Abstract
Objective:
The menstrual cycle may influence vulvodynia through hormonal pathways or vulvar irritation due to menstruation or menstrual hygiene. We assessed menstrual cycle characteristics in those with and without clinically confirmed vulvodynia.
Materials and Methods:
Participants were recruited from the administrative database of a health care network serving ∼27% of Minneapolis–Saint Paul residents. For 220 clinically confirmed cases and 224 controls, menstrual cycle characteristics were retrospectively assessed at three time points: before age 18, the year before onset of vulvar pain, and 3 months before study participation. Logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between menstrual characteristics at all three time points and vulvodynia. Models adjusted for prespecified confounders were evaluated against crude effect estimates.
Results:
Women with heavier menstrual flows had higher odds of vulvodynia compared with women with lighter menstrual flows during their adolescent years (OR 1.62, 95% CI 0.91–2.86), the year before onset of vulvar pain (OR = 2.11, 95% CI 1.10–4.02), and during the 3 months before study participation (OR = 1.67, 95% CI 0.91–3.06). Women with more severe cramps also had higher odds of vulvodynia compared with women with no or mild cramps during their adolescent years (OR = 2.45, 95% CI 1.45–4.15), the year before onset of vulvar pain (OR = 3.30, 95% CI 1.67–6.51), and during the 3 months before study participation (OR = 4.96, 95% CI 1.99–12.36). Women with specific premenstrual symptoms also reported higher odds of vulvodynia. Among those with vulvodynia, half reported a change in vulvar pain across the menstrual cycle, with 60% of these reporting greater pain just before and during menstruation. Furthermore, we observe a trend of decreased tampon use and increased use of sanitary pads as women with vulvodynia moved closer to their date of diagnosis.
Conclusions:
Menstrual cycle characteristics were associated with vulvodynia, and associations were consistent across different phases of the reproductive life cycle.
Keywords: case–control study, menstruation, premenstrual syndrome, vulvodynia
Introduction
Vulvodynia is defined as idiopathic vulvar pain lasting at least 3 months, with an estimated prevalence of 8% among women during their reproductive years.1,2 It is characterized by debilitating burning, knife-like pain, or pain on contact, and generally is not explained by vulvovaginal infections, dermatoses, neurological, or other identifiable disorders.
Research has suggested that women who develop symptoms consistent with vulvodynia may begin to experience discomfort as early as menarche.3 In a study of women with primary and secondary vulvodynia, Brotto et al.4 reported that ∼80% experienced pain with their menstrual cycles. This is substantially greater than that observed by Harlow et al. in a population-based study of healthy women aged 36–44 years where 36% reported moderate-to-severe pain with periods.5 It is unknown whether characteristics of the menstrual cycle at any point in a woman's life are associated with subsequent vulvodynia onset.
It has been previously hypothesized that vulvodynia may be the consequence of an altered immunoinflammatory mechanism.6,7 Menstruation is now speculated to be a complex inflammatory process composed of uterine immune cell populations in addition to an endocrine process.8 In fact, it has been proposed that menstruating tissue, especially hormonally responsive extrauterine endometrial lesions, may serve as a trigger for inflammatory pain in such conditions as endometriosis through activation of innate immune cells and peripheral nerve endings.9 Additionally, previous research has hypothesized that certain menstrual products may induce greater pain among those with vulvodynia.20
The current study uses data from a community-based case–control study to examine the associations between a variety of menstrual characteristics, including menstrual regularity, flow, and use of menstrual products, and clinically confirmed vulvodynia. We were able to assess menstrual characteristics at three distinct time points: the onset of menarche, the year before onset of vulvar pain, and at the current time of data collection.
Materials and Methods
Study population
The University of Minnesota and Boston University Institutional Review Boards approved this study, and all participants provided written consent. We used an administrative database of a large health care network that serves ∼27% of the Minneapolis–Saint Paul metropolitan area, to identify women aged 18–40 years who had been seen for any reason in 1 of more than 40 community health clinics between March 2010 and October 2013.
These women were asked to complete by mail a self-reported screener survey designed to identify those who might meet the diagnostic criteria for vulvodynia by assessing the characteristics of pain with tampon insertion, generalized burning, or excessive pain on contact. Details of these screening methods have been described elsewhere.1 In brief, based on women's responses regarding their self-reported history of vulvar pain, those likely to meet the diagnostic criteria set by the International Society for the Study of Vulvovaginal Disease were invited to participate in this study to determine whether they met the clinical criteria for a vulvodynia diagnosis.10
Of the 30,676 screener surveys received (45.9% of those queried), 1,398 women were invited for a clinical examination. Of these women, 350 completed the examination and 234 were clinically confirmed as cases of vulvodynia (see Supplementary Fig. S1 for recruitment details). We compared screener questionnaire characteristics of women who agreed and did not agree to a clinical evaluation and found no substantial differences in demographic characteristics or reproductive histories. Self-reported characteristics of vulvar pain were similar between those who agreed and those who did not agree to a clinical examination.11
Women who completed screener questionnaires and reported no history of vulvar pain were randomly selected and invited to serve as controls. Of the 2,287 women invited, 251 agreed and 234 were clinically confirmed as having no past or current vulvar pain. Each control was matched to a case and assigned a reference age identical to the age of first self-reported vulvar pain onset by the matched case. Controls were required to be older than the age of vulvar pain onset for their matched case.
Measures
All participants completed background, psychosocial, psychiatric, and medical history questionnaires by telephone with trained study staff as part of an extended baseline assessment that occurred within a 2-month period. We examined menstrual cycle characteristics in three time periods: (1) early reproductive years, defined as the age of menarche to 18 years of age or age of onset of vulvar pain for cases/reference age for controls if before 18 years of age, (2) the year before onset of vulvar pain for cases and the year before assigned reference age for controls, and (3) in the 3 months before the survey. Menstrual cycle characteristics included cycle length and heaviness of flow, use of menstrual products, typical amount of menstrual pain, and details about tampon use, if applicable.
