Abstract
Cardiovascular disease (CVD) remains the leading cause of death in the United States today and a major contributor to total health care costs. Psychosocial stress has been implicated in CVD, and psychosocial approaches to primary and secondary prevention are gaining research support. This third article in the series on psychosocial stress and CVD continues the evaluation of one such approach, the Maharishi Transcendental Meditation® program, a psychophysiological approach from the Vedic tradition that is systematically taught by qualified teachers throughout the world. Evidence suggests not only that this program can provide benefits in prevention but also that it may reduce CVD-related and other health care expenses. On the basis of data from the studies available to date, the Transcendental Meditation program may be responsible for reductions of 80% or greater in medical insurance claims and payments to physicians. This article evaluates the implications of research on the Transcendental Meditation program for health care policy and for large-scale clinical implementation of the program. The Transcendental Meditation program can be used by individuals of any ethnic or cultural background, and compliance with the practice regimen is generally high. The main steps necessary for wider adoption appear to be: (1) educating health care providers and patients about the nature and expected benefits of the program, and (2) adjustments in public policies at the state and national levels to allow this program to be included in private and public health insurance plans.
Keywords: meditation and cardiovascular disease, preventive cardiology, psychosocial interventions for CVD, team approach in CVD prevention
According to the World Health Organization (WHO), cardiovascular diseases (CVDs) cause the premature deaths of as many as 17 million people a year worldwide.1 In the United States, the annual death rate from heart disease and stroke is nearly 1,000,000, with an annual cost of $396 billion.2–4 This is half the estimated cost of all chronic diseases in this country.5 Furthermore, the portion of the US population with these and other chronic diseases rose from 22% in 1935 to 45% in 1987, the latest available analysis.5 Thus, CVD is a major cause of the high disease rates and health care costs in the United States today, and the health care community is searching for new ways to reduce the costs and human suffering caused by this disease.
The authors of the WHO MONICA Project propose that death and disability from heart disease could be cut by more than 50% through a combination of simple, cost-effective actions to reduce major risk factors, such as high blood pressure, high cholesterol, obesity, and smoking.1 As reviewed in part 1 of this series, psychosocial stress can contribute to all these risk factors and to most other aspects of the progression of CVD, including the clustering of traditional risk factors, endothelial dysfunction, atherosclerosis, myocardial ischemia, plaque rupture, thrombosis, and lethal arrhythmias.6 Because of such effects, psychosocial stress is being recognized as a major contributor to the outcomes of CVD and other chronic diseases. For example, studies indicate that 40% of deaths7 and 70% of diseases8,9 in the United States are caused in whole or part by stress-related lifestyle patterns, such as smoking, drug and alcohol abuse, poor diet, and physical inactivity.
Part 2 in this series reviewed research on the clinical effectiveness of approaches to reducing the physiological and behavioral effects of psychosocial stress, with a focus on one such approach, the Transcendental Meditation (TM) program.10 The TM program alone or in combination with other approaches may support a continued decline in CVD risk factors, CVD morbidity and mortality, and health care costs. The present article focuses on the effects of the TM program on health insurance claims, along with the evaluation of additional issues important for health care policy and the large-scale implementation of the program. These issues include: (a) degree of standardization of instructional procedures, (b) availability of properly trained instructors, (c) competency of patients to comply with the intervention, (d) prior record of patient compliance, (e) cost reimbursement, and (f) an empirically testable hypothesis or theory by which to understand the intervention and its effectiveness.
The task of achieving widespread implementation of any effective psychosocial intervention is largely dependent on the proper education of doctors and patients. The need to revise medical practice and medical education to emphasize more comprehensive, prevention-oriented approaches is urgent and widely recognized.11 Less than 6% of the US health care budget is devoted to medical and lifestyle changes that focus on preventing the onset or progression of atherosclerotic heart disease,4 with the majority of the total health care budget being spent for acute and chronic disease care. Despite the paucity of funds going to prevention, a systematic team approach to reducing the social burden of CVD has proven practical.12 Such teams typically include nurses, nutritionists, exercise physiologists, and behavioral experts, along with the treating physician, and are promoted by many in the field of preventive cardiology.13 Addition of new psychosocial interventions, such as the TM program, even if it necessitates adding another team member, may be a prudent path to further reductions in the burden of CVD.
RESEARCH ON HEALTH INSURANCE CLAIMS AND PHYSICIAN REIMBURSEMENTS
Formal cost-effectiveness studies for psychosocial intervenions are rare. A few studies have been conducted on risk-factor management through specific changes in lifestyle,14 with smoking cessation and exercise programs being the main areas studied.14–18 Exercise training and unsupervised exercise programs are taught by special instructors, can be practiced long term on one’s own, and can be combined generally with other interventions, including the TM program. The following studies of effects of the TM program on insurance claims and physician reimbursements, the only studies of this type found through extensive literature searches and personal contacts with researchers, may have implications for cost-effectiveness. Furthermore, the results of these studies appear to confirm the predictions of effective CVD prevention based on the clinical trials and laboratory research reviewed in part 2 of this series9 and offer additional evidence that this program could be a sound addition to preventive cardiology.
MEDICAL INSURANCE UTILIZATION
Although formal cost-effectiveness research has not been performed on the TM program to date, 4 studies have been conducted on the possible influence of this program on medical insurance usage. Two of these studies were in the United States and 2 in the Canadian province of Quebec. The data for these studies were provided by the carrier’s annual reports (US) and by the government health insurance agency for the province of Quebec.
Lower Inpatient and Outpatient Claims
The first investigation into the effects of the TM program on medical insurance claims compared 5 years of claim statistics from 2,000 TM practitioners with claim statistics from the database norm for all 600,000 members under the same main carrier (Blue Cross/Blue Shield).19 The TM group was represented by all members of a special insurance group whose only requirement for membership was that individuals sign an affidavit stating that they had practiced the TM technique regularly for at least 6 months and that they intended to continue the practice. Eighty percent of the membership in this group was distributed throughout the United States. Researchers tested the hypothesis of a difference in claims between the TM and control groups using the chi-square statistic, with utilization rates for the control groups as the expected values. The TM group had significantly lower medical claims in all disease categories for both inpatient and outpatient treatments. The TM group had 53% and 44% fewer inpatient and outpatient admissions, respectively, for the average of all 17 major illness treatment categories (Figure 1). The largest reduction (87%) was for the category of heart and blood vessel diseases. Similar results were obtained when comparing the TM group with 5 demographically matched control groups of similar size and benefits.19
FIGURE 1.
