Abstract
The objective of this peripheral nerve stimulation consensus guideline is to add to the current family of consensus practice guidelines and incorporate a systematic review process. The published literature was searched from relevant electronic databases, including PubMed, Scopus, Cochrane Central Register of Controlled Trials, and Web of Science from database inception to March 29, 2021. Inclusion criteria encompassed studies that described peripheral nerve stimulation in patients in terms of clinical outcomes for various pain conditions, physiological mechanism of action, surgical technique, technique of placement, and adverse events. Twenty randomized controlled trials and 33 prospective observational studies were included in the systematic review process. There is Level I evidence supporting the efficacy of PNS for treatment of chronic migraine headaches via occipital nerve stimulation; chronic hemiplegic shoulder pain via stimulation of nerves innervating the trapezius, supraspinatus, and deltoid muscles; failed back surgery syndrome via subcutaneous peripheral field stimulation; and lower extremity neuropathic and lower extremity post-amputation pain. Evidence from current Level I studies combined with newer technologies facilitating less invasive and easier electrode placement make peripheral nerve stimulation an attractive alternative for managing patients with complex pain disorders. Peripheral nerve stimulation should be used judiciously as an adjunct for chronic and acute postoperative pain following adequate patient screening and positive diagnostic nerve block or stimulation trial.
Keywords: post-amputation pain, low back pain, peripheral neuropathy, chronic postoperative pain
Introduction
Background
While the use of peripheral nerve stimulation (PNS) originated more than five decades ago, this therapy has only recently experienced a resurgence after falling out of favor for many years. In the 1960s, after the publication of the gate control theory,1 Wall and Sweet published their first case series demonstrating decreases in pain perception throughout the entire episode of electrical stimulation of the infraorbital foramina2,3 and Shelden reported that temporary pain relief was achieved through implantation of PNS electrodes stimulated via an implanted receiver at 14,000 Hz.4 Over the next three decades, as evident in multiple publications, PNS treatment was mired by suboptimal outcomes, poor long-term success rates, and complications such as nerve damage or stimulation-induced fibrosis.3,5,6 Many of the adverse occurrences could be attributed to lead migration, pulse generator locations, and other technical problems.
In the 1990s, interest in PNS was revived after Weiner and Reed first described a percutaneous technique of electrode insertion in the vicinity of the greater occipital nerves to treat occipital neuralgia.7 More recently, the emergence of a minimally invasive percutaneous approach, typically performed under ultrasound, has led to even more widespread interest in PNS as an alternative to neurosurgically implanted spinal cord stimulator (SCS) systems.8,9 Multiple options exist for the percutaneous placement of leads which are stimulated directly with an external power source/impulse generator (IPG) or hybrid systems that have an internal IPG that is powered via an external power source.
Mechanism of Action
Although the exact mechanism of action of PNS is unknown, there is evidence that both central and peripheral mechanisms contribute to its analgesic effect. Like SCS, PNS is thought to provide analgesia based at least in part on the gate-control theory of pain, as described by Melzack and Wall.1 Centrally, the stimulation of large-diameter, low-threshold, non-nociceptive Aβ fibers results in the excitation of inhibitory dorsal horn interneurons that are involved in the processing and transmission of nociceptive information from the Aδ and C nerve fibers, thus inhibiting pain signal transmission from the spinal cord to higher centers in the central nervous system (CNS).10 Furthermore, PNS decreases central sensitization and hyperalgesia by reducing excessive peripheral nociceptive activity in the spinal cord, inhibiting wide dynamic range of neurons in the dorsal horn, and decreasing Aβ fiber–induced activity in the medial lemniscal pathway in the brain.11–13 Additionally, animal research has demonstrated that the analgesic effects of PNS may involve the serotonergic (5HT2, 5HT3), GABAergic, and glycinergic pathways.14,15
Studies in the peripheral nervous system have demonstrated that PNS disrupts the transmission of nociceptive afferent fibers. On a molecular level, PNS has been shown to modulate the biochemistry of the local microenvironment by downregulating neurotransmitters, endorphins, and local inflammatory mediators.16 Electrophysiological studies have also demonstrated reduced ectopic discharges with PNS.16 A human study by Torebjork and Hallin showed that repeated electrical stimulation of intact radial nerves and saphenous nerves resulted in excitation failure of A and C fibers.17 The concept of peripheral reconditioning of the central nervous system through longer-term changes in central plasticity has also been proposed.18
Indications
Indications for PNS for treatment of neuropathic pain are similar to those for SCS procedures. However, PNS may offer greater selectivity and accuracy for cases with well-defined neuronal targets. In addition, PNS for chronic, nociceptive pain of the knee, shoulder, and zygapophyseal joints can be effective. In general, good PNS candidates have had pain that is chronic, severe, negatively affecting their functionality, and refractory to usual medical treatments, including medications, physical therapy, and less invasive interventions such as injection therapy.18 In many cases, PNS may provide a less invasive implant to treat neuropathic pain, including posttraumatic, postsurgical neuropathy, occipital neuralgia, hemiplegic shoulder pain, phantom limb pain, and complex regional pain syndrome (CRPS).19 Moreover, recent studies have demonstrated the role of PNS in peripheral and central analgesic mechanisms by modulating the inflammatory pathways, autonomic nervous system, endogenous pain inhibition pathways, and cortical and subcortical areas.20,21
Materials and Methods
Development Process
The American Society of Pain and Neuroscience (ASPN) applied a systematic approach to appraise the current level of evidence in the peer-reviewed literature regarding PNS neuromodulation interventions for treatment of chronic pain. Similar systematic approaches were utilized to produce the first guidelines from the Neurostimulation Appropriateness Consensus Committee (NACC) in 2014,22–24 and these guidelines are regularly updated based on new and emerging evidence. This current consensus guideline for PNS stimulation adds to the current family of consensus practice guidelines and incorporates a systematic review process.
The ASPN society formed an international multidisciplinary panel consisting of anesthesiologists, neurosurgeons, and pain medicine physicians who are experts in the field of PNS neuromodulation to create these consensus practice guidelines. To qualify for inclusion on the expert panel, each author was required to have experience with performing PNS trials and lead implantation, publications and ongoing research pertaining to PNS neuromodulation, and impact on the field of neuromodulation. Financial conflicts of interest were disclosed and managed before initiation of the consensus guideline development process. Per society protocol, one of the primary authors was non-conflicted (NS) and served as the editor of the paper for bias. In addition, where any conflict of interest existed, the panel member recused themselves from any opinion on any relevant issue.
PNS neuromodulation continues to be a relatively novel and emerging technology. While the systematic review and meta-analysis approach are standard for forming consensus guidelines, in some scenarios the development of new techniques, disease applications, and other innovations may advance the field faster than randomized controlled trials (RCTs) or large-scale prospective observational trials. Thus, in these instances, available literature with lower levels of evidence based on study design will be coupled with clinical expertise from the expert panel to fill the gap. The methods below describe the search strategy, systematic review process, and consensus guideline creation and grading.
Literature Search Methods
A comprehensive, a priori search protocol was utilized to broadly query databases and identify relevant studies on PNS neuromodulation. Extensive electronic searches were conducted in relevant databases, including PubMed, Scopus, Cochrane Central Register of Controlled Trials, and Web of Science, from database inception to March 29, 2021. We also hand-searched reference lists of identified publications to identify relevant publications not captured in the search strategy.
Broad MeSH terms and Boolean operators were selected for each database search, including terms and synonyms for PNS, peripheral nerve stimulator, occipital nerve stimulation, occipital nerve stimulator, peripheral nerve neuromodulation, peripheral field stimulation, peripheral neurostimulation, and analgesia/pain/neuropathy.
Inclusion criteria encompassed studies that described PNS for patients in terms of clinical outcomes for various pain conditions (head and neck, upper and lower extremities, low back and trunk, cCRPS, post-amputation pain, peripheral neuropathies, and other conditions), physiological mechanism of action, surgical technique, technique of placement (landmark-based, ultrasonography, paresthesia, and stimulator-based localization), adverse events, and other aspects. Study designs that were identified and included in our search strategy included RCTs, prospective observational studies, retrospective observational studies (eg case-control, cross-sectional), and case series and reports. Exclusion criteria comprised of non-peer reviewed publications and certain study designs (eg review articles, non-human trials). Two authors (RSD and NS) independently selected abstracts as well as full-text articles from the above listed databases using the aforementioned search strategies. This search strategy was verified by a librarian experienced in systematic review methods and is displayed in the Supplemental Material.
Systematic Evaluation of Evidence
A total of 3811 studies were identified with the initial search. Abstracts for each study were reviewed independently by two authors (RSD and NS) to identify studies for full-text review. Two hundred articles were identified for full-text review and, of these, 162 articles were included for full review and again were reviewed by two independent authors (RSD and NS). Only RCTs and prospective observational trials were reviewed in a systematic fashion, using guidelines from the Cochrane Collaboration.25 For other studies including retrospective observational studies, case series, and case reports, evaluation in a systematic fashion was not performed. However, given the emerging body of the literature pertaining to peripheral neuromodulation, the authors felt that these manuscripts held value to help inform consensus guidelines.
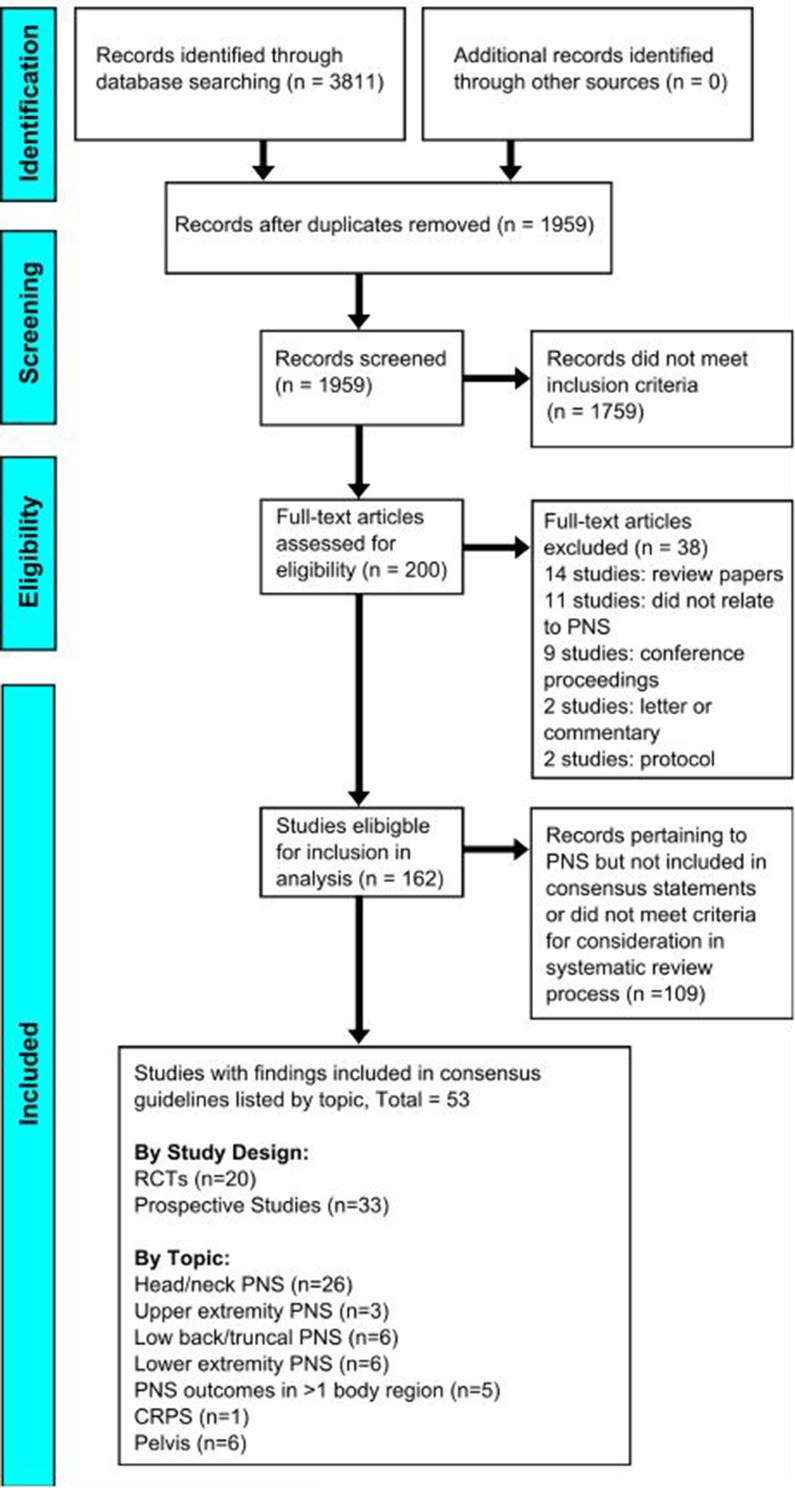
Twenty RCTs and 33 prospective observational studies were included in the systematic review process (Figure 1). Evidence was appraised using the United States Preventive Services Task Force (USPSTF) criteria for evidence level (Table 1) and degree of recommendation (Table 2). A degree of recommendation of A indicates the highest degree of recommendation, while D indicates the lowest degree of recommendation.
