Abstract
Background
Neurodegenerative diseases are devastating conditions that most commonly affect individuals 65 years and older. Currently there are no effective treatments or cures for neurodegenerative diseases, and therapeutics that selectively target the underlying causes of these diseases are needed. Epichaperomes play a major role in the maintenance and progression of neuronal pathology. Inhibiting epichaperomes induces degradation of disease associated proteins and is a promising therapeutic approach to treat neurodegenerative diseases, in particular Alzheimer’s Disease and amyotrophic lateral sclerosis.
Objectives
This Phase 1 clinical study evaluated the safety, tolerability, pharmacokinetics, and bioavailability of icapamespib, a purine scaffold inhibitor of epichaperomes that is specific to epichaperomes, in healthy subjects.
Design
Double-blind, placebo-controlled dose escalating single ascending dose and multiple ascending doses and an unblinded two-period cross-over bioavailability study design.
Setting
Single site in the United States.
Participants
Healthy men or women of 18 to 60 years of age, inclusive, for Part 1 (single ascending dose), ≥ 60 years of age for Part 2 (multiple ascending dose), or 18 to 49 years of age for Part 3 (bioavailability).
Treatment
In the single ascending dose group, oral single doses (10, 20, and 30 mg icapamespib or placebo) were administered to healthy non-elderly subjects. In the multiple ascending dose group, multiple doses (20 and 30 mg icapamespib once daily for 7 days or placebo) were administered to healthy elderly subjects. In the bioavailability group, the bioavailability of once daily oral icapamespib solution and tablet was assessed in healthy non elderly subjects.
Measurements
Safety was evaluated based on assessments of treatment-emergent adverse events, physical examinations, clinical laboratory tests (hematology, clinical chemistry, and urinalysis), vital signs, and 12-lead electrocardiograms. Icapamespib concentration was evaluated in plasma and cerebrospinal fluid, the latter in Part 2 (multiple ascending dose) only.
Results
Forty-eight subjects in total were randomized and assessed for tolerability, pharmacokinetics, and bioavailability parameters as follows: 24 subjects in Part 1 (single ascending dose) with PU-AD 10 mg (n = 6), 20 mg (n = 6), 30 mg (n = 6), and placebo (n = 6); 16 subjects in Part 2 (multiple ascending dose) with icapamespib 20 mg (n = 6), 30 mg (n = 6), and placebo (n = 4); and 8 subjects in Part 3 (bioavailability) crossed-over between icapamespib 30 mg (tablet) and icapamespib 30 mg (oral solution). Single doses of icapamespib up to 30 mg and multiple doses of icapamespib up to 30 mg for 7 days were generally safe and well tolerated in healthy non-elderly and elderly subjects. Treatment-emergent adverse events were mild, with headache being the most common treatment-emergent adverse event. Mean icapamespib exposure (area under the curve) was dose-proportional over the dose range tested. The median time to maximum observed plasma concentration ranged from 1.00 to 2.00 h across single ascending dose, multiple ascending dose, and bioavailability groups; icapamespib exposure was 50% higher in elderly subjects compared with non-elderly subjects but was well tolerated.
Conclusions
The study provides clinical evidence of the safety of icapamespib in healthy non elderly and elderly subjects and supports the advancement of icapamespib to Phase 2 evaluation in Alzheimer’s Disease and other neurodegenerative diseases.
Key words: PU-AD, icapamespib, PU-HZ151, epichaperome, neurodegenerative disease, Alzheimer’s disease, amyotrophic lateral sclerosis, pharmacokinetics, tolerability
Introduction
Neurodegenerative diseases (NDD) are debilitating diseases resulting in progressive degeneration and eventually death of neurons, affecting many physical and mental activities. Neurodegenerative diseases include Alzheimer’s Disease (AD) and amyotrophic lateral sclerosis (ALS), both life threatening and debilitating diseases without effective current treatment (1). Loss of proteostasis is recognized as a key initiating event in the pathogenesis of neurodegenerative conditions. Proteostasis is a coordinated network of intracellular processes of protein synthesis, folding, oligomerization, modification, localization, and degradation required to maintain the integrity of the proteome and cellular viability. Chronic stress, such as in aging and neurodegenerative diseases (NDDs), triggers imbalances in protein homeostasis resulting in misfolding, aberrant post-modifications, and aggregation of neuronal proteins (2, 3). In normal cells chaperones and regulatory proteins form complexes called chaperomes that fulfill the function of maintaining homeostasis. Under chronic stress such as in NDDs tight complexes form, called epichaperomes, which consist of chaperomes, the major heat shock proteins such as Hsp90, scaffolding and regulatory proteins to assure cell survival under the elevated proteome demand and thus propagate the cellular pathologic phenotype (3–6).
Alzheimer’s Disease is a slow, progressive neurodegenerative disease that affects over 50 million people worldwide and is the most common form of dementia (7). Alzheimer’s Disease has been defined as a protein misfolding disease (proteopathy) and is characterized by plaque formation of extracellular beta amyloid and intraneuronal abnormally folded tau protein forming paired helical filaments of hyperphosphorylated tau in the brain. Major pathological features of AD include cerebral plaques laden with beta-amyloid peptides, degeneration of neurites in neocortical terminals, medial temporal-lobe structures containing prominent neurofibrillary tangles, aggregation of phosphorylated tau, inflammation, oxidative damage, loss of neurons leading to loss of synaptic functions (8). Patients diagnosed with AD experience symptoms such as difficulty in learning, cognitive decline, and loss of memory as a consequence of decreased synaptic functions and irreparable synaptic damage.
Amyotrophic lateral sclerosis is a progressive NDD that affects nerve cells in the brain and spinal cord controlling voluntary muscle movements. Early symptoms include muscle weakness and stiffness which gradually affect all muscles under voluntary control, loss of strength and the ability to speak, eat and breathe. Most patients die from respiratory failure within an average survival time of 3 to 5 years from diagnosis. About 20% of ALS patients with certain mutations live about 5 years and 10% will survive 10 years. Currently there is no cure or disease-modifying treatment for ALS (9).
Amyotrophic lateral sclerosis is a complex disease with both environmental and genetic contributing factors, and no known general underlying cause. To date, about 30 gene mutations have been identified that cause or contribute to ALS as well as numerous cellular functions including inflammation, oxidative and endoplasmic reticulum stress, and aberrant ribonucleic acid processing. Like in many other neurogenerative diseases the hallmark of the disease is the accumulation of aggregated and misfolded proteins in the central nervous system and the inability to clear these proteins (10–12).
