Abstract
Background
The World Health Organization recommends that pregnant women should receive a vaccine against COVID-19. However, COVID-19 vaccine hesitance was one of the barriers to delivering the vaccine, and this issue was not well addressed in Ethiopia. Therefore, we aimed to determine the prevalence of COVID-19 vaccination acceptability and the factors that influence it among pregnant women in Northeast Ethiopia.
Methods
A mixed-methods approach comprising both qualitative interviews and a quantitative survey was conducted from January 1–30, 2022. For the quantitative part, a multi-stage sampling technique was used to recruit the study participants (n=702). Data was collected through face-to-face interviews using pretested and structured questionnaires. Bivariate and multivariable logistic regression analyses were employed. The statistical difference was considered at P-0.05, and the strength of association was assessed by the odds ratio and respective 95% confidence intervals. For the qualitative part, 18 participants were selected purposively for in-depth interviews, an interviewer guide was used for data collection and thematic content analysis was performed.
Results
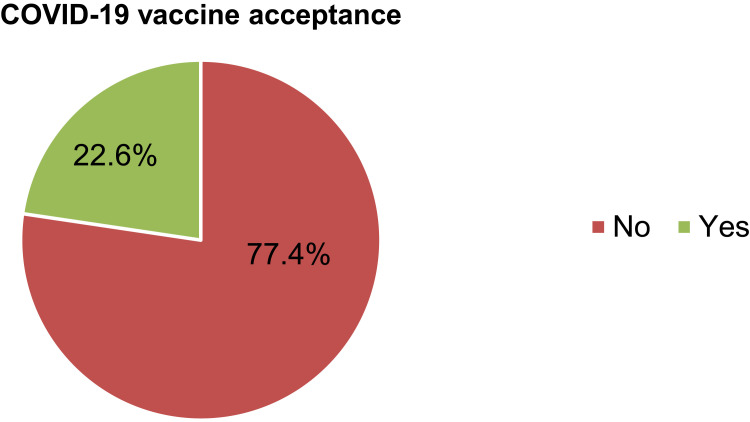
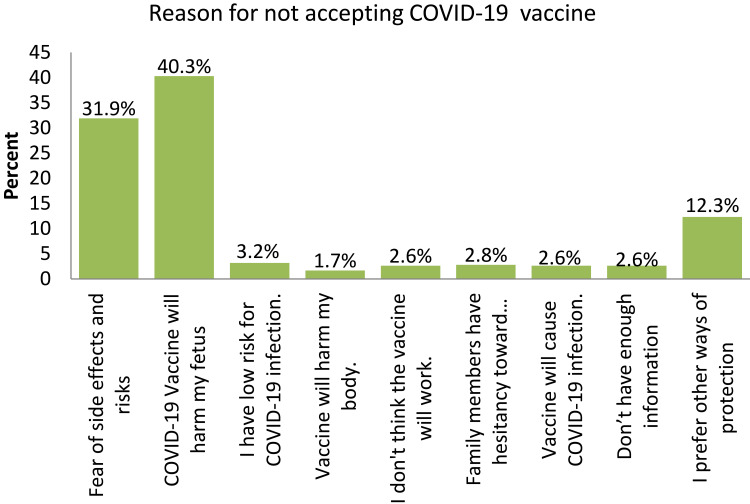
In this study, a total of 702 pregnant women were included with the response rate of 100%. The rate of COVID-19 vaccine acceptance was 22.6% (95% CI: 19.6%, 25.9%). The husbands’ educational level (AOR = 1.99, 95% CI: 1.09, 3.64), chronic medical illness (AOR = 2.41, 95% CI: 1.28, 4.54), positive attitude (AOR = 1.59, 95% CI: 1.09, 2.31), and good practice of COVID-19 preventive measures (AOR = 1.59, 95% CI: 1.09, 2.31) were determinant factors of COVID-19 vaccine acceptance. According to the qualitative findings, the most common reasons for COVID-19 vaccine hesitancy were fear of fetal side effects, misconceptions about the vaccine, and religious beliefs.
Conclusion
In this study, the acceptability of the COVID-19 vaccine was low. Therefore, health professionals should disseminate accurate vaccination information and address misinformation to boost vaccine acceptance among pregnant women.
Keywords: COVID-19 vaccine, a mixed method, pregnant women, Northeast Ethiopia
Introduction
COVID-19 has expanded to over 228 countries worldwide, causing a variety of severe issues that affect humanity, such as mortality and morbidity, as well as social and economic challenges.1,2 According to the World Health Organization (WHO) Coronavirus (COVID-19) Dashboard, as of December 27, 2021, there have been 290, 726,856 confirmed cases and 5,459,051 deaths reported worldwide, and in Ethiopia, 424,750 confirmed cases and 6947 deaths were reported.3 Findings from the WHO collaborating center for global women’s health show that COVID-19 was found in 9% of pregnant women who were admitted for any reason.4 According to a survey from Mexico, COVID-19 was the cause of 22.93% of maternal deaths.5 According to a study conducted in Iran, 7 of 9 pregnant women with severe COVID-19 disease died at the time of reporting, 1 of 9 was extremely ill and on a ventilator, and 1 of 9 recovered after protracted hospitalization.6
Pregnant women are known to be vulnerable to COVID-19 infection and are at risk of getting severe respiratory infections due to physiologic changes in their respiratory and immune systems.7,8 It has been observed that the clinical course of COVID-19 infection in pregnant women is worse than in non-pregnant women, which means that pregnant women with COVID-19 are more likely to require hospitalization, intensive care, and invasive ventilation to help with breathing.9–11 Pregnant women with severe and critical diseases had a higher rate of cesarean delivery, an increased risk for preterm birth, and pregnancy loss.12,13 Preventing critical COVID-19 infection is thus critical for both mother and child.