Figure 1 .
PRISMA diagram depicting the flow of information through the different phases of the systematic review. It shows the data identified, included and excluded, and the reasons for exclusions.
Notes: PRISMA figure adapted from Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Creative Commons.
Table 1.
Hierarchy of Studies by the Type of Design (US Preventive Services Task Force)
| Evidence Level | Study Type |
|---|---|
| I | At least 1 controlled and RCT, properly designed |
| II-1 | Well-designed, controlled, nonRCTs |
| II-2 | Cohort or case studies and well-designed controls, preferable multicenter |
| II-3 | Multiple series compared over time, with or without intervention, and surprising results in noncontrolled experiences |
| III | Clinical experience-based opinions, descriptive studies, clinical observations, or reports of expert committee |
Notes: Reprinted from Harris RP, Helfand M, Woolf SH, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 Suppl):21–35. Copyright 2001, with permission from Elsevier.112
Table 2.
Meaning of Recommendation Degrees (I.S. Preventive Services Task Force)
| Degree of Recommendation | Meaning |
|---|---|
| A | Extremely recommendable (good evidence that the measure if effective and that benefits outweigh the harms) |
| B | Recommendable (at least moderate evidence that the measure if effective and that benefits exceed harms) |
| C | Neither recommendable nor inadvisable (at least moderate evidence that the measure is effective, but benefits are similar to harms and a general recommendation cannot be justified) |
| D | Inadvisable (at least moderate evidence that the measure is ineffective or that the harms exceed the benefits) |
| I | Insufficient, low-quality, or contradictory evidence; the balance between benefit and harms cannot be determined |
The patient population of interest was 18 years or older with chronic pain of greater than six months duration and failure of prior conservative therapy consisting of physical therapy, pharmacologic treatment, or injection therapy. The primary outcome of interest was pain relief graded via a validated pain scale (eg, numerical pain scale, visual analog scale). Secondary outcomes included functional improvement, reduction in analgesic medications, physiological mechanism of action, surgical technique, technique of placement (landmark-based, ultrasonography, paresthesia, and stimulator-based localization), and adverse events.
Consensus Best Practices Development
Given the early state and emerging literature pertaining to PNS neuromodulation, one goal of this assessment was to fill in gaps of knowledge through consensus from our expert panel. Thus, expert consensus was sought when higher levels of evidence were lacking in the literature.
Summary of Literature
Head and Neck
Migraine and Occipital Neuralgia
Historically, neuropathic head and neck pain has been challenging to treat. There is emerging evidence that chronic pain syndromes in these regions can be treated with PNS. It should be noted that only some of the currently commercially available percutaneous PNS devices are cleared by the FDA for head and neck usage. Because of this, some implantation of PNS systems in the craniofacial area could be considered off-label use.114
The evidence for PNS in the head and neck region has largely focused on stimulation of the occipital nerves. The greater and lesser occipital nerves have long been a target for treatment of certain headache disorders and chronic post-traumatic pain.26 In many cases, stimulation has been used in headache patients, particularly those suffering from chronic migraines.
It has been reported that headache disorders are the second most prevalent disease and the second most common cause of disability worldwide.27 PNS has been used in those who may suffer from occipital neuralgia (ON).28 In ON, pain may occur in the distributions of the greater, lesser, or third occipital nerves and patients frequently describe sharp, severe, and lancinating pain. The greater occipital nerve (GON) is strongly implicated in ON due to its circuitous course as it emerges from the suboccipital triangle. In most cases, landmark or fluoroscopic techniques have been employed with placement of leads at the nuchal line.29 With the increasing use of high-resolution ultrasound, the greater occipital nerve may also be targeted in the upper neck at C2.
Multiple randomized trials have shown the benefit of occipital nerve stimulation for chronic migraine.30–34
In a recent randomized, double-blind, controlled trial, 20 patients were implanted with occipital PNS. They were randomized to an active or control group for 12 weeks, and received open-label treatment for additional 40 weeks. At one year, headache days per month were reduced by 8.51 (±9.81) days (P < 0.0001). The proportion of patients who achieved a 30% or 50% reduction in headache days and/or pain intensity was 60% and 35%, respectively.31
Facial Pain
PNS has also been employed for facial pain, particularly in the distribution of the supraorbital and infraorbital nerves.35 In a prospective study of 30 patients with neuropathic craniofacial pain, 22 were eventually implanted with permanent systems. The targets included supraorbital, infraorbital, and 13 occipital nerves. A total of 16 of the 22 patients reported >50% pain relief.36 Despite the promising results of facial stimulation, there are no RCT level data and this area presently requires additional study.
Summary of Evidence Level
Stimulation of occipital nerves may be offered to patients with chronic migraine headache when conservative treatments have failed. The average effect size for relief of migraine symptoms is modest to moderate (Level I, Grade B).
There is presently insufficient evidence to recommend stimulation of supraorbital and infraorbital nerves for neuropathic craniofacial pain (Level II-3, Grade C).
Upper Extremities
To date, two RCTs have been performed to evaluate the utility of PNS for chronic upper extremity pain.37,38 Wilson et al37 performed a single-site, RCT comparing single-lead, three-week PNS versus usual care for treatment of chronic hemiplegic shoulder pain in stroke survivors. This study reported significantly greater reduction in pain intensity in the PNS cohort compared to the cohort receiving usual care at the 6-week and 12-week period. Furthermore, both PNS and usual care led to improvements in pain interference and quality of life. Another single-site RCT by the same authors38 compared single-lead PNS versus physical therapy for chronic shoulder pain after stroke. The authors reported that PNS and physical therapy each led to improvements in maximum isometric shoulder abduction strength, external rotation without pain, and Fugl-Meyer motor assessment.
An ongoing multicenter randomized sham control pragmatic study is evaluating the prospective role of PNS to reduce postoperative opioid consumption in the acute postoperative setting. Although PNS is traditionally used for chronic pain, this ongoing trial highlights that it may also be relevant for acute postoperative pain.39 Specifically, the authors are investigating whether PNS of the suprascapular, axillary, ulnar, and median nerves may provide reproducible and effective targets for stimulation in certain upper extremity (UE) pain conditions. Given that shoulder pain is the second most common musculoskeletal complaint and is associated with considerable socioeconomic impact, it is important to establish greater recognition of the potential benefits of PNS for treatment of UE pain that is not responsive to conservative measures or surgical instrumentation.
Evidence established through observational studies and case series/reports further demonstrates the utility of PNS for various upper extremity pain manifestations, including mononeuropathies, brachial plexopathies, CRPS, and trauma. A series of 26 patients who were afflicted with refractory neuropathic pain in the upper extremity including 16 patients with CRPS were treated with brachial plexus or suprascapular PNS.40 At a mean follow-up period of 27.5 months, 20 patients were still reporting great pain relief (mean 67.1% pain relief). Seventeen patients reported ≥50% pain relief, and 12 patients reported ≥70% pain relief. Long-term follow-up in patients who reported outcomes at >2 years revealed a mean reported pain relief of 68%. At the last follow-up visit, 18 of 20 patients were still using stimulation and reported that they were either satisfied or very satisfied.
Summary of Evidence Level
PNS may offer modest and short-term pain relief, improved physical function, and better quality of life for chronic hemiplegic shoulder pain. (Level I, Grade B)
PNS for mononeuropathies of the upper extremity may be offered following a positive diagnostic ultrasound-guided nerve block of the targeted nerve and is associated with modest to moderate pain relief. (Level II-2, Grade B)
Low Back and Trunk
Chronic low back pain is the leading cause of years lived with disability (YLD) and is one of the most challenging conditions to treat.41 This condition is associated with decreased quality of life and frequently interferes with functions of daily living including walking, household chores, and personal care.42 Even after recovery of the initial insult or injury, long-term and persistent low back pain and disability may lead to a cycle of central sensitization resulting in hypersensitivity to nociceptive stimuli.43 Conventional treatment modalities for the treatment of chronic low back pain are frequently inadequate. Superior analgesia and functionality scores have been noted with the advent of neuromodulation, including SCS and PNS.44–46 Although systematic reviews of SCS for the treatment of chronic low back pain have been published,47,48 evidence supporting PNS for the treatment of this condition is currently emerging.
In a multicenter RCT, Eldabe et al49 compared 38 patients with failed back surgery syndrome (FBSS) who received subcutaneous PNS plus optimized medical management with those who received optimized medical management alone (n = 36). In the interventional arm, a maximum of two leads were placed subcutaneously in the area of pain. Patients were evaluated at baseline and at one, three, six, and nine months after study arm assignment. The primary endpoint was the percentage of participants who reported a ≥50% improvement at six months and ≥30% improvement at nine months in intensity of back pain. A significant proportion (33.9%) of patients who received both subcutaneous PNS placement and optimal medication management were responders at nine months versus only 1.7% of patients who received optimal medication management alone (P < 0.0001).49
The remaining evidence consisted of observational studies and case reports/series. The evidence of PNS field stimulation for low back pain discussed above was further substantiated by a prospective multicenter study by Kloimstein et al,50 which reported statistically significant improvements in pain intensity, disability, depression, and quality of life up to six months after PNS. There was also a reduction in use of opioids, non-steroidal anti-inflammatory drugs, and anti-convulsant dose. Other retrospective studies51 have also highlighted the efficacy of subcutaneous field stimulation in the treatment of low back pain. The spectrum of low back pain also includes sacroiliac joint pain. A retrospective case series52 described PNS placement to stimulate nerves innervating. This study evaluated PNS in sacroiliac joint pain refractory to conservative measures and injection therapy and followed patients for up to four years. Significant reductions were noted in mean pain scores at one year (Visual analog scale (VAS) from 8.8 to 1.6), at two years (VAS from 8.8 to 1.9), and at three years (VAS from 8.8 to 2.0). Two of three patients reported satisfaction with PNS placement at the fourth year.
Another approach for the treatment of chronic axial low back pain is to utilize PNS to stimulate medial branch nerves. A high-quality prospective multicenter cohort study53 investigated PNS of lumbar medial branch nerves to treat chronic axial low back pain in patients who had undergone prior lumbar radiofrequency ablation. Participants had bilateral temporary PNS leads placed using either ultrasound or fluoroscopy and targeting medial branch nerves at the level of their pain. After stimulation testing, activation of the lumbar multifidi muscles confirmed stimulation of medial branch nerves. PNS was performed for up to 60 days, and outcomes were assessed at baseline, and up to 5 months after initiation of PNS. The study reported that 67% of patients (10/15) reported ≥50% improvement in pain intensity, 87% of patients (13/15) reported a ≥50% improvement in disability, and 80% of patients (12/15) reported a ≥50% improvement in pain interference. These effects persisted into the five-month follow-up period when 93% of patients (14/15) reported ≥50% improvement in one or more of the clinical outcome categories. A similar prospective cohort study by Gilmore et al54 substantiated these findings and reported that PNS of lumbar medial branch nerves was associated with ≥50% reduction in pain intensity in 67% of participants (6/9) at 1 month and 12 months after PNS initiation.