The formation of epichaperomes has been recognized as a major cellular event in the propagation and maintenance of diseases such as NDDs. Epichaperomes are complexes of chaperones, co chaperones and regulatory proteins nucleating on the cytosolic chaperones Hsp 90 and Hsp70, and form in response to chronic cellular stress. Epichaperomes act as protein scaffolds that pathologically remodel proteome-wide regulatory pathways and among other functions prevent the degradation of misfolded or aggregated disease associated proteins (5, 6, 13). As central players in the tau pathology, epichaperomes are involved in the causation and propagation of aberrant tau, also known as tauopathies, in neurons (14). Disruption of epichaperome complexes by icapamespib induces the degradation of misfolded proteins and restoration of cellular functions, thus representing a potentially potent treatment of diseases characterized by malfunction of proteins and pathways (15, 16). Inhibition of epichaperomes in transgenic mouse models of ALS resulted in clearance of TAR DNA-binding protein 43 or superoxide dismutase 1 and relief of ALS-like symptoms in these models (17–22).
Icapamespib (PU-AD or PU-HZ151 in previous publications) is a blood brain barrier permeable small molecule purine analogue and specifically designed to inhibit epichaperome activity. Icapamespib is highly selective for the conformationally altered Hsp90 adenosine triphosphate binding site when part of the epichaperome. Importantly, the function of Hsp90 in normal cells remains essentially unaltered by icapamespib (6). Icapamespib is selective for diseased neurons in that it targets epichaperomes and epichaperomes are only formed in diseased neurons (15, 16). In the present study, the safety, tolerability, plasma pharmacokinetics (PK), and relative bioavailability (BA, tablet vs. liquid) of icapamespib were evaluated in healthy non-elderly and elderly human subjects. Results from this trial showed that single and multiple doses of icapamespib were well-tolerated and provide support for the use of icapamespib in a future Phase 2 trial in NDDs.
Methods
Study Design
Study PU-AD-01-001 was a Phase 1, placebo-controlled study of icapamespib in healthy adults. The objectives of this study were to assess the safety, tolerability, and PK of single and multiple doses of icapamespib. The relative BA of a single 30 mg dose of icapamespib administered as an oral tablet compared to an oral solution of icapamespib was also assessed. The study consisted of 3 parts: single-ascending dose (SAD; Part 1), multiple ascending dose (MAD; Part 2), and Part 3 (BA). Part 1 (SAD) and Part 2 (MAD) were double-blind, and Part 3 (BA) was unblinded.
Study PU-AD-01-001 was conducted at ICON Early Phase Services, LLC (ICON; San Antonio, TX, USA). The study protocol was reviewed and approved by the IntegReview Institutional Review Board. In this study, ICON named an unblinded statistician to provide the randomization code. The pharmacists were unblinded. The principal investigator, site staff, subjects, and sponsor remained blinded to individual subjects’ treatment assignment for the duration of the study until study unblinding was authorized.
Single Ascending Dose (Part 1): The single dose escalation was a first-in-man evaluation of icapamespib. Three cohorts receiving 10, 20, or 30 mg of icapamespib or placebo were evaluated. The starting dose was selected in accordance with the current United States Food and Drug Administration guidance for estimating the safe starting dose in clinical studies for therapeutics in adult healthy subjects. The 10-mg dose represented a 30-fold safety margin from the human equivalent dose of the no-observed adverse event level in rats. Twenty-four healthy male and female subjects, 18 to 60 years of age, inclusive, were eligible to participate in this part of the study. Each cohort contained 8 subjects randomized to active treatment or placebo (6 subjects received icapamespib, and 2 subjects received placebo). The cohorts of Part 1 (SAD) were conducted with sentinel dosing, in which the first 2 subjects were dosed (1 active, 1 placebo) and then the remainder of the cohort (6 subjects; 5 active, 1 placebo) were randomized and dosed at least 48 hours after the sentinel dosing, provided no significant safety or tolerability issues were observed in the sentinel subjects. Subjects received an oral solution of icapamespib or placebo under fasted conditions (at least 1 hour pre-dose through 4 hours post dose).
Multiple Ascending Dose (Part 2): Part 2 consisted of 2 cohorts receiving a once daily (QD) oral dose of 20 mg or 30 mg of icapamespib or placebo for 7 days. Sixteen healthy male and female subjects, ≥ 60 years of age, participated in this part of the study. Each cohort contained 8 subjects randomized to active treatment or placebo (6 subjects received icapamespib, and 2 subjects received placebo). Subjects received an oral solution of icapamespib or placebo under fasted conditions (at least 1 hour pre-dose through 4 hours post-dose).
Bioavailability (Part 3): In Part 3 (BA), subjects received an oral solution of icapamespib or icapamespib in tablet form under fasting conditions (at least 1 hour pre-dose through 4 hours post-dose). The Part 3 (BA) cohort contained 8 subjects randomized into 2 treatment groups (4 subjects received 30 mg icapamespib oral solution in Period 1 followed by 30 mg icapamespib in tablet form in Period 2 [Group 1]; while the other 4 subjects received 30 mg icapamespib in tablet form in Period 1 followed by 30 mg icapamespib oral solution in Period 2 [Group 2]). A washout of at least 2 days occurred between doses in Period 1 and Period 2.
