Abstract
The COVID-19 pandemic continues driving unprecedented disruptions to health care provision, including HIV pre-exposure prophylaxis (PrEP) services. We explored service provider experiences promoting and prescribing PrEP to marginalized populations during the COVID-19 pandemic in Baltimore, Maryland. In February to April 2021, we facilitated four virtual focus group discussions with 20 PrEP providers, representing various professional cadres and practice settings. Employing an iterative, team-based thematic analysis, we identified salient enablers and constraints to PrEP promotion, initiation, and maintenance in the COVID-19 era, along with innovative adaptations to PrEP service delivery. Discussants described attenuated demands for PrEP early in the pandemic, exemplified by high PrEP discontinuation rates. This was attributed to changes in clients' sexual behaviors and shifting priorities, including caregiving responsibilities, during the pandemic. Substantial systems-level disruptions impacting PrEP provision were identified, including outreach service suspension, personnel shortages, and facility restrictions on face-to-face visits. Providers emphasized that these disruptions, though occurring early in the pandemic, had protracted impacts on PrEP accessibility. The transition to telemedicine rendered health care services, including PrEP, more accessible/convenient to some clients and expeditious to providers. However, structural barriers to telehealth engagement (telephone/internet access), coupled with limitations of the virtual care environment (difficulty establishing rapport), impeded efforts to equitably promote and prescribe PrEP. Expanding the PrEP outreach workforce and availing alternatives to telemedicine (e.g., community-based PrEP provision, specimen self-collection) could facilitate PrEP care continuity, especially as COVID-19 transitions from an acute to a protracted health crisis.
Keywords: PrEP, HIV prevention, telehealth, SARS-CoV-2, qualitative research, United States
Introduction
Pre-exposure prophylaxis (PrEP) is a critical biomedical strategy for HIV prevention, but it remains under-prescribed and underutilized by eligible populations in the United States. Approximately 1.1 million US adults exhibit PrEP indications,1 but fewer than 25% of them have been prescribed PrEP.2 Gaps in PrEP prescribing are disproportionately observed in populations with elevated HIV burdens, including people who inject drugs (PWID), Black and Latinx men who have sex with men (MSM), and racial minority women.2–4
The COVID-19 pandemic has further exacerbated pre-existing inequities in PrEP access. The emergence of SARS-CoV-2 in late 2019, catalyzing a global pandemic in 2020, required transformation of existing service delivery models to support care continuity while safeguarding client/patient and provider health and safety. In March 2020, following detection of COVID-19 transmission clusters within the United States, numerous mitigation measures (e.g., shelter-in-place ordinances, business/school closures) were introduced to curb COVID-19 incidence.5 Nationwide, these measures restricted in-person interactions within health care institutions, community-based organizations, and other agencies providing essential services. Service providers adapted by modifying their service delivery approaches (e.g., transitioning to telephone/messaging-based or virtual platforms) or, in some unfortunate cases, suspending operations altogether.6–8
The impact of these service delivery modifications on HIV treatment and prevention outcomes has varied across settings and populations. Some studies have attributed diminished engagement in HIV care [e.g., missed appointments, declines in HIV/sexually transmitted infection (STI) testing] to the COVID-19 pandemic,9–15 while others describe maintenance of—and in some cases improvements to—HIV outcomes (e.g., viral suppression) as in-person clinical services were minimized and transitioned to telehealth platforms or mobile community-based modalities.16–18 Collectively, these findings underscore the pandemic's heterogeneous impact on HIV-related outcomes.
Moreover, studies assessing the COVID-19 pandemic's impact along the PrEP care continuum, from initiation to continuation and adherence, are scant. One observational study found that PrEP-related visits in health care settings increased significantly among cisgender men in three US states after COVID-19 restrictions were introduced.9 Another survey reported decreased PrEP adherence and prescription refill challenges among PWID in Connecticut.19 In one study of MSM in the southern United States, PrEP adherence and access challenges experienced early in the pandemic were complemented by heightened sexual risk-taking, including more frequent condomless sexual encounters.20 Importantly, there is a dearth of studies examining how domestic health systems have responded to shifting client PrEP demands and service provision restrictions in the COVID-19 era.
To characterize COVID-19-precipitated shifts in client PrEP demands, PrEP service delivery interruptions, and health systems transformations impacting PrEP provision, we qualitatively elicited service providers' experiences with prescribing and promoting PrEP among marginalized client/patient populations during the COVID-19 pandemic in Baltimore, Maryland. Our findings identify immediate and long-term systems-level solutions for minimizing disruptions to PrEP service delivery, especially as the COVID-19 pandemic transitioned from an acute emergency to a protracted crisis.