Other pain syndromes successfully treated with PNS have been described, although evidence is limited to small studies and case series. One small prospective pilot study55 reviewed truncal involvement in oncologic pain and reported that PNS improved pain intensity in post-mastectomy pain syndrome, cervical and lumbar radiculopathy, and femoral nerve neuropathy. Neuropathic pain manifestations involving the trunk and low back have been described in case series and reports. Significant improvements in pain intensity have been reported in post-herpetic neuralgia56–59 and dermatomal pain by targeting proximal cervical, thoracic, or lumbar spinal nerves.60
Summary of Evidence Level
Subcutaneous peripheral field stimulation combined with optimal medication management may offer moderate improvement in pain intensity for failed back surgery syndrome compared to optimal medication management alone (Level I, Grade B).
There is evidence that PNS of medial branch nerves may improve pain intensity, physical function, and pain interference in patients with axial, mechanical low back pain (Level II-2, Grade B).
There is limited evidence that PNS alleviates pain in neuropathic pain syndrome involving the trunk and back, including radiculopathy and post-herpetic neuralgia (Level III, Grade C).
Lower Extremities
The evidence for PNS in the treatment of lower extremity chronic pain is reported in 2 RCTs, 1 prospective observational study, and 19 retrospective studies. Deer et al performed the initial prospective, multicenter, double-blind, partial crossover RCT studying the use of PNS for peripheral nerve chronic pain of a variety of anatomical regions, with lower extremity comprising a large proportion of the cohort.61 A total of 94 patients were randomized to the study (45 treatment group and 49 control group). Regarding the lower extremity specifically, 27 patients were randomized to the study (13 treatment group and 14 control group).
The purpose of the study was to evaluate the safety and efficacy of the StimRouter System (Bioventus/Bioness Inc., Valencia, Santa Clarita, CA, USA) for use in the treatment of severe, intractable pain of peripheral nerve origin associated with posttraumatic or postsurgical neuralgia. Primary outcomes included pain relief, measured by average pain at rest using NRS. Patients were followed for 3 months and safety was determined by assessment of adverse events during the one-year study period. Responders were defined as those experiencing >30% pain relief compared to baseline. Secondary outcome measures included changes in medication dose, type, and frequency; quality of life using the Brief Pain Inventory (BPI) and Quality of Life SF-12v2 Health Survey (QoLSF-12v2); patient impression of improvement with treatment using the patient global impression of change scale (PGIC); change in worst pain using the NRS; change in interference of pain with physical and emotional functioning; patient satisfaction; and long-term safety at one year. Inclusion criteria included age >22 years, severe intractable chronic pain of peripheral nerve origin associated with posttraumatic/postsurgical neuralgia for at least 3 months, worst pain levels greater than 5/10, and stable regimen of medications for at least 4 weeks before screening.
The treatment group received electrical stimulation and stable pain medication dosing, while the control group received no stimulation and a stable dose of pain medications, both for 90 days. Follow-up continued for safety and secondary measures at 6 and 12 months. In the lower extremity at 3 months, there was a 38% responder rate in the treatment group versus 14% in the control group. The average pain reduction at 3 months was 21% in the treatment group versus 1.2% in the control group. These results were similar to the overall cohort (p < 0.0001). The secondary outcomes showed the treatment group had better improvement than the control group in multiple domains, including worst pain score, BPI scores, quality of life, and PGIC. At 12 months, there were no serious device-related events.
Gilmore et al reported on the use of PNS for chronic neuropathic lower extremity postamputation pain in a multicenter, randomized, double-blind, placebo-controlled study design.62 Inclusion criteria included traumatic lower extremity amputation with healed and healthy residual limb, residual limb pain and/or phantom limb pain with an average daily score ≥4 on a 0–10 pain rating scale, and age ≥18 years. Subjects were allowed to maintain or reduce dosages of pain medications but were asked to avoid increasing dosages above documented baseline levels. After being deemed an appropriate candidate, subjects were randomized 1:1 to either a percutaneous PNS therapy group (SPR Therapeutics, Cleveland, Ohio) or a placebo control group. Subjects and outcome evaluators were masked for group assignment, while treating physicians were unmasked to allow them to administer interventions accordingly.
The PNS group received active percutaneous femoral and sciatic nerve stimulation for 4 weeks during the primary outcome evaluation period, while the placebo control group received sham stimulation. Following the initial 4 weeks, the PNS group received four additional weeks of stimulation (up to 60 days total) and the placebo group crossed over to receive active stimulation for 4 weeks. Interventions ended at the end of the 8-week therapy period and leads were removed at this time. Both groups were followed monthly for up to 12 months from the time of PNS implantation. The primary outcome was the proportion of subjects in the PNS and placebo control groups that experienced ≥50% reductions in average pain during weeks 1–4 of the therapy period. Secondary outcomes included pain relief during weeks 5–8, Brief Pain Inventory-Short Form (BPI-SF), Patient Global Impression of Change (PGIC), BDI-II, and medication usage.
A total of 28 patients were randomized with 26 entering the study arms (12 PNS therapy group and 14 placebo control group). At week 4, 58% of the PNS group reported >50% pain relief compared to 14% of the placebo group (p = 0.037). At week 8, 67% of the PNS group reported >50% pain relief and, following crossover of the placebo group to receive PNS therapy, response remained at 14%. The secondary outcomes improved as well, with the PNS group showing greater improvements than the placebo control group. There were no serious or unanticipated study-related adverse events, but a lead fracture rate of 15% (5 of 34) was reported.
In a follow-up report, the same authors assessed 12-month outcomes among 15 patients (9 PNS group and 6 crossover placebo control group).63 At 12 months, 67% of the PNS group was reporting >50% pain reduction versus 17% of the crossover placebo control group. Similarly, 56% of the PNS group had >50% reduction in pain interference compared to 18% in the crossover placebo control group (p = 0.074). In the PNS group, BDI-II scores were reduced by 33% at 12 months. The authors reported no serious or unanticipated study-related adverse events.
In 2014, Rauck et al published the results of a six-week prospective observational study for post-amputation pain involving a two-week PNS stimulation period with follow-up at four-week post-stimulation (Maxima® II or Rehabilicare® NT2000, Empi, Inc., St. Paul, MN, USA).64 Leads were placed with ultrasound guidance around the sciatic and/or femoral nerves. A total of 16 patients were enrolled, 14 had appropriate paresthesia coverage, and 9 completed the two weeks of PNS stimulation. At the follow-up visit, four weeks after the end of the stimulation period, the mean worst daily post-amputation pain was reduced by 56% (p < 0.005). 7 patients reported clinically significant relief at the four-week post-stimulation visit and 5 patients reported being “improved” or “much improved.”
A number of retrospective case studies and small case series have been published reporting clinical benefit of PNS in the lower extremity, including many conducted within larger, heterogenous patient cohorts.2,65–82
Others
The authors have shown therapeutic benefits to the use of percutaneous PNS for a variety of neuropathic complaints or invasive PNS for acute postoperative pain, but these modalities and uses are outside of the scope of this manuscript.39,83–88
Summary of Evidence Level
PNS may be considered for lower extremity neuropathic pain following failure of conservative treatment options and is associated with modest pain relief (Level I, Grade B).
PNS may be considered for lower extremity post-amputation pain following failure of conservative treatment options and is associated with modest to moderate pain relief (Level I, Grade B).
CRPS
Neuromodulation has long-standing use as treatment for CRPS and experts agree that this condition, which is often refractory to treatment, benefits from early intervention with this therapy. Neuromodulation has been shown to improve pain intensity and provide functional restoration89,90 in patients with CRPS.
CRPS Type 1 and CRPS Type II often involve diffuse pain that may overlap multiple nerve distributions, presenting challenges for the use of PNS, which is more straightforward when pain is localized to the distribution of a single nerve. Moreover, even though CRPS Type II typically involves injury to a specific nerve, there is presence of central sensitization, wind-up phenomenon, and reorganization of the central nervous system leading to more diffuse pain not localized to a single nerve distribution.
As long as 25 years ago, the benefits of PNS were explored for the treatment of CRPS. One prospective series published in 1996 followed 32 patients with CRPS who underwent a PNS trial. Ninety-four percent (94%) of those tested went on to permanent PNS placement, and long-term relief was reported in 63%.91 Since then, vast improvements in technology have led to continued growth and usage of PNS for CRPS, and data has improved regarding PNS outcomes.
Our comprehensive search strategy did not identify any RCTs for utilization of PNS for CRPS or causalgia. One retrospective study identified 165 subjects with CRPS who had been treated with permanent PNS systems.92 Of these, 76% had a diagnosis of CRPS type 1, 15% had CRPS type 2, and 8% had CRPS not otherwise specified (NOS).92 VAS pain scores decreased from 7.4 to 5.5 on average at 12 months, and percentage of patients utilizing any opioid decreased from 62% at baseline to 41% at 12 months. Interestingly, these results were obtained using traditional SCS leads and were not optimized or specifically designed for PNS. This fact may be relevant to the relatively high rate of explantation (19%) due to lack of efficacy, infection, device discomfort, or other reasons.
The majority of data on usage of PNS for CRPS is in the form of case reports and case series. Frederico et al described a series of 14 patients with refractory CRPS of the upper limb.93 Of those 14 patients trialed with PNS of the brachial plexus, 10 underwent permanent implantation and had significant improvements in VAS and neuropathic pain after 12 months.93 Buwembo et al reported a case of direct sciatic nerve stimulation reducing intractable pain from CRPS by 59% along with cessation of autonomic features such as color changes, swelling, and sensory dysfunction.94
Summary of Evidence Level
As a less-invasive modality compared to SCS therapy, PNS may be offered to patients with CRPS Type I/II or peripheral causalgia, and may be associated with modest improvement in pain intensity and functional outcomes. However, high-quality evidence is limited and other neuromodulation interventions such as dorsal root ganglion SCS are recommended. (Level III, Grade C).
Perioperative Considerations, Image Guidance, and General Techniques
Perioperative Considerations: Patient Selection, Risk Assessment, and Preprocedural Optimization
There is a paucity of data describing best practices for appropriate patient selection for PNS. In general, patients who have pain localized to a discrete nerve distribution or focal area involving few nerves should be considered for PNS. As aforementioned in sections above, we summarize clinical indications for PNS based on the location of pain in Table 3. There are over 20 peripheral nerves that are appropriate targets for PNS, and each is associated with unique anatomical concerns, risks, and implications for the placement of external wearables/power sources. We recommend that clinicians consider feasibility of device placement, appraise evidence of clinical efficacy, and remain vigilant of potential adverse events. For headache and facial pain, most evidence highlights the effectiveness of PNS for occipital neuralgia, although other nerves may be targeted. Upper extremity pain localized to the radial, median, and/or ulnar nerve distributions, as well as shoulder pain from suprascapular and/or axillary nerve distributions, are suitable targets for PNS. In more diffuse pain manifestations of the upper extremity, PNS of the brachial plexus may also be offered with placement via the interscalene approach or infraclavicular approach. Similarly, lower extremity pain localized to sciatic, femoral, obturator, lateral femoral cutaneous, saphenous, posterior femoral cutaneous, common peroneal, tibial, sural, superficial peroneal, and genicular nerves are suitable PNS targets. Depending on the distribution of groin pain and pelvic pain, PNS of genitofemoral, ilioinguinal, iliohypogastric, and/or pudendal nerves may be pursued. Intercostal PNS may provide effective analgesia in rib pain, post-thoracotomy pain, intercostal neuralgia, and post-herpetic neuralgia located within thoracic dermatomes. Medial branch nerve PNS and cluneal nerve PNS may alleviate low back or gluteal pain. Other neuropathic and central pain etiologies may also respond to PNS, most notably CRPS, hemiplegic (post-stroke) shoulder pain, and lower extremity phantom limb pain.37,62–64,95 Due to the wide range of approaches and practices, we will focus attention on the implant techniques for the following five nerves: suprascapular, axillary, sciatic, tibial, and medial branch nerves (Table 3).