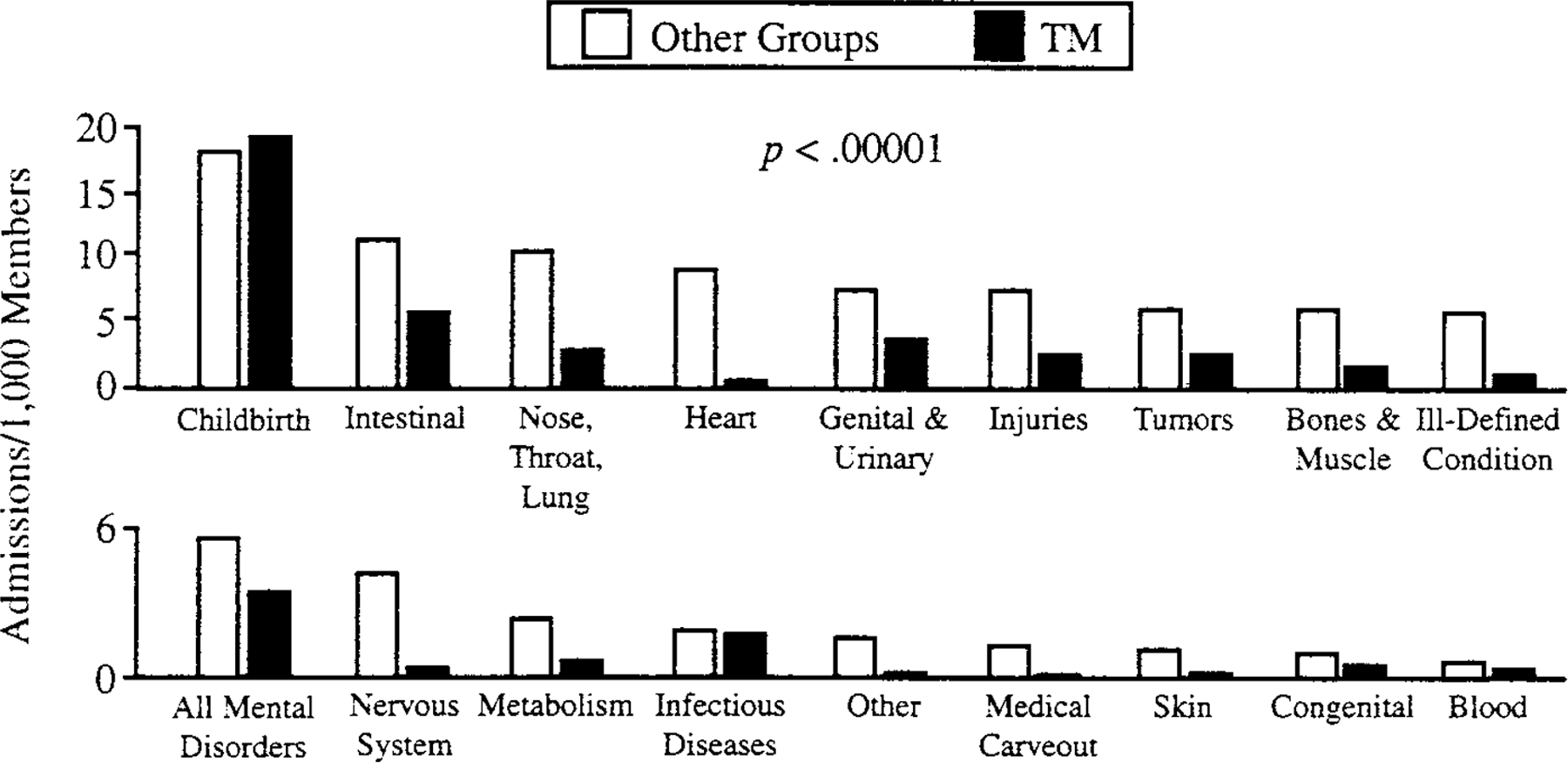
Hospital admissions rate in 18 treatment categories for the 2,000-member transcendental meditation (TM) group and the 600,000-member normative control group.
Source. Orme-Johnson,19 reprinted with permission.
This was a retrospective study, and subjects had no prior knowledge that their claims data would later be used in research. Participation in the study, instruction in the TM program, or any aspect of the practice of TM are not likely to have influenced subjects who were ill to voluntarily reduce their claims by avoiding needed treatments. Moreover, the admissions rate for childbirth in the TM group was identical to that of the normative group, suggesting that the lower admissions rates for the various other treatment areas actually reflected lower disease rates or less debilitating diseases in this group.
A later retrospective study20 assessed the impact of the TM program when combined with other components of Maharishi Consciousness-Based Health Care (also known as the Maharishi Vedic Approach to Health—MVAH), of which the TM program is a key part. Medical insurance claims of all of the members of the faculty and staff of Maharishi University of Management (mean = 693), where everyone practices the TM program and most also use one or more of the other modalities of Maharishi Consciousness-Based Health Care, such as herbal food supplements and specific dietary changes, were compared with claims of a demographically matched control group (n = 4,148) and with a large normative database (n = 600,000), again using archival health insurance annual reports provided by the insurance carrier Blue Cross/Blue Shield of Iowa. For heart or vessel disease, hospital admission rates for the MVAH group were reduced by 92% when compared with the normative group, and somewhat more when compared with the matched control group. This is close to the 87% reduction obtained with the TM program alone in the more diverse group described above, which was studied before the other modalities of MVAH became available in the United States. Researchers observed similar reductions in hospitalization and outpatient rates and for total length of hospitalizations across all 11 years under observation. The greatest savings were observed among patients older than 45 years. When all disease categories were combined, the 11-year mean total expenditure per person in the MVAH group was 63% lower than in the normative control. Although the savings in expenditures were not calculated for heart or vessel diseases, the greater reduction in claims for this disease category in the MVAH group would make the percentage reduction in expenditures greater than 63%.