Methods
Procedures
Optimizing PrEP among Women Living in Baltimore City (OPAL) is a multiphase, formative research study guiding conception and implementation of a workforce-development intervention for frontline harm reduction workers to support PrEP awareness-building and uptake among women who inject drugs. The first phase qualitatively characterized the PrEP implementation environment, including the impact of COVID-19 pandemic on PrEP service delivery to various populations, in Baltimore City.
Between February and April 2021, ∼12 months after the emergence of COVID-19 in the United States, we identified and invited adult (≥18 years) service providers from various institutions in Baltimore City with established PrEP programs to join virtual focus group discussions (FGDs). We purposively recruited providers representing a variety of health workforce cadres (e.g., physicians, nurses, case managers, outreach workers) and practice settings (e.g., hospital–outpatient, primary health care centers, community-based organizations) to participate. We also prioritized recruitment of providers from institutions serving lower-income, marginalized populations, including PWID, MSM, people who exchange sex, transgender women, and racial minorities experiencing homelessness.
Providers completed a brief interviewer-administered telephone survey capturing sociodemographic and professional characteristics. A session moderator, aided by an appointed notetaker and logistics coordinator from the study team, facilitated four FGDs via secure video-conferencing platform. Two experienced qualitative researchers and one physician-researcher served as the FGD moderators. We segmented service providers into four discussion groups according to their professional cadre: prescribers (i.e., nurse practitioners, registered nurses, physicians, physician assistants; two FGDs, n = 5 and n = 6); clinical case managers (one FGD, n = 5); and outreach workers (one FGD, n = 4). We developed a semi-structured guide to facilitate FGDs and piloted the final guide with a physician-researcher who served as a mock discussant. Topics discussed during FGDs, lasting 60 to 120 min, included PrEP implementation strategies for various marginalized populations in Baltimore City; barriers and facilitators to PrEP promotion, initiation, and persistence; and the impact of COVID-19 on PrEP demand and service delivery across practice settings. We mailed providers a $50 prepaid gift card for their participation.
Analysis
FGDs were professionally transcribed and quality checked by facilitators for comprehension and fidelity to the recorded discussion. We employed an iterative, team-based thematic analysis approach to identify salient themes and patterns emerging from the transcripts.21 First, we generated a list of key constructs, derived deductively from the semi-structured FGD facilitation guide, to categorize emerging themes into discrete preliminary codes. Next, six study team members read all transcripts twice, line-by-line, and prepared memos summarizing preliminary findings across FGDs.22 We convened multiple times to discuss and compare memos, iteratively revisiting emerging themes to produce a comprehensive set of open (preliminary) codes, each nested within the aforementioned data dimensions. We then consolidated open codes into focused (condensed) codes through subsequent rounds of team discussion.23 We piloted an initial codebook by assigning two study team members to apply codes to text segments across transcripts, documenting sources of agreement and discrepancies in code applications.
After refining the codebook, we uploaded survey responses and FGD transcripts into Dedoose 9.0 (SocioCultural Research Consultants, Manhattan Beach, CA). Two study team members independently coded each transcript, ensuring coded text segments across FGDs were generated by more than one coder. Survey responses and coded text segments were attributed to individual discussants within each FGD, facilitating a mixed intra-group and inter-group thematic analysis, whereby sources of concordance at the group (cadre) level and sources of disagreement between discussants within each group could be identified.24 We then reassembled coded text segments into standalone themes through continuous discussion among study team members, aided by code reports, analytic memos, and session notes.25 We qualitatively ascertained thematic salience by inspecting the presence or absence of specific codes within each FGD.26 Finally, we reorganized and presented salient themes using the following taxonomy: (1) pandemic impact on client PrEP demand and engagement; (2) PrEP service provision and quality during the pandemic; and (3) progress and pitfalls of PrEP service delivery adaptations during the pandemic.
Ethics
The study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board (Baltimore, MD). Participants provided verbal informed consent before completing study procedures.
Results
Table 1 summarizes demographic and professional characteristics of service provider discussants (N = 20) participating in FGDs. Most were younger than 45 years (65%), cisgender women (70%), and non-Hispanic White (60%). Nurse practitioners and registered nurses (35%) were the most represented professional group, followed by clinical case managers (25%), outreach workers (20%), physicians (15%), and physician assistants (5%). Most could prescribe PrEP to patients (75%). Providers reported practice tenures of 11 years on average (range: 1–33 years). Most providers practiced in hospital–outpatient settings (30%) or health department clinics (30%).
Table 1.