Subjects
Subjects signed a written informed consent form prior to enrollment into the study. Subjects were considered eligible for enrollment if they were men or women between 18 to 60 years of age, inclusive, for Part 1 (SAD), ≥ 60 years of age for Part 2 (MAD), or 18 to 49 years of age, inclusive, for Part 3 (BA); were in general good health based on medical history, physical examination, brief neurological examination, vital signs, 12-lead electrocardiogram (ECG) evaluation, and clinical laboratory evaluations; and had a body mass index within 18 to 32 kg/m2. Females in this study were of non-childbearing potential (e.g., post-menopausal or surgically sterile by hysterectomy, bilateral oophorectomy, or bilateral tubal ligation). Males who were sexually active and whose partners were females of childbearing potential agreed to use condoms from screening through 5 half lives or 90 days, whichever was longer, after administration of the last dose of study drug, and their partners used a medically acceptable method of contraception (a barrier method, intrauterine device, or hormonal contraception) from screening through 5 half-lives or 90 days after administration of the last dose of study drug. Subjects were excluded from the study if they had any of the following: history or presence of conditions, which in the judgment of the investigator, were known to interfere with the absorption, distribution, metabolism, or excretion of drugs, or that may have placed the subject at increased risk; history of surgery or major trauma within 12 weeks of screening, or surgery planned during the study; history of alcohol abuse, illicit drug use, significant mental illness, physical dependence to any opioid, or any history of drug abuse or addiction within 12 months of screening; used prescription medications within 14 days or any drugs that induced, inhibited, or were metabolized by PU-AD-specific cytochrome P450s within 14 days or 5 half-lives (if known), whichever was longer, prior to administration of the first dose of study drug; or used over the counter drugs (including herbal preparations) within 7 days or 5 half-lives (if known), whichever was longer, prior to administration of the first dose of study drug. By exception, acetaminophen 650 mg/day was permitted.
Safety Monitoring
Safety was evaluated based on assessments of treatment-emergent adverse events (TEAEs), physical examinations, clinical laboratory tests (hematology, clinical chemistry and urinalysis), vital signs, and 12-lead ECGs for Part 1 (SAD), Part 2 (MAD), and Part 3 (BA). All observed adverse events were classified by severity and relationship to treatment. Ophthalmological examinations and treatment-emergent suicidal ideation and behavior, as measured by Columbia Suicide Severity Rating Scale (C-SSRS), were evaluated for Part 2 (MAD) only.
Blood and Cerebrospinal Fluid Sampling
For Part 1 (SAD) of the study, blood samples were collected prior to dosing (0 hour) and at 0.25, 0.5, 1, 2, 3, 4, 6, 8, 12, 18, 24, 36, and 48 hours after dosing. For Part 2 (MAD), blood samples were collected prior to dosing (0 hour) and at 0.25, 0.5, 1, 2, 3, 4, 6, 9, and 12 hours after dosing on Days 1 and 7; and prior to dosing (0 hour) on days 2, 3, 4, 5, and 6. For Part 3 (BA), blood samples were collected prior to dosing (0 hour) and at 0.25, 0.5, 1, 2, 3, 4, 6, 8, and 12 hours after dosing on Day 1 during Period 1 and Period 2. The blood samples were centrifuged using a refrigerated centrifuge to separate the plasma. The plasma samples were frozen within 1 hour after collection and maintained frozen until bioanalysis. Plasma concentrations of icapamespib were determined using Turbo Ion Spray liquid chromatography with tandem mass spectrometry at Q2 Solutions Laboratories validated over the concentration range of 5.00 — 5000 ng/mL (Ithaca, NY, USA).
Cerebrospinal fluid was collected on Day 7 (between 2.5 and 4 hours post-dose) for measurement of icapamespib. Cerebrospinal concentrations were determined at Q2 Solutions Laboratories using liquid chromatography with tandem mass spectrophotometry validated over the concentration rage of 0.020 to 20 ng/mL (Ithaca, NY, USA).
Pharmacokinetic Analysis
Plasma PK parameters of icapamespib were calculated from the plasma concentration data using non compartmental methods (Phoenix WinNonlin®, Version 8.0.0.3176; Certara LP, Princeton, New Jersey, USA) and actual sampling times. The PK parameters included the maximum observed plasma concentration (Cmax), time to Cmax (tmax), area under the plasma concentration time curve (AUC) from time 0 to time of the last quantifiable concentration (AUC0-t), AUC from time 0 extrapolated to infinity (AUC0-∞), terminal elimination half-life (t1/2), terminal elimination rate constant (λz), apparent plasma clearance (CL/F), and apparent volume of distribution during the terminal phase (Vz/F). For Part 1 (SAD), the AUC from time 0 the 24 hours (AUC0-24) (the planned dosing interval for Part 2 [MAD]) was also calculated. For Part 2 (MAD), the AUC to the end of the dosing period (AUCtau), minimum plasma concentration (Cmin), and accumulation ratio based on AUCtau (Rac) were calculated. For Part 3 (BA), in addition to the parameters calculated in Part 1 (SAD), the AUC to the 12-hour time point (AUC0-12) was calculated.
Statistical Analysis
Statistical analyses were performed using SAS software (Version 9.4; SAS Institute Inc., Cary, NC USA). To assess dose proportionality following a single dose of icapamespib in Part 1 (SAD), the log transformed primary PK parameters were evaluated in a power model with log transformed dose as fixed effect. A linear regression model was fitted with the logarithm of the PK parameter (Cmax, AUCO-t, and AUC0-∞) as the dependent variable and the logarithm of the dose as the independent variable. Dose proportionality was not performed in Part 2 (MAD), as there were only 2 doses available for analysis.
To assess the relative BA of the tablet formulation of icapamespib to the oral solution of icapamespib, mixed-effects analysis of variance (ANOVA) models were used in the analysis of log transformed PU-AD PK parameters (Cmax, AUCO-t, and AUC0-∞). The ANOVA models included treatment, period, and sequence as fixed effects and subject within sequence as a random effect. The mean differences of icapamespib PK parameters (log-transformed Cmax, AUCO-t, and AUC0-∞) between the 30 mg tablet formulation and the oral solution, and the corresponding 90% confidence intervals (CIs) for the differences were calculated.
Sample Size
No formal statistical analyses were performed to determine the sample size.
Results
Subject Disposition and Demographics
A total of 48 healthy male and female subjects (24 in Part 1 [SAD], 16 in Part 2 [MAD], and 8 in Part 3 [BA]) were enrolled in Study PU-AD-01-001. No subject discontinued from the study.
A summary of the demographics of the study subjects is presented in Table 1. The median age for subjects in Part 2 (MAD; which enrolled elderly, healthy subjects) was higher than the median age for subjects in Part 1 (SAD) and Part 3 (BA). The majority of subjects in the study were white and Hispanic or Latino. In general, demographic characteristics were comparable for subjects assigned to study drug or placebo in Part 1 (SAD) and Part 2 (MAD).
Table 1.