As studies indicate, vaccination against COVID-19 reduces the overall infection rate of COVID-19 and reduces deaths and hospitalization due to COVID-19 infection.14,15 Increasing evidence on the safety and effectiveness of COVID-19 vaccination during pregnancy suggests that the benefits of vaccination during pregnancy outweigh potential risks whenever there is ongoing or anticipated community transmission of the virus.9 WHO recommends that pregnant women should receive a vaccine against COVID-19.9 The American College of Obstetricians and Gynecologists (ACOG) also strongly recommends that pregnant individuals be vaccinated against COVID-19.16 The Society of Obstetricians and Gynecologists of Canada (SOGC) also recommends that all pregnant women should be prioritized to receive a COVID-19 vaccination.17
Studies suggested that having less knowledge about the COVID-19, more false perceptions or a poor attitude toward the COVID-19 vaccine, and not being willing to take the vaccine were the identified barriers to taking the COVID-19 vaccine.18–21 To improve COVID-19 vaccine uptake among pregnant women, it’s critical to first identify the obstacles to usage, which includes examining the socio-cultural factors that influence pregnant women’s refusal to take the vaccination.
As far as our knowledge, information on COVID-19 vaccine acceptance among pregnant women is limited in Ethiopia, and no studies have been conducted in the study area. Therefore, we aimed to determine the prevalence of COVID-19 vaccination acceptability and the factors that influence it among pregnant women in Northeast Ethiopia. We also attempted to examine the socio-cultural factors of COVID-19 vaccine hesitancy using qualitative analysis. In order to effectively enhance the uptake of the COVID-19 vaccine, the finding will help policymakers, health authorities, and other stakeholders establish targeted immunization campaigns and evidence-based recommendations.
Methods and Materials
Study Design and Setting
An institutional-based cross-section mixed-methods approach comprising both qualitative interviews and a quantitative survey was conducted from January 1–30, 2022 in public hospitals in the South Wollo Zone. South Wollo is one of the 12 zones in the Amhara Region of Ethiopia. There are 12 public hospitals in the south Wollo zone, namely: Mekaneselam Hospital, Hidar 11 Hospital, Nigist Zewditu Hospital, Jama Hospital, Haik Hospital, Tenta Hospital, Wegidi Hospital, Mekidela Hospital, Saint Hospital, Delanta Hospital, and Kelala Hospital Kombolcha General Hospital. These hospitals serve a population of 2,243,013.22
Population
All pregnant women attending antenatal care at South Wollo Zone public hospitals were the source population, whereas, pregnant women who were found in selected hospitals during the data collection period were the study population.
Eligibility Criteria
All pregnant mothers who were attending antenatal care follow-up at public hospitals in the south Wollo zone during the data collection period were included.
Sample Size Determination and Sampling Technique
The required sample size (n) for the quantitative part of the study was determined using a single population proportion formula considering the following assumptions: P = 70.7% of respondents in Southwest Ethiopia accepted the COVID-19 vaccine;23 confidence level (Z) = 95%; 5% margin of error (d); n=Z2/2 n=(1.96)2.707x 0.293/(.05)2 = 319. By considering a 10% non-response rate and a design effect of two, the final sample size for this study was 702. For the qualitative part, 18 participants were included in the study based on information saturation. A multistage sampling technique was employed to select study participants for the quantitative parts of the study. There are twelve public hospitals in South Wollo; five public hospitals (42%) were selected by a simple random sampling technique, namely, Haik primary hospital, Hidar 11 general hospital, Mekaneselam General Hospital, Nigist Zewdidu primary hospital, and Jama Hospital. The numbers of study participants for each hospital were estimated proportionally based on the hospital’s monthly average case flow by taking three consecutive months. Finally, the study participants were selected by a systematic random sampling method. For the qualitative parts of the study, the study participants were recruited purposively until data saturation was achieved.
Data Collection Procedure
For the qualitative parts of the study, face-to-face interviews with a pretested structured questionnaire were used to collect data. The questionnaire was adapted from previous similar literature23–28 and it includes information related to socio-demographic characteristics, medical and obstetric characteristics, knowledge, attitude, and practice of respondents on COVID-19 preventive measures, and the intention of COVID-19 vaccine acceptance among pregnant women. Five trained degree midwives used the Amharic version of the questionnaire to collect the data. In-depth interviews were conducted by the investigators for the qualitative part of the study.
Data Quality Control
The questionnaire was prepared originally in English and was translated into Amharic (the local language) and back to English by two independent persons to maintain the consistency of the questionnaire. The training was given to data collectors and supervisors. A pre-test was conducted using 5% of the questioners at Kemissie General Hospital and a necessary modification was made before the actual data collection.