The main limitation of these 2 studies was the lack of information on the health insurance claims of TM subjects prior to their starting the program. It is possible that TM subjects were healthier even before they began the practice. This limitation may not be a serious one because published studies on the TM program that compared controls with those who would later learn TM have not found significant differences, nor have differences been found between groups of subjects who are interested in learning TM compared with groups who are not interested.21,22 Also, the 2 studies described next did control for health care expenses prior to learning TM, with no indication of a difference between the control subjects and the TM subjects prior to learning the technique.
Payments to Physicians in Quebec
Physicians’ expenses in Canada are covered by government insurance agencies. Two studies in the province of Quebec by Herron et al23 made use of available government statistics to estimate effects of the TM program on medical expenditures. Herron et al recruited volunteer study participants practicing TM by distributing questionnaires to the program participants who attended events at their local TM Center and by mailing questionnaires to program participants throughout the province. These researchers did not offer any financial or other incentives for participation in the study. They retrospectively followed physician reimbursements for treating TM subjects, made available by the government health insurance agency for the province of Quebec for several years before subjects elected to begin the TM program and retrospectively or prospectively for several years after starting the program. No breakdown of expenditures by disease type was available. However, the worldwide preponderance of CVD, especially in technologically developed countries, makes it likely that the Canadian outcomes also reflect a substantial component of CVD-related physician costs.
Payments to medical doctors in the United States and Canada are approximately 20% of the total annual medical spending.24 These payments provide a reasonable estimate of total medical expenses, because doctors’ decisions determine most other medical expenditures, such as hospitalization, prescription medications, medical tests, and further doctor’s visits.
In the first study, Herron et al analyzed data from 677 practitioners of the TM program for 3 years before and 3 years after beginning the program.23 At the time of their decision to begin the TM program, subjects were not aware that they would later be asked to participate in a research study of this sort. Because there was no separate control group in this study, the subjects’ physician payment records prior to beginning the program served as the control. In the 3 years before starting the practice, there was no significant change in payments to physicians. In the 3 years after beginning, however, payments declined significantly (p < .05), by 5% to 7% annually.23
The second study expanded on the first one in 3 ways: (1) by increasing the number of TM subjects to 1,418; (2) by adding a control group in which each TM subject was matched through random selection (executed by the government health insurance agency) to a comparison subject from all non-TM insurance enrollees of the same age, sex, and region as the TM subject; and (3) by the addition of 2 more years of data before starting and 3 more years after starting the TM program.24 For the 5 years before the TM group started the TM program, the 2 groups did not differ in rate of increase in payments to physicians (p > .17). After beginning the program, however, payments for the TM group decreased by an average of more than 13% per year for the next 6 years, in comparison with the matched controls (p = .0017).
In a subanalysis of all 163 TM participants aged older than 65 years,25 Herron and Cavanaugh compared inflation-adjusted payments to physicians with payments to physicians for 163 control subjects matched for age, sex, and median preintervention payments. They used separate least squares regressions for pre- and postintervention periods to estimate yearly changes in payments. Prior to learning TM, changes in payments were not different between groups (p = .27). After learning the TM technique, the annual change for TM subjects was significantly lower than for controls (p = .001), resulting in a 5-year cumulative reduction of 69.8% relative to controls. This outcome agrees well with sub-analyses of the older subgroups in the 2 health insurance studies described earlier.19,20
A noteworthy limitation in the design of these quasi-experimental Canadian studies relates to the generalizability of the results. The protocol for selecting volunteers was not designed to reach all potential subjects in Quebec who had learned the TM program nor to track the response rate of those who were contacted. Thus, the subjects who chose to learn the TM program may not have been representative of the general population. Likewise, those practitioners who chose to enter the study were not necessarily representative of the population of individuals who begin TM. The individuals involved made both choices (self-selection), and such choices might conceivably be related to open-mindedness or some other quality relevant to potential to improve. Nevertheless, the ability of the TM program to promote a reduction in health care costs in a significant number of people is consistent with the outcomes of the clinical trials, where volunteer subjects were randomly assigned to learn the program.10
NATURE AND EFFECTS OF TM
The TM program is one of many methods that have been used for reducing stress or reducing the effects of stress. Other approaches include autogenic training techniques, biofeedback methods, progressive muscle relaxation, concentrative meditation, clinically standardized meditation, relaxation response techniques, cognitive techniques, hypnosis, psychotherapy, mindfulness meditation, and a variety of other techniques. The nature and efficacy of these approaches vary widely. Meta-analyses showing the effectiveness of psychosocial interventions for improving the outcomes in coronary artery disease have typically lumped many approaches together rather than compared the effectiveness of different individual approaches.25–28 Ten meta-analyses of outcomes from 475 studies of different approaches that may be relevant to preventive cardiology show that techniques derived from the oldest traditions (eg, the Vedic tradition) tend to be the most effective in producing the specified outcomes.29 Among all the approaches, the TM technique appears to have been the most thoroughly studied.30
ORIGIN AND STANDARDIZED INSTRUCTION
The TM program was introduced to the West in 1957, when Maharishi Mahesh Yogi, a teacher and scholar in the Vedic tradition, first began teaching it on a wide scale.31 The TM technique is both taught and practiced systematically in the same way worldwide. Teachers are trained over a period of 1 year, with the extensive, in-residence component of the training lasting 4 to 8 months, depending on the type of course. The technique is said to have been available from the beginning of the Vedic tradition, but Maharishi Mahesh Yogi standardized the instructional procedure for people of all cultural and educational backgrounds.31 This universal applicability and the worldwide availability of the identical instruction methods are important characteristics of the program.