Demographic Characteristics of Study Participants
| Demographic | Part 1 (SAD) N = 24 | Part 2 (MAD) N = 16 | Part 3 (BA) N = 8 |
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 49.4 (8.07) | 67.9 (5.47) | 37.8 (7.25) |
| Median | 49.5 | 67.0 | 39.0 |
| Min, Max | 27, 60 | 62, 79 | 24, 48 |
| Sex (n [%]) | |||
| Male | 11 (45.8%) | 6 (37.5%) | 6 (75.0%) |
| Female | 13 (54.2%) | 10 (62.5%) | 2 (25.0%) |
| Ethnicity (n [%]) | |||
| Hispanic or Latino | 17 (70.8%) | 10 (62.5%) | 5 (62.5%) |
| Not Hispanic or Latino | 7 (29.2%) | 6 (37.5%) | 3 (37.5%) |
| Race | |||
| Asian | 1 (4.2%) | 0 | 0 |
| Black or African American | 4 (16.7%) | 1 (6.3%) | 2 (25.0%) |
| White | 16 (79.2%) | 14 (87.5%) | 6 (75.0%) |
| Other | 0 | 1 (6.3%) | 0 |
| Weight (kg) | |||
| Mean (SD) | 76.48 (11.49) | 72.38 (11.27) | 79.80 (18.91) |
| Median | 76.40 | 70.35 | 70.75 |
| Min, Max | 57.5, 101.2 | 53.2, 91.2 | 60.9, 118.7 |
| Height (cm) | |||
| Mean (SD) | 165.40 (10.85) | 163.48 (11.04) | 171.61 (11.64) |
| Median | 164.65 | 158.95 | 171.45 |
| Min, Max | 151.5, 191.1 | 148.0, 188.2 | 158.0, 195.0 |
| Body Mass Index (kg/m2) | |||
| Mean (SD) | 27.85 (2.27) | 27.04 (3.03) | 26.79 (3.34) |
| Median | 27.35 | 27.35 | 26.40 |
| Min, Max | 23.9, 32.0 | 20.9, 31.1 | 22.9, 31.2 |
Abbreviations: MAD = multiple ascending dose; Max = maximum; Min = minimum; N = total number of subjects; SAD = single ascending dose; SD = standard deviation;
Note: Percentages are calculated as 100 ⋆ (number of subjects [n]/N).
Safety and Tolerability
Single doses of icapamespib up to 30 mg were generally well tolerated in healthy adults, and multiple doses of icapamespib up to 30 mg once-daily for 7 days were generally well tolerated in healthy elderly adults. No dose limiting TEAEs were observed.
In Part 1 (SAD, non-elderly population), 4 subjects (16.7%) reported 5 TEAEs. No subject reported a TEAE in the 10 mg dose group or placebo group. The most frequently reported TEAE was headache (2 events in 2 subjects overall [8.3% of subjects]); followed by somnolence, dry mouth, and influenza-like illness, which occurred as 1 event each (1 subject overall [4.2% of subjects]). All 5 TEAEs were classified as mild in severity and assessed by the investigator to be related to study drug.
In Part 2 (MAD, elderly population), 8 subjects (50.0%) reported 11 TEAEs. The most frequently reported TEAE was headache (5 events in 4 subjects overall [25.0% of subjects]); followed by constipation, diarrhea, back pain, musculoskeletal discomfort, decreased systolic blood pressure, and phlebitis, which occurred as 1 event each (1 subject overall [6.3% of subjects]). Of the 11 TEAEs, all were classified as mild in severity with the exception of 3 Grade 2 (moderate) TEAEs (headache [3 events]). Of the 11 TEAEs reported, 2 were considered by the investigator to be related to study drug (headache [2 events]).
In Part 3 (BA), 2 subjects (25.0%) reported 5 TEAEs. The most frequently reported TEAE was increased orthostatic heart rate response (3 events in 2 subjects overall [25.0%]); followed by blurred vision and postural dizziness, which occurred as 1 event each (1 subject overall [12.5% of subjects]). All 5 TEAEs were classified as mild in severity. Of the 5 TEAEs reported, 4 were considered by the investigator to be related to study drug (increased orthostatic heart rate response [3 events] and postural dizziness [1 event]).
No serious adverse events or deaths occurred during the study. No TEAE lead to study drug withdrawal or study discontinuation. Clinically significant abnormalities were not observed in vital signs, laboratory measurements, ECG findings, physical examination findings, ophthalmic examinations, or C-SSRS scores.
Single-dose Escalation Pharmacokinetics in Healthy Adults
Single dose PK parameters and dose proportionality of PU-AD were evaluated in Part 1 (SAD) (Cohorts 1, 2, and 3) in subjects receiving active treatment. Plasma PK parameters for icapamespib administered as single oral doses of 10, 20, and 30 mg of icapamespib to healthy adults are summarized in Table 2. The mean plasma concentration time profiles of icapamespib following single doses are shown in Figure 1A. Geometric mean peak plasma concentrations of icapamespib (Cmax) increased in a dose proportional manner over the dosing regimen of 10 to 30 mg. Icapamespib exposure steadily increased as doses approached the highest dose level tested. The median tmax was approximately 1.50 hours for 10, 20, and 30 mg single doses. The geometric mean AUC0-t and AUC0-∞ measurements increased over the dose range (10 to 30 mg) among subjects in Cohorts 1, 2, and 3. Dose proportionality for AUC0-∞was not assessed since extrapolation could only be performed in 2 subjects in Cohort 1. The 90% CI for the slope of the regression line for Cmax and AUC0-t included 1. While not adequately powered, icapamespib exposure appeared to increase in a dose-proportional manner over the single dose range of 10 to 30 mg. The t1/2 was short for all doses based on a half-life range of 1.72 to 2.19 hours. Plasma concentrations of oral icapamespib in all subjects were measurable up to 4 hours after the 10 mg dose and up to 6 hours post administration of 20 mg and 30 mg single doses. As shown in Figure 1A, several healthy subjects had measurable plasma concentrations 12 hours after the administration of the 20 mg (1 subject) and 30 mg (3 subjects) doses, respectively. In Part 1 (SAD), inter-subject variability presented as geometric percent coefficient of variation (GeoCV%) was higher (ranging from 56 to 103 GeoCV %) at 10 mg in Cohort 1 compared with Cohorts 2 (20 mg) and 3 (30 mg). This could be attributed to the length of time over which concentrations remained above the lower limit of quantitation among dose groups. The CL/F and Vz/F were similar across single oral doses of icapamespib. The elimination of icapamespib appeared to follow a biphasic pattern for all doses tested.
Table 2.