Data Processing and Analysis
Before entering the data into Epi Data version 4.6 for the quantitative portion of the study, the collected data were checked for completeness and consistency. For analysis, the data was exported to SPSS version 25 software. The exported data was categorized and summarized using descriptive statistics like frequency tables, graphs, and proportions. Then bivariate analysis was carried out to assess the crude association between the independent and outcome variables. The variables with a P-value <0.2 in bivariate analysis were entered into a multivariable logistic regression to assess the net effect by controlling confounders. The variables with p < 0.05 in multivariable logistic regression were considered statistically significant factors for the knowledge and desire of antenatal clients about labor companions. The adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to assess the strength of the association. For the qualitative parts of the study, the data analysis was initiated by transcription and translation of the interviews, then coded and analyzed by thematic analysis.
Operational Definition
Vaccine Acceptance
COVID-19 vaccine acceptance was measured using “Yes” and “No” questions. Respondents were asked, “If the COVID-19 vaccine is available, are you willing to take it?” Those who answered “yes” received a score of 1, while those who answered “no” received a score of 0. Accordingly, respondents who scored 1 were thought of as having an intention to accept the COVID-19 vaccine and respondents.29
Knowledge About COVID-19
The respondents’ level of knowledge about COVID-19 was reported as good knowledge if the study participant correctly responded to more than or equal to 80% of the knowledge assessment tools, and poor for <80%.23
Attitudes Towards COVID-19
The participant’s attitude was classified as positive or favorable if they responded positively to more than 80% of the attitude-related items and negative if they responded negatively to less than 80% of the attitude-related items.23
The Practice of COVID-19 Preventive Measures
The respondents’ level of practice of COVID-19 preventive measures was reported as “good practice” if the study participant correctly responded to more than or equal to 80% of the practice assessment tools, and poor for 80%.23
Ethical Consideration
The study was carried out in accordance with the Helsinki Declaration. The research team confirm that this research caused no harm (physical or mental) to any participants. Ethical clearance was obtained from Wollo University, College of Medicine and Health Sciences Ethical Review Committee. A letter of cooperation was obtained from the South Wollo zone health office. The research process complies with the Declaration of Helsinki. Written consent was obtained from individual respondents. Information on the study was explained to the study participants, including the objective, procedure, and benefit of the study. The respondents were informed that they have the right to refuse or decline participation in the study at any time. The participants’ confidentiality was secured throughout the study, and information regarding the identification of the patient was recorded anonymously.
Results
Quantitative
Socio-Demographic Characteristics
A total of 702 pregnant women were interviewed successfully, making a response rate of 100%. Of those, 622 (88.6%) respondents were in the age range of 20–34 years. The great majority (98.4%) of the study participants were married. More than half (69.9%) of the respondents were Muslim, followed by Orthodox Christians (28.8%). Regarding educational status, 384 (54.7%) of the study subjects had completed secondary school and above. The majority of the respondents (62.8%) lived in urban areas (Table 1).
Table 1.
Socio-Demographic Characteristics of the Respondents in South Wollo Northeast Ethiopia, 2022
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age the mother | ||
| <20 | 19 | 2.7% |
| 20–34 | 622 | 88.6% |
| 35–49 | 61 | 8.7% |
| Marital status | ||
| Single | 7 | 1% |
| Married | 691 | 98.4% |
| Divorced | 4 | 0.6% |
| Religion | ||
| Orthodox | 202 | 28.8% |
| Muslim | 491 | 69.9% |
| Protestant | 6 | 0.9% |
| Catholic | 3 | 0.4% |
| Place of residence | ||
| Urban | 441 | 62.8% |
| Rural | 261 | 37.2% |
| Educational level | ||
| No formal education | 156 | 22.2% |
| Primary school | 162 | 23.1% |
| Secondary School and above | 384 | 54.7% |
| Occupational status | ||
| Housewife | 103 | 14.7% |
| Government employee | 216 | 30.8% |
| Farmer | 181 | 25.8% |
| Student | 57 | 8.1% |
| Merchant | 145 | 20.7% |
| Husbands educational level | ||
| No formal education | 142 | 20.2% |
| Primary education | 205 | 29.2% |
| Secondary education | 168 | 23.9% |
| Diploma and above | 187 | 26.6% |
| Husbands occupational status | ||
| Government Employee | 272 | 38.7% |
| Private employee | 194 | 27.6% |
| Merchant | 109 | 15.5% |
| Student | 69 | 9.8% |
| Farmer | 58 | 8.3% |
Maternal Medical and Obstetric Related Characteristics
The majority of the responders, 507(72.2%), were multigravida. The second antenatal care appointment was attended by around a quarter of the respondents (34.6%). A percentage of the respondents (7.3%) had a medical history. In terms of medical conditions, 18 (35.3%) had a history of hypertension, followed by diabetes mellitus (27.5) (Table 2).
Table 2.