In addition, for each time period, we asked whether their menstrual cycles were predictable within 10 days. For cases only, we asked if women experienced changes (none, increase, or decrease) in vulvar pain at four different time points across the menstrual cycle: (1) right before their period; (2) during their period; (3) directly after their period; and (4) mid-cycle or at the time of ovulation. Finally, we asked participants to respond to 10 questions that comprise the Menstrual Distress Questionnaire12 about premenstrual symptoms in the year before onset of vulvar pain for cases and reference age for controls.
In selecting potential confounders, we restricted to only those variables that would have predated the onset of menses. This is because we are unsure of the potential etiologic pathway between menstrual characteristics and vulvodynia and thus do not want to adjust for anything that could be on the causal pathway. As a result, models were adjusted for history of childhood abuse (none, no incidents of abuse; moderate, one to four instances of physical or sexual abuse; severe, five or more instances of physical or sexual abuse) and age at menarche.
Additionally, for analyses of premenstrual syndrome symptoms, we further adjusted for a history of anxiety and depression, as premenstrual symptoms can be exacerbated in women who have depression or anxiety at times other than during the late luteal phase. Cases and controls were similar by actual age, and thus, no adjustment for age was necessary.
Statistical analysis
Descriptive statistics were calculated for baseline characteristics. Missing data were minimal, with no variable exceeding 3% missingness (Table 1 contains the number of missing values by covariate). Fully conditional specification was used in Proc MI in SAS to impute missing variables for menstrual characteristics and covariates. Proc MI created five complete data sets in which the values of any missing variables were imputed using a predictive model based on the values of nonmissing variables. The imputed values can differ across the data sets. This enables analysis of the full data set while also accounting for variability in the imputed values.
Table 1.
Baseline Demographics of Sample (N = 443)
| Characteristic | Cases (n = 220) | Controls (n = 223) |
|---|---|---|
| Current age (years), mean (SD) | 29.6 (5.3) | 32.7 (5.1) |
| Reference age (years), mean (SD) | 21.2 (5.5) | 21.4 (5.6) |
| Race, n (%) | ||
| White | 203 (92.3) | 207 (92.8) |
| Non-white | 17 (7.7) | 16 (7.2) |
| Age (years) of menarche, n (%) | ||
| ≤10 | 16 (7.3) | 20 (9.0) |
| 11 | 34 (15.5) | 25 (11.2) |
| 12 | 59 (26.8) | 69 (30.9) |
| 13 | 58 (26.4) | 48 (21.5) |
| 14 | 30 (13.6) | 41 (18.4) |
| ≥15 | 23 (10.4) | 20 (9.0) |
| Age (years) of first vaginal intercourse (5 cases and 5 controls missing), n (%) | ||
| <16 | 44 (20.0) | 48 (21.5) |
| 16–17 | 53 (24.1) | 64 (28.7) |
| ≥18 | 118 (53.6) | 106 (47.5) |
| Lifetime vaginal intercourse partners (6 cases and 1 control missing), n (%) | ||
| ≤2 | 62 (28.2) | 65 (29.2) |
| 3–6 | 66 (30.0) | 56 (25.1) |
| 7–12 | 48 (21.8) | 56 (25.1) |
| >12 | 38 (17.3) | 45 (20.2) |
| History of physical or sexual abuse before age 11a (4 cases missing), n (%) | ||
| None | 88 (40.0) | 108 (48.4) |
| Moderate | 40 (18.2) | 54 (24.2) |
| Severe | 88 (40.0) | 61 (27.4) |
| History of anxiety (2 cases and 1 control missing), n (%) | ||
| Yes, diagnosed | 66 (30.0) | 31 (13.9) |
| Yes, not diagnosed | 27 (12.3) | 29 (13.9) |
| No | 125 (56.8) | 162 (72.7) |
| History of depression (2 controls missing), n (%) | ||
| Yes, diagnosed | 69 (31.4) | 52 (23.3) |
| Yes, not diagnosed | 15 (6.8) | 24 (10.8) |
| No | 136 (61.8) | 145 (65.0) |
| History of bacterial vaginosis, n (%) | ||
| Yes | 29 (13.2) | 17 (7.6) |
| No | 191 (86.8) | 206 (92.4) |
| Ever had a urinary tract infection, n (%) | ||
| Yes | 98 (44.6) | 66 (30.1) |
| No | 122 (55.5) | 153 (69.9) |
| History of chronic constipation (1 control missing), n (%) | ||
| Yes | 20 (9.1) | 5 (2.2) |
| No | 200 (90.9) | 217 (97.3) |
| Any allergies to medications (1 case and 1 control missing), n (%) | ||
| Yes | 78 (35.5) | 50 (22.4) |
| No | 141 (64.1) | 172 (77.1) |
| History of chronic pain or fatigue disordersb, n (%) | ||
| Yes | 62 (28.2) | 21 (9.4) |
| No | 158 (71.8) | 202 (90.6) |
| Hormonal contraceptive use before age 18, n (%) | ||
| Yes | 147 (66.8) | 128 (57.4) |
| No | 73 (33.2) | 95 (42.6) |
| Hormonal contraceptive use in the year before reference agec, n (%) | ||
| Yes | 155 (70.5) | 122 (54.7) |
| No | 65 (29.6) | 101 (45.3) |
| Hormonal contraceptive use at time of survey, n (%) | ||
| Yes | 107 (48.6) | 87 (39.0) |
| No | 113 (51.4) | 136 (61.0) |
| Endometriosis, n (%) | ||
| Yes | 27 (12.3) | 13 (5.8) |
| No | 193 (87.7) | 210 (94.2) |
| Polycystic ovarian syndrome, n (%) | ||
| Yes | 10 (4.6) | 14 (6.4) |
| No | 210 (95.5) | 205 (93.6) |
| Age (years) of first tampon use (10 cases and 3 controls missing), n (%) | ||
| ≤10 | 2 (0.9) | 1 (0.5) |
| 11 | 6 (2.7) | 10 (4.5) |
| 12–13 | 67 (30.5) | 59 (26.5) |
| 14 | 37 (16.8) | 47 (21.1) |
| ≥15 | 98 (44.6) | 103 (46.2) |
| Pain or difficulty with first tampon use (1 case and 1 control missing), n (%) | ||
| Never used tampons | 5 (2.3) | 2 (0.9) |
| No difficulty/difficulty, but no pain | 51 (23.2) | 137 (61.4) |
| Difficulty and some pain | 106 (48.2) | 73 (32.7) |
| Difficulty, with great pain | 57 (25.9) | 10 (4.5) |
| Ever stopped tampon use due to pain (1 case missing), n (%) | ||
| Yes | 98 (44.6) | 9 (4.0) |
| No | 121 (55.0) | 214 (96.0) |
Categorization of abuse: none, no incidents of abuse; moderate, one to four instances of physical or sexual abuse; severe, five or more instances of physical or sexual abuse.