Summary of Statistics of Plasma Icapamespib Pharmacokinetic Parameters Following a Single Dose of 10, 20, or 30 mg Icapamespib (Evaluable PK Population)
| Parameter | Statistic | Cohort 1 – 10 mg PU-AD (N=6) | Cohort 2 – 20 mg PU-(N=6) | Cohort 3 - 30 mg PU-AD N=6) |
|---|---|---|---|---|
| tmax (h) | n | 6 | 6 | 6 |
| Median | 1.51 | 1.50 | 1.50 | |
| (Min, Max) | (1.00, 3.00) | (0.53, 3.00) | (0.50, 6.00) | |
| Cmax (ng/mL) | n | 6 | 6 | 6 |
| GeoMean | 23.1 | 50.0 | 76.5 | |
| GeoCV% | 77.4 | 36.2 | 34.3 | |
| AUC0-t (ng⋆h/mL) | n | 6 | 6 | 6 |
| GeoMean | 69.6 | 220 | 385 | |
| GeoCV% | 103 | 58.9 | 54.8 | |
| AUC0-∞ (ng⋆h/mL) | n | 2 | 6 | 5 |
| GeoMean | 193 | 239 | 398 | |
| GeoCV% | 55.8 | 56.0 | 61.4 | |
| AUC0-24 (ng⋆h/mL) | n | 3 | 6 | 5 |
| GeoMean | 144 | 239 | 397 | |
| GeoCV% | 69.5 | 56.0 | 61.1 | |
| t1/2 (h) | n | 3 | 6 | 5 |
| Mean | 2.19 | 1.72 | 2.16 | |
| SD | 0.0365 | 0.227 | 0.742 | |
| CL/F (L/h) | n | 2 | 6 | 5 |
| GeoMean | 51.8 | 83.5 | 75.3 | |
| GeoCV% | 55.8 | 56.0 | 61.4 | |
| Vz/F (L) | n | 2 | 6 | 5 |
| GeoMean | 174 | 205 | 224 | |
| GeoCV% | 37.3 | 41.6 | 29.0 |
Abbreviations: AUC = area under the plasma concentration-time curve; AUC0-24 = AUC from time 0 to 24 hours postdose; AUC0-∞ = AUC from time 0 to infinity; AUC0-t = AUC from time 0 to last quantifiable concentration; CL/F = apparent oral clearance; Cmax = maximum observed plasma concentration; CV% = percent coefficient of variation; Geo = geometric; GeoCV% = geometric coefficient of variation; Max = maximum; Min = minimum; N = total number of subjects; n = number of nonmissing observations; PK = pharmacokinetic; SD = standard deviation; t1/2 = terminal elimination half-life; Tmax = time to Cmax; Vz/F = apparent volume of distribution associated with the terminal phase.
Figure 1.
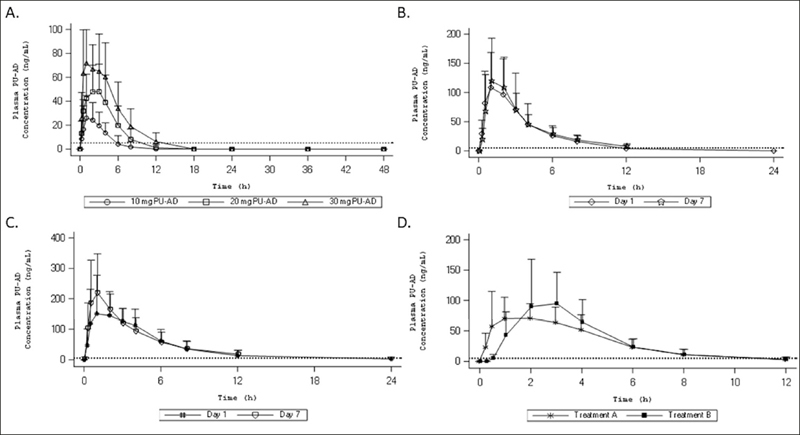
Mean (+ SD) Plasma Concentration-Time Profiles for Icapamespib Following Oral Administration
A) Mean (+ SD) Plasma Concentration-Time Profiles for Icapamespib Following Oral Administration of a Single Dose of 10, 20, or 30 mg Icapamespib Linear Plots (PK Full Population). Concentrations that are below the limit of quantitation (BLQ) are treated as zero. Dotted line represents below the BLQ (5.00 ng/mL). Cohort 1: 10 mg icapamespib or placebo; Cohort 2: 20 mg icapamespib or placebo; or Cohort 3: 30 mg icapamespib or placebo. B) Mean (+ SD) Plasma Concentration-Time Profiles for Icapamespib Following Oral Administration of a Single and Multiple Dose of 20 mg Icapamespib Linear Plots of Days 1 and 7 (PK Full Population, elderly subjects). Concentrations BLQ are treated as zero. Dotted line represents BLQ (5.00 ng/mL). Cohort 4: 20 mg icapamespib or placebo. C) Mean (+ SD) Plasma Concentration-Time Profiles for Icapamespib Following Oral Administration of a Single and Multiple Dose of 30 mg Icapamespib Linear Plots of Days 1 and 7 (PK Full Population, elderly subjects). Concentrations BLQ are treated as zero. Dotted line represents BLQ (5.00 ng/mL). Cohort 5: 30 mg icapamespib or placebo. D) Mean (+ SD) Plasma Concentration-Time Profiles for Icapamespib Following Oral Administration of a Single Dose of 30 mg Solution or Tablet of Icapamespib Linear Plots (PK Full Population). Concentrations BLQ are treated as zero. Dotted line represents BLQ (5.00 ng/mL). Cohort 6: Treatment A: 30 mg icapamespib solution; Treatment B: 30 mg icapamespib tablet
Multiple Dose Escalation Pharmacokinetics in Healthy Adults Over 60 Years of Age
Multiple dose PK parameters of icapamespib in healthy, elderly subjects were evaluated in the Part 2 (MAD; Cohorts 4 and 5). Plasma PK parameters for icapamespib following oral administration of single or multiple QD doses of icapamespib at 20 or 30 mg are summarized in Table 3. Single and multiple dose mean plasma concentration-time profiles of icapamespib are shown in Figures 1B and 1C, respectively. On Day 1 and Day 7, mean plasma concentration time profiles increased in a dose-proportional manner and were similarly depicted by semi logarithmic plots for each dose. The elimination of icapamespib exhibited a biphasic profile following single and multiple oral administrations of 20 mg and 30 mg doses. Variability of the Cmax and AUCtau were moderate to high after single and multiple doses of icapamespib (20 and 30 mg), shown by the GeoCV% range of 45 to 65%. Both Cmax and AUCtau geometric mean values were lower in the 20 mg cohort than in the 30 mg cohort. Median tmax was approximately 1 hour for both single and multiple doses of icapamespib. Since Part 2 (MAD) only tested 2 dose levels, dose proportionality of the PK parameters was not assessed. Accumulation for Cmax and AUCtau was not observed following 7 QD doses of either 20 or 30 mg icapamespib.