Table 3.
A List of Common Peripheral Nerve Targets Amenable to Percutaneous PNS Treatment
| Upper Extremity | Lower Extremity | Trunk/Pelvis | Head/Neck |
|---|---|---|---|
| ● Suprascapular** ● Axillary** ● Radial ● Median ● Ulnar ● Brachial plexus (at interscalene interval) |
● Sciatic** ● Femoral ● Obturator ● Lateral femoral cutaneous ● Saphenous ● Posterior femoral cutaneous ● Common peroneal ● Tibial** ● Sural ● Superficial peroneal ● Genicular nerves (knee) |
● Genitofemoral ● Ilioinguinal ● Iliohypogastric ● Pudendal ● Cluneal ● Medial Branch** |
● Greater occipital |
Note: Nerves targets denoted by a double asterisk and are in bold (**) are described in detail below.
Preoperative evaluation is critical to assess the likelihood of success for PNS candidates. PNS is not without risk, and placing leads in proximity to nerves can lead to direct trauma, nerve compression, bleeding, or infection.96 A thorough preoperative history and physical focused on peripheral nerve function should be performed. As for SCS, optimization of bleeding disorders, diabetes mellitus, and infections is important. Examination of the affected limb or area should include an assessment of sensory and motor function (if applicable). Clinicians should document abnormalities including sudomotor, vasomotor, and trophic changes. In some cases, scanning the nerve in question with ultrasound in the clinic can give clues about potential abnormalities including entrapment or injury and may inform surgical planning. Additional studies that may be helpful in the preoperative workup include electromyography (EMG), nerve conduction studies (NCS) and magnetic resonance neurography. These tests may provide additional clues about the location of potential nerve lesions. Similar to SCS, all patients should be sent for a psychological evaluation prior to any PNS intervention. This assessment is important for understanding ongoing comorbid mood issues, life stressors, and patient expectations of therapy.
Regarding bleeding risk assessment, it should be noted that PNS is considered to be a low to intermediate risk procedure as classified by the American Society of Regional Anesthesiologists (ASRA).97 Unlike SCS or DRG stimulation, PNS is usually performed in areas of the body that are readily compressible, thus it can be assumed that the risk of bleeding complications associated with bleeding are small for most patients. Patients with increased risk for bleeding include those with advanced liver and kidney disease, prior history of bleeding, or coexistent use of anticoagulants. (Table 4) The proposed location of the PNS implant also affects bleeding risk. Patients who are undergoing PNS of nerves located in close proximity to large vascular structures (eg, femoral, saphenous, tibial) may be at increased risk for bleeding as well due to the risk of inadvertent vascular injury. The use of high-resolution ultrasound may help to mitigate this risk. In general, many implanters may reasonably opt to continue anticoagulation medications given the perceived low risk of bleeding associated with PNS. More study is needed to characterize bleeding risk and best practices associated with PNS procedures.
Table 4.
ASRA Risk Classification of Pain Procedures
| High-Risk Procedures | Intermediate-Risk Procedures | Low-Risk Procedures |
|---|---|---|
| Spinal cord stimulation trial and implant | Interlaminar ESIs (C,T,L,S) | Peripheral nerve blocks |
| Dorsal Root Stimulation | Transforaminal ESIs (C,T,L,S) | Peripheral joints and musculoskeletal injections |
| Intrathecal catheter and pump implant | Cervical facet MBNB and RFA | Trigger point injections including piriformis injection |
| Percutaneous decompression laminotomy | Sympathetic Blocks (stellate, T, splanchnic, celiac, lumbar, hypogastric) | Thoracic and lumbar facet MBNB and RFA |
| Epiduroscopy and epidural decompression | Trigeminal and sphenopalatine ganglia blocks | PNS trial and implant |
Note: PNS is considered a low to intermediate risk procedure.
Summary of Evidence Level
PNS carries a low-to-intermediate risk for bleeding complications and depends on the proximity of the targeted nerve to critical vessels and invasiveness of PNS implantation (Level III, Grade I).
Image Guidance
Most current PNS systems require that leads be placed close to peripheral nerves and thus precision is critical. High-resolution ultrasound has become an essential tool for successful lead placement. Much of the advancement and understanding of the utilization of ultrasound for PNS implantation techniques can be traced to techniques developed for perioperative pain control in the field of regional anesthesiology. Ultrasound allows for precise visualization of nerves and vascular structures as well as real-time assessment of lead position. Because patients are typically awake during PNS placement without sedation (preferable for intraoperative testing), ultrasound facilitates quick deployment of leads safely while maximizing patient comfort. We advocate using this imaging modality whenever possible to facilitate placement of PNS leads.
It should be noted that while ultrasound is widely used for PNS procedures, there are situations when fluoroscopy may be a useful adjunct or preferred modality. In cases when bony structures impede ultrasonographic visualization, patients present with challenging anatomy, or body habitus limits ultrasound resolution, fluoroscopy may be used as part of a combination technique with ultrasound. Additionally, there are a select group of nerves which have predictable courses over bony prominences and in these cases, fluoroscopy may be used exclusively. Nerves which may be potential fluoroscopic targets include the suprascapular, axillary, intercostal, cluneal, greater occipital, and genicular nerves. There are no large studies comparing the placement of peripheral nerve stimulators using ultrasound versus fluoroscopic guidance.
Nerve Localization and Planning: Diagnostic Blocks vs PNS Trials
In some cases, it may be difficult to identify a single culprit nerve that is causing a patient’s pain. This is particularly true in areas of the body that have convergence of multiple nerve distributions like in the foot and ankle. Diagnostic nerve blocks can be helpful in these situations, as they frequently provide clues about which peripheral nerve(s) are major pain generators. However, patients with longstanding chronic pain syndromes like phantom limb pain, CRPS, or hemiplegic shoulder pain may not have a robust response to peripheral blocks, even though these individuals may still have a good response to PNS. Therefore, we recommend that results of peripheral blocks be interpreted with caution.
With the advancements of percutaneous systems, there are now options for brief and extended PNS trial periods. When a PNS trial is being used as a precursor to a permanent implant, leads are typically implanted for 5–10 days although some systems have FDA clearance for up to 30 days of use. Alternatively, treatment with a 60-day, temporary PNS system (Sprint, SPR Therapeutics; Cleveland, OH) has been considered by some to serve as an “extended trial.” Increasingly, there are data to suggest that brief periods of stimulation often provide durable pain relief. In general, PNS trials are likely to better predict the long-term response to therapy.
General Techniques: Approaches to Nerves
Sciatic Nerve (SN)
The sciatic nerve (SN) is formed from the L4, L5, S1, S2, and S3 nerve roots. As it traverses from the low back posteriorly to the lower limb through the greater sciatic foramen and progresses distally in the posterior thigh compartment, it splits into two branches (tibial nerve and common peroneal nerve) just before the popliteal fossa.98 The SN and its divisions provide sensory innervation to the foot and lower extremity except for the medial leg and ankle which are supplied by the saphenous nerve.
Common access for SN stimulation with permanent PNS systems is at the region of the sciatic nerve proximal from the popliteal fossa. With the patient prone, the transducer is placed at the popliteal fossa to identify the popliteal artery between the biceps femoris laterally and the semimembranosus along with the semitendinosus medially. The transducer is then moved proximal to identify the branches of the tibial nerve (lateral to popliteal vein) and the common peroneal nerve (lateral to tibial nerve). Once identified, the nerve pair is followed proximally until they coalesce into a singular sciatic nerve.
Due to the large diameter of the SN, leads are typically placed perpendicular to the nerve from lateral to medial. Tunneling of leads and/or IPGs should be toward the lateral thigh as this is an ergonomically convenient location. In some patients including lower extremity amputees, a subgluteal approach may be a preferable approach to the SN. Depending on the body habitus of the patient, visualization of the SN at this proximal point can be more challenging and the distance of tissue that the introducer/lead must traverse is greater when compared to the popliteal fossa.
Suprascapular Nerve (SSN)
The suprascapular nerve (SSN) is made up of fibers from the C4, C5, and C6 nerve roots. Anteriorly in the neck, it runs underneath the trapezius and omohyoid muscles. It then travels posteriorly and enters the supraspinous fossa by the suprascapular notch underneath the transversscapular ligament. It has both a motor and sensory component, providing motor innervation to the supraspinatus and infraspinatus muscles while providing sensation to the posterior shoulder, the acromioclavicular joint, subacromial bursa, coracoclavicular ligament, and the coracoacromial ligaments.99,100
In many cases, the suprascapular nerve can be visualized at the suprascapular notch. The notch lies along the scapula under the trapezius and supraspinatus muscle. The relationship of the suprascapular artery, nerve, and vein is variable, but the artery is frequently seen running above the ligament, while the nerve traverses underneath.101 During needle placement, care is exercised to avoid entering the suprascapular artery which is in close proximity to the SSN. An in-plane, medial-to-lateral approach is usually preferred. This technique avoids the acromion laterally, and the lead can travel in a more parallel orientation to the nerve. SSN lead positioning is accomplished either with the patient prone to a bump, lateral decubitus, or sitting (usually with a Beach chair). Due to the mobility of the shoulder, lead migration is a significant concern and thoughtful preoperative planning is essential. For permanent systems, the implanter and patient should decide on the best site for the external power source, keeping in mind that the lead should not cross the shoulder joint if possible.
An alternative technique has also been described where the nerve is approached from the spinoglenoid notch, inferior to the scapular spine. The introducer/lead is then directed from inferior to superior toward the suprascapular notch. This method is more technically challenging than the suprascapular approach, but it can maximize lead contact with the nerve. Due to the predictable course of the nerve, implanters utilizing this technique may also elect to use fluoroscopy.
Axillary Nerve (AN)
The axillary nerve (AN) is composed of the C5 and C6 posterior cords of the brachial plexus. It provides motor innervation to the teres minor and deltoid while providing sensory innervation to the shoulder joint and the skin of the shoulder. The quadrangular space is one of three axillary spaces and is made up of the teres minor superiorly, teres major inferiorly, long head of the triceps brachii medially, and laterally by the neck of the humerus containing the axillary nerve and the posterior humoral circumflex artery (PHCA).102,103
With the patient in the lateral or prone position, the ultrasound probe is placed posteriorly and vertically, in-plane with the humeral shaft. The probe is moved superiorly toward the surgical neck of the humerus. With the humoral head in view, the deltoid should be visualized most superficially and the teres minor deep to this muscle. Moving distally and medially, the axillary nerve and PHCA can be visualized just inferior to the teres minor. The probe can then be rotated 90 degrees and the artery can be visualized in long axis.
For lead placement, one technique is to insert the PNS introducer via an out-of-plane approach from a lateral to medial trajectory toward the nerve. It is then directed toward the quadrangular space. Another option is to identify the artery in long axis and insert the introducer in plane from lateral to medial. For this technique, the lead is placed on top of or adjacent to the artery. Given the artery’s close proximity to the nerve, stimulation can usually be achieved by this method.
Tibial Nerve (TN)
The tibial nerve (TN) is a terminal branch of the SN with innervation from L4, L5, S1, S2, and S3. It travels from the popliteal fossa through the deep posterior compartment of the leg before passing through the tarsal tunnel at the medial ankle, posterior to the medial malleolus. The nerve divides into the lateral plantar nerve (LPN), medial plantar nerve (MPN), and medial calcaneal nerve (MCN), providing sensation to the plantar surface of the foot. More proximally, the nerve also gives off the medial sural cutaneous nerve, a contributor to the sural nerve which gives sensation to the posterior leg.
