Abstract
Moving THA off of the Inpatient Only (IPO) List for Center of Medicaid and Medicare Services (CMS) beneficiaries and the COVID-19 pandemic has caused a shift in delivery away from inpatient services and a decrease in demand. Medicare payments dramatically declined from 2019 to 2020. LOS decreases and shift to outpatient designations were accelerated by IPO list changes and COVID-19 issues. The percentage of SDD cases also increased. Other metrics favorable to decreased spending by CMS were increased discharge to home and decreased volume. These changes have a profound impact on surgeon-hospital relationships and surgeon compensation.
Keywords: IPO rule, RUC, ASC, HOPD, SDD, COVID-19
This symposium examined the changing economic value and leverage of orthopedic surgeons as total joint arthroplasty (TJA) cases continue to shift from being primarily performed as hospital inpatient only to hospital outpatient and ultimately to ambulatory surgery centers (ASC). Using 100% Medicare Part A and B claims data for the country, this symposium presented the following trends:
-
•
From 2017 to 2021, arthroplasty cases were being performed less frequently as inpatients, and increasingly as outpatients in hospital outpatient departments (HOPD) and ASCs
-
•
Due to the changes brought about by the removal of TJA from the Inpatient Only List, hospital reimbursement for TJA for the first time has trended lower. Additionally, due to decreases in reimbursement brought about by regulatory changes at the Relative Value Scale Update Committee (RUC), these changes have negatively impacted surgeon income as well. These trends over time of decreasing revenue per case, which varies by care setting, have begun to impact the value of arthroplasty surgeons to hospitals.
-
•
As total professional fees and facility fees generated by arthroplasty surgeons continue to decrease, a projection of how this trend will likely continue prospectively based on the expected continued migration of site of surgery to the outpatient setting has implications on the hospital employment of arthroplasty surgeons in the future.
-
•
