asian ethnic groups,53 and between Black Africans and Black Caribbeans.54 PsyMetRiC cannot at present capture those differences. Due to sample size limitations, we could not consider examining predictive performance stratified by ethnic group, yet even large-scale general population-based algorithms like QRISK2 and the Framingham score perform worse in ethnic minority groups.55 A future refinement of PsyMetRiC must therefore aim to capture ethnicity in greater detail, and this could be achieved in a larger, more ethnically diverse sample which may also permit analysis stratified by ethnicity, to ensure that PsyMetRiC performs equally well for all patients. Furthermore, the prevalence of cardiometabolic disorders differs between native ethnic minority groups compared with migrants,56 suggesting other factors are also relevant, such as deprivation. A deprivation score, such as the UK's Townsend deprivation index57 might also be considered in future, though this would limit international transportability.
The prevailing strength of this study is the inclusion of two relatively large independent samples from distinct European nations, each well-characterized, permitting detailed external validation analyses. Analyses were conducted independently by researchers locally in Switzerland and Spain. That the results were similar across both samples, and similar to the original PsyMetRiC study fosters confidence in the international transportability of the algorithm. We performed detailed sample size calculations to determine the likely precision of our analyses. We followed best-practice methods58 in the conduct and reporting of the analysis and adhered to TRIPOD reporting guidelines.30 Nevertheless, the results should be considered together with the following limitations. The PsyMetab study was not designed to include drug-naïve and/or early psychosis patients specifically. Drug-naïve patients were assumed as so based on having no health record of prior antipsychotic exposure. Because other institutions/private practitioners can also introduce these treatments some patients may have been misclassified. Patients with affective psychosis were not included in the PAFIP cohort, though in reality an EIS might not exclude those patients. Both the PsyMetab and PAFIP samples were less ethnically diverse that the original PsyMetRiC study. Selection bias may have affected our analysis, since we excluded participants who had complete missing data at baseline and/or follow-up. This methodological step was deemed preferable to imputing complete participant data. Multiple imputation can be biased when data are missing not at random, although we included auxiliary variables to reduce the fraction of missing information, limiting the effect of this bias. While the sample sizes of PsyMetab and PAFIP were large enough to conduct relatively precise external validation analyses, larger samples in the future will permit analyses stratified by certain protected characteristics, to ensure that the algorithm performs equally well for marginalized or under-represented groups. Finally, PsyMetRiC has only been tested in Western populations so far. To advance toward a truly globally useful tool, PsyMetRiC requires validation in diverse populations.
To conclude, we have performed the first international external validation study of the PsyMetRiC cardiometabolic risk prediction algorithm tailored for young people with psychosis, and the results suggest that its accuracy is likely to be generalizable to at least some Western European nations. This is encouraging, but further validation studies both in the UK and internationally are required before PsyMetRiC can be rolled out for routine use globally.
Data access statement
Analyses of data from PsyMetab and PAFIP were run independently by researchers in Switzerland and Spain respectively. FV and CBE directly accessed and verified the underlying data for analyses of PsyMetab. NG, VO, JV-B and BC-F directly accessed and verified the underlying data for analyses of PAFIP.
Contributors
BIP, FV, NG-T: conceptualization, investigation, methodology, project administration, resources, formal analysis, data interpretation, software, visualization, writing - original draft, writing - review & editing; EFO: resources, methodology, writing - review & editing; MP: project administration, data curation, resources, writing – review & editing; JV-B: conceptualization, investigation, project administration, resources, writing - review & editing; RU: conceptualization, supervision, writing - review & editing; CG: project administration, data curation, resources, writing – review & editing; VO: investigation, methodology, resources, formal analysis, visualization, writing - review & editing; PBJ: conceptualization, supervision, writing - review & editing; NL: project administration, data curation, resources, writing – review & editing; MR-V: investigation, methodology, writing - review & editing; JS: methodology, supervision, writing - review & editing; CD: project administration, data curation, resources, writing – review & editing; MC-R: investigation, review - writing & editing; PKM: supervision, writing - review & editing; AR-D: project administration, data curation, resources, writing – review & editing; NA: resources, writing – review & editing; EF-E: supervision, writing - review & editing; SC: resources, writing – review & editing; FG: project administration, resources, writing – review & editing; KVP: project administration, resources, writing – review & editing; PC: project administration, resources, writing – review & editing; GMK, GKM, CBE, BC-F: conceptualization, resources, project administration, supervision, writing - review & editing.