Chronic pain or fatigue disorders included interstitial cystitis, fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and temporomandibular joint disorder.
Reference age was the year of onset of vulvar pain for cases with vulvodynia and the same age for matched controls.
SD, standard deviation.
The imputation model included all potential covariates, all menstrual variables, and case–control status. “Proc MI analyze” was used to combine coefficient and standard error estimates from the five data sets.
We used logistic regression models to calculate odds ratios (ORs) with 95% confidence intervals (CIs) estimating the association between menstrual characteristics and vulvodynia. Because menstrual characteristics were assessed over three distinct time periods, women who reported not menstruating during a given time period were excluded from the analyses for that specific time period. In addition, we carried out sensitivity analyses to determine whether menstrual cycle characteristics differed between women with localized provoked vulvodynia (pain confined to a specific location within the vestibule) versus generalized pain, and between women with primary onset of vulvar pain (never having had pain-free intercourse) versus those with secondary onset vulvodynia (onset occurred after having had a time period of pain-free intercourse).
Among cases who reported changes in vulvar pain over the course of the menstrual cycle, the percentage of women reporting a change in pain is presented during four time periods: mid-cycle, days before menstruation, during menstruation, and days after menstruation. All data were analyzed using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
Of the original 234 cases and 234 controls, 10 cases and 4 controls did not complete the medical history questionnaire. In addition, one case failed to complete a majority of key menstrual history questions. There were an additional three cases and seven controls excluded due to age of vulvar pain onset or reference age before age of menarche. Thus, the analysis was conducted among 220 cases and 223 controls.
One case reported an age of menarche after age 18 and was excluded from the analyses for that time period; 21 cases and 19 controls reported no menstruation in the year before reference age and were excluded from that analysis; 41 cases and 29 controls reported no menstruation for the 3 months before the survey and were excluded from that analysis. Reasons for amenorrhea included hormonal contraception, pregnancy or breastfeeding, hysterectomy, endometrial ablation, or polycystic ovarian syndrome (PCOS).
As shown in Table 1, the majority of the sample was white, and controls were on average about 3 years older than cases (mean age 32.7 vs. 29.6 years). There was no consistent trend in case–control differences by current age, age at menarche, age at first intercourse, or number of intercourse partners.
Compared with controls, women with vulvodynia were more likely to have experienced childhood abuse and a history of anxiety and depression. They also reported greater history of bacterial vaginosis, urinary tract infections, chronic constipation, chronic pain or fatigue disorders, and endometriosis. Hormonal contraceptive use was more prevalent among women with vulvodynia before onset of vulvar pain compared with a comparable time period among controls. We also observed that women with vulvodynia reported substantially greater difficulty and pain at the time of first tampon use and were much more likely to discontinue tampon use compared with controls.
Table 2 shows the ORs and 95% CIs for menstrual cycle characteristics across the three studied time periods (before age 18, the year before onset of vulvar pain in cases or reference age among controls, and 3 months before completion of the survey), after adjustment for age at menarche and history of childhood abuse. Cycle regularity did not differ between cases and controls. However, among those reporting regular menstrual cycles, cases had three times the odds of reporting shorter cycle lengths before age 18 compared with controls.
Table 2.