When the tibial nerve is targeted distally, a parallel approach to the nerve is usually necessary. This is because there is little muscle and subcutaneous fat in the area for perpendicular approaches. The lead can be placed either distal-to-proximal or proximal-to-distal. Positioning is lateral decubitus with the affected foot down and leg flexed at the knee to allow for access to the nerve. Care should be taken to avoid the tibial artery and vein(s) which travel adjacent to the nerve. Leads for permanent systems are tunneled toward the medial leg or calf area.
Medial Branch Nerves (MBN)
The medial branch nerves (MBNs) innervate the zygapophysial joint, a synovial joint of the lumbar spine. These joints are dually innervated by the medial branches of the posterior primary rami at the same level as well as the level above the joint. The nerve traverses the transverse process at the same vertebral level where the nerve emerges and courses through the intertransverse ligament at the base of the transverse process.104 The nerve then descends down the junction of the transverse and superior articular process beneath the mamillo-accessory ligament and divides into numerous branches as it traverses the vertebral lamina.105 The MBN provides sensory innervation for the zygapophysial joint, interspinous ligament, and the periosteum of the neural arch. The MBN also provides motor function to the multifidus and interspinous muscles.
When MBN stimulation is performed using ultrasound, the patient is placed in a prone position and their lumbar spine is palpated over the area where they report pain. This area is then prepped sterilely and the ultrasound probe is placed out-of-plane to be perpendicular to the lumbar spine. The probe is placed in midline positioning to visualize the bilateral lamina with the overlying multifidus muscle. A judicious amount of local anesthesia is then injected, taking care to avoid application to the multifidus muscles. The needle is placed out-of-plane, and motion artifact is assessed until the needle has entered the multifidus muscle. Stimulation is utilized to confirm multifidus activation under ultrasound prior to placement of the stimulation lead. MBN stimulation can also be performed utilizing fluoroscopy.
The emergence of PNS as an effective and precise tool for neuropathic pain of a peripheral nerve origin is predicated on a deep understanding of ultrasound technology for the safe and effective execution of the therapy. Several well-described techniques have been established for various targets. As ultrasound technology and user experience continue to advance, PNS will most certainly continue to progress with improved patient safety and efficacy.
Fluoroscopy
There are no large studies comparing ultrasound and fluoroscopic guidance for the placement of PNS. Nerve blocks for peripheral nerves have been described using both fluoroscopy and ultrasound, and similar block techniques for identifying peripheral nerves can be used to place PNS. Key factors to consider include the size of the lead, need for entrance at a distance from the target nerve to allow for appropriate lead placement, planning placement of the lead(s) parallel or crossing in relation to the nerve and tunneling needed. Ultrasound has the advantage of direct visualization of the nerve with a dynamic view of lead placement, enabling accurate determination of the distance between the PNS lead(s) and the target nerve.
Technologies
Table 5 provides an overview of PNS Systems currently used in the treatment of acute or chronic pain. Detailed descriptions of these systems are provided below.
Table 5.
Overview of Percutaneous PNS Systems
| PNS Device (Manufacturer) | Device Characteristics | Permanent vs Temporary | FDA Cleared Indication | MRI Capability |
|---|---|---|---|---|
| StimRouter (Bioness/Bioventus) |
|
Permanent | Severe, intractable chronic pain of peripheral nerve origin. | Conditional |
| Nalu Neurostimulation System (Nalu Medical) |
|
Permanent | Severe, intractable chronic pain of peripheral nerve origin. | Conditional |
| StimQ PNS System (Stimwave Technologies) |
|
Permanent | Severe, intractable chronic pain of peripheral nerve origin. | Conditional, full body 1.5T with 4 contact lead |
| SPRINT PNS System (SPR Therapeutics) |
|
Temporary | Up to 60 days in the back, extremities, head, neck, and/or torso for: 1. Symptomatic relief of chronic, intractable pain, postsurgical and posttraumatic acute pain 2. Symptomatic relief of posttraumatic pain 3. Symptomatic relief of postoperative pain *Not intended to treat pain in the region innervated by the cranial and facial nerves. |
Not compatible |
| ReActiv8 Implantage Neurostimulation System (Mainstay Medical) |
|
Permanent | To aid in treatment of intractable chronic low back pain associated with multifidus muscle dysfunction | Not compatible |
Bioventus/Bioness
The Bioness StimRouter® device (Bioventus/Bioness Inc., Valencia, Santa Clarita, CA, USA) is specifically designed for the treatment of peripheral nerve pain in the lower and upper extremities, pelvis, and trunk.106 The system requires implantation of a peripheral lead that is powered by a rechargeable, lithium battery within the external pulse transmitter (EPT). The implanted lead is 15 cm in length and 1.2 mm in diameter, and contains the receiver coil and three stimulation electrodes. To implant the lead, a 1–2 cm incision is created approximately 5–10 cm from the targeted nerve. A stimulation probe is used to stimulate the targeted nerve and ensure stimulation is possible.
Once the stimulation response is confirmed, an introducer is placed over the stimulation probe and the probe is removed. The peripheral lead is placed through the introducer and the stimulation response is again confirmed through the implanted lead. The introducer is removed and this deploys the four-pronged anchor to hold the lead in place. Then the proximal end of the peripheral lead is tunneled subcutaneously, after which the incisions are closed and covered with sterile dressings.
The EPT powers the system and is positioned directly over the receiver of the implanted lead by attaching it to a disposable electrode patch placed on the skin for programming and daily wear. The clinician/representative has a device programmer to test multiple stimulation settings, including waveform, amplitude, pulse rate, phase duration, and time. Once programmed by the clinician, the patient can power on or off the device, select from among the various settings, and change amplitude through a different patient programmer. The StimRouter® system is MRI Conditional for head and extremities under specific conditions.107
Nalu Medical
The Nalu™ Neurostimulation System (Nalu Medical Inc., Carlsbad, CA, USA) offers both central and peripheral nervous system stimulation devices using battery-free microstimulation constructs.108 The PNS functionality of the system is indicated for intractable chronic pain of peripheral nerve origin. The system uses tined four-contact lead(s) of either 25 cm or 40 cm length, which are inserted subcutaneously near the targeted nerve. The implantable pulse generator (IPG) is battery-free and is powered by an external therapy disc worn over the IPG site.
To perform the implant procedure, a puncture incision may need to be created. The needle and introducer sheath are advanced through the incision in the direction of the peripheral nerve using ultrasound or fluoroscopic guidance. Once in appropriate position, the needle is removed, leaving the introducer sheath in place. The lead is pre-loaded with a straight stylet and inserted through the introducer sheath. Once the lead is visualized in the appropriate position, the introducer sheath is retracted to expose the lead’s contacts. The proximal end of the lead is then connected to the electrode interface cable and paresthesia production may be attempted.
Once appropriate stimulation is obtained, the tines may be deployed. Holding the lead in place, the introducer sheath is slowly retracted until it approaches the correct white marker band on the lead (distal marker band for the 10 cm introducer sheath; proximal marker band for the 14 cm introducer sheath). Deployment of the first lead tine is initiated when the white marker band enters the introducer sheath. The introducer sheath is then slowly removed until a drop in resistance is felt. At this point, confirmation of lead location by performing stimulation or visualizing through fluoroscopic or ultrasound imaging is recommended. The desired IPG location is then finalized and the placement of the therapy disc is outlined with a surgical marker, after which an incision is made 7 cm from the center of the therapy disc in the direction of the PNS lead.
Depending on the desired site of the IPG, the PNS lead may need to be connected to a lead extension and/or tunneled to the IPG incision. To accomplish this, the pocket tunneller tool can be used to create a shallow subcutaneous pocket, 1 cm deep and up to 10 cm in length, advancing towards the center of the therapy disc outline. The proximal end of the lead is then cleaned, inserted into the IPG, and locked in place using the torque wrench, after which the tip of the IPG insertion tool is inserted into the specified IPG site with the Nalu logo facing towards the skin. The IPG is then advanced with a pushing motion along the subcutaneous path until it reaches the center of the therapy disc outline. Finally, the IPG insertion tool is removed, leaving the IPG in place.
At this point, the impedances should be checked and excess lead should be looped into the incision site. The incision(s) are closed in a standard fashion and sterile dressings applied. The patient is given two therapy discs to ensure proper charging and minimize disruption of therapy. Using the therapy disc, the patient can power on or off the device, change programs, and adjust stimulation intensity. The Nalu PNS system is MRI Conditional for head and extremities under specific conditions.106
Stimwave
The StimQ Peripheral Nerve Stimulator (PNS) System (Stimwave Technologies Inc., Fort Lauderdale, FL, USA) is indicated for intractable pain in adults who have pain of peripheral nerve origin.109 The system consists of an implantable stimulator, implantable receiver, and an external transmitter to power the device. Prior to implantation, patients will typically undergo a trial using a trial lead to determine efficacy.
To implant the device, the distal end of the PNS lead, which contains the electrodes, is inserted around the targeted peripheral nerve and the proximal end is anchored and buried in the superficial soft tissues. The PNS lead has tines to anchor it in place. The external transmitter is placed over the proximal end of the lead to power the device. Multiple programming options are available, including traditional and burst waveforms, and stimulation frequencies up to 1500 Hz. The device is full body MRI conditional.
SPR Therapeutics
The SPRINT® PNS System (SPR Therapeutics, Cleveland, OH, USA) is indicated for up to 60 days in the back and/or extremities for relief of chronic intractable pain, in addition to acute post-surgical and post-traumatic pain.110 In 2021, the device gained expanded FDA clearance for placement in regions including the head, neck, and the front of the torso (but not including regions innervated by facial or cranial nerves).
To perform the implant procedure, a monopolar needle electrode is inserted percutaneously and directed towards the targeted nerve (within 0.5 to 3 cm) using ultrasound and/or fluoroscopy guidance. Test stimulation is performed through the needle to confirm paresthesia production in the expected and desired locations. Once optimal location is identified, the needle electrode is removed. A 20G introducer needle preloaded with the Sprint MicroLead is then directed to the same location using ultrasound and/or fluoroscopy guidance. Correct lead positioning is confirmed by performing test stimulation through the lead. If successful, the lead is deployed by withdrawing the needle introducer while applying downward pressure at the skin surface. Typically, the lead is coiled outside the skin, trimmed accordingly, and the skin exit site is covered with a bandage. The lead is then connected to an EPG, which is attached to the body using an adhesive pad. At the end of the 60-day therapy period (or before if necessary), the lead is removed from the subcutaneous tissues along with the EPG. The SPRINT® PNS System is MRI unsafe while implanted and must be removed before an MRI can be performed. Following removal, a retained lead fragment is considered MRI conditional.106
Mainstay Medical
The ReActiv8® Implantable Neurostimulation System (Mainstay Medical Limited, Dublin, Ireland) is indicated for patients with intractable low back pain associated with multifidus muscle dysfunction, as evidenced by multifidus atrophy on advanced imaging.111 The ReActiv8® system consists of an IPG and implantable stimulation leads. The non-rechargeable ReActiv8® IPG allows two to four-electrode leads. The leads are fitted with bi-directional tines at the distal electrode which engage with the soft tissues upon lead deployment to anchor the lead in place. A hand-held activator allows the patient to start and stop stimulation. The IPG is programmed to deliver episodic electrical stimulation with varying stimulation times and episodes per day. The goal of stimulation is to elicit a contraction of the lumbar multifidus muscles.
To implant the device, the patient is positioned prone on an operating room table A midline incision is performed and the leads are placed adjacent to the descending medial branch dorsal rami, bilaterally at the transverse processes of L3. The leads are introduced with fluoroscopic visualization using an introducer needle, guide wire, delivery sheath, and dilator. The implanting physician then creates a subcutaneous pocket where the IPG will be implanted. The leads are tunneled subcutaneously between the lead implant incision and the IPG pocket, leaving a strain relief loop at the midline lead incision. Following lead placement and connection of the leads to the IPG, the wounds are irrigated and closed in a layered fashion. Sterile dressings should be applied.