Demographic and Professional Characteristics of Individual Service Providers (N = 20) Participating in Virtual Focus Group Discussions
| Characteristics | n | % |
|---|---|---|
| Age group, years | ||
| 18–34 | 7 | 35 |
| 35–44 | 6 | 30 |
| 45–54 | 5 | 25 |
| 55 or older | 2 | 10 |
| Gender | ||
| Cisgender woman | 14 | 70 |
| Cisgender man | 4 | 20 |
| Non-binary | 2 | 10 |
| Race and ethnicity | ||
| Non-Hispanic White | 12 | 60 |
| Non-Hispanic Black | 7 | 35 |
| Non-Hispanic Asian | 1 | 5 |
| Professional cadre | ||
| Registered nurse or nurse practitioner | 7 | 35 |
| Clinical case manager | 5 | 25 |
| Outreach worker | 4 | 20 |
| Physician | 3 | 15 |
| Physician assistant | 1 | 5 |
| Prescribing capacity | ||
| Prescriber | 15 | 75 |
| Non-prescriber | 5 | 25 |
| Professional tenure, in years, mean, range | 11 | 1–33 |
| Practice setting | ||
| Hospital–outpatient | 6 | 30 |
| Health department | 6 | 30 |
| Primary health care center | 4 | 20 |
| Community-based organization | 4 | 20 |
The COVID-19 pandemic's impact on client PrEP demand and engagement
Providers universally described reduced demands for PrEP across client populations within the first year of the COVID-19 pandemic, which were evidenced by high rates of PrEP discontinuation and losses to follow-up among existing PrEP patients. PrEP discontinuation was perceived to be driven by two competing, although complementary, factors: (1) changes in patients' sexual behaviors and (2) shifting priorities and survival needs during the pandemic. Providers explained that COVID-19 mitigation measures implemented early in the pandemic (i.e., shelter-in-place ordinances, physical distancing measures) may have reduced casual sexual encounters among PrEP users, which attenuated perceived HIV risk and, subsequently, demand for PrEP.
The hesitance that I'm seeing during COVID is, “Does it make sense to stay on PrEP right now? I'm quarantining.I'm not engaging in the same behaviors that I was pre-COVID. I don't feel at risk anymore, and I think I want to come off of it.” (Nurse, Health Department)
Providers also explained that the pandemic amplified pre-existing financial and social stressors (e.g., new caregiving responsibilities, unemployment-related income loss, housing instability due to evictions) in their patient populations, especially among women, which competed with providers' efforts to promote, initiate, or retain clients in PrEP care.
I'm thinking of two patients who were unable to use condoms in their relationships and were accessing PrEP. But because of some shifts in their life due to COVID—having to be home with children, having to navigate homeschooling.They just dropped out of accessing PrEP. (Nurse, Health Department)
Client/patient concerns about accessing health services during the pandemic, largely driven by fears of contracting COVID-19 during health care encounters, further motivated client disengagement with PrEP services.
When the pandemic started in March, I didn't have a single [PrEP] referral.They brought us back into the office in October [2020] to cold call some patients. “No, I'm not interested in PrEP. I'm interested in staying away from COVID.” (Outreach Worker, Primary Healthcare Center)
PrEP service provision and quality during the COVID-19 pandemic
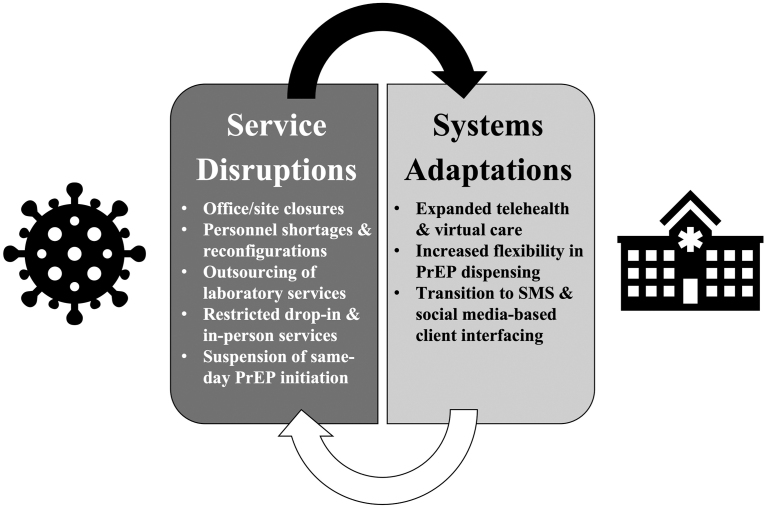
In addition to shifting client demands for PrEP, the COVID-19 pandemic precipitated major health system adaptations, radically transforming PrEP service delivery (Fig. 1). In the first year of the pandemic, providers unanimously reported temporary suspensions and/or modifications to health services, including PrEP promotion and prescription. Prescribers described changes in personnel availability early in the pandemic, including personnel shortages due to COVID-19 infections/exposures and facility restrictions on patient volumes to minimize COVID-19 transmission risk.
FIG. 1.
PrEP service disruptions and health systems adaptations during the COVID-19 pandemic, gleaned from focus groups discussions with service providers. PrEP, pre-exposure prophylaxis.