Adjusted Odds Ratios for Menstrual Cycle Characteristics and Vulvodynia
| Self-reported menstrual cycle characteristic | Time period |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Time between the first period and the year before reference age or 18 years old, whichever was youngera,b |
Year before reference agea,c |
3 Months before surveyd |
|||||||
| Cases (n = 219) (%) | Controls (n = 223) (%) | Adjustede OR (95% CI) | Cases (n = 199) (%) | Controls (n = 204) (%) | Adjustede OR (95% CI) | Cases (n = 179) (%) | Controls (n = 194) (%) | Adjustede OR (95% CI) | |
| Cycle regularity | |||||||||
| Irregular | 26.9 | 25.1 | 1.04 (0.67–1.60) | 18.6 | 15.2 | 1.13 (0.64–1.98) | 21.2 | 17.0 | 1.14 (0.66–1.98) |
| Regular (cycle within 10 days) | 73.1 | 74.9 | 1.0 | 81.4 | 84.8 | 1.0 | 78.8 | 83.0 | 1.0 |
| Cycle lengthf | |||||||||
| <25 days | 14.4 | 6.0 | 2.96 (1.33–6.58) | 11.9 | 5.2 | 2.08 (0.86–5.00) | 7.1 | 8.1 | 0.99 (0.39–2.50) |
| 26–29 days | 67.5 | 76.1 | 1.0 | 74.4 | 77.3 | 1.0 | 68.1 | 71.4 | 1.0 |
| ≥30 days | 18.1 | 18.0 | 1.18 (0.65–2.13) | 13.8 | 17.4 | 0.76 (0.40–1.46) | 24.8 | 20.5 | 1.33 (0.75–2.37) |
| Days of menstrual flow | |||||||||
| <5 | 14.6 | 29.6 | 0.44 (0.27–0.74) | 20.6 | 31.4 | 0.58 (0.34–0.97) | 37.4 | 39.7 | 1.04 (0.65–1.68) |
| 5–6 | 50.7 | 45.3 | 1.0 | 51.3 | 48.5 | 1.0 | 41.9 | 45.4 | 1.0 |
| >6 | 34.7 | 25.1 | 1.20 (0.77–1.89) | 28.1 | 20.1 | 1.18 (0.70–2.00) | 20.7 | 15.0 | 1.55 (0.84–2.84) |
| Total amount of menstrual flowg | |||||||||
| Light | 13.7 | 17.9 | 1.0 | 13.6 | 18.7 | 1.0 | 26.8 | 31.4 | 1.0 |
| Moderate | 42.9 | 48.4 | 1.06 (0.61–1.86) | 47.7 | 53.2 | 1.21 (0.66–2.24) | 45.8 | 46.4 | 1.10 (0.66–1.83) |
| Heavy | 43.4 | 33.6 | 1.62 (0.91–2.86) | 38.7 | 28.1 | 2.11 (1.10–4.02) | 27.4 | 22.2 | 1.67 (0.91–3.06) |
| Days/amount of menstrual flowg | |||||||||
| <5 days and light flow | 6.9 | 11.2 | 1.0 | 8.0 | 10.3 | 1.0 | 17.9 | 21.1 | 1.0 |
| Any other day or flow | 69.0 | 72.7 | 1.37 (0.69–2.74) | 70.9 | 77.9 | 1.23 (0.58–2.58) | 66.5 | 71.7 | 1.03 (0.59–1.80) |
| >6 days and heavy flow | 24.2 | 16.1 | 2.15 (0.98–4.73) | 21.1 | 12.8 | 2.13 (0.88–5.15) | 15.6 | 7.2 | 2.35 (1.01–5.46) |
| Pain with menstrual periodsh | |||||||||
| No cramps/mild cramps | 42.5 | 53.8 | 1.0 | 48.7 | 60.6 | 1.0 | 58.1 | 78.9 | 1.0 |
| Moderate cramps | 29.7 | 33.6 | 1.12 (0.72–1.73) | 29.7 | 31.0 | 1.29 (0.79–2.10) | 28.5 | 17.5 | 2.34 (1.37–4.01) |
| Severe cramps | 27.9 | 13.5 | 2.45 (1.45–4.15) | 21.6 | 8.4 | 3.30 (1.67–6.51) | 13.4 | 3.6 | 4.96 (1.99–12.36) |
Reference age was the year of onset of vulvar pain for cases with vulvodynia and the same age for matched controls.
Excludes 1 case who was not menstruating during this time period.
Excludes 21 cases and 19 controls who were no longer menstruating during this time period.
Excludes 41 cases and 29 controls who were no longer menstruating during this time period.
Model was adjusted for age at menarche (continuous) and history of physical or sexual abuse before age 11 (no incidents of abuse, one to four instances of physical or sexual abuse, and five or more instances of physical or sexual abuse).
Only assessed among women who reported regular menstrual cycles.
Menstrual flow amount quantified as: light (10 or fewer pads or tampons used during duration of period), moderate (11–20 pads or tampons used during duration of period), and heavy (21 or more pads or tampons used during duration of period).
Menstrual cramps severity described as: mild (medication seldom needed), moderate (medication usually needed), and severe (medication and bed rest needed).
CI, confidence interval; OR, odds ratio.
This association waned when assessed the year before onset of vulvar pain in cases and reference age in controls and became null at the time of survey completion. There was also a trend toward more days and heavier menstrual flow among cases compared with controls at each of the three time periods. Compared with controls, women with vulvodynia had two to three times the odds of severe cramps with their menstrual periods before age 18 (95% CI 1.45–4.15) and approximately three times the odds of severe cramping 1 year before vulvar pain onset (95% CI 1.67–6.51) compared with a comparable time period among controls.
In a cases-only sensitivity analysis, we compared women with localized provoked vulvodynia (n = 108) with women with generalized vulvodynia (n = 91) and saw no major differences with respect to shorter cycle lengths (OR = 0.59, 95% CI 0.22–1.61), longer days and heavier flow (OR = 0.55, 95% CI 0.17–1.82), or severe pain with periods (OR = 0.90, 95% CI 0.42–1.93) the year before vulvar pain onset. When we compared women with primary onset (n = 92) versus secondary onset (n = 107) of vulvodynia, we saw no differences by longer days and heavier flow (OR = 1.10, 95% CI 0.33–3.62).
However, there was some suggestion that the overall association between shorter cycle length and vulvodynia the year before vulvar pain onset may be driven more so by women with secondary as opposed to primary onset of vulvodynia (OR = 2.19, 95% CI 0.75–6.36) and that the association between severe pain with periods and vulvodynia the year before vulvar pain onset may be driven more so by women with secondary versus primary onset of vulvodynia as well (OR = 1.68, 95% CI 0.79–3.60). However, in this case-only sensitivity analysis, our sample size was small, and the CIs around these estimates were quite wide.