Conclusion
Electrical neuromodulation has been employed in the treatment of refractory pain conditions since the publication of the Gate Control Theory in 1965. Given recent advances in technology, we should anticipate corresponding refinements in techniques, applications, and targets of stimulation therapies. Unlike stimulation of the central nervous system via epidural spinal cord electrodes, stimulation of the peripheral nervous system has not gained widespread adoption, despite its longer history of use. Current evidence from high-quality RCTs combined with newer technologies facilitating less invasive and easier electrode placement make PNS an attractive option for physicians and patients in the management complex pain disorders.113
With the expansion of treatment into both acute and chronic pain, our goal is to provide best practice guidelines and recommendations based on the level of current evidence for the utilization of PNS for recalcitrant pain. Please see a summary in Table 6: ASPN best practices PNS guidelines. As our understanding of the effect that PNS has on nociceptive pain progresses, so too will our knowledge as to its best application. PNS should be used judiciously as an adjunct for chronic pain following adequate patient screening and positive diagnostic nerve block or stimulation trial. Further robust clinical studies identifying specific conditions, waveforms, programming, and lead placements are necessary to ensure standardization of patient and treatment selection.
Table 6.
ASPN Best Practices PNS Guidelines
| ASPN Best Practices PNS Guidelines | Level of Evidence | Grade |
|---|---|---|
| Head/Neck | ||
| Stimulation of occipital nerves may be offered to patients with chronic migraine headache when conservative treatments have failed. The average effect size for relief of migraine symptoms is modest to moderate. | I | B |
| There is insufficient evidence to recommend stimulation of supraorbital and infraorbital nerves for neuropathic craniofacial pain. | II-3 | C |
| Upper Extremities | ||
| PNS may offer modest and short-term pain relief, improved physical function, and better quality of life for chronic hemiplegic shoulder pain. | I | B |
| PNS for mononeuropathies of the upper extremity may be offered following a positive diagnostic ultrasound-guided nerve block of the targeted nerve and is associated with modest to moderate pain relief. | II-2 | B |
| Low Back/Trunk | ||
| Subcutaneous peripheral field stimulation and optimal medication management may offer moderate improvement in pain intensity for failed back surgery compared to optimal medication management alone. | I | B |
| There is evidence that PNS of lumbar medial branch nerves may improve pain intensity, physical function, and pain interference in patients with axial, mechanical low back pain. | II-2 | B |
| There is limited evidence that PNS may alleviate pain in neuropathic pain syndrome involving the trunk and back including radiculopathy and post-herpetic neuralgia. | III | C |
| Lower Extremities | ||
| PNS may be considered for lower extremity neuropathic pain following failure of conservative treatment options and is associated with modest pain relief. | I | B |
| PNS may be considered for lower extremity post-amputation pain following failure of conservative treatment options and is associated with modest to moderate pain relief. | I | B |
| Other Considerations | ||
| As a less-invasive modality compared to SCS therapy, PNS may be offered to patients with CRPS Type I or Type II, and may be associated with modest improvement in pain intensity and functional outcomes. However, high-quality evidence is limited and other neuromodulation interventions such as dorsal root ganglion SCS are recommended for CRPS. | III | C |
| PNS carries a low-to-intermediate risk for bleeding complications and depends on the proximity of the targeted nerve to critical vessels and invasiveness of PNS implantation. | III | I |
Acknowledgments
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Dr Jonathan M Hagedorn reports personal fees from Abbott, Boston Scientific, Medtronic, Nevro, and Saluda, outside the submitted work. Dr Scott Pritzlaff reports personal fees from EBT Medical, SPR Therapeutics, and Nalu Medical, during the conduct of the study. Dr Dawood Sayed reports grants from Spr, during the conduct of the study; personal fees from Spr, Nevro, Medtronic, and Abbott, outside the submitted work. Dr Alexander Escobar reports personal fees from Abbott, personal fees from Boston Scientific, personal fees from Medtronic, personal fees from Nevro, outside the submitted work. Dr Mark Huntoon reports fees from SPR for consulting and teaching, outside the submitted work; and Saluda- Membership on Clinical Events Committee for national study. Dr Timothy R Deer reports personal fees, from Abbott, personal fees, from Vertos, grants from Flowonix, personal fees, from SpineThera, personal fees, from Saluda, from Mainstay, personal fees, from Nalu, personal fees, from Cornerloc, personal fees, from Ethos, personal fees, from SPR Therapuetics, personal fees from SI Bone, personal fees from Nevro, personal fees from Medtronic, personal fees, from Boston Scientific, personal fees, from PainTeq, personal fees from Tissue Tech, personal fees, from Spinal Simplicity, from Avanos, outside the submitted work; in addition, Dr Timothy R Deer has a patent Abbott pending to DRG Leads pending. The authors report no other conflicts of interest in this work.
References
- 1.Melzack R, Wall PD. Wall. Pain mechanism: a new theory. Science. 1965;150(3699):971–979. doi: 10.1126/science.150.3699.971 [DOI] [PubMed] [Google Scholar]
- 2.Wall PD, Sweet WH. Temporary abolition of pain in man. Science. 1967;155:108–109. doi: 10.1126/science.155.3758.108 [DOI] [PubMed] [Google Scholar]
- 3.White JC, Sweet WH. Pain and the Neurosurgeon: A Forty-Year Experience. Springfield: Thomas; 1969:894–899. [Google Scholar]
- 4.Shelden CH. Depolarization in the treatment of trigeminal neuralgia. Evaluation of compression and electrical methods; clinical concept of neurophysiological mechanism. In: Knighton RS, vDumke PR, editors. Pain. Boston: Little, Brown; 1966:373–386. [Google Scholar]
- 5.Kirsch WM, Lewis JA, Simon RH. Experiences with electrical stimulation devices for the control of chronic pain. Med Instrum. 1975;9:217–220. [PubMed] [Google Scholar]
- 6.Nielson KD, Watts C, Clark WK. Peripheral nerve injury from implantation of chronic stimulating electrodes for pain control. Surg Neurol. 1976;5:51–53. [PubMed] [Google Scholar]
- 7.Weiner RL, Reed KL. Peripheral neurostimulation for control of intractable occipital neuralgia. Neuromodulation. 1999;2:217–221. doi: 10.1046/j.1525-1403.1999.00217.x [DOI] [PubMed] [Google Scholar]
- 8.Huntoon MA, Huntoon EA, Obray JB, Lamer TJ. Feasibility of ultrasound-guided percutaneous placement of peripheral nerve stimulation electrodes in a cadaver model: part one, lower extremity. Reg Anesth Pain Med. 2008;33(6):551–557. doi: 10.1016/j.rapm.2008.04.007 [DOI] [PubMed] [Google Scholar]
- 9.Huntoon MA, Burgher AH. Ultrasound-guided permanent implantation of peripheral nerve stimulation (PNS) system for neuropathic pain of the extremities: original cases and outcomes. Pain Med. 2009;10(8):1369–1377. doi: 10.1111/j.1526-4637.2009.00745.x [DOI] [PubMed] [Google Scholar]
- 10.Goroszeniuk T, Pang D. Peripheral neuromodulation: a review. Curr Pain Headache Rep. 2014;18:412. doi: 10.1007/s11916-014-0412-9 [DOI] [PubMed] [Google Scholar]
- 11.Deer TR, Jain S, Hunter C, et al. Neurostimulation for intractable chronic pain. Brain Sci. 2019;9(2):23. doi: 10.3390/brainsci9020023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer-Friebem CH, Wiegand T, Eitner L, et al. Effects of spinal cord and peripheral nerve stimulation reflected in sensory profiles and endogenous pain modulation. Clin J Pain. 2019;35(2):111–120. doi: 10.1097/AJP.0000000000000661 [DOI] [PubMed] [Google Scholar]
- 13.Yang F, Zhang T, Tiwari V, et al. Effects of combined electrical stimulation of the dorsal column and dorsal roots on wide dynamic-range neuronal activity in nerve-injured rats. Neuromodulation. 2015;18(7):592–598. doi: 10.1111/ner.12341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang F, Xu Q, Cheong Y, et al. Comparison of intensity dependent inhibition of spinal wide-dynamic range neurons by dorsal column and peripheral nerve stimulation in a rat model of neuropathic pain. Eur J Pain. 2014;18(7):978–988. doi: 10.1002/j.1532-2149.2013.00443.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radhakrishnan R, King E, Dickman J, et al. Spinal 5-HT2 and 5-HT3 receptors mediate low, but not high, frequency TENS-induced antihyperalgesia in rats. Pain. 2003;105(1):205–213. doi: 10.1016/S0304-3959(03)00207-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong Y, Baik E, Nam T, Paik K. Effects of iontophoretically applied naloxone, picrotoxin and strychnine on dorsal horn neuron activities treated with high frequency conditioning stimulation in cats. Yonsei Med J. 1995;36(4):336–347. doi: 10.3349/ymj.1995.36.4.336 [DOI] [PubMed] [Google Scholar]
- 17.Torebjork HE, Hallin RG. Responses in human A and C fibres to repeated electrical intradermal stimulation. J Neurol Neurosurg Psychiatry. 1974;37(6):653–656. doi: 10.1136/jnnp.37.6.653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deer TR, Eldabe S, Falowski SM, et al. Peripherally induced reconditioning of the central nervous system: a proposed mechanistic theory for sustained relief of chronic pain with percutaneous peripheral nerve stimulation. J Pain Res. 2021;14:721–736. doi: 10.2147/JPR.S297091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slavin KV. Peripheral nerve stimulation for neuropathic pain. Neurotherapeutics. 2008;5:100–106. doi: 10.1016/j.nurt.2007.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gilmore CA, Desai MJ, Hopkins TJ, et al. Treatment of chronic axial back pain with 60- day percutaneous medial branch PNS: primary end point results from a prospective, multicenter study. Pain Pract. 2021;21(8):877–889. doi: 10.1111/papr.13055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin T, Gargya A, Singh H, Sivanesan E, Gulati A. Mechanism of peripheral nerve stimulation in chronic pain. Pain Med. 2020;21(Suppl 1):S6–S12. doi: 10.1093/pm/pnaa164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deer TR, Mekhail N, Provenzano D, et al. The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: the Neuromodulation Appropriateness Consensus Committee. Neuromodulation. 2014;17(6):515–550. doi: 10.1111/ner.12208 [DOI] [PubMed] [Google Scholar]
- 23.Deer TR, Krames E, Mekhail N, et al.; for Neuromodulation Appropriateness Consensus Committee. The appropriate use of neurostimulation: new and evolving neurostimulation therapies and applicable treatment for chronic pain and selected disease states. Neuromodulation. 2014;17(6):599–615. doi: 10.1111/ner.12204 [DOI] [PubMed] [Google Scholar]