Medical and Obstetrics Related Characteristics of Respondents in South Wollo Northeast Ethiopia, 2022
| Characteristics | Frequency | Percentage |
|---|---|---|
| Gravidity | ||
| Primigravida | 195 | 27.8% |
| Multigravida | 507 | 72.2% |
| ANC visit | ||
| 1st Visit | 226 | 32.2% |
| 2nd visit | 243 | 34.6% |
| 3rd visit | 165 | 23.5% |
| 4th visit | 68 | 9.7% |
| Medical illness | ||
| Yes | 51 | 7.3% |
| No | 651 | 92.7% |
| Types of medical illness | ||
| Hypertension | 18 | 35.3% |
| Diabetic Mellitus | 14 | 27.5% |
| Kidney disease | 8 | 15.7% |
| Asthma | 9 | 17.6% |
| Cardiac disease | 2 | 3.9% |
| ANC= Antenatal care | ||
Knowledge of the Pregnant Women About COVID-19
All of the 702 study participants (100%) reported that they had ever heard about the coronavirus pandemic. The majority (81.6%) of the pregnant women responded that they knew at least one common symptom of COVID-19 infection. Eighty-eight percent of all respondents were aware that COVID-19 currently has no effective treatment, and 98.6% were aware that COVID-19 can infect anyone (Table 3).
Table 3.
Knowledge of Pregnant Women About COVID-19 in Northeast Ethiopia, 2022
| No | Variables | Yes (%) | No (%) |
|---|---|---|---|
| 1 | Heard about COVID-19 | 702(100%) | 0(0%) |
| 2 | Re-infection can occur with COVID-19 | 490(69.8%) | 212(30.2%) |
| 3 | COVID-19 has effective treatment presently | 84(12.0%) | 618(88.0%) |
| 4 | Do you know the symptom of COVID-19 infection | 573(81.6%) | 129(18.4%) |
| 5 | Everybody can be infected by COVID-19 | 692(98.6%) | 10(1.4%) |
| 6 | COVID-19 is severe in Co-morbid and elderly people | 451(64.2%) | 251(35.8%) |
| 7 | Avoiding crowding can decrease the risk of COVID-19 | 656 (93.4%) | 46(6.6%) |
| 8 | Avoiding touching eyes and nose prevents COVID-19 | 680 (96.9%) | 22(3.1%) |
| 9 | COVID-19 infection can be transmitted by air droplets | 699(99.6%) | 3(0.4%) |
| 10 | Ordinary people should use the mask to prevent COVID | 668(95.2%) | 34(4.8%) |
| 11 | Isolation is important after contact with an infected person | 619(88.2%) | 83(11.8%) |
| 12 | Reporting the suspected symptom is recommended | 626(89.2%) | 76 (10.8%) |
Attitude and Perception Toward COVID-19
The great majority (90.3%) of study participants thought that COVID-19 infection increases in crowding and gatherings. Most of them (82.8%) believe that health education can protect against COVID-19. More than half (65.4%) of the respondents believe that disinfection of the public and buildings protects against COVID-19 (Table 4).
Table 4.
Attitude of Respondents Towards COVID-19 Infection in South Wollo Northeast Ethiopia, 2022
| No | Variables | Agree | Disagree |
|---|---|---|---|
| 1 | COVID-19 infection increases in crowding and gatherings | 634(90.3%) | 68(9.7%) |
| 2 | Health education can protect against COVID-19 | 581(82.8%) | 121(17.2%) |
| 3 | Disinfection of the public and buildings protect against COVID-19 | 459(65.4%) | 243(34.6%) |
| 4 | Country instructions are taken to limit the spread of COVID-19 | 550(78.3%) | 152(21.7%) |
| 5 | Country instructions are enough | 467(66.5%) | 235(33.5%) |
| 6 | All people are committed to the country’s instructions | 528(75.2%) | 174(24.8%) |
| 7 | COVID-19 will be contained soon | 349(49.7%) | 353(50.3%) |
The Practice of COVID-19 Preventive Measures
The women’s responses regarding the practice of preventive measures against COVID-19 infection were frequent handwashing with water and soap (94.6%), covering the mouth with an elbow while sneezing (81.9%), wearing a face mask when going out (47.4%), keeping a physical distance (54.6%), and avoiding going to social gatherings (52.8%) (Table 5).
Table 5.
Practice of COVID-19 Preventive Measures Among Pregnant Women in Northeast Ethiopia, 2022
| No | Practice Question | Yes | No |
|---|---|---|---|
| 1 | Wash hand with soap/use sanitizer | 664(94.6%) | 38(5.4%) |
| 2 | Covering mouth with an elbow while sneezing | 575(81.9%) | 127(18.1%) |
| 3 | Wearing a face mask when going out | 333(47.4%) | 369(52.6%) |
| 4 | Reporting COVID-19 symptoms to the health facility | 547(77.9%) | 155(22.1%) |
| 5 | Keeping physical distancing | 383(54.6%) | 319(45.4%) |
| 6 | Avoiding going to the social gathering | 528(75.2%) | 174(24.8%) |
| 7 | Staying at home /working from home | 136(19.4%) | 566(80.6%) |
| 8 | Changing travel | 423(60.3%) | 279(39.7%) |
| 9 | Stop handshaking with people | 304(43.3%) | 398(56.7%) |
| 10 | Health care seeking when getting ill | 542(77.2%) | 160(22.8%) |
COVID-19 Vaccine Acceptance Among Pregnant Women
The COVID-19 vaccine acceptance if it is available was found to be 22.6% (95% CI; 19.6–25.9%). While (77.4%) of pregnant women refused to use the COVID-19 vaccine (Figure 1), The highest number (40.3%) of COVID-19 vaccine hesitance was because the respondents believed that the COVID-19 vaccine would harm their fetus, followed by fear of side effects and risks (31.9%) (Figure 2).
Figure 1.