We also assessed menstrual hygiene practices (Table 3) and found that women with vulvodynia had 1.26 times the odds of never using a tampon before age 18 compared with controls (95% CI 0.78–2.02), and this association strengthened as women moved closer to their reported age at first onset of vulvar pain compared with comparable times periods among controls. Furthermore, among women who chose to use tampons before age 18, those with vulvodynia had 7.18 times the odds of reporting moderate-to-severe discomfort with tampon insertion (95% CI 3.66–14.06) compared with controls, and when assessed 1 year before onset of vulvar pain and comparable time period among controls, those with vulvodynia had 20 times the odds of reporting moderate-to-severe discomfort while inserting a tampon (95% CI 7.1–55.3). This is also reflected in the greater use of pads and panty liners for menstrual protection among women with vulvodynia compared with controls across all the time periods.
Table 3.
Adjusted Odds Ratios for Menstrual Protection Characteristics and Vulvodynia
| Self-reported menstrual protection characteristic | Time period |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Time between the first period and the year before reference age or 18 years old, whichever was youngera,b |
Year before reference agea,c |
3 Months before surveyd |
|||||||
| Cases (n = 219) (%) | Controls (n = 223) (%) | Adjustede OR (95% CI) | Cases (n = 199) (%) | Controls (n = 204) (%) | Adjustede OR (95% CI) | Cases (n = 179) (%) | Controls (n = 194) (%) | Adjustede OR (95% CI) | |
| How often use only tampons | |||||||||
| Never | 41.1 | 37.2 | 1.26 (0.78–2.02) | 36.7 | 27.1 | 2.28 (1.37–3.80) | 38.0 | 25.8 | 2.66 (1.57–4.51) |
| Rarely/sometimes | 33.3 | 33.6 | 1.11 (0.68–1.82) | 24.1 | 25.1 | 1.17 (0.68–1.99) | 24.0 | 26.3 | 1.23 (0.71–2.13) |
| Usually/always | 25.6 | 29.2 | 1.0 | 39.2 | 47.8 | 1.0 | 38.0 | 47.9 | 1.0 |
| How often use tampons with panty liner or pad | |||||||||
| Never | 44.3 | 44.0 | 1.0 | 41.7 | 36.0 | 1.0 | 44.7 | 42.8 | 1.0 |
| Rarely/sometimes | 32.9 | 35.4 | 0.92 (0.60–1.42) | 33.7 | 37.9 | 0.69 (0.43–1.14) | 28.5 | 34.0 | 0.81 (0.49–1.35) |
| Usually/always | 22.8 | 20.6 | 1.04 (0.64–1.73) | 24.6 | 26.1 | 0.78 (0.46–1.34) | 26.8 | 23.2 | 1.15 (0.67–1.97) |
| How often use only maxi pads | |||||||||
| Never | 16.9 | 18.8 | 1.0 | 35.2 | 35.5 | 1.0 | 41.3 | 45.4 | 1.0 |
| Rarely/sometimes | 37.4 | 42.6 | 1.01 (0.59–1.74) | 34.2 | 43.4 | 0.90 (0.55–1.48) | 36.3 | 37.1 | 1.16 (0.71–1.88) |
| Usually/always | 45.7 | 38.6 | 1.33 (0.78–2.30) | 30.7 | 21.2 | 2.09 (1.18–3.67) | 22.4 | 17.5 | 1.80 (0.99–3.26) |
| Menstrual protection usually used | |||||||||
| Tampons only | 20.6 | 25.6 | 1.0 | 34.7 | 49.4 | 1.0 | 33.0 | 44.3 | 1.0 |
| Pads only | 43.4 | 33.2 | 1.72 (1.03–2.87) | 27.1 | 16.3 | 2.76 (1.52–5.01) | 21.2 | 10.8 | 3.91 (1.98–7.73) |
| Combination | 36.1 | 41.3 | 1.14 (0.69–1.89) | 38.2 | 44.3 | 1.12 (0.69–1.81) | 45.8 | 44.9 | 1.48 (0.91–2.39) |
| Use of panty liners on average per month | |||||||||
| Never | 34.7 | 39.9 | 1.0 | 33.2 | 38.7 | 1.0 | 30.7 | 38.1 | 1.0 |
| 1–6 days | 48.0 | 48.4 | 1.16 (0.77–1.76) | 47.7 | 49.0 | 1.26 (0.79–2.00) | 45.8 | 47.4 | 1.27 (0.78–2.08) |
| 7–12 days | 11.9 | 8.1 | 1.88 (0.94–3.78) | 12.1 | 8.8 | 1.88 (0.90–3.94) | 11.7 | 7.7 | 2.81 (1.25–6.32) |
| 13+ days | 5.5 | 3.6 | 1.59 (0.61–4.15) | 7.0 | 3.4 | 2.53 (0.90–7.09) | 11.7 | 6.7 | 2.57 (1.13–5.87) |
| Discomfort while inserting tampon | |||||||||
| No tampon use | 24.2 | 20.6 | 2.76 (1.55–4.92) | 17.6 | 11.8 | 5.57 (2.83–10.97) | |||
| No discomfort | 15.5 | 35.0 | 1.0 | 26.6 | 68.1 | 1.0 | |||
| Mild discomfort | 33.8 | 36.3 | 2.22 (1.32–3.74) | 36.7 | 17.7 | 5.94 (3.40–10.39) | |||
| Moderate/severe discomfort | 26.5 | 8.1 | 7.18 (3.66–14.06) | 19.1 | 2.5 | 19.84 (7.11–55.31) | |||
| Discomfort while using tampon | |||||||||
| No tampon use | 25.1 | 21.1 | 2.23 (1.36–3.67) | 17.6 | 11.3 | 4.05 (2.12–7.75) | |||
| No discomfort | 30.1 | 56.1 | 1.0 | 42.9 | 78.8 | 1.0 | |||
| Mild discomfort | 27.9 | 19.3 | 2.66 (1.61–4.37) | 26.2 | 8.4 | 6.64 (3.37–13.07) | |||
| Moderate/severe discomfort | 16.9 | 3.6 | 7.93 (3.46–18.14) | 13.1 | 1.5 | 17.65 (4.99–62.49) | |||
| Discomfort removing tampon | |||||||||
| No tampon use | 25.1 | 21.6 | 2.54 (1.52–4.23) | 17.6 | 12.3 | 5.11 (2.64–9.88) | |||
| No discomfort | 24.2 | 53.2 | 1.0 | 28.1 | 73.5 | 1.0 | |||
| Mild discomfort | 32.0 | 22.1 | 3.07 (1.87–5.04) | 34.7 | 13.2 | 6.03 (3.40–10,70) | |||
| Moderate/severe discomfort | 18.7 | 3.2 | 11.78 (4.94–28.12) | 19.6 | 1.0 | 51.65 (11.72–227.52) | |||
Reference age was the year of onset of vulvar pain for cases with vulvodynia and the same age for matched controls.