- 24.Deer TR, Mekhail N, Petersen E, et al.; for Neuromodulation Appropriateness Consensus Committee. The appropriate use of neurostimulation: stimulation of the intracranial and extracranial space and head for chronic pain. Neuromodulation. 2014;17(6):551–570. doi: 10.1111/ner.12215 [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Slavin KV, Isagulyan ED, Gomez C, Yin D. Occipital nerve stimulation. Neurosurg Clin N Am. 2019;30(2):211–217. doi: 10.1016/j.nec.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 27.GBD Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kapural L, Mekhail N, Hayek SM, Stanton-Hicks M, Malak O. Occipital nerve electrical stimulation via the midline approach and subcutaneous surgical leads for treatment of severe occipital neuralgia: a pilot study. Anesth Analg. 2005;101(1):171–174. doi: 10.1213/01.ANE.0000156207.73396.8E [DOI] [PubMed] [Google Scholar]
- 29.Hayek SM, Jasper JF, Deer TR, Narouze SN. Occipital neurostimulation-induced muscle spasms: implications for lead placement. Pain Physician. 2009;12(5):867–876. doi: 10.36076/ppj.2009/12/867 [DOI] [PubMed] [Google Scholar]
- 30.Dodick DW, Silberstein SD, Reed KL, et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: longterm results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia. 2015;35:344–358. doi: 10.1177/0333102414543331 [DOI] [PubMed] [Google Scholar]
- 31.Mekhail NA, Estemalik E, Azer G, et al. Safety and efficacy of occipital nerves stimulation for the treatment of chronic migraines: randomized, double-blind, controlled single-center experience. Pain Pract. 2017;17:669–677. doi: 10.1111/papr.12504 [DOI] [PubMed] [Google Scholar]
- 32.Saper JR, Dodick DW, Silberstein SD, et al. Occipital nerve stimulation for the treatment of intractable chronic migraine headache: ONSTIM feasibility study. Cephalalgia. 2011;31:271–285. doi: 10.1177/0333102410381142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serra G, Marchioretto F. Occipital nerve stimulation for chronic migraine: a randomized trial. Pain Physician. 2012;15:245–253. doi: 10.36076/ppj.2012/15/245 [DOI] [PubMed] [Google Scholar]
- 34.Silberstein SD, Dodick DW, Saper J, et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, doubleblinded, controlled study. Cephalalgia. 2012;32:1165–1179. doi: 10.1177/0333102412462642 [DOI] [PubMed] [Google Scholar]
- 35.Antony AB, Mazzola AJ, Dhaliwal GS, Hunter CW. Neurostimulation for the treatment of chronic head and facial pain: a literature review. Pain Physician. 2019;22(5):447–477. doi: 10.36076/ppj/2019.22.447 [DOI] [PubMed] [Google Scholar]
- 36.Slavin KV, Colpan ME, Munawar N, Wess C, Nersesyan H. Trigeminal and occipital peripheral nerve stimulation for craniofacial pain: a single-institution experience and review of the literature. Neurosurg Focus. 2006;21(6):1–5. doi: 10.3171/foc.2006.21.6.8 [DOI] [PubMed] [Google Scholar]
- 37.Wilson RD, Gunzler DD, Bennett ME, Chae J. Peripheral nerve stimulation compared with usual care for pain relief of hemiplegic shoulder pain: a randomized controlled trial. Am J Phys Med Rehabil. 2014;93(1):17–28. doi: 10.1097/PHM.0000000000000011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilson RD, Knutson JS, Bennett ME, Chae J. The effect of peripheral nerve stimulation on shoulder biomechanics: a randomized controlled trial in comparison to physical therapy. Am J Phys Med Rehabil. 2017;96(3):191–198. doi: 10.1097/PHM.0000000000000677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ilfeld BM, Gelfand H, Dhanjal S, et al. Ultrasound-guided percutaneous peripheral nerve stimulation: a pragmatic effectiveness trial of a nonpharmacologic alternative for the treatment of postoperative pain. Pain Med. 2020;21(Suppl 2):S53–S61. doi: 10.1093/pm/pnaa332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bouche B, Manfiotto M, Rigoard P, et al. Peripheral nerve stimulation of brachial plexus nerve roots and supra-scapular nerve for chronic refractory neuropathic pain of the upper limb. Neuromodulation. 2017;20(7):684–689. doi: 10.1111/ner.12573 [DOI] [PubMed] [Google Scholar]
- 41.Wu A, March L, Zheng X, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299. doi: 10.21037/atm.2020.02.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169(3):251–258. doi: 10.1001/archinternmed.2008.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nijs J, Van Houdenhove B, Oostendorp RA. Recognition of central sensitization in patients with musculoskeletal pain: application of pain neurophysiology in manual therapy practice. Man Ther. 2010;15(2):135–141. doi: 10.1016/j.math.2009.12.001 [DOI] [PubMed] [Google Scholar]
- 44.Verrills P, Sinclair C, Barnard A. A review of spinal cord stimulation systems for chronic pain. J Pain Res. 2016;9:481–492. doi: 10.2147/JPR.S108884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.D’Souza RS, Strand N. Neuromodulation with burst and tonic stimulation decreases opioid consumption: a post hoc analysis of the success using neuromodulation with BURST (SUNBURST) randomized controlled trial. Neuromodulation. 2021;24(1):135–141. doi: 10.1111/ner.13273 [DOI] [PubMed] [Google Scholar]
- 46.Kapural L, Peterson E, Provenzano DA, Staats P. Clinical evidence for spinal cord stimulation for Failed Back Surgery Syndrome (FBSS): systematic review. Spine. 2017;42(Suppl 14):S61–S66. doi: 10.1097/BRS.0000000000002213 [DOI] [PubMed] [Google Scholar]
- 47.Odonkor CA, Orman S, Orhurhu V, Stone ME, Ahmed S. Spinal cord stimulation vs conventional therapies for the treatment of chronic low back and leg pain: a systematic review of health care resource utilization and outcomes in the last decade. Pain Med. 2019;20(12):2479–2494. doi: 10.1093/pm/pnz185 [DOI] [PubMed] [Google Scholar]
- 48.Conger A, Sperry BP, Cheney CW, et al. The effectiveness of spinal cord stimulation for the treatment of axial low back pain: a systematic review with narrative synthesis. Pain Med. 2020;21(11):2699–2712. doi: 10.1093/pm/pnaa142 [DOI] [PubMed] [Google Scholar]
- 49.Eldabe SS, Taylor RS, Goossens S, et al. A randomized controlled trial of subcutaneous nerve stimulation for back pain due to failed back surgery syndrome: the SubQStim study. Neuromodulation. 2019;22(5):519–528. doi: 10.1111/ner.12784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kloimstein H, Likar R, Kern M, et al. Peripheral nerve field stimulation (PNFS) in chronic low back pain: a prospective multicenter study. Neuromodulation. 2014;17(2):180–187. doi: 10.1111/ner.12139 [DOI] [PubMed] [Google Scholar]
- 51.Burgher AH, Huntoon MA, Turley TW, Doust MW, Stearns LJ. Subcutaneous peripheral nerve stimulation with inter-lead stimulation for axial neck and low back pain: case series and review of the literature. Neuromodulation. 2012;15(2):100–107. doi: 10.1111/j.1525-1403.2011.00388.x [DOI] [PubMed] [Google Scholar]
- 52.Guentchev M, Preuss C, Rink R, Peter L, Sailer MHM, Tuettenberg J. Long-term reduction of sacroiliac joint pain with peripheral nerve stimulation. Oper Neurosurg. 2017;13(5):634–639. doi: 10.1093/ons/opx017 [DOI] [PubMed] [Google Scholar]
- 53.Deer TR, Gilmore CA, Desai MJ, et al. Percutaneous peripheral nerve stimulation of the medial branch nerves for the treatment of chronic axial back pain in patients after radiofrequency ablation. Pain Med. 2021;22(3):548–560. doi: 10.1093/pm/pnaa432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gilmore CA, Kapural L, McGee MJ, Boggs JW. Percutaneous peripheral nerve stimulation for chronic low back pain: prospective case series with 1 year of sustained relief following short-term implant. Pain Pract. 2020;20(3):310–320. doi: 10.1111/papr.12856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mainkar O, Solla CA, Chen G, Legler A, Gulati A. Pilot study in temporary peripheral nerve stimulation in oncologic pain. Neuromodulation. 2020;23(6):819–826. doi: 10.1111/ner.13139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Billet B, Wynendaele R, Vanquathem NE. A novel minimally invasive wireless technology for neuromodulation via percutaneous intercostal nerve stimulation for post-herpetic neuralgia: a case report with short-term follow-up. Pain Pract. 2018;18(3):374–379. doi: 10.1111/papr.12607 [DOI] [PubMed] [Google Scholar]
- 57.Kouroukli I, Neofytos D, Panaretou V, et al. Peripheral subcutaneous stimulation for the treatment of intractable postherpetic neuralgia: two case reports and literature review. Pain Pract. 2009;9(3):225–229. doi: 10.1111/j.1533-2500.2009.00263.x [DOI] [PubMed] [Google Scholar]
- 58.Peyravi M, Capelle HH, Fischer S, Haverich A, Krauss JK. Subcutaneous peripheral neurostimulation for the treatment of severe chronic poststernotomy neuralgia. Stereotact Funct Neurosurg. 2011;89(4):253–257. doi: 10.1159/000328271 [DOI] [PubMed] [Google Scholar]
- 59.Yakovlev AE, Peterson AT. Peripheral nerve stimulation in treatment of intractable postherpetic neuralgia. Neuromodulation. 2007;10(4):373–375. doi: 10.1111/j.1525-1403.2007.00126.x [DOI] [PubMed] [Google Scholar]
- 60.Mainkar O, Singh H, Gargya A, Lee J, Valimahomed A, Gulati A. Ultrasound-guided peripheral nerve stimulation of cervical, thoracic, and lumbar spinal nerves for dermatomal pain: a case series. Neuromodulation. 2021;24(6):1059–1066. doi: 10.1111/ner.13334 [DOI] [PubMed] [Google Scholar]
- 61.Deer T, Pope J, Benyamin R, et al. Prospective, multicenter, randomized, double-blinded, partial crossover study to assess the safety and efficacy of the novel neuromodulation system in the treatment of patients with chronic pain of peripheral nerve origin. Neuromodulation. 2016;19(1):91–100. doi: 10.1111/ner.12381 [DOI] [PubMed] [Google Scholar]
- 62.Gilmore C, Ilfeld B, Rosenow J, et al. Percutaneous peripheral nerve stimulation for the treatment of chronic neuropathic postamputation pain: a multicenter, randomized, placebo-controlled trial. Reg Anesth Pain Med. 2019;44(6):637–645. doi: 10.1136/rapm-2018-100109 [DOI] [PubMed] [Google Scholar]
- 63.Gilmore CA, Ilfeld BM, Rosenow JM, et al. Percutaneous 60-day peripheral nerve stimulation implant provides sustained relief of chronic pain following amputation: 12-month follow-up of a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2020;45:44–51. doi: 10.1136/rapm-2019-100937 [DOI] [PubMed] [Google Scholar]
- 64.Rauck RL, Cohen SP, Gilmore CA, et al. Treatment of post-amputation pain with peripheral nerve stimulation. Neuromodulation. 2014;17(2):188–197. doi: 10.1111/ner.12102 [DOI] [PubMed] [Google Scholar]
- 65.Campbell JN, Long DM. Peripheral nerve stimulation in the treatment of intractable pain. J Neurosurg. 1976;45(6):692–699. doi: 10.3171/jns.1976.45.6.0692 [DOI] [PubMed] [Google Scholar]
- 66.Colini Baldeschi G, Dario A, De Carolis G, et al. Peripheral nerve stimulation in the treatment of chronic pain syndromes from nerve injury: a multicenter observational study. Neuromodulation. 2016;20:369–374. doi: 10.1111/ner.12539 [DOI] [PubMed] [Google Scholar]
- 67.Cornish P, Wall C. Successful peripheral neuromodulation for phantom limb pain. Pain Med. 2015;16(4):761–764. doi: 10.1111/pme.12532 [DOI] [PubMed] [Google Scholar]
- 68.Dabby R, Sadeh M, Goldberg I, Finkelshtein V. Electrical stimulation of the posterior tibial nerve reduces neuropathic pain in patients with polyneuropathy. J Pain Res. 2017;10:2717–2723. doi: 10.2147/JPR.S137420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Deogaonkar M. Peripheral neuromodulation for chronic pain. Neurol India. 2020;68(8):S224–S230. doi: 10.4103/0028-3886.302451 [DOI] [PubMed] [Google Scholar]