Taught in a standardized 7-step program over a period of 4 to 7 days, the TM program is easy to learn and practice. The instructional procedure includes the following 7 steps: Step 1—Introductory Lecture: A vision of the possibilities through the Maharishi TM program (1 hour); Step 2—Preparatory Lecture: The mechanics and origin of the TM program (1 hour); Step 3—Personal Interview: Interview with a qualified teacher (15 minutes); Step 4—Personal Instruction: Learning the technique (1 hour); Step 5: Verification and validation of experiences, part 1: Verifying the correctness of the practice (90 minutes); Step 6—Verification and validation of experiences, part 2: Understanding the mechanics of stabilizing the benefits (90 minutes); and Step 7—Verification and validation of experiences, part 3: Understanding the mechanics of the development of higher states of consciousness through the TM technique (90 minutes). Both the interview (Step 3) and personal instruction (Step 4) are private, involving only the teacher and the pupil. Other meetings are generally held in a group to increase the number and types of individual experiences that are discussed. This allows the pupils to gain a deep understanding of correct and incorrect practice and to explore in detail the range of results expected from the practice. This 7-step course fully trains the students to continue the TM program on their own, but to ensure maintenance of correct practice and to further strengthen each pupil’s understanding of the mechanics and benefits of the program, follow-up advanced lectures and individual checking of meditation are recommended. These are included in the one-time fee.
HOLISTIC BENEFITS
The benefits of the TM program are said to be holistic, according to evidence in more than 600 published articles from 200 universities and research institutions in 30 countries.9,32–34 Beneficial effects are apparent at the psychological, physiological, behavioral, and sociological levels.
The outcomes examined in meta-analyses of the effects of the TM technique include substance use (cigarettes, alcohol, and illicit drugs), anxiety, hypertension, physiological signs of stress, affective health, and overall mental health. Individual meditation programs other than the TM program have not been examined in a sufficient number of studies to evaluate their effectiveness using the meta-analytic approach. However, in the meta-analyses conducted to date, when results of the TM program were compared with the outcomes of other meditation techniques, the TM program has always shown the largest effect sizes, in some cases 2 and 3 times larger than combinations of other meditation techniques or of other approaches to stress reduction.29 A theory providing the basis for understanding the physiological changes underlying the effectiveness of the TM program exists and has been an area of research focus.
A large portion of the observed benefits can be explained by the ability of the program to reduce stress and the effects of stress, particularly the long-term deleterious effects of stress.35 In this context, stress is viewed as anything that activates the adaptive mechanisms of the body. The concept, in the Vedic tradition, that a basic field of intelligence or consciousness is primary and that the mind and body, along with behavior and social actions, derive from this field, is a major part of the theory underlying the TM technique and other components of the Maharishi Consciousness-Based Health Care system.36
The health implications of an inner intelligence that underlies all expressed values of mind, body, and behavior have not been addressed by modern health care. On the basis of this unique theory and its supporting research, the Maharishi Consciousness-Based Health Care approach has already provided a number of solutions to the problems facing modern medicine.37 The TM program, and the more advanced TM-Sidhi program, are consciousness-based technologies found to promote the health of all aspects of life—mental, physical, behavioral, and social.
COMPLIANCE
Compliance with the recommended regimen of twice-daily practice of the TM program (15–20 minutes each time) has been surprisingly high, varying from 70% to 97% in the clinical trials reviewed in part 2 or reported elsewhere.10,38,39 These data were obtained from monthly logs of the starting times for each practice session recorded by the patients. Patients returned these logs monthly to clinic personnel, not to program instructors. Even in elderly African Americans, where compliance with pharmaceutical treatments is notoriously low, the rate of compliance with the TM program has been as high as 97%.39 The conditions of these clinical trials encouraged patients to maintain a schedule of frequent contacts with their TM instructors, which generally serves as a reinforcer. Similar conditions could be maintained easily in normal medical practice if an instructor were an integral part of a team approach to CVD care.
Compliance with conventional CVD treatments and risk-reduction approaches is approximately 33% over the long term.40 This low compliance rate continues to plague these therapies, but has been somewhat overcome through the use of the team approach to CVD treatment.12,40 Instructors in different aspects of the treatment regimen, whether doctors, nurses, exercise trainers, psychologists, or other specialists, can help improve compliance with the treatment regimen by focusing with the patient on a particular approach.
THEORY AND MECHANISM OF EFFECTS OF TM ON HEALTH
The occurrence of beneficial effects from the practice of the TM program, even in apparently healthy individuals, is consistent with the origins and theoretical conception of this program.31 The standardized TM technique derives from an ancient tradition of knowledge, the Vedic tradition, in which an understanding of both subjective and objective realities is propounded as more complete in many ways than that of modern science.
The realization that the TM technique was not developed as a treatment for disease but rather as a means of enhancing growth of human awareness, indeed growth of the entire human potential, is crucial to understanding effects of the TM technique. Integral to understanding its mechanism of effects is the description of higher states of consciousness, as outlined by Maharishi Mahesh Yogi.31,41 Higher states, although not precluding experiences of the usual waking, dreaming, and sleeping states, are characterized by physiological and mental phenomena distinct from these 3 states. Aside from descriptions of higher states in the Vedic literature and the personal reports of practitioners of the TM program, a growing body of empirical evidence indicates that these states confer greater abilities for successful interactions with the internal and external environments.41–46
Particularly relevant to the ability of the TM technique to lower psychosocial stress or to correct deleterious effects of stress are the results of studies suggesting restoration of adaptive mechanisms by this technique.47–51 Adaptive mechanisms involving the autonomic nervous system, neuroendocrine axes, and the cardiovascular system are responsible for maintaining a stable and efficient functional state of the physiology through the frequently changing conditions of life.52,53 These mechanisms are altered by psychosocial stress in ways that decrease their ability to foster effective adaptation, thereby leading to physical and mental declines. Allostatic load is a term applied to such alterations of adaptive mechanisms. Allostatic load is an index of the wear and tear on the body caused by repeated or prolonged experiences of stress; increased allostatic load predicts not only declines in cognitive and physical functioning but also increased CVD events and risk.52–54
From the perspective of Maharishi Consciousness-Based Health Care, it is the inner intelligence of the body that maintains optimal mental and physical functioning in life.37 The ability of the TM technique to beneficially affect adaptive mechanisms and thereby reduce allostatic load is consistent with this Vedic understanding. Beneficial effects of the TM program include improved functioning of autonomic, neuroendocrine, and metabolic systems, as reviewed in part 2 of this series and elsewhere.10,35,50 Furthermore, accumulating evidence supports the theory that the ability of TM to promote the experience of transcendental or pure consciousness (the first higher state of consciousness described in the Vedic tradition) is what makes the technique effective in normalizing adaptive mechanisms.41,42,45,46 A more extensive analysis of the mechanisms through which the TM program might specifically affect risk for and recovery from CVD is beyond the purview of this article, but some of the possibilities are explored in more detail elsewhere, including effects on blood pressure48,55 and on health-related behaviors such as smoking and alcohol consumption.56
The following are reasons for using the Transcendental Meditation program in preventative cardiology and CVD treatment programs: (1) Lowers cardiac events—both morbidity and mortality; (2) Reduces both traditional and psychosocial risk factors; (3) Has beneficial effects on the pathophysiological mechanisms mediating CVD; (4) Is low in cost compared with surgical procedures and most drug-based interventions; (5) Can be used by anyone regardless of educational, ethnic, and cultural background; (6) Has high compliance with the recommended twice-daily schedule of practice; (7) Has a uniform, 7-step instruction that leads to the same, standardized practice by everyone; (8) Has a wide availability of trained teachers who could participate in a team approach; (9) Is backed by a testable theory.