Hospitals and health systems are changing compensation for employed surgeons in response to the decrease in revenue per arthroplasty case. Hospitals are experiencing lower profitability due to declining arthroplasty revenue, and thus, there is an increased emphasis on cost reduction regarding arthroplasty cases. This has profound implications on innovation, implant cost, and employed surgeon salary expectations [1].
Discussion
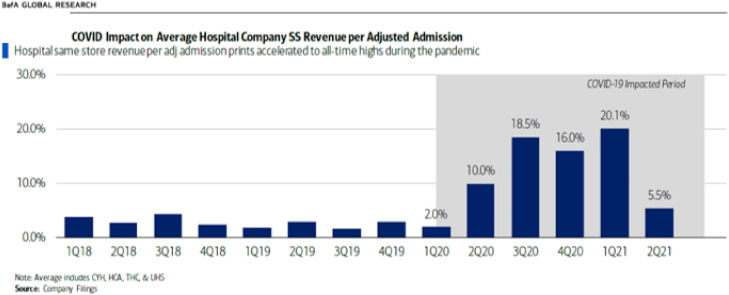
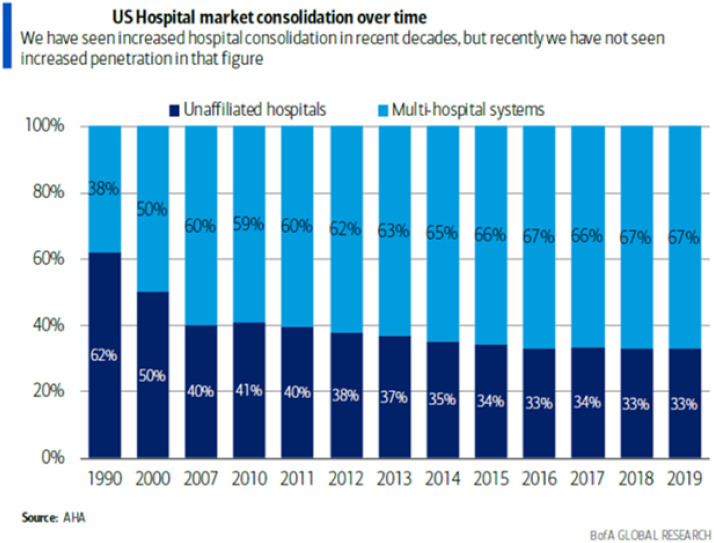
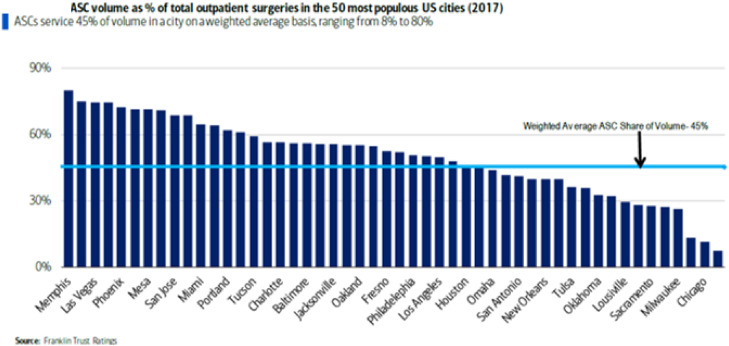
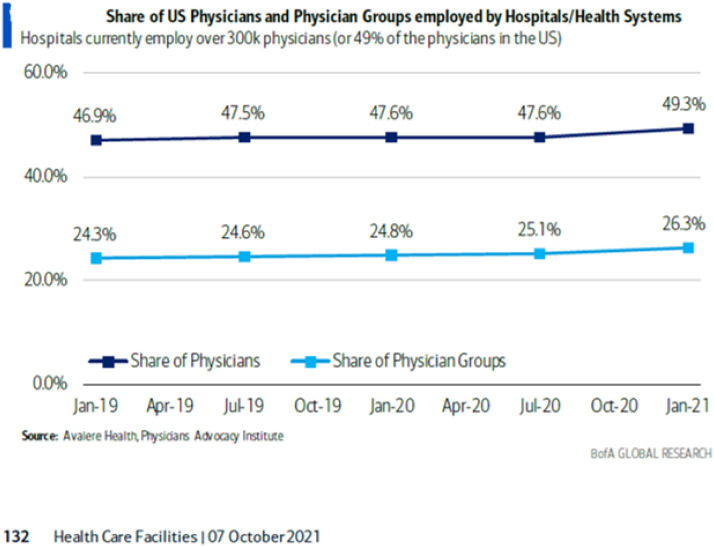
Hospitals have done very well over the 2019 to 2021 time period (Fig. 1 ). It remains to be seen whether more hospitals will participate in gainsharing or co-management arrangements with their aligned and nonaligned surgeons in order to encourage retaining cases at the hospital rather than having them done in a nonaligned surgery center. Hospitals and hospital systems continue to consolidate (Fig. 2 ). The shift of arthroplasty volume (especially non-CMS beneficiaries) to nonaligned ASCs is potentially damaging to the hospital surgeon relationship (Fig. 3 ). This is likely to negatively affect the trend of increasing hospital employment of arthroplasty surgeons. It is likely that hospitals, aligned physicians, implant vendors, and ASCs will develop new strategies to control costs and optimize care delivery under the evolving regulatory environment [2].
Fig. 1.
Quarterly Hospital Revenue since 2018.
Fig. 2.
Consolidation of the United States Hospital Market.
Fig. 3.
United States Ambulatory Surgery Center Volume.
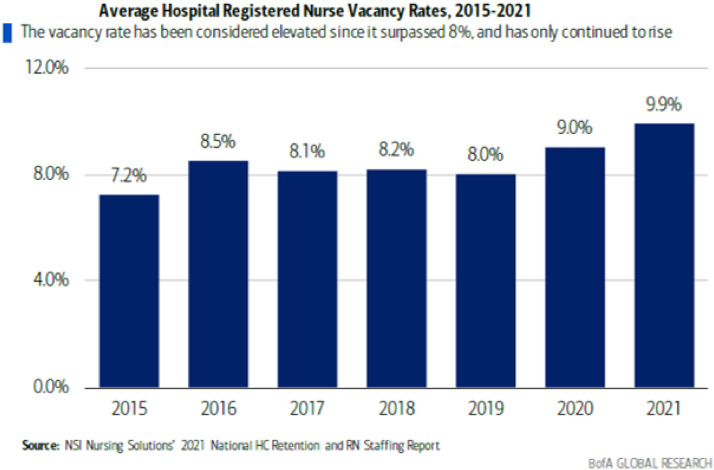
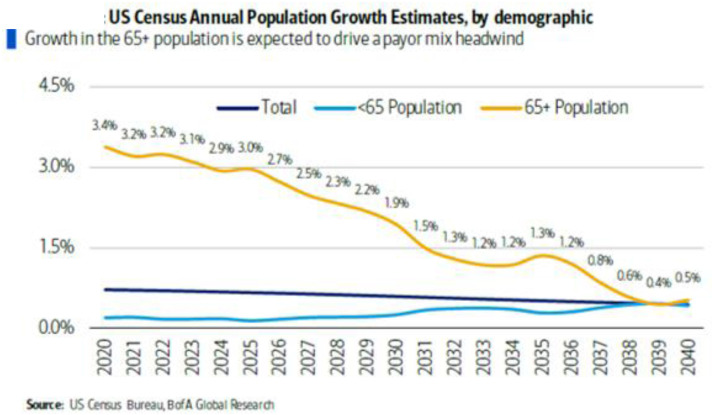
Dramatic shifts in demand, capacity, and site of service have impacted TJA volumes and revenues over the 2019-21 time period. Other factors impacting arthroplasty care delivery include nursing and perioperative staffing challenges (Fig. 4 ); we are modifying surgical and procedural schedules to align with current staffing and capacity issues. Analytics are being applied to inform how best to reduce the impact on inpatient capacity while taking care of patients safely, optimize the site of care, and most importantly, ensure timely interventions for patients’ health situations. Our population is aging, and this trend will continue to preserve the demand for arthroplasty services (Fig. 5 ). However, hospital systems are consolidating, and that may limit the opportunity for arthroplasty surgeons (Fig. 6 ).