- 70.Freitas TDS, Fonoff ET, Marquez Neto OR, et al. Peripheral nerve stimulation for painful mononeuropathy secondary to leprosy: a 12-month follow-up study. Neuromodulation. 2018;21(3):310–316. doi: 10.1111/ner.12714 [DOI] [PubMed] [Google Scholar]
- 71.Langford B, Mauck WD. Advancement in neuromodulation technology with the innovation of design-specific peripheral nerve stimulators: sural nerve stimulation for radiculopathy. Pain Med. 2020;21(6):1297–1300. doi: 10.1093/pm/pnaa077 [DOI] [PubMed] [Google Scholar]
- 72.Langford B, Mauck WD. Peripheral nerve stimulation: a new treatment for meralgia paresthetica. Pain Med. 2021;22(1):213–216. doi: 10.1093/pm/pnaa326 [DOI] [PubMed] [Google Scholar]
- 73.Law JD, Swett J, Kirsch WM. Retrospective analysis of 22 patients with chronic pain treated by peripheral nerve stimulation. J Neurosurg. 1980;52(4):482–485. doi: 10.3171/jns.1980.52.4.0482 [DOI] [PubMed] [Google Scholar]
- 74.Marvel RP. Obturator neuromodulation with laparoscopic placement of an obturator lead for the treatment of intractable opioid-dependent chronic pelvic pain due to obturator neuralgia. J Minim Invasive Gynecol. 2018;25(7):1295–1299. doi: 10.1016/j.jmig.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 75.Meier K, Bendtsen TF, Sørensen JC, Nikolajsen L. Peripheral neuromodulation for the treatment of postamputation neuroma pain: a case report. A Case Rep. 2017;8(2):29–30. doi: 10.1213/XAA.0000000000000413 [DOI] [PubMed] [Google Scholar]
- 76.Narouze SN, Zakari A, Vydyanathan A. Ultrasound-guided placement of a permanent percutaneous femoral nerve stimulator leads for the treatment of intractable femoral neuropathy. Pain Physician. 2009;12(4):E305–E308. doi: 10.36076/ppj.2009/12/E305 [DOI] [PubMed] [Google Scholar]
- 77.Ramineni T, Prusik J, De La Cruz P, et al. The impact of peripheral nerve stimulation on disability and depression. Neuromodulation. 2016;19(3):306–310. doi: 10.1111/ner.12363 [DOI] [PubMed] [Google Scholar]
- 78.Rauck RL, Kapural L, Cohen SP, et al. Peripheral nerve stimulation for the treatment of postamputation pain–a case report. Pain Pract. 2012;12(8):649–655. doi: 10.1111/j.1533-2500.2012.00552.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Reverberi C, Dario A, Barolat G, Zuccon G. Using peripheral nerve stimulation (PNS) to treat neuropathic pain: a clinical series. Neuromodulation. 2014;17(8):777–783. doi: 10.1111/ner.12157 [DOI] [PubMed] [Google Scholar]
- 80.Sokal P, Harat M, Zieliński P, Kierońska S. Tibial nerve stimulation with a miniature, wireless stimulator in chronic peripheral neuropathic pain. J Pain Res. 2017;10:613–619. doi: 10.2147/JPR.S128861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Van Calenbergh F, Gybels J, Van Laere K, et al. Long term clinical outcome of peripheral nerve stimulation in patients with chronic peripheral neuropathic pain. Surg Neurol. 2009;72(4):330–335. doi: 10.1016/j.surneu.2009.03.006 [DOI] [PubMed] [Google Scholar]
- 82.Warner NS, Schaefer KK, Eldrige JS, et al. Peripheral nerve stimulation and clinical outcomes: a retrospective case series. Pain Pract. 2021;21(4):411–418. doi: 10.1111/papr.12968 [DOI] [PubMed] [Google Scholar]
- 83.Johnson S, Ayling H, Sharma M, Goebel A. External noninvasive peripheral nerve stimulation treatment of neuropathic pain: a prospective audit. Neuromodulation. 2015;18(5):384–391. doi: 10.1111/ner.12244 [DOI] [PubMed] [Google Scholar]
- 84.Rossi M, DeCarolis G, Liberatoscioli G, Iemma D, Nosella P, Nardi LF. A novel mini-invasive approach to the treatment of neuropathic pain: the PENS study. Pain Physician. 2016;19(1):E121–E128. [PubMed] [Google Scholar]
- 85.Ilfeld BM, Ball ST, Gabriel RA, et al. A feasibility study of percutaneous peripheral nerve stimulation for the treatment of postoperative pain following total knee arthroplasty. Neuromodulation. 2019;22(5):653–660. doi: 10.1111/ner.12790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ilfeld BM, Gilmore CA, Grant SA, et al. Ultrasound-guided percutaneous peripheral nerve stimulation for analgesia following total knee arthroplasty: a prospective feasibility study. J Orthop Surg Res. 2017;12(1):4. doi: 10.1186/s13018-016-0506-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ilfeld BM, Ball ST, Cohen SP, et al. Percutaneous peripheral nerve stimulation to control postoperative pain, decrease opioid use, and accelerate functional recovery following orthopedic trauma. Mil Med. 2019;184(Suppl 1):557–564. doi: 10.1093/milmed/usy378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ilfeld BM, Gabriel RA, Said ET, et al. Ultrasound-guided percutaneous peripheral nerve stimulation: neuromodulation of the sciatic nerve for postoperative analgesia following ambulatory foot surgery, a proof-of-concept study. Reg Anesth Pain Med. 2018;43(6):580–589. doi: 10.1097/AAP.0000000000000819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stanton-Hicks M, Burton AW, Bruehl SP, et al. An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract. 2002;2(1):1–16. doi: 10.1046/j.1533-2500.2002.02009.x [DOI] [PubMed] [Google Scholar]
- 90.Stanton-Hicks M, Baron R, Boas R, et al. Complex regional pain syndromes: guidelines for therapy. Clin J Pain. 1998;14:155–166. doi: 10.1097/00002508-199806000-00012 [DOI] [PubMed] [Google Scholar]
- 91.Hassenbusch SJ, Stanton-Hicks M, Schoppa D, Walsh JG, Covington EC. Long-term results of peripheral nerve stimulation for reflex sympathetic dystrophy. J Neurosurg. 1996;84(3):415–423. doi: 10.3171/jns.1996.84.3.0415 [DOI] [PubMed] [Google Scholar]
- 92.Chmiela MA, Hendrickson M, Hale J, et al. Direct peripheral nerve stimulation for the treatment of complex regional pain syndrome: a 30-year review. Neuromodulation. 2021;24(6):971–982. doi: 10.1111/ner.13295 [DOI] [PubMed] [Google Scholar]
- 93.Frederico TN, da Silva Freitas T. Peripheral nerve stimulation of the brachial plexus for chronic refractory CRPS pain of the upper limb: description of a new technique and case series. Pain Med. 2020;21(Suppl 1):S18–S26. doi: 10.1093/pm/pnaa201 [DOI] [PubMed] [Google Scholar]
- 94.Buwembo J, Munson R, Rizvi SA, Ijaz A, Gupta S. Direct sciatic nerve electrical stimulation for complex regional pain syndrome type 1. Neuromodulation. 2021;24(6):1075–1082. doi: 10.1111/ner.13294 [DOI] [PubMed] [Google Scholar]
- 95.Wilson RD, Bennett ME, Nguyen VQC, et al. Fully implantable peripheral nerve stimulation for hemiplegic shoulder pain: a multi-site case series with two-year follow-up. Neuromodulation. 2018;21(3):290–295. doi: 10.1111/ner.12726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Deer TR, Lamer TJ, Pope JE, et al. The Neurostimulation Appropriateness Consensus Committee (NACC) safety guidelines for the reduction of severe neurological injury. Neuromodulation. 2017;20(1):15–30. doi: 10.1111/ner.12564 [DOI] [PubMed] [Google Scholar]
- 97.Narouze S, Benzon HT, Provenzano D, et al. Interventional spine and pain procedures in patients on antiplatelet and anticoagulant medications (second edition): guidelines from the American Society of Regional Anesthesia and Pain Medicine, the European Society of Regional Anaesthesia and Pain Therapy, the American Academy of Pain Medicine, the International Neuromodulation Society, the North American Neuromodulation Society, and the World Institute of Pain. Reg Anesth Pain Med. 2018;43(3):225–262. doi: 10.1097/AAP.0000000000000700 [DOI] [PubMed] [Google Scholar]
- 98.Poutoglidou F, Piagkou M, Totlis T, Tzika M, Natsis K. Sciatic nerve variants and the piriformis muscle: a systematic review and meta-analysis. Cureus. 2020;12(11):e11531. doi: 10.7759/cureus.11531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chang KV, Mezian K, Naňka O, Wu WT, Lin CP, Özçakar L. Ultrasound-guided interventions for painful shoulder: from anatomy to evidence. J Pain Res. 2018;11:2311–2322. doi: 10.2147/JPR.S169434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Laumonerie P, Lapègue F, Chantalat E, Sans N, Mansat P, Faruch M. Description and ultrasound targeting of the origin of the suprascapular nerve. Clin Anat. 2017;30(6):747–752. doi: 10.1002/ca.22936 [DOI] [PubMed] [Google Scholar]
- 101.Polguj M, Rożniecki J, Sibiński M, et al. The variable morphology of suprascapular nerve and vessels at suprascapular notch: a proposal for classification and its potential clinical implications. Knee Surg Sports Traumatol Arthrosc. 2015;23:1542–1548. doi: 10.1007/s00167-014-2937-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Leechavengvongs S, Teerawutthichaikit T, Witoonchart K, et al. Surgical anatomy of the axillary nerve branches to the deltoid muscle. Clin Anat. 2015;28:118–122. doi: 10.1002/ca.22352 [DOI] [PubMed] [Google Scholar]
- 103.Mazzola A, Spinner D. Ultrasound-guided peripheral nerve stimulation for shoulder pain: anatomic review and assessment of the current clinical evidence. Pain Physician. 2020;23(5):E461–E474. [PubMed] [Google Scholar]
- 104.Binder DS, Nampiaparampil DE. The provocative lumbar facet joint. Curr Rev Musculoskelet Med. 2009;2(1):15–24. doi: 10.1007/s12178-008-9039-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bogduk N. The lumbar mamillo-accessory ligament. Its anatomical and neurosurgical significance. Spine. 1981;6(2):162–167. doi: 10.1097/00007632-198103000-00010 [DOI] [PubMed] [Google Scholar]
- 106.U.S. Food and Drug Administration. Bioness Inc. StimRouter neuromodulation system K200482 approval letter; 2020. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf20/K200482.pdf. Accessed July 29, 2022.
- 107.Sayed D, Chakravarthy K, Amirdelfan K, et al. A comprehensive practice guideline for magnetic resonance imaging compatibility in implanted neuromodulation devices. Neuromodulation. 2020;23:893–911. doi: 10.1111/ner.13233 [DOI] [PubMed] [Google Scholar]
- 108.U.S. Food and Drug Administration. Nalu Medical Inc. Neuromodulation system for peripheral nerve stimulation K183579 approval letter; 2019. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf18/K183579.pdf. Accessed July 29, 2022.
- 109.U.S. Food and Drug Administration. Stimwave Technologies Inc. StimQ peripheral nerve stimulator system K171366 approval letter; 2017. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf17/K171366.pdf. Accessed July 29, 2022.
- 110.U.S. Food and Drug Administration. SPR therapeutics Inc. SPRINT peripheral nerve stimulation system K181422 approval letter; 2018. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf18/K181422.pdf. Accessed July 29, 2022.
- 111.U.S. Food and Drug Administration. Mainstay medical limited ReActiv8 implantable neurostimulation system P190021 approval letter; 2020. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf19/P190021C.pdf. Accessed July 29, 2022.
- 112.Harris RP, Helfand M, Woolf SH, et al.; for Methods Work Group, Third US Preventive Services Task Force. Current methods of the US Preventive Services Task Force: a review of the process. AM J Prev Med. 2001;20(Suppl 3):24–35. doi: 10.1016/S0749-3797(01)00261-6 [DOI] [PubMed] [Google Scholar]
- 113.Abd-Elsayed A, D’Souza RS. Peripheral nerve stimulation: the evolution in pain medicine. Biomedicines. 2021;10(1):18. doi: 10.3390/biomedicines10010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Food and Drug Administration. Section 510(k) premarket notification. Available from: https://www.accessdata.fda.gov/cdrh_docs/pdf21/K211801.pdf. Accessed August 10, 2022. [Google Scholar]