THE NEED FOR EDUCATION
Much to its detriment, and despite evidence of an epidemic of iatrogenic disease—disease produced by medical treatment—modern medicine has been slow to recognize the potential offered by some psychosocial or mind and body interventions. Epidemiological research indicates that 180,000 people die in the United States each year from problems that are partly or completely iatrogenic,57 dwarfing the mortality rate caused by automobile accidents (45,000) and exceeding those from all other accidents combined.58 This unfortunate situation is borne out in the cardiovascular arena as well. Studies exist showing that the choice of treatment is a vital factor in determining how quickly, after a first infarction, a patient will suffer a second infarction, and how likely the second one is to be fatal. For example, a study tracking 920 heart attack patients found that after the first arrest, a significantly greater number in the group receiving surgical treatment died or had another heart attack, compared with a group receiving noninvasive treatment.59 Furthermore, results of a study of 208 cardiac arrests in people undergoing modern treatments reported that at least 9% could have been prevented; medication errors and toxic effects of drugs were the leading causes of these potentially preventable iatrogenic arrests.60 Observations such as these offer evidence that modern medicine can be deadly and should be open to fundamentally different approaches that may be less risky. Although it is now widely recognized that medical training and practice must emphasize more comprehensive, effective approaches to disease prevention and health promotion,11 alternatives to high-tech, drag-centered therapies and diagnostic procedures have been largely ignored, even in the face of evidence that more than 40% of patients use alternative therapies.61,62
Fortunately, however, some practitioners of modern medicine are beginning to learn about natural, complementary therapies, either through their own independent inquiries or through introductory or continuing-education courses that provide knowledge of these topics. A recent survey found that more than 60% of all physicians make referrals to natural practitioners and that nearly 25% of the modern practitioners use complementary techniques in their own practice.63 This trend is supported by public opinion. A survey found that 89% of the American public is dissatisfied with the current status of medical practices and desires fundamental change in the direction and structure of the US health care system.64 A review in the Journal of NIH Research concluded that conventional health care practitioners need to know more about the research and medical practice modalities of natural and complementary medicine, and that physicians should be educated to understand how and where natural medical practices fit into the health care delivery system.65
Partly in response to this need for greater knowledge of natural and complementary medical practice, the United States Congress and the National Institutes of Health established the Office of Alternative Medicine, which later became the National Center for Complementary and Alternative Medicine. This initiative has inspired medical schools to offer courses on natural and complementary medicine, and such courses have become popular at most medical schools.66 However, with few exceptions, these courses offer only a brief, fragmented exposure to natural and complementary medicine techniques. Most of them attempt to cover an eclectic array of approaches,66 many of which have not been studied or have not proven effective.29
Against this backdrop, several avenues are open for providing knowledge of the TM program and the Maharishi Consciousness-Based Health Care system. Through new courses in existing schools and through adding new schools specializing in this knowledge, the TM program could be quickly integrated into treatment and prevention strategies. This may be the most effective means to enhance the use of these more comprehensive, scientifically tested technologies in mainstream health practice.
EDUCATING DOCTORS AND THE PUBLIC ON THE BENEFITS
In addition to trained teachers of the TM program in most cities, doctors and college-level instructors are available who are qualified to give out information on the TM program as an adjunct treatment or prevention modality. Instructors can be accessed through several organizations, mainly the Maharishi Vedic universities, colleges, and schools, which have campuses or facilities in most states of the United States and in most countries of the world. The College of Maharishi Consciousness-Based Health Care in Fairfield, Iowa, a part of Maharishi University of Management, offers accredited degree programs to train health consultants and health educators in providing prevention-oriented, natural healthcare that is reported to be free of hazardous side effects and effective in promoting perfect health.
These educational programs not only offer the means for individuals to become qualified in the use of the Maharishi Consciousness-Based Health Care system, but also provide an environment and daily schedule conducive to development of higher states of consciousness. The students practice the technologies of consciousness as part of their training. In addition, short courses for medical doctors and other health professionals are offered so these professionals can learn about the medical use of the TM program and other aspects of the Maharishi Consciousness-Based Health Care program. These short courses for professionals are generally offered at selected sites around the country, but could be taught on a periodic basis at any university or college if the demand is sufficient. In addition, courses taught on the Internet and through communication satellites could be developed through Maharishi Open University, a university conducted over satellite television channels, by simply adding classes to existing satellite programming in most countries.
Given adequate demand for the courses, educating doctors and health professionals on the nature and benefits of TM and other Maharishi Consciousness-Based Health Care programs appears simple. Consequently, the most expeditious method for reaching the general public may be accomplished by first training existing doctors and paramedical professionals in the nature and availability of these programs through courses at Maharishi Open University. In the 33rd Bethesda Conference, which focused on preventive cardiology, presenters emphasized the value of the inclusion of nonphysician personnel and community resources in preventing CVD.13,67 This means that practices specializing in CVD could be encouraged to use a team approach and to include a TM teacher or a specialist in the whole range of Maharishi Consciousness-Based Health Care programs. And in practices where the team approach to CVD treatment and secondary prevention is already used,12 doctors could refer their patients to a team member who is a qualified TM instructor or a health consultant trained in Maharishi Consciousness-Based Health Care programs. The beneficial effects of the TM program have been obtained in minority ethnic groups as well as majority groups, and in many countries and cultures of the world.36,38,39,68
POLICY RECOMMENDATIONS
In addition to the aforementioned recommendations in the area of education, there are other recommendations that can be made regarding providers, certification and licensure, reimbursement, and implementation of the TM program or other aspects of the Maharishi Consciousness-Based Health Care program.