Data sharing statement
Data from PAFIP and PsyMetab cannot be publicly deposited due to patient and participant confidentiality purposes. Data from PAFIP or PsyMetab can be accessed after formal application to and ethical review by the respective scientific committee. See study group websites for further details (https://psynal.eu/ and http://www.chuv.ch/cnp-psymetab).
Declaration of interests
RU has in the past 3 years received honoraria for speaking events from Oktuska, Synovion and Vyalife; has participated as a Chair TSC for an NIHR-funded clinical trial on antipsychotic medication for treatment resistant depression, and as an Expert Member for an NIHR-funded clinical trial on psychological therapies for common mental disorders; is honorary general secretary for the British Association of Psychopharmacology and a Deputy Editor for British Journal of Psychiatry. PBJ is Chair of the MQ Mental Health Sciences Council and has participated in an advisory board for MSD on an unrelated mental health topic. FV received in the past 3 years honoraria for conferences or teaching CME courses from Forum für MedizinischeFortbildung and Sysmex Suisse AG. NA received in the past 3 years honoraria for a conference from Sysmex Suisse AG. SC received in the past 3 years honoraria for teaching CME courses from Forum pour la formation médicale, Barr Switzerland and for consultancy from the Swiss Health Observatory (Obsan) of the Swiss Federal Office of Public Health. CBE received in the past 3 years honoraria for conferences or teaching CME courses from Janssen-Cilag, Lundbeck, Otsuka, Sandoz, Servier, Sunovion, Sysmex Suisse AG, Takeda, Vifor-Pharma and Zeller. All other authors declare no potential conflicts of interest.
Acknowledgements
EFO acknowledges funding support from the Medical Research Council (MRC) and the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC). This research was supported by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. GMK acknowledges funding support from the Wellcome Trust (Intermediate Clinical Fellowship; grant code: 201486/Z/16/Z), The MQ: Transforming Mental Health (Data Science Award; grant code: MQDS17/40), the UK Medical Research Council (MICA: Mental Health Data Pathfinder; grant code: MC_PC_17213; and Therapeutic Target Validation in Mental Health; grant code: MR/S037675/1), and the BMA Foundation (J Moulton grant 2019). PBJ acknowledges funding from the MRC and MQ (as above), programmatic funding from NIHR (RP-PG- 0616-20003) and support from the Applied Research Collaboration East of England. RU acknowledges funding support from the NIHR (HTA grant code): 127700 and MRC (Therapeutic Target Validation in Mental Health grant code: MR/S037675/1). This work has been funded in part by the Swiss National Research Foundation (CE and PC: 320030-120686, 324730- 144064, and 320030-173211; CBE, PC and KJP: 320030_200602). NG-T acknowledges funding support from The Carlos III Health Institute (Rio Hortega contract: CM20/00015). JV-B acknowledges funding support from IDIVAL (grant codes: INT/A21/10 and INT/A20/04). MR-V acknowledges funding support from The Andalusian Regional Government (grant codes: A1-0055-2020 and A1-0005-2021). BC-F acknowledges the PAFIP researchers who have carried out a great number of outstanding investigations that have notably contributed to improving our knowledge in the field of early psychosis treatment. We would also like to thank the participants and their families for enrolling in these studies. The Santander (Spain) cohort was funded by the following grants to Dr Crespo-Facorro: Instituto de Salud Carlos III (grants FIS00/3095, PI020499, PI050427, and PI060507), Plan Nacional de Drogas Research (grant 2005-Orden sco/3246/2004), SENY Fundacion Research (grant 2005-0308007), Fundacion Marques de Valdecilla (grant A/02/07, API07/011) and Ministry of Economy and Competitiveness and the European Fund for Regional Development (grants SAF2016-76046-R and SAF2013-46292-R). The funding sources had no role in the writing of the manuscript or in the decision to submit it for publication.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2022.100493.
Contributor Information
Benjamin I. Perry, Email: bip20@medschl.cam.ac.uk.
Frederik Vandenberghe, Email: frederik.vandenberghe@chuv.ch.
Javier Vazquez-Bourgon, Email: javier.vazquez@scsalud.es.