We had [COVID]-positive staff, and we had staff who had spouses that were [COVID]-positive. We're a small organization.You have people that have to quarantine.We were really short-staffed. (Clinical Case Manager, Community-Based Organization)
Although facility closures and service suspensions were temporary, providers nonetheless acknowledged their protracted impact beyond the first few months of the COVID-19 pandemic. Reductions in patient volume, for instance, resulted in decentralization of specific on-site health services, reducing accessibility to ancillary services that are integral to co-located PrEP service delivery. One prescriber explained how the loss of in-house phlebotomists and outsourcing of laboratory services during the pandemic bottlenecked multiple entry points into the PrEP care continuum, especially for uninsured patients or those without transportation.
We had two lab technicians.and we lost one at the beginning of COVID because our volume wasn't high enough.We would have to refer people out.But with transportation issues, and once people knew they had to go somewhere else, they never made it there. (Clinical Case Manager, Primary Healthcare Center)
Other providers explained how personnel and service restructuring in response to the pandemic limited opportunities for educating and referring clients to PrEP services, effectively de-prioritizing HIV prevention services like PrEP.
Almost everyone from our PrEP program was pulled at least part-time into COVID efforts.[We] are still 100% COVID and 50% PrEP.We're still nowhere close to 100% capacity. (Clinical Case Manager, Health Department)
Non-prescribers emphasized suspension of outreach as a chief constraint to PrEP service continuity. Because outreach activities were a primary vehicle for PrEP promotion, their modification (i.e., shortened client interaction times) or outright suspension restricted opportunities for outreach workers to educate, counsel, and link clients to PrEP services. Many relied solely on virtual platforms or ad hoc mobile services (e.g., supply/medication drop-offs) to interact with clients, which interfered with the rapport-building efforts outreach workers deemed essential to PrEP uptake.
Because we're behind the mask and six feet apart, there's no togetherness or intimacy in the conversations that we need to have to help people understand exactly what PrEP can do for them.You need to be able to sit down together and talk.[but] we can't do that. (Outreach Worker, Community-Based Organization)
Providers explained how other pandemic-related service delivery modifications, specifically suspension of same-day/rapid PrEP initiations and walk-in services, disrupted efforts to promote, initiate, and retain clients in PrEP services.
We aren't doing rapid starts because we're doing mostly telehealth.Because the providers are doing a lot of telehealth, they're not interacting with our PrEP nurses, so sometimes PrEP falls off the radar.There's not that direct handoff, so people have been falling through the cracks. (Clinical Case Manager, Health Department)
PrEP service delivery adaptations during the COVID-19 pandemic: progress and pitfalls
Expansion of virtual care platforms was the most frequently cited PrEP service delivery adaptation to the evolving COVD-19 pandemic. Collectively, prescribers acknowledged how the implementation of telehealth services during the pandemic bifurcated their patient populations along an axis of accessibility. For some patients, virtual care platforms rendered services like PrEP more convenient.
There are people who have been utilizing telemedicine well. I was not doing it prior to COVID. There are people who I am able to prescribe PrEP, who I wouldn't have been able to, had it not been for telemedicine. (Nurse, Health Department)
Nonetheless, prescribers articulated the inherent inequities of telehealth-based service delivery models. For marginalized or more transient/unstable patients (e.g., PWID, individuals experiencing homelessness), the technological and resource requirements of telehealth platforms reinforced pre-existing barriers to care.
Telemedicine for some of our populations does not work.Our most vulnerable patients. don't have an address to send medication to.They don't have access to phones or smart devices that would make the video component of a telemedicine encounter that much more helpful. (Physician, Hospital–Outpatient)
Prescribers also shared mixed perspectives on the quality of health services, including PrEP, delivered in the virtual care environment. Some prescribers described more expedient and efficient clinical encounters in the telehealth environment, increasing the number of patients they could serve and, in some cases, increasing the frequency of patient interactions.
I'm able to make more frequent phone calls than I would be able to make visits with people and that has given me a deeper connection with people that I might not have had otherwise, because they just wouldn't have left home to come to their appointment. (Nurse, Hospital–Outpatient)
Others, however, expressed dissatisfaction over the brevity of patient encounters in the telehealth environment and the limitations of telemedicine platforms in supporting provider task-sharing and team-based care. For many prescribers, virtual care platforms could neither recreate the types of clinical encounters patients received in-person nor facilitate timely follow-up for specific health problems. The inability to leverage ancillary support staff (i.e., case managers, PrEP navigators) during telehealth encounters, for example, interfered with prescriber efforts to make PrEP referrals.