WHO SHOULD PROVIDE THESE SERVICES
Currently, the TM program is provided mainly by specially trained teachers in most cities. However, a few doctors and college-level instructors are available who are qualified to give information on the TM program as an adjunct treatment or prevention modality. Also, physicians and other licensed modern health professionals who have received this specialized training as part of their continuing education practice the Maharishi Consciousness-Based Health Care program. Trained professionals with a bachelor’s degree, PhD degree, or certificate from the College of Maharishi Consciousness-Based Health Care at Maharishi University of Management in Iowa may practice either as consultants to licensed physicians or independently as unlicensed practitioners.
Two categories of practitioners are recommended to provide these services in the future: (a) conventional medical practitioners with additional training in Maharishi Consciousness-Based Health Care (eg, medical doctors, osteopaths, chiropractors, nurse clinicians, and (b) specialists trained solely in Maharishi Consciousness-Based Health Care. Training is currently available in the Maharishi Consciousness-Based Health Care at the BA and PhD levels for consultants to physicians and for independent practitioners, where allowed by law.
CERTIFICATION AND LICENSURE
We recommend that governments encourage or legislate a 2-stage certification and licensure process for Maharishi Consciousness-Based Health Care practice in all states. In the short term (eg, the next 5 years), all states are recommended to follow the recent models in California and Minnesota, where complementary and alternative medical practitioners who are practicing an approved form of natural medicine and who have been certified in their specialty by a national organization are allowed to practice clinically. As a second stage, and for the long term, we recommend that the federal government encourage or mandate adoption of licensing procedures for doctoral-level practitioners in all states. Qualification for licensure would require, among other things, successful completion of a predefined level of education in an approved educational institution and certification by a national professional organization in the field.
STAND-ALONE VERSUS COMPLEMENTARY USE
We recommend the TM program in a complementary manner with effective modern medicine approaches, but in locations where other aspects of Maharishi Consciousness-Based Health Care can be prescribed along with TM, this approach could serve as a stand-alone treatment for many CVD conditions and other diseases. Such an approach might involve medical center for each community or congressional district that specialize in Maharishi Consciousness-Based Health Care, as well as programs integrating specially trained practitioners into modern health care delivery systems. These specialized centers would allow for provision of other modalities of Maharishi Consciousness-Based Health Care that might not be available in the usual modern medical settings.
COST REIMBURSEMENT
Instruction in the TM program, with costs comparable to those of other formalized behavioral medicine programs, along with other modalities of Maharishi Consciousness-Based Health Care, should be reimbursed by third-party payers (eg, Medicare, Medicaid, as well as indemnity insurance and prepaid health plans) if controlled clinical research published in peer-reviewed scientific journals finds these modalities generally effective. Also, we recommend reimbursement for CVD prevention using these approaches.
CONCLUSIONS
Evidence from preclinical, clinical, and health insurance studies supports the feasibility and practicality of including the TM program in doctors’ recommendations for primary and secondary prevention of CVD, and also in the coverage packages of health insurance carriers. Based on the proven success of a team approach to secondary prevention, addition of TM instructors and other practitioners specially trained in Maharishi Consciousness-Based Health Care would seem appropriate both for the optimum health of patients and for reasons of economy.
ACKNOWLEDGMENT
This review was funded in part by a grant from the NTH National Center for Complementary and Alternative Medicine (Grant No. IP50AT00082-01). The authors thank Erika H. Vivier, ND, PhD, for valuable assistance on one section of the manuscript.
REFERENCES
- 1.Tunstall-Pedoe H. MONICA Monograph and Multimedia Sourcebook: World’s Largest Study of Heart Disease, Stroke, Risk Factors, and Population Trends 1979–2002 Geneva, Switzerland: World Health Organization, WHO MONICA Project; 2003:244. [Google Scholar]
- 2.National Institutes of Health, Office of Science Policy. Disease-Specific Estimates of Direct and Indirect Costs of Illness and NIH Support Washington, DC: National Institutes of Health, Office of Science Policy; 2000. [Google Scholar]
- 3.National Heart, Lung, and Blood Institute. Morbidity and Mortality, 2004: Chart Book on Cardiovascular, Lung, and Blood Diseases Bethesda, MD: National Institutes of Health; 2004. [Google Scholar]
- 4.American Heart Association. Heart Disease and Stroke Statistics 2005 Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 5.Hoffman C, Rice D, Sung H. Persons with chronic conditions: their prevalence and costs. JAMA 1996;276:1473–1479. [PubMed] [Google Scholar]
- 6.Bairey Merz C, Dwyer J, Nordstrom C, Walton K, Salerno J, Schneider R. Psychosocial stress and cardiovascular disease: pathophysiological links. Behav Med 2002;27:141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mokdad A, Marks J, Stroup D, Gerberding J. Actual casuses of death in the United States 2000. JAMA 2004;291:1238–1245. [DOI] [PubMed] [Google Scholar]
- 8.US Department of Health and Human Services. Healthy People 2000: National Health Promotion and Disease Prevention Objectives 1991 Washington, DC: Government Printing Office; 1991. [Google Scholar]