COVID-19 vaccine acceptance among pregnant women in northeast Ethiopia, 2022.
Figure 2.
Reason for COVID-19 vaccine hesitance among pregnant women Northeast Ethiopia, 2022.
Determinants of COVID-19 Vaccine Acceptance Among Pregnant Women
Bivariate and multivariate logistic regression analyses were done to identify factors associated with the COVID-19 vaccine acceptance among pregnant women. The bivariate analysis reveals that urban residence, woman’s educational level, husbands educational level, gravidity, history of chronic medical illness, attitude towards COVID-19 and practicing COVID-19 preventive measures were found to have association with COVID-19 vaccine acceptance. After controlling for potential confounds in multiple logistic regression analyses, the husband’s educational level, women’s medical illness, attitude towards the COVID-19 infection, and practicing COVID-19 prevention measures were found to be determinants for COVID-19 vaccine acceptance.
As a result, women whose husband’s educational level was a diploma or above were 1.99 times more likely to accept the COVID-19 vaccine compared to their counterparts (AOR = 1.99, 95% CI: 1.09, 3.64). Pregnant women who had a history of medical illness were 2.41 times more likely to accept the COVID-19 vaccine compared to their counterparts (AOR = 2.41, 95% CI: 1.28, 4.54). Similarly, pregnant women who had a positive attitude towards the COVID-19 pandemic were 1.59 times more likely to accept the COVID vaccine as compared to those women who had negative attitudes (AOR = 1.59, 95% CI: 1.09, 2.31). Pregnant women who practiced COVID-19 prevention methods well were 1.94 times more likely to accept the COVID-19 vaccine than those who practiced COVID-19 prevention methods poorly (AOR = 1.94, 95% CI: 1.31, 2.85) (Table 6).
Table 6.
Determinants of COVID-19 Vaccine Acceptance Among Pregnant Women in Northeast Ethiopia, Multivariate Logistic Regression Model, 2022
| Variables | COVID-19 Vaccine Acceptance | COR(95% CI) | AOR(95% CI) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Residence | ||||
| Urban | 112(25.4) | 329 (74.6) | 1.55(1.06, 2.27)* | 0.88(0.51, 1.49) |
| Rural | 47(18.0) | 214(82.0) | 1 | 1 |
| Maternal educational level | ||||
| No formal education | 22(14.1) | 134(85.9) | 1 | 1 |
| Primary school | 35(21.6) | 127(78.4) | 1.68(0.93, 3.02) | 1.77(0.97, 3.24) |
| Secondary and above | 102(26.6) | 282(73.4) | 2.2(1.33, 3.65)* | 1.53(0.84, 2.82) |
| Husbands educational level | ||||
| No formal education | 25(17.6) | 117(82.4) | 1 | 1 |
| Primary school | 37(18.0) | 168(82.0) | 1.03(0.59, 1.80) | 1.08(0.59, 1.96) |
| Secondary school | 38(22.6) | 130(77.4) | 1.37(0.78, 2.40) | 1.18(0.64, 2.18) |
| Diploma and above | 59(31.6) | 128(68.4) | 2.16(1.27, 3.67)* | 1.99(1.09, 3.64)* |
| Gravidity | ||||
| Primigravida | 36(18.5) | 159(81.5) | 1 | 1 |
| Multigravida | 123(24.3) | 384(75.7) | 1.42 (1.12, 2.14)* | 1.44(0.92, 2.27) |
| Chronic medical illness | ||||
| Yes | 20(39.2) | 31(60.8) | 2.38(1.31, 4.29)* | 2.41(1.28, 4.54)* |
| No | 139(21.4) | 512(78.6) | 1 | 1 |
| Attitude | ||||
| Positive attitude | 80 (28.0) | 206(72.0) | 1.66(1.16, 2.36)* | 1.59(1.09, 2.31)* |
| Negative attitude | 79(19.0) | 337(81.0) | 1 | 1 |
| Practice | ||||
| Good practice | 78(28.0) | 201(72.0) | 1.64(1.15, 2.34)* | 1.94(1.31, 2.85)** |
| Poor practice | 81(19.1) | 342(80.9) | 1 | 1 |
Note: **p-value<001, *p-value<0.05, 1=reference.
Abbreviations: COR, Crud odds ratio; AOR, Adjusted odds ratio.
Qualitative
Socio-Demographic and Obstetric Characteristics of the Respondents
Eighteen participants were included for an in-depth interview on the reasons for not accepting the COVID-19 vaccine. About fifty-six percent of the respondents were in the age group of 20–34 years old. A majority (77.8%) of the study subjects were Muslim, and 72.2% of the respondents lived in urban areas. All of the participants were married. Half of the study participants (50%) attained secondary and above educational levels, followed by elementary school. Regarding their occupational status, 44.4% were government employees, followed by merchants (27.8%). About seventy-two percent of the study subjects were multigravida and nearly half (46.2%) of them were multiparous. About a quarter (33.3%) and (27.8%) of the respondents were coming for their second and third visit at the time of the interview.
Reason for Not Accepting the COVID-19 Vaccine
Pregnant women who come for antenatal care visits were selected for the in-depth interview purposively. Those respondents who answered “no: to the question “are you willing to take the COVID-19 vaccine if it is available?” were included in an in-depth interview on the reason for COVID-19 vaccine hesitance. Study participants are concerned that the COVID-19 vaccine may harm their fetus. They said,
I am scared that the vaccine will pass to my baby and my baby will die. My baby couldn’t resist the side effects. (Participant # 1, 3, 7, 11, 15 and 16).