Fig. 4.
United States Nursing Vacancy Rates.
Fig. 5.
United States Annual Census Growth by Age Demographic.
Fig. 6.
Share of Hospital Employed Physicians in the United States.
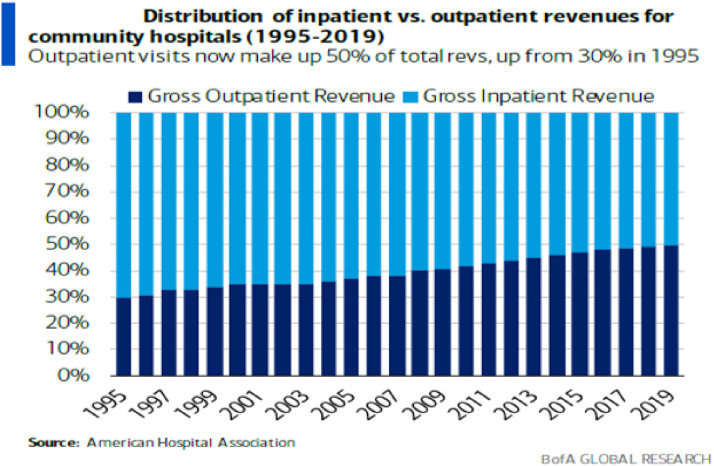
The understanding of how the IPO rule, Merit-Based Incentive Payment System (MIPS), Alternative Payment Models (such as episode-based arthroplasty bundles and disease management longitudinal bundles), and the RUC reimbursement and coding changes affect orthopedic arthroplasty practices is critical to financial survival in this rapidly changing environment. The shift in emphasis from intervention-based reimbursement to cognitive-based reimbursement has profound implications for orthopedic surgeons. Ambulatory and outpatient care will continue to grow in importance (Fig. 7 ). We need to assert our control as the primary providers of musculoskeletal care in order to have a role in the future disease-based population management models for care delivery [3].
Fig. 7.
Inpatient vs Outpatient Hospital Revenues in the United States.
Conclusions
The shift to value-based care (VBC) is happening slowly, but the pace seems to be accelerating. CMS and managed care have been increasingly looking for ways to change the incentives in the healthcare system away from fee for service toward the fee for value.
With health systems and investment groups (Managed Care Organizations, Venture Capital, and hospitals alike) acquiring physician groups and increasingly taking on risk or entering into capitation agreements, we are seeing this shift accelerate. VBC will have significant impacts on the industry, but given that healthcare tends to be evolutionary rather than revolutionary, the change will take some time.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2022.03.035.
Appendix A. Supplementary Data
References
- 1.Bank of America Global Research . Bank of America; Charlotte, NC: 2021. Health Care Facilities Hospital Primer – Everything you need to know about the $1.4T industry. 12:05AM EDT. [Google Scholar]
- 2.Iorio R., Peavy P.R., Keyes D., Dempsey S., McCready D.O., Kang J.D. Improving arthroplasty efficiency and quality through concentrating service volume by complexity: surviving the Medicare policy changes. J Arthroplasty. 2021;36:3055–3059. doi: 10.1016/j.arth.2021.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Skeehan C.D., Ortiz D., Sicat C.S., Iorio R., Slover J., Bosco J. The 2021 CMS fee schedule’s impact on adult reconstruction surgeon productivity and reimbursement. J Arthroplasty. 2021;36:3381–3387. doi: 10.1016/jarth.2021.06.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.