- 9.US Department of Health and Human Services. Healthy People 2000: Midcourse Review and 1995 Revisions Washington, DC: Government Printing Office; 1996. [Google Scholar]
- 10.Walton KG, Schneider RH, Nidich SI, Salerno JW, Nordstrom CK, Bairey Merz CN. Psychosocial stress and cardiovascular disease part 2: effectiveness of the Transcendental Meditation program in treatment and prevention. Behav Med 2002;28: 106–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Pew Health Professions Commission. Executive Summary San Francisco, CA: The Pew Charitable Trusts; 1995. [Google Scholar]
- 12.Smith S. How the health care system can influence cardiovascular disease risk factors. Prev Med 1999;29:S66–S71. [DOI] [PubMed] [Google Scholar]
- 13.Ades PA, Kottke TE, Miller NH, McGrath JC, Record NB, Record SS. Task force #3—getting results: who, where, and how? J Am Coll Cardiol 2002;40:579–651. [DOI] [PubMed] [Google Scholar]
- 14.Oldridge N, Furlong W, Feeny D, et al. Economic evaluation of cardiac rehabilitation soon after acute myocardial infarction. Am J Cardiol 1993;72:154–161. [DOI] [PubMed] [Google Scholar]
- 15.Levin L, Perk J, Hedback B. Cardiac rehabilitation: a cost analysis. J Intern Med 1991;230:427–434. [DOI] [PubMed] [Google Scholar]
- 16.Ades P, Huang D, Weaver S. Cardiac rehabilitation participation predicts lower rehospitalization costs. Am Heart J 1992;123:916–921. [DOI] [PubMed] [Google Scholar]
- 17.Hatziandreu E, Koplan J, Weinstein M, Caspersen C, Warner K. A cost-effectiveness analysis of exercise as a health promotion activity. Am J Public Health 1988;78:1417–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowensteyn I, Coupal L, Zowall H, Grover A. The cost-effectiveness of exercise training for the primary and secondary prevention of cardiovascular disease. J Cardiopulm Rehabil 2000;20:147–155. [DOI] [PubMed] [Google Scholar]
- 19.Orme-Johnson DW. Medical care utilization and the Transcendental Meditation program. Psychosom Med 1987;49:493–507. [DOI] [PubMed] [Google Scholar]
- 20.Orme-Johnson DW, Herron RE. An innovative approach to reducing medical care utilization and expenditures. Am J Manag Care 1997;3:135–144. [PubMed] [Google Scholar]
- 21.Alexander C, Walton K, Goodman R. Walpole study of the Transcendental Meditation program in maximum security prisoners I: cross-sectional differences in development and psychopathology. J Offend Rehabil 2003;36:97–126. [Google Scholar]
- 22.Alexander CN, Orme-Johnson DW. Walpole study of the Transcendental Meditation program in maximum security prisoners II: longitudinal study of development and psychopathology. J Offend Rehabil 2003;36:127–160. [Google Scholar]
- 23.Herron RE, Hillis SL, Mandarino JV, Orme-Johnson DW, Walton KG. The impact of the Transcendental Meditation program on government payments to physicians in Quebec. Am J Health Promot 1996;10:208–216. [DOI] [PubMed] [Google Scholar]
- 24.Herron R, Hillis S. The impact of the Transcendental Meditation program on government payments to physicians in Quebec: an update. Am J Health Promot 2000;14:284–291. [DOI] [PubMed] [Google Scholar]
- 25.Herron R, Cavanaugh K. Can the Transcendental Meditation program reduce the medical expenditures of older people? A longitudinal cost reduction study in Canada. J Soc Behav Pers In press. [Google Scholar]
- 26.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease. Arch Intern Med 1996;156:745–752. [PubMed] [Google Scholar]
- 27.Nunes E, Frank K, Kornfeld D. Psychologic treatment for Type A behavior pattern and for coronary artery disease: a meta-analysis of the literature. Psychosom Med 1987;49: 159–173. [DOI] [PubMed] [Google Scholar]
- 28.Bairey Merz CN. Efficacy of psychosocial interventions and stress management for reduction of coronary artery disease events. Prev Cardiol 1999;1:1–6. [Google Scholar]
- 29.Orme-Johnson DW, Walton KG. All approaches to preventing or reversing effects of stress are not the same. Am J Health Promot 1998;12:297–299. [DOI] [PubMed] [Google Scholar]
- 30.Lin MC, Nahin R, Gershwin ME, Longhurst JC, Wu KK. State of complementary and alternative medicine in cardiovascular, lung, and blood research: executive summary of a workshop. Circulation 2001; 103:2038–2041. [DOI] [PubMed] [Google Scholar]
- 31.Roth R. Maharishi Mahesh Yogi’s Transcendental Meditation Washington, DC: Primus Press; 2002:90–92. [Google Scholar]
- 32.Orme-Johnson DW, Farrow J. Scientific Research on the Transcendental Meditation Program: Collected Papers (Vol. I) Rheinweiler, West Germany: MERU Press; 1977:722. [Google Scholar]
- 33.Chalmers R, Clements G, Schenkluhn H, Weinless M. Scientific Research on the Transcendental Meditation Program: Collected Papers (Vol. 2–4) Vlodrop, The Netherlands: MVU Press; 1990. [Google Scholar]
- 34.Wallace RK, Orme-Johnson DW, Dillbeck MC. Scientific Research on the Transcendental Meditation Program: Collected Papers, Vol. 5 Fairfield, IA: MIU Press; 1990. [Google Scholar]
- 35.Walton K, Pugh N. Stress, steroids, and “ojas”: neuroendocrine mechanisms and current promise of ancient approaches to disease prevention. Indian J Physiol Pharmacol 1995;39:3–36. [PubMed] [Google Scholar]
- 36.Schneider RS, Charles B, Sands D, Gerace DD, Averbach RE, Rothenberg S. The significance of the Maharishi Vedic Approach to Health for modern health care and medical education. Mod Sci Vedic Sci 1997;7:299–315. [Google Scholar]
- 37.Nader T, Rothenberg S, Averbach R, Charles B, Fields J, Schneider R. Improvements in chronic diseases with a comprehensive natural medicine approach: a review and case studies. Behav Med 2000;26:34–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alexander CN, Langer EJ, Newman RI, Chandler HM, Davies JL. Transcendental meditation, mindfulness, and longevity: an experimental study with the elderly. J Pers Soc Psychol 1989;57:950–964. [DOI] [PubMed] [Google Scholar]
- 39.Schneider RH, Staggers F, Alexander C, et al. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension 1995;26:820–827. [DOI] [PubMed] [Google Scholar]