Appendix. Supplementary materials
References
- 1.Plana-Ripoll O, Pedersen CB, Agerbo E, et al. A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet. 2019;394(10211):1827–1835. doi: 10.1016/S0140-6736(19)32316-5. [DOI] [PubMed] [Google Scholar]
- 2.Firth J, Siddiqi N, Koyanagi A, et al. The lancet psychiatry commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry. 2019;6(8):675–712. doi: 10.1016/S2215-0366(19)30132-4. [DOI] [PubMed] [Google Scholar]
- 3.Ride J, Kasteridis P, Gutacker N, Aragon Aragon MJ, Jacobs R. Healthcare costs for people with serious mental illness in England: an analysis of costs across primary care, hospital care, and specialist mental healthcare. Appl Health Econ Health Policy. 2020;18(2):177–188. doi: 10.1007/s40258-019-00530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dubath C, Delacretaz A, Glatard A, et al. Evaluation of cardiometabolic risk in a large psychiatric cohort and comparison with a population-based sample in Switzerland. J Clin Psychiatry. 2020;81(3) doi: 10.4088/JCP.19m12796. [DOI] [PubMed] [Google Scholar]
- 5.Vandenberghe F, Gholam-Rezaee M, Saigi-Morgui N, et al. Importance of early weight changes to predict long-term weight gain during psychotropic drug treatment. J Clin Psychiatry. 2015;76(11):e1417–e1423. doi: 10.4088/JCP.14m09358. [DOI] [PubMed] [Google Scholar]
- 6.Vazquez-Bourgon J, Mayoral-van Son J, Gomez-Revuelta M, et al. Treatment discontinuation impact on long-term (10-Year) weight gain and lipid metabolism in first-episode psychosis: results from the PAFIP-10 cohort. Int J Neuropsychopharmacol. 2021;24(1):1–7. doi: 10.1093/ijnp/pyaa066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morlan-Coarasa MJ, Arias-Loste MT, Ortiz-Garcia de la Foz V, et al. Incidence of non-alcoholic fatty liver disease and metabolic dysfunction in first episode schizophrenia and related psychotic disorders: a 3-year prospective randomized interventional study. Psychopharmacology (Berl) 2016;233(23-24):3947–3952. doi: 10.1007/s00213-016-4422-7. [DOI] [PubMed] [Google Scholar]
- 8.Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry. 2014;71(12):1350–1363. doi: 10.1001/jamapsychiatry.2014.1314. [DOI] [PubMed] [Google Scholar]
- 9.Gordon PC, Xavier JC, Louza MR. Weight gain, metabolic disturbances, and physical health care in a Brazilian sample of outpatients with schizophrenia. Neuropsychiatr Dis Treat. 2013;9:133–138. doi: 10.2147/NDT.S37019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morell R, Curtis J, Watkins A, et al. Cardio-metabolic risk in individuals prescribed long-acting injectable antipsychotic medication. Psychiatry Res. 2019;281 doi: 10.1016/j.psychres.2019.112606. [DOI] [PubMed] [Google Scholar]
- 11.Sugawara N, Yasui-Furukori N, Sato Y, et al. Comparison of prevalence of metabolic syndrome in hospital and community-based Japanese patients with schizophrenia. Ann Gen Psychiatry. 2011;10:21. doi: 10.1186/1744-859X-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saloojee S, Burns JK, Motala AA. Metabolic syndrome in South African patients with severe mental illness: prevalence and associated risk factors. PLoS One. 2016;11(2) doi: 10.1371/journal.pone.0149209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shin JA, Lee JH, Lim SY, et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig. 2013;4(4):334–343. doi: 10.1111/jdi.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112(20):3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 15.Younis A, Younis A, Tzur B, et al. Metabolic syndrome is independently associated with increased 20-year mortality in patients with stable coronary artery disease. Cardiovasc Diabetol. 2016;15(1):149. doi: 10.1186/s12933-016-0466-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boden-Albala B, Sacco RL, Lee HS, et al. Metabolic syndrome and ischemic stroke risk: Northern Manhattan study. Stroke. 2008;39(1):30–35. doi: 10.1161/STROKEAHA.107.496588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hildrum B, Mykletun A, Dahl AA, Midthjell K. Metabolic syndrome and risk of mortality in middle-aged versus elderly individuals: the Nord-Trondelag Health Study (HUNT) Diabetologia. 2009;52(4):583–590. doi: 10.1007/s00125-009-1271-5. [DOI] [PubMed] [Google Scholar]