Table 3.
Summary Statistics of Plasma Icapamespib Pharmacokinetic Parameters and CSF Following a Single and Multiple Dose of 20 or 30 mg Icapamespib in Elderly Volunteers (Evaluable PK Population)
| Parameter | Statistic | Cohort 4 – 20 mg PU-AD (N=6) | Cohort 5 - 30 mg PU-AD (N=6) | ||
|---|---|---|---|---|---|
| Day 1 | Day 7 | Day 1 | Day 7 | ||
| tmax (h) | n | 6 | 6 | 6 | 6 |
| Median | 1.00 | 1.00 | 1.00 | 1.00 | |
| (Min, Max) | (1.00, 2.00) | (1.00, 2.00) | (0.50, 4.00) | (0.50, 3.00) | |
| Cmax (ng/mL) | n | 6 | 6 | 6 | 6 |
| GeoMean | 106 | 115 | 162 | 215 | |
| GeoCV% | 49.0 | 45.1 | 57.9 | 46.0 | |
| AUC0-t (ng⋆h/mL) | n | 6 | 6 | 6 | 6 |
| GeoMean | 374 | 447 | 764 | 868 | |
| GeoCV% | 67.0 | 41.8 | 72.0 | 42.5 | |
| AUCtau (ng⋆h/mL) | n | 6 | 6 | 6 | 6 |
| GeoMean | 414 | 489 | 908 | 943 | |
| GeoCV% | 62.2 | 39.6 | 64.5 | 45.1 | |
| CL/F (L/h) | n | 6 | 6 | 5 | 6 |
| GeoMean | 48.3 | 40.9 | 33.0 | 31.8 | |
| GeoCV% | 62.2 | 39.6 | 64.5 | 45.1 | |
| Vz/F (L) | n | 6 | 6 | 6 | 6 |
| GeoMean | 182 | 195 | 132 | 157 | |
| GeoCV% | 65.1 | 48.8 | 51.2 | 36.9 | |
| Rac | n | N/A | 6 | N/A | 5 |
| GeoMean | N/A | 1.18 | N/A | 1.13 | |
| GeoCV% | N/A | 23.4 | N/A | 30.3 | |
| CSF | n | N/A | 6 | N/A | 6 |
| GeoMean | N/A | 0.821 | N/A | 1.39 | |
| GeoCV% | N/A | 58.52 | N/A | 43.23 | |
Abbreviations: AUC = area under the plasma concentration-time curve; AUCtau = AUC over the dosing interval; AUC0-t = AUC from time 0 to last quantifiable concentration; CL/F = apparent oral clearance; Cmax = maximum observed plasma concentration; CSF = cerebrospinal fluid; CV% = percent coefficient of variation; Geo = geometric; GeoCV% = geometric coefficient of variation; Max = maximum; Min = minimum; N = total number of subjects; n = number of nonmissing observations; N/A= not available; PK = pharmacokinetic; Rac = accumulation ratio; Tmax = time to Cmax; Vz/F = apparent volume of distribution associated with the terminal phase.
The blood-brain barrier penetration of icapamespib in healthy elderly subjects was also evaluated in Part 2 (MAD). On Day 7, multiple doses of icapamespib resulted in geometric mean cerebrospinal fluid (CSF) concentrations of 0.821 ng/mL after the administration of 20 mg and 1.39 ng/mL after the administration of 30 mg. Detectable CSF concentrations of icapamespib illustrate icapamespib penetration of the blood-brain barrier.
Relative BA of Single Dose Icapamespib Solution and Tablet in Healthy Subjects
In Part 3 (BA), mean plasma concentration-time profiles of icapamespib solution (30 mg) and icapamespib tablet (30 mg) formulations were evaluated in healthy subjects. Plasma PK parameter data of oral single dose solution and tablet formulations of icapamespib are presented in Table 4. Administration of the icapamespib tablet showed higher mean plasma concentration time measurements and a delayed peak compared with the solution formulation, shown in Figure 1D. However, plasma concentrations of the tablet formulation were more variable. Both formulations showed elimination profiles that appeared to be biphasic in nature. Variability of Cmax and AUC values ranged from moderate to high (GeoCV% range of 48 to 70%) for both solution and tablet treatments of icapamespib. The Cmax after the administration of the icapamespib tablet was 31% higher than that of the oral solution but the AUCs were similar. Both treatments resulted in a median tmax of 2 hours post-dosing with a range of 2.04 to 2.18 hours in healthy subjects. The CL/F and Vz/F values resulted in similar measurements across the oral solution and tablet formulations of icapamespib.
Table 4.