Some of the participants believe that the risk of getting COVID is low and they believe that Allah will keep them from any risks. They said,
I believe my risk of getting COVID is low because none of my relatives have been infected with COVID up to this point. I am a firm believer in Allah. Allah will protect my family and me from infection. (Participant # 4, 9, and 17)
some said,
I am not afraid because I expected this to happen; we brought this on ourselves and we are paying for our sins. We must pray, believe in, and obey our Creator. (Participant # 6, 12, and 14).
Others have insufficient information on the benefits and safety of the COVID-19 vaccine for pregnant women. They said,
I don’t have sufficient information about the vaccine and whether it is safe for me and my baby. During my antenatal care visit, my health care professional says nothing about the vaccine. (Participant # 2, 5, and 8).
Some pregnant women are afraid of injections and do not believe in the vaccine. They said, “I’m afraid of the injection and don’t believe the vaccine. I feel the vaccine contained a chemical that could affect my reproductive ability”. (Participants # 10 and 18).
A 32 years participant also believes that the side effects of the COVID-19 vaccine will make them ill. She said,
I know that one of my neighbors stayed in bed for 2 weeks after she took the vaccine. I think the vaccine would make me ill if I took it as my neighbor. (Participant # 13)
Discussion
The viral disease COVID-19 has adverse effects on pregnant mothers and their unborn fetuses.30–33 In the event of a breakthrough infection, vaccination will reduce the severity of the illness and lower the likelihood of acquiring COVID-19.16,34–36 The safety of delivering the currently available SARS-CoV-2 vaccines before, during, and after pregnancy is supported by all available research.37,38 However, vaccine hesitancy becomes one of the greatest challenges globally.39–41
In this study, the overall COVID-19 vaccine acceptance among pregnant women was substantially low (22.6%) with a 95% confidence interval of 19.6% to 25.9%. This finding is in line with a recent finding in Debre Markos, Northwest Ethiopia (18.5%).42 However, the acceptance rate in our study was lower than studies conducted in southwest Ethiopia (70.7%),23 Northwest Ethiopia (40.08%),29 Northern Nigeria (33.8%),43 Singapore(30.5%),44 Thailand (60.8%),25 Saudi Arabia (68%)45 and China (77.4%)46 and Czechia (76.6%)47 and low-and middle-income countries (80.3%).28 The possible explanations for these differences are differences in sample size, study setting, and study population differences.
The current study shows that pregnant women whose husband’s educational level was a diploma or above were 1.99 times more likely to accept the COVID-19 vaccine compared to their counterparts. The possible explanation might be that those husbands who had attain higher educational level could read the news and follow social media related to the COVID-19 virus’s impact on the general population and its fatality and will share the information to their wives. However, this finding contradicts the previous study conducted in northwest Ethiopia.29 The difference may be due to the difference in sample size, in which the sample size of the current study was nearly double that of the study conducted in northwest Ethiopia.
Pregnant women who have chronic medical illnesses were 2.41 times more likely to accept the COVID-19 vaccine as compared with healthy participants. This is supported by the studies done in Ethiopia.23,42 The most important justification Perhaps people with chronic medical illnesses are more afraid of the COVID-19 pandemic because they know more about COVID-19ʹs behavior, which has a greater impact on patients with chronic health problems. Women’s attitude toward the COVID-19 infection was assessed and the finding reveals that 40.7% of respondents had a positive attitude towards the COVID-19 pandemic, which was lower than studies conducted in southwest Ethiopia (66.7%).23 The finding also shows that pregnant women who had a positive attitude toward the COVID-19 were 1.59 times more likely to accept the COVID vaccine as compared to those women who had a poor attitude. The finding was in line with a previous study conducted in northwest Ethiopia in which women who had a favorable attitude towards the COVID-19 pandemic were 8.54 times more likely to accept the vaccine.29 However, this finding was contrary to a previous study conducted in southwest Ethiopia.23 The difference may be due to the difference in sample size.
Similarly, the findings of this study reveal that 39.7% of pregnant women had good practice toward COVID-19 preventive measures, which was lower than studies conducted in southwest Ethiopia (61.4%) and Wollega Zones, Ethiopia (43.6%). Pregnant women who had good practice of COVID-19 prevention methods were 1.94 times more likely to accept the COVID-19 vaccine compared to those women who practiced the preventive measure of COVID-19 poorly. The current study’s findings were consistent with a study conducted in southwest Ethiopia.23 This study had the drawback of not proving the cause-and-effect link because of its cross-sectional design.
Conclusion
The COVID-19 vaccination was found to have low acceptance among pregnant women in this investigation. Acceptance of the COVID-19 vaccine, assuming it becomes available, was connected with the husband’s higher educational level, chronic medical illness, positive views regarding the COVID-19 pandemic and good practice of the COVID-19 infection prevention strategy. Health care providers and health extension workers in collaboration with the zonal and regional health bureaus should pay extensive attention to the dissemination of accurate vaccination information and address misinformation to boost vaccine acceptance among pregnant women.
Acknowledgments
The authors would like to express their gratitude to Wollo University for its ethical permission and the study participants for their time and cooperation as well as the data collectors and supervisors for their dedication during the data collection procedure.