Excludes 1 case who was not menstruating during this time period.
Excludes 21 cases and 19 controls who were no longer menstruating during this time period.
Excludes 41 cases and 29 controls who were no longer menstruating during this time period.
Model was adjusted for age at menarche (continuous) and history of physical or sexual abuse before age 11 (no incidents of abuse, one to four instances of physical or sexual abuse, and five or more instances of physical or sexual abuse).
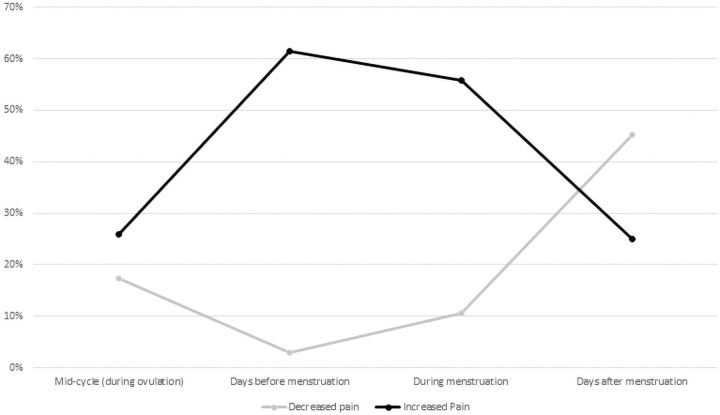
Figure 1 shows the cross-sectional proportion of cases who reported changes in their vulvar pain at various time periods during the menstrual cycle (mid-cycle, days before menstruation, during menstruation, and days after menstruation). Of our 220 cases, 104 (47%) reported a change in their vulvar pain at one or more times during the menstrual cycle. The remaining cases reported no change at any time and were thus excluded from this figure. Among those who reported an increase in pain, the greatest proportion of women reported that it occurred just before menstruation (∼62%) and during menstruation (∼58%), whereas less than 30% reported an increase in pain after menstruation or during the mid-cycle time period. In contrast, among those who reported a decrease in pain, the greatest proportion indicated that it occurred after menstruation had ceased (∼48%), whereas less than 20% of women reported a decrease in their vulvar pain at other times.
FIG. 1.
Proportion of cases with pain changes at each of the four menstrual cycle time periods. We excluded 108 cases who reported no change in their vulvar pain at any point during their menstrual cycles, and 8 cases who reported they did not know if their pain changed at any point during their menstrual cycle.
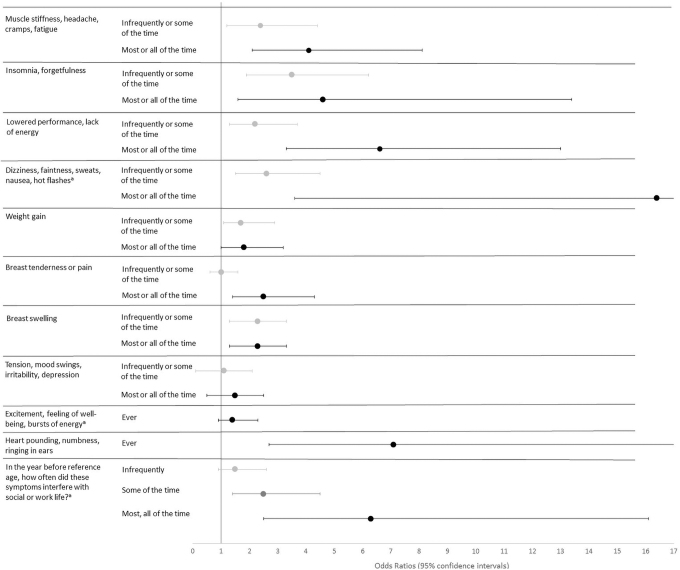
Figure 2 shows the OR of self-reported frequency of premenstrual symptoms reported during the year before onset of vulvar pain in cases and a comparable time period among controls. The reference group are those not endorsing a particular symptom. For all premenstrual symptoms, women with vulvodynia reported experiencing them most or all the time more often than controls. Additionally, women with vulvodynia reported 2.7 times the odds, compared with controls, that these symptoms interfered with their social and work life most or all the time. The actual risk estimates from this figure are shown in Supplementary Table S1.
FIG. 2.
Adjusted odds ratios and 95% CIs for the association of premenstrual symptoms reported in the year before onset of vulvar pain in cases and comparable time periods among controls. The reference category for all models was “Not at all.” All models were adjusted for age at menarche (continuous), history of physical or sexual abuse before age 11 (no incidents of abuse, one to four instances of physical or sexual abuse, and five or more instances of physical or sexual abuse), history of depression, and history of anxiety. a95% CIs extend beyond the bounds of the figure. The upper CI for “dizziness, faintness, sweats, nausea, hot flashes” is 74.7. The upper CI for “heart pounding, numbness, ringing in ears” is 18.6. CI, confidence interval.