- 18.Garrido-Torres N, Rocha-Gonzalez I, Alameda L, et al. Metabolic syndrome in antipsychotic-naive patients with first-episode psychosis: a systematic review and meta-analysis. Psychol Med. 2021;51(14):2307–2320. doi: 10.1017/S0033291721002853. [DOI] [PubMed] [Google Scholar]
- 19.Correll CU, Solmi M, Veronese N, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16(2):163–180. doi: 10.1002/wps.20420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perry BI, Stochl J, Upthegrove R, et al. Longitudinal trends in childhood insulin levels and body mass index and associations with risks of psychosis and depression in young adults. JAMA Psychiatry. 2021;78:416–425. doi: 10.1001/jamapsychiatry.2020.4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perry BI, McIntosh G, Weich S, Singh S, Rees K. The association between first-episode psychosis and abnormal glycaemic control: systematic review and meta-analysis. Lancet Psychiatry. 2016;3(11):1049–1058. doi: 10.1016/S2215-0366(16)30262-0. [DOI] [PubMed] [Google Scholar]
- 22.Pillinger T, Beck K, Stubbs B, Howes OD. Cholesterol and triglyceride levels in first-episode psychosis: systematic review and meta-analysis. Br J Psychiatry. 2017;211(6):339–349. doi: 10.1192/bjp.bp.117.200907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pillinger T, McCutcheon RA, Vano L, et al. Comparative effects of 18 antipsychotics on metabolic function in patients with schizophrenia, predictors of metabolic dysregulation, and association with psychopathology: a systematic review and network meta-analysis. Lancet Psychiatry. 2020;7(1):64–77. doi: 10.1016/S2215-0366(19)30416-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perry BI, Upthegrove R, Crawford O, et al. Cardiometabolic risk prediction algorithms for young people with psychosis: a systematic review and exploratory analysis. Acta Psychiatr Scand. 2020;142(3):215–232. doi: 10.1111/acps.13212. [DOI] [PubMed] [Google Scholar]
- 25.Perry BI, Osimo EF, Upthegrove R, et al. Development and external validation of the Psychosis Metabolic Risk Calculator (PsyMetRiC): a cardiometabolic risk prediction algorithm for young people with psychosis. Lancet Psychiatry. 2021;8(7):589–598. doi: 10.1016/S2215-0366(21)00114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 27.Read SH, van Diepen M, Colhoun HM, et al. Performance of cardiovascular disease risk scores in people diagnosed with Type 2 diabetes: external validation using data from the national scottish diabetes register. Diabetes Care. 2018;41(9):2010–2018. doi: 10.2337/dc18-0578. [DOI] [PubMed] [Google Scholar]
- 28.Damen JA, Pajouheshnia R, Heus P, et al. Performance of the Framingham risk models and pooled cohort equations for predicting 10-year risk of cardiovascular disease: a systematic review and meta-analysis. BMC Med. 2019;17(1):109. doi: 10.1186/s12916-019-1340-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pike MM, Decker PA, Larson NB, et al. Improvement in cardiovascular risk prediction with electronic health records. J Cardiovasc Transl Res. 2016;9(3):214–222. doi: 10.1007/s12265-016-9687-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594. doi: 10.1136/bmj.g7594. [DOI] [PubMed] [Google Scholar]
- 31.R Core Team. R: a language and environment for statistical computing. 2017. https://www.R-project.org/.
- 32.Son JM, Gomez-Revuelta M, Ayesa-Arriola R, et al. Comparison of aripiprazole and risperidone effectiveness in first episode non-affective psychosis: rationale and design of a prospective, randomized, 3-phase, investigator-initiated study (PAFIP-3) Rev Psiquiatr Salud Ment (Engl Ed) 2021;14(3):157–163. doi: 10.1016/j.rpsmen.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Pelayo-Teran JM, Perez-Iglesias R, Ramirez-Bonilla M, et al. Epidemiological factors associated with treated incidence of first-episode non-affective psychosis in Cantabria: insights from the clinical programme on early phases of psychosis. Early Interv Psychiatry. 2008;2(3):178–187. doi: 10.1111/j.1751-7893.2008.00074.x. [DOI] [PubMed] [Google Scholar]
- 34.Estadistica INd. INEbase: actividad, ocupación y paro. 2021. https://www.ine.es.