Summary Statistics of Plasma Icapamespib Pharmacokinetic Parameters Following an Oral Administration of a Single Dose of 30 mg Oral Solution or Tablet Icapamespib
| Parameter | Statistic | Cohort 6 | |
|---|---|---|---|
| 30 mg PU-AD Solution (N=6) | 30 mg PU-AD Tablet (N=6) | ||
| tmax(h) | n | 8 | 8 |
| Median | 2.00 | 2.00 | |
| (Min, Max) | (0.50, 4.00) | (1.00, 3.00) | |
| Cmax (ng/mL) | n | 8 | 8 |
| GeoMean | 79.9 | 105 | |
| GeoCV% | 56.5 | 60.6 | |
| AUC0-t (ng⋆h/mL) | n | 8 | 8 |
| GeoMean | 330 | 325 | |
| GeoCV% | 53.1 | 69.5 | |
| AUC0-∞ (ng⋆h/mL) | n | 8 | 7 |
| GeoMean | 357 | 393 | |
| GeoCV% | 49.9 | 58.8 | |
| AUC0-12 (ng⋆h/mL) | n | 8 | 7 |
| GeoMean | 346 | 381 | |
| GeoCV% | 47.9 | 58.8 | |
| t1/2 (h) | n | 8 | 7 |
| GeoMean | 2.18 | 2.04 | |
| GeoCV% | 0.79 | 0.80 | |
| CL/F (L/h) | n | 8 | 7 |
| GeoMean | 84.0 | 76.3 | |
| GeoCV% | 49.9 | 58.8 | |
| Vz/F (L) | n | 8 | 7 |
| GeoMean | 250 | 211 | |
| GeoCV% | 44.3 | 51.9 | |
Abbreviations: AUC = area under the plasma concentration-time curve; AUC0-12 = AUC from time 0 to12 hours post-dose; AUC0-∞ = AUC from time 0 to infinity; AUC0-t = AUC from time 0 to last quantifiable concentration; CL/F = apparent oral clearance; Cmax = maximum observed plasma concentration; CV% = percent coefficient of variation; Geo = geometric; GeoCV% = geometric coefficient of variation; Max = maximum; Min = minimum; N = total number of subjects; n = number of non-missing observations; PK = pharmacokinetics; SD = standard deviation; t1/2 = terminal elimination half-life; Tmax = time to Cmax; Vz/F = apparent volume of distribution associated with the terminal phase; Note: Cohort 6: Treatment A = 30 mg PU-AD Solution; Treatment B = 30 mg PU-AD Tablet.
Discussion
Icapamespib, a purine scaffold inhibitor of epichaperomes, has demonstrated an inhibitory effect on neurodegenerative-related cellular mechanisms in nonclinical models (14, 16). These promising findings from icapamespib studies have presented an opportunity to address the therapeutic challenges with AD.
In this Phase 1, double-blind, placebo-controlled study, single oral doses (up to 30 mg) and multiple oral doses (up to 30 mg) of icapamespib were generally safe and well-tolerated in healthy non-elderly and elderly adults. No trend nor significant change from baseline was observed in vital signs, laboratory tests, physical examination findings, or ECG results. The reported TEAEs were mild or moderate. None of the reported TEAEs resulted in the mortality of any study subject, any study drug discontinuation, or any subject withdrawal.
The icapamespib PK following single and multiple oral doses were also evaluated in non elderly and elderly, healthy subjects. In the Part 1 (SAD) cohorts, single oral doses of 10, 20, and 30 mg of icapamespib or placebo produced detectable levels of icapamespib in plasma of healthy, non elderly subjects. Icapamespib exposure showed a short t1/2 (1.72 to 2.19 hours) and geometric mean plasma concentrations that increased from the lowest to highest dose in a dose proportional manner in healthy subjects over the dose range of 10 mg to 30 mg. The tmax of icapamespib was approximately 1.50 hours for 10, 20, and 30 mg doses. In the Part 2 (MAD) cohorts, QD oral doses of 20 and 30 mg of icapamespib over a treatment period of 7 days showed higher plasma concentrations of icapamespib in healthy, elderly subjects compared with the Part 1 (SAD) cohorts. Plasma concentrations of icapamespib increased (geometric mean Cmax and AUCtau) after administration of both a single and multiple QD dose of 20 or 30 mg of icapamespib. For single and multiple doses of 20 and 30 mg, the median time to icapamespib Cmax was approximately 1 hour. Dose proportionality was not assessed, as only 2 dose levels were evaluated. However, the mean icapamespib multiple dose exposure data appears to have a greater than proportional increase. Following multiple doses of icapamespib, Rac values were close to 1 on Day 7 (1.18, Cohort 4; 1.13, Cohort 5). The CL/F and Vz/F measurements were similar for Day 1 and Day 7 for the 20 and 30 mg doses but were higher for the lower dose level compared with the 30 mg dose. The Rac values close to 1 suggested no accumulation of icapamespib following multiple doses.
Following multiple QD doses, geometric mean CSF concentrations of icapamespib on Day 7 were 0.821 ng/mL and 1.39 ng/mL for the 20 and 30 mg doses, respectively. These data are consistent with expected free concentrations of icapamespib in plasma at the time of CSF sampling and indicate that PU-AD did penetrate the blood brain barrier. In preclinical studies in mice using LC-MS/MS analysis following oral administration of 10 mg/kg PU-AD about 70% of plasma concentration was found in brain tissue. This was corroborated by using 131I-PU-AD and gamma counting of radioactivity in mice. In a Parkinson’s disease mouse model, a dose of 6 mg/kg administered orally, daily was an effective dose to decrease several Parkinson’s symptoms (Samus, unpublished observations). In humans, using 124I-PU-AD PET analysis in a subject with no brain lesions, and therefore no epichaperomes, AUC values for brain were equal to that determined in lung and muscle. Uptake of 124I-PU-AD in brain was rapid and due to the lack of epichaperomes secretion from brain was also rapid with t1/2 3h (6).
One difference in the PK of icapamespib between elderly and non-elderly subjects was the higher exposure observed following single doses (20 and 30 mg) on Day 1 in Part 2 (MAD; elderly) compared with the same doses in Part 1 (SAD; non-elderly). At the dose levels of 20 and 30 mg, icapamespib mean geometric AUC0-t values (374 and 764 ng⋆h/mL) in healthy elderly subjects on Day 1 were approximately 50% higher relative to AUC0-t values determined (220 and 385 ng⋆h/mL) in healthy non-elderly subjects on Day 1 after a single dose. Mean geometric clearance of icapamespib was lower in Part 2 (MAD) on Day 1 with elderly subjects (48.3 and 33.0 L/h) compared with the non-elderly population in Part 1 (SAD; 83.5 and 75.3 L/h). After the administration of the 30 mg dose, the apparent volume distribution was higher in healthy non elderly subjects in Part 1 (SAD; 224 L) compared with Part 2 (MAD) on Day 1 (132 L). However, apparent volume distribution was comparable at the 20 mg dose level in both Part 1 (SAD) and Part 2 (MAD).
The relative BA of a single dose icapamespib was also assessed between 2 formulations of icapamespib. An oral solution and oral tablet of icapamespib at a single dose level of 30 mg were evaluated in healthy non-elderly subjects. Washout periods used in Part 3 (BA) would normally have been 7 days but were truncated by coronavirus disease-19 rules precluding multiple clinic re entries. The icapamespib tablet formulation achieved a Cmax that was 31% higher compared to the oral solution with no increase in AUC. Both the solution and tablet formulations had a median tmax of 2.00 hours and had comparable t1/2 values (2.04 to 2.18 hours). The CL/F and Vz/F of icapamespib were similar for both the tablet and solution formulations. These data support the use of a tablet formulation in future studies.