Discussion
We observed associations between a variety of menstrual cycle characteristics and vulvodynia. Women with vulvodynia were more likely to report shorter cycle lengths during their early menstrual years and the year before their reference age compared with controls. In addition, women with vulvodynia reported heavier menstrual flows lasting longer than 6 days compared with controls who reported lighter and/or shorter menstrual flows, and this was consistent across the three time periods evaluated. Not surprisingly, we also showed that the use of tampons were significantly less prevalent among cases, and the use of pads for menstrual protection was more common among cases, suggesting that women with vulvodynia avoid using menstrual protection products and methods that can further exacerbate their pain.
Finally, women with vulvodynia more often reported severe menstrual cramps compared with controls who were more likely to report none, mild, or moderate cramps. This association was present during all three time periods evaluated but strengthened as women aged. Among cases who reported pain changes across the menstrual cycle, increased pain in the days before and during menstruation was most common.
Previous research into menstrual cycle characteristics in relation to vulvodynia is limited. One study used telephone screening to identify 100 women with symptoms of vulvodynia and 325 asymmetric controls.2 This study was not able to clinically confirm the vulvodynia status of cases, and they did not specify a time period for menstrual characteristics. The authors reported that women with vulvodynia compared with controls had higher odds of a history of irregular menstruation. Additionally, women with vulvodynia compared with controls had higher odds of a history of painful periods and premenstrual syndrome. Despite methodological differences between these two studies, our results are generally consistent with their findings. However, we did not find a strong association between irregular cycle length and vulvodynia. This may be due to differences in the classification of irregular periods between the studies.
Bachmann et al.13 assessed predictors of chronic vulvar pain in a sample of ambulatory patients responding to a questionnaire and reported no association between menopausal status and vulvar pain. The authors went on to conclude that the etiology of vulvar pain is not related to menstruation. Our findings do not support their conclusion regarding menstruation, and since our sample was restricted to women younger than 40 years, we cannot comment on the potential role of menopause in vulvar pain.
There are multiple potential pathways through which menstrual cycle characteristics may influence the onset of vulvodynia. Research suggests that vulvar tissue is sensitive to hormones,14 and some research has suggested a link between use of hormonal contraceptives and vulvodynia,15–17 although other studies have not.18 Menstrual characteristics may be reflective of underlying reproductive hormone levels and/or changes in endogenous hormone levels over the course of the cycle.19 Our findings may suggest that endogenous levels of reproductive hormones that influence menstrual cycle characteristics may also influence the risk of vulvodynia.
This possibility may be supported by the fact that many menstrual cycle characteristics that were associated with vulvodynia showed associations across all time periods, including early menstrual years. Additionally, we and others previously reported that women with vulvodynia have higher odds of reporting moderate/severe discomfort with tampon use during their early menstrual years compared with women with no history of vulvar pain,3,20 which is often years before their diagnosis. The fact that almost half of cases in our study reported changes in vulvar pain over the course of their menstrual cycles may also support the idea that for some women, hormones affect vulvodynia symptoms.
It is also possible that menstrual flow influences the risk of vulvodynia independent of endogenous hormone levels, potentially by informing menstrual hygiene practices. We found that women with vulvodynia were more likely to report using only sanitary pads for menstrual protection compared with controls. This was true across all time periods evaluated, including early menstrual years.
Others have speculated that the use of sanitary pads may influence the vaginal microbiome,21 which has recently been studied in relation to vulvodynia.7,22 However, a more likely scenario is that women who develop vulvodynia have pain in their early menstrual years, which precludes them from regular tampon use. It is also possible that heavier menstrual flow irritates vaginal tissue over time. Our findings differ from another study, which reported that women with vulvodynia-like symptoms were not more likely to use sanitary pads only.20 This may be reflective of differences in the samples, or the fact that we separated menstrual cycle characteristics into discrete time periods.
Our study should be interpreted in the context of important limitations. Reports of menstrual characteristics can be subjective (i.e., moderate vs. severe cramping). When possible, we tried to provide quantitative benchmarks to guide women's reporting and to standardize the qualitative responses. There is also the possibility of recall bias. We asked women about early reproductive years, and for some participants, there may have been considerable time between early reproductive years and completion of the survey. Women with vulvodynia may also remember more pain associated with early menstrual experiences, such as tampon use, than women without vulvodynia. Additionally, our sample size was reduced during some time periods assessed as many women ceased to menstruate for various reasons.
This limited the precision of our estimates when assessing menstrual characteristics in the year before the reference age, and in the 3 months before the survey. Finally, although all women with vulvodynia were clinically confirmed, we recognize that women's self-reported age at first onset of vulvar pain may not accurately reflect the true age when vulvar pain began, nor the age at which a diagnosis would have been obtained. A strength of our study was the clinical confirmation of vulvodynia. Additionally, we recruited women using a survey mailed to a large proportion of the population in the twin cities area, meaning that our sample was not restricted to women seeking care for vulvodynia, which may increase generalizability.
Future research may benefit from using assays to evaluate menstrual-timed levels of endogenous hormones to examine whether our observed associations could be driven by hormonal differences underlying differing menstrual characteristics, particularly cycle length and flow. Furthermore, more research into the relationship between menstrual cycle characteristics and vulvar pain, outside the context of vulvodynia specifically, may be warranted. It is possible that the menstrual cycle is also related to vulvar pain that does not meet the clinical threshold of vulvodynia but may nonetheless be disruptive to the lives of those who menstruate. Because menstrual hygiene involves the use of products that come in close contact with vulvar tissue, this is a particularly important connection to pursue.