Our telehealth workflow is not sophisticated in terms of utilizing other staff. The providers go at it alone.I was utilizing our peer specialist for patients that had difficulties establishing rapport.I struggle to return to this in a telehealth environment. I refer patients to her, but it's not the same as bringing her into a room and having her initiate the visits.When the appointment is about something else, you don't do everything every time. (Physician, Primary Healthcare Center)
In other instances, familiarizing providers and patients with telehealth platforms absorbed the time and resources needed to screen and refer clients to PrEP, further de-prioritizing PrEP in the telemedicine environment.
Pre-pandemic, providers were prescribing and providing PrEP services. But once the pandemic hit, their focus shifted from having those conversations with patients and just trying to get patients acclimated to the telehealth platform.[PrEP] slipped off their radar. (Clinical Case Manager, Primary Healthcare Center)
Outreach workers specifically expressed dissatisfaction with telemedicine's impact on rapport-building with clients, which they deemed necessary to building PrEP awareness and promoting PrEP engagement among their clients.
Our main interactions with clients are via Instagram or our Facebook page or [telephone] calls.which changes how comfortable people feel speaking about certain things. Which changes how much they want to divulge.Which changes how we can serve them. I can't meet someone's needs if they can't communicate them. (Outreach Worker, Community-Based Organization)
To circumvent accessibility issues related to service disruptions and to support the transition to virtual care appointments during the COVID-19 pandemic, some prescribers reported exercising greater flexibility with PrEP dispensing or medication refill protocols. If patients had incomplete laboratory orders or missed follow-up appointments, prescribers refilled prescriptions to prevent gaps in PrEP access.
With COVID, a lot of responsibility has been shifted to the patient, especially for PrEP—having to find labs, schedule things on their own.I'm being more innovative and re-prescribing a refill, even when there might be a lag with lab updates. I'm a little more flexible with PrEP.I find getting consistent labs has been an issue because a lot of the responsibility has fallen on the patient. (Nurse, Health Department)
Unlike telehealth, however, these PrEP dispensing practices were neither universally implemented across practice settings nor consistently practiced among prescribers from the same institution and were instead dependent on individual providers' capacities and discretion.
Discussion
Our qualitative findings demonstrate that the COVID-19 pandemic substantially disrupted PrEP service provision in Baltimore City, requiring innovative and flexible adaptations within the health system to maintain care continuity (Fig. 1). One immediate consequence of COVID-19 was the restructuring of the health workforce and service delivery models, which disrupted PrEP care continuity. Between temporary closures, in-person service provision restrictions, personnel reconfigurations, and staff shortages, prescribers and non-prescribers alike described suboptimal service provision environments for promoting and prescribing PrEP. More specifically, the suspension of walk-in services, same-day/rapid PrEP starts, and community outreach activities early in the COVID-19 pandemic bottlenecked entry points into the PrEP care continuum. While some US-based studies have reported increased client engagement with PrEP services during the COVID-19 pandemic (primarily facilitated by telemedicine),9,27,28 these findings belie the upstream impacts of COVID-19 on health systems' capacities to maintain PrEP implementation for marginalized populations during a pandemic.
Importantly, these temporary service interruptions had protracted impacts on PrEP service delivery beyond initial health systems adaptations to the emergence of COVID-19. For example, personnel commissioned to support public health emergency operations early in the pandemic continued splitting time between PrEP services and COVID-19 efforts (surveillance, care/treatment, vaccinations). Likewise, in-person service restrictions and reduced patient volume resulted in outsourcing of onsite services (i.e., phlebotomists, laboratory), detracting from the co-located nature of PrEP delivery. Comparable service delivery disruptions have been reported internationally, but have been seldom described within the United States.29–32 Our study, therefore, makes an important contribution to the literature by documenting the downstream implications of restructured health systems on PrEP provision during the COVID-19 pandemic.
Pandemic-precipitated transitions to telemedicine elicited mixed reactions from providers in our study. In some cases, telehealth platforms expedited patient encounters and facilitated care continuity. For example, the transition to telehealth services early in the COVID-19 pandemic increased patient appointment attendance at HIV clinics in San Francisco and Chicago, offering patients greater flexibility with respect to how they engage with clinical services.33,34 The success of “TelePrEP” programs and other online PrEP prescribing initiatives in urban and rural US settings underscores the increased accessibility and convenience telehealth platforms can offer patients,9,27,35–37 in addition to circumventing barriers to in-person PrEP service engagement (e.g., stigma, privacy and confidentiality concerns).38
These virtual care platforms, nonetheless, require resources (telephone/internet access), which may preclude marginalized groups from engaging. Providers in our study explained how telehealth platforms were not optimized for rapport-building with clients/patients, and how the rigidity of these platforms posed challenges to offering PrEP services in comparable ways to in-person care. Responsive, multi-modal PrEP service models, such as Montefiore Medical Center's introduction of home-based STI testing and PrEP (re)starts for clients who cannot access telemedicine,39 could minimize these disparities in PrEP access and improve the quality of telehealth services, especially as telemedicine becomes increasingly ubiquitous.