- 40.Smith S, Blair S, Criqui M, et al. American Heart Association consensus panel statement: preventing heart attack and death in patients with coronary disease. The secondary prevention panel. J Am Coll Cardiol 1995;26:2912–2914. [DOI] [PubMed] [Google Scholar]
- 41.Alexander CN, Davies JL, Dixon CA, et al. Growth of higher stages of consciousness: Maharishi’s Vedic psychology of human development. In: Alexander CN, Langer EL, eds. Higher Stages of Human Development: Perspectives on Adult Growth New York, NY: Oxford University Press; 1990:286–341. [Google Scholar]
- 42.Mason LI, Alexander CN, Travis FT, et al. Electrophysiological correlates of higher states of consciousness during sleep in long-term practitioners of the Transcendental Meditation program. Sleep 1997;20:102–110. [DOI] [PubMed] [Google Scholar]
- 43.Alexander CN, Rainforth MY, Gelderloos P. Transcendental meditation, self-actualization and psychological health: a conceptual overview and statistical meta-analysis. J Soc Behav Pers 1991;6:189–247. [Google Scholar]
- 44.Travis F, Wallace RK. Autonomic patterns during respiration suspensions: possible markers of transcendental consciousness. Psychophysiology 1997;34:39–46. [DOI] [PubMed] [Google Scholar]
- 45.Travis F, Wallace RK. Autonomic and EEG patterns during eyes-closed rest and transcendental meditation (TM) practice: the basis for a neural model of TM practice. Conscious Cogn 1999;8:302–318. [DOI] [PubMed] [Google Scholar]
- 46.Travis F, Pearson C. Pure consciousness: distinct phenomenological and physiological correlates of “consciousness itself.” Int J Neurosci 2000;100:77–89. [PubMed] [Google Scholar]
- 47.MacLean C, Walton K, Wenneberg S, et al. Effects of the Transcendental Meditation program on adaptive mechanisms: changes in hormone levels and responses to stress after 4 months of practice. Psychoneuroendocrinology 1997;22: 277–295. [DOI] [PubMed] [Google Scholar]
- 48.Walton KG, Pugh N, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support for a psychoneuroendocrine mechanism. J Altem Complement Med 1995;1:263–283. [DOI] [PubMed] [Google Scholar]
- 49.Infante JR, Torres-Avisbal M, Pinel P, et al. Catecholamines in practitioners of the transcendental meditation technique. Physiol Behav 2001;72:141–146. [DOI] [PubMed] [Google Scholar]
- 50.Dillbeck MC, Orme-Johnson DW. Physiological differences between transcendental meditation and rest. Am Psychol 1987;42:879–881. [Google Scholar]
- 51.Mills PJ, Schneider RH, Hill D, Walton KG, Wallace RK. Beta-adrenergic receptor sensitivity in subjects practicing transcendental meditation. J Psychosom Res 1990;34:29–33. [DOI] [PubMed] [Google Scholar]
- 52.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—allostatic load and its health consequences: MacArthur studies of successful aging. Arch Intern Med 1997;157:2259–2268. [PubMed] [Google Scholar]
- 53.McEwen B. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology 2000; 22:108–124. [DOI] [PubMed] [Google Scholar]
- 54.Epel ES, McEwen BS, Seeman T, et al. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med 2000;62:623–632. [DOI] [PubMed] [Google Scholar]
- 55.Barnes VA, Treiber FA, Turner JR, Davis H, Strong WB. Acute effects of transcendental meditation on hemodynamic functioning in middle-aged adults. Psychosom Med 1999;61(4): 525–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alexander CN, Robinson P, Rainforth M. Treating and preventing alcohol, nicotine and drug abuse through transcendental meditation technique: a review and statistical analysis. In: O’Connell DF, Alexander CN, eds. Self Recovery—Treating Addictions Using Transcendental Meditation and Maharishi Ayur-Veda New York, NY: Haworth Press; 1994:13–88. [Google Scholar]
- 57.Leape L. Error in medicine. JAMA 1994;272:1851–1857. [PubMed] [Google Scholar]
- 58.Bates D, Cullen D, Laird N, et al. Incidence of adverse drug events and potential adverse drug events: Implications for prevention. ADE Prevention Study Group. JAMA 1995;274:29–34. [PubMed] [Google Scholar]
- 59.Boden W, O’Rourke R, Crawford M, et al. Outcomes in patients with acute non-Q-wave myocardial infarction randomly assigned to an invasive as compared to a conservative management strategy. Veterans Affairs Non-Q-Wave Infarction Strategies in Hospital (VANQWISH) trial investigators. N Engl J Med 1998;338:1785–1792. [DOI] [PubMed] [Google Scholar]
- 60.Bedell S, Deitz D, Leeman D, Delbanco T. Incidence and characteristics of preventable cardiac arrests. JAMA 1991. ;265: 2815–2820. [PubMed] [Google Scholar]
- 61.Eisenberg D, Kessler R, Foster C, et al. Unconventional medicine in the United States: prevalence, costs, and patterns of use. N Engl J Med 1993;328:246–252. [DOI] [PubMed] [Google Scholar]
- 62.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA 1998;280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 63.Borkan J, Neher J, Anson O, Smoker B. Referrals for alternative therapy. J Fam Pract 1994;39:545–550. [PubMed] [Google Scholar]
- 64.Blendon RJ, Taylor H. Views on health care: public opinion in three nations. Health Aff 1989;8:150–157. [DOI] [PubMed] [Google Scholar]
- 65.Fogle S. Darwin takes on mainstream medicine. J NIH Res 1993;5:64–66. [Google Scholar]
- 66.Wetzel M, Eisenberg D, Kaptchuk T. Courses involving complementary and alternative medicine at US medical schools. JAMA 1998;280:784–787. [DOI] [PubMed] [Google Scholar]
- 67.Fletcher GF. 33rd Bethesda Conference. Preventive cardiology: how can we do better? Introduction. J Am Coll Cardiol 2002;40:579–587. [Google Scholar]
- 68.Schneider RH, Alexander CN, Wallace RK. In search of an optimal behavioral treatment for hypertension: a review and focus on transcendental meditation. In: Johnson EH, Gentry WD, Julius S, eds. Personality, Elevated Blood Pressure, and Essential Hypertension Washington, DC: Hemisphere Publishing Corporation; 1992:291–312. [Google Scholar]