Data Sharing Statement
On request, the corresponding author can provide the dataset for this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interests.
References
- 1.Temesgan WZ, Aklil MB, Yacob HS, et al. Adherence to COVID-19 preventive practice and associated factors among pregnant women in Gondar city, northwest Ethiopia, 2021: community-based cross-sectional study. PLoS One. 2022;17:1–14. doi: 10.1371/journal.pone.0264237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wondimu W, Girma B. Challenges and silver linings of COVID-19 in Ethiopia –short review. J Multidiscip Healthc. 2020;13:917–922. doi: 10.2147/JMDH.S269359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. WHO coronavirus (COVID-19) dashboard. WHO Website. WHO; 2020:18–19. [Google Scholar]
- 4.Health W Collaborating Center for Global Women’s. Prevalence of COVID-19 in pregnant and postnatal. 2021.
- 5.Mendez-dominguez N, Santos-zaldívar K, Gomez-carro S, Datta-banik S, Carrillo G. Maternal mortality during the COVID-19 pandemic in Mexico: a preliminary analysis during the first year. BMC Public Health. 2021;3:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. Maternal death due to COVID-19. Am J Obstet Gynecol. 2020;223(1):109.e1–109.e16. doi: 10.1016/j.ajog.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laibl V, Sheffield J. The management of respiratory infections during pregnancy. Immunol Allergy Clin North Am. 2006;26(1):155–172. doi: 10.1016/j.iac.2005.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu H, Wang LL, Zhao SJ, Kwak-Kim J, Mor G, Liao AH. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139:103122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Questions and Answers: COVID-19 Vaccines and Pregnancy. WHO; 2022:1–5. [Google Scholar]
- 10.Liu F, Liu H, Hou L, et al. Clinico-radiological features and outcomes in pregnant women with COVID-19 pneumonia compared with age-matched non-pregnant women. Infect Drug Resist. 2020;13:2845–2854. doi: 10.2147/IDR.S264541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lokken EM, Taylor GG, Huebner EM, et al.Higher severe acute respiratory syndrome coronavirus 2 infection rate in pregnant patients. Am J Obstetr Gynecol. 2020;2507:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samadi P, Alipour Z, Ghaedrahmati M, Ahangari R. The severity of COVID- - 19 among pregnant women and the risk of adverse maternal outcomes. J Gynecol Obstetr. 2021;1–8. DOI: 10.1002/ijgo.13700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adhikari EH, Spong CY. COVID-19 vaccination in pregnant and lactating women. JAMA. 2021;2019:2021–2022. doi: 10.1093/cid/ciw634 [DOI] [PubMed] [Google Scholar]
- 14.Moghadas SM, Vilches TN, Zhang K, et al. The impact of vaccination on COVID-19 outbreaks in the United States. Clin Infect Dis. 2021;73:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haghpanah F, Lin G, Levin SA, Klein E. EClinicalMedicine analysis of the potential impact of durability, timing, and transmission blocking of COVID-19 vaccine on morbidity and mortality. EClinicalMedicine. 2021;35:100863. doi: 10.1016/j.eclinm.2021.100863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists. COVID-19 vaccines and pregnancy: key recommendations and messaging for clinicians. 2022:1–2.
- 17.Schalkwyk VAN. SOGC statement on COVID-19 vaccination in pregnancy CONSENSUS STATEMENTS: SARS-CoV-2 and the impact on pregnancy COVID-19 vaccines approved for use in Canada mRNA vaccine platforms. 2022.
- 18.Dubik SD. Understanding the facilitators and barriers to COVID-19 vaccine uptake among teachers in the Sagnarigu Municipality of Northern Ghana: a cross-sectional study. Risk Management and Healthcare Policy. 2022;15:311–322. doi: 10.2147/RMHP.S352584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kashif M, Fatima I, Ahmed AM, et al. Perception, willingness, barriers, and hesitancy towards COVID-19 vaccine in Pakistan: comparison between healthcare workers and general population. Cureus. 2021;2019(10). doi: 10.7759/cureus.19106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Safo SA. Exploring barriers and facilitators to COVID-19 vaccine uptake among black and latinx communities. JAMA Netw Open. 2021;4(10):2021–2022. doi: 10.1056/NEJMp2103104 [DOI] [PubMed] [Google Scholar]
- 21.Altulahi N, Alnujaim S, Alabdulqader A, Alkharashi A, Almalki A, Alsiari F. Willingness, beliefs, and barriers regarding the COVID ‑ 19 vaccine in Saudi Arabia: a multiregional cross ‑ sectional study. BMC Fam Pract. 2021;22:1–11. doi: 10.1186/s12875-021-01606-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tadesse T, Mesfin F, Chane T. Prevalence and associated factors of non-exclusive breastfeeding of infants during the first six months in rural area of Sorro District, Southern Ethiopia: a cross-sectional study. Int Breastfeeding J. 2021. doi: 10.1186/s13006-016-0085-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mose A, Yeshaneh A. COVID-19 vaccine acceptance and its associated factors among pregnant women attending antenatal care clinic in Southwest Ethiopia: institutional-based cross-sectional study. Int J General Med. 2021;14:2385–2395. doi: 10.2147/IJGM.S314346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kasemy ZA, Bahbah WA, Zewain SK, et al. Knowledge, attitude and practice toward COVID-19 among Egyptians. J Epidemiol Glob Health. 