Although our study focused on service-related PrEP disruptions and adaptations in the COVID-19 era, providers also emphasized critical shifts in patient PrEP demand during the pandemic. Consistent with findings from other US studies, providers attributed reductions in new PrEP initiations and high discontinuation rates to shifting client/patient circumstances early in the COVID-19 pandemic, from amplified competing survival priorities (e.g., housing, childcare) to fewer sexual encounters. Reported reductions in sexual activity in a cohort of PrEP-using MSM in the southern United States may have driven PrEP discontinuation in the study population.20 Other studies have linked concerns surrounding COVID-19 risk during health care encounters and reduced appointment availability to heightened PrEP service disengagement early in the COVID-19 pandemic.19,40 To distinguish intentional PrEP discontinuation from unintended attrition, future studies should directly interview clients about their motivations for PrEP (dis)continuation in the COVID-19 era.
A noteworthy strength of our study was our inclusion of both prescribing and non-prescribing PrEP providers, representing the full landscape of PrEP service provision activities, in the context of COVID-19. Nevertheless, our findings should be considered with several limitations in mind. First, given our focus on systems-level interruptions and adaptations to the COVID-19 pandemic, we did not sample PrEP clients/patients for firsthand accounts of the COVID-19 pandemic's impact on their PrEP willingness or persistence. Nonetheless, provider narratives of changes in PrEP demand and service engagement patterns among clients/patients are corroborated by findings from other studies, reinforcing the credibility of our results.41 Second, our study did not prospectively or longitudinally interrogate changes in PrEP service delivery as the COVID-19 pandemic unfolded in real time. Insights gleaned from FGDs, therefore, may be constrained by participant recall. Third, we leveraged FGDs to identify sources of agreement and discordance among service providers but did not use other qualitative data collection methods (i.e., individual interviews), through which other insights might have emerged. Lastly, our inquiry focused exclusively on PrEP service disruptions and adaptations in Baltimore City, and thus, findings may not be transferable to health systems elsewhere in the United States.
Our study contributes to the burgeoning literature on PrEP service delivery interruptions and adaptations following the emergence of COVID-19. Despite the advent and promise of telemedicine, telehealth platforms are neither a panacea for suspension of face-to-face clinical encounters nor an adequate substitute for the client experience of in-person services, especially in settings where PrEP is co-located with other wraparound services. In high-burden settings, COVID-19 adaptations to HIV treatment models—including pharmacy-based medication delivery/provision, multi-month antiretroviral therapy (ART) dispensing, and client-led ART distribution in community settings—offer valuable insights for maintaining service continuity and even expanding access to PrEP services domestically.42–45 Mitigating disruptions to PrEP services while supporting competing client priorities during the COVID-19 pandemic requires innovative service delivery approaches beyond traditional telehealth platforms.
Acknowledgments
We thank all service providers who graciously shared their time and insights while participating in this study. We wish to acknowledge Drs. Susan Sherman, Saba Rouhani, Laura Beres, and Sheree Schwartz for their input into the study's design, including development of data collection instruments.
Authors' Contributions
J.G.R.: Conceptualization (supporting); data curation (equal); formal analysis (lead); investigation (equal); methodology (equal); writing—original draft (lead); writing—review and editing (lead). L.Z.: Conceptualization (supporting); data curation (equal); formal analysis (supporting); investigation (equal); project administration (equal); writing—review and editing (supporting). D.P.: Conceptualization (supporting); investigation (supporting); project administration (equal); writing—review and editing (supporting). J.S.C.: Conceptualization (supporting); funding acquisition (supporting); investigation (equal); writing—review and editing (supporting). C.T.: Formal analysis (supporting); investigation (supporting); writing—review and editing (supporting). L.C.: Formal analysis (supporting); investigation (supporting); writing—review and editing (supporting). P.F.O.: Formal analysis (supporting); writing—review and editing (supporting). T.T.: Formal analysis (supporting); writing—review and editing (supporting). J.L.G.: Supervision (equal); writing—review and editing (supporting). J.N.P.: Conceptualization (lead); funding acquisition (lead); methodology (equal); supervision (equal); writing—review and editing (supporting).
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was supported by the Johns Hopkins University Center for AIDS Research, an NIH-funded program (1P30AI094189). Joseph G. Rosen was supported by a predoctoral training grant from the National Institute of Mental Health (F31MH126796). Jenell S. Coleman was supported by a grant from the National Institute of Child Health and Human Development (R01HD092013). Ju Nyeong Park was supported by a grant from the National Institute of General Medical Sciences (P20GM125507). The content is solely the responsibility of the authors and does not represent the official views of the NIH.