Conclusions
Our study adds important insights to the literature evaluating the etiology of vulvodynia. A strength is that our study evaluates the association between menstrual characteristics and vulvodynia in a sample of women with and without clinically confirmed vulvodynia. Our findings suggest that associations between menstrual characteristics such as severe pain and heavy menstrual flow can begin during the early reproductive years for women who ultimately go on to develop vulvodynia, which may suggest the relevance of etiologic factors that appear early in life, and influence both menstruation and the risk of vulvodynia. Providers may wish to encourage patients to note changes in vulvar pain when discussing menstruation and invite patients to share updates or concerns as they develop.
Supplementary Material
Acknowledgment
The authors would like to thank Alexis McCullough, MPH, for her assistance with data analysis.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was partially funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant No. NIH-NICHD R01 HD058608). The funder had no role in study design, collection, analysis, or interpretation of data, article writing, nor decision to submit the article for publication.
Supplementary Material
References
- 1. Harlow BL, Kunitz CG, Nguyen RHN, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: Population-based estimates from 2 geographic regions. Am J Obstet Gynecol 2014;210:40..e1–40.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arnold LD, Bachmann GA, Rosen R, Rhoads GG. Assessment of vulvodynia symptoms in a sample of US women: A prevalence survey with a nested case control study. Am J Obstet Gynecol 2007;196:128..e1–128.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: Have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc (1972) 2003;58:82–88. [PubMed] [Google Scholar]
- 4. Brotto LA, Sadownik LA, Thomson S, et al. A comparison of demographic and psychosexual characteristics of women with primary versus secondary provoked vestibulodynia. Clin J Pain 2014;30:428–435. [DOI] [PubMed] [Google Scholar]
- 5. Harlow BL, Cohen LS, Otto MW, Spiegelman D, Cramer DW. Early life menstrual characteristics and pregnancy experiences among women with and without major depression: The Harvard study of moods and cycles. J Affect Disord 2004;79:167–176. [DOI] [PubMed] [Google Scholar]
- 6. Havemann LM, Cool DR, Gagneux P, et al. Vulvodynia: What we know and where we should be going. J Lower Gen Tract Dis 2017;21:1–7. [DOI] [PubMed] [Google Scholar]
- 7. Bedford L, Parker SE, Davis E, et al. Characteristics of the vaginal microbiome in women with and without clinically confirmed vulvodynia. Am J Obstet Gynecol 2020;223:406..e1–406.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berbic M, Fraser IS. Immunology of normal and abnormal menstruation. Womens Health (Lond) 2013;9:387–395. [DOI] [PubMed] [Google Scholar]
- 9. Laux-Biehlmann A, d'Hooghe T, Zollner TM. Menstruation pulls the trigger for inflammation and pain in endometriosis. Trend Pharmacol Sci 2015;36:270–276. [DOI] [PubMed] [Google Scholar]
- 10. Bornstein J, Goldstein AT, Stockdale CK, et al. Consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal Disease (ISSVD); International Society for the Study of Women's Sexual Health (ISSWSH); International Pelvic Pain Society (IPPS). 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet Gynecol 2016;127:745–751. [DOI] [PubMed] [Google Scholar]
- 11. Harlow BL, Caron RE, Parker SE, Chatterjea D, Fox MP, Nguyen RHN. Recurrent yeast infections and vulvodynia: Can we believe associations based on self-reported data? J Womens Health (Larchmt) 2017;26:1069–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moos RH. The development of a menstrual distress questionnaire. Psychosom Med 1968;30:853–867. [DOI] [PubMed] [Google Scholar]
- 13. Bachmann GA, Rosen R, Arnold LD, et al. Chronic vulvar and gynecologic pain: Prevalence and characteristics in a self-reported survey. J Reprod Med 2006;51:3–9. [PMC free article] [PubMed] [Google Scholar]
- 14. Johannesson U, Sahlin L, Masironi B, Rylander E, Bohm-Starke N. Steroid receptor expression in the vulvar vestibular mucosa—effects of oral contraceptives and menstrual cycle. Contraception 2007;76:319–325. [DOI] [PubMed] [Google Scholar]
- 15. Bazin S, Bouchard C, Brisson J, Morin C, Meisels A, Fortier M. Vulvar vestibulitis syndrome: An exploratory case-control study. Obstet Gynecol 1994;83:47–50. [PubMed] [Google Scholar]
- 16. Bouchard C, Brisson J, Fortier M, Morin C, Blanchette C. Use of oral contraceptive pills and vulvar vestibulitis: A case-control study. Am J Epidemiol 2002;156:254–261. [DOI] [PubMed] [Google Scholar]
- 17. Harlow BL, Vitonis AF, Stewart EG. Influence of oral contraceptive use on the risk of adult-onset vulvodynia. J Reprod Med 2008;53:102–110. [PubMed] [Google Scholar]
- 18. Reed BD, Harlow SD, Legocki LH, et al. Oral contraceptive use and risk of vulvodynia: A population-based longitudinal study. BJOG 2013;120:1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Windham GC, Elkin E, Fenster L, et al. Ovarian hormones in premenopausal women: Variation by demographic, reproductive and menstrual cycle characteristics. Epidemiology 2002:675–684. [DOI] [PubMed] [Google Scholar]
- 20. Sutton JT, Bachmann GA, Arnold LD, Rhoads GG, Rosen RC. Assessment of vulvodynia symptoms in a sample of US women: A follow-up national incidence survey. J Womens Health 2008;17:1285–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Noyes N, Cho KC, Ravel J, Forney LJ, Abdo Z. Associations between sexual habits, menstrual hygiene practices, demographics and the vaginal microbiome as revealed by Bayesian network analysis. PLoS One 2018;13:e0191625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Park SY, Lee ES, Lee SR, Kim SH, Chae HD. Vaginal microbiome is associated with vulvodynia, vulvar pain syndrome: A case control study. Sex Med 2021;9:100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.