2020;10:378–385. doi: 10.2991/jegh.k.200909.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pairat K, Phaloprakarn C. Acceptance of COVID ‑ 19 vaccination during pregnancy among Thai pregnant women and their spouses: a prospective survey. Reprod Health. 2022;1–11. doi: 10.1186/s12978-022-01383-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Besho M, Mulisa D, Yilma MT. Knowledge, attitude and practice toward corona virus infection among pregnant women attending antenatal care at public hospitals in Three Wollega Zones, Ethiopia. Int J General Med. 2021;14:3563–3573. doi: 10.2147/IJGM.S295490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arce JSS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27. doi: 10.1038/s41591-021-01454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bishaw E, Wasie Z, Alem H, Tesfa N. COVID-19 vaccine acceptance and associated factors among women attending antenatal and postnatal cares in Central Gondar Zone public hospitals, Northwest Ethiopia. 2020. [DOI] [PMC free article] [PubMed]
- 30.Jummaat F, Yahya EB, Adnan AS. Impact of COVID-19 on pregnancy and maternal health: an update. Biomed Res Ther. 2021;8(10):4655–4667. doi: 10.15419/bmrat.v8i10.701 [DOI] [Google Scholar]
- 31.Yang R, Mei H, Zheng T, et al. Pregnant women with COVID-19 and risk of adverse birth outcomes and maternal-fetal vertical transmission: a population-based cohort study in Wuhan, China. BMC Med. 2020;18(1):1–7. doi: 10.1186/s12916-020-01798-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID ‑ 19 pandemic on maternal and perinatal health: a scoping review. BioMed Central. 2021. doi: 10.1186/s12978-021-01070-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. Cmaj. 2021. Apr 19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amanatidou E, Gkiouliava A, Pella E, et al. Breakthrough infections after COVID-19 vaccination: insights, perspectives and challenges. Metab Open. 2022;14:100180. doi: 10.1016/j.metop.2022.100180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Coburn SB, Humes E, Lang R, et al. Analysis of postvaccination breakthrough COVID-19 infections among adults with HIV in the United States. JAMA Netw Open. 2022;5(6):e2215934. doi: 10.1001/jamanetworkopen.2022.15934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.State W. SARS-CoV-2 vaccine breakthrough surveillance and case information resource. 2021.
- 37.Donders GGG, Grinceviciene S, Haldre K, et al. Isidog consensus guidelines on covid-19 vaccination for women before, during and after pregnancy. J Clin Med. 2021;10(13):1–11. doi: 10.3390/jcm10132902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dick A, Rosenbloom JI, Gutman-Ido E, Lessans N, Cahen-Peretz A, Chill HH. Safety of SARS-CoV-2 vaccination during pregnancy- obstetric outcomes from a large cohort study. BMC Pregnancy Childbirth. 2022;22(1):1–7. doi: 10.1186/s12884-022-04505-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vogel J, Burni A. Why rebuilding trust in governments is key to end COVID-19. 2022.
- 40.Dhama K, Sharun K, Tiwari R, et al. COVID-19 vaccine hesitancy - reasons and solutions to achieve a successful global vaccination campaign to tackle the ongoing pandemic. Hum Vaccin Immunother. 2021;17(10):3495–3499. doi: 10.1080/21645515.2021.1926183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Male V. SARS-CoV-2 infection and COVID-19 vaccination in pregnancy. Nat Rev Immunol. 2022;22(5):277–282. doi: 10.1038/s41577-022-00703-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aynalem BY, Melesse MF, Bewket L. COVID-19 vaccine acceptability and determinants among pregnant mothers attending antenatal care services at Debre Markos town public health institutions, Debre Markos Northwest Ethiopia: mixed study Bewket. Pan African Med J. 2022;41:293. doi: 10.11604/pamj.2022.41.293.32618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iliyasu Z, Perkins JM, Tsiga-Ahmed FI. COVID-19 vaccine acceptability among pregnant women in Northern Nigeria. J Obstetr Gynaecol Canada. 2022;44(4):349–350.e1. doi: 10.1016/j.jogc.2022.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koon KL, Wai KC, Chan JKY, Mathur M, Chien M. Perceptions and acceptance of COVID-19 vaccine among pregnant and lactating women in Singapore: a cross-sectional study. 2021:19. [DOI] [PMC free article] [PubMed]
- 45.Alshahrani AA, Othman SS, Alhiniah MH, Alelyani RH, Badawi AM, Alshahrani AA. Acceptance of COVID-19 vaccine and associated factors among pregnant women in Saudi Arabia. Patient Preference and Adherence. 2022;16:861–873. doi: 10.2147/PPA.S357653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tao L, Wang R, Han N, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi- center cross-sectional study based on health belief model. Hum Vaccin Immunother. 2021;17(8):2378–2388. doi: 10.1080/21645515.2021.1892432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riad A, Jouzov A, Üstün B, et al. COVID-19 vaccine acceptance of Pregnant and Lactating Women (PLW) in Czechia: an analytical cross-sectional study. Int J Environ Res Public Health. 2021;18:13373. doi: 10.3390/ijerph182413373 [DOI] [PMC free article] [PubMed] [Google Scholar]