Collectively, the clinical evidence has shown a safe and well-tolerated product with a well characterized PK profile. These results warrant further evaluation of icapamespib in Phase 2 clinical studies of AD and other NDDs.
Conflicts of Interest: GB and BW are full-time employees of Samus Therapeutics. SD is a former full-time employee of Samus Therapeutics. MS is a paid consultant of Samus Therapeutics and represents Samus Therapeutics as a medical expert on multiple safety review committees. CK, MM, LR and BS are employees of ICON, a contract service provider for Samus Therapeutics.
Ethical standards: This study was conducted in accordance with the Declaration of Helsinki, the International Conference on Harmonization Good Clinical Practice guideline, and local regulatory requirements. The study protocol was approved by an institutional review board at the study site. All patients provided written consent before the start of the study. The study is registered at ClinicalTrials.gov (NCT03935568).
References
- 1.Cavazzoni P. The path forward: Advancing treatments and cures for neurodegenerative diseases, congressional testimony. FDA. 2021. https://www.fda.gov/news-events/congressional-testimony/path-forward-advancing-treatments-and-cures-neurodegenerative-diseases-07292021. Accessed 25 May 2022
- 2.Hipp MS, Kasturi P, Hartl FU. The proteostasis network and its decline in ageing. Nat Rev Mol Cell Biol. 2019;20(7):421–435. doi: 10.1038/s41580-019-0101-y. [DOI] [PubMed] [Google Scholar]
- 3.Taipale M, Tucker G, Peng J, et al. A quantitative chaperone interaction network reveals the architecture of cellular protein homeostasis pathways. Cell. 2014;158(2):434–448. doi: 10.1016/j.cell.2014.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taipale M, Jarosz DF, Lindquist S. HSP90 at the hub of protein homeostasis: emerging mechanistic insights. Nat Rev Mol Cell Biol. 2010;11(7):515–28. doi: 10.1038/nrm2918. [DOI] [PubMed] [Google Scholar]
- 5.Inda MC, Joshi S, Wang T, et al. The epichaperome is a mediator of toxic hippocampal stress and leads to protein connectivity-based dysfunction. Nat Commun. 2020;11(1):319. doi: 10.1038/s41467-019-14082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolaender A, Zatorska D, He H, et al. Chemical tools for epichaperomemediated interactome dysfunctions of the central nervous system. Nat Commun. 2021;12(1):4669. doi: 10.1038/s41467-021-24821-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Breijyeh Z, Karaman R. Comprehensive review on Alzheimer’s disease: causes and treatment. Molecules. 2020;25(24):5789. doi: 10.3390/molecules25245789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun W, Samimi H, Gamez M, et al. Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies. Nat Neurosci. 2018;21(8):1038–1048. doi: 10.1038/s41593-018-0194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talbott EO, Malek AM, Lacomis D. The epidemiology of amyotrophic lateral sclerosis. Handb Clin Neurol. 2016;138:225–38. doi: 10.1016/B978-0-12-802973-2.00013-6. [DOI] [PubMed] [Google Scholar]
- 10.Masrori P, Van Damme P. Amyotrophic lateral sclerosis: a clinical review. Eur J Neurol. 2020;27(10):1918–1929. doi: 10.1111/ene.14393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mejzini R, Flynn LL, Pitout IL, et al. ALS genetics, mechanisms, and therapeutics: where are we now? Front Neurosci. 2019;13:1310. doi: 10.3389/fnins.2019.01310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xu X, Shen D, Gao Y, et al. A perspective on therapies for amyotrophic lateral sclerosis: can disease progression be curbed? Transl Neurodegener. 2021;10(1):29. doi: 10.1186/s40035-021-00250-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodina A, Wang T, Yan P, et al. The epichaperome is an integrated chaperome network that facilitates tumour survival. Nature. 2016;538(7625):397–401. doi: 10.1038/nature19807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carman A, Kishinevsky S, Koren J, 3rd, et al. Chaperone-dependent neurodegeneration: a molecular perspective on therapeutic intervention. J Alzheimers Dis Parkinsonism. 2013;2013(Suppl10):007. doi: 10.4172/2161-0460.S10-007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luo W, Sun W, Taldone T, et al. Heat shock protein 90 in neurodegenerative diseases. Mol Neurodegener. 2010;5:24. doi: 10.1186/1750-1326-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiosis G. Editorial (Thematic Issue: Heat shock proteins in disease — from molecular mechanisms to therapeutics) Curr Top Med Chem. 2016;16(25):2727–8. doi: 10.2174/156802661625160816181132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalmar B, Greensmith L. Cellular chaperones as therapeutic targets in ALS to restore protein homeostasis and improve cellular function. Front Mol Neurosci. 2017;10:251. doi: 10.3389/fnmol.2017.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kieran D, Kalmar B, Dick JR, et al. Treatment with arimoclomol, a coinducer of heat shock proteins, delays disease progression in ALS mice. Nat Med. 2004;10(4):402–5. doi: 10.1038/nm1021. [DOI] [PubMed] [Google Scholar]
- 19.San Gil R, Ooi L, Yerbury JJ, et al. The heat shock response in neurons and astroglia and its role in neurodegenerative diseases. Mol Neurodegener. 2017;12(1):65. doi: 10.1186/s13024-017-0208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morrice JR, Gregory-Evans CY, Shaw CA. Animal models of amyotrophic lateral sclerosis: A comparison of model validity. Neural Regener Res. 2018;13(12):2050–2054. doi: 10.4103/1673-5374.241445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lutz C. Mouse models of ALS: Past, present and future. Brain Res. 2018;1693:1–10. doi: 10.1016/j.brainres.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 22.Mandrioli J, Crippa V, Cereda C, et al. Proteostasis and ALS: protocol for a phase II, randomised, double-blind, placebo-controlled, multicentre clinical trial for colchicine in ALS (Co-ALS) BMJ Open. 2019;9(5):e028486. doi: 10.1136/bmjopen-2018-028486. [DOI] [PMC free article] [PubMed] [Google Scholar]