References
- 1. Smith DK, Van Handel M, Grey J. Estimates of adults with indications for HIV pre-exposure prophylaxis by jurisdiction, transmission risk group, and race/ethnicity, United States, 2015. Ann Epidemiol 2018;28:850–857.e9. [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention (CDC). Monitoring Selected National HIV Prevention and Care Objectives by Using Surveillance Data, United States and 6 Dependent Areas, 2019. CDC; 2021:1–158. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-vol-26-no-2.pdf (Last accessed November 30, 2021).
- 3. Song HJ, Squires P, Wilson D, et al. Trends in HIV preexposure prophylaxis prescribing in the United States, 2012–2018. JAMA 2020;324:395–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hojilla JC, Hurley LB, Marcus JL, et al. Characterization of HIV preexposure prophylaxis use behaviors and HIV incidence among US adults in an integrated health care system. JAMA Network Open 2021;4:e2122692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR Morb Mortal Wkly Rep 2020;69:6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beima-Sofie K, Ortblad KF, Swanson F, et al. “Keep It Going if You Can”: HIV service provision for priority populations during the COVID-19 pandemic in Seattle, WA. AIDS Behav 2020;24:2760–2763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brody JK, Rajabiun S, Strupp Allen HJ, Baggett T. Enhanced telehealth case management plus emergency financial assistance for homeless-experienced people living with HIV during the COVID-19 pandemic. Am J Public Health 2021;111:835–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Quirke S, Quinn L, Hegarty D, et al. Virtual HIV pre-exposure prophylaxis outpatient service in the era of COVID-19. Int J STD AIDS 2021;32:100–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hill BJ, Anderson B, Lock L. COVID-19 pandemic, pre-exposure prophylaxis (PrEP) care, and HIV/STI testing among patients receiving care in three HIV epidemic priority states. AIDS Behav 2021;25:1361–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Spinelli MA, Hickey MD, Glidden DV, et al. Viral suppression rates in a safety-net HIV clinic in San Francisco destabilized during COVID-19. AIDS 2020;34:2328–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hochstatter KR, Akhtar WZ, Dietz S, et al. Potential influences of the COVID-19 pandemic on drug use and HIV care among people living with HIV and substance use disorders: Experience from a Pilot mHealth Intervention. AIDS Behav 2021;25:354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Menza TW, Zlot AI, Garai J, et al. The impact of the SARS-CoV-2 pandemic on human immunodeficiency virus and bacterial sexually transmitted infection testing and diagnosis in Oregon. Sex Transm Dis 2021;48:e59–e63. [DOI] [PubMed] [Google Scholar]
- 13. Qiao S, Li Z, Weissman S, et al. Disparity in HIV service interruption in the outbreak of COVID-19 in South Carolina. AIDS Behav 2021;25:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rao A, Rucinski K, Jarrett BA, et al. Perceived interruptions to HIV prevention and treatment services associated with COVID-19 for gay, bisexual, and other men who have sex with men in 20 countries. J Acquir Immune Defic Syndr 2021;87:644–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Restar AJ, Garrison-Desany HM, Adamson T, et al. HIV treatment engagement in the context of COVID-19: An observational global sample of transgender and nonbinary people living with HIV. BMC Public Health 2021;21:901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dorward J, Khubone T, Gate K, et al. The impact of the COVID-19 lockdown on HIV care in 65 South African primary care clinics: An interrupted time series analysis. Lancet HIV 2021;8:e158–e165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. El-Nahal WG, Shen NM, Keruly JC, et al. Telemedicine and visit completion among people with HIV during the COVID-19 pandemic compared to pre-pandemic. AIDS 2022;36:355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hickey MD, Imbert E, Glidden DV, et al. Viral suppression during COVID-19 among people with HIV experiencing homelessness in a low-barrier clinic-based program. AIDS 2021;35:517–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mistler CB, Curley CM, Rosen AO, et al. The impact of COVID-19 on access to HIV prevention services among opioid-dependent individuals. J Community Health 2021;46:960–966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pampati S, Emrick K, Siegler AJ, Jones J. Changes in sexual behavior, PrEP adherence, and access to sexual health services because of the COVID-19 pandemic among a cohort of PrEP-using MSM in the South. J Acquir Immune Defic Syndr 2021;87:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guest G, MacQueen KM. Handbook for Team-Based Qualitative Research. Lanham, MD: Rowman Altamira; 2008. [Google Scholar]
- 22. Richards L. Handling Qualitative Data: A Practical Guide. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 23. Miles MB, Huberman AM, Saldana J.. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA: SAGE Publications; 2013. [Google Scholar]
- 24. Onwuegbuzie AJ, Dickinson WB, Leech NL, Zoran AG. A qualitative framework for collecting and analyzing data in focus group research. Int J Qual Methods 2009;8:1–21. [Google Scholar]
- 25. Yin RK. Qualitative Research from Start to Finish. New York, NY: Guilford Press; 2010. [Google Scholar]
- 26. Sandelowski M. Real qualitative researchers do not count: The use of numbers in qualitative research. Res Nurs Health 2001;24:230–240. [DOI] [PubMed] [Google Scholar]
- 27. Rogers BG, Coats CS, Adams E, et al. Development of telemedicine infrastructure at an LGBTQ+ clinic to support HIV prevention and care in response to COVID-19, Providence, RI. AIDS Behav 2020;24:2743–2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rogers BG, Tao J, Maynard M, et al. Characterizing the impact of COVID-19 on pre-exposure prophylaxis (PrEP) care. AIDS Behav 2021;25:3754–3757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dourado I, Magno L, Soares F, et al. Adapting to the COVID-19 pandemic: Continuing HIV prevention services for adolescents through telemonitoring, Brazil. AIDS Behav 2020;24:1994–1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lagat H, Sharma M, Kariithi E, et al. Impact of the COVID-19 pandemic on HIV testing and assisted partner notification services, Western Kenya. AIDS Behav 2020;24:3010–3013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Odinga MM, Kuria S, Muindi O, et al. HIV testing amid COVID-19: Community efforts to reach men who have sex with men in three Kenyan counties. Gates Open Res 2020;4:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Sun Y, Zhan Y, Li H, et al. Stakeholder efforts to mitigate antiretroviral therapy interruption among people living with HIV during the COVID-19 pandemic in China: A qualitative study. J Int AIDS Soc 2021;24:e25781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Auchus IC, Jaradeh K, Tang A, et al. Transitioning to telehealth during the COVID-19 pandemic: Patient perspectives and attendance at an HIV Clinic in San Francisco. AIDS Patient Care STDS 2021;35:249–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Boshara AI, Patton ME, Hunt BR, et al. Supporting retention in HIV care: Comparing in-person and telehealth visits in a Chicago-Based Infectious Disease Clinic. AIDS Behav 2022. [Epub ahead of print]; DOI: 10.1007/s10461-022-03604-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoth AB, Shafer C, Dillon DB, et al. Iowa TelePrEP: A public-health-partnered telehealth model for human immunodeficiency virus preexposure prophylaxis delivery in a rural state. Sex Transm Dis 2019;46:507–512. [DOI] [PubMed] [Google Scholar]
- 36. Chasco EE, Shafer C, Dillon DMB, et al. Bringing Iowa TelePrEP to scale: A qualitative evaluation. Am J Prev Med 2021;61:S108–S117. [DOI] [PubMed] [Google Scholar]
- 37. Hughes SD, Koester KA, Engesaeth E, et al. Human enough: A qualitative study of client experience with internet-based access to pre-exposure prophylaxis. J Med Internet Res 2021;23:e22650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wille L, Parent MC. Online prescriptions to HIV pre-exposure prophylaxis and pre-exposure prophylaxis uptake. AIDS Patient Care STDS 2020;34:499–501. [DOI] [PubMed] [Google Scholar]
- 39. Patel VV, Beil R, Slawek D, Akiyama MJ. HIV prevention and treatment in the context of the COVID-19 in the Bronx, New York: Implications for practice and research. AIDS Rev 2020;22:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zapata JP, Dang M, Quinn KG, et al. COVID-19-related disruptions to HIV testing and prevention among young sexual minority men 17–24 years old: A qualitative study using synchronous online focus groups, April-September 2020. Arch Sex Behav 2022;51:303–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lincoln YS, Guba EG. But is it rigorous? Trustworthiness and authenticity in naturalistic evaluation. New Dir Prog Eval 1986;1986:73–84. [Google Scholar]
- 42. Boyd AT, Jahun I, Dirlikov E, et al. Expanding access to HIV services during the COVID-19 pandemic-Nigeria, 2020. AIDS Res Ther 2021;18:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mpofu M, Moyo T, Gilbert M, et al. Distribution of antiretroviral therapy through private pharmacies and postal courier services during COVID-19 in Botswana: Acceptability and reach of two out-of-facility individual differentiated service delivery models. J Int AIDS Soc 2021;24(Suppl 6):e25814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Matambanadzo P, Busza J, Mafaune H, et al. “It went through the roof”: An observation study exploring the rise in PrEP uptake among Zimbabwean female sex workers in response to adaptations during Covid-19. J Int AIDS Soc 2021;24(Suppl 6):e25813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pollard R, Gopinath U, Reddy YA, et al. HIV service delivery in the time of COVID-19: Focus group discussions with key populations in India. J Int AIDS Soc 2021;24(Suppl 6):e25800. [DOI] [PMC free article] [PubMed] [Google Scholar]