- 35.Garrido-Torres N, Suarez-Suarez ML, Rocha-Gonzalez I, et al. Higher rates of first episode psychosis in immigrants admitted in inpatient unit at southwest Spain. Psychiatry Res. 2022;308 doi: 10.1016/j.psychres.2021.114352. [DOI] [PubMed] [Google Scholar]
- 36.Jongsma HE, Gayer-Anderson C, Lasalvia A, et al. Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry. 2018;75(1):36–46. doi: 10.1001/jamapsychiatry.2017.3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Romero-Pardo V, Mascayano F, Susser ES, Martinez-Ales G. Schizophrenia incidence in Spain: More questions than facts. Rev Psiquiatr Salud Ment (Engl Ed) 2022;15(1):61–62. doi: 10.1016/j.rpsmen.2022.01.004. [DOI] [PubMed] [Google Scholar]
- 38.Schmid M, Michaud L, Bovio N. Guseva Canu I, Swiss National C. Prevalence of somatic and psychiatric morbidity across occupations in Switzerland and its correlation with suicide mortality: results from the Swiss National Cohort (1990–2014) BMC Psychiatry. 2020;20(1):324. doi: 10.1186/s12888-020-02733-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneeberger AR, Schwartz BJ. The Swiss mental health care system. Psychiatr Serv. 2018;69(2):126–128. doi: 10.1176/appi.ps.201700412. [DOI] [PubMed] [Google Scholar]
- 40.Federal Statistical Office Switzerland. Swiss health survey 2017: overweight and obesity. https://dam-api.bfs.admin.ch/hub/api/dam/assets/14147722/master, 2020.
- 41.Dubath C, Gholam-Rezaee M, Sjaarda J, et al. Socio-economic position as a moderator of cardiometabolic outcomes in patients receiving psychotropic treatment associated with weight gain: results from a prospective 12-month inception cohort study and a large population-based cohort. Transl Psychiatry. 2021;11(1):360. doi: 10.1038/s41398-021-01482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Panczak R, Galobardes B, Voorpostel M, et al. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health. 2012;66(12):1129–1136. doi: 10.1136/jech-2011-200699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 44.Pavlou M, Qu C, Omar RZ, et al. Estimation of required sample size for external validation of risk models for binary outcomes. Stat Methods Med Res. 2021;30(10):2187–2206. doi: 10.1177/09622802211007522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Steyerberg EW, Borsboom GJ, van Houwelingen HC, Eijkemans MJ, Habbema JDF. Validation and updating of predictive logistic regression models: a study on sample size and shrinkage. Stat Med. 2004;23(16):2567–2586. doi: 10.1002/sim.1844. [DOI] [PubMed] [Google Scholar]
- 46.Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–574. doi: 10.1177/0272989X06295361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vickers AJ, van Calster B, Steyerberg EW. A simple, step-by-step guide to interpreting decision curve analysis. Diagn Progn Res. 2019;3:18. doi: 10.1186/s41512-019-0064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murguia-Romero M, Jimenez-Flores JR, Sigrist-Flores SC, et al. Plasma triglyceride/HDL-cholesterol ratio, insulin resistance, and cardiometabolic risk in young adults. J Lipid Res. 2013;54(10):2795–2799. doi: 10.1194/jlr.M040584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pantoja-Torres B, Toro-Huamanchumo CJ, Urrunaga-Pastor D, et al. High triglycerides to HDL-cholesterol ratio is associated with insulin resistance in normal-weight healthy adults. Diabetes Metab Syndr. 2019;13(1):382–388. doi: 10.1016/j.dsx.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 50.Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–1482. doi: 10.1136/bmj.39609.449676.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Institute for Health and Care Excellence Cardiovascular disease: risk assessment and reduction, including lipid modification. Clin Guidel [CG181] 2016 London, UK. [Google Scholar]
- 52.Collins GS, Altman DG. Predicting the 10 year risk of cardiovascular disease in the United Kingdom: independent and external validation of an updated version of QRISK2. BMJ. 2012;344:e4181. doi: 10.1136/bmj.e4181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Satish P, Sadaf MI, Valero-Elizondo J, et al. Heterogeneity in cardio-metabolic risk factors and atherosclerotic cardiovascular disease among Asian groups in the United States. Am J Prev Cardiol. 2021;7 doi: 10.1016/j.ajpc.2021.100219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harding S, Silva MJ, Molaodi OR, et al. Longitudinal study of cardiometabolic risk from early adolescence to early adulthood in an ethnically diverse cohort. BMJ Open. 2016;6(12) doi: 10.1136/bmjopen-2016-013221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tillin T, Hughes AD, Whincup P, et al. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri-ethnic prospective cohort study (SABRE–Southall And Brent REvisited) Heart. 2014;100(1):60–67. doi: 10.1136/heartjnl-2013-304474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turkson-Ocran RN, Nmezi NA, Botchway MO, et al. Comparison of cardiovascular disease risk factors among African immigrants and African Americans: an analysis of the 2010 to 2016 national health interview surveys. J Am Heart Assoc. 2020;9(5) doi: 10.1161/JAHA.119.013220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the north, 1988.
- 58.Steyerberg EW, Vergouwe Y. Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J. 2014;35(29):1925–1931. doi: 10.1093/eurheartj/